User login
James J. Stevermer is in the Department of Family and Community Medicine at the University of Missouri–Columbia.
A-fib and rate control: Don’t go too low
Aim for a heart rate of <110 beats per minute (bpm) in patients with permanent atrial fibrillation. Maintaining this rate requires less medication than more stringent rate control, resulting in fewer side effects and no increased risk of cardiovascular events.1
STRENGTH OF RECOMMENDATION
B: Based on 1 long-term randomized controlled trial (RCT).
Van Gelder IC, Groenveld HF, Crijns HJ, et al. Lenient versus strict rate control in patients with atrial fibrillation. N Engl J Med. 2010;362: 1363-1373.
Illustrative case
A 67-year-old man comes in for a follow-up visit after being hospitalized for atrial fibrillation with a rapid ventricular rate. Before being discharged, he was put on warfarin and metoprolol, and his heart rate today is 96 bpm. You consider increasing the dose of his beta-blocker. What should his target heart rate be?
Atrial fibrillation, the most common sustained arrhythmia,2 can lead to life-threatening events such as heart failure and stroke. Studies, including the Atrial Fibrillation Follow-Up Investigation of Rhythm Management (AFFIRM) and Rate Control versus Electrical Cardioversion (RACE) trials, have found no difference in morbidity or mortality between rate control and rhythm control strategies.2,3 Thus, rate control is usually preferred for patients with atrial fibrillation because of adverse effects associated with antiarrhythmic drugs.
Guidelines cite stringent targets
The American College of Cardiology/American Heart Association Task Force/European Society of Cardiology (ACC/AHA/ESC) guidelines make no definite recommendations about heart rate targets. The guidelines do indicate, however, that rate control criteria vary based on age, “but usually involve achieving ventricular rates between 60 and 80 [bpm] at rest and between 90 and 115 [bpm] during moderate exercise.”4
This guidance is based on data from epidemiologic studies suggesting that faster heart rates in sinus rhythm may increase mortality from cardiovascular causes.5 However, strict control often requires higher doses of rate-controlling medications, which can lead to adverse events such as symptomatic bradycardia, dizziness, and syncope, as well as pacemaker implantation.
Pooled data suggest a more relaxed rate is better
A retrospective analysis of pooled data from the rate-control arms of the AFFIRM and RACE trials found no difference in all-cause mortality between the more stringent rate-control group in AFFIRM and the more lenient control in RACE.6 This finding suggested that more lenient heart rate targets may be preferred to avoid the adverse effects often associated with the higher doses of rate-controlling drugs needed to achieve strict control. The Rate Control Efficacy in Permanent Atrial Fibrillation: a Comparison between Lenient versus Strict Rate Control II (RACE II) study we report on here provides strong evidence in favor of lenient rate control.
STUDY SUMMARY: Lenient control is as effective, easier to achieve
RACE II was the first RCT to directly compare lenient rate control (resting heart rate <110 bpm) with strict rate control (resting heart rate <80 bpm, and <110 bpm during moderate exercise). This prospective, multi-center study in Holland randomized patients with permanent atrial fibrillation (N=614) to either a lenient or strict rate-control group. Eligibility criteria were (1) permanent atrial fibrillation for up to 12 months; (2) ≤80 years of age (3) mean resting heart rate >80 bpm; and (4) current use of oral anticoagulation therapy (or aspirin, in the absence of risk factors for thromboembolic complications).
Patients received various doses of beta-blockers, nondihydropyridine calcium-channel blockers, or digoxin, singly or in combination as needed to reach the target heart rate. In both groups, the resting heart rate was determined by 12-lead electrocardiogram after the patient remained in a supine position for 2 to 3 minutes. In the strict-control group, heart rate was also measured during moderate exercise on a stationary bicycle after the resting rate goal had been achieved. In addition, patients in the strict-control group wore a Holter monitor for 24 hours to check for bradycardia.
Participants in both groups were seen every 2 weeks until their heart rate goals were achieved, with follow-up at 1, 2, and 3 years. The primary composite outcome included death from cardiovascular causes; hospitalization for heart failure, stroke, systemic embolism, major bleeding, or life-threatening adverse effects of rate-control drugs; arrhythmic events, including sustained ventricular tachycardia, syncope, or cardiac arrest; and implantation of a pacemaker or cardioverter-defibrillator.
At the end of 3 years, the estimated cumulative incidence of the primary outcome was 12.9% in the lenient-control group vs 14.9% in the strict-control group. The absolute difference was -2.0 (90% confidence interval [CI], -7.6 to 3.5); a 90% CI was acceptable because the study only tested whether lenient control was worse than strict control. The frequency of reported symptoms and adverse events was similar between the 2 groups, but the lenient-control group had fewer visits for rate control (75 vs 684; P<.001), required fewer medications, and took lower doses of some medications.
Heart rate targets were met in 97.7% of patients in the lenient-control group, compared with 67% in the strict-control group (P<.001). Of those not meeting the strict control targets, 25% were due to an adverse medication event. There were no differences between the 2 groups in symptoms or in New York Heart Association functional class status.
WHAT'S NEW: Now we know: It doesn’t pay to go too low
A heart rate <80 at rest and <110 during exercise is difficult to maintain. This more stringent target often requires high dosages of drugs and/or multiple medications, which may lead to adverse effects. This RCT—the first to compare outcomes in patients with lenient vs strict heart rate control—found that morbidity and mortality were similar between the 2 groups. This means that, in many cases, patients will need less medication—leading to a reduction in risk of side effects and interactions.
CAVEATS: Unblinded study excluded very old, high risk
This was not a blinded study, so both patients and providers knew the target heart rates. However, the major outcomes were determined with relative objectivity and were not different between the 2 groups, so it is unlikely that this knowledge would have a major effect on the results. Nonetheless, this is a single study, and the findings are not yet supported by other large, prospective studies.
The researchers did not enroll patients >80 years, who have a higher incidence of atrial fibrillation and are less likely than younger patients to tolerate higher doses of rate-controlling medications. Also excluded were sedentary patients and those with a history of stroke, which resulted in a lower-risk study population. However, 40% of the subjects had a CHADS score ≥2 (an indication of high risk of stroke in patients with atrial fibrillation), and subgroup analysis found that the results applied to higher-risk groups.
Finally, it is possible that it may take longer than 3 years (the duration of study follow-up) for higher ventricular rates to result in adverse cardiovascular outcomes and that there could be a benefit of strict rate control over a longer period of time.
CHALLENGES TO IMPLEMENTATION: Guidelines do not reflect these findings
These findings are not yet incorporated into the ACC/AHA/ESC guidelines or those issued by other organizations. Clinical inertia may stop some physicians from reducing medications for patients with atrial fibrillation, but in general, both doctors and patients should welcome an easing of the drug burden.
Click here to view PURL METHODOLOGY
1. Van Gelder IC, Groenveld HF, Crijns HJ, et al. Lenient versus strict rate control in patients with atrial fibrillation. N Engl J Med. 2010;362:1363-1373.
2. Wyse DG, Waldo AL, DiMarco JP, et al. A comparison of rate control and rhythm control in patients with atrial fibrillation. N Engl J Med. 2002;347:1825-1833.
3. Hagens VE, Ranchor AV, Van SE, et al. Effect of rate or rhythm control on quality of life in persistent atrial fibrillation. Results from the Rate Control Versus Electrical Cardioversion (RACE) Study. J Am Coll Cardiol. 2004;43:241-247.
4. Fuster V, Ryden LE, Cannom DS, et al. ACC/AHA/ESC 2006 Guidelines for the Management of Patients with Atrial Fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Revise the 2001 Guidelines for the Management of Patients With Atrial Fibrillation): developed in collaboration with the European Heart Rhythm Association and the Heart Rhythm Society. Circulation. 2006;114:e257-e354.
5. Dorian P. Rate control in atrial fibrillation. N Engl J Med. 2010;362:1439-1441.
6. Van Gelder IC, Wyse DG, Chandler ML, et al. Does intensity of rate-control influence outcome in atrial fibrillation? An analysis of pooled data from the RACE and AFFIRM studies. Europace. 2006;8:935-942.
Aim for a heart rate of <110 beats per minute (bpm) in patients with permanent atrial fibrillation. Maintaining this rate requires less medication than more stringent rate control, resulting in fewer side effects and no increased risk of cardiovascular events.1
STRENGTH OF RECOMMENDATION
B: Based on 1 long-term randomized controlled trial (RCT).
Van Gelder IC, Groenveld HF, Crijns HJ, et al. Lenient versus strict rate control in patients with atrial fibrillation. N Engl J Med. 2010;362: 1363-1373.
Illustrative case
A 67-year-old man comes in for a follow-up visit after being hospitalized for atrial fibrillation with a rapid ventricular rate. Before being discharged, he was put on warfarin and metoprolol, and his heart rate today is 96 bpm. You consider increasing the dose of his beta-blocker. What should his target heart rate be?
Atrial fibrillation, the most common sustained arrhythmia,2 can lead to life-threatening events such as heart failure and stroke. Studies, including the Atrial Fibrillation Follow-Up Investigation of Rhythm Management (AFFIRM) and Rate Control versus Electrical Cardioversion (RACE) trials, have found no difference in morbidity or mortality between rate control and rhythm control strategies.2,3 Thus, rate control is usually preferred for patients with atrial fibrillation because of adverse effects associated with antiarrhythmic drugs.
Guidelines cite stringent targets
The American College of Cardiology/American Heart Association Task Force/European Society of Cardiology (ACC/AHA/ESC) guidelines make no definite recommendations about heart rate targets. The guidelines do indicate, however, that rate control criteria vary based on age, “but usually involve achieving ventricular rates between 60 and 80 [bpm] at rest and between 90 and 115 [bpm] during moderate exercise.”4
This guidance is based on data from epidemiologic studies suggesting that faster heart rates in sinus rhythm may increase mortality from cardiovascular causes.5 However, strict control often requires higher doses of rate-controlling medications, which can lead to adverse events such as symptomatic bradycardia, dizziness, and syncope, as well as pacemaker implantation.
Pooled data suggest a more relaxed rate is better
A retrospective analysis of pooled data from the rate-control arms of the AFFIRM and RACE trials found no difference in all-cause mortality between the more stringent rate-control group in AFFIRM and the more lenient control in RACE.6 This finding suggested that more lenient heart rate targets may be preferred to avoid the adverse effects often associated with the higher doses of rate-controlling drugs needed to achieve strict control. The Rate Control Efficacy in Permanent Atrial Fibrillation: a Comparison between Lenient versus Strict Rate Control II (RACE II) study we report on here provides strong evidence in favor of lenient rate control.
STUDY SUMMARY: Lenient control is as effective, easier to achieve
RACE II was the first RCT to directly compare lenient rate control (resting heart rate <110 bpm) with strict rate control (resting heart rate <80 bpm, and <110 bpm during moderate exercise). This prospective, multi-center study in Holland randomized patients with permanent atrial fibrillation (N=614) to either a lenient or strict rate-control group. Eligibility criteria were (1) permanent atrial fibrillation for up to 12 months; (2) ≤80 years of age (3) mean resting heart rate >80 bpm; and (4) current use of oral anticoagulation therapy (or aspirin, in the absence of risk factors for thromboembolic complications).
Patients received various doses of beta-blockers, nondihydropyridine calcium-channel blockers, or digoxin, singly or in combination as needed to reach the target heart rate. In both groups, the resting heart rate was determined by 12-lead electrocardiogram after the patient remained in a supine position for 2 to 3 minutes. In the strict-control group, heart rate was also measured during moderate exercise on a stationary bicycle after the resting rate goal had been achieved. In addition, patients in the strict-control group wore a Holter monitor for 24 hours to check for bradycardia.
Participants in both groups were seen every 2 weeks until their heart rate goals were achieved, with follow-up at 1, 2, and 3 years. The primary composite outcome included death from cardiovascular causes; hospitalization for heart failure, stroke, systemic embolism, major bleeding, or life-threatening adverse effects of rate-control drugs; arrhythmic events, including sustained ventricular tachycardia, syncope, or cardiac arrest; and implantation of a pacemaker or cardioverter-defibrillator.
At the end of 3 years, the estimated cumulative incidence of the primary outcome was 12.9% in the lenient-control group vs 14.9% in the strict-control group. The absolute difference was -2.0 (90% confidence interval [CI], -7.6 to 3.5); a 90% CI was acceptable because the study only tested whether lenient control was worse than strict control. The frequency of reported symptoms and adverse events was similar between the 2 groups, but the lenient-control group had fewer visits for rate control (75 vs 684; P<.001), required fewer medications, and took lower doses of some medications.
Heart rate targets were met in 97.7% of patients in the lenient-control group, compared with 67% in the strict-control group (P<.001). Of those not meeting the strict control targets, 25% were due to an adverse medication event. There were no differences between the 2 groups in symptoms or in New York Heart Association functional class status.
WHAT'S NEW: Now we know: It doesn’t pay to go too low
A heart rate <80 at rest and <110 during exercise is difficult to maintain. This more stringent target often requires high dosages of drugs and/or multiple medications, which may lead to adverse effects. This RCT—the first to compare outcomes in patients with lenient vs strict heart rate control—found that morbidity and mortality were similar between the 2 groups. This means that, in many cases, patients will need less medication—leading to a reduction in risk of side effects and interactions.
CAVEATS: Unblinded study excluded very old, high risk
This was not a blinded study, so both patients and providers knew the target heart rates. However, the major outcomes were determined with relative objectivity and were not different between the 2 groups, so it is unlikely that this knowledge would have a major effect on the results. Nonetheless, this is a single study, and the findings are not yet supported by other large, prospective studies.
The researchers did not enroll patients >80 years, who have a higher incidence of atrial fibrillation and are less likely than younger patients to tolerate higher doses of rate-controlling medications. Also excluded were sedentary patients and those with a history of stroke, which resulted in a lower-risk study population. However, 40% of the subjects had a CHADS score ≥2 (an indication of high risk of stroke in patients with atrial fibrillation), and subgroup analysis found that the results applied to higher-risk groups.
Finally, it is possible that it may take longer than 3 years (the duration of study follow-up) for higher ventricular rates to result in adverse cardiovascular outcomes and that there could be a benefit of strict rate control over a longer period of time.
CHALLENGES TO IMPLEMENTATION: Guidelines do not reflect these findings
These findings are not yet incorporated into the ACC/AHA/ESC guidelines or those issued by other organizations. Clinical inertia may stop some physicians from reducing medications for patients with atrial fibrillation, but in general, both doctors and patients should welcome an easing of the drug burden.
Click here to view PURL METHODOLOGY
Aim for a heart rate of <110 beats per minute (bpm) in patients with permanent atrial fibrillation. Maintaining this rate requires less medication than more stringent rate control, resulting in fewer side effects and no increased risk of cardiovascular events.1
STRENGTH OF RECOMMENDATION
B: Based on 1 long-term randomized controlled trial (RCT).
Van Gelder IC, Groenveld HF, Crijns HJ, et al. Lenient versus strict rate control in patients with atrial fibrillation. N Engl J Med. 2010;362: 1363-1373.
Illustrative case
A 67-year-old man comes in for a follow-up visit after being hospitalized for atrial fibrillation with a rapid ventricular rate. Before being discharged, he was put on warfarin and metoprolol, and his heart rate today is 96 bpm. You consider increasing the dose of his beta-blocker. What should his target heart rate be?
Atrial fibrillation, the most common sustained arrhythmia,2 can lead to life-threatening events such as heart failure and stroke. Studies, including the Atrial Fibrillation Follow-Up Investigation of Rhythm Management (AFFIRM) and Rate Control versus Electrical Cardioversion (RACE) trials, have found no difference in morbidity or mortality between rate control and rhythm control strategies.2,3 Thus, rate control is usually preferred for patients with atrial fibrillation because of adverse effects associated with antiarrhythmic drugs.
Guidelines cite stringent targets
The American College of Cardiology/American Heart Association Task Force/European Society of Cardiology (ACC/AHA/ESC) guidelines make no definite recommendations about heart rate targets. The guidelines do indicate, however, that rate control criteria vary based on age, “but usually involve achieving ventricular rates between 60 and 80 [bpm] at rest and between 90 and 115 [bpm] during moderate exercise.”4
This guidance is based on data from epidemiologic studies suggesting that faster heart rates in sinus rhythm may increase mortality from cardiovascular causes.5 However, strict control often requires higher doses of rate-controlling medications, which can lead to adverse events such as symptomatic bradycardia, dizziness, and syncope, as well as pacemaker implantation.
Pooled data suggest a more relaxed rate is better
A retrospective analysis of pooled data from the rate-control arms of the AFFIRM and RACE trials found no difference in all-cause mortality between the more stringent rate-control group in AFFIRM and the more lenient control in RACE.6 This finding suggested that more lenient heart rate targets may be preferred to avoid the adverse effects often associated with the higher doses of rate-controlling drugs needed to achieve strict control. The Rate Control Efficacy in Permanent Atrial Fibrillation: a Comparison between Lenient versus Strict Rate Control II (RACE II) study we report on here provides strong evidence in favor of lenient rate control.
STUDY SUMMARY: Lenient control is as effective, easier to achieve
RACE II was the first RCT to directly compare lenient rate control (resting heart rate <110 bpm) with strict rate control (resting heart rate <80 bpm, and <110 bpm during moderate exercise). This prospective, multi-center study in Holland randomized patients with permanent atrial fibrillation (N=614) to either a lenient or strict rate-control group. Eligibility criteria were (1) permanent atrial fibrillation for up to 12 months; (2) ≤80 years of age (3) mean resting heart rate >80 bpm; and (4) current use of oral anticoagulation therapy (or aspirin, in the absence of risk factors for thromboembolic complications).
Patients received various doses of beta-blockers, nondihydropyridine calcium-channel blockers, or digoxin, singly or in combination as needed to reach the target heart rate. In both groups, the resting heart rate was determined by 12-lead electrocardiogram after the patient remained in a supine position for 2 to 3 minutes. In the strict-control group, heart rate was also measured during moderate exercise on a stationary bicycle after the resting rate goal had been achieved. In addition, patients in the strict-control group wore a Holter monitor for 24 hours to check for bradycardia.
Participants in both groups were seen every 2 weeks until their heart rate goals were achieved, with follow-up at 1, 2, and 3 years. The primary composite outcome included death from cardiovascular causes; hospitalization for heart failure, stroke, systemic embolism, major bleeding, or life-threatening adverse effects of rate-control drugs; arrhythmic events, including sustained ventricular tachycardia, syncope, or cardiac arrest; and implantation of a pacemaker or cardioverter-defibrillator.
At the end of 3 years, the estimated cumulative incidence of the primary outcome was 12.9% in the lenient-control group vs 14.9% in the strict-control group. The absolute difference was -2.0 (90% confidence interval [CI], -7.6 to 3.5); a 90% CI was acceptable because the study only tested whether lenient control was worse than strict control. The frequency of reported symptoms and adverse events was similar between the 2 groups, but the lenient-control group had fewer visits for rate control (75 vs 684; P<.001), required fewer medications, and took lower doses of some medications.
Heart rate targets were met in 97.7% of patients in the lenient-control group, compared with 67% in the strict-control group (P<.001). Of those not meeting the strict control targets, 25% were due to an adverse medication event. There were no differences between the 2 groups in symptoms or in New York Heart Association functional class status.
WHAT'S NEW: Now we know: It doesn’t pay to go too low
A heart rate <80 at rest and <110 during exercise is difficult to maintain. This more stringent target often requires high dosages of drugs and/or multiple medications, which may lead to adverse effects. This RCT—the first to compare outcomes in patients with lenient vs strict heart rate control—found that morbidity and mortality were similar between the 2 groups. This means that, in many cases, patients will need less medication—leading to a reduction in risk of side effects and interactions.
CAVEATS: Unblinded study excluded very old, high risk
This was not a blinded study, so both patients and providers knew the target heart rates. However, the major outcomes were determined with relative objectivity and were not different between the 2 groups, so it is unlikely that this knowledge would have a major effect on the results. Nonetheless, this is a single study, and the findings are not yet supported by other large, prospective studies.
The researchers did not enroll patients >80 years, who have a higher incidence of atrial fibrillation and are less likely than younger patients to tolerate higher doses of rate-controlling medications. Also excluded were sedentary patients and those with a history of stroke, which resulted in a lower-risk study population. However, 40% of the subjects had a CHADS score ≥2 (an indication of high risk of stroke in patients with atrial fibrillation), and subgroup analysis found that the results applied to higher-risk groups.
Finally, it is possible that it may take longer than 3 years (the duration of study follow-up) for higher ventricular rates to result in adverse cardiovascular outcomes and that there could be a benefit of strict rate control over a longer period of time.
CHALLENGES TO IMPLEMENTATION: Guidelines do not reflect these findings
These findings are not yet incorporated into the ACC/AHA/ESC guidelines or those issued by other organizations. Clinical inertia may stop some physicians from reducing medications for patients with atrial fibrillation, but in general, both doctors and patients should welcome an easing of the drug burden.
Click here to view PURL METHODOLOGY
1. Van Gelder IC, Groenveld HF, Crijns HJ, et al. Lenient versus strict rate control in patients with atrial fibrillation. N Engl J Med. 2010;362:1363-1373.
2. Wyse DG, Waldo AL, DiMarco JP, et al. A comparison of rate control and rhythm control in patients with atrial fibrillation. N Engl J Med. 2002;347:1825-1833.
3. Hagens VE, Ranchor AV, Van SE, et al. Effect of rate or rhythm control on quality of life in persistent atrial fibrillation. Results from the Rate Control Versus Electrical Cardioversion (RACE) Study. J Am Coll Cardiol. 2004;43:241-247.
4. Fuster V, Ryden LE, Cannom DS, et al. ACC/AHA/ESC 2006 Guidelines for the Management of Patients with Atrial Fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Revise the 2001 Guidelines for the Management of Patients With Atrial Fibrillation): developed in collaboration with the European Heart Rhythm Association and the Heart Rhythm Society. Circulation. 2006;114:e257-e354.
5. Dorian P. Rate control in atrial fibrillation. N Engl J Med. 2010;362:1439-1441.
6. Van Gelder IC, Wyse DG, Chandler ML, et al. Does intensity of rate-control influence outcome in atrial fibrillation? An analysis of pooled data from the RACE and AFFIRM studies. Europace. 2006;8:935-942.
1. Van Gelder IC, Groenveld HF, Crijns HJ, et al. Lenient versus strict rate control in patients with atrial fibrillation. N Engl J Med. 2010;362:1363-1373.
2. Wyse DG, Waldo AL, DiMarco JP, et al. A comparison of rate control and rhythm control in patients with atrial fibrillation. N Engl J Med. 2002;347:1825-1833.
3. Hagens VE, Ranchor AV, Van SE, et al. Effect of rate or rhythm control on quality of life in persistent atrial fibrillation. Results from the Rate Control Versus Electrical Cardioversion (RACE) Study. J Am Coll Cardiol. 2004;43:241-247.
4. Fuster V, Ryden LE, Cannom DS, et al. ACC/AHA/ESC 2006 Guidelines for the Management of Patients with Atrial Fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Revise the 2001 Guidelines for the Management of Patients With Atrial Fibrillation): developed in collaboration with the European Heart Rhythm Association and the Heart Rhythm Society. Circulation. 2006;114:e257-e354.
5. Dorian P. Rate control in atrial fibrillation. N Engl J Med. 2010;362:1439-1441.
6. Van Gelder IC, Wyse DG, Chandler ML, et al. Does intensity of rate-control influence outcome in atrial fibrillation? An analysis of pooled data from the RACE and AFFIRM studies. Europace. 2006;8:935-942.
Copyright © 2010 The Family Physicians Inquiries Network. All rights reserved.
Fracture pain relief for kids? Ibuprofen does it better
Use ibuprofen instead of acetaminophen with codeine for pediatric arm fractures. It controls the pain at least as well and is better tolerated.1-3
Strength of Recommendation
A: Based on 1 longer-term and 2 short-term randomized controlled trials (RCTs).
1. Drendel AL, Gorelick MH, Weisman SJ, et al. A randomized clinical trial of ibuprofen versus acetaminophen with codeine for acute pediatric arm fracture pain. Ann Emerg Med. 2009;54:553-560.
2. Koller DM, Myers AB, Lorenz D, et al. Effectiveness of oxycodone, ibuprofen, or the combination in the initial management of orthopedic injury-related pain in children. Pediatr Emerg Care. 2007;23:627-633.
3. Clark E, Plint AC, Correll R, et al. A randomized controlled clinical trial of acetaminophen, ibuprofen, and codeine for acute pain relief in children with musculoskeletal trauma. Pediatrics. 2007;119:460-467.
Illustrative case
A mother brings her 6-year-old son to the emergency department (ED) for treatment of forearm pain after a bicycle accident. clinical examination reveals a swollen and tender wrist. A radiograph confirms a diagnosis of a nondisplaced distal radial fracture. After proper stabilization, the little boy is discharged home, with a visit to his primary care physician scheduled for the following week. if he were your patient, what would you prescribe for outpatient analgesia?
Musculoskeletal trauma is a common pediatric presentation, in both emergency and office settings. In fact, it is estimated that by age 15, one-half to two-thirds of children will have fractured a bone.4 Physicians commonly prescribe nonsteroidal anti-inflammatory drugs (NSAIDs) and opioids—especially acetaminophen with codeine—as analgesia for children with fractures,5 but few studies have directly compared these medications in pediatric patients.
No consensus on analgesia for musculoskeletal pain in kids
Pain associated with an acute fracture is substantial, and most children who incur fractures are managed at home, and thus require effective and well-tolerated oral analgesia. However, prescribing practices vary widely, and there is no consensus regarding the first-line medication for kids with fracture.
A Cochrane review of adult postoperative pain concluded that NSAIDs are effective, and they are commonly prescribed to adult patients for various types of pain.6 Fewer studies of pain control in children exist. Before the 2009 study reported on here, there were just 2 RCTs that addressed pediatric musculoskeletal pain in patients presenting to the ED.
In single-dose studies, ibuprofen comes out ahead
The smaller of the 2 trials (N=66) compared ibuprofen alone vs ibuprofen plus oxycodone for suspected orthopedic injury. The researchers found that pain relief was equivalent, but the oxycodone group had more adverse effects.2 The larger trial (N=336) compared ibuprofen, acetaminophen, and codeine for acute pediatric musculoskeletal injuries. An hour after receiving their study drug, children in the ibuprofen group had significantly greater reduction in pain than those in either the acetaminophen group or the codeine group. They were also more likely to report adequate analgesia.3 Neither study followed patients after discharge from the ED.
STUDY SUMMARY: New RCT evaluates pain relief once patients go home
The Drendel study was a randomized, controlled, double-blind trial of outpatient analgesia for pediatric fractures.1 The investigators randomized 336 children ages 4 to 18 years with radiographically confirmed arm fractures to a suspension of either ibuprofen (10 mg/kg) or acetaminophen with codeine (1 mg/kg codeine component per dose), which are recommended dosages. They enrolled a convenience sample of children with nondisplaced fractures that did not require reduction in the ED.
Children were excluded if they weighed more than 60 kg, preferred tablets to liquid medication, sought care more than 12 hours after injury, or had developmental delays or contraindications to any study medication. Also excluded were children—or their parents—who did not speak English and those who were inaccessible by telephone for follow-up.
Study groups had similar baseline demographic and fracture characteristics, and similar pain scores. Patients and their parents were blinded to the assigned drug; all received the same discharge instructions and 2 doses of a rescue medication (the alternate study drug). The primary outcome was use of rescue medication due to failure of the assigned study drug. Secondary outcomes included decrease in pain score, functional outcomes (play, school, eating, sleeping), and satisfaction with the medication.
During the 72 hours after discharge from the ED, patients and parents filled out a standard diary recording pain and medication use. The diaries were returned by mail. Follow-up was good, with about 75% of diaries returned.
Ibuprofen users had fewer problems
Analysis of 244 diaries revealed that less rescue medication was used in the ibuprofen group, although the difference was not statistically significant (20.3% vs 31% [absolute risk reduction, 10.7%], 95% confidence interval, -0.2% to 21.6%). Decrease in mean pain score was the same in both groups. Functional status the day after the injury was better in the ibuprofen group compared with the acetaminophen/codeine group. In addition, 50.9% of patients in the acetaminophen/codeine group reported adverse events, vs 29.5% of those in the ibuprofen group (number needed to harm=4.7).
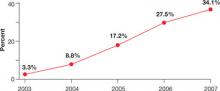
At the study’s end, children were more satisfied with ibuprofen. Only 10% of patients who took ibuprofen said they would not use it for future fractures; in comparison, 27.5% of patients in the acetaminophen/codeine group said they would not choose to use codeine again.
The authors followed participants for 1 to 4 years through orthopedic clinic records and telephone calls for any long-term adverse orthopedic outcomes. Four cases of refracture at the same site occurred (1.6%), 3 of which were in the acetaminophen/codeine group. There were no cases of nonunion.
WHAT'S NEW: Ibuprofen emerges as first-line agent for kids
Both ibuprofen and acetaminophen with codeine are commonly prescribed for outpatient pediatric analgesia, but this is the first study to compare them head-to-head for outpatient management of postfracture pain. Ibuprofen worked at least as well as acetaminophen with codeine for fracture pain control, and had fewer adverse effects. Children given ibuprofen were better able to eat and play than those given acetaminophen with codeine—an important patient-oriented functional outcome. Patients and their parents were also more satisfied when ED physicians prescribed ibuprofen. This study is consistent with short-term (single-dose) studies and confirms that ibuprofen should be the first-line agent for outpatient analgesia in this group.
CAVEATS: Study did not address NSAIDs’ effect on bone healing
In theory, ibuprofen—like other NSAIDs—can diminish the proinflammatory milieu required for bone turnover and fracture healing. Chart reviews of up to 4 years after the incident fracture found no evidence that ibuprofen delayed healing or increased rates of refracture. However, this study was neither designed nor powered to examine this outcome. Previous studies have found no conclusive evidence that short-term use of NSAIDs impairs fracture healing.7,8
Results apply only to simple fractures. Patients in this study did not require manipulation or reduction of their fracture, limiting the scope of the authors’ recommendation to simple arm fractures. More severe injury may require narcotic analgesia. One can assume, based on this and other supporting literature, that the findings extrapolate to other similarly painful pediatric musculoskeletal injuries.2
Twenty-five percent of subjects were lost to follow-up. Follow-up diaries were available from about 75% of the participants. It is possible that a clearer beneficial outcome would have been found with 1 of the analgesics studied if the response rate had been higher. Because this study is consistent with the previous ED-only studies comparing ibuprofen with acetaminophen plus codeine, however, it is unlikely that a higher response rate would find ibuprofen inferior to acetaminophen plus codeine.
CHALLENGES TO IMPLEMENTATION: Parents—or patients—may expect an Rx
Prescribing an effective, common, inexpensive, and well-tolerated oral medication should have no barriers to implementation. Still, use of an over-the-counter medication, however effective, may face resistance from patients or parents who expect “something more” for fracture pain.
Acknowledgement
The PURLs Surveillance System is supported in part by Grant Number UL1RR024999 from the National Center for Research Resources; the grant is a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
Click here to view PURL METHODOLOGY
1. Drendel AL, Gorelick MH, Weisman SJ, et al. A randomized clinical trial of ibuprofen versus acetaminophen with codeine for acute pediatric arm fracture pain. Ann Emerg Med. 2009;54:553-560.
2. Koller DM, Myers AB, Lorenz D, et al. Effectiveness of oxycodone, ibuprofen, or the combination in the initial management of orthopedic injury-related pain in children. Pediatr Emerg Care. 2007;23:627-633.
3. Clark E, Plint AC, Correll R, et al. A randomized, controlled trial of acetaminophen, ibuprofen, and codeine for acute pain relief in children with musculoskeletal trauma. Pediatrics. 2007;119:460-467.
4. Lyons RA, Delahunty AM, Kraus D, et al. Children’s fractures: a population based study. Inj Prev. 1999;5:129-132.
5. Drendel AL, Lyon R, Bergholte J, et al. Outpatient pediatric pain management practices for fractures. Pediatr Emerg Care. 2006;22:94-99.
6. Derry C, Derry S, Moore RA, et al. Single dose oral ibuprofen for acute postoperative pain in adults. Cochrane Database Syst Rev. 2009;(3):CD001548.-
7. Clarke S, Lecky F. Best evidence topic report. Do non-steroidal anti-inflammatory drugs cause a delay in fracture healing? Emerg Med J. 2005;22:652-653.
8. Wheeler P, Batt ME. Do non-steroidal anti-inflammatory drugs adversely affect stress fracture healing? A short review. Br J Sports Med. 2005;39:65-69.
Use ibuprofen instead of acetaminophen with codeine for pediatric arm fractures. It controls the pain at least as well and is better tolerated.1-3
Strength of Recommendation
A: Based on 1 longer-term and 2 short-term randomized controlled trials (RCTs).
1. Drendel AL, Gorelick MH, Weisman SJ, et al. A randomized clinical trial of ibuprofen versus acetaminophen with codeine for acute pediatric arm fracture pain. Ann Emerg Med. 2009;54:553-560.
2. Koller DM, Myers AB, Lorenz D, et al. Effectiveness of oxycodone, ibuprofen, or the combination in the initial management of orthopedic injury-related pain in children. Pediatr Emerg Care. 2007;23:627-633.
3. Clark E, Plint AC, Correll R, et al. A randomized controlled clinical trial of acetaminophen, ibuprofen, and codeine for acute pain relief in children with musculoskeletal trauma. Pediatrics. 2007;119:460-467.
Illustrative case
A mother brings her 6-year-old son to the emergency department (ED) for treatment of forearm pain after a bicycle accident. clinical examination reveals a swollen and tender wrist. A radiograph confirms a diagnosis of a nondisplaced distal radial fracture. After proper stabilization, the little boy is discharged home, with a visit to his primary care physician scheduled for the following week. if he were your patient, what would you prescribe for outpatient analgesia?
Musculoskeletal trauma is a common pediatric presentation, in both emergency and office settings. In fact, it is estimated that by age 15, one-half to two-thirds of children will have fractured a bone.4 Physicians commonly prescribe nonsteroidal anti-inflammatory drugs (NSAIDs) and opioids—especially acetaminophen with codeine—as analgesia for children with fractures,5 but few studies have directly compared these medications in pediatric patients.
No consensus on analgesia for musculoskeletal pain in kids
Pain associated with an acute fracture is substantial, and most children who incur fractures are managed at home, and thus require effective and well-tolerated oral analgesia. However, prescribing practices vary widely, and there is no consensus regarding the first-line medication for kids with fracture.
A Cochrane review of adult postoperative pain concluded that NSAIDs are effective, and they are commonly prescribed to adult patients for various types of pain.6 Fewer studies of pain control in children exist. Before the 2009 study reported on here, there were just 2 RCTs that addressed pediatric musculoskeletal pain in patients presenting to the ED.
In single-dose studies, ibuprofen comes out ahead
The smaller of the 2 trials (N=66) compared ibuprofen alone vs ibuprofen plus oxycodone for suspected orthopedic injury. The researchers found that pain relief was equivalent, but the oxycodone group had more adverse effects.2 The larger trial (N=336) compared ibuprofen, acetaminophen, and codeine for acute pediatric musculoskeletal injuries. An hour after receiving their study drug, children in the ibuprofen group had significantly greater reduction in pain than those in either the acetaminophen group or the codeine group. They were also more likely to report adequate analgesia.3 Neither study followed patients after discharge from the ED.
STUDY SUMMARY: New RCT evaluates pain relief once patients go home
The Drendel study was a randomized, controlled, double-blind trial of outpatient analgesia for pediatric fractures.1 The investigators randomized 336 children ages 4 to 18 years with radiographically confirmed arm fractures to a suspension of either ibuprofen (10 mg/kg) or acetaminophen with codeine (1 mg/kg codeine component per dose), which are recommended dosages. They enrolled a convenience sample of children with nondisplaced fractures that did not require reduction in the ED.
Children were excluded if they weighed more than 60 kg, preferred tablets to liquid medication, sought care more than 12 hours after injury, or had developmental delays or contraindications to any study medication. Also excluded were children—or their parents—who did not speak English and those who were inaccessible by telephone for follow-up.
Study groups had similar baseline demographic and fracture characteristics, and similar pain scores. Patients and their parents were blinded to the assigned drug; all received the same discharge instructions and 2 doses of a rescue medication (the alternate study drug). The primary outcome was use of rescue medication due to failure of the assigned study drug. Secondary outcomes included decrease in pain score, functional outcomes (play, school, eating, sleeping), and satisfaction with the medication.
During the 72 hours after discharge from the ED, patients and parents filled out a standard diary recording pain and medication use. The diaries were returned by mail. Follow-up was good, with about 75% of diaries returned.
Ibuprofen users had fewer problems
Analysis of 244 diaries revealed that less rescue medication was used in the ibuprofen group, although the difference was not statistically significant (20.3% vs 31% [absolute risk reduction, 10.7%], 95% confidence interval, -0.2% to 21.6%). Decrease in mean pain score was the same in both groups. Functional status the day after the injury was better in the ibuprofen group compared with the acetaminophen/codeine group. In addition, 50.9% of patients in the acetaminophen/codeine group reported adverse events, vs 29.5% of those in the ibuprofen group (number needed to harm=4.7).
At the study’s end, children were more satisfied with ibuprofen. Only 10% of patients who took ibuprofen said they would not use it for future fractures; in comparison, 27.5% of patients in the acetaminophen/codeine group said they would not choose to use codeine again.
The authors followed participants for 1 to 4 years through orthopedic clinic records and telephone calls for any long-term adverse orthopedic outcomes. Four cases of refracture at the same site occurred (1.6%), 3 of which were in the acetaminophen/codeine group. There were no cases of nonunion.
WHAT'S NEW: Ibuprofen emerges as first-line agent for kids
Both ibuprofen and acetaminophen with codeine are commonly prescribed for outpatient pediatric analgesia, but this is the first study to compare them head-to-head for outpatient management of postfracture pain. Ibuprofen worked at least as well as acetaminophen with codeine for fracture pain control, and had fewer adverse effects. Children given ibuprofen were better able to eat and play than those given acetaminophen with codeine—an important patient-oriented functional outcome. Patients and their parents were also more satisfied when ED physicians prescribed ibuprofen. This study is consistent with short-term (single-dose) studies and confirms that ibuprofen should be the first-line agent for outpatient analgesia in this group.
CAVEATS: Study did not address NSAIDs’ effect on bone healing
In theory, ibuprofen—like other NSAIDs—can diminish the proinflammatory milieu required for bone turnover and fracture healing. Chart reviews of up to 4 years after the incident fracture found no evidence that ibuprofen delayed healing or increased rates of refracture. However, this study was neither designed nor powered to examine this outcome. Previous studies have found no conclusive evidence that short-term use of NSAIDs impairs fracture healing.7,8
Results apply only to simple fractures. Patients in this study did not require manipulation or reduction of their fracture, limiting the scope of the authors’ recommendation to simple arm fractures. More severe injury may require narcotic analgesia. One can assume, based on this and other supporting literature, that the findings extrapolate to other similarly painful pediatric musculoskeletal injuries.2
Twenty-five percent of subjects were lost to follow-up. Follow-up diaries were available from about 75% of the participants. It is possible that a clearer beneficial outcome would have been found with 1 of the analgesics studied if the response rate had been higher. Because this study is consistent with the previous ED-only studies comparing ibuprofen with acetaminophen plus codeine, however, it is unlikely that a higher response rate would find ibuprofen inferior to acetaminophen plus codeine.
CHALLENGES TO IMPLEMENTATION: Parents—or patients—may expect an Rx
Prescribing an effective, common, inexpensive, and well-tolerated oral medication should have no barriers to implementation. Still, use of an over-the-counter medication, however effective, may face resistance from patients or parents who expect “something more” for fracture pain.
Acknowledgement
The PURLs Surveillance System is supported in part by Grant Number UL1RR024999 from the National Center for Research Resources; the grant is a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
Click here to view PURL METHODOLOGY
Use ibuprofen instead of acetaminophen with codeine for pediatric arm fractures. It controls the pain at least as well and is better tolerated.1-3
Strength of Recommendation
A: Based on 1 longer-term and 2 short-term randomized controlled trials (RCTs).
1. Drendel AL, Gorelick MH, Weisman SJ, et al. A randomized clinical trial of ibuprofen versus acetaminophen with codeine for acute pediatric arm fracture pain. Ann Emerg Med. 2009;54:553-560.
2. Koller DM, Myers AB, Lorenz D, et al. Effectiveness of oxycodone, ibuprofen, or the combination in the initial management of orthopedic injury-related pain in children. Pediatr Emerg Care. 2007;23:627-633.
3. Clark E, Plint AC, Correll R, et al. A randomized controlled clinical trial of acetaminophen, ibuprofen, and codeine for acute pain relief in children with musculoskeletal trauma. Pediatrics. 2007;119:460-467.
Illustrative case
A mother brings her 6-year-old son to the emergency department (ED) for treatment of forearm pain after a bicycle accident. clinical examination reveals a swollen and tender wrist. A radiograph confirms a diagnosis of a nondisplaced distal radial fracture. After proper stabilization, the little boy is discharged home, with a visit to his primary care physician scheduled for the following week. if he were your patient, what would you prescribe for outpatient analgesia?
Musculoskeletal trauma is a common pediatric presentation, in both emergency and office settings. In fact, it is estimated that by age 15, one-half to two-thirds of children will have fractured a bone.4 Physicians commonly prescribe nonsteroidal anti-inflammatory drugs (NSAIDs) and opioids—especially acetaminophen with codeine—as analgesia for children with fractures,5 but few studies have directly compared these medications in pediatric patients.
No consensus on analgesia for musculoskeletal pain in kids
Pain associated with an acute fracture is substantial, and most children who incur fractures are managed at home, and thus require effective and well-tolerated oral analgesia. However, prescribing practices vary widely, and there is no consensus regarding the first-line medication for kids with fracture.
A Cochrane review of adult postoperative pain concluded that NSAIDs are effective, and they are commonly prescribed to adult patients for various types of pain.6 Fewer studies of pain control in children exist. Before the 2009 study reported on here, there were just 2 RCTs that addressed pediatric musculoskeletal pain in patients presenting to the ED.
In single-dose studies, ibuprofen comes out ahead
The smaller of the 2 trials (N=66) compared ibuprofen alone vs ibuprofen plus oxycodone for suspected orthopedic injury. The researchers found that pain relief was equivalent, but the oxycodone group had more adverse effects.2 The larger trial (N=336) compared ibuprofen, acetaminophen, and codeine for acute pediatric musculoskeletal injuries. An hour after receiving their study drug, children in the ibuprofen group had significantly greater reduction in pain than those in either the acetaminophen group or the codeine group. They were also more likely to report adequate analgesia.3 Neither study followed patients after discharge from the ED.
STUDY SUMMARY: New RCT evaluates pain relief once patients go home
The Drendel study was a randomized, controlled, double-blind trial of outpatient analgesia for pediatric fractures.1 The investigators randomized 336 children ages 4 to 18 years with radiographically confirmed arm fractures to a suspension of either ibuprofen (10 mg/kg) or acetaminophen with codeine (1 mg/kg codeine component per dose), which are recommended dosages. They enrolled a convenience sample of children with nondisplaced fractures that did not require reduction in the ED.
Children were excluded if they weighed more than 60 kg, preferred tablets to liquid medication, sought care more than 12 hours after injury, or had developmental delays or contraindications to any study medication. Also excluded were children—or their parents—who did not speak English and those who were inaccessible by telephone for follow-up.
Study groups had similar baseline demographic and fracture characteristics, and similar pain scores. Patients and their parents were blinded to the assigned drug; all received the same discharge instructions and 2 doses of a rescue medication (the alternate study drug). The primary outcome was use of rescue medication due to failure of the assigned study drug. Secondary outcomes included decrease in pain score, functional outcomes (play, school, eating, sleeping), and satisfaction with the medication.
During the 72 hours after discharge from the ED, patients and parents filled out a standard diary recording pain and medication use. The diaries were returned by mail. Follow-up was good, with about 75% of diaries returned.
Ibuprofen users had fewer problems
Analysis of 244 diaries revealed that less rescue medication was used in the ibuprofen group, although the difference was not statistically significant (20.3% vs 31% [absolute risk reduction, 10.7%], 95% confidence interval, -0.2% to 21.6%). Decrease in mean pain score was the same in both groups. Functional status the day after the injury was better in the ibuprofen group compared with the acetaminophen/codeine group. In addition, 50.9% of patients in the acetaminophen/codeine group reported adverse events, vs 29.5% of those in the ibuprofen group (number needed to harm=4.7).
At the study’s end, children were more satisfied with ibuprofen. Only 10% of patients who took ibuprofen said they would not use it for future fractures; in comparison, 27.5% of patients in the acetaminophen/codeine group said they would not choose to use codeine again.
The authors followed participants for 1 to 4 years through orthopedic clinic records and telephone calls for any long-term adverse orthopedic outcomes. Four cases of refracture at the same site occurred (1.6%), 3 of which were in the acetaminophen/codeine group. There were no cases of nonunion.
WHAT'S NEW: Ibuprofen emerges as first-line agent for kids
Both ibuprofen and acetaminophen with codeine are commonly prescribed for outpatient pediatric analgesia, but this is the first study to compare them head-to-head for outpatient management of postfracture pain. Ibuprofen worked at least as well as acetaminophen with codeine for fracture pain control, and had fewer adverse effects. Children given ibuprofen were better able to eat and play than those given acetaminophen with codeine—an important patient-oriented functional outcome. Patients and their parents were also more satisfied when ED physicians prescribed ibuprofen. This study is consistent with short-term (single-dose) studies and confirms that ibuprofen should be the first-line agent for outpatient analgesia in this group.
CAVEATS: Study did not address NSAIDs’ effect on bone healing
In theory, ibuprofen—like other NSAIDs—can diminish the proinflammatory milieu required for bone turnover and fracture healing. Chart reviews of up to 4 years after the incident fracture found no evidence that ibuprofen delayed healing or increased rates of refracture. However, this study was neither designed nor powered to examine this outcome. Previous studies have found no conclusive evidence that short-term use of NSAIDs impairs fracture healing.7,8
Results apply only to simple fractures. Patients in this study did not require manipulation or reduction of their fracture, limiting the scope of the authors’ recommendation to simple arm fractures. More severe injury may require narcotic analgesia. One can assume, based on this and other supporting literature, that the findings extrapolate to other similarly painful pediatric musculoskeletal injuries.2
Twenty-five percent of subjects were lost to follow-up. Follow-up diaries were available from about 75% of the participants. It is possible that a clearer beneficial outcome would have been found with 1 of the analgesics studied if the response rate had been higher. Because this study is consistent with the previous ED-only studies comparing ibuprofen with acetaminophen plus codeine, however, it is unlikely that a higher response rate would find ibuprofen inferior to acetaminophen plus codeine.
CHALLENGES TO IMPLEMENTATION: Parents—or patients—may expect an Rx
Prescribing an effective, common, inexpensive, and well-tolerated oral medication should have no barriers to implementation. Still, use of an over-the-counter medication, however effective, may face resistance from patients or parents who expect “something more” for fracture pain.
Acknowledgement
The PURLs Surveillance System is supported in part by Grant Number UL1RR024999 from the National Center for Research Resources; the grant is a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
Click here to view PURL METHODOLOGY
1. Drendel AL, Gorelick MH, Weisman SJ, et al. A randomized clinical trial of ibuprofen versus acetaminophen with codeine for acute pediatric arm fracture pain. Ann Emerg Med. 2009;54:553-560.
2. Koller DM, Myers AB, Lorenz D, et al. Effectiveness of oxycodone, ibuprofen, or the combination in the initial management of orthopedic injury-related pain in children. Pediatr Emerg Care. 2007;23:627-633.
3. Clark E, Plint AC, Correll R, et al. A randomized, controlled trial of acetaminophen, ibuprofen, and codeine for acute pain relief in children with musculoskeletal trauma. Pediatrics. 2007;119:460-467.
4. Lyons RA, Delahunty AM, Kraus D, et al. Children’s fractures: a population based study. Inj Prev. 1999;5:129-132.
5. Drendel AL, Lyon R, Bergholte J, et al. Outpatient pediatric pain management practices for fractures. Pediatr Emerg Care. 2006;22:94-99.
6. Derry C, Derry S, Moore RA, et al. Single dose oral ibuprofen for acute postoperative pain in adults. Cochrane Database Syst Rev. 2009;(3):CD001548.-
7. Clarke S, Lecky F. Best evidence topic report. Do non-steroidal anti-inflammatory drugs cause a delay in fracture healing? Emerg Med J. 2005;22:652-653.
8. Wheeler P, Batt ME. Do non-steroidal anti-inflammatory drugs adversely affect stress fracture healing? A short review. Br J Sports Med. 2005;39:65-69.
1. Drendel AL, Gorelick MH, Weisman SJ, et al. A randomized clinical trial of ibuprofen versus acetaminophen with codeine for acute pediatric arm fracture pain. Ann Emerg Med. 2009;54:553-560.
2. Koller DM, Myers AB, Lorenz D, et al. Effectiveness of oxycodone, ibuprofen, or the combination in the initial management of orthopedic injury-related pain in children. Pediatr Emerg Care. 2007;23:627-633.
3. Clark E, Plint AC, Correll R, et al. A randomized, controlled trial of acetaminophen, ibuprofen, and codeine for acute pain relief in children with musculoskeletal trauma. Pediatrics. 2007;119:460-467.
4. Lyons RA, Delahunty AM, Kraus D, et al. Children’s fractures: a population based study. Inj Prev. 1999;5:129-132.
5. Drendel AL, Lyon R, Bergholte J, et al. Outpatient pediatric pain management practices for fractures. Pediatr Emerg Care. 2006;22:94-99.
6. Derry C, Derry S, Moore RA, et al. Single dose oral ibuprofen for acute postoperative pain in adults. Cochrane Database Syst Rev. 2009;(3):CD001548.-
7. Clarke S, Lecky F. Best evidence topic report. Do non-steroidal anti-inflammatory drugs cause a delay in fracture healing? Emerg Med J. 2005;22:652-653.
8. Wheeler P, Batt ME. Do non-steroidal anti-inflammatory drugs adversely affect stress fracture healing? A short review. Br J Sports Med. 2005;39:65-69.
Copyright © 2010 The Family Physicians Inquiries Network.
All rights reserved.
Start a statin prior to vascular surgery
HMG-CoA reductase inhibitors (statins), initiated 30 days before noncardiac vascular surgery, reduce the incidence of postoperative cardiac complications, including fatal myocardial infarction.1,2
STRENGTH OF RECOMMENDATION
A: 1 new randomized controlled trial (RCT), and 1 smaller, older RCT.
Schouten O, Boersma E, Hoeks S, et al. Fluvastatin and perioperative events in patients undergoing vascular surgery. N Engl J Med. 2009;361:980-989.
Durazzo AE, Machado FS, Ikeoka DT, et al. Reduction in cardiovascular events after vascular surgery with atorvastatin: a randomized trial. J Vasc Surg. 2004;39:967-975.
ILLUSTRATIVE CASE
A 67-year-old man with recurrent transient ischemic attacks comes in for a preoperative evaluation for carotid endarterectomy. The patient’s total cholesterol is 207 mg/dL and his low-density lipoprotein cholesterol (LDL-C) is 109 mg/dL. He takes metoprolol and lisinopril for hypertension.
Should you start him on a statin before surgery?
Nearly 25% of patients with peripheral vascular disease suffer from a cardiac event within 72 hours of elective, noncardiac vascular surgery.3 While most of these “complications” have minimal clinical impact and are detected by biochemical markers alone, some patients experience serious cardiac complications—including fatal myocardial infarction (MI).
That’s not surprising, given that most patients who require noncardiac vascular surgery suffer from severe coronary vascular disease.4 What is surprising is that most candidates for noncardiac vascular surgery are not put on statins prior to undergoing surgery.1,2,5
Statins were thought to increase—not prevent—complications
Until recently, taking statins during the perioperative period was believed to increase complications, including statin-associated myopathy. Indeed, guidelines from the American Heart Association (AHA), American College of Cardiology (ACC), and National Heart, Lung and Blood Institute (NHLBI) suggest that it is prudent to withhold statins during hospitalization for major surgery.6
1 small study hinted at value of perioperative statins
A small Brazilian trial conducted in 2004 called the AHA/ACC/NHLBI guidelines into question. the researchers studied 100 patients slated for noncardiac vascular surgery who were randomized to receive either 20 mg atorvastatin (Lipitor) or placebo preoperatively —and monitored them for cardiac events 6 months postoperatively. They found that the incidence of cardiac events (cardiac death, nonfatal MI, stroke, or unstable angina) was more than 3 times higher in the placebo group compared with patients receiving atorvastatin (26% vs 8%, number needed to treat [NNT]=5.6; P=.031).2
The results of this small single study, although suggestive, were not sufficiently convincing to change recommendations about the preoperative use of statins, however. A more comprehensive study was needed to alter standard practice, and the Schouten study that we report on below fits the bill.1
STUDY SUMMARY: Preoperative statin use cuts risk in half
Schouten et al followed 500 patients, who were randomized to receive either 80 mg extended-release fluvastatin (Lescol XL) or placebo for a median of 37 days prior to surgery.1 All enrollees were older than 40 years of age and were scheduled for noncardiac vascular surgery. the reasons for the surgery were abdominal aortic aneurysm repair (47.5%), lower limb arterial reconstruction (38.6%), or carotid artery endarterectomy (13.9%). Patients who were taking long-term beta-blocker therapy were continued on it; otherwise, bisoprolol 2.5 mg was initiated at the screening visit. Patients who were already taking statins (<50% of potential subjects) were excluded. Other exclusions were a contraindication to statin therapy; emergent surgery; and a repeat procedure within the last 29 days. Patients with unstable coronary artery disease or extensive stress-induced ischemia consistent with left main artery disease (or its equivalent) were also excluded.
The primary study outcome was myocardial ischemia, determined by continuous electrocardiogram (EKG) monitoring in the first 48 hours postsurgery and by 12-lead EKG recordings on days 3, 7, and 30. Troponin T levels were measured on postoperative days 1, 3, 7, and 30, as well. the principal secondary end point was either death from cardiovascular causes or nonfatal MI. MI was diagnosed by characteristic ischemic symptoms, with EKG evidence of ischemia or positive troponin T with characteristic rising and falling values.
To gauge fluvastatin’s effect on biomarkers, lipids, high-sensitivity C-reactive protein, and interleukin-6 were measured upon initiation of the medication and on the day of admission for surgery. Serum creatine kinase, alanine aminotransferase (ALT) levels, clinical myopathy, and rhabdomyolysis were monitored as safety measures, with levels measured prior to randomization, on the day of admission, and on postoperative days 1, 3, 7, and 30.
Both groups were similar in age (mean of 66 years), total serum cholesterol levels, risk factors for cardiac events, and medication use. About 75% of the enrollees were men. At baseline, 51% of the participants had a total cholesterol <213 mg/dL, and 39% had an LDL-C <116 mg/dL. Within 30 days after surgery, 27 (10.8%) of those in the fluvastatin group and 47 (19%) of patients in the placebo group had evidence of myocardial ischemia (hazard ratio=0.55; 95% confidence interval [CI], 0.34-0.88; P=.01). the NNT to prevent 1 patient from experiencing myocardial ischemia was 12.
Statin users had fewer MIs. A total of 6 patients receiving fluvastatin died, with 4 deaths attributed to cardiovascular causes. In the placebo group, 12 patients died, 8 of which were ascribed to cardiovascular causes. Eight patients in the fluvastatin group experienced nonfatal MIs, compared with 17 patients in the placebo group (NNT=19 to prevent 1 nonfatal MI or cardiac death (hazard ratio= 0.47; 95% CI, 0.24-0.94; P=.03).
Effects of statins were evident preoperatively. At the time of surgery, patients in the fluvastatin group had, on average, a 20% reduction in their total cholesterol and a 24% reduction in LDL-C; in the placebo group, total cholesterol had fallen by 4% and LDL-C, by 3%.
Patients receiving fluvastatin had an average 21% decrease in C-reactive protein, compared with a 3% increase for the placebo group. Interleukin-6 levels also were reduced far more in the fluvastatin group (33% vs a 4% reduction in the placebo group [P<.001]).
The medication was well tolerated. Overall, 6.8% of participants discontinued the study because of side effects, including 16 (6.4%) patients in the fluvastatin group and 18 (7.3%) in the placebo group. (After surgery, 115 [23.1%] of patients in the statin group temporarily discontinued the drug because of an inability to take oral medications for a median of 2 days.)
Rates of increase in creatine kinase of >10× the upper limit of normal (ULN) were similar between the fluvastatin and placebo groups (4% vs 3.2%, respectively). Increases in ALT to >3× ULN were more frequent in the placebo group compared with the fluvastatin group (5.3%, placebo; 3.2%, fluvastatin). No cases of myopathy or rhabdomyolysis were observed in either group.
WHAT’S NEW: Preop statins can be a lifesaver
The initiation of fluvastatin prior to vascular surgery reduced the incidence of cardiovascular events by 50%—a remarkable result. While patients at the highest risk were excluded from the study, those with lower cardiac risk nonetheless benefi ted from statin therapy. Experts have not typically recommended statins in the perioperative period for this patient population. the results of this study make it clear that they should.
CAVEATS: Extended-release formulation may have affected outcome
The statin used in this study was a longacting formulation, which may have protected patients who were unable to take oral medicines postoperatively. While we don’t know if the extended-release formulation made a difference in this study, we do know that atorvastatin was effective in the Brazilian study discussed earlier.
CHALLENGES TO IMPLEMENTATION: Preop statins may be overlooked
Not all patients see a primary care physician prior to undergoing vascular surgery. This means that it will sometimes be left to surgeons or other specialists to initiate statin therapy prior to surgery, and they may or may not do so.
Optimal timing is unknown. It is not clear how little time a patient scheduled for vascular surgery could spend on a statin and still reap these benefits. Nor do we know if the benefits would extend to patients undergoing other types of surgery; in a large study of patients undergoing all kinds of major noncardiac surgery, no benefits of perioperative statins were found.7
Adherence to the medication regimen presents another challenge, at least for some patients. In this case, however, we think the prospect of preventing major cardiac events postoperatively simply by taking statins for a month should be compelling enough to convince patients to take their medicine.
Acknowledgement
The PURLs Surveillance System is supported in part by Grant Number UL1RR024999 from the National Center for Research Resources; the grant is a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the ofcial views of either the National Center for Research Resources or the National Institutes of Health.
Click here to view PURL METHODOLOGY
1. Schouten O, Boersma E, Hoeks SE, et al. Fluvastatin and perioperative events in patients undergoing vascular surgery. N Engl J Med. 2009;361:980-989.
2. Durazzo AE, Machado FS, Ikeoka DT, et al. Reduction in cardiovascular events after vascular surgery with atorvastatin: a randomized trial. J Vasc Surg. 2004;39:967-975.
3. Pasternak RC, Smith SC, Jr, Bairey-Merz CN, et al. ACC/AHA/ NHLBI Clinical advisory on the use and safety of statins. Circulation. 2002;106:1024-1028.
4. Landesberg G, Shatz V, Akopnik I, et al. Association of cardiac troponin, CK-MB, and postoperative myocardial ischemia with long-term survival after major vascular surgery. J Am Coll Cardiol. 2003;42:1547-1554.
5. Hertzer NR, Beven EG, Young JR, et al. Coronary artery disease in peripheral vascular patients. A classification of 1000 coronary angiograms and results of surgical management. Ann Surg. 1984;199:223-233.
6. Brady AR, Gibbs JS, Greenhalgh RM, et al. Perioperative betablockade (POBBLE) for patients undergoing infrarenal vascular surgery: results of a randomized double-blind controlled trial. J Vasc Surg. 2005;41:602-609.
7. Dunkelgrun M, Boersma E, Schouten O, et al. Bisoprolol and fluvastatin for the reduction of perioperative cardiac mortality and myocardial infarction in intermediate-risk patients undergoing noncardiovascular surgery: a randomized controlled trial (DECREASE-IV). Ann Surg. 2009;249:921-926.
HMG-CoA reductase inhibitors (statins), initiated 30 days before noncardiac vascular surgery, reduce the incidence of postoperative cardiac complications, including fatal myocardial infarction.1,2
STRENGTH OF RECOMMENDATION
A: 1 new randomized controlled trial (RCT), and 1 smaller, older RCT.
Schouten O, Boersma E, Hoeks S, et al. Fluvastatin and perioperative events in patients undergoing vascular surgery. N Engl J Med. 2009;361:980-989.
Durazzo AE, Machado FS, Ikeoka DT, et al. Reduction in cardiovascular events after vascular surgery with atorvastatin: a randomized trial. J Vasc Surg. 2004;39:967-975.
ILLUSTRATIVE CASE
A 67-year-old man with recurrent transient ischemic attacks comes in for a preoperative evaluation for carotid endarterectomy. The patient’s total cholesterol is 207 mg/dL and his low-density lipoprotein cholesterol (LDL-C) is 109 mg/dL. He takes metoprolol and lisinopril for hypertension.
Should you start him on a statin before surgery?
Nearly 25% of patients with peripheral vascular disease suffer from a cardiac event within 72 hours of elective, noncardiac vascular surgery.3 While most of these “complications” have minimal clinical impact and are detected by biochemical markers alone, some patients experience serious cardiac complications—including fatal myocardial infarction (MI).
That’s not surprising, given that most patients who require noncardiac vascular surgery suffer from severe coronary vascular disease.4 What is surprising is that most candidates for noncardiac vascular surgery are not put on statins prior to undergoing surgery.1,2,5
Statins were thought to increase—not prevent—complications
Until recently, taking statins during the perioperative period was believed to increase complications, including statin-associated myopathy. Indeed, guidelines from the American Heart Association (AHA), American College of Cardiology (ACC), and National Heart, Lung and Blood Institute (NHLBI) suggest that it is prudent to withhold statins during hospitalization for major surgery.6
1 small study hinted at value of perioperative statins
A small Brazilian trial conducted in 2004 called the AHA/ACC/NHLBI guidelines into question. the researchers studied 100 patients slated for noncardiac vascular surgery who were randomized to receive either 20 mg atorvastatin (Lipitor) or placebo preoperatively —and monitored them for cardiac events 6 months postoperatively. They found that the incidence of cardiac events (cardiac death, nonfatal MI, stroke, or unstable angina) was more than 3 times higher in the placebo group compared with patients receiving atorvastatin (26% vs 8%, number needed to treat [NNT]=5.6; P=.031).2
The results of this small single study, although suggestive, were not sufficiently convincing to change recommendations about the preoperative use of statins, however. A more comprehensive study was needed to alter standard practice, and the Schouten study that we report on below fits the bill.1
STUDY SUMMARY: Preoperative statin use cuts risk in half
Schouten et al followed 500 patients, who were randomized to receive either 80 mg extended-release fluvastatin (Lescol XL) or placebo for a median of 37 days prior to surgery.1 All enrollees were older than 40 years of age and were scheduled for noncardiac vascular surgery. the reasons for the surgery were abdominal aortic aneurysm repair (47.5%), lower limb arterial reconstruction (38.6%), or carotid artery endarterectomy (13.9%). Patients who were taking long-term beta-blocker therapy were continued on it; otherwise, bisoprolol 2.5 mg was initiated at the screening visit. Patients who were already taking statins (<50% of potential subjects) were excluded. Other exclusions were a contraindication to statin therapy; emergent surgery; and a repeat procedure within the last 29 days. Patients with unstable coronary artery disease or extensive stress-induced ischemia consistent with left main artery disease (or its equivalent) were also excluded.
The primary study outcome was myocardial ischemia, determined by continuous electrocardiogram (EKG) monitoring in the first 48 hours postsurgery and by 12-lead EKG recordings on days 3, 7, and 30. Troponin T levels were measured on postoperative days 1, 3, 7, and 30, as well. the principal secondary end point was either death from cardiovascular causes or nonfatal MI. MI was diagnosed by characteristic ischemic symptoms, with EKG evidence of ischemia or positive troponin T with characteristic rising and falling values.
To gauge fluvastatin’s effect on biomarkers, lipids, high-sensitivity C-reactive protein, and interleukin-6 were measured upon initiation of the medication and on the day of admission for surgery. Serum creatine kinase, alanine aminotransferase (ALT) levels, clinical myopathy, and rhabdomyolysis were monitored as safety measures, with levels measured prior to randomization, on the day of admission, and on postoperative days 1, 3, 7, and 30.
Both groups were similar in age (mean of 66 years), total serum cholesterol levels, risk factors for cardiac events, and medication use. About 75% of the enrollees were men. At baseline, 51% of the participants had a total cholesterol <213 mg/dL, and 39% had an LDL-C <116 mg/dL. Within 30 days after surgery, 27 (10.8%) of those in the fluvastatin group and 47 (19%) of patients in the placebo group had evidence of myocardial ischemia (hazard ratio=0.55; 95% confidence interval [CI], 0.34-0.88; P=.01). the NNT to prevent 1 patient from experiencing myocardial ischemia was 12.
Statin users had fewer MIs. A total of 6 patients receiving fluvastatin died, with 4 deaths attributed to cardiovascular causes. In the placebo group, 12 patients died, 8 of which were ascribed to cardiovascular causes. Eight patients in the fluvastatin group experienced nonfatal MIs, compared with 17 patients in the placebo group (NNT=19 to prevent 1 nonfatal MI or cardiac death (hazard ratio= 0.47; 95% CI, 0.24-0.94; P=.03).
Effects of statins were evident preoperatively. At the time of surgery, patients in the fluvastatin group had, on average, a 20% reduction in their total cholesterol and a 24% reduction in LDL-C; in the placebo group, total cholesterol had fallen by 4% and LDL-C, by 3%.
Patients receiving fluvastatin had an average 21% decrease in C-reactive protein, compared with a 3% increase for the placebo group. Interleukin-6 levels also were reduced far more in the fluvastatin group (33% vs a 4% reduction in the placebo group [P<.001]).
The medication was well tolerated. Overall, 6.8% of participants discontinued the study because of side effects, including 16 (6.4%) patients in the fluvastatin group and 18 (7.3%) in the placebo group. (After surgery, 115 [23.1%] of patients in the statin group temporarily discontinued the drug because of an inability to take oral medications for a median of 2 days.)
Rates of increase in creatine kinase of >10× the upper limit of normal (ULN) were similar between the fluvastatin and placebo groups (4% vs 3.2%, respectively). Increases in ALT to >3× ULN were more frequent in the placebo group compared with the fluvastatin group (5.3%, placebo; 3.2%, fluvastatin). No cases of myopathy or rhabdomyolysis were observed in either group.
WHAT’S NEW: Preop statins can be a lifesaver
The initiation of fluvastatin prior to vascular surgery reduced the incidence of cardiovascular events by 50%—a remarkable result. While patients at the highest risk were excluded from the study, those with lower cardiac risk nonetheless benefi ted from statin therapy. Experts have not typically recommended statins in the perioperative period for this patient population. the results of this study make it clear that they should.
CAVEATS: Extended-release formulation may have affected outcome
The statin used in this study was a longacting formulation, which may have protected patients who were unable to take oral medicines postoperatively. While we don’t know if the extended-release formulation made a difference in this study, we do know that atorvastatin was effective in the Brazilian study discussed earlier.
CHALLENGES TO IMPLEMENTATION: Preop statins may be overlooked
Not all patients see a primary care physician prior to undergoing vascular surgery. This means that it will sometimes be left to surgeons or other specialists to initiate statin therapy prior to surgery, and they may or may not do so.
Optimal timing is unknown. It is not clear how little time a patient scheduled for vascular surgery could spend on a statin and still reap these benefits. Nor do we know if the benefits would extend to patients undergoing other types of surgery; in a large study of patients undergoing all kinds of major noncardiac surgery, no benefits of perioperative statins were found.7
Adherence to the medication regimen presents another challenge, at least for some patients. In this case, however, we think the prospect of preventing major cardiac events postoperatively simply by taking statins for a month should be compelling enough to convince patients to take their medicine.
Acknowledgement
The PURLs Surveillance System is supported in part by Grant Number UL1RR024999 from the National Center for Research Resources; the grant is a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the ofcial views of either the National Center for Research Resources or the National Institutes of Health.
Click here to view PURL METHODOLOGY
HMG-CoA reductase inhibitors (statins), initiated 30 days before noncardiac vascular surgery, reduce the incidence of postoperative cardiac complications, including fatal myocardial infarction.1,2
STRENGTH OF RECOMMENDATION
A: 1 new randomized controlled trial (RCT), and 1 smaller, older RCT.
Schouten O, Boersma E, Hoeks S, et al. Fluvastatin and perioperative events in patients undergoing vascular surgery. N Engl J Med. 2009;361:980-989.
Durazzo AE, Machado FS, Ikeoka DT, et al. Reduction in cardiovascular events after vascular surgery with atorvastatin: a randomized trial. J Vasc Surg. 2004;39:967-975.
ILLUSTRATIVE CASE
A 67-year-old man with recurrent transient ischemic attacks comes in for a preoperative evaluation for carotid endarterectomy. The patient’s total cholesterol is 207 mg/dL and his low-density lipoprotein cholesterol (LDL-C) is 109 mg/dL. He takes metoprolol and lisinopril for hypertension.
Should you start him on a statin before surgery?
Nearly 25% of patients with peripheral vascular disease suffer from a cardiac event within 72 hours of elective, noncardiac vascular surgery.3 While most of these “complications” have minimal clinical impact and are detected by biochemical markers alone, some patients experience serious cardiac complications—including fatal myocardial infarction (MI).
That’s not surprising, given that most patients who require noncardiac vascular surgery suffer from severe coronary vascular disease.4 What is surprising is that most candidates for noncardiac vascular surgery are not put on statins prior to undergoing surgery.1,2,5
Statins were thought to increase—not prevent—complications
Until recently, taking statins during the perioperative period was believed to increase complications, including statin-associated myopathy. Indeed, guidelines from the American Heart Association (AHA), American College of Cardiology (ACC), and National Heart, Lung and Blood Institute (NHLBI) suggest that it is prudent to withhold statins during hospitalization for major surgery.6
1 small study hinted at value of perioperative statins
A small Brazilian trial conducted in 2004 called the AHA/ACC/NHLBI guidelines into question. the researchers studied 100 patients slated for noncardiac vascular surgery who were randomized to receive either 20 mg atorvastatin (Lipitor) or placebo preoperatively —and monitored them for cardiac events 6 months postoperatively. They found that the incidence of cardiac events (cardiac death, nonfatal MI, stroke, or unstable angina) was more than 3 times higher in the placebo group compared with patients receiving atorvastatin (26% vs 8%, number needed to treat [NNT]=5.6; P=.031).2
The results of this small single study, although suggestive, were not sufficiently convincing to change recommendations about the preoperative use of statins, however. A more comprehensive study was needed to alter standard practice, and the Schouten study that we report on below fits the bill.1
STUDY SUMMARY: Preoperative statin use cuts risk in half
Schouten et al followed 500 patients, who were randomized to receive either 80 mg extended-release fluvastatin (Lescol XL) or placebo for a median of 37 days prior to surgery.1 All enrollees were older than 40 years of age and were scheduled for noncardiac vascular surgery. the reasons for the surgery were abdominal aortic aneurysm repair (47.5%), lower limb arterial reconstruction (38.6%), or carotid artery endarterectomy (13.9%). Patients who were taking long-term beta-blocker therapy were continued on it; otherwise, bisoprolol 2.5 mg was initiated at the screening visit. Patients who were already taking statins (<50% of potential subjects) were excluded. Other exclusions were a contraindication to statin therapy; emergent surgery; and a repeat procedure within the last 29 days. Patients with unstable coronary artery disease or extensive stress-induced ischemia consistent with left main artery disease (or its equivalent) were also excluded.
The primary study outcome was myocardial ischemia, determined by continuous electrocardiogram (EKG) monitoring in the first 48 hours postsurgery and by 12-lead EKG recordings on days 3, 7, and 30. Troponin T levels were measured on postoperative days 1, 3, 7, and 30, as well. the principal secondary end point was either death from cardiovascular causes or nonfatal MI. MI was diagnosed by characteristic ischemic symptoms, with EKG evidence of ischemia or positive troponin T with characteristic rising and falling values.
To gauge fluvastatin’s effect on biomarkers, lipids, high-sensitivity C-reactive protein, and interleukin-6 were measured upon initiation of the medication and on the day of admission for surgery. Serum creatine kinase, alanine aminotransferase (ALT) levels, clinical myopathy, and rhabdomyolysis were monitored as safety measures, with levels measured prior to randomization, on the day of admission, and on postoperative days 1, 3, 7, and 30.
Both groups were similar in age (mean of 66 years), total serum cholesterol levels, risk factors for cardiac events, and medication use. About 75% of the enrollees were men. At baseline, 51% of the participants had a total cholesterol <213 mg/dL, and 39% had an LDL-C <116 mg/dL. Within 30 days after surgery, 27 (10.8%) of those in the fluvastatin group and 47 (19%) of patients in the placebo group had evidence of myocardial ischemia (hazard ratio=0.55; 95% confidence interval [CI], 0.34-0.88; P=.01). the NNT to prevent 1 patient from experiencing myocardial ischemia was 12.
Statin users had fewer MIs. A total of 6 patients receiving fluvastatin died, with 4 deaths attributed to cardiovascular causes. In the placebo group, 12 patients died, 8 of which were ascribed to cardiovascular causes. Eight patients in the fluvastatin group experienced nonfatal MIs, compared with 17 patients in the placebo group (NNT=19 to prevent 1 nonfatal MI or cardiac death (hazard ratio= 0.47; 95% CI, 0.24-0.94; P=.03).
Effects of statins were evident preoperatively. At the time of surgery, patients in the fluvastatin group had, on average, a 20% reduction in their total cholesterol and a 24% reduction in LDL-C; in the placebo group, total cholesterol had fallen by 4% and LDL-C, by 3%.
Patients receiving fluvastatin had an average 21% decrease in C-reactive protein, compared with a 3% increase for the placebo group. Interleukin-6 levels also were reduced far more in the fluvastatin group (33% vs a 4% reduction in the placebo group [P<.001]).
The medication was well tolerated. Overall, 6.8% of participants discontinued the study because of side effects, including 16 (6.4%) patients in the fluvastatin group and 18 (7.3%) in the placebo group. (After surgery, 115 [23.1%] of patients in the statin group temporarily discontinued the drug because of an inability to take oral medications for a median of 2 days.)
Rates of increase in creatine kinase of >10× the upper limit of normal (ULN) were similar between the fluvastatin and placebo groups (4% vs 3.2%, respectively). Increases in ALT to >3× ULN were more frequent in the placebo group compared with the fluvastatin group (5.3%, placebo; 3.2%, fluvastatin). No cases of myopathy or rhabdomyolysis were observed in either group.
WHAT’S NEW: Preop statins can be a lifesaver
The initiation of fluvastatin prior to vascular surgery reduced the incidence of cardiovascular events by 50%—a remarkable result. While patients at the highest risk were excluded from the study, those with lower cardiac risk nonetheless benefi ted from statin therapy. Experts have not typically recommended statins in the perioperative period for this patient population. the results of this study make it clear that they should.
CAVEATS: Extended-release formulation may have affected outcome
The statin used in this study was a longacting formulation, which may have protected patients who were unable to take oral medicines postoperatively. While we don’t know if the extended-release formulation made a difference in this study, we do know that atorvastatin was effective in the Brazilian study discussed earlier.
CHALLENGES TO IMPLEMENTATION: Preop statins may be overlooked
Not all patients see a primary care physician prior to undergoing vascular surgery. This means that it will sometimes be left to surgeons or other specialists to initiate statin therapy prior to surgery, and they may or may not do so.
Optimal timing is unknown. It is not clear how little time a patient scheduled for vascular surgery could spend on a statin and still reap these benefits. Nor do we know if the benefits would extend to patients undergoing other types of surgery; in a large study of patients undergoing all kinds of major noncardiac surgery, no benefits of perioperative statins were found.7
Adherence to the medication regimen presents another challenge, at least for some patients. In this case, however, we think the prospect of preventing major cardiac events postoperatively simply by taking statins for a month should be compelling enough to convince patients to take their medicine.
Acknowledgement
The PURLs Surveillance System is supported in part by Grant Number UL1RR024999 from the National Center for Research Resources; the grant is a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the ofcial views of either the National Center for Research Resources or the National Institutes of Health.
Click here to view PURL METHODOLOGY
1. Schouten O, Boersma E, Hoeks SE, et al. Fluvastatin and perioperative events in patients undergoing vascular surgery. N Engl J Med. 2009;361:980-989.
2. Durazzo AE, Machado FS, Ikeoka DT, et al. Reduction in cardiovascular events after vascular surgery with atorvastatin: a randomized trial. J Vasc Surg. 2004;39:967-975.
3. Pasternak RC, Smith SC, Jr, Bairey-Merz CN, et al. ACC/AHA/ NHLBI Clinical advisory on the use and safety of statins. Circulation. 2002;106:1024-1028.
4. Landesberg G, Shatz V, Akopnik I, et al. Association of cardiac troponin, CK-MB, and postoperative myocardial ischemia with long-term survival after major vascular surgery. J Am Coll Cardiol. 2003;42:1547-1554.
5. Hertzer NR, Beven EG, Young JR, et al. Coronary artery disease in peripheral vascular patients. A classification of 1000 coronary angiograms and results of surgical management. Ann Surg. 1984;199:223-233.
6. Brady AR, Gibbs JS, Greenhalgh RM, et al. Perioperative betablockade (POBBLE) for patients undergoing infrarenal vascular surgery: results of a randomized double-blind controlled trial. J Vasc Surg. 2005;41:602-609.
7. Dunkelgrun M, Boersma E, Schouten O, et al. Bisoprolol and fluvastatin for the reduction of perioperative cardiac mortality and myocardial infarction in intermediate-risk patients undergoing noncardiovascular surgery: a randomized controlled trial (DECREASE-IV). Ann Surg. 2009;249:921-926.
1. Schouten O, Boersma E, Hoeks SE, et al. Fluvastatin and perioperative events in patients undergoing vascular surgery. N Engl J Med. 2009;361:980-989.
2. Durazzo AE, Machado FS, Ikeoka DT, et al. Reduction in cardiovascular events after vascular surgery with atorvastatin: a randomized trial. J Vasc Surg. 2004;39:967-975.
3. Pasternak RC, Smith SC, Jr, Bairey-Merz CN, et al. ACC/AHA/ NHLBI Clinical advisory on the use and safety of statins. Circulation. 2002;106:1024-1028.
4. Landesberg G, Shatz V, Akopnik I, et al. Association of cardiac troponin, CK-MB, and postoperative myocardial ischemia with long-term survival after major vascular surgery. J Am Coll Cardiol. 2003;42:1547-1554.
5. Hertzer NR, Beven EG, Young JR, et al. Coronary artery disease in peripheral vascular patients. A classification of 1000 coronary angiograms and results of surgical management. Ann Surg. 1984;199:223-233.
6. Brady AR, Gibbs JS, Greenhalgh RM, et al. Perioperative betablockade (POBBLE) for patients undergoing infrarenal vascular surgery: results of a randomized double-blind controlled trial. J Vasc Surg. 2005;41:602-609.
7. Dunkelgrun M, Boersma E, Schouten O, et al. Bisoprolol and fluvastatin for the reduction of perioperative cardiac mortality and myocardial infarction in intermediate-risk patients undergoing noncardiovascular surgery: a randomized controlled trial (DECREASE-IV). Ann Surg. 2009;249:921-926.
Copyright © 2010 The Family Physicians Inquiries Network.
All rights reserved.
Should patients with acute DVT limit activity?
PROBABLY NOT. Ambulation, combined with compression of the affected extremity, appears to be safe for medically stable patients with deep venous thromboses (DVT) (strength of recommendation [SOR]: A, consistent randomized controlled trials [RCTs]). Leg compression and ambulation, compared with bed rest without compression, can effectively decrease swelling and pain (SOR: A, consistent RCTs).
Only weak data exist to suggest that early ambulation can reduce mortality (SOR: C, cohort studies with historical controls).
Evidence summary
Patients with acute DVT have traditionally been treated with immobilization and bed rest, combined with anticoagulation, for days. This approach is motivated by fear of dislodging an unstable thrombus and causing a pulmonary embolism (PE) and by the belief that inactivity relieves local pain and swelling. On the other hand, bed rest promotes stasis, an element in Virchow’s triad.
Early ambulation doesn’t raise risk of PE
We performed a structured literature review, which found 6 RCTs and 3 cohort studies that address this problem. All 6 RCTs included patients with acute DVT but without life-threatening conditions.1-6 They assessed various outcomes, including incidence of new PE, change in leg circumference, leg pain, patient well-being, and progression of DVT.
The studies consistently found that early ambulation, along with compression, is safe when compared with bed rest ( TABLE ). Although the sample size of all the RCTs was small, the RCTs showed consistent trends in favor of ambulation and compression.
A prospective cohort study of new PE in patients treated with ambulation and compression plus anticoagulation found that the incidence of PE was significantly lower than historical incidence rates in patients managed with bed rest.7
Another study using the RIETE registry, a Spanish registry of consecutively enrolled patients with objectively confirmed acute DVT or PE, found no significant difference in occurrence of new PE between immobilized and mobilized patients.8 Patients with DVT who were immobilized were generally sicker, more likely to have PaO2 <60, and more likely to have received lower doses of low-molecular-weight heparin (LMWH) compared with the group that walked (P<.005).
TABLE
Early ambulation and compression: What RCTs show
| Subjects | Study groups | Results |
|---|---|---|
| 129 patients with DVT, treated with LMWH1 | Strict immobilization for 4 days Ambulation for ≥4 h/d, along with compression for 4 days or until swelling subsided | At 4 days: No difference in PE, leg pain, leg size, mortality At 3 months: No difference in PE, mortality |
| 146 patients with DVT, all anticoagulated5 | Hospital treatment with 5 days of bed rest Home care with early walking and compression stockings | No difference in occurrence of new PE after 10 days |
| 126 patients with DVT, treated with LMWH, compression6 | Strict bed rest for 8 days with leg elevation Began full ambulation on day 2 | No difference in PE |
| 102 patients with DVT, treated with LMWH, compression4 | Bed rest for 5 days Ambulation | No differences in PE, thrombus progression, serious adverse events, or leg pain Study didn’t recruit expected number of patients Study showed a trend toward benefit from ambulation |
| 53 patients with DVT2,7 | Ambulation and use of firm, inelastic Unna boot bandages Ambulation and elastic compression stockings Strict bed rest for 9 days and no compression | No difference in quality of life or PE DVT-related symptoms, leg pain, and circumference improved in compression/ambulation groups No changes noted at 2 years |
| 72 patients with DVT, treated with anticoagulation and compression3 | Daily walking exercise and weekly group exercise Control group | No difference in DVT, PE, phlebography results, or calf circumference |
| DVT, deep vein thrombosis; LMWH, low-molecular-weight heparin; PE, pulmonary embolism. | ||
Does ambulation affect thrombus propagation?
A multicenter RCT showed that thrombus progression occurred more often in patients who were treated with bed rest compared with patients treated with ambulation and compression (P<.01).2
Another RCT revealed a similar trend, though the difference didn’t reach statistical significance because of small sample size.4 The clinical importance of these phlebographic studies isn’t clear.
Is it the walking, or compression, that works?
RCTs have shown that ambulation with leg compression, compared with bed rest without compression, can effectively decrease leg swelling and pain1,2,4 The difference was detectable 2 years after DVT.7
In contrast, RCTs in which both ambulating and resting patients received compression therapy showed no significant difference in leg circumference at 1 or 6 months.3 This finding suggests that the benefit on local symptoms may result from compression rather than ambulation.
Reduced mortality? Evidence is weak
Estimates of the possible effect on mortality of ambulation compared with bed rest are based on cohort studies. A cohort study in which 691 patients were kept walking with compression therapy reported a mortality rate of 0.2%.9 In another cohort, the mortality rate was also 0.2%, and all deaths occurred in patients older than 70 years.10
This rate is lower than rates reported in the historic literature, which typically are 1% among patients treated with unfractionated heparin and bed rest.9,10 A retrospective, multicenter cohort of 1647 patients treated with unfractionated heparin and bed rest in different German hospitals reported a rate of fatal PE of 2.33%.11
Data from the RIETE registry indicated that overall mortality was significantly higher in immobilized patients with a PE (3.6% vs 0.5% in mobile patients; P=.01).8 Notably, immobilized patients with a PE were more likely to be hypoxic and also tended to receive lower doses of LMWH. No differences were found in outcomes for patients with DVT.
Recommendations
The American College of Chest Physicians (ACCP) doesn’t recommend bed rest in its guidelines for treating acute venous thromboembolism, but rather ambulation as tolerated after starting anticoagulation. Patients who are not hemodynamically stable should be stabilized first.
The ACCP also recommends wearing an elastic compression stocking with a pressure of 30 to 40 mm Hg at the ankle for 2 years after an episode of DVT and a course of intermittent pneumatic compression for patients with severe edema of the leg resulting from post-thrombotic syndrome.12
A joint guideline from the American College of Physicians and the American Academy of Family Physicians doesn’t make recommendations about ambulation for therapy of DVT and PE.13
1. Aschwanden M, Labs KH, Engel H, et al. Acute deep vein thrombosis: early mobilization does not increase the frequency of pulmonary embolism. Thromb Haemost. 2001;85:42-46.
2. Blattler W, Partsch H. Leg compression and ambulation is better than bed rest for the treatment of acute deep venous thrombosis. Int Angiol. 2003;22:393-400.
3. Isma N, Johanssson E, Bjork A, et al. Does supervised exercise after deep venous thrombosis improve recanalization of occluded vein segments? A randomized study. J Thromb Thrombolysis. 2007;23:25-30.
4. Junger M, Diehm C, Storiko H, et al. Mobilization versus immobilization in the treatment of acute proximal deep venous thrombosis: a prospective, randomized, open, multicentre trial. Curr Med Res Opin. 2006;22:593-602.
5. Romera A, Vila R, Perez-Piqueras A, et al. Early mobilization in patients with acute deep vein thrombosis: does it increase the incidence of symptomatic pulmonary embolism? Phlebology. 2005;20:141.-
6. Schellong SM, Schwarz T, Kropp J, et al. Bed rest in deep vein thrombosis and the incidence of scintigraphic pulmonary embolism. Thromb Haemost. 1999;82(suppl 1):127-129.
7. Partsch H, Kaulich M, Mayer W. Immediate mobilisation in acute vein thrombosis reduces post-thrombotic syndrome. Int Angiol. 2004;23:206-212.
8. Trujillo-Santos J, Perea-Milla E, Jimenez-Puente A, et al. Bed rest or ambulation in the initial treatment of patients with acute deep vein thrombosis or pulmonary embolism: findings from the RIETE registry. Chest. 2005;127:1631-1636.
9. Partsch H, Kechavarz B, Kohn H, et al. The effect of mobilisation of patients during treatment of thromboembolic disorders with low-molecular-weight heparin. Int Angiol. 1997;16:189-192.
10. Partsch H. Therapy of deep vein thrombosis with low molecular weight heparin, leg compression and immediate ambulation. Vasa. 2001;30:195-204.
11. Martin M. PHLECO: a multicenter study of the fate of 1647 hospital patients treated conservatively without fibrinolysis and surgery. Clin Invest. 1993;71:471-477.
12. Buller HR, Agnelli G, Hull RD, et al. Antithrombotic therapy for venous thromboembolic disease: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest. 2004;126 (suppl 3):401S-428S.
13. Snow V, Qaseem A, Barry P, et al. Management of venous thromboembolism: a clinical practice guideline from the American College of Physicians and the American Academy of Family Physicians. Ann Intern Med. 2007;146:204-210.
PROBABLY NOT. Ambulation, combined with compression of the affected extremity, appears to be safe for medically stable patients with deep venous thromboses (DVT) (strength of recommendation [SOR]: A, consistent randomized controlled trials [RCTs]). Leg compression and ambulation, compared with bed rest without compression, can effectively decrease swelling and pain (SOR: A, consistent RCTs).
Only weak data exist to suggest that early ambulation can reduce mortality (SOR: C, cohort studies with historical controls).
Evidence summary
Patients with acute DVT have traditionally been treated with immobilization and bed rest, combined with anticoagulation, for days. This approach is motivated by fear of dislodging an unstable thrombus and causing a pulmonary embolism (PE) and by the belief that inactivity relieves local pain and swelling. On the other hand, bed rest promotes stasis, an element in Virchow’s triad.
Early ambulation doesn’t raise risk of PE
We performed a structured literature review, which found 6 RCTs and 3 cohort studies that address this problem. All 6 RCTs included patients with acute DVT but without life-threatening conditions.1-6 They assessed various outcomes, including incidence of new PE, change in leg circumference, leg pain, patient well-being, and progression of DVT.
The studies consistently found that early ambulation, along with compression, is safe when compared with bed rest ( TABLE ). Although the sample size of all the RCTs was small, the RCTs showed consistent trends in favor of ambulation and compression.
A prospective cohort study of new PE in patients treated with ambulation and compression plus anticoagulation found that the incidence of PE was significantly lower than historical incidence rates in patients managed with bed rest.7
Another study using the RIETE registry, a Spanish registry of consecutively enrolled patients with objectively confirmed acute DVT or PE, found no significant difference in occurrence of new PE between immobilized and mobilized patients.8 Patients with DVT who were immobilized were generally sicker, more likely to have PaO2 <60, and more likely to have received lower doses of low-molecular-weight heparin (LMWH) compared with the group that walked (P<.005).
TABLE
Early ambulation and compression: What RCTs show
| Subjects | Study groups | Results |
|---|---|---|
| 129 patients with DVT, treated with LMWH1 | Strict immobilization for 4 days Ambulation for ≥4 h/d, along with compression for 4 days or until swelling subsided | At 4 days: No difference in PE, leg pain, leg size, mortality At 3 months: No difference in PE, mortality |
| 146 patients with DVT, all anticoagulated5 | Hospital treatment with 5 days of bed rest Home care with early walking and compression stockings | No difference in occurrence of new PE after 10 days |
| 126 patients with DVT, treated with LMWH, compression6 | Strict bed rest for 8 days with leg elevation Began full ambulation on day 2 | No difference in PE |
| 102 patients with DVT, treated with LMWH, compression4 | Bed rest for 5 days Ambulation | No differences in PE, thrombus progression, serious adverse events, or leg pain Study didn’t recruit expected number of patients Study showed a trend toward benefit from ambulation |
| 53 patients with DVT2,7 | Ambulation and use of firm, inelastic Unna boot bandages Ambulation and elastic compression stockings Strict bed rest for 9 days and no compression | No difference in quality of life or PE DVT-related symptoms, leg pain, and circumference improved in compression/ambulation groups No changes noted at 2 years |
| 72 patients with DVT, treated with anticoagulation and compression3 | Daily walking exercise and weekly group exercise Control group | No difference in DVT, PE, phlebography results, or calf circumference |
| DVT, deep vein thrombosis; LMWH, low-molecular-weight heparin; PE, pulmonary embolism. | ||
Does ambulation affect thrombus propagation?
A multicenter RCT showed that thrombus progression occurred more often in patients who were treated with bed rest compared with patients treated with ambulation and compression (P<.01).2
Another RCT revealed a similar trend, though the difference didn’t reach statistical significance because of small sample size.4 The clinical importance of these phlebographic studies isn’t clear.
Is it the walking, or compression, that works?
RCTs have shown that ambulation with leg compression, compared with bed rest without compression, can effectively decrease leg swelling and pain1,2,4 The difference was detectable 2 years after DVT.7
In contrast, RCTs in which both ambulating and resting patients received compression therapy showed no significant difference in leg circumference at 1 or 6 months.3 This finding suggests that the benefit on local symptoms may result from compression rather than ambulation.
Reduced mortality? Evidence is weak
Estimates of the possible effect on mortality of ambulation compared with bed rest are based on cohort studies. A cohort study in which 691 patients were kept walking with compression therapy reported a mortality rate of 0.2%.9 In another cohort, the mortality rate was also 0.2%, and all deaths occurred in patients older than 70 years.10
This rate is lower than rates reported in the historic literature, which typically are 1% among patients treated with unfractionated heparin and bed rest.9,10 A retrospective, multicenter cohort of 1647 patients treated with unfractionated heparin and bed rest in different German hospitals reported a rate of fatal PE of 2.33%.11
Data from the RIETE registry indicated that overall mortality was significantly higher in immobilized patients with a PE (3.6% vs 0.5% in mobile patients; P=.01).8 Notably, immobilized patients with a PE were more likely to be hypoxic and also tended to receive lower doses of LMWH. No differences were found in outcomes for patients with DVT.
Recommendations
The American College of Chest Physicians (ACCP) doesn’t recommend bed rest in its guidelines for treating acute venous thromboembolism, but rather ambulation as tolerated after starting anticoagulation. Patients who are not hemodynamically stable should be stabilized first.
The ACCP also recommends wearing an elastic compression stocking with a pressure of 30 to 40 mm Hg at the ankle for 2 years after an episode of DVT and a course of intermittent pneumatic compression for patients with severe edema of the leg resulting from post-thrombotic syndrome.12
A joint guideline from the American College of Physicians and the American Academy of Family Physicians doesn’t make recommendations about ambulation for therapy of DVT and PE.13
PROBABLY NOT. Ambulation, combined with compression of the affected extremity, appears to be safe for medically stable patients with deep venous thromboses (DVT) (strength of recommendation [SOR]: A, consistent randomized controlled trials [RCTs]). Leg compression and ambulation, compared with bed rest without compression, can effectively decrease swelling and pain (SOR: A, consistent RCTs).
Only weak data exist to suggest that early ambulation can reduce mortality (SOR: C, cohort studies with historical controls).
Evidence summary
Patients with acute DVT have traditionally been treated with immobilization and bed rest, combined with anticoagulation, for days. This approach is motivated by fear of dislodging an unstable thrombus and causing a pulmonary embolism (PE) and by the belief that inactivity relieves local pain and swelling. On the other hand, bed rest promotes stasis, an element in Virchow’s triad.
Early ambulation doesn’t raise risk of PE
We performed a structured literature review, which found 6 RCTs and 3 cohort studies that address this problem. All 6 RCTs included patients with acute DVT but without life-threatening conditions.1-6 They assessed various outcomes, including incidence of new PE, change in leg circumference, leg pain, patient well-being, and progression of DVT.
The studies consistently found that early ambulation, along with compression, is safe when compared with bed rest ( TABLE ). Although the sample size of all the RCTs was small, the RCTs showed consistent trends in favor of ambulation and compression.
A prospective cohort study of new PE in patients treated with ambulation and compression plus anticoagulation found that the incidence of PE was significantly lower than historical incidence rates in patients managed with bed rest.7
Another study using the RIETE registry, a Spanish registry of consecutively enrolled patients with objectively confirmed acute DVT or PE, found no significant difference in occurrence of new PE between immobilized and mobilized patients.8 Patients with DVT who were immobilized were generally sicker, more likely to have PaO2 <60, and more likely to have received lower doses of low-molecular-weight heparin (LMWH) compared with the group that walked (P<.005).
TABLE
Early ambulation and compression: What RCTs show
| Subjects | Study groups | Results |
|---|---|---|
| 129 patients with DVT, treated with LMWH1 | Strict immobilization for 4 days Ambulation for ≥4 h/d, along with compression for 4 days or until swelling subsided | At 4 days: No difference in PE, leg pain, leg size, mortality At 3 months: No difference in PE, mortality |
| 146 patients with DVT, all anticoagulated5 | Hospital treatment with 5 days of bed rest Home care with early walking and compression stockings | No difference in occurrence of new PE after 10 days |
| 126 patients with DVT, treated with LMWH, compression6 | Strict bed rest for 8 days with leg elevation Began full ambulation on day 2 | No difference in PE |
| 102 patients with DVT, treated with LMWH, compression4 | Bed rest for 5 days Ambulation | No differences in PE, thrombus progression, serious adverse events, or leg pain Study didn’t recruit expected number of patients Study showed a trend toward benefit from ambulation |
| 53 patients with DVT2,7 | Ambulation and use of firm, inelastic Unna boot bandages Ambulation and elastic compression stockings Strict bed rest for 9 days and no compression | No difference in quality of life or PE DVT-related symptoms, leg pain, and circumference improved in compression/ambulation groups No changes noted at 2 years |
| 72 patients with DVT, treated with anticoagulation and compression3 | Daily walking exercise and weekly group exercise Control group | No difference in DVT, PE, phlebography results, or calf circumference |
| DVT, deep vein thrombosis; LMWH, low-molecular-weight heparin; PE, pulmonary embolism. | ||
Does ambulation affect thrombus propagation?
A multicenter RCT showed that thrombus progression occurred more often in patients who were treated with bed rest compared with patients treated with ambulation and compression (P<.01).2
Another RCT revealed a similar trend, though the difference didn’t reach statistical significance because of small sample size.4 The clinical importance of these phlebographic studies isn’t clear.
Is it the walking, or compression, that works?
RCTs have shown that ambulation with leg compression, compared with bed rest without compression, can effectively decrease leg swelling and pain1,2,4 The difference was detectable 2 years after DVT.7
In contrast, RCTs in which both ambulating and resting patients received compression therapy showed no significant difference in leg circumference at 1 or 6 months.3 This finding suggests that the benefit on local symptoms may result from compression rather than ambulation.
Reduced mortality? Evidence is weak
Estimates of the possible effect on mortality of ambulation compared with bed rest are based on cohort studies. A cohort study in which 691 patients were kept walking with compression therapy reported a mortality rate of 0.2%.9 In another cohort, the mortality rate was also 0.2%, and all deaths occurred in patients older than 70 years.10
This rate is lower than rates reported in the historic literature, which typically are 1% among patients treated with unfractionated heparin and bed rest.9,10 A retrospective, multicenter cohort of 1647 patients treated with unfractionated heparin and bed rest in different German hospitals reported a rate of fatal PE of 2.33%.11
Data from the RIETE registry indicated that overall mortality was significantly higher in immobilized patients with a PE (3.6% vs 0.5% in mobile patients; P=.01).8 Notably, immobilized patients with a PE were more likely to be hypoxic and also tended to receive lower doses of LMWH. No differences were found in outcomes for patients with DVT.
Recommendations
The American College of Chest Physicians (ACCP) doesn’t recommend bed rest in its guidelines for treating acute venous thromboembolism, but rather ambulation as tolerated after starting anticoagulation. Patients who are not hemodynamically stable should be stabilized first.
The ACCP also recommends wearing an elastic compression stocking with a pressure of 30 to 40 mm Hg at the ankle for 2 years after an episode of DVT and a course of intermittent pneumatic compression for patients with severe edema of the leg resulting from post-thrombotic syndrome.12
A joint guideline from the American College of Physicians and the American Academy of Family Physicians doesn’t make recommendations about ambulation for therapy of DVT and PE.13
1. Aschwanden M, Labs KH, Engel H, et al. Acute deep vein thrombosis: early mobilization does not increase the frequency of pulmonary embolism. Thromb Haemost. 2001;85:42-46.
2. Blattler W, Partsch H. Leg compression and ambulation is better than bed rest for the treatment of acute deep venous thrombosis. Int Angiol. 2003;22:393-400.
3. Isma N, Johanssson E, Bjork A, et al. Does supervised exercise after deep venous thrombosis improve recanalization of occluded vein segments? A randomized study. J Thromb Thrombolysis. 2007;23:25-30.
4. Junger M, Diehm C, Storiko H, et al. Mobilization versus immobilization in the treatment of acute proximal deep venous thrombosis: a prospective, randomized, open, multicentre trial. Curr Med Res Opin. 2006;22:593-602.
5. Romera A, Vila R, Perez-Piqueras A, et al. Early mobilization in patients with acute deep vein thrombosis: does it increase the incidence of symptomatic pulmonary embolism? Phlebology. 2005;20:141.-
6. Schellong SM, Schwarz T, Kropp J, et al. Bed rest in deep vein thrombosis and the incidence of scintigraphic pulmonary embolism. Thromb Haemost. 1999;82(suppl 1):127-129.
7. Partsch H, Kaulich M, Mayer W. Immediate mobilisation in acute vein thrombosis reduces post-thrombotic syndrome. Int Angiol. 2004;23:206-212.
8. Trujillo-Santos J, Perea-Milla E, Jimenez-Puente A, et al. Bed rest or ambulation in the initial treatment of patients with acute deep vein thrombosis or pulmonary embolism: findings from the RIETE registry. Chest. 2005;127:1631-1636.
9. Partsch H, Kechavarz B, Kohn H, et al. The effect of mobilisation of patients during treatment of thromboembolic disorders with low-molecular-weight heparin. Int Angiol. 1997;16:189-192.
10. Partsch H. Therapy of deep vein thrombosis with low molecular weight heparin, leg compression and immediate ambulation. Vasa. 2001;30:195-204.
11. Martin M. PHLECO: a multicenter study of the fate of 1647 hospital patients treated conservatively without fibrinolysis and surgery. Clin Invest. 1993;71:471-477.
12. Buller HR, Agnelli G, Hull RD, et al. Antithrombotic therapy for venous thromboembolic disease: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest. 2004;126 (suppl 3):401S-428S.
13. Snow V, Qaseem A, Barry P, et al. Management of venous thromboembolism: a clinical practice guideline from the American College of Physicians and the American Academy of Family Physicians. Ann Intern Med. 2007;146:204-210.
1. Aschwanden M, Labs KH, Engel H, et al. Acute deep vein thrombosis: early mobilization does not increase the frequency of pulmonary embolism. Thromb Haemost. 2001;85:42-46.
2. Blattler W, Partsch H. Leg compression and ambulation is better than bed rest for the treatment of acute deep venous thrombosis. Int Angiol. 2003;22:393-400.
3. Isma N, Johanssson E, Bjork A, et al. Does supervised exercise after deep venous thrombosis improve recanalization of occluded vein segments? A randomized study. J Thromb Thrombolysis. 2007;23:25-30.
4. Junger M, Diehm C, Storiko H, et al. Mobilization versus immobilization in the treatment of acute proximal deep venous thrombosis: a prospective, randomized, open, multicentre trial. Curr Med Res Opin. 2006;22:593-602.
5. Romera A, Vila R, Perez-Piqueras A, et al. Early mobilization in patients with acute deep vein thrombosis: does it increase the incidence of symptomatic pulmonary embolism? Phlebology. 2005;20:141.-
6. Schellong SM, Schwarz T, Kropp J, et al. Bed rest in deep vein thrombosis and the incidence of scintigraphic pulmonary embolism. Thromb Haemost. 1999;82(suppl 1):127-129.
7. Partsch H, Kaulich M, Mayer W. Immediate mobilisation in acute vein thrombosis reduces post-thrombotic syndrome. Int Angiol. 2004;23:206-212.
8. Trujillo-Santos J, Perea-Milla E, Jimenez-Puente A, et al. Bed rest or ambulation in the initial treatment of patients with acute deep vein thrombosis or pulmonary embolism: findings from the RIETE registry. Chest. 2005;127:1631-1636.
9. Partsch H, Kechavarz B, Kohn H, et al. The effect of mobilisation of patients during treatment of thromboembolic disorders with low-molecular-weight heparin. Int Angiol. 1997;16:189-192.
10. Partsch H. Therapy of deep vein thrombosis with low molecular weight heparin, leg compression and immediate ambulation. Vasa. 2001;30:195-204.
11. Martin M. PHLECO: a multicenter study of the fate of 1647 hospital patients treated conservatively without fibrinolysis and surgery. Clin Invest. 1993;71:471-477.
12. Buller HR, Agnelli G, Hull RD, et al. Antithrombotic therapy for venous thromboembolic disease: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest. 2004;126 (suppl 3):401S-428S.
13. Snow V, Qaseem A, Barry P, et al. Management of venous thromboembolism: a clinical practice guideline from the American College of Physicians and the American Academy of Family Physicians. Ann Intern Med. 2007;146:204-210.
Evidence-based answers from the Family Physicians Inquiries Network
Vertebroplasty for osteoporotic fracture? Think twice
Think twice before recommending vertebroplasty (VP) for symptomatic osteoporotic compression fractures. New studies suggest that it has little benefit; thus, VP should be considered only after other, more conservative options fail.1,2
STRENGTH OF RECOMMENDATION
A: Consistent, high-quality randomized controlled trials (RCTs)
Kallmes DF, Comstock BA, Heagerty PJ, et al. A randomized trial of vertebroplasty for osteoporotic spinal fractures. N Engl J Med. 2009;361:569-579.
Buchbinder R, Osborne RH, Ebeling PR, et al. A randomized trial of vertebroplasty for painful osteoporotic vertebral fractures. N Engl J Med. 2009;361:557-568.
ILLUSTRATIVE CASE
A 72-year-old woman with a history of osteoporosis is being treated with a bisphosphonate, calcium, and vitamin D. She’s in your office today because of the sudden onset of midline lower back pain after minor trauma. X-ray reveals an uncomplicated osteoporotic fracture of L2, with 50% loss of vertebral height. When she returns in a few weeks, the patient still has significant pain (7 on a scale of 0-10) that is not well controlled with hydrocodone and acetaminophen. Should you refer her for vertebroplasty?
Each year in the United States, approximately 750,000 vertebral fractures occur.3 The traditional treatments for osteoporotic vertebral compression fractures include bed rest, pain medication, braces, and therapy for osteoporosis. Since the late 1990s, however, vertebroplasty (VP)—the percutaneous injection of acrylic bone cement (polymethylmethacrylate, or PMMA) into the affected vertebra under radiologic guidance—has become the preferred treatment, particularly for painful vertebral fractures that do not respond to conservative treatment.
Widely used, but not much evidence
Despite a lack of rigorous scientific evidence of VP’s efficacy, the number of procedures nearly doubled from 2001 to 2005 among Medicare enrollees—from 45 per 100,000 to 87 per 100,000.4 A meta-analysis of 74 (mostly observational) studies of VP for osteoporotic compression fractures found good evidence for improved pain control in the first 2 weeks. At 3 months, the analysis found only fair evidence of benefit, and at 2 years, there was no apparent benefit.5
Complications are primarily related to cement extravasation, but are usually not symptomatic. The overall symptomatic complication rate is less than 4%.6 There is conflicting evidence regarding whether VP increases the risk of fracture in other vertebrae.7
Prior to the 2 studies reviewed in this PURL, there were only 2 RCTs comparing vertebroplasty with conservative medical management. The VERTOS trial8 randomized 34 people with osteoporotic vertebral compression fractures (of 6 weeks’ to 6 months’ duration and refractory to medical therapy) to either VP or conservative treatment. The VP patients had improved pain scores and decreased use of analgesic agents at 24 hours, compared with the conservative treatment group. But at the end of the 2-week trial, there was no difference in pain scores between the 2 groups.
The other RCT of VP vs conservative therapy randomized 50 patients with acute or subacute osteoporotic fractures (the average age of fracture was 6-8 days) to VP or conservative care.9 There was significant pain improvement in VP patients at 24 hours, but no significant difference in pain scores between the 2 groups at 3 months. This study was significantly flawed, however, because the researchers failed to collect pain measurements at study entry for a substantial number of patients.
STUDY SUMMARIES: Vertebroplasty lacks benefits
Both INVEST (the Kallmes study)1 and the Buchbinder study2 were blinded, randomized, placebo-controlled trials of VP. INVEST, performed at 11 sites in the United States, United Kingdom, and Australia, enrolled 131 patients. The Buchbinder study enrolled 78 patients at 4 sites in Australia. Both enrolled patients with painful osteoporotic fractures of less than 1 year’s duration. Exclusions for both trials included a suspicion of neoplasm in the vertebral body, substantial retropulsion of bony fragments, medical conditions that would preclude surgery, and an inability to obtain consent or conduct follow-up.
Participants in both trials had similar baseline characteristics: They were primarily Caucasian and female, with an average age in the mid-70s. The average pain intensity at enrollment was about 7 on a 0- to 10-point visual analog scale (VAS). The average time since the fracture causing the pain was 4 to 5 months in INVEST and about 2 months in the Buchbinder study. Both trials used appropriate randomization, blinding, and intention-to-treat analysis.
Blinding featured sham procedures. In both studies, the researchers used elaborate measures to ensure blinding: The control patients were prepped in the fluoroscopy suite as if they were about to undergo VP. They received local anesthesia down to the periosteum of the vertebra. The PMMA was opened and mixed in the room to allow its distinctive smell to permeate. Patients also received verbal and physical cues that simulated the procedure, and spinal images were obtained.
INVEST used pain and disability at 1 month as the primary end points. There was minimal difference in pain intensity (3.9 on VAS for the VP group, vs 4.6 for the controls). There was also little difference in back pain-related disability at 1 month, with scores on the Roland Morris Disability scale decreasing (from a baseline of 16.6 for the VP group and 17.5 for the control group) to 12 and 13, respectively (P=.49). Nor were there any statistically significant differences in pain or disability at earlier intervals (the researchers compared the scores of the VP and control groups at 3 days and 14 days.) The authors also looked at 7 other measures of pain and functioning and found no significant differences in any of them at the end of 1 month.
To encourage enrollment, patients in the INVEST trial were allowed to cross over after 1 month. At that time, 12% of those in the VP group and 43% of those in the control group took advantage of this provision and had the alternate “procedure.” Both groups of cross-over patients had more pain than those who did not make the switch. Although both of these groups showed improvement at the 3-month mark, they still had higher pain levels than their counterparts who did not cross over.
The Buchbinder study used overall pain on a 10-point VAS at 3 months as its primary end point. The researchers also recorded 7 other measurements and assessed participants at 1 week, 1 month, 3 months, and 6 months. At 3 months, there was no significant difference in the change in pain scores between the treatment and placebo groups: Mean pain scores for those who underwent VP decreased from 7.4 to 5.1, while the placebo group’s average pain scores went from 7.1 to 5.4. Similarly, there was no difference between the treatment and placebo groups in the change in pain scores at 1 week or 6 months—and no difference between the groups at any time for the other 7 measures of pain and function.
WHAT’S NEW: Trials cast doubt on established procedure
VP has essentially become the standard of care for painful osteoporotic vertebral fractures, bolstered by a long list of methodologically inferior studies that have lent support to the procedure’s efficacy. These 2 studies are the first to incorporate a sham procedure that supports true placebo control. The complete lack of benefit for VP compared with conservative management in these well-done trials calls into question the results of prior reports.
CAVEATS: Sample size, study design
Researchers in both studies had considerable difficulty enrolling patients. Both were multi center trials and enrolled patients over a 4-year period; nonetheless, taken together, only about 200 patients consented. The researchers faced opposition from referring doctors and patients alike, who believed that the possibility of receiving a placebo treatment rather than VP constituted inferior care.
In addition to their relatively small size, these studies enrolled patients with fairly chronic fractures. It has been postulated that VP has a higher likelihood of success with acute fractures, but that was not the focus of these trials. The majority of the fractures in trial participants were not acute (<4 weeks). Neither trial was designed for analysis based on the chronicity of the fracture, and neither found a difference in outcome based on fracture duration.
Because these trials were not designed, or robust enough, for subgroup analysis, we don’t know if there is a population that might benefit (ie, severity of the compression, acuteness of the fracture, or premorbid health, etc). In addition, these results do not apply to the use of VP for other reasons—malignant spinal neoplasms or vertebral hemangiomas, for example.
Finally, it is important to remember that these trials did not strictly compare VP with conservative treatment. The sham treatment may have had significant placebo power that is greater than that of typical conservative treatment.
CHALLENGES TO IMPLEMENTATION: Support for VP is well established
Anecdotal results, established treatment patterns, and numerous low-quality studies support the use of VP for vertebral compression fracture. Medicare and other insurers had reviewed the evidence prior to these 2 trials and agreed to reimburse for the procedure. It remains to be seen whether these 2 trials will be sufficient to overcome these barriers and change practice patterns.
At a minimum, however, it is prudent to reserve VP for patients who have intractable symptoms until further trials are undertaken to determine whether VP really works, and if so, for which patients.
Acknowledgement
The PURLs Surveillance System is supported in part by Grant Number UL1RR024999 from the National Center for Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
1. Kallmes DF, Comstock BA, Heagerty PJ, et al. A randomized trial of vertebroplasty for osteoporotic spinal fractures. N Engl J Med. 2009;361:569-579.
2. Buchbinder R, Osborne RH, Ebeling PR, et al. A randomized trial of vertebroplasty for painful osteoporotic vertebral fractures. N Engl J Med. 2009;361:557-568.
3. Weinstein JN. Balancing science and informed choice in decisions about vertebroplasty. N Engl J Med. 2009;361:619-621.
4. Gray DT, Hollingworth W, Onwudiwe N, et al. Thoracic and lumbar vertebroplasties performed in US Medicare enrollees, 2001-2005. JAMA. 2007;298:1760-1762.
5. McGirt MJ, Parker SL, Wolinsky JP, et al. Vertebroplasty and kyphoplasty for the treatment of vertebral compression fractures: an evidenced-based review of the literature. Spine J. 2009;9:501-508.
6. Lee MJ, Dumonski M, Cahill P, et al. Percutaneous treatment of vertebral compression fractures: a meta-analysis of complications. Spine. 2009;34:1228-1232.
7. Hulme PA, Krebs J, Ferguson S, et al. Vertebroplasty and kyphoplasty: a systematic review of 69 clinical studies. Spine. 2006;31:1983-2001.
8. Voormolen MH, Mali WP, Lohle PN, et al. Percutaneous vertebroplasty compared with optimal pain medication treatment: short-term clinical outcome of patients with subacute or chronic painful osteoporotic vertebral compression fractures. The VERTOS study. AJNR Am J Neuroradiol. 2007;28:555-560.
9. Rousing R, Andersen MO, Jespersen SM, et al. Percutaneous vertebroplasty compared to conservative treatment in patients with painful acute or subacute osteoporotic vertebral fractures: three-months follow-up in a clinical randomized study. Spine. 2009;34:1349-1354.
Think twice before recommending vertebroplasty (VP) for symptomatic osteoporotic compression fractures. New studies suggest that it has little benefit; thus, VP should be considered only after other, more conservative options fail.1,2
STRENGTH OF RECOMMENDATION
A: Consistent, high-quality randomized controlled trials (RCTs)
Kallmes DF, Comstock BA, Heagerty PJ, et al. A randomized trial of vertebroplasty for osteoporotic spinal fractures. N Engl J Med. 2009;361:569-579.
Buchbinder R, Osborne RH, Ebeling PR, et al. A randomized trial of vertebroplasty for painful osteoporotic vertebral fractures. N Engl J Med. 2009;361:557-568.
ILLUSTRATIVE CASE
A 72-year-old woman with a history of osteoporosis is being treated with a bisphosphonate, calcium, and vitamin D. She’s in your office today because of the sudden onset of midline lower back pain after minor trauma. X-ray reveals an uncomplicated osteoporotic fracture of L2, with 50% loss of vertebral height. When she returns in a few weeks, the patient still has significant pain (7 on a scale of 0-10) that is not well controlled with hydrocodone and acetaminophen. Should you refer her for vertebroplasty?
Each year in the United States, approximately 750,000 vertebral fractures occur.3 The traditional treatments for osteoporotic vertebral compression fractures include bed rest, pain medication, braces, and therapy for osteoporosis. Since the late 1990s, however, vertebroplasty (VP)—the percutaneous injection of acrylic bone cement (polymethylmethacrylate, or PMMA) into the affected vertebra under radiologic guidance—has become the preferred treatment, particularly for painful vertebral fractures that do not respond to conservative treatment.
Widely used, but not much evidence
Despite a lack of rigorous scientific evidence of VP’s efficacy, the number of procedures nearly doubled from 2001 to 2005 among Medicare enrollees—from 45 per 100,000 to 87 per 100,000.4 A meta-analysis of 74 (mostly observational) studies of VP for osteoporotic compression fractures found good evidence for improved pain control in the first 2 weeks. At 3 months, the analysis found only fair evidence of benefit, and at 2 years, there was no apparent benefit.5
Complications are primarily related to cement extravasation, but are usually not symptomatic. The overall symptomatic complication rate is less than 4%.6 There is conflicting evidence regarding whether VP increases the risk of fracture in other vertebrae.7
Prior to the 2 studies reviewed in this PURL, there were only 2 RCTs comparing vertebroplasty with conservative medical management. The VERTOS trial8 randomized 34 people with osteoporotic vertebral compression fractures (of 6 weeks’ to 6 months’ duration and refractory to medical therapy) to either VP or conservative treatment. The VP patients had improved pain scores and decreased use of analgesic agents at 24 hours, compared with the conservative treatment group. But at the end of the 2-week trial, there was no difference in pain scores between the 2 groups.
The other RCT of VP vs conservative therapy randomized 50 patients with acute or subacute osteoporotic fractures (the average age of fracture was 6-8 days) to VP or conservative care.9 There was significant pain improvement in VP patients at 24 hours, but no significant difference in pain scores between the 2 groups at 3 months. This study was significantly flawed, however, because the researchers failed to collect pain measurements at study entry for a substantial number of patients.
STUDY SUMMARIES: Vertebroplasty lacks benefits
Both INVEST (the Kallmes study)1 and the Buchbinder study2 were blinded, randomized, placebo-controlled trials of VP. INVEST, performed at 11 sites in the United States, United Kingdom, and Australia, enrolled 131 patients. The Buchbinder study enrolled 78 patients at 4 sites in Australia. Both enrolled patients with painful osteoporotic fractures of less than 1 year’s duration. Exclusions for both trials included a suspicion of neoplasm in the vertebral body, substantial retropulsion of bony fragments, medical conditions that would preclude surgery, and an inability to obtain consent or conduct follow-up.
Participants in both trials had similar baseline characteristics: They were primarily Caucasian and female, with an average age in the mid-70s. The average pain intensity at enrollment was about 7 on a 0- to 10-point visual analog scale (VAS). The average time since the fracture causing the pain was 4 to 5 months in INVEST and about 2 months in the Buchbinder study. Both trials used appropriate randomization, blinding, and intention-to-treat analysis.
Blinding featured sham procedures. In both studies, the researchers used elaborate measures to ensure blinding: The control patients were prepped in the fluoroscopy suite as if they were about to undergo VP. They received local anesthesia down to the periosteum of the vertebra. The PMMA was opened and mixed in the room to allow its distinctive smell to permeate. Patients also received verbal and physical cues that simulated the procedure, and spinal images were obtained.
INVEST used pain and disability at 1 month as the primary end points. There was minimal difference in pain intensity (3.9 on VAS for the VP group, vs 4.6 for the controls). There was also little difference in back pain-related disability at 1 month, with scores on the Roland Morris Disability scale decreasing (from a baseline of 16.6 for the VP group and 17.5 for the control group) to 12 and 13, respectively (P=.49). Nor were there any statistically significant differences in pain or disability at earlier intervals (the researchers compared the scores of the VP and control groups at 3 days and 14 days.) The authors also looked at 7 other measures of pain and functioning and found no significant differences in any of them at the end of 1 month.
To encourage enrollment, patients in the INVEST trial were allowed to cross over after 1 month. At that time, 12% of those in the VP group and 43% of those in the control group took advantage of this provision and had the alternate “procedure.” Both groups of cross-over patients had more pain than those who did not make the switch. Although both of these groups showed improvement at the 3-month mark, they still had higher pain levels than their counterparts who did not cross over.
The Buchbinder study used overall pain on a 10-point VAS at 3 months as its primary end point. The researchers also recorded 7 other measurements and assessed participants at 1 week, 1 month, 3 months, and 6 months. At 3 months, there was no significant difference in the change in pain scores between the treatment and placebo groups: Mean pain scores for those who underwent VP decreased from 7.4 to 5.1, while the placebo group’s average pain scores went from 7.1 to 5.4. Similarly, there was no difference between the treatment and placebo groups in the change in pain scores at 1 week or 6 months—and no difference between the groups at any time for the other 7 measures of pain and function.
WHAT’S NEW: Trials cast doubt on established procedure
VP has essentially become the standard of care for painful osteoporotic vertebral fractures, bolstered by a long list of methodologically inferior studies that have lent support to the procedure’s efficacy. These 2 studies are the first to incorporate a sham procedure that supports true placebo control. The complete lack of benefit for VP compared with conservative management in these well-done trials calls into question the results of prior reports.
CAVEATS: Sample size, study design
Researchers in both studies had considerable difficulty enrolling patients. Both were multi center trials and enrolled patients over a 4-year period; nonetheless, taken together, only about 200 patients consented. The researchers faced opposition from referring doctors and patients alike, who believed that the possibility of receiving a placebo treatment rather than VP constituted inferior care.
In addition to their relatively small size, these studies enrolled patients with fairly chronic fractures. It has been postulated that VP has a higher likelihood of success with acute fractures, but that was not the focus of these trials. The majority of the fractures in trial participants were not acute (<4 weeks). Neither trial was designed for analysis based on the chronicity of the fracture, and neither found a difference in outcome based on fracture duration.
Because these trials were not designed, or robust enough, for subgroup analysis, we don’t know if there is a population that might benefit (ie, severity of the compression, acuteness of the fracture, or premorbid health, etc). In addition, these results do not apply to the use of VP for other reasons—malignant spinal neoplasms or vertebral hemangiomas, for example.
Finally, it is important to remember that these trials did not strictly compare VP with conservative treatment. The sham treatment may have had significant placebo power that is greater than that of typical conservative treatment.
CHALLENGES TO IMPLEMENTATION: Support for VP is well established
Anecdotal results, established treatment patterns, and numerous low-quality studies support the use of VP for vertebral compression fracture. Medicare and other insurers had reviewed the evidence prior to these 2 trials and agreed to reimburse for the procedure. It remains to be seen whether these 2 trials will be sufficient to overcome these barriers and change practice patterns.
At a minimum, however, it is prudent to reserve VP for patients who have intractable symptoms until further trials are undertaken to determine whether VP really works, and if so, for which patients.
Acknowledgement
The PURLs Surveillance System is supported in part by Grant Number UL1RR024999 from the National Center for Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
Think twice before recommending vertebroplasty (VP) for symptomatic osteoporotic compression fractures. New studies suggest that it has little benefit; thus, VP should be considered only after other, more conservative options fail.1,2
STRENGTH OF RECOMMENDATION
A: Consistent, high-quality randomized controlled trials (RCTs)
Kallmes DF, Comstock BA, Heagerty PJ, et al. A randomized trial of vertebroplasty for osteoporotic spinal fractures. N Engl J Med. 2009;361:569-579.
Buchbinder R, Osborne RH, Ebeling PR, et al. A randomized trial of vertebroplasty for painful osteoporotic vertebral fractures. N Engl J Med. 2009;361:557-568.
ILLUSTRATIVE CASE
A 72-year-old woman with a history of osteoporosis is being treated with a bisphosphonate, calcium, and vitamin D. She’s in your office today because of the sudden onset of midline lower back pain after minor trauma. X-ray reveals an uncomplicated osteoporotic fracture of L2, with 50% loss of vertebral height. When she returns in a few weeks, the patient still has significant pain (7 on a scale of 0-10) that is not well controlled with hydrocodone and acetaminophen. Should you refer her for vertebroplasty?
Each year in the United States, approximately 750,000 vertebral fractures occur.3 The traditional treatments for osteoporotic vertebral compression fractures include bed rest, pain medication, braces, and therapy for osteoporosis. Since the late 1990s, however, vertebroplasty (VP)—the percutaneous injection of acrylic bone cement (polymethylmethacrylate, or PMMA) into the affected vertebra under radiologic guidance—has become the preferred treatment, particularly for painful vertebral fractures that do not respond to conservative treatment.
Widely used, but not much evidence
Despite a lack of rigorous scientific evidence of VP’s efficacy, the number of procedures nearly doubled from 2001 to 2005 among Medicare enrollees—from 45 per 100,000 to 87 per 100,000.4 A meta-analysis of 74 (mostly observational) studies of VP for osteoporotic compression fractures found good evidence for improved pain control in the first 2 weeks. At 3 months, the analysis found only fair evidence of benefit, and at 2 years, there was no apparent benefit.5
Complications are primarily related to cement extravasation, but are usually not symptomatic. The overall symptomatic complication rate is less than 4%.6 There is conflicting evidence regarding whether VP increases the risk of fracture in other vertebrae.7
Prior to the 2 studies reviewed in this PURL, there were only 2 RCTs comparing vertebroplasty with conservative medical management. The VERTOS trial8 randomized 34 people with osteoporotic vertebral compression fractures (of 6 weeks’ to 6 months’ duration and refractory to medical therapy) to either VP or conservative treatment. The VP patients had improved pain scores and decreased use of analgesic agents at 24 hours, compared with the conservative treatment group. But at the end of the 2-week trial, there was no difference in pain scores between the 2 groups.
The other RCT of VP vs conservative therapy randomized 50 patients with acute or subacute osteoporotic fractures (the average age of fracture was 6-8 days) to VP or conservative care.9 There was significant pain improvement in VP patients at 24 hours, but no significant difference in pain scores between the 2 groups at 3 months. This study was significantly flawed, however, because the researchers failed to collect pain measurements at study entry for a substantial number of patients.
STUDY SUMMARIES: Vertebroplasty lacks benefits
Both INVEST (the Kallmes study)1 and the Buchbinder study2 were blinded, randomized, placebo-controlled trials of VP. INVEST, performed at 11 sites in the United States, United Kingdom, and Australia, enrolled 131 patients. The Buchbinder study enrolled 78 patients at 4 sites in Australia. Both enrolled patients with painful osteoporotic fractures of less than 1 year’s duration. Exclusions for both trials included a suspicion of neoplasm in the vertebral body, substantial retropulsion of bony fragments, medical conditions that would preclude surgery, and an inability to obtain consent or conduct follow-up.
Participants in both trials had similar baseline characteristics: They were primarily Caucasian and female, with an average age in the mid-70s. The average pain intensity at enrollment was about 7 on a 0- to 10-point visual analog scale (VAS). The average time since the fracture causing the pain was 4 to 5 months in INVEST and about 2 months in the Buchbinder study. Both trials used appropriate randomization, blinding, and intention-to-treat analysis.
Blinding featured sham procedures. In both studies, the researchers used elaborate measures to ensure blinding: The control patients were prepped in the fluoroscopy suite as if they were about to undergo VP. They received local anesthesia down to the periosteum of the vertebra. The PMMA was opened and mixed in the room to allow its distinctive smell to permeate. Patients also received verbal and physical cues that simulated the procedure, and spinal images were obtained.
INVEST used pain and disability at 1 month as the primary end points. There was minimal difference in pain intensity (3.9 on VAS for the VP group, vs 4.6 for the controls). There was also little difference in back pain-related disability at 1 month, with scores on the Roland Morris Disability scale decreasing (from a baseline of 16.6 for the VP group and 17.5 for the control group) to 12 and 13, respectively (P=.49). Nor were there any statistically significant differences in pain or disability at earlier intervals (the researchers compared the scores of the VP and control groups at 3 days and 14 days.) The authors also looked at 7 other measures of pain and functioning and found no significant differences in any of them at the end of 1 month.
To encourage enrollment, patients in the INVEST trial were allowed to cross over after 1 month. At that time, 12% of those in the VP group and 43% of those in the control group took advantage of this provision and had the alternate “procedure.” Both groups of cross-over patients had more pain than those who did not make the switch. Although both of these groups showed improvement at the 3-month mark, they still had higher pain levels than their counterparts who did not cross over.
The Buchbinder study used overall pain on a 10-point VAS at 3 months as its primary end point. The researchers also recorded 7 other measurements and assessed participants at 1 week, 1 month, 3 months, and 6 months. At 3 months, there was no significant difference in the change in pain scores between the treatment and placebo groups: Mean pain scores for those who underwent VP decreased from 7.4 to 5.1, while the placebo group’s average pain scores went from 7.1 to 5.4. Similarly, there was no difference between the treatment and placebo groups in the change in pain scores at 1 week or 6 months—and no difference between the groups at any time for the other 7 measures of pain and function.
WHAT’S NEW: Trials cast doubt on established procedure
VP has essentially become the standard of care for painful osteoporotic vertebral fractures, bolstered by a long list of methodologically inferior studies that have lent support to the procedure’s efficacy. These 2 studies are the first to incorporate a sham procedure that supports true placebo control. The complete lack of benefit for VP compared with conservative management in these well-done trials calls into question the results of prior reports.
CAVEATS: Sample size, study design
Researchers in both studies had considerable difficulty enrolling patients. Both were multi center trials and enrolled patients over a 4-year period; nonetheless, taken together, only about 200 patients consented. The researchers faced opposition from referring doctors and patients alike, who believed that the possibility of receiving a placebo treatment rather than VP constituted inferior care.
In addition to their relatively small size, these studies enrolled patients with fairly chronic fractures. It has been postulated that VP has a higher likelihood of success with acute fractures, but that was not the focus of these trials. The majority of the fractures in trial participants were not acute (<4 weeks). Neither trial was designed for analysis based on the chronicity of the fracture, and neither found a difference in outcome based on fracture duration.
Because these trials were not designed, or robust enough, for subgroup analysis, we don’t know if there is a population that might benefit (ie, severity of the compression, acuteness of the fracture, or premorbid health, etc). In addition, these results do not apply to the use of VP for other reasons—malignant spinal neoplasms or vertebral hemangiomas, for example.
Finally, it is important to remember that these trials did not strictly compare VP with conservative treatment. The sham treatment may have had significant placebo power that is greater than that of typical conservative treatment.
CHALLENGES TO IMPLEMENTATION: Support for VP is well established
Anecdotal results, established treatment patterns, and numerous low-quality studies support the use of VP for vertebral compression fracture. Medicare and other insurers had reviewed the evidence prior to these 2 trials and agreed to reimburse for the procedure. It remains to be seen whether these 2 trials will be sufficient to overcome these barriers and change practice patterns.
At a minimum, however, it is prudent to reserve VP for patients who have intractable symptoms until further trials are undertaken to determine whether VP really works, and if so, for which patients.
Acknowledgement
The PURLs Surveillance System is supported in part by Grant Number UL1RR024999 from the National Center for Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
1. Kallmes DF, Comstock BA, Heagerty PJ, et al. A randomized trial of vertebroplasty for osteoporotic spinal fractures. N Engl J Med. 2009;361:569-579.
2. Buchbinder R, Osborne RH, Ebeling PR, et al. A randomized trial of vertebroplasty for painful osteoporotic vertebral fractures. N Engl J Med. 2009;361:557-568.
3. Weinstein JN. Balancing science and informed choice in decisions about vertebroplasty. N Engl J Med. 2009;361:619-621.
4. Gray DT, Hollingworth W, Onwudiwe N, et al. Thoracic and lumbar vertebroplasties performed in US Medicare enrollees, 2001-2005. JAMA. 2007;298:1760-1762.
5. McGirt MJ, Parker SL, Wolinsky JP, et al. Vertebroplasty and kyphoplasty for the treatment of vertebral compression fractures: an evidenced-based review of the literature. Spine J. 2009;9:501-508.
6. Lee MJ, Dumonski M, Cahill P, et al. Percutaneous treatment of vertebral compression fractures: a meta-analysis of complications. Spine. 2009;34:1228-1232.
7. Hulme PA, Krebs J, Ferguson S, et al. Vertebroplasty and kyphoplasty: a systematic review of 69 clinical studies. Spine. 2006;31:1983-2001.
8. Voormolen MH, Mali WP, Lohle PN, et al. Percutaneous vertebroplasty compared with optimal pain medication treatment: short-term clinical outcome of patients with subacute or chronic painful osteoporotic vertebral compression fractures. The VERTOS study. AJNR Am J Neuroradiol. 2007;28:555-560.
9. Rousing R, Andersen MO, Jespersen SM, et al. Percutaneous vertebroplasty compared to conservative treatment in patients with painful acute or subacute osteoporotic vertebral fractures: three-months follow-up in a clinical randomized study. Spine. 2009;34:1349-1354.
1. Kallmes DF, Comstock BA, Heagerty PJ, et al. A randomized trial of vertebroplasty for osteoporotic spinal fractures. N Engl J Med. 2009;361:569-579.
2. Buchbinder R, Osborne RH, Ebeling PR, et al. A randomized trial of vertebroplasty for painful osteoporotic vertebral fractures. N Engl J Med. 2009;361:557-568.
3. Weinstein JN. Balancing science and informed choice in decisions about vertebroplasty. N Engl J Med. 2009;361:619-621.
4. Gray DT, Hollingworth W, Onwudiwe N, et al. Thoracic and lumbar vertebroplasties performed in US Medicare enrollees, 2001-2005. JAMA. 2007;298:1760-1762.
5. McGirt MJ, Parker SL, Wolinsky JP, et al. Vertebroplasty and kyphoplasty for the treatment of vertebral compression fractures: an evidenced-based review of the literature. Spine J. 2009;9:501-508.
6. Lee MJ, Dumonski M, Cahill P, et al. Percutaneous treatment of vertebral compression fractures: a meta-analysis of complications. Spine. 2009;34:1228-1232.
7. Hulme PA, Krebs J, Ferguson S, et al. Vertebroplasty and kyphoplasty: a systematic review of 69 clinical studies. Spine. 2006;31:1983-2001.
8. Voormolen MH, Mali WP, Lohle PN, et al. Percutaneous vertebroplasty compared with optimal pain medication treatment: short-term clinical outcome of patients with subacute or chronic painful osteoporotic vertebral compression fractures. The VERTOS study. AJNR Am J Neuroradiol. 2007;28:555-560.
9. Rousing R, Andersen MO, Jespersen SM, et al. Percutaneous vertebroplasty compared to conservative treatment in patients with painful acute or subacute osteoporotic vertebral fractures: three-months follow-up in a clinical randomized study. Spine. 2009;34:1349-1354.
Copyright © 2009 The Family Physicians Inquiries Network.
All rights reserved.
Bisphosphonate therapy: When not to monitor BMD
After starting patients on bisphosphonates for osteoporosis, wait at least 3 years before ordering a repeat dual-energy x-ray absorptiometry (DXA) scan.1
STRENGTH OF RECOMMENDATION
C: Based on a secondary analysis of a large randomized controlled trial.
Bell KL, Hayen A, Macaskill P, et al. Value of routine monitoring of bone mineral density after starting bisphosphonate treatment: secondary analysis of treatment data. BMJ. 2009;338:b2266.
ILLUSTRATIVE CASE
CASE: Ms. K, a 68-year-old woman diagnosed with osteoporosis on a screening DXA scan a year ago, has been taking a bisphosphonate ever since. She’s anxious to know whether the medication is working and asks if it’s time for a repeat DXA scan. What should you tell her?
Fragility fractures from osteoporosis are common in postmenopausal women. In the year 2000 alone, an estimated 9 million such fractures occurred worldwide.2 Treatment with bisphosphonates has been found to reduce the risk of fragility fractures,3 and the United States Preventive Services Task Force (USPSTF) recommends a DXA scan to screen for osteoporosis in women older than 65 years and some younger women at increased risk.4
Monitoring treatment: How often?
Although recommendations for how often to monitor bone mineral density (BMD) after initiating treatment vary, the consensus has been that periodic monitoring is useful. But there have been no randomized trials evaluating BMD testing in patients taking bisphosphonates.
The use of DXA scans to identify osteoporosis has been shown to be a cost-effective strategy in women older than 65 years,5 but there has not been a cost/benefit analysis of follow-up DXA scanning after initiating treatment. The cost of a scan ranges from about $150 to $300, and it is not known how many patients undergo repeat DXA scanning after starting treatment.
STUDY SUMMARY: Yearly scans are not helpful
The study we report on here is a secondary analysis of data from the Fracture Intervention Trial (FIT).6 In 1993, FIT randomized 6457 US women ages 55 to 80 years with low hip bone density to either alendronate or placebo. The initial dose of alendronate was 5 mg/d, but was later increased to 10 mg/d when other studies found that the higher dose was more effective. FIT showed that alendronate increased BMD and decreased the risk of vertebral fracture.7
Bell et al1 used a mixed-model statistical analysis to compare “within-person variation” in BMD (variation in DXA results over time in individuals) and “between-person variation” in BMD (variation in DXA results over time in the population of patients). The BMD of all FIT participants in both the control and treatment groups was measured at baseline and at the 1-, 2-, and 3-year marks. Each individual was always tested on the same scanner to minimize differences in machinery.
Individual results vary from year to year. The researchers found that the within-person variation was about 10 times greater than the between-person variation. This finding suggests that the precision of DXA scan measurements is not that reliable from 1 test to another.
The average annual increase in BMD in patients in the alendronate group was 0.0085 g/cm2—which is smaller than the typical year-to-year (within-person) variation of 0.013 g/cm2. It would therefore be difficult to differentiate the medication’s effect from the random variation inherent in DXA scans.
Response is favorable after 3 years of treatment. While there is variation in test results from year to year, longer-term findings are more reliable. After 3 years of treatment, 97.5% of patients taking alendronate had an increase in hip BMD of at least 0.019 g/cm2, with a strong correlation between hip and spine measurements. Although this represents a relatively small change in Z and T scores, this increase in hip BMD is considered a favorable response that warrants continued treatment. These findings are consistent with a previous analysis of BMD monitoring in women taking bisphosphonates, in which those who had the largest drop in BMD after the first year of treatment typically had a large gain over the second year.8
WHAT’S NEW: Now we know early testing is unnecessary
Not many studies are available to provide guidance about the interval between BMD measurements after starting a bisphosphonate. This study advises us that it is not necessary to recheck BMD for at least 3 years after starting treatment. Elimination of early repeat DXA testing could result in significant cost savings.
CAVEATS: Findings contradict usual recommendations
Physicians should be aware that the conclusion of this study is not in line with recommendations from a number of prominent organizations. The American Association of Clinical Endocrinology,9 the National Osteoporosis Foundation,10 and the North American Menopause Society11 all recommend follow-up DXA testing in 1 or 2 years.
High-risk patient exception. The delay in repeat DXA testing may not be appropriate for patients at higher risk of bone density loss. However, a separate analysis of higher-risk groups was not done.
Finally, while the findings of Bell et al suggest that we should wait at least 3 years before retesting, it is still not clear whether there is any benefit to repeat DXA testing at any interval, given the nearly universal response rate. It is also possible that advances in DXA technology will reduce some of the variation in BMD results.
CHALLENGES TO IMPLEMENTATION: Anxious patients
Patients like Ms. K may ask their physicians to retest well before 3 years. Yet those who undergo scanning after a shorter interval may be discouraged by early results. Advising patients that the treatment is almost uniformly effective in increasing BMD should reassure them that sticking with treatment is worthwhile.
Acknowledgment
The PURLs Surveillance System is supported in part by Grant Number UL1RR024999 from the National Center for Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
1. Bell KL, Hayen A, Macaskill P, et al. Value of routine monitoring of bone mineral density after starting bisphosphonate treatment: secondary analysis of treatment data. BMJ. 2009;338:b2266.-
2. Johnell O, Kanis JA. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int. 2006;17:1726.-
3. MacLean C, Newberry S, et al. Systematic review: comparative effectiveness of treatments to prevent fractures in men and women with low bone density or osteoporosis. Ann Intern Med. 2008;148:197-213.
4. Agency for Healthcare Research and Quality United States Preventive Services Task Force. Screening for osteoporosis in postmenopausal women. Available at: http://www.ahrq.gov/clinic/3rduspstf/osteoporosis/osteorr.htm . Accessed October 13, 2009.
5. Schousboe JT. Cost effectiveness of screen-and-treat strategies for low bone mineral density: how do we screen, who do we screen, and who do we treat? Appl Health Econ Health Policy. 2008;6:1-18.
6. Black DM, Nevitt MC, Cauley J, et al. Design of the fracture intervention trial. Osteopor Int. 2003;3(suppl 3):S29-S39.
7. Cummings S, Black D, Thompson D, et al. Effect of alendronate on risk of fracture in women with low bone density but without vertebral fractures. JAMA. 1998;280:2077-2082.
8. Cummings S, Palermo B, Browner W, et al. Monitoring osteoporosis therapy with bone densitometry: misleading changes and regression to the mean. Fracture Intervention Trial Research Group. JAMA. 2000;283:1318-1321.
9. AACE Osteoporosis Task Force American Association of Clinical Endocrinologists medical guidelines for clinical practice for the prevention and treatment of postmenopausal osteoporosis: 2001 edition with selected updates for 2003. Endocr Pract. 2003;9:544-564.
10. National Osteoporosis Foundation Clinician’s Guide to Prevention and Treatment of Osteoporosis. Washington DC: NOF; 2008.
11. Management of postmenopausal osteoporosis: position statement of the North American Menopause Society Menopause. 2002;9:84-101.
After starting patients on bisphosphonates for osteoporosis, wait at least 3 years before ordering a repeat dual-energy x-ray absorptiometry (DXA) scan.1
STRENGTH OF RECOMMENDATION
C: Based on a secondary analysis of a large randomized controlled trial.
Bell KL, Hayen A, Macaskill P, et al. Value of routine monitoring of bone mineral density after starting bisphosphonate treatment: secondary analysis of treatment data. BMJ. 2009;338:b2266.
ILLUSTRATIVE CASE
CASE: Ms. K, a 68-year-old woman diagnosed with osteoporosis on a screening DXA scan a year ago, has been taking a bisphosphonate ever since. She’s anxious to know whether the medication is working and asks if it’s time for a repeat DXA scan. What should you tell her?
Fragility fractures from osteoporosis are common in postmenopausal women. In the year 2000 alone, an estimated 9 million such fractures occurred worldwide.2 Treatment with bisphosphonates has been found to reduce the risk of fragility fractures,3 and the United States Preventive Services Task Force (USPSTF) recommends a DXA scan to screen for osteoporosis in women older than 65 years and some younger women at increased risk.4
Monitoring treatment: How often?
Although recommendations for how often to monitor bone mineral density (BMD) after initiating treatment vary, the consensus has been that periodic monitoring is useful. But there have been no randomized trials evaluating BMD testing in patients taking bisphosphonates.
The use of DXA scans to identify osteoporosis has been shown to be a cost-effective strategy in women older than 65 years,5 but there has not been a cost/benefit analysis of follow-up DXA scanning after initiating treatment. The cost of a scan ranges from about $150 to $300, and it is not known how many patients undergo repeat DXA scanning after starting treatment.
STUDY SUMMARY: Yearly scans are not helpful
The study we report on here is a secondary analysis of data from the Fracture Intervention Trial (FIT).6 In 1993, FIT randomized 6457 US women ages 55 to 80 years with low hip bone density to either alendronate or placebo. The initial dose of alendronate was 5 mg/d, but was later increased to 10 mg/d when other studies found that the higher dose was more effective. FIT showed that alendronate increased BMD and decreased the risk of vertebral fracture.7
Bell et al1 used a mixed-model statistical analysis to compare “within-person variation” in BMD (variation in DXA results over time in individuals) and “between-person variation” in BMD (variation in DXA results over time in the population of patients). The BMD of all FIT participants in both the control and treatment groups was measured at baseline and at the 1-, 2-, and 3-year marks. Each individual was always tested on the same scanner to minimize differences in machinery.
Individual results vary from year to year. The researchers found that the within-person variation was about 10 times greater than the between-person variation. This finding suggests that the precision of DXA scan measurements is not that reliable from 1 test to another.
The average annual increase in BMD in patients in the alendronate group was 0.0085 g/cm2—which is smaller than the typical year-to-year (within-person) variation of 0.013 g/cm2. It would therefore be difficult to differentiate the medication’s effect from the random variation inherent in DXA scans.
Response is favorable after 3 years of treatment. While there is variation in test results from year to year, longer-term findings are more reliable. After 3 years of treatment, 97.5% of patients taking alendronate had an increase in hip BMD of at least 0.019 g/cm2, with a strong correlation between hip and spine measurements. Although this represents a relatively small change in Z and T scores, this increase in hip BMD is considered a favorable response that warrants continued treatment. These findings are consistent with a previous analysis of BMD monitoring in women taking bisphosphonates, in which those who had the largest drop in BMD after the first year of treatment typically had a large gain over the second year.8
WHAT’S NEW: Now we know early testing is unnecessary
Not many studies are available to provide guidance about the interval between BMD measurements after starting a bisphosphonate. This study advises us that it is not necessary to recheck BMD for at least 3 years after starting treatment. Elimination of early repeat DXA testing could result in significant cost savings.
CAVEATS: Findings contradict usual recommendations
Physicians should be aware that the conclusion of this study is not in line with recommendations from a number of prominent organizations. The American Association of Clinical Endocrinology,9 the National Osteoporosis Foundation,10 and the North American Menopause Society11 all recommend follow-up DXA testing in 1 or 2 years.
High-risk patient exception. The delay in repeat DXA testing may not be appropriate for patients at higher risk of bone density loss. However, a separate analysis of higher-risk groups was not done.
Finally, while the findings of Bell et al suggest that we should wait at least 3 years before retesting, it is still not clear whether there is any benefit to repeat DXA testing at any interval, given the nearly universal response rate. It is also possible that advances in DXA technology will reduce some of the variation in BMD results.
CHALLENGES TO IMPLEMENTATION: Anxious patients
Patients like Ms. K may ask their physicians to retest well before 3 years. Yet those who undergo scanning after a shorter interval may be discouraged by early results. Advising patients that the treatment is almost uniformly effective in increasing BMD should reassure them that sticking with treatment is worthwhile.
Acknowledgment
The PURLs Surveillance System is supported in part by Grant Number UL1RR024999 from the National Center for Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
After starting patients on bisphosphonates for osteoporosis, wait at least 3 years before ordering a repeat dual-energy x-ray absorptiometry (DXA) scan.1
STRENGTH OF RECOMMENDATION
C: Based on a secondary analysis of a large randomized controlled trial.
Bell KL, Hayen A, Macaskill P, et al. Value of routine monitoring of bone mineral density after starting bisphosphonate treatment: secondary analysis of treatment data. BMJ. 2009;338:b2266.
ILLUSTRATIVE CASE
CASE: Ms. K, a 68-year-old woman diagnosed with osteoporosis on a screening DXA scan a year ago, has been taking a bisphosphonate ever since. She’s anxious to know whether the medication is working and asks if it’s time for a repeat DXA scan. What should you tell her?
Fragility fractures from osteoporosis are common in postmenopausal women. In the year 2000 alone, an estimated 9 million such fractures occurred worldwide.2 Treatment with bisphosphonates has been found to reduce the risk of fragility fractures,3 and the United States Preventive Services Task Force (USPSTF) recommends a DXA scan to screen for osteoporosis in women older than 65 years and some younger women at increased risk.4
Monitoring treatment: How often?
Although recommendations for how often to monitor bone mineral density (BMD) after initiating treatment vary, the consensus has been that periodic monitoring is useful. But there have been no randomized trials evaluating BMD testing in patients taking bisphosphonates.
The use of DXA scans to identify osteoporosis has been shown to be a cost-effective strategy in women older than 65 years,5 but there has not been a cost/benefit analysis of follow-up DXA scanning after initiating treatment. The cost of a scan ranges from about $150 to $300, and it is not known how many patients undergo repeat DXA scanning after starting treatment.
STUDY SUMMARY: Yearly scans are not helpful
The study we report on here is a secondary analysis of data from the Fracture Intervention Trial (FIT).6 In 1993, FIT randomized 6457 US women ages 55 to 80 years with low hip bone density to either alendronate or placebo. The initial dose of alendronate was 5 mg/d, but was later increased to 10 mg/d when other studies found that the higher dose was more effective. FIT showed that alendronate increased BMD and decreased the risk of vertebral fracture.7
Bell et al1 used a mixed-model statistical analysis to compare “within-person variation” in BMD (variation in DXA results over time in individuals) and “between-person variation” in BMD (variation in DXA results over time in the population of patients). The BMD of all FIT participants in both the control and treatment groups was measured at baseline and at the 1-, 2-, and 3-year marks. Each individual was always tested on the same scanner to minimize differences in machinery.
Individual results vary from year to year. The researchers found that the within-person variation was about 10 times greater than the between-person variation. This finding suggests that the precision of DXA scan measurements is not that reliable from 1 test to another.
The average annual increase in BMD in patients in the alendronate group was 0.0085 g/cm2—which is smaller than the typical year-to-year (within-person) variation of 0.013 g/cm2. It would therefore be difficult to differentiate the medication’s effect from the random variation inherent in DXA scans.
Response is favorable after 3 years of treatment. While there is variation in test results from year to year, longer-term findings are more reliable. After 3 years of treatment, 97.5% of patients taking alendronate had an increase in hip BMD of at least 0.019 g/cm2, with a strong correlation between hip and spine measurements. Although this represents a relatively small change in Z and T scores, this increase in hip BMD is considered a favorable response that warrants continued treatment. These findings are consistent with a previous analysis of BMD monitoring in women taking bisphosphonates, in which those who had the largest drop in BMD after the first year of treatment typically had a large gain over the second year.8
WHAT’S NEW: Now we know early testing is unnecessary
Not many studies are available to provide guidance about the interval between BMD measurements after starting a bisphosphonate. This study advises us that it is not necessary to recheck BMD for at least 3 years after starting treatment. Elimination of early repeat DXA testing could result in significant cost savings.
CAVEATS: Findings contradict usual recommendations
Physicians should be aware that the conclusion of this study is not in line with recommendations from a number of prominent organizations. The American Association of Clinical Endocrinology,9 the National Osteoporosis Foundation,10 and the North American Menopause Society11 all recommend follow-up DXA testing in 1 or 2 years.
High-risk patient exception. The delay in repeat DXA testing may not be appropriate for patients at higher risk of bone density loss. However, a separate analysis of higher-risk groups was not done.
Finally, while the findings of Bell et al suggest that we should wait at least 3 years before retesting, it is still not clear whether there is any benefit to repeat DXA testing at any interval, given the nearly universal response rate. It is also possible that advances in DXA technology will reduce some of the variation in BMD results.
CHALLENGES TO IMPLEMENTATION: Anxious patients
Patients like Ms. K may ask their physicians to retest well before 3 years. Yet those who undergo scanning after a shorter interval may be discouraged by early results. Advising patients that the treatment is almost uniformly effective in increasing BMD should reassure them that sticking with treatment is worthwhile.
Acknowledgment
The PURLs Surveillance System is supported in part by Grant Number UL1RR024999 from the National Center for Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
1. Bell KL, Hayen A, Macaskill P, et al. Value of routine monitoring of bone mineral density after starting bisphosphonate treatment: secondary analysis of treatment data. BMJ. 2009;338:b2266.-
2. Johnell O, Kanis JA. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int. 2006;17:1726.-
3. MacLean C, Newberry S, et al. Systematic review: comparative effectiveness of treatments to prevent fractures in men and women with low bone density or osteoporosis. Ann Intern Med. 2008;148:197-213.
4. Agency for Healthcare Research and Quality United States Preventive Services Task Force. Screening for osteoporosis in postmenopausal women. Available at: http://www.ahrq.gov/clinic/3rduspstf/osteoporosis/osteorr.htm . Accessed October 13, 2009.
5. Schousboe JT. Cost effectiveness of screen-and-treat strategies for low bone mineral density: how do we screen, who do we screen, and who do we treat? Appl Health Econ Health Policy. 2008;6:1-18.
6. Black DM, Nevitt MC, Cauley J, et al. Design of the fracture intervention trial. Osteopor Int. 2003;3(suppl 3):S29-S39.
7. Cummings S, Black D, Thompson D, et al. Effect of alendronate on risk of fracture in women with low bone density but without vertebral fractures. JAMA. 1998;280:2077-2082.
8. Cummings S, Palermo B, Browner W, et al. Monitoring osteoporosis therapy with bone densitometry: misleading changes and regression to the mean. Fracture Intervention Trial Research Group. JAMA. 2000;283:1318-1321.
9. AACE Osteoporosis Task Force American Association of Clinical Endocrinologists medical guidelines for clinical practice for the prevention and treatment of postmenopausal osteoporosis: 2001 edition with selected updates for 2003. Endocr Pract. 2003;9:544-564.
10. National Osteoporosis Foundation Clinician’s Guide to Prevention and Treatment of Osteoporosis. Washington DC: NOF; 2008.
11. Management of postmenopausal osteoporosis: position statement of the North American Menopause Society Menopause. 2002;9:84-101.
1. Bell KL, Hayen A, Macaskill P, et al. Value of routine monitoring of bone mineral density after starting bisphosphonate treatment: secondary analysis of treatment data. BMJ. 2009;338:b2266.-
2. Johnell O, Kanis JA. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int. 2006;17:1726.-
3. MacLean C, Newberry S, et al. Systematic review: comparative effectiveness of treatments to prevent fractures in men and women with low bone density or osteoporosis. Ann Intern Med. 2008;148:197-213.
4. Agency for Healthcare Research and Quality United States Preventive Services Task Force. Screening for osteoporosis in postmenopausal women. Available at: http://www.ahrq.gov/clinic/3rduspstf/osteoporosis/osteorr.htm . Accessed October 13, 2009.
5. Schousboe JT. Cost effectiveness of screen-and-treat strategies for low bone mineral density: how do we screen, who do we screen, and who do we treat? Appl Health Econ Health Policy. 2008;6:1-18.
6. Black DM, Nevitt MC, Cauley J, et al. Design of the fracture intervention trial. Osteopor Int. 2003;3(suppl 3):S29-S39.
7. Cummings S, Black D, Thompson D, et al. Effect of alendronate on risk of fracture in women with low bone density but without vertebral fractures. JAMA. 1998;280:2077-2082.
8. Cummings S, Palermo B, Browner W, et al. Monitoring osteoporosis therapy with bone densitometry: misleading changes and regression to the mean. Fracture Intervention Trial Research Group. JAMA. 2000;283:1318-1321.
9. AACE Osteoporosis Task Force American Association of Clinical Endocrinologists medical guidelines for clinical practice for the prevention and treatment of postmenopausal osteoporosis: 2001 edition with selected updates for 2003. Endocr Pract. 2003;9:544-564.
10. National Osteoporosis Foundation Clinician’s Guide to Prevention and Treatment of Osteoporosis. Washington DC: NOF; 2008.
11. Management of postmenopausal osteoporosis: position statement of the North American Menopause Society Menopause. 2002;9:84-101.
Copyright © 2009 The Family Physicians Inquiries Network.
All rights reserved.
Hypertension with metabolic syndrome: Think thiazides are old hat? ALLHAT says think again
ILLUSTRATIVE CASE
Your new patient is a 57-year-old African American man. His blood pressure is 150/95 mm Hg, fasting glucose 115 mg/dL, body mass index 32, and triglycerides 155 mg/dL; he is on no prior medications. During the course of his care you diagnose hypertension with metabolic syndrome and decide to recommend an antihypertensive. Thiazide-type diuretics are your standard initial therapy, but this patient has metabolic syndrome, and you know that certain antihypertensive agents have a more favorable metabolic profile than thiazide diuretics. Furthermore, metabolic differences among races have been touted as reason to use other agents in black patients. Should you recommend a thiazide diuretic, or another agent?
Until now, we’ve had no simple approach to treating hypertension in patients with metabolic syndrome—and half or more of our hypertensive patients over the age of 55 have this disorder.
Now, however, we can base decisions on clinical outcomes data from a subgroup analysis of the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT).1 This new subgroup analysis supports use of thiazide-type diuretics in these patients—particularly in black patients—despite the more favorable metabolic profile of calcium channel blockers, alpha-blockers, and angiotensin-converting enzyme (ACE) inhibitors.
Cost is no longer as big a factor as it once was, now that ACE inhibitors and alpha-blockers, as well as thiazide diuretics, are available generically.
Does a better metabolic profile improve outcomes?
We have had reason to be concerned about the metabolic adverse effects of thiazide-type diuretics in the past. Studies published before this ALLHAT subgroup analysis showed that hydrochlorothiazide for essential hypertension had adverse effects on potassium, glucose, and lipid metabolism. Some speculated that these changes aggravate the metabolic changes in early diabetes2-4 and may contribute to increased coronary heart disease risk.5,6
FIGURE
Outcomes favor thiazides
We know many physicians who have adopted thiazide-type diuretics as the first-line treatment for hypertension in metabolic syndrome, but until now, data have been inadequate to support this decision.
A subgroup analysis from the ALLHAT1 concludes: “The ALLHAT findings fail to support the preference for calcium channel blockers, alpha-blockers, or angiotensin-converting enzyme inhibitors compared with thiazide-type diuretics in patients with the metabolic syndrome, despite their more favorable metabolic profiles. This was particularly true for black participants.”
| Hypertension Blood pressure target for patients enrolled in the ALLHAT was <140/90 mm Hg | Metabolic syndrome, in the subgroup analysis, was defined as hypertension plus 2 of the following risk factors for coronary heart disease: | ||
| 1. Obesity Body mass index at least 30 | 2. Lipid disorder Fasting triglyceride level >150 mg/dL and high-density lipoprotein cholesterol level <40 mg/dL in men, or <50 mg/dL in women | 3. Glycemic disorder Fasting glucose level >100 mg/dL, or nonfasting glucose level >200 mg/dL, or history of diabetes | |
ACE inhibitors and ARBs
The metabolic benefits of ACE inhibitors and angiotensin-receptor blockers (ARBs) are widely known. In comparative studies prior to this ALLHAT subgroup analysis, ACE inhibitors were thought to be preferable to thiazide diuretics and beta-blockers for patients with obesity7 or the metabolic syndrome.8 These agents also protect against diabetic nephropathy.9 Other studies attribute additional vascular benefits to ACE inhibitors,10 beyond that of lowering blood pressure.
A 2005 meta-analysis by Abuissa et al11 showed that ACE inhibitors and ARBs were associated with significant reductions in the incidence of newly diagnosed diabetes, which, in turn, might lead to reduced heart disease. That report concluded that use of ACE inhibitors or ARBs should be considered in patients with prediabetic conditions such as metabolic syndrome, hypertension, impaired fasting glucose, family history of diabetes, obesity, congestive heart failure, or coronary heart disease.
Calcium-channel blockers and alpha-blockers
Calcium-channel blockers and alpha-blockers also do not appear to have the adverse metabolic effects of thiazides, and have also been advocated over beta-blockers and thiazides for hypertensive patients with metabolic syndrome.12-15
Racial differences
In a consensus statement developed before the findings from the ALLHAT subgroup analysis were available, it was noted that racial differences in metabolic syndrome may make the selection of antihypertensive agents particularly important in African American patients.16
ALLHAT and JNC7 recommendations
The 2002 ALLHAT demonstrated that chlorthalidone (a thiazide-type diuretic) is superior to lisinopril, amlodipine, and doxazosin in preventing 1 or more major forms of cardiovascular disease. No difference was observed, however, for fatal coronary heart disease, nonfatal myocardial infarction, or all-cause mortality.17 These findings persisted in sub-group analyses stratified by race, diabetic status, and level of renal function, but ALLHAT did not identify patients with metabolic syndrome a priori.
The ALLHAT influenced the 2003 Joint National Commission VII (JNC7) Report, which recommends thiazide diuretics for first-line treatment of hypertension in the absence of compelling indications to begin an alternative antihypertensive agent.18
Special consideration, but no recommendation. The JNC7 Report mentions the metabolic syndrome as a special consideration, but does not explicitly recommend a first-line therapy other than thiazides.
Anecdotally, we know many physicians who have adopted thiazide-type diuretics as the first-line treatment for hypertension in metabolic syndrome, but until now, data have been inadequate to support this decision.
It is unclear to us how this conflicting information has played out in current practice. We know that many physicians already choose thiazides as their first-line agent for hypertensive patients with metabolic syndrome. And we suspect that many choose other agents.
We analyzed the National Ambulatory Medical Care Survey data (http://www.cdc.gov/nchs/about/major/ahcd/ahcd1.htm) from 2004 and 2005 and found that only 3% to 5% of outpatients with diabetes and hypertension were taking thiazides at all (unpublished data). Metabolic syndrome is not a variable in this dataset, so we could not determine the use of thiazides in hypertension and metabolic syndrome.
Our informal polling of colleagues suggested that large numbers of hypertensive patients with metabolic syndrome are not currently receiving the more beneficial thiazides.
STUDY SUMMARY: Chlorthalidone outcomes were equivalent or better
Wright and colleagues analyzed a sub-group1 of the ALLHAT cohort, which consisted of 42,418 participants, aged ≥55, with hypertension and at least 1 other cardiovascular risk factor ( FIGURE ).
Patients were randomly assigned to therapy with chlorthalidone, amlodipine, lisinopril, or doxazosin. After randomization, if patients failed to reach the target blood pressure (<140/90 mm Hg) with their assigned therapy, they were started on atenolol, clonidine, or reserpine. If they required a third agent, they received hydralazine. The doxazosin arm was stopped early due to increased stroke and heart failure risk.
The ALLHAT was well done and designed for adequate power to evaluate clinical outcomes in racial subgroups, as well as the general population.
Outcomes were compared by race in hypertensive patients with and without metabolic syndrome.
A total of 23,077 (54%) patients met all criteria; 12,818 were black, 7327 (57%) of whom had metabolic syndrome.
Not surprisingly in a study of this size, the expected metabolic effects of all 4 antihypertensive agents were detected. Patients taking chlorthalidone had higher glucose levels (1–4 mg/dL) and higher levels of cholesterol, although these higher glucose and cholesterol levels were not statistically significant for all comparisons over time and between different drugs.
Outcomes in the chlorthalidone group were equivalent or superior to the 3 other therapies, generally. This pattern held true regardless of race ( TABLE ):
Heart failure rates were significantly higher in patients with metabolic syndrome across all treatments compared with chlorthalidone.
Combined cardiovascular disease rates were higher with lisinopril and doxazosin compared with chlorthalidone.
Stroke rates were higher among black participants only in the lisinopril group.
TABLE
Number needed to treat to prevent blood pressure-related adverse outcomes in patients with hypertension and metabolic syndrome
| NUMBER NEEDED TO TREAT (NNT)= number of patients that would need to take chlorthalidone to prevent 1 outcome, compared with the alternate drug (4.9 years of chlorthalidone instead of lisinopril or amlodipine or 3.2 years of chlorthalidone instead of doxazosin). Smaller numbers indicate a bigger effect. | ||||||
|---|---|---|---|---|---|---|
| OUTCOME | CHLORTHALIDONE VS AMLODIPINE | CHLORTHALIDONE VS LISINOPRIL | CHLORTHALIDONE VS DOXAZOSIN | |||
| Black | Non-black | Black | Non-black | Black | Non-black | |
| Combined cardiovascular disease | 22 | NS | 18 | 53 | 14 | 34 |
| Stroke | NS | -111 | 59 | NS | 37 | NS |
| Heart failure | 29 | 48 | 28 | 143 | 28 | 25 |
| All-cause mortality | NS | NS | NS | NS | NS | NS |
| NS=not significant. | ||||||
| Source: The authors calculated the NNTs from the event rates reported.1 | ||||||
WHAT’S NEW: Most effective, least expensive
First-line use of thiazide diuretics for hypertension gained major support from the findings of the first ALLHAT report, published in 2002. A year later, JNC7 supported the practice. Yet questions have persisted about whether the choice of initial antihypertensive agent in patients with metabolic syndrome warrants special consideration.
The difference for one patient is small, but when you consider the high prevalence of hypertension, the cumulative benefit at a population level is significant. This subgroup analysis confirms that there is no harm, and potentially a small benefit, in using chlorthalidone as a first-line agent for treating hypertension in patients with metabolic syndrome, regardless of race—despite the measurable and presumably adverse effects of diuretic agents on metabolic measurements.
How large is the benefit of first-line thiazides, overall?
Although, statistically, the relative risks (RR) are not large, the sheer number of patients means that there is significant benefit to the selection of thiazides as first-line treatment in most patients.
CAVEATS: Is stroke a concern? Was follow-up sufficient?
In this study, the only finding of harm in the diuretic group was an increased risk for stroke compared with amlodipine among non-black patients with metabolic syndrome. While this finding does raise some uncertainty, we still think that, on balance, thiazides are the most beneficial, even in this subgroup, as there was a larger benefit in preventing heart failure.
Another theoretical possibility is that follow-up was too short to demonstrate harm from the metabolic effects of thiazides. However, the metabolic effects of thiazides are very small and we believe that the evidence of benefit shown during this study period easily outweighs any such theoretical harms.
We also assume that hydrochlorothiazide, a commonly prescribed thiazide, has the same benefits as chlorthalidone, the medication studied.
Most ALLHAT participants with metabolic syndrome already had diabetes: 67.6% of black participants and 51.8% of non-black participants. Another sub-group analysis of the ALLHAT studied patients with metabolic syndrome without diabetes, and found similar results.19
Of note, lisinopril reduced the onset of diabetes over 5 years (number needed to treat [NNT]=22.2), at the cost of increased heart failure (RR=1.31; 95% confidence interval [CI], 1.04-1.64) and combined cardiovascular disease (RR=1.19; 95% CI, 1.07-1.32). This potentially confounds the claim that thiazides are effective in preventing diabetes, since so many people had it to begin with.
The criteria for metabolic syndrome did not include waist circumference, which is the National Cholesterol Education Program definition. The World Health Organization definition, however, does allow substitution of BMI. Purists would have you believe waist circumference is necessary. In practice, we have come to use BMI as an adequate surrogate. Some say it has, in fact, replaced waist circumference.
CHALLENGES TO IMPLEMENTATION: Inertia
Few interventions are as simple as this. Thiazide diuretics are well tolerated, need to be taken only once daily, and are inexpensive. Because generics are available, little to no pharmaceutical marketing is done to promote their use. The major barriers to implementing this practice may be overcoming clinical inertia, and the message of pharmaceutical marketing on behalf of the more expensive alternatives.
Acknowledgement
We acknowledge Sofia Medvedev, PhD, University HealthSystem Consortium, Oak Brook, IL for analysis of the National Ambulatory Medical Care Survey data.
PURLs methodology
This study was selected and evaluated using FPIN’s Priority Updates from the Research Literature (PURL) Surveillance System methodology. The criteria and findings leading to the selection of this study as a PURL can be accessed at here.
1. Wright JT, Jr, Harris-Haywood S, Pressel S, et al. Clinical outcomes by race in hypertensive patients with and without the metabolic syndrome: Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). Arch Intern Med. 2008;168:207-217.
2. Law MR, Wald NJ, Morris JK, Jordan RE. Value of low dose combination treatment with blood pressure lowering drugs: analysis of 354 randomised trials. BMJ. 2003;326:1427.-
3. Eberly LE, Cohen JD, Prineas R, Yang L. Intervention Trial Research group. Impact of incident diabetes and incident nonfatal cardiovascular disease on 18-year mortality: the Multiple Risk Factor Intervention Trial experience. Diabetes Care. 2003;26:848-854.
4. Pollare T, Lithell H, Berne C. A comparison of the effects of hydrochlorothiazide and captopril on glucose and lipid metabolism in patients with hyper-tension. N Engl J Med. 1989;321:868-873.
5. Mancia G, Grassi G, Zanchetti A. New-onset diabetes and antihypertensive drugs. J Hypertens. 2006;24:3-10.
6. Skarfors ET, Lithell HO, Selinus I, Aberg H. Do antihypertensive drugs precipitate diabetes? BMJ. 1989;298:1147-1152
7. Scholze J, Grimm E, Herrmann D, Unger T, Kintscher U. Optimal treatment of obesity-related hypertension: the Hypertension-Obesity-Sibutra-mine (HOS) study. Circulation. 2007;115:1991-1998.
8. Bakris G, Molitch M, Hewkin A, et al. STAR Investigators. Differences in glucose tolerance between fixed-dose antihypertensive drug combinations in people with metabolic syndrome. Diabetes Care. 2006;29:2592-2597.
9. Lewis EJ, Hunsicker LG, Bain RP, Rohde RD. The effect of angiotensin-converting-enzyme inhibition on diabetic nephropathy. The Collaborative Study Group. N Engl J Med. 1993;329:1456-1462.
10. Gianni M, Bosch J, Pogue J, et al. Effect of long-term ACE-inhibitor therapy in elderly vascular disease patients. Eur Heart J. 2007;28:1382-1388.
11. Abuissa H, Jones PG, Marso SP, O’Keefe JH Jr. Angiotensin-converting enzyme inhibitors or angiotensin receptor blockers for prevention of type 2 diabetes: a meta-analysis of randomized clinical trials. J Am Coll Cardiol. 2005;46:821-826.
12. Mykkänen L, Kuusisto J, Pyörälä K, Laakso M, Haffner SM. Increased risk of non-insulin-dependent diabetes mellitus in elderly hypertensive subjects. J Hypertens. 1994;12:1425-1432.
13. Giles TD, Sander GE. Pathophysiologic, diagnostic, and therapeutic aspects of the metabolic syndrome. J Clin Hypertens (Greenwich). 2005;7:669-678.
14. Mancia G. The association of hypertension and diabetes: prevalence, cardiovascular risk and protection by blood pressure reduction. Acta Diabetol. 2005;42(suppl 1):S17-S25.
15. Wagh A, Stone NJ. Treatment of metabolic syndrome. Expert Rev Cardiovasc Ther. 2004;2:213-228.
16. Hall WD, Clark LT, Wenger NK, et al. African-American Lipid and Cardiovascular Council. The metabolic syndrome in African Americans: a review. Ethn Dis. 2003;13:414-428.
17. ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group, Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial. Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). JAMA. 2002;288:2981-2997.
18. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7). Bethesda, MD: US Department of Health and Human Services, National Heart, Lung, and Blood Institute; December 2003. Available at: http://www.nhlbi.nih.gov/guidelines/hypertension. Accessed March 31, 2008.
19. Black HR, Davis B, Barzilay J, et al. Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial. Metabolic and clinical outcomes in nondiabetic individuals with the metabolic syndrome assigned to chlorthalidone, amlodipine, or lisinopril as initial treatment for hypertension: a report from the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). Diabetes Care. 2008;31:353-360.
ILLUSTRATIVE CASE
Your new patient is a 57-year-old African American man. His blood pressure is 150/95 mm Hg, fasting glucose 115 mg/dL, body mass index 32, and triglycerides 155 mg/dL; he is on no prior medications. During the course of his care you diagnose hypertension with metabolic syndrome and decide to recommend an antihypertensive. Thiazide-type diuretics are your standard initial therapy, but this patient has metabolic syndrome, and you know that certain antihypertensive agents have a more favorable metabolic profile than thiazide diuretics. Furthermore, metabolic differences among races have been touted as reason to use other agents in black patients. Should you recommend a thiazide diuretic, or another agent?
Until now, we’ve had no simple approach to treating hypertension in patients with metabolic syndrome—and half or more of our hypertensive patients over the age of 55 have this disorder.
Now, however, we can base decisions on clinical outcomes data from a subgroup analysis of the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT).1 This new subgroup analysis supports use of thiazide-type diuretics in these patients—particularly in black patients—despite the more favorable metabolic profile of calcium channel blockers, alpha-blockers, and angiotensin-converting enzyme (ACE) inhibitors.
Cost is no longer as big a factor as it once was, now that ACE inhibitors and alpha-blockers, as well as thiazide diuretics, are available generically.
Does a better metabolic profile improve outcomes?
We have had reason to be concerned about the metabolic adverse effects of thiazide-type diuretics in the past. Studies published before this ALLHAT subgroup analysis showed that hydrochlorothiazide for essential hypertension had adverse effects on potassium, glucose, and lipid metabolism. Some speculated that these changes aggravate the metabolic changes in early diabetes2-4 and may contribute to increased coronary heart disease risk.5,6
FIGURE
Outcomes favor thiazides
We know many physicians who have adopted thiazide-type diuretics as the first-line treatment for hypertension in metabolic syndrome, but until now, data have been inadequate to support this decision.
A subgroup analysis from the ALLHAT1 concludes: “The ALLHAT findings fail to support the preference for calcium channel blockers, alpha-blockers, or angiotensin-converting enzyme inhibitors compared with thiazide-type diuretics in patients with the metabolic syndrome, despite their more favorable metabolic profiles. This was particularly true for black participants.”
| Hypertension Blood pressure target for patients enrolled in the ALLHAT was <140/90 mm Hg | Metabolic syndrome, in the subgroup analysis, was defined as hypertension plus 2 of the following risk factors for coronary heart disease: | ||
| 1. Obesity Body mass index at least 30 | 2. Lipid disorder Fasting triglyceride level >150 mg/dL and high-density lipoprotein cholesterol level <40 mg/dL in men, or <50 mg/dL in women | 3. Glycemic disorder Fasting glucose level >100 mg/dL, or nonfasting glucose level >200 mg/dL, or history of diabetes | |
ACE inhibitors and ARBs
The metabolic benefits of ACE inhibitors and angiotensin-receptor blockers (ARBs) are widely known. In comparative studies prior to this ALLHAT subgroup analysis, ACE inhibitors were thought to be preferable to thiazide diuretics and beta-blockers for patients with obesity7 or the metabolic syndrome.8 These agents also protect against diabetic nephropathy.9 Other studies attribute additional vascular benefits to ACE inhibitors,10 beyond that of lowering blood pressure.
A 2005 meta-analysis by Abuissa et al11 showed that ACE inhibitors and ARBs were associated with significant reductions in the incidence of newly diagnosed diabetes, which, in turn, might lead to reduced heart disease. That report concluded that use of ACE inhibitors or ARBs should be considered in patients with prediabetic conditions such as metabolic syndrome, hypertension, impaired fasting glucose, family history of diabetes, obesity, congestive heart failure, or coronary heart disease.
Calcium-channel blockers and alpha-blockers
Calcium-channel blockers and alpha-blockers also do not appear to have the adverse metabolic effects of thiazides, and have also been advocated over beta-blockers and thiazides for hypertensive patients with metabolic syndrome.12-15
Racial differences
In a consensus statement developed before the findings from the ALLHAT subgroup analysis were available, it was noted that racial differences in metabolic syndrome may make the selection of antihypertensive agents particularly important in African American patients.16
ALLHAT and JNC7 recommendations
The 2002 ALLHAT demonstrated that chlorthalidone (a thiazide-type diuretic) is superior to lisinopril, amlodipine, and doxazosin in preventing 1 or more major forms of cardiovascular disease. No difference was observed, however, for fatal coronary heart disease, nonfatal myocardial infarction, or all-cause mortality.17 These findings persisted in sub-group analyses stratified by race, diabetic status, and level of renal function, but ALLHAT did not identify patients with metabolic syndrome a priori.
The ALLHAT influenced the 2003 Joint National Commission VII (JNC7) Report, which recommends thiazide diuretics for first-line treatment of hypertension in the absence of compelling indications to begin an alternative antihypertensive agent.18
Special consideration, but no recommendation. The JNC7 Report mentions the metabolic syndrome as a special consideration, but does not explicitly recommend a first-line therapy other than thiazides.
Anecdotally, we know many physicians who have adopted thiazide-type diuretics as the first-line treatment for hypertension in metabolic syndrome, but until now, data have been inadequate to support this decision.
It is unclear to us how this conflicting information has played out in current practice. We know that many physicians already choose thiazides as their first-line agent for hypertensive patients with metabolic syndrome. And we suspect that many choose other agents.
We analyzed the National Ambulatory Medical Care Survey data (http://www.cdc.gov/nchs/about/major/ahcd/ahcd1.htm) from 2004 and 2005 and found that only 3% to 5% of outpatients with diabetes and hypertension were taking thiazides at all (unpublished data). Metabolic syndrome is not a variable in this dataset, so we could not determine the use of thiazides in hypertension and metabolic syndrome.
Our informal polling of colleagues suggested that large numbers of hypertensive patients with metabolic syndrome are not currently receiving the more beneficial thiazides.
STUDY SUMMARY: Chlorthalidone outcomes were equivalent or better
Wright and colleagues analyzed a sub-group1 of the ALLHAT cohort, which consisted of 42,418 participants, aged ≥55, with hypertension and at least 1 other cardiovascular risk factor ( FIGURE ).
Patients were randomly assigned to therapy with chlorthalidone, amlodipine, lisinopril, or doxazosin. After randomization, if patients failed to reach the target blood pressure (<140/90 mm Hg) with their assigned therapy, they were started on atenolol, clonidine, or reserpine. If they required a third agent, they received hydralazine. The doxazosin arm was stopped early due to increased stroke and heart failure risk.
The ALLHAT was well done and designed for adequate power to evaluate clinical outcomes in racial subgroups, as well as the general population.
Outcomes were compared by race in hypertensive patients with and without metabolic syndrome.
A total of 23,077 (54%) patients met all criteria; 12,818 were black, 7327 (57%) of whom had metabolic syndrome.
Not surprisingly in a study of this size, the expected metabolic effects of all 4 antihypertensive agents were detected. Patients taking chlorthalidone had higher glucose levels (1–4 mg/dL) and higher levels of cholesterol, although these higher glucose and cholesterol levels were not statistically significant for all comparisons over time and between different drugs.
Outcomes in the chlorthalidone group were equivalent or superior to the 3 other therapies, generally. This pattern held true regardless of race ( TABLE ):
Heart failure rates were significantly higher in patients with metabolic syndrome across all treatments compared with chlorthalidone.
Combined cardiovascular disease rates were higher with lisinopril and doxazosin compared with chlorthalidone.
Stroke rates were higher among black participants only in the lisinopril group.
TABLE
Number needed to treat to prevent blood pressure-related adverse outcomes in patients with hypertension and metabolic syndrome
| NUMBER NEEDED TO TREAT (NNT)= number of patients that would need to take chlorthalidone to prevent 1 outcome, compared with the alternate drug (4.9 years of chlorthalidone instead of lisinopril or amlodipine or 3.2 years of chlorthalidone instead of doxazosin). Smaller numbers indicate a bigger effect. | ||||||
|---|---|---|---|---|---|---|
| OUTCOME | CHLORTHALIDONE VS AMLODIPINE | CHLORTHALIDONE VS LISINOPRIL | CHLORTHALIDONE VS DOXAZOSIN | |||
| Black | Non-black | Black | Non-black | Black | Non-black | |
| Combined cardiovascular disease | 22 | NS | 18 | 53 | 14 | 34 |
| Stroke | NS | -111 | 59 | NS | 37 | NS |
| Heart failure | 29 | 48 | 28 | 143 | 28 | 25 |
| All-cause mortality | NS | NS | NS | NS | NS | NS |
| NS=not significant. | ||||||
| Source: The authors calculated the NNTs from the event rates reported.1 | ||||||
WHAT’S NEW: Most effective, least expensive
First-line use of thiazide diuretics for hypertension gained major support from the findings of the first ALLHAT report, published in 2002. A year later, JNC7 supported the practice. Yet questions have persisted about whether the choice of initial antihypertensive agent in patients with metabolic syndrome warrants special consideration.
The difference for one patient is small, but when you consider the high prevalence of hypertension, the cumulative benefit at a population level is significant. This subgroup analysis confirms that there is no harm, and potentially a small benefit, in using chlorthalidone as a first-line agent for treating hypertension in patients with metabolic syndrome, regardless of race—despite the measurable and presumably adverse effects of diuretic agents on metabolic measurements.
How large is the benefit of first-line thiazides, overall?
Although, statistically, the relative risks (RR) are not large, the sheer number of patients means that there is significant benefit to the selection of thiazides as first-line treatment in most patients.
CAVEATS: Is stroke a concern? Was follow-up sufficient?
In this study, the only finding of harm in the diuretic group was an increased risk for stroke compared with amlodipine among non-black patients with metabolic syndrome. While this finding does raise some uncertainty, we still think that, on balance, thiazides are the most beneficial, even in this subgroup, as there was a larger benefit in preventing heart failure.
Another theoretical possibility is that follow-up was too short to demonstrate harm from the metabolic effects of thiazides. However, the metabolic effects of thiazides are very small and we believe that the evidence of benefit shown during this study period easily outweighs any such theoretical harms.
We also assume that hydrochlorothiazide, a commonly prescribed thiazide, has the same benefits as chlorthalidone, the medication studied.
Most ALLHAT participants with metabolic syndrome already had diabetes: 67.6% of black participants and 51.8% of non-black participants. Another sub-group analysis of the ALLHAT studied patients with metabolic syndrome without diabetes, and found similar results.19
Of note, lisinopril reduced the onset of diabetes over 5 years (number needed to treat [NNT]=22.2), at the cost of increased heart failure (RR=1.31; 95% confidence interval [CI], 1.04-1.64) and combined cardiovascular disease (RR=1.19; 95% CI, 1.07-1.32). This potentially confounds the claim that thiazides are effective in preventing diabetes, since so many people had it to begin with.
The criteria for metabolic syndrome did not include waist circumference, which is the National Cholesterol Education Program definition. The World Health Organization definition, however, does allow substitution of BMI. Purists would have you believe waist circumference is necessary. In practice, we have come to use BMI as an adequate surrogate. Some say it has, in fact, replaced waist circumference.
CHALLENGES TO IMPLEMENTATION: Inertia
Few interventions are as simple as this. Thiazide diuretics are well tolerated, need to be taken only once daily, and are inexpensive. Because generics are available, little to no pharmaceutical marketing is done to promote their use. The major barriers to implementing this practice may be overcoming clinical inertia, and the message of pharmaceutical marketing on behalf of the more expensive alternatives.
Acknowledgement
We acknowledge Sofia Medvedev, PhD, University HealthSystem Consortium, Oak Brook, IL for analysis of the National Ambulatory Medical Care Survey data.
PURLs methodology
This study was selected and evaluated using FPIN’s Priority Updates from the Research Literature (PURL) Surveillance System methodology. The criteria and findings leading to the selection of this study as a PURL can be accessed at here.
ILLUSTRATIVE CASE
Your new patient is a 57-year-old African American man. His blood pressure is 150/95 mm Hg, fasting glucose 115 mg/dL, body mass index 32, and triglycerides 155 mg/dL; he is on no prior medications. During the course of his care you diagnose hypertension with metabolic syndrome and decide to recommend an antihypertensive. Thiazide-type diuretics are your standard initial therapy, but this patient has metabolic syndrome, and you know that certain antihypertensive agents have a more favorable metabolic profile than thiazide diuretics. Furthermore, metabolic differences among races have been touted as reason to use other agents in black patients. Should you recommend a thiazide diuretic, or another agent?
Until now, we’ve had no simple approach to treating hypertension in patients with metabolic syndrome—and half or more of our hypertensive patients over the age of 55 have this disorder.
Now, however, we can base decisions on clinical outcomes data from a subgroup analysis of the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT).1 This new subgroup analysis supports use of thiazide-type diuretics in these patients—particularly in black patients—despite the more favorable metabolic profile of calcium channel blockers, alpha-blockers, and angiotensin-converting enzyme (ACE) inhibitors.
Cost is no longer as big a factor as it once was, now that ACE inhibitors and alpha-blockers, as well as thiazide diuretics, are available generically.
Does a better metabolic profile improve outcomes?
We have had reason to be concerned about the metabolic adverse effects of thiazide-type diuretics in the past. Studies published before this ALLHAT subgroup analysis showed that hydrochlorothiazide for essential hypertension had adverse effects on potassium, glucose, and lipid metabolism. Some speculated that these changes aggravate the metabolic changes in early diabetes2-4 and may contribute to increased coronary heart disease risk.5,6
FIGURE
Outcomes favor thiazides
We know many physicians who have adopted thiazide-type diuretics as the first-line treatment for hypertension in metabolic syndrome, but until now, data have been inadequate to support this decision.
A subgroup analysis from the ALLHAT1 concludes: “The ALLHAT findings fail to support the preference for calcium channel blockers, alpha-blockers, or angiotensin-converting enzyme inhibitors compared with thiazide-type diuretics in patients with the metabolic syndrome, despite their more favorable metabolic profiles. This was particularly true for black participants.”
| Hypertension Blood pressure target for patients enrolled in the ALLHAT was <140/90 mm Hg | Metabolic syndrome, in the subgroup analysis, was defined as hypertension plus 2 of the following risk factors for coronary heart disease: | ||
| 1. Obesity Body mass index at least 30 | 2. Lipid disorder Fasting triglyceride level >150 mg/dL and high-density lipoprotein cholesterol level <40 mg/dL in men, or <50 mg/dL in women | 3. Glycemic disorder Fasting glucose level >100 mg/dL, or nonfasting glucose level >200 mg/dL, or history of diabetes | |
ACE inhibitors and ARBs
The metabolic benefits of ACE inhibitors and angiotensin-receptor blockers (ARBs) are widely known. In comparative studies prior to this ALLHAT subgroup analysis, ACE inhibitors were thought to be preferable to thiazide diuretics and beta-blockers for patients with obesity7 or the metabolic syndrome.8 These agents also protect against diabetic nephropathy.9 Other studies attribute additional vascular benefits to ACE inhibitors,10 beyond that of lowering blood pressure.
A 2005 meta-analysis by Abuissa et al11 showed that ACE inhibitors and ARBs were associated with significant reductions in the incidence of newly diagnosed diabetes, which, in turn, might lead to reduced heart disease. That report concluded that use of ACE inhibitors or ARBs should be considered in patients with prediabetic conditions such as metabolic syndrome, hypertension, impaired fasting glucose, family history of diabetes, obesity, congestive heart failure, or coronary heart disease.
Calcium-channel blockers and alpha-blockers
Calcium-channel blockers and alpha-blockers also do not appear to have the adverse metabolic effects of thiazides, and have also been advocated over beta-blockers and thiazides for hypertensive patients with metabolic syndrome.12-15
Racial differences
In a consensus statement developed before the findings from the ALLHAT subgroup analysis were available, it was noted that racial differences in metabolic syndrome may make the selection of antihypertensive agents particularly important in African American patients.16
ALLHAT and JNC7 recommendations
The 2002 ALLHAT demonstrated that chlorthalidone (a thiazide-type diuretic) is superior to lisinopril, amlodipine, and doxazosin in preventing 1 or more major forms of cardiovascular disease. No difference was observed, however, for fatal coronary heart disease, nonfatal myocardial infarction, or all-cause mortality.17 These findings persisted in sub-group analyses stratified by race, diabetic status, and level of renal function, but ALLHAT did not identify patients with metabolic syndrome a priori.
The ALLHAT influenced the 2003 Joint National Commission VII (JNC7) Report, which recommends thiazide diuretics for first-line treatment of hypertension in the absence of compelling indications to begin an alternative antihypertensive agent.18
Special consideration, but no recommendation. The JNC7 Report mentions the metabolic syndrome as a special consideration, but does not explicitly recommend a first-line therapy other than thiazides.
Anecdotally, we know many physicians who have adopted thiazide-type diuretics as the first-line treatment for hypertension in metabolic syndrome, but until now, data have been inadequate to support this decision.
It is unclear to us how this conflicting information has played out in current practice. We know that many physicians already choose thiazides as their first-line agent for hypertensive patients with metabolic syndrome. And we suspect that many choose other agents.
We analyzed the National Ambulatory Medical Care Survey data (http://www.cdc.gov/nchs/about/major/ahcd/ahcd1.htm) from 2004 and 2005 and found that only 3% to 5% of outpatients with diabetes and hypertension were taking thiazides at all (unpublished data). Metabolic syndrome is not a variable in this dataset, so we could not determine the use of thiazides in hypertension and metabolic syndrome.
Our informal polling of colleagues suggested that large numbers of hypertensive patients with metabolic syndrome are not currently receiving the more beneficial thiazides.
STUDY SUMMARY: Chlorthalidone outcomes were equivalent or better
Wright and colleagues analyzed a sub-group1 of the ALLHAT cohort, which consisted of 42,418 participants, aged ≥55, with hypertension and at least 1 other cardiovascular risk factor ( FIGURE ).
Patients were randomly assigned to therapy with chlorthalidone, amlodipine, lisinopril, or doxazosin. After randomization, if patients failed to reach the target blood pressure (<140/90 mm Hg) with their assigned therapy, they were started on atenolol, clonidine, or reserpine. If they required a third agent, they received hydralazine. The doxazosin arm was stopped early due to increased stroke and heart failure risk.
The ALLHAT was well done and designed for adequate power to evaluate clinical outcomes in racial subgroups, as well as the general population.
Outcomes were compared by race in hypertensive patients with and without metabolic syndrome.
A total of 23,077 (54%) patients met all criteria; 12,818 were black, 7327 (57%) of whom had metabolic syndrome.
Not surprisingly in a study of this size, the expected metabolic effects of all 4 antihypertensive agents were detected. Patients taking chlorthalidone had higher glucose levels (1–4 mg/dL) and higher levels of cholesterol, although these higher glucose and cholesterol levels were not statistically significant for all comparisons over time and between different drugs.
Outcomes in the chlorthalidone group were equivalent or superior to the 3 other therapies, generally. This pattern held true regardless of race ( TABLE ):
Heart failure rates were significantly higher in patients with metabolic syndrome across all treatments compared with chlorthalidone.
Combined cardiovascular disease rates were higher with lisinopril and doxazosin compared with chlorthalidone.
Stroke rates were higher among black participants only in the lisinopril group.
TABLE
Number needed to treat to prevent blood pressure-related adverse outcomes in patients with hypertension and metabolic syndrome
| NUMBER NEEDED TO TREAT (NNT)= number of patients that would need to take chlorthalidone to prevent 1 outcome, compared with the alternate drug (4.9 years of chlorthalidone instead of lisinopril or amlodipine or 3.2 years of chlorthalidone instead of doxazosin). Smaller numbers indicate a bigger effect. | ||||||
|---|---|---|---|---|---|---|
| OUTCOME | CHLORTHALIDONE VS AMLODIPINE | CHLORTHALIDONE VS LISINOPRIL | CHLORTHALIDONE VS DOXAZOSIN | |||
| Black | Non-black | Black | Non-black | Black | Non-black | |
| Combined cardiovascular disease | 22 | NS | 18 | 53 | 14 | 34 |
| Stroke | NS | -111 | 59 | NS | 37 | NS |
| Heart failure | 29 | 48 | 28 | 143 | 28 | 25 |
| All-cause mortality | NS | NS | NS | NS | NS | NS |
| NS=not significant. | ||||||
| Source: The authors calculated the NNTs from the event rates reported.1 | ||||||
WHAT’S NEW: Most effective, least expensive
First-line use of thiazide diuretics for hypertension gained major support from the findings of the first ALLHAT report, published in 2002. A year later, JNC7 supported the practice. Yet questions have persisted about whether the choice of initial antihypertensive agent in patients with metabolic syndrome warrants special consideration.
The difference for one patient is small, but when you consider the high prevalence of hypertension, the cumulative benefit at a population level is significant. This subgroup analysis confirms that there is no harm, and potentially a small benefit, in using chlorthalidone as a first-line agent for treating hypertension in patients with metabolic syndrome, regardless of race—despite the measurable and presumably adverse effects of diuretic agents on metabolic measurements.
How large is the benefit of first-line thiazides, overall?
Although, statistically, the relative risks (RR) are not large, the sheer number of patients means that there is significant benefit to the selection of thiazides as first-line treatment in most patients.
CAVEATS: Is stroke a concern? Was follow-up sufficient?
In this study, the only finding of harm in the diuretic group was an increased risk for stroke compared with amlodipine among non-black patients with metabolic syndrome. While this finding does raise some uncertainty, we still think that, on balance, thiazides are the most beneficial, even in this subgroup, as there was a larger benefit in preventing heart failure.
Another theoretical possibility is that follow-up was too short to demonstrate harm from the metabolic effects of thiazides. However, the metabolic effects of thiazides are very small and we believe that the evidence of benefit shown during this study period easily outweighs any such theoretical harms.
We also assume that hydrochlorothiazide, a commonly prescribed thiazide, has the same benefits as chlorthalidone, the medication studied.
Most ALLHAT participants with metabolic syndrome already had diabetes: 67.6% of black participants and 51.8% of non-black participants. Another sub-group analysis of the ALLHAT studied patients with metabolic syndrome without diabetes, and found similar results.19
Of note, lisinopril reduced the onset of diabetes over 5 years (number needed to treat [NNT]=22.2), at the cost of increased heart failure (RR=1.31; 95% confidence interval [CI], 1.04-1.64) and combined cardiovascular disease (RR=1.19; 95% CI, 1.07-1.32). This potentially confounds the claim that thiazides are effective in preventing diabetes, since so many people had it to begin with.
The criteria for metabolic syndrome did not include waist circumference, which is the National Cholesterol Education Program definition. The World Health Organization definition, however, does allow substitution of BMI. Purists would have you believe waist circumference is necessary. In practice, we have come to use BMI as an adequate surrogate. Some say it has, in fact, replaced waist circumference.
CHALLENGES TO IMPLEMENTATION: Inertia
Few interventions are as simple as this. Thiazide diuretics are well tolerated, need to be taken only once daily, and are inexpensive. Because generics are available, little to no pharmaceutical marketing is done to promote their use. The major barriers to implementing this practice may be overcoming clinical inertia, and the message of pharmaceutical marketing on behalf of the more expensive alternatives.
Acknowledgement
We acknowledge Sofia Medvedev, PhD, University HealthSystem Consortium, Oak Brook, IL for analysis of the National Ambulatory Medical Care Survey data.
PURLs methodology
This study was selected and evaluated using FPIN’s Priority Updates from the Research Literature (PURL) Surveillance System methodology. The criteria and findings leading to the selection of this study as a PURL can be accessed at here.
1. Wright JT, Jr, Harris-Haywood S, Pressel S, et al. Clinical outcomes by race in hypertensive patients with and without the metabolic syndrome: Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). Arch Intern Med. 2008;168:207-217.
2. Law MR, Wald NJ, Morris JK, Jordan RE. Value of low dose combination treatment with blood pressure lowering drugs: analysis of 354 randomised trials. BMJ. 2003;326:1427.-
3. Eberly LE, Cohen JD, Prineas R, Yang L. Intervention Trial Research group. Impact of incident diabetes and incident nonfatal cardiovascular disease on 18-year mortality: the Multiple Risk Factor Intervention Trial experience. Diabetes Care. 2003;26:848-854.
4. Pollare T, Lithell H, Berne C. A comparison of the effects of hydrochlorothiazide and captopril on glucose and lipid metabolism in patients with hyper-tension. N Engl J Med. 1989;321:868-873.
5. Mancia G, Grassi G, Zanchetti A. New-onset diabetes and antihypertensive drugs. J Hypertens. 2006;24:3-10.
6. Skarfors ET, Lithell HO, Selinus I, Aberg H. Do antihypertensive drugs precipitate diabetes? BMJ. 1989;298:1147-1152
7. Scholze J, Grimm E, Herrmann D, Unger T, Kintscher U. Optimal treatment of obesity-related hypertension: the Hypertension-Obesity-Sibutra-mine (HOS) study. Circulation. 2007;115:1991-1998.
8. Bakris G, Molitch M, Hewkin A, et al. STAR Investigators. Differences in glucose tolerance between fixed-dose antihypertensive drug combinations in people with metabolic syndrome. Diabetes Care. 2006;29:2592-2597.
9. Lewis EJ, Hunsicker LG, Bain RP, Rohde RD. The effect of angiotensin-converting-enzyme inhibition on diabetic nephropathy. The Collaborative Study Group. N Engl J Med. 1993;329:1456-1462.
10. Gianni M, Bosch J, Pogue J, et al. Effect of long-term ACE-inhibitor therapy in elderly vascular disease patients. Eur Heart J. 2007;28:1382-1388.
11. Abuissa H, Jones PG, Marso SP, O’Keefe JH Jr. Angiotensin-converting enzyme inhibitors or angiotensin receptor blockers for prevention of type 2 diabetes: a meta-analysis of randomized clinical trials. J Am Coll Cardiol. 2005;46:821-826.
12. Mykkänen L, Kuusisto J, Pyörälä K, Laakso M, Haffner SM. Increased risk of non-insulin-dependent diabetes mellitus in elderly hypertensive subjects. J Hypertens. 1994;12:1425-1432.
13. Giles TD, Sander GE. Pathophysiologic, diagnostic, and therapeutic aspects of the metabolic syndrome. J Clin Hypertens (Greenwich). 2005;7:669-678.
14. Mancia G. The association of hypertension and diabetes: prevalence, cardiovascular risk and protection by blood pressure reduction. Acta Diabetol. 2005;42(suppl 1):S17-S25.
15. Wagh A, Stone NJ. Treatment of metabolic syndrome. Expert Rev Cardiovasc Ther. 2004;2:213-228.
16. Hall WD, Clark LT, Wenger NK, et al. African-American Lipid and Cardiovascular Council. The metabolic syndrome in African Americans: a review. Ethn Dis. 2003;13:414-428.
17. ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group, Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial. Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). JAMA. 2002;288:2981-2997.
18. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7). Bethesda, MD: US Department of Health and Human Services, National Heart, Lung, and Blood Institute; December 2003. Available at: http://www.nhlbi.nih.gov/guidelines/hypertension. Accessed March 31, 2008.
19. Black HR, Davis B, Barzilay J, et al. Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial. Metabolic and clinical outcomes in nondiabetic individuals with the metabolic syndrome assigned to chlorthalidone, amlodipine, or lisinopril as initial treatment for hypertension: a report from the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). Diabetes Care. 2008;31:353-360.
1. Wright JT, Jr, Harris-Haywood S, Pressel S, et al. Clinical outcomes by race in hypertensive patients with and without the metabolic syndrome: Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). Arch Intern Med. 2008;168:207-217.
2. Law MR, Wald NJ, Morris JK, Jordan RE. Value of low dose combination treatment with blood pressure lowering drugs: analysis of 354 randomised trials. BMJ. 2003;326:1427.-
3. Eberly LE, Cohen JD, Prineas R, Yang L. Intervention Trial Research group. Impact of incident diabetes and incident nonfatal cardiovascular disease on 18-year mortality: the Multiple Risk Factor Intervention Trial experience. Diabetes Care. 2003;26:848-854.
4. Pollare T, Lithell H, Berne C. A comparison of the effects of hydrochlorothiazide and captopril on glucose and lipid metabolism in patients with hyper-tension. N Engl J Med. 1989;321:868-873.
5. Mancia G, Grassi G, Zanchetti A. New-onset diabetes and antihypertensive drugs. J Hypertens. 2006;24:3-10.
6. Skarfors ET, Lithell HO, Selinus I, Aberg H. Do antihypertensive drugs precipitate diabetes? BMJ. 1989;298:1147-1152
7. Scholze J, Grimm E, Herrmann D, Unger T, Kintscher U. Optimal treatment of obesity-related hypertension: the Hypertension-Obesity-Sibutra-mine (HOS) study. Circulation. 2007;115:1991-1998.
8. Bakris G, Molitch M, Hewkin A, et al. STAR Investigators. Differences in glucose tolerance between fixed-dose antihypertensive drug combinations in people with metabolic syndrome. Diabetes Care. 2006;29:2592-2597.
9. Lewis EJ, Hunsicker LG, Bain RP, Rohde RD. The effect of angiotensin-converting-enzyme inhibition on diabetic nephropathy. The Collaborative Study Group. N Engl J Med. 1993;329:1456-1462.
10. Gianni M, Bosch J, Pogue J, et al. Effect of long-term ACE-inhibitor therapy in elderly vascular disease patients. Eur Heart J. 2007;28:1382-1388.
11. Abuissa H, Jones PG, Marso SP, O’Keefe JH Jr. Angiotensin-converting enzyme inhibitors or angiotensin receptor blockers for prevention of type 2 diabetes: a meta-analysis of randomized clinical trials. J Am Coll Cardiol. 2005;46:821-826.
12. Mykkänen L, Kuusisto J, Pyörälä K, Laakso M, Haffner SM. Increased risk of non-insulin-dependent diabetes mellitus in elderly hypertensive subjects. J Hypertens. 1994;12:1425-1432.
13. Giles TD, Sander GE. Pathophysiologic, diagnostic, and therapeutic aspects of the metabolic syndrome. J Clin Hypertens (Greenwich). 2005;7:669-678.
14. Mancia G. The association of hypertension and diabetes: prevalence, cardiovascular risk and protection by blood pressure reduction. Acta Diabetol. 2005;42(suppl 1):S17-S25.
15. Wagh A, Stone NJ. Treatment of metabolic syndrome. Expert Rev Cardiovasc Ther. 2004;2:213-228.
16. Hall WD, Clark LT, Wenger NK, et al. African-American Lipid and Cardiovascular Council. The metabolic syndrome in African Americans: a review. Ethn Dis. 2003;13:414-428.
17. ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group, Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial. Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). JAMA. 2002;288:2981-2997.
18. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7). Bethesda, MD: US Department of Health and Human Services, National Heart, Lung, and Blood Institute; December 2003. Available at: http://www.nhlbi.nih.gov/guidelines/hypertension. Accessed March 31, 2008.
19. Black HR, Davis B, Barzilay J, et al. Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial. Metabolic and clinical outcomes in nondiabetic individuals with the metabolic syndrome assigned to chlorthalidone, amlodipine, or lisinopril as initial treatment for hypertension: a report from the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). Diabetes Care. 2008;31:353-360.
Copyright © 2008 The Family Physicians Inquiries Network.
All rights reserved.
Drugs help pass more ureteral stones
Prescribe tamsulosin (typically 0.4 mg daily) or nifedipine (typically 30 mg daily) for patients with lower ureteral calculi, to speed stone passage and to avoid surgical intervention
Strength of recommendation
A: Meta-analysis of randomized controlled trials
Singh A, Alter HJ, Littlepage A. A systematic review of medical therapy to facilitate passage of ureteral calculi. Ann Emerg Med. 2007; 50:552-563.1
ILLUSTRATIVE CASE
A 52-year-old man presents to your office for follow-up 2 days after he was seen in the ED and diagnosed with a distal ureteral calculus, his first. His pain is reasonably well controlled, but he has not yet passed the stone. Is there anything you can do to help him pass the stone?
Yes. Patients who are candidates for observation should be offered a trial of “medical expulsive therapy” using an α-antagonist or a calcium channel blocker. Until now, medical therapy for kidney stones consisted of pain relief only.
The ordeal of a first stone is all too common—the lifetime prevalence of kidney stones is 5.2%—and the probability of recurrence is about 50%.2,3
NHANES data show increasing prevalence between the periods 1976-1980 and 1988-1996.3 One fifth to one third of kidney stones require surgical intervention.4 In a cohort of 245 patients presenting to an ED in Canada, 50 (20%) required further procedures, including lithotripsy. Stones ≥ 6 mm in size were much less likely to pass (OR=10.7, 95% CI 4.6-24.8).5 The burden on the healthcare system is significant; there are approximately 2 million out-patient visits annually for this problem, and diagnosis and treatment costs about $2 billion annually.6
Watch and wait
The standard approach is a period of watchful waiting and pain control, with urgent urological referral for patients with evidence of upper urinary tract infection, high grade obstruction, inadequate pain or nausea control, or insufficient renal reserve.2,4 Most patients treated with watchful waiting pass their stone within 4 weeks. Any stones that don’t pass within 8 weeks are unlikely to pass spontaneously.2,7
Medical therapy has been proposed for decades
Medications that relax ureteral smooth muscle to help pass ureteral stones have been proposed for decades.8 Prior to 2000, however, only 1 randomized controlled trial (RCT) of medical therapy for ureteral stones had been published.9 A subsequent meta-analysis found 9 studies and showed that medical therapy did increase the chances that a stone would pass.10 The Singh meta-analysis found 13 subsequently published studies and nearly tripled the number of patients evaluated.
STUDY SUMMARY: A well-done meta-analysis
This meta-analysis is based on 16 studies of α-antagonists (most used tamsulosin) and 9 studies of nifedipine, a calcium channel blocker.1 The studies were identified by a comprehensive search strategy that included Medline, EMBASE, and the Cochrane Controlled Trials Register from January 1980 to January 2007. The authors included all randomized trials or controlled clinical trials of medical therapy for adults with acute ureteral colic.
The authors assessed the studies for quality using the Jadad scale, a validated scale of study quality. Higher scores represent better quality, including better documentation of randomization, blinding, and follow-up. The authors specified their planned sensitivity analyses, and used the random effects model to synthesize the results, which tends to provide a more conservative estimate of the effect.
In other words, this was a very well done meta-analysis.
Twenty-two studies met the inclusion criteria: 13 of α-antagonists, 6 of nifedipine, and 3 of both. In 13 of the 16 studies of α-antagonists, tamsulosin (Flomax) was the study drug. The results from the terazosin (Hytrin) and doxazosin (Cardura) studies were included with the tamsulosin studies. The Jadad quality scores of the 22 studies were fairly low, with a median of 2 (range of 0 to 3) on the 5-point scale. The most common deduction was because the study was not double-blinded.
Medical therapy makes sense
“Therapy using either α-antagonists or calcium channel blockers augments the stone expulsion rate compared to standard therapy for moderately sized distal ureteral stones.” 1 CT showing distal ureteral stone
α-Antagonist studies
These 16 studies enrolled 1235 patients with distal ureteral stones. Mean stone size ranged from 4.3 to 7.8 mm. α-Antagonists improved the stone expulsion rate (RR= 1.59, 95% CI 1.44-1.75; NNT=3.3).
The mean time to expulsion of the stone ranged from 2.7 to 14.2 days and duration of therapy ranged from 1 to 7 weeks. In the 9 trials that reported the time to stone expulsion, the stone came out between 2 and 6 days earlier than the control groups.
Adverse effects were reported in 4% of patients receiving the active medication; most were mild.
Nifedipine studies
There were 686 patients in the 9 trials of nifedipine. The mean stone size was 3.9 to 12.8 mm. Some studies included stones in the more proximal as well as the distal ureter.
Nifedipine treatment increased the rate of stone expulsion (RR=1.5, 95% CI 1.34-1.68; NNT=3.9). Time to stone expulsion was shorter in 7 of the 9 studies.
Adverse effects were reported in 15% of the patients. Most of these were mild— nausea, vomiting, asthenia, and dyspepsia.
WHAT’S NEW: Strong evidence for use of medical therapy
The new findings from the Singh meta-analysis reviewed in this PURL supports physicians who have already adopted this practice and should encourage usage by those who have not yet done so.
Inpatients in academic medical centers
There is a growing trend to use tamsulosin to facilitate passage of ureteral stones. The University Health System Consortium (www.uhc.org) has complete clinical data on inpatients with ureteral stones, from 64 academic medical centers and teaching hospitals, between 2003 and 2007. We used this database to analyze trends in the use of tamsulosin in 4300 inpatients with ureteral stones (ICD 9 code 5921).
In 2003, only 3.3% of patients with a discharge diagnosis of ureteral stone received tamsulosin. In 2007, 34.1% of patients with ureteral stones discharged from these hospitals received tamsulosin, with similar rates of use when stratified by the specialty of the attending physician at discharge (family medicine, emergency medicine, internal medicine, urology) (FIGURE 1). We noted a wide range in the rate of adoption of this practice among academic medical centers: 48% in the centers with the highest rate of usage and 4.4% in the centers with the lowest rate.
FIGURE 1
% of inpatients in academic medical centers who received tamsulosin for ureteral stones, by year
Source: Unpublished data from the University Health System Consortium
Outpatients from a sample of US practices
The use of tamsulosin or nifedipine in outpatient practice was infrequent even 2 or 3 years ago. We used the National Ambulatory Medical Care Survey data (www.cdc.gov/nchs/about/major/ahcd/ahcd1.htm) from 2004 and 2005 (the most recent available), which provides a sample of all US outpatient practices. Only 7% of an estimated 1,345,000 patients diagnosed with ureteral stones were prescribed either tamsulosin or nifedipine, and urologists cared for most of those.
These unpublished data show that physicians in academic medical centers are increasingly adopting the practice of using tamsulosin or nifedipine for expulsion of ureteral stones, that urologists appear to be the first to begin using these medications in outpatients several years ago, and that this practice is being adopted actively in selected academic medical centers.
CAVEATS: Is either drug better? Too little data to tell
Our conclusion is that the strengths of this meta-analysis outweigh the weaknesses, the findings across studies are consistent, and the use of smooth-muscle relaxants for this indication makes sense from a mechanistic point of view.
The quality of a meta-analysis is only as good as the quality of the included studies, and, in this case, the overall quality of studies was not uniformly high. Median Jadad score, a summary measure of study quality, was 2, and the highest score was 3 (of a maximum of 5). The most common problem was lack of blinding, which can be critical in studies with subjective outcomes such as pain. We doubt that the lack of blinding led to any significant misclassification of outcome in this study, however.
Patients either passed the stone or they didn’t, or had a surgical intervention or not. It is reassuring that, when the best quality studies (Jadad score= 3) were analyzed separately, the results were equally good.
There have not been sufficient head-to-head trials to know if one is better than the other. We prefer α-antagonists because of the lower apparent side-effect profile. Our analysis of the UHC data shows that most of the physicians who are using medical therapy are using tamsulosin primarily for this diagnosis.
The majority of the patients in the studies included in the meta-analysis had been referred to a urologist. This raises the possibility that this treatment may not be as effective in patients with less severe symptoms for whom urological consultation is not necessary.
CHALLENGES TO IMPLEMENTATION: This change should be easy to put into practice
Tamsulosin is the best studied of the drugs, but also the most expensive. Based on the estimated number need to treat (NNT) of between 3 and 4 to prevent a surgical intervention and an estimated cost of around $90 for 1 month (www. drugstore.com, February 16, 2008), tamsulosin seems like a good investment to avoid surgical intervention.
The evidence for the other α-antagonists is consistent with that of tamsulosin, but there are fewer data, so it is not clear that the other agents will work as well.
Many people with renal colic are diagnosed and treated in the emergency department; they may not see their family physician until some time after the stone is diagnosed. It is unclear what effect this delay might have on medication effectiveness.
Neither tamsulosin nor nifedipine have an FDA indication for ureterolithiasis. However, they are prescribed commonly, and most physicians are familiar with their use and adverse-effect profiles.
Drugs used in the meta-analysis studies
α-Antagonists
Tamsulosin (Flomax)
Terazosin (Hytrin)
Doxazosin (Cardura)
Calcium channel blockers
Nifedipine (Adalat, Nifedical, Procardia)
Acknowledgement
We acknowledge Sofia Medvedev, PhD of the University HealthSystem Consortium (UHC) in Oak Brook, IL for analysis of the UHC Clinical Database and the National Ambulatory Medical Care Survey data.
PURLs methodology
This study was selected and evaluated using FPIN’s Priority Updates from the Research Literature (PURL) Surveillance System methodology. The criteria and findings leading to the selection of this study as a PURL can be accessed at www.jfponline.com/purls.
1. Singh A, Alter HJ, Littlepage A. A systematic review of medical therapy to facilitate passage of ureteral calculi. Ann Emerg Med. 2007;50:552-563.
2. Teichman JM. Clinical practice. Acute renal colic from ureteral calculus. N Engl J Med. 2004;350:684-693.
3. Stamatelou KK, Francis ME, Jones CA, Nyberg LM. Curhan GC. Time trends in reported prevalence of kidney stones in the United States: 1976-1994. Kidney International. 2003;63:1817-1823.
4. American Urological Association. Clinical Guidelines: Ureteral Calculi. Last updated 2007. Available at: http://www.auanet.org/guidelines/uretcal07.cfm. Accessed February 11, 2008.
5. Papa L, Stiell IG, Wells GA, Ball I, Battram E, Mahoney JE. Predicting intervention in renal colic patients after emergency department evaluation. Can J Emerg Med. 2005;7:78-86.
6. Pearle MS, Calhoun EA, Curhan GC. Urologic Diseases of America Project. Urologic diseases in America project: urolithiasis. J Urol. 2005;173:848-857.
7. Morse RM, Resnick MI. Ureteral calculi: natural history and treatment in an era of advanced technology. J Urol. 1991;145:263-265.
8. Peters HJ, Eckstein W. Possible pharmacological means of treating renal colic. Urol Res. 1975;3:55-59.
9. Borghi L, Meschi T, Amato F, Novarini A, Giannini A, Quarantelli C, et al. Nifedipine and methylpredniso-lone in facilitating ureteral stone passage: a randomized, double-blind, placebo-controlled study. J Urol. 1994;152:1095-1098.
10. Hollingsworth JM, Rogers MA, Kaufman SR, Bradford TJ, Saint S, Wei JT, et al. Medical therapy to facilitate urinary stone passage: a meta-analysis. Lancet. 2006;368:1171-1179.
Prescribe tamsulosin (typically 0.4 mg daily) or nifedipine (typically 30 mg daily) for patients with lower ureteral calculi, to speed stone passage and to avoid surgical intervention
Strength of recommendation
A: Meta-analysis of randomized controlled trials
Singh A, Alter HJ, Littlepage A. A systematic review of medical therapy to facilitate passage of ureteral calculi. Ann Emerg Med. 2007; 50:552-563.1
ILLUSTRATIVE CASE
A 52-year-old man presents to your office for follow-up 2 days after he was seen in the ED and diagnosed with a distal ureteral calculus, his first. His pain is reasonably well controlled, but he has not yet passed the stone. Is there anything you can do to help him pass the stone?
Yes. Patients who are candidates for observation should be offered a trial of “medical expulsive therapy” using an α-antagonist or a calcium channel blocker. Until now, medical therapy for kidney stones consisted of pain relief only.
The ordeal of a first stone is all too common—the lifetime prevalence of kidney stones is 5.2%—and the probability of recurrence is about 50%.2,3
NHANES data show increasing prevalence between the periods 1976-1980 and 1988-1996.3 One fifth to one third of kidney stones require surgical intervention.4 In a cohort of 245 patients presenting to an ED in Canada, 50 (20%) required further procedures, including lithotripsy. Stones ≥ 6 mm in size were much less likely to pass (OR=10.7, 95% CI 4.6-24.8).5 The burden on the healthcare system is significant; there are approximately 2 million out-patient visits annually for this problem, and diagnosis and treatment costs about $2 billion annually.6
Watch and wait
The standard approach is a period of watchful waiting and pain control, with urgent urological referral for patients with evidence of upper urinary tract infection, high grade obstruction, inadequate pain or nausea control, or insufficient renal reserve.2,4 Most patients treated with watchful waiting pass their stone within 4 weeks. Any stones that don’t pass within 8 weeks are unlikely to pass spontaneously.2,7
Medical therapy has been proposed for decades
Medications that relax ureteral smooth muscle to help pass ureteral stones have been proposed for decades.8 Prior to 2000, however, only 1 randomized controlled trial (RCT) of medical therapy for ureteral stones had been published.9 A subsequent meta-analysis found 9 studies and showed that medical therapy did increase the chances that a stone would pass.10 The Singh meta-analysis found 13 subsequently published studies and nearly tripled the number of patients evaluated.
STUDY SUMMARY: A well-done meta-analysis
This meta-analysis is based on 16 studies of α-antagonists (most used tamsulosin) and 9 studies of nifedipine, a calcium channel blocker.1 The studies were identified by a comprehensive search strategy that included Medline, EMBASE, and the Cochrane Controlled Trials Register from January 1980 to January 2007. The authors included all randomized trials or controlled clinical trials of medical therapy for adults with acute ureteral colic.
The authors assessed the studies for quality using the Jadad scale, a validated scale of study quality. Higher scores represent better quality, including better documentation of randomization, blinding, and follow-up. The authors specified their planned sensitivity analyses, and used the random effects model to synthesize the results, which tends to provide a more conservative estimate of the effect.
In other words, this was a very well done meta-analysis.
Twenty-two studies met the inclusion criteria: 13 of α-antagonists, 6 of nifedipine, and 3 of both. In 13 of the 16 studies of α-antagonists, tamsulosin (Flomax) was the study drug. The results from the terazosin (Hytrin) and doxazosin (Cardura) studies were included with the tamsulosin studies. The Jadad quality scores of the 22 studies were fairly low, with a median of 2 (range of 0 to 3) on the 5-point scale. The most common deduction was because the study was not double-blinded.
Medical therapy makes sense
“Therapy using either α-antagonists or calcium channel blockers augments the stone expulsion rate compared to standard therapy for moderately sized distal ureteral stones.” 1 CT showing distal ureteral stone
α-Antagonist studies
These 16 studies enrolled 1235 patients with distal ureteral stones. Mean stone size ranged from 4.3 to 7.8 mm. α-Antagonists improved the stone expulsion rate (RR= 1.59, 95% CI 1.44-1.75; NNT=3.3).
The mean time to expulsion of the stone ranged from 2.7 to 14.2 days and duration of therapy ranged from 1 to 7 weeks. In the 9 trials that reported the time to stone expulsion, the stone came out between 2 and 6 days earlier than the control groups.
Adverse effects were reported in 4% of patients receiving the active medication; most were mild.
Nifedipine studies
There were 686 patients in the 9 trials of nifedipine. The mean stone size was 3.9 to 12.8 mm. Some studies included stones in the more proximal as well as the distal ureter.
Nifedipine treatment increased the rate of stone expulsion (RR=1.5, 95% CI 1.34-1.68; NNT=3.9). Time to stone expulsion was shorter in 7 of the 9 studies.
Adverse effects were reported in 15% of the patients. Most of these were mild— nausea, vomiting, asthenia, and dyspepsia.
WHAT’S NEW: Strong evidence for use of medical therapy
The new findings from the Singh meta-analysis reviewed in this PURL supports physicians who have already adopted this practice and should encourage usage by those who have not yet done so.
Inpatients in academic medical centers
There is a growing trend to use tamsulosin to facilitate passage of ureteral stones. The University Health System Consortium (www.uhc.org) has complete clinical data on inpatients with ureteral stones, from 64 academic medical centers and teaching hospitals, between 2003 and 2007. We used this database to analyze trends in the use of tamsulosin in 4300 inpatients with ureteral stones (ICD 9 code 5921).
In 2003, only 3.3% of patients with a discharge diagnosis of ureteral stone received tamsulosin. In 2007, 34.1% of patients with ureteral stones discharged from these hospitals received tamsulosin, with similar rates of use when stratified by the specialty of the attending physician at discharge (family medicine, emergency medicine, internal medicine, urology) (FIGURE 1). We noted a wide range in the rate of adoption of this practice among academic medical centers: 48% in the centers with the highest rate of usage and 4.4% in the centers with the lowest rate.
FIGURE 1
% of inpatients in academic medical centers who received tamsulosin for ureteral stones, by year
Source: Unpublished data from the University Health System Consortium
Outpatients from a sample of US practices
The use of tamsulosin or nifedipine in outpatient practice was infrequent even 2 or 3 years ago. We used the National Ambulatory Medical Care Survey data (www.cdc.gov/nchs/about/major/ahcd/ahcd1.htm) from 2004 and 2005 (the most recent available), which provides a sample of all US outpatient practices. Only 7% of an estimated 1,345,000 patients diagnosed with ureteral stones were prescribed either tamsulosin or nifedipine, and urologists cared for most of those.
These unpublished data show that physicians in academic medical centers are increasingly adopting the practice of using tamsulosin or nifedipine for expulsion of ureteral stones, that urologists appear to be the first to begin using these medications in outpatients several years ago, and that this practice is being adopted actively in selected academic medical centers.
CAVEATS: Is either drug better? Too little data to tell
Our conclusion is that the strengths of this meta-analysis outweigh the weaknesses, the findings across studies are consistent, and the use of smooth-muscle relaxants for this indication makes sense from a mechanistic point of view.
The quality of a meta-analysis is only as good as the quality of the included studies, and, in this case, the overall quality of studies was not uniformly high. Median Jadad score, a summary measure of study quality, was 2, and the highest score was 3 (of a maximum of 5). The most common problem was lack of blinding, which can be critical in studies with subjective outcomes such as pain. We doubt that the lack of blinding led to any significant misclassification of outcome in this study, however.
Patients either passed the stone or they didn’t, or had a surgical intervention or not. It is reassuring that, when the best quality studies (Jadad score= 3) were analyzed separately, the results were equally good.
There have not been sufficient head-to-head trials to know if one is better than the other. We prefer α-antagonists because of the lower apparent side-effect profile. Our analysis of the UHC data shows that most of the physicians who are using medical therapy are using tamsulosin primarily for this diagnosis.
The majority of the patients in the studies included in the meta-analysis had been referred to a urologist. This raises the possibility that this treatment may not be as effective in patients with less severe symptoms for whom urological consultation is not necessary.
CHALLENGES TO IMPLEMENTATION: This change should be easy to put into practice
Tamsulosin is the best studied of the drugs, but also the most expensive. Based on the estimated number need to treat (NNT) of between 3 and 4 to prevent a surgical intervention and an estimated cost of around $90 for 1 month (www. drugstore.com, February 16, 2008), tamsulosin seems like a good investment to avoid surgical intervention.
The evidence for the other α-antagonists is consistent with that of tamsulosin, but there are fewer data, so it is not clear that the other agents will work as well.
Many people with renal colic are diagnosed and treated in the emergency department; they may not see their family physician until some time after the stone is diagnosed. It is unclear what effect this delay might have on medication effectiveness.
Neither tamsulosin nor nifedipine have an FDA indication for ureterolithiasis. However, they are prescribed commonly, and most physicians are familiar with their use and adverse-effect profiles.
Drugs used in the meta-analysis studies
α-Antagonists
Tamsulosin (Flomax)
Terazosin (Hytrin)
Doxazosin (Cardura)
Calcium channel blockers
Nifedipine (Adalat, Nifedical, Procardia)
Acknowledgement
We acknowledge Sofia Medvedev, PhD of the University HealthSystem Consortium (UHC) in Oak Brook, IL for analysis of the UHC Clinical Database and the National Ambulatory Medical Care Survey data.
PURLs methodology
This study was selected and evaluated using FPIN’s Priority Updates from the Research Literature (PURL) Surveillance System methodology. The criteria and findings leading to the selection of this study as a PURL can be accessed at www.jfponline.com/purls.
Prescribe tamsulosin (typically 0.4 mg daily) or nifedipine (typically 30 mg daily) for patients with lower ureteral calculi, to speed stone passage and to avoid surgical intervention
Strength of recommendation
A: Meta-analysis of randomized controlled trials
Singh A, Alter HJ, Littlepage A. A systematic review of medical therapy to facilitate passage of ureteral calculi. Ann Emerg Med. 2007; 50:552-563.1
ILLUSTRATIVE CASE
A 52-year-old man presents to your office for follow-up 2 days after he was seen in the ED and diagnosed with a distal ureteral calculus, his first. His pain is reasonably well controlled, but he has not yet passed the stone. Is there anything you can do to help him pass the stone?
Yes. Patients who are candidates for observation should be offered a trial of “medical expulsive therapy” using an α-antagonist or a calcium channel blocker. Until now, medical therapy for kidney stones consisted of pain relief only.
The ordeal of a first stone is all too common—the lifetime prevalence of kidney stones is 5.2%—and the probability of recurrence is about 50%.2,3
NHANES data show increasing prevalence between the periods 1976-1980 and 1988-1996.3 One fifth to one third of kidney stones require surgical intervention.4 In a cohort of 245 patients presenting to an ED in Canada, 50 (20%) required further procedures, including lithotripsy. Stones ≥ 6 mm in size were much less likely to pass (OR=10.7, 95% CI 4.6-24.8).5 The burden on the healthcare system is significant; there are approximately 2 million out-patient visits annually for this problem, and diagnosis and treatment costs about $2 billion annually.6
Watch and wait
The standard approach is a period of watchful waiting and pain control, with urgent urological referral for patients with evidence of upper urinary tract infection, high grade obstruction, inadequate pain or nausea control, or insufficient renal reserve.2,4 Most patients treated with watchful waiting pass their stone within 4 weeks. Any stones that don’t pass within 8 weeks are unlikely to pass spontaneously.2,7
Medical therapy has been proposed for decades
Medications that relax ureteral smooth muscle to help pass ureteral stones have been proposed for decades.8 Prior to 2000, however, only 1 randomized controlled trial (RCT) of medical therapy for ureteral stones had been published.9 A subsequent meta-analysis found 9 studies and showed that medical therapy did increase the chances that a stone would pass.10 The Singh meta-analysis found 13 subsequently published studies and nearly tripled the number of patients evaluated.
STUDY SUMMARY: A well-done meta-analysis
This meta-analysis is based on 16 studies of α-antagonists (most used tamsulosin) and 9 studies of nifedipine, a calcium channel blocker.1 The studies were identified by a comprehensive search strategy that included Medline, EMBASE, and the Cochrane Controlled Trials Register from January 1980 to January 2007. The authors included all randomized trials or controlled clinical trials of medical therapy for adults with acute ureteral colic.
The authors assessed the studies for quality using the Jadad scale, a validated scale of study quality. Higher scores represent better quality, including better documentation of randomization, blinding, and follow-up. The authors specified their planned sensitivity analyses, and used the random effects model to synthesize the results, which tends to provide a more conservative estimate of the effect.
In other words, this was a very well done meta-analysis.
Twenty-two studies met the inclusion criteria: 13 of α-antagonists, 6 of nifedipine, and 3 of both. In 13 of the 16 studies of α-antagonists, tamsulosin (Flomax) was the study drug. The results from the terazosin (Hytrin) and doxazosin (Cardura) studies were included with the tamsulosin studies. The Jadad quality scores of the 22 studies were fairly low, with a median of 2 (range of 0 to 3) on the 5-point scale. The most common deduction was because the study was not double-blinded.
Medical therapy makes sense
“Therapy using either α-antagonists or calcium channel blockers augments the stone expulsion rate compared to standard therapy for moderately sized distal ureteral stones.” 1 CT showing distal ureteral stone
α-Antagonist studies
These 16 studies enrolled 1235 patients with distal ureteral stones. Mean stone size ranged from 4.3 to 7.8 mm. α-Antagonists improved the stone expulsion rate (RR= 1.59, 95% CI 1.44-1.75; NNT=3.3).
The mean time to expulsion of the stone ranged from 2.7 to 14.2 days and duration of therapy ranged from 1 to 7 weeks. In the 9 trials that reported the time to stone expulsion, the stone came out between 2 and 6 days earlier than the control groups.
Adverse effects were reported in 4% of patients receiving the active medication; most were mild.
Nifedipine studies
There were 686 patients in the 9 trials of nifedipine. The mean stone size was 3.9 to 12.8 mm. Some studies included stones in the more proximal as well as the distal ureter.
Nifedipine treatment increased the rate of stone expulsion (RR=1.5, 95% CI 1.34-1.68; NNT=3.9). Time to stone expulsion was shorter in 7 of the 9 studies.
Adverse effects were reported in 15% of the patients. Most of these were mild— nausea, vomiting, asthenia, and dyspepsia.
WHAT’S NEW: Strong evidence for use of medical therapy
The new findings from the Singh meta-analysis reviewed in this PURL supports physicians who have already adopted this practice and should encourage usage by those who have not yet done so.
Inpatients in academic medical centers
There is a growing trend to use tamsulosin to facilitate passage of ureteral stones. The University Health System Consortium (www.uhc.org) has complete clinical data on inpatients with ureteral stones, from 64 academic medical centers and teaching hospitals, between 2003 and 2007. We used this database to analyze trends in the use of tamsulosin in 4300 inpatients with ureteral stones (ICD 9 code 5921).
In 2003, only 3.3% of patients with a discharge diagnosis of ureteral stone received tamsulosin. In 2007, 34.1% of patients with ureteral stones discharged from these hospitals received tamsulosin, with similar rates of use when stratified by the specialty of the attending physician at discharge (family medicine, emergency medicine, internal medicine, urology) (FIGURE 1). We noted a wide range in the rate of adoption of this practice among academic medical centers: 48% in the centers with the highest rate of usage and 4.4% in the centers with the lowest rate.
FIGURE 1
% of inpatients in academic medical centers who received tamsulosin for ureteral stones, by year
Source: Unpublished data from the University Health System Consortium
Outpatients from a sample of US practices
The use of tamsulosin or nifedipine in outpatient practice was infrequent even 2 or 3 years ago. We used the National Ambulatory Medical Care Survey data (www.cdc.gov/nchs/about/major/ahcd/ahcd1.htm) from 2004 and 2005 (the most recent available), which provides a sample of all US outpatient practices. Only 7% of an estimated 1,345,000 patients diagnosed with ureteral stones were prescribed either tamsulosin or nifedipine, and urologists cared for most of those.
These unpublished data show that physicians in academic medical centers are increasingly adopting the practice of using tamsulosin or nifedipine for expulsion of ureteral stones, that urologists appear to be the first to begin using these medications in outpatients several years ago, and that this practice is being adopted actively in selected academic medical centers.
CAVEATS: Is either drug better? Too little data to tell
Our conclusion is that the strengths of this meta-analysis outweigh the weaknesses, the findings across studies are consistent, and the use of smooth-muscle relaxants for this indication makes sense from a mechanistic point of view.
The quality of a meta-analysis is only as good as the quality of the included studies, and, in this case, the overall quality of studies was not uniformly high. Median Jadad score, a summary measure of study quality, was 2, and the highest score was 3 (of a maximum of 5). The most common problem was lack of blinding, which can be critical in studies with subjective outcomes such as pain. We doubt that the lack of blinding led to any significant misclassification of outcome in this study, however.
Patients either passed the stone or they didn’t, or had a surgical intervention or not. It is reassuring that, when the best quality studies (Jadad score= 3) were analyzed separately, the results were equally good.
There have not been sufficient head-to-head trials to know if one is better than the other. We prefer α-antagonists because of the lower apparent side-effect profile. Our analysis of the UHC data shows that most of the physicians who are using medical therapy are using tamsulosin primarily for this diagnosis.
The majority of the patients in the studies included in the meta-analysis had been referred to a urologist. This raises the possibility that this treatment may not be as effective in patients with less severe symptoms for whom urological consultation is not necessary.
CHALLENGES TO IMPLEMENTATION: This change should be easy to put into practice
Tamsulosin is the best studied of the drugs, but also the most expensive. Based on the estimated number need to treat (NNT) of between 3 and 4 to prevent a surgical intervention and an estimated cost of around $90 for 1 month (www. drugstore.com, February 16, 2008), tamsulosin seems like a good investment to avoid surgical intervention.
The evidence for the other α-antagonists is consistent with that of tamsulosin, but there are fewer data, so it is not clear that the other agents will work as well.
Many people with renal colic are diagnosed and treated in the emergency department; they may not see their family physician until some time after the stone is diagnosed. It is unclear what effect this delay might have on medication effectiveness.
Neither tamsulosin nor nifedipine have an FDA indication for ureterolithiasis. However, they are prescribed commonly, and most physicians are familiar with their use and adverse-effect profiles.
Drugs used in the meta-analysis studies
α-Antagonists
Tamsulosin (Flomax)
Terazosin (Hytrin)
Doxazosin (Cardura)
Calcium channel blockers
Nifedipine (Adalat, Nifedical, Procardia)
Acknowledgement
We acknowledge Sofia Medvedev, PhD of the University HealthSystem Consortium (UHC) in Oak Brook, IL for analysis of the UHC Clinical Database and the National Ambulatory Medical Care Survey data.
PURLs methodology
This study was selected and evaluated using FPIN’s Priority Updates from the Research Literature (PURL) Surveillance System methodology. The criteria and findings leading to the selection of this study as a PURL can be accessed at www.jfponline.com/purls.
1. Singh A, Alter HJ, Littlepage A. A systematic review of medical therapy to facilitate passage of ureteral calculi. Ann Emerg Med. 2007;50:552-563.
2. Teichman JM. Clinical practice. Acute renal colic from ureteral calculus. N Engl J Med. 2004;350:684-693.
3. Stamatelou KK, Francis ME, Jones CA, Nyberg LM. Curhan GC. Time trends in reported prevalence of kidney stones in the United States: 1976-1994. Kidney International. 2003;63:1817-1823.
4. American Urological Association. Clinical Guidelines: Ureteral Calculi. Last updated 2007. Available at: http://www.auanet.org/guidelines/uretcal07.cfm. Accessed February 11, 2008.
5. Papa L, Stiell IG, Wells GA, Ball I, Battram E, Mahoney JE. Predicting intervention in renal colic patients after emergency department evaluation. Can J Emerg Med. 2005;7:78-86.
6. Pearle MS, Calhoun EA, Curhan GC. Urologic Diseases of America Project. Urologic diseases in America project: urolithiasis. J Urol. 2005;173:848-857.
7. Morse RM, Resnick MI. Ureteral calculi: natural history and treatment in an era of advanced technology. J Urol. 1991;145:263-265.
8. Peters HJ, Eckstein W. Possible pharmacological means of treating renal colic. Urol Res. 1975;3:55-59.
9. Borghi L, Meschi T, Amato F, Novarini A, Giannini A, Quarantelli C, et al. Nifedipine and methylpredniso-lone in facilitating ureteral stone passage: a randomized, double-blind, placebo-controlled study. J Urol. 1994;152:1095-1098.
10. Hollingsworth JM, Rogers MA, Kaufman SR, Bradford TJ, Saint S, Wei JT, et al. Medical therapy to facilitate urinary stone passage: a meta-analysis. Lancet. 2006;368:1171-1179.
1. Singh A, Alter HJ, Littlepage A. A systematic review of medical therapy to facilitate passage of ureteral calculi. Ann Emerg Med. 2007;50:552-563.
2. Teichman JM. Clinical practice. Acute renal colic from ureteral calculus. N Engl J Med. 2004;350:684-693.
3. Stamatelou KK, Francis ME, Jones CA, Nyberg LM. Curhan GC. Time trends in reported prevalence of kidney stones in the United States: 1976-1994. Kidney International. 2003;63:1817-1823.
4. American Urological Association. Clinical Guidelines: Ureteral Calculi. Last updated 2007. Available at: http://www.auanet.org/guidelines/uretcal07.cfm. Accessed February 11, 2008.
5. Papa L, Stiell IG, Wells GA, Ball I, Battram E, Mahoney JE. Predicting intervention in renal colic patients after emergency department evaluation. Can J Emerg Med. 2005;7:78-86.
6. Pearle MS, Calhoun EA, Curhan GC. Urologic Diseases of America Project. Urologic diseases in America project: urolithiasis. J Urol. 2005;173:848-857.
7. Morse RM, Resnick MI. Ureteral calculi: natural history and treatment in an era of advanced technology. J Urol. 1991;145:263-265.
8. Peters HJ, Eckstein W. Possible pharmacological means of treating renal colic. Urol Res. 1975;3:55-59.
9. Borghi L, Meschi T, Amato F, Novarini A, Giannini A, Quarantelli C, et al. Nifedipine and methylpredniso-lone in facilitating ureteral stone passage: a randomized, double-blind, placebo-controlled study. J Urol. 1994;152:1095-1098.
10. Hollingsworth JM, Rogers MA, Kaufman SR, Bradford TJ, Saint S, Wei JT, et al. Medical therapy to facilitate urinary stone passage: a meta-analysis. Lancet. 2006;368:1171-1179.
Copyright © 2008 The Family Physicians Inquiries Network.
All rights reserved.
Give vitamin C to avert lingering pain after fracture
Vitamin C 500 mg daily for 50 days reduced the risk of complex regional pain syndrome for patients with a wrist fracture.
We think vitamin C 500 mg a day for 7 weeks is well worth recommending.1
Strength of recommendation
A: Based on 2 consistent, well-designed randomized controlled trials (RCTs)
Zollinger PE, Tuinebreijer WE, Breederveld RS, Kreis RW. Can vitamin C prevent complex regional pain syndrome in patients with wrist fractures? A randomized, controlled, multicenter dose-response study. J Bone Joint Surg Am 2007; 89:1424–1431.1
Illustrative case
Your patient is an 83-year-old woman who fell at home. radiographs show a distal radial fracture, which is treated with casting. You know that a quarter of patients with wrist fractures will suffer from complex regional pain syndrome, and there is no well-established treatment for it. Is there any way to reduce this woman’s chance of getting this painful syndrome?
BACKGROUND: Often misdiagnosed
We were surprised to learn how commonly patients suffer from complex regional pain syndrome (CRPS) after a fracture.
We think this diagnosis is frequently missed or misdiagnosed. Even with resolution, however, symptoms can be bothersome—and in 1% to 2% of cases, quite severe.
CRPS, a syndrome of pain and autonomic dysfunction after trauma, is divided into 2 types:
- type I has no obvious damage to nerves
- type II is due to definite damage to nerves (causalgia).
The etiology of CRPS (all further references here will be to type I) is still unclear, but not for lack of proposed theories. Sigmund Freud suggested that it has an origin in personality; there is little evidence to support his theory.2
Other theories include microtrauma to nerves, sympathetic nervous system abnormalities (hence the former name, reflex sympathetic dystrophy), abnormalities of the inflammatory response, and physiologic responses to immobilization. It is often described as a biphasic syndrome, with early edema followed by contracture and stiffness. It typically affects the extremities.2
CRPS more likely in women. A population-based study in Olmsted County, MN found an incidence of 5.5 per 100,000 person-years, with a prevalence of 20.6 per 100,000. Women were affected 4 times more than men.3 Fracture (46%) and sprain (12%) were the leading triggers, followed by other injuries, including crush, stroke, and contusion.
Bernard Ewigman, MD, MSPH
Department of Family Medicine
The University of Chicago
Apparently quite a few patients with complex regional pain syndrome (CRPS) saw me during my 20 years of practice, but I did not see them, or at least I did not recognize their symptoms.
As many as 50% of cast complaints—or post-cast complaints—probably represented CRPS. I wrote them off in all but the most severe cases, which were so dramatic they couldn’t be written off.
I vividly remember the suffering those patients experienced, as well as my feelings of helplessness to offer any relief. CRPS is still not treatable, but now we know that vitamin C can help prevent it, or at least shorten its severity and duration. Granted, the symptoms can be mild, and most resolve spontaneously, but it can go on for months and it can be truly horrific in a small percent (1%–2%).
Here is an instance in which an ounce of prevention is worth more than a pound of cure.
Over half of patients may suffer
Despite typically reported rates of 1% to 2% for severe, chronic CRPS following these injuries, it appears that milder cases are substantially more common.
In a cohort of 274 patients with Colles’s fractures, at 2 weeks, 24% met all 4 of the criteria used in the study to define CRPS, specifically:
- tenderness
- vascular instability
- stiffness
- objective swelling of areas distal to and distinctive from the fracture.
Although 48% met none of the criteria, the remaining 28% had at least some of the criteria.4
Most patients recover. Patients with partial CRPS improved more rapidly than those with CRPS; by 5 months, most had recovered completely. Patients with definitive CRPS also improved, although about 65% still reported stiffness in hands and wrists at 5 months. Another cohort study of 100 patients, also with Colles’s fractures, found similar rates of CRPS 9 weeks.5
CLINICAL CONTEXT: Treatments are not very effective
A systematic review of therapeutic options found 18 randomized controlled studies evaluating possible therapies for CRPS.6 The overall quality of data was low. The authors concluded there was little to no evidence for sympathetic blockade (either via stellate ganglion block or RIS block), radical scavenging with DMSO, prednisolone, acupuncture, or manual lymph drainage. Bisphosphonates and calcitonin, as well as qigong exercises, did show some potential, but data were too limited to draw a firm conclusion.
Guidelines recommend early intervention with physical and psychological therapy, as well as adequate pain control.7
The systematic review also identified 2 studies of preventive interventions. A pilot study of vitamin C (by the authors of the trial that is the subject of this PURL) showed some efficacy.8 An RCT of IV guanethidine found no benefit compared with saline.6
STUDY SUMMARY: Vitamin C reduced the rate of CRPS
This randomized, multicenter, dose-ranging, placebo-controlled trial was performed at 3 hospitals in the Netherlands.1 Any adult (>18 years of age) with a fracture of one or both wrists treated in the emergency departments of these hospitals was invited to participate. During 2001–2004, there were 2137 patients with wrist fractures. Of these, 416 (19.5%) patients (with 427 fractures) were enrolled in the study. The study was double-blinded, and allocation was adequately concealed. There was 100% follow-up of all patients. Of enrolled patients, 82.4% were women, and the average age of all subjects was 62.4 years.
Patients were randomized into 1 of 4 groups: placebo, vitamin C 200 mg daily, vitamin C 500 mg daily, or vitamin C 1500 mg daily for 50 days. Other fracture therapy was undertaken at the discretion of the treating physician. Patients were evaluated at 1 week, 4 or 5 weeks (or cast removal), 6 or 7 weeks, 12 weeks, and 26 weeks. After 1 year, patients were contacted by phone or mail to confirm their status using Veldman’s criteria (TABLE 1).8
TABLE 1
Veldman’s criteria for diagnosis of complex regional pain syndrome, type 1
| Must have 4 of the 5 symptoms below, at the affected hand or wrist, or during activity with that wrist: |
|---|
|
10% of the placebo group had CRPS after 1 year
One year after the fracture, 10% of placebo patients had a diagnosis of CRPS. Rates of CRPS were 4%, 2%, and 2% in the 200 mg, 500 mg, 1500 mg daily dosing of vitamin C, respectively (TABLE 2).
There was no association between the development of CRPS and site of fracture, whether the fracture was displaced or intraarticular, or whether surgical therapy was chosen (although 90% of the fractures were treated with casting). Of note: all of the patients who developed CRPS were female; however, only 75 men were enrolled (18%).
Older patients were at increased risk, and patients with complaints about their cast were substantially more likely to have CRPS (number needed to harm [NNH]=2.6; odds ratio [OR]=5.73; 95% confidence interval [CI], 2.11–15.57).
TABLE 2
Rates of complex regional pain syndrome at 1 year: 10% placebo, 2.4% vitamin C
| TREATMENT GROUP | PERCENT WITH CRPS | RR (95% CI ) | ARR | NNT |
|---|---|---|---|---|
| Placebo | 10% | |||
| Vitamin C | ||||
| All doses combined | 2.4% | 0.24 (0.10–0.60) | 0.076 | 13 |
| 200 mg | 4% | 0.41 (0.13–1.27) | 0.06 | 17 |
| 500 mg | 2% | 0.17 (0.04–0.77) | 0.08 | 13 |
| 1500 mg | 2% | 0.17 (0.04–0.75) | 0.08 | 13 |
| CRPS, complex regional pain syndrome; RR, relative risk; CI, confidence interval; ARR, absolute risk reduction; NNT, number needed to treat. | ||||
| Source: Zollinger et al, 2007.1 | ||||
WHAT’S NEW?: Effective dose: 500 mg/d vitamin C for 50 days
Vitamin C at a dose of at least 500 mg/day for 50 days reduced the rate of CRPS from 10% to 2% (number needed to treat [NNT]=13). This is the second study undertaken by the same investigators to demonstrate risk reduction.8 The previous study enrolled only 129 patients, but found an absolute risk reduction of 15% (NNT=7; P<.05) for patients taking 500 mg of vitamin C.
Patients who complained about their casts were at substantially higher risk of being diagnosed with CRPS (OR=10.0; 95% CI, 2.9–33), suggesting that cast complaints may be a harbinger.
The more recent study was also designed to determine the effective dose for vitamin C. Doses of 200 mg daily reduced the risk, but the effect was not statistically significant. The effect size for the 500 mg and 1500 mg doses, on the other hand, were essentially identical, and both statistically and clinically significant.1
CAVEATS: Selection bias?
The study enrolled less than 20% of potentially eligible patients, raising the possibility that only patients who might benefit from vitamin C prophylaxis were enrolled. However, almost two thirds of those eligible were either never approached due to the emergency department being busy (43%), or refused randomization (14%) after they were informed in the consent process that there was evidence of benefit of vitamin C, based on the prior trial.8 Therefore, selection bias seems an unlikely explanation for the positive results. This is the second trial to show the same finding, which is reassuring.
No men had CRPS in either group in this study, so there is no evidence to show whether or not this intervention works in men. We are unaware of any physiologic reason to suggest that vitamin C would have a differential effect in men. In the earlier study, only 1 man (in the placebo group) got CRPS, for an absolute risk difference of 0.08 (95% CI, –0.07 to 0.27).8
What are the diagnostic criteria?
There is no universal agreement on the diagnostic criteria for CRPS. This study used Veldman’s criteria (TABLE 1), which is the standard criteria used in The Netherlands, and has the best inter-rater reliability of the current criteria.9 Criteria from the International Association of Studies in Pain are the most widely cited in the literature, but are not particularly specific or reproducible.9
CHALLENGES TO IMPLEMENTATION: Getting vitamin C started
Recommending 500 mg of vitamin C daily for 7 weeks is a simple and low-cost intervention. Many of our patients will be treated acutely in emergency rooms or by orthopedic surgeons. If these clinicians do not initiate the vitamin C, it may be some time before the primary physician can begin this therapy. We don’t have any information on whether a delay in initiation affects the efficacy of vitamin C.
The evidence presented here is for Colles’s fractures, but CRPS definitely follows other fractures. We are unaware of any physiologic reason why vitamin C therapy would behave any differently for other fracture locations.
It’s a mistake to think CRPS is rare
Perhaps the greatest challenge to implementation is the perception that CRPS is a rare phenomenon or at least generally resolves spontaneously.
The rate in the placebo group (1 in 10 diagnosed at 1 year) and the rates reported through systematic surveillance (1 in 4 diagnosed at some point following Colles’s fracture) struck both us and the clinicians reviewing this study as high.
We suspect symptoms are often missed or misdiagnosed. Even with resolution, the symptoms can be bothersome, and quite severe in a few cases (1% to 2%). We think vitamin C 500 mg/day for 7 weeks is well worth recommending.
PURLs methodology
This study was selected and evaluated using FPIN’s Priority Updates from the Research Literature (PURL) Surveillance System methodology. The criteria and findings leading to the selection of this study as a PURL can be accessed at www.jfponline.com/purls.
1. Zollinger PE, Tuinebreijer WE, Breederveld RS, Kreis RW. Can vitamin C prevent complex regional pain syndrome in patients with wrist fractures? A randomized, controlled, multicenter dose-response study. J Bone Joint Surg Am 2007;89:1424-1431
2. Atkins RM. Complex regional pain syndrome. J Bone Joint Surg Br 2003;85:1100-1106
3. Sandroni P, Benrud-Larson LM, McClelland RL, Low PA. Complex regional pain syndrome type I: incidence and prevalence in Olmsted county, a population-based study. Pain 2003;103:199-207
4. Bickerstaff DR, Kanis JA. Algodystrophy: an under-recognized complication of minor trauma. Br J Rheumatol 1994;33:240-248
5. Field J, Atkins RM. Algodystrophy is an early complication of Colles’ fracture. What are the implications? J Hand Surg [Br] 1997;22:178-182
6. Forouzanfar T, Koke AJ, van Kleef M, Weber WE. Treatment of complex regional pain syndrome type I. Eur J Pain 2002;6:105-122
7. Quisel A, Gill JM, Witherell P. Complex regional pain syndrome: which treatments show promise? J Fam Pract 2005;54:599-603
8. Zollinger PE, Tuinebreijer WE, Kreis RW, Breederveld RS. Effect of vitamin C on frequency of reflex sympathetic dystrophy in wrist fractures: a randomised trial. Lancet 1999;354:2025-2028
9. Quisel A, Gill JM, Witherell P. Complex regional pain syndrome underdiagnosed. J Fam Pract 2005;54:524-532
Vitamin C 500 mg daily for 50 days reduced the risk of complex regional pain syndrome for patients with a wrist fracture.
We think vitamin C 500 mg a day for 7 weeks is well worth recommending.1
Strength of recommendation
A: Based on 2 consistent, well-designed randomized controlled trials (RCTs)
Zollinger PE, Tuinebreijer WE, Breederveld RS, Kreis RW. Can vitamin C prevent complex regional pain syndrome in patients with wrist fractures? A randomized, controlled, multicenter dose-response study. J Bone Joint Surg Am 2007; 89:1424–1431.1
Illustrative case
Your patient is an 83-year-old woman who fell at home. radiographs show a distal radial fracture, which is treated with casting. You know that a quarter of patients with wrist fractures will suffer from complex regional pain syndrome, and there is no well-established treatment for it. Is there any way to reduce this woman’s chance of getting this painful syndrome?
BACKGROUND: Often misdiagnosed
We were surprised to learn how commonly patients suffer from complex regional pain syndrome (CRPS) after a fracture.
We think this diagnosis is frequently missed or misdiagnosed. Even with resolution, however, symptoms can be bothersome—and in 1% to 2% of cases, quite severe.
CRPS, a syndrome of pain and autonomic dysfunction after trauma, is divided into 2 types:
- type I has no obvious damage to nerves
- type II is due to definite damage to nerves (causalgia).
The etiology of CRPS (all further references here will be to type I) is still unclear, but not for lack of proposed theories. Sigmund Freud suggested that it has an origin in personality; there is little evidence to support his theory.2
Other theories include microtrauma to nerves, sympathetic nervous system abnormalities (hence the former name, reflex sympathetic dystrophy), abnormalities of the inflammatory response, and physiologic responses to immobilization. It is often described as a biphasic syndrome, with early edema followed by contracture and stiffness. It typically affects the extremities.2
CRPS more likely in women. A population-based study in Olmsted County, MN found an incidence of 5.5 per 100,000 person-years, with a prevalence of 20.6 per 100,000. Women were affected 4 times more than men.3 Fracture (46%) and sprain (12%) were the leading triggers, followed by other injuries, including crush, stroke, and contusion.
Bernard Ewigman, MD, MSPH
Department of Family Medicine
The University of Chicago
Apparently quite a few patients with complex regional pain syndrome (CRPS) saw me during my 20 years of practice, but I did not see them, or at least I did not recognize their symptoms.
As many as 50% of cast complaints—or post-cast complaints—probably represented CRPS. I wrote them off in all but the most severe cases, which were so dramatic they couldn’t be written off.
I vividly remember the suffering those patients experienced, as well as my feelings of helplessness to offer any relief. CRPS is still not treatable, but now we know that vitamin C can help prevent it, or at least shorten its severity and duration. Granted, the symptoms can be mild, and most resolve spontaneously, but it can go on for months and it can be truly horrific in a small percent (1%–2%).
Here is an instance in which an ounce of prevention is worth more than a pound of cure.
Over half of patients may suffer
Despite typically reported rates of 1% to 2% for severe, chronic CRPS following these injuries, it appears that milder cases are substantially more common.
In a cohort of 274 patients with Colles’s fractures, at 2 weeks, 24% met all 4 of the criteria used in the study to define CRPS, specifically:
- tenderness
- vascular instability
- stiffness
- objective swelling of areas distal to and distinctive from the fracture.
Although 48% met none of the criteria, the remaining 28% had at least some of the criteria.4
Most patients recover. Patients with partial CRPS improved more rapidly than those with CRPS; by 5 months, most had recovered completely. Patients with definitive CRPS also improved, although about 65% still reported stiffness in hands and wrists at 5 months. Another cohort study of 100 patients, also with Colles’s fractures, found similar rates of CRPS 9 weeks.5
CLINICAL CONTEXT: Treatments are not very effective
A systematic review of therapeutic options found 18 randomized controlled studies evaluating possible therapies for CRPS.6 The overall quality of data was low. The authors concluded there was little to no evidence for sympathetic blockade (either via stellate ganglion block or RIS block), radical scavenging with DMSO, prednisolone, acupuncture, or manual lymph drainage. Bisphosphonates and calcitonin, as well as qigong exercises, did show some potential, but data were too limited to draw a firm conclusion.
Guidelines recommend early intervention with physical and psychological therapy, as well as adequate pain control.7
The systematic review also identified 2 studies of preventive interventions. A pilot study of vitamin C (by the authors of the trial that is the subject of this PURL) showed some efficacy.8 An RCT of IV guanethidine found no benefit compared with saline.6
STUDY SUMMARY: Vitamin C reduced the rate of CRPS
This randomized, multicenter, dose-ranging, placebo-controlled trial was performed at 3 hospitals in the Netherlands.1 Any adult (>18 years of age) with a fracture of one or both wrists treated in the emergency departments of these hospitals was invited to participate. During 2001–2004, there were 2137 patients with wrist fractures. Of these, 416 (19.5%) patients (with 427 fractures) were enrolled in the study. The study was double-blinded, and allocation was adequately concealed. There was 100% follow-up of all patients. Of enrolled patients, 82.4% were women, and the average age of all subjects was 62.4 years.
Patients were randomized into 1 of 4 groups: placebo, vitamin C 200 mg daily, vitamin C 500 mg daily, or vitamin C 1500 mg daily for 50 days. Other fracture therapy was undertaken at the discretion of the treating physician. Patients were evaluated at 1 week, 4 or 5 weeks (or cast removal), 6 or 7 weeks, 12 weeks, and 26 weeks. After 1 year, patients were contacted by phone or mail to confirm their status using Veldman’s criteria (TABLE 1).8
TABLE 1
Veldman’s criteria for diagnosis of complex regional pain syndrome, type 1
| Must have 4 of the 5 symptoms below, at the affected hand or wrist, or during activity with that wrist: |
|---|
|
10% of the placebo group had CRPS after 1 year
One year after the fracture, 10% of placebo patients had a diagnosis of CRPS. Rates of CRPS were 4%, 2%, and 2% in the 200 mg, 500 mg, 1500 mg daily dosing of vitamin C, respectively (TABLE 2).
There was no association between the development of CRPS and site of fracture, whether the fracture was displaced or intraarticular, or whether surgical therapy was chosen (although 90% of the fractures were treated with casting). Of note: all of the patients who developed CRPS were female; however, only 75 men were enrolled (18%).
Older patients were at increased risk, and patients with complaints about their cast were substantially more likely to have CRPS (number needed to harm [NNH]=2.6; odds ratio [OR]=5.73; 95% confidence interval [CI], 2.11–15.57).
TABLE 2
Rates of complex regional pain syndrome at 1 year: 10% placebo, 2.4% vitamin C
| TREATMENT GROUP | PERCENT WITH CRPS | RR (95% CI ) | ARR | NNT |
|---|---|---|---|---|
| Placebo | 10% | |||
| Vitamin C | ||||
| All doses combined | 2.4% | 0.24 (0.10–0.60) | 0.076 | 13 |
| 200 mg | 4% | 0.41 (0.13–1.27) | 0.06 | 17 |
| 500 mg | 2% | 0.17 (0.04–0.77) | 0.08 | 13 |
| 1500 mg | 2% | 0.17 (0.04–0.75) | 0.08 | 13 |
| CRPS, complex regional pain syndrome; RR, relative risk; CI, confidence interval; ARR, absolute risk reduction; NNT, number needed to treat. | ||||
| Source: Zollinger et al, 2007.1 | ||||
WHAT’S NEW?: Effective dose: 500 mg/d vitamin C for 50 days
Vitamin C at a dose of at least 500 mg/day for 50 days reduced the rate of CRPS from 10% to 2% (number needed to treat [NNT]=13). This is the second study undertaken by the same investigators to demonstrate risk reduction.8 The previous study enrolled only 129 patients, but found an absolute risk reduction of 15% (NNT=7; P<.05) for patients taking 500 mg of vitamin C.
Patients who complained about their casts were at substantially higher risk of being diagnosed with CRPS (OR=10.0; 95% CI, 2.9–33), suggesting that cast complaints may be a harbinger.
The more recent study was also designed to determine the effective dose for vitamin C. Doses of 200 mg daily reduced the risk, but the effect was not statistically significant. The effect size for the 500 mg and 1500 mg doses, on the other hand, were essentially identical, and both statistically and clinically significant.1
CAVEATS: Selection bias?
The study enrolled less than 20% of potentially eligible patients, raising the possibility that only patients who might benefit from vitamin C prophylaxis were enrolled. However, almost two thirds of those eligible were either never approached due to the emergency department being busy (43%), or refused randomization (14%) after they were informed in the consent process that there was evidence of benefit of vitamin C, based on the prior trial.8 Therefore, selection bias seems an unlikely explanation for the positive results. This is the second trial to show the same finding, which is reassuring.
No men had CRPS in either group in this study, so there is no evidence to show whether or not this intervention works in men. We are unaware of any physiologic reason to suggest that vitamin C would have a differential effect in men. In the earlier study, only 1 man (in the placebo group) got CRPS, for an absolute risk difference of 0.08 (95% CI, –0.07 to 0.27).8
What are the diagnostic criteria?
There is no universal agreement on the diagnostic criteria for CRPS. This study used Veldman’s criteria (TABLE 1), which is the standard criteria used in The Netherlands, and has the best inter-rater reliability of the current criteria.9 Criteria from the International Association of Studies in Pain are the most widely cited in the literature, but are not particularly specific or reproducible.9
CHALLENGES TO IMPLEMENTATION: Getting vitamin C started
Recommending 500 mg of vitamin C daily for 7 weeks is a simple and low-cost intervention. Many of our patients will be treated acutely in emergency rooms or by orthopedic surgeons. If these clinicians do not initiate the vitamin C, it may be some time before the primary physician can begin this therapy. We don’t have any information on whether a delay in initiation affects the efficacy of vitamin C.
The evidence presented here is for Colles’s fractures, but CRPS definitely follows other fractures. We are unaware of any physiologic reason why vitamin C therapy would behave any differently for other fracture locations.
It’s a mistake to think CRPS is rare
Perhaps the greatest challenge to implementation is the perception that CRPS is a rare phenomenon or at least generally resolves spontaneously.
The rate in the placebo group (1 in 10 diagnosed at 1 year) and the rates reported through systematic surveillance (1 in 4 diagnosed at some point following Colles’s fracture) struck both us and the clinicians reviewing this study as high.
We suspect symptoms are often missed or misdiagnosed. Even with resolution, the symptoms can be bothersome, and quite severe in a few cases (1% to 2%). We think vitamin C 500 mg/day for 7 weeks is well worth recommending.
PURLs methodology
This study was selected and evaluated using FPIN’s Priority Updates from the Research Literature (PURL) Surveillance System methodology. The criteria and findings leading to the selection of this study as a PURL can be accessed at www.jfponline.com/purls.
Vitamin C 500 mg daily for 50 days reduced the risk of complex regional pain syndrome for patients with a wrist fracture.
We think vitamin C 500 mg a day for 7 weeks is well worth recommending.1
Strength of recommendation
A: Based on 2 consistent, well-designed randomized controlled trials (RCTs)
Zollinger PE, Tuinebreijer WE, Breederveld RS, Kreis RW. Can vitamin C prevent complex regional pain syndrome in patients with wrist fractures? A randomized, controlled, multicenter dose-response study. J Bone Joint Surg Am 2007; 89:1424–1431.1
Illustrative case
Your patient is an 83-year-old woman who fell at home. radiographs show a distal radial fracture, which is treated with casting. You know that a quarter of patients with wrist fractures will suffer from complex regional pain syndrome, and there is no well-established treatment for it. Is there any way to reduce this woman’s chance of getting this painful syndrome?
BACKGROUND: Often misdiagnosed
We were surprised to learn how commonly patients suffer from complex regional pain syndrome (CRPS) after a fracture.
We think this diagnosis is frequently missed or misdiagnosed. Even with resolution, however, symptoms can be bothersome—and in 1% to 2% of cases, quite severe.
CRPS, a syndrome of pain and autonomic dysfunction after trauma, is divided into 2 types:
- type I has no obvious damage to nerves
- type II is due to definite damage to nerves (causalgia).
The etiology of CRPS (all further references here will be to type I) is still unclear, but not for lack of proposed theories. Sigmund Freud suggested that it has an origin in personality; there is little evidence to support his theory.2
Other theories include microtrauma to nerves, sympathetic nervous system abnormalities (hence the former name, reflex sympathetic dystrophy), abnormalities of the inflammatory response, and physiologic responses to immobilization. It is often described as a biphasic syndrome, with early edema followed by contracture and stiffness. It typically affects the extremities.2
CRPS more likely in women. A population-based study in Olmsted County, MN found an incidence of 5.5 per 100,000 person-years, with a prevalence of 20.6 per 100,000. Women were affected 4 times more than men.3 Fracture (46%) and sprain (12%) were the leading triggers, followed by other injuries, including crush, stroke, and contusion.
Bernard Ewigman, MD, MSPH
Department of Family Medicine
The University of Chicago
Apparently quite a few patients with complex regional pain syndrome (CRPS) saw me during my 20 years of practice, but I did not see them, or at least I did not recognize their symptoms.
As many as 50% of cast complaints—or post-cast complaints—probably represented CRPS. I wrote them off in all but the most severe cases, which were so dramatic they couldn’t be written off.
I vividly remember the suffering those patients experienced, as well as my feelings of helplessness to offer any relief. CRPS is still not treatable, but now we know that vitamin C can help prevent it, or at least shorten its severity and duration. Granted, the symptoms can be mild, and most resolve spontaneously, but it can go on for months and it can be truly horrific in a small percent (1%–2%).
Here is an instance in which an ounce of prevention is worth more than a pound of cure.
Over half of patients may suffer
Despite typically reported rates of 1% to 2% for severe, chronic CRPS following these injuries, it appears that milder cases are substantially more common.
In a cohort of 274 patients with Colles’s fractures, at 2 weeks, 24% met all 4 of the criteria used in the study to define CRPS, specifically:
- tenderness
- vascular instability
- stiffness
- objective swelling of areas distal to and distinctive from the fracture.
Although 48% met none of the criteria, the remaining 28% had at least some of the criteria.4
Most patients recover. Patients with partial CRPS improved more rapidly than those with CRPS; by 5 months, most had recovered completely. Patients with definitive CRPS also improved, although about 65% still reported stiffness in hands and wrists at 5 months. Another cohort study of 100 patients, also with Colles’s fractures, found similar rates of CRPS 9 weeks.5
CLINICAL CONTEXT: Treatments are not very effective
A systematic review of therapeutic options found 18 randomized controlled studies evaluating possible therapies for CRPS.6 The overall quality of data was low. The authors concluded there was little to no evidence for sympathetic blockade (either via stellate ganglion block or RIS block), radical scavenging with DMSO, prednisolone, acupuncture, or manual lymph drainage. Bisphosphonates and calcitonin, as well as qigong exercises, did show some potential, but data were too limited to draw a firm conclusion.
Guidelines recommend early intervention with physical and psychological therapy, as well as adequate pain control.7
The systematic review also identified 2 studies of preventive interventions. A pilot study of vitamin C (by the authors of the trial that is the subject of this PURL) showed some efficacy.8 An RCT of IV guanethidine found no benefit compared with saline.6
STUDY SUMMARY: Vitamin C reduced the rate of CRPS
This randomized, multicenter, dose-ranging, placebo-controlled trial was performed at 3 hospitals in the Netherlands.1 Any adult (>18 years of age) with a fracture of one or both wrists treated in the emergency departments of these hospitals was invited to participate. During 2001–2004, there were 2137 patients with wrist fractures. Of these, 416 (19.5%) patients (with 427 fractures) were enrolled in the study. The study was double-blinded, and allocation was adequately concealed. There was 100% follow-up of all patients. Of enrolled patients, 82.4% were women, and the average age of all subjects was 62.4 years.
Patients were randomized into 1 of 4 groups: placebo, vitamin C 200 mg daily, vitamin C 500 mg daily, or vitamin C 1500 mg daily for 50 days. Other fracture therapy was undertaken at the discretion of the treating physician. Patients were evaluated at 1 week, 4 or 5 weeks (or cast removal), 6 or 7 weeks, 12 weeks, and 26 weeks. After 1 year, patients were contacted by phone or mail to confirm their status using Veldman’s criteria (TABLE 1).8
TABLE 1
Veldman’s criteria for diagnosis of complex regional pain syndrome, type 1
| Must have 4 of the 5 symptoms below, at the affected hand or wrist, or during activity with that wrist: |
|---|
|
10% of the placebo group had CRPS after 1 year
One year after the fracture, 10% of placebo patients had a diagnosis of CRPS. Rates of CRPS were 4%, 2%, and 2% in the 200 mg, 500 mg, 1500 mg daily dosing of vitamin C, respectively (TABLE 2).
There was no association between the development of CRPS and site of fracture, whether the fracture was displaced or intraarticular, or whether surgical therapy was chosen (although 90% of the fractures were treated with casting). Of note: all of the patients who developed CRPS were female; however, only 75 men were enrolled (18%).
Older patients were at increased risk, and patients with complaints about their cast were substantially more likely to have CRPS (number needed to harm [NNH]=2.6; odds ratio [OR]=5.73; 95% confidence interval [CI], 2.11–15.57).
TABLE 2
Rates of complex regional pain syndrome at 1 year: 10% placebo, 2.4% vitamin C
| TREATMENT GROUP | PERCENT WITH CRPS | RR (95% CI ) | ARR | NNT |
|---|---|---|---|---|
| Placebo | 10% | |||
| Vitamin C | ||||
| All doses combined | 2.4% | 0.24 (0.10–0.60) | 0.076 | 13 |
| 200 mg | 4% | 0.41 (0.13–1.27) | 0.06 | 17 |
| 500 mg | 2% | 0.17 (0.04–0.77) | 0.08 | 13 |
| 1500 mg | 2% | 0.17 (0.04–0.75) | 0.08 | 13 |
| CRPS, complex regional pain syndrome; RR, relative risk; CI, confidence interval; ARR, absolute risk reduction; NNT, number needed to treat. | ||||
| Source: Zollinger et al, 2007.1 | ||||
WHAT’S NEW?: Effective dose: 500 mg/d vitamin C for 50 days
Vitamin C at a dose of at least 500 mg/day for 50 days reduced the rate of CRPS from 10% to 2% (number needed to treat [NNT]=13). This is the second study undertaken by the same investigators to demonstrate risk reduction.8 The previous study enrolled only 129 patients, but found an absolute risk reduction of 15% (NNT=7; P<.05) for patients taking 500 mg of vitamin C.
Patients who complained about their casts were at substantially higher risk of being diagnosed with CRPS (OR=10.0; 95% CI, 2.9–33), suggesting that cast complaints may be a harbinger.
The more recent study was also designed to determine the effective dose for vitamin C. Doses of 200 mg daily reduced the risk, but the effect was not statistically significant. The effect size for the 500 mg and 1500 mg doses, on the other hand, were essentially identical, and both statistically and clinically significant.1
CAVEATS: Selection bias?
The study enrolled less than 20% of potentially eligible patients, raising the possibility that only patients who might benefit from vitamin C prophylaxis were enrolled. However, almost two thirds of those eligible were either never approached due to the emergency department being busy (43%), or refused randomization (14%) after they were informed in the consent process that there was evidence of benefit of vitamin C, based on the prior trial.8 Therefore, selection bias seems an unlikely explanation for the positive results. This is the second trial to show the same finding, which is reassuring.
No men had CRPS in either group in this study, so there is no evidence to show whether or not this intervention works in men. We are unaware of any physiologic reason to suggest that vitamin C would have a differential effect in men. In the earlier study, only 1 man (in the placebo group) got CRPS, for an absolute risk difference of 0.08 (95% CI, –0.07 to 0.27).8
What are the diagnostic criteria?
There is no universal agreement on the diagnostic criteria for CRPS. This study used Veldman’s criteria (TABLE 1), which is the standard criteria used in The Netherlands, and has the best inter-rater reliability of the current criteria.9 Criteria from the International Association of Studies in Pain are the most widely cited in the literature, but are not particularly specific or reproducible.9
CHALLENGES TO IMPLEMENTATION: Getting vitamin C started
Recommending 500 mg of vitamin C daily for 7 weeks is a simple and low-cost intervention. Many of our patients will be treated acutely in emergency rooms or by orthopedic surgeons. If these clinicians do not initiate the vitamin C, it may be some time before the primary physician can begin this therapy. We don’t have any information on whether a delay in initiation affects the efficacy of vitamin C.
The evidence presented here is for Colles’s fractures, but CRPS definitely follows other fractures. We are unaware of any physiologic reason why vitamin C therapy would behave any differently for other fracture locations.
It’s a mistake to think CRPS is rare
Perhaps the greatest challenge to implementation is the perception that CRPS is a rare phenomenon or at least generally resolves spontaneously.
The rate in the placebo group (1 in 10 diagnosed at 1 year) and the rates reported through systematic surveillance (1 in 4 diagnosed at some point following Colles’s fracture) struck both us and the clinicians reviewing this study as high.
We suspect symptoms are often missed or misdiagnosed. Even with resolution, the symptoms can be bothersome, and quite severe in a few cases (1% to 2%). We think vitamin C 500 mg/day for 7 weeks is well worth recommending.
PURLs methodology
This study was selected and evaluated using FPIN’s Priority Updates from the Research Literature (PURL) Surveillance System methodology. The criteria and findings leading to the selection of this study as a PURL can be accessed at www.jfponline.com/purls.
1. Zollinger PE, Tuinebreijer WE, Breederveld RS, Kreis RW. Can vitamin C prevent complex regional pain syndrome in patients with wrist fractures? A randomized, controlled, multicenter dose-response study. J Bone Joint Surg Am 2007;89:1424-1431
2. Atkins RM. Complex regional pain syndrome. J Bone Joint Surg Br 2003;85:1100-1106
3. Sandroni P, Benrud-Larson LM, McClelland RL, Low PA. Complex regional pain syndrome type I: incidence and prevalence in Olmsted county, a population-based study. Pain 2003;103:199-207
4. Bickerstaff DR, Kanis JA. Algodystrophy: an under-recognized complication of minor trauma. Br J Rheumatol 1994;33:240-248
5. Field J, Atkins RM. Algodystrophy is an early complication of Colles’ fracture. What are the implications? J Hand Surg [Br] 1997;22:178-182
6. Forouzanfar T, Koke AJ, van Kleef M, Weber WE. Treatment of complex regional pain syndrome type I. Eur J Pain 2002;6:105-122
7. Quisel A, Gill JM, Witherell P. Complex regional pain syndrome: which treatments show promise? J Fam Pract 2005;54:599-603
8. Zollinger PE, Tuinebreijer WE, Kreis RW, Breederveld RS. Effect of vitamin C on frequency of reflex sympathetic dystrophy in wrist fractures: a randomised trial. Lancet 1999;354:2025-2028
9. Quisel A, Gill JM, Witherell P. Complex regional pain syndrome underdiagnosed. J Fam Pract 2005;54:524-532
1. Zollinger PE, Tuinebreijer WE, Breederveld RS, Kreis RW. Can vitamin C prevent complex regional pain syndrome in patients with wrist fractures? A randomized, controlled, multicenter dose-response study. J Bone Joint Surg Am 2007;89:1424-1431
2. Atkins RM. Complex regional pain syndrome. J Bone Joint Surg Br 2003;85:1100-1106
3. Sandroni P, Benrud-Larson LM, McClelland RL, Low PA. Complex regional pain syndrome type I: incidence and prevalence in Olmsted county, a population-based study. Pain 2003;103:199-207
4. Bickerstaff DR, Kanis JA. Algodystrophy: an under-recognized complication of minor trauma. Br J Rheumatol 1994;33:240-248
5. Field J, Atkins RM. Algodystrophy is an early complication of Colles’ fracture. What are the implications? J Hand Surg [Br] 1997;22:178-182
6. Forouzanfar T, Koke AJ, van Kleef M, Weber WE. Treatment of complex regional pain syndrome type I. Eur J Pain 2002;6:105-122
7. Quisel A, Gill JM, Witherell P. Complex regional pain syndrome: which treatments show promise? J Fam Pract 2005;54:599-603
8. Zollinger PE, Tuinebreijer WE, Kreis RW, Breederveld RS. Effect of vitamin C on frequency of reflex sympathetic dystrophy in wrist fractures: a randomised trial. Lancet 1999;354:2025-2028
9. Quisel A, Gill JM, Witherell P. Complex regional pain syndrome underdiagnosed. J Fam Pract 2005;54:524-532
What are effective therapies for Clostridium difficile-associated diarrhea?
Oral metronidazole and oral vancomycin are equally effective treatments for Clostridium difficile–associated diarrhea (CDAD) (strength of recommendation [SOR]: A, based on randomized trials). Oral vancomycin is considerably more expensive and may select for colonization with vancomycin-resistant enterococci, leading the American College of Gastroenterology to recommend oral metronidazole as preferred therapy (SOR: C, expert opinion). They recommend therapy with vancomycin for those who are pregnant, breast feeding, less than 10 years old, nonresponders to metronidazole, critically ill, or allergic or intolerant to metronidazole (SOR: C, expert opinion).
Treat first recurrences the same as primary infection. In persons with recurrent infection, addition of the probiotic agent Saccharomyces boulardii. reduces the risk of further recurrences (SOR: B, single RCT). Little other evidence exists to guide therapy for subsequent recurrences.
Evidence summary
Two randomized controlled trials have compared the efficacy of oral metronidazole and oral vancomycin for treatment of CDAD.1,2 Both studies demonstrated statistically equivalent cure rates exceeding 90%, with relapse rates of 10% to 20% for each drug. These small trials lacked the power to detect small but potentially significant differences in treatment response.
No published data exist indicating that vancomycin is more effective than metronidazole in any clinical setting. A dose-range study showed that 125 mg of oral vancomycin 4 times a day is as effective as higher doses.3 Patients who cannot take medication by mouth should receive intravenous metronidazole, 500 mg 4 times per day. Unlike vancomycin, metronidazole achieves potentially effective concentrations in the intestinal lumen following intravenous administration.4
Treatment of first recurrences of infection with metronidazole or vancomycin produces response rates similar to treatment of initial infections.5 A minority of patients suffers multiple relapses of infection, and there are few data to guide therapy in this setting.
A randomized, double-blinded, placebocontrolled study evaluated the impact of adding the probiotic agent Saccharomyces boulardii. to either metronidazole or vancomycin.6 For persons with recurrent infection, addition of S boulardii. led to a 30% decrease in the absolute risk of relapse (64% relapse vs 34%; number needed to treat=3; P.<.05). There was also a nonsignificant trend toward reduced recurrences in the treatment of primary infections. The 2 minor side effects noted with this treatment were dry mouth (number needed to harm [NNH]=11) and constipation (NNH=9). S boulardii. capsules are available from health food stores and via the Internet. Several published case series describe various additional approaches to therapy of recurrent CDAD (Table).
TABLE
Medical treatment of C difficile–.associated diarrhea
| Indication | Treatment |
|---|---|
| First episode of C difficile.–associated diarrhea (SOR: A; SOR: C for preference over vancomycin) | Metronidazole, 500 mg orally 3 times daily for 10 days |
| First episode, allergy, or intolerance to metronidazole, pregnant, breast feeding, or age <10 years (SOR: A; SOR: C for preference over metronidazole) | Vancomycin, 125 mg orally 4 times daily for 10 days |
| Unable to take oral medication (SOR: C) | Metronidazole 500 mg IV 4 times daily |
| First recurrence (SOR: C) | As for first episode or Option #1 below |
| Second or greater recurrence: | |
| Option #1 (SOR: B, single RCT) | Metronidazole or vancomycin, plus S boulardii. (500 mg twice daily [3 x 1010 CFUs]) |
| Option #2 (SOR: C) | Vancomycin or metronidazole plus rifampin 300 mg oral twice daily for 10 days |
| Option #3 (SOR: C) | Vancomycin tapered dose: |
| 125 mg orally 4 times daily for 7 days | |
| 125 mg orally twice daily for 7 days | |
| 125 mg orally once daily for 7 days | |
| 125 mg orally every other day for 7 days | |
| 125 mg orally every 3 days for 14 days | |
| Option #4 (SOR: C) | Vancomycin plus cholestyramine 4 g twice daily for 10 days |
Recommendations from others
The American College of Gastroenterology and the American College of Physicians treatment guidelines for CDAD both call for treatment with oral metronidazole 250 mg 4 times daily or 500 mg 3 times daily.7,8 The American College of Gastroenterology recommends vancomycin (125 mg orally 4 times daily) when there is an intolerance or confirmed resistance to metronidazole, failure of response, when the patient is pregnant, breast feeding, or under 10 years of age, critically ill from colitis, or when the diarrhea could be related to Staphylococcus aureus.. In milder cases, treatment may involve only discontinuation of antibiotics and supportive therapy with observation. Opiates and antispasmodics should be avoided. These guidelines do not recommend any treatment over another for therapy of multiple recurrences.
Discontinue the offending antibiotic and treat the infection; prevent outbreaks via patient-to-patient transmission
Joe Tribuna, MD
Kimdary Chek, MD, MDH
Most cases of Clostridium difficile–.associated diarrhea are caused by antibiotic use; it is therefore one of the most common nosocomial infections. In addition to discontinuing use of the offending antibiotic and treating the infection, it is also important to prevent further outbreaks via patient-to-patient transmission. In our hospital, once a patient is diagnosed with C difficile., contact precautions are instituted. If the patient is incontinent, isolation in a single room is required. If the patient is continent
1. Teasley DG, Gerding DN, Olson MM, et al. Prospective randomised trial of metronidazole versus vancomycin for Clostridium-difficile-associated diarrhoea and colitis. Lancet 1983;2:1043-1046.
2. Wenisch C, Parschalk B, Hasenhundl M, Hirschl AM, Graninger W. Comparison of vancomycin, teicoplanin, metronidazole, and fusidic acid for the treatment of Clostridium difficile-associated diarrhea. Clin Infect Dis 1996;22:813-818.
3. Fekety R, Silva J, Kauffman C, Buggy B, Deery HG. Treatment of antibiotic-associated Clostridium difficile colitis with oral vancomycin: comparison of two dosage regimens. Am J Med 1989;86:15-19.
4. Bolton RP, Culshaw MA. Faecal metronidazole concentrations during oral and intravenous therapy for antibiotic associated colitis due to Clostridium difficile. Gut 1986;27:1169-1172.
5. Bartlett JG, Tedesco FJ, Shull S, Lowe B, Chang T. Symptomatic relapse after oral vancomycin therapy of antibiotic-associated pseudomembranous colitis. Gastroenterology 1980;78:431-434.
6. McFarland LV, Surawicz CM, Greenberg RN, Fekety R, Elmer GW, Moyer KA, et al. A randomized placebo-controlled trial of Saccharomyces boulardii in combination with standard antibiotics for Clostridium difficile disease. JAMA 1994;271:1913-1918.
7. Fekety R. Guidelines for the diagnosis and management of Clostridium difficile-associated diarrhea and colitis. American College of Gastroenterology, Practice Parameters Committee. Am J Gastroenterol 1997;92:739-750.
8. Hurley B.W., Nguyen C. C. Drug therapy: use of antimicrobial agents as first-line drug therapy for CDAD. PIER: Clinical Guidance from ACP, 2004. Available at: pier.acponline.org/physicians/diseases/d320/d320.html. Accessed on July 14, 2004.
Oral metronidazole and oral vancomycin are equally effective treatments for Clostridium difficile–associated diarrhea (CDAD) (strength of recommendation [SOR]: A, based on randomized trials). Oral vancomycin is considerably more expensive and may select for colonization with vancomycin-resistant enterococci, leading the American College of Gastroenterology to recommend oral metronidazole as preferred therapy (SOR: C, expert opinion). They recommend therapy with vancomycin for those who are pregnant, breast feeding, less than 10 years old, nonresponders to metronidazole, critically ill, or allergic or intolerant to metronidazole (SOR: C, expert opinion).
Treat first recurrences the same as primary infection. In persons with recurrent infection, addition of the probiotic agent Saccharomyces boulardii. reduces the risk of further recurrences (SOR: B, single RCT). Little other evidence exists to guide therapy for subsequent recurrences.
Evidence summary
Two randomized controlled trials have compared the efficacy of oral metronidazole and oral vancomycin for treatment of CDAD.1,2 Both studies demonstrated statistically equivalent cure rates exceeding 90%, with relapse rates of 10% to 20% for each drug. These small trials lacked the power to detect small but potentially significant differences in treatment response.
No published data exist indicating that vancomycin is more effective than metronidazole in any clinical setting. A dose-range study showed that 125 mg of oral vancomycin 4 times a day is as effective as higher doses.3 Patients who cannot take medication by mouth should receive intravenous metronidazole, 500 mg 4 times per day. Unlike vancomycin, metronidazole achieves potentially effective concentrations in the intestinal lumen following intravenous administration.4
Treatment of first recurrences of infection with metronidazole or vancomycin produces response rates similar to treatment of initial infections.5 A minority of patients suffers multiple relapses of infection, and there are few data to guide therapy in this setting.
A randomized, double-blinded, placebocontrolled study evaluated the impact of adding the probiotic agent Saccharomyces boulardii. to either metronidazole or vancomycin.6 For persons with recurrent infection, addition of S boulardii. led to a 30% decrease in the absolute risk of relapse (64% relapse vs 34%; number needed to treat=3; P.<.05). There was also a nonsignificant trend toward reduced recurrences in the treatment of primary infections. The 2 minor side effects noted with this treatment were dry mouth (number needed to harm [NNH]=11) and constipation (NNH=9). S boulardii. capsules are available from health food stores and via the Internet. Several published case series describe various additional approaches to therapy of recurrent CDAD (Table).
TABLE
Medical treatment of C difficile–.associated diarrhea
| Indication | Treatment |
|---|---|
| First episode of C difficile.–associated diarrhea (SOR: A; SOR: C for preference over vancomycin) | Metronidazole, 500 mg orally 3 times daily for 10 days |
| First episode, allergy, or intolerance to metronidazole, pregnant, breast feeding, or age <10 years (SOR: A; SOR: C for preference over metronidazole) | Vancomycin, 125 mg orally 4 times daily for 10 days |
| Unable to take oral medication (SOR: C) | Metronidazole 500 mg IV 4 times daily |
| First recurrence (SOR: C) | As for first episode or Option #1 below |
| Second or greater recurrence: | |
| Option #1 (SOR: B, single RCT) | Metronidazole or vancomycin, plus S boulardii. (500 mg twice daily [3 x 1010 CFUs]) |
| Option #2 (SOR: C) | Vancomycin or metronidazole plus rifampin 300 mg oral twice daily for 10 days |
| Option #3 (SOR: C) | Vancomycin tapered dose: |
| 125 mg orally 4 times daily for 7 days | |
| 125 mg orally twice daily for 7 days | |
| 125 mg orally once daily for 7 days | |
| 125 mg orally every other day for 7 days | |
| 125 mg orally every 3 days for 14 days | |
| Option #4 (SOR: C) | Vancomycin plus cholestyramine 4 g twice daily for 10 days |
Recommendations from others
The American College of Gastroenterology and the American College of Physicians treatment guidelines for CDAD both call for treatment with oral metronidazole 250 mg 4 times daily or 500 mg 3 times daily.7,8 The American College of Gastroenterology recommends vancomycin (125 mg orally 4 times daily) when there is an intolerance or confirmed resistance to metronidazole, failure of response, when the patient is pregnant, breast feeding, or under 10 years of age, critically ill from colitis, or when the diarrhea could be related to Staphylococcus aureus.. In milder cases, treatment may involve only discontinuation of antibiotics and supportive therapy with observation. Opiates and antispasmodics should be avoided. These guidelines do not recommend any treatment over another for therapy of multiple recurrences.
Discontinue the offending antibiotic and treat the infection; prevent outbreaks via patient-to-patient transmission
Joe Tribuna, MD
Kimdary Chek, MD, MDH
Most cases of Clostridium difficile–.associated diarrhea are caused by antibiotic use; it is therefore one of the most common nosocomial infections. In addition to discontinuing use of the offending antibiotic and treating the infection, it is also important to prevent further outbreaks via patient-to-patient transmission. In our hospital, once a patient is diagnosed with C difficile., contact precautions are instituted. If the patient is incontinent, isolation in a single room is required. If the patient is continent
Oral metronidazole and oral vancomycin are equally effective treatments for Clostridium difficile–associated diarrhea (CDAD) (strength of recommendation [SOR]: A, based on randomized trials). Oral vancomycin is considerably more expensive and may select for colonization with vancomycin-resistant enterococci, leading the American College of Gastroenterology to recommend oral metronidazole as preferred therapy (SOR: C, expert opinion). They recommend therapy with vancomycin for those who are pregnant, breast feeding, less than 10 years old, nonresponders to metronidazole, critically ill, or allergic or intolerant to metronidazole (SOR: C, expert opinion).
Treat first recurrences the same as primary infection. In persons with recurrent infection, addition of the probiotic agent Saccharomyces boulardii. reduces the risk of further recurrences (SOR: B, single RCT). Little other evidence exists to guide therapy for subsequent recurrences.
Evidence summary
Two randomized controlled trials have compared the efficacy of oral metronidazole and oral vancomycin for treatment of CDAD.1,2 Both studies demonstrated statistically equivalent cure rates exceeding 90%, with relapse rates of 10% to 20% for each drug. These small trials lacked the power to detect small but potentially significant differences in treatment response.
No published data exist indicating that vancomycin is more effective than metronidazole in any clinical setting. A dose-range study showed that 125 mg of oral vancomycin 4 times a day is as effective as higher doses.3 Patients who cannot take medication by mouth should receive intravenous metronidazole, 500 mg 4 times per day. Unlike vancomycin, metronidazole achieves potentially effective concentrations in the intestinal lumen following intravenous administration.4
Treatment of first recurrences of infection with metronidazole or vancomycin produces response rates similar to treatment of initial infections.5 A minority of patients suffers multiple relapses of infection, and there are few data to guide therapy in this setting.
A randomized, double-blinded, placebocontrolled study evaluated the impact of adding the probiotic agent Saccharomyces boulardii. to either metronidazole or vancomycin.6 For persons with recurrent infection, addition of S boulardii. led to a 30% decrease in the absolute risk of relapse (64% relapse vs 34%; number needed to treat=3; P.<.05). There was also a nonsignificant trend toward reduced recurrences in the treatment of primary infections. The 2 minor side effects noted with this treatment were dry mouth (number needed to harm [NNH]=11) and constipation (NNH=9). S boulardii. capsules are available from health food stores and via the Internet. Several published case series describe various additional approaches to therapy of recurrent CDAD (Table).
TABLE
Medical treatment of C difficile–.associated diarrhea
| Indication | Treatment |
|---|---|
| First episode of C difficile.–associated diarrhea (SOR: A; SOR: C for preference over vancomycin) | Metronidazole, 500 mg orally 3 times daily for 10 days |
| First episode, allergy, or intolerance to metronidazole, pregnant, breast feeding, or age <10 years (SOR: A; SOR: C for preference over metronidazole) | Vancomycin, 125 mg orally 4 times daily for 10 days |
| Unable to take oral medication (SOR: C) | Metronidazole 500 mg IV 4 times daily |
| First recurrence (SOR: C) | As for first episode or Option #1 below |
| Second or greater recurrence: | |
| Option #1 (SOR: B, single RCT) | Metronidazole or vancomycin, plus S boulardii. (500 mg twice daily [3 x 1010 CFUs]) |
| Option #2 (SOR: C) | Vancomycin or metronidazole plus rifampin 300 mg oral twice daily for 10 days |
| Option #3 (SOR: C) | Vancomycin tapered dose: |
| 125 mg orally 4 times daily for 7 days | |
| 125 mg orally twice daily for 7 days | |
| 125 mg orally once daily for 7 days | |
| 125 mg orally every other day for 7 days | |
| 125 mg orally every 3 days for 14 days | |
| Option #4 (SOR: C) | Vancomycin plus cholestyramine 4 g twice daily for 10 days |
Recommendations from others
The American College of Gastroenterology and the American College of Physicians treatment guidelines for CDAD both call for treatment with oral metronidazole 250 mg 4 times daily or 500 mg 3 times daily.7,8 The American College of Gastroenterology recommends vancomycin (125 mg orally 4 times daily) when there is an intolerance or confirmed resistance to metronidazole, failure of response, when the patient is pregnant, breast feeding, or under 10 years of age, critically ill from colitis, or when the diarrhea could be related to Staphylococcus aureus.. In milder cases, treatment may involve only discontinuation of antibiotics and supportive therapy with observation. Opiates and antispasmodics should be avoided. These guidelines do not recommend any treatment over another for therapy of multiple recurrences.
Discontinue the offending antibiotic and treat the infection; prevent outbreaks via patient-to-patient transmission
Joe Tribuna, MD
Kimdary Chek, MD, MDH
Most cases of Clostridium difficile–.associated diarrhea are caused by antibiotic use; it is therefore one of the most common nosocomial infections. In addition to discontinuing use of the offending antibiotic and treating the infection, it is also important to prevent further outbreaks via patient-to-patient transmission. In our hospital, once a patient is diagnosed with C difficile., contact precautions are instituted. If the patient is incontinent, isolation in a single room is required. If the patient is continent
1. Teasley DG, Gerding DN, Olson MM, et al. Prospective randomised trial of metronidazole versus vancomycin for Clostridium-difficile-associated diarrhoea and colitis. Lancet 1983;2:1043-1046.
2. Wenisch C, Parschalk B, Hasenhundl M, Hirschl AM, Graninger W. Comparison of vancomycin, teicoplanin, metronidazole, and fusidic acid for the treatment of Clostridium difficile-associated diarrhea. Clin Infect Dis 1996;22:813-818.
3. Fekety R, Silva J, Kauffman C, Buggy B, Deery HG. Treatment of antibiotic-associated Clostridium difficile colitis with oral vancomycin: comparison of two dosage regimens. Am J Med 1989;86:15-19.
4. Bolton RP, Culshaw MA. Faecal metronidazole concentrations during oral and intravenous therapy for antibiotic associated colitis due to Clostridium difficile. Gut 1986;27:1169-1172.
5. Bartlett JG, Tedesco FJ, Shull S, Lowe B, Chang T. Symptomatic relapse after oral vancomycin therapy of antibiotic-associated pseudomembranous colitis. Gastroenterology 1980;78:431-434.
6. McFarland LV, Surawicz CM, Greenberg RN, Fekety R, Elmer GW, Moyer KA, et al. A randomized placebo-controlled trial of Saccharomyces boulardii in combination with standard antibiotics for Clostridium difficile disease. JAMA 1994;271:1913-1918.
7. Fekety R. Guidelines for the diagnosis and management of Clostridium difficile-associated diarrhea and colitis. American College of Gastroenterology, Practice Parameters Committee. Am J Gastroenterol 1997;92:739-750.
8. Hurley B.W., Nguyen C. C. Drug therapy: use of antimicrobial agents as first-line drug therapy for CDAD. PIER: Clinical Guidance from ACP, 2004. Available at: pier.acponline.org/physicians/diseases/d320/d320.html. Accessed on July 14, 2004.
1. Teasley DG, Gerding DN, Olson MM, et al. Prospective randomised trial of metronidazole versus vancomycin for Clostridium-difficile-associated diarrhoea and colitis. Lancet 1983;2:1043-1046.
2. Wenisch C, Parschalk B, Hasenhundl M, Hirschl AM, Graninger W. Comparison of vancomycin, teicoplanin, metronidazole, and fusidic acid for the treatment of Clostridium difficile-associated diarrhea. Clin Infect Dis 1996;22:813-818.
3. Fekety R, Silva J, Kauffman C, Buggy B, Deery HG. Treatment of antibiotic-associated Clostridium difficile colitis with oral vancomycin: comparison of two dosage regimens. Am J Med 1989;86:15-19.
4. Bolton RP, Culshaw MA. Faecal metronidazole concentrations during oral and intravenous therapy for antibiotic associated colitis due to Clostridium difficile. Gut 1986;27:1169-1172.
5. Bartlett JG, Tedesco FJ, Shull S, Lowe B, Chang T. Symptomatic relapse after oral vancomycin therapy of antibiotic-associated pseudomembranous colitis. Gastroenterology 1980;78:431-434.
6. McFarland LV, Surawicz CM, Greenberg RN, Fekety R, Elmer GW, Moyer KA, et al. A randomized placebo-controlled trial of Saccharomyces boulardii in combination with standard antibiotics for Clostridium difficile disease. JAMA 1994;271:1913-1918.
7. Fekety R. Guidelines for the diagnosis and management of Clostridium difficile-associated diarrhea and colitis. American College of Gastroenterology, Practice Parameters Committee. Am J Gastroenterol 1997;92:739-750.
8. Hurley B.W., Nguyen C. C. Drug therapy: use of antimicrobial agents as first-line drug therapy for CDAD. PIER: Clinical Guidance from ACP, 2004. Available at: pier.acponline.org/physicians/diseases/d320/d320.html. Accessed on July 14, 2004.
Evidence-based answers from the Family Physicians Inquiries Network