User login
How much does weight loss affect hypertension?
WEIGHT LOSS OF 4 KG by diet reduces systolic and diastolic blood pressure (BP) by 4.5 and 3.2 mm Hg, respectively (SOR: A, systematic review with consistent findings).
Weight loss of 1 to 1.2 kg by exercise may produce small reductions in systolic or diastolic BP (SOR: B, mixed quality of studies).
Available evidence is inadequate to examine the combined effects of diet and exercise.
Evidence summary
A meta-analysis of 8 randomized controlled trials (RCTs) with a total of 2000 patients found that weight loss through diet reduced BP in hypertensive patients.1 Investigators recruited adult outpatients, 45 to 66 years of age, with primary hypertension (systolic BP, 128-178 mm Hg, diastolic BP, 72-107 mm Hg) and randomized them to dietary advice or usual care for 6 to 12 months.
Dietary advice resulted in greater weight loss over 6 to 12 months of follow-up (weighted mean difference [WMD], –4.0 kg; 95% confidence interval [CI], –4.8 to –3.2 kg) and greater BP reduction (WMD for systolic BP, –4.5 mm Hg; 95% CI, –7.2 to –1.8 mm Hg; WMD for diastolic BP, –3.2 mm Hg; 95% CI, –4.8 to –1.5 mm Hg).
Investigators didn’t report how long patients maintained the weight loss. Although 3 RCTs included encouragement to exercise, this meta-analysis didn’t evaluate benefits of combining these interventions.
The effects of exercise are less clear
A meta-analysis of 24 RCTs examined exercise and weight loss in adult outpatients with a mean age of 51.6 years; baseline body mass index (BMI), 25.9 kg/m2; resting systolic BP, 127 mm Hg; and resting diastolic BP, 77.7 mm Hg.2 On average, participants walked for 38.3 minutes, 4.4 days per week, for 34.9 weeks at a relative intensity of 70.1% of predicted maximum heart rate (in 6 studies) or 56.3% oxygen consumption intensity (VO2) (in 14 studies).
Walking significantly reduced body weight (WMD, –0.95 kg; P<.001) and BMI (WMD, –0.28 kg/m2; P = .015), leading to a significant reduction in diastolic BP (WMD, –1.54 mm Hg; P = .026) but not systolic BP (WMD, –1.06 mm Hg; P = .316). The authors didn’t report whether participants maintained the weight loss after the interventions.
In a meta-analysis of 8 RCTs and 18 observational studies, adult outpatients described as generally normotensive and overweight (mean age 49 years) wore pedometers to encourage weight loss with the goal of decreasing BP.3
Pedometer use for 3 to 104 weeks increased physical activity (for RCTs, a 2491-steps-per-day increase; 95% CI, 1098-3885 steps per day; for observational studies, a 2183-steps-per-day increase; 95% CI, 1571-2796 steps per day) and decreased BMI by 0.38 kg/m2 (95% CI, 0.05-0.72 kg/m2). For an 80-kg, 170-cm tall person with a BMI of 27.7 kg/m2, reducing BMI by 0.4 units translates to a 1.2-kg weight loss. This weight loss reduced systolic BP by 3.8 mm Hg (95% CI, 1.7-5.9 mm Hg), but not diastolic BP (–0.3 mm Hg; 95% CI, 0.02 to –0.46). Using a 10,000-steps-per-day goal (P = .001) and a step diary (P<.001) further increased walking.
Recommendations
The National Heart, Lung, and Blood Institute’s Joint National Committee says that healthy lifestyles are critical to preventing hypertension and reducing BP in people who are already hypertensive.4 Specifically, the Committee recommends weight reduction in overweight or obese individuals by increasing physical activity and using the Dietary Approaches to Stop Hypertension (DASH) eating plan. Combining 2 or more lifestyle modifications may enhance results.
The Committee also notes that a positive, empathetic relationship with a clinician is crucial in building trust and enhancing motivation to make lifestyle changes. It recommends setting mutual goals, ensuring adequate patient education, using frequent feedback, and involving all members of the health care team.
1. Siebenhofer A, Jeitler K, Berghold A, et al. Long-term effects of weight-reducing diets in hypertensive patients. Cochrane Database Syst Rev. 2011;(9):CD008274.-
2. Murphy MH, Nevill AM, Murtagh EM, et al. The effect of walking on fitness, fatness and resting blood pressure: a meta-analysis of randomised, controlled trials. Prev Med. 2007;44:377-385.
3. Bravata DM, Smith-Spangler C, Sundaram V, et al. Using pedometers to increase physical activity and improve health: a systematic review. JAMA. 2007;298:2296-2304.
4. United States Department of Health and Human Services. The seventh report of the Joint National Committee on Prevention, Detection, and Treatment of High Blood Pressure. Available at: http://www.nhlbi.nih.gov/guidelines/hypertension/jnc7full.pdf. Accessed March 13, 2013.
WEIGHT LOSS OF 4 KG by diet reduces systolic and diastolic blood pressure (BP) by 4.5 and 3.2 mm Hg, respectively (SOR: A, systematic review with consistent findings).
Weight loss of 1 to 1.2 kg by exercise may produce small reductions in systolic or diastolic BP (SOR: B, mixed quality of studies).
Available evidence is inadequate to examine the combined effects of diet and exercise.
Evidence summary
A meta-analysis of 8 randomized controlled trials (RCTs) with a total of 2000 patients found that weight loss through diet reduced BP in hypertensive patients.1 Investigators recruited adult outpatients, 45 to 66 years of age, with primary hypertension (systolic BP, 128-178 mm Hg, diastolic BP, 72-107 mm Hg) and randomized them to dietary advice or usual care for 6 to 12 months.
Dietary advice resulted in greater weight loss over 6 to 12 months of follow-up (weighted mean difference [WMD], –4.0 kg; 95% confidence interval [CI], –4.8 to –3.2 kg) and greater BP reduction (WMD for systolic BP, –4.5 mm Hg; 95% CI, –7.2 to –1.8 mm Hg; WMD for diastolic BP, –3.2 mm Hg; 95% CI, –4.8 to –1.5 mm Hg).
Investigators didn’t report how long patients maintained the weight loss. Although 3 RCTs included encouragement to exercise, this meta-analysis didn’t evaluate benefits of combining these interventions.
The effects of exercise are less clear
A meta-analysis of 24 RCTs examined exercise and weight loss in adult outpatients with a mean age of 51.6 years; baseline body mass index (BMI), 25.9 kg/m2; resting systolic BP, 127 mm Hg; and resting diastolic BP, 77.7 mm Hg.2 On average, participants walked for 38.3 minutes, 4.4 days per week, for 34.9 weeks at a relative intensity of 70.1% of predicted maximum heart rate (in 6 studies) or 56.3% oxygen consumption intensity (VO2) (in 14 studies).
Walking significantly reduced body weight (WMD, –0.95 kg; P<.001) and BMI (WMD, –0.28 kg/m2; P = .015), leading to a significant reduction in diastolic BP (WMD, –1.54 mm Hg; P = .026) but not systolic BP (WMD, –1.06 mm Hg; P = .316). The authors didn’t report whether participants maintained the weight loss after the interventions.
In a meta-analysis of 8 RCTs and 18 observational studies, adult outpatients described as generally normotensive and overweight (mean age 49 years) wore pedometers to encourage weight loss with the goal of decreasing BP.3
Pedometer use for 3 to 104 weeks increased physical activity (for RCTs, a 2491-steps-per-day increase; 95% CI, 1098-3885 steps per day; for observational studies, a 2183-steps-per-day increase; 95% CI, 1571-2796 steps per day) and decreased BMI by 0.38 kg/m2 (95% CI, 0.05-0.72 kg/m2). For an 80-kg, 170-cm tall person with a BMI of 27.7 kg/m2, reducing BMI by 0.4 units translates to a 1.2-kg weight loss. This weight loss reduced systolic BP by 3.8 mm Hg (95% CI, 1.7-5.9 mm Hg), but not diastolic BP (–0.3 mm Hg; 95% CI, 0.02 to –0.46). Using a 10,000-steps-per-day goal (P = .001) and a step diary (P<.001) further increased walking.
Recommendations
The National Heart, Lung, and Blood Institute’s Joint National Committee says that healthy lifestyles are critical to preventing hypertension and reducing BP in people who are already hypertensive.4 Specifically, the Committee recommends weight reduction in overweight or obese individuals by increasing physical activity and using the Dietary Approaches to Stop Hypertension (DASH) eating plan. Combining 2 or more lifestyle modifications may enhance results.
The Committee also notes that a positive, empathetic relationship with a clinician is crucial in building trust and enhancing motivation to make lifestyle changes. It recommends setting mutual goals, ensuring adequate patient education, using frequent feedback, and involving all members of the health care team.
WEIGHT LOSS OF 4 KG by diet reduces systolic and diastolic blood pressure (BP) by 4.5 and 3.2 mm Hg, respectively (SOR: A, systematic review with consistent findings).
Weight loss of 1 to 1.2 kg by exercise may produce small reductions in systolic or diastolic BP (SOR: B, mixed quality of studies).
Available evidence is inadequate to examine the combined effects of diet and exercise.
Evidence summary
A meta-analysis of 8 randomized controlled trials (RCTs) with a total of 2000 patients found that weight loss through diet reduced BP in hypertensive patients.1 Investigators recruited adult outpatients, 45 to 66 years of age, with primary hypertension (systolic BP, 128-178 mm Hg, diastolic BP, 72-107 mm Hg) and randomized them to dietary advice or usual care for 6 to 12 months.
Dietary advice resulted in greater weight loss over 6 to 12 months of follow-up (weighted mean difference [WMD], –4.0 kg; 95% confidence interval [CI], –4.8 to –3.2 kg) and greater BP reduction (WMD for systolic BP, –4.5 mm Hg; 95% CI, –7.2 to –1.8 mm Hg; WMD for diastolic BP, –3.2 mm Hg; 95% CI, –4.8 to –1.5 mm Hg).
Investigators didn’t report how long patients maintained the weight loss. Although 3 RCTs included encouragement to exercise, this meta-analysis didn’t evaluate benefits of combining these interventions.
The effects of exercise are less clear
A meta-analysis of 24 RCTs examined exercise and weight loss in adult outpatients with a mean age of 51.6 years; baseline body mass index (BMI), 25.9 kg/m2; resting systolic BP, 127 mm Hg; and resting diastolic BP, 77.7 mm Hg.2 On average, participants walked for 38.3 minutes, 4.4 days per week, for 34.9 weeks at a relative intensity of 70.1% of predicted maximum heart rate (in 6 studies) or 56.3% oxygen consumption intensity (VO2) (in 14 studies).
Walking significantly reduced body weight (WMD, –0.95 kg; P<.001) and BMI (WMD, –0.28 kg/m2; P = .015), leading to a significant reduction in diastolic BP (WMD, –1.54 mm Hg; P = .026) but not systolic BP (WMD, –1.06 mm Hg; P = .316). The authors didn’t report whether participants maintained the weight loss after the interventions.
In a meta-analysis of 8 RCTs and 18 observational studies, adult outpatients described as generally normotensive and overweight (mean age 49 years) wore pedometers to encourage weight loss with the goal of decreasing BP.3
Pedometer use for 3 to 104 weeks increased physical activity (for RCTs, a 2491-steps-per-day increase; 95% CI, 1098-3885 steps per day; for observational studies, a 2183-steps-per-day increase; 95% CI, 1571-2796 steps per day) and decreased BMI by 0.38 kg/m2 (95% CI, 0.05-0.72 kg/m2). For an 80-kg, 170-cm tall person with a BMI of 27.7 kg/m2, reducing BMI by 0.4 units translates to a 1.2-kg weight loss. This weight loss reduced systolic BP by 3.8 mm Hg (95% CI, 1.7-5.9 mm Hg), but not diastolic BP (–0.3 mm Hg; 95% CI, 0.02 to –0.46). Using a 10,000-steps-per-day goal (P = .001) and a step diary (P<.001) further increased walking.
Recommendations
The National Heart, Lung, and Blood Institute’s Joint National Committee says that healthy lifestyles are critical to preventing hypertension and reducing BP in people who are already hypertensive.4 Specifically, the Committee recommends weight reduction in overweight or obese individuals by increasing physical activity and using the Dietary Approaches to Stop Hypertension (DASH) eating plan. Combining 2 or more lifestyle modifications may enhance results.
The Committee also notes that a positive, empathetic relationship with a clinician is crucial in building trust and enhancing motivation to make lifestyle changes. It recommends setting mutual goals, ensuring adequate patient education, using frequent feedback, and involving all members of the health care team.
1. Siebenhofer A, Jeitler K, Berghold A, et al. Long-term effects of weight-reducing diets in hypertensive patients. Cochrane Database Syst Rev. 2011;(9):CD008274.-
2. Murphy MH, Nevill AM, Murtagh EM, et al. The effect of walking on fitness, fatness and resting blood pressure: a meta-analysis of randomised, controlled trials. Prev Med. 2007;44:377-385.
3. Bravata DM, Smith-Spangler C, Sundaram V, et al. Using pedometers to increase physical activity and improve health: a systematic review. JAMA. 2007;298:2296-2304.
4. United States Department of Health and Human Services. The seventh report of the Joint National Committee on Prevention, Detection, and Treatment of High Blood Pressure. Available at: http://www.nhlbi.nih.gov/guidelines/hypertension/jnc7full.pdf. Accessed March 13, 2013.
1. Siebenhofer A, Jeitler K, Berghold A, et al. Long-term effects of weight-reducing diets in hypertensive patients. Cochrane Database Syst Rev. 2011;(9):CD008274.-
2. Murphy MH, Nevill AM, Murtagh EM, et al. The effect of walking on fitness, fatness and resting blood pressure: a meta-analysis of randomised, controlled trials. Prev Med. 2007;44:377-385.
3. Bravata DM, Smith-Spangler C, Sundaram V, et al. Using pedometers to increase physical activity and improve health: a systematic review. JAMA. 2007;298:2296-2304.
4. United States Department of Health and Human Services. The seventh report of the Joint National Committee on Prevention, Detection, and Treatment of High Blood Pressure. Available at: http://www.nhlbi.nih.gov/guidelines/hypertension/jnc7full.pdf. Accessed March 13, 2013.
Evidence-based answers from the Family Physicians Inquiries Network
What’s the best way to motivate patients to exercise?
THERE IS NO SINGLE BEST STRATEGY, given the lack of data from rigorous comparison studies. There are, however, several interventions for adults that are effective. They include:
- writing a patient-specific behavioral health "green" prescription
- encouraging patients to join forces with accountability partners or support groups
- recommending the use of pedometers (strength of recommendation [SOR]: A, meta-analyses).
In children and adolescents, multicomponent strategies that include school-based interventions combined with either family or community involvement increase physical activity (SOR: A, systematic review).
Evidence summary
The Healthy People 2010 report calls for increasing the proportion of Americans who engage in moderate physical activity (activities that use large muscle groups and are at least equivalent to brisk walking) from 15% to 30%.1 The report doesn’t describe how best to achieve this objective.
Systematic review reveals approaches worth trying
The US Department of Health and Human Services (DHHS) and the Centers for Disease Control and Prevention (CDC) conducted a systematic review of 94 qualifying trials and assigned interventions to 1 of 3 approaches: “information based,” “behavioral and social,” and “facilities and activities.”2
Behavioral and social interventions have the best data support.2 Within this category, strong evidence backed school-based physical education and accountability partners or exercise support groups. School-based physical education resulted in a median net increase in physical activity time of 50.3% (range 6.0%-125.3%); accountability partners or support groups produced a mean net increase of 44.2% (interquartile range 19.9%-45.6%).
“Green” prescriptions are primary care behavioral interventions that include measurable goals, self-reward, structured problem-solving, social network reinforcement, and relapse prevention counseling. In the DHHS review, 10 trials studied green prescriptions; the median net increase in physical activity time was 35.4% (interquartile range 16.7%-83.3%).2 A trial in 42 rural and urban New Zealand general practices that added 3 telephone follow-up sessions to the green prescription showed a 10% increase in achieving 150 minutes of vigorous exercise weekly among green prescription participants compared with controls (number needed to treat=10).3
Pedometers. A systematic review using meta-regression to calculate summary effects evaluated the use of pedometers by study participants for an average of 18 weeks.4 Pedometer users increased their physical activity significantly, by 2491 steps per day compared with controls (95% confidence interval [CI], 1098-3885 steps per day).4 In adults, walking normally and walking briskly for an average of 2500 steps burns 100 and 150 kcal, respectively.5
Here’s what works with kids
A British systematic review of 24 high-quality controlled trials involving adolescents and children reported significant improvements with interventions that were school-based and either community- or family-based. Multidimensional outcomes included a 42% increase in participation in regular physical activity and an increase of 83 minutes weekly in moderate-to-vigorous physical activity.6
A US meta-analysis of 11 after-school programs with an average contact time of 275 minutes per week showed a positive standardized mean difference effect size for physical activity (0.44; 95% CI, 0.28-0.60).7
Evidence for other interventions is lacking
Insufficient evidence exists to support other interventions, such as classroom-based informational health education, mass media campaigns, college-based health and physical education, and classroom-based education focused on reducing television viewing and video-game playing.2
Recommendations
The British National Institute for Health and Clinical Excellence (NICE) has found sufficient evidence to recommend brief interventions in primary care. They include:
- using a validated tool to identify inactive patients
- recommending at least 30 minutes of patient-specific exercise at least 5 days per week
- establishing exercise goals
- presenting patients with written material on the benefits of exercise and local exercise opportunities
- following up several times over a 3-to 6-month period.8
Acknowledgments
The opinions and assertions contained herein are the private views of the authors and not to be construed as official, or as reflecting the views of the US Air Force Medical Service or the US Air Force at large.
1. Physical activity and fitness (chapter 22). In: Healthy People 2010: Understanding and Improving Health. 2nd ed. Washington, DC: US Department of Health and Human Services; 2000. Available at: www.healthypeople.gov/Document/HTML/Volume2/22Physical.htm#_Toc490380800. Accessed July 6, 2009.
2. Kahn EB, Ramsey LT, Brownson RC, et al. The effectiveness of interventions to increase physical activity.A systematic review. Am J Prev Med. 2002;22(4 suppl):73-107.
3. Elley CR, Kerse N, Arroll B, et al. Effectiveness of counselling patients on physical activity in general practice: cluster randomised controlled trial. BMJ. 2003;326:793.-Available at: www.bmj.com/cgi/reprint/326/7393/793.pdf. Accessed July 6, 2009.
4. Bravata DM, Smith-Spangler C, Sundaram V, et al. Using pedometers to increase physical activity and improve health: a systematic review. JAMA. 2007;298:2296-2304.
5. Peters JC, Melanson EL, Knoll JR, et al. Predicting the net energy cost of walking at self-selected speeds in healthy adults. Med Sci Sports Exerc. 2003;35(suppl 1):S155.-
6. van Sluijs EM, McMinn AM, Griffin SJ. Effectiveness of interventions to promote physical activity in children and adolescents: systematic review of controlled trials. Br J Sports Med. 2008;42:653-657.
7. Beets MW, Beighle A, Erwin HE, et al. After-school program impact on physical activity and fitness: a meta-analysis. Am J Prev Med. 2009;36:527-537.
8. National Institute for Health and Clinical Excellence (NICE). Four Commonly Used Methods to Increase Physical Activity: Brief Interventions in Primary Care, Exercise Referral Schemes, Pedometers and Community-Based Exercise Programmes for Walking and Cycling. London, UK: National Institute for Health and Clinical Excellence; 2006 (Public health intervention guidance; no. 2). Available at: www.nice.org.uk/nicemedia/pdf/PH002_physical_activity.pdf. Accessed July 6, 2009.
THERE IS NO SINGLE BEST STRATEGY, given the lack of data from rigorous comparison studies. There are, however, several interventions for adults that are effective. They include:
- writing a patient-specific behavioral health "green" prescription
- encouraging patients to join forces with accountability partners or support groups
- recommending the use of pedometers (strength of recommendation [SOR]: A, meta-analyses).
In children and adolescents, multicomponent strategies that include school-based interventions combined with either family or community involvement increase physical activity (SOR: A, systematic review).
Evidence summary
The Healthy People 2010 report calls for increasing the proportion of Americans who engage in moderate physical activity (activities that use large muscle groups and are at least equivalent to brisk walking) from 15% to 30%.1 The report doesn’t describe how best to achieve this objective.
Systematic review reveals approaches worth trying
The US Department of Health and Human Services (DHHS) and the Centers for Disease Control and Prevention (CDC) conducted a systematic review of 94 qualifying trials and assigned interventions to 1 of 3 approaches: “information based,” “behavioral and social,” and “facilities and activities.”2
Behavioral and social interventions have the best data support.2 Within this category, strong evidence backed school-based physical education and accountability partners or exercise support groups. School-based physical education resulted in a median net increase in physical activity time of 50.3% (range 6.0%-125.3%); accountability partners or support groups produced a mean net increase of 44.2% (interquartile range 19.9%-45.6%).
“Green” prescriptions are primary care behavioral interventions that include measurable goals, self-reward, structured problem-solving, social network reinforcement, and relapse prevention counseling. In the DHHS review, 10 trials studied green prescriptions; the median net increase in physical activity time was 35.4% (interquartile range 16.7%-83.3%).2 A trial in 42 rural and urban New Zealand general practices that added 3 telephone follow-up sessions to the green prescription showed a 10% increase in achieving 150 minutes of vigorous exercise weekly among green prescription participants compared with controls (number needed to treat=10).3
Pedometers. A systematic review using meta-regression to calculate summary effects evaluated the use of pedometers by study participants for an average of 18 weeks.4 Pedometer users increased their physical activity significantly, by 2491 steps per day compared with controls (95% confidence interval [CI], 1098-3885 steps per day).4 In adults, walking normally and walking briskly for an average of 2500 steps burns 100 and 150 kcal, respectively.5
Here’s what works with kids
A British systematic review of 24 high-quality controlled trials involving adolescents and children reported significant improvements with interventions that were school-based and either community- or family-based. Multidimensional outcomes included a 42% increase in participation in regular physical activity and an increase of 83 minutes weekly in moderate-to-vigorous physical activity.6
A US meta-analysis of 11 after-school programs with an average contact time of 275 minutes per week showed a positive standardized mean difference effect size for physical activity (0.44; 95% CI, 0.28-0.60).7
Evidence for other interventions is lacking
Insufficient evidence exists to support other interventions, such as classroom-based informational health education, mass media campaigns, college-based health and physical education, and classroom-based education focused on reducing television viewing and video-game playing.2
Recommendations
The British National Institute for Health and Clinical Excellence (NICE) has found sufficient evidence to recommend brief interventions in primary care. They include:
- using a validated tool to identify inactive patients
- recommending at least 30 minutes of patient-specific exercise at least 5 days per week
- establishing exercise goals
- presenting patients with written material on the benefits of exercise and local exercise opportunities
- following up several times over a 3-to 6-month period.8
Acknowledgments
The opinions and assertions contained herein are the private views of the authors and not to be construed as official, or as reflecting the views of the US Air Force Medical Service or the US Air Force at large.
THERE IS NO SINGLE BEST STRATEGY, given the lack of data from rigorous comparison studies. There are, however, several interventions for adults that are effective. They include:
- writing a patient-specific behavioral health "green" prescription
- encouraging patients to join forces with accountability partners or support groups
- recommending the use of pedometers (strength of recommendation [SOR]: A, meta-analyses).
In children and adolescents, multicomponent strategies that include school-based interventions combined with either family or community involvement increase physical activity (SOR: A, systematic review).
Evidence summary
The Healthy People 2010 report calls for increasing the proportion of Americans who engage in moderate physical activity (activities that use large muscle groups and are at least equivalent to brisk walking) from 15% to 30%.1 The report doesn’t describe how best to achieve this objective.
Systematic review reveals approaches worth trying
The US Department of Health and Human Services (DHHS) and the Centers for Disease Control and Prevention (CDC) conducted a systematic review of 94 qualifying trials and assigned interventions to 1 of 3 approaches: “information based,” “behavioral and social,” and “facilities and activities.”2
Behavioral and social interventions have the best data support.2 Within this category, strong evidence backed school-based physical education and accountability partners or exercise support groups. School-based physical education resulted in a median net increase in physical activity time of 50.3% (range 6.0%-125.3%); accountability partners or support groups produced a mean net increase of 44.2% (interquartile range 19.9%-45.6%).
“Green” prescriptions are primary care behavioral interventions that include measurable goals, self-reward, structured problem-solving, social network reinforcement, and relapse prevention counseling. In the DHHS review, 10 trials studied green prescriptions; the median net increase in physical activity time was 35.4% (interquartile range 16.7%-83.3%).2 A trial in 42 rural and urban New Zealand general practices that added 3 telephone follow-up sessions to the green prescription showed a 10% increase in achieving 150 minutes of vigorous exercise weekly among green prescription participants compared with controls (number needed to treat=10).3
Pedometers. A systematic review using meta-regression to calculate summary effects evaluated the use of pedometers by study participants for an average of 18 weeks.4 Pedometer users increased their physical activity significantly, by 2491 steps per day compared with controls (95% confidence interval [CI], 1098-3885 steps per day).4 In adults, walking normally and walking briskly for an average of 2500 steps burns 100 and 150 kcal, respectively.5
Here’s what works with kids
A British systematic review of 24 high-quality controlled trials involving adolescents and children reported significant improvements with interventions that were school-based and either community- or family-based. Multidimensional outcomes included a 42% increase in participation in regular physical activity and an increase of 83 minutes weekly in moderate-to-vigorous physical activity.6
A US meta-analysis of 11 after-school programs with an average contact time of 275 minutes per week showed a positive standardized mean difference effect size for physical activity (0.44; 95% CI, 0.28-0.60).7
Evidence for other interventions is lacking
Insufficient evidence exists to support other interventions, such as classroom-based informational health education, mass media campaigns, college-based health and physical education, and classroom-based education focused on reducing television viewing and video-game playing.2
Recommendations
The British National Institute for Health and Clinical Excellence (NICE) has found sufficient evidence to recommend brief interventions in primary care. They include:
- using a validated tool to identify inactive patients
- recommending at least 30 minutes of patient-specific exercise at least 5 days per week
- establishing exercise goals
- presenting patients with written material on the benefits of exercise and local exercise opportunities
- following up several times over a 3-to 6-month period.8
Acknowledgments
The opinions and assertions contained herein are the private views of the authors and not to be construed as official, or as reflecting the views of the US Air Force Medical Service or the US Air Force at large.
1. Physical activity and fitness (chapter 22). In: Healthy People 2010: Understanding and Improving Health. 2nd ed. Washington, DC: US Department of Health and Human Services; 2000. Available at: www.healthypeople.gov/Document/HTML/Volume2/22Physical.htm#_Toc490380800. Accessed July 6, 2009.
2. Kahn EB, Ramsey LT, Brownson RC, et al. The effectiveness of interventions to increase physical activity.A systematic review. Am J Prev Med. 2002;22(4 suppl):73-107.
3. Elley CR, Kerse N, Arroll B, et al. Effectiveness of counselling patients on physical activity in general practice: cluster randomised controlled trial. BMJ. 2003;326:793.-Available at: www.bmj.com/cgi/reprint/326/7393/793.pdf. Accessed July 6, 2009.
4. Bravata DM, Smith-Spangler C, Sundaram V, et al. Using pedometers to increase physical activity and improve health: a systematic review. JAMA. 2007;298:2296-2304.
5. Peters JC, Melanson EL, Knoll JR, et al. Predicting the net energy cost of walking at self-selected speeds in healthy adults. Med Sci Sports Exerc. 2003;35(suppl 1):S155.-
6. van Sluijs EM, McMinn AM, Griffin SJ. Effectiveness of interventions to promote physical activity in children and adolescents: systematic review of controlled trials. Br J Sports Med. 2008;42:653-657.
7. Beets MW, Beighle A, Erwin HE, et al. After-school program impact on physical activity and fitness: a meta-analysis. Am J Prev Med. 2009;36:527-537.
8. National Institute for Health and Clinical Excellence (NICE). Four Commonly Used Methods to Increase Physical Activity: Brief Interventions in Primary Care, Exercise Referral Schemes, Pedometers and Community-Based Exercise Programmes for Walking and Cycling. London, UK: National Institute for Health and Clinical Excellence; 2006 (Public health intervention guidance; no. 2). Available at: www.nice.org.uk/nicemedia/pdf/PH002_physical_activity.pdf. Accessed July 6, 2009.
1. Physical activity and fitness (chapter 22). In: Healthy People 2010: Understanding and Improving Health. 2nd ed. Washington, DC: US Department of Health and Human Services; 2000. Available at: www.healthypeople.gov/Document/HTML/Volume2/22Physical.htm#_Toc490380800. Accessed July 6, 2009.
2. Kahn EB, Ramsey LT, Brownson RC, et al. The effectiveness of interventions to increase physical activity.A systematic review. Am J Prev Med. 2002;22(4 suppl):73-107.
3. Elley CR, Kerse N, Arroll B, et al. Effectiveness of counselling patients on physical activity in general practice: cluster randomised controlled trial. BMJ. 2003;326:793.-Available at: www.bmj.com/cgi/reprint/326/7393/793.pdf. Accessed July 6, 2009.
4. Bravata DM, Smith-Spangler C, Sundaram V, et al. Using pedometers to increase physical activity and improve health: a systematic review. JAMA. 2007;298:2296-2304.
5. Peters JC, Melanson EL, Knoll JR, et al. Predicting the net energy cost of walking at self-selected speeds in healthy adults. Med Sci Sports Exerc. 2003;35(suppl 1):S155.-
6. van Sluijs EM, McMinn AM, Griffin SJ. Effectiveness of interventions to promote physical activity in children and adolescents: systematic review of controlled trials. Br J Sports Med. 2008;42:653-657.
7. Beets MW, Beighle A, Erwin HE, et al. After-school program impact on physical activity and fitness: a meta-analysis. Am J Prev Med. 2009;36:527-537.
8. National Institute for Health and Clinical Excellence (NICE). Four Commonly Used Methods to Increase Physical Activity: Brief Interventions in Primary Care, Exercise Referral Schemes, Pedometers and Community-Based Exercise Programmes for Walking and Cycling. London, UK: National Institute for Health and Clinical Excellence; 2006 (Public health intervention guidance; no. 2). Available at: www.nice.org.uk/nicemedia/pdf/PH002_physical_activity.pdf. Accessed July 6, 2009.
Evidence-based answers from the Family Physicians Inquiries Network
What's the best way to monitor low-risk patients with a history of differentiated thyroid cancer?
A recombinant human thyrotropin (rhTSH)-stimulated serum thyroglobulin (Tg) level alone is sufficient to monitor for recurrent disease in low-risk patients with a history of differentiated thyroid cancer (DTC) (strength of recommendation [SOR] A, meta-analysis). Low-risk patients are defined as patients who have undergone total thyroidectomy and radioactive iodine (I131) remnant ablation therapy and show no clinical evidence of recurrent disease.
Evidence summary
An estimated 37,340 new cases of thyroid cancer are diagnosed annually in the United States, typically in people between 20 and 55 years of age. The most common type of thyroid cancer is DTC, which includes papillary and follicular carcinoma. Papillary carcinoma accounts for 80% of all thyroid cancers, and follicular carcinoma accounts for 10%.
The 5-year survival rate for all cases of DTC is 97%. Although the disease has a favorable prognosis, an estimated 1630 patients were expected to die of it in 2009 because of its prevalence.1
The goal: Find recurrent disease early
The purpose of surveillance protocols in thyroid cancer is early detection of recurrent disease. Expert debate about DTC surveillance centers on the disease’s low incidence and prolonged clinical course, as well as a lack of prospective randomized clinical trials. Current guidelines were developed from large retrospective cohort studies of patients observed over several decades.
rhTSH-stimulated Tg is the new surveillance standard
All major professional organizations support the consensus that an rhTSH-stimulated serum Tg is adequate to follow-up low-risk patients. This test replaces the previous accepted standard of thyroid hormone withdrawal (THW)-stimulated measurements. Moreover, rhTSH-stimulated serum Tg is comparable to a THW-stimulated measurement for detecting recurrent disease, when a cutoff value of 2 mcg/L is used.2
rhTSH testing has similar sensitivity to THW
A 2004 meta-analysis examined 46 studies with a total of 9094 patients. THW-stimulated Tg measurements after thyroid remnant ablation had a sensitivity of 96% (95% confidence interval [CI], 93.5%-98.7%) and a specificity of 94% (95% CI, 93.3%-96.1%). For rhTSH-stimulated serum Tg measurements, sensitivity and specificity were 92% (95% CI, 88.9%-96.1%) and 88% (95% CI, 85.4%-90.6%), respectively.
Because the difference in sensitivity between THW-stimulated and rhTSH-stimulated serum Tg isn’t statistically significant, rhTSH can be used for Tg testing without significantly decreasing detection of DTC recurrence. The slightly lower specificity of rhTSH may lead to unnecessary additional testing because of a few more false-positive results. However, this risk should be weighed against the benefits of reducing morbidity by avoiding the need to withhold thyroid hormone replacement therapy before testing.3
Thyroglobulin measurements: How they compare to body scanning
A 1999 prospective cohort study of 229 patients with DTC compared the accuracy of I131 whole body scanning with serum Tg measurement after both rhTSH and THW stimulation (TABLE). The results of the whole body scan were concordant with the rhTSH-stimulated and THW-stimulated Tg measurements in 89% of the patients (P=.108).
Using a cutoff value of ≥2 mcg/L for recurrent disease, an elevated Tg level was detected in 52% of patients with localized thyroid bed disease after rhTSH stimulation and in 56% of patients after THW stimulation. An elevated Tg level after rhTSH stimulation was found in 100% of patients with metastatic disease. Symptoms of hypothyroidism, including overall quality-of-life scores, were significantly better in the rhTSH group than the THW group (P<.01).4
rhTSH-stimulated Tg: Accuracy with a lower cost
A retrospective cohort study of 107 patients determined that rhTSH-stimulated serum Tg levels alone are sensitive enough to identify recurrent disease in low-risk patients. Levels greater than 2 mcg/L had a sensitivity and negative predictive value of 100% and a false-positive rate of 9%—a statistically and clinically significant improvement in accuracy over a whole body scan obtained after rhTSH stimulation, which had a sensitivity of only 27%, negative predictive value of 92%, and false-positive rate of 9% (P<.05). In low-risk patients, rhTSH-stimulated serum Tg measurement is the most accurate and least costly method of surveillance because of its high negative predictive value.5
Whole body scanning doesn’t enhance surveillance accuracy
This conclusion is supported by a cohort study that prospectively followed 99 patients with a history of DTC who underwent serum Tg measurement and an I131 whole body scan obtained after rhTSH stimulation and were followed by neck ultrasound 6 to 12 months after ablation treatment. The whole body scan was negative in 95% of the patients, with a sensitivity of 0%. Serum Tg was positive in 19 of these patients. Neck ultrasound confirmed positive lymph nodes in 7 patients, of whom 5 were Tg-positive. The I131 whole body scan added no benefit to the accuracy of surveillance.6
Recommendations
The British Thyroid Association and the American Thyroid Association recommend performing a physical examination with serum TSH, Tg, and antithyroglobulin antibodies at 6 and 12 months postablation, then annually if the patient is disease free.7,8
In low-risk patients, stimulated serum Tg measurement alone is an acceptable initial follow-up; a value of ≥2 mcg/L indicates a need for further evaluation. If serum Tg is undetectable under TSH stimulation, subsequent long-term follow-up by serum Tg levels alone while under TSH suppression is sufficient. TSH stimulation can be achieved by THW or rhTSH.7-9
A whole body scan rarely adds valuable additional information. Periodic neck ultrasound should be performed, however.7-9
Acknowledgement
The opinions and assertions contained herein are the private views of the authors and not to be construed as official or as reflecting the views of the US Air Force Medical Service or the US Air Force at large.
A recombinant human thyrotropin (rhTSH)-stimulated serum thyroglobulin (Tg) level alone is sufficient to monitor for recurrent disease in low-risk patients with a history of differentiated thyroid cancer (DTC) (strength of recommendation [SOR] A, meta-analysis). Low-risk patients are defined as patients who have undergone total thyroidectomy and radioactive iodine (I131) remnant ablation therapy and show no clinical evidence of recurrent disease.
Evidence summary
An estimated 37,340 new cases of thyroid cancer are diagnosed annually in the United States, typically in people between 20 and 55 years of age. The most common type of thyroid cancer is DTC, which includes papillary and follicular carcinoma. Papillary carcinoma accounts for 80% of all thyroid cancers, and follicular carcinoma accounts for 10%.
The 5-year survival rate for all cases of DTC is 97%. Although the disease has a favorable prognosis, an estimated 1630 patients were expected to die of it in 2009 because of its prevalence.1
The goal: Find recurrent disease early
The purpose of surveillance protocols in thyroid cancer is early detection of recurrent disease. Expert debate about DTC surveillance centers on the disease’s low incidence and prolonged clinical course, as well as a lack of prospective randomized clinical trials. Current guidelines were developed from large retrospective cohort studies of patients observed over several decades.
rhTSH-stimulated Tg is the new surveillance standard
All major professional organizations support the consensus that an rhTSH-stimulated serum Tg is adequate to follow-up low-risk patients. This test replaces the previous accepted standard of thyroid hormone withdrawal (THW)-stimulated measurements. Moreover, rhTSH-stimulated serum Tg is comparable to a THW-stimulated measurement for detecting recurrent disease, when a cutoff value of 2 mcg/L is used.2
rhTSH testing has similar sensitivity to THW
A 2004 meta-analysis examined 46 studies with a total of 9094 patients. THW-stimulated Tg measurements after thyroid remnant ablation had a sensitivity of 96% (95% confidence interval [CI], 93.5%-98.7%) and a specificity of 94% (95% CI, 93.3%-96.1%). For rhTSH-stimulated serum Tg measurements, sensitivity and specificity were 92% (95% CI, 88.9%-96.1%) and 88% (95% CI, 85.4%-90.6%), respectively.
Because the difference in sensitivity between THW-stimulated and rhTSH-stimulated serum Tg isn’t statistically significant, rhTSH can be used for Tg testing without significantly decreasing detection of DTC recurrence. The slightly lower specificity of rhTSH may lead to unnecessary additional testing because of a few more false-positive results. However, this risk should be weighed against the benefits of reducing morbidity by avoiding the need to withhold thyroid hormone replacement therapy before testing.3
Thyroglobulin measurements: How they compare to body scanning
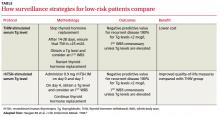
A 1999 prospective cohort study of 229 patients with DTC compared the accuracy of I131 whole body scanning with serum Tg measurement after both rhTSH and THW stimulation (TABLE). The results of the whole body scan were concordant with the rhTSH-stimulated and THW-stimulated Tg measurements in 89% of the patients (P=.108).
Using a cutoff value of ≥2 mcg/L for recurrent disease, an elevated Tg level was detected in 52% of patients with localized thyroid bed disease after rhTSH stimulation and in 56% of patients after THW stimulation. An elevated Tg level after rhTSH stimulation was found in 100% of patients with metastatic disease. Symptoms of hypothyroidism, including overall quality-of-life scores, were significantly better in the rhTSH group than the THW group (P<.01).4
rhTSH-stimulated Tg: Accuracy with a lower cost
A retrospective cohort study of 107 patients determined that rhTSH-stimulated serum Tg levels alone are sensitive enough to identify recurrent disease in low-risk patients. Levels greater than 2 mcg/L had a sensitivity and negative predictive value of 100% and a false-positive rate of 9%—a statistically and clinically significant improvement in accuracy over a whole body scan obtained after rhTSH stimulation, which had a sensitivity of only 27%, negative predictive value of 92%, and false-positive rate of 9% (P<.05). In low-risk patients, rhTSH-stimulated serum Tg measurement is the most accurate and least costly method of surveillance because of its high negative predictive value.5
Whole body scanning doesn’t enhance surveillance accuracy
This conclusion is supported by a cohort study that prospectively followed 99 patients with a history of DTC who underwent serum Tg measurement and an I131 whole body scan obtained after rhTSH stimulation and were followed by neck ultrasound 6 to 12 months after ablation treatment. The whole body scan was negative in 95% of the patients, with a sensitivity of 0%. Serum Tg was positive in 19 of these patients. Neck ultrasound confirmed positive lymph nodes in 7 patients, of whom 5 were Tg-positive. The I131 whole body scan added no benefit to the accuracy of surveillance.6
Recommendations
The British Thyroid Association and the American Thyroid Association recommend performing a physical examination with serum TSH, Tg, and antithyroglobulin antibodies at 6 and 12 months postablation, then annually if the patient is disease free.7,8
In low-risk patients, stimulated serum Tg measurement alone is an acceptable initial follow-up; a value of ≥2 mcg/L indicates a need for further evaluation. If serum Tg is undetectable under TSH stimulation, subsequent long-term follow-up by serum Tg levels alone while under TSH suppression is sufficient. TSH stimulation can be achieved by THW or rhTSH.7-9
A whole body scan rarely adds valuable additional information. Periodic neck ultrasound should be performed, however.7-9
Acknowledgement
The opinions and assertions contained herein are the private views of the authors and not to be construed as official or as reflecting the views of the US Air Force Medical Service or the US Air Force at large.
A recombinant human thyrotropin (rhTSH)-stimulated serum thyroglobulin (Tg) level alone is sufficient to monitor for recurrent disease in low-risk patients with a history of differentiated thyroid cancer (DTC) (strength of recommendation [SOR] A, meta-analysis). Low-risk patients are defined as patients who have undergone total thyroidectomy and radioactive iodine (I131) remnant ablation therapy and show no clinical evidence of recurrent disease.
Evidence summary
An estimated 37,340 new cases of thyroid cancer are diagnosed annually in the United States, typically in people between 20 and 55 years of age. The most common type of thyroid cancer is DTC, which includes papillary and follicular carcinoma. Papillary carcinoma accounts for 80% of all thyroid cancers, and follicular carcinoma accounts for 10%.
The 5-year survival rate for all cases of DTC is 97%. Although the disease has a favorable prognosis, an estimated 1630 patients were expected to die of it in 2009 because of its prevalence.1
The goal: Find recurrent disease early
The purpose of surveillance protocols in thyroid cancer is early detection of recurrent disease. Expert debate about DTC surveillance centers on the disease’s low incidence and prolonged clinical course, as well as a lack of prospective randomized clinical trials. Current guidelines were developed from large retrospective cohort studies of patients observed over several decades.
rhTSH-stimulated Tg is the new surveillance standard
All major professional organizations support the consensus that an rhTSH-stimulated serum Tg is adequate to follow-up low-risk patients. This test replaces the previous accepted standard of thyroid hormone withdrawal (THW)-stimulated measurements. Moreover, rhTSH-stimulated serum Tg is comparable to a THW-stimulated measurement for detecting recurrent disease, when a cutoff value of 2 mcg/L is used.2
rhTSH testing has similar sensitivity to THW
A 2004 meta-analysis examined 46 studies with a total of 9094 patients. THW-stimulated Tg measurements after thyroid remnant ablation had a sensitivity of 96% (95% confidence interval [CI], 93.5%-98.7%) and a specificity of 94% (95% CI, 93.3%-96.1%). For rhTSH-stimulated serum Tg measurements, sensitivity and specificity were 92% (95% CI, 88.9%-96.1%) and 88% (95% CI, 85.4%-90.6%), respectively.
Because the difference in sensitivity between THW-stimulated and rhTSH-stimulated serum Tg isn’t statistically significant, rhTSH can be used for Tg testing without significantly decreasing detection of DTC recurrence. The slightly lower specificity of rhTSH may lead to unnecessary additional testing because of a few more false-positive results. However, this risk should be weighed against the benefits of reducing morbidity by avoiding the need to withhold thyroid hormone replacement therapy before testing.3
Thyroglobulin measurements: How they compare to body scanning
A 1999 prospective cohort study of 229 patients with DTC compared the accuracy of I131 whole body scanning with serum Tg measurement after both rhTSH and THW stimulation (TABLE). The results of the whole body scan were concordant with the rhTSH-stimulated and THW-stimulated Tg measurements in 89% of the patients (P=.108).
Using a cutoff value of ≥2 mcg/L for recurrent disease, an elevated Tg level was detected in 52% of patients with localized thyroid bed disease after rhTSH stimulation and in 56% of patients after THW stimulation. An elevated Tg level after rhTSH stimulation was found in 100% of patients with metastatic disease. Symptoms of hypothyroidism, including overall quality-of-life scores, were significantly better in the rhTSH group than the THW group (P<.01).4
rhTSH-stimulated Tg: Accuracy with a lower cost
A retrospective cohort study of 107 patients determined that rhTSH-stimulated serum Tg levels alone are sensitive enough to identify recurrent disease in low-risk patients. Levels greater than 2 mcg/L had a sensitivity and negative predictive value of 100% and a false-positive rate of 9%—a statistically and clinically significant improvement in accuracy over a whole body scan obtained after rhTSH stimulation, which had a sensitivity of only 27%, negative predictive value of 92%, and false-positive rate of 9% (P<.05). In low-risk patients, rhTSH-stimulated serum Tg measurement is the most accurate and least costly method of surveillance because of its high negative predictive value.5
Whole body scanning doesn’t enhance surveillance accuracy
This conclusion is supported by a cohort study that prospectively followed 99 patients with a history of DTC who underwent serum Tg measurement and an I131 whole body scan obtained after rhTSH stimulation and were followed by neck ultrasound 6 to 12 months after ablation treatment. The whole body scan was negative in 95% of the patients, with a sensitivity of 0%. Serum Tg was positive in 19 of these patients. Neck ultrasound confirmed positive lymph nodes in 7 patients, of whom 5 were Tg-positive. The I131 whole body scan added no benefit to the accuracy of surveillance.6
Recommendations
The British Thyroid Association and the American Thyroid Association recommend performing a physical examination with serum TSH, Tg, and antithyroglobulin antibodies at 6 and 12 months postablation, then annually if the patient is disease free.7,8
In low-risk patients, stimulated serum Tg measurement alone is an acceptable initial follow-up; a value of ≥2 mcg/L indicates a need for further evaluation. If serum Tg is undetectable under TSH stimulation, subsequent long-term follow-up by serum Tg levels alone while under TSH suppression is sufficient. TSH stimulation can be achieved by THW or rhTSH.7-9
A whole body scan rarely adds valuable additional information. Periodic neck ultrasound should be performed, however.7-9
Acknowledgement
The opinions and assertions contained herein are the private views of the authors and not to be construed as official or as reflecting the views of the US Air Force Medical Service or the US Air Force at large.
Evidence-based answers from the Family Physicians Inquiries Network