User login
Patient and physician explanatory models for acute bronchitis
- Patients often do not understand the difference between viral and bacterial infections.
- Patients think that acute bronchitis will not improve and will probably get worse if not treated with antibiotics.
- Physicians and patients tend to falsely equate productive coughs (green-yellow sputum) with having a bacterial infection that requires antibiotic treatment.
- Physicians report significant internal conflict regarding treatment of acute bronchitis, characterized by a recognition that antibiotics are of little value, a universal assumption that patients expect antibiotics, a desire for patient satisfaction, perceived pressure from employers to get the patient “back to work,” and fear of “missing” a more serious infection.
- OBJECTIVES: Our goals were to develop explanatory models to better understand how physicians diagnose and treat acute bronchitis; to describe patient expectations and needs when experiencing an episode of acute bronchitis; and to enhance communication between physician and patient.
- STUDY DESIGN: We used qualitative, semi-structured, in-depth interviews to generate patient and physician explanatory models.
- POPULATION: We had a purposeful, homogeneous sample of 30 family physicians and 30 adult patients.
- OUTCOMES MEASURED: Our multidisciplinary team of investigators used an editing style of analysis to develop patient and physician explanatory models based on the following topics: (1) what caused my illness/etiology, (2) what symptoms I had/onset of symptoms, (3) what my sickness did to me/pathophysiology, (4) how severe is my sickness/course of illness, and (5) what kind of treatment should I receive/treatment.
- RESULTS: We found that patient and physician models were congruous for symptoms of acute bronchitis and incongruous for etiology and course of illness. Models were congruous for treatment, although for different reasons.
- CONCLUSIONS: Patients may have a very vague understanding of the process of infection and the difference between bacteria and viruses. Compounding this confusion is frequent miscommunication from physicians regarding the clinical course of untreated illness. These factors and non-communicated expectations from patients and fear of missing something on the part of physicians contribute to the decision to treat with antibiotics.
Clinical trials and meta-analyses of these trials1-3 have found that antibiotics do not provide clinically relevant improvements in patient outcomes in the treatment of otherwise healthy adults with acute bronchitis. Despite these findings, antibiotics remain the traditional choice of therapy.4-6 To better understand the process of making a diagnosis and deciding to treat, further study is needed to explore the complex interaction between patients and physicians.
Explanatory models of illness, pioneered by Arthur Kleinman, provide insight into the dynamics of physician and patient processes in a clinical encounter.7-10 Physician and patient models are elicited through the use of semi-structured, in-depth interviews. The physician’s model has 5 basic topics: etiology, onset of symptoms, pathophysiology, course of illness, and treatment of illness. A patient will generally consider these same issues in a different framework: What caused my illness?, What symptoms have I had?, What does my sickness do to me?, How severe is my sickness?, and What kind of treatment should I receive? The patient model, which is often drawn from cultural traditions and norms and may not be fully articulated, tends to be less abstract, possibly inconsistent, and even self-contradictory. 8 Differences between patient and physician explanatory models may lead to conflict, poor communication, low compliance, decreased patient satisfaction, and worse patient outcomes.
The purpose of this study was to elicit and analyze explanatory models to better understand how physicians make the diagnosis of acute bronchitis and decide on treatment for a given patient and describe patient expectations and needs when experiencing an episode of acute bronchitis.
Methods
Participants
This qualitative study used a purposeful, homogeneous sample of 30 family physicians and 30 patients from several types of medical practices in the Dallas, Texas area. It was purposeful in that we deliberately tried to include patients and physicians from a variety of settings. The study was approved by the institutional review boards of University of Texas Southwestern Medical Center and Southern Methodist University.
A letter inviting participation was mailed to physicians. This letter also requested access to adult patients who were seen with an episode of acute bronchitis from 4 weeks to 6 months previously. This mailing was followed by a telephone call from a research assistant to set up an interview. A similar process was followed for patients.
In-depth interviews and data collection
Interview scripts had open-ended questions and standard probes to elicit information about the explanatory model. After obtaining informed consent, interviews were conducted by 1 trained interviewer and audio recorded, transcribed, and checked for accuracy.
Data analysis
An editing style of analysis was used in which the text of the interviews was read line by line and data were grouped into themes.11 Two data management software programs were used to develop codes and labeling, Ethnograph version 4.0 (Qualis Research Association, Salt Lake City, UT) and NVivo (Revision 1.2, Qualitative Solutions and Research Pty Ltd, Cambridge, MA). We explored the data for linkages and connections of the coded groups for hierarchical and non-hierarchical relationships.
The data were analyzed and interpreted by a multidisciplinary team consisting of a family physician (K.C.O.), an epidemiologist (L.M.S.), 2 medical anthropologists (R.P.W., C.S.), a medical anthropology graduate student (K.M.C.), and a qualitative research assistant (O.C.). Through a series of meetings, we shared findings, discussed relationships, explored areas of discrepancy and outlying data, and developed the explanatory models.
Results
Participant demographics are provided in the Table. To contrast models, results are presented for the 5 statements with the patient model followed by the physician model.
TABLE 1
Physician and patient demographic data
| Physicians (n = 30) | Patients (n = 30) | |||
|---|---|---|---|---|
| Frequency | % | Frequency | % | |
| Age, y | ||||
| 25–35 | 9 | 30 | 9 | 30 |
| 36–45 | 10 | 33 | 10 | 33 |
| 46–55 | 8 | 27 | 6 | 20 |
| ≥55 | 3 | 10 | 5 | 17 |
| Sex | ||||
| Male | 21 | 70 | 11 | 37 |
| Female | 9 | 30 | 19 | 63 |
| Race/ethnicity | ||||
| European American | 24 | 79 | 24 | 80 |
| ;African American | 2 | 7 | 4 | 13 |
| Hispanic | 2 | 7 | 1 | 4 |
| Asian | 2 | 7 | 1 | 4 |
What caused my illness/etiology
About one third of the patients felt that their bronchitis was triggered by external factors such as allergies, pollution, smoking, or cold weather. As 1 patient stated, “I think that living here, in being exposed to a lot of pollutants over a period of years, has weakened our bronchial areas and therefore, I am more susceptible to the weather changes, the dampness, wind blowing, cold.”
Approximately one third referred to an infectious agent or an infection causing the bronchitis, using words such as bug and germ. Only 2 patients mentioned the words viral or bacterial and the references were nonspecific. One stated, “I assumed a bug of some sort and I am utterly unclear about, you know, what’s a virus, a bacteria, viral versus bacterial infection.” Others talked about how being stressed or tired lowered their resistance and caused the bronchitis. There was another group of patients who felt that they did not know what caused their bronchitis.
Most physicians reported that acute bronchitis is generally viral, but added that it could also be due to Mycoplasma pneumoniae, Chlamydia pneumoniae, Haemophilus influenzae, or Streptococcal pneumoniae and that it was difficult to say what caused an individual’s illness. Environmental exposures, such as smoking, air pollution, and allergies, were also felt to play a role in etiology. This was typified by 1 physician who stated, “I see it most frequently in people who are smokers or passive smokers.” A few physicians expressed the view that the cause of bronchitis was not really understood.
Symptoms I have had/onset of symptoms
Patients tended to report symptoms in order of occurrence. An example was, “My head stopped up and I felt … head congestion, my chest was congested. Sometimes it was hard for me to breathe, and coughing and sneezing and I hurt.”
Patients were asked to rank their symptoms in order of seriousness. Approximately one third reported coughing as their most serious complaint. Another third listed difficulty breathing. Comments about this symptom reflected a strong sense of concern or fear such as, “I had a hard time breathing at night. That was one of the things that was kind of scary … it was something I couldn’t relate to at first and is probably the worst symptom.” When asked if there was 1 symptom that particularly worried them, coughing was the most common response followed by breathing difficulties and then a wide array of symptoms such as fever and chest pain.
When patients described their cough, there tended to be those who used adjectives such as dry, mild, and tickle, and those who used terms such as deep, substernal, barking, goes down below your hips. The cough was commonly described as productive or nonproductive and ongoing or constant. In general, patients fell into 2 camps: those who reported being sick for a short time (1–3 days) and those who waited longer (1–3 weeks) before going to a doctor. Most patients had experienced prior episodes of bronchitis. Those with more experience tended to feel that they needed to see a physician.
All physicians reported cough as the classic symptom of bronchitis. Approximately half indicated that the cough was typically productive and described the color of the phlegm. The others stated that cough was the classic symptom but did not specify the characteristics. Other symptoms listed were fever, shortness of breath, wheezing, congestion, malaise, aches, and chills.
When patients were asked what they felt would be the most worrisome symptom of bronchitis, over two thirds reported coughing, especially when it affected sleep or work functioning and was persistent and productive. When reporting their own most worrisome symptoms, however, physicians listed high fever, chest pain, or purulent sputum and were concerned about serious underlying diseases such as pneumonia.
Physicians felt there was wide variation in the time that patients with bronchitis symptoms waited to be seen. Approximately half of the physicians reported that patients were sick for 1 week or less before their appointment. The other half reported wide intervals ranging from 1 day to 3 weeks.
What my sickness did to me/pathophysiology
Most patients responded that they had never thought about what the illness did to them. When probed, patients generally responded that they had an infection “in the bronchial pipes” or a “cold in the chest.”
Physicians were asked to describe the pathophysiology of acute bronchitis and discuss how they arrive at a diagnosis. In general, they described how a virus or bacteria “invades” the respiratory tract, causing inflammation of the airways and bronchioles, resulting in increased mucus production. Several physicians described bacterial overgrowth occurring. Physicians separated acute bronchitis from an upper respiratory infection based on the cough, especially if it was productive, and from pneumonia by the absence of more severe signs or symptoms, such as high fever, shortness of breath, or presence of rales. Several physicians tied their diagnosis to treatment, as illustrated by a physician who stated, “I think that many doctors use bronchitis as the excuse to give an antibiotic. And I sometimes fall into that trap. So if I want them to think they deserve an antibiotic, then sometimes I will give them the diagnosis of bronchitis.”
How severe is my sickness/course of illness
One third of patients reported feeling very bad and one third felt moderately bad. The remainder reported variability in the way they felt or not feeling ill at all. Similarly, one third reported a cough duration of 3 weeks or longer and one third felt that the illness had a major impact on their work and daily routine. When asked what would have happened if they had not seen the doctor, patients consistently reported that they would have been sick longer, would not have recovered, or would have gotten pneumonia. Three patients felt they could have died. None said that they would have recovered on their own.
Physicians were asked how many days of work were missed by patients with acute bronchitis. More than two thirds estimated that patients missed from 1 to 3 days. A number of physicians mentioned that factors such as work motivation, attitudes about illness, and availability of paid sick leave influenced the number of days off. Most physicians thought it would take patients 1 week or longer before they felt well enough to return to their normal routine.
What kind of treatment should I receive/treatment
All patients recalled that the primary treatment for their acute bronchitis was a prescription medication such as an antibiotic, cough suppressant, or decongestant. Twenty-seven reported receiving an antibiotic prescription. An inhaler was prescribed for about one third of patients. Several patients commented on the inhaler’s effectiveness for relieving symptoms. This is illustrated by a patient who stated, “the inhaler is the thing that helped me instantaneously.” About one third of patients reported receiving medical advice such as drinking lots of liquids and resting.
Most patients agreed that the treatment they received was what they expected, but when asked to articulate what they “expected,” they had problems doing so. After probing by the interviewer, more than 50% stated that an antibiotic was what they needed for treating their illness. This is typified by the response of one patient, “I would like [bronchitis] to be treated more aggressively. … [Physicians] want to wait until you’ve got a full blown infection before they do anything and I wish that would be different next time.”
When patients were asked about treatment satisfaction, about two thirds reported that they were satisfied because they felt better “pretty fast.” There was wide variation in their definition of “pretty fast,” ranging from 1 day to 3 weeks. Several patients were somewhat dissatisfied with their treatment but felt that nothing else could have been done. A few patients expressed strong dissatisfaction because of slow recovery time or because the prescribed medications did not relieve the symptoms.
Two major treatment approaches emerged from the physician interviews: use of antibiotics or a primary focus on symptom relief. Most physicians who commonly used antibiotics were concerned about which antibiotics were more effective. They also were concerned about patients who were sick longer than 1 week, had discolored sputum, were members of high-risk populations (especially smokers), and who did not improve with treatment. A few physicians who focused on symptom relief prescribed cough suppressants, ß-agonist inhalers, or decongestants. These physicians felt it was important to educate patients about differences between viral and bacterial diseases, disadvantages of overusing antibiotics, and ways to relieve symptoms at home instead of relying on prescribed medications.
When asked about expectations of treatment, all 30 physicians thought that their patients wanted them to prescribe antibiotics. About one third reported that patients also expected to have a “prescribed cough medicine.” Three fourths of the physicians perceived patients’ “antibiotic expectations” as a pressure, although with different rationales. Several physicians admitted that they prescribed antibiotics “to make the patient happy.” One said, “I think people expect it. If you get somebody that has come in and has done everything they can figure out to do to try to get better, then you can certainly end up with patients that are unhappy if you refuse to give them antibiotics.” Some physicians suggested that the pressure of prescribing antibiotics was not from the individual, but from the system, including the employer, the legal system, and the health insurance system.
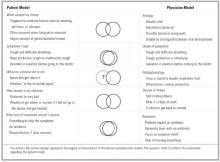
Physicians who did not feel pressure to prescribe antibiotics could be grouped into those who usually used antibiotics to treat acute bronchitis and those who took time to explain to their patients why they did not want to prescribe antibiotics. Some quotations that illustrate the views of this latter group were: “Usually I try to involve the patient in my thinking, until we feel some sort of consensus” and “I basically lay out why I’m not [prescribing an antibiotic].” A synopsis of the models is presented in Figure 1.
FIGURE 1
Discussion
It is well recognized in the literature that antibiotic usage in the therapy of acute bronchitis in the otherwise healthy adult (1) does not confer a clinically relevant shorter course of illness, (2) does not prevent the rare progression to pneumonia any better than placebo, (3) has a significantly negative impact on public health by contributing to antibiotic resistance, and thus (4) is not warranted.1-3,5,12,13 Nevertheless, antibiotic usage patterns have not changed significantly in the past 10 years, and antibiotics are still the traditional first-line therapy in practice. Reasons for this dichotomy are complex. The purpose of this qualitative study was to begin to clarify some of the complexities by determining incongruous areas of patient and physician beliefs regarding the diagnosis and management of acute bronchitis. Similarities and differences in 3 areas of patient and physician models warrant further discussion: etiology of acute bronchitis, course if untreated, and factors affecting the decision to treat.
Patients in this study had a vague understanding of the concept of infection and differences between bacteria and viruses. This finding has been reported in other patient-centered studies13-15 regarding respiratory infections and is likely due to inadequate or contradictory information imparted by the medical community through individual physician-specific communications and from the medical system as a whole. In contrast, physicians in the study uniformly noted a viral cause of most cases of bronchitis but often qualified the statements with concern of not knowing which individuals might have bacterial infections and the lack of tools to distinguish between viral and bacterial etiologies.
Further complicating this paradigm of conflict and confusion regarding viral and bacterial causes, patients consistently thought that not treating acute bronchitis with antibiotics would lead to prolonged, worsening, and potentially life-threatening illness. There is a lack of understanding among patients that acute bronchitis often results in a cough lasting longer than 2 weeks, and this may contribute to the misconception that prolonged duration of illness is evidence of more serious infection.
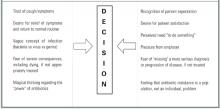
One cannot separate these 2 themes—confusion regarding etiology and miscommunication about the clinical course of untreated illness—from the decision to treat and the role of antibiotics. From the patients’ perspective, without antibiotics they would not get better. Compounding this belief is the patients’ urgent desire for symptom relief. Physicians reported significant internal conflict regarding treatment, characterized by a recognition that antibiotics were of little value, a universal assumption that patients expected antibiotics, a desire for patient satisfaction, perceived pressures from employers, and a fear of “missing” a more serious disease or making a mistake (from the desire to heal and the fear of medicolegal actions). These complex and conflicting perceptions, emotions, and cognitions are illustrated in Figure 2.
Over the past several decades, medical and lay traditions have evolved to imply that productive coughs with green-yellow sputum or colds with green-yellow nasal discharge represent bacterial infections or something that requires an antibiotic.4,5,16,17 Randomized clinical trials have not shown that treatment with antibiotics leads to significantly improved clinical outcomes.1-3,5 In a study of 1398 children, Vinson and Lutz reported that parental expectation of an antibiotic was second only to the presence of rales in increasing the likelihood of the diagnosis of bronchitis.18 With little in history or examination to distinguish between viral and bacterial infections and the fear of “missing something,” the presence or absence of yellow-green nasal secretions and sputum have become the “key” questions in our medical history. This has created a medical tradition that falsely implies to patients a different illness or outcome from those without secretion production or clear discharge. Is it any surprise that patients expect antibiotics?
In evaluating the generalizability of this study, potential biases and limitations of qualitative studies should be considered. First, the creation of this explanatory model was designed to generate ideas and hypotheses, not to test them. Second, the views represented were from a single medical specialty in one geographic area and based on physicians’ and patients’ subjective perceptions. Nevertheless, the goal of such a study was to provide a theoretical model of communication between patient and physician that generates questions for further exploration and areas for potential intervention.
In summary, if, as a medical community, we hope to develop new strategies to decrease unwarranted antibiotic usage, we need to educate patients and health care professionals regarding the causation and natural history of respiratory infections. Gonzales and associates reported impressive results with office-based interventions targeting physicians and patients, and this work needs to be generalized.19,20 However, until there is a major public health emphasis on education at the community level regarding respiratory infections concurrent with an educational effort targeted for health care professionals to dispel the “myth” that characteristics of sputum and nasal discharge are good predictors of clinical outcomes, progress will be slow. To enhance communication between patient and physician, it is important that we elicit and appropriately address patient fears and concerns regarding the natural course of illness with an episode of bronchitis.
FIGURE 2
1. Fahey T, Stocks N, Thomas T. Quantitative systematic review of randomized controlled trials comparing antibiotic with placebo for acute cough in adults. BMJ 1998;316:906-10.
2. Smucny J, Becker L, Glazier R, McIssaac W. Are antibiotics effective treatment for acute bronchitis? J Fam Pract 1998;47:453-60.
3. Bent S, Saint S, Bittinghoff E, Grady D. Antibiotics in acute bronchitis: a meta-analysis. Am J Med 1999;107:62-7.
4. Mainous A, Zoorob R, Hueston W. Current management of acute bronchitis in ambulatory care. Arch Fam Med 1996;5:79-83.
5. Oeffinger K, Snell L, Foster B, Panico K, Archer R. Treatment of acute bronchitis in adults: results of a national survey of family physicians. J Fam Pract 1998;46:469-75.
6. Metlay J, Stafford R, Singer D. National trends in the use of antibiotics by primary care physicians for adult patients with cough. Arch Intern Med 1998;158:1813-8.
7. Kleinman A, Eisenberg L, Good B. Culture, illness, and care. Arch Intern Med 1978;88:258.-
8. Kleinman A. Patients and Healers in the Context of Culture. Berkeley: University of California Press; 1980.
9. Kleinman A. The cultural meanings and social uses of illness. J Fam Pract 1983;16:539-45.
10. Cohen M, Tripp-Reimer T, Smith C, Sorofman B, Lively S. Explanatory models of diabetes; patient practitioner variation. Soc Sci Med 1993;38:59-66.
11. Crabtree B, Miller W. Doing Qualitative Research. 2nd ed. Thousand Oaks, CA: Sage Publications; 1999.
12. King D, Williams W, Bishop L, Schechter A. Effectiveness of eryth-romycin in the treatment of acute bronchitis. J Fam Pract 1996;42:601-5.
13. Butler C, Rollnick S, Kinnersley P, Jones A, Stott N. Reducing antibiotics for respiratory tract symptoms in primary care: consolidating “why” and considering “how.” Br J Gen Pract 1998;48:1865-70.
14. Hamm R, Hicks R, Bemben D. Antibiotics and respiratory infections: are patients more satisfied when expectations are met? J Fam Pract 1996;43:56-62.
15. Bergh K. The patient’s differential diagnosis. Unpredictable concerns in visits for acute cough. J Fam Pract 1998;46:153-8.
16. McKee M, Mills L, Mainous A. Antibiotic use for the treatment of upper respiratory infections in a diverse community. J Fam Pract 1999;48:993-6.
17. Mainous A, Zoorob R, Oler M, Haynes D. Patient knowledge of upper respiratory infections: implications for antibiotic expectations and unnecessary utilization. J Fam Pract 1997;45:75-83.
18. Vinson D, Lutz L. The effect of parental expectations on treatment of children with a cough: a report from ASPN. J Fam Pract 1993;37:23-7.
19. Gonzales R, Steiner J, Lum A, Barrett P. Decreasing antibiotic use in ambulatory practice. JAMA 1999;281:1512-9.
20. Gonzales R, Steiner J, Maselli J, Lum A, Barrett P. Impact of reducing antibiotic prescribing for acute bronchitis on patient satisfaction. Effect Clin Pract 2001;4:105-11.
- Patients often do not understand the difference between viral and bacterial infections.
- Patients think that acute bronchitis will not improve and will probably get worse if not treated with antibiotics.
- Physicians and patients tend to falsely equate productive coughs (green-yellow sputum) with having a bacterial infection that requires antibiotic treatment.
- Physicians report significant internal conflict regarding treatment of acute bronchitis, characterized by a recognition that antibiotics are of little value, a universal assumption that patients expect antibiotics, a desire for patient satisfaction, perceived pressure from employers to get the patient “back to work,” and fear of “missing” a more serious infection.
- OBJECTIVES: Our goals were to develop explanatory models to better understand how physicians diagnose and treat acute bronchitis; to describe patient expectations and needs when experiencing an episode of acute bronchitis; and to enhance communication between physician and patient.
- STUDY DESIGN: We used qualitative, semi-structured, in-depth interviews to generate patient and physician explanatory models.
- POPULATION: We had a purposeful, homogeneous sample of 30 family physicians and 30 adult patients.
- OUTCOMES MEASURED: Our multidisciplinary team of investigators used an editing style of analysis to develop patient and physician explanatory models based on the following topics: (1) what caused my illness/etiology, (2) what symptoms I had/onset of symptoms, (3) what my sickness did to me/pathophysiology, (4) how severe is my sickness/course of illness, and (5) what kind of treatment should I receive/treatment.
- RESULTS: We found that patient and physician models were congruous for symptoms of acute bronchitis and incongruous for etiology and course of illness. Models were congruous for treatment, although for different reasons.
- CONCLUSIONS: Patients may have a very vague understanding of the process of infection and the difference between bacteria and viruses. Compounding this confusion is frequent miscommunication from physicians regarding the clinical course of untreated illness. These factors and non-communicated expectations from patients and fear of missing something on the part of physicians contribute to the decision to treat with antibiotics.
Clinical trials and meta-analyses of these trials1-3 have found that antibiotics do not provide clinically relevant improvements in patient outcomes in the treatment of otherwise healthy adults with acute bronchitis. Despite these findings, antibiotics remain the traditional choice of therapy.4-6 To better understand the process of making a diagnosis and deciding to treat, further study is needed to explore the complex interaction between patients and physicians.
Explanatory models of illness, pioneered by Arthur Kleinman, provide insight into the dynamics of physician and patient processes in a clinical encounter.7-10 Physician and patient models are elicited through the use of semi-structured, in-depth interviews. The physician’s model has 5 basic topics: etiology, onset of symptoms, pathophysiology, course of illness, and treatment of illness. A patient will generally consider these same issues in a different framework: What caused my illness?, What symptoms have I had?, What does my sickness do to me?, How severe is my sickness?, and What kind of treatment should I receive? The patient model, which is often drawn from cultural traditions and norms and may not be fully articulated, tends to be less abstract, possibly inconsistent, and even self-contradictory. 8 Differences between patient and physician explanatory models may lead to conflict, poor communication, low compliance, decreased patient satisfaction, and worse patient outcomes.
The purpose of this study was to elicit and analyze explanatory models to better understand how physicians make the diagnosis of acute bronchitis and decide on treatment for a given patient and describe patient expectations and needs when experiencing an episode of acute bronchitis.
Methods
Participants
This qualitative study used a purposeful, homogeneous sample of 30 family physicians and 30 patients from several types of medical practices in the Dallas, Texas area. It was purposeful in that we deliberately tried to include patients and physicians from a variety of settings. The study was approved by the institutional review boards of University of Texas Southwestern Medical Center and Southern Methodist University.
A letter inviting participation was mailed to physicians. This letter also requested access to adult patients who were seen with an episode of acute bronchitis from 4 weeks to 6 months previously. This mailing was followed by a telephone call from a research assistant to set up an interview. A similar process was followed for patients.
In-depth interviews and data collection
Interview scripts had open-ended questions and standard probes to elicit information about the explanatory model. After obtaining informed consent, interviews were conducted by 1 trained interviewer and audio recorded, transcribed, and checked for accuracy.
Data analysis
An editing style of analysis was used in which the text of the interviews was read line by line and data were grouped into themes.11 Two data management software programs were used to develop codes and labeling, Ethnograph version 4.0 (Qualis Research Association, Salt Lake City, UT) and NVivo (Revision 1.2, Qualitative Solutions and Research Pty Ltd, Cambridge, MA). We explored the data for linkages and connections of the coded groups for hierarchical and non-hierarchical relationships.
The data were analyzed and interpreted by a multidisciplinary team consisting of a family physician (K.C.O.), an epidemiologist (L.M.S.), 2 medical anthropologists (R.P.W., C.S.), a medical anthropology graduate student (K.M.C.), and a qualitative research assistant (O.C.). Through a series of meetings, we shared findings, discussed relationships, explored areas of discrepancy and outlying data, and developed the explanatory models.
Results
Participant demographics are provided in the Table. To contrast models, results are presented for the 5 statements with the patient model followed by the physician model.
TABLE 1
Physician and patient demographic data
| Physicians (n = 30) | Patients (n = 30) | |||
|---|---|---|---|---|
| Frequency | % | Frequency | % | |
| Age, y | ||||
| 25–35 | 9 | 30 | 9 | 30 |
| 36–45 | 10 | 33 | 10 | 33 |
| 46–55 | 8 | 27 | 6 | 20 |
| ≥55 | 3 | 10 | 5 | 17 |
| Sex | ||||
| Male | 21 | 70 | 11 | 37 |
| Female | 9 | 30 | 19 | 63 |
| Race/ethnicity | ||||
| European American | 24 | 79 | 24 | 80 |
| ;African American | 2 | 7 | 4 | 13 |
| Hispanic | 2 | 7 | 1 | 4 |
| Asian | 2 | 7 | 1 | 4 |
What caused my illness/etiology
About one third of the patients felt that their bronchitis was triggered by external factors such as allergies, pollution, smoking, or cold weather. As 1 patient stated, “I think that living here, in being exposed to a lot of pollutants over a period of years, has weakened our bronchial areas and therefore, I am more susceptible to the weather changes, the dampness, wind blowing, cold.”
Approximately one third referred to an infectious agent or an infection causing the bronchitis, using words such as bug and germ. Only 2 patients mentioned the words viral or bacterial and the references were nonspecific. One stated, “I assumed a bug of some sort and I am utterly unclear about, you know, what’s a virus, a bacteria, viral versus bacterial infection.” Others talked about how being stressed or tired lowered their resistance and caused the bronchitis. There was another group of patients who felt that they did not know what caused their bronchitis.
Most physicians reported that acute bronchitis is generally viral, but added that it could also be due to Mycoplasma pneumoniae, Chlamydia pneumoniae, Haemophilus influenzae, or Streptococcal pneumoniae and that it was difficult to say what caused an individual’s illness. Environmental exposures, such as smoking, air pollution, and allergies, were also felt to play a role in etiology. This was typified by 1 physician who stated, “I see it most frequently in people who are smokers or passive smokers.” A few physicians expressed the view that the cause of bronchitis was not really understood.
Symptoms I have had/onset of symptoms
Patients tended to report symptoms in order of occurrence. An example was, “My head stopped up and I felt … head congestion, my chest was congested. Sometimes it was hard for me to breathe, and coughing and sneezing and I hurt.”
Patients were asked to rank their symptoms in order of seriousness. Approximately one third reported coughing as their most serious complaint. Another third listed difficulty breathing. Comments about this symptom reflected a strong sense of concern or fear such as, “I had a hard time breathing at night. That was one of the things that was kind of scary … it was something I couldn’t relate to at first and is probably the worst symptom.” When asked if there was 1 symptom that particularly worried them, coughing was the most common response followed by breathing difficulties and then a wide array of symptoms such as fever and chest pain.
When patients described their cough, there tended to be those who used adjectives such as dry, mild, and tickle, and those who used terms such as deep, substernal, barking, goes down below your hips. The cough was commonly described as productive or nonproductive and ongoing or constant. In general, patients fell into 2 camps: those who reported being sick for a short time (1–3 days) and those who waited longer (1–3 weeks) before going to a doctor. Most patients had experienced prior episodes of bronchitis. Those with more experience tended to feel that they needed to see a physician.
All physicians reported cough as the classic symptom of bronchitis. Approximately half indicated that the cough was typically productive and described the color of the phlegm. The others stated that cough was the classic symptom but did not specify the characteristics. Other symptoms listed were fever, shortness of breath, wheezing, congestion, malaise, aches, and chills.
When patients were asked what they felt would be the most worrisome symptom of bronchitis, over two thirds reported coughing, especially when it affected sleep or work functioning and was persistent and productive. When reporting their own most worrisome symptoms, however, physicians listed high fever, chest pain, or purulent sputum and were concerned about serious underlying diseases such as pneumonia.
Physicians felt there was wide variation in the time that patients with bronchitis symptoms waited to be seen. Approximately half of the physicians reported that patients were sick for 1 week or less before their appointment. The other half reported wide intervals ranging from 1 day to 3 weeks.
What my sickness did to me/pathophysiology
Most patients responded that they had never thought about what the illness did to them. When probed, patients generally responded that they had an infection “in the bronchial pipes” or a “cold in the chest.”
Physicians were asked to describe the pathophysiology of acute bronchitis and discuss how they arrive at a diagnosis. In general, they described how a virus or bacteria “invades” the respiratory tract, causing inflammation of the airways and bronchioles, resulting in increased mucus production. Several physicians described bacterial overgrowth occurring. Physicians separated acute bronchitis from an upper respiratory infection based on the cough, especially if it was productive, and from pneumonia by the absence of more severe signs or symptoms, such as high fever, shortness of breath, or presence of rales. Several physicians tied their diagnosis to treatment, as illustrated by a physician who stated, “I think that many doctors use bronchitis as the excuse to give an antibiotic. And I sometimes fall into that trap. So if I want them to think they deserve an antibiotic, then sometimes I will give them the diagnosis of bronchitis.”
How severe is my sickness/course of illness
One third of patients reported feeling very bad and one third felt moderately bad. The remainder reported variability in the way they felt or not feeling ill at all. Similarly, one third reported a cough duration of 3 weeks or longer and one third felt that the illness had a major impact on their work and daily routine. When asked what would have happened if they had not seen the doctor, patients consistently reported that they would have been sick longer, would not have recovered, or would have gotten pneumonia. Three patients felt they could have died. None said that they would have recovered on their own.
Physicians were asked how many days of work were missed by patients with acute bronchitis. More than two thirds estimated that patients missed from 1 to 3 days. A number of physicians mentioned that factors such as work motivation, attitudes about illness, and availability of paid sick leave influenced the number of days off. Most physicians thought it would take patients 1 week or longer before they felt well enough to return to their normal routine.
What kind of treatment should I receive/treatment
All patients recalled that the primary treatment for their acute bronchitis was a prescription medication such as an antibiotic, cough suppressant, or decongestant. Twenty-seven reported receiving an antibiotic prescription. An inhaler was prescribed for about one third of patients. Several patients commented on the inhaler’s effectiveness for relieving symptoms. This is illustrated by a patient who stated, “the inhaler is the thing that helped me instantaneously.” About one third of patients reported receiving medical advice such as drinking lots of liquids and resting.
Most patients agreed that the treatment they received was what they expected, but when asked to articulate what they “expected,” they had problems doing so. After probing by the interviewer, more than 50% stated that an antibiotic was what they needed for treating their illness. This is typified by the response of one patient, “I would like [bronchitis] to be treated more aggressively. … [Physicians] want to wait until you’ve got a full blown infection before they do anything and I wish that would be different next time.”
When patients were asked about treatment satisfaction, about two thirds reported that they were satisfied because they felt better “pretty fast.” There was wide variation in their definition of “pretty fast,” ranging from 1 day to 3 weeks. Several patients were somewhat dissatisfied with their treatment but felt that nothing else could have been done. A few patients expressed strong dissatisfaction because of slow recovery time or because the prescribed medications did not relieve the symptoms.
Two major treatment approaches emerged from the physician interviews: use of antibiotics or a primary focus on symptom relief. Most physicians who commonly used antibiotics were concerned about which antibiotics were more effective. They also were concerned about patients who were sick longer than 1 week, had discolored sputum, were members of high-risk populations (especially smokers), and who did not improve with treatment. A few physicians who focused on symptom relief prescribed cough suppressants, ß-agonist inhalers, or decongestants. These physicians felt it was important to educate patients about differences between viral and bacterial diseases, disadvantages of overusing antibiotics, and ways to relieve symptoms at home instead of relying on prescribed medications.
When asked about expectations of treatment, all 30 physicians thought that their patients wanted them to prescribe antibiotics. About one third reported that patients also expected to have a “prescribed cough medicine.” Three fourths of the physicians perceived patients’ “antibiotic expectations” as a pressure, although with different rationales. Several physicians admitted that they prescribed antibiotics “to make the patient happy.” One said, “I think people expect it. If you get somebody that has come in and has done everything they can figure out to do to try to get better, then you can certainly end up with patients that are unhappy if you refuse to give them antibiotics.” Some physicians suggested that the pressure of prescribing antibiotics was not from the individual, but from the system, including the employer, the legal system, and the health insurance system.
Physicians who did not feel pressure to prescribe antibiotics could be grouped into those who usually used antibiotics to treat acute bronchitis and those who took time to explain to their patients why they did not want to prescribe antibiotics. Some quotations that illustrate the views of this latter group were: “Usually I try to involve the patient in my thinking, until we feel some sort of consensus” and “I basically lay out why I’m not [prescribing an antibiotic].” A synopsis of the models is presented in Figure 1.
FIGURE 1
Discussion
It is well recognized in the literature that antibiotic usage in the therapy of acute bronchitis in the otherwise healthy adult (1) does not confer a clinically relevant shorter course of illness, (2) does not prevent the rare progression to pneumonia any better than placebo, (3) has a significantly negative impact on public health by contributing to antibiotic resistance, and thus (4) is not warranted.1-3,5,12,13 Nevertheless, antibiotic usage patterns have not changed significantly in the past 10 years, and antibiotics are still the traditional first-line therapy in practice. Reasons for this dichotomy are complex. The purpose of this qualitative study was to begin to clarify some of the complexities by determining incongruous areas of patient and physician beliefs regarding the diagnosis and management of acute bronchitis. Similarities and differences in 3 areas of patient and physician models warrant further discussion: etiology of acute bronchitis, course if untreated, and factors affecting the decision to treat.
Patients in this study had a vague understanding of the concept of infection and differences between bacteria and viruses. This finding has been reported in other patient-centered studies13-15 regarding respiratory infections and is likely due to inadequate or contradictory information imparted by the medical community through individual physician-specific communications and from the medical system as a whole. In contrast, physicians in the study uniformly noted a viral cause of most cases of bronchitis but often qualified the statements with concern of not knowing which individuals might have bacterial infections and the lack of tools to distinguish between viral and bacterial etiologies.
Further complicating this paradigm of conflict and confusion regarding viral and bacterial causes, patients consistently thought that not treating acute bronchitis with antibiotics would lead to prolonged, worsening, and potentially life-threatening illness. There is a lack of understanding among patients that acute bronchitis often results in a cough lasting longer than 2 weeks, and this may contribute to the misconception that prolonged duration of illness is evidence of more serious infection.
One cannot separate these 2 themes—confusion regarding etiology and miscommunication about the clinical course of untreated illness—from the decision to treat and the role of antibiotics. From the patients’ perspective, without antibiotics they would not get better. Compounding this belief is the patients’ urgent desire for symptom relief. Physicians reported significant internal conflict regarding treatment, characterized by a recognition that antibiotics were of little value, a universal assumption that patients expected antibiotics, a desire for patient satisfaction, perceived pressures from employers, and a fear of “missing” a more serious disease or making a mistake (from the desire to heal and the fear of medicolegal actions). These complex and conflicting perceptions, emotions, and cognitions are illustrated in Figure 2.
Over the past several decades, medical and lay traditions have evolved to imply that productive coughs with green-yellow sputum or colds with green-yellow nasal discharge represent bacterial infections or something that requires an antibiotic.4,5,16,17 Randomized clinical trials have not shown that treatment with antibiotics leads to significantly improved clinical outcomes.1-3,5 In a study of 1398 children, Vinson and Lutz reported that parental expectation of an antibiotic was second only to the presence of rales in increasing the likelihood of the diagnosis of bronchitis.18 With little in history or examination to distinguish between viral and bacterial infections and the fear of “missing something,” the presence or absence of yellow-green nasal secretions and sputum have become the “key” questions in our medical history. This has created a medical tradition that falsely implies to patients a different illness or outcome from those without secretion production or clear discharge. Is it any surprise that patients expect antibiotics?
In evaluating the generalizability of this study, potential biases and limitations of qualitative studies should be considered. First, the creation of this explanatory model was designed to generate ideas and hypotheses, not to test them. Second, the views represented were from a single medical specialty in one geographic area and based on physicians’ and patients’ subjective perceptions. Nevertheless, the goal of such a study was to provide a theoretical model of communication between patient and physician that generates questions for further exploration and areas for potential intervention.
In summary, if, as a medical community, we hope to develop new strategies to decrease unwarranted antibiotic usage, we need to educate patients and health care professionals regarding the causation and natural history of respiratory infections. Gonzales and associates reported impressive results with office-based interventions targeting physicians and patients, and this work needs to be generalized.19,20 However, until there is a major public health emphasis on education at the community level regarding respiratory infections concurrent with an educational effort targeted for health care professionals to dispel the “myth” that characteristics of sputum and nasal discharge are good predictors of clinical outcomes, progress will be slow. To enhance communication between patient and physician, it is important that we elicit and appropriately address patient fears and concerns regarding the natural course of illness with an episode of bronchitis.
FIGURE 2
- Patients often do not understand the difference between viral and bacterial infections.
- Patients think that acute bronchitis will not improve and will probably get worse if not treated with antibiotics.
- Physicians and patients tend to falsely equate productive coughs (green-yellow sputum) with having a bacterial infection that requires antibiotic treatment.
- Physicians report significant internal conflict regarding treatment of acute bronchitis, characterized by a recognition that antibiotics are of little value, a universal assumption that patients expect antibiotics, a desire for patient satisfaction, perceived pressure from employers to get the patient “back to work,” and fear of “missing” a more serious infection.
- OBJECTIVES: Our goals were to develop explanatory models to better understand how physicians diagnose and treat acute bronchitis; to describe patient expectations and needs when experiencing an episode of acute bronchitis; and to enhance communication between physician and patient.
- STUDY DESIGN: We used qualitative, semi-structured, in-depth interviews to generate patient and physician explanatory models.
- POPULATION: We had a purposeful, homogeneous sample of 30 family physicians and 30 adult patients.
- OUTCOMES MEASURED: Our multidisciplinary team of investigators used an editing style of analysis to develop patient and physician explanatory models based on the following topics: (1) what caused my illness/etiology, (2) what symptoms I had/onset of symptoms, (3) what my sickness did to me/pathophysiology, (4) how severe is my sickness/course of illness, and (5) what kind of treatment should I receive/treatment.
- RESULTS: We found that patient and physician models were congruous for symptoms of acute bronchitis and incongruous for etiology and course of illness. Models were congruous for treatment, although for different reasons.
- CONCLUSIONS: Patients may have a very vague understanding of the process of infection and the difference between bacteria and viruses. Compounding this confusion is frequent miscommunication from physicians regarding the clinical course of untreated illness. These factors and non-communicated expectations from patients and fear of missing something on the part of physicians contribute to the decision to treat with antibiotics.
Clinical trials and meta-analyses of these trials1-3 have found that antibiotics do not provide clinically relevant improvements in patient outcomes in the treatment of otherwise healthy adults with acute bronchitis. Despite these findings, antibiotics remain the traditional choice of therapy.4-6 To better understand the process of making a diagnosis and deciding to treat, further study is needed to explore the complex interaction between patients and physicians.
Explanatory models of illness, pioneered by Arthur Kleinman, provide insight into the dynamics of physician and patient processes in a clinical encounter.7-10 Physician and patient models are elicited through the use of semi-structured, in-depth interviews. The physician’s model has 5 basic topics: etiology, onset of symptoms, pathophysiology, course of illness, and treatment of illness. A patient will generally consider these same issues in a different framework: What caused my illness?, What symptoms have I had?, What does my sickness do to me?, How severe is my sickness?, and What kind of treatment should I receive? The patient model, which is often drawn from cultural traditions and norms and may not be fully articulated, tends to be less abstract, possibly inconsistent, and even self-contradictory. 8 Differences between patient and physician explanatory models may lead to conflict, poor communication, low compliance, decreased patient satisfaction, and worse patient outcomes.
The purpose of this study was to elicit and analyze explanatory models to better understand how physicians make the diagnosis of acute bronchitis and decide on treatment for a given patient and describe patient expectations and needs when experiencing an episode of acute bronchitis.
Methods
Participants
This qualitative study used a purposeful, homogeneous sample of 30 family physicians and 30 patients from several types of medical practices in the Dallas, Texas area. It was purposeful in that we deliberately tried to include patients and physicians from a variety of settings. The study was approved by the institutional review boards of University of Texas Southwestern Medical Center and Southern Methodist University.
A letter inviting participation was mailed to physicians. This letter also requested access to adult patients who were seen with an episode of acute bronchitis from 4 weeks to 6 months previously. This mailing was followed by a telephone call from a research assistant to set up an interview. A similar process was followed for patients.
In-depth interviews and data collection
Interview scripts had open-ended questions and standard probes to elicit information about the explanatory model. After obtaining informed consent, interviews were conducted by 1 trained interviewer and audio recorded, transcribed, and checked for accuracy.
Data analysis
An editing style of analysis was used in which the text of the interviews was read line by line and data were grouped into themes.11 Two data management software programs were used to develop codes and labeling, Ethnograph version 4.0 (Qualis Research Association, Salt Lake City, UT) and NVivo (Revision 1.2, Qualitative Solutions and Research Pty Ltd, Cambridge, MA). We explored the data for linkages and connections of the coded groups for hierarchical and non-hierarchical relationships.
The data were analyzed and interpreted by a multidisciplinary team consisting of a family physician (K.C.O.), an epidemiologist (L.M.S.), 2 medical anthropologists (R.P.W., C.S.), a medical anthropology graduate student (K.M.C.), and a qualitative research assistant (O.C.). Through a series of meetings, we shared findings, discussed relationships, explored areas of discrepancy and outlying data, and developed the explanatory models.
Results
Participant demographics are provided in the Table. To contrast models, results are presented for the 5 statements with the patient model followed by the physician model.
TABLE 1
Physician and patient demographic data
| Physicians (n = 30) | Patients (n = 30) | |||
|---|---|---|---|---|
| Frequency | % | Frequency | % | |
| Age, y | ||||
| 25–35 | 9 | 30 | 9 | 30 |
| 36–45 | 10 | 33 | 10 | 33 |
| 46–55 | 8 | 27 | 6 | 20 |
| ≥55 | 3 | 10 | 5 | 17 |
| Sex | ||||
| Male | 21 | 70 | 11 | 37 |
| Female | 9 | 30 | 19 | 63 |
| Race/ethnicity | ||||
| European American | 24 | 79 | 24 | 80 |
| ;African American | 2 | 7 | 4 | 13 |
| Hispanic | 2 | 7 | 1 | 4 |
| Asian | 2 | 7 | 1 | 4 |
What caused my illness/etiology
About one third of the patients felt that their bronchitis was triggered by external factors such as allergies, pollution, smoking, or cold weather. As 1 patient stated, “I think that living here, in being exposed to a lot of pollutants over a period of years, has weakened our bronchial areas and therefore, I am more susceptible to the weather changes, the dampness, wind blowing, cold.”
Approximately one third referred to an infectious agent or an infection causing the bronchitis, using words such as bug and germ. Only 2 patients mentioned the words viral or bacterial and the references were nonspecific. One stated, “I assumed a bug of some sort and I am utterly unclear about, you know, what’s a virus, a bacteria, viral versus bacterial infection.” Others talked about how being stressed or tired lowered their resistance and caused the bronchitis. There was another group of patients who felt that they did not know what caused their bronchitis.
Most physicians reported that acute bronchitis is generally viral, but added that it could also be due to Mycoplasma pneumoniae, Chlamydia pneumoniae, Haemophilus influenzae, or Streptococcal pneumoniae and that it was difficult to say what caused an individual’s illness. Environmental exposures, such as smoking, air pollution, and allergies, were also felt to play a role in etiology. This was typified by 1 physician who stated, “I see it most frequently in people who are smokers or passive smokers.” A few physicians expressed the view that the cause of bronchitis was not really understood.
Symptoms I have had/onset of symptoms
Patients tended to report symptoms in order of occurrence. An example was, “My head stopped up and I felt … head congestion, my chest was congested. Sometimes it was hard for me to breathe, and coughing and sneezing and I hurt.”
Patients were asked to rank their symptoms in order of seriousness. Approximately one third reported coughing as their most serious complaint. Another third listed difficulty breathing. Comments about this symptom reflected a strong sense of concern or fear such as, “I had a hard time breathing at night. That was one of the things that was kind of scary … it was something I couldn’t relate to at first and is probably the worst symptom.” When asked if there was 1 symptom that particularly worried them, coughing was the most common response followed by breathing difficulties and then a wide array of symptoms such as fever and chest pain.
When patients described their cough, there tended to be those who used adjectives such as dry, mild, and tickle, and those who used terms such as deep, substernal, barking, goes down below your hips. The cough was commonly described as productive or nonproductive and ongoing or constant. In general, patients fell into 2 camps: those who reported being sick for a short time (1–3 days) and those who waited longer (1–3 weeks) before going to a doctor. Most patients had experienced prior episodes of bronchitis. Those with more experience tended to feel that they needed to see a physician.
All physicians reported cough as the classic symptom of bronchitis. Approximately half indicated that the cough was typically productive and described the color of the phlegm. The others stated that cough was the classic symptom but did not specify the characteristics. Other symptoms listed were fever, shortness of breath, wheezing, congestion, malaise, aches, and chills.
When patients were asked what they felt would be the most worrisome symptom of bronchitis, over two thirds reported coughing, especially when it affected sleep or work functioning and was persistent and productive. When reporting their own most worrisome symptoms, however, physicians listed high fever, chest pain, or purulent sputum and were concerned about serious underlying diseases such as pneumonia.
Physicians felt there was wide variation in the time that patients with bronchitis symptoms waited to be seen. Approximately half of the physicians reported that patients were sick for 1 week or less before their appointment. The other half reported wide intervals ranging from 1 day to 3 weeks.
What my sickness did to me/pathophysiology
Most patients responded that they had never thought about what the illness did to them. When probed, patients generally responded that they had an infection “in the bronchial pipes” or a “cold in the chest.”
Physicians were asked to describe the pathophysiology of acute bronchitis and discuss how they arrive at a diagnosis. In general, they described how a virus or bacteria “invades” the respiratory tract, causing inflammation of the airways and bronchioles, resulting in increased mucus production. Several physicians described bacterial overgrowth occurring. Physicians separated acute bronchitis from an upper respiratory infection based on the cough, especially if it was productive, and from pneumonia by the absence of more severe signs or symptoms, such as high fever, shortness of breath, or presence of rales. Several physicians tied their diagnosis to treatment, as illustrated by a physician who stated, “I think that many doctors use bronchitis as the excuse to give an antibiotic. And I sometimes fall into that trap. So if I want them to think they deserve an antibiotic, then sometimes I will give them the diagnosis of bronchitis.”
How severe is my sickness/course of illness
One third of patients reported feeling very bad and one third felt moderately bad. The remainder reported variability in the way they felt or not feeling ill at all. Similarly, one third reported a cough duration of 3 weeks or longer and one third felt that the illness had a major impact on their work and daily routine. When asked what would have happened if they had not seen the doctor, patients consistently reported that they would have been sick longer, would not have recovered, or would have gotten pneumonia. Three patients felt they could have died. None said that they would have recovered on their own.
Physicians were asked how many days of work were missed by patients with acute bronchitis. More than two thirds estimated that patients missed from 1 to 3 days. A number of physicians mentioned that factors such as work motivation, attitudes about illness, and availability of paid sick leave influenced the number of days off. Most physicians thought it would take patients 1 week or longer before they felt well enough to return to their normal routine.
What kind of treatment should I receive/treatment
All patients recalled that the primary treatment for their acute bronchitis was a prescription medication such as an antibiotic, cough suppressant, or decongestant. Twenty-seven reported receiving an antibiotic prescription. An inhaler was prescribed for about one third of patients. Several patients commented on the inhaler’s effectiveness for relieving symptoms. This is illustrated by a patient who stated, “the inhaler is the thing that helped me instantaneously.” About one third of patients reported receiving medical advice such as drinking lots of liquids and resting.
Most patients agreed that the treatment they received was what they expected, but when asked to articulate what they “expected,” they had problems doing so. After probing by the interviewer, more than 50% stated that an antibiotic was what they needed for treating their illness. This is typified by the response of one patient, “I would like [bronchitis] to be treated more aggressively. … [Physicians] want to wait until you’ve got a full blown infection before they do anything and I wish that would be different next time.”
When patients were asked about treatment satisfaction, about two thirds reported that they were satisfied because they felt better “pretty fast.” There was wide variation in their definition of “pretty fast,” ranging from 1 day to 3 weeks. Several patients were somewhat dissatisfied with their treatment but felt that nothing else could have been done. A few patients expressed strong dissatisfaction because of slow recovery time or because the prescribed medications did not relieve the symptoms.
Two major treatment approaches emerged from the physician interviews: use of antibiotics or a primary focus on symptom relief. Most physicians who commonly used antibiotics were concerned about which antibiotics were more effective. They also were concerned about patients who were sick longer than 1 week, had discolored sputum, were members of high-risk populations (especially smokers), and who did not improve with treatment. A few physicians who focused on symptom relief prescribed cough suppressants, ß-agonist inhalers, or decongestants. These physicians felt it was important to educate patients about differences between viral and bacterial diseases, disadvantages of overusing antibiotics, and ways to relieve symptoms at home instead of relying on prescribed medications.
When asked about expectations of treatment, all 30 physicians thought that their patients wanted them to prescribe antibiotics. About one third reported that patients also expected to have a “prescribed cough medicine.” Three fourths of the physicians perceived patients’ “antibiotic expectations” as a pressure, although with different rationales. Several physicians admitted that they prescribed antibiotics “to make the patient happy.” One said, “I think people expect it. If you get somebody that has come in and has done everything they can figure out to do to try to get better, then you can certainly end up with patients that are unhappy if you refuse to give them antibiotics.” Some physicians suggested that the pressure of prescribing antibiotics was not from the individual, but from the system, including the employer, the legal system, and the health insurance system.
Physicians who did not feel pressure to prescribe antibiotics could be grouped into those who usually used antibiotics to treat acute bronchitis and those who took time to explain to their patients why they did not want to prescribe antibiotics. Some quotations that illustrate the views of this latter group were: “Usually I try to involve the patient in my thinking, until we feel some sort of consensus” and “I basically lay out why I’m not [prescribing an antibiotic].” A synopsis of the models is presented in Figure 1.
FIGURE 1
Discussion
It is well recognized in the literature that antibiotic usage in the therapy of acute bronchitis in the otherwise healthy adult (1) does not confer a clinically relevant shorter course of illness, (2) does not prevent the rare progression to pneumonia any better than placebo, (3) has a significantly negative impact on public health by contributing to antibiotic resistance, and thus (4) is not warranted.1-3,5,12,13 Nevertheless, antibiotic usage patterns have not changed significantly in the past 10 years, and antibiotics are still the traditional first-line therapy in practice. Reasons for this dichotomy are complex. The purpose of this qualitative study was to begin to clarify some of the complexities by determining incongruous areas of patient and physician beliefs regarding the diagnosis and management of acute bronchitis. Similarities and differences in 3 areas of patient and physician models warrant further discussion: etiology of acute bronchitis, course if untreated, and factors affecting the decision to treat.
Patients in this study had a vague understanding of the concept of infection and differences between bacteria and viruses. This finding has been reported in other patient-centered studies13-15 regarding respiratory infections and is likely due to inadequate or contradictory information imparted by the medical community through individual physician-specific communications and from the medical system as a whole. In contrast, physicians in the study uniformly noted a viral cause of most cases of bronchitis but often qualified the statements with concern of not knowing which individuals might have bacterial infections and the lack of tools to distinguish between viral and bacterial etiologies.
Further complicating this paradigm of conflict and confusion regarding viral and bacterial causes, patients consistently thought that not treating acute bronchitis with antibiotics would lead to prolonged, worsening, and potentially life-threatening illness. There is a lack of understanding among patients that acute bronchitis often results in a cough lasting longer than 2 weeks, and this may contribute to the misconception that prolonged duration of illness is evidence of more serious infection.
One cannot separate these 2 themes—confusion regarding etiology and miscommunication about the clinical course of untreated illness—from the decision to treat and the role of antibiotics. From the patients’ perspective, without antibiotics they would not get better. Compounding this belief is the patients’ urgent desire for symptom relief. Physicians reported significant internal conflict regarding treatment, characterized by a recognition that antibiotics were of little value, a universal assumption that patients expected antibiotics, a desire for patient satisfaction, perceived pressures from employers, and a fear of “missing” a more serious disease or making a mistake (from the desire to heal and the fear of medicolegal actions). These complex and conflicting perceptions, emotions, and cognitions are illustrated in Figure 2.
Over the past several decades, medical and lay traditions have evolved to imply that productive coughs with green-yellow sputum or colds with green-yellow nasal discharge represent bacterial infections or something that requires an antibiotic.4,5,16,17 Randomized clinical trials have not shown that treatment with antibiotics leads to significantly improved clinical outcomes.1-3,5 In a study of 1398 children, Vinson and Lutz reported that parental expectation of an antibiotic was second only to the presence of rales in increasing the likelihood of the diagnosis of bronchitis.18 With little in history or examination to distinguish between viral and bacterial infections and the fear of “missing something,” the presence or absence of yellow-green nasal secretions and sputum have become the “key” questions in our medical history. This has created a medical tradition that falsely implies to patients a different illness or outcome from those without secretion production or clear discharge. Is it any surprise that patients expect antibiotics?
In evaluating the generalizability of this study, potential biases and limitations of qualitative studies should be considered. First, the creation of this explanatory model was designed to generate ideas and hypotheses, not to test them. Second, the views represented were from a single medical specialty in one geographic area and based on physicians’ and patients’ subjective perceptions. Nevertheless, the goal of such a study was to provide a theoretical model of communication between patient and physician that generates questions for further exploration and areas for potential intervention.
In summary, if, as a medical community, we hope to develop new strategies to decrease unwarranted antibiotic usage, we need to educate patients and health care professionals regarding the causation and natural history of respiratory infections. Gonzales and associates reported impressive results with office-based interventions targeting physicians and patients, and this work needs to be generalized.19,20 However, until there is a major public health emphasis on education at the community level regarding respiratory infections concurrent with an educational effort targeted for health care professionals to dispel the “myth” that characteristics of sputum and nasal discharge are good predictors of clinical outcomes, progress will be slow. To enhance communication between patient and physician, it is important that we elicit and appropriately address patient fears and concerns regarding the natural course of illness with an episode of bronchitis.
FIGURE 2
1. Fahey T, Stocks N, Thomas T. Quantitative systematic review of randomized controlled trials comparing antibiotic with placebo for acute cough in adults. BMJ 1998;316:906-10.
2. Smucny J, Becker L, Glazier R, McIssaac W. Are antibiotics effective treatment for acute bronchitis? J Fam Pract 1998;47:453-60.
3. Bent S, Saint S, Bittinghoff E, Grady D. Antibiotics in acute bronchitis: a meta-analysis. Am J Med 1999;107:62-7.
4. Mainous A, Zoorob R, Hueston W. Current management of acute bronchitis in ambulatory care. Arch Fam Med 1996;5:79-83.
5. Oeffinger K, Snell L, Foster B, Panico K, Archer R. Treatment of acute bronchitis in adults: results of a national survey of family physicians. J Fam Pract 1998;46:469-75.
6. Metlay J, Stafford R, Singer D. National trends in the use of antibiotics by primary care physicians for adult patients with cough. Arch Intern Med 1998;158:1813-8.
7. Kleinman A, Eisenberg L, Good B. Culture, illness, and care. Arch Intern Med 1978;88:258.-
8. Kleinman A. Patients and Healers in the Context of Culture. Berkeley: University of California Press; 1980.
9. Kleinman A. The cultural meanings and social uses of illness. J Fam Pract 1983;16:539-45.
10. Cohen M, Tripp-Reimer T, Smith C, Sorofman B, Lively S. Explanatory models of diabetes; patient practitioner variation. Soc Sci Med 1993;38:59-66.
11. Crabtree B, Miller W. Doing Qualitative Research. 2nd ed. Thousand Oaks, CA: Sage Publications; 1999.
12. King D, Williams W, Bishop L, Schechter A. Effectiveness of eryth-romycin in the treatment of acute bronchitis. J Fam Pract 1996;42:601-5.
13. Butler C, Rollnick S, Kinnersley P, Jones A, Stott N. Reducing antibiotics for respiratory tract symptoms in primary care: consolidating “why” and considering “how.” Br J Gen Pract 1998;48:1865-70.
14. Hamm R, Hicks R, Bemben D. Antibiotics and respiratory infections: are patients more satisfied when expectations are met? J Fam Pract 1996;43:56-62.
15. Bergh K. The patient’s differential diagnosis. Unpredictable concerns in visits for acute cough. J Fam Pract 1998;46:153-8.
16. McKee M, Mills L, Mainous A. Antibiotic use for the treatment of upper respiratory infections in a diverse community. J Fam Pract 1999;48:993-6.
17. Mainous A, Zoorob R, Oler M, Haynes D. Patient knowledge of upper respiratory infections: implications for antibiotic expectations and unnecessary utilization. J Fam Pract 1997;45:75-83.
18. Vinson D, Lutz L. The effect of parental expectations on treatment of children with a cough: a report from ASPN. J Fam Pract 1993;37:23-7.
19. Gonzales R, Steiner J, Lum A, Barrett P. Decreasing antibiotic use in ambulatory practice. JAMA 1999;281:1512-9.
20. Gonzales R, Steiner J, Maselli J, Lum A, Barrett P. Impact of reducing antibiotic prescribing for acute bronchitis on patient satisfaction. Effect Clin Pract 2001;4:105-11.
1. Fahey T, Stocks N, Thomas T. Quantitative systematic review of randomized controlled trials comparing antibiotic with placebo for acute cough in adults. BMJ 1998;316:906-10.
2. Smucny J, Becker L, Glazier R, McIssaac W. Are antibiotics effective treatment for acute bronchitis? J Fam Pract 1998;47:453-60.
3. Bent S, Saint S, Bittinghoff E, Grady D. Antibiotics in acute bronchitis: a meta-analysis. Am J Med 1999;107:62-7.
4. Mainous A, Zoorob R, Hueston W. Current management of acute bronchitis in ambulatory care. Arch Fam Med 1996;5:79-83.
5. Oeffinger K, Snell L, Foster B, Panico K, Archer R. Treatment of acute bronchitis in adults: results of a national survey of family physicians. J Fam Pract 1998;46:469-75.
6. Metlay J, Stafford R, Singer D. National trends in the use of antibiotics by primary care physicians for adult patients with cough. Arch Intern Med 1998;158:1813-8.
7. Kleinman A, Eisenberg L, Good B. Culture, illness, and care. Arch Intern Med 1978;88:258.-
8. Kleinman A. Patients and Healers in the Context of Culture. Berkeley: University of California Press; 1980.
9. Kleinman A. The cultural meanings and social uses of illness. J Fam Pract 1983;16:539-45.
10. Cohen M, Tripp-Reimer T, Smith C, Sorofman B, Lively S. Explanatory models of diabetes; patient practitioner variation. Soc Sci Med 1993;38:59-66.
11. Crabtree B, Miller W. Doing Qualitative Research. 2nd ed. Thousand Oaks, CA: Sage Publications; 1999.
12. King D, Williams W, Bishop L, Schechter A. Effectiveness of eryth-romycin in the treatment of acute bronchitis. J Fam Pract 1996;42:601-5.
13. Butler C, Rollnick S, Kinnersley P, Jones A, Stott N. Reducing antibiotics for respiratory tract symptoms in primary care: consolidating “why” and considering “how.” Br J Gen Pract 1998;48:1865-70.
14. Hamm R, Hicks R, Bemben D. Antibiotics and respiratory infections: are patients more satisfied when expectations are met? J Fam Pract 1996;43:56-62.
15. Bergh K. The patient’s differential diagnosis. Unpredictable concerns in visits for acute cough. J Fam Pract 1998;46:153-8.
16. McKee M, Mills L, Mainous A. Antibiotic use for the treatment of upper respiratory infections in a diverse community. J Fam Pract 1999;48:993-6.
17. Mainous A, Zoorob R, Oler M, Haynes D. Patient knowledge of upper respiratory infections: implications for antibiotic expectations and unnecessary utilization. J Fam Pract 1997;45:75-83.
18. Vinson D, Lutz L. The effect of parental expectations on treatment of children with a cough: a report from ASPN. J Fam Pract 1993;37:23-7.
19. Gonzales R, Steiner J, Lum A, Barrett P. Decreasing antibiotic use in ambulatory practice. JAMA 1999;281:1512-9.
20. Gonzales R, Steiner J, Maselli J, Lum A, Barrett P. Impact of reducing antibiotic prescribing for acute bronchitis on patient satisfaction. Effect Clin Pract 2001;4:105-11.