User login
Survey: Steady Increase in Complementary Alternative Medicine (CAM) Offerings in U.S. Hospitals
According to a survey released last fall by the Health Forum, a subsidiary of the American Hospital Association, and the Samueli Institute of Alexandria, Va., complementary and alternative medicine (CAM) services in responding hospitals increased to 42% in 2010 from 37% in 2007.
The fourth Complementary and Alternative Medicine Survey of Hospitals is a follow-up report to the 2007 survey, which The Hospitalist featured in January 2010.
Twelve percent of 5,858 hospitals answered a 42-question instrument in 2010, according to Sita Ananth, MHA, director of knowledge services at the Samueli Institute and study report author. The results, Ananth says, showed that the hospitals most likely to offer CAM were urban and tended to be either medium-size (50-299 beds) or large (500+ beds) institutions.
What’s driving the increase? She believes that hospitals are simply responding to patients’ desire to have “the best that both conventional and alternative medicine can offer.”

—Sita Ananth, MHA, director of knowledge services at the Samueli Institute and study report author
Sixty-five percent of hospitals responding to the survey offer CAM therapies for pain management. That figure is echoed in a 2008 National Health Statistics report (PDF) published by the Centers for Disease Control and Prevention. Back pain, neck pain, and joint pain were the three top reasons for using CAM, according to the CDC report.
“Adjacent” Treatment
Hospitalist Sanjay Reddy, MD, assistant clinical professor of medicine in the Department of Medicine at the University of California at San Francisco (UCSF), says acupuncture can be a valuable adjunct when treating patients for pain, chemotherapy-induced nausea, and insomnia. He is a trained acupuncturist and has studied complementary therapies extensively. He also is interested in exploring ways to incorporate acupuncture into the UCSF’s Osher Center for Integrative Medicine program.
David H. Gorski, MD, PhD, FACS, associate professor of surgery and director of the Breast Cancer Multidisciplinary Team at the Barbara Ann Karmanos Cancer Institute at Wayne State University School of Medicine in Detroit, strenuously objects to the incorporation of alternative therapies (often under the moniker of “integrative medicine”) in the hospital setting.
“If you accept the premise that medicine should be based in sound science and evidence, then we have an obligation not to be offering treatments that are not based in science,” he asserts. Dr. Gorski, who also blogs on such topics, finds that many of those who endorse integrative medicine have become “true believers,” and that some are mixing pseudo-science with science.
In an August 2011 post regarding the College of Physicians and Surgeons of Ontario’s draft policy on alternative treatments, Dr. Gorski wrote: “Competent adults have every right to seek out non-science-based medicine if that is what they desire. However, informed consent mandates that physicians who encounter such patients provide an honest professional assessment of such treatments based on science.”
Dr. Reddy notes that with appropriate disclosure, offering a modality such as acupuncture can be appropriate. For example, in the setting of pain relief, acupuncture offers a less sedative approach. He explains that Chinese diagnostics and treatment approaches are slightly different, so it’s difficult to study them in the context of randomized trials. (Click here to listen to more of Dr. Reddy’s discussion of appropriate indications for acupuncture.)
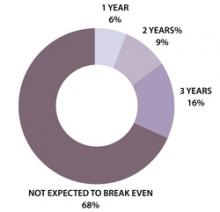
In the Health Forum/Samueli Institute survey, 57% of hospitals reported that their programs were not yet breaking even and only 16% said they'd be breaking even in three years (see Figure 1). In light of these results, Ananth says, hospitals undertaking complementary services should “start small and not have high expectations of breaking even for several years.”
Gretchen Henkel is a freelance writer in California.
Herbals another Matter
In the 2010 Health Forum/Samueli Institute survey, 82% of responding hospitals reported that they did not offer herbal supplements in their hospital pharmacies. Study author Sita Ananth surmises that most hospitals may be “playing it safe” by offering noninvasive therapies. Hospitalists are aware of the potentially dangerous interactions between herbal supplements and mainstream treatments, Dr. Reddy says.
A majority of the hospitals Ananth queried (67%) reported having existing policies regarding patients’ use of herbal and nutritional supplements during hospitalization. To avoid adverse events, “It’s really crucial that they are asking the right questions of their patients,” she says.—GH
According to a survey released last fall by the Health Forum, a subsidiary of the American Hospital Association, and the Samueli Institute of Alexandria, Va., complementary and alternative medicine (CAM) services in responding hospitals increased to 42% in 2010 from 37% in 2007.
The fourth Complementary and Alternative Medicine Survey of Hospitals is a follow-up report to the 2007 survey, which The Hospitalist featured in January 2010.
Twelve percent of 5,858 hospitals answered a 42-question instrument in 2010, according to Sita Ananth, MHA, director of knowledge services at the Samueli Institute and study report author. The results, Ananth says, showed that the hospitals most likely to offer CAM were urban and tended to be either medium-size (50-299 beds) or large (500+ beds) institutions.
What’s driving the increase? She believes that hospitals are simply responding to patients’ desire to have “the best that both conventional and alternative medicine can offer.”

—Sita Ananth, MHA, director of knowledge services at the Samueli Institute and study report author
Sixty-five percent of hospitals responding to the survey offer CAM therapies for pain management. That figure is echoed in a 2008 National Health Statistics report (PDF) published by the Centers for Disease Control and Prevention. Back pain, neck pain, and joint pain were the three top reasons for using CAM, according to the CDC report.
“Adjacent” Treatment
Hospitalist Sanjay Reddy, MD, assistant clinical professor of medicine in the Department of Medicine at the University of California at San Francisco (UCSF), says acupuncture can be a valuable adjunct when treating patients for pain, chemotherapy-induced nausea, and insomnia. He is a trained acupuncturist and has studied complementary therapies extensively. He also is interested in exploring ways to incorporate acupuncture into the UCSF’s Osher Center for Integrative Medicine program.
David H. Gorski, MD, PhD, FACS, associate professor of surgery and director of the Breast Cancer Multidisciplinary Team at the Barbara Ann Karmanos Cancer Institute at Wayne State University School of Medicine in Detroit, strenuously objects to the incorporation of alternative therapies (often under the moniker of “integrative medicine”) in the hospital setting.
“If you accept the premise that medicine should be based in sound science and evidence, then we have an obligation not to be offering treatments that are not based in science,” he asserts. Dr. Gorski, who also blogs on such topics, finds that many of those who endorse integrative medicine have become “true believers,” and that some are mixing pseudo-science with science.
In an August 2011 post regarding the College of Physicians and Surgeons of Ontario’s draft policy on alternative treatments, Dr. Gorski wrote: “Competent adults have every right to seek out non-science-based medicine if that is what they desire. However, informed consent mandates that physicians who encounter such patients provide an honest professional assessment of such treatments based on science.”
Dr. Reddy notes that with appropriate disclosure, offering a modality such as acupuncture can be appropriate. For example, in the setting of pain relief, acupuncture offers a less sedative approach. He explains that Chinese diagnostics and treatment approaches are slightly different, so it’s difficult to study them in the context of randomized trials. (Click here to listen to more of Dr. Reddy’s discussion of appropriate indications for acupuncture.)
In the Health Forum/Samueli Institute survey, 57% of hospitals reported that their programs were not yet breaking even and only 16% said they'd be breaking even in three years (see Figure 1). In light of these results, Ananth says, hospitals undertaking complementary services should “start small and not have high expectations of breaking even for several years.”
Gretchen Henkel is a freelance writer in California.
Herbals another Matter
In the 2010 Health Forum/Samueli Institute survey, 82% of responding hospitals reported that they did not offer herbal supplements in their hospital pharmacies. Study author Sita Ananth surmises that most hospitals may be “playing it safe” by offering noninvasive therapies. Hospitalists are aware of the potentially dangerous interactions between herbal supplements and mainstream treatments, Dr. Reddy says.
A majority of the hospitals Ananth queried (67%) reported having existing policies regarding patients’ use of herbal and nutritional supplements during hospitalization. To avoid adverse events, “It’s really crucial that they are asking the right questions of their patients,” she says.—GH
According to a survey released last fall by the Health Forum, a subsidiary of the American Hospital Association, and the Samueli Institute of Alexandria, Va., complementary and alternative medicine (CAM) services in responding hospitals increased to 42% in 2010 from 37% in 2007.
The fourth Complementary and Alternative Medicine Survey of Hospitals is a follow-up report to the 2007 survey, which The Hospitalist featured in January 2010.
Twelve percent of 5,858 hospitals answered a 42-question instrument in 2010, according to Sita Ananth, MHA, director of knowledge services at the Samueli Institute and study report author. The results, Ananth says, showed that the hospitals most likely to offer CAM were urban and tended to be either medium-size (50-299 beds) or large (500+ beds) institutions.
What’s driving the increase? She believes that hospitals are simply responding to patients’ desire to have “the best that both conventional and alternative medicine can offer.”

—Sita Ananth, MHA, director of knowledge services at the Samueli Institute and study report author
Sixty-five percent of hospitals responding to the survey offer CAM therapies for pain management. That figure is echoed in a 2008 National Health Statistics report (PDF) published by the Centers for Disease Control and Prevention. Back pain, neck pain, and joint pain were the three top reasons for using CAM, according to the CDC report.
“Adjacent” Treatment
Hospitalist Sanjay Reddy, MD, assistant clinical professor of medicine in the Department of Medicine at the University of California at San Francisco (UCSF), says acupuncture can be a valuable adjunct when treating patients for pain, chemotherapy-induced nausea, and insomnia. He is a trained acupuncturist and has studied complementary therapies extensively. He also is interested in exploring ways to incorporate acupuncture into the UCSF’s Osher Center for Integrative Medicine program.
David H. Gorski, MD, PhD, FACS, associate professor of surgery and director of the Breast Cancer Multidisciplinary Team at the Barbara Ann Karmanos Cancer Institute at Wayne State University School of Medicine in Detroit, strenuously objects to the incorporation of alternative therapies (often under the moniker of “integrative medicine”) in the hospital setting.
“If you accept the premise that medicine should be based in sound science and evidence, then we have an obligation not to be offering treatments that are not based in science,” he asserts. Dr. Gorski, who also blogs on such topics, finds that many of those who endorse integrative medicine have become “true believers,” and that some are mixing pseudo-science with science.
In an August 2011 post regarding the College of Physicians and Surgeons of Ontario’s draft policy on alternative treatments, Dr. Gorski wrote: “Competent adults have every right to seek out non-science-based medicine if that is what they desire. However, informed consent mandates that physicians who encounter such patients provide an honest professional assessment of such treatments based on science.”
Dr. Reddy notes that with appropriate disclosure, offering a modality such as acupuncture can be appropriate. For example, in the setting of pain relief, acupuncture offers a less sedative approach. He explains that Chinese diagnostics and treatment approaches are slightly different, so it’s difficult to study them in the context of randomized trials. (Click here to listen to more of Dr. Reddy’s discussion of appropriate indications for acupuncture.)
In the Health Forum/Samueli Institute survey, 57% of hospitals reported that their programs were not yet breaking even and only 16% said they'd be breaking even in three years (see Figure 1). In light of these results, Ananth says, hospitals undertaking complementary services should “start small and not have high expectations of breaking even for several years.”
Gretchen Henkel is a freelance writer in California.
Herbals another Matter
In the 2010 Health Forum/Samueli Institute survey, 82% of responding hospitals reported that they did not offer herbal supplements in their hospital pharmacies. Study author Sita Ananth surmises that most hospitals may be “playing it safe” by offering noninvasive therapies. Hospitalists are aware of the potentially dangerous interactions between herbal supplements and mainstream treatments, Dr. Reddy says.
A majority of the hospitals Ananth queried (67%) reported having existing policies regarding patients’ use of herbal and nutritional supplements during hospitalization. To avoid adverse events, “It’s really crucial that they are asking the right questions of their patients,” she says.—GH
ONLINE EXCLUSIVE: Patient Engagement Critical
Because “med rec” is a responsibility shared by providers, patients, and families, it’s important to engage everyone in the process.
Although the patient is—and should be, if capable—the ultimate owner of the correct healthcare record, “We have a responsibility as healthcare providers to help them be successful,” says Blake Lesselroth, MD, assistant professor of medicine at Oregon Health Sciences University and director of the Portland Patient Safety Center of Inquiry at the Portland VA Medical Center. “We haven’t done that.”
Hospitals and healthcare systems use varied strategies for including and empowering patients in the med-rec process:
- The Joint Commission launched its “Speak Up” program (PDF), which gives patients tools to help avoid mistakes with their medications.
- Last year, Southern California Kaiser Permanente rolled out its “medicine in a bag” initiative, according to hospitalist David Wong, MD. Patients are instructed to bring all of their medications (in their respective containers) to the hospital when they are admitted. Then, as the med-rec process is completed, medications are placed in green (take these meds), red (stop these meds), and yellow bags (which may include herbal supplements or other questionable items). In addition, orders are written and explained in simple language: i.e., “twice per day” instead of b.i.d. When patients visit their PCP after discharge, they are instructed to bring the color-coded bags so that the PCPs can verify the coherence of the orders. Clarity reports are filed for each physician, allowing a feedback mechanism to make sure that med rec is taking place.
- Open charting at Griffin Hospital in Derby, Conn., in affiliation with the principles of the nonprofit, patient-centered Planetree organization, supplies another means of double-checking the veracity of patients’ medication lists. It also allows for meaningful patient education and dialogue about treatment and discharge plans, says Dorothea Wild, MD, Griffin Hospital’s chief hospitalist.
Gretchen Henkel is a freelance writer based in California.
Because “med rec” is a responsibility shared by providers, patients, and families, it’s important to engage everyone in the process.
Although the patient is—and should be, if capable—the ultimate owner of the correct healthcare record, “We have a responsibility as healthcare providers to help them be successful,” says Blake Lesselroth, MD, assistant professor of medicine at Oregon Health Sciences University and director of the Portland Patient Safety Center of Inquiry at the Portland VA Medical Center. “We haven’t done that.”
Hospitals and healthcare systems use varied strategies for including and empowering patients in the med-rec process:
- The Joint Commission launched its “Speak Up” program (PDF), which gives patients tools to help avoid mistakes with their medications.
- Last year, Southern California Kaiser Permanente rolled out its “medicine in a bag” initiative, according to hospitalist David Wong, MD. Patients are instructed to bring all of their medications (in their respective containers) to the hospital when they are admitted. Then, as the med-rec process is completed, medications are placed in green (take these meds), red (stop these meds), and yellow bags (which may include herbal supplements or other questionable items). In addition, orders are written and explained in simple language: i.e., “twice per day” instead of b.i.d. When patients visit their PCP after discharge, they are instructed to bring the color-coded bags so that the PCPs can verify the coherence of the orders. Clarity reports are filed for each physician, allowing a feedback mechanism to make sure that med rec is taking place.
- Open charting at Griffin Hospital in Derby, Conn., in affiliation with the principles of the nonprofit, patient-centered Planetree organization, supplies another means of double-checking the veracity of patients’ medication lists. It also allows for meaningful patient education and dialogue about treatment and discharge plans, says Dorothea Wild, MD, Griffin Hospital’s chief hospitalist.
Gretchen Henkel is a freelance writer based in California.
Because “med rec” is a responsibility shared by providers, patients, and families, it’s important to engage everyone in the process.
Although the patient is—and should be, if capable—the ultimate owner of the correct healthcare record, “We have a responsibility as healthcare providers to help them be successful,” says Blake Lesselroth, MD, assistant professor of medicine at Oregon Health Sciences University and director of the Portland Patient Safety Center of Inquiry at the Portland VA Medical Center. “We haven’t done that.”
Hospitals and healthcare systems use varied strategies for including and empowering patients in the med-rec process:
- The Joint Commission launched its “Speak Up” program (PDF), which gives patients tools to help avoid mistakes with their medications.
- Last year, Southern California Kaiser Permanente rolled out its “medicine in a bag” initiative, according to hospitalist David Wong, MD. Patients are instructed to bring all of their medications (in their respective containers) to the hospital when they are admitted. Then, as the med-rec process is completed, medications are placed in green (take these meds), red (stop these meds), and yellow bags (which may include herbal supplements or other questionable items). In addition, orders are written and explained in simple language: i.e., “twice per day” instead of b.i.d. When patients visit their PCP after discharge, they are instructed to bring the color-coded bags so that the PCPs can verify the coherence of the orders. Clarity reports are filed for each physician, allowing a feedback mechanism to make sure that med rec is taking place.
- Open charting at Griffin Hospital in Derby, Conn., in affiliation with the principles of the nonprofit, patient-centered Planetree organization, supplies another means of double-checking the veracity of patients’ medication lists. It also allows for meaningful patient education and dialogue about treatment and discharge plans, says Dorothea Wild, MD, Griffin Hospital’s chief hospitalist.
Gretchen Henkel is a freelance writer based in California.
ONLINE EXCLUSIVE: Med-Rec Experts Discuss Prevention Strategies
Click here to listen to Dr. Tsomides
Click here to listen to Dr. Lesselroth
Click here to listen to Dr. Tsomides
Click here to listen to Dr. Lesselroth
Click here to listen to Dr. Tsomides
Click here to listen to Dr. Lesselroth
Put Medical School Debt in Perspective As You Enter Job Market
According to the Association of American Medical Colleges, the average debt for a young physician graduating from medical school in 2010 was $158,000. How do you keep that debt in perspective as you plot your career path?
Look at the Bigger Picture
Making plans for repaying medical school debt should start before your job search, says Danielle Salovich, president of the American Medical Student Association in Sterling, Va. “Part of your medical school exit interview should include campus financial advisors who give you options for loan repayment,” she says.
—Danielle Salovich, president, American Medical Student Association, Sterling, Va.
Consider what payment schedule will work best with your projected budget. Many medical students do not have financial or business backgrounds, so she advises enlisting the services of a trusted financial advisor.
Variety of Options
Recruitment packages for early-career hospitalists vary from region to region, based on an area’s appeal and marketplace pressures, says Kent McMackin, senior vice president of Physician Services for Cogent HMG in Brentwood, Tenn. Hospitals are looking to control costs in the wake of regulatory and reimbursement pressures. One alternative is to investigate loan repayment and scholarship programs.
Bonuses and Benefits
Many young physicians are especially interested in the size of signing bonuses, which can be a plus, Salovich says, if they’re planning on making a down payment on a house or taking a chunk out of their school loan principal. Joel Greenwald, MD, CFP, partner at Sterling Retirement Resources in St. Louis Park, Minn., cautions against the “lure” of a big signing bonus. More important, he says, is the total compensation and benefits package. Comprehensive disability insurance should be at the top of the list, he says, since your ability to work is your most important asset.
Another factor to consider, McMackin says, is the type of mentoring available when you start that first job.
“Physicians work so hard in medical school, where they are not taught about how to develop and understand the inter-relationships between executives in the C-suite, X-ray, dietary, and other services in the hospital,” he says. “We need to make sure that physicians have access to national networks of mentors and to best practices and information-sharing.”
Those principles—taught at Cogent HMG Academy, SHM’s Leadership Academy, and others—help build career sustainability, he says.
Above all, keep your individual goals in mind and make a decision that works best with your particular situation. “I still believe,” Salovich says, “that a medical education is a wise investment.”
Gretchen Henkel is a freelance writer based in California.
Know What You Owe
Debt management “starts with getting a handle on your loan obligations,” Dr. Greenwald says. Start with a spreadsheet listing all your lenders, principal balances, and interest rates. Then arrange those obligations in descending order, with the highest-interest balances at the top. It’s more important to chisel down the high-interest loans first (e.g. credit-card debt) and to keep paying the minimum amounts on the lower ones. In addition, some interest is tax-deductible, so it is not as toxic as a high-interest credit card balance.
Here are some resources to help:
- Loan Repayment and Scholarship Program Resources.
- The National Health Service Corps offers student loan assistance for providers serving in communities with limited access to healthcare.
- AMSA offers a variety of information and tools to help organize a student-loan payoff plan.
According to the Association of American Medical Colleges, the average debt for a young physician graduating from medical school in 2010 was $158,000. How do you keep that debt in perspective as you plot your career path?
Look at the Bigger Picture
Making plans for repaying medical school debt should start before your job search, says Danielle Salovich, president of the American Medical Student Association in Sterling, Va. “Part of your medical school exit interview should include campus financial advisors who give you options for loan repayment,” she says.
—Danielle Salovich, president, American Medical Student Association, Sterling, Va.
Consider what payment schedule will work best with your projected budget. Many medical students do not have financial or business backgrounds, so she advises enlisting the services of a trusted financial advisor.
Variety of Options
Recruitment packages for early-career hospitalists vary from region to region, based on an area’s appeal and marketplace pressures, says Kent McMackin, senior vice president of Physician Services for Cogent HMG in Brentwood, Tenn. Hospitals are looking to control costs in the wake of regulatory and reimbursement pressures. One alternative is to investigate loan repayment and scholarship programs.
Bonuses and Benefits
Many young physicians are especially interested in the size of signing bonuses, which can be a plus, Salovich says, if they’re planning on making a down payment on a house or taking a chunk out of their school loan principal. Joel Greenwald, MD, CFP, partner at Sterling Retirement Resources in St. Louis Park, Minn., cautions against the “lure” of a big signing bonus. More important, he says, is the total compensation and benefits package. Comprehensive disability insurance should be at the top of the list, he says, since your ability to work is your most important asset.
Another factor to consider, McMackin says, is the type of mentoring available when you start that first job.
“Physicians work so hard in medical school, where they are not taught about how to develop and understand the inter-relationships between executives in the C-suite, X-ray, dietary, and other services in the hospital,” he says. “We need to make sure that physicians have access to national networks of mentors and to best practices and information-sharing.”
Those principles—taught at Cogent HMG Academy, SHM’s Leadership Academy, and others—help build career sustainability, he says.
Above all, keep your individual goals in mind and make a decision that works best with your particular situation. “I still believe,” Salovich says, “that a medical education is a wise investment.”
Gretchen Henkel is a freelance writer based in California.
Know What You Owe
Debt management “starts with getting a handle on your loan obligations,” Dr. Greenwald says. Start with a spreadsheet listing all your lenders, principal balances, and interest rates. Then arrange those obligations in descending order, with the highest-interest balances at the top. It’s more important to chisel down the high-interest loans first (e.g. credit-card debt) and to keep paying the minimum amounts on the lower ones. In addition, some interest is tax-deductible, so it is not as toxic as a high-interest credit card balance.
Here are some resources to help:
- Loan Repayment and Scholarship Program Resources.
- The National Health Service Corps offers student loan assistance for providers serving in communities with limited access to healthcare.
- AMSA offers a variety of information and tools to help organize a student-loan payoff plan.
According to the Association of American Medical Colleges, the average debt for a young physician graduating from medical school in 2010 was $158,000. How do you keep that debt in perspective as you plot your career path?
Look at the Bigger Picture
Making plans for repaying medical school debt should start before your job search, says Danielle Salovich, president of the American Medical Student Association in Sterling, Va. “Part of your medical school exit interview should include campus financial advisors who give you options for loan repayment,” she says.
—Danielle Salovich, president, American Medical Student Association, Sterling, Va.
Consider what payment schedule will work best with your projected budget. Many medical students do not have financial or business backgrounds, so she advises enlisting the services of a trusted financial advisor.
Variety of Options
Recruitment packages for early-career hospitalists vary from region to region, based on an area’s appeal and marketplace pressures, says Kent McMackin, senior vice president of Physician Services for Cogent HMG in Brentwood, Tenn. Hospitals are looking to control costs in the wake of regulatory and reimbursement pressures. One alternative is to investigate loan repayment and scholarship programs.
Bonuses and Benefits
Many young physicians are especially interested in the size of signing bonuses, which can be a plus, Salovich says, if they’re planning on making a down payment on a house or taking a chunk out of their school loan principal. Joel Greenwald, MD, CFP, partner at Sterling Retirement Resources in St. Louis Park, Minn., cautions against the “lure” of a big signing bonus. More important, he says, is the total compensation and benefits package. Comprehensive disability insurance should be at the top of the list, he says, since your ability to work is your most important asset.
Another factor to consider, McMackin says, is the type of mentoring available when you start that first job.
“Physicians work so hard in medical school, where they are not taught about how to develop and understand the inter-relationships between executives in the C-suite, X-ray, dietary, and other services in the hospital,” he says. “We need to make sure that physicians have access to national networks of mentors and to best practices and information-sharing.”
Those principles—taught at Cogent HMG Academy, SHM’s Leadership Academy, and others—help build career sustainability, he says.
Above all, keep your individual goals in mind and make a decision that works best with your particular situation. “I still believe,” Salovich says, “that a medical education is a wise investment.”
Gretchen Henkel is a freelance writer based in California.
Know What You Owe
Debt management “starts with getting a handle on your loan obligations,” Dr. Greenwald says. Start with a spreadsheet listing all your lenders, principal balances, and interest rates. Then arrange those obligations in descending order, with the highest-interest balances at the top. It’s more important to chisel down the high-interest loans first (e.g. credit-card debt) and to keep paying the minimum amounts on the lower ones. In addition, some interest is tax-deductible, so it is not as toxic as a high-interest credit card balance.
Here are some resources to help:
- Loan Repayment and Scholarship Program Resources.
- The National Health Service Corps offers student loan assistance for providers serving in communities with limited access to healthcare.
- AMSA offers a variety of information and tools to help organize a student-loan payoff plan.
Reconciliation Act
Pharmacist Kristine M. Gleason, RPh, got the chance to personally test her ability to help ED providers with medication reconciliation—known by most in healthcare as “med rec”—when she broke her leg a couple of years ago. No problem, she thought: “I’ve been involved in med-rec efforts for eight-plus years.”
But when asked to provide her current medications, Gleason, who is the clinical quality leader in the department of clinical quality and analytics at Northwestern Memorial Hospital in Chicago, says she was in pain and overwhelmed. “I couldn’t even remember my children’s names, let alone the names and dosages of my aspirin and my thyroid medication,” she says. Moreover, she didn’t carry a list in her wallet because “I’m a pharmacist and I do med rec,” she says.
Gleason’s experience highlights why, six years after The Joint Commission introduced medication reconciliation as National Patient Safety Goal (NPSG) No. 8, hospitals and providers still struggle with the process.1 As a younger patient, Gleason took few medications. But for the majority of elderly inpatients with comorbid conditions, just establishing the patient’s medication list can bring the whole process to a halt; without that foundational list, reconciling other medications becomes problematic.
Although the commission has taken the goals under review and has, since July 1, required compliance with the revised NPSG 03.06.01 (see “Additional Resources,”), hospitalization-associated adverse drug events continue to mount. A recent Canadian study caused a ripple this summer with its findings that patients discharged from acute-care hospitals were at higher risk for unintentional discontinuation of their medications prescribed for chronic diseases than control groups, and those who had an ICU stay are at even higher risk.2
There’s been no shortage of med-rec initiatives in recent years. Medication reconciliation was at the top of the list for ways to prevent errors when the Institute for Healthcare Improvement launched its “5 Million Lives Campaign” in December 2006. SHM weighed in on the issue in 2010 with a consensus statement on key principles and necessary first steps in med rec.3
“This isn’t a new problem,” Gleason says. “Med rec has become more heightened because we have many more medications and complex therapies, more care providers, more specialists—more players, if you will.”
The March launch of the Hospital Readmissions Reduction Program, part of the Centers for Medicaid & Medicare Services’ (CMS) Inpatient Prospective Payment System, will again shine the spotlight on med rec’s role in the prevention of 30-day readmissions. The Hospitalist talked with researchers, pharmacists, and hospitalists about the reasons behind medication discrepancies, and their strategies for addressing mismatches.
Why So Difficult?
The goal of medication reconciliation is to generate and maintain an accurate and coherent record of patients’ medications across all transitions of care, which sounds straightforward enough. But the process involves much more than just checking items off a list, says Jeffrey Schnipper, MD, MPH, FHM, currently the principal investigator for the $1.5 million study funded by the Agency for Healthcare Research and Quality (AHRQ) to research and implement best practices in med rec, dubbed MARQUIS (Multicenter Medication Reconciliation Quality Improvement Study). Those immersed in med rec know that it’s nonlinear, multilayered, and surprisingly complex, requiring partnerships among diverse providers across many domains of care.
“Medication reconciliation gets right at all the weaknesses of our healthcare system,” says Dr. Schnipper, a hospitalist and director of clinical research for the HM service at Brigham and Women’s Hospital (BWH) and assistant professor of medicine at Harvard Medical School, both in Boston. “We have an excellent healthcare system in so many ways, but what we do not do such a good job of is coordination of care across settings, easy transfer of information, and having one person who is responsible for the accuracy of a patient’s health information.”
Dr. Schnipper’s studies attest to the common occurrence of unintentional medical discrepancies, pointing to the need for accurate medication histories, identifying high-risk patients for intensive interventions, and careful med rec at time of discharge.4
Other factors might come into play, says Ted Tsomides, MD, PhD, an attending physician on the HM service at WakeMed Hospital and assistant professor of medicine at the University of North Carolina’s School of Medicine in Raleigh, N.C. For example, he surmises that a “fatigue factor” sets in for some providers. “After five years of working on any initiative, people get worn out and push it to the back burner, unless they are really incentivized to stay on it,” he says.
List Capture
Medication reconciliation is a multifaceted process, and the first step is to gather the history of medications the patient has been taking. Hospitalist Blake J. Lesselroth, MD, MBI, assistant professor of medicine and medical informatics and director of the Portland Patient Safety Center of Inquiry at the Portland VA Medical Center in Oregon, points out that “the initial exposure to the patient is like a pencil sketch. You start to realize that med rec involves iterative loops of communication between you, the patient, and other knowledge resources (see Figure 1). As you start to pull in more information, you begin to complete your narrative. At the end of hospitalization, you’ve got a vibrant portrait with much more nuance to it. So it can’t be a linear process.”
—Kristine M. Gleason, RPh, clinical quality leader, department of clinical quality and analytics, Northwestern Memorial Hospital, Chicago
The list is dynamic, especially in the ICU setting, says Gleason, where it represents only one point in time.
In a closed system, such as the Veterans Administration or Kaiser Permanente, it’s often easier to establish a patient’s ongoing medications. With an integrated electronic health record (EHR), providers can call up the patient’s list of medications during admittance to the hospital. Verifying those medications remains critical: The health record lists patients’ prescriptions, but that doesn’t always mean they have actually filled or are taking those medications.
At the Kaiser Permanente Southern California site in Santa Clarita, Calif., where hospitalist David W. Wong, MD, works, pharmacists review their medications with patients when they are admitted, provide any needed consultation, then repeat the process at discharge. “So far,” Dr. Wong says, “this has resulted in the best medication reconciliation that we’ve seen.”
Pharmacy Is Key
In 2006, Kenneth Boockvar, MD, of the James J. Peters VA Medical Center in Bronx, N.Y., found in a pre- and post-intervention study that using pharmacists to ferret out and communicate prescribing discrepancies to physicians resulted in lower risk of adverse drug events (ADEs) for patients transferred between the hospital and the nursing home.5 Likewise, Dr. Schnipper and his colleagues found that using pharmacists to conduct medication reviews, counsel patients at discharge, and make follow-up telephone calls to patients was associated with a lower rate of preventable ADEs 30 days after hospital discharge.6
At United Hospital System’s (UHS) Kenosha Medical Center campus in Kenosha, Wis., pharmacists play a key role in generating medication lists for incoming patients. Hospitalist Corey Black, MD, regional medical director for Cogent HMG, says many patients do not recall their medications or the dosages, so UHS utilizes a team approach: If patients come in during evenings or weekends, pharmacists start calling local pharmacies to track down patients’ medication lists. “We also try to have family members bring in any medication containers they can find,” he adds. Due to a Wisconsin state law mandating nursing homes to send medication lists along with patients, generating a list is much easier.
Dr. Tsomides is a physician sponsor of a new med-rec initiative at WakeMed. With a steering committee that includes representatives from stakeholder services (medicine, nursing, pharmacy, administration, etc.), the group plans to hire and train pharmacy techs who will take home medication lists in the ED, lifting that responsibility from physicians’ task lists.
Is IT the Answer?
Would many of the barriers to med rec go away with universal EHR? So far, the literature has not borne out the superiority of using EHR to facilitate better med rec.
Peter Kaboli and colleagues found that the computerized medication record reflected what patients were actually taking for only 5.3% of the 493 VA patients enrolled in a study at the Iowa City VA.7 Kenneth Boockvar and colleagues at the Bronx VA found no difference in the overall incidence of ADEs caused by medication discrepancies between VA patients with an EHR and non-VA patients without an EHR.8 A group of researchers with Partners HealthCare in Boston evaluated a secure, Web-based patient portal to produce more accurate medication lists. The patients using this system had just as many discrepancies between medication lists and self-reporting as those who did not.9
Dr. Lesselroth, who has devised a patient kiosk touch-screen tool for reconciling patients’ medication lists and has faced barriers when implementing said technology, says med rec is much more “organic” than strictly mechanical. “It invokes theories of learning from the cognitive sciences,” he says. “We haven’t actually built tools that help people with their problem representation, with understanding not just how medications reconcile with the prior setting of care, but whether they make clinical sense within the new context of care. That requires a quantum leap in thinking.”
Re-Brand the Message
Drs. Schnipper and Tsomides believe that when The Joint Committee first coined the term “medication reconciliation” and advanced it as a mandate, most providers associated it with a regulatory requirement, and understandably so. Dr. Schnipper says med rec could be improved if providers think about it in the context of accurate orders that translate to greater patient safety. “After all,” he says, “hospitalists are ultimately responsible for the medication orders written for their patients.
“This is not about regulatory requirements,” he continues. “This is about medication safety and transitions of care. You can spend an hour on deciding what dose of Lasix you want to send this patient home on, but if the patient then takes the wrong dose of Lasix because they don’t know what they were supposed to be taking, then all that good medical care is undone.”
The med rec conversation has come full circle, then, as being truly an issue of delivering patient-centered care. (For more on this topic, visit the-hospitalist.org to read “Patient Engagement Critical.”) Rather than focusing on the sometimes-befuddling term of medication reconciliation, providers should see med rec as part of an integrated medication management process that aims to take better care of patients through prevention and treatment, Gleason says.
The med rec issue is about effective communication at every transition of care. And that’s why, says Dr. Schnipper, “Hospitalists should own this process. We don’t have to do the process entirely by ourselves—and shouldn’t. But we are responsible for errors that happen during transitions in care and we should own these initiatives.”
He notes that all six hospitals enrolled in the MARQUIS study have hospitalists at the forefront of their quality-improvement (QI) efforts.
“Medication reconciliation is potentially a high-risk process, and there are no silver bullets” for globally addressing the process, says Dorothea Wild, MD, chief hospitalist at Griffin Hospital, a 160-bed acute care hospital in Derby, Conn.
—Jeffrey Schnipper, MD, MPH, FHM, hospitalist and director of clinical research, Brigham and Women’s Hospital Hospitalist Service, assistant professor of medicine, Harvard Medical School, Boston
Dr. Wild draws a parallel between med rec and blood transfusions. Just as with correct transfusing procedures, “we envision a process where at least two people independently verify what patients’ medications are,” she says. The meds list is started in the ED by nursing staff, is verified by the ED attending, verified again by the admitting team, and triple-checked by the admitting attending. Thus, says Dr. Wild, med rec becomes a shared responsibility.
Dr. Lesselroth wholeheartedly agrees with the approach.
“This is everybody’s job,” he says. “In a larger world view, med rec is all about trying to find a medication regimen that harmonizes with what the patient can do, that improves their probability of adherence, and that also helps us gather information when the patient returns and we re-embrace them in the care model. Theoretically, then, everybody [interfacing with a patient] becomes a clutch player.”
Gretchen Henkel is a freelance writer in California.
References
- Joint Commission on Accreditation of Healthcare Organizations. 2005 Hospital Accreditation Standards. JCO website. Available at: http://www.jointcommissioninternational.org/ JCI-Accredited-Organizations/. Accessed Dec. 7, 2011.
- Bell CM, Brener SS, Gunraj N, et al. Association of ICU or hospital admission with unintentional discontinuation of medications for chronic diseases. JAMA. 2011;306:840-847.
- Greenwald JL, Halasyamani L, Green J, et al. Making inpatient medication patient centered, clinically relevant and implementable: a consensus statement on key principles and necessary first steps. J Hosp Med. 2010;5:477-485.
- Pippins JR, Gandhi TK, Hamann C, et al. Classifying and predicting errors of inpatient medication reconciliation. J Gen Intern Med. 2008;23:1414-1422.
- Boockvar KS, Carlson HL, Giambanco V, et al. Medication reconciliation for reducing drug-discrepancy adverse events. Am J Geriatr Pharmacother. 2006;4:236-243.
- Schnipper JL, Kirwin JL, Cotugno MC, et al. Role of pharmacist counseling in preventing adverse drug events after hospitalization. Arch Intern Med. 2006;166:565-571.
- Kaboli PJ, McClimon JB, Hoth AB, et al. Assessing the accuracy of computerized medication histories. Am J Manag Care. 2004;10(11 Pt 2):872-877.
- Boockvar KS, Livote EE, Goldstein N, et al. Electronic health records and adverse drug events after patient transfer. Qual Saf Health Care. 2010;5:Epub(Aug 19).
- Staroselsky M, Volk LA, Tsurikova R, et al. An effort to improve electronic health record medication list accuracy between visits: patients’ and physicians’ responses. Int J Med Inform. 2008;77:153-160.
- Gleason KM, McDaniel MR, Feinglass J, et al. Results of the Medications at Transitions and Clinical Handoffs (MATCH) study: an analysis of medication reconciliation errors and risk factors at hospital admission. J Gen Intern Med. 2010;25:441-447.
Pharmacist Kristine M. Gleason, RPh, got the chance to personally test her ability to help ED providers with medication reconciliation—known by most in healthcare as “med rec”—when she broke her leg a couple of years ago. No problem, she thought: “I’ve been involved in med-rec efforts for eight-plus years.”
But when asked to provide her current medications, Gleason, who is the clinical quality leader in the department of clinical quality and analytics at Northwestern Memorial Hospital in Chicago, says she was in pain and overwhelmed. “I couldn’t even remember my children’s names, let alone the names and dosages of my aspirin and my thyroid medication,” she says. Moreover, she didn’t carry a list in her wallet because “I’m a pharmacist and I do med rec,” she says.
Gleason’s experience highlights why, six years after The Joint Commission introduced medication reconciliation as National Patient Safety Goal (NPSG) No. 8, hospitals and providers still struggle with the process.1 As a younger patient, Gleason took few medications. But for the majority of elderly inpatients with comorbid conditions, just establishing the patient’s medication list can bring the whole process to a halt; without that foundational list, reconciling other medications becomes problematic.
Although the commission has taken the goals under review and has, since July 1, required compliance with the revised NPSG 03.06.01 (see “Additional Resources,”), hospitalization-associated adverse drug events continue to mount. A recent Canadian study caused a ripple this summer with its findings that patients discharged from acute-care hospitals were at higher risk for unintentional discontinuation of their medications prescribed for chronic diseases than control groups, and those who had an ICU stay are at even higher risk.2
There’s been no shortage of med-rec initiatives in recent years. Medication reconciliation was at the top of the list for ways to prevent errors when the Institute for Healthcare Improvement launched its “5 Million Lives Campaign” in December 2006. SHM weighed in on the issue in 2010 with a consensus statement on key principles and necessary first steps in med rec.3
“This isn’t a new problem,” Gleason says. “Med rec has become more heightened because we have many more medications and complex therapies, more care providers, more specialists—more players, if you will.”
The March launch of the Hospital Readmissions Reduction Program, part of the Centers for Medicaid & Medicare Services’ (CMS) Inpatient Prospective Payment System, will again shine the spotlight on med rec’s role in the prevention of 30-day readmissions. The Hospitalist talked with researchers, pharmacists, and hospitalists about the reasons behind medication discrepancies, and their strategies for addressing mismatches.
Why So Difficult?
The goal of medication reconciliation is to generate and maintain an accurate and coherent record of patients’ medications across all transitions of care, which sounds straightforward enough. But the process involves much more than just checking items off a list, says Jeffrey Schnipper, MD, MPH, FHM, currently the principal investigator for the $1.5 million study funded by the Agency for Healthcare Research and Quality (AHRQ) to research and implement best practices in med rec, dubbed MARQUIS (Multicenter Medication Reconciliation Quality Improvement Study). Those immersed in med rec know that it’s nonlinear, multilayered, and surprisingly complex, requiring partnerships among diverse providers across many domains of care.
“Medication reconciliation gets right at all the weaknesses of our healthcare system,” says Dr. Schnipper, a hospitalist and director of clinical research for the HM service at Brigham and Women’s Hospital (BWH) and assistant professor of medicine at Harvard Medical School, both in Boston. “We have an excellent healthcare system in so many ways, but what we do not do such a good job of is coordination of care across settings, easy transfer of information, and having one person who is responsible for the accuracy of a patient’s health information.”
Dr. Schnipper’s studies attest to the common occurrence of unintentional medical discrepancies, pointing to the need for accurate medication histories, identifying high-risk patients for intensive interventions, and careful med rec at time of discharge.4
Other factors might come into play, says Ted Tsomides, MD, PhD, an attending physician on the HM service at WakeMed Hospital and assistant professor of medicine at the University of North Carolina’s School of Medicine in Raleigh, N.C. For example, he surmises that a “fatigue factor” sets in for some providers. “After five years of working on any initiative, people get worn out and push it to the back burner, unless they are really incentivized to stay on it,” he says.
List Capture
Medication reconciliation is a multifaceted process, and the first step is to gather the history of medications the patient has been taking. Hospitalist Blake J. Lesselroth, MD, MBI, assistant professor of medicine and medical informatics and director of the Portland Patient Safety Center of Inquiry at the Portland VA Medical Center in Oregon, points out that “the initial exposure to the patient is like a pencil sketch. You start to realize that med rec involves iterative loops of communication between you, the patient, and other knowledge resources (see Figure 1). As you start to pull in more information, you begin to complete your narrative. At the end of hospitalization, you’ve got a vibrant portrait with much more nuance to it. So it can’t be a linear process.”
—Kristine M. Gleason, RPh, clinical quality leader, department of clinical quality and analytics, Northwestern Memorial Hospital, Chicago
The list is dynamic, especially in the ICU setting, says Gleason, where it represents only one point in time.
In a closed system, such as the Veterans Administration or Kaiser Permanente, it’s often easier to establish a patient’s ongoing medications. With an integrated electronic health record (EHR), providers can call up the patient’s list of medications during admittance to the hospital. Verifying those medications remains critical: The health record lists patients’ prescriptions, but that doesn’t always mean they have actually filled or are taking those medications.
At the Kaiser Permanente Southern California site in Santa Clarita, Calif., where hospitalist David W. Wong, MD, works, pharmacists review their medications with patients when they are admitted, provide any needed consultation, then repeat the process at discharge. “So far,” Dr. Wong says, “this has resulted in the best medication reconciliation that we’ve seen.”
Pharmacy Is Key
In 2006, Kenneth Boockvar, MD, of the James J. Peters VA Medical Center in Bronx, N.Y., found in a pre- and post-intervention study that using pharmacists to ferret out and communicate prescribing discrepancies to physicians resulted in lower risk of adverse drug events (ADEs) for patients transferred between the hospital and the nursing home.5 Likewise, Dr. Schnipper and his colleagues found that using pharmacists to conduct medication reviews, counsel patients at discharge, and make follow-up telephone calls to patients was associated with a lower rate of preventable ADEs 30 days after hospital discharge.6
At United Hospital System’s (UHS) Kenosha Medical Center campus in Kenosha, Wis., pharmacists play a key role in generating medication lists for incoming patients. Hospitalist Corey Black, MD, regional medical director for Cogent HMG, says many patients do not recall their medications or the dosages, so UHS utilizes a team approach: If patients come in during evenings or weekends, pharmacists start calling local pharmacies to track down patients’ medication lists. “We also try to have family members bring in any medication containers they can find,” he adds. Due to a Wisconsin state law mandating nursing homes to send medication lists along with patients, generating a list is much easier.
Dr. Tsomides is a physician sponsor of a new med-rec initiative at WakeMed. With a steering committee that includes representatives from stakeholder services (medicine, nursing, pharmacy, administration, etc.), the group plans to hire and train pharmacy techs who will take home medication lists in the ED, lifting that responsibility from physicians’ task lists.
Is IT the Answer?
Would many of the barriers to med rec go away with universal EHR? So far, the literature has not borne out the superiority of using EHR to facilitate better med rec.
Peter Kaboli and colleagues found that the computerized medication record reflected what patients were actually taking for only 5.3% of the 493 VA patients enrolled in a study at the Iowa City VA.7 Kenneth Boockvar and colleagues at the Bronx VA found no difference in the overall incidence of ADEs caused by medication discrepancies between VA patients with an EHR and non-VA patients without an EHR.8 A group of researchers with Partners HealthCare in Boston evaluated a secure, Web-based patient portal to produce more accurate medication lists. The patients using this system had just as many discrepancies between medication lists and self-reporting as those who did not.9
Dr. Lesselroth, who has devised a patient kiosk touch-screen tool for reconciling patients’ medication lists and has faced barriers when implementing said technology, says med rec is much more “organic” than strictly mechanical. “It invokes theories of learning from the cognitive sciences,” he says. “We haven’t actually built tools that help people with their problem representation, with understanding not just how medications reconcile with the prior setting of care, but whether they make clinical sense within the new context of care. That requires a quantum leap in thinking.”
Re-Brand the Message
Drs. Schnipper and Tsomides believe that when The Joint Committee first coined the term “medication reconciliation” and advanced it as a mandate, most providers associated it with a regulatory requirement, and understandably so. Dr. Schnipper says med rec could be improved if providers think about it in the context of accurate orders that translate to greater patient safety. “After all,” he says, “hospitalists are ultimately responsible for the medication orders written for their patients.
“This is not about regulatory requirements,” he continues. “This is about medication safety and transitions of care. You can spend an hour on deciding what dose of Lasix you want to send this patient home on, but if the patient then takes the wrong dose of Lasix because they don’t know what they were supposed to be taking, then all that good medical care is undone.”
The med rec conversation has come full circle, then, as being truly an issue of delivering patient-centered care. (For more on this topic, visit the-hospitalist.org to read “Patient Engagement Critical.”) Rather than focusing on the sometimes-befuddling term of medication reconciliation, providers should see med rec as part of an integrated medication management process that aims to take better care of patients through prevention and treatment, Gleason says.
The med rec issue is about effective communication at every transition of care. And that’s why, says Dr. Schnipper, “Hospitalists should own this process. We don’t have to do the process entirely by ourselves—and shouldn’t. But we are responsible for errors that happen during transitions in care and we should own these initiatives.”
He notes that all six hospitals enrolled in the MARQUIS study have hospitalists at the forefront of their quality-improvement (QI) efforts.
“Medication reconciliation is potentially a high-risk process, and there are no silver bullets” for globally addressing the process, says Dorothea Wild, MD, chief hospitalist at Griffin Hospital, a 160-bed acute care hospital in Derby, Conn.
—Jeffrey Schnipper, MD, MPH, FHM, hospitalist and director of clinical research, Brigham and Women’s Hospital Hospitalist Service, assistant professor of medicine, Harvard Medical School, Boston
Dr. Wild draws a parallel between med rec and blood transfusions. Just as with correct transfusing procedures, “we envision a process where at least two people independently verify what patients’ medications are,” she says. The meds list is started in the ED by nursing staff, is verified by the ED attending, verified again by the admitting team, and triple-checked by the admitting attending. Thus, says Dr. Wild, med rec becomes a shared responsibility.
Dr. Lesselroth wholeheartedly agrees with the approach.
“This is everybody’s job,” he says. “In a larger world view, med rec is all about trying to find a medication regimen that harmonizes with what the patient can do, that improves their probability of adherence, and that also helps us gather information when the patient returns and we re-embrace them in the care model. Theoretically, then, everybody [interfacing with a patient] becomes a clutch player.”
Gretchen Henkel is a freelance writer in California.
References
- Joint Commission on Accreditation of Healthcare Organizations. 2005 Hospital Accreditation Standards. JCO website. Available at: http://www.jointcommissioninternational.org/ JCI-Accredited-Organizations/. Accessed Dec. 7, 2011.
- Bell CM, Brener SS, Gunraj N, et al. Association of ICU or hospital admission with unintentional discontinuation of medications for chronic diseases. JAMA. 2011;306:840-847.
- Greenwald JL, Halasyamani L, Green J, et al. Making inpatient medication patient centered, clinically relevant and implementable: a consensus statement on key principles and necessary first steps. J Hosp Med. 2010;5:477-485.
- Pippins JR, Gandhi TK, Hamann C, et al. Classifying and predicting errors of inpatient medication reconciliation. J Gen Intern Med. 2008;23:1414-1422.
- Boockvar KS, Carlson HL, Giambanco V, et al. Medication reconciliation for reducing drug-discrepancy adverse events. Am J Geriatr Pharmacother. 2006;4:236-243.
- Schnipper JL, Kirwin JL, Cotugno MC, et al. Role of pharmacist counseling in preventing adverse drug events after hospitalization. Arch Intern Med. 2006;166:565-571.
- Kaboli PJ, McClimon JB, Hoth AB, et al. Assessing the accuracy of computerized medication histories. Am J Manag Care. 2004;10(11 Pt 2):872-877.
- Boockvar KS, Livote EE, Goldstein N, et al. Electronic health records and adverse drug events after patient transfer. Qual Saf Health Care. 2010;5:Epub(Aug 19).
- Staroselsky M, Volk LA, Tsurikova R, et al. An effort to improve electronic health record medication list accuracy between visits: patients’ and physicians’ responses. Int J Med Inform. 2008;77:153-160.
- Gleason KM, McDaniel MR, Feinglass J, et al. Results of the Medications at Transitions and Clinical Handoffs (MATCH) study: an analysis of medication reconciliation errors and risk factors at hospital admission. J Gen Intern Med. 2010;25:441-447.
Pharmacist Kristine M. Gleason, RPh, got the chance to personally test her ability to help ED providers with medication reconciliation—known by most in healthcare as “med rec”—when she broke her leg a couple of years ago. No problem, she thought: “I’ve been involved in med-rec efforts for eight-plus years.”
But when asked to provide her current medications, Gleason, who is the clinical quality leader in the department of clinical quality and analytics at Northwestern Memorial Hospital in Chicago, says she was in pain and overwhelmed. “I couldn’t even remember my children’s names, let alone the names and dosages of my aspirin and my thyroid medication,” she says. Moreover, she didn’t carry a list in her wallet because “I’m a pharmacist and I do med rec,” she says.
Gleason’s experience highlights why, six years after The Joint Commission introduced medication reconciliation as National Patient Safety Goal (NPSG) No. 8, hospitals and providers still struggle with the process.1 As a younger patient, Gleason took few medications. But for the majority of elderly inpatients with comorbid conditions, just establishing the patient’s medication list can bring the whole process to a halt; without that foundational list, reconciling other medications becomes problematic.
Although the commission has taken the goals under review and has, since July 1, required compliance with the revised NPSG 03.06.01 (see “Additional Resources,”), hospitalization-associated adverse drug events continue to mount. A recent Canadian study caused a ripple this summer with its findings that patients discharged from acute-care hospitals were at higher risk for unintentional discontinuation of their medications prescribed for chronic diseases than control groups, and those who had an ICU stay are at even higher risk.2
There’s been no shortage of med-rec initiatives in recent years. Medication reconciliation was at the top of the list for ways to prevent errors when the Institute for Healthcare Improvement launched its “5 Million Lives Campaign” in December 2006. SHM weighed in on the issue in 2010 with a consensus statement on key principles and necessary first steps in med rec.3
“This isn’t a new problem,” Gleason says. “Med rec has become more heightened because we have many more medications and complex therapies, more care providers, more specialists—more players, if you will.”
The March launch of the Hospital Readmissions Reduction Program, part of the Centers for Medicaid & Medicare Services’ (CMS) Inpatient Prospective Payment System, will again shine the spotlight on med rec’s role in the prevention of 30-day readmissions. The Hospitalist talked with researchers, pharmacists, and hospitalists about the reasons behind medication discrepancies, and their strategies for addressing mismatches.
Why So Difficult?
The goal of medication reconciliation is to generate and maintain an accurate and coherent record of patients’ medications across all transitions of care, which sounds straightforward enough. But the process involves much more than just checking items off a list, says Jeffrey Schnipper, MD, MPH, FHM, currently the principal investigator for the $1.5 million study funded by the Agency for Healthcare Research and Quality (AHRQ) to research and implement best practices in med rec, dubbed MARQUIS (Multicenter Medication Reconciliation Quality Improvement Study). Those immersed in med rec know that it’s nonlinear, multilayered, and surprisingly complex, requiring partnerships among diverse providers across many domains of care.
“Medication reconciliation gets right at all the weaknesses of our healthcare system,” says Dr. Schnipper, a hospitalist and director of clinical research for the HM service at Brigham and Women’s Hospital (BWH) and assistant professor of medicine at Harvard Medical School, both in Boston. “We have an excellent healthcare system in so many ways, but what we do not do such a good job of is coordination of care across settings, easy transfer of information, and having one person who is responsible for the accuracy of a patient’s health information.”
Dr. Schnipper’s studies attest to the common occurrence of unintentional medical discrepancies, pointing to the need for accurate medication histories, identifying high-risk patients for intensive interventions, and careful med rec at time of discharge.4
Other factors might come into play, says Ted Tsomides, MD, PhD, an attending physician on the HM service at WakeMed Hospital and assistant professor of medicine at the University of North Carolina’s School of Medicine in Raleigh, N.C. For example, he surmises that a “fatigue factor” sets in for some providers. “After five years of working on any initiative, people get worn out and push it to the back burner, unless they are really incentivized to stay on it,” he says.
List Capture
Medication reconciliation is a multifaceted process, and the first step is to gather the history of medications the patient has been taking. Hospitalist Blake J. Lesselroth, MD, MBI, assistant professor of medicine and medical informatics and director of the Portland Patient Safety Center of Inquiry at the Portland VA Medical Center in Oregon, points out that “the initial exposure to the patient is like a pencil sketch. You start to realize that med rec involves iterative loops of communication between you, the patient, and other knowledge resources (see Figure 1). As you start to pull in more information, you begin to complete your narrative. At the end of hospitalization, you’ve got a vibrant portrait with much more nuance to it. So it can’t be a linear process.”
—Kristine M. Gleason, RPh, clinical quality leader, department of clinical quality and analytics, Northwestern Memorial Hospital, Chicago
The list is dynamic, especially in the ICU setting, says Gleason, where it represents only one point in time.
In a closed system, such as the Veterans Administration or Kaiser Permanente, it’s often easier to establish a patient’s ongoing medications. With an integrated electronic health record (EHR), providers can call up the patient’s list of medications during admittance to the hospital. Verifying those medications remains critical: The health record lists patients’ prescriptions, but that doesn’t always mean they have actually filled or are taking those medications.
At the Kaiser Permanente Southern California site in Santa Clarita, Calif., where hospitalist David W. Wong, MD, works, pharmacists review their medications with patients when they are admitted, provide any needed consultation, then repeat the process at discharge. “So far,” Dr. Wong says, “this has resulted in the best medication reconciliation that we’ve seen.”
Pharmacy Is Key
In 2006, Kenneth Boockvar, MD, of the James J. Peters VA Medical Center in Bronx, N.Y., found in a pre- and post-intervention study that using pharmacists to ferret out and communicate prescribing discrepancies to physicians resulted in lower risk of adverse drug events (ADEs) for patients transferred between the hospital and the nursing home.5 Likewise, Dr. Schnipper and his colleagues found that using pharmacists to conduct medication reviews, counsel patients at discharge, and make follow-up telephone calls to patients was associated with a lower rate of preventable ADEs 30 days after hospital discharge.6
At United Hospital System’s (UHS) Kenosha Medical Center campus in Kenosha, Wis., pharmacists play a key role in generating medication lists for incoming patients. Hospitalist Corey Black, MD, regional medical director for Cogent HMG, says many patients do not recall their medications or the dosages, so UHS utilizes a team approach: If patients come in during evenings or weekends, pharmacists start calling local pharmacies to track down patients’ medication lists. “We also try to have family members bring in any medication containers they can find,” he adds. Due to a Wisconsin state law mandating nursing homes to send medication lists along with patients, generating a list is much easier.
Dr. Tsomides is a physician sponsor of a new med-rec initiative at WakeMed. With a steering committee that includes representatives from stakeholder services (medicine, nursing, pharmacy, administration, etc.), the group plans to hire and train pharmacy techs who will take home medication lists in the ED, lifting that responsibility from physicians’ task lists.
Is IT the Answer?
Would many of the barriers to med rec go away with universal EHR? So far, the literature has not borne out the superiority of using EHR to facilitate better med rec.
Peter Kaboli and colleagues found that the computerized medication record reflected what patients were actually taking for only 5.3% of the 493 VA patients enrolled in a study at the Iowa City VA.7 Kenneth Boockvar and colleagues at the Bronx VA found no difference in the overall incidence of ADEs caused by medication discrepancies between VA patients with an EHR and non-VA patients without an EHR.8 A group of researchers with Partners HealthCare in Boston evaluated a secure, Web-based patient portal to produce more accurate medication lists. The patients using this system had just as many discrepancies between medication lists and self-reporting as those who did not.9
Dr. Lesselroth, who has devised a patient kiosk touch-screen tool for reconciling patients’ medication lists and has faced barriers when implementing said technology, says med rec is much more “organic” than strictly mechanical. “It invokes theories of learning from the cognitive sciences,” he says. “We haven’t actually built tools that help people with their problem representation, with understanding not just how medications reconcile with the prior setting of care, but whether they make clinical sense within the new context of care. That requires a quantum leap in thinking.”
Re-Brand the Message
Drs. Schnipper and Tsomides believe that when The Joint Committee first coined the term “medication reconciliation” and advanced it as a mandate, most providers associated it with a regulatory requirement, and understandably so. Dr. Schnipper says med rec could be improved if providers think about it in the context of accurate orders that translate to greater patient safety. “After all,” he says, “hospitalists are ultimately responsible for the medication orders written for their patients.
“This is not about regulatory requirements,” he continues. “This is about medication safety and transitions of care. You can spend an hour on deciding what dose of Lasix you want to send this patient home on, but if the patient then takes the wrong dose of Lasix because they don’t know what they were supposed to be taking, then all that good medical care is undone.”
The med rec conversation has come full circle, then, as being truly an issue of delivering patient-centered care. (For more on this topic, visit the-hospitalist.org to read “Patient Engagement Critical.”) Rather than focusing on the sometimes-befuddling term of medication reconciliation, providers should see med rec as part of an integrated medication management process that aims to take better care of patients through prevention and treatment, Gleason says.
The med rec issue is about effective communication at every transition of care. And that’s why, says Dr. Schnipper, “Hospitalists should own this process. We don’t have to do the process entirely by ourselves—and shouldn’t. But we are responsible for errors that happen during transitions in care and we should own these initiatives.”
He notes that all six hospitals enrolled in the MARQUIS study have hospitalists at the forefront of their quality-improvement (QI) efforts.
“Medication reconciliation is potentially a high-risk process, and there are no silver bullets” for globally addressing the process, says Dorothea Wild, MD, chief hospitalist at Griffin Hospital, a 160-bed acute care hospital in Derby, Conn.
—Jeffrey Schnipper, MD, MPH, FHM, hospitalist and director of clinical research, Brigham and Women’s Hospital Hospitalist Service, assistant professor of medicine, Harvard Medical School, Boston
Dr. Wild draws a parallel between med rec and blood transfusions. Just as with correct transfusing procedures, “we envision a process where at least two people independently verify what patients’ medications are,” she says. The meds list is started in the ED by nursing staff, is verified by the ED attending, verified again by the admitting team, and triple-checked by the admitting attending. Thus, says Dr. Wild, med rec becomes a shared responsibility.
Dr. Lesselroth wholeheartedly agrees with the approach.
“This is everybody’s job,” he says. “In a larger world view, med rec is all about trying to find a medication regimen that harmonizes with what the patient can do, that improves their probability of adherence, and that also helps us gather information when the patient returns and we re-embrace them in the care model. Theoretically, then, everybody [interfacing with a patient] becomes a clutch player.”
Gretchen Henkel is a freelance writer in California.
References
- Joint Commission on Accreditation of Healthcare Organizations. 2005 Hospital Accreditation Standards. JCO website. Available at: http://www.jointcommissioninternational.org/ JCI-Accredited-Organizations/. Accessed Dec. 7, 2011.
- Bell CM, Brener SS, Gunraj N, et al. Association of ICU or hospital admission with unintentional discontinuation of medications for chronic diseases. JAMA. 2011;306:840-847.
- Greenwald JL, Halasyamani L, Green J, et al. Making inpatient medication patient centered, clinically relevant and implementable: a consensus statement on key principles and necessary first steps. J Hosp Med. 2010;5:477-485.
- Pippins JR, Gandhi TK, Hamann C, et al. Classifying and predicting errors of inpatient medication reconciliation. J Gen Intern Med. 2008;23:1414-1422.
- Boockvar KS, Carlson HL, Giambanco V, et al. Medication reconciliation for reducing drug-discrepancy adverse events. Am J Geriatr Pharmacother. 2006;4:236-243.
- Schnipper JL, Kirwin JL, Cotugno MC, et al. Role of pharmacist counseling in preventing adverse drug events after hospitalization. Arch Intern Med. 2006;166:565-571.
- Kaboli PJ, McClimon JB, Hoth AB, et al. Assessing the accuracy of computerized medication histories. Am J Manag Care. 2004;10(11 Pt 2):872-877.
- Boockvar KS, Livote EE, Goldstein N, et al. Electronic health records and adverse drug events after patient transfer. Qual Saf Health Care. 2010;5:Epub(Aug 19).
- Staroselsky M, Volk LA, Tsurikova R, et al. An effort to improve electronic health record medication list accuracy between visits: patients’ and physicians’ responses. Int J Med Inform. 2008;77:153-160.
- Gleason KM, McDaniel MR, Feinglass J, et al. Results of the Medications at Transitions and Clinical Handoffs (MATCH) study: an analysis of medication reconciliation errors and risk factors at hospital admission. J Gen Intern Med. 2010;25:441-447.
AMA Policy Opposes Switch to ICD-10
On Nov. 10, the American Medical Association’s House of Delegates approved a policy opposing implementation of the International Classification of Diseases and Related Health Problems, 10th Revision (ICD-10-CM) at a policy meeting in New Orleans. Following the vote, Robert M. Wah, MD, AMA board chair, stated, “The AMA will work vigorously to stop implementation of ICD-10, which will create a significant burden on the practice of medicine with no direct benefit to individual patients’ care.”
Organizations tied to hospitals, however, are fully supportive of the switch.
“We strongly support ICD-10 and the enhancements it will bring to the care that’s provided in hospitals,” says Don May, the American Hospital Association’s (AHA) vice president for policy. “The current coding system has really run its course in its ability to keep up with modern medicine.”
SHM has taken a “neutral” stance on this issue, for the time being, says SHM’s AMA delegate Bradley E. Flansbaum, DO, MPH, SFHM, director of hospitalist services at Lenox Hill Hospital in New York City. “But [SHM is] cautiously optimistic as the inpatient ecosystem evolves, hopefully, for the better.”
History of Opposition
In 2003, the AMA wrote to the National Committee on Vital and Health Statistics regarding plans to adopt ICD-10. The 55 signees of the letter (including the American College of Surgeons and other specialty societies) urged the committee to “confine your recommendation [to HHS] to the uses of ICD-10-PCS [the procedural codes portion] as a coding system for inpatient hospital services.” Another letter in 2006 to Bill Frist, then the U.S. Senate majority leader, expressed concern over a “rapid transition” from ICD-9 to ICD-10.
The AMA contends that switching to ICD-10 disproportionately burdens physicians in practice. “Depending on the size of a medical practice,” Dr. Wah says, “the total cost of impact of the ICD-10 mandate will range from $83,290 to more than $2.7 million. Physicians should not be expected to carry a disproportionate burden of the implementation costs when others in the health sector stand to reap the primary financial benefits.”
Upgrade: The Time Has Come
Organizations in support of the changeover, however, see the implementation of ICD-10 coding as a necessary step forward in improving patient care.
—Robert M. Wah, MD, board chair, American Medical Association
“It’s not unreasonable to replace a 30-year-old, out-of-date system,” says Sue Bowman, RHIA, CCS, director of coding policy and compliance with the American Health Information Management Association (AHIMA). Bowman says she is surprised that the AMA maintains the switch will not benefit patient care. “Everything nowadays has to do with healthcare data,” she says. “Without good data, you cannot measure quality of care, patient outcomes, or effectiveness of treatments. The expectation is that ICD-10 will better mirror the terminology already used in medical records.”
May agrees. “We understand the concerns,” he says, “but if you think about how much better we’ll be able to track disease and how it affects patients, there will be a much more rich data set at our disposal. This will help us develop evidence-based medicine and quality standards in a much more robust way than we can do today.”
In addition, May says, hospitalists may be able to function as a “huge resource” to their community physician colleagues, to help them understand the benefits of making the switch, and help them find the short cuts to manage the new system.
AHIMA is aware, Bowman notes, that some physician groups “were struggling with moving forward with ICD-10, but our message to the industry is for people to continue working toward implementation. CMS has made it pretty clear that there’s not going to be a delay or a grace period.”
In response to the AMA action, a spokesperson for CMS says, “Implementation of this new coding system will mean better information to improve the quality of healthcare, and more accurate payments to providers. CMS is giving significant transition time and flexibility to providers to switch over, and we will continue to work with the healthcare community to ensure successful compliance.”
Gretchen Henkel is a freelance writer based in California.
On Nov. 10, the American Medical Association’s House of Delegates approved a policy opposing implementation of the International Classification of Diseases and Related Health Problems, 10th Revision (ICD-10-CM) at a policy meeting in New Orleans. Following the vote, Robert M. Wah, MD, AMA board chair, stated, “The AMA will work vigorously to stop implementation of ICD-10, which will create a significant burden on the practice of medicine with no direct benefit to individual patients’ care.”
Organizations tied to hospitals, however, are fully supportive of the switch.
“We strongly support ICD-10 and the enhancements it will bring to the care that’s provided in hospitals,” says Don May, the American Hospital Association’s (AHA) vice president for policy. “The current coding system has really run its course in its ability to keep up with modern medicine.”
SHM has taken a “neutral” stance on this issue, for the time being, says SHM’s AMA delegate Bradley E. Flansbaum, DO, MPH, SFHM, director of hospitalist services at Lenox Hill Hospital in New York City. “But [SHM is] cautiously optimistic as the inpatient ecosystem evolves, hopefully, for the better.”
History of Opposition
In 2003, the AMA wrote to the National Committee on Vital and Health Statistics regarding plans to adopt ICD-10. The 55 signees of the letter (including the American College of Surgeons and other specialty societies) urged the committee to “confine your recommendation [to HHS] to the uses of ICD-10-PCS [the procedural codes portion] as a coding system for inpatient hospital services.” Another letter in 2006 to Bill Frist, then the U.S. Senate majority leader, expressed concern over a “rapid transition” from ICD-9 to ICD-10.
The AMA contends that switching to ICD-10 disproportionately burdens physicians in practice. “Depending on the size of a medical practice,” Dr. Wah says, “the total cost of impact of the ICD-10 mandate will range from $83,290 to more than $2.7 million. Physicians should not be expected to carry a disproportionate burden of the implementation costs when others in the health sector stand to reap the primary financial benefits.”
Upgrade: The Time Has Come
Organizations in support of the changeover, however, see the implementation of ICD-10 coding as a necessary step forward in improving patient care.
—Robert M. Wah, MD, board chair, American Medical Association
“It’s not unreasonable to replace a 30-year-old, out-of-date system,” says Sue Bowman, RHIA, CCS, director of coding policy and compliance with the American Health Information Management Association (AHIMA). Bowman says she is surprised that the AMA maintains the switch will not benefit patient care. “Everything nowadays has to do with healthcare data,” she says. “Without good data, you cannot measure quality of care, patient outcomes, or effectiveness of treatments. The expectation is that ICD-10 will better mirror the terminology already used in medical records.”
May agrees. “We understand the concerns,” he says, “but if you think about how much better we’ll be able to track disease and how it affects patients, there will be a much more rich data set at our disposal. This will help us develop evidence-based medicine and quality standards in a much more robust way than we can do today.”
In addition, May says, hospitalists may be able to function as a “huge resource” to their community physician colleagues, to help them understand the benefits of making the switch, and help them find the short cuts to manage the new system.
AHIMA is aware, Bowman notes, that some physician groups “were struggling with moving forward with ICD-10, but our message to the industry is for people to continue working toward implementation. CMS has made it pretty clear that there’s not going to be a delay or a grace period.”
In response to the AMA action, a spokesperson for CMS says, “Implementation of this new coding system will mean better information to improve the quality of healthcare, and more accurate payments to providers. CMS is giving significant transition time and flexibility to providers to switch over, and we will continue to work with the healthcare community to ensure successful compliance.”
Gretchen Henkel is a freelance writer based in California.
On Nov. 10, the American Medical Association’s House of Delegates approved a policy opposing implementation of the International Classification of Diseases and Related Health Problems, 10th Revision (ICD-10-CM) at a policy meeting in New Orleans. Following the vote, Robert M. Wah, MD, AMA board chair, stated, “The AMA will work vigorously to stop implementation of ICD-10, which will create a significant burden on the practice of medicine with no direct benefit to individual patients’ care.”
Organizations tied to hospitals, however, are fully supportive of the switch.
“We strongly support ICD-10 and the enhancements it will bring to the care that’s provided in hospitals,” says Don May, the American Hospital Association’s (AHA) vice president for policy. “The current coding system has really run its course in its ability to keep up with modern medicine.”
SHM has taken a “neutral” stance on this issue, for the time being, says SHM’s AMA delegate Bradley E. Flansbaum, DO, MPH, SFHM, director of hospitalist services at Lenox Hill Hospital in New York City. “But [SHM is] cautiously optimistic as the inpatient ecosystem evolves, hopefully, for the better.”
History of Opposition
In 2003, the AMA wrote to the National Committee on Vital and Health Statistics regarding plans to adopt ICD-10. The 55 signees of the letter (including the American College of Surgeons and other specialty societies) urged the committee to “confine your recommendation [to HHS] to the uses of ICD-10-PCS [the procedural codes portion] as a coding system for inpatient hospital services.” Another letter in 2006 to Bill Frist, then the U.S. Senate majority leader, expressed concern over a “rapid transition” from ICD-9 to ICD-10.
The AMA contends that switching to ICD-10 disproportionately burdens physicians in practice. “Depending on the size of a medical practice,” Dr. Wah says, “the total cost of impact of the ICD-10 mandate will range from $83,290 to more than $2.7 million. Physicians should not be expected to carry a disproportionate burden of the implementation costs when others in the health sector stand to reap the primary financial benefits.”
Upgrade: The Time Has Come
Organizations in support of the changeover, however, see the implementation of ICD-10 coding as a necessary step forward in improving patient care.
—Robert M. Wah, MD, board chair, American Medical Association
“It’s not unreasonable to replace a 30-year-old, out-of-date system,” says Sue Bowman, RHIA, CCS, director of coding policy and compliance with the American Health Information Management Association (AHIMA). Bowman says she is surprised that the AMA maintains the switch will not benefit patient care. “Everything nowadays has to do with healthcare data,” she says. “Without good data, you cannot measure quality of care, patient outcomes, or effectiveness of treatments. The expectation is that ICD-10 will better mirror the terminology already used in medical records.”
May agrees. “We understand the concerns,” he says, “but if you think about how much better we’ll be able to track disease and how it affects patients, there will be a much more rich data set at our disposal. This will help us develop evidence-based medicine and quality standards in a much more robust way than we can do today.”
In addition, May says, hospitalists may be able to function as a “huge resource” to their community physician colleagues, to help them understand the benefits of making the switch, and help them find the short cuts to manage the new system.
AHIMA is aware, Bowman notes, that some physician groups “were struggling with moving forward with ICD-10, but our message to the industry is for people to continue working toward implementation. CMS has made it pretty clear that there’s not going to be a delay or a grace period.”
In response to the AMA action, a spokesperson for CMS says, “Implementation of this new coding system will mean better information to improve the quality of healthcare, and more accurate payments to providers. CMS is giving significant transition time and flexibility to providers to switch over, and we will continue to work with the healthcare community to ensure successful compliance.”
Gretchen Henkel is a freelance writer based in California.
Partner with Pharmacy to Maximize Patient Care
You’re ready to discharge a patient, but you don’t know whether the medication you’ve ordered will be available in the outpatient setting. Who do you ask? Your pharmacy service will have the answers, and if you’ve established a collegial relationship with the pharmacists there, most likely you can get a quick answer via page, text, or phone call. But if you don’t have personal contact with your pharmacists, chances are the interchange will impersonal—and that could mean missing ou
“Pharmacists may be underutilized, especially if the range of clinical services they offer are not recognized,” notes Kristine Gleason, RPh, clinical quality leader at Northwestern Memorial Hospital in Chicago. “We can be an excellent resource for young hospitalists and clinicians, offering information on clinical dosing and monitoring of complex, high-risk medications.”
Pharmacists also can be valuable resources for medication reconciliation and patient counseling, Gleason says, adding that “our goal is to work collaboratively with our clinicians to help ensure patients receive evidence-based medication regimens that are safe and without error and that are tailored to each patient’s individualized characteristics.”
Benefits of Rounding
Interactions between hospital pharmacies and HM services vary by institution size and organization. Roberta Barber, PharmD, MPH, is assistant vice president of pharmacy for Virtua Health’s four hospital campuses in New Jersey. At Memorial Hospital, where Erik DeLue, MD, MBA, SFHM, first established a hospitalist program, pharmacists are present in the ICU units and participate in care-coordination rounds.
Barber is crafting policies to extend the decentralized pharmacist model to all of Virtua’s hospitals. Equipped with cordless phones and tablet computers, pharmacists will be able to round with the HM team without sacrificing availability to other physicians and hospital staff. In this way, she says, “physicians will be able to consult with pharmacists as they’re creating their treatment plans, and the pharmacist can intervene regarding potential problem orders right then and there.”
At the University of California at San Francisco Medical Center, clinical pharmacists in the general medicine division work closely with the nine medicine teams run by hospitalists. That means 24/7 availability by pager, participating in multidisciplinary rounds, and furnishing new physicians with a “contacts” card and an orientation guide to help hospitalists write better orders, says Vicki Ising Jue, PharmD.
The personal touch is appreciated. “If I am in the pharmacy making a call and not on the unit, it just makes the phone call so much easier if the caller happens to be someone I’ve worked with before,” says UCSF’s Alan Tan, PharmD.
View hundreds of HM opportunities at SHM's Career Center
The degree of communication with pharmacy services may depend on whether you’re working in a teaching hospital with a structured orientation program or starting out in a community hospital. No matter the setting, though, Gleason says the pharmacist’s mission stays the same.
“We’re all striving to get to the same goal: safe, effective and patient-centered care to achieve positive outcomes for our patients,” she says. “Partnering with pharmacists can really move all of us closer to that goal.”
Gretchen Henkel is a freelance writer based in California.
Be PROACTIVE
One excellent way to foster collaboration with your hospital pharmacists and gain a better understanding of the medication management services they can provide, Gleason says, is to visit the department. “Spend an hour with us, shadow us, come to a meeting, and understand what we do professionally,” she explains.
Barber agrees: “If your hospital doesn’t offer training on the range of pharmacy services, solicit that yourself. Orient yourself to pharmacy rules and regulations; familiarize yourself with your hospital’s formulary and the role of the P&T committee in placing drugs on the formulary.”—GH
You’re ready to discharge a patient, but you don’t know whether the medication you’ve ordered will be available in the outpatient setting. Who do you ask? Your pharmacy service will have the answers, and if you’ve established a collegial relationship with the pharmacists there, most likely you can get a quick answer via page, text, or phone call. But if you don’t have personal contact with your pharmacists, chances are the interchange will impersonal—and that could mean missing ou
“Pharmacists may be underutilized, especially if the range of clinical services they offer are not recognized,” notes Kristine Gleason, RPh, clinical quality leader at Northwestern Memorial Hospital in Chicago. “We can be an excellent resource for young hospitalists and clinicians, offering information on clinical dosing and monitoring of complex, high-risk medications.”
Pharmacists also can be valuable resources for medication reconciliation and patient counseling, Gleason says, adding that “our goal is to work collaboratively with our clinicians to help ensure patients receive evidence-based medication regimens that are safe and without error and that are tailored to each patient’s individualized characteristics.”
Benefits of Rounding
Interactions between hospital pharmacies and HM services vary by institution size and organization. Roberta Barber, PharmD, MPH, is assistant vice president of pharmacy for Virtua Health’s four hospital campuses in New Jersey. At Memorial Hospital, where Erik DeLue, MD, MBA, SFHM, first established a hospitalist program, pharmacists are present in the ICU units and participate in care-coordination rounds.
Barber is crafting policies to extend the decentralized pharmacist model to all of Virtua’s hospitals. Equipped with cordless phones and tablet computers, pharmacists will be able to round with the HM team without sacrificing availability to other physicians and hospital staff. In this way, she says, “physicians will be able to consult with pharmacists as they’re creating their treatment plans, and the pharmacist can intervene regarding potential problem orders right then and there.”
At the University of California at San Francisco Medical Center, clinical pharmacists in the general medicine division work closely with the nine medicine teams run by hospitalists. That means 24/7 availability by pager, participating in multidisciplinary rounds, and furnishing new physicians with a “contacts” card and an orientation guide to help hospitalists write better orders, says Vicki Ising Jue, PharmD.
The personal touch is appreciated. “If I am in the pharmacy making a call and not on the unit, it just makes the phone call so much easier if the caller happens to be someone I’ve worked with before,” says UCSF’s Alan Tan, PharmD.
View hundreds of HM opportunities at SHM's Career Center
The degree of communication with pharmacy services may depend on whether you’re working in a teaching hospital with a structured orientation program or starting out in a community hospital. No matter the setting, though, Gleason says the pharmacist’s mission stays the same.
“We’re all striving to get to the same goal: safe, effective and patient-centered care to achieve positive outcomes for our patients,” she says. “Partnering with pharmacists can really move all of us closer to that goal.”
Gretchen Henkel is a freelance writer based in California.
Be PROACTIVE
One excellent way to foster collaboration with your hospital pharmacists and gain a better understanding of the medication management services they can provide, Gleason says, is to visit the department. “Spend an hour with us, shadow us, come to a meeting, and understand what we do professionally,” she explains.
Barber agrees: “If your hospital doesn’t offer training on the range of pharmacy services, solicit that yourself. Orient yourself to pharmacy rules and regulations; familiarize yourself with your hospital’s formulary and the role of the P&T committee in placing drugs on the formulary.”—GH
You’re ready to discharge a patient, but you don’t know whether the medication you’ve ordered will be available in the outpatient setting. Who do you ask? Your pharmacy service will have the answers, and if you’ve established a collegial relationship with the pharmacists there, most likely you can get a quick answer via page, text, or phone call. But if you don’t have personal contact with your pharmacists, chances are the interchange will impersonal—and that could mean missing ou
“Pharmacists may be underutilized, especially if the range of clinical services they offer are not recognized,” notes Kristine Gleason, RPh, clinical quality leader at Northwestern Memorial Hospital in Chicago. “We can be an excellent resource for young hospitalists and clinicians, offering information on clinical dosing and monitoring of complex, high-risk medications.”
Pharmacists also can be valuable resources for medication reconciliation and patient counseling, Gleason says, adding that “our goal is to work collaboratively with our clinicians to help ensure patients receive evidence-based medication regimens that are safe and without error and that are tailored to each patient’s individualized characteristics.”
Benefits of Rounding
Interactions between hospital pharmacies and HM services vary by institution size and organization. Roberta Barber, PharmD, MPH, is assistant vice president of pharmacy for Virtua Health’s four hospital campuses in New Jersey. At Memorial Hospital, where Erik DeLue, MD, MBA, SFHM, first established a hospitalist program, pharmacists are present in the ICU units and participate in care-coordination rounds.
Barber is crafting policies to extend the decentralized pharmacist model to all of Virtua’s hospitals. Equipped with cordless phones and tablet computers, pharmacists will be able to round with the HM team without sacrificing availability to other physicians and hospital staff. In this way, she says, “physicians will be able to consult with pharmacists as they’re creating their treatment plans, and the pharmacist can intervene regarding potential problem orders right then and there.”
At the University of California at San Francisco Medical Center, clinical pharmacists in the general medicine division work closely with the nine medicine teams run by hospitalists. That means 24/7 availability by pager, participating in multidisciplinary rounds, and furnishing new physicians with a “contacts” card and an orientation guide to help hospitalists write better orders, says Vicki Ising Jue, PharmD.
The personal touch is appreciated. “If I am in the pharmacy making a call and not on the unit, it just makes the phone call so much easier if the caller happens to be someone I’ve worked with before,” says UCSF’s Alan Tan, PharmD.
View hundreds of HM opportunities at SHM's Career Center
The degree of communication with pharmacy services may depend on whether you’re working in a teaching hospital with a structured orientation program or starting out in a community hospital. No matter the setting, though, Gleason says the pharmacist’s mission stays the same.
“We’re all striving to get to the same goal: safe, effective and patient-centered care to achieve positive outcomes for our patients,” she says. “Partnering with pharmacists can really move all of us closer to that goal.”
Gretchen Henkel is a freelance writer based in California.
Be PROACTIVE
One excellent way to foster collaboration with your hospital pharmacists and gain a better understanding of the medication management services they can provide, Gleason says, is to visit the department. “Spend an hour with us, shadow us, come to a meeting, and understand what we do professionally,” she explains.
Barber agrees: “If your hospital doesn’t offer training on the range of pharmacy services, solicit that yourself. Orient yourself to pharmacy rules and regulations; familiarize yourself with your hospital’s formulary and the role of the P&T committee in placing drugs on the formulary.”—GH
Fear Not the Switch from ICD-9 to ICD-10
Some people adopt a “Chicken Little” mentality when faced with making big changes, says Kathy DeVault, RHIS, CCS, CCS-P, manager of professional practice resources for the American Health Information Management Association (AHIMA). The change she’s referring to is the switch from the current version of the International Statistical Classification of Diseases coding system (ICD-9-CM) to the ICD-10-CM/ICD-10-PCS, which must be effective in hospitals by Oct. 1, 2013.
Hospitalist Jeffrey Farber, MD, assistant professor of geriatrics and palliative medicine and director of the Mobile ACE Service at Mount Sinai Hospital in New York City, also is director of the Clinical Documentation Improvement Department at Mount Sinai. He already is intimately involved with his hospital’s ICD-10 implementation process.
“For hospitals, this is a very big deal,” Dr. Farber says, “because it affects not just the coding department, but quality, compliance, and public reporting. On the physician side, there will be major changes in clinical documentation. Hospitalists who also do procedures, even bedside procedures, need to understand what is required.”
Why the Change?
Surprisingly, the U.S. is the last industrialized country in the world to upgrade to the ICD-10 system. The older system, in use since 1979, does not reflect three decades of change in medicine. “ICD-10 allows for a much better capture of specific types of treated diagnoses, provided services, and performed procedures,” Dr. Farber says, “and allows a lot more room to grow for the future.”
At first glance, the sheer numbers of new codes appear daunting. For example, procedures codes will increase from the current 4,000 to approximately 87,000. Hospitalists who perform procedures must include more description in their notes, including devices used and anatomical location of device placement.
Even if you’re not doing procedures, you may not relish the prospect of going from the current 14,000 ICD-9-CM diagnoses codes to nearly 70,000 ICD-10 codes. But, Dr. Farber explains, many of the increased descriptors have to do with laterality, which previously was not captured. To note a diagnosis of stroke, you will have to write not only whether it occurred in the posterior cerebral blood vessel, but also whether it was right or left posterior cerebral.
Ultimately, he believes, this type of specificity will relieve a burden on hospitalists, because providing more specific documentation should reduce queries from coders.
Common-Sense Approach
The October 2013 deadline allows plenty of time for physician training, says DeVault, who has been training coders through AHIMA’s ICD-10 Academy the past two years. Breaking the process down into manageable steps is helpful, she says.
—Jeffrey Farber, MD, assistant professor, geriatrics and palliative medicine, director, Clinical Documentation Improvement Department, Mount Sinai Hospital, New York City
“Look at your group’s most common, acute conditions, for example, and ask, ‘What is missing in the documentation?’ Especially if you can make bridges with your health information management (HIM) department, you will find that there are many opportunities to teach each other,” she says.
Hospitalists can do several things to ready their group for ICD-10, Dr. Farber says. Take a proactive stance, he advises, and select your group’s top 25 diagnoses. Then work with coding staff to map them from ICD-9 to ICD-10. On a macro level, understand what your hospital’s timeline is for the change. DeVault says that HIM departments are eager to collaborate with physician champions.
The good news: The sky isn’t really falling, according to DeVault. And the change to ICD-10 actually offers lots of opportunities for collaborations between hospitalists and health information departments.
Gretchen Henkel is a freelance writer based in California.
Watch Out for GEMs
Physicians often are encouraged to use general equivalence maps (GEMs) to acquaint themselves with the differences between coding sets. Relying solely on GEMs, however, is not a good idea for the long term, DeVault cautions. “GEMs are meant to serve as a transition tool but are not designed to code from,” she says. “It’s imperative that coders—and providers—actually learn the new system and that they not rely on GEMs for coding.”—GH
Resources for Physicians
- The AHIMA ICD-10 website offers a timeline for assessment and implementation of ICD-10 under the “Physician Office Role-Based Model” heading.
- The AMA’s resources include a physician timeline for ICD-10 implementation (PDF).
- SHM’s website offers a wealth of resources on documentation billing and coding for hospitalists.
Some people adopt a “Chicken Little” mentality when faced with making big changes, says Kathy DeVault, RHIS, CCS, CCS-P, manager of professional practice resources for the American Health Information Management Association (AHIMA). The change she’s referring to is the switch from the current version of the International Statistical Classification of Diseases coding system (ICD-9-CM) to the ICD-10-CM/ICD-10-PCS, which must be effective in hospitals by Oct. 1, 2013.
Hospitalist Jeffrey Farber, MD, assistant professor of geriatrics and palliative medicine and director of the Mobile ACE Service at Mount Sinai Hospital in New York City, also is director of the Clinical Documentation Improvement Department at Mount Sinai. He already is intimately involved with his hospital’s ICD-10 implementation process.
“For hospitals, this is a very big deal,” Dr. Farber says, “because it affects not just the coding department, but quality, compliance, and public reporting. On the physician side, there will be major changes in clinical documentation. Hospitalists who also do procedures, even bedside procedures, need to understand what is required.”
Why the Change?
Surprisingly, the U.S. is the last industrialized country in the world to upgrade to the ICD-10 system. The older system, in use since 1979, does not reflect three decades of change in medicine. “ICD-10 allows for a much better capture of specific types of treated diagnoses, provided services, and performed procedures,” Dr. Farber says, “and allows a lot more room to grow for the future.”
At first glance, the sheer numbers of new codes appear daunting. For example, procedures codes will increase from the current 4,000 to approximately 87,000. Hospitalists who perform procedures must include more description in their notes, including devices used and anatomical location of device placement.
Even if you’re not doing procedures, you may not relish the prospect of going from the current 14,000 ICD-9-CM diagnoses codes to nearly 70,000 ICD-10 codes. But, Dr. Farber explains, many of the increased descriptors have to do with laterality, which previously was not captured. To note a diagnosis of stroke, you will have to write not only whether it occurred in the posterior cerebral blood vessel, but also whether it was right or left posterior cerebral.
Ultimately, he believes, this type of specificity will relieve a burden on hospitalists, because providing more specific documentation should reduce queries from coders.
Common-Sense Approach
The October 2013 deadline allows plenty of time for physician training, says DeVault, who has been training coders through AHIMA’s ICD-10 Academy the past two years. Breaking the process down into manageable steps is helpful, she says.
—Jeffrey Farber, MD, assistant professor, geriatrics and palliative medicine, director, Clinical Documentation Improvement Department, Mount Sinai Hospital, New York City
“Look at your group’s most common, acute conditions, for example, and ask, ‘What is missing in the documentation?’ Especially if you can make bridges with your health information management (HIM) department, you will find that there are many opportunities to teach each other,” she says.
Hospitalists can do several things to ready their group for ICD-10, Dr. Farber says. Take a proactive stance, he advises, and select your group’s top 25 diagnoses. Then work with coding staff to map them from ICD-9 to ICD-10. On a macro level, understand what your hospital’s timeline is for the change. DeVault says that HIM departments are eager to collaborate with physician champions.
The good news: The sky isn’t really falling, according to DeVault. And the change to ICD-10 actually offers lots of opportunities for collaborations between hospitalists and health information departments.
Gretchen Henkel is a freelance writer based in California.
Watch Out for GEMs
Physicians often are encouraged to use general equivalence maps (GEMs) to acquaint themselves with the differences between coding sets. Relying solely on GEMs, however, is not a good idea for the long term, DeVault cautions. “GEMs are meant to serve as a transition tool but are not designed to code from,” she says. “It’s imperative that coders—and providers—actually learn the new system and that they not rely on GEMs for coding.”—GH
Resources for Physicians
- The AHIMA ICD-10 website offers a timeline for assessment and implementation of ICD-10 under the “Physician Office Role-Based Model” heading.
- The AMA’s resources include a physician timeline for ICD-10 implementation (PDF).
- SHM’s website offers a wealth of resources on documentation billing and coding for hospitalists.
Some people adopt a “Chicken Little” mentality when faced with making big changes, says Kathy DeVault, RHIS, CCS, CCS-P, manager of professional practice resources for the American Health Information Management Association (AHIMA). The change she’s referring to is the switch from the current version of the International Statistical Classification of Diseases coding system (ICD-9-CM) to the ICD-10-CM/ICD-10-PCS, which must be effective in hospitals by Oct. 1, 2013.
Hospitalist Jeffrey Farber, MD, assistant professor of geriatrics and palliative medicine and director of the Mobile ACE Service at Mount Sinai Hospital in New York City, also is director of the Clinical Documentation Improvement Department at Mount Sinai. He already is intimately involved with his hospital’s ICD-10 implementation process.
“For hospitals, this is a very big deal,” Dr. Farber says, “because it affects not just the coding department, but quality, compliance, and public reporting. On the physician side, there will be major changes in clinical documentation. Hospitalists who also do procedures, even bedside procedures, need to understand what is required.”
Why the Change?
Surprisingly, the U.S. is the last industrialized country in the world to upgrade to the ICD-10 system. The older system, in use since 1979, does not reflect three decades of change in medicine. “ICD-10 allows for a much better capture of specific types of treated diagnoses, provided services, and performed procedures,” Dr. Farber says, “and allows a lot more room to grow for the future.”
At first glance, the sheer numbers of new codes appear daunting. For example, procedures codes will increase from the current 4,000 to approximately 87,000. Hospitalists who perform procedures must include more description in their notes, including devices used and anatomical location of device placement.
Even if you’re not doing procedures, you may not relish the prospect of going from the current 14,000 ICD-9-CM diagnoses codes to nearly 70,000 ICD-10 codes. But, Dr. Farber explains, many of the increased descriptors have to do with laterality, which previously was not captured. To note a diagnosis of stroke, you will have to write not only whether it occurred in the posterior cerebral blood vessel, but also whether it was right or left posterior cerebral.
Ultimately, he believes, this type of specificity will relieve a burden on hospitalists, because providing more specific documentation should reduce queries from coders.
Common-Sense Approach
The October 2013 deadline allows plenty of time for physician training, says DeVault, who has been training coders through AHIMA’s ICD-10 Academy the past two years. Breaking the process down into manageable steps is helpful, she says.
—Jeffrey Farber, MD, assistant professor, geriatrics and palliative medicine, director, Clinical Documentation Improvement Department, Mount Sinai Hospital, New York City
“Look at your group’s most common, acute conditions, for example, and ask, ‘What is missing in the documentation?’ Especially if you can make bridges with your health information management (HIM) department, you will find that there are many opportunities to teach each other,” she says.
Hospitalists can do several things to ready their group for ICD-10, Dr. Farber says. Take a proactive stance, he advises, and select your group’s top 25 diagnoses. Then work with coding staff to map them from ICD-9 to ICD-10. On a macro level, understand what your hospital’s timeline is for the change. DeVault says that HIM departments are eager to collaborate with physician champions.
The good news: The sky isn’t really falling, according to DeVault. And the change to ICD-10 actually offers lots of opportunities for collaborations between hospitalists and health information departments.
Gretchen Henkel is a freelance writer based in California.
Watch Out for GEMs
Physicians often are encouraged to use general equivalence maps (GEMs) to acquaint themselves with the differences between coding sets. Relying solely on GEMs, however, is not a good idea for the long term, DeVault cautions. “GEMs are meant to serve as a transition tool but are not designed to code from,” she says. “It’s imperative that coders—and providers—actually learn the new system and that they not rely on GEMs for coding.”—GH
Resources for Physicians
- The AHIMA ICD-10 website offers a timeline for assessment and implementation of ICD-10 under the “Physician Office Role-Based Model” heading.
- The AMA’s resources include a physician timeline for ICD-10 implementation (PDF).
- SHM’s website offers a wealth of resources on documentation billing and coding for hospitalists.
How Hospitalists Can Team with Nursing to Improve Patient Care
Establishing mutual respect and trust between hospitalists and nurses is an important part of ensuring patient safety, whether you’re on your first job or your 20th, says Angela Beck, RN, director of critical-care services at Nebraska Medical Center in Omaha.
“Nurses are important coordinators of care,” she says. “Recognizing and valuing nurses for that is truly the most important thing for the patient, and can also help hospitalists build relationships.”
Key Partners
Forming a collaborative relationship with the nursing service might depend on where you start. At Northwestern Memorial Hospital in Chicago, the nursing service enjoys a “close and collaborative relationship” with hospitalists, according to Kristin Ramsey, RN, MSN, MPPM, NE-BC, associate chief nurse and executive director of operations. New hospitalists are oriented to the care-delivery models on the inpatient care units. In addition, hospitalists are acculturated into the hospital’s coleadership model.
“We have partnered with our hospitalists to create a model in which the physician and nurse leader collaboratively lead the development of multidisciplinary, subspecialty teams to ensure quality outcomes,” Ramsey says. “The model is so successful with the hospitalists that we are now extending it to other areas in the organization.”
Round Sharing
Absent a formalized training protocol for partnering with nursing, hospitalists still can learn a great deal by listening to and communicating with the nursing staff, says Connie Ogden, RN, MSN, NEA-BC, executive director of adult acute services at Nebraska Medical Center. “Nurses are there around the clock caring for patients and may have a different insight” about patients’ evolving conditions, she says.
Care for the patient improves if everyone is on the same page, Ogden adds. That’s why it makes sense, she says, to include nurses during rounds. Beck agrees: “If nurses aren’t there to hear how the plan of care comes about, there is no reason to believe they can effectively describe it once the physician turns around and walks away to see another patient.”
In critical-care units, according to Beck, nurses can function as a bridge between patients and physicians. For example, they can help patients define and express their goals. Some of these goals can be incremental, she notes, such as “I really want to get out of bed this afternoon,” or “I really want my family here to listen to this message.”
Different Role, Same Goal
As director of adult acute services, Ogden often receives complaints from physicians about calls they receive from nurses. Often, these calls emanate from a concern for the patient (e.g. a 2 a.m. call for a Tylenol order to address a headache) or from the requirement that nurses follow policy and clarify orders. If hospitalists understand the back story of the call, their perception of its purpose can change.
Although there have been strides toward better nurse-physician collaboration, “we still have a lot of opportunities for improvement,” Beck asserts.
Establishing mutual respect and trust is not an overnight accomplishment. As Ogden explains, physicians and nurses have different roles, but they share the same goal: quality outcomes in patient care.
Gretchen Henkel is a freelance writer based in southern California.
Best Ways to Improve Hospitalist-Nursing Collaboration
“A good portion of nurses are relationship builders,” says Beck, director of critical-care services at Nebraska Medical Center. She urges hospitalists on a new job to just “be physically present, in the beginning, on inpatient units” whenever possible. “Acting like you care is really important, and nurses will respond to that,” she says. “You can create an environment in which nurses’ feedback is valued.”
She also recommends, especially for new hospitalists, Dr. Peter J. Pronovost’s three-part talk “The Science of Safety,” delivered to incoming residents at Johns Hopkins University Medical Center in Baltimore, where Dr. Provonost is medical director of the quality and safety research group.—GH
Establishing mutual respect and trust between hospitalists and nurses is an important part of ensuring patient safety, whether you’re on your first job or your 20th, says Angela Beck, RN, director of critical-care services at Nebraska Medical Center in Omaha.
“Nurses are important coordinators of care,” she says. “Recognizing and valuing nurses for that is truly the most important thing for the patient, and can also help hospitalists build relationships.”
Key Partners
Forming a collaborative relationship with the nursing service might depend on where you start. At Northwestern Memorial Hospital in Chicago, the nursing service enjoys a “close and collaborative relationship” with hospitalists, according to Kristin Ramsey, RN, MSN, MPPM, NE-BC, associate chief nurse and executive director of operations. New hospitalists are oriented to the care-delivery models on the inpatient care units. In addition, hospitalists are acculturated into the hospital’s coleadership model.
“We have partnered with our hospitalists to create a model in which the physician and nurse leader collaboratively lead the development of multidisciplinary, subspecialty teams to ensure quality outcomes,” Ramsey says. “The model is so successful with the hospitalists that we are now extending it to other areas in the organization.”
Round Sharing
Absent a formalized training protocol for partnering with nursing, hospitalists still can learn a great deal by listening to and communicating with the nursing staff, says Connie Ogden, RN, MSN, NEA-BC, executive director of adult acute services at Nebraska Medical Center. “Nurses are there around the clock caring for patients and may have a different insight” about patients’ evolving conditions, she says.
Care for the patient improves if everyone is on the same page, Ogden adds. That’s why it makes sense, she says, to include nurses during rounds. Beck agrees: “If nurses aren’t there to hear how the plan of care comes about, there is no reason to believe they can effectively describe it once the physician turns around and walks away to see another patient.”
In critical-care units, according to Beck, nurses can function as a bridge between patients and physicians. For example, they can help patients define and express their goals. Some of these goals can be incremental, she notes, such as “I really want to get out of bed this afternoon,” or “I really want my family here to listen to this message.”
Different Role, Same Goal
As director of adult acute services, Ogden often receives complaints from physicians about calls they receive from nurses. Often, these calls emanate from a concern for the patient (e.g. a 2 a.m. call for a Tylenol order to address a headache) or from the requirement that nurses follow policy and clarify orders. If hospitalists understand the back story of the call, their perception of its purpose can change.
Although there have been strides toward better nurse-physician collaboration, “we still have a lot of opportunities for improvement,” Beck asserts.
Establishing mutual respect and trust is not an overnight accomplishment. As Ogden explains, physicians and nurses have different roles, but they share the same goal: quality outcomes in patient care.
Gretchen Henkel is a freelance writer based in southern California.
Best Ways to Improve Hospitalist-Nursing Collaboration
“A good portion of nurses are relationship builders,” says Beck, director of critical-care services at Nebraska Medical Center. She urges hospitalists on a new job to just “be physically present, in the beginning, on inpatient units” whenever possible. “Acting like you care is really important, and nurses will respond to that,” she says. “You can create an environment in which nurses’ feedback is valued.”
She also recommends, especially for new hospitalists, Dr. Peter J. Pronovost’s three-part talk “The Science of Safety,” delivered to incoming residents at Johns Hopkins University Medical Center in Baltimore, where Dr. Provonost is medical director of the quality and safety research group.—GH
Establishing mutual respect and trust between hospitalists and nurses is an important part of ensuring patient safety, whether you’re on your first job or your 20th, says Angela Beck, RN, director of critical-care services at Nebraska Medical Center in Omaha.
“Nurses are important coordinators of care,” she says. “Recognizing and valuing nurses for that is truly the most important thing for the patient, and can also help hospitalists build relationships.”
Key Partners
Forming a collaborative relationship with the nursing service might depend on where you start. At Northwestern Memorial Hospital in Chicago, the nursing service enjoys a “close and collaborative relationship” with hospitalists, according to Kristin Ramsey, RN, MSN, MPPM, NE-BC, associate chief nurse and executive director of operations. New hospitalists are oriented to the care-delivery models on the inpatient care units. In addition, hospitalists are acculturated into the hospital’s coleadership model.
“We have partnered with our hospitalists to create a model in which the physician and nurse leader collaboratively lead the development of multidisciplinary, subspecialty teams to ensure quality outcomes,” Ramsey says. “The model is so successful with the hospitalists that we are now extending it to other areas in the organization.”
Round Sharing
Absent a formalized training protocol for partnering with nursing, hospitalists still can learn a great deal by listening to and communicating with the nursing staff, says Connie Ogden, RN, MSN, NEA-BC, executive director of adult acute services at Nebraska Medical Center. “Nurses are there around the clock caring for patients and may have a different insight” about patients’ evolving conditions, she says.
Care for the patient improves if everyone is on the same page, Ogden adds. That’s why it makes sense, she says, to include nurses during rounds. Beck agrees: “If nurses aren’t there to hear how the plan of care comes about, there is no reason to believe they can effectively describe it once the physician turns around and walks away to see another patient.”
In critical-care units, according to Beck, nurses can function as a bridge between patients and physicians. For example, they can help patients define and express their goals. Some of these goals can be incremental, she notes, such as “I really want to get out of bed this afternoon,” or “I really want my family here to listen to this message.”
Different Role, Same Goal
As director of adult acute services, Ogden often receives complaints from physicians about calls they receive from nurses. Often, these calls emanate from a concern for the patient (e.g. a 2 a.m. call for a Tylenol order to address a headache) or from the requirement that nurses follow policy and clarify orders. If hospitalists understand the back story of the call, their perception of its purpose can change.
Although there have been strides toward better nurse-physician collaboration, “we still have a lot of opportunities for improvement,” Beck asserts.
Establishing mutual respect and trust is not an overnight accomplishment. As Ogden explains, physicians and nurses have different roles, but they share the same goal: quality outcomes in patient care.
Gretchen Henkel is a freelance writer based in southern California.
Best Ways to Improve Hospitalist-Nursing Collaboration
“A good portion of nurses are relationship builders,” says Beck, director of critical-care services at Nebraska Medical Center. She urges hospitalists on a new job to just “be physically present, in the beginning, on inpatient units” whenever possible. “Acting like you care is really important, and nurses will respond to that,” she says. “You can create an environment in which nurses’ feedback is valued.”
She also recommends, especially for new hospitalists, Dr. Peter J. Pronovost’s three-part talk “The Science of Safety,” delivered to incoming residents at Johns Hopkins University Medical Center in Baltimore, where Dr. Provonost is medical director of the quality and safety research group.—GH
Super-Commuters
A “long commute” once meant 60 minutes of drive time or a long haul on public transit from the suburbs to city centers. That definition has changed quite a bit as the nation’s workforce becomes more mobile.
Take, for instance, hospitalist Yun Namkung, MD, who lives in Queens, N.Y., but works at Leflore Hospital, a 248-bed regional medical center in Greenwood, Miss., about 130 miles south of Memphis. “I’m something called a ‘firefighter’ within the company,” says Dr. Namkung, who’s been traveling long distances to work for his employer, Brentwood, Tenn.-based Cogent-HMG.
Dr. Namkung’s first long-distance commute was an interim assignment: He was an HMG program director in upstate New York anticipating a move to California. The move didn’t materialize, and now, after two years as a “super-commuter,” he says, “Traveling is actually fulfilling. You get to meet different people and supporting staff. You get exposed to a variety of patients, so clinically, you get better. I think I can continue to do this for a while.”
Super-commuters go by various names and monikers—“firefighters,” “travelers,” “vagabonds”—but they share a common reality: one or two weeks a month, and in some cases every week, they’re traveling long distances from home to work. And while it might not be for every hospitalist, this mega-commute phenomenon has pros and cons, hidden costs, and unexpected perks.

—Charles Barnett, MD, Knoxville, Tenn.
An Upward Trend?
Transportation policy consultant Alan E. Pisarski, author of “Commuting in America (Vols. 1-3),” often testifies before Congress on transportation issues for policy planning and investment requirements. The third volume of his “Commuting in America” series, published in 2006, found that the number of workers with commutes of more than 60 minutes increased almost 50% from 1990 to 2000.1 That duration probably rose even more following the economic downturn that began in 2008, he says, as the notion of an “acceptable” commute changes when the job market is tight.
The long-distance commuting trend is likely to increase, he says, because highly skilled workers (e.g. physicians) are in short supply. In our mobile society, he adds, “professionals are more willing to accept long distance separation from their families, on at least some kind of scheduled basis.”
In addition, as millions of baby boomers retire, replacing their skill sets is proving difficult. Companies are trying to hold boomers in the labor force longer, offering attractive perks so that they will stay.
Many jobs, even in a telecommuting society, still require in-person deliveries. And for some, super-commuting is a better alternative to relocation. For others, it might be the only alternative, given the poor housing market. That’s the way Anthony Venturato sees it.
“In my business, [we] have to be where the project is,” says Venturato, a project manager for passenger rail projects for STV Inc., a leading architectural, engineering, and construction management firm. “We have virtual meeting rooms, but we’ve got a long way to go before working closely together and being physically far away are equivalent—like that great scene in “Star Wars” where holograms of ‘attendees’ were interacting around a conference table. To run a project, at least in the early 21st century, you’ve gotta be there.” (see “Nomadic Lifestyle Works for Some,”)
—Yun Namkung, MD, Queens, N.Y.
Models Differ
Mark Dotson, vice president of recruiting at Cogent-HMG, says his company instituted a “travelers” model in October of 2009 to reduce its locum tenens usage. Travelers, he says, are hospitalists licensed in several states who can be placed in different programs, most within driving distance. Some request a remote location, such as one Cogent-HMG hospitalist who resides in Dallas and has been commuting to Great Falls, Tenn., for more two years.
Dotson explains that the company’s travelers “are not typical locums who may just say, ‘I’ll be here for two months and then I’m out of here.’ They are employed by us, get full benefits [plus a 10% premium over regular employees] and training from our academy,” he says. “They are looked upon as part of the team when we place them in a program, and not an interim solution.”
Travelers contribute to program stability and improved quality and productivity metrics, Dotson adds. In Great Falls, for instance, the hospitalist team, which includes a traveler on every rotation, has regularly met its quality performance measures and RVU requirements since being fully staffed. Dotson estimates that 10% of the hospitalists hired by Cogent-HMG last year were travelers, and he’d like to see that percentage grow to 25% to meet increasing demand.
EmCare Inpatient Services in Dallas takes a different approach. They use super-commuters only for short-term startups, says CEO Mark Hamm, who’s “never been an advocate of flying people in and out. You don’t ever get the continuity that you need within the practice.”
To establish trust with referring primary-care physicians (PCPs), hospitalist programs need to comprise 80% to 90% of residential hospitalists, he says. Otherwise, EmCare becomes “just a staffing company and not a partner” with client hospitals. This is especially essential when it comes to hiring medical directors, he says, who must be present for meetings and administering program operations.
A Good Fit
So who are the super-commuter hospitalists? Dotson, of Cogent-HMG, says that the majority of those willing to travel tend to be single. Hospitalists who are in between residency and starting a fellowship find this type of assignment provides consistent scheduling, income, and benefits to them and their families. Another contingent: mature career hospitalists with grown children.
Eric Kerley, MD, FAAP, FACP lives and works primarily in eastern Tennessee, where he is a full-time medical director. He saw his friend and colleague Charles Barnett, MD, taking assignments in Wyoming, and thought traveling for work “sounded interesting.”
“I’m a Southern boy who has lived my entire life between Orlando [Fla.], Tennessee, and Texas,” he says, “so I picked my locations based on places I would want to go.”
Dr. Kerley’s first yearlong assignment, in 2009-2010, was in central Alaska at a 75-bed facility. He worked as a nocturnist. “To see minus-20-degree Fahrenheit temperatures and frozen rivers, and days that are 22 hours long, that was pretty amazing,” he says. Being away for one week a month is really not much different than a week of day shifts at home, he adds.
Dr. Barnett began super-commuting four years ago from his home in Knoxville, Tenn., to Gillette, Wyo. Traveling to Wyoming is his regular commuter gig—he stays at the hospital—and he enjoys working in another environment.
The away time also works for his marriage, he says. “Just before I leave for an assignment, my wife’s ready to see me go,” he says. “And then, when I come home, she’s anxious for me to be there, so it’s sort of like a honeymoon once a month for both of us.”
Continued below...
Pros and Cons
Although he misses his family when he’s traveling, Dr. Namkung now spends more quality time with them, “because I realize how precious that time is.” His wife, a pharmacist, makes it a point to take time off when he’s home, and they do more things together as a family.
Another bonus: “I meet different docs, nursing staffs, and administrators,” Dr. Namkung says. “Since I’m here alone, we have the chance to have dinner together and spend time. In that way, I bond with a lot more people than I would normally if I stayed in one place.”
Dr. Kerley racked up the frequent-flier miles during his one-year assignment to Alaska, which was a plus when it came to financing family vacations.
Working in other states entails meeting state-specific licensing requirements. Some companies, such as Cogent-HMG, pay the costs of obtaining those state licenses. Others do not, and the paperwork, says Dr. Barnett, can be “a nightmare.” Locum Leaders CEO Will Drescher, MD, says his company pays for licenses in some states and assists with paperwork in others.

—Eric Kerley, MD, medical director, Morristown, Tenn, nocturnist, PeaceHealth Medical Group, Ketchikan, Ak.
Unless hospitalists are full-time employees of the organization, such as Dr. Namkung with Cogent-HMG, their income likely will be considered independent contracting by the IRS. That means you’ll be filing an extra form (1099) with your return, and you may have to pay quarterly estimated self-employment tax. Hospitalists are encouraged to consult their financial advisors to make sure they are set up properly. Hospitalists who live in one state and work in another also need to beware of state and municipal tax guidelines.
One hidden cost of super-commuting is less time for household upkeep. Tony Venturato does not have the luxury of a week-on/week-off schedule, and with travel, his weekends are cut down to a day or a day and a half twice a month. That doesn’t leave much time for household chores and home improvement projects.
“The same way that you cannot run a project from the road, it’s also pretty hard to run a household from remote, and that puts a burden on your spouse,” he says. “That leaky faucet that might have been a small fix-it project? Now my wife has to find a plumber to come fix it. Do-it-yourself home improvement projects? Fuhgeddaboudit.”
Dr. Kerley nearly missed the birth of his first grandchild the first week he had agreed to work in Alaska. However, his state license to practice was delayed, so he was there for the important event. “After that, I realized that I did need to be more intentional about dates and scheduling,” he says. “Since then, the scheduling has become more rhythmic.”
Good Career Move?
Super-commuting adds to the bank account, widens travel experiences, and sharpens clinical skills. But does it work for career advancement? Dotson believes that working with various types of teams in different settings helps hospitalists mature quickly.
Venturato thinks that accepting long-distance assignments will become even more necessary for career-building. “There’s still the aggravation of flying,” he admits. “But the jobs you get, the opportunities that you have, make it all worthwhile. If you limit yourself to not going to these interesting projects, you’re limiting your career.”
Dotson seconds that notion. “If people are willing to do the traveling, and they are good people, there are lots of opportunities for them,” he says.
Gretchen Henkel is a freelance writer in Southern California.
References
- Pisarski, AE. Commuting in America III: The Third National Reporter on Commuting Patterns and Trends. 2006: Transportation Research Board of the National Academies; Washington, D.C.
- Sandow E. Till work do us part: The social fallacy of long-distance commuting [dissertation]. Available at: http://umu.diva-portal.org. Accessed June 22, 2011.
A “long commute” once meant 60 minutes of drive time or a long haul on public transit from the suburbs to city centers. That definition has changed quite a bit as the nation’s workforce becomes more mobile.
Take, for instance, hospitalist Yun Namkung, MD, who lives in Queens, N.Y., but works at Leflore Hospital, a 248-bed regional medical center in Greenwood, Miss., about 130 miles south of Memphis. “I’m something called a ‘firefighter’ within the company,” says Dr. Namkung, who’s been traveling long distances to work for his employer, Brentwood, Tenn.-based Cogent-HMG.
Dr. Namkung’s first long-distance commute was an interim assignment: He was an HMG program director in upstate New York anticipating a move to California. The move didn’t materialize, and now, after two years as a “super-commuter,” he says, “Traveling is actually fulfilling. You get to meet different people and supporting staff. You get exposed to a variety of patients, so clinically, you get better. I think I can continue to do this for a while.”
Super-commuters go by various names and monikers—“firefighters,” “travelers,” “vagabonds”—but they share a common reality: one or two weeks a month, and in some cases every week, they’re traveling long distances from home to work. And while it might not be for every hospitalist, this mega-commute phenomenon has pros and cons, hidden costs, and unexpected perks.

—Charles Barnett, MD, Knoxville, Tenn.
An Upward Trend?
Transportation policy consultant Alan E. Pisarski, author of “Commuting in America (Vols. 1-3),” often testifies before Congress on transportation issues for policy planning and investment requirements. The third volume of his “Commuting in America” series, published in 2006, found that the number of workers with commutes of more than 60 minutes increased almost 50% from 1990 to 2000.1 That duration probably rose even more following the economic downturn that began in 2008, he says, as the notion of an “acceptable” commute changes when the job market is tight.
The long-distance commuting trend is likely to increase, he says, because highly skilled workers (e.g. physicians) are in short supply. In our mobile society, he adds, “professionals are more willing to accept long distance separation from their families, on at least some kind of scheduled basis.”
In addition, as millions of baby boomers retire, replacing their skill sets is proving difficult. Companies are trying to hold boomers in the labor force longer, offering attractive perks so that they will stay.
Many jobs, even in a telecommuting society, still require in-person deliveries. And for some, super-commuting is a better alternative to relocation. For others, it might be the only alternative, given the poor housing market. That’s the way Anthony Venturato sees it.
“In my business, [we] have to be where the project is,” says Venturato, a project manager for passenger rail projects for STV Inc., a leading architectural, engineering, and construction management firm. “We have virtual meeting rooms, but we’ve got a long way to go before working closely together and being physically far away are equivalent—like that great scene in “Star Wars” where holograms of ‘attendees’ were interacting around a conference table. To run a project, at least in the early 21st century, you’ve gotta be there.” (see “Nomadic Lifestyle Works for Some,”)
—Yun Namkung, MD, Queens, N.Y.
Models Differ
Mark Dotson, vice president of recruiting at Cogent-HMG, says his company instituted a “travelers” model in October of 2009 to reduce its locum tenens usage. Travelers, he says, are hospitalists licensed in several states who can be placed in different programs, most within driving distance. Some request a remote location, such as one Cogent-HMG hospitalist who resides in Dallas and has been commuting to Great Falls, Tenn., for more two years.
Dotson explains that the company’s travelers “are not typical locums who may just say, ‘I’ll be here for two months and then I’m out of here.’ They are employed by us, get full benefits [plus a 10% premium over regular employees] and training from our academy,” he says. “They are looked upon as part of the team when we place them in a program, and not an interim solution.”
Travelers contribute to program stability and improved quality and productivity metrics, Dotson adds. In Great Falls, for instance, the hospitalist team, which includes a traveler on every rotation, has regularly met its quality performance measures and RVU requirements since being fully staffed. Dotson estimates that 10% of the hospitalists hired by Cogent-HMG last year were travelers, and he’d like to see that percentage grow to 25% to meet increasing demand.
EmCare Inpatient Services in Dallas takes a different approach. They use super-commuters only for short-term startups, says CEO Mark Hamm, who’s “never been an advocate of flying people in and out. You don’t ever get the continuity that you need within the practice.”
To establish trust with referring primary-care physicians (PCPs), hospitalist programs need to comprise 80% to 90% of residential hospitalists, he says. Otherwise, EmCare becomes “just a staffing company and not a partner” with client hospitals. This is especially essential when it comes to hiring medical directors, he says, who must be present for meetings and administering program operations.
A Good Fit
So who are the super-commuter hospitalists? Dotson, of Cogent-HMG, says that the majority of those willing to travel tend to be single. Hospitalists who are in between residency and starting a fellowship find this type of assignment provides consistent scheduling, income, and benefits to them and their families. Another contingent: mature career hospitalists with grown children.
Eric Kerley, MD, FAAP, FACP lives and works primarily in eastern Tennessee, where he is a full-time medical director. He saw his friend and colleague Charles Barnett, MD, taking assignments in Wyoming, and thought traveling for work “sounded interesting.”
“I’m a Southern boy who has lived my entire life between Orlando [Fla.], Tennessee, and Texas,” he says, “so I picked my locations based on places I would want to go.”
Dr. Kerley’s first yearlong assignment, in 2009-2010, was in central Alaska at a 75-bed facility. He worked as a nocturnist. “To see minus-20-degree Fahrenheit temperatures and frozen rivers, and days that are 22 hours long, that was pretty amazing,” he says. Being away for one week a month is really not much different than a week of day shifts at home, he adds.
Dr. Barnett began super-commuting four years ago from his home in Knoxville, Tenn., to Gillette, Wyo. Traveling to Wyoming is his regular commuter gig—he stays at the hospital—and he enjoys working in another environment.
The away time also works for his marriage, he says. “Just before I leave for an assignment, my wife’s ready to see me go,” he says. “And then, when I come home, she’s anxious for me to be there, so it’s sort of like a honeymoon once a month for both of us.”
Continued below...
Pros and Cons
Although he misses his family when he’s traveling, Dr. Namkung now spends more quality time with them, “because I realize how precious that time is.” His wife, a pharmacist, makes it a point to take time off when he’s home, and they do more things together as a family.
Another bonus: “I meet different docs, nursing staffs, and administrators,” Dr. Namkung says. “Since I’m here alone, we have the chance to have dinner together and spend time. In that way, I bond with a lot more people than I would normally if I stayed in one place.”
Dr. Kerley racked up the frequent-flier miles during his one-year assignment to Alaska, which was a plus when it came to financing family vacations.
Working in other states entails meeting state-specific licensing requirements. Some companies, such as Cogent-HMG, pay the costs of obtaining those state licenses. Others do not, and the paperwork, says Dr. Barnett, can be “a nightmare.” Locum Leaders CEO Will Drescher, MD, says his company pays for licenses in some states and assists with paperwork in others.

—Eric Kerley, MD, medical director, Morristown, Tenn, nocturnist, PeaceHealth Medical Group, Ketchikan, Ak.
Unless hospitalists are full-time employees of the organization, such as Dr. Namkung with Cogent-HMG, their income likely will be considered independent contracting by the IRS. That means you’ll be filing an extra form (1099) with your return, and you may have to pay quarterly estimated self-employment tax. Hospitalists are encouraged to consult their financial advisors to make sure they are set up properly. Hospitalists who live in one state and work in another also need to beware of state and municipal tax guidelines.
One hidden cost of super-commuting is less time for household upkeep. Tony Venturato does not have the luxury of a week-on/week-off schedule, and with travel, his weekends are cut down to a day or a day and a half twice a month. That doesn’t leave much time for household chores and home improvement projects.
“The same way that you cannot run a project from the road, it’s also pretty hard to run a household from remote, and that puts a burden on your spouse,” he says. “That leaky faucet that might have been a small fix-it project? Now my wife has to find a plumber to come fix it. Do-it-yourself home improvement projects? Fuhgeddaboudit.”
Dr. Kerley nearly missed the birth of his first grandchild the first week he had agreed to work in Alaska. However, his state license to practice was delayed, so he was there for the important event. “After that, I realized that I did need to be more intentional about dates and scheduling,” he says. “Since then, the scheduling has become more rhythmic.”
Good Career Move?
Super-commuting adds to the bank account, widens travel experiences, and sharpens clinical skills. But does it work for career advancement? Dotson believes that working with various types of teams in different settings helps hospitalists mature quickly.
Venturato thinks that accepting long-distance assignments will become even more necessary for career-building. “There’s still the aggravation of flying,” he admits. “But the jobs you get, the opportunities that you have, make it all worthwhile. If you limit yourself to not going to these interesting projects, you’re limiting your career.”
Dotson seconds that notion. “If people are willing to do the traveling, and they are good people, there are lots of opportunities for them,” he says.
Gretchen Henkel is a freelance writer in Southern California.
References
- Pisarski, AE. Commuting in America III: The Third National Reporter on Commuting Patterns and Trends. 2006: Transportation Research Board of the National Academies; Washington, D.C.
- Sandow E. Till work do us part: The social fallacy of long-distance commuting [dissertation]. Available at: http://umu.diva-portal.org. Accessed June 22, 2011.
A “long commute” once meant 60 minutes of drive time or a long haul on public transit from the suburbs to city centers. That definition has changed quite a bit as the nation’s workforce becomes more mobile.
Take, for instance, hospitalist Yun Namkung, MD, who lives in Queens, N.Y., but works at Leflore Hospital, a 248-bed regional medical center in Greenwood, Miss., about 130 miles south of Memphis. “I’m something called a ‘firefighter’ within the company,” says Dr. Namkung, who’s been traveling long distances to work for his employer, Brentwood, Tenn.-based Cogent-HMG.
Dr. Namkung’s first long-distance commute was an interim assignment: He was an HMG program director in upstate New York anticipating a move to California. The move didn’t materialize, and now, after two years as a “super-commuter,” he says, “Traveling is actually fulfilling. You get to meet different people and supporting staff. You get exposed to a variety of patients, so clinically, you get better. I think I can continue to do this for a while.”
Super-commuters go by various names and monikers—“firefighters,” “travelers,” “vagabonds”—but they share a common reality: one or two weeks a month, and in some cases every week, they’re traveling long distances from home to work. And while it might not be for every hospitalist, this mega-commute phenomenon has pros and cons, hidden costs, and unexpected perks.

—Charles Barnett, MD, Knoxville, Tenn.
An Upward Trend?
Transportation policy consultant Alan E. Pisarski, author of “Commuting in America (Vols. 1-3),” often testifies before Congress on transportation issues for policy planning and investment requirements. The third volume of his “Commuting in America” series, published in 2006, found that the number of workers with commutes of more than 60 minutes increased almost 50% from 1990 to 2000.1 That duration probably rose even more following the economic downturn that began in 2008, he says, as the notion of an “acceptable” commute changes when the job market is tight.
The long-distance commuting trend is likely to increase, he says, because highly skilled workers (e.g. physicians) are in short supply. In our mobile society, he adds, “professionals are more willing to accept long distance separation from their families, on at least some kind of scheduled basis.”
In addition, as millions of baby boomers retire, replacing their skill sets is proving difficult. Companies are trying to hold boomers in the labor force longer, offering attractive perks so that they will stay.
Many jobs, even in a telecommuting society, still require in-person deliveries. And for some, super-commuting is a better alternative to relocation. For others, it might be the only alternative, given the poor housing market. That’s the way Anthony Venturato sees it.
“In my business, [we] have to be where the project is,” says Venturato, a project manager for passenger rail projects for STV Inc., a leading architectural, engineering, and construction management firm. “We have virtual meeting rooms, but we’ve got a long way to go before working closely together and being physically far away are equivalent—like that great scene in “Star Wars” where holograms of ‘attendees’ were interacting around a conference table. To run a project, at least in the early 21st century, you’ve gotta be there.” (see “Nomadic Lifestyle Works for Some,”)
—Yun Namkung, MD, Queens, N.Y.
Models Differ
Mark Dotson, vice president of recruiting at Cogent-HMG, says his company instituted a “travelers” model in October of 2009 to reduce its locum tenens usage. Travelers, he says, are hospitalists licensed in several states who can be placed in different programs, most within driving distance. Some request a remote location, such as one Cogent-HMG hospitalist who resides in Dallas and has been commuting to Great Falls, Tenn., for more two years.
Dotson explains that the company’s travelers “are not typical locums who may just say, ‘I’ll be here for two months and then I’m out of here.’ They are employed by us, get full benefits [plus a 10% premium over regular employees] and training from our academy,” he says. “They are looked upon as part of the team when we place them in a program, and not an interim solution.”
Travelers contribute to program stability and improved quality and productivity metrics, Dotson adds. In Great Falls, for instance, the hospitalist team, which includes a traveler on every rotation, has regularly met its quality performance measures and RVU requirements since being fully staffed. Dotson estimates that 10% of the hospitalists hired by Cogent-HMG last year were travelers, and he’d like to see that percentage grow to 25% to meet increasing demand.
EmCare Inpatient Services in Dallas takes a different approach. They use super-commuters only for short-term startups, says CEO Mark Hamm, who’s “never been an advocate of flying people in and out. You don’t ever get the continuity that you need within the practice.”
To establish trust with referring primary-care physicians (PCPs), hospitalist programs need to comprise 80% to 90% of residential hospitalists, he says. Otherwise, EmCare becomes “just a staffing company and not a partner” with client hospitals. This is especially essential when it comes to hiring medical directors, he says, who must be present for meetings and administering program operations.
A Good Fit
So who are the super-commuter hospitalists? Dotson, of Cogent-HMG, says that the majority of those willing to travel tend to be single. Hospitalists who are in between residency and starting a fellowship find this type of assignment provides consistent scheduling, income, and benefits to them and their families. Another contingent: mature career hospitalists with grown children.
Eric Kerley, MD, FAAP, FACP lives and works primarily in eastern Tennessee, where he is a full-time medical director. He saw his friend and colleague Charles Barnett, MD, taking assignments in Wyoming, and thought traveling for work “sounded interesting.”
“I’m a Southern boy who has lived my entire life between Orlando [Fla.], Tennessee, and Texas,” he says, “so I picked my locations based on places I would want to go.”
Dr. Kerley’s first yearlong assignment, in 2009-2010, was in central Alaska at a 75-bed facility. He worked as a nocturnist. “To see minus-20-degree Fahrenheit temperatures and frozen rivers, and days that are 22 hours long, that was pretty amazing,” he says. Being away for one week a month is really not much different than a week of day shifts at home, he adds.
Dr. Barnett began super-commuting four years ago from his home in Knoxville, Tenn., to Gillette, Wyo. Traveling to Wyoming is his regular commuter gig—he stays at the hospital—and he enjoys working in another environment.
The away time also works for his marriage, he says. “Just before I leave for an assignment, my wife’s ready to see me go,” he says. “And then, when I come home, she’s anxious for me to be there, so it’s sort of like a honeymoon once a month for both of us.”
Continued below...
Pros and Cons
Although he misses his family when he’s traveling, Dr. Namkung now spends more quality time with them, “because I realize how precious that time is.” His wife, a pharmacist, makes it a point to take time off when he’s home, and they do more things together as a family.
Another bonus: “I meet different docs, nursing staffs, and administrators,” Dr. Namkung says. “Since I’m here alone, we have the chance to have dinner together and spend time. In that way, I bond with a lot more people than I would normally if I stayed in one place.”
Dr. Kerley racked up the frequent-flier miles during his one-year assignment to Alaska, which was a plus when it came to financing family vacations.
Working in other states entails meeting state-specific licensing requirements. Some companies, such as Cogent-HMG, pay the costs of obtaining those state licenses. Others do not, and the paperwork, says Dr. Barnett, can be “a nightmare.” Locum Leaders CEO Will Drescher, MD, says his company pays for licenses in some states and assists with paperwork in others.

—Eric Kerley, MD, medical director, Morristown, Tenn, nocturnist, PeaceHealth Medical Group, Ketchikan, Ak.
Unless hospitalists are full-time employees of the organization, such as Dr. Namkung with Cogent-HMG, their income likely will be considered independent contracting by the IRS. That means you’ll be filing an extra form (1099) with your return, and you may have to pay quarterly estimated self-employment tax. Hospitalists are encouraged to consult their financial advisors to make sure they are set up properly. Hospitalists who live in one state and work in another also need to beware of state and municipal tax guidelines.
One hidden cost of super-commuting is less time for household upkeep. Tony Venturato does not have the luxury of a week-on/week-off schedule, and with travel, his weekends are cut down to a day or a day and a half twice a month. That doesn’t leave much time for household chores and home improvement projects.
“The same way that you cannot run a project from the road, it’s also pretty hard to run a household from remote, and that puts a burden on your spouse,” he says. “That leaky faucet that might have been a small fix-it project? Now my wife has to find a plumber to come fix it. Do-it-yourself home improvement projects? Fuhgeddaboudit.”
Dr. Kerley nearly missed the birth of his first grandchild the first week he had agreed to work in Alaska. However, his state license to practice was delayed, so he was there for the important event. “After that, I realized that I did need to be more intentional about dates and scheduling,” he says. “Since then, the scheduling has become more rhythmic.”
Good Career Move?
Super-commuting adds to the bank account, widens travel experiences, and sharpens clinical skills. But does it work for career advancement? Dotson believes that working with various types of teams in different settings helps hospitalists mature quickly.
Venturato thinks that accepting long-distance assignments will become even more necessary for career-building. “There’s still the aggravation of flying,” he admits. “But the jobs you get, the opportunities that you have, make it all worthwhile. If you limit yourself to not going to these interesting projects, you’re limiting your career.”
Dotson seconds that notion. “If people are willing to do the traveling, and they are good people, there are lots of opportunities for them,” he says.
Gretchen Henkel is a freelance writer in Southern California.
References
- Pisarski, AE. Commuting in America III: The Third National Reporter on Commuting Patterns and Trends. 2006: Transportation Research Board of the National Academies; Washington, D.C.
- Sandow E. Till work do us part: The social fallacy of long-distance commuting [dissertation]. Available at: http://umu.diva-portal.org. Accessed June 22, 2011.