User login
Understanding Hospital Readmissions
Hospital readmissions pose a major problem both to the patient and the fiscal stability of our health care system.1 Many interventions have attempted to tackle this problem. Interventions exist that utilize transition coaches working intensively with hospitalized patients or nurses performing postdischarge home visits or phoning patients.2, 3 Although beneficial, these strategies are costly and require additional, highly trained personnel. Consequently, they have been difficult to sustain financially in a fee‐for‐service environment, and difficult to generalize at other locales. Recent policies to decrease hospital payments for readmissions will incentivize hospitals to implement discharge programs.4 However, all hospital systems will still want to do this in the most efficient manner possible.
One important way to maximize benefits and minimize costs is to target the most intensive, expensive interventions to the highest risk patients who are most likely to be rehospitalized. By targeting the highest risk patients, we could significantly reduce costs. However, models predicting rehospitalization have had limited accuracy, even for condition‐specific models such as heart failure. Two studies in this issue work to better identify high‐risk patients. Mudge and colleagues5 prospectively examined risk factors for recurrent readmissions in an Australian hospital and found that chronic disease, depression, and underweight were independent risk factors for repeat readmission. Allaudeen6 examined risk factors for readmission to their own institution among general medicine patients. In a retrospective analysis of administrative data, they found that several variables predicted hospital readmission, including black race, insurance coverage through Medicaid, prescription of steroids or narcotics, and diagnoses of heart failure, renal disease, cancer, anemia, and weight loss.
These studies raise two questions that are critical if we are to develop better predictive modeling of who will benefit most from intensive interventions to reduce readmissions. First, what are the risk factors for preventable hospitalizations? People with multiple readmissions seem an obvious target on which to focus. However, it may be that these individuals are just very sick with multiple comorbidities, and many of their readmissions may not be preventable. Rich and colleagues reported that a multidisciplinary discharge intervention reduced readmissions for heart failure by 56%.7 What is often forgotten is that in their pilot study they were not able to reduce admissions for the most severely ill, and their final study population excluded the sickest patients. By targeting moderate‐risk patients, they were able to reduce readmissions significantly.8 In the studies by Mudge et al.5 and Allaudeen,6 the fact that chronic diseases predicted rehospitalization is only moderately helpful. It is possible, perhaps likely, that many of the readmissions for heart failure were preventable while many of the readmissions for cancer were not. The challenge for researchers is to develop methods for classifying admissions/readmissions as preventable.9 Using a defined set of diagnostic categories to classify readmissions (eg, ambulatory care sensitive conditions) may misclassify many cases.10 Determining preventable hospitalizations through detailed chart review is expensive and may have limited interobserver reliability. Nevertheless, physician review and classification may be necessary for future research to advance the field.
Second, what predictor variables are causally related to preventable hospitalizations (and presumably actionable), and which are merely markers of true causal factors and therefore harder to interpret and more difficult to act upon? In addition to chronic disease, Mudge et al.5 found that depression and low body mass index were independent risk factors for readmission. These conditions often go hand in hand. Patients who are burdened with chronic disease may be depressed and not eat. Conversely, patients who are depressed may not eat and allow their chronic disease to worsen. But it seems that depression is the more likely of the two to be causal. Depression is an important predictor of medication nonadherence and worsening illness.11, 12 Screening hospitalized patients for depression could provide valuable information on which patients may need treatment or more rigorous postdischarge follow‐up. In contrast, being underweight may not truly cause readmissions, but could be a marker of frailty and difficulty in meeting activities of daily living.
Similarly, Allaudeen6 found that black race, Medicaid use, steroid use, and narcotic use were independently associated with hospital readmission (in addition to chronic diseases and weight loss). Can being on steroids or narcotics cause readmissions? Does enrollment in Medicaid or being of black race cause one to be readmitted? While these may be markers which are statistically significant, they are unlikely to be true causes of rehospitalization. It is more likely that these variables are markers for true causal factors, such as financial barriers to medications or access barriers to primary care. Many other studies have used administrative databases to examine variables linked to readmission. We need to drill deeper to determine what is actually causing readmissions. Did the patient misinterpret how to take their steroid taper or were they so sick that they needed to return to the hospital? Perhaps they decided to wait on taking the steroids until they spoke with their primary care physician. This deeper level of understanding cannot be ascertained through third party administrative data sets. Primary data collection is needed to correctly determine who to target and the specific foci of interventions.
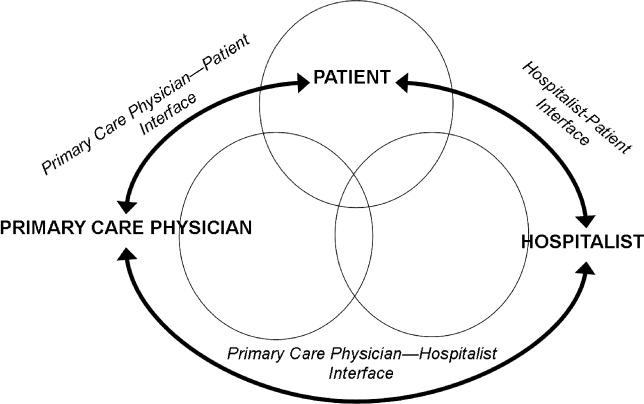
Future research on risk factors for readmissions (and interventions to decrease readmissions) should begin with a theoretical framework that addresses the patient, the hospital, and the receiving outpatient primary care physician or specialist, and the interfaces between each pair that could lead to preventable readmissions (see Figure 1).
With every potential variable affecting readmission, we need to systematically evaluate whether they are causal and preventable. When a variable is both causal and modifiable, we can then develop interventions to target these variables. We designed Table 1 as a framework to consider when moving forward in creating and implementing interventions.
| Factor | Potential Intervention |
|---|---|
| |
| Patient | |
| Cognition | Screening for cognition at discharge. Increase support at home. Inclusion of surrogate or caregiver in explaining discharge instructions. Additional use of a surrogate in explaining discharge instructions. |
| Depression | Screening for depression during the hospitalization and at discharge. Treatment of depression. Increased outpatient support to monitor depression. |
| Health literacy | Screening for health literacy. Involvement of hospital staff, social support network, and outpatient primary care physician to reinforce discharge instructions. |
| Support at home | Assess home support for patient. Increase phone call and home aid support following discharge for those with inadequate support. |
| Functional ability | Assess physical function throughout hospitalization and at discharge. Involve physical therapy early in the hospitalization and postdischarge. |
| Financial assets | Assess ability to pay for medications and transportation to follow‐up appointments. Work with social work on improving access. |
| Chronic disease (ie, congestive heart failure) | Improve patient education of disease and medications. Increase home support to monitor health status. Increase frequency of outpatient visits as needed. |
| Primary care physician | |
| PatientPCP interface | Via phone call to patient at discharge, reinforce so the patient understands disease process (eg, heart failure exacerbation triggers), will take medications started during hospitalization, and recognizes early precipitants of hospitalization. |
| PCPHospitalist interface | Encourage adequate communication about past medical problems and individualized issues pertinent to care plans. |
| Quality of outpatient primary care | Adhere to guidelines of care recommended by advisory standards. Ensure patients receive optimal outpatient care. |
| Medication reconciliation | Ensure that admission and discharge medication reconciliation is perfect. Update outpatient medication list with inpatient medication changes. |
| Follow‐up of pending tests | Create trigger system of pending tests for recently discharged patients. |
| Access to rapid follow‐up appointments | Incentivize physicians of recently discharged patients to offer follow‐up appointments in 1 week or less. |
| Hospitalist | |
| PatientHospitalist interface | Improve communication with patient on how to access physicians if residual postdischarge questions. |
| HospitalistPCP interface | Encourage adequate communication of hospital course and postdischarge plan. |
| Quality of inpatient hospital care | Ensure patients receive optimal inpatient care. Assess patient clinical stability and determine optimal time for discharge. |
| Written discharge instructions | Create easily understandable discharge instructions. Install checks to limit human errors. Ensure patient has copy on discharge. |
| Verbal discharge instructions | Learn to use teach‐back methodology to assess patient understanding of discharge instructions. Work to eliminate multiple sources (eg, consulting physicians, nurses, therapists) giving conflicting verbal discharge information. |
| Medication reconciliation | Utilize outpatient physician notes and pharmacy records to corroborate patient lists. Ensure that admission and discharge medication reconciliation is perfect. |
| Pending tests | Ensure discharge summary includes information and is communicated to PCP for follow‐up in timely manner. |
| Home services | Arrange for home support and nursing services to assist with patients needs postdischarge. Assess whether the patient knows of pending home services and means of contacting services if they do not occur. |
To advance this area, we need to be stringent about how we perform research and interpret findings. Studies that examine risk factors for readmission to a single hospital may be biased; for example, in the study by Allaudeen,6 it is possible that patients with Medicaid may have been equally likely to be readmitted to any hospital but more likely to be readmitted to the hospital that was the sole source of admission data. Even if findings from a single site are valid, they may not be generalizable. Ideally, studies of risk factors (and interventions to reduce readmissions) should be conducted in multiple sites that can track all hospitalizations and examine differences in risk factors for rehospitalization across hospitals. We have learned a tremendous amount over the last few years about risk markers for all‐cause readmission, and interventions to improve safety and quality of transitions in care. To advance further, multicenter studies are needed that focus on plausible causal variables of preventable readmissions and risk factors beyond the walls of the hospital (eg, access and quality of outpatient care for newly discharged patients). Only then will we better understand which patients can have their readmissions prevented and how to improve upon current strategies to improve outcomes.
- ,,. Nationwide Frequency and Costs of Potentially Preventable Hospitalizations,2006. April 2009. Available at: http://www.hcup‐us.ahrq.gov/reports/statbriefs/sb72.jsp. Accessed December 8, 2010.
- ,,,,,.Preparing patients and caregivers to participate in care delivered across settings: the care transitions intervention.J Am Geriatr Soc.2004;52(11):1817–1825.
- ,,, et al.A reengineered hospital discharge program to decrease rehospitalization: a randomized trial.Ann Int Med.2009;150(3):178–187.
- Sec. 3025.Hospital readmissions reduction program. The Patient Protection and Affordable Care Act. HR 3590. Acts of Congress, 111th second session. January 5,2010.
- ,,,,,,.Recurrent readmissions in medical patients: a prospective study.J Hosp Med.2011;6 (this issue).
- ,,,.Redefining identifiable readmission risk factors for general medicine patients.J Hosp Med.2011;6 (this issue).
- ,,,,,.A multidisciplinary intervention to prevent the readmission of elderly patients with congestive heart failure.N Engl J Med.1995;333(18):1190–1195.
- ,,, et al.Prevention of readmission in elderly patients with congestive heart failure: results of a prospective, randomized pilot study.J Gen Intern Med.1993;8(11):585–590.
- ,,,,,.Hospital readmissions and quality of care.Med Care.1999;37(5):490–501.
- ,,,.Ambulatory care sensitive conditions: terminology and disease coding need to be more specific to aid policy makers and clinicians.Public Health.2009;123(2):169–173.
- ,,,,.Depression is an important contributor to low medication adherence in hemodialyzed patients and transplant recipients.Kidney Int.2009;75(11):1223–1229.
- ,,, et al.Depression, medication adherence, and service utilization in systemic lupus erythematosus.Arthritis Rheum.2009;61(2):240–246.
Hospital readmissions pose a major problem both to the patient and the fiscal stability of our health care system.1 Many interventions have attempted to tackle this problem. Interventions exist that utilize transition coaches working intensively with hospitalized patients or nurses performing postdischarge home visits or phoning patients.2, 3 Although beneficial, these strategies are costly and require additional, highly trained personnel. Consequently, they have been difficult to sustain financially in a fee‐for‐service environment, and difficult to generalize at other locales. Recent policies to decrease hospital payments for readmissions will incentivize hospitals to implement discharge programs.4 However, all hospital systems will still want to do this in the most efficient manner possible.
One important way to maximize benefits and minimize costs is to target the most intensive, expensive interventions to the highest risk patients who are most likely to be rehospitalized. By targeting the highest risk patients, we could significantly reduce costs. However, models predicting rehospitalization have had limited accuracy, even for condition‐specific models such as heart failure. Two studies in this issue work to better identify high‐risk patients. Mudge and colleagues5 prospectively examined risk factors for recurrent readmissions in an Australian hospital and found that chronic disease, depression, and underweight were independent risk factors for repeat readmission. Allaudeen6 examined risk factors for readmission to their own institution among general medicine patients. In a retrospective analysis of administrative data, they found that several variables predicted hospital readmission, including black race, insurance coverage through Medicaid, prescription of steroids or narcotics, and diagnoses of heart failure, renal disease, cancer, anemia, and weight loss.
These studies raise two questions that are critical if we are to develop better predictive modeling of who will benefit most from intensive interventions to reduce readmissions. First, what are the risk factors for preventable hospitalizations? People with multiple readmissions seem an obvious target on which to focus. However, it may be that these individuals are just very sick with multiple comorbidities, and many of their readmissions may not be preventable. Rich and colleagues reported that a multidisciplinary discharge intervention reduced readmissions for heart failure by 56%.7 What is often forgotten is that in their pilot study they were not able to reduce admissions for the most severely ill, and their final study population excluded the sickest patients. By targeting moderate‐risk patients, they were able to reduce readmissions significantly.8 In the studies by Mudge et al.5 and Allaudeen,6 the fact that chronic diseases predicted rehospitalization is only moderately helpful. It is possible, perhaps likely, that many of the readmissions for heart failure were preventable while many of the readmissions for cancer were not. The challenge for researchers is to develop methods for classifying admissions/readmissions as preventable.9 Using a defined set of diagnostic categories to classify readmissions (eg, ambulatory care sensitive conditions) may misclassify many cases.10 Determining preventable hospitalizations through detailed chart review is expensive and may have limited interobserver reliability. Nevertheless, physician review and classification may be necessary for future research to advance the field.
Second, what predictor variables are causally related to preventable hospitalizations (and presumably actionable), and which are merely markers of true causal factors and therefore harder to interpret and more difficult to act upon? In addition to chronic disease, Mudge et al.5 found that depression and low body mass index were independent risk factors for readmission. These conditions often go hand in hand. Patients who are burdened with chronic disease may be depressed and not eat. Conversely, patients who are depressed may not eat and allow their chronic disease to worsen. But it seems that depression is the more likely of the two to be causal. Depression is an important predictor of medication nonadherence and worsening illness.11, 12 Screening hospitalized patients for depression could provide valuable information on which patients may need treatment or more rigorous postdischarge follow‐up. In contrast, being underweight may not truly cause readmissions, but could be a marker of frailty and difficulty in meeting activities of daily living.
Similarly, Allaudeen6 found that black race, Medicaid use, steroid use, and narcotic use were independently associated with hospital readmission (in addition to chronic diseases and weight loss). Can being on steroids or narcotics cause readmissions? Does enrollment in Medicaid or being of black race cause one to be readmitted? While these may be markers which are statistically significant, they are unlikely to be true causes of rehospitalization. It is more likely that these variables are markers for true causal factors, such as financial barriers to medications or access barriers to primary care. Many other studies have used administrative databases to examine variables linked to readmission. We need to drill deeper to determine what is actually causing readmissions. Did the patient misinterpret how to take their steroid taper or were they so sick that they needed to return to the hospital? Perhaps they decided to wait on taking the steroids until they spoke with their primary care physician. This deeper level of understanding cannot be ascertained through third party administrative data sets. Primary data collection is needed to correctly determine who to target and the specific foci of interventions.
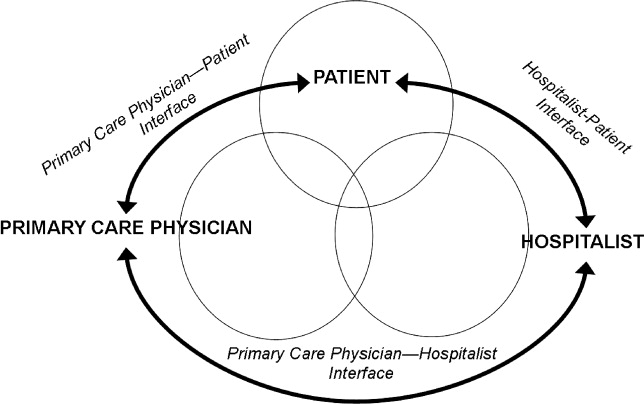
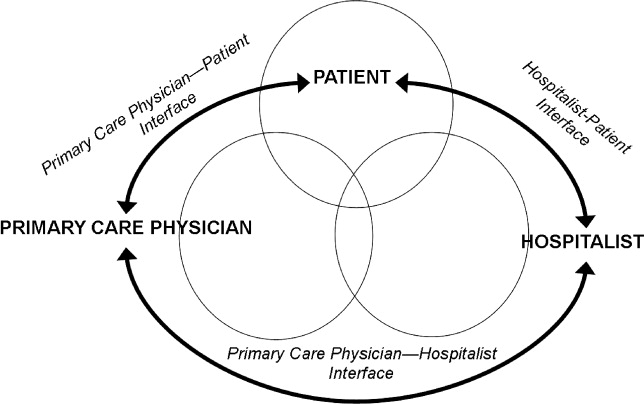
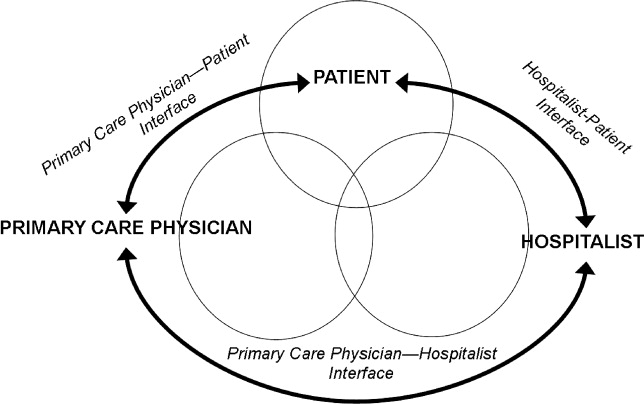
Future research on risk factors for readmissions (and interventions to decrease readmissions) should begin with a theoretical framework that addresses the patient, the hospital, and the receiving outpatient primary care physician or specialist, and the interfaces between each pair that could lead to preventable readmissions (see Figure 1).
With every potential variable affecting readmission, we need to systematically evaluate whether they are causal and preventable. When a variable is both causal and modifiable, we can then develop interventions to target these variables. We designed Table 1 as a framework to consider when moving forward in creating and implementing interventions.
| Factor | Potential Intervention |
|---|---|
| |
| Patient | |
| Cognition | Screening for cognition at discharge. Increase support at home. Inclusion of surrogate or caregiver in explaining discharge instructions. Additional use of a surrogate in explaining discharge instructions. |
| Depression | Screening for depression during the hospitalization and at discharge. Treatment of depression. Increased outpatient support to monitor depression. |
| Health literacy | Screening for health literacy. Involvement of hospital staff, social support network, and outpatient primary care physician to reinforce discharge instructions. |
| Support at home | Assess home support for patient. Increase phone call and home aid support following discharge for those with inadequate support. |
| Functional ability | Assess physical function throughout hospitalization and at discharge. Involve physical therapy early in the hospitalization and postdischarge. |
| Financial assets | Assess ability to pay for medications and transportation to follow‐up appointments. Work with social work on improving access. |
| Chronic disease (ie, congestive heart failure) | Improve patient education of disease and medications. Increase home support to monitor health status. Increase frequency of outpatient visits as needed. |
| Primary care physician | |
| PatientPCP interface | Via phone call to patient at discharge, reinforce so the patient understands disease process (eg, heart failure exacerbation triggers), will take medications started during hospitalization, and recognizes early precipitants of hospitalization. |
| PCPHospitalist interface | Encourage adequate communication about past medical problems and individualized issues pertinent to care plans. |
| Quality of outpatient primary care | Adhere to guidelines of care recommended by advisory standards. Ensure patients receive optimal outpatient care. |
| Medication reconciliation | Ensure that admission and discharge medication reconciliation is perfect. Update outpatient medication list with inpatient medication changes. |
| Follow‐up of pending tests | Create trigger system of pending tests for recently discharged patients. |
| Access to rapid follow‐up appointments | Incentivize physicians of recently discharged patients to offer follow‐up appointments in 1 week or less. |
| Hospitalist | |
| PatientHospitalist interface | Improve communication with patient on how to access physicians if residual postdischarge questions. |
| HospitalistPCP interface | Encourage adequate communication of hospital course and postdischarge plan. |
| Quality of inpatient hospital care | Ensure patients receive optimal inpatient care. Assess patient clinical stability and determine optimal time for discharge. |
| Written discharge instructions | Create easily understandable discharge instructions. Install checks to limit human errors. Ensure patient has copy on discharge. |
| Verbal discharge instructions | Learn to use teach‐back methodology to assess patient understanding of discharge instructions. Work to eliminate multiple sources (eg, consulting physicians, nurses, therapists) giving conflicting verbal discharge information. |
| Medication reconciliation | Utilize outpatient physician notes and pharmacy records to corroborate patient lists. Ensure that admission and discharge medication reconciliation is perfect. |
| Pending tests | Ensure discharge summary includes information and is communicated to PCP for follow‐up in timely manner. |
| Home services | Arrange for home support and nursing services to assist with patients needs postdischarge. Assess whether the patient knows of pending home services and means of contacting services if they do not occur. |
To advance this area, we need to be stringent about how we perform research and interpret findings. Studies that examine risk factors for readmission to a single hospital may be biased; for example, in the study by Allaudeen,6 it is possible that patients with Medicaid may have been equally likely to be readmitted to any hospital but more likely to be readmitted to the hospital that was the sole source of admission data. Even if findings from a single site are valid, they may not be generalizable. Ideally, studies of risk factors (and interventions to reduce readmissions) should be conducted in multiple sites that can track all hospitalizations and examine differences in risk factors for rehospitalization across hospitals. We have learned a tremendous amount over the last few years about risk markers for all‐cause readmission, and interventions to improve safety and quality of transitions in care. To advance further, multicenter studies are needed that focus on plausible causal variables of preventable readmissions and risk factors beyond the walls of the hospital (eg, access and quality of outpatient care for newly discharged patients). Only then will we better understand which patients can have their readmissions prevented and how to improve upon current strategies to improve outcomes.
Hospital readmissions pose a major problem both to the patient and the fiscal stability of our health care system.1 Many interventions have attempted to tackle this problem. Interventions exist that utilize transition coaches working intensively with hospitalized patients or nurses performing postdischarge home visits or phoning patients.2, 3 Although beneficial, these strategies are costly and require additional, highly trained personnel. Consequently, they have been difficult to sustain financially in a fee‐for‐service environment, and difficult to generalize at other locales. Recent policies to decrease hospital payments for readmissions will incentivize hospitals to implement discharge programs.4 However, all hospital systems will still want to do this in the most efficient manner possible.
One important way to maximize benefits and minimize costs is to target the most intensive, expensive interventions to the highest risk patients who are most likely to be rehospitalized. By targeting the highest risk patients, we could significantly reduce costs. However, models predicting rehospitalization have had limited accuracy, even for condition‐specific models such as heart failure. Two studies in this issue work to better identify high‐risk patients. Mudge and colleagues5 prospectively examined risk factors for recurrent readmissions in an Australian hospital and found that chronic disease, depression, and underweight were independent risk factors for repeat readmission. Allaudeen6 examined risk factors for readmission to their own institution among general medicine patients. In a retrospective analysis of administrative data, they found that several variables predicted hospital readmission, including black race, insurance coverage through Medicaid, prescription of steroids or narcotics, and diagnoses of heart failure, renal disease, cancer, anemia, and weight loss.
These studies raise two questions that are critical if we are to develop better predictive modeling of who will benefit most from intensive interventions to reduce readmissions. First, what are the risk factors for preventable hospitalizations? People with multiple readmissions seem an obvious target on which to focus. However, it may be that these individuals are just very sick with multiple comorbidities, and many of their readmissions may not be preventable. Rich and colleagues reported that a multidisciplinary discharge intervention reduced readmissions for heart failure by 56%.7 What is often forgotten is that in their pilot study they were not able to reduce admissions for the most severely ill, and their final study population excluded the sickest patients. By targeting moderate‐risk patients, they were able to reduce readmissions significantly.8 In the studies by Mudge et al.5 and Allaudeen,6 the fact that chronic diseases predicted rehospitalization is only moderately helpful. It is possible, perhaps likely, that many of the readmissions for heart failure were preventable while many of the readmissions for cancer were not. The challenge for researchers is to develop methods for classifying admissions/readmissions as preventable.9 Using a defined set of diagnostic categories to classify readmissions (eg, ambulatory care sensitive conditions) may misclassify many cases.10 Determining preventable hospitalizations through detailed chart review is expensive and may have limited interobserver reliability. Nevertheless, physician review and classification may be necessary for future research to advance the field.
Second, what predictor variables are causally related to preventable hospitalizations (and presumably actionable), and which are merely markers of true causal factors and therefore harder to interpret and more difficult to act upon? In addition to chronic disease, Mudge et al.5 found that depression and low body mass index were independent risk factors for readmission. These conditions often go hand in hand. Patients who are burdened with chronic disease may be depressed and not eat. Conversely, patients who are depressed may not eat and allow their chronic disease to worsen. But it seems that depression is the more likely of the two to be causal. Depression is an important predictor of medication nonadherence and worsening illness.11, 12 Screening hospitalized patients for depression could provide valuable information on which patients may need treatment or more rigorous postdischarge follow‐up. In contrast, being underweight may not truly cause readmissions, but could be a marker of frailty and difficulty in meeting activities of daily living.
Similarly, Allaudeen6 found that black race, Medicaid use, steroid use, and narcotic use were independently associated with hospital readmission (in addition to chronic diseases and weight loss). Can being on steroids or narcotics cause readmissions? Does enrollment in Medicaid or being of black race cause one to be readmitted? While these may be markers which are statistically significant, they are unlikely to be true causes of rehospitalization. It is more likely that these variables are markers for true causal factors, such as financial barriers to medications or access barriers to primary care. Many other studies have used administrative databases to examine variables linked to readmission. We need to drill deeper to determine what is actually causing readmissions. Did the patient misinterpret how to take their steroid taper or were they so sick that they needed to return to the hospital? Perhaps they decided to wait on taking the steroids until they spoke with their primary care physician. This deeper level of understanding cannot be ascertained through third party administrative data sets. Primary data collection is needed to correctly determine who to target and the specific foci of interventions.
Future research on risk factors for readmissions (and interventions to decrease readmissions) should begin with a theoretical framework that addresses the patient, the hospital, and the receiving outpatient primary care physician or specialist, and the interfaces between each pair that could lead to preventable readmissions (see Figure 1).
With every potential variable affecting readmission, we need to systematically evaluate whether they are causal and preventable. When a variable is both causal and modifiable, we can then develop interventions to target these variables. We designed Table 1 as a framework to consider when moving forward in creating and implementing interventions.
| Factor | Potential Intervention |
|---|---|
| |
| Patient | |
| Cognition | Screening for cognition at discharge. Increase support at home. Inclusion of surrogate or caregiver in explaining discharge instructions. Additional use of a surrogate in explaining discharge instructions. |
| Depression | Screening for depression during the hospitalization and at discharge. Treatment of depression. Increased outpatient support to monitor depression. |
| Health literacy | Screening for health literacy. Involvement of hospital staff, social support network, and outpatient primary care physician to reinforce discharge instructions. |
| Support at home | Assess home support for patient. Increase phone call and home aid support following discharge for those with inadequate support. |
| Functional ability | Assess physical function throughout hospitalization and at discharge. Involve physical therapy early in the hospitalization and postdischarge. |
| Financial assets | Assess ability to pay for medications and transportation to follow‐up appointments. Work with social work on improving access. |
| Chronic disease (ie, congestive heart failure) | Improve patient education of disease and medications. Increase home support to monitor health status. Increase frequency of outpatient visits as needed. |
| Primary care physician | |
| PatientPCP interface | Via phone call to patient at discharge, reinforce so the patient understands disease process (eg, heart failure exacerbation triggers), will take medications started during hospitalization, and recognizes early precipitants of hospitalization. |
| PCPHospitalist interface | Encourage adequate communication about past medical problems and individualized issues pertinent to care plans. |
| Quality of outpatient primary care | Adhere to guidelines of care recommended by advisory standards. Ensure patients receive optimal outpatient care. |
| Medication reconciliation | Ensure that admission and discharge medication reconciliation is perfect. Update outpatient medication list with inpatient medication changes. |
| Follow‐up of pending tests | Create trigger system of pending tests for recently discharged patients. |
| Access to rapid follow‐up appointments | Incentivize physicians of recently discharged patients to offer follow‐up appointments in 1 week or less. |
| Hospitalist | |
| PatientHospitalist interface | Improve communication with patient on how to access physicians if residual postdischarge questions. |
| HospitalistPCP interface | Encourage adequate communication of hospital course and postdischarge plan. |
| Quality of inpatient hospital care | Ensure patients receive optimal inpatient care. Assess patient clinical stability and determine optimal time for discharge. |
| Written discharge instructions | Create easily understandable discharge instructions. Install checks to limit human errors. Ensure patient has copy on discharge. |
| Verbal discharge instructions | Learn to use teach‐back methodology to assess patient understanding of discharge instructions. Work to eliminate multiple sources (eg, consulting physicians, nurses, therapists) giving conflicting verbal discharge information. |
| Medication reconciliation | Utilize outpatient physician notes and pharmacy records to corroborate patient lists. Ensure that admission and discharge medication reconciliation is perfect. |
| Pending tests | Ensure discharge summary includes information and is communicated to PCP for follow‐up in timely manner. |
| Home services | Arrange for home support and nursing services to assist with patients needs postdischarge. Assess whether the patient knows of pending home services and means of contacting services if they do not occur. |
To advance this area, we need to be stringent about how we perform research and interpret findings. Studies that examine risk factors for readmission to a single hospital may be biased; for example, in the study by Allaudeen,6 it is possible that patients with Medicaid may have been equally likely to be readmitted to any hospital but more likely to be readmitted to the hospital that was the sole source of admission data. Even if findings from a single site are valid, they may not be generalizable. Ideally, studies of risk factors (and interventions to reduce readmissions) should be conducted in multiple sites that can track all hospitalizations and examine differences in risk factors for rehospitalization across hospitals. We have learned a tremendous amount over the last few years about risk markers for all‐cause readmission, and interventions to improve safety and quality of transitions in care. To advance further, multicenter studies are needed that focus on plausible causal variables of preventable readmissions and risk factors beyond the walls of the hospital (eg, access and quality of outpatient care for newly discharged patients). Only then will we better understand which patients can have their readmissions prevented and how to improve upon current strategies to improve outcomes.
- ,,. Nationwide Frequency and Costs of Potentially Preventable Hospitalizations,2006. April 2009. Available at: http://www.hcup‐us.ahrq.gov/reports/statbriefs/sb72.jsp. Accessed December 8, 2010.
- ,,,,,.Preparing patients and caregivers to participate in care delivered across settings: the care transitions intervention.J Am Geriatr Soc.2004;52(11):1817–1825.
- ,,, et al.A reengineered hospital discharge program to decrease rehospitalization: a randomized trial.Ann Int Med.2009;150(3):178–187.
- Sec. 3025.Hospital readmissions reduction program. The Patient Protection and Affordable Care Act. HR 3590. Acts of Congress, 111th second session. January 5,2010.
- ,,,,,,.Recurrent readmissions in medical patients: a prospective study.J Hosp Med.2011;6 (this issue).
- ,,,.Redefining identifiable readmission risk factors for general medicine patients.J Hosp Med.2011;6 (this issue).
- ,,,,,.A multidisciplinary intervention to prevent the readmission of elderly patients with congestive heart failure.N Engl J Med.1995;333(18):1190–1195.
- ,,, et al.Prevention of readmission in elderly patients with congestive heart failure: results of a prospective, randomized pilot study.J Gen Intern Med.1993;8(11):585–590.
- ,,,,,.Hospital readmissions and quality of care.Med Care.1999;37(5):490–501.
- ,,,.Ambulatory care sensitive conditions: terminology and disease coding need to be more specific to aid policy makers and clinicians.Public Health.2009;123(2):169–173.
- ,,,,.Depression is an important contributor to low medication adherence in hemodialyzed patients and transplant recipients.Kidney Int.2009;75(11):1223–1229.
- ,,, et al.Depression, medication adherence, and service utilization in systemic lupus erythematosus.Arthritis Rheum.2009;61(2):240–246.
- ,,. Nationwide Frequency and Costs of Potentially Preventable Hospitalizations,2006. April 2009. Available at: http://www.hcup‐us.ahrq.gov/reports/statbriefs/sb72.jsp. Accessed December 8, 2010.
- ,,,,,.Preparing patients and caregivers to participate in care delivered across settings: the care transitions intervention.J Am Geriatr Soc.2004;52(11):1817–1825.
- ,,, et al.A reengineered hospital discharge program to decrease rehospitalization: a randomized trial.Ann Int Med.2009;150(3):178–187.
- Sec. 3025.Hospital readmissions reduction program. The Patient Protection and Affordable Care Act. HR 3590. Acts of Congress, 111th second session. January 5,2010.
- ,,,,,,.Recurrent readmissions in medical patients: a prospective study.J Hosp Med.2011;6 (this issue).
- ,,,.Redefining identifiable readmission risk factors for general medicine patients.J Hosp Med.2011;6 (this issue).
- ,,,,,.A multidisciplinary intervention to prevent the readmission of elderly patients with congestive heart failure.N Engl J Med.1995;333(18):1190–1195.
- ,,, et al.Prevention of readmission in elderly patients with congestive heart failure: results of a prospective, randomized pilot study.J Gen Intern Med.1993;8(11):585–590.
- ,,,,,.Hospital readmissions and quality of care.Med Care.1999;37(5):490–501.
- ,,,.Ambulatory care sensitive conditions: terminology and disease coding need to be more specific to aid policy makers and clinicians.Public Health.2009;123(2):169–173.
- ,,,,.Depression is an important contributor to low medication adherence in hemodialyzed patients and transplant recipients.Kidney Int.2009;75(11):1223–1229.
- ,,, et al.Depression, medication adherence, and service utilization in systemic lupus erythematosus.Arthritis Rheum.2009;61(2):240–246.