User login
How to prevent serotonin syndrome from drug-drug interactions
• Know which drugs are associated with serotonin syndrome.
• Understand the types of drug interactions that may precipitate serotonin syndrome and use drug information resources such as Micromedex, Lexicomp, Physicians’ Desk Reference, AHFS Drug Information, and Facts and Comparisons.
• Know what prescription medications your patient is receiving from other providers as well as any over-the-counter and illicit drugs they may be using.
Ms. B, age 22, is brought to the emergency department (ED) by her roommate for evaluation of confusion. Ms. B has a history of migraines and major depressive disorder and has been taking fluoxetine, 40 mg/d, for 1 year. A week ago, she started amitriptyline, 50 mg/d, when her migraines became more frequent. According to her roommate, Ms. B experienced a migraine early in the morning and had taken 2 doses of sumatriptan, 50 mg. She later complained of nausea and vomiting, and when her roommate returned from work that evening Ms. B was disoriented and her leg muscles would not stop twitching.
In the ED, Ms. B is diaphoretic and increasingly agitated. Blood alcohol and urine drug screens are negative. Blood glucose is 95 mg/dL. Complete blood count, basic metabolic panel, liver function, and kidney function tests are within normal limits. Her physical examination reveals a blood pressure of 130/85 mm Hg, heart rate of 130 beats per minute, respiratory rate of 21 breaths per minute, and body temperature of 38.6°C (101. 4°F). Myoclonus and hyperreflexia affect her lower extremities. Ms. B is admitted with a preliminary diagnosis of serotonin (5-HT) syndrome.
Serotonin syndrome: What is it?
Serotonin syndrome is a rare but potentially serious adverse event resulting from excess serotonergic activity at central and peripheral 5-HT2A and 5-HT1A receptors. Serotonin syndrome toxicity ranges from relatively mild to severe, and may be lethal. Symptoms develop rapidly—within hours—and may include altered mental status, clonus, tremor, hyperthermia, diaphoresis, tachycardia, mydriasis, and akathisia ( Table 1 ).1-3 Fortunately, if recognized promptly and offending agents are discontinued, serotonin syndrome often resolves within a couple of days.
The differential diagnosis includes neuroleptic malignant syndrome (NMS), anticholinergic toxicity, and malignant hyperthermia.1 Differentiating serotonin syndrome from NMS can be difficult. NMS results from dopamine blockade; however, many NMS symptoms are similar to those experienced with serotonin syndrome. Obtaining a history of recent medication and/or illicit drug use, conducting a physical exam, and evaluating the patient’s clinical course help clarify a likely diagnosis. NMS generally has a slower onset—within days—and patients demonstrate neuromuscular rigidity and bradykinesia rather than the neuromuscular hyperreactivity (myoclonus, hyperreflexia) seen with serotonin syndrome.
Table 1
Characteristics of serotonin syndrome*
| Recent addition or dose increase of a serotonergic agent |
| Tremor plus hyperreflexia |
| Muscle rigidity plus fever plus clonus |
| Spontaneous clonus |
| Ocular clonus plus agitation or diaphoresis |
| Inducible clonus plus agitation or diaphoresis |
| *A combination of these characteristics may indicate serotonin syndrome |
| Source: References 1-3 |
Interactions that increase risk
A drug interaction is a pharmacologic or clinical response to a combination of medications that differs from the agents’ known effects if given on their own. In the context of serotonin syndrome, the serotonergic activity of a drug can be increased as a result of a pharmacokinetic (PK) interaction, a pharmacodynamic (PD) interaction, or a combination of both.
PK interactions may result from the coadministration of a drug that alters absorption, distribution, metabolism, or elimination parameters of \>1 other drugs. Serotonergic antidepressants usually are metabolized by cytochrome P450 (CYP450) enzymes. Any drug that inhibits a CYP450 enzyme responsible for biotransformation of 1 of these antidepressants may increase exposure to the antidepressant and raise the risk of serotonin syndrome. CYP450 inhibitors include prescription medications as well as seemingly benign over-the-counter (OTC) drugs.
PD interactions may result from an additive or synergistic pharmacologic effect caused by coadministration of 2 agents that produce the same or similar end result. In Ms. B’s case, agents inhibiting 5-HT reuptake (fluoxetine and amitriptyline) were combined with a direct 5-HT agonist (sumatriptan). The resulting potentiation of 5-HT via 2 distinct mechanisms increased Ms. B’s risk of serotonin syndrome. Similarly, simultaneous use of 2 agents potentiating 5-HT through identical mechanisms, such as combining 2 serotonin reuptake inhibitors, also may increase the risk of serotonin syndrome ( Table 2 ).1
A combination of PK and PD interactions also may increase the risk of serotonin syndrome. For example, Ms. B is taking fluoxetine and amitriptyline for different therapeutic reasons. Both of these agents inhibit 5-HT reuptake, potentiating 5-HT. In addition, amitriptyline is a substrate for CYP2D6 and fluoxetine is a robust CYP2D6 inhibitor. The coadministration of fluoxetine with tricyclic antidepressants (TCAs) results in a 4- to 5-fold increase in TCA exposure, which may increase the risk of serotonin syndrome and other sequelae from TCA toxicity.4,5
Table 2
Drugs associated with serotonin syndrome
| Drugs that increase 5-HT release | Amphetamine, cocaine, MDMA (ecstasy), mirtazapine, phentermine, reserpine |
| Drugs that inhibit 5-HT reuptake | Amitriptyline, amphetamine, bupropion, Citalopram, clomipramine, cocaine, desipramine, dextromethorphan, doxepin, duloxetine, escitalopram, fentanyl, fluoxetine, fluvoxamine, Hypericum perforatum (St. John’s wort), imipramine, MDMA, meperidine, nefazodone, nortriptyline, paroxetine, protriptyline, sertraline, tramadol, trazodone, venlafaxine |
| Drugs that decrease 5-HT metabolism | Isocarboxazid, linezolid, phenelzine, selegiline, tranylcypromine |
| Drugs that are direct 5-HT agonists | Almotriptan, buspirone, dihydroergotamine, eletriptan, frovatriptan, LSD, naratriptan, rizatriptan, sumatriptan, zolmitriptan |
| Others | L-tryptophan, carbamazepine, carisoprodol, droperidol, levodopa, lithium, metoclopramide, pentazocine, phenylpropanolamine |
| 5-HT: serotonin; LSD: lysergic acid; MDMA: methylenedioxymethamphetamine | |
| Source: Reference 1 | |
Preventing serotonin syndrome
The warnings highlighted in drug interaction references or pharmacy databases often mean that clinicians have to evaluate whether the risk of combining medications outweighs the therapeutic benefits. It is unknown why some patients tolerate multiple agents potentiating 5-HT, and practitioners cannot predict when and in whom serotonin syndrome may occur. However, the following strategies may help minimize these risks:
Know which drugs are associated with serotonin syndrome. Concomitant use of these drugs and agents that inhibit metabolism of these drugs increases risk.
Know which drugs your patient is taking. Patients may see several prescribers, which makes it essential to ask what they are receiving from other practitioners. Also inquire about OTC and illicit drug use.
Check for interactions. If you are unfamiliar with a new drug or drug-drug combination, check multiple resources for potential interactions. The potential severity of an interaction and the detail in which interactions are described—such as class effects vs documented cases or studies—differs among drug interaction resources, which means a potential interaction may be “flagged” in 1 source but not another. Electronic resources such as Micromedex and Lexicomp often have detailed literature summaries and citations so clinicians can review primary literature that lead to the categorization of an interaction. Using multiple sources is helpful when trying to translate warnings in the context of a clinical scenario.
Weigh the risks and benefits. Prescribers know that not all treatments are benign, but not treating a condition also may be detrimental. Identify potential alternative pharmacologic or nonpharmacologic treatments when possible. Discuss the risks and benefits of drug therapy with patients.
Counsel your patients. Although it is not possible to predict who may experience serotonin syndrome, educate patients on what symptoms to look for. Instruct them to call their prescriber or pharmacist if they show symptoms that may be consistent with serotonin syndrome.
Related Resource
• MedWatch: The FDA Safety Information and Adverse Event Reporting Program. www.fda.gov/Safety/MedWatch.
Drug Brand Names
- Aripiprazole • Abilify
- Almotriptan • Axert
- Amitriptyline • Elavil
- Bupropion • Wellbutrin, Zyban
- Buspirone • BuSpar
- Carbamazepine • Carbatrol, Equetro, others
- Carisoprodol • Soma
- Citalopram • Celexa
- Desipramine • Norpramin
- Dihydroergotamine • Migranal
- Doxepin • Adapin, Silenor
- Droperidol • Inapsine
- Duloxetine • Cymbalta
- Eletriptan • Relpax
- Escitalopram • Lexapro
- Fentanyl • Sublimaze, others
- Fluoxetine • Prozac
- Fluvoxamine • Luvox
- Frovatriptan • Frova
- Imipramine • Tofranil
- Isocarboxazid • Marplan
- Levodopa • Dopar, Larodopa, others
- Linezolid • Zyvox
- Lithium • Eskalith, Lithobid
- Meperidine • Demerol
- Metoclopramide • Reglan, Metozol
- Mirtazapine • Remeron
- Naratriptan • Amerge
- Nefazodone • Serzone
- Nortriptyline • Aventyl, Pamelor
- Paroxetine • Paxil
- Pentazocine • Talwin
- Phenelzine • Nardil
- Phentermine • Fastin, Adipex-P
- Protriptyline • Vivactil
- Reserpine • Serpasil
- Rizatriptan • Maxalt
- Selegiline • Carbex, Eldepryl, others
- Sertraline • Zoloft
- Sumatriptan • Imitrex, Alsuma
- Tramadol • Ultram, Ultracet, others
- Tranylcypromine • Parnate
- Trazodone • Desyrel, Oleptro
- Venlafaxine • Effexor
- Zolmitriptan • Zomig
Disclosures
Dr. Jeffrey Bishop receives grant/research support from Ortho-McNeil-Janssen.
Dr. Danielle Bishop reports no financial relationship with any company whose products are mentioned in this article, or with manufacturers of competing products.
1. Beyer EW, Shannon M. The serotonin syndrome. N Engl J Med. 2005;352:1112-1120.
2. Dunkley EJ, Isbister GK, Sibbritt D, et al. The TTunter Serotonin Toxicity Criteria: simple and accurate diagnostic decision rules for serotonin toxicity. QJM. 2003;96:635-642.
3. Sternbach H. The serotonin syndrome. Am J Psychiatry. 1991;148:705-713.
4. Preskorn SH, Beber JH, Faul JC, et al. Serious adverse effects of combining fluoxetine and tricyclic antidepressants. Am J Psychiatry. 1990;147-532.
5. Preskorn SH, Alderman J, Chung M, et al. Pharmacokinetics of desipramine coadministered with sertraline or fluoxetine. J Clin Psychopharmacol. 1994;14:90-98.
• Know which drugs are associated with serotonin syndrome.
• Understand the types of drug interactions that may precipitate serotonin syndrome and use drug information resources such as Micromedex, Lexicomp, Physicians’ Desk Reference, AHFS Drug Information, and Facts and Comparisons.
• Know what prescription medications your patient is receiving from other providers as well as any over-the-counter and illicit drugs they may be using.
Ms. B, age 22, is brought to the emergency department (ED) by her roommate for evaluation of confusion. Ms. B has a history of migraines and major depressive disorder and has been taking fluoxetine, 40 mg/d, for 1 year. A week ago, she started amitriptyline, 50 mg/d, when her migraines became more frequent. According to her roommate, Ms. B experienced a migraine early in the morning and had taken 2 doses of sumatriptan, 50 mg. She later complained of nausea and vomiting, and when her roommate returned from work that evening Ms. B was disoriented and her leg muscles would not stop twitching.
In the ED, Ms. B is diaphoretic and increasingly agitated. Blood alcohol and urine drug screens are negative. Blood glucose is 95 mg/dL. Complete blood count, basic metabolic panel, liver function, and kidney function tests are within normal limits. Her physical examination reveals a blood pressure of 130/85 mm Hg, heart rate of 130 beats per minute, respiratory rate of 21 breaths per minute, and body temperature of 38.6°C (101. 4°F). Myoclonus and hyperreflexia affect her lower extremities. Ms. B is admitted with a preliminary diagnosis of serotonin (5-HT) syndrome.
Serotonin syndrome: What is it?
Serotonin syndrome is a rare but potentially serious adverse event resulting from excess serotonergic activity at central and peripheral 5-HT2A and 5-HT1A receptors. Serotonin syndrome toxicity ranges from relatively mild to severe, and may be lethal. Symptoms develop rapidly—within hours—and may include altered mental status, clonus, tremor, hyperthermia, diaphoresis, tachycardia, mydriasis, and akathisia ( Table 1 ).1-3 Fortunately, if recognized promptly and offending agents are discontinued, serotonin syndrome often resolves within a couple of days.
The differential diagnosis includes neuroleptic malignant syndrome (NMS), anticholinergic toxicity, and malignant hyperthermia.1 Differentiating serotonin syndrome from NMS can be difficult. NMS results from dopamine blockade; however, many NMS symptoms are similar to those experienced with serotonin syndrome. Obtaining a history of recent medication and/or illicit drug use, conducting a physical exam, and evaluating the patient’s clinical course help clarify a likely diagnosis. NMS generally has a slower onset—within days—and patients demonstrate neuromuscular rigidity and bradykinesia rather than the neuromuscular hyperreactivity (myoclonus, hyperreflexia) seen with serotonin syndrome.
Table 1
Characteristics of serotonin syndrome*
| Recent addition or dose increase of a serotonergic agent |
| Tremor plus hyperreflexia |
| Muscle rigidity plus fever plus clonus |
| Spontaneous clonus |
| Ocular clonus plus agitation or diaphoresis |
| Inducible clonus plus agitation or diaphoresis |
| *A combination of these characteristics may indicate serotonin syndrome |
| Source: References 1-3 |
Interactions that increase risk
A drug interaction is a pharmacologic or clinical response to a combination of medications that differs from the agents’ known effects if given on their own. In the context of serotonin syndrome, the serotonergic activity of a drug can be increased as a result of a pharmacokinetic (PK) interaction, a pharmacodynamic (PD) interaction, or a combination of both.
PK interactions may result from the coadministration of a drug that alters absorption, distribution, metabolism, or elimination parameters of \>1 other drugs. Serotonergic antidepressants usually are metabolized by cytochrome P450 (CYP450) enzymes. Any drug that inhibits a CYP450 enzyme responsible for biotransformation of 1 of these antidepressants may increase exposure to the antidepressant and raise the risk of serotonin syndrome. CYP450 inhibitors include prescription medications as well as seemingly benign over-the-counter (OTC) drugs.
PD interactions may result from an additive or synergistic pharmacologic effect caused by coadministration of 2 agents that produce the same or similar end result. In Ms. B’s case, agents inhibiting 5-HT reuptake (fluoxetine and amitriptyline) were combined with a direct 5-HT agonist (sumatriptan). The resulting potentiation of 5-HT via 2 distinct mechanisms increased Ms. B’s risk of serotonin syndrome. Similarly, simultaneous use of 2 agents potentiating 5-HT through identical mechanisms, such as combining 2 serotonin reuptake inhibitors, also may increase the risk of serotonin syndrome ( Table 2 ).1
A combination of PK and PD interactions also may increase the risk of serotonin syndrome. For example, Ms. B is taking fluoxetine and amitriptyline for different therapeutic reasons. Both of these agents inhibit 5-HT reuptake, potentiating 5-HT. In addition, amitriptyline is a substrate for CYP2D6 and fluoxetine is a robust CYP2D6 inhibitor. The coadministration of fluoxetine with tricyclic antidepressants (TCAs) results in a 4- to 5-fold increase in TCA exposure, which may increase the risk of serotonin syndrome and other sequelae from TCA toxicity.4,5
Table 2
Drugs associated with serotonin syndrome
| Drugs that increase 5-HT release | Amphetamine, cocaine, MDMA (ecstasy), mirtazapine, phentermine, reserpine |
| Drugs that inhibit 5-HT reuptake | Amitriptyline, amphetamine, bupropion, Citalopram, clomipramine, cocaine, desipramine, dextromethorphan, doxepin, duloxetine, escitalopram, fentanyl, fluoxetine, fluvoxamine, Hypericum perforatum (St. John’s wort), imipramine, MDMA, meperidine, nefazodone, nortriptyline, paroxetine, protriptyline, sertraline, tramadol, trazodone, venlafaxine |
| Drugs that decrease 5-HT metabolism | Isocarboxazid, linezolid, phenelzine, selegiline, tranylcypromine |
| Drugs that are direct 5-HT agonists | Almotriptan, buspirone, dihydroergotamine, eletriptan, frovatriptan, LSD, naratriptan, rizatriptan, sumatriptan, zolmitriptan |
| Others | L-tryptophan, carbamazepine, carisoprodol, droperidol, levodopa, lithium, metoclopramide, pentazocine, phenylpropanolamine |
| 5-HT: serotonin; LSD: lysergic acid; MDMA: methylenedioxymethamphetamine | |
| Source: Reference 1 | |
Preventing serotonin syndrome
The warnings highlighted in drug interaction references or pharmacy databases often mean that clinicians have to evaluate whether the risk of combining medications outweighs the therapeutic benefits. It is unknown why some patients tolerate multiple agents potentiating 5-HT, and practitioners cannot predict when and in whom serotonin syndrome may occur. However, the following strategies may help minimize these risks:
Know which drugs are associated with serotonin syndrome. Concomitant use of these drugs and agents that inhibit metabolism of these drugs increases risk.
Know which drugs your patient is taking. Patients may see several prescribers, which makes it essential to ask what they are receiving from other practitioners. Also inquire about OTC and illicit drug use.
Check for interactions. If you are unfamiliar with a new drug or drug-drug combination, check multiple resources for potential interactions. The potential severity of an interaction and the detail in which interactions are described—such as class effects vs documented cases or studies—differs among drug interaction resources, which means a potential interaction may be “flagged” in 1 source but not another. Electronic resources such as Micromedex and Lexicomp often have detailed literature summaries and citations so clinicians can review primary literature that lead to the categorization of an interaction. Using multiple sources is helpful when trying to translate warnings in the context of a clinical scenario.
Weigh the risks and benefits. Prescribers know that not all treatments are benign, but not treating a condition also may be detrimental. Identify potential alternative pharmacologic or nonpharmacologic treatments when possible. Discuss the risks and benefits of drug therapy with patients.
Counsel your patients. Although it is not possible to predict who may experience serotonin syndrome, educate patients on what symptoms to look for. Instruct them to call their prescriber or pharmacist if they show symptoms that may be consistent with serotonin syndrome.
Related Resource
• MedWatch: The FDA Safety Information and Adverse Event Reporting Program. www.fda.gov/Safety/MedWatch.
Drug Brand Names
- Aripiprazole • Abilify
- Almotriptan • Axert
- Amitriptyline • Elavil
- Bupropion • Wellbutrin, Zyban
- Buspirone • BuSpar
- Carbamazepine • Carbatrol, Equetro, others
- Carisoprodol • Soma
- Citalopram • Celexa
- Desipramine • Norpramin
- Dihydroergotamine • Migranal
- Doxepin • Adapin, Silenor
- Droperidol • Inapsine
- Duloxetine • Cymbalta
- Eletriptan • Relpax
- Escitalopram • Lexapro
- Fentanyl • Sublimaze, others
- Fluoxetine • Prozac
- Fluvoxamine • Luvox
- Frovatriptan • Frova
- Imipramine • Tofranil
- Isocarboxazid • Marplan
- Levodopa • Dopar, Larodopa, others
- Linezolid • Zyvox
- Lithium • Eskalith, Lithobid
- Meperidine • Demerol
- Metoclopramide • Reglan, Metozol
- Mirtazapine • Remeron
- Naratriptan • Amerge
- Nefazodone • Serzone
- Nortriptyline • Aventyl, Pamelor
- Paroxetine • Paxil
- Pentazocine • Talwin
- Phenelzine • Nardil
- Phentermine • Fastin, Adipex-P
- Protriptyline • Vivactil
- Reserpine • Serpasil
- Rizatriptan • Maxalt
- Selegiline • Carbex, Eldepryl, others
- Sertraline • Zoloft
- Sumatriptan • Imitrex, Alsuma
- Tramadol • Ultram, Ultracet, others
- Tranylcypromine • Parnate
- Trazodone • Desyrel, Oleptro
- Venlafaxine • Effexor
- Zolmitriptan • Zomig
Disclosures
Dr. Jeffrey Bishop receives grant/research support from Ortho-McNeil-Janssen.
Dr. Danielle Bishop reports no financial relationship with any company whose products are mentioned in this article, or with manufacturers of competing products.
• Know which drugs are associated with serotonin syndrome.
• Understand the types of drug interactions that may precipitate serotonin syndrome and use drug information resources such as Micromedex, Lexicomp, Physicians’ Desk Reference, AHFS Drug Information, and Facts and Comparisons.
• Know what prescription medications your patient is receiving from other providers as well as any over-the-counter and illicit drugs they may be using.
Ms. B, age 22, is brought to the emergency department (ED) by her roommate for evaluation of confusion. Ms. B has a history of migraines and major depressive disorder and has been taking fluoxetine, 40 mg/d, for 1 year. A week ago, she started amitriptyline, 50 mg/d, when her migraines became more frequent. According to her roommate, Ms. B experienced a migraine early in the morning and had taken 2 doses of sumatriptan, 50 mg. She later complained of nausea and vomiting, and when her roommate returned from work that evening Ms. B was disoriented and her leg muscles would not stop twitching.
In the ED, Ms. B is diaphoretic and increasingly agitated. Blood alcohol and urine drug screens are negative. Blood glucose is 95 mg/dL. Complete blood count, basic metabolic panel, liver function, and kidney function tests are within normal limits. Her physical examination reveals a blood pressure of 130/85 mm Hg, heart rate of 130 beats per minute, respiratory rate of 21 breaths per minute, and body temperature of 38.6°C (101. 4°F). Myoclonus and hyperreflexia affect her lower extremities. Ms. B is admitted with a preliminary diagnosis of serotonin (5-HT) syndrome.
Serotonin syndrome: What is it?
Serotonin syndrome is a rare but potentially serious adverse event resulting from excess serotonergic activity at central and peripheral 5-HT2A and 5-HT1A receptors. Serotonin syndrome toxicity ranges from relatively mild to severe, and may be lethal. Symptoms develop rapidly—within hours—and may include altered mental status, clonus, tremor, hyperthermia, diaphoresis, tachycardia, mydriasis, and akathisia ( Table 1 ).1-3 Fortunately, if recognized promptly and offending agents are discontinued, serotonin syndrome often resolves within a couple of days.
The differential diagnosis includes neuroleptic malignant syndrome (NMS), anticholinergic toxicity, and malignant hyperthermia.1 Differentiating serotonin syndrome from NMS can be difficult. NMS results from dopamine blockade; however, many NMS symptoms are similar to those experienced with serotonin syndrome. Obtaining a history of recent medication and/or illicit drug use, conducting a physical exam, and evaluating the patient’s clinical course help clarify a likely diagnosis. NMS generally has a slower onset—within days—and patients demonstrate neuromuscular rigidity and bradykinesia rather than the neuromuscular hyperreactivity (myoclonus, hyperreflexia) seen with serotonin syndrome.
Table 1
Characteristics of serotonin syndrome*
| Recent addition or dose increase of a serotonergic agent |
| Tremor plus hyperreflexia |
| Muscle rigidity plus fever plus clonus |
| Spontaneous clonus |
| Ocular clonus plus agitation or diaphoresis |
| Inducible clonus plus agitation or diaphoresis |
| *A combination of these characteristics may indicate serotonin syndrome |
| Source: References 1-3 |
Interactions that increase risk
A drug interaction is a pharmacologic or clinical response to a combination of medications that differs from the agents’ known effects if given on their own. In the context of serotonin syndrome, the serotonergic activity of a drug can be increased as a result of a pharmacokinetic (PK) interaction, a pharmacodynamic (PD) interaction, or a combination of both.
PK interactions may result from the coadministration of a drug that alters absorption, distribution, metabolism, or elimination parameters of \>1 other drugs. Serotonergic antidepressants usually are metabolized by cytochrome P450 (CYP450) enzymes. Any drug that inhibits a CYP450 enzyme responsible for biotransformation of 1 of these antidepressants may increase exposure to the antidepressant and raise the risk of serotonin syndrome. CYP450 inhibitors include prescription medications as well as seemingly benign over-the-counter (OTC) drugs.
PD interactions may result from an additive or synergistic pharmacologic effect caused by coadministration of 2 agents that produce the same or similar end result. In Ms. B’s case, agents inhibiting 5-HT reuptake (fluoxetine and amitriptyline) were combined with a direct 5-HT agonist (sumatriptan). The resulting potentiation of 5-HT via 2 distinct mechanisms increased Ms. B’s risk of serotonin syndrome. Similarly, simultaneous use of 2 agents potentiating 5-HT through identical mechanisms, such as combining 2 serotonin reuptake inhibitors, also may increase the risk of serotonin syndrome ( Table 2 ).1
A combination of PK and PD interactions also may increase the risk of serotonin syndrome. For example, Ms. B is taking fluoxetine and amitriptyline for different therapeutic reasons. Both of these agents inhibit 5-HT reuptake, potentiating 5-HT. In addition, amitriptyline is a substrate for CYP2D6 and fluoxetine is a robust CYP2D6 inhibitor. The coadministration of fluoxetine with tricyclic antidepressants (TCAs) results in a 4- to 5-fold increase in TCA exposure, which may increase the risk of serotonin syndrome and other sequelae from TCA toxicity.4,5
Table 2
Drugs associated with serotonin syndrome
| Drugs that increase 5-HT release | Amphetamine, cocaine, MDMA (ecstasy), mirtazapine, phentermine, reserpine |
| Drugs that inhibit 5-HT reuptake | Amitriptyline, amphetamine, bupropion, Citalopram, clomipramine, cocaine, desipramine, dextromethorphan, doxepin, duloxetine, escitalopram, fentanyl, fluoxetine, fluvoxamine, Hypericum perforatum (St. John’s wort), imipramine, MDMA, meperidine, nefazodone, nortriptyline, paroxetine, protriptyline, sertraline, tramadol, trazodone, venlafaxine |
| Drugs that decrease 5-HT metabolism | Isocarboxazid, linezolid, phenelzine, selegiline, tranylcypromine |
| Drugs that are direct 5-HT agonists | Almotriptan, buspirone, dihydroergotamine, eletriptan, frovatriptan, LSD, naratriptan, rizatriptan, sumatriptan, zolmitriptan |
| Others | L-tryptophan, carbamazepine, carisoprodol, droperidol, levodopa, lithium, metoclopramide, pentazocine, phenylpropanolamine |
| 5-HT: serotonin; LSD: lysergic acid; MDMA: methylenedioxymethamphetamine | |
| Source: Reference 1 | |
Preventing serotonin syndrome
The warnings highlighted in drug interaction references or pharmacy databases often mean that clinicians have to evaluate whether the risk of combining medications outweighs the therapeutic benefits. It is unknown why some patients tolerate multiple agents potentiating 5-HT, and practitioners cannot predict when and in whom serotonin syndrome may occur. However, the following strategies may help minimize these risks:
Know which drugs are associated with serotonin syndrome. Concomitant use of these drugs and agents that inhibit metabolism of these drugs increases risk.
Know which drugs your patient is taking. Patients may see several prescribers, which makes it essential to ask what they are receiving from other practitioners. Also inquire about OTC and illicit drug use.
Check for interactions. If you are unfamiliar with a new drug or drug-drug combination, check multiple resources for potential interactions. The potential severity of an interaction and the detail in which interactions are described—such as class effects vs documented cases or studies—differs among drug interaction resources, which means a potential interaction may be “flagged” in 1 source but not another. Electronic resources such as Micromedex and Lexicomp often have detailed literature summaries and citations so clinicians can review primary literature that lead to the categorization of an interaction. Using multiple sources is helpful when trying to translate warnings in the context of a clinical scenario.
Weigh the risks and benefits. Prescribers know that not all treatments are benign, but not treating a condition also may be detrimental. Identify potential alternative pharmacologic or nonpharmacologic treatments when possible. Discuss the risks and benefits of drug therapy with patients.
Counsel your patients. Although it is not possible to predict who may experience serotonin syndrome, educate patients on what symptoms to look for. Instruct them to call their prescriber or pharmacist if they show symptoms that may be consistent with serotonin syndrome.
Related Resource
• MedWatch: The FDA Safety Information and Adverse Event Reporting Program. www.fda.gov/Safety/MedWatch.
Drug Brand Names
- Aripiprazole • Abilify
- Almotriptan • Axert
- Amitriptyline • Elavil
- Bupropion • Wellbutrin, Zyban
- Buspirone • BuSpar
- Carbamazepine • Carbatrol, Equetro, others
- Carisoprodol • Soma
- Citalopram • Celexa
- Desipramine • Norpramin
- Dihydroergotamine • Migranal
- Doxepin • Adapin, Silenor
- Droperidol • Inapsine
- Duloxetine • Cymbalta
- Eletriptan • Relpax
- Escitalopram • Lexapro
- Fentanyl • Sublimaze, others
- Fluoxetine • Prozac
- Fluvoxamine • Luvox
- Frovatriptan • Frova
- Imipramine • Tofranil
- Isocarboxazid • Marplan
- Levodopa • Dopar, Larodopa, others
- Linezolid • Zyvox
- Lithium • Eskalith, Lithobid
- Meperidine • Demerol
- Metoclopramide • Reglan, Metozol
- Mirtazapine • Remeron
- Naratriptan • Amerge
- Nefazodone • Serzone
- Nortriptyline • Aventyl, Pamelor
- Paroxetine • Paxil
- Pentazocine • Talwin
- Phenelzine • Nardil
- Phentermine • Fastin, Adipex-P
- Protriptyline • Vivactil
- Reserpine • Serpasil
- Rizatriptan • Maxalt
- Selegiline • Carbex, Eldepryl, others
- Sertraline • Zoloft
- Sumatriptan • Imitrex, Alsuma
- Tramadol • Ultram, Ultracet, others
- Tranylcypromine • Parnate
- Trazodone • Desyrel, Oleptro
- Venlafaxine • Effexor
- Zolmitriptan • Zomig
Disclosures
Dr. Jeffrey Bishop receives grant/research support from Ortho-McNeil-Janssen.
Dr. Danielle Bishop reports no financial relationship with any company whose products are mentioned in this article, or with manufacturers of competing products.
1. Beyer EW, Shannon M. The serotonin syndrome. N Engl J Med. 2005;352:1112-1120.
2. Dunkley EJ, Isbister GK, Sibbritt D, et al. The TTunter Serotonin Toxicity Criteria: simple and accurate diagnostic decision rules for serotonin toxicity. QJM. 2003;96:635-642.
3. Sternbach H. The serotonin syndrome. Am J Psychiatry. 1991;148:705-713.
4. Preskorn SH, Beber JH, Faul JC, et al. Serious adverse effects of combining fluoxetine and tricyclic antidepressants. Am J Psychiatry. 1990;147-532.
5. Preskorn SH, Alderman J, Chung M, et al. Pharmacokinetics of desipramine coadministered with sertraline or fluoxetine. J Clin Psychopharmacol. 1994;14:90-98.
1. Beyer EW, Shannon M. The serotonin syndrome. N Engl J Med. 2005;352:1112-1120.
2. Dunkley EJ, Isbister GK, Sibbritt D, et al. The TTunter Serotonin Toxicity Criteria: simple and accurate diagnostic decision rules for serotonin toxicity. QJM. 2003;96:635-642.
3. Sternbach H. The serotonin syndrome. Am J Psychiatry. 1991;148:705-713.
4. Preskorn SH, Beber JH, Faul JC, et al. Serious adverse effects of combining fluoxetine and tricyclic antidepressants. Am J Psychiatry. 1990;147-532.
5. Preskorn SH, Alderman J, Chung M, et al. Pharmacokinetics of desipramine coadministered with sertraline or fluoxetine. J Clin Psychopharmacol. 1994;14:90-98.
Should you order genetic testing to identify how patients metabolize antipsychotics?
Two months ago, Mr. P, age 20, experienced paranoid thoughts, anxiety, agitation, and auditory hallucinations. During a brief hospitalization 1 month later, he received IM haloperidol, 2 mg, which he said “made his neck stiff.” After he was discharged, Mr. P, who is White, stopped taking his antipsychotics. During a recent outpatient evaluation, the clinician gives Mr. P a working diagnosis of schizophrenia and prescribes risperidone, 2 mg/d, with plans to titrate to 4 mg/d in the next 2 weeks. However, a week later, Mr. P complains of extreme sedation and feeling “knocked out” and does not want to continue taking the medication. Physical exam reveals slight cogwheel rigidity. His delusional thought content is not improved. The treating physician considers ordering a genetic test to determine Mr. P’s cytochrome P450 (CYP) 2D6 metabolizer status.
Studies investigating relationships among genetic variants thought to impact pharmacokinetics and pharmacodynamics of psychotropic medications have had mixed results.1 Metabolism of most antipsychotics depends on the CYP450 enzyme system, which is expressed predominantly in the liver (Table 1). CYP2D6 is one of these enzymes and may be responsible for metabolizing approximately 20% to 50% of all medications, including a number of antipsychotics.2 Genetic variations of CYP2D6 are common and the frequencies of these variants differ among racial groups.3
The half-life and other pharmacokinetic parameters of an antipsychotic metabolized by CYP2D6 may differ based on whether someone is a poor metabolizer (PM), intermediate metabolizer (IM), extensive metabolizer (EM), or ultrarapid metabolizer (UM).4 Regarding CYP2D6 metabolism among Whites, 3% to 5% are UMs, 70% to 80% are EMs, 10% to 17% are IMs, and 5% to 10% are PMs.5 By contrast, the percentage of PMs and UMs in the Asian population is low—about 1% for each phenotype; the IM phenotype is more common (65% to 70% in the Chinese population).5,6 The percentage of PMs in African Americans is roughly 2% to 6%.2
- Genetic variants of CYP2D6 may result in decreased or increased metabolism of some drugs, including risperidone, iloperidone, perphenazine, haloperidol, and thioridazine.
- The effect of reduced CYP2D6 activity may increase a patient’s risk for dose-related adverse effects.
- It is currently unknown if clinical genotyping for CYP2D6 variants and using this information to guide drug selection or dosing improves patient outcomes.
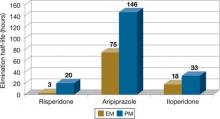
The clinical effect of altered metabolizer status depends on the extent the metabolism of a given agent is dependent on CYP2D6. PM status results in an approximately 2- to 6-fold increase in elimination half-life and overall exposure of aripiprazole,7 risperidone,8 and iloperidone9 (Figure). On the other end of the spectrum are UMs. Because of gene duplication, patients who fall into this category have enhanced metabolic activity. As a result, the therapeutic effect of several medications may be decreased because of faster clearance from the body, leading some physicians to label them as treatment-resistant.
Because side effects of many antipsychotics are dose-dependent, genotyping may be valuable for patients taking agents that are primarily metabolized by CYP2D6.10 Clinicians now have access to laboratory resources and FDA-approved methods for assessing CYP2D6 gene variants.11 It is debatable, however, whether this testing—which is expensive (≥$400) and may not be covered by health insurance—improves patient outcomes. In Mr. P’s case, if he had been genotyped as a CYP2D6 PM before treatment, his physicians might not have prescribed haloperidol and could have prevented a mild dystonic reaction. Also, they could have lowered the initial risperidone dose or chosen an antipsychotic such as ziprasidone, paliperidone, or quetiapine where the pharmacokinetic consequences of 2D6 poor metabolism are not as severe. Theoretically, one may argue that this could have reduced the risk for antipsychotic-associated side effects that now are a barrier to Mr. P’s desire to continue antipsychotics. On the other hand one may also reasonably argue that there may be other/additional reasons (genetic or non-genetic) that make some patients more sensitive to the side effects of antipsychotics and that simply assessing CYP2D6 status is not enough to guide drug selection and dosing.
Table 1
Cytochrome P450 (CYP) metabolism of commonly used antipsychotics*
| Drug | CYP1A2 | CYP2C9 | CYP2C19 | CYP2D6 | CYP3A4/5 |
|---|---|---|---|---|---|
| Aripiprazole | X | X | |||
| Asenapine | X | X | X | ||
| Chlorpromazine | X | X | X | ||
| Clozapine | X | X | X | X | X |
| Fluphenazine | X | ||||
| Haloperidol | X | X | X | ||
| Iloperidone | X | X | |||
| Olanzapine | X | X | |||
| Paliperidone | X† | X† | |||
| Perphenazine | X | X | X | X | X |
| Quetiapine | X | X | |||
| Risperidone | X | X | |||
| Thioridazine | X | X | |||
| Ziprasidone | X | X | |||
| *Information obtained from the most recent prescribing information available from each drug’s manufacturer †According to paliperidone’s prescribing information, in vitro studies identify that CYP2D6 and CYP3A4 may be involved in paliperidone metabolism, but in vivo studies indicate that their role in eliminating paliperidone is minimal | |||||
Figure: Effects of CYP2D6 poor metabolizer status on the half-life of risperidone, aripiprazole, and iloperidone
EM: extensive metabolizer; PM: poor metabolizer
Source: References 7-9
Use in clinical practice
Proposed expert guidelines recommend halving the normal target dose of risperidone and avoiding haloperidol and phenothiazine antipsychotics in CYP2D6 PMs.12 These guidelines are based on expert review of the pharmacokinetic effects of CYP2D6 PM status as well as case reports and studies associating CYP2D6 with poor outcomes, usually side effects. Although these studies suggest that determining metabolizer status may be clinically important, many other studies—some very large—have not found evidence for associations between drug metabolizing enzyme variants and clinical outcomes from antipsychotics.13
There are 2 clinical scenarios in which one may consider obtaining CYP2D6 genotype information:
- before initiating treatment (Table 2)
- after trying ≥1 agent primarily dependent on CYP2D6 with evidence of dose-related side effect (Table 3).
Identifying PMs could influence drug selection and dosing if this information is available before antipsychotic exposure. Studies have found evidence that CYP2D6 PMs may be at greater risk of experiencing adverse reactions to risperidone compared with other metabolizer groups.14 Also, prescribing information for aripiprazole and iloperidone recommends halving the dose of these drugs in the presence of CYP2D6 inhibitors, a condition that pharmacokinetically mimics PM status.
Knowing genotype information after ≥1 drugs have been tried may not be as useful. Clinicians often base drug switches or dose titrations on a patient’s experience with present or past doses of the antipsychotic. Examples include slowing titrations or reducing a target dose when a patient, such as Mr. P, experiences side effects, or selecting non-2D6 substrate agents after detecting a pattern of drug sensitivity.
Table 2
CYP2D6 testing before initiating antipsychotics: Benefits vs drawbacks
| Benefits | Drawbacks |
|---|---|
| Clinicians could avoid 2D6 substrate drugs with high likelihood for ADEs or increased risk of 2D6-based interactions in PMs | No empiric evidence shows that routine genotyping produces better clinical outcomes (eg, fewer side effects and better treatment adherence) |
| May lower initial dose, slow titration, and lower initial target dose to minimize risk of side effects in PMs | Many clinicians titrate slowly or adjust titration schedule and target doses based on initial tolerability as part of routine practice |
| The test would need to be done only once and the information may be useful for other therapy decisions | Patients who need immediate drug therapy may not be able to wait for test results |
| Testing may not be covered by a patient’s health insurance | |
| ADEs: adverse drug events; PMs: poor metabolizers | |
Table 3
Genotype testing after a patient experiences side effects
| Benefits |
| Identifying a biologic reason for side effect sensitivity may aid choice and dosing of subsequent antipsychotics and other medications |
| Drawbacks |
| In clinical practice, antipsychotic switching because of tolerability (and response) often is guided by outcomes experienced from previously used agents. In general, patients with a history of experiencing side effects at lower doses of antipsychotics are likely to be initiated at lower doses and titrated more cautiously during subsequent therapy choices regardless of whether side effects were caused by metabolizer status or other factor(s) |
Better patient outcomes?
It is not known if obtaining genotype information will provide better outcomes than a “trial and error” approach. Currently, obtaining genotype information before antipsychotic treatment is not standard clinical practice. Because this testing is expensive and requires prior approval from third party payers or out-of-pocket financial resources, testing is not recommended for all patients at this time.
However, a growing body of evidence suggests that knowing metabolizer status could be useful in drug selection or dosing for antipsychotics. This scientific knowledge continues to accumulate, and CYP2D6 genotyping may some day be integrated into routine clinical care. Currently, for patients and physicians with the resources to obtain and the ability to appropriately interpret the test results, this information may prove useful on an individual basis. However, additional studies are needed to support better outcomes from dosing and drug selection based on CYP2D6 genotype information.
Related Resources
- Evaluation of Genomic Applications in Practice and Prevention (EGAPP). www.egappreviews.org.
- Pharmacogenomics Knowledge Base. www.pharmgkb.org.
- Indiana University School of Medicine. P450 drug interaction table. http://medicine.iupui.edu/clinpharm/ddis/table.asp.
Drug Brand Names
- Aripiprazole • Abilify
- Asenapine • Saphris
- Chlorpromazine • Thorazine
- Clozapine • Clozaril
- Fluphenazine • Prolixin
- Haloperidol • Haldol
- Iloperidone • Fanapt
- Olanzapine • Zyprexa
- Paliperidone • Invega
- Perphenazine • Trilafon
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Thioridazine • Mellaril
- Ziprasidone • Geodon
Disclosures
Dr. Bishop receives grant/research support from the National Institute of Mental Health, NARSAD, and Ortho-McNeil-Janssen and has received honoraria from Eli Lilly and Company.
Ms. Chae reports no financial relationship with any company whose products are mentioned in this article, or with manufacturers of competing products.
1. Leckband SG, Bishop JR, Ellingrod VL. Pharmacogenomics in psychiatry. J Pharm Pract. 2007;20:252-264.
2. Neafsey P, Ginsberg G, Hattis D, et al. Genetic polymorphism in cytochrome P450 2D6 (CYP2D6): population distribution of CYP2D6 activity. J Toxicol Environ Health B Crit Rev. 2009;12(5-6):334-361.
3. Bradford LD, Gaedigk A, Leeder JS. High frequency of CYP2D6 poor and “intermediate” metabolizers in black populations: a review and preliminary data. Psychopharmacol Bull. 1998;34:797-804.
4. Gaedigk A, Simon SD, Pearce RE, et al. The CYP2D6 activity score: translating genotype information into a qualitative measure of phenotype. Clin Pharmacol Ther. 2008;83:234-242.
5. Zhou SF. Polymorphism of human cytochrome P450 2D6 and its clinical significance: part II. Clin Pharmacokinet. 2009;48(12):761-804.
6. Cascorbi I. Pharmacogenetics of cytochrome P4502D6: genetic background and clinical implication. Eur J Clin Invest. 2003;33(suppl 2):17-22.
7. Risperdal [package insert]. Titusville, NJ: Janssen; 2010.
8. Abilify [package insert]. Tokyo, Japan: Otsuka Pharmaceutical Co.; 2009.
9. Fanapt [package insert]. Rockville, MD: Vanda Pharmaceuticals, Inc.; 2009.
10. Kirchheiner J, Rodriguez-Antona C. Cytochrome P450 2D6 genotyping: potential role in improving treatment outcomes in psychiatric disorders. CNS Drugs. 2009;23:181-191.
11. de Leon J, Susce MT, Murray-Carmichael E. The AmpliChip CYP450 genotyping test: integrating a new clinical tool. Mol Diagn Ther. 2006;10:135-151.
12. de Leon J, Armstrong SC, Cozza KL. Clinical guidelines for psychiatrists for the use of pharmacogenetic testing for CYP450 2D6 and CYP450 2C19. Psychosomatics. 2006;47:75-85.
13. Grossman I, Sullivan PF, Walley N, et al. Genetic determinants of variable metabolism have little impact on the clinical use of leading antipsychotics in the CATIE study. Genet Med. 2008;10:720-729.
14. Rodriguez-Antona C, Gurwitz D, de Leon J, et al. CYP2D6 genotyping for psychiatric patients treated with risperidone: considerations for cost-effectiveness studies. Pharmacogenomics. 2009;10:685-699.
Two months ago, Mr. P, age 20, experienced paranoid thoughts, anxiety, agitation, and auditory hallucinations. During a brief hospitalization 1 month later, he received IM haloperidol, 2 mg, which he said “made his neck stiff.” After he was discharged, Mr. P, who is White, stopped taking his antipsychotics. During a recent outpatient evaluation, the clinician gives Mr. P a working diagnosis of schizophrenia and prescribes risperidone, 2 mg/d, with plans to titrate to 4 mg/d in the next 2 weeks. However, a week later, Mr. P complains of extreme sedation and feeling “knocked out” and does not want to continue taking the medication. Physical exam reveals slight cogwheel rigidity. His delusional thought content is not improved. The treating physician considers ordering a genetic test to determine Mr. P’s cytochrome P450 (CYP) 2D6 metabolizer status.
Studies investigating relationships among genetic variants thought to impact pharmacokinetics and pharmacodynamics of psychotropic medications have had mixed results.1 Metabolism of most antipsychotics depends on the CYP450 enzyme system, which is expressed predominantly in the liver (Table 1). CYP2D6 is one of these enzymes and may be responsible for metabolizing approximately 20% to 50% of all medications, including a number of antipsychotics.2 Genetic variations of CYP2D6 are common and the frequencies of these variants differ among racial groups.3
The half-life and other pharmacokinetic parameters of an antipsychotic metabolized by CYP2D6 may differ based on whether someone is a poor metabolizer (PM), intermediate metabolizer (IM), extensive metabolizer (EM), or ultrarapid metabolizer (UM).4 Regarding CYP2D6 metabolism among Whites, 3% to 5% are UMs, 70% to 80% are EMs, 10% to 17% are IMs, and 5% to 10% are PMs.5 By contrast, the percentage of PMs and UMs in the Asian population is low—about 1% for each phenotype; the IM phenotype is more common (65% to 70% in the Chinese population).5,6 The percentage of PMs in African Americans is roughly 2% to 6%.2
- Genetic variants of CYP2D6 may result in decreased or increased metabolism of some drugs, including risperidone, iloperidone, perphenazine, haloperidol, and thioridazine.
- The effect of reduced CYP2D6 activity may increase a patient’s risk for dose-related adverse effects.
- It is currently unknown if clinical genotyping for CYP2D6 variants and using this information to guide drug selection or dosing improves patient outcomes.
The clinical effect of altered metabolizer status depends on the extent the metabolism of a given agent is dependent on CYP2D6. PM status results in an approximately 2- to 6-fold increase in elimination half-life and overall exposure of aripiprazole,7 risperidone,8 and iloperidone9 (Figure). On the other end of the spectrum are UMs. Because of gene duplication, patients who fall into this category have enhanced metabolic activity. As a result, the therapeutic effect of several medications may be decreased because of faster clearance from the body, leading some physicians to label them as treatment-resistant.
Because side effects of many antipsychotics are dose-dependent, genotyping may be valuable for patients taking agents that are primarily metabolized by CYP2D6.10 Clinicians now have access to laboratory resources and FDA-approved methods for assessing CYP2D6 gene variants.11 It is debatable, however, whether this testing—which is expensive (≥$400) and may not be covered by health insurance—improves patient outcomes. In Mr. P’s case, if he had been genotyped as a CYP2D6 PM before treatment, his physicians might not have prescribed haloperidol and could have prevented a mild dystonic reaction. Also, they could have lowered the initial risperidone dose or chosen an antipsychotic such as ziprasidone, paliperidone, or quetiapine where the pharmacokinetic consequences of 2D6 poor metabolism are not as severe. Theoretically, one may argue that this could have reduced the risk for antipsychotic-associated side effects that now are a barrier to Mr. P’s desire to continue antipsychotics. On the other hand one may also reasonably argue that there may be other/additional reasons (genetic or non-genetic) that make some patients more sensitive to the side effects of antipsychotics and that simply assessing CYP2D6 status is not enough to guide drug selection and dosing.
Table 1
Cytochrome P450 (CYP) metabolism of commonly used antipsychotics*
| Drug | CYP1A2 | CYP2C9 | CYP2C19 | CYP2D6 | CYP3A4/5 |
|---|---|---|---|---|---|
| Aripiprazole | X | X | |||
| Asenapine | X | X | X | ||
| Chlorpromazine | X | X | X | ||
| Clozapine | X | X | X | X | X |
| Fluphenazine | X | ||||
| Haloperidol | X | X | X | ||
| Iloperidone | X | X | |||
| Olanzapine | X | X | |||
| Paliperidone | X† | X† | |||
| Perphenazine | X | X | X | X | X |
| Quetiapine | X | X | |||
| Risperidone | X | X | |||
| Thioridazine | X | X | |||
| Ziprasidone | X | X | |||
| *Information obtained from the most recent prescribing information available from each drug’s manufacturer †According to paliperidone’s prescribing information, in vitro studies identify that CYP2D6 and CYP3A4 may be involved in paliperidone metabolism, but in vivo studies indicate that their role in eliminating paliperidone is minimal | |||||
Figure: Effects of CYP2D6 poor metabolizer status on the half-life of risperidone, aripiprazole, and iloperidone
EM: extensive metabolizer; PM: poor metabolizer
Source: References 7-9
Use in clinical practice
Proposed expert guidelines recommend halving the normal target dose of risperidone and avoiding haloperidol and phenothiazine antipsychotics in CYP2D6 PMs.12 These guidelines are based on expert review of the pharmacokinetic effects of CYP2D6 PM status as well as case reports and studies associating CYP2D6 with poor outcomes, usually side effects. Although these studies suggest that determining metabolizer status may be clinically important, many other studies—some very large—have not found evidence for associations between drug metabolizing enzyme variants and clinical outcomes from antipsychotics.13
There are 2 clinical scenarios in which one may consider obtaining CYP2D6 genotype information:
- before initiating treatment (Table 2)
- after trying ≥1 agent primarily dependent on CYP2D6 with evidence of dose-related side effect (Table 3).
Identifying PMs could influence drug selection and dosing if this information is available before antipsychotic exposure. Studies have found evidence that CYP2D6 PMs may be at greater risk of experiencing adverse reactions to risperidone compared with other metabolizer groups.14 Also, prescribing information for aripiprazole and iloperidone recommends halving the dose of these drugs in the presence of CYP2D6 inhibitors, a condition that pharmacokinetically mimics PM status.
Knowing genotype information after ≥1 drugs have been tried may not be as useful. Clinicians often base drug switches or dose titrations on a patient’s experience with present or past doses of the antipsychotic. Examples include slowing titrations or reducing a target dose when a patient, such as Mr. P, experiences side effects, or selecting non-2D6 substrate agents after detecting a pattern of drug sensitivity.
Table 2
CYP2D6 testing before initiating antipsychotics: Benefits vs drawbacks
| Benefits | Drawbacks |
|---|---|
| Clinicians could avoid 2D6 substrate drugs with high likelihood for ADEs or increased risk of 2D6-based interactions in PMs | No empiric evidence shows that routine genotyping produces better clinical outcomes (eg, fewer side effects and better treatment adherence) |
| May lower initial dose, slow titration, and lower initial target dose to minimize risk of side effects in PMs | Many clinicians titrate slowly or adjust titration schedule and target doses based on initial tolerability as part of routine practice |
| The test would need to be done only once and the information may be useful for other therapy decisions | Patients who need immediate drug therapy may not be able to wait for test results |
| Testing may not be covered by a patient’s health insurance | |
| ADEs: adverse drug events; PMs: poor metabolizers | |
Table 3
Genotype testing after a patient experiences side effects
| Benefits |
| Identifying a biologic reason for side effect sensitivity may aid choice and dosing of subsequent antipsychotics and other medications |
| Drawbacks |
| In clinical practice, antipsychotic switching because of tolerability (and response) often is guided by outcomes experienced from previously used agents. In general, patients with a history of experiencing side effects at lower doses of antipsychotics are likely to be initiated at lower doses and titrated more cautiously during subsequent therapy choices regardless of whether side effects were caused by metabolizer status or other factor(s) |
Better patient outcomes?
It is not known if obtaining genotype information will provide better outcomes than a “trial and error” approach. Currently, obtaining genotype information before antipsychotic treatment is not standard clinical practice. Because this testing is expensive and requires prior approval from third party payers or out-of-pocket financial resources, testing is not recommended for all patients at this time.
However, a growing body of evidence suggests that knowing metabolizer status could be useful in drug selection or dosing for antipsychotics. This scientific knowledge continues to accumulate, and CYP2D6 genotyping may some day be integrated into routine clinical care. Currently, for patients and physicians with the resources to obtain and the ability to appropriately interpret the test results, this information may prove useful on an individual basis. However, additional studies are needed to support better outcomes from dosing and drug selection based on CYP2D6 genotype information.
Related Resources
- Evaluation of Genomic Applications in Practice and Prevention (EGAPP). www.egappreviews.org.
- Pharmacogenomics Knowledge Base. www.pharmgkb.org.
- Indiana University School of Medicine. P450 drug interaction table. http://medicine.iupui.edu/clinpharm/ddis/table.asp.
Drug Brand Names
- Aripiprazole • Abilify
- Asenapine • Saphris
- Chlorpromazine • Thorazine
- Clozapine • Clozaril
- Fluphenazine • Prolixin
- Haloperidol • Haldol
- Iloperidone • Fanapt
- Olanzapine • Zyprexa
- Paliperidone • Invega
- Perphenazine • Trilafon
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Thioridazine • Mellaril
- Ziprasidone • Geodon
Disclosures
Dr. Bishop receives grant/research support from the National Institute of Mental Health, NARSAD, and Ortho-McNeil-Janssen and has received honoraria from Eli Lilly and Company.
Ms. Chae reports no financial relationship with any company whose products are mentioned in this article, or with manufacturers of competing products.
Two months ago, Mr. P, age 20, experienced paranoid thoughts, anxiety, agitation, and auditory hallucinations. During a brief hospitalization 1 month later, he received IM haloperidol, 2 mg, which he said “made his neck stiff.” After he was discharged, Mr. P, who is White, stopped taking his antipsychotics. During a recent outpatient evaluation, the clinician gives Mr. P a working diagnosis of schizophrenia and prescribes risperidone, 2 mg/d, with plans to titrate to 4 mg/d in the next 2 weeks. However, a week later, Mr. P complains of extreme sedation and feeling “knocked out” and does not want to continue taking the medication. Physical exam reveals slight cogwheel rigidity. His delusional thought content is not improved. The treating physician considers ordering a genetic test to determine Mr. P’s cytochrome P450 (CYP) 2D6 metabolizer status.
Studies investigating relationships among genetic variants thought to impact pharmacokinetics and pharmacodynamics of psychotropic medications have had mixed results.1 Metabolism of most antipsychotics depends on the CYP450 enzyme system, which is expressed predominantly in the liver (Table 1). CYP2D6 is one of these enzymes and may be responsible for metabolizing approximately 20% to 50% of all medications, including a number of antipsychotics.2 Genetic variations of CYP2D6 are common and the frequencies of these variants differ among racial groups.3
The half-life and other pharmacokinetic parameters of an antipsychotic metabolized by CYP2D6 may differ based on whether someone is a poor metabolizer (PM), intermediate metabolizer (IM), extensive metabolizer (EM), or ultrarapid metabolizer (UM).4 Regarding CYP2D6 metabolism among Whites, 3% to 5% are UMs, 70% to 80% are EMs, 10% to 17% are IMs, and 5% to 10% are PMs.5 By contrast, the percentage of PMs and UMs in the Asian population is low—about 1% for each phenotype; the IM phenotype is more common (65% to 70% in the Chinese population).5,6 The percentage of PMs in African Americans is roughly 2% to 6%.2
- Genetic variants of CYP2D6 may result in decreased or increased metabolism of some drugs, including risperidone, iloperidone, perphenazine, haloperidol, and thioridazine.
- The effect of reduced CYP2D6 activity may increase a patient’s risk for dose-related adverse effects.
- It is currently unknown if clinical genotyping for CYP2D6 variants and using this information to guide drug selection or dosing improves patient outcomes.
The clinical effect of altered metabolizer status depends on the extent the metabolism of a given agent is dependent on CYP2D6. PM status results in an approximately 2- to 6-fold increase in elimination half-life and overall exposure of aripiprazole,7 risperidone,8 and iloperidone9 (Figure). On the other end of the spectrum are UMs. Because of gene duplication, patients who fall into this category have enhanced metabolic activity. As a result, the therapeutic effect of several medications may be decreased because of faster clearance from the body, leading some physicians to label them as treatment-resistant.
Because side effects of many antipsychotics are dose-dependent, genotyping may be valuable for patients taking agents that are primarily metabolized by CYP2D6.10 Clinicians now have access to laboratory resources and FDA-approved methods for assessing CYP2D6 gene variants.11 It is debatable, however, whether this testing—which is expensive (≥$400) and may not be covered by health insurance—improves patient outcomes. In Mr. P’s case, if he had been genotyped as a CYP2D6 PM before treatment, his physicians might not have prescribed haloperidol and could have prevented a mild dystonic reaction. Also, they could have lowered the initial risperidone dose or chosen an antipsychotic such as ziprasidone, paliperidone, or quetiapine where the pharmacokinetic consequences of 2D6 poor metabolism are not as severe. Theoretically, one may argue that this could have reduced the risk for antipsychotic-associated side effects that now are a barrier to Mr. P’s desire to continue antipsychotics. On the other hand one may also reasonably argue that there may be other/additional reasons (genetic or non-genetic) that make some patients more sensitive to the side effects of antipsychotics and that simply assessing CYP2D6 status is not enough to guide drug selection and dosing.
Table 1
Cytochrome P450 (CYP) metabolism of commonly used antipsychotics*
| Drug | CYP1A2 | CYP2C9 | CYP2C19 | CYP2D6 | CYP3A4/5 |
|---|---|---|---|---|---|
| Aripiprazole | X | X | |||
| Asenapine | X | X | X | ||
| Chlorpromazine | X | X | X | ||
| Clozapine | X | X | X | X | X |
| Fluphenazine | X | ||||
| Haloperidol | X | X | X | ||
| Iloperidone | X | X | |||
| Olanzapine | X | X | |||
| Paliperidone | X† | X† | |||
| Perphenazine | X | X | X | X | X |
| Quetiapine | X | X | |||
| Risperidone | X | X | |||
| Thioridazine | X | X | |||
| Ziprasidone | X | X | |||
| *Information obtained from the most recent prescribing information available from each drug’s manufacturer †According to paliperidone’s prescribing information, in vitro studies identify that CYP2D6 and CYP3A4 may be involved in paliperidone metabolism, but in vivo studies indicate that their role in eliminating paliperidone is minimal | |||||
Figure: Effects of CYP2D6 poor metabolizer status on the half-life of risperidone, aripiprazole, and iloperidone
EM: extensive metabolizer; PM: poor metabolizer
Source: References 7-9
Use in clinical practice
Proposed expert guidelines recommend halving the normal target dose of risperidone and avoiding haloperidol and phenothiazine antipsychotics in CYP2D6 PMs.12 These guidelines are based on expert review of the pharmacokinetic effects of CYP2D6 PM status as well as case reports and studies associating CYP2D6 with poor outcomes, usually side effects. Although these studies suggest that determining metabolizer status may be clinically important, many other studies—some very large—have not found evidence for associations between drug metabolizing enzyme variants and clinical outcomes from antipsychotics.13
There are 2 clinical scenarios in which one may consider obtaining CYP2D6 genotype information:
- before initiating treatment (Table 2)
- after trying ≥1 agent primarily dependent on CYP2D6 with evidence of dose-related side effect (Table 3).
Identifying PMs could influence drug selection and dosing if this information is available before antipsychotic exposure. Studies have found evidence that CYP2D6 PMs may be at greater risk of experiencing adverse reactions to risperidone compared with other metabolizer groups.14 Also, prescribing information for aripiprazole and iloperidone recommends halving the dose of these drugs in the presence of CYP2D6 inhibitors, a condition that pharmacokinetically mimics PM status.
Knowing genotype information after ≥1 drugs have been tried may not be as useful. Clinicians often base drug switches or dose titrations on a patient’s experience with present or past doses of the antipsychotic. Examples include slowing titrations or reducing a target dose when a patient, such as Mr. P, experiences side effects, or selecting non-2D6 substrate agents after detecting a pattern of drug sensitivity.
Table 2
CYP2D6 testing before initiating antipsychotics: Benefits vs drawbacks
| Benefits | Drawbacks |
|---|---|
| Clinicians could avoid 2D6 substrate drugs with high likelihood for ADEs or increased risk of 2D6-based interactions in PMs | No empiric evidence shows that routine genotyping produces better clinical outcomes (eg, fewer side effects and better treatment adherence) |
| May lower initial dose, slow titration, and lower initial target dose to minimize risk of side effects in PMs | Many clinicians titrate slowly or adjust titration schedule and target doses based on initial tolerability as part of routine practice |
| The test would need to be done only once and the information may be useful for other therapy decisions | Patients who need immediate drug therapy may not be able to wait for test results |
| Testing may not be covered by a patient’s health insurance | |
| ADEs: adverse drug events; PMs: poor metabolizers | |
Table 3
Genotype testing after a patient experiences side effects
| Benefits |
| Identifying a biologic reason for side effect sensitivity may aid choice and dosing of subsequent antipsychotics and other medications |
| Drawbacks |
| In clinical practice, antipsychotic switching because of tolerability (and response) often is guided by outcomes experienced from previously used agents. In general, patients with a history of experiencing side effects at lower doses of antipsychotics are likely to be initiated at lower doses and titrated more cautiously during subsequent therapy choices regardless of whether side effects were caused by metabolizer status or other factor(s) |
Better patient outcomes?
It is not known if obtaining genotype information will provide better outcomes than a “trial and error” approach. Currently, obtaining genotype information before antipsychotic treatment is not standard clinical practice. Because this testing is expensive and requires prior approval from third party payers or out-of-pocket financial resources, testing is not recommended for all patients at this time.
However, a growing body of evidence suggests that knowing metabolizer status could be useful in drug selection or dosing for antipsychotics. This scientific knowledge continues to accumulate, and CYP2D6 genotyping may some day be integrated into routine clinical care. Currently, for patients and physicians with the resources to obtain and the ability to appropriately interpret the test results, this information may prove useful on an individual basis. However, additional studies are needed to support better outcomes from dosing and drug selection based on CYP2D6 genotype information.
Related Resources
- Evaluation of Genomic Applications in Practice and Prevention (EGAPP). www.egappreviews.org.
- Pharmacogenomics Knowledge Base. www.pharmgkb.org.
- Indiana University School of Medicine. P450 drug interaction table. http://medicine.iupui.edu/clinpharm/ddis/table.asp.
Drug Brand Names
- Aripiprazole • Abilify
- Asenapine • Saphris
- Chlorpromazine • Thorazine
- Clozapine • Clozaril
- Fluphenazine • Prolixin
- Haloperidol • Haldol
- Iloperidone • Fanapt
- Olanzapine • Zyprexa
- Paliperidone • Invega
- Perphenazine • Trilafon
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Thioridazine • Mellaril
- Ziprasidone • Geodon
Disclosures
Dr. Bishop receives grant/research support from the National Institute of Mental Health, NARSAD, and Ortho-McNeil-Janssen and has received honoraria from Eli Lilly and Company.
Ms. Chae reports no financial relationship with any company whose products are mentioned in this article, or with manufacturers of competing products.
1. Leckband SG, Bishop JR, Ellingrod VL. Pharmacogenomics in psychiatry. J Pharm Pract. 2007;20:252-264.
2. Neafsey P, Ginsberg G, Hattis D, et al. Genetic polymorphism in cytochrome P450 2D6 (CYP2D6): population distribution of CYP2D6 activity. J Toxicol Environ Health B Crit Rev. 2009;12(5-6):334-361.
3. Bradford LD, Gaedigk A, Leeder JS. High frequency of CYP2D6 poor and “intermediate” metabolizers in black populations: a review and preliminary data. Psychopharmacol Bull. 1998;34:797-804.
4. Gaedigk A, Simon SD, Pearce RE, et al. The CYP2D6 activity score: translating genotype information into a qualitative measure of phenotype. Clin Pharmacol Ther. 2008;83:234-242.
5. Zhou SF. Polymorphism of human cytochrome P450 2D6 and its clinical significance: part II. Clin Pharmacokinet. 2009;48(12):761-804.
6. Cascorbi I. Pharmacogenetics of cytochrome P4502D6: genetic background and clinical implication. Eur J Clin Invest. 2003;33(suppl 2):17-22.
7. Risperdal [package insert]. Titusville, NJ: Janssen; 2010.
8. Abilify [package insert]. Tokyo, Japan: Otsuka Pharmaceutical Co.; 2009.
9. Fanapt [package insert]. Rockville, MD: Vanda Pharmaceuticals, Inc.; 2009.
10. Kirchheiner J, Rodriguez-Antona C. Cytochrome P450 2D6 genotyping: potential role in improving treatment outcomes in psychiatric disorders. CNS Drugs. 2009;23:181-191.
11. de Leon J, Susce MT, Murray-Carmichael E. The AmpliChip CYP450 genotyping test: integrating a new clinical tool. Mol Diagn Ther. 2006;10:135-151.
12. de Leon J, Armstrong SC, Cozza KL. Clinical guidelines for psychiatrists for the use of pharmacogenetic testing for CYP450 2D6 and CYP450 2C19. Psychosomatics. 2006;47:75-85.
13. Grossman I, Sullivan PF, Walley N, et al. Genetic determinants of variable metabolism have little impact on the clinical use of leading antipsychotics in the CATIE study. Genet Med. 2008;10:720-729.
14. Rodriguez-Antona C, Gurwitz D, de Leon J, et al. CYP2D6 genotyping for psychiatric patients treated with risperidone: considerations for cost-effectiveness studies. Pharmacogenomics. 2009;10:685-699.
1. Leckband SG, Bishop JR, Ellingrod VL. Pharmacogenomics in psychiatry. J Pharm Pract. 2007;20:252-264.
2. Neafsey P, Ginsberg G, Hattis D, et al. Genetic polymorphism in cytochrome P450 2D6 (CYP2D6): population distribution of CYP2D6 activity. J Toxicol Environ Health B Crit Rev. 2009;12(5-6):334-361.
3. Bradford LD, Gaedigk A, Leeder JS. High frequency of CYP2D6 poor and “intermediate” metabolizers in black populations: a review and preliminary data. Psychopharmacol Bull. 1998;34:797-804.
4. Gaedigk A, Simon SD, Pearce RE, et al. The CYP2D6 activity score: translating genotype information into a qualitative measure of phenotype. Clin Pharmacol Ther. 2008;83:234-242.
5. Zhou SF. Polymorphism of human cytochrome P450 2D6 and its clinical significance: part II. Clin Pharmacokinet. 2009;48(12):761-804.
6. Cascorbi I. Pharmacogenetics of cytochrome P4502D6: genetic background and clinical implication. Eur J Clin Invest. 2003;33(suppl 2):17-22.
7. Risperdal [package insert]. Titusville, NJ: Janssen; 2010.
8. Abilify [package insert]. Tokyo, Japan: Otsuka Pharmaceutical Co.; 2009.
9. Fanapt [package insert]. Rockville, MD: Vanda Pharmaceuticals, Inc.; 2009.
10. Kirchheiner J, Rodriguez-Antona C. Cytochrome P450 2D6 genotyping: potential role in improving treatment outcomes in psychiatric disorders. CNS Drugs. 2009;23:181-191.
11. de Leon J, Susce MT, Murray-Carmichael E. The AmpliChip CYP450 genotyping test: integrating a new clinical tool. Mol Diagn Ther. 2006;10:135-151.
12. de Leon J, Armstrong SC, Cozza KL. Clinical guidelines for psychiatrists for the use of pharmacogenetic testing for CYP450 2D6 and CYP450 2C19. Psychosomatics. 2006;47:75-85.
13. Grossman I, Sullivan PF, Walley N, et al. Genetic determinants of variable metabolism have little impact on the clinical use of leading antipsychotics in the CATIE study. Genet Med. 2008;10:720-729.
14. Rodriguez-Antona C, Gurwitz D, de Leon J, et al. CYP2D6 genotyping for psychiatric patients treated with risperidone: considerations for cost-effectiveness studies. Pharmacogenomics. 2009;10:685-699.