User login
The emotionally exhausted physician
CASE ‘I’m stuck’
Dr. D, age 48, an internist practicing general medicine who is a married mother of 2 teenagers, presents with emotional exhaustion. Her medical history is unremarkable other than hyperlipidemia controlled by diet. She describes an episode of reactive depressive symptoms and anxiety when in college, which was related to the stress of final exams, finances, and the dissolution of a long-standing relationship. Regardless, she functioned well and graduated summa cum laude. She says her current feelings of being “stuck” have gradually increased during the past 3 to 4 years. Although she describes being mildly anxious and dysphoric, she also said she feels like her “wheels are spinning” and that she doesn’t even seem to care. Dr. D had been a high achiever, yet says she feels like she isn’t getting anywhere at work or at home.
[polldaddy:10064977]
The authors’ observations
As psychiatrists in the business of diagnosis and treatment, we immediately considered common diagnoses, such as major depressive disorder and persistent depressive disorder. However, despite our training in pathology, we believe patients should be considered well until proven sick. This paradigm shift is in line with the definition of mental health per the World Health Organization: “A state of well-being in which every individual realizes his or her own potential, can cope with the normal stresses of life, can work productively and fruitfully, and is able to make a contribution to her or his community.”1
In Dr. D’s case, there was not enough information yet to fully support any of the diagnoses. She did not exhibit enough depressive symptoms to support a diagnosis of a depressive disorder. She said that she didn’t feel like she was getting anywhere at work or home. Yet there was no objective information that suggested impairment in functioning, which would preclude a diagnosis of adjustment disorder. At this point, we would support the “V code” diagnosis of phase of life problem, or even what is rarely seen in a psychiatric evaluation: “no diagnosis.”
EVALUATION Is work the problem?
We diligently conduct a thorough review of systems with Dr. D and confirm there is not enough information to diagnose a depressive disorder, anxiety disorder, or other psychiatric disorder. Collateral history suggests her teenagers are well-adjusted and doing well in high school, and she is well-respected at work with reportedly excellent performance ratings. We identify strongly with her and her situation.
Dr. D admits she is an idealist and half-jokingly says she entered into medicine “to save the world.” Yet she laments the long hours and finding herself mired in paperwork. She is barely making it to her kids’ school events and says she can’t believe her first child will be graduating within a year. She has had some particularly challenging patients recently, and although she is still diligent about their care, she is shocked she doesn’t seem to care as much about “solving the medical puzzle.” This came to light for her when a longtime patient observed that Dr. D didn’t seem herself and asked, “Are you all right, Doc?”
Dr. D is professionally dressed and has excellent grooming and hygiene. She looks tired, yet has a full affect, a witty conversational style, and responds appropriately to humor.
[polldaddy:10064980]
The authors’ observations
It can be difficult to know what to do next when there isn’t an established “playbook” for a problem without a diagnosis. We realized Dr. D was describing burnout, a syndrome of depersonalization (detached and not caring, to the point of viewing people as objects), emotional exhaustion, and low personal accomplishment that leads to decreased effectiveness at work.2 DSM-5 does not include “burnout” as a diagnosis3; however, if symptoms evolve to the point where they affect occupational or social functioning, burnout can be similar to adjustment disorder. Treatment with an antidepressant medication is not appropriate. It is possible that CBT might be helpful for many patients, yet there is no evidence that Dr. D has any cognitive distortions. Although we already had some collateral information, it is never wrong to gather additional collateral. However, because burnout is common, we may not need additional information. We could reassure her and send her on her way, but we want to add therapeutic value. We advocated exploring issues in her life and work related to meaning.
Continue to: Physician burnout
Physician burnout
Burnout is an alarmingly common problem among physicians that affects approximately half of psychiatrists. In 2014, 54.4% of physicians, and slightly less than 50% of psychiatrists, had at least 1 symptom of burnout.4 This was up from the 45.5% of physicians and a little more than 40% of psychiatrists who reported burnout in 2011,4 which suggests that as medicine continues to change, doctors may increasingly feel the brunt of this change. The rate of burnout is highest in front-line specialties (family medicine, general internal medicine, and emergency medicine) and lowest in preventive medicine.5 Physician burnout leads to real-world occupational issues, such as medical errors, poor relationships with coworkers and patients, decreased patient satisfaction, and medical malpractice suits.6,7
Even though burnout is clearly a concern for our colleagues, don’t expect them to proactively line up outside our offices. In a survey of 7,197 surgeons, 86.6% of respondents answered it was not important that “I have regular meetings with a psychologist/psychiatrist to discuss stress.”8 At the same time, the idea of meeting with a psychologist/psychiatrist was rated more highly by surgeons who were burnt out and found to be a factor independently associated with burnout.8 Perhaps we have some work to do in marketing our services in a way that welcomes our colleagues.
Although physician burnout has been a focus of recent studies, burnout in general has been studied for decades in other working populations. There are 2 useful models describing burnout:
- The job demand-control(-support) model suggests that individuals experience strain and subsequent ill effects when the demands of their job exceed the control they have,9 and social support from supervisors and colleagues can buffer the harmful effects of job strain.10
- The effort-reward imbalance model suggests that high-effort, low-reward occupational conditions are particularly stressful.11
Both models are simple, intuitive, and suggest solutions.
When engaging your physician colleagues about their burnout, remember that physicians are people, too, and have the same difficulties that everyone else does in successfully practicing healthy behaviors. As physicians, we have significant demands on our time that make it difficult to control our ability to eat, sleep, and exercise. In general, the food available where we work is not nutritious,12 half of us are overweight or obese,13 and working more than 40 hours per week increases the likelihood we’ll have a higher body mass index.14 We don’t sleep well, either—we get less sleep than the general population,15 and more sleep equates to less burnout.16 Regarding exercise, doctors who cannot prioritize exercise tend to have more burnout.17
Continue to: When evaluating a physician colleague for symptoms of burnout...
When evaluating a physician colleague for symptoms of burnout, start by assessing the basics: eating, sleeping, and moving. In Dr. D’s case, this also included taking a quick inventory of what demands were on her proverbial plate. Taking inventory of these demands (ie, demand-control[-support] model) may lead to new insights about what she can control. Prioritization is important to determine where efforts go (ie, effort-reward imbalance model). This is where your skills as a psychiatrist can especially help, as you explore values and bring trade-offs to light.
EVALUATION Permission not to be perfect
As we interview Dr. D, we realize she has some obsessive-compulsive personality traits that are mostly self-serving. She places a high value on being thorough and having elegant clinical notes. Yet this value competes with her desire to be efficient and get home on time to see her kids’ school events. You point this out to her and see if she can come up with some solutions. You also discuss with Dr. D the tension everyone feels between valuing career and valuing family and friends. You normalize her situation, and give her permission to pick something about which she will allow herself not to be perfect.
[polldaddy:10064981]
The authors’ observations
Since perfectionism is a common trait among physicians,18 failure doesn’t seem to be compatible with their DNA. We encourage other physicians to be scientific about their own lives, just as they are in the profession they have chosen. Physicians can delude themselves into thinking they can have it all, not recognizing that every choice has its cost. For example, a physician who decides that it’s okay to publish one fewer research paper this year might have more time to enjoy spending time with his or her children. In our work with physicians, we strive to normalize their experiences, helping them reframe their perfectionistic viewpoint to recognize that everyone struggles with work-life balance issues. We validate that physicians have difficult choices to make in finding what works for them, and we challenge and support them in exploring these choices.
Choosing where to put one’s efforts is also contingent upon the expected rewards. Sometime before the daily grind of our careers in medicine started, we had strong visions of what such careers would mean to us. We visualized the ideal of helping people and making a difference. Then, at some point, many of us took this for granted and forgot about the intrinsic rewards of our work. In a 2014-2015 survey of U.S. physicians across all specialties, only 64.6% of respondents who were highly burned out said they found their work personally rewarding. This is a sharp contrast to the 97.5% of respondents who were not burned out who reported that they found their work personally rewarding.19
As psychiatrists, we can challenge our physician colleagues to dare to dream again. We can help them rediscover the rewarding aspects of their work (ie, per effort-reward imbalance model) that drew them into medicine in the first place. This may include exploring their future legacy. How do they want to be remembered at retirement? Such consideration is linked to mental simulation and meaning in their lives.20 We guide our colleagues to reframe their current situation to see the myriad of choices they have based upon their own specific value system. If family and friends are currently taking priority over work, it also helps to reframe that working allows us to make a good living so we can fully enjoy that time spent with family and friends.
Continue to: If we do our jobs well...
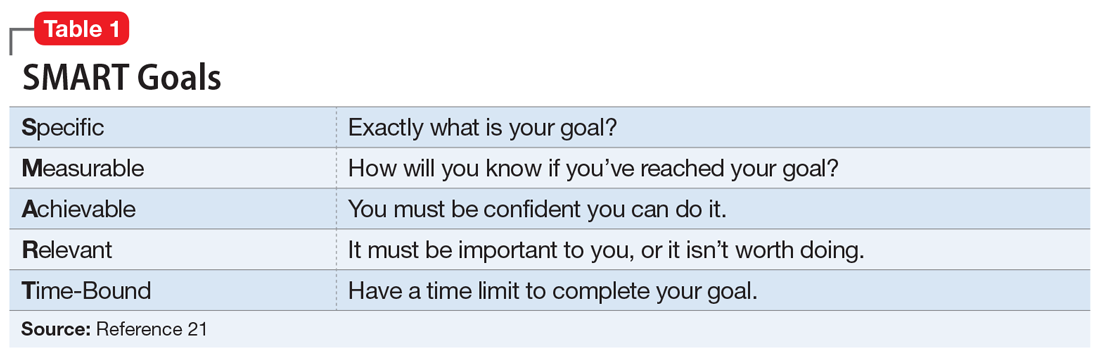
If we do our jobs well, the next part is easy. We have them set specific short- and long-term goals related to their situation. This is something we do every day in our practices. It may help to make sure we’re using SMART (Specific, Measurable, Achievable, Relevant, Time-Bound), a well-known mnemonic used for goals (Table 121), and brush up on our motivational interviewing skills (see Related Resources). It is especially important to make sure our colleagues have goals that are relevant—the “R” in the SMART mnemonic—to their situation.
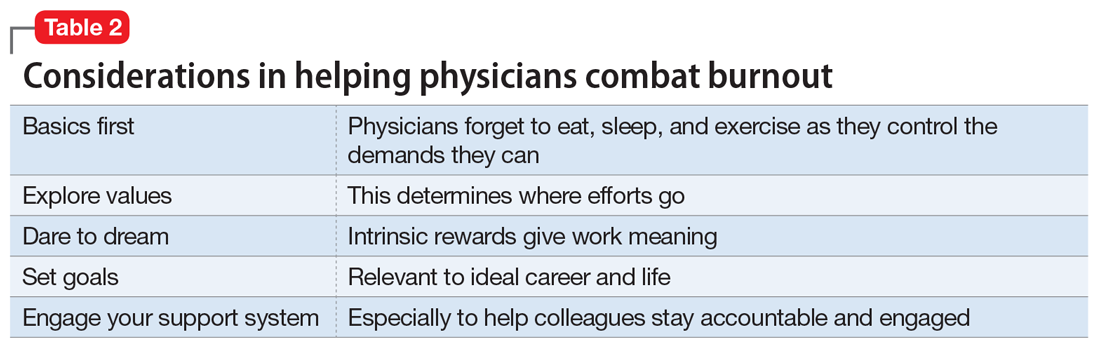
Finally, we do a better job of reaching our goals and engaging more at work and at home when we have good social support. For physicians, co-worker support has been found to be directly related to our well-being as well as buffering the negative effects of work demands.22 Furthermore, our colleagues are the most acceptable sources of support when we are faced with stressful situations.23 Thus, as psychiatrists, we can doubly help our physician patients by providing collegial support and doing our usual job of holding them accountable to their goals (Table 2).
OUTCOME Goal-setting, priorities, accountability
As we’re exploring goals with Dr. D, she makes a conscious decision to spend less time on documentation and start focusing on being present with her patients. She returns in 1 month to tell you time management is still a struggle, but her visit with you was instrumental in making her realize how important it was to get home on time for her kids’ activities. She says it greatly helped that you kept her accountable, yet also validated her struggles and gave her permission to design her life within the constraints of her situation and without the burden of having to be perfect at everything.
Bottom Line
We can best help our physician colleagues who are experiencing burnout by shifting our paradigm to a wellness model that focuses on helping them reach their potential and balance their professional and personal lives.
Related Resources
- Balch CM, Shanafelt TD. Combating stress and burnout in surgical practice: a review. Thorac Surg Clin. 2011;21(3):417-430.
- Miller WR, Rollnick S. Motivational interviewing: preparing people for change, 2nd ed. New York, NY: The Guilford Press; 2002.
- Stanford Medicine WellMD. Stress & Burnout. https://wellmd.stanford.edu.
1. World Health Organization. Mental health: a state of well-being. http://www.who.int/features/factfiles/mental_health/en/. Updated August 2014. Accessed March 17, 2017.
2. Maslach C, Jackson S, Leiter M. Maslach burnout inventory manual, 3rd ed. Palo Alto, CA: Consulting Psychologists Press; 1996.
3. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013.
4. Shanafelt TD, Hasan O, Dyrbye LN, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin Proc. 2015;90(12):1600-1613.
5. Shanafelt TD, Boone S, Tan L, et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med. 2012;172(18):1377-1385.
6. Shanafelt TD, Sloan JA, Habermann TM. The well-being of physicians. Am J Med. 2003;114(6):513-519.
7. Balch CM, Shanafelt TD. Combating stress and burnout in surgical practice: a review. Adv Surg. 2010;44:29-47.
8. Shanafelt TD, Oreskovich MR, Dyrbye LN, et al. Avoiding burnout: the personal health habits and wellness practices of US Surgeons. Ann Surg. 2012;255(4):625-633.
9. Karasek RA Jr. Job demands, job decision latitude, and mental strain: implications for job redesign. Adm Sci Q. 1979;24(2):285-308.
10. Johnson JV. Collective control: strategies for survival in the workplace. Int J Health Serv. 1989;19(3):469-480.
11. Siegrist J. Adverse health effects of high-effort/low-reward conditions. J Occup Health Psychol. 1996;1(1):27-41.
12. Lesser LI, Cohen DA, Brook RH. Changing eating habits for the medical profession. JAMA. 2012;308(10):983-984.
13. Bleich SN, Bennett WL, Gudzune KA, et al. Impact of physician BMI on obesity care and beliefs. Obesity (Silver Spring). 2012;20(5):999-1005.
14. Stanford FC, Durkin MW, Blair SN, et al. Determining levels of physical activity in attending physicians, resident and fellow physicians, and medical students in the USA. Br J Sports Med. 2012;46(5):360-364.
15. Tucker P, Bejerot E, Kecklund G, et al. Stress Research Institute at Stockholm University. Stress Research Report-doctors’ work hours in Sweden: their impact on sleep, health, work-family balance, patient care and thoughts about work. https://www.stressforskning.su.se/polopoly_fs/1.233341.1429526778!/menu/standard/file/sfr325.pdf. Accessed March 17, 2017.
16. Wisetborisut A, Angkurawaranon C, Jiraporncharoen W, et al. Shift work and burnout among health care workers. Occup Med (Lond). 2014;64(4):279-286.
17. Eckleberry-Hunt J, Lick D, Boura J, et al. An exploratory study of resident burnout and wellness. Acad Med. 2009;84(2):269-277.
18. Peters M, King J. Perfectionism in doctors. BMJ. 2012;344:e1674. doi: https://doi.org/10.1136/bmj.e1674.
19. Jager AJ, Tutty MA, Kao AC. Association between physician burnout and identification with medicine as a calling. Mayo Clin Proc. 2017;92(3):415-422.
20. Waytz A, Hershfield HE, Tamir DI. Neural and behavioral evidence for the role of mental simulation in meaning in life. J Pers Soc Psychol. 2015;108(2):336-355.
21. SMART Criteria. https://en.wikipedia.org/wiki/SMART_criteria. Accessed March 17, 2017.
22. Hu YY, Fix ML, Hevelone ND, et al. Physicians’ needs in coping with emotional stressors: the case for peer support. Arch Surg. 2012;147(3):212-217.
23. Wallace JE, Lemaire J. On physician well being–you’ll get by with a little help from your friends. Soc Sci Med. 2007;64(12):2565-2577.
CASE ‘I’m stuck’
Dr. D, age 48, an internist practicing general medicine who is a married mother of 2 teenagers, presents with emotional exhaustion. Her medical history is unremarkable other than hyperlipidemia controlled by diet. She describes an episode of reactive depressive symptoms and anxiety when in college, which was related to the stress of final exams, finances, and the dissolution of a long-standing relationship. Regardless, she functioned well and graduated summa cum laude. She says her current feelings of being “stuck” have gradually increased during the past 3 to 4 years. Although she describes being mildly anxious and dysphoric, she also said she feels like her “wheels are spinning” and that she doesn’t even seem to care. Dr. D had been a high achiever, yet says she feels like she isn’t getting anywhere at work or at home.
[polldaddy:10064977]
The authors’ observations
As psychiatrists in the business of diagnosis and treatment, we immediately considered common diagnoses, such as major depressive disorder and persistent depressive disorder. However, despite our training in pathology, we believe patients should be considered well until proven sick. This paradigm shift is in line with the definition of mental health per the World Health Organization: “A state of well-being in which every individual realizes his or her own potential, can cope with the normal stresses of life, can work productively and fruitfully, and is able to make a contribution to her or his community.”1
In Dr. D’s case, there was not enough information yet to fully support any of the diagnoses. She did not exhibit enough depressive symptoms to support a diagnosis of a depressive disorder. She said that she didn’t feel like she was getting anywhere at work or home. Yet there was no objective information that suggested impairment in functioning, which would preclude a diagnosis of adjustment disorder. At this point, we would support the “V code” diagnosis of phase of life problem, or even what is rarely seen in a psychiatric evaluation: “no diagnosis.”
EVALUATION Is work the problem?
We diligently conduct a thorough review of systems with Dr. D and confirm there is not enough information to diagnose a depressive disorder, anxiety disorder, or other psychiatric disorder. Collateral history suggests her teenagers are well-adjusted and doing well in high school, and she is well-respected at work with reportedly excellent performance ratings. We identify strongly with her and her situation.
Dr. D admits she is an idealist and half-jokingly says she entered into medicine “to save the world.” Yet she laments the long hours and finding herself mired in paperwork. She is barely making it to her kids’ school events and says she can’t believe her first child will be graduating within a year. She has had some particularly challenging patients recently, and although she is still diligent about their care, she is shocked she doesn’t seem to care as much about “solving the medical puzzle.” This came to light for her when a longtime patient observed that Dr. D didn’t seem herself and asked, “Are you all right, Doc?”
Dr. D is professionally dressed and has excellent grooming and hygiene. She looks tired, yet has a full affect, a witty conversational style, and responds appropriately to humor.
[polldaddy:10064980]
The authors’ observations
It can be difficult to know what to do next when there isn’t an established “playbook” for a problem without a diagnosis. We realized Dr. D was describing burnout, a syndrome of depersonalization (detached and not caring, to the point of viewing people as objects), emotional exhaustion, and low personal accomplishment that leads to decreased effectiveness at work.2 DSM-5 does not include “burnout” as a diagnosis3; however, if symptoms evolve to the point where they affect occupational or social functioning, burnout can be similar to adjustment disorder. Treatment with an antidepressant medication is not appropriate. It is possible that CBT might be helpful for many patients, yet there is no evidence that Dr. D has any cognitive distortions. Although we already had some collateral information, it is never wrong to gather additional collateral. However, because burnout is common, we may not need additional information. We could reassure her and send her on her way, but we want to add therapeutic value. We advocated exploring issues in her life and work related to meaning.
Continue to: Physician burnout
Physician burnout
Burnout is an alarmingly common problem among physicians that affects approximately half of psychiatrists. In 2014, 54.4% of physicians, and slightly less than 50% of psychiatrists, had at least 1 symptom of burnout.4 This was up from the 45.5% of physicians and a little more than 40% of psychiatrists who reported burnout in 2011,4 which suggests that as medicine continues to change, doctors may increasingly feel the brunt of this change. The rate of burnout is highest in front-line specialties (family medicine, general internal medicine, and emergency medicine) and lowest in preventive medicine.5 Physician burnout leads to real-world occupational issues, such as medical errors, poor relationships with coworkers and patients, decreased patient satisfaction, and medical malpractice suits.6,7
Even though burnout is clearly a concern for our colleagues, don’t expect them to proactively line up outside our offices. In a survey of 7,197 surgeons, 86.6% of respondents answered it was not important that “I have regular meetings with a psychologist/psychiatrist to discuss stress.”8 At the same time, the idea of meeting with a psychologist/psychiatrist was rated more highly by surgeons who were burnt out and found to be a factor independently associated with burnout.8 Perhaps we have some work to do in marketing our services in a way that welcomes our colleagues.
Although physician burnout has been a focus of recent studies, burnout in general has been studied for decades in other working populations. There are 2 useful models describing burnout:
- The job demand-control(-support) model suggests that individuals experience strain and subsequent ill effects when the demands of their job exceed the control they have,9 and social support from supervisors and colleagues can buffer the harmful effects of job strain.10
- The effort-reward imbalance model suggests that high-effort, low-reward occupational conditions are particularly stressful.11
Both models are simple, intuitive, and suggest solutions.
When engaging your physician colleagues about their burnout, remember that physicians are people, too, and have the same difficulties that everyone else does in successfully practicing healthy behaviors. As physicians, we have significant demands on our time that make it difficult to control our ability to eat, sleep, and exercise. In general, the food available where we work is not nutritious,12 half of us are overweight or obese,13 and working more than 40 hours per week increases the likelihood we’ll have a higher body mass index.14 We don’t sleep well, either—we get less sleep than the general population,15 and more sleep equates to less burnout.16 Regarding exercise, doctors who cannot prioritize exercise tend to have more burnout.17
Continue to: When evaluating a physician colleague for symptoms of burnout...
When evaluating a physician colleague for symptoms of burnout, start by assessing the basics: eating, sleeping, and moving. In Dr. D’s case, this also included taking a quick inventory of what demands were on her proverbial plate. Taking inventory of these demands (ie, demand-control[-support] model) may lead to new insights about what she can control. Prioritization is important to determine where efforts go (ie, effort-reward imbalance model). This is where your skills as a psychiatrist can especially help, as you explore values and bring trade-offs to light.
EVALUATION Permission not to be perfect
As we interview Dr. D, we realize she has some obsessive-compulsive personality traits that are mostly self-serving. She places a high value on being thorough and having elegant clinical notes. Yet this value competes with her desire to be efficient and get home on time to see her kids’ school events. You point this out to her and see if she can come up with some solutions. You also discuss with Dr. D the tension everyone feels between valuing career and valuing family and friends. You normalize her situation, and give her permission to pick something about which she will allow herself not to be perfect.
[polldaddy:10064981]
The authors’ observations
Since perfectionism is a common trait among physicians,18 failure doesn’t seem to be compatible with their DNA. We encourage other physicians to be scientific about their own lives, just as they are in the profession they have chosen. Physicians can delude themselves into thinking they can have it all, not recognizing that every choice has its cost. For example, a physician who decides that it’s okay to publish one fewer research paper this year might have more time to enjoy spending time with his or her children. In our work with physicians, we strive to normalize their experiences, helping them reframe their perfectionistic viewpoint to recognize that everyone struggles with work-life balance issues. We validate that physicians have difficult choices to make in finding what works for them, and we challenge and support them in exploring these choices.
Choosing where to put one’s efforts is also contingent upon the expected rewards. Sometime before the daily grind of our careers in medicine started, we had strong visions of what such careers would mean to us. We visualized the ideal of helping people and making a difference. Then, at some point, many of us took this for granted and forgot about the intrinsic rewards of our work. In a 2014-2015 survey of U.S. physicians across all specialties, only 64.6% of respondents who were highly burned out said they found their work personally rewarding. This is a sharp contrast to the 97.5% of respondents who were not burned out who reported that they found their work personally rewarding.19
As psychiatrists, we can challenge our physician colleagues to dare to dream again. We can help them rediscover the rewarding aspects of their work (ie, per effort-reward imbalance model) that drew them into medicine in the first place. This may include exploring their future legacy. How do they want to be remembered at retirement? Such consideration is linked to mental simulation and meaning in their lives.20 We guide our colleagues to reframe their current situation to see the myriad of choices they have based upon their own specific value system. If family and friends are currently taking priority over work, it also helps to reframe that working allows us to make a good living so we can fully enjoy that time spent with family and friends.
Continue to: If we do our jobs well...
If we do our jobs well, the next part is easy. We have them set specific short- and long-term goals related to their situation. This is something we do every day in our practices. It may help to make sure we’re using SMART (Specific, Measurable, Achievable, Relevant, Time-Bound), a well-known mnemonic used for goals (Table 121), and brush up on our motivational interviewing skills (see Related Resources). It is especially important to make sure our colleagues have goals that are relevant—the “R” in the SMART mnemonic—to their situation.
Finally, we do a better job of reaching our goals and engaging more at work and at home when we have good social support. For physicians, co-worker support has been found to be directly related to our well-being as well as buffering the negative effects of work demands.22 Furthermore, our colleagues are the most acceptable sources of support when we are faced with stressful situations.23 Thus, as psychiatrists, we can doubly help our physician patients by providing collegial support and doing our usual job of holding them accountable to their goals (Table 2).
OUTCOME Goal-setting, priorities, accountability
As we’re exploring goals with Dr. D, she makes a conscious decision to spend less time on documentation and start focusing on being present with her patients. She returns in 1 month to tell you time management is still a struggle, but her visit with you was instrumental in making her realize how important it was to get home on time for her kids’ activities. She says it greatly helped that you kept her accountable, yet also validated her struggles and gave her permission to design her life within the constraints of her situation and without the burden of having to be perfect at everything.
Bottom Line
We can best help our physician colleagues who are experiencing burnout by shifting our paradigm to a wellness model that focuses on helping them reach their potential and balance their professional and personal lives.
Related Resources
- Balch CM, Shanafelt TD. Combating stress and burnout in surgical practice: a review. Thorac Surg Clin. 2011;21(3):417-430.
- Miller WR, Rollnick S. Motivational interviewing: preparing people for change, 2nd ed. New York, NY: The Guilford Press; 2002.
- Stanford Medicine WellMD. Stress & Burnout. https://wellmd.stanford.edu.
CASE ‘I’m stuck’
Dr. D, age 48, an internist practicing general medicine who is a married mother of 2 teenagers, presents with emotional exhaustion. Her medical history is unremarkable other than hyperlipidemia controlled by diet. She describes an episode of reactive depressive symptoms and anxiety when in college, which was related to the stress of final exams, finances, and the dissolution of a long-standing relationship. Regardless, she functioned well and graduated summa cum laude. She says her current feelings of being “stuck” have gradually increased during the past 3 to 4 years. Although she describes being mildly anxious and dysphoric, she also said she feels like her “wheels are spinning” and that she doesn’t even seem to care. Dr. D had been a high achiever, yet says she feels like she isn’t getting anywhere at work or at home.
[polldaddy:10064977]
The authors’ observations
As psychiatrists in the business of diagnosis and treatment, we immediately considered common diagnoses, such as major depressive disorder and persistent depressive disorder. However, despite our training in pathology, we believe patients should be considered well until proven sick. This paradigm shift is in line with the definition of mental health per the World Health Organization: “A state of well-being in which every individual realizes his or her own potential, can cope with the normal stresses of life, can work productively and fruitfully, and is able to make a contribution to her or his community.”1
In Dr. D’s case, there was not enough information yet to fully support any of the diagnoses. She did not exhibit enough depressive symptoms to support a diagnosis of a depressive disorder. She said that she didn’t feel like she was getting anywhere at work or home. Yet there was no objective information that suggested impairment in functioning, which would preclude a diagnosis of adjustment disorder. At this point, we would support the “V code” diagnosis of phase of life problem, or even what is rarely seen in a psychiatric evaluation: “no diagnosis.”
EVALUATION Is work the problem?
We diligently conduct a thorough review of systems with Dr. D and confirm there is not enough information to diagnose a depressive disorder, anxiety disorder, or other psychiatric disorder. Collateral history suggests her teenagers are well-adjusted and doing well in high school, and she is well-respected at work with reportedly excellent performance ratings. We identify strongly with her and her situation.
Dr. D admits she is an idealist and half-jokingly says she entered into medicine “to save the world.” Yet she laments the long hours and finding herself mired in paperwork. She is barely making it to her kids’ school events and says she can’t believe her first child will be graduating within a year. She has had some particularly challenging patients recently, and although she is still diligent about their care, she is shocked she doesn’t seem to care as much about “solving the medical puzzle.” This came to light for her when a longtime patient observed that Dr. D didn’t seem herself and asked, “Are you all right, Doc?”
Dr. D is professionally dressed and has excellent grooming and hygiene. She looks tired, yet has a full affect, a witty conversational style, and responds appropriately to humor.
[polldaddy:10064980]
The authors’ observations
It can be difficult to know what to do next when there isn’t an established “playbook” for a problem without a diagnosis. We realized Dr. D was describing burnout, a syndrome of depersonalization (detached and not caring, to the point of viewing people as objects), emotional exhaustion, and low personal accomplishment that leads to decreased effectiveness at work.2 DSM-5 does not include “burnout” as a diagnosis3; however, if symptoms evolve to the point where they affect occupational or social functioning, burnout can be similar to adjustment disorder. Treatment with an antidepressant medication is not appropriate. It is possible that CBT might be helpful for many patients, yet there is no evidence that Dr. D has any cognitive distortions. Although we already had some collateral information, it is never wrong to gather additional collateral. However, because burnout is common, we may not need additional information. We could reassure her and send her on her way, but we want to add therapeutic value. We advocated exploring issues in her life and work related to meaning.
Continue to: Physician burnout
Physician burnout
Burnout is an alarmingly common problem among physicians that affects approximately half of psychiatrists. In 2014, 54.4% of physicians, and slightly less than 50% of psychiatrists, had at least 1 symptom of burnout.4 This was up from the 45.5% of physicians and a little more than 40% of psychiatrists who reported burnout in 2011,4 which suggests that as medicine continues to change, doctors may increasingly feel the brunt of this change. The rate of burnout is highest in front-line specialties (family medicine, general internal medicine, and emergency medicine) and lowest in preventive medicine.5 Physician burnout leads to real-world occupational issues, such as medical errors, poor relationships with coworkers and patients, decreased patient satisfaction, and medical malpractice suits.6,7
Even though burnout is clearly a concern for our colleagues, don’t expect them to proactively line up outside our offices. In a survey of 7,197 surgeons, 86.6% of respondents answered it was not important that “I have regular meetings with a psychologist/psychiatrist to discuss stress.”8 At the same time, the idea of meeting with a psychologist/psychiatrist was rated more highly by surgeons who were burnt out and found to be a factor independently associated with burnout.8 Perhaps we have some work to do in marketing our services in a way that welcomes our colleagues.
Although physician burnout has been a focus of recent studies, burnout in general has been studied for decades in other working populations. There are 2 useful models describing burnout:
- The job demand-control(-support) model suggests that individuals experience strain and subsequent ill effects when the demands of their job exceed the control they have,9 and social support from supervisors and colleagues can buffer the harmful effects of job strain.10
- The effort-reward imbalance model suggests that high-effort, low-reward occupational conditions are particularly stressful.11
Both models are simple, intuitive, and suggest solutions.
When engaging your physician colleagues about their burnout, remember that physicians are people, too, and have the same difficulties that everyone else does in successfully practicing healthy behaviors. As physicians, we have significant demands on our time that make it difficult to control our ability to eat, sleep, and exercise. In general, the food available where we work is not nutritious,12 half of us are overweight or obese,13 and working more than 40 hours per week increases the likelihood we’ll have a higher body mass index.14 We don’t sleep well, either—we get less sleep than the general population,15 and more sleep equates to less burnout.16 Regarding exercise, doctors who cannot prioritize exercise tend to have more burnout.17
Continue to: When evaluating a physician colleague for symptoms of burnout...
When evaluating a physician colleague for symptoms of burnout, start by assessing the basics: eating, sleeping, and moving. In Dr. D’s case, this also included taking a quick inventory of what demands were on her proverbial plate. Taking inventory of these demands (ie, demand-control[-support] model) may lead to new insights about what she can control. Prioritization is important to determine where efforts go (ie, effort-reward imbalance model). This is where your skills as a psychiatrist can especially help, as you explore values and bring trade-offs to light.
EVALUATION Permission not to be perfect
As we interview Dr. D, we realize she has some obsessive-compulsive personality traits that are mostly self-serving. She places a high value on being thorough and having elegant clinical notes. Yet this value competes with her desire to be efficient and get home on time to see her kids’ school events. You point this out to her and see if she can come up with some solutions. You also discuss with Dr. D the tension everyone feels between valuing career and valuing family and friends. You normalize her situation, and give her permission to pick something about which she will allow herself not to be perfect.
[polldaddy:10064981]
The authors’ observations
Since perfectionism is a common trait among physicians,18 failure doesn’t seem to be compatible with their DNA. We encourage other physicians to be scientific about their own lives, just as they are in the profession they have chosen. Physicians can delude themselves into thinking they can have it all, not recognizing that every choice has its cost. For example, a physician who decides that it’s okay to publish one fewer research paper this year might have more time to enjoy spending time with his or her children. In our work with physicians, we strive to normalize their experiences, helping them reframe their perfectionistic viewpoint to recognize that everyone struggles with work-life balance issues. We validate that physicians have difficult choices to make in finding what works for them, and we challenge and support them in exploring these choices.
Choosing where to put one’s efforts is also contingent upon the expected rewards. Sometime before the daily grind of our careers in medicine started, we had strong visions of what such careers would mean to us. We visualized the ideal of helping people and making a difference. Then, at some point, many of us took this for granted and forgot about the intrinsic rewards of our work. In a 2014-2015 survey of U.S. physicians across all specialties, only 64.6% of respondents who were highly burned out said they found their work personally rewarding. This is a sharp contrast to the 97.5% of respondents who were not burned out who reported that they found their work personally rewarding.19
As psychiatrists, we can challenge our physician colleagues to dare to dream again. We can help them rediscover the rewarding aspects of their work (ie, per effort-reward imbalance model) that drew them into medicine in the first place. This may include exploring their future legacy. How do they want to be remembered at retirement? Such consideration is linked to mental simulation and meaning in their lives.20 We guide our colleagues to reframe their current situation to see the myriad of choices they have based upon their own specific value system. If family and friends are currently taking priority over work, it also helps to reframe that working allows us to make a good living so we can fully enjoy that time spent with family and friends.
Continue to: If we do our jobs well...
If we do our jobs well, the next part is easy. We have them set specific short- and long-term goals related to their situation. This is something we do every day in our practices. It may help to make sure we’re using SMART (Specific, Measurable, Achievable, Relevant, Time-Bound), a well-known mnemonic used for goals (Table 121), and brush up on our motivational interviewing skills (see Related Resources). It is especially important to make sure our colleagues have goals that are relevant—the “R” in the SMART mnemonic—to their situation.
Finally, we do a better job of reaching our goals and engaging more at work and at home when we have good social support. For physicians, co-worker support has been found to be directly related to our well-being as well as buffering the negative effects of work demands.22 Furthermore, our colleagues are the most acceptable sources of support when we are faced with stressful situations.23 Thus, as psychiatrists, we can doubly help our physician patients by providing collegial support and doing our usual job of holding them accountable to their goals (Table 2).
OUTCOME Goal-setting, priorities, accountability
As we’re exploring goals with Dr. D, she makes a conscious decision to spend less time on documentation and start focusing on being present with her patients. She returns in 1 month to tell you time management is still a struggle, but her visit with you was instrumental in making her realize how important it was to get home on time for her kids’ activities. She says it greatly helped that you kept her accountable, yet also validated her struggles and gave her permission to design her life within the constraints of her situation and without the burden of having to be perfect at everything.
Bottom Line
We can best help our physician colleagues who are experiencing burnout by shifting our paradigm to a wellness model that focuses on helping them reach their potential and balance their professional and personal lives.
Related Resources
- Balch CM, Shanafelt TD. Combating stress and burnout in surgical practice: a review. Thorac Surg Clin. 2011;21(3):417-430.
- Miller WR, Rollnick S. Motivational interviewing: preparing people for change, 2nd ed. New York, NY: The Guilford Press; 2002.
- Stanford Medicine WellMD. Stress & Burnout. https://wellmd.stanford.edu.
1. World Health Organization. Mental health: a state of well-being. http://www.who.int/features/factfiles/mental_health/en/. Updated August 2014. Accessed March 17, 2017.
2. Maslach C, Jackson S, Leiter M. Maslach burnout inventory manual, 3rd ed. Palo Alto, CA: Consulting Psychologists Press; 1996.
3. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013.
4. Shanafelt TD, Hasan O, Dyrbye LN, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin Proc. 2015;90(12):1600-1613.
5. Shanafelt TD, Boone S, Tan L, et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med. 2012;172(18):1377-1385.
6. Shanafelt TD, Sloan JA, Habermann TM. The well-being of physicians. Am J Med. 2003;114(6):513-519.
7. Balch CM, Shanafelt TD. Combating stress and burnout in surgical practice: a review. Adv Surg. 2010;44:29-47.
8. Shanafelt TD, Oreskovich MR, Dyrbye LN, et al. Avoiding burnout: the personal health habits and wellness practices of US Surgeons. Ann Surg. 2012;255(4):625-633.
9. Karasek RA Jr. Job demands, job decision latitude, and mental strain: implications for job redesign. Adm Sci Q. 1979;24(2):285-308.
10. Johnson JV. Collective control: strategies for survival in the workplace. Int J Health Serv. 1989;19(3):469-480.
11. Siegrist J. Adverse health effects of high-effort/low-reward conditions. J Occup Health Psychol. 1996;1(1):27-41.
12. Lesser LI, Cohen DA, Brook RH. Changing eating habits for the medical profession. JAMA. 2012;308(10):983-984.
13. Bleich SN, Bennett WL, Gudzune KA, et al. Impact of physician BMI on obesity care and beliefs. Obesity (Silver Spring). 2012;20(5):999-1005.
14. Stanford FC, Durkin MW, Blair SN, et al. Determining levels of physical activity in attending physicians, resident and fellow physicians, and medical students in the USA. Br J Sports Med. 2012;46(5):360-364.
15. Tucker P, Bejerot E, Kecklund G, et al. Stress Research Institute at Stockholm University. Stress Research Report-doctors’ work hours in Sweden: their impact on sleep, health, work-family balance, patient care and thoughts about work. https://www.stressforskning.su.se/polopoly_fs/1.233341.1429526778!/menu/standard/file/sfr325.pdf. Accessed March 17, 2017.
16. Wisetborisut A, Angkurawaranon C, Jiraporncharoen W, et al. Shift work and burnout among health care workers. Occup Med (Lond). 2014;64(4):279-286.
17. Eckleberry-Hunt J, Lick D, Boura J, et al. An exploratory study of resident burnout and wellness. Acad Med. 2009;84(2):269-277.
18. Peters M, King J. Perfectionism in doctors. BMJ. 2012;344:e1674. doi: https://doi.org/10.1136/bmj.e1674.
19. Jager AJ, Tutty MA, Kao AC. Association between physician burnout and identification with medicine as a calling. Mayo Clin Proc. 2017;92(3):415-422.
20. Waytz A, Hershfield HE, Tamir DI. Neural and behavioral evidence for the role of mental simulation in meaning in life. J Pers Soc Psychol. 2015;108(2):336-355.
21. SMART Criteria. https://en.wikipedia.org/wiki/SMART_criteria. Accessed March 17, 2017.
22. Hu YY, Fix ML, Hevelone ND, et al. Physicians’ needs in coping with emotional stressors: the case for peer support. Arch Surg. 2012;147(3):212-217.
23. Wallace JE, Lemaire J. On physician well being–you’ll get by with a little help from your friends. Soc Sci Med. 2007;64(12):2565-2577.
1. World Health Organization. Mental health: a state of well-being. http://www.who.int/features/factfiles/mental_health/en/. Updated August 2014. Accessed March 17, 2017.
2. Maslach C, Jackson S, Leiter M. Maslach burnout inventory manual, 3rd ed. Palo Alto, CA: Consulting Psychologists Press; 1996.
3. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013.
4. Shanafelt TD, Hasan O, Dyrbye LN, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin Proc. 2015;90(12):1600-1613.
5. Shanafelt TD, Boone S, Tan L, et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med. 2012;172(18):1377-1385.
6. Shanafelt TD, Sloan JA, Habermann TM. The well-being of physicians. Am J Med. 2003;114(6):513-519.
7. Balch CM, Shanafelt TD. Combating stress and burnout in surgical practice: a review. Adv Surg. 2010;44:29-47.
8. Shanafelt TD, Oreskovich MR, Dyrbye LN, et al. Avoiding burnout: the personal health habits and wellness practices of US Surgeons. Ann Surg. 2012;255(4):625-633.
9. Karasek RA Jr. Job demands, job decision latitude, and mental strain: implications for job redesign. Adm Sci Q. 1979;24(2):285-308.
10. Johnson JV. Collective control: strategies for survival in the workplace. Int J Health Serv. 1989;19(3):469-480.
11. Siegrist J. Adverse health effects of high-effort/low-reward conditions. J Occup Health Psychol. 1996;1(1):27-41.
12. Lesser LI, Cohen DA, Brook RH. Changing eating habits for the medical profession. JAMA. 2012;308(10):983-984.
13. Bleich SN, Bennett WL, Gudzune KA, et al. Impact of physician BMI on obesity care and beliefs. Obesity (Silver Spring). 2012;20(5):999-1005.
14. Stanford FC, Durkin MW, Blair SN, et al. Determining levels of physical activity in attending physicians, resident and fellow physicians, and medical students in the USA. Br J Sports Med. 2012;46(5):360-364.
15. Tucker P, Bejerot E, Kecklund G, et al. Stress Research Institute at Stockholm University. Stress Research Report-doctors’ work hours in Sweden: their impact on sleep, health, work-family balance, patient care and thoughts about work. https://www.stressforskning.su.se/polopoly_fs/1.233341.1429526778!/menu/standard/file/sfr325.pdf. Accessed March 17, 2017.
16. Wisetborisut A, Angkurawaranon C, Jiraporncharoen W, et al. Shift work and burnout among health care workers. Occup Med (Lond). 2014;64(4):279-286.
17. Eckleberry-Hunt J, Lick D, Boura J, et al. An exploratory study of resident burnout and wellness. Acad Med. 2009;84(2):269-277.
18. Peters M, King J. Perfectionism in doctors. BMJ. 2012;344:e1674. doi: https://doi.org/10.1136/bmj.e1674.
19. Jager AJ, Tutty MA, Kao AC. Association between physician burnout and identification with medicine as a calling. Mayo Clin Proc. 2017;92(3):415-422.
20. Waytz A, Hershfield HE, Tamir DI. Neural and behavioral evidence for the role of mental simulation in meaning in life. J Pers Soc Psychol. 2015;108(2):336-355.
21. SMART Criteria. https://en.wikipedia.org/wiki/SMART_criteria. Accessed March 17, 2017.
22. Hu YY, Fix ML, Hevelone ND, et al. Physicians’ needs in coping with emotional stressors: the case for peer support. Arch Surg. 2012;147(3):212-217.
23. Wallace JE, Lemaire J. On physician well being–you’ll get by with a little help from your friends. Soc Sci Med. 2007;64(12):2565-2577.
The nurse who worked the system
CASE: A ‘high utilizer’
Ms. Y, a 49-year-old intensive care registered nurse, is admitted to the psychiatric hospital for suicidal ideation for the eighth time in 1 year. Ms. Y has chronic suicidal ideation with multiple attempts and has been on disability for 3 years for treatment of severe depression. She has been hospitalized for depression with suicide ideation 49 times since her divorce 6 years ago. She is prescribed fluoxetine, 60 mg/d, quetiapine, 400 mg/d, and clonazepam, 2 mg/d.
The authors’ observations
Ms. Y possesses 7 of the 11 characteristics of a high utilizer of psychiatric services (Table 1),1,2 defined as a patient who is:
- 2 standard deviations above the mean number of visits to an urban psychiatric emergency service in 6 months or
- has 4 inpatient admissions in a quarter or 6 inpatient admissions in 1 year.
Table 1
Common characteristics of high utilizers* of psychiatric services
| Homelessness |
| Developmental delays |
| Enrolled in a mental health plan |
| History of voluntary and involuntary hospitalization |
| Personality disorders |
| Likely to be uncooperative |
| Substance abuse or dependence (or history) |
| History of incarceration |
| Unreliable social support |
| Young Caucasian women |
| * Defined as having either 2 standard deviations above the mean number of visits to an urban psychiatric emergency service in 6 months or 4 inpatient admissions in a quarter or 6 inpatient admissions in 1 year |
| Source: References 1,2 |
The author’s observations
Because previous hospitalizations and courses of ECT have provided Ms. Y with only minimal, short-lived improvement, the treatment team decides to reconsider her diagnosis and treatment plan. Ms. Y’s first psychiatrist diagnosed her with major depressive disorder. After thoroughly interviewing Ms. Y and reviewing her history, the hospital psychiatrist determines that she meets criteria for borderline personality disorder (BPD) in addition to major depression. The psychiatrist explains this diagnosis to Ms. Y, provides her with education and support, and recommends dialectical behavioral therapy (DBT) and case management. She rejects the new diagnosis and treatment plan and pleads for help establishing treatment with a new psychiatrist.
The team at the psychiatric hospital feels Ms. Y needs to receive ongoing treatment from a psychiatrist. In the hope that she will be able to establish a therapeutic alliance with a new psychiatrist and therapist, they decide to continue working with Ms. Y if she accepts the BPD diagnosis and agrees to undergo DBT.
EVALUATION: A troubling pattern
Before Ms. Y’s husband divorced her, she had not received psychiatric care and had no psychiatric diagnosis. During the contentious divorce, she experienced depressive symptoms that later intensified, and she was unable to return to her previous high level of functioning.
Ms. Y became suicidal and was hospitalized for the first time shortly after the divorce was finalized and her ex-husband remarried. She began treatment with a psychiatrist, whom she idealized and saw for 5 years.
When this psychiatrist—who had been one of the few stable relationships in Ms. Y’s life—moved to another state, Ms. Y experienced a rapid recurrence of depression. She began treatment with 3 other psychiatrists but fired them because they “never understand me” like her first psychiatrist did, and she never felt she received the consistent, supportive care she deserved. She become suicidal and again required psychiatric hospitalization. This pattern continued up to her current admission.
The authors’ observations
Ms. Y briefly returns to work between hospitalizations but is not able to tolerate the stress. At one point she was admitted to an out-of-state facility; after this 2-month stay, she remained out of the local psychiatric hospital for 6 months but then became unable to function and was readmitted to the local psychiatric hospital.
When interviewed, Ms. Y describes feeling hopeless, empty, and alone each time 2 of her 3 children return to college after summer break. Her youngest child lives at home but is involved in extracurricular high school activities, and doesn’t seem to need her. Ms. Y is estranged from both parents. Her social support is unreliable because she tends to push others away and isolate herself.
The authors’ observations
Because she has no history of mania, Ms. Y does not meet criteria for bipolar affective disorder. Her multidisciplinary treatment team feels she is too fragile to transfer care to new providers or to foster care, so we schedule a care conference and carefully compose a 6-month contract to formally articulate limits and boundaries within which we will continue to treat her.
The contract specifies that Ms. Y will participate in DBT, take her medications exactly as prescribed, and not receive any early refills of her prescriptions. We arrange with Ms. Y’s health plan to have a home healthcare agency provide her medications weekly. This benefit was not available to other health plan members. Ms. Y signs the contract.
TREATMENT: Contract violation
Ms. Y complies with the contract for 2 months, then abruptly fires her long-term therapist, whom she claims violated confidentiality by giving false information to another provider. At her next session, Ms. Y will not provide details about the alleged incident, and the issue never is resolved. She admits she did not start DBT and is not taking her medications as prescribed.
Ms. Y expresses her disagreement with the terms of the contract. She becomes very upset and asks for her care to be transferred to another psychiatrist. She demands to be followed at the current clinic because “I was born here.” She denies being actively suicidal and terminates the session early. That afternoon, she calls 1 of the inpatient psychiatrists and asks if he would treat her. She also calls the first psychiatrist she had seen to enlist help in obtaining care.
The authors’ observations
In Groves’ description of 4 types of “hateful patients,” Ms. Y represents a combination of an entitled demander and a manipulative help-rejecter. The behaviors and personality disorders associated with these types of patients—and effective management strategies—are listed in (Table 2).3 (Table 3) offers tips for successfully dealing with high utilizers of psychiatric services. High utilizers of medical services other than psychiatry are more likely than patients who are not high utilizers to have a psychiatric disorder (Box).4-9
Patients who are high utilizers of medical services other than psychiatry have up to 50% higher rates of psychiatric disorders—particularly depression—compared with less-frequent utilizers.4-6 Screening medical patients for depression helps ensure that these patients are correctly diagnosed and treated.
Depression is a risk factor for nonadherence with medical treatment, and treating depression leads to decreased utilization of medical services.7,8 Patients with successfully treated depression may have reduced functional disability as well.9
Some members of our treatment team began to experience countertransference, which also interfered with Ms. Y’s treatment. They viewed her behavior as entitled, demanding, and manipulative and dreaded caring for her. Failing to recognize such defenses can lead to consequences such as malignant alienation—a progressive deterioration in the patient’s relationship with others that includes loss of sympathy and support from staff members—which can put a patient at high risk for suicide.10
After a lengthy discussion among several psychiatrists, therapists, nurses, and attorneys, the treatment team decided to terminate outpatient care for Ms. Y at our facility because of her chronic nonadherence to treatment recommendations. Ms. Y had manipulated numerous providers in our department, called multiple doctors in our facility to ask them to care for her, and asked her ex-husband to contact the department administration on her behalf. Her behavior bordered on harassment. In addition, the interventions we provided were making her worse, not better. Factors that influenced our decision included:
- fear of Ms. Y committing suicide
- fear of setting limits
- fear of being reported to the Medical Board
- fear of a lawsuit.
Table 2
Strategies for helping 4 types of ‘hateful patients’
| Dependent clinger | |
| Behaviors | Shows extreme gratitude with flattery |
| Associated personality traits/disorders | Codependent |
| Management strategies | As early and as tactfully as possible, set firm limits on the patient’s expectations for an intense doctor-patient relationship. Tell the patient that you have limits not only on knowledge and skill but also on time and stamina |
| Entitled demander | |
| Behaviors | Intimidates, devalues, induces guilt, may try to control with threats; terrified of abandonment |
| Associated personality traits/disorders | Narcissistic, borderline personality disorder |
| Management strategies | Try to rechannel your patient’s feelings of entitlement into a partnership that acknowledges his or her entitlement not to unrealistic demands but to good medical care. Help your patient stop directing anger at the healthcare team |
| Manipulative help-rejecter | |
| Behaviors | Resists treatment; may seem happy with treatment failures |
| Associated personality traits/disorders | Psychopathy, paranoia, borderline personality disorder, negativistic, passive/aggressive |
| Management strategies | Diminish your patient’s notion that losing the symptom or illness implies losing the doctor by ‘sharing’ your patient’s pessimism. Tell your patient that treatment may not cure the illness. Schedule regular follow-up visits |
| Self-destructive denier | |
| Behaviors | Denial helps them survive |
| Associated personality traits/disorders | Borderline personality disorder, histrionic, schizoid, schizotypal |
| Management strategies | Recognize that this type of patient can make clinicians wish the patient would die and that the chance of helping a self-destructive denier is minimal. Lower unrealistic expectations of delivering perfect care. Evaluate the patient for a treatable mental illness, such as depression, anxiety, etc. |
| Source: Reference 3 | |
Table 3
Tips for managing high utilizers
Establish a collaborative treatment plan with firm limits and expectations
|
Acknowledge your feelings and countertransference
|
Explore your patient’s expectations and commitment to treatment by asking:
|
Practice safely and proactively
|
OUTCOME: The pattern continues
Ms. Y continues to receive treatment with a different outpatient psychiatrist and therapist in the area. She has not been hospitalized for almost 2 years but her financial state has deteriorated and she has had a recurrence of depression. Ms. Y’s psychiatrist recently called the hospital to ask for direct admission on the patient’s behalf, stating that Ms. Y did not want to wait hours to be seen in the ER. Hospital staff explained that she needs to first come to the ER for evaluation. Ms. Y refused to come to the ER and was not admitted. About 1 month later, Ms. Y’s psychiatrist called again, and she was directly admitted to the psychiatric hospital.
Related resource
- National Suicide Prevention Lifeline. 1-800-273-TALK (8255). www.suicidepreventionlifeline.org.
- Clonazepam • Klonopin
- Fluoxetine • Prozac
- Quetiapine • Seroquel
The authors report no financial relationship with any company whose products are mentioned in this article or manufacturers of competing products.
1. Pasic J, Russo J, Roy-Byrne P. High utilizers of psychiatric emergency services. Psychiatr Serv. 2005;56(6):678-684.
2. Geller J, Fisher W, McDermeit M, et al. The effects of public managed care on patterns of intensive use of inpatient psychiatric services. Psychiatr Serv. 1998;49:327-332.
3. Groves JE. Taking care of the hateful patient. N Engl J Med. 1978;298(16):883-887.
4. Karlsson H, Lehtinen V, Joukamaa M. Are frequent attenders of primary health care distressed? Scan J Health Care. 1995;13:32-38.
5. Karlsson H, Lehtinen V, Joukamaa M. Psychiatric morbidity among frequent attenders in primary care. Gen Hosp Psychiatry. 1995;17:19-25.
6. Lefevre F, Refiler D, Lee P, et al. Screening for undetected mental disorders in high utilizers of primary care services. J Gen Int Med. 1999;14:425-431.
7. Pearson S, Katzelnick D, Simon G, et al. Depression among high utilizers of medical care. J Gen Intern Med. 1999;14:461-468.
8. DiMatteo MR, Lepper HS, Croghan TW. Depression is a risk factor for noncompliance with medical treatment: meta-analysis of the effects of anxiety and depression on medical adherence. Arch Intern Med. 2000;160:2101-2107.
9. Von Korff M, Ormel J, Katon W, et al. Disability and depression among high utilizers of health care. A longitudinal analysis. Arch Gen Psychiatry. 1992;49(2):91-100.
10. Watts D, Morgan G. Malignant alienation dangers for patients who are hard to like. Br J Psychiatry. 1994;164:11-15.
CASE: A ‘high utilizer’
Ms. Y, a 49-year-old intensive care registered nurse, is admitted to the psychiatric hospital for suicidal ideation for the eighth time in 1 year. Ms. Y has chronic suicidal ideation with multiple attempts and has been on disability for 3 years for treatment of severe depression. She has been hospitalized for depression with suicide ideation 49 times since her divorce 6 years ago. She is prescribed fluoxetine, 60 mg/d, quetiapine, 400 mg/d, and clonazepam, 2 mg/d.
The authors’ observations
Ms. Y possesses 7 of the 11 characteristics of a high utilizer of psychiatric services (Table 1),1,2 defined as a patient who is:
- 2 standard deviations above the mean number of visits to an urban psychiatric emergency service in 6 months or
- has 4 inpatient admissions in a quarter or 6 inpatient admissions in 1 year.
Table 1
Common characteristics of high utilizers* of psychiatric services
| Homelessness |
| Developmental delays |
| Enrolled in a mental health plan |
| History of voluntary and involuntary hospitalization |
| Personality disorders |
| Likely to be uncooperative |
| Substance abuse or dependence (or history) |
| History of incarceration |
| Unreliable social support |
| Young Caucasian women |
| * Defined as having either 2 standard deviations above the mean number of visits to an urban psychiatric emergency service in 6 months or 4 inpatient admissions in a quarter or 6 inpatient admissions in 1 year |
| Source: References 1,2 |
The author’s observations
Because previous hospitalizations and courses of ECT have provided Ms. Y with only minimal, short-lived improvement, the treatment team decides to reconsider her diagnosis and treatment plan. Ms. Y’s first psychiatrist diagnosed her with major depressive disorder. After thoroughly interviewing Ms. Y and reviewing her history, the hospital psychiatrist determines that she meets criteria for borderline personality disorder (BPD) in addition to major depression. The psychiatrist explains this diagnosis to Ms. Y, provides her with education and support, and recommends dialectical behavioral therapy (DBT) and case management. She rejects the new diagnosis and treatment plan and pleads for help establishing treatment with a new psychiatrist.
The team at the psychiatric hospital feels Ms. Y needs to receive ongoing treatment from a psychiatrist. In the hope that she will be able to establish a therapeutic alliance with a new psychiatrist and therapist, they decide to continue working with Ms. Y if she accepts the BPD diagnosis and agrees to undergo DBT.
EVALUATION: A troubling pattern
Before Ms. Y’s husband divorced her, she had not received psychiatric care and had no psychiatric diagnosis. During the contentious divorce, she experienced depressive symptoms that later intensified, and she was unable to return to her previous high level of functioning.
Ms. Y became suicidal and was hospitalized for the first time shortly after the divorce was finalized and her ex-husband remarried. She began treatment with a psychiatrist, whom she idealized and saw for 5 years.
When this psychiatrist—who had been one of the few stable relationships in Ms. Y’s life—moved to another state, Ms. Y experienced a rapid recurrence of depression. She began treatment with 3 other psychiatrists but fired them because they “never understand me” like her first psychiatrist did, and she never felt she received the consistent, supportive care she deserved. She become suicidal and again required psychiatric hospitalization. This pattern continued up to her current admission.
The authors’ observations
Ms. Y briefly returns to work between hospitalizations but is not able to tolerate the stress. At one point she was admitted to an out-of-state facility; after this 2-month stay, she remained out of the local psychiatric hospital for 6 months but then became unable to function and was readmitted to the local psychiatric hospital.
When interviewed, Ms. Y describes feeling hopeless, empty, and alone each time 2 of her 3 children return to college after summer break. Her youngest child lives at home but is involved in extracurricular high school activities, and doesn’t seem to need her. Ms. Y is estranged from both parents. Her social support is unreliable because she tends to push others away and isolate herself.
The authors’ observations
Because she has no history of mania, Ms. Y does not meet criteria for bipolar affective disorder. Her multidisciplinary treatment team feels she is too fragile to transfer care to new providers or to foster care, so we schedule a care conference and carefully compose a 6-month contract to formally articulate limits and boundaries within which we will continue to treat her.
The contract specifies that Ms. Y will participate in DBT, take her medications exactly as prescribed, and not receive any early refills of her prescriptions. We arrange with Ms. Y’s health plan to have a home healthcare agency provide her medications weekly. This benefit was not available to other health plan members. Ms. Y signs the contract.
TREATMENT: Contract violation
Ms. Y complies with the contract for 2 months, then abruptly fires her long-term therapist, whom she claims violated confidentiality by giving false information to another provider. At her next session, Ms. Y will not provide details about the alleged incident, and the issue never is resolved. She admits she did not start DBT and is not taking her medications as prescribed.
Ms. Y expresses her disagreement with the terms of the contract. She becomes very upset and asks for her care to be transferred to another psychiatrist. She demands to be followed at the current clinic because “I was born here.” She denies being actively suicidal and terminates the session early. That afternoon, she calls 1 of the inpatient psychiatrists and asks if he would treat her. She also calls the first psychiatrist she had seen to enlist help in obtaining care.
The authors’ observations
In Groves’ description of 4 types of “hateful patients,” Ms. Y represents a combination of an entitled demander and a manipulative help-rejecter. The behaviors and personality disorders associated with these types of patients—and effective management strategies—are listed in (Table 2).3 (Table 3) offers tips for successfully dealing with high utilizers of psychiatric services. High utilizers of medical services other than psychiatry are more likely than patients who are not high utilizers to have a psychiatric disorder (Box).4-9
Patients who are high utilizers of medical services other than psychiatry have up to 50% higher rates of psychiatric disorders—particularly depression—compared with less-frequent utilizers.4-6 Screening medical patients for depression helps ensure that these patients are correctly diagnosed and treated.
Depression is a risk factor for nonadherence with medical treatment, and treating depression leads to decreased utilization of medical services.7,8 Patients with successfully treated depression may have reduced functional disability as well.9
Some members of our treatment team began to experience countertransference, which also interfered with Ms. Y’s treatment. They viewed her behavior as entitled, demanding, and manipulative and dreaded caring for her. Failing to recognize such defenses can lead to consequences such as malignant alienation—a progressive deterioration in the patient’s relationship with others that includes loss of sympathy and support from staff members—which can put a patient at high risk for suicide.10
After a lengthy discussion among several psychiatrists, therapists, nurses, and attorneys, the treatment team decided to terminate outpatient care for Ms. Y at our facility because of her chronic nonadherence to treatment recommendations. Ms. Y had manipulated numerous providers in our department, called multiple doctors in our facility to ask them to care for her, and asked her ex-husband to contact the department administration on her behalf. Her behavior bordered on harassment. In addition, the interventions we provided were making her worse, not better. Factors that influenced our decision included:
- fear of Ms. Y committing suicide
- fear of setting limits
- fear of being reported to the Medical Board
- fear of a lawsuit.
Table 2
Strategies for helping 4 types of ‘hateful patients’
| Dependent clinger | |
| Behaviors | Shows extreme gratitude with flattery |
| Associated personality traits/disorders | Codependent |
| Management strategies | As early and as tactfully as possible, set firm limits on the patient’s expectations for an intense doctor-patient relationship. Tell the patient that you have limits not only on knowledge and skill but also on time and stamina |
| Entitled demander | |
| Behaviors | Intimidates, devalues, induces guilt, may try to control with threats; terrified of abandonment |
| Associated personality traits/disorders | Narcissistic, borderline personality disorder |
| Management strategies | Try to rechannel your patient’s feelings of entitlement into a partnership that acknowledges his or her entitlement not to unrealistic demands but to good medical care. Help your patient stop directing anger at the healthcare team |
| Manipulative help-rejecter | |
| Behaviors | Resists treatment; may seem happy with treatment failures |
| Associated personality traits/disorders | Psychopathy, paranoia, borderline personality disorder, negativistic, passive/aggressive |
| Management strategies | Diminish your patient’s notion that losing the symptom or illness implies losing the doctor by ‘sharing’ your patient’s pessimism. Tell your patient that treatment may not cure the illness. Schedule regular follow-up visits |
| Self-destructive denier | |
| Behaviors | Denial helps them survive |
| Associated personality traits/disorders | Borderline personality disorder, histrionic, schizoid, schizotypal |
| Management strategies | Recognize that this type of patient can make clinicians wish the patient would die and that the chance of helping a self-destructive denier is minimal. Lower unrealistic expectations of delivering perfect care. Evaluate the patient for a treatable mental illness, such as depression, anxiety, etc. |
| Source: Reference 3 | |
Table 3
Tips for managing high utilizers
Establish a collaborative treatment plan with firm limits and expectations
|
Acknowledge your feelings and countertransference
|
Explore your patient’s expectations and commitment to treatment by asking:
|
Practice safely and proactively
|
OUTCOME: The pattern continues
Ms. Y continues to receive treatment with a different outpatient psychiatrist and therapist in the area. She has not been hospitalized for almost 2 years but her financial state has deteriorated and she has had a recurrence of depression. Ms. Y’s psychiatrist recently called the hospital to ask for direct admission on the patient’s behalf, stating that Ms. Y did not want to wait hours to be seen in the ER. Hospital staff explained that she needs to first come to the ER for evaluation. Ms. Y refused to come to the ER and was not admitted. About 1 month later, Ms. Y’s psychiatrist called again, and she was directly admitted to the psychiatric hospital.
Related resource
- National Suicide Prevention Lifeline. 1-800-273-TALK (8255). www.suicidepreventionlifeline.org.
- Clonazepam • Klonopin
- Fluoxetine • Prozac
- Quetiapine • Seroquel
The authors report no financial relationship with any company whose products are mentioned in this article or manufacturers of competing products.
CASE: A ‘high utilizer’
Ms. Y, a 49-year-old intensive care registered nurse, is admitted to the psychiatric hospital for suicidal ideation for the eighth time in 1 year. Ms. Y has chronic suicidal ideation with multiple attempts and has been on disability for 3 years for treatment of severe depression. She has been hospitalized for depression with suicide ideation 49 times since her divorce 6 years ago. She is prescribed fluoxetine, 60 mg/d, quetiapine, 400 mg/d, and clonazepam, 2 mg/d.
The authors’ observations
Ms. Y possesses 7 of the 11 characteristics of a high utilizer of psychiatric services (Table 1),1,2 defined as a patient who is:
- 2 standard deviations above the mean number of visits to an urban psychiatric emergency service in 6 months or
- has 4 inpatient admissions in a quarter or 6 inpatient admissions in 1 year.
Table 1
Common characteristics of high utilizers* of psychiatric services
| Homelessness |
| Developmental delays |
| Enrolled in a mental health plan |
| History of voluntary and involuntary hospitalization |
| Personality disorders |
| Likely to be uncooperative |
| Substance abuse or dependence (or history) |
| History of incarceration |
| Unreliable social support |
| Young Caucasian women |
| * Defined as having either 2 standard deviations above the mean number of visits to an urban psychiatric emergency service in 6 months or 4 inpatient admissions in a quarter or 6 inpatient admissions in 1 year |
| Source: References 1,2 |
The author’s observations
Because previous hospitalizations and courses of ECT have provided Ms. Y with only minimal, short-lived improvement, the treatment team decides to reconsider her diagnosis and treatment plan. Ms. Y’s first psychiatrist diagnosed her with major depressive disorder. After thoroughly interviewing Ms. Y and reviewing her history, the hospital psychiatrist determines that she meets criteria for borderline personality disorder (BPD) in addition to major depression. The psychiatrist explains this diagnosis to Ms. Y, provides her with education and support, and recommends dialectical behavioral therapy (DBT) and case management. She rejects the new diagnosis and treatment plan and pleads for help establishing treatment with a new psychiatrist.
The team at the psychiatric hospital feels Ms. Y needs to receive ongoing treatment from a psychiatrist. In the hope that she will be able to establish a therapeutic alliance with a new psychiatrist and therapist, they decide to continue working with Ms. Y if she accepts the BPD diagnosis and agrees to undergo DBT.
EVALUATION: A troubling pattern
Before Ms. Y’s husband divorced her, she had not received psychiatric care and had no psychiatric diagnosis. During the contentious divorce, she experienced depressive symptoms that later intensified, and she was unable to return to her previous high level of functioning.
Ms. Y became suicidal and was hospitalized for the first time shortly after the divorce was finalized and her ex-husband remarried. She began treatment with a psychiatrist, whom she idealized and saw for 5 years.
When this psychiatrist—who had been one of the few stable relationships in Ms. Y’s life—moved to another state, Ms. Y experienced a rapid recurrence of depression. She began treatment with 3 other psychiatrists but fired them because they “never understand me” like her first psychiatrist did, and she never felt she received the consistent, supportive care she deserved. She become suicidal and again required psychiatric hospitalization. This pattern continued up to her current admission.
The authors’ observations
Ms. Y briefly returns to work between hospitalizations but is not able to tolerate the stress. At one point she was admitted to an out-of-state facility; after this 2-month stay, she remained out of the local psychiatric hospital for 6 months but then became unable to function and was readmitted to the local psychiatric hospital.
When interviewed, Ms. Y describes feeling hopeless, empty, and alone each time 2 of her 3 children return to college after summer break. Her youngest child lives at home but is involved in extracurricular high school activities, and doesn’t seem to need her. Ms. Y is estranged from both parents. Her social support is unreliable because she tends to push others away and isolate herself.
The authors’ observations
Because she has no history of mania, Ms. Y does not meet criteria for bipolar affective disorder. Her multidisciplinary treatment team feels she is too fragile to transfer care to new providers or to foster care, so we schedule a care conference and carefully compose a 6-month contract to formally articulate limits and boundaries within which we will continue to treat her.
The contract specifies that Ms. Y will participate in DBT, take her medications exactly as prescribed, and not receive any early refills of her prescriptions. We arrange with Ms. Y’s health plan to have a home healthcare agency provide her medications weekly. This benefit was not available to other health plan members. Ms. Y signs the contract.
TREATMENT: Contract violation
Ms. Y complies with the contract for 2 months, then abruptly fires her long-term therapist, whom she claims violated confidentiality by giving false information to another provider. At her next session, Ms. Y will not provide details about the alleged incident, and the issue never is resolved. She admits she did not start DBT and is not taking her medications as prescribed.
Ms. Y expresses her disagreement with the terms of the contract. She becomes very upset and asks for her care to be transferred to another psychiatrist. She demands to be followed at the current clinic because “I was born here.” She denies being actively suicidal and terminates the session early. That afternoon, she calls 1 of the inpatient psychiatrists and asks if he would treat her. She also calls the first psychiatrist she had seen to enlist help in obtaining care.
The authors’ observations
In Groves’ description of 4 types of “hateful patients,” Ms. Y represents a combination of an entitled demander and a manipulative help-rejecter. The behaviors and personality disorders associated with these types of patients—and effective management strategies—are listed in (Table 2).3 (Table 3) offers tips for successfully dealing with high utilizers of psychiatric services. High utilizers of medical services other than psychiatry are more likely than patients who are not high utilizers to have a psychiatric disorder (Box).4-9
Patients who are high utilizers of medical services other than psychiatry have up to 50% higher rates of psychiatric disorders—particularly depression—compared with less-frequent utilizers.4-6 Screening medical patients for depression helps ensure that these patients are correctly diagnosed and treated.
Depression is a risk factor for nonadherence with medical treatment, and treating depression leads to decreased utilization of medical services.7,8 Patients with successfully treated depression may have reduced functional disability as well.9
Some members of our treatment team began to experience countertransference, which also interfered with Ms. Y’s treatment. They viewed her behavior as entitled, demanding, and manipulative and dreaded caring for her. Failing to recognize such defenses can lead to consequences such as malignant alienation—a progressive deterioration in the patient’s relationship with others that includes loss of sympathy and support from staff members—which can put a patient at high risk for suicide.10
After a lengthy discussion among several psychiatrists, therapists, nurses, and attorneys, the treatment team decided to terminate outpatient care for Ms. Y at our facility because of her chronic nonadherence to treatment recommendations. Ms. Y had manipulated numerous providers in our department, called multiple doctors in our facility to ask them to care for her, and asked her ex-husband to contact the department administration on her behalf. Her behavior bordered on harassment. In addition, the interventions we provided were making her worse, not better. Factors that influenced our decision included:
- fear of Ms. Y committing suicide
- fear of setting limits
- fear of being reported to the Medical Board
- fear of a lawsuit.
Table 2
Strategies for helping 4 types of ‘hateful patients’
| Dependent clinger | |
| Behaviors | Shows extreme gratitude with flattery |
| Associated personality traits/disorders | Codependent |
| Management strategies | As early and as tactfully as possible, set firm limits on the patient’s expectations for an intense doctor-patient relationship. Tell the patient that you have limits not only on knowledge and skill but also on time and stamina |
| Entitled demander | |
| Behaviors | Intimidates, devalues, induces guilt, may try to control with threats; terrified of abandonment |
| Associated personality traits/disorders | Narcissistic, borderline personality disorder |
| Management strategies | Try to rechannel your patient’s feelings of entitlement into a partnership that acknowledges his or her entitlement not to unrealistic demands but to good medical care. Help your patient stop directing anger at the healthcare team |
| Manipulative help-rejecter | |
| Behaviors | Resists treatment; may seem happy with treatment failures |
| Associated personality traits/disorders | Psychopathy, paranoia, borderline personality disorder, negativistic, passive/aggressive |
| Management strategies | Diminish your patient’s notion that losing the symptom or illness implies losing the doctor by ‘sharing’ your patient’s pessimism. Tell your patient that treatment may not cure the illness. Schedule regular follow-up visits |
| Self-destructive denier | |
| Behaviors | Denial helps them survive |
| Associated personality traits/disorders | Borderline personality disorder, histrionic, schizoid, schizotypal |
| Management strategies | Recognize that this type of patient can make clinicians wish the patient would die and that the chance of helping a self-destructive denier is minimal. Lower unrealistic expectations of delivering perfect care. Evaluate the patient for a treatable mental illness, such as depression, anxiety, etc. |
| Source: Reference 3 | |
Table 3
Tips for managing high utilizers
Establish a collaborative treatment plan with firm limits and expectations
|
Acknowledge your feelings and countertransference
|
Explore your patient’s expectations and commitment to treatment by asking:
|
Practice safely and proactively
|
OUTCOME: The pattern continues
Ms. Y continues to receive treatment with a different outpatient psychiatrist and therapist in the area. She has not been hospitalized for almost 2 years but her financial state has deteriorated and she has had a recurrence of depression. Ms. Y’s psychiatrist recently called the hospital to ask for direct admission on the patient’s behalf, stating that Ms. Y did not want to wait hours to be seen in the ER. Hospital staff explained that she needs to first come to the ER for evaluation. Ms. Y refused to come to the ER and was not admitted. About 1 month later, Ms. Y’s psychiatrist called again, and she was directly admitted to the psychiatric hospital.
Related resource
- National Suicide Prevention Lifeline. 1-800-273-TALK (8255). www.suicidepreventionlifeline.org.
- Clonazepam • Klonopin
- Fluoxetine • Prozac
- Quetiapine • Seroquel
The authors report no financial relationship with any company whose products are mentioned in this article or manufacturers of competing products.
1. Pasic J, Russo J, Roy-Byrne P. High utilizers of psychiatric emergency services. Psychiatr Serv. 2005;56(6):678-684.
2. Geller J, Fisher W, McDermeit M, et al. The effects of public managed care on patterns of intensive use of inpatient psychiatric services. Psychiatr Serv. 1998;49:327-332.
3. Groves JE. Taking care of the hateful patient. N Engl J Med. 1978;298(16):883-887.
4. Karlsson H, Lehtinen V, Joukamaa M. Are frequent attenders of primary health care distressed? Scan J Health Care. 1995;13:32-38.
5. Karlsson H, Lehtinen V, Joukamaa M. Psychiatric morbidity among frequent attenders in primary care. Gen Hosp Psychiatry. 1995;17:19-25.
6. Lefevre F, Refiler D, Lee P, et al. Screening for undetected mental disorders in high utilizers of primary care services. J Gen Int Med. 1999;14:425-431.
7. Pearson S, Katzelnick D, Simon G, et al. Depression among high utilizers of medical care. J Gen Intern Med. 1999;14:461-468.
8. DiMatteo MR, Lepper HS, Croghan TW. Depression is a risk factor for noncompliance with medical treatment: meta-analysis of the effects of anxiety and depression on medical adherence. Arch Intern Med. 2000;160:2101-2107.
9. Von Korff M, Ormel J, Katon W, et al. Disability and depression among high utilizers of health care. A longitudinal analysis. Arch Gen Psychiatry. 1992;49(2):91-100.
10. Watts D, Morgan G. Malignant alienation dangers for patients who are hard to like. Br J Psychiatry. 1994;164:11-15.
1. Pasic J, Russo J, Roy-Byrne P. High utilizers of psychiatric emergency services. Psychiatr Serv. 2005;56(6):678-684.
2. Geller J, Fisher W, McDermeit M, et al. The effects of public managed care on patterns of intensive use of inpatient psychiatric services. Psychiatr Serv. 1998;49:327-332.
3. Groves JE. Taking care of the hateful patient. N Engl J Med. 1978;298(16):883-887.
4. Karlsson H, Lehtinen V, Joukamaa M. Are frequent attenders of primary health care distressed? Scan J Health Care. 1995;13:32-38.
5. Karlsson H, Lehtinen V, Joukamaa M. Psychiatric morbidity among frequent attenders in primary care. Gen Hosp Psychiatry. 1995;17:19-25.
6. Lefevre F, Refiler D, Lee P, et al. Screening for undetected mental disorders in high utilizers of primary care services. J Gen Int Med. 1999;14:425-431.
7. Pearson S, Katzelnick D, Simon G, et al. Depression among high utilizers of medical care. J Gen Intern Med. 1999;14:461-468.
8. DiMatteo MR, Lepper HS, Croghan TW. Depression is a risk factor for noncompliance with medical treatment: meta-analysis of the effects of anxiety and depression on medical adherence. Arch Intern Med. 2000;160:2101-2107.
9. Von Korff M, Ormel J, Katon W, et al. Disability and depression among high utilizers of health care. A longitudinal analysis. Arch Gen Psychiatry. 1992;49(2):91-100.
10. Watts D, Morgan G. Malignant alienation dangers for patients who are hard to like. Br J Psychiatry. 1994;164:11-15.
Is your patient too sick to work?
Ms. S, age 34, is a hard-working, single mother of two who works full-time at a local factory. She has recurrent major depression and has been struggling for 2 months. As you write the script to increase her fluoxetine dosage, she asks, “Hey, Doc, can you sign this form so I can have some time off work?”
If you feel uncomfortable signing work forms, approach your patients’ employment issues as you would any medical problem. Your job is to assess capacity to work, and the employer—based on restrictions you write in the medical report—decides if an accommodation can be made.
By answering five questions (Table 1), you can make informed decisions about your patients’ ability to work while:
- minimizing recovery time
- maintaining their daily structure and functioning
- reducing risk of chronic disability.
Table 1
Can a mentally ill patient work? 5 questions to consider
| What is the employee’s diagnosis? |
| What work can the employee do today? |
| To reduce risk of medical harm, what work should the employee not do? |
| Does an impairment prevent the employee from performing essential job functions? |
| What must occur to get the patient back to work? |
QUESTION 1: What is the employee’s diagnosis?
Diagnosis gives you a framework to understand what an employee can and cannot do on the job. Because Ms. S’ diagnosis is major depressive disorder, she may have low mood, low energy, decreased concentration, slowed movement, and disturbed sleep.
But diagnosis alone does not mean she is unable to work. Being separated from work can destabilize a person’s life (Box),1-4 and debilitating depressive symptoms can change from day to day.
QUESTION 2: What work can the employee do today?
Four capacities are needed to function in the workplace:
- understanding and memory
- sustained concentration and persistence
- social interaction
- adaptation.5
A mildly depressed custodian could follow instructions, perform repetitive tasks, and keep pace on a daily shift. A depressed school principal, on the other hand, might lack the decision-making and social skills to relate to teachers, students, and parents. If she can follow instructions and perform simple tasks, however, she might be able to return to work and catch up on paperwork. She could postpone meetings and appointments until she feels well enough resume her full duties.
For almost any job, an employee must have understanding and memory to follow instructions and perform simple tasks.
Table 2
Can your patient work? Assess work functions by required capacities
| Work function* | Capacity required to perform work function† |
|---|---|
| Comprehend and follow instructions | Understanding and memory |
| Perform simple and repetitive tasks | Understanding and memory |
| Maintain a work pace appropriate to a given workload | Sustained concentration and persistence |
| Perform complex or varied tasks | Understanding and memory; adaptation |
| Relate to other people beyond giving and receiving instructions | Social interaction; adaptation |
| Influence people | Social interaction; adaptation |
| Make generalizations, evaluations, or decisions without immediate supervision | Understanding and memory; adaptation |
| Accept and carry out responsibility for direction, control, and planning | Understanding and memory; adaptation |
| *Defined by the California Division of Industrial Accidents. | |
| †Analogous capacities developed by the American Medical Association and Social Security Administration | |
| Source: References 5 and 6 | |
Case continued: assessing capacity
To assess ability to comprehend and follow instructions, you could ask Ms. S to:
- take the yellow book off the bookshelf with her right hand
- turn to page 23
- set the book down on your desk.
To assess ability to perform simple tasks, you might ask Ms. S to describe what she does on a typical day. If she brushes her teeth, makes meals, does laundry, and buys groceries, she can probably do similar tasks at work. If she’s lying on the couch, staring at the wall, and neglecting self care, she might not have the motivation or concentration to complete simple tasks.
It might help to know how Ms. S arrived to see you. Driving is a more complicated task than having a friend or family member bring her. Ms. S’ story may include inconsistencies, and ideally you would have her sign releases to obtain collateral history from family, friends, or perhaps her supervisor.
Watching Ms. S leave can offer information about her functioning. Does she talk to anyone? Does she look the same as when she was in the office? Did she appear slowed when you saw her, yet could easily walk to the car and drive off?
QUESTION 3: To reduce risk of medical harm, what work should the patient not do?
A suicidal or homicidal patient may need to be hospitalized and should not go to work. Someone who is neglecting self care—such as eating—probably does not belong at work and could be at risk for harm.
Symptoms such as decreased concentration, psychomotor slowing, and decreased alertness are absolute contraindications for hazardous jobs that require sustained concentration and quick decisions—such as driving fork lifts or operating heavy machinery.
If potential exists for harm, recommend that the employee be treated before you re-evaluate return to work. Ideally, a case manager from the employer’s occupational health provider would check with the employee during treatment to reassess safety factors and facilitate a smooth return to work.
If medical harm is unlikely, recommending time off work becomes “medical discretion” and is not necessarily “medically required.”7
QUESTION 4: Does an impairment prevent the patient from performing essential job functions?
Impairment—a medical term—is often confused with disability, an administrative term:
- Impairment is “a loss, loss of use, or derangement of a body part, organ system, or organ function.”
- Disability is “an alteration of an individual’s capacity to meet personal, social, or occupational demands because of an impairment.”5
The longer a person is away from work with an injury or illness, the less likely he or she will return:
- 50% of persons off work for 8 weeks will not return.
- >85% of persons off work for 6 months will not return to long-term employment and are at risk for long-term disability.1
Unemployment increases mortality rates, physical and mental illness, and use of medical services.2 The unemployed may be more likely than the employed to visit physicians, take medications, or be admitted to hospitals.3
A disability mindset can develop after only 2 to 4 weeks off work, even in capable workers. An estimated 60% to 80% of time away from work is medically unnecessary.4 Returning to work as soon as possible after an illness or injury maximizes health outcomes and ability to function.
An employee who can perform essential job functions despite an impairment should stay at work. If he or she cannot do those functions, clearly state the impairment—such as decreased concentration, problems with persistence and pace—on the medical form so that the employer can decide if an accommodation can be made.
If essential job functions are high-order—such as air traffic control—even slight impairment could prevent the employee from safely doing the job. An impaired air traffic controller probably could do less-complex activities, however, such as clerical work.
Medical discretion. Most depressed patients can follow instructions and complete simple tasks, but many cannot keep up with the usual work pace because of low energy and slowed thinking and movements. Using medical discretion to recommend a short time off might help a depressed person return to full productivity more quickly if intensive treatment is available.
Limit discretionary time off to short periods when a treatment program is available. When blanket restrictions are written, the patient too often sits idle at home, getting worse and not better. At least excuse your patient from work to attend medical appointments and engage in depression treatment.
QUESTION 5: What must occur to get the patient back to work?
Returning to work as soon as possible can be therapeutic. Having a regular routine and daily structure gives the depressed person a sense of normalcy not found while sitting at home. Beyond stating the impairment on the medical form, suggest possible accommodations the employer could make to expedite return to work.
For your depressed patient, you could suggest reduced work hours (to accommodate low energy) or allowing more time to complete tasks. Whatever the diagnosis, addressing conflict in the workplace often helps. Strategies include:
- working individually with your patient
- alerting the patient to the employer’s conflict resolution policies and employee assistance programs.
CASE RESOLUTION: WORK AS THERAPY
Ms. S shows good eye contact, is appropriately dressed, shows no psychomotor abnormalities, and is not suicidal or homicidal. Mental status exam is normal. You determine that she can follow instructions, perform tasks, and keep up with her workload. She can probably do her job but initially might have difficulties because of depression’s effects on socialization and executive functioning.
You encourage Ms. S to return to work for the therapeutic benefits of a daily routine, but you suggest she postpone big projects or major decisions until she feels better.
Reassure your patient when you find no compelling reason why she cannot return to work. Explain that feeling ambivalent about maintaining function at work is normal, and staying at work is crucial to confidence and self-esteem.
Recognize the potential attraction of secondary gain—such as attention from family and medical providers and financial incentives to stay off work—but also normalize the experience for your patient. Help her regain her independence and start thinking about how she can improve her work situation.
Related resources
- Academy of Organizational and Occupational Psychiatry. www.aoop.org.
- National Partnership for Workplace Mental Health. www.workplacementalhealth.org
- Talmage JB, Melhorn JM (eds). A physician’s guide to return to work. Chicago: AMA Press; 2005.
- Fluoxetine • Prozac
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Pilley M. How the primary care physician can help patients negotiate the return-to-work disability dilemma. In: Talmage JB, Melhorn JM, eds. A physician’s guide to return to work. Chicago: AMA Press; 2005:151.
2. Mathers CD, Schofield DJ. The health consequences of unemployment: the evidence. Med J Aust 1998;168:178-82.
3. Jin RL, Shah CP, Svoboda TJ. The impact of unemployment on health: a review of the evidence. Can Med Assoc J 1995;153:529-40.
4. Christian J. Reducing disability days: healing more than the injury. Journal of Workers Compensation 2000;9:30-55.
5. Cocchiarella L, Andersson BJ. Mental and behavioral disorders. In: Cocchiarella L, Andersson BJ, eds. Guides to the evaluation of permanent impairment, 5th ed. Chicago: American Medical Association; 2001:361–4.
6. Enelow AJ. Psychiatric disorders and work function. Psychiatr Ann 1991;21(1):27-35.
7. American College of Occupational and Environmental Medicine. Preventing needless work disability by helping people stay employed. Available at: http://www.acoem.org/position/statements.asp?CATA_ID=100. Accessed Aug. 8, 2006.
8. United States Department of Labor. Office of Disability Employment Policy. Glossary of commonly used terms. Available at: http://www.dol.gov/odep/pubs/ek00/glossary.htm. Accessed Aug. 8, 2006.
Ms. S, age 34, is a hard-working, single mother of two who works full-time at a local factory. She has recurrent major depression and has been struggling for 2 months. As you write the script to increase her fluoxetine dosage, she asks, “Hey, Doc, can you sign this form so I can have some time off work?”
If you feel uncomfortable signing work forms, approach your patients’ employment issues as you would any medical problem. Your job is to assess capacity to work, and the employer—based on restrictions you write in the medical report—decides if an accommodation can be made.
By answering five questions (Table 1), you can make informed decisions about your patients’ ability to work while:
- minimizing recovery time
- maintaining their daily structure and functioning
- reducing risk of chronic disability.
Table 1
Can a mentally ill patient work? 5 questions to consider
| What is the employee’s diagnosis? |
| What work can the employee do today? |
| To reduce risk of medical harm, what work should the employee not do? |
| Does an impairment prevent the employee from performing essential job functions? |
| What must occur to get the patient back to work? |
QUESTION 1: What is the employee’s diagnosis?
Diagnosis gives you a framework to understand what an employee can and cannot do on the job. Because Ms. S’ diagnosis is major depressive disorder, she may have low mood, low energy, decreased concentration, slowed movement, and disturbed sleep.
But diagnosis alone does not mean she is unable to work. Being separated from work can destabilize a person’s life (Box),1-4 and debilitating depressive symptoms can change from day to day.
QUESTION 2: What work can the employee do today?
Four capacities are needed to function in the workplace:
- understanding and memory
- sustained concentration and persistence
- social interaction
- adaptation.5
A mildly depressed custodian could follow instructions, perform repetitive tasks, and keep pace on a daily shift. A depressed school principal, on the other hand, might lack the decision-making and social skills to relate to teachers, students, and parents. If she can follow instructions and perform simple tasks, however, she might be able to return to work and catch up on paperwork. She could postpone meetings and appointments until she feels well enough resume her full duties.
For almost any job, an employee must have understanding and memory to follow instructions and perform simple tasks.
Table 2
Can your patient work? Assess work functions by required capacities
| Work function* | Capacity required to perform work function† |
|---|---|
| Comprehend and follow instructions | Understanding and memory |
| Perform simple and repetitive tasks | Understanding and memory |
| Maintain a work pace appropriate to a given workload | Sustained concentration and persistence |
| Perform complex or varied tasks | Understanding and memory; adaptation |
| Relate to other people beyond giving and receiving instructions | Social interaction; adaptation |
| Influence people | Social interaction; adaptation |
| Make generalizations, evaluations, or decisions without immediate supervision | Understanding and memory; adaptation |
| Accept and carry out responsibility for direction, control, and planning | Understanding and memory; adaptation |
| *Defined by the California Division of Industrial Accidents. | |
| †Analogous capacities developed by the American Medical Association and Social Security Administration | |
| Source: References 5 and 6 | |
Case continued: assessing capacity
To assess ability to comprehend and follow instructions, you could ask Ms. S to:
- take the yellow book off the bookshelf with her right hand
- turn to page 23
- set the book down on your desk.
To assess ability to perform simple tasks, you might ask Ms. S to describe what she does on a typical day. If she brushes her teeth, makes meals, does laundry, and buys groceries, she can probably do similar tasks at work. If she’s lying on the couch, staring at the wall, and neglecting self care, she might not have the motivation or concentration to complete simple tasks.
It might help to know how Ms. S arrived to see you. Driving is a more complicated task than having a friend or family member bring her. Ms. S’ story may include inconsistencies, and ideally you would have her sign releases to obtain collateral history from family, friends, or perhaps her supervisor.
Watching Ms. S leave can offer information about her functioning. Does she talk to anyone? Does she look the same as when she was in the office? Did she appear slowed when you saw her, yet could easily walk to the car and drive off?
QUESTION 3: To reduce risk of medical harm, what work should the patient not do?
A suicidal or homicidal patient may need to be hospitalized and should not go to work. Someone who is neglecting self care—such as eating—probably does not belong at work and could be at risk for harm.
Symptoms such as decreased concentration, psychomotor slowing, and decreased alertness are absolute contraindications for hazardous jobs that require sustained concentration and quick decisions—such as driving fork lifts or operating heavy machinery.
If potential exists for harm, recommend that the employee be treated before you re-evaluate return to work. Ideally, a case manager from the employer’s occupational health provider would check with the employee during treatment to reassess safety factors and facilitate a smooth return to work.
If medical harm is unlikely, recommending time off work becomes “medical discretion” and is not necessarily “medically required.”7
QUESTION 4: Does an impairment prevent the patient from performing essential job functions?
Impairment—a medical term—is often confused with disability, an administrative term:
- Impairment is “a loss, loss of use, or derangement of a body part, organ system, or organ function.”
- Disability is “an alteration of an individual’s capacity to meet personal, social, or occupational demands because of an impairment.”5
The longer a person is away from work with an injury or illness, the less likely he or she will return:
- 50% of persons off work for 8 weeks will not return.
- >85% of persons off work for 6 months will not return to long-term employment and are at risk for long-term disability.1
Unemployment increases mortality rates, physical and mental illness, and use of medical services.2 The unemployed may be more likely than the employed to visit physicians, take medications, or be admitted to hospitals.3
A disability mindset can develop after only 2 to 4 weeks off work, even in capable workers. An estimated 60% to 80% of time away from work is medically unnecessary.4 Returning to work as soon as possible after an illness or injury maximizes health outcomes and ability to function.
An employee who can perform essential job functions despite an impairment should stay at work. If he or she cannot do those functions, clearly state the impairment—such as decreased concentration, problems with persistence and pace—on the medical form so that the employer can decide if an accommodation can be made.
If essential job functions are high-order—such as air traffic control—even slight impairment could prevent the employee from safely doing the job. An impaired air traffic controller probably could do less-complex activities, however, such as clerical work.
Medical discretion. Most depressed patients can follow instructions and complete simple tasks, but many cannot keep up with the usual work pace because of low energy and slowed thinking and movements. Using medical discretion to recommend a short time off might help a depressed person return to full productivity more quickly if intensive treatment is available.
Limit discretionary time off to short periods when a treatment program is available. When blanket restrictions are written, the patient too often sits idle at home, getting worse and not better. At least excuse your patient from work to attend medical appointments and engage in depression treatment.
QUESTION 5: What must occur to get the patient back to work?
Returning to work as soon as possible can be therapeutic. Having a regular routine and daily structure gives the depressed person a sense of normalcy not found while sitting at home. Beyond stating the impairment on the medical form, suggest possible accommodations the employer could make to expedite return to work.
For your depressed patient, you could suggest reduced work hours (to accommodate low energy) or allowing more time to complete tasks. Whatever the diagnosis, addressing conflict in the workplace often helps. Strategies include:
- working individually with your patient
- alerting the patient to the employer’s conflict resolution policies and employee assistance programs.
CASE RESOLUTION: WORK AS THERAPY
Ms. S shows good eye contact, is appropriately dressed, shows no psychomotor abnormalities, and is not suicidal or homicidal. Mental status exam is normal. You determine that she can follow instructions, perform tasks, and keep up with her workload. She can probably do her job but initially might have difficulties because of depression’s effects on socialization and executive functioning.
You encourage Ms. S to return to work for the therapeutic benefits of a daily routine, but you suggest she postpone big projects or major decisions until she feels better.
Reassure your patient when you find no compelling reason why she cannot return to work. Explain that feeling ambivalent about maintaining function at work is normal, and staying at work is crucial to confidence and self-esteem.
Recognize the potential attraction of secondary gain—such as attention from family and medical providers and financial incentives to stay off work—but also normalize the experience for your patient. Help her regain her independence and start thinking about how she can improve her work situation.
Related resources
- Academy of Organizational and Occupational Psychiatry. www.aoop.org.
- National Partnership for Workplace Mental Health. www.workplacementalhealth.org
- Talmage JB, Melhorn JM (eds). A physician’s guide to return to work. Chicago: AMA Press; 2005.
- Fluoxetine • Prozac
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Ms. S, age 34, is a hard-working, single mother of two who works full-time at a local factory. She has recurrent major depression and has been struggling for 2 months. As you write the script to increase her fluoxetine dosage, she asks, “Hey, Doc, can you sign this form so I can have some time off work?”
If you feel uncomfortable signing work forms, approach your patients’ employment issues as you would any medical problem. Your job is to assess capacity to work, and the employer—based on restrictions you write in the medical report—decides if an accommodation can be made.
By answering five questions (Table 1), you can make informed decisions about your patients’ ability to work while:
- minimizing recovery time
- maintaining their daily structure and functioning
- reducing risk of chronic disability.
Table 1
Can a mentally ill patient work? 5 questions to consider
| What is the employee’s diagnosis? |
| What work can the employee do today? |
| To reduce risk of medical harm, what work should the employee not do? |
| Does an impairment prevent the employee from performing essential job functions? |
| What must occur to get the patient back to work? |
QUESTION 1: What is the employee’s diagnosis?
Diagnosis gives you a framework to understand what an employee can and cannot do on the job. Because Ms. S’ diagnosis is major depressive disorder, she may have low mood, low energy, decreased concentration, slowed movement, and disturbed sleep.
But diagnosis alone does not mean she is unable to work. Being separated from work can destabilize a person’s life (Box),1-4 and debilitating depressive symptoms can change from day to day.
QUESTION 2: What work can the employee do today?
Four capacities are needed to function in the workplace:
- understanding and memory
- sustained concentration and persistence
- social interaction
- adaptation.5
A mildly depressed custodian could follow instructions, perform repetitive tasks, and keep pace on a daily shift. A depressed school principal, on the other hand, might lack the decision-making and social skills to relate to teachers, students, and parents. If she can follow instructions and perform simple tasks, however, she might be able to return to work and catch up on paperwork. She could postpone meetings and appointments until she feels well enough resume her full duties.
For almost any job, an employee must have understanding and memory to follow instructions and perform simple tasks.
Table 2
Can your patient work? Assess work functions by required capacities
| Work function* | Capacity required to perform work function† |
|---|---|
| Comprehend and follow instructions | Understanding and memory |
| Perform simple and repetitive tasks | Understanding and memory |
| Maintain a work pace appropriate to a given workload | Sustained concentration and persistence |
| Perform complex or varied tasks | Understanding and memory; adaptation |
| Relate to other people beyond giving and receiving instructions | Social interaction; adaptation |
| Influence people | Social interaction; adaptation |
| Make generalizations, evaluations, or decisions without immediate supervision | Understanding and memory; adaptation |
| Accept and carry out responsibility for direction, control, and planning | Understanding and memory; adaptation |
| *Defined by the California Division of Industrial Accidents. | |
| †Analogous capacities developed by the American Medical Association and Social Security Administration | |
| Source: References 5 and 6 | |
Case continued: assessing capacity
To assess ability to comprehend and follow instructions, you could ask Ms. S to:
- take the yellow book off the bookshelf with her right hand
- turn to page 23
- set the book down on your desk.
To assess ability to perform simple tasks, you might ask Ms. S to describe what she does on a typical day. If she brushes her teeth, makes meals, does laundry, and buys groceries, she can probably do similar tasks at work. If she’s lying on the couch, staring at the wall, and neglecting self care, she might not have the motivation or concentration to complete simple tasks.
It might help to know how Ms. S arrived to see you. Driving is a more complicated task than having a friend or family member bring her. Ms. S’ story may include inconsistencies, and ideally you would have her sign releases to obtain collateral history from family, friends, or perhaps her supervisor.
Watching Ms. S leave can offer information about her functioning. Does she talk to anyone? Does she look the same as when she was in the office? Did she appear slowed when you saw her, yet could easily walk to the car and drive off?
QUESTION 3: To reduce risk of medical harm, what work should the patient not do?
A suicidal or homicidal patient may need to be hospitalized and should not go to work. Someone who is neglecting self care—such as eating—probably does not belong at work and could be at risk for harm.
Symptoms such as decreased concentration, psychomotor slowing, and decreased alertness are absolute contraindications for hazardous jobs that require sustained concentration and quick decisions—such as driving fork lifts or operating heavy machinery.
If potential exists for harm, recommend that the employee be treated before you re-evaluate return to work. Ideally, a case manager from the employer’s occupational health provider would check with the employee during treatment to reassess safety factors and facilitate a smooth return to work.
If medical harm is unlikely, recommending time off work becomes “medical discretion” and is not necessarily “medically required.”7
QUESTION 4: Does an impairment prevent the patient from performing essential job functions?
Impairment—a medical term—is often confused with disability, an administrative term:
- Impairment is “a loss, loss of use, or derangement of a body part, organ system, or organ function.”
- Disability is “an alteration of an individual’s capacity to meet personal, social, or occupational demands because of an impairment.”5
The longer a person is away from work with an injury or illness, the less likely he or she will return:
- 50% of persons off work for 8 weeks will not return.
- >85% of persons off work for 6 months will not return to long-term employment and are at risk for long-term disability.1
Unemployment increases mortality rates, physical and mental illness, and use of medical services.2 The unemployed may be more likely than the employed to visit physicians, take medications, or be admitted to hospitals.3
A disability mindset can develop after only 2 to 4 weeks off work, even in capable workers. An estimated 60% to 80% of time away from work is medically unnecessary.4 Returning to work as soon as possible after an illness or injury maximizes health outcomes and ability to function.
An employee who can perform essential job functions despite an impairment should stay at work. If he or she cannot do those functions, clearly state the impairment—such as decreased concentration, problems with persistence and pace—on the medical form so that the employer can decide if an accommodation can be made.
If essential job functions are high-order—such as air traffic control—even slight impairment could prevent the employee from safely doing the job. An impaired air traffic controller probably could do less-complex activities, however, such as clerical work.
Medical discretion. Most depressed patients can follow instructions and complete simple tasks, but many cannot keep up with the usual work pace because of low energy and slowed thinking and movements. Using medical discretion to recommend a short time off might help a depressed person return to full productivity more quickly if intensive treatment is available.
Limit discretionary time off to short periods when a treatment program is available. When blanket restrictions are written, the patient too often sits idle at home, getting worse and not better. At least excuse your patient from work to attend medical appointments and engage in depression treatment.
QUESTION 5: What must occur to get the patient back to work?
Returning to work as soon as possible can be therapeutic. Having a regular routine and daily structure gives the depressed person a sense of normalcy not found while sitting at home. Beyond stating the impairment on the medical form, suggest possible accommodations the employer could make to expedite return to work.
For your depressed patient, you could suggest reduced work hours (to accommodate low energy) or allowing more time to complete tasks. Whatever the diagnosis, addressing conflict in the workplace often helps. Strategies include:
- working individually with your patient
- alerting the patient to the employer’s conflict resolution policies and employee assistance programs.
CASE RESOLUTION: WORK AS THERAPY
Ms. S shows good eye contact, is appropriately dressed, shows no psychomotor abnormalities, and is not suicidal or homicidal. Mental status exam is normal. You determine that she can follow instructions, perform tasks, and keep up with her workload. She can probably do her job but initially might have difficulties because of depression’s effects on socialization and executive functioning.
You encourage Ms. S to return to work for the therapeutic benefits of a daily routine, but you suggest she postpone big projects or major decisions until she feels better.
Reassure your patient when you find no compelling reason why she cannot return to work. Explain that feeling ambivalent about maintaining function at work is normal, and staying at work is crucial to confidence and self-esteem.
Recognize the potential attraction of secondary gain—such as attention from family and medical providers and financial incentives to stay off work—but also normalize the experience for your patient. Help her regain her independence and start thinking about how she can improve her work situation.
Related resources
- Academy of Organizational and Occupational Psychiatry. www.aoop.org.
- National Partnership for Workplace Mental Health. www.workplacementalhealth.org
- Talmage JB, Melhorn JM (eds). A physician’s guide to return to work. Chicago: AMA Press; 2005.
- Fluoxetine • Prozac
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Pilley M. How the primary care physician can help patients negotiate the return-to-work disability dilemma. In: Talmage JB, Melhorn JM, eds. A physician’s guide to return to work. Chicago: AMA Press; 2005:151.
2. Mathers CD, Schofield DJ. The health consequences of unemployment: the evidence. Med J Aust 1998;168:178-82.
3. Jin RL, Shah CP, Svoboda TJ. The impact of unemployment on health: a review of the evidence. Can Med Assoc J 1995;153:529-40.
4. Christian J. Reducing disability days: healing more than the injury. Journal of Workers Compensation 2000;9:30-55.
5. Cocchiarella L, Andersson BJ. Mental and behavioral disorders. In: Cocchiarella L, Andersson BJ, eds. Guides to the evaluation of permanent impairment, 5th ed. Chicago: American Medical Association; 2001:361–4.
6. Enelow AJ. Psychiatric disorders and work function. Psychiatr Ann 1991;21(1):27-35.
7. American College of Occupational and Environmental Medicine. Preventing needless work disability by helping people stay employed. Available at: http://www.acoem.org/position/statements.asp?CATA_ID=100. Accessed Aug. 8, 2006.
8. United States Department of Labor. Office of Disability Employment Policy. Glossary of commonly used terms. Available at: http://www.dol.gov/odep/pubs/ek00/glossary.htm. Accessed Aug. 8, 2006.
1. Pilley M. How the primary care physician can help patients negotiate the return-to-work disability dilemma. In: Talmage JB, Melhorn JM, eds. A physician’s guide to return to work. Chicago: AMA Press; 2005:151.
2. Mathers CD, Schofield DJ. The health consequences of unemployment: the evidence. Med J Aust 1998;168:178-82.
3. Jin RL, Shah CP, Svoboda TJ. The impact of unemployment on health: a review of the evidence. Can Med Assoc J 1995;153:529-40.
4. Christian J. Reducing disability days: healing more than the injury. Journal of Workers Compensation 2000;9:30-55.
5. Cocchiarella L, Andersson BJ. Mental and behavioral disorders. In: Cocchiarella L, Andersson BJ, eds. Guides to the evaluation of permanent impairment, 5th ed. Chicago: American Medical Association; 2001:361–4.
6. Enelow AJ. Psychiatric disorders and work function. Psychiatr Ann 1991;21(1):27-35.
7. American College of Occupational and Environmental Medicine. Preventing needless work disability by helping people stay employed. Available at: http://www.acoem.org/position/statements.asp?CATA_ID=100. Accessed Aug. 8, 2006.
8. United States Department of Labor. Office of Disability Employment Policy. Glossary of commonly used terms. Available at: http://www.dol.gov/odep/pubs/ek00/glossary.htm. Accessed Aug. 8, 2006.
When every minute counts: What workup is sufficient for diagnosis under pressure?
Police officers bring Mr. A, age 25, to the emergency department (ED) in handcuffs after an alleged assault at work. He is calm but will provide no information about himself. ED staff don’t know if he has been using illicit substances, is on medications, or has any medical conditions.
Mr. A says the FBI is after him, but he makes no threats to ED staff. He talks about milking cows on a farm and of hearing animal sounds, though he lives in the city. After about 30 minutes, he consents to a lab draw and provides a urine sample.
Because no charges are pending and Mr. A is semi-cooperative, police remove his handcuffs and leave him in the care of two ED security officers. He is given something to eat and drink and seems fairly content. He asks how long he will need to stay in the room but does not demand to leave.
In a fast-paced ED, physicians might not notice signs of psychiatric illness, such as Mr. A’s paranoid and delusional thinking. By being familiar with techniques to manage patients’ psychiatric emergencies, you can help your ED colleagues:
- establish working psychiatric diagnoses and medical causes of psychiatric symptoms in the fast-paced ED
- maintain a safe ED environment for patients and clinicians.
What ed patients want
To understand how ED patients feel, put yourself in Mr. A’s shoes. You were at work and began to hallucinate. You believed your boss was out to harm you, and in fear you made comments perceived as threatening.
The next thing you know, you’re in a police car with handcuffs on. All of your coworkers witnessed your embarrassment. Now you are in a small ED room, wondering what’s going to happen next. Are you going to be put in a straight jacket and a padded room?
Patients may experience anxiety-provoking thoughts whether they come to the ED voluntarily or involuntarily. Fear and confusion can affect their behavior in the ED, and how providers respond to patients in crisis can escalate or de-escalate an already-difficult situation.
Psychiatric illness in the ed
Mr. A may have a psychiatric disorder, as do at least 3% of patients seen in EDs.1 This figure may be low, however:
- Kunen et al2 asserted that EDs are underdiagnosing psychiatric disorders, given a U.S. Department of Health and Human Services 1999 estimate that 20% to 28% of Americans have psychiatric illnesses. Using ED discharge records across 6 months in three emergency departments, the authors found the psychiatric diagnosis rate to be 5.27% in 33,000 ED visits.
- Another study, done in a university teaching hospital ED, showed that ED physicians trained to focus on patients’ presenting problems often missed comorbid medical or psychiatric illnesses.
In the randomized, controlled trial by Schriger et al,3 218 patients with nonspecific complaints suggesting occult psychiatric illness (such as chronic headache, abdominal pain, or back pain) completed the Primary Care Evaluation of Mental Disorders (PRIME-MD) questionnaire. This 27-item self-report asks questions about mood, alcohol use, obsessive-compulsive symptoms, phobias, and somatoform symptoms.
Participants were then randomly assigned to “report” or “nonreport” groups, depending on whether or not ED physicians received their PRIME-MD scores. Even when informed of patients’ psychiatric symptoms, ED physicians rarely diagnosed or treated psychiatric disorders. Lack of mental status documentation and psychiatric interviews was apparent, the authors noted.
Case continued: a toxic cocktail
Mr. A’s urine drug screen and lab results are positive for benzodiazepines, methamphetamines, and cannabis. The staff decide Mr. A will require further observation and detoxification, and he is told this. A bed is not available at the hospital, however, and calls to nearby facilities find no empty beds.
As time passes, Mr. A shows signs of agitation and arousal. He paces the examination room—his jaw clenched and his face flushed—and begins raising his voice, asking to be discharged.
Recommendations. Unpleasantness is sometimes unavoidable, but no one in the ED has tried to create an alliance with Mr. A (Box). Try to make patients’ ED experiences as positive as possible. Make it clear that you share a common goal: to help the patient feel better. In fact, psychiatric patients and emergency psychiatrists have similar ideas about what constitutes quality ED care. When surveyed,4 ED patients said they preferred:
- verbal interventions compared with medications
- a collaborative approach with ED physicians
- having medications selected for their specific problems, medication experiences, and choices
- benzodiazepines rather than conventional antipsychotics such as haloperidol.
Treat patients with respect, and preserve their sense of dignity
Offer patients choices when reasonable to help them feel they have some control
Strongly (and early) encourage smokers to accept nicotine replacement to avoid withdrawal and heightened arousal
Offer food, beverages, a blanket, or other comfort measures that would not compromise safety (do not give hot coffee, in case the patient throws the cup at someone)
Allow patients to call a loved one, friend, or pastor (offer a cordless phone to avoid strangulation attempts)
Allow relatives or friends to sit and talk with the patient if this would not compromise safety
Keep patients informed on what is going on and why
Answer questions asked by the patient and family or friends
Offer oral medications first
Get to know your security staff well
A pragmatic workup
Medical illnesses such as delirium, stroke, drug toxicity, or urinary tract infections can trigger or worsen psychiatric illness (Table 1).5 Comorbidities such as diabetes, hypertension, obesity, and heart disease are common in patients with psychiatric disorders, and psychotropics can cause or exacerbate these conditions.
In the high-pressure ED, a sufficient workup for complicated medical conditions lies somewhere between extensive/unnecessary and inadequate. Thus, determining an exact diagnosis is not as important as establishing a diagnostic category to guide emergency treatment.
Think of psychiatric disorders as they are organized in DSM-IV-TR—mood, anxiety, psychotic, substance use/withdrawal/intoxication, cognitive, adjustment, somatoform, and personality disorders—and whether they are primary or secondary to a general medical condition or substance use. For example:
- Anxiety disorder secondary to a general medical condition means the history, physical exam, or lab reports suggest a medical condition is the direct physiologic cause of the mood disturbance.
- Methamphetamine-induced psychotic disorder would be the diagnosis if methamphetamines are presumed to be causing a patient’s psychotic symptoms.
Hospitalization. ED staff often develop a treatment plan based on a patient’s clinical picture and a working diagnosis. The plan hinges on deciding if the patient needs to be admitted to the hospital. Admission may be warranted for life-threatening medical conditions or safety issues, such as threats to self or others or inability to care for oneself at home. Other issues come into play—such as starting or changing medications and follow-up to ensure continuity of care—if you decide to discharge the patient.
Even after medical clearance, patients in the psychiatric emergency service may have underlying medical illnesses (Table 2).6
Table 1
Medical disorders that can cause psychiatric symptoms
| Medical/toxic disorders | Examples |
|---|---|
| Alcohol and drugs of abuse | Amphetamines (including methamphetamine), cocaine, heroin, Jimson weed, ketamine, marijuana, MDMA (‘Ecstasy’), LSD, PCP |
| Prescription drugs | Antibiotics, anticholinergics, anticonvulsants, antihypertensives, benzodiazepines, chemotherapeutic agents, cimetidine, corticosteroids, digitalis, narcotics, propranolol, sleep medications, tricyclic antidepressants |
| CNS disease | Hypertensive encephalopathy, intracranial aneurysm, metastases, normal pressure hydrocephalus, postictal nonconvulsive status, primary CNS infection, seizure disorders, stroke, subdural hematoma, tumor |
| Infections | Acute rheumatic fever, diphtheria, malaria, Legionnaires’ disease, pneumonia, Rocky Mountain spotted fever, sepsis, syphilis, typhoid fever, urinary tract infection |
| Metabolic/endocrine disorders | Adrenal disease, diabetic ketoacidosis, hepatic encephalopathy, hypoglycemia, pituitary dysfunction, renal disease, serum electrolyte imbalances (sodium, potassium, calcium), thyroid disease, vitamin deficiencies, Wilson’s disease |
| Cardiopulmonary disease | Arrhythmias, congestive heart failure, COPD/asthma, myocardial infarction, pulmonary embolism |
| Miscellaneous | Anemia, lupus, multiple sclerosis, temporal arteritis, vasculitis |
| Source: Reprinted with permission from Williams ER, Shepherd SM. Medical clearance of psychiatric patients. Emerg Med Clin North Am 2000;18(2):185-90. Copyright 2000, Elsevier. | |
Table 2
Reasonable medical assessment in psychiatric emergencies
| DO |
| Obtain a medical history, the best determinant of medical need |
| Listen to patients. If they say they have a medical condition, believe them; if they say they don’t, try to believe them |
| Thoroughly check vital signs |
| Conduct a focused physical examination |
| Maintain a high index of suspicion |
Be selective with laboratory testing. Check:
|
| DON’T |
| Order blanket laboratory screening |
| Order an ECG in healthy young patients in the absence of clinical findings |
| Order chest radiography in the absence of known disease/exposure/symptoms |
| Source: Reprinted from Currier GW. Medical assessment on the psychiatric emergency service. Psychiatric Issues in Emergency Care Settings 2004;3(July):17, with permission from Cliggott Publishing Group of CMP Healthcare Media. Copyright 2004. |
Overwhelming demand
In the study of ED patient preferences,4 one-fifth of patients said they went to the ED because they lacked access to routine mental health care. Therefore, besides psychiatric conditions caused by medical illnesses, ED physicians can see patients with any primary psychiatric diagnosis, including mood and anxiety disorders and psychosis.
Under pressures of time and limited collateral information, ED staff must:
- individualize psychiatric treatment
- consider use of medications and/or restraints
- rule out life-threatening causes for psychiatric symptoms
- stabilize patients and prevent injury to self and others.
These tasks are becoming increasingly difficult as more and more patients present to emergency rooms. Nationally, ED visits increased from 19 million in 1992 to 108 million in 2000, according to the U.S. Department of Health and Human Services.1
Psychiatric patients are seeking ED care in greater numbers, and the number of those staying longer than anticipated (“boarding”) also has increased, according to a 2004 survey of 340 physicians by the American College of Emergency Physicians, American Psychiatric Association, National Mental Health Association, and National Alliance for the Mentally Ill. Surveyed physicians blamed inadequate Medicaid funding and bed shortages for the increasing ED visits.7
In crowded emergency rooms, where patients wait longer and longer to be seen, the influx of acutely ill psychiatric patients increases the risks of agitation, violence, and injury, as well as litigation.8
Case continued: going up in smoke
Recognizing Mr. A’s arousal, ED staff tries to reassure him and offers him food, something to drink, a phone Call, and a magazine. When these attempts fail to de-escalate his agitation, staff offers to make him more comfortable by giving oral lorazepam, which he adamantly refuses. He is told again that he must stay until a transfer facility is found for him.
Mr. A then demands to go outside “for a smoke.” When he is told ED patients cannot leave to smoke and is offered nicotine replacement, he begins to scream and lunges at one of the security officers. He is extremely strong, and additional officers are summoned. He retreats inside the room, slams the door, shatters the door window with a chair, and begins punching the broken glass. He slides to the floor in a vasovagal reaction at the sight of his bleeding hands but soon becomes combative again.
Staff give Mr. A IM haloperidol, 10 mg, and lorazepam, 2 mg, to manage his extreme agitation and place him in physical restraints to protect him and others. Within 25 to 30 minutes he is calm, and a safe environment has been re-established. The lacerations on his hands are sutured, and he is admitted to an inpatient psychiatric hospital for further stabilization and treatment.
No place for complacency
Mr. A’s experience illustrates how situations can become dangerous when precautions are not taken. Five steps can help you prepare and protect yourself when evaluating patients in the ED:
- seek the patient history
- evaluate the context in which the patient is being assessed
- identify arousal states (fear, anger, confusion, and humiliation)
- structure the interview for safety
- keep your guard up during the clinical encounter.9
Risk is high when law enforcement officers bring a patient to the ED. Be on guard, even if the patient is 80 years old and in a wheelchair. Complacency has no place in the ED; prepare as much as you can before interviewing the patient.
When restraints are needed. Involuntary medication and/or restraints may be necessary when reasonable interventions have failed, the patient will not cooperate, and he or she is exhibiting behavior/symptoms that could result in injury. Approximately 10% to 20% of psychiatric patients require physical or chemical restraint in the ED.10
Expert consensus guidelines suggest starting with verbal intervention, voluntary medication, and show of force, although emergency medication may be a reasonable first treatment (Algorithm).11 Offer oral medication first; IM medications carry risks including acute dystonia and akathisia, although these can be treated.
Lorazepam, 1 to 2 mg oral/IM, combined with haloperidol, 2 to 5 mg oral/IM, is a reasonable start in most cases. If the patient remains extremely agitated, the same medications and dosages can be repeated 30 to 60 minutes after the initial administration.12
Conventional oral/IM agents are usually more readily available in the ED than atypical antipsychotics, which must be ordered from the pharmacy. Recent FDA black-box warnings also emphasize that atypical antipsychotics are approved only for treating schizophrenia, acute manic and mixed episodes of bipolar I disorder, and for maintenance treatment in bipolar disorder. When compared with placebo, atypical antipsychotics have been associated with:
- increased risk for cerebrovascular events in elderly patients with dementia
- death in elderly patients with dementia-related psychosis.
Atypicals may be more appropriate than conventional antipsychotics for emergency treatment of agitation and aggression in some patients with complicating medical conditions or histories. For example, avoid high-potency conventional antipsychotics in patients with a history of extrapyramidal side effects and in those with mental retardation/developmental delay.11 Similarly, avoid benzodiazepines in patients with chronic obstructive pulmonary disease (COPD) or a history of drug-seeking behavior or drug abuse.
Of course not all psychiatric interventions in the ED are involuntary. For example, the ED physician may start an antidepressant for a patient diagnosed with mild to moderate depression for whom hospitalization is not indicated. Characteristics of patients who may be good candidates for starting antidepressants in the ED include a clear diagnosis, no substance abuse, low suicide risk, no psychosis or agitation, available social supports, clear follow-up plan, desire to begin treatment, and ability to pay for and obtain medications.13
Algorithm Consensus guideline for treating a behavioral emergency
Related resources
- Allen MH, Currier GW, Hughes DH, et al. The Expert Consensus Guideline Series: Treatment of behavioral emergencies. Postgrad Med 2001;May(Spec No):1-88.
- American College of Emergency Physicians. www.acep.org
- National Alliance on Mental Illness. www.nami.org
Drug brand names
- Fluoxetine • Prozac
- Haloperidol • Haldol
- Lorazepam • Ativan
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. McCaig LF, Ly N. National Hospital Ambulatory Medical Care Survey: 2000 emergency department summary. Adv Data 2002;327:1-27.
2. Kunen S, Niederhauser R, Smith PO, et al. Race disparities in psychiatric rates in emergency departments. J Consult Clin Psychol 2005;73(1):116-126.
3. Schriger DL, Gibbons PS, Langone CA, et al. Enabling the diagnosis of occult psychiatric illness in the emergency department: a randomized, controlled trial of the computerized, self-administered PRIME-MD diagnostic system. Ann Emerg Med 2001;37(2):132-40.
4. Allen M, Carpenter D, Sheets JL, et al. What do consumers say they want and need during a psychiatric emergency? J Psychiatr Pract 2003;9(1):39-58.
5. Williams ER, Shepherd SM. Medical clearance of psychiatric patients. Emerg Med Clin North Am 2000;18(2):185-98.
6. Allen MH, Currier GW. Medical assessment on the psychiatric emergency service. New Dir Ment Health Serv 1999;82:21-8.
7. Mulligan K. ER docs report large increase in psychiatric patients. Psychiatr News 2004;39(12):10.-
8. Karcz A, Holbrook J, Auerbach BS, et al. Preventability of malpractice claims in emergency medicine: a closed claims study. Ann Emerg Med 1990;19(8):865-73.
9. Battaglia J. Is this patient dangerous? 5 steps to assess risk for violence. Current Psychiatry 2004;3(2):14-21.
10. De Fruyt J, Demyttenaere K. Rapid tranquilization: new approaches in the emergency treatment of behavioral disturbances. Eur Psychiatry 2004;19:243-9.
11. Allen MH, Currier GW, Hughes DH, et al. The Expert Consensus Guideline Series: Treatment of behavioral emergencies. Postgrad Med 2001;May(Spec No):1-88.
12. Hughes DH. Acute psychopharmacological management of the aggressive psychotic patient. Psychiatr Serv 1999;50(9):1135-7.
13. Glick RL. Starting antidepressant treatment in the emergency setting. Psychiatric Issues in Emergency Care Settings 2004;3(2):6-10.
Police officers bring Mr. A, age 25, to the emergency department (ED) in handcuffs after an alleged assault at work. He is calm but will provide no information about himself. ED staff don’t know if he has been using illicit substances, is on medications, or has any medical conditions.
Mr. A says the FBI is after him, but he makes no threats to ED staff. He talks about milking cows on a farm and of hearing animal sounds, though he lives in the city. After about 30 minutes, he consents to a lab draw and provides a urine sample.
Because no charges are pending and Mr. A is semi-cooperative, police remove his handcuffs and leave him in the care of two ED security officers. He is given something to eat and drink and seems fairly content. He asks how long he will need to stay in the room but does not demand to leave.
In a fast-paced ED, physicians might not notice signs of psychiatric illness, such as Mr. A’s paranoid and delusional thinking. By being familiar with techniques to manage patients’ psychiatric emergencies, you can help your ED colleagues:
- establish working psychiatric diagnoses and medical causes of psychiatric symptoms in the fast-paced ED
- maintain a safe ED environment for patients and clinicians.
What ed patients want
To understand how ED patients feel, put yourself in Mr. A’s shoes. You were at work and began to hallucinate. You believed your boss was out to harm you, and in fear you made comments perceived as threatening.
The next thing you know, you’re in a police car with handcuffs on. All of your coworkers witnessed your embarrassment. Now you are in a small ED room, wondering what’s going to happen next. Are you going to be put in a straight jacket and a padded room?
Patients may experience anxiety-provoking thoughts whether they come to the ED voluntarily or involuntarily. Fear and confusion can affect their behavior in the ED, and how providers respond to patients in crisis can escalate or de-escalate an already-difficult situation.
Psychiatric illness in the ed
Mr. A may have a psychiatric disorder, as do at least 3% of patients seen in EDs.1 This figure may be low, however:
- Kunen et al2 asserted that EDs are underdiagnosing psychiatric disorders, given a U.S. Department of Health and Human Services 1999 estimate that 20% to 28% of Americans have psychiatric illnesses. Using ED discharge records across 6 months in three emergency departments, the authors found the psychiatric diagnosis rate to be 5.27% in 33,000 ED visits.
- Another study, done in a university teaching hospital ED, showed that ED physicians trained to focus on patients’ presenting problems often missed comorbid medical or psychiatric illnesses.
In the randomized, controlled trial by Schriger et al,3 218 patients with nonspecific complaints suggesting occult psychiatric illness (such as chronic headache, abdominal pain, or back pain) completed the Primary Care Evaluation of Mental Disorders (PRIME-MD) questionnaire. This 27-item self-report asks questions about mood, alcohol use, obsessive-compulsive symptoms, phobias, and somatoform symptoms.
Participants were then randomly assigned to “report” or “nonreport” groups, depending on whether or not ED physicians received their PRIME-MD scores. Even when informed of patients’ psychiatric symptoms, ED physicians rarely diagnosed or treated psychiatric disorders. Lack of mental status documentation and psychiatric interviews was apparent, the authors noted.
Case continued: a toxic cocktail
Mr. A’s urine drug screen and lab results are positive for benzodiazepines, methamphetamines, and cannabis. The staff decide Mr. A will require further observation and detoxification, and he is told this. A bed is not available at the hospital, however, and calls to nearby facilities find no empty beds.
As time passes, Mr. A shows signs of agitation and arousal. He paces the examination room—his jaw clenched and his face flushed—and begins raising his voice, asking to be discharged.
Recommendations. Unpleasantness is sometimes unavoidable, but no one in the ED has tried to create an alliance with Mr. A (Box). Try to make patients’ ED experiences as positive as possible. Make it clear that you share a common goal: to help the patient feel better. In fact, psychiatric patients and emergency psychiatrists have similar ideas about what constitutes quality ED care. When surveyed,4 ED patients said they preferred:
- verbal interventions compared with medications
- a collaborative approach with ED physicians
- having medications selected for their specific problems, medication experiences, and choices
- benzodiazepines rather than conventional antipsychotics such as haloperidol.
Treat patients with respect, and preserve their sense of dignity
Offer patients choices when reasonable to help them feel they have some control
Strongly (and early) encourage smokers to accept nicotine replacement to avoid withdrawal and heightened arousal
Offer food, beverages, a blanket, or other comfort measures that would not compromise safety (do not give hot coffee, in case the patient throws the cup at someone)
Allow patients to call a loved one, friend, or pastor (offer a cordless phone to avoid strangulation attempts)
Allow relatives or friends to sit and talk with the patient if this would not compromise safety
Keep patients informed on what is going on and why
Answer questions asked by the patient and family or friends
Offer oral medications first
Get to know your security staff well
A pragmatic workup
Medical illnesses such as delirium, stroke, drug toxicity, or urinary tract infections can trigger or worsen psychiatric illness (Table 1).5 Comorbidities such as diabetes, hypertension, obesity, and heart disease are common in patients with psychiatric disorders, and psychotropics can cause or exacerbate these conditions.
In the high-pressure ED, a sufficient workup for complicated medical conditions lies somewhere between extensive/unnecessary and inadequate. Thus, determining an exact diagnosis is not as important as establishing a diagnostic category to guide emergency treatment.
Think of psychiatric disorders as they are organized in DSM-IV-TR—mood, anxiety, psychotic, substance use/withdrawal/intoxication, cognitive, adjustment, somatoform, and personality disorders—and whether they are primary or secondary to a general medical condition or substance use. For example:
- Anxiety disorder secondary to a general medical condition means the history, physical exam, or lab reports suggest a medical condition is the direct physiologic cause of the mood disturbance.
- Methamphetamine-induced psychotic disorder would be the diagnosis if methamphetamines are presumed to be causing a patient’s psychotic symptoms.
Hospitalization. ED staff often develop a treatment plan based on a patient’s clinical picture and a working diagnosis. The plan hinges on deciding if the patient needs to be admitted to the hospital. Admission may be warranted for life-threatening medical conditions or safety issues, such as threats to self or others or inability to care for oneself at home. Other issues come into play—such as starting or changing medications and follow-up to ensure continuity of care—if you decide to discharge the patient.
Even after medical clearance, patients in the psychiatric emergency service may have underlying medical illnesses (Table 2).6
Table 1
Medical disorders that can cause psychiatric symptoms
| Medical/toxic disorders | Examples |
|---|---|
| Alcohol and drugs of abuse | Amphetamines (including methamphetamine), cocaine, heroin, Jimson weed, ketamine, marijuana, MDMA (‘Ecstasy’), LSD, PCP |
| Prescription drugs | Antibiotics, anticholinergics, anticonvulsants, antihypertensives, benzodiazepines, chemotherapeutic agents, cimetidine, corticosteroids, digitalis, narcotics, propranolol, sleep medications, tricyclic antidepressants |
| CNS disease | Hypertensive encephalopathy, intracranial aneurysm, metastases, normal pressure hydrocephalus, postictal nonconvulsive status, primary CNS infection, seizure disorders, stroke, subdural hematoma, tumor |
| Infections | Acute rheumatic fever, diphtheria, malaria, Legionnaires’ disease, pneumonia, Rocky Mountain spotted fever, sepsis, syphilis, typhoid fever, urinary tract infection |
| Metabolic/endocrine disorders | Adrenal disease, diabetic ketoacidosis, hepatic encephalopathy, hypoglycemia, pituitary dysfunction, renal disease, serum electrolyte imbalances (sodium, potassium, calcium), thyroid disease, vitamin deficiencies, Wilson’s disease |
| Cardiopulmonary disease | Arrhythmias, congestive heart failure, COPD/asthma, myocardial infarction, pulmonary embolism |
| Miscellaneous | Anemia, lupus, multiple sclerosis, temporal arteritis, vasculitis |
| Source: Reprinted with permission from Williams ER, Shepherd SM. Medical clearance of psychiatric patients. Emerg Med Clin North Am 2000;18(2):185-90. Copyright 2000, Elsevier. | |
Table 2
Reasonable medical assessment in psychiatric emergencies
| DO |
| Obtain a medical history, the best determinant of medical need |
| Listen to patients. If they say they have a medical condition, believe them; if they say they don’t, try to believe them |
| Thoroughly check vital signs |
| Conduct a focused physical examination |
| Maintain a high index of suspicion |
Be selective with laboratory testing. Check:
|
| DON’T |
| Order blanket laboratory screening |
| Order an ECG in healthy young patients in the absence of clinical findings |
| Order chest radiography in the absence of known disease/exposure/symptoms |
| Source: Reprinted from Currier GW. Medical assessment on the psychiatric emergency service. Psychiatric Issues in Emergency Care Settings 2004;3(July):17, with permission from Cliggott Publishing Group of CMP Healthcare Media. Copyright 2004. |
Overwhelming demand
In the study of ED patient preferences,4 one-fifth of patients said they went to the ED because they lacked access to routine mental health care. Therefore, besides psychiatric conditions caused by medical illnesses, ED physicians can see patients with any primary psychiatric diagnosis, including mood and anxiety disorders and psychosis.
Under pressures of time and limited collateral information, ED staff must:
- individualize psychiatric treatment
- consider use of medications and/or restraints
- rule out life-threatening causes for psychiatric symptoms
- stabilize patients and prevent injury to self and others.
These tasks are becoming increasingly difficult as more and more patients present to emergency rooms. Nationally, ED visits increased from 19 million in 1992 to 108 million in 2000, according to the U.S. Department of Health and Human Services.1
Psychiatric patients are seeking ED care in greater numbers, and the number of those staying longer than anticipated (“boarding”) also has increased, according to a 2004 survey of 340 physicians by the American College of Emergency Physicians, American Psychiatric Association, National Mental Health Association, and National Alliance for the Mentally Ill. Surveyed physicians blamed inadequate Medicaid funding and bed shortages for the increasing ED visits.7
In crowded emergency rooms, where patients wait longer and longer to be seen, the influx of acutely ill psychiatric patients increases the risks of agitation, violence, and injury, as well as litigation.8
Case continued: going up in smoke
Recognizing Mr. A’s arousal, ED staff tries to reassure him and offers him food, something to drink, a phone Call, and a magazine. When these attempts fail to de-escalate his agitation, staff offers to make him more comfortable by giving oral lorazepam, which he adamantly refuses. He is told again that he must stay until a transfer facility is found for him.
Mr. A then demands to go outside “for a smoke.” When he is told ED patients cannot leave to smoke and is offered nicotine replacement, he begins to scream and lunges at one of the security officers. He is extremely strong, and additional officers are summoned. He retreats inside the room, slams the door, shatters the door window with a chair, and begins punching the broken glass. He slides to the floor in a vasovagal reaction at the sight of his bleeding hands but soon becomes combative again.
Staff give Mr. A IM haloperidol, 10 mg, and lorazepam, 2 mg, to manage his extreme agitation and place him in physical restraints to protect him and others. Within 25 to 30 minutes he is calm, and a safe environment has been re-established. The lacerations on his hands are sutured, and he is admitted to an inpatient psychiatric hospital for further stabilization and treatment.
No place for complacency
Mr. A’s experience illustrates how situations can become dangerous when precautions are not taken. Five steps can help you prepare and protect yourself when evaluating patients in the ED:
- seek the patient history
- evaluate the context in which the patient is being assessed
- identify arousal states (fear, anger, confusion, and humiliation)
- structure the interview for safety
- keep your guard up during the clinical encounter.9
Risk is high when law enforcement officers bring a patient to the ED. Be on guard, even if the patient is 80 years old and in a wheelchair. Complacency has no place in the ED; prepare as much as you can before interviewing the patient.
When restraints are needed. Involuntary medication and/or restraints may be necessary when reasonable interventions have failed, the patient will not cooperate, and he or she is exhibiting behavior/symptoms that could result in injury. Approximately 10% to 20% of psychiatric patients require physical or chemical restraint in the ED.10
Expert consensus guidelines suggest starting with verbal intervention, voluntary medication, and show of force, although emergency medication may be a reasonable first treatment (Algorithm).11 Offer oral medication first; IM medications carry risks including acute dystonia and akathisia, although these can be treated.
Lorazepam, 1 to 2 mg oral/IM, combined with haloperidol, 2 to 5 mg oral/IM, is a reasonable start in most cases. If the patient remains extremely agitated, the same medications and dosages can be repeated 30 to 60 minutes after the initial administration.12
Conventional oral/IM agents are usually more readily available in the ED than atypical antipsychotics, which must be ordered from the pharmacy. Recent FDA black-box warnings also emphasize that atypical antipsychotics are approved only for treating schizophrenia, acute manic and mixed episodes of bipolar I disorder, and for maintenance treatment in bipolar disorder. When compared with placebo, atypical antipsychotics have been associated with:
- increased risk for cerebrovascular events in elderly patients with dementia
- death in elderly patients with dementia-related psychosis.
Atypicals may be more appropriate than conventional antipsychotics for emergency treatment of agitation and aggression in some patients with complicating medical conditions or histories. For example, avoid high-potency conventional antipsychotics in patients with a history of extrapyramidal side effects and in those with mental retardation/developmental delay.11 Similarly, avoid benzodiazepines in patients with chronic obstructive pulmonary disease (COPD) or a history of drug-seeking behavior or drug abuse.
Of course not all psychiatric interventions in the ED are involuntary. For example, the ED physician may start an antidepressant for a patient diagnosed with mild to moderate depression for whom hospitalization is not indicated. Characteristics of patients who may be good candidates for starting antidepressants in the ED include a clear diagnosis, no substance abuse, low suicide risk, no psychosis or agitation, available social supports, clear follow-up plan, desire to begin treatment, and ability to pay for and obtain medications.13
Algorithm Consensus guideline for treating a behavioral emergency
Related resources
- Allen MH, Currier GW, Hughes DH, et al. The Expert Consensus Guideline Series: Treatment of behavioral emergencies. Postgrad Med 2001;May(Spec No):1-88.
- American College of Emergency Physicians. www.acep.org
- National Alliance on Mental Illness. www.nami.org
Drug brand names
- Fluoxetine • Prozac
- Haloperidol • Haldol
- Lorazepam • Ativan
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Police officers bring Mr. A, age 25, to the emergency department (ED) in handcuffs after an alleged assault at work. He is calm but will provide no information about himself. ED staff don’t know if he has been using illicit substances, is on medications, or has any medical conditions.
Mr. A says the FBI is after him, but he makes no threats to ED staff. He talks about milking cows on a farm and of hearing animal sounds, though he lives in the city. After about 30 minutes, he consents to a lab draw and provides a urine sample.
Because no charges are pending and Mr. A is semi-cooperative, police remove his handcuffs and leave him in the care of two ED security officers. He is given something to eat and drink and seems fairly content. He asks how long he will need to stay in the room but does not demand to leave.
In a fast-paced ED, physicians might not notice signs of psychiatric illness, such as Mr. A’s paranoid and delusional thinking. By being familiar with techniques to manage patients’ psychiatric emergencies, you can help your ED colleagues:
- establish working psychiatric diagnoses and medical causes of psychiatric symptoms in the fast-paced ED
- maintain a safe ED environment for patients and clinicians.
What ed patients want
To understand how ED patients feel, put yourself in Mr. A’s shoes. You were at work and began to hallucinate. You believed your boss was out to harm you, and in fear you made comments perceived as threatening.
The next thing you know, you’re in a police car with handcuffs on. All of your coworkers witnessed your embarrassment. Now you are in a small ED room, wondering what’s going to happen next. Are you going to be put in a straight jacket and a padded room?
Patients may experience anxiety-provoking thoughts whether they come to the ED voluntarily or involuntarily. Fear and confusion can affect their behavior in the ED, and how providers respond to patients in crisis can escalate or de-escalate an already-difficult situation.
Psychiatric illness in the ed
Mr. A may have a psychiatric disorder, as do at least 3% of patients seen in EDs.1 This figure may be low, however:
- Kunen et al2 asserted that EDs are underdiagnosing psychiatric disorders, given a U.S. Department of Health and Human Services 1999 estimate that 20% to 28% of Americans have psychiatric illnesses. Using ED discharge records across 6 months in three emergency departments, the authors found the psychiatric diagnosis rate to be 5.27% in 33,000 ED visits.
- Another study, done in a university teaching hospital ED, showed that ED physicians trained to focus on patients’ presenting problems often missed comorbid medical or psychiatric illnesses.
In the randomized, controlled trial by Schriger et al,3 218 patients with nonspecific complaints suggesting occult psychiatric illness (such as chronic headache, abdominal pain, or back pain) completed the Primary Care Evaluation of Mental Disorders (PRIME-MD) questionnaire. This 27-item self-report asks questions about mood, alcohol use, obsessive-compulsive symptoms, phobias, and somatoform symptoms.
Participants were then randomly assigned to “report” or “nonreport” groups, depending on whether or not ED physicians received their PRIME-MD scores. Even when informed of patients’ psychiatric symptoms, ED physicians rarely diagnosed or treated psychiatric disorders. Lack of mental status documentation and psychiatric interviews was apparent, the authors noted.
Case continued: a toxic cocktail
Mr. A’s urine drug screen and lab results are positive for benzodiazepines, methamphetamines, and cannabis. The staff decide Mr. A will require further observation and detoxification, and he is told this. A bed is not available at the hospital, however, and calls to nearby facilities find no empty beds.
As time passes, Mr. A shows signs of agitation and arousal. He paces the examination room—his jaw clenched and his face flushed—and begins raising his voice, asking to be discharged.
Recommendations. Unpleasantness is sometimes unavoidable, but no one in the ED has tried to create an alliance with Mr. A (Box). Try to make patients’ ED experiences as positive as possible. Make it clear that you share a common goal: to help the patient feel better. In fact, psychiatric patients and emergency psychiatrists have similar ideas about what constitutes quality ED care. When surveyed,4 ED patients said they preferred:
- verbal interventions compared with medications
- a collaborative approach with ED physicians
- having medications selected for their specific problems, medication experiences, and choices
- benzodiazepines rather than conventional antipsychotics such as haloperidol.
Treat patients with respect, and preserve their sense of dignity
Offer patients choices when reasonable to help them feel they have some control
Strongly (and early) encourage smokers to accept nicotine replacement to avoid withdrawal and heightened arousal
Offer food, beverages, a blanket, or other comfort measures that would not compromise safety (do not give hot coffee, in case the patient throws the cup at someone)
Allow patients to call a loved one, friend, or pastor (offer a cordless phone to avoid strangulation attempts)
Allow relatives or friends to sit and talk with the patient if this would not compromise safety
Keep patients informed on what is going on and why
Answer questions asked by the patient and family or friends
Offer oral medications first
Get to know your security staff well
A pragmatic workup
Medical illnesses such as delirium, stroke, drug toxicity, or urinary tract infections can trigger or worsen psychiatric illness (Table 1).5 Comorbidities such as diabetes, hypertension, obesity, and heart disease are common in patients with psychiatric disorders, and psychotropics can cause or exacerbate these conditions.
In the high-pressure ED, a sufficient workup for complicated medical conditions lies somewhere between extensive/unnecessary and inadequate. Thus, determining an exact diagnosis is not as important as establishing a diagnostic category to guide emergency treatment.
Think of psychiatric disorders as they are organized in DSM-IV-TR—mood, anxiety, psychotic, substance use/withdrawal/intoxication, cognitive, adjustment, somatoform, and personality disorders—and whether they are primary or secondary to a general medical condition or substance use. For example:
- Anxiety disorder secondary to a general medical condition means the history, physical exam, or lab reports suggest a medical condition is the direct physiologic cause of the mood disturbance.
- Methamphetamine-induced psychotic disorder would be the diagnosis if methamphetamines are presumed to be causing a patient’s psychotic symptoms.
Hospitalization. ED staff often develop a treatment plan based on a patient’s clinical picture and a working diagnosis. The plan hinges on deciding if the patient needs to be admitted to the hospital. Admission may be warranted for life-threatening medical conditions or safety issues, such as threats to self or others or inability to care for oneself at home. Other issues come into play—such as starting or changing medications and follow-up to ensure continuity of care—if you decide to discharge the patient.
Even after medical clearance, patients in the psychiatric emergency service may have underlying medical illnesses (Table 2).6
Table 1
Medical disorders that can cause psychiatric symptoms
| Medical/toxic disorders | Examples |
|---|---|
| Alcohol and drugs of abuse | Amphetamines (including methamphetamine), cocaine, heroin, Jimson weed, ketamine, marijuana, MDMA (‘Ecstasy’), LSD, PCP |
| Prescription drugs | Antibiotics, anticholinergics, anticonvulsants, antihypertensives, benzodiazepines, chemotherapeutic agents, cimetidine, corticosteroids, digitalis, narcotics, propranolol, sleep medications, tricyclic antidepressants |
| CNS disease | Hypertensive encephalopathy, intracranial aneurysm, metastases, normal pressure hydrocephalus, postictal nonconvulsive status, primary CNS infection, seizure disorders, stroke, subdural hematoma, tumor |
| Infections | Acute rheumatic fever, diphtheria, malaria, Legionnaires’ disease, pneumonia, Rocky Mountain spotted fever, sepsis, syphilis, typhoid fever, urinary tract infection |
| Metabolic/endocrine disorders | Adrenal disease, diabetic ketoacidosis, hepatic encephalopathy, hypoglycemia, pituitary dysfunction, renal disease, serum electrolyte imbalances (sodium, potassium, calcium), thyroid disease, vitamin deficiencies, Wilson’s disease |
| Cardiopulmonary disease | Arrhythmias, congestive heart failure, COPD/asthma, myocardial infarction, pulmonary embolism |
| Miscellaneous | Anemia, lupus, multiple sclerosis, temporal arteritis, vasculitis |
| Source: Reprinted with permission from Williams ER, Shepherd SM. Medical clearance of psychiatric patients. Emerg Med Clin North Am 2000;18(2):185-90. Copyright 2000, Elsevier. | |
Table 2
Reasonable medical assessment in psychiatric emergencies
| DO |
| Obtain a medical history, the best determinant of medical need |
| Listen to patients. If they say they have a medical condition, believe them; if they say they don’t, try to believe them |
| Thoroughly check vital signs |
| Conduct a focused physical examination |
| Maintain a high index of suspicion |
Be selective with laboratory testing. Check:
|
| DON’T |
| Order blanket laboratory screening |
| Order an ECG in healthy young patients in the absence of clinical findings |
| Order chest radiography in the absence of known disease/exposure/symptoms |
| Source: Reprinted from Currier GW. Medical assessment on the psychiatric emergency service. Psychiatric Issues in Emergency Care Settings 2004;3(July):17, with permission from Cliggott Publishing Group of CMP Healthcare Media. Copyright 2004. |
Overwhelming demand
In the study of ED patient preferences,4 one-fifth of patients said they went to the ED because they lacked access to routine mental health care. Therefore, besides psychiatric conditions caused by medical illnesses, ED physicians can see patients with any primary psychiatric diagnosis, including mood and anxiety disorders and psychosis.
Under pressures of time and limited collateral information, ED staff must:
- individualize psychiatric treatment
- consider use of medications and/or restraints
- rule out life-threatening causes for psychiatric symptoms
- stabilize patients and prevent injury to self and others.
These tasks are becoming increasingly difficult as more and more patients present to emergency rooms. Nationally, ED visits increased from 19 million in 1992 to 108 million in 2000, according to the U.S. Department of Health and Human Services.1
Psychiatric patients are seeking ED care in greater numbers, and the number of those staying longer than anticipated (“boarding”) also has increased, according to a 2004 survey of 340 physicians by the American College of Emergency Physicians, American Psychiatric Association, National Mental Health Association, and National Alliance for the Mentally Ill. Surveyed physicians blamed inadequate Medicaid funding and bed shortages for the increasing ED visits.7
In crowded emergency rooms, where patients wait longer and longer to be seen, the influx of acutely ill psychiatric patients increases the risks of agitation, violence, and injury, as well as litigation.8
Case continued: going up in smoke
Recognizing Mr. A’s arousal, ED staff tries to reassure him and offers him food, something to drink, a phone Call, and a magazine. When these attempts fail to de-escalate his agitation, staff offers to make him more comfortable by giving oral lorazepam, which he adamantly refuses. He is told again that he must stay until a transfer facility is found for him.
Mr. A then demands to go outside “for a smoke.” When he is told ED patients cannot leave to smoke and is offered nicotine replacement, he begins to scream and lunges at one of the security officers. He is extremely strong, and additional officers are summoned. He retreats inside the room, slams the door, shatters the door window with a chair, and begins punching the broken glass. He slides to the floor in a vasovagal reaction at the sight of his bleeding hands but soon becomes combative again.
Staff give Mr. A IM haloperidol, 10 mg, and lorazepam, 2 mg, to manage his extreme agitation and place him in physical restraints to protect him and others. Within 25 to 30 minutes he is calm, and a safe environment has been re-established. The lacerations on his hands are sutured, and he is admitted to an inpatient psychiatric hospital for further stabilization and treatment.
No place for complacency
Mr. A’s experience illustrates how situations can become dangerous when precautions are not taken. Five steps can help you prepare and protect yourself when evaluating patients in the ED:
- seek the patient history
- evaluate the context in which the patient is being assessed
- identify arousal states (fear, anger, confusion, and humiliation)
- structure the interview for safety
- keep your guard up during the clinical encounter.9
Risk is high when law enforcement officers bring a patient to the ED. Be on guard, even if the patient is 80 years old and in a wheelchair. Complacency has no place in the ED; prepare as much as you can before interviewing the patient.
When restraints are needed. Involuntary medication and/or restraints may be necessary when reasonable interventions have failed, the patient will not cooperate, and he or she is exhibiting behavior/symptoms that could result in injury. Approximately 10% to 20% of psychiatric patients require physical or chemical restraint in the ED.10
Expert consensus guidelines suggest starting with verbal intervention, voluntary medication, and show of force, although emergency medication may be a reasonable first treatment (Algorithm).11 Offer oral medication first; IM medications carry risks including acute dystonia and akathisia, although these can be treated.
Lorazepam, 1 to 2 mg oral/IM, combined with haloperidol, 2 to 5 mg oral/IM, is a reasonable start in most cases. If the patient remains extremely agitated, the same medications and dosages can be repeated 30 to 60 minutes after the initial administration.12
Conventional oral/IM agents are usually more readily available in the ED than atypical antipsychotics, which must be ordered from the pharmacy. Recent FDA black-box warnings also emphasize that atypical antipsychotics are approved only for treating schizophrenia, acute manic and mixed episodes of bipolar I disorder, and for maintenance treatment in bipolar disorder. When compared with placebo, atypical antipsychotics have been associated with:
- increased risk for cerebrovascular events in elderly patients with dementia
- death in elderly patients with dementia-related psychosis.
Atypicals may be more appropriate than conventional antipsychotics for emergency treatment of agitation and aggression in some patients with complicating medical conditions or histories. For example, avoid high-potency conventional antipsychotics in patients with a history of extrapyramidal side effects and in those with mental retardation/developmental delay.11 Similarly, avoid benzodiazepines in patients with chronic obstructive pulmonary disease (COPD) or a history of drug-seeking behavior or drug abuse.
Of course not all psychiatric interventions in the ED are involuntary. For example, the ED physician may start an antidepressant for a patient diagnosed with mild to moderate depression for whom hospitalization is not indicated. Characteristics of patients who may be good candidates for starting antidepressants in the ED include a clear diagnosis, no substance abuse, low suicide risk, no psychosis or agitation, available social supports, clear follow-up plan, desire to begin treatment, and ability to pay for and obtain medications.13
Algorithm Consensus guideline for treating a behavioral emergency
Related resources
- Allen MH, Currier GW, Hughes DH, et al. The Expert Consensus Guideline Series: Treatment of behavioral emergencies. Postgrad Med 2001;May(Spec No):1-88.
- American College of Emergency Physicians. www.acep.org
- National Alliance on Mental Illness. www.nami.org
Drug brand names
- Fluoxetine • Prozac
- Haloperidol • Haldol
- Lorazepam • Ativan
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. McCaig LF, Ly N. National Hospital Ambulatory Medical Care Survey: 2000 emergency department summary. Adv Data 2002;327:1-27.
2. Kunen S, Niederhauser R, Smith PO, et al. Race disparities in psychiatric rates in emergency departments. J Consult Clin Psychol 2005;73(1):116-126.
3. Schriger DL, Gibbons PS, Langone CA, et al. Enabling the diagnosis of occult psychiatric illness in the emergency department: a randomized, controlled trial of the computerized, self-administered PRIME-MD diagnostic system. Ann Emerg Med 2001;37(2):132-40.
4. Allen M, Carpenter D, Sheets JL, et al. What do consumers say they want and need during a psychiatric emergency? J Psychiatr Pract 2003;9(1):39-58.
5. Williams ER, Shepherd SM. Medical clearance of psychiatric patients. Emerg Med Clin North Am 2000;18(2):185-98.
6. Allen MH, Currier GW. Medical assessment on the psychiatric emergency service. New Dir Ment Health Serv 1999;82:21-8.
7. Mulligan K. ER docs report large increase in psychiatric patients. Psychiatr News 2004;39(12):10.-
8. Karcz A, Holbrook J, Auerbach BS, et al. Preventability of malpractice claims in emergency medicine: a closed claims study. Ann Emerg Med 1990;19(8):865-73.
9. Battaglia J. Is this patient dangerous? 5 steps to assess risk for violence. Current Psychiatry 2004;3(2):14-21.
10. De Fruyt J, Demyttenaere K. Rapid tranquilization: new approaches in the emergency treatment of behavioral disturbances. Eur Psychiatry 2004;19:243-9.
11. Allen MH, Currier GW, Hughes DH, et al. The Expert Consensus Guideline Series: Treatment of behavioral emergencies. Postgrad Med 2001;May(Spec No):1-88.
12. Hughes DH. Acute psychopharmacological management of the aggressive psychotic patient. Psychiatr Serv 1999;50(9):1135-7.
13. Glick RL. Starting antidepressant treatment in the emergency setting. Psychiatric Issues in Emergency Care Settings 2004;3(2):6-10.
1. McCaig LF, Ly N. National Hospital Ambulatory Medical Care Survey: 2000 emergency department summary. Adv Data 2002;327:1-27.
2. Kunen S, Niederhauser R, Smith PO, et al. Race disparities in psychiatric rates in emergency departments. J Consult Clin Psychol 2005;73(1):116-126.
3. Schriger DL, Gibbons PS, Langone CA, et al. Enabling the diagnosis of occult psychiatric illness in the emergency department: a randomized, controlled trial of the computerized, self-administered PRIME-MD diagnostic system. Ann Emerg Med 2001;37(2):132-40.
4. Allen M, Carpenter D, Sheets JL, et al. What do consumers say they want and need during a psychiatric emergency? J Psychiatr Pract 2003;9(1):39-58.
5. Williams ER, Shepherd SM. Medical clearance of psychiatric patients. Emerg Med Clin North Am 2000;18(2):185-98.
6. Allen MH, Currier GW. Medical assessment on the psychiatric emergency service. New Dir Ment Health Serv 1999;82:21-8.
7. Mulligan K. ER docs report large increase in psychiatric patients. Psychiatr News 2004;39(12):10.-
8. Karcz A, Holbrook J, Auerbach BS, et al. Preventability of malpractice claims in emergency medicine: a closed claims study. Ann Emerg Med 1990;19(8):865-73.
9. Battaglia J. Is this patient dangerous? 5 steps to assess risk for violence. Current Psychiatry 2004;3(2):14-21.
10. De Fruyt J, Demyttenaere K. Rapid tranquilization: new approaches in the emergency treatment of behavioral disturbances. Eur Psychiatry 2004;19:243-9.
11. Allen MH, Currier GW, Hughes DH, et al. The Expert Consensus Guideline Series: Treatment of behavioral emergencies. Postgrad Med 2001;May(Spec No):1-88.
12. Hughes DH. Acute psychopharmacological management of the aggressive psychotic patient. Psychiatr Serv 1999;50(9):1135-7.
13. Glick RL. Starting antidepressant treatment in the emergency setting. Psychiatric Issues in Emergency Care Settings 2004;3(2):6-10.