User login
Hospitalist‐Led Medicine ED Team
Emergency department (ED) crowding leads to ambulance diversion,1 which can delay care and worsen outcomes, including mortality.2 A national survey showed that 90% of EDs were overcrowded, and 70% reported time on diversion.3 One of the causes of ED crowding is boarding of admitted patients.4 Boarding admitted patients decreases quality of care and satisfaction.57
Improved ED triage, bedside registration, physical expansion of hospitals, and regional ambulance programs have been implemented to decrease ED diversion.812 Despite these attempts, ED diversion continues to be prevalent.
Interventions involving hospitalists have been tested to improve throughput and quality of care for admitted medicine patients boarded in the ED. Howell and colleagues decreased ED diversion through active bed management by hospitalists.13 Briones and colleagues dedicated a hospitalist team to patients boarded in the ED and improved their quality of care.14
Denver Health Medical Center (DHMC) is an urban, academic safety net hospital. In 2009, the ED saw an average of 133 patients daily and an average of 25 were admitted to the medical service. DHMC's ED diversion rate was a mean of 12.4% in 2009. Boarded medicine patients occupied 16% of ED medicine bed capacity. Teaching and nonteaching medical floor teams cared for patients in the ED awaiting inpatient beds, who were the last to be seen. Nursing supervisors transferred boarded patients from the ED to hospital units. Patients with the greatest duration of time in the ED had priority for open beds.
ED diversion is costly.15, 16 DHMC implemented codified diversion criteria, calling the administrator on‐call prior to diversion, and increasing frequency of rounding in the ED, with no sustained effect seen in the rate of ED diversion.
In 2009, the DHMC Hospital Medicine Service addressed the issue of ED crowding, ED diversion, and care of boarded ED patients by creating a hospital medicine ED (HMED) team with 2 functions: (1) to provide ongoing care for medicine patients in the ED awaiting inpatient beds; and (2) to work with nursing supervisors to improve patient flow by adding physician clinical expertise to bed management.
METHODS
Setting and Design
This study took place at DHMC, a 477licensed‐bed academic safety net hospital in Denver, Colorado. We used a prepost design to assess measures of patient flow and timeliness of care. We surveyed ED attendings and nursing supervisors after the intervention to determine perceptions of the HMED team. This study was approved by the local institutional review board (IRB protocol number 09‐0892).
Intervention
In 2009, DHMC, which uses Toyota Lean for quality improvement, performed a Rapid Improvement Event (RIE) to address ED diversion and care of admitted patients boarded in the ED. The RIE team consisted of hospital medicine physicians, ED physicians, social workers, and nurses. Over a 4‐day period, the team examined the present state, created an ideal future state, devised a solution, and tested this solution.
Based upon the results of the RIE, DHMC implemented an HMED team to care for admitted patients boarded in the ED and assist in active bed management. The HMED team is a 24/7 service. During the day shift, the HMED team is composed of 1 dedicated attending and 1 allied health provider (AHP). Since the medicine services were already staffing existing patients in the ED, the 2.0 full‐time equivalent (FTE) needed to staff the HMED team attending and the AHP was reallocated from existing FTE within the hospitalist division. During the evening and night shifts, the HMED team's responsibilities were rolled into existing hospitalist duties.
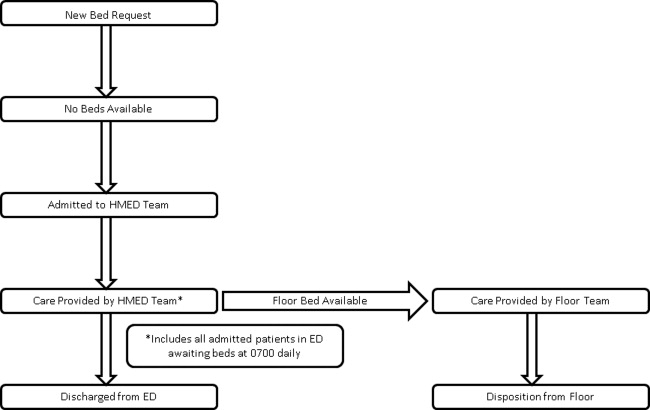
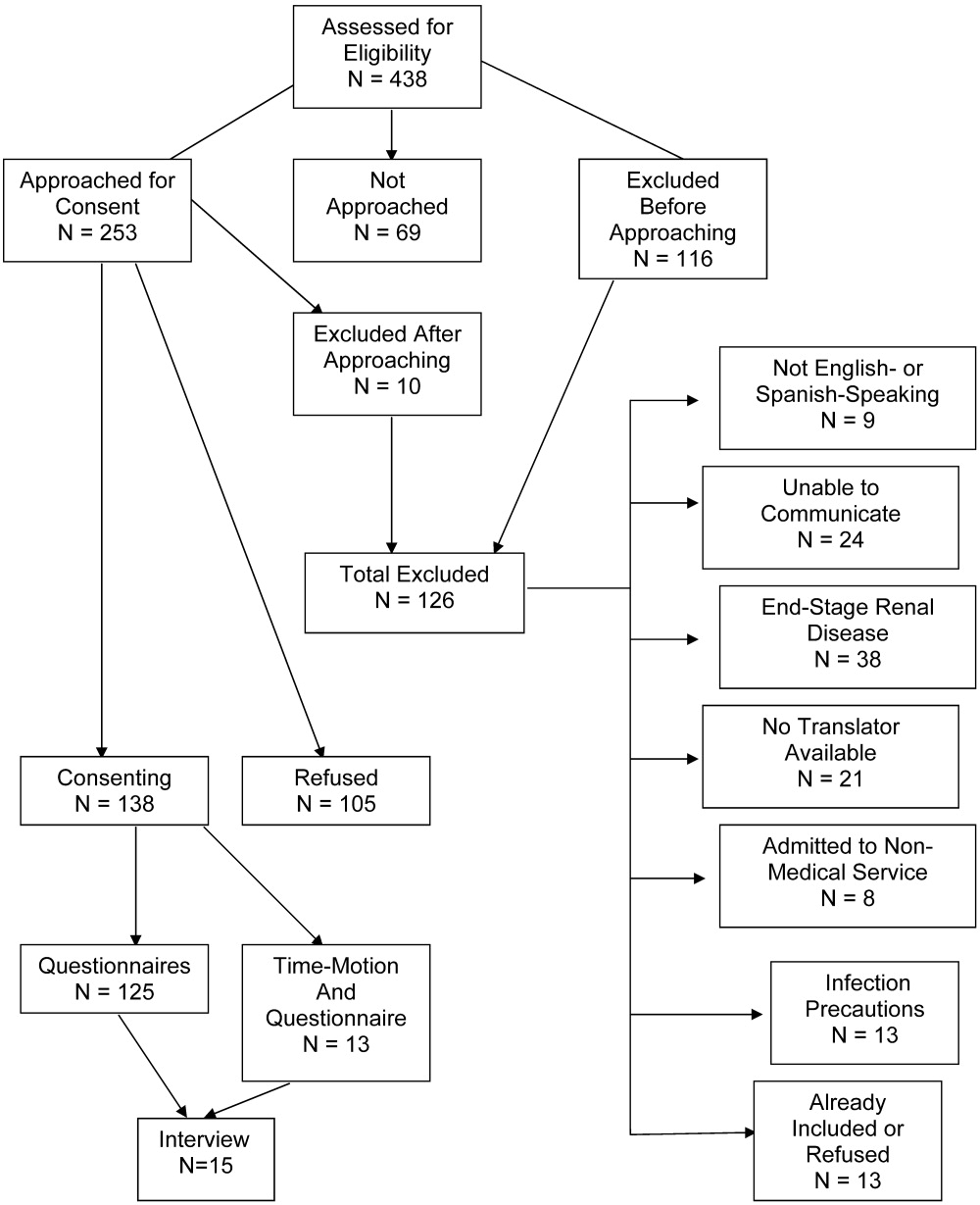
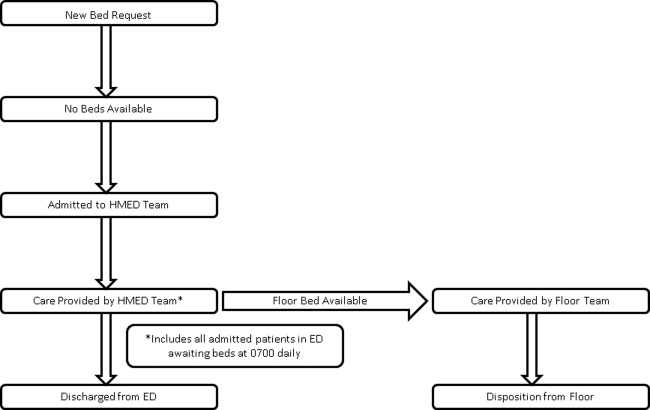
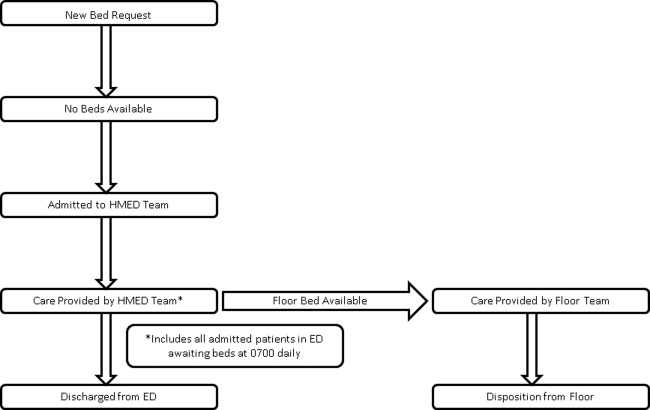
The HMED team provides clinical care for 2 groups of patients in the ED. The first group represents admitted patients who are still awaiting a medicine ward bed as of 7:00 AM. The HMED team provides ongoing care until discharge from the ED or transfer to a medicine floor. The second group of patients includes new admissions that need to stay in the ED due to a lack of available medicine floor beds. For these patients, the HMED team initiates and continues care until discharge from the ED or transfer to a medical floor (Figure 1).
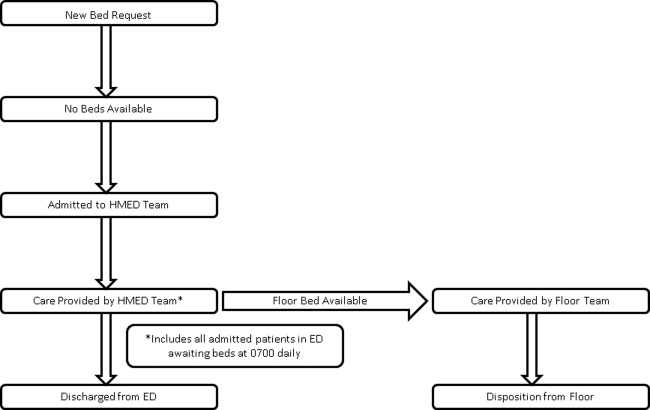
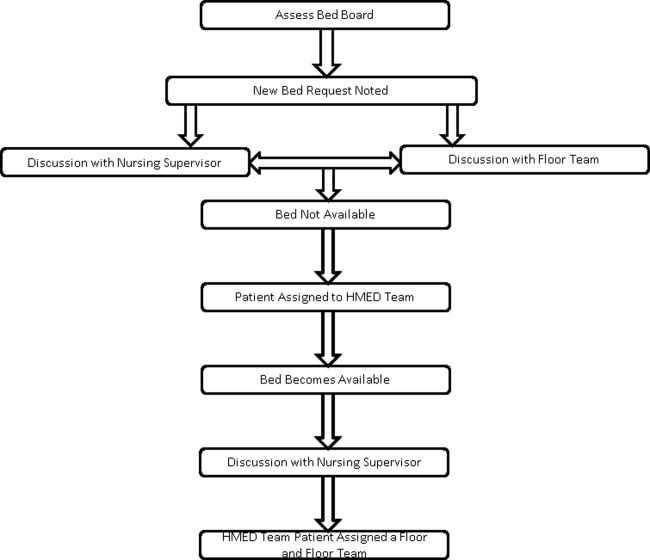
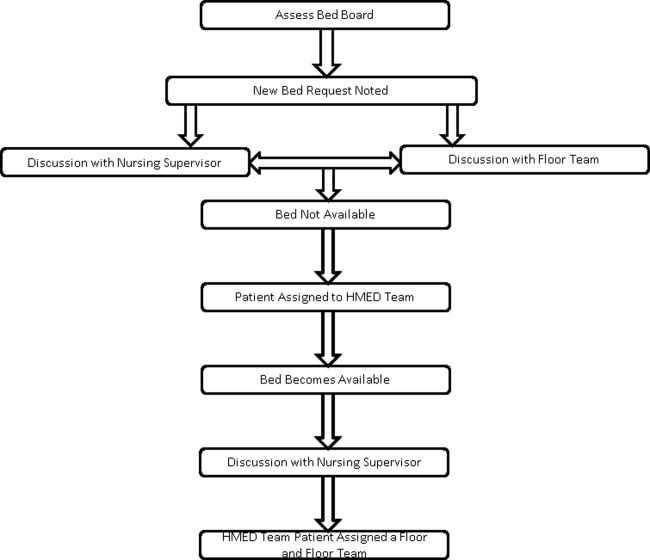
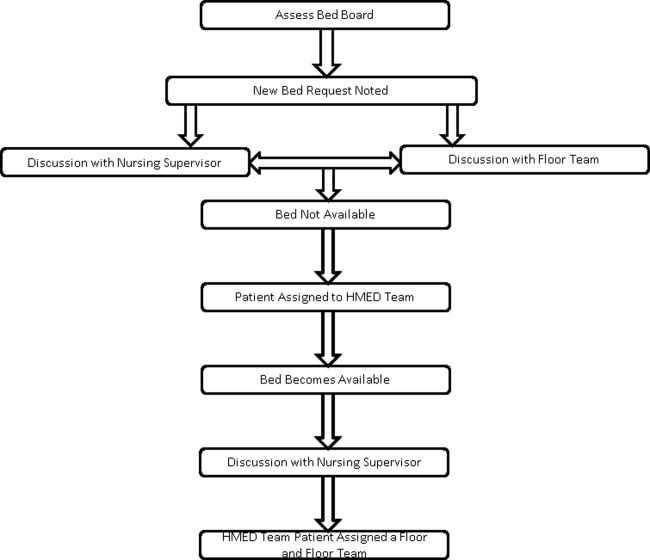
The physician on the HMED team assists nursing supervisors with bed management by providing detailed clinical knowledge, including proximity to discharge as well as updated information on telemetry and intensive care unit (ICU) appropriateness. The HMED team's physician maintains constant knowledge of hospital census via an electronic bed board, and communicates regularly with medical floors about anticipated discharges and transfers to understand the hospital's patient flow status (Figure 2).
The RIE that resulted in the HMED team was part of the Inpatient Medicine Value Stream, which had the overall goal of saving DHMC $300,000 for 2009. Ten RIEs were planned for this value stream in 2009, with an average of $30,000 of savings expected from each RIE.
Determination of ED Diversion Time
DHMC places responsibility for putting the hospital on an ED Diversion status in the hands of the Emergency Medicine Attending Physician. Diversion is categorized as either due to: (1) excessive ED volume for available ED bedsfull or nearly full department, or full resuscitation rooms without the ability to release a room; or (2) excessive boardingmore than 12 admitted patients awaiting beds in the ED. Other reasons for diversion, such as acute, excessive resource utilization (multiple patients from a single event) and temporary limitation of resources (critical equipment becoming inoperative), are also infrequent causes of diversion that are recorded. The elapsed time during which the ED is on diversion status is recorded and reported as a percentage of the total time on a monthly basis.
Determination of ED Diversion Costs
The cost of diversion at DHMC is calculated by multiplying the average number of ambulance drop‐offs per hour times the number of diversion hours to determine the number of missed patients. The historical mean charges for each ambulance patient are used to determine total missed charge opportunity, which is then applied to the hospital realization rate to calculate missed revenue. In addition, the marginal costs related to Denver Health Medical Plan patients that were unable to be repatriated to DHMC from outlying hospitals, as a result of diversion, is added to the net missed revenue figure. This figure is then divided by the number of diversion hours for the year to determine the cost of each diversion hour. For 2009, the cost of each hour of diversion at DHMC was $5000.
Statistical Analysis
All analyses were performed using SAS Enterprise Guide 4.1 (SAS Institute, Inc, Cary, NC). A Student t test or Wilcoxon rank sum test was used to compare continuous variables, and a chi‐square test was used to compare categorical variables.
Our primary outcome was ED diversion due to hospital bed capacity. These data are recorded, maintained, and analyzed by a DHMC internally developed emergency medical services information system (EMeSIS) that interfaces with computerized laboratory reporting systems, and stores, in part, demographic data as well as real‐time data related to the timing of patient encounters for all patients evaluated in the ED. To assess the effect of the intervention on ED diversion, the proportion of total hours on diversion due to medicine bed capacity was compared preimplementation and postimplementation with a chi‐squared test.
Secondary outcomes for patient flow included: (1) the proportion of patients discharged within 8 hours of transfer to a medical floor; and (2) the proportion of admitted medicine patients discharged from the ED. These data were gathered from the Denver Health Data Warehouse which pools data from both administrative and clinical applications used in patient care. Chi‐squared tests were also used to compare secondary outcomes preintervention and postintervention.
To measure the quality and safety of the HMED team, pre‐ED and post‐ED length of stay (LOS), 48‐hour patient return rate, intensive care unit (ICU) transfer rate, and the total LOS for patients admitted to the HMED team and handed off to a medicine floor team were assessed with the Student t test. To assess timeliness of clinical care provided to boarded medicine patients, self‐reported rounding times were compared preintervention and postintervention with the Student t test.
To assess satisfaction with the HMED team, an anonymous paper survey was administered to ED attendings and nursing supervisors 1 year after the intervention was introduced. The survey consisted of 5 questions, and used a 5‐point Likert scale ranging from strongly disagree (1) to strongly agree (5). Those answering agree or strongly agree were compared to those who were neutral, disagreed, or strongly disagreed.
RESULTS
The ED saw 48,595 patients during the intervention period (August 1, 2009June 30,2010) which did not differ statistically from the 50,469 patients seen in the control period (August 1, 2008June 30, 2009). The number of admissions to the medicine service during the control period (9727) and intervention period (10,013), and the number of total medical/surgical admissions during the control (20,716) and intervention (20,574) periods did not statistically differ. ED staffing during the intervention did not change. The overall number of licensed beds did not increase during the study period. During the control period, staffed medical/surgical beds increased from 395 to 400 beds, while the number of staffed medical/surgical beds decreased from 400 to 397 beds during the intervention period. Patient characteristics were similar during the 2 time periods, with the exception of race (Table 1).
| Patients Admitted to Medicine and Transferred to a Medicine Floor | Pre | Post | P Value |
|---|---|---|---|
| |||
| No. | 1901 | 1828 | |
| Age* | 53 15 | 54 14 | 0.59 |
| Gender (% male) | 55% | 52% | 0.06 |
| Race (% white) | 40% | 34% | <0.0001 |
| Insurance (% insured) | 67% | 63% | 0.08 |
| Charlson Comorbidity Index | 1.0 [1.0, 1.0] | 1.0 [1.0, 1.0] | 0.52 |
Diversion Hours
After implementation of the HMED team, there was a relative reduction of diversion due to medicine bed capacity of 27% (4.5%3.3%; P < 0.01) (Table 2). During the same time period, the relative proportion of hours on diversion due to ED capacity decreased by 55% (9.9%5.4%).
| Pre | Post | P Value | |
|---|---|---|---|
| |||
| Divert hours due to bed capacity (%, hours)* | 4.5% (3624) | 3.3% (3624) | 0.009 |
| Admitted ED patients transferred to floor | |||
| Discharged within 8 h (%, N) | 1.3% (1901) | 0.5% (1828) | 0.03 |
| Boarded patients rounded on in the ED and transferred to the medical floor | |||
| Total length of stay (days, N) | 2.6 [2.4, 3.2] (154) | 2.5 [2.4, 2.6] (364) | 0.21 |
| All discharges and transfers to the floor | |||
| Discharged from ED [%, (N)] | 4.9% (2009) | 7.5% (1981) | <0.001 |
| ED length of stay [hours, (N)] | 12:09 8:44 (2009) | 12:48 10:00 (1981) | 0.46 |
| Return to hospital <48 h [%, (N)] | 4.6% (2009) | 4.8% (1981) | 0.75 |
| Transfer to the ICU [%, (N)] | 3.3% (2009) | 4.2% (1981) | 0.13 |
Bed Management and Patient Flow
The HMED team rounded on boarded ED patients a mean of 2 hours and 9 minutes earlier (10:59 AM 1:09 vs 8:50 AM 1:20; P < 0.0001). After implementation of the HMED team, patients transferred to a medicine floor and discharged within 8 hours decreased relatively by 67% (1.5%0.5%; P < 0.01), and discharges from the ED of admitted medicine patients increased relatively by 61% (4.9%7.9%; P < 0.001) (Table 2). ED LOS, total LOS, 48‐hour returns to the ED, and ICU transfer rate for patients managed by the HMED team did not change (Table 2).
Perception and Satisfaction
Nine out of 15 (60%) ED attendings and 7 out of 8 (87%) nursing supervisors responded to the survey. The survey demonstrated that ED attendings and nursing supervisors believe the HMED team improves clinical care for boarded patients, communication, collegiality, and patient flow (Table 3).
| Postimplementation of the HMED Team | Total (n = 16) | ED Attendings (n = 9) | Nursing Supervisors (n = 7) |
|---|---|---|---|
| |||
| Quality of care has improved | 94 | 89 | 100 |
| Communication has improved | 94 | 89 | 100 |
| Collegiality and clinical decision‐making has improved | 94 | 100 | 89 |
| Patient flow has improved | 81 | 67 | 100 |
| HMED team is an asset to DHMC | 94 | 89 | 100 |
Financial
The 27% relative reduction in ED diversion due to hospital bed capacity extrapolates to 105.1 hours a year of decreased diversion, accounting for $525,600 of increased annual revenues.
DISCUSSION
This study suggests that an HMED team can decrease ED diversion, due to hospital bed capacity, by improving patient flow and timeliness of care for boarded medicine patients in the ED.
After participating in bed management, ED diversion due to a lack of medicine beds decreased. This is consistent with findings by Howell and colleagues who were able to improve throughput and decrease ED diversion with active bed management.13 Howell and colleagues decreased diversion hours due to temporary ED overload, and diversion hours due to a lack of telemetry or critical care beds. At DHMC, diversion is attributed to either a lack of ED capacity or lack of hospital beds. The primary outcome was the diversion rate due to lack of hospital beds, but it is possible that increased discharges directly from the ED contributed to the decrease in diversion due to ED capacity, underestimating the effect our intervention had on total ED diversion. There were no other initiatives to decrease diversion due to ED capacity during the study periods, and ED capacity and volume did not change during the intervention period.
While there were no statistically significant changes in staffed medical/surgical beds or medicine admissions, staffed medical/surgical beds during the intervention period decreased while there were more admissions to medicine. Both of these variables would increase diversion, resulting in an underestimation of the effect of the intervention.
Howell and colleagues improved throughput in the ED by implementing a service which provided active bed management without clinical responsibilities,13 while Briones and colleagues improved clinical care of patients boarded in the ED without affecting throughput.14 The HMED team improved throughput and decreased ED diversion while improving timeliness of care and perception of care quality for patients boarding in the ED.
By decreasing unnecessary transfers to medicine units and increasing discharges from the ED, patient flow was improved. While there was no difference in ED LOS, there was a trend towards decreased total LOS. A larger sample size or a longer period of observation would be necessary to determine if the trend toward decreased total LOS is statistically significant. ED LOS may not have been decreased because patients who would have been sent to the floor only to be discharged within 8 hours were kept in the ED to expedite testing and discharge, while sicker patients were sent to the medical floor. This decreased the turnover time of inpatient beds and allowed more boarded patients to be moved to floor units.
There was concern that an HMED team would fragment care, which would lead to an increased LOS for those patients who were transferred to a medical floor and cared for by an additional medicine team before discharge.17 As noted, there was a trend towards a decreased LOS for patients initially cared for by the HMED team.
In this intervention, hospital medicine physicians provided information regarding ongoing care of patients boarded in the ED to nursing supervisors. Prior to the intervention, nursing supervisors relied upon information from the ED staff and the boarded patient's time in the ED to assign a medical floor. However, ED staff was not providing care to boarded patients and did not know the most up‐to‐date status of the patient. This queuing process and lack of communication resulted in patients ready for discharge being transferred to floor beds and discharged within a few hours of transfer. The HMED team allowed nursing supervisors to have direct knowledge regarding clinical status, including telemetry and ICU criteria (similar to Howell and colleagues13), and readiness for discharge from the physician taking care of the patient.
By managing boarded patients, an HMED team can improve timeliness and coordination of care. Prior to the intervention, boarded ED patients were the last to be seen on rounds. The HMED team rounds only in the ED, expediting care and discharges. The increased proportion of boarded patients discharged from the ED by the HMED team is consistent with Briones and colleagues' clinically oriented team managing boarding patients in the ED.14
Potential adverse effects of our intervention included increased returns to the ED, increased ICU transfer rate, and decreased housestaff satisfaction. There was no increase in the 48‐hour return rate and no increase in the ICU transfer rate for patients cared for by the HMED team. Housestaff at DHMC are satisfied with the HMED team, since the presence of the HMED team allows them to concentrate on patients on the medical floors.
This intervention provides DHMC with an additional $525,600 in revenue annually. Since existing FTE were reallocated to create the HMED team, no additional FTE were required. In our facility, AHPs take on duties of housestaff. However, only 1 physician may be needed to staff an HMED team. This physician's clinical productivity is about 75% of other physicians; therefore, 25% of time is spent in bed management. At DHMC, other medicine teams picked up for the decreased clinical productivity of the HMED team, so the budget was neutral. However, using 2 FTE to staff 1 physician daily for 365 days a year, one would need to allocate 0.5 physician FTE (0.25 decrease in clinical productivity 2 FTE) for an HMED team.
Our study has several limitations. As a single center study, our findings may not extrapolate to other settings. The study used historical controls, therefore, undetected confounders may exist. We could not control for simultaneous changes in the hospital, however, we did not know of any other concurrent interventions aimed at decreasing ED diversion. Also, the decision to admit or not is partially based on individual ED attendings, which causes variability in practice. Finally, while we were able to measure rounding times as a process measure to reflect timeliness of care and staff perceptions of quality of care, due to our data infrastructure and the way our housestaff and attendings rotate, we were not able to assess more downstream measures of quality of care.
CONCLUSION
ED crowding decreases throughput and worsens clinical care; there are few proven solutions. This study demonstrates an intervention that reduced the percentage of patients transferred to a medicine floor and discharged within 8 hours, increased the number of discharges from the ED of admitted medicine patients, and decreased ED diversion while improving the timeliness of clinical care for patients boarded in the ED.
Acknowledgements
Disclosure: Nothing to report.
- ,,.Access block causes emergency department overcrowding and ambulance diversion in Perth, Western Australia.Emerg Med J.2005;22:351–354.
- ,,,.The relationship between distance to hospital and patient mortality in emergencies: an observational study.Emerg Med J.2007;24:665–668.
- Institute of Medicine.Committee on the Future of Emergency Care in the United States Health System.Hospital‐Based Emergency Care: At the Breaking Point.Washington, DC:National Academies Press;2007.
- ,.Systematic review of emergency department crowding: causes, effects, and solutions.Ann Emerg Med.2008;52:126–136.
- ,.Emergency department crowding is associated with poor care for patients with severe pain.Ann Emerg Med.2008;51:1–5.
- ,,, et al.The impact of emergency department crowding measures on time to antibiotics for patients with community‐acquired pneumonia.Ann Emerg Med.2007;50:510–516.
- ,,, et al;for the DELAYED‐ED Study Group.Impact of delayed transfer of critically ill patients from the emergency department to the intensive care unit.Crit Care Med.2007;35:1477–1483.
- ,,, et al.Impact of a triage liaison physician on emergency department overcrowding and throughput: a randomized controlled trial.Acad Emerg Med.2007;14:702–708.
- ,,.Strategies for dealing with emergency department overcrowding: a one‐year study on how bedside registration affects patient throughput times.Emerg Med J.2007;32:337–342.
- ,,, et al.The effect of emergency department expansion on emergency department overcrowding.Acad Emerg Med.2007;14:338–343.
- ,,,,,.Effect of increased ICU capacity on emergency department length of stay and ambulance diversion.Ann Emerg Med.2005;5:471–478.
- ,,,,.Ambulance diversion reduction: the Sacramento solution.Am J Emerg Med.2006;357:608–613.
- ,,,,,.Active bed management by hospitalists and emergency department throughput.Ann Intern Med.2008;149:804–810.
- ,,, et al.A model of hospitalist role in the care of admitted patients in the emergency department.J Hosp Med.2010;5:360–364.
- ,,,,.Ambulance diversion and lost hospital revenues.Ann Emerg Med.2006;48(6):702–710.
- ,,,.The financial impact of ambulance diversion and patient elopements.Acad Emerg Med.2007;14(1):58–62.
- ,,,,.The impact of fragmentation of hospitalist care on length of stay.J. Hosp. Med.2010;5:335–338.
Emergency department (ED) crowding leads to ambulance diversion,1 which can delay care and worsen outcomes, including mortality.2 A national survey showed that 90% of EDs were overcrowded, and 70% reported time on diversion.3 One of the causes of ED crowding is boarding of admitted patients.4 Boarding admitted patients decreases quality of care and satisfaction.57
Improved ED triage, bedside registration, physical expansion of hospitals, and regional ambulance programs have been implemented to decrease ED diversion.812 Despite these attempts, ED diversion continues to be prevalent.
Interventions involving hospitalists have been tested to improve throughput and quality of care for admitted medicine patients boarded in the ED. Howell and colleagues decreased ED diversion through active bed management by hospitalists.13 Briones and colleagues dedicated a hospitalist team to patients boarded in the ED and improved their quality of care.14
Denver Health Medical Center (DHMC) is an urban, academic safety net hospital. In 2009, the ED saw an average of 133 patients daily and an average of 25 were admitted to the medical service. DHMC's ED diversion rate was a mean of 12.4% in 2009. Boarded medicine patients occupied 16% of ED medicine bed capacity. Teaching and nonteaching medical floor teams cared for patients in the ED awaiting inpatient beds, who were the last to be seen. Nursing supervisors transferred boarded patients from the ED to hospital units. Patients with the greatest duration of time in the ED had priority for open beds.
ED diversion is costly.15, 16 DHMC implemented codified diversion criteria, calling the administrator on‐call prior to diversion, and increasing frequency of rounding in the ED, with no sustained effect seen in the rate of ED diversion.
In 2009, the DHMC Hospital Medicine Service addressed the issue of ED crowding, ED diversion, and care of boarded ED patients by creating a hospital medicine ED (HMED) team with 2 functions: (1) to provide ongoing care for medicine patients in the ED awaiting inpatient beds; and (2) to work with nursing supervisors to improve patient flow by adding physician clinical expertise to bed management.
METHODS
Setting and Design
This study took place at DHMC, a 477licensed‐bed academic safety net hospital in Denver, Colorado. We used a prepost design to assess measures of patient flow and timeliness of care. We surveyed ED attendings and nursing supervisors after the intervention to determine perceptions of the HMED team. This study was approved by the local institutional review board (IRB protocol number 09‐0892).
Intervention
In 2009, DHMC, which uses Toyota Lean for quality improvement, performed a Rapid Improvement Event (RIE) to address ED diversion and care of admitted patients boarded in the ED. The RIE team consisted of hospital medicine physicians, ED physicians, social workers, and nurses. Over a 4‐day period, the team examined the present state, created an ideal future state, devised a solution, and tested this solution.
Based upon the results of the RIE, DHMC implemented an HMED team to care for admitted patients boarded in the ED and assist in active bed management. The HMED team is a 24/7 service. During the day shift, the HMED team is composed of 1 dedicated attending and 1 allied health provider (AHP). Since the medicine services were already staffing existing patients in the ED, the 2.0 full‐time equivalent (FTE) needed to staff the HMED team attending and the AHP was reallocated from existing FTE within the hospitalist division. During the evening and night shifts, the HMED team's responsibilities were rolled into existing hospitalist duties.
The HMED team provides clinical care for 2 groups of patients in the ED. The first group represents admitted patients who are still awaiting a medicine ward bed as of 7:00 AM. The HMED team provides ongoing care until discharge from the ED or transfer to a medicine floor. The second group of patients includes new admissions that need to stay in the ED due to a lack of available medicine floor beds. For these patients, the HMED team initiates and continues care until discharge from the ED or transfer to a medical floor (Figure 1).
The physician on the HMED team assists nursing supervisors with bed management by providing detailed clinical knowledge, including proximity to discharge as well as updated information on telemetry and intensive care unit (ICU) appropriateness. The HMED team's physician maintains constant knowledge of hospital census via an electronic bed board, and communicates regularly with medical floors about anticipated discharges and transfers to understand the hospital's patient flow status (Figure 2).
The RIE that resulted in the HMED team was part of the Inpatient Medicine Value Stream, which had the overall goal of saving DHMC $300,000 for 2009. Ten RIEs were planned for this value stream in 2009, with an average of $30,000 of savings expected from each RIE.
Determination of ED Diversion Time
DHMC places responsibility for putting the hospital on an ED Diversion status in the hands of the Emergency Medicine Attending Physician. Diversion is categorized as either due to: (1) excessive ED volume for available ED bedsfull or nearly full department, or full resuscitation rooms without the ability to release a room; or (2) excessive boardingmore than 12 admitted patients awaiting beds in the ED. Other reasons for diversion, such as acute, excessive resource utilization (multiple patients from a single event) and temporary limitation of resources (critical equipment becoming inoperative), are also infrequent causes of diversion that are recorded. The elapsed time during which the ED is on diversion status is recorded and reported as a percentage of the total time on a monthly basis.
Determination of ED Diversion Costs
The cost of diversion at DHMC is calculated by multiplying the average number of ambulance drop‐offs per hour times the number of diversion hours to determine the number of missed patients. The historical mean charges for each ambulance patient are used to determine total missed charge opportunity, which is then applied to the hospital realization rate to calculate missed revenue. In addition, the marginal costs related to Denver Health Medical Plan patients that were unable to be repatriated to DHMC from outlying hospitals, as a result of diversion, is added to the net missed revenue figure. This figure is then divided by the number of diversion hours for the year to determine the cost of each diversion hour. For 2009, the cost of each hour of diversion at DHMC was $5000.
Statistical Analysis
All analyses were performed using SAS Enterprise Guide 4.1 (SAS Institute, Inc, Cary, NC). A Student t test or Wilcoxon rank sum test was used to compare continuous variables, and a chi‐square test was used to compare categorical variables.
Our primary outcome was ED diversion due to hospital bed capacity. These data are recorded, maintained, and analyzed by a DHMC internally developed emergency medical services information system (EMeSIS) that interfaces with computerized laboratory reporting systems, and stores, in part, demographic data as well as real‐time data related to the timing of patient encounters for all patients evaluated in the ED. To assess the effect of the intervention on ED diversion, the proportion of total hours on diversion due to medicine bed capacity was compared preimplementation and postimplementation with a chi‐squared test.
Secondary outcomes for patient flow included: (1) the proportion of patients discharged within 8 hours of transfer to a medical floor; and (2) the proportion of admitted medicine patients discharged from the ED. These data were gathered from the Denver Health Data Warehouse which pools data from both administrative and clinical applications used in patient care. Chi‐squared tests were also used to compare secondary outcomes preintervention and postintervention.
To measure the quality and safety of the HMED team, pre‐ED and post‐ED length of stay (LOS), 48‐hour patient return rate, intensive care unit (ICU) transfer rate, and the total LOS for patients admitted to the HMED team and handed off to a medicine floor team were assessed with the Student t test. To assess timeliness of clinical care provided to boarded medicine patients, self‐reported rounding times were compared preintervention and postintervention with the Student t test.
To assess satisfaction with the HMED team, an anonymous paper survey was administered to ED attendings and nursing supervisors 1 year after the intervention was introduced. The survey consisted of 5 questions, and used a 5‐point Likert scale ranging from strongly disagree (1) to strongly agree (5). Those answering agree or strongly agree were compared to those who were neutral, disagreed, or strongly disagreed.
RESULTS
The ED saw 48,595 patients during the intervention period (August 1, 2009June 30,2010) which did not differ statistically from the 50,469 patients seen in the control period (August 1, 2008June 30, 2009). The number of admissions to the medicine service during the control period (9727) and intervention period (10,013), and the number of total medical/surgical admissions during the control (20,716) and intervention (20,574) periods did not statistically differ. ED staffing during the intervention did not change. The overall number of licensed beds did not increase during the study period. During the control period, staffed medical/surgical beds increased from 395 to 400 beds, while the number of staffed medical/surgical beds decreased from 400 to 397 beds during the intervention period. Patient characteristics were similar during the 2 time periods, with the exception of race (Table 1).
| Patients Admitted to Medicine and Transferred to a Medicine Floor | Pre | Post | P Value |
|---|---|---|---|
| |||
| No. | 1901 | 1828 | |
| Age* | 53 15 | 54 14 | 0.59 |
| Gender (% male) | 55% | 52% | 0.06 |
| Race (% white) | 40% | 34% | <0.0001 |
| Insurance (% insured) | 67% | 63% | 0.08 |
| Charlson Comorbidity Index | 1.0 [1.0, 1.0] | 1.0 [1.0, 1.0] | 0.52 |
Diversion Hours
After implementation of the HMED team, there was a relative reduction of diversion due to medicine bed capacity of 27% (4.5%3.3%; P < 0.01) (Table 2). During the same time period, the relative proportion of hours on diversion due to ED capacity decreased by 55% (9.9%5.4%).
| Pre | Post | P Value | |
|---|---|---|---|
| |||
| Divert hours due to bed capacity (%, hours)* | 4.5% (3624) | 3.3% (3624) | 0.009 |
| Admitted ED patients transferred to floor | |||
| Discharged within 8 h (%, N) | 1.3% (1901) | 0.5% (1828) | 0.03 |
| Boarded patients rounded on in the ED and transferred to the medical floor | |||
| Total length of stay (days, N) | 2.6 [2.4, 3.2] (154) | 2.5 [2.4, 2.6] (364) | 0.21 |
| All discharges and transfers to the floor | |||
| Discharged from ED [%, (N)] | 4.9% (2009) | 7.5% (1981) | <0.001 |
| ED length of stay [hours, (N)] | 12:09 8:44 (2009) | 12:48 10:00 (1981) | 0.46 |
| Return to hospital <48 h [%, (N)] | 4.6% (2009) | 4.8% (1981) | 0.75 |
| Transfer to the ICU [%, (N)] | 3.3% (2009) | 4.2% (1981) | 0.13 |
Bed Management and Patient Flow
The HMED team rounded on boarded ED patients a mean of 2 hours and 9 minutes earlier (10:59 AM 1:09 vs 8:50 AM 1:20; P < 0.0001). After implementation of the HMED team, patients transferred to a medicine floor and discharged within 8 hours decreased relatively by 67% (1.5%0.5%; P < 0.01), and discharges from the ED of admitted medicine patients increased relatively by 61% (4.9%7.9%; P < 0.001) (Table 2). ED LOS, total LOS, 48‐hour returns to the ED, and ICU transfer rate for patients managed by the HMED team did not change (Table 2).
Perception and Satisfaction
Nine out of 15 (60%) ED attendings and 7 out of 8 (87%) nursing supervisors responded to the survey. The survey demonstrated that ED attendings and nursing supervisors believe the HMED team improves clinical care for boarded patients, communication, collegiality, and patient flow (Table 3).
| Postimplementation of the HMED Team | Total (n = 16) | ED Attendings (n = 9) | Nursing Supervisors (n = 7) |
|---|---|---|---|
| |||
| Quality of care has improved | 94 | 89 | 100 |
| Communication has improved | 94 | 89 | 100 |
| Collegiality and clinical decision‐making has improved | 94 | 100 | 89 |
| Patient flow has improved | 81 | 67 | 100 |
| HMED team is an asset to DHMC | 94 | 89 | 100 |
Financial
The 27% relative reduction in ED diversion due to hospital bed capacity extrapolates to 105.1 hours a year of decreased diversion, accounting for $525,600 of increased annual revenues.
DISCUSSION
This study suggests that an HMED team can decrease ED diversion, due to hospital bed capacity, by improving patient flow and timeliness of care for boarded medicine patients in the ED.
After participating in bed management, ED diversion due to a lack of medicine beds decreased. This is consistent with findings by Howell and colleagues who were able to improve throughput and decrease ED diversion with active bed management.13 Howell and colleagues decreased diversion hours due to temporary ED overload, and diversion hours due to a lack of telemetry or critical care beds. At DHMC, diversion is attributed to either a lack of ED capacity or lack of hospital beds. The primary outcome was the diversion rate due to lack of hospital beds, but it is possible that increased discharges directly from the ED contributed to the decrease in diversion due to ED capacity, underestimating the effect our intervention had on total ED diversion. There were no other initiatives to decrease diversion due to ED capacity during the study periods, and ED capacity and volume did not change during the intervention period.
While there were no statistically significant changes in staffed medical/surgical beds or medicine admissions, staffed medical/surgical beds during the intervention period decreased while there were more admissions to medicine. Both of these variables would increase diversion, resulting in an underestimation of the effect of the intervention.
Howell and colleagues improved throughput in the ED by implementing a service which provided active bed management without clinical responsibilities,13 while Briones and colleagues improved clinical care of patients boarded in the ED without affecting throughput.14 The HMED team improved throughput and decreased ED diversion while improving timeliness of care and perception of care quality for patients boarding in the ED.
By decreasing unnecessary transfers to medicine units and increasing discharges from the ED, patient flow was improved. While there was no difference in ED LOS, there was a trend towards decreased total LOS. A larger sample size or a longer period of observation would be necessary to determine if the trend toward decreased total LOS is statistically significant. ED LOS may not have been decreased because patients who would have been sent to the floor only to be discharged within 8 hours were kept in the ED to expedite testing and discharge, while sicker patients were sent to the medical floor. This decreased the turnover time of inpatient beds and allowed more boarded patients to be moved to floor units.
There was concern that an HMED team would fragment care, which would lead to an increased LOS for those patients who were transferred to a medical floor and cared for by an additional medicine team before discharge.17 As noted, there was a trend towards a decreased LOS for patients initially cared for by the HMED team.
In this intervention, hospital medicine physicians provided information regarding ongoing care of patients boarded in the ED to nursing supervisors. Prior to the intervention, nursing supervisors relied upon information from the ED staff and the boarded patient's time in the ED to assign a medical floor. However, ED staff was not providing care to boarded patients and did not know the most up‐to‐date status of the patient. This queuing process and lack of communication resulted in patients ready for discharge being transferred to floor beds and discharged within a few hours of transfer. The HMED team allowed nursing supervisors to have direct knowledge regarding clinical status, including telemetry and ICU criteria (similar to Howell and colleagues13), and readiness for discharge from the physician taking care of the patient.
By managing boarded patients, an HMED team can improve timeliness and coordination of care. Prior to the intervention, boarded ED patients were the last to be seen on rounds. The HMED team rounds only in the ED, expediting care and discharges. The increased proportion of boarded patients discharged from the ED by the HMED team is consistent with Briones and colleagues' clinically oriented team managing boarding patients in the ED.14
Potential adverse effects of our intervention included increased returns to the ED, increased ICU transfer rate, and decreased housestaff satisfaction. There was no increase in the 48‐hour return rate and no increase in the ICU transfer rate for patients cared for by the HMED team. Housestaff at DHMC are satisfied with the HMED team, since the presence of the HMED team allows them to concentrate on patients on the medical floors.
This intervention provides DHMC with an additional $525,600 in revenue annually. Since existing FTE were reallocated to create the HMED team, no additional FTE were required. In our facility, AHPs take on duties of housestaff. However, only 1 physician may be needed to staff an HMED team. This physician's clinical productivity is about 75% of other physicians; therefore, 25% of time is spent in bed management. At DHMC, other medicine teams picked up for the decreased clinical productivity of the HMED team, so the budget was neutral. However, using 2 FTE to staff 1 physician daily for 365 days a year, one would need to allocate 0.5 physician FTE (0.25 decrease in clinical productivity 2 FTE) for an HMED team.
Our study has several limitations. As a single center study, our findings may not extrapolate to other settings. The study used historical controls, therefore, undetected confounders may exist. We could not control for simultaneous changes in the hospital, however, we did not know of any other concurrent interventions aimed at decreasing ED diversion. Also, the decision to admit or not is partially based on individual ED attendings, which causes variability in practice. Finally, while we were able to measure rounding times as a process measure to reflect timeliness of care and staff perceptions of quality of care, due to our data infrastructure and the way our housestaff and attendings rotate, we were not able to assess more downstream measures of quality of care.
CONCLUSION
ED crowding decreases throughput and worsens clinical care; there are few proven solutions. This study demonstrates an intervention that reduced the percentage of patients transferred to a medicine floor and discharged within 8 hours, increased the number of discharges from the ED of admitted medicine patients, and decreased ED diversion while improving the timeliness of clinical care for patients boarded in the ED.
Acknowledgements
Disclosure: Nothing to report.
Emergency department (ED) crowding leads to ambulance diversion,1 which can delay care and worsen outcomes, including mortality.2 A national survey showed that 90% of EDs were overcrowded, and 70% reported time on diversion.3 One of the causes of ED crowding is boarding of admitted patients.4 Boarding admitted patients decreases quality of care and satisfaction.57
Improved ED triage, bedside registration, physical expansion of hospitals, and regional ambulance programs have been implemented to decrease ED diversion.812 Despite these attempts, ED diversion continues to be prevalent.
Interventions involving hospitalists have been tested to improve throughput and quality of care for admitted medicine patients boarded in the ED. Howell and colleagues decreased ED diversion through active bed management by hospitalists.13 Briones and colleagues dedicated a hospitalist team to patients boarded in the ED and improved their quality of care.14
Denver Health Medical Center (DHMC) is an urban, academic safety net hospital. In 2009, the ED saw an average of 133 patients daily and an average of 25 were admitted to the medical service. DHMC's ED diversion rate was a mean of 12.4% in 2009. Boarded medicine patients occupied 16% of ED medicine bed capacity. Teaching and nonteaching medical floor teams cared for patients in the ED awaiting inpatient beds, who were the last to be seen. Nursing supervisors transferred boarded patients from the ED to hospital units. Patients with the greatest duration of time in the ED had priority for open beds.
ED diversion is costly.15, 16 DHMC implemented codified diversion criteria, calling the administrator on‐call prior to diversion, and increasing frequency of rounding in the ED, with no sustained effect seen in the rate of ED diversion.
In 2009, the DHMC Hospital Medicine Service addressed the issue of ED crowding, ED diversion, and care of boarded ED patients by creating a hospital medicine ED (HMED) team with 2 functions: (1) to provide ongoing care for medicine patients in the ED awaiting inpatient beds; and (2) to work with nursing supervisors to improve patient flow by adding physician clinical expertise to bed management.
METHODS
Setting and Design
This study took place at DHMC, a 477licensed‐bed academic safety net hospital in Denver, Colorado. We used a prepost design to assess measures of patient flow and timeliness of care. We surveyed ED attendings and nursing supervisors after the intervention to determine perceptions of the HMED team. This study was approved by the local institutional review board (IRB protocol number 09‐0892).
Intervention
In 2009, DHMC, which uses Toyota Lean for quality improvement, performed a Rapid Improvement Event (RIE) to address ED diversion and care of admitted patients boarded in the ED. The RIE team consisted of hospital medicine physicians, ED physicians, social workers, and nurses. Over a 4‐day period, the team examined the present state, created an ideal future state, devised a solution, and tested this solution.
Based upon the results of the RIE, DHMC implemented an HMED team to care for admitted patients boarded in the ED and assist in active bed management. The HMED team is a 24/7 service. During the day shift, the HMED team is composed of 1 dedicated attending and 1 allied health provider (AHP). Since the medicine services were already staffing existing patients in the ED, the 2.0 full‐time equivalent (FTE) needed to staff the HMED team attending and the AHP was reallocated from existing FTE within the hospitalist division. During the evening and night shifts, the HMED team's responsibilities were rolled into existing hospitalist duties.
The HMED team provides clinical care for 2 groups of patients in the ED. The first group represents admitted patients who are still awaiting a medicine ward bed as of 7:00 AM. The HMED team provides ongoing care until discharge from the ED or transfer to a medicine floor. The second group of patients includes new admissions that need to stay in the ED due to a lack of available medicine floor beds. For these patients, the HMED team initiates and continues care until discharge from the ED or transfer to a medical floor (Figure 1).
The physician on the HMED team assists nursing supervisors with bed management by providing detailed clinical knowledge, including proximity to discharge as well as updated information on telemetry and intensive care unit (ICU) appropriateness. The HMED team's physician maintains constant knowledge of hospital census via an electronic bed board, and communicates regularly with medical floors about anticipated discharges and transfers to understand the hospital's patient flow status (Figure 2).
The RIE that resulted in the HMED team was part of the Inpatient Medicine Value Stream, which had the overall goal of saving DHMC $300,000 for 2009. Ten RIEs were planned for this value stream in 2009, with an average of $30,000 of savings expected from each RIE.
Determination of ED Diversion Time
DHMC places responsibility for putting the hospital on an ED Diversion status in the hands of the Emergency Medicine Attending Physician. Diversion is categorized as either due to: (1) excessive ED volume for available ED bedsfull or nearly full department, or full resuscitation rooms without the ability to release a room; or (2) excessive boardingmore than 12 admitted patients awaiting beds in the ED. Other reasons for diversion, such as acute, excessive resource utilization (multiple patients from a single event) and temporary limitation of resources (critical equipment becoming inoperative), are also infrequent causes of diversion that are recorded. The elapsed time during which the ED is on diversion status is recorded and reported as a percentage of the total time on a monthly basis.
Determination of ED Diversion Costs
The cost of diversion at DHMC is calculated by multiplying the average number of ambulance drop‐offs per hour times the number of diversion hours to determine the number of missed patients. The historical mean charges for each ambulance patient are used to determine total missed charge opportunity, which is then applied to the hospital realization rate to calculate missed revenue. In addition, the marginal costs related to Denver Health Medical Plan patients that were unable to be repatriated to DHMC from outlying hospitals, as a result of diversion, is added to the net missed revenue figure. This figure is then divided by the number of diversion hours for the year to determine the cost of each diversion hour. For 2009, the cost of each hour of diversion at DHMC was $5000.
Statistical Analysis
All analyses were performed using SAS Enterprise Guide 4.1 (SAS Institute, Inc, Cary, NC). A Student t test or Wilcoxon rank sum test was used to compare continuous variables, and a chi‐square test was used to compare categorical variables.
Our primary outcome was ED diversion due to hospital bed capacity. These data are recorded, maintained, and analyzed by a DHMC internally developed emergency medical services information system (EMeSIS) that interfaces with computerized laboratory reporting systems, and stores, in part, demographic data as well as real‐time data related to the timing of patient encounters for all patients evaluated in the ED. To assess the effect of the intervention on ED diversion, the proportion of total hours on diversion due to medicine bed capacity was compared preimplementation and postimplementation with a chi‐squared test.
Secondary outcomes for patient flow included: (1) the proportion of patients discharged within 8 hours of transfer to a medical floor; and (2) the proportion of admitted medicine patients discharged from the ED. These data were gathered from the Denver Health Data Warehouse which pools data from both administrative and clinical applications used in patient care. Chi‐squared tests were also used to compare secondary outcomes preintervention and postintervention.
To measure the quality and safety of the HMED team, pre‐ED and post‐ED length of stay (LOS), 48‐hour patient return rate, intensive care unit (ICU) transfer rate, and the total LOS for patients admitted to the HMED team and handed off to a medicine floor team were assessed with the Student t test. To assess timeliness of clinical care provided to boarded medicine patients, self‐reported rounding times were compared preintervention and postintervention with the Student t test.
To assess satisfaction with the HMED team, an anonymous paper survey was administered to ED attendings and nursing supervisors 1 year after the intervention was introduced. The survey consisted of 5 questions, and used a 5‐point Likert scale ranging from strongly disagree (1) to strongly agree (5). Those answering agree or strongly agree were compared to those who were neutral, disagreed, or strongly disagreed.
RESULTS
The ED saw 48,595 patients during the intervention period (August 1, 2009June 30,2010) which did not differ statistically from the 50,469 patients seen in the control period (August 1, 2008June 30, 2009). The number of admissions to the medicine service during the control period (9727) and intervention period (10,013), and the number of total medical/surgical admissions during the control (20,716) and intervention (20,574) periods did not statistically differ. ED staffing during the intervention did not change. The overall number of licensed beds did not increase during the study period. During the control period, staffed medical/surgical beds increased from 395 to 400 beds, while the number of staffed medical/surgical beds decreased from 400 to 397 beds during the intervention period. Patient characteristics were similar during the 2 time periods, with the exception of race (Table 1).
| Patients Admitted to Medicine and Transferred to a Medicine Floor | Pre | Post | P Value |
|---|---|---|---|
| |||
| No. | 1901 | 1828 | |
| Age* | 53 15 | 54 14 | 0.59 |
| Gender (% male) | 55% | 52% | 0.06 |
| Race (% white) | 40% | 34% | <0.0001 |
| Insurance (% insured) | 67% | 63% | 0.08 |
| Charlson Comorbidity Index | 1.0 [1.0, 1.0] | 1.0 [1.0, 1.0] | 0.52 |
Diversion Hours
After implementation of the HMED team, there was a relative reduction of diversion due to medicine bed capacity of 27% (4.5%3.3%; P < 0.01) (Table 2). During the same time period, the relative proportion of hours on diversion due to ED capacity decreased by 55% (9.9%5.4%).
| Pre | Post | P Value | |
|---|---|---|---|
| |||
| Divert hours due to bed capacity (%, hours)* | 4.5% (3624) | 3.3% (3624) | 0.009 |
| Admitted ED patients transferred to floor | |||
| Discharged within 8 h (%, N) | 1.3% (1901) | 0.5% (1828) | 0.03 |
| Boarded patients rounded on in the ED and transferred to the medical floor | |||
| Total length of stay (days, N) | 2.6 [2.4, 3.2] (154) | 2.5 [2.4, 2.6] (364) | 0.21 |
| All discharges and transfers to the floor | |||
| Discharged from ED [%, (N)] | 4.9% (2009) | 7.5% (1981) | <0.001 |
| ED length of stay [hours, (N)] | 12:09 8:44 (2009) | 12:48 10:00 (1981) | 0.46 |
| Return to hospital <48 h [%, (N)] | 4.6% (2009) | 4.8% (1981) | 0.75 |
| Transfer to the ICU [%, (N)] | 3.3% (2009) | 4.2% (1981) | 0.13 |
Bed Management and Patient Flow
The HMED team rounded on boarded ED patients a mean of 2 hours and 9 minutes earlier (10:59 AM 1:09 vs 8:50 AM 1:20; P < 0.0001). After implementation of the HMED team, patients transferred to a medicine floor and discharged within 8 hours decreased relatively by 67% (1.5%0.5%; P < 0.01), and discharges from the ED of admitted medicine patients increased relatively by 61% (4.9%7.9%; P < 0.001) (Table 2). ED LOS, total LOS, 48‐hour returns to the ED, and ICU transfer rate for patients managed by the HMED team did not change (Table 2).
Perception and Satisfaction
Nine out of 15 (60%) ED attendings and 7 out of 8 (87%) nursing supervisors responded to the survey. The survey demonstrated that ED attendings and nursing supervisors believe the HMED team improves clinical care for boarded patients, communication, collegiality, and patient flow (Table 3).
| Postimplementation of the HMED Team | Total (n = 16) | ED Attendings (n = 9) | Nursing Supervisors (n = 7) |
|---|---|---|---|
| |||
| Quality of care has improved | 94 | 89 | 100 |
| Communication has improved | 94 | 89 | 100 |
| Collegiality and clinical decision‐making has improved | 94 | 100 | 89 |
| Patient flow has improved | 81 | 67 | 100 |
| HMED team is an asset to DHMC | 94 | 89 | 100 |
Financial
The 27% relative reduction in ED diversion due to hospital bed capacity extrapolates to 105.1 hours a year of decreased diversion, accounting for $525,600 of increased annual revenues.
DISCUSSION
This study suggests that an HMED team can decrease ED diversion, due to hospital bed capacity, by improving patient flow and timeliness of care for boarded medicine patients in the ED.
After participating in bed management, ED diversion due to a lack of medicine beds decreased. This is consistent with findings by Howell and colleagues who were able to improve throughput and decrease ED diversion with active bed management.13 Howell and colleagues decreased diversion hours due to temporary ED overload, and diversion hours due to a lack of telemetry or critical care beds. At DHMC, diversion is attributed to either a lack of ED capacity or lack of hospital beds. The primary outcome was the diversion rate due to lack of hospital beds, but it is possible that increased discharges directly from the ED contributed to the decrease in diversion due to ED capacity, underestimating the effect our intervention had on total ED diversion. There were no other initiatives to decrease diversion due to ED capacity during the study periods, and ED capacity and volume did not change during the intervention period.
While there were no statistically significant changes in staffed medical/surgical beds or medicine admissions, staffed medical/surgical beds during the intervention period decreased while there were more admissions to medicine. Both of these variables would increase diversion, resulting in an underestimation of the effect of the intervention.
Howell and colleagues improved throughput in the ED by implementing a service which provided active bed management without clinical responsibilities,13 while Briones and colleagues improved clinical care of patients boarded in the ED without affecting throughput.14 The HMED team improved throughput and decreased ED diversion while improving timeliness of care and perception of care quality for patients boarding in the ED.
By decreasing unnecessary transfers to medicine units and increasing discharges from the ED, patient flow was improved. While there was no difference in ED LOS, there was a trend towards decreased total LOS. A larger sample size or a longer period of observation would be necessary to determine if the trend toward decreased total LOS is statistically significant. ED LOS may not have been decreased because patients who would have been sent to the floor only to be discharged within 8 hours were kept in the ED to expedite testing and discharge, while sicker patients were sent to the medical floor. This decreased the turnover time of inpatient beds and allowed more boarded patients to be moved to floor units.
There was concern that an HMED team would fragment care, which would lead to an increased LOS for those patients who were transferred to a medical floor and cared for by an additional medicine team before discharge.17 As noted, there was a trend towards a decreased LOS for patients initially cared for by the HMED team.
In this intervention, hospital medicine physicians provided information regarding ongoing care of patients boarded in the ED to nursing supervisors. Prior to the intervention, nursing supervisors relied upon information from the ED staff and the boarded patient's time in the ED to assign a medical floor. However, ED staff was not providing care to boarded patients and did not know the most up‐to‐date status of the patient. This queuing process and lack of communication resulted in patients ready for discharge being transferred to floor beds and discharged within a few hours of transfer. The HMED team allowed nursing supervisors to have direct knowledge regarding clinical status, including telemetry and ICU criteria (similar to Howell and colleagues13), and readiness for discharge from the physician taking care of the patient.
By managing boarded patients, an HMED team can improve timeliness and coordination of care. Prior to the intervention, boarded ED patients were the last to be seen on rounds. The HMED team rounds only in the ED, expediting care and discharges. The increased proportion of boarded patients discharged from the ED by the HMED team is consistent with Briones and colleagues' clinically oriented team managing boarding patients in the ED.14
Potential adverse effects of our intervention included increased returns to the ED, increased ICU transfer rate, and decreased housestaff satisfaction. There was no increase in the 48‐hour return rate and no increase in the ICU transfer rate for patients cared for by the HMED team. Housestaff at DHMC are satisfied with the HMED team, since the presence of the HMED team allows them to concentrate on patients on the medical floors.
This intervention provides DHMC with an additional $525,600 in revenue annually. Since existing FTE were reallocated to create the HMED team, no additional FTE were required. In our facility, AHPs take on duties of housestaff. However, only 1 physician may be needed to staff an HMED team. This physician's clinical productivity is about 75% of other physicians; therefore, 25% of time is spent in bed management. At DHMC, other medicine teams picked up for the decreased clinical productivity of the HMED team, so the budget was neutral. However, using 2 FTE to staff 1 physician daily for 365 days a year, one would need to allocate 0.5 physician FTE (0.25 decrease in clinical productivity 2 FTE) for an HMED team.
Our study has several limitations. As a single center study, our findings may not extrapolate to other settings. The study used historical controls, therefore, undetected confounders may exist. We could not control for simultaneous changes in the hospital, however, we did not know of any other concurrent interventions aimed at decreasing ED diversion. Also, the decision to admit or not is partially based on individual ED attendings, which causes variability in practice. Finally, while we were able to measure rounding times as a process measure to reflect timeliness of care and staff perceptions of quality of care, due to our data infrastructure and the way our housestaff and attendings rotate, we were not able to assess more downstream measures of quality of care.
CONCLUSION
ED crowding decreases throughput and worsens clinical care; there are few proven solutions. This study demonstrates an intervention that reduced the percentage of patients transferred to a medicine floor and discharged within 8 hours, increased the number of discharges from the ED of admitted medicine patients, and decreased ED diversion while improving the timeliness of clinical care for patients boarded in the ED.
Acknowledgements
Disclosure: Nothing to report.
- ,,.Access block causes emergency department overcrowding and ambulance diversion in Perth, Western Australia.Emerg Med J.2005;22:351–354.
- ,,,.The relationship between distance to hospital and patient mortality in emergencies: an observational study.Emerg Med J.2007;24:665–668.
- Institute of Medicine.Committee on the Future of Emergency Care in the United States Health System.Hospital‐Based Emergency Care: At the Breaking Point.Washington, DC:National Academies Press;2007.
- ,.Systematic review of emergency department crowding: causes, effects, and solutions.Ann Emerg Med.2008;52:126–136.
- ,.Emergency department crowding is associated with poor care for patients with severe pain.Ann Emerg Med.2008;51:1–5.
- ,,, et al.The impact of emergency department crowding measures on time to antibiotics for patients with community‐acquired pneumonia.Ann Emerg Med.2007;50:510–516.
- ,,, et al;for the DELAYED‐ED Study Group.Impact of delayed transfer of critically ill patients from the emergency department to the intensive care unit.Crit Care Med.2007;35:1477–1483.
- ,,, et al.Impact of a triage liaison physician on emergency department overcrowding and throughput: a randomized controlled trial.Acad Emerg Med.2007;14:702–708.
- ,,.Strategies for dealing with emergency department overcrowding: a one‐year study on how bedside registration affects patient throughput times.Emerg Med J.2007;32:337–342.
- ,,, et al.The effect of emergency department expansion on emergency department overcrowding.Acad Emerg Med.2007;14:338–343.
- ,,,,,.Effect of increased ICU capacity on emergency department length of stay and ambulance diversion.Ann Emerg Med.2005;5:471–478.
- ,,,,.Ambulance diversion reduction: the Sacramento solution.Am J Emerg Med.2006;357:608–613.
- ,,,,,.Active bed management by hospitalists and emergency department throughput.Ann Intern Med.2008;149:804–810.
- ,,, et al.A model of hospitalist role in the care of admitted patients in the emergency department.J Hosp Med.2010;5:360–364.
- ,,,,.Ambulance diversion and lost hospital revenues.Ann Emerg Med.2006;48(6):702–710.
- ,,,.The financial impact of ambulance diversion and patient elopements.Acad Emerg Med.2007;14(1):58–62.
- ,,,,.The impact of fragmentation of hospitalist care on length of stay.J. Hosp. Med.2010;5:335–338.
- ,,.Access block causes emergency department overcrowding and ambulance diversion in Perth, Western Australia.Emerg Med J.2005;22:351–354.
- ,,,.The relationship between distance to hospital and patient mortality in emergencies: an observational study.Emerg Med J.2007;24:665–668.
- Institute of Medicine.Committee on the Future of Emergency Care in the United States Health System.Hospital‐Based Emergency Care: At the Breaking Point.Washington, DC:National Academies Press;2007.
- ,.Systematic review of emergency department crowding: causes, effects, and solutions.Ann Emerg Med.2008;52:126–136.
- ,.Emergency department crowding is associated with poor care for patients with severe pain.Ann Emerg Med.2008;51:1–5.
- ,,, et al.The impact of emergency department crowding measures on time to antibiotics for patients with community‐acquired pneumonia.Ann Emerg Med.2007;50:510–516.
- ,,, et al;for the DELAYED‐ED Study Group.Impact of delayed transfer of critically ill patients from the emergency department to the intensive care unit.Crit Care Med.2007;35:1477–1483.
- ,,, et al.Impact of a triage liaison physician on emergency department overcrowding and throughput: a randomized controlled trial.Acad Emerg Med.2007;14:702–708.
- ,,.Strategies for dealing with emergency department overcrowding: a one‐year study on how bedside registration affects patient throughput times.Emerg Med J.2007;32:337–342.
- ,,, et al.The effect of emergency department expansion on emergency department overcrowding.Acad Emerg Med.2007;14:338–343.
- ,,,,,.Effect of increased ICU capacity on emergency department length of stay and ambulance diversion.Ann Emerg Med.2005;5:471–478.
- ,,,,.Ambulance diversion reduction: the Sacramento solution.Am J Emerg Med.2006;357:608–613.
- ,,,,,.Active bed management by hospitalists and emergency department throughput.Ann Intern Med.2008;149:804–810.
- ,,, et al.A model of hospitalist role in the care of admitted patients in the emergency department.J Hosp Med.2010;5:360–364.
- ,,,,.Ambulance diversion and lost hospital revenues.Ann Emerg Med.2006;48(6):702–710.
- ,,,.The financial impact of ambulance diversion and patient elopements.Acad Emerg Med.2007;14(1):58–62.
- ,,,,.The impact of fragmentation of hospitalist care on length of stay.J. Hosp. Med.2010;5:335–338.
Copyright © 2012 Society of Hospital Medicine
Evolving Practice of Hospital Medicine
Hospitalists are physicians whose primary focus is the general medical care of hospitalized patients. Hospitalists are uniquely positioned to implement strategies to improve patient flow and efficiency.1 With emergency department (ED) diversion reaching rates upward of 70%, lack of access to inpatient beds leads to delayed care with worsened outcomes.25
To improve access to hospital beds, hospitals may increase capacity by either adding beds or by more efficiently using existing beds. Operations management principles have been applied to healthcare to ensure efficient use of beds. These include: reducing variability of scheduled admissions, remeasuring length of stay (LOS) and bed demand after implementing strategies to reduce practice variation, and employing queuing theory to generate predictions of optimal beds needed.6 The Joint Commission implemented a leadership standard (LD 04.03.11) that hospitals develop and implement plans to identify and mitigate impediments to efficient patient flow through the hospital.
To improve access, hospital leaders expect hospitalists to staff in inpatient medicine programs, surgical comanagement, short stay and chest pain units, and active bed management.7 In the following review, we define hospitalists' roles in the aforementioned programs and their effect on patient flow. We also touch on preoperative clinics, palliative care, geographic rounding, and flexible staffing models.
ACUTE INPATIENT CARE
Hospitalists are one of the fastest growing physician groups in the United States.810 Hospitalists improve efficiency and quality of care across a variety of demographic, geographic, and healthcare settings.11, 12 A 2002 retrospective cohort study in a community‐based urban teaching hospital showed that hospitalists decreased LOS by 0.61 days and lowered risk for death in the hospital (adjusted relative hazard, 0.71; 95% confidence interval [CI], 0.540.93).13 A 2004 prospective quasi‐experimental observational study done at an academic teaching hospital showed an adjusted LOS that was 16.2% lower, and adjusted cost 9.7% lower, for patients on the hospitalists' service.14 In 2007, Lindenauer and colleagues found that a national sample of hospitalists decreased LOS by 0.4 days and lowered cost by $286 per patient.15 The findings of these individual studies were supported in a 2009 systematic review of 33 studies by Peterson which showed that hospitalists decrease LOS.16 In a recent study, Kuo and Goodwin showed that while hospitalists decrease LOS and cost, the patients they care for have higher Medicare costs after discharge by $322 per patient, and are more likely to be readmitted (odds ratio, 1.08; CI, 1.041.14).17
The hospitalist model of care continues to grow, and hospitalists will soon number as many as 30,000.18 For acute medical inpatients, the evidence suggests that hospitalists improve patient flow by decreasing LOS while improving other aspects of quality of care. However, Kuo and Goodwin's findings suggest that the transition of care from inpatient to outpatient settings still requires attention.17
SURGICAL COMANAGEMENT
The Society of Hospital Medicine (SHM) core competencies include perioperative medicine.19, 20 In the 2006 SHM national survey, 85% of hospital medicine groups indicated that they participated in surgical comanagement.21
Hospitalists have improved patient flow and outcomes for orthopedic patients. Hospitalist management of hip fracture patients decreases time to surgery and LOS compared to standard care.2224 Phy and colleagues studied 466 patients for 2 years after the inception of hospital medicine comanagement of surgical patients, and found that care by hospitalists decreased LOS by 2.2 days.22 In a retrospective study of 118 patients, Roy and colleagues found that hospitalist‐managed patients had shorter time to consultation and surgery, decreased LOS, and lower costs.23 In a retrospective cohort study, Batsis looked at mortality in 466 patients with hip fracture, and found no difference between hospitalist management and standard care.24 In patients undergoing elective hip and knee arthroplasty, Huddleston and colleagues reported that patients managed by hospitalists had fewer complications and shorter LOS. The nurses and orthopedic surgeons preferred the hospitalistorthopedist comanagement model.25
The benefits of hospitalist comanagement are not limited to adult patients undergoing orthopedic surgery. For high‐risk patients undergoing lower extremity reconstruction surgery, Pinzur and colleagues noted that LOS was shorter for a cohort of patients managed by hospitalists than for a group of historical controls not treated by hospitalists.26 Simon and colleagues studied comanagement for pediatric spinal fusion patients, and found a decrease in LOS from 6.5 to 4.8 days.27
Several factors should be considered in developing and implementing a successful comanagement program. Since comanagement duties may fall upon hospitalists in order to protect surgeons' time,28 hospital medicine groups should ensure adequate staffing prior to taking on additional services. Clear guidelines to delineate roles and responsibilities of the comanaging groups also need to be developed and implemented.29, 30
Comanaging may also involve additional training. Hospitalists who manage neurologic, neurosurgical, trauma, and psychiatric patients report being undertrained for such conditions.31, 32 Hospital medicine groups need to ensure training needs are met and supported. Given the successes of comanagement and the increasing complexity of surgical patients,33 this practice will likely expand to a greater variety of non‐medical patients.
SHORT STAY UNITS
In 2003, short stay units (SSU) were present in approximately 20% of US hospitals, with 11% of hospitals planning on opening one in the next year.34 SSU are designed to manage acute, self‐limited medical conditions that require brief staysusually less than 72 hours. Approximately 80% of SSU patients are discharged home, avoiding hospitalization.35 Historically, SSU have been under the domain of the ED; however, there is an emerging role for hospitalist‐run SSU.36
Despite demand for SSU, little research has been performed on hospitalist‐led SSU. In 2000, Abenhaim and colleagues showed that a hospitalist‐run SSU at a university‐affiliated teaching hospital had a shorter LOS and lower rates of complications and readmissions when compared to medicine teaching services.37 In 2008, Northwestern Memorial Hospital opened a 30‐bed hospitalist‐run SSU; for those patients, LOS decreased by 2 days.38 In 2010, Leykum and colleagues showed that a hospitalist‐run observation unit can decrease LOS from 2.4 days to 2.2 days.39 Careful selection of SSU patients is needed to obtain these results. Lucas and colleagues found that whether or not SSU patients required assistance of specialists was the strongest predictor of unsuccessful stays (>72 hours or inpatient conversion) in SSU.36
Whether SSU are run by hospital medicine or emergency medicine is decided at an institutional level. Location of SSU in a specifically designated area is crucial, as it allows physicians to round efficiently on patients and to work with staff trained in observation services. Development of admission criteria that include specific diagnoses which match hospitalists' scope of practice is also important (Table 1).32
| Evaluation of Diagnostic Syndromes | Treatment of Emergent Conditions |
|---|---|
| |
| Chest pain | Asthma |
| Abdominal pain | Congestive heart failure |
| Fever | Dehydration |
| Gastrointestinal bleed | Hypoglycemia or hyperglycemia |
| Syncope | Hypercalcemia |
| Dizziness | Atrial fibrillation |
| Headache | |
| Chest trauma | |
| Abdominal trauma | |
The protocol‐based and diagnosis‐specific nature of SSU may enhance quality of care through standardization. Future research may delineate the utility of SSU.
CHEST PAIN UNITS
In the United States, in 2004, approximately 6 million patients present annually to EDs with chest pain.40 Cost of care of patients unnecessarily admitted to coronary care units has been estimated to be nearly $3 billion annually.41 Still, as many as 3% of patients with acute myocardial infarction are discharged home.42 Chest pain units (CPU) were developed to facilitate evaluation of patients with chest pain, at low risk for acute coronary syndrome, without requiring inpatient admission. A number of studies have suggested that admission to a CPU is a safe and cost‐effective alternative to hospital admission.4348
CPU have traditionally been staffed by ED physicians and/or cardiologists. In a prepost study, Krantz and colleagues found that a CPU model, incorporating hospitalists at an academic public safety‐net hospital, decreased ED LOS with no difference in 30‐day cardiac event rate.49 Myers and colleagues created a hospitalist‐directed nonteaching service in an academic medical center to admit low‐risk chest pain patients. Patients admitted to the hospitalist service had a statistically significant lower median LOS (23 hours vs 33 hours) and approximately half the median hospital charges than those admitted to teaching services.50 At the same academic medical center, Bayley and colleagues showed that 91% of patients admitted for chest pain waited more than 3 hours for a bed. This adversely affected ED revenue by tying up beds, resulting in an estimated annual loss of $168,300 of hospital revenue. Creation of a hospitalist‐managed service for low‐acuity chest pain patients reduced hospital LOS by 7 hours.51 Somekh and colleagues demonstrated that a protocol‐driven, cardiologist‐run CPU results in a decreased LOS and readmission rate compared to usual care.52 In a non‐peer reviewed case study, Cox Health opened an 8‐bed, hospitalist‐led CPU in 2003. They decreased LOS from 72 to 18 hours, while increasing revenue by $2.5 million a year.53 These studies suggest that hospitalist‐run CPU can decrease LOS, increase revenue, and relieve ED overcrowding.
Development of a successful CPU depends upon clear inclusion/exclusion criteria; close collaboration among ED physicians, hospitalists, and cardiologists; the development of evidence‐based protocols, and the availability of stress testing.
ACTIVE BED MANAGEMENT
As of 2007, 90% of EDs were crowded beyond their capacity.2 ED crowding leads to ambulance diversion,54 which can delay care and increase mortality rates.55 One of the main causes of ED crowding is the boarding of admitted patients.56 Boarded, admitted patients have been shown to have decreased quality of care and patient satisfaction.35
Active bed management (ABM) by hospitalists can decrease ED diversion. Howell and colleagues instituted ABM where hospitalists, as active bed managers, facilitate placement of patients to their inpatient destinations to assist ED flow.57 This 24‐hour, hospitalist‐led, active bed management service decreased both ED LOS and ambulance diversion. The bed manager collaborated real‐time with medicine and ED attending physicians, nursing supervisors, and charge nurses to change patient care status, and assign and facilitate transfer of patients to appropriate units. These hospitalist bed managers were also empowered to activate additional resources when pre‐diversion rounds identified resource limitations and impending ED divert. They found overall ED LOS for admitted patients decreased by 98 minutes, while LOS for non‐admitted patients stayed the same. AMB decreased diversion due to critically ill and telemetry patients by 28% (786 hours), and diversion due to lower acuity patients by 6% (182 hours). This intervention proved cost‐effective. Three full‐time equivalent (FTE) hospitalists' salaries staff 1 active bed manager working 24/7. Nearly 1000 hours of diversion were avoided at an annual savings of $1086 per hour of diversion decreased.
ABM is a new frontier for hospitals in general, and hospitalists in particular. Chadaga and colleagues found that a hospital medicine‐ED team participating in active bed management, while caring for admitted patients boarded in the ED, can decrease ED diversion and improve patient flow. The percentage of patients transferred to a medicine floor and discharged within 8 hours was reduced by 67% (P 0.01), while the number of discharges from the ED of admitted medicine patients increased by 61% (P 0.001).58
To decrease initial investment, components of ABM (ED triage, bed assignment, discharge facilitation) can be instituted in parts. Hospital medicine groups with limited resources may only provide a triage service by phone for difficult ED cases. Bedside evaluations and collaboration with nursing staff to improve bed placement may be a next step, with floor and/or intensive care unit (ICU) rounds to facilitate early discharges as a final component.
OTHER AREAS
Preoperative Clinics
In 2005, SHM cited preoperative clinics as an important aspect of preoperative care.59 Sehgal and Wachter included preoperative clinics as an area for expanding the role of hospitalists in the United States.60 These clinics can decrease delays to surgery, LOS, and cancellations on the day of surgery.61 The Cleveland Clinic established the Internal Medicine Preoperative Assessment, Consultation, and Treatment (IMPACT) Center in 1997, and has decreased surgery delay rate by 49%.59 At Kaiser Bellflower Medical Center, a preoperative medicine service that provides preoperative screening decreased the number of surgical procedures cancelled on the day of surgery by more than half.62 Gates Hospitalists LLC's perioperative care decreased delay to surgery and lost operating room time.63 In order for a preoperative service to be successful, there must be buy‐in from hospitalists, surgeons, and primary care physicians, as well as adequate staffing and clinical support.59
Palliative Care
Palliative care has been identified by SHM as a core competency in hospital medicine.64 There are several key components in delivery of quality palliative care, including communication about prognosis, pain and symptom control, and hospice eligibility.65 Hospitalists are in a unique position to offer and improve palliative care for hospitalized patients. The majority of hospitalists report spending significant amounts of time caring for dying patients; thereby, hospitalists frequently provide end‐of‐life care.66, 67 Compared to community‐based physicians, patients cared for by hospitalists have higher odds of having documented family discussions regarding end‐of‐life care, and have fewer or no key symptoms (pain, anxiety, or dyspnea).66 In addition, hospitalists' availability improves response time when a patient's clinical status changes or deteriorates, leading to prompter delivery of symptom alleviation.65 Hospitalists are becoming more experienced with end‐of‐life care, as they are exposed to terminally ill patients on a daily basis. More experience leads to improved recognition of patients with limited prognosis, which leads to earlier discussions about goals of care and faster delivery of palliative care. Perhaps this could decrease LOS and be a future area of study.
Geographic Rounding
In the last 5 years, hospital administrators have promoted geographic rounding, where hospitalists see all their patients in 1 geographic location.69 The driving forces behind this include poor patient satisfaction with physician availability, large amounts of time spent by hospitalists in transit to and from patient locations, and frustrations regarding communication with nursing.70 Several groups have instituted this with success. Cleveland Clinic and Virtua Memorial Hospital have found improved patient satisfaction and decreased LOS.69, 70 O'Leary and colleagues found improved awareness of care plans by the entire team.71 Caution should be taken to assure proper physician‐to‐patient ratios, avoid physician isolation, and coordinate physician shifts with bed assignments.69 To address some of these issues, groups have used a hybrid model where a hospitalist is primarily located on one unit but can flex or overflow onto another unit.70 Steps to success with geographic rounding include buy‐in from the institution and nursing, assuring a safe physician‐to‐patient ratio, avoiding wasted beds, and facilitating multidisciplinary rounds.69
Flexible Staffing Models
In SHM's 2010 State of Hospital Medicine Report, 70% of hospitalist groups used a fixed shift‐based staffing model (ie, 7 days on/7 days off).72 Flexible staffing models in which physician coverage is adjusted to patient volume are growing in popularity. This model can be tailored for each institution by examining admission and patient volume trends to increase coverage during busy periods and decrease coverage during slower periods. Potential benefits include alleviating burn out, reducing LOS, and improving patient outcomes. Nursing data suggests that a higher patient‐to‐nursing ratio is associated with increased 30‐day mortality,73 and an ED study found that increasing physician coverage during the evening shift shortened ED LOS by 20%.74 To date, none of these endpoints have been studied for hospital medicine.
CONCLUSION
While many hospital medicine groups were started to provide acute inpatient medical care, most have found that their value to hospitals reaches beyond bedside care. With an epidemic of ED diversion and lack of access to hospital beds and services, optimizing throughput has become imperative for hospital systems. While hospital access can be improved with addition of new beds, improving throughput by decreasing LOS maximizes utilization of existing resources.
We have reviewed how hospitalists improve patient flow in acute inpatient medicine, surgical comanagement, short stay units, chest pain units, and active bed management. In each instance, the literature supports measures for decreasing LOS while maintaining or improving quality of care. Hinami and colleagues showed physician satisfaction with hospitalist‐provided patient care.75 Most studies have been limited by tracking upstream effects of improved efficiency. As there is now some evidence that decreasing LOS may increase readmissions,17 future studies should incorporate this metric into their outcomes. The effect of formal operations management principles on patient flow and bed efficiency is not well known and should be further examined.
In addition, we have touched on other areas (perioperative clinics, palliative care, geographic rounding, and flexible staffing models) where hospitalists may impact patient throughput. These areas represent excellent opportunities for future research.
Hospitalist participation in many of these areas is in its infancy. Hospital medicine programs interested in expanding their services, beyond acute inpatient care, have the opportunity to develop standards and continue research on the effect of hospital medicine‐led services on patient care and flow.
Acknowledgements
Disclosure: All authors disclose no relevant or financial conflicts of interest.
- SHM Benchmarks Committee. Maximizing throughput and improving patient flow. The Hospitalist, Supplement: How Hospitalists Add Value. Philadelphia, PA: Society of Hospital Medicine; 2005. Available online at http://www.the‐hospitalist.org/details/article/279433/Maximizing_Throughput_and_Improving_Patient_Flow.html. Accessed on July 2009.
- Institute of Medicine, Committee on the Future of Emergency Care in the United States Health System. Hospital‐Based Emergency Care: At the Breaking Point. Washington, DC: National Academies Press; 2007.
- , . Emergency department crowding is associated with poor care for patients with severe pain. Ann Emerg Med. 2008;51:1–5.
- , , , et al. The impact of emergency department crowding measures on time to antibiotics for patients with community‐acquired pneumonia. Ann Emerg Med. 2007;50:510–516.
- , , , , ; for the DELAYED‐ED Study Group. Impact of delayed transfer of critically ill patients from the emergency department to the intensive care unit. Crit Care Med. 2007;35:1477–1483.
- . Managing Patient Flow in Hospitals: Strategies and Solutions, 2nd ed. In: Beurhaus P, Rudolph M, Prenney B, et al, eds. Joint Commission Resources, Joint Commission Resources, Inc., 2009.
- , , , . California hospital leader's view of hospitalists: meeting needs of the present and the future. J Hosp Med. 2009;4(9):528–534.
- , . The emerging role of “hospitalists” in the American health care system. N Engl J Med. 1996;335:514–517.
- , , , et al. Trends in market demand for internal medicine 1999–2004: an analysis of physician job advertisements. J Gen Intern Med. 2006;21:1079–1085.
- , , , et al. Hospitalists and the practice of inpatient medicine: results of a survey of the National Association of Inpatient Physicians. Ann Intern Med. 1999;130:343–349.
- , , , et al. Reorganizing an academic medical service impact on cost, quality, patient satisfaction, and education. JAMA. 1998;279:1560–1565.
- , . The hospitalist movement 5 years later. JAMA. 2002;287:487–494.
- , , , , , . Implementation of a voluntary hospitalist service at a community teaching hospital: improved clinical efficiency and patient outcomes. Ann Intern Med. 2002;137(11):859–865.
- , , . Associations with reduced length of stay and costs on an academic hospitalist service. Am J Manag Care. 2004;10(8):561–568.
- , , , et al. Outcomes of care by hospitalists, general internists and family physicians. N Engl J Med. 2007;357(25):2589–2600.
- . Systematic review of outcomes and quality measures in adult patients cared for by hospitalists vs nonhospitalists. Mayo Clin Proc. 2009;84(3):248–254.
- , . Association of hospitalist care with medical utilization after discharge: evidence of cost shift from a cohort study. Ann Intern Med. 2011;155:152–159.
- , , , et al. The potential size of the hospitalist workforce in the United States. Am Med. 1999;106(4):441–445.
- , . Surgical co‐management: a natural evolution of hospitalist practice. J Hosp Med. 2008;3:394–397.
- , , , et al. The core competencies in hospital medicine: a framework for curriculum development. J Hosp Med. 2006;1(suppl 1):1–30.
- Society of Hospital Medicine. Co‐Management Task Force Page. Available at: http://www.hospitalmedicine.org/AM/Template.cfm? Section=Home165(7):796–801.
- , , , et al. Associations between the hospitalist model of care and quality‐of‐care‐related outcomes in patients undergoing hip fracture surgery. Mayo Clin Proc. 2006;81(1):28–31.
- . Effects of a hospitalist care model on mortality of elderly patients with hip fractures. J Hosp Med. 2007;2(4):219–225.
- , , , et al; for the Hospital‐Orthopedic Team Trial Investigators. Medical and surgical co‐management after elective hip and knee arthroplasty: a randomized, controlled trial. Ann Intern Med. 2004;141(1):28–38.
- , , , et al. Hospitalist‐orthopedic co‐management of high‐risk patients undergoing lower extremity reconstruction surgery. Orthopedics. 2009;32(7):495.
- , , , et al. Pediatric hospitalist co‐management of spinal fusion surgery patients. J Hosp Med. 2007;2:23–29.
- . Just because you can, doesn't mean that you should: a call for the rational application of hospitalist co‐management. J Hosp Med. 2008;3:398–402.
- Society of Hospital Medicine. SHM White Paper: Co‐Management White Paper. Philadelphia, PA: 2010.
- American Medical Association, Council on Ethical and Judicial Affairs. CEJA Report 5–I‐99. Ethical Implications of Surgical Co‐Management. Available at: http://www.ama‐assn.org/resources/doc/code‐medical‐ethics/8043a.pdf. Accessed November 17, 2011.
- , , , et al. Hospitalist care and length of stay in patients requiring complex discharge planning and close clinical monitoring. Arch Intern Med. 2007;167:1869–1874.
- , , , et al. Hospitalist's perceptions of their residency training needs: results of a national survey. Am J Med. 2001;111:247–254.
- , . Why perioperative medicine matters more than ever. Cleve Clin J Med. 2006;73(supp 1):S1.
- , , , et al. A national survey of observation units in the United States. Am J Emerg Med. 2003;12:529–533.
- Society of Hospital Medicine. SHM White Paper: Observation Unit White Paper. Philadelphia, PA: 2009.
- , , , et al. A hospitalist‐run short‐stay unit: features that predict length‐of‐stay and eventual admission to traditional inpatient services. J Hosp Med. 2009;4(5):276–284.
- , , , . Program description: a hospitalist‐run medical short‐stay unit in a teaching hospital. Can Med Assoc J. 2000:163(11):1477–1480.
- . Hospitalists can cut ED overcrowding. ACEP News. 2010.
- , , . Implementation of a hospitalist‐run observation unit and impact on length of stay (LOS): a brief report. J Hosp Med. 2010;5(9):E2–E5.
- , . National Hospital Ambulatory Medical Care survey: 2004 emergency department summary. Adv Data. 2006;23:1–29.
- , . Identification of chest pain patients appropriate for an emergency department observation unit. Emerg Med Clin North Am. 2001;19:35–66.
- , , . Stress testing for risk stratification of patients with low to moderate probability of acute cardiac ischemia. Emerg Med Clin North Am. 2001;19:87–103.
- , , , et al. An evaluation of a chest pain diagnostic protocol to exclude acute cardiac ischemia in the emergency department. Arch Intern Med. 1997;157:1085–1091.
- , , . The Chest Pain Evaluation Center at the University of Maryland Medical Center. Md Med J. 1994;43:1047–1052.
- , , , , . Cost effectiveness of mandatory stress testing in chest pain center patients. Ann Emerg Med. 1997;29:88–98.
- , , , et al. A rapid diagnostic and treatment center for patients with chest pain in the emergency department. Ann Emerg Med. 1995;25:1–8.
- , , , , . An emergency department‐based protocol for rapidly ruling out myocardial ischemia reduces hospital time and expense: results of a randomized study (ROMIO). J Am Coll Cardiol. 1996;28:25–33.
- , , , et al. Randomized controlled trial and economic evaluation of a chest pain observation unit compared with routine care. BMJ. 2004;328:254.
- , , , et al. A cooperative care model: cardiologists and hospitalists reduce length of stay in a chest pain observation unit. Crit Pathw Cardiol. 2005;4(2):55–58.
- , , , et al. Improving resource utilization in a teaching hospital: development of a nonteaching service for chest pain admissions. Acad Med. 2006;81(5):432–435.
- , , , et al. The financial burden of emergency department congestion and hospital crowding for chest pain patients awaiting admission. Ann Emerg Med. 2005;45(2):110–117.
- , , , , . Differences in diagnostic evaluation and clinical outcomes in the care of patients with chest pain based on admitting service: the benefits of a dedicated chest pain unit. J Nucl Cardiol. 2008;15(2):186–192.
- . Taking charge of observation units. Today's Hospitalist. July 2007.
- , , . Access block cause emergency department overcrowding and ambulance diversion in Perth, Western Australia. Emerg Med J. 2005;22:351–354.
- , , , . The relationship between distance to hospital and patient mortality in emergencies: an observational study. Emerg Med J. 2007;24:665–668.
- , . Systematic review of emergency department crowding: causes, effects, and solutions. Ann Emerg Med. 2008;52:126–136.
- , , , , , . Active bed management by hospitalists and emergency department throughput. Ann Intern Med. 2008;149:804–810.
- , , , et al. A hospitalist‐led emergency department team improves hospital bed efficiency. J Hosp Med. 2010;5(suppl 1):17–18.
- Society of Hospital Medicine. Perioperative care (a special supplement to The Hospitalist). Philadelphia, PA: Society of Hospital Medicine; 2005. Available at: http://www.hospitalmedicine.org/AM/Template.cfm?Section=Home136:591–596.
- Hospitalist Management Advisor. Hospitalist branch into preoperative medicine with preop assessments. Marblehead, MA: HCPro, 2006. Available at: http://www.hcpro.com/HOM‐57460–3615/Hospitalists‐branch‐into‐perioperative‐medicine‐with‐preop‐assessments.html. Accessed February 15, 2012.
- . The preoperative medicine service: an innovative practice at Kaiser Bellflower Medical Center. The Permanente Journal. 2002;6:13–16.
- . A preop evaluation service delivers unexpected benefits. Today's Hospitalist. January 2008.
- , , , , . The core competencies in hospital medicine: a framework for curriculum development. J Hosp Med. 2006;1:1–67.
- , , , , , . Common myths about caring for patients with terminal illness: opportunities to improve care in the hospital setting. J Hosp Med. 2007;2:357–365.
- . End‐of‐life care in a voluntary hospitalist model: effects on communication, processes of care, and patient symptoms. Am J Med. 2004;116:669–675.
- , , , . Hospitalists and the practice of inpatient medicine: results of a survey of the National Association of Inpatient Physicians. Ann Intern Med. 1999;130:343–349.
- , . Palliative care and hospitalist: an opportunity for cross‐fertilization. Am J Med. 2001;111(suppl):10S–14S.
- . Giving hospitalists their space. ACP Hospitalist. February 2008.
- . Having problems findings your patients? Today's Hospitalists. June 2010.
- , , , et al. Impact of localizing physicians to hospital units on nurse–physician communication and agreement on the plan of care. J Gen Intern Med. 24(11):1223–1227.
- Medical Group Management Association and Society of Hospital Medicine (SHM). State of Hospital Medicine 2010 Report Based on 2009. Available online at http://www.mgma.com/store/Surveys‐and‐Benchmarking/State‐of‐Hospital‐Medicine‐2010‐Report‐Based‐on‐2009 ‐Data‐Print‐Edition/.
- , , , et al. Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. JAMA. 2002;288(16):1987–1993.
- , . Reduced length of stay in medical emergency department patients: a prospective controlled study on emergency physician staffing. Eur J Emerg Med. 2004;11(1):29–34.
- , , , . Provider expectations and experiences of comanagement. J Hosp Med. 2011;6(7):401–404.
Hospitalists are physicians whose primary focus is the general medical care of hospitalized patients. Hospitalists are uniquely positioned to implement strategies to improve patient flow and efficiency.1 With emergency department (ED) diversion reaching rates upward of 70%, lack of access to inpatient beds leads to delayed care with worsened outcomes.25
To improve access to hospital beds, hospitals may increase capacity by either adding beds or by more efficiently using existing beds. Operations management principles have been applied to healthcare to ensure efficient use of beds. These include: reducing variability of scheduled admissions, remeasuring length of stay (LOS) and bed demand after implementing strategies to reduce practice variation, and employing queuing theory to generate predictions of optimal beds needed.6 The Joint Commission implemented a leadership standard (LD 04.03.11) that hospitals develop and implement plans to identify and mitigate impediments to efficient patient flow through the hospital.
To improve access, hospital leaders expect hospitalists to staff in inpatient medicine programs, surgical comanagement, short stay and chest pain units, and active bed management.7 In the following review, we define hospitalists' roles in the aforementioned programs and their effect on patient flow. We also touch on preoperative clinics, palliative care, geographic rounding, and flexible staffing models.
ACUTE INPATIENT CARE
Hospitalists are one of the fastest growing physician groups in the United States.810 Hospitalists improve efficiency and quality of care across a variety of demographic, geographic, and healthcare settings.11, 12 A 2002 retrospective cohort study in a community‐based urban teaching hospital showed that hospitalists decreased LOS by 0.61 days and lowered risk for death in the hospital (adjusted relative hazard, 0.71; 95% confidence interval [CI], 0.540.93).13 A 2004 prospective quasi‐experimental observational study done at an academic teaching hospital showed an adjusted LOS that was 16.2% lower, and adjusted cost 9.7% lower, for patients on the hospitalists' service.14 In 2007, Lindenauer and colleagues found that a national sample of hospitalists decreased LOS by 0.4 days and lowered cost by $286 per patient.15 The findings of these individual studies were supported in a 2009 systematic review of 33 studies by Peterson which showed that hospitalists decrease LOS.16 In a recent study, Kuo and Goodwin showed that while hospitalists decrease LOS and cost, the patients they care for have higher Medicare costs after discharge by $322 per patient, and are more likely to be readmitted (odds ratio, 1.08; CI, 1.041.14).17
The hospitalist model of care continues to grow, and hospitalists will soon number as many as 30,000.18 For acute medical inpatients, the evidence suggests that hospitalists improve patient flow by decreasing LOS while improving other aspects of quality of care. However, Kuo and Goodwin's findings suggest that the transition of care from inpatient to outpatient settings still requires attention.17
SURGICAL COMANAGEMENT
The Society of Hospital Medicine (SHM) core competencies include perioperative medicine.19, 20 In the 2006 SHM national survey, 85% of hospital medicine groups indicated that they participated in surgical comanagement.21
Hospitalists have improved patient flow and outcomes for orthopedic patients. Hospitalist management of hip fracture patients decreases time to surgery and LOS compared to standard care.2224 Phy and colleagues studied 466 patients for 2 years after the inception of hospital medicine comanagement of surgical patients, and found that care by hospitalists decreased LOS by 2.2 days.22 In a retrospective study of 118 patients, Roy and colleagues found that hospitalist‐managed patients had shorter time to consultation and surgery, decreased LOS, and lower costs.23 In a retrospective cohort study, Batsis looked at mortality in 466 patients with hip fracture, and found no difference between hospitalist management and standard care.24 In patients undergoing elective hip and knee arthroplasty, Huddleston and colleagues reported that patients managed by hospitalists had fewer complications and shorter LOS. The nurses and orthopedic surgeons preferred the hospitalistorthopedist comanagement model.25
The benefits of hospitalist comanagement are not limited to adult patients undergoing orthopedic surgery. For high‐risk patients undergoing lower extremity reconstruction surgery, Pinzur and colleagues noted that LOS was shorter for a cohort of patients managed by hospitalists than for a group of historical controls not treated by hospitalists.26 Simon and colleagues studied comanagement for pediatric spinal fusion patients, and found a decrease in LOS from 6.5 to 4.8 days.27
Several factors should be considered in developing and implementing a successful comanagement program. Since comanagement duties may fall upon hospitalists in order to protect surgeons' time,28 hospital medicine groups should ensure adequate staffing prior to taking on additional services. Clear guidelines to delineate roles and responsibilities of the comanaging groups also need to be developed and implemented.29, 30
Comanaging may also involve additional training. Hospitalists who manage neurologic, neurosurgical, trauma, and psychiatric patients report being undertrained for such conditions.31, 32 Hospital medicine groups need to ensure training needs are met and supported. Given the successes of comanagement and the increasing complexity of surgical patients,33 this practice will likely expand to a greater variety of non‐medical patients.
SHORT STAY UNITS
In 2003, short stay units (SSU) were present in approximately 20% of US hospitals, with 11% of hospitals planning on opening one in the next year.34 SSU are designed to manage acute, self‐limited medical conditions that require brief staysusually less than 72 hours. Approximately 80% of SSU patients are discharged home, avoiding hospitalization.35 Historically, SSU have been under the domain of the ED; however, there is an emerging role for hospitalist‐run SSU.36
Despite demand for SSU, little research has been performed on hospitalist‐led SSU. In 2000, Abenhaim and colleagues showed that a hospitalist‐run SSU at a university‐affiliated teaching hospital had a shorter LOS and lower rates of complications and readmissions when compared to medicine teaching services.37 In 2008, Northwestern Memorial Hospital opened a 30‐bed hospitalist‐run SSU; for those patients, LOS decreased by 2 days.38 In 2010, Leykum and colleagues showed that a hospitalist‐run observation unit can decrease LOS from 2.4 days to 2.2 days.39 Careful selection of SSU patients is needed to obtain these results. Lucas and colleagues found that whether or not SSU patients required assistance of specialists was the strongest predictor of unsuccessful stays (>72 hours or inpatient conversion) in SSU.36
Whether SSU are run by hospital medicine or emergency medicine is decided at an institutional level. Location of SSU in a specifically designated area is crucial, as it allows physicians to round efficiently on patients and to work with staff trained in observation services. Development of admission criteria that include specific diagnoses which match hospitalists' scope of practice is also important (Table 1).32
| Evaluation of Diagnostic Syndromes | Treatment of Emergent Conditions |
|---|---|
| |
| Chest pain | Asthma |
| Abdominal pain | Congestive heart failure |
| Fever | Dehydration |
| Gastrointestinal bleed | Hypoglycemia or hyperglycemia |
| Syncope | Hypercalcemia |
| Dizziness | Atrial fibrillation |
| Headache | |
| Chest trauma | |
| Abdominal trauma | |
The protocol‐based and diagnosis‐specific nature of SSU may enhance quality of care through standardization. Future research may delineate the utility of SSU.
CHEST PAIN UNITS
In the United States, in 2004, approximately 6 million patients present annually to EDs with chest pain.40 Cost of care of patients unnecessarily admitted to coronary care units has been estimated to be nearly $3 billion annually.41 Still, as many as 3% of patients with acute myocardial infarction are discharged home.42 Chest pain units (CPU) were developed to facilitate evaluation of patients with chest pain, at low risk for acute coronary syndrome, without requiring inpatient admission. A number of studies have suggested that admission to a CPU is a safe and cost‐effective alternative to hospital admission.4348
CPU have traditionally been staffed by ED physicians and/or cardiologists. In a prepost study, Krantz and colleagues found that a CPU model, incorporating hospitalists at an academic public safety‐net hospital, decreased ED LOS with no difference in 30‐day cardiac event rate.49 Myers and colleagues created a hospitalist‐directed nonteaching service in an academic medical center to admit low‐risk chest pain patients. Patients admitted to the hospitalist service had a statistically significant lower median LOS (23 hours vs 33 hours) and approximately half the median hospital charges than those admitted to teaching services.50 At the same academic medical center, Bayley and colleagues showed that 91% of patients admitted for chest pain waited more than 3 hours for a bed. This adversely affected ED revenue by tying up beds, resulting in an estimated annual loss of $168,300 of hospital revenue. Creation of a hospitalist‐managed service for low‐acuity chest pain patients reduced hospital LOS by 7 hours.51 Somekh and colleagues demonstrated that a protocol‐driven, cardiologist‐run CPU results in a decreased LOS and readmission rate compared to usual care.52 In a non‐peer reviewed case study, Cox Health opened an 8‐bed, hospitalist‐led CPU in 2003. They decreased LOS from 72 to 18 hours, while increasing revenue by $2.5 million a year.53 These studies suggest that hospitalist‐run CPU can decrease LOS, increase revenue, and relieve ED overcrowding.
Development of a successful CPU depends upon clear inclusion/exclusion criteria; close collaboration among ED physicians, hospitalists, and cardiologists; the development of evidence‐based protocols, and the availability of stress testing.
ACTIVE BED MANAGEMENT
As of 2007, 90% of EDs were crowded beyond their capacity.2 ED crowding leads to ambulance diversion,54 which can delay care and increase mortality rates.55 One of the main causes of ED crowding is the boarding of admitted patients.56 Boarded, admitted patients have been shown to have decreased quality of care and patient satisfaction.35
Active bed management (ABM) by hospitalists can decrease ED diversion. Howell and colleagues instituted ABM where hospitalists, as active bed managers, facilitate placement of patients to their inpatient destinations to assist ED flow.57 This 24‐hour, hospitalist‐led, active bed management service decreased both ED LOS and ambulance diversion. The bed manager collaborated real‐time with medicine and ED attending physicians, nursing supervisors, and charge nurses to change patient care status, and assign and facilitate transfer of patients to appropriate units. These hospitalist bed managers were also empowered to activate additional resources when pre‐diversion rounds identified resource limitations and impending ED divert. They found overall ED LOS for admitted patients decreased by 98 minutes, while LOS for non‐admitted patients stayed the same. AMB decreased diversion due to critically ill and telemetry patients by 28% (786 hours), and diversion due to lower acuity patients by 6% (182 hours). This intervention proved cost‐effective. Three full‐time equivalent (FTE) hospitalists' salaries staff 1 active bed manager working 24/7. Nearly 1000 hours of diversion were avoided at an annual savings of $1086 per hour of diversion decreased.
ABM is a new frontier for hospitals in general, and hospitalists in particular. Chadaga and colleagues found that a hospital medicine‐ED team participating in active bed management, while caring for admitted patients boarded in the ED, can decrease ED diversion and improve patient flow. The percentage of patients transferred to a medicine floor and discharged within 8 hours was reduced by 67% (P 0.01), while the number of discharges from the ED of admitted medicine patients increased by 61% (P 0.001).58
To decrease initial investment, components of ABM (ED triage, bed assignment, discharge facilitation) can be instituted in parts. Hospital medicine groups with limited resources may only provide a triage service by phone for difficult ED cases. Bedside evaluations and collaboration with nursing staff to improve bed placement may be a next step, with floor and/or intensive care unit (ICU) rounds to facilitate early discharges as a final component.
OTHER AREAS
Preoperative Clinics
In 2005, SHM cited preoperative clinics as an important aspect of preoperative care.59 Sehgal and Wachter included preoperative clinics as an area for expanding the role of hospitalists in the United States.60 These clinics can decrease delays to surgery, LOS, and cancellations on the day of surgery.61 The Cleveland Clinic established the Internal Medicine Preoperative Assessment, Consultation, and Treatment (IMPACT) Center in 1997, and has decreased surgery delay rate by 49%.59 At Kaiser Bellflower Medical Center, a preoperative medicine service that provides preoperative screening decreased the number of surgical procedures cancelled on the day of surgery by more than half.62 Gates Hospitalists LLC's perioperative care decreased delay to surgery and lost operating room time.63 In order for a preoperative service to be successful, there must be buy‐in from hospitalists, surgeons, and primary care physicians, as well as adequate staffing and clinical support.59
Palliative Care
Palliative care has been identified by SHM as a core competency in hospital medicine.64 There are several key components in delivery of quality palliative care, including communication about prognosis, pain and symptom control, and hospice eligibility.65 Hospitalists are in a unique position to offer and improve palliative care for hospitalized patients. The majority of hospitalists report spending significant amounts of time caring for dying patients; thereby, hospitalists frequently provide end‐of‐life care.66, 67 Compared to community‐based physicians, patients cared for by hospitalists have higher odds of having documented family discussions regarding end‐of‐life care, and have fewer or no key symptoms (pain, anxiety, or dyspnea).66 In addition, hospitalists' availability improves response time when a patient's clinical status changes or deteriorates, leading to prompter delivery of symptom alleviation.65 Hospitalists are becoming more experienced with end‐of‐life care, as they are exposed to terminally ill patients on a daily basis. More experience leads to improved recognition of patients with limited prognosis, which leads to earlier discussions about goals of care and faster delivery of palliative care. Perhaps this could decrease LOS and be a future area of study.
Geographic Rounding
In the last 5 years, hospital administrators have promoted geographic rounding, where hospitalists see all their patients in 1 geographic location.69 The driving forces behind this include poor patient satisfaction with physician availability, large amounts of time spent by hospitalists in transit to and from patient locations, and frustrations regarding communication with nursing.70 Several groups have instituted this with success. Cleveland Clinic and Virtua Memorial Hospital have found improved patient satisfaction and decreased LOS.69, 70 O'Leary and colleagues found improved awareness of care plans by the entire team.71 Caution should be taken to assure proper physician‐to‐patient ratios, avoid physician isolation, and coordinate physician shifts with bed assignments.69 To address some of these issues, groups have used a hybrid model where a hospitalist is primarily located on one unit but can flex or overflow onto another unit.70 Steps to success with geographic rounding include buy‐in from the institution and nursing, assuring a safe physician‐to‐patient ratio, avoiding wasted beds, and facilitating multidisciplinary rounds.69
Flexible Staffing Models
In SHM's 2010 State of Hospital Medicine Report, 70% of hospitalist groups used a fixed shift‐based staffing model (ie, 7 days on/7 days off).72 Flexible staffing models in which physician coverage is adjusted to patient volume are growing in popularity. This model can be tailored for each institution by examining admission and patient volume trends to increase coverage during busy periods and decrease coverage during slower periods. Potential benefits include alleviating burn out, reducing LOS, and improving patient outcomes. Nursing data suggests that a higher patient‐to‐nursing ratio is associated with increased 30‐day mortality,73 and an ED study found that increasing physician coverage during the evening shift shortened ED LOS by 20%.74 To date, none of these endpoints have been studied for hospital medicine.
CONCLUSION
While many hospital medicine groups were started to provide acute inpatient medical care, most have found that their value to hospitals reaches beyond bedside care. With an epidemic of ED diversion and lack of access to hospital beds and services, optimizing throughput has become imperative for hospital systems. While hospital access can be improved with addition of new beds, improving throughput by decreasing LOS maximizes utilization of existing resources.
We have reviewed how hospitalists improve patient flow in acute inpatient medicine, surgical comanagement, short stay units, chest pain units, and active bed management. In each instance, the literature supports measures for decreasing LOS while maintaining or improving quality of care. Hinami and colleagues showed physician satisfaction with hospitalist‐provided patient care.75 Most studies have been limited by tracking upstream effects of improved efficiency. As there is now some evidence that decreasing LOS may increase readmissions,17 future studies should incorporate this metric into their outcomes. The effect of formal operations management principles on patient flow and bed efficiency is not well known and should be further examined.
In addition, we have touched on other areas (perioperative clinics, palliative care, geographic rounding, and flexible staffing models) where hospitalists may impact patient throughput. These areas represent excellent opportunities for future research.
Hospitalist participation in many of these areas is in its infancy. Hospital medicine programs interested in expanding their services, beyond acute inpatient care, have the opportunity to develop standards and continue research on the effect of hospital medicine‐led services on patient care and flow.
Acknowledgements
Disclosure: All authors disclose no relevant or financial conflicts of interest.
Hospitalists are physicians whose primary focus is the general medical care of hospitalized patients. Hospitalists are uniquely positioned to implement strategies to improve patient flow and efficiency.1 With emergency department (ED) diversion reaching rates upward of 70%, lack of access to inpatient beds leads to delayed care with worsened outcomes.25
To improve access to hospital beds, hospitals may increase capacity by either adding beds or by more efficiently using existing beds. Operations management principles have been applied to healthcare to ensure efficient use of beds. These include: reducing variability of scheduled admissions, remeasuring length of stay (LOS) and bed demand after implementing strategies to reduce practice variation, and employing queuing theory to generate predictions of optimal beds needed.6 The Joint Commission implemented a leadership standard (LD 04.03.11) that hospitals develop and implement plans to identify and mitigate impediments to efficient patient flow through the hospital.
To improve access, hospital leaders expect hospitalists to staff in inpatient medicine programs, surgical comanagement, short stay and chest pain units, and active bed management.7 In the following review, we define hospitalists' roles in the aforementioned programs and their effect on patient flow. We also touch on preoperative clinics, palliative care, geographic rounding, and flexible staffing models.
ACUTE INPATIENT CARE
Hospitalists are one of the fastest growing physician groups in the United States.810 Hospitalists improve efficiency and quality of care across a variety of demographic, geographic, and healthcare settings.11, 12 A 2002 retrospective cohort study in a community‐based urban teaching hospital showed that hospitalists decreased LOS by 0.61 days and lowered risk for death in the hospital (adjusted relative hazard, 0.71; 95% confidence interval [CI], 0.540.93).13 A 2004 prospective quasi‐experimental observational study done at an academic teaching hospital showed an adjusted LOS that was 16.2% lower, and adjusted cost 9.7% lower, for patients on the hospitalists' service.14 In 2007, Lindenauer and colleagues found that a national sample of hospitalists decreased LOS by 0.4 days and lowered cost by $286 per patient.15 The findings of these individual studies were supported in a 2009 systematic review of 33 studies by Peterson which showed that hospitalists decrease LOS.16 In a recent study, Kuo and Goodwin showed that while hospitalists decrease LOS and cost, the patients they care for have higher Medicare costs after discharge by $322 per patient, and are more likely to be readmitted (odds ratio, 1.08; CI, 1.041.14).17
The hospitalist model of care continues to grow, and hospitalists will soon number as many as 30,000.18 For acute medical inpatients, the evidence suggests that hospitalists improve patient flow by decreasing LOS while improving other aspects of quality of care. However, Kuo and Goodwin's findings suggest that the transition of care from inpatient to outpatient settings still requires attention.17
SURGICAL COMANAGEMENT
The Society of Hospital Medicine (SHM) core competencies include perioperative medicine.19, 20 In the 2006 SHM national survey, 85% of hospital medicine groups indicated that they participated in surgical comanagement.21
Hospitalists have improved patient flow and outcomes for orthopedic patients. Hospitalist management of hip fracture patients decreases time to surgery and LOS compared to standard care.2224 Phy and colleagues studied 466 patients for 2 years after the inception of hospital medicine comanagement of surgical patients, and found that care by hospitalists decreased LOS by 2.2 days.22 In a retrospective study of 118 patients, Roy and colleagues found that hospitalist‐managed patients had shorter time to consultation and surgery, decreased LOS, and lower costs.23 In a retrospective cohort study, Batsis looked at mortality in 466 patients with hip fracture, and found no difference between hospitalist management and standard care.24 In patients undergoing elective hip and knee arthroplasty, Huddleston and colleagues reported that patients managed by hospitalists had fewer complications and shorter LOS. The nurses and orthopedic surgeons preferred the hospitalistorthopedist comanagement model.25
The benefits of hospitalist comanagement are not limited to adult patients undergoing orthopedic surgery. For high‐risk patients undergoing lower extremity reconstruction surgery, Pinzur and colleagues noted that LOS was shorter for a cohort of patients managed by hospitalists than for a group of historical controls not treated by hospitalists.26 Simon and colleagues studied comanagement for pediatric spinal fusion patients, and found a decrease in LOS from 6.5 to 4.8 days.27
Several factors should be considered in developing and implementing a successful comanagement program. Since comanagement duties may fall upon hospitalists in order to protect surgeons' time,28 hospital medicine groups should ensure adequate staffing prior to taking on additional services. Clear guidelines to delineate roles and responsibilities of the comanaging groups also need to be developed and implemented.29, 30
Comanaging may also involve additional training. Hospitalists who manage neurologic, neurosurgical, trauma, and psychiatric patients report being undertrained for such conditions.31, 32 Hospital medicine groups need to ensure training needs are met and supported. Given the successes of comanagement and the increasing complexity of surgical patients,33 this practice will likely expand to a greater variety of non‐medical patients.
SHORT STAY UNITS
In 2003, short stay units (SSU) were present in approximately 20% of US hospitals, with 11% of hospitals planning on opening one in the next year.34 SSU are designed to manage acute, self‐limited medical conditions that require brief staysusually less than 72 hours. Approximately 80% of SSU patients are discharged home, avoiding hospitalization.35 Historically, SSU have been under the domain of the ED; however, there is an emerging role for hospitalist‐run SSU.36
Despite demand for SSU, little research has been performed on hospitalist‐led SSU. In 2000, Abenhaim and colleagues showed that a hospitalist‐run SSU at a university‐affiliated teaching hospital had a shorter LOS and lower rates of complications and readmissions when compared to medicine teaching services.37 In 2008, Northwestern Memorial Hospital opened a 30‐bed hospitalist‐run SSU; for those patients, LOS decreased by 2 days.38 In 2010, Leykum and colleagues showed that a hospitalist‐run observation unit can decrease LOS from 2.4 days to 2.2 days.39 Careful selection of SSU patients is needed to obtain these results. Lucas and colleagues found that whether or not SSU patients required assistance of specialists was the strongest predictor of unsuccessful stays (>72 hours or inpatient conversion) in SSU.36
Whether SSU are run by hospital medicine or emergency medicine is decided at an institutional level. Location of SSU in a specifically designated area is crucial, as it allows physicians to round efficiently on patients and to work with staff trained in observation services. Development of admission criteria that include specific diagnoses which match hospitalists' scope of practice is also important (Table 1).32
| Evaluation of Diagnostic Syndromes | Treatment of Emergent Conditions |
|---|---|
| |
| Chest pain | Asthma |
| Abdominal pain | Congestive heart failure |
| Fever | Dehydration |
| Gastrointestinal bleed | Hypoglycemia or hyperglycemia |
| Syncope | Hypercalcemia |
| Dizziness | Atrial fibrillation |
| Headache | |
| Chest trauma | |
| Abdominal trauma | |
The protocol‐based and diagnosis‐specific nature of SSU may enhance quality of care through standardization. Future research may delineate the utility of SSU.
CHEST PAIN UNITS
In the United States, in 2004, approximately 6 million patients present annually to EDs with chest pain.40 Cost of care of patients unnecessarily admitted to coronary care units has been estimated to be nearly $3 billion annually.41 Still, as many as 3% of patients with acute myocardial infarction are discharged home.42 Chest pain units (CPU) were developed to facilitate evaluation of patients with chest pain, at low risk for acute coronary syndrome, without requiring inpatient admission. A number of studies have suggested that admission to a CPU is a safe and cost‐effective alternative to hospital admission.4348
CPU have traditionally been staffed by ED physicians and/or cardiologists. In a prepost study, Krantz and colleagues found that a CPU model, incorporating hospitalists at an academic public safety‐net hospital, decreased ED LOS with no difference in 30‐day cardiac event rate.49 Myers and colleagues created a hospitalist‐directed nonteaching service in an academic medical center to admit low‐risk chest pain patients. Patients admitted to the hospitalist service had a statistically significant lower median LOS (23 hours vs 33 hours) and approximately half the median hospital charges than those admitted to teaching services.50 At the same academic medical center, Bayley and colleagues showed that 91% of patients admitted for chest pain waited more than 3 hours for a bed. This adversely affected ED revenue by tying up beds, resulting in an estimated annual loss of $168,300 of hospital revenue. Creation of a hospitalist‐managed service for low‐acuity chest pain patients reduced hospital LOS by 7 hours.51 Somekh and colleagues demonstrated that a protocol‐driven, cardiologist‐run CPU results in a decreased LOS and readmission rate compared to usual care.52 In a non‐peer reviewed case study, Cox Health opened an 8‐bed, hospitalist‐led CPU in 2003. They decreased LOS from 72 to 18 hours, while increasing revenue by $2.5 million a year.53 These studies suggest that hospitalist‐run CPU can decrease LOS, increase revenue, and relieve ED overcrowding.
Development of a successful CPU depends upon clear inclusion/exclusion criteria; close collaboration among ED physicians, hospitalists, and cardiologists; the development of evidence‐based protocols, and the availability of stress testing.
ACTIVE BED MANAGEMENT
As of 2007, 90% of EDs were crowded beyond their capacity.2 ED crowding leads to ambulance diversion,54 which can delay care and increase mortality rates.55 One of the main causes of ED crowding is the boarding of admitted patients.56 Boarded, admitted patients have been shown to have decreased quality of care and patient satisfaction.35
Active bed management (ABM) by hospitalists can decrease ED diversion. Howell and colleagues instituted ABM where hospitalists, as active bed managers, facilitate placement of patients to their inpatient destinations to assist ED flow.57 This 24‐hour, hospitalist‐led, active bed management service decreased both ED LOS and ambulance diversion. The bed manager collaborated real‐time with medicine and ED attending physicians, nursing supervisors, and charge nurses to change patient care status, and assign and facilitate transfer of patients to appropriate units. These hospitalist bed managers were also empowered to activate additional resources when pre‐diversion rounds identified resource limitations and impending ED divert. They found overall ED LOS for admitted patients decreased by 98 minutes, while LOS for non‐admitted patients stayed the same. AMB decreased diversion due to critically ill and telemetry patients by 28% (786 hours), and diversion due to lower acuity patients by 6% (182 hours). This intervention proved cost‐effective. Three full‐time equivalent (FTE) hospitalists' salaries staff 1 active bed manager working 24/7. Nearly 1000 hours of diversion were avoided at an annual savings of $1086 per hour of diversion decreased.
ABM is a new frontier for hospitals in general, and hospitalists in particular. Chadaga and colleagues found that a hospital medicine‐ED team participating in active bed management, while caring for admitted patients boarded in the ED, can decrease ED diversion and improve patient flow. The percentage of patients transferred to a medicine floor and discharged within 8 hours was reduced by 67% (P 0.01), while the number of discharges from the ED of admitted medicine patients increased by 61% (P 0.001).58
To decrease initial investment, components of ABM (ED triage, bed assignment, discharge facilitation) can be instituted in parts. Hospital medicine groups with limited resources may only provide a triage service by phone for difficult ED cases. Bedside evaluations and collaboration with nursing staff to improve bed placement may be a next step, with floor and/or intensive care unit (ICU) rounds to facilitate early discharges as a final component.
OTHER AREAS
Preoperative Clinics
In 2005, SHM cited preoperative clinics as an important aspect of preoperative care.59 Sehgal and Wachter included preoperative clinics as an area for expanding the role of hospitalists in the United States.60 These clinics can decrease delays to surgery, LOS, and cancellations on the day of surgery.61 The Cleveland Clinic established the Internal Medicine Preoperative Assessment, Consultation, and Treatment (IMPACT) Center in 1997, and has decreased surgery delay rate by 49%.59 At Kaiser Bellflower Medical Center, a preoperative medicine service that provides preoperative screening decreased the number of surgical procedures cancelled on the day of surgery by more than half.62 Gates Hospitalists LLC's perioperative care decreased delay to surgery and lost operating room time.63 In order for a preoperative service to be successful, there must be buy‐in from hospitalists, surgeons, and primary care physicians, as well as adequate staffing and clinical support.59
Palliative Care
Palliative care has been identified by SHM as a core competency in hospital medicine.64 There are several key components in delivery of quality palliative care, including communication about prognosis, pain and symptom control, and hospice eligibility.65 Hospitalists are in a unique position to offer and improve palliative care for hospitalized patients. The majority of hospitalists report spending significant amounts of time caring for dying patients; thereby, hospitalists frequently provide end‐of‐life care.66, 67 Compared to community‐based physicians, patients cared for by hospitalists have higher odds of having documented family discussions regarding end‐of‐life care, and have fewer or no key symptoms (pain, anxiety, or dyspnea).66 In addition, hospitalists' availability improves response time when a patient's clinical status changes or deteriorates, leading to prompter delivery of symptom alleviation.65 Hospitalists are becoming more experienced with end‐of‐life care, as they are exposed to terminally ill patients on a daily basis. More experience leads to improved recognition of patients with limited prognosis, which leads to earlier discussions about goals of care and faster delivery of palliative care. Perhaps this could decrease LOS and be a future area of study.
Geographic Rounding
In the last 5 years, hospital administrators have promoted geographic rounding, where hospitalists see all their patients in 1 geographic location.69 The driving forces behind this include poor patient satisfaction with physician availability, large amounts of time spent by hospitalists in transit to and from patient locations, and frustrations regarding communication with nursing.70 Several groups have instituted this with success. Cleveland Clinic and Virtua Memorial Hospital have found improved patient satisfaction and decreased LOS.69, 70 O'Leary and colleagues found improved awareness of care plans by the entire team.71 Caution should be taken to assure proper physician‐to‐patient ratios, avoid physician isolation, and coordinate physician shifts with bed assignments.69 To address some of these issues, groups have used a hybrid model where a hospitalist is primarily located on one unit but can flex or overflow onto another unit.70 Steps to success with geographic rounding include buy‐in from the institution and nursing, assuring a safe physician‐to‐patient ratio, avoiding wasted beds, and facilitating multidisciplinary rounds.69
Flexible Staffing Models
In SHM's 2010 State of Hospital Medicine Report, 70% of hospitalist groups used a fixed shift‐based staffing model (ie, 7 days on/7 days off).72 Flexible staffing models in which physician coverage is adjusted to patient volume are growing in popularity. This model can be tailored for each institution by examining admission and patient volume trends to increase coverage during busy periods and decrease coverage during slower periods. Potential benefits include alleviating burn out, reducing LOS, and improving patient outcomes. Nursing data suggests that a higher patient‐to‐nursing ratio is associated with increased 30‐day mortality,73 and an ED study found that increasing physician coverage during the evening shift shortened ED LOS by 20%.74 To date, none of these endpoints have been studied for hospital medicine.
CONCLUSION
While many hospital medicine groups were started to provide acute inpatient medical care, most have found that their value to hospitals reaches beyond bedside care. With an epidemic of ED diversion and lack of access to hospital beds and services, optimizing throughput has become imperative for hospital systems. While hospital access can be improved with addition of new beds, improving throughput by decreasing LOS maximizes utilization of existing resources.
We have reviewed how hospitalists improve patient flow in acute inpatient medicine, surgical comanagement, short stay units, chest pain units, and active bed management. In each instance, the literature supports measures for decreasing LOS while maintaining or improving quality of care. Hinami and colleagues showed physician satisfaction with hospitalist‐provided patient care.75 Most studies have been limited by tracking upstream effects of improved efficiency. As there is now some evidence that decreasing LOS may increase readmissions,17 future studies should incorporate this metric into their outcomes. The effect of formal operations management principles on patient flow and bed efficiency is not well known and should be further examined.
In addition, we have touched on other areas (perioperative clinics, palliative care, geographic rounding, and flexible staffing models) where hospitalists may impact patient throughput. These areas represent excellent opportunities for future research.
Hospitalist participation in many of these areas is in its infancy. Hospital medicine programs interested in expanding their services, beyond acute inpatient care, have the opportunity to develop standards and continue research on the effect of hospital medicine‐led services on patient care and flow.
Acknowledgements
Disclosure: All authors disclose no relevant or financial conflicts of interest.
- SHM Benchmarks Committee. Maximizing throughput and improving patient flow. The Hospitalist, Supplement: How Hospitalists Add Value. Philadelphia, PA: Society of Hospital Medicine; 2005. Available online at http://www.the‐hospitalist.org/details/article/279433/Maximizing_Throughput_and_Improving_Patient_Flow.html. Accessed on July 2009.
- Institute of Medicine, Committee on the Future of Emergency Care in the United States Health System. Hospital‐Based Emergency Care: At the Breaking Point. Washington, DC: National Academies Press; 2007.
- , . Emergency department crowding is associated with poor care for patients with severe pain. Ann Emerg Med. 2008;51:1–5.
- , , , et al. The impact of emergency department crowding measures on time to antibiotics for patients with community‐acquired pneumonia. Ann Emerg Med. 2007;50:510–516.
- , , , , ; for the DELAYED‐ED Study Group. Impact of delayed transfer of critically ill patients from the emergency department to the intensive care unit. Crit Care Med. 2007;35:1477–1483.
- . Managing Patient Flow in Hospitals: Strategies and Solutions, 2nd ed. In: Beurhaus P, Rudolph M, Prenney B, et al, eds. Joint Commission Resources, Joint Commission Resources, Inc., 2009.
- , , , . California hospital leader's view of hospitalists: meeting needs of the present and the future. J Hosp Med. 2009;4(9):528–534.
- , . The emerging role of “hospitalists” in the American health care system. N Engl J Med. 1996;335:514–517.
- , , , et al. Trends in market demand for internal medicine 1999–2004: an analysis of physician job advertisements. J Gen Intern Med. 2006;21:1079–1085.
- , , , et al. Hospitalists and the practice of inpatient medicine: results of a survey of the National Association of Inpatient Physicians. Ann Intern Med. 1999;130:343–349.
- , , , et al. Reorganizing an academic medical service impact on cost, quality, patient satisfaction, and education. JAMA. 1998;279:1560–1565.
- , . The hospitalist movement 5 years later. JAMA. 2002;287:487–494.
- , , , , , . Implementation of a voluntary hospitalist service at a community teaching hospital: improved clinical efficiency and patient outcomes. Ann Intern Med. 2002;137(11):859–865.
- , , . Associations with reduced length of stay and costs on an academic hospitalist service. Am J Manag Care. 2004;10(8):561–568.
- , , , et al. Outcomes of care by hospitalists, general internists and family physicians. N Engl J Med. 2007;357(25):2589–2600.
- . Systematic review of outcomes and quality measures in adult patients cared for by hospitalists vs nonhospitalists. Mayo Clin Proc. 2009;84(3):248–254.
- , . Association of hospitalist care with medical utilization after discharge: evidence of cost shift from a cohort study. Ann Intern Med. 2011;155:152–159.
- , , , et al. The potential size of the hospitalist workforce in the United States. Am Med. 1999;106(4):441–445.
- , . Surgical co‐management: a natural evolution of hospitalist practice. J Hosp Med. 2008;3:394–397.
- , , , et al. The core competencies in hospital medicine: a framework for curriculum development. J Hosp Med. 2006;1(suppl 1):1–30.
- Society of Hospital Medicine. Co‐Management Task Force Page. Available at: http://www.hospitalmedicine.org/AM/Template.cfm? Section=Home165(7):796–801.
- , , , et al. Associations between the hospitalist model of care and quality‐of‐care‐related outcomes in patients undergoing hip fracture surgery. Mayo Clin Proc. 2006;81(1):28–31.
- . Effects of a hospitalist care model on mortality of elderly patients with hip fractures. J Hosp Med. 2007;2(4):219–225.
- , , , et al; for the Hospital‐Orthopedic Team Trial Investigators. Medical and surgical co‐management after elective hip and knee arthroplasty: a randomized, controlled trial. Ann Intern Med. 2004;141(1):28–38.
- , , , et al. Hospitalist‐orthopedic co‐management of high‐risk patients undergoing lower extremity reconstruction surgery. Orthopedics. 2009;32(7):495.
- , , , et al. Pediatric hospitalist co‐management of spinal fusion surgery patients. J Hosp Med. 2007;2:23–29.
- . Just because you can, doesn't mean that you should: a call for the rational application of hospitalist co‐management. J Hosp Med. 2008;3:398–402.
- Society of Hospital Medicine. SHM White Paper: Co‐Management White Paper. Philadelphia, PA: 2010.
- American Medical Association, Council on Ethical and Judicial Affairs. CEJA Report 5–I‐99. Ethical Implications of Surgical Co‐Management. Available at: http://www.ama‐assn.org/resources/doc/code‐medical‐ethics/8043a.pdf. Accessed November 17, 2011.
- , , , et al. Hospitalist care and length of stay in patients requiring complex discharge planning and close clinical monitoring. Arch Intern Med. 2007;167:1869–1874.
- , , , et al. Hospitalist's perceptions of their residency training needs: results of a national survey. Am J Med. 2001;111:247–254.
- , . Why perioperative medicine matters more than ever. Cleve Clin J Med. 2006;73(supp 1):S1.
- , , , et al. A national survey of observation units in the United States. Am J Emerg Med. 2003;12:529–533.
- Society of Hospital Medicine. SHM White Paper: Observation Unit White Paper. Philadelphia, PA: 2009.
- , , , et al. A hospitalist‐run short‐stay unit: features that predict length‐of‐stay and eventual admission to traditional inpatient services. J Hosp Med. 2009;4(5):276–284.
- , , , . Program description: a hospitalist‐run medical short‐stay unit in a teaching hospital. Can Med Assoc J. 2000:163(11):1477–1480.
- . Hospitalists can cut ED overcrowding. ACEP News. 2010.
- , , . Implementation of a hospitalist‐run observation unit and impact on length of stay (LOS): a brief report. J Hosp Med. 2010;5(9):E2–E5.
- , . National Hospital Ambulatory Medical Care survey: 2004 emergency department summary. Adv Data. 2006;23:1–29.
- , . Identification of chest pain patients appropriate for an emergency department observation unit. Emerg Med Clin North Am. 2001;19:35–66.
- , , . Stress testing for risk stratification of patients with low to moderate probability of acute cardiac ischemia. Emerg Med Clin North Am. 2001;19:87–103.
- , , , et al. An evaluation of a chest pain diagnostic protocol to exclude acute cardiac ischemia in the emergency department. Arch Intern Med. 1997;157:1085–1091.
- , , . The Chest Pain Evaluation Center at the University of Maryland Medical Center. Md Med J. 1994;43:1047–1052.
- , , , , . Cost effectiveness of mandatory stress testing in chest pain center patients. Ann Emerg Med. 1997;29:88–98.
- , , , et al. A rapid diagnostic and treatment center for patients with chest pain in the emergency department. Ann Emerg Med. 1995;25:1–8.
- , , , , . An emergency department‐based protocol for rapidly ruling out myocardial ischemia reduces hospital time and expense: results of a randomized study (ROMIO). J Am Coll Cardiol. 1996;28:25–33.
- , , , et al. Randomized controlled trial and economic evaluation of a chest pain observation unit compared with routine care. BMJ. 2004;328:254.
- , , , et al. A cooperative care model: cardiologists and hospitalists reduce length of stay in a chest pain observation unit. Crit Pathw Cardiol. 2005;4(2):55–58.
- , , , et al. Improving resource utilization in a teaching hospital: development of a nonteaching service for chest pain admissions. Acad Med. 2006;81(5):432–435.
- , , , et al. The financial burden of emergency department congestion and hospital crowding for chest pain patients awaiting admission. Ann Emerg Med. 2005;45(2):110–117.
- , , , , . Differences in diagnostic evaluation and clinical outcomes in the care of patients with chest pain based on admitting service: the benefits of a dedicated chest pain unit. J Nucl Cardiol. 2008;15(2):186–192.
- . Taking charge of observation units. Today's Hospitalist. July 2007.
- , , . Access block cause emergency department overcrowding and ambulance diversion in Perth, Western Australia. Emerg Med J. 2005;22:351–354.
- , , , . The relationship between distance to hospital and patient mortality in emergencies: an observational study. Emerg Med J. 2007;24:665–668.
- , . Systematic review of emergency department crowding: causes, effects, and solutions. Ann Emerg Med. 2008;52:126–136.
- , , , , , . Active bed management by hospitalists and emergency department throughput. Ann Intern Med. 2008;149:804–810.
- , , , et al. A hospitalist‐led emergency department team improves hospital bed efficiency. J Hosp Med. 2010;5(suppl 1):17–18.
- Society of Hospital Medicine. Perioperative care (a special supplement to The Hospitalist). Philadelphia, PA: Society of Hospital Medicine; 2005. Available at: http://www.hospitalmedicine.org/AM/Template.cfm?Section=Home136:591–596.
- Hospitalist Management Advisor. Hospitalist branch into preoperative medicine with preop assessments. Marblehead, MA: HCPro, 2006. Available at: http://www.hcpro.com/HOM‐57460–3615/Hospitalists‐branch‐into‐perioperative‐medicine‐with‐preop‐assessments.html. Accessed February 15, 2012.
- . The preoperative medicine service: an innovative practice at Kaiser Bellflower Medical Center. The Permanente Journal. 2002;6:13–16.
- . A preop evaluation service delivers unexpected benefits. Today's Hospitalist. January 2008.
- , , , , . The core competencies in hospital medicine: a framework for curriculum development. J Hosp Med. 2006;1:1–67.
- , , , , , . Common myths about caring for patients with terminal illness: opportunities to improve care in the hospital setting. J Hosp Med. 2007;2:357–365.
- . End‐of‐life care in a voluntary hospitalist model: effects on communication, processes of care, and patient symptoms. Am J Med. 2004;116:669–675.
- , , , . Hospitalists and the practice of inpatient medicine: results of a survey of the National Association of Inpatient Physicians. Ann Intern Med. 1999;130:343–349.
- , . Palliative care and hospitalist: an opportunity for cross‐fertilization. Am J Med. 2001;111(suppl):10S–14S.
- . Giving hospitalists their space. ACP Hospitalist. February 2008.
- . Having problems findings your patients? Today's Hospitalists. June 2010.
- , , , et al. Impact of localizing physicians to hospital units on nurse–physician communication and agreement on the plan of care. J Gen Intern Med. 24(11):1223–1227.
- Medical Group Management Association and Society of Hospital Medicine (SHM). State of Hospital Medicine 2010 Report Based on 2009. Available online at http://www.mgma.com/store/Surveys‐and‐Benchmarking/State‐of‐Hospital‐Medicine‐2010‐Report‐Based‐on‐2009 ‐Data‐Print‐Edition/.
- , , , et al. Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. JAMA. 2002;288(16):1987–1993.
- , . Reduced length of stay in medical emergency department patients: a prospective controlled study on emergency physician staffing. Eur J Emerg Med. 2004;11(1):29–34.
- , , , . Provider expectations and experiences of comanagement. J Hosp Med. 2011;6(7):401–404.
- SHM Benchmarks Committee. Maximizing throughput and improving patient flow. The Hospitalist, Supplement: How Hospitalists Add Value. Philadelphia, PA: Society of Hospital Medicine; 2005. Available online at http://www.the‐hospitalist.org/details/article/279433/Maximizing_Throughput_and_Improving_Patient_Flow.html. Accessed on July 2009.
- Institute of Medicine, Committee on the Future of Emergency Care in the United States Health System. Hospital‐Based Emergency Care: At the Breaking Point. Washington, DC: National Academies Press; 2007.
- , . Emergency department crowding is associated with poor care for patients with severe pain. Ann Emerg Med. 2008;51:1–5.
- , , , et al. The impact of emergency department crowding measures on time to antibiotics for patients with community‐acquired pneumonia. Ann Emerg Med. 2007;50:510–516.
- , , , , ; for the DELAYED‐ED Study Group. Impact of delayed transfer of critically ill patients from the emergency department to the intensive care unit. Crit Care Med. 2007;35:1477–1483.
- . Managing Patient Flow in Hospitals: Strategies and Solutions, 2nd ed. In: Beurhaus P, Rudolph M, Prenney B, et al, eds. Joint Commission Resources, Joint Commission Resources, Inc., 2009.
- , , , . California hospital leader's view of hospitalists: meeting needs of the present and the future. J Hosp Med. 2009;4(9):528–534.
- , . The emerging role of “hospitalists” in the American health care system. N Engl J Med. 1996;335:514–517.
- , , , et al. Trends in market demand for internal medicine 1999–2004: an analysis of physician job advertisements. J Gen Intern Med. 2006;21:1079–1085.
- , , , et al. Hospitalists and the practice of inpatient medicine: results of a survey of the National Association of Inpatient Physicians. Ann Intern Med. 1999;130:343–349.
- , , , et al. Reorganizing an academic medical service impact on cost, quality, patient satisfaction, and education. JAMA. 1998;279:1560–1565.
- , . The hospitalist movement 5 years later. JAMA. 2002;287:487–494.
- , , , , , . Implementation of a voluntary hospitalist service at a community teaching hospital: improved clinical efficiency and patient outcomes. Ann Intern Med. 2002;137(11):859–865.
- , , . Associations with reduced length of stay and costs on an academic hospitalist service. Am J Manag Care. 2004;10(8):561–568.
- , , , et al. Outcomes of care by hospitalists, general internists and family physicians. N Engl J Med. 2007;357(25):2589–2600.
- . Systematic review of outcomes and quality measures in adult patients cared for by hospitalists vs nonhospitalists. Mayo Clin Proc. 2009;84(3):248–254.
- , . Association of hospitalist care with medical utilization after discharge: evidence of cost shift from a cohort study. Ann Intern Med. 2011;155:152–159.
- , , , et al. The potential size of the hospitalist workforce in the United States. Am Med. 1999;106(4):441–445.
- , . Surgical co‐management: a natural evolution of hospitalist practice. J Hosp Med. 2008;3:394–397.
- , , , et al. The core competencies in hospital medicine: a framework for curriculum development. J Hosp Med. 2006;1(suppl 1):1–30.
- Society of Hospital Medicine. Co‐Management Task Force Page. Available at: http://www.hospitalmedicine.org/AM/Template.cfm? Section=Home165(7):796–801.
- , , , et al. Associations between the hospitalist model of care and quality‐of‐care‐related outcomes in patients undergoing hip fracture surgery. Mayo Clin Proc. 2006;81(1):28–31.
- . Effects of a hospitalist care model on mortality of elderly patients with hip fractures. J Hosp Med. 2007;2(4):219–225.
- , , , et al; for the Hospital‐Orthopedic Team Trial Investigators. Medical and surgical co‐management after elective hip and knee arthroplasty: a randomized, controlled trial. Ann Intern Med. 2004;141(1):28–38.
- , , , et al. Hospitalist‐orthopedic co‐management of high‐risk patients undergoing lower extremity reconstruction surgery. Orthopedics. 2009;32(7):495.
- , , , et al. Pediatric hospitalist co‐management of spinal fusion surgery patients. J Hosp Med. 2007;2:23–29.
- . Just because you can, doesn't mean that you should: a call for the rational application of hospitalist co‐management. J Hosp Med. 2008;3:398–402.
- Society of Hospital Medicine. SHM White Paper: Co‐Management White Paper. Philadelphia, PA: 2010.
- American Medical Association, Council on Ethical and Judicial Affairs. CEJA Report 5–I‐99. Ethical Implications of Surgical Co‐Management. Available at: http://www.ama‐assn.org/resources/doc/code‐medical‐ethics/8043a.pdf. Accessed November 17, 2011.
- , , , et al. Hospitalist care and length of stay in patients requiring complex discharge planning and close clinical monitoring. Arch Intern Med. 2007;167:1869–1874.
- , , , et al. Hospitalist's perceptions of their residency training needs: results of a national survey. Am J Med. 2001;111:247–254.
- , . Why perioperative medicine matters more than ever. Cleve Clin J Med. 2006;73(supp 1):S1.
- , , , et al. A national survey of observation units in the United States. Am J Emerg Med. 2003;12:529–533.
- Society of Hospital Medicine. SHM White Paper: Observation Unit White Paper. Philadelphia, PA: 2009.
- , , , et al. A hospitalist‐run short‐stay unit: features that predict length‐of‐stay and eventual admission to traditional inpatient services. J Hosp Med. 2009;4(5):276–284.
- , , , . Program description: a hospitalist‐run medical short‐stay unit in a teaching hospital. Can Med Assoc J. 2000:163(11):1477–1480.
- . Hospitalists can cut ED overcrowding. ACEP News. 2010.
- , , . Implementation of a hospitalist‐run observation unit and impact on length of stay (LOS): a brief report. J Hosp Med. 2010;5(9):E2–E5.
- , . National Hospital Ambulatory Medical Care survey: 2004 emergency department summary. Adv Data. 2006;23:1–29.
- , . Identification of chest pain patients appropriate for an emergency department observation unit. Emerg Med Clin North Am. 2001;19:35–66.
- , , . Stress testing for risk stratification of patients with low to moderate probability of acute cardiac ischemia. Emerg Med Clin North Am. 2001;19:87–103.
- , , , et al. An evaluation of a chest pain diagnostic protocol to exclude acute cardiac ischemia in the emergency department. Arch Intern Med. 1997;157:1085–1091.
- , , . The Chest Pain Evaluation Center at the University of Maryland Medical Center. Md Med J. 1994;43:1047–1052.
- , , , , . Cost effectiveness of mandatory stress testing in chest pain center patients. Ann Emerg Med. 1997;29:88–98.
- , , , et al. A rapid diagnostic and treatment center for patients with chest pain in the emergency department. Ann Emerg Med. 1995;25:1–8.
- , , , , . An emergency department‐based protocol for rapidly ruling out myocardial ischemia reduces hospital time and expense: results of a randomized study (ROMIO). J Am Coll Cardiol. 1996;28:25–33.
- , , , et al. Randomized controlled trial and economic evaluation of a chest pain observation unit compared with routine care. BMJ. 2004;328:254.
- , , , et al. A cooperative care model: cardiologists and hospitalists reduce length of stay in a chest pain observation unit. Crit Pathw Cardiol. 2005;4(2):55–58.
- , , , et al. Improving resource utilization in a teaching hospital: development of a nonteaching service for chest pain admissions. Acad Med. 2006;81(5):432–435.
- , , , et al. The financial burden of emergency department congestion and hospital crowding for chest pain patients awaiting admission. Ann Emerg Med. 2005;45(2):110–117.
- , , , , . Differences in diagnostic evaluation and clinical outcomes in the care of patients with chest pain based on admitting service: the benefits of a dedicated chest pain unit. J Nucl Cardiol. 2008;15(2):186–192.
- . Taking charge of observation units. Today's Hospitalist. July 2007.
- , , . Access block cause emergency department overcrowding and ambulance diversion in Perth, Western Australia. Emerg Med J. 2005;22:351–354.
- , , , . The relationship between distance to hospital and patient mortality in emergencies: an observational study. Emerg Med J. 2007;24:665–668.
- , . Systematic review of emergency department crowding: causes, effects, and solutions. Ann Emerg Med. 2008;52:126–136.
- , , , , , . Active bed management by hospitalists and emergency department throughput. Ann Intern Med. 2008;149:804–810.
- , , , et al. A hospitalist‐led emergency department team improves hospital bed efficiency. J Hosp Med. 2010;5(suppl 1):17–18.
- Society of Hospital Medicine. Perioperative care (a special supplement to The Hospitalist). Philadelphia, PA: Society of Hospital Medicine; 2005. Available at: http://www.hospitalmedicine.org/AM/Template.cfm?Section=Home136:591–596.
- Hospitalist Management Advisor. Hospitalist branch into preoperative medicine with preop assessments. Marblehead, MA: HCPro, 2006. Available at: http://www.hcpro.com/HOM‐57460–3615/Hospitalists‐branch‐into‐perioperative‐medicine‐with‐preop‐assessments.html. Accessed February 15, 2012.
- . The preoperative medicine service: an innovative practice at Kaiser Bellflower Medical Center. The Permanente Journal. 2002;6:13–16.
- . A preop evaluation service delivers unexpected benefits. Today's Hospitalist. January 2008.
- , , , , . The core competencies in hospital medicine: a framework for curriculum development. J Hosp Med. 2006;1:1–67.
- , , , , , . Common myths about caring for patients with terminal illness: opportunities to improve care in the hospital setting. J Hosp Med. 2007;2:357–365.
- . End‐of‐life care in a voluntary hospitalist model: effects on communication, processes of care, and patient symptoms. Am J Med. 2004;116:669–675.
- , , , . Hospitalists and the practice of inpatient medicine: results of a survey of the National Association of Inpatient Physicians. Ann Intern Med. 1999;130:343–349.
- , . Palliative care and hospitalist: an opportunity for cross‐fertilization. Am J Med. 2001;111(suppl):10S–14S.
- . Giving hospitalists their space. ACP Hospitalist. February 2008.
- . Having problems findings your patients? Today's Hospitalists. June 2010.
- , , , et al. Impact of localizing physicians to hospital units on nurse–physician communication and agreement on the plan of care. J Gen Intern Med. 24(11):1223–1227.
- Medical Group Management Association and Society of Hospital Medicine (SHM). State of Hospital Medicine 2010 Report Based on 2009. Available online at http://www.mgma.com/store/Surveys‐and‐Benchmarking/State‐of‐Hospital‐Medicine‐2010‐Report‐Based‐on‐2009 ‐Data‐Print‐Edition/.
- , , , et al. Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. JAMA. 2002;288(16):1987–1993.
- , . Reduced length of stay in medical emergency department patients: a prospective controlled study on emergency physician staffing. Eur J Emerg Med. 2004;11(1):29–34.
- , , , . Provider expectations and experiences of comanagement. J Hosp Med. 2011;6(7):401–404.
ACUTE Center for Eating Disorders
Anorexia nervosa occurs in 0.9% of women and 0.3% of men in the United States1 and is associated with a prolonged course,2 extensive medical complications that can affect almost every organ system,3, 4 and a 5% mean crude mortality rate9.6 times expected for age‐matched women in the United States.2, 5 Those with anorexia nervosa die as a complication of their illness more frequently than any other mental illness.3 Anorexia nervosa is commonly diagnosed during the adolescent years,2 with almost 25% going on to develop chronic anorexia nervosa.2, 6 Consequently, many patients with severe anorexia nervosa will receive treatment by adult medicine practitioners.
Patients with anorexia nervosa frequently require hospitalization. Published guidelines suggest that those who are 70% or less than ideal body weight, bradycardic, hypotensive, or those with severe electrolyte disturbances warrant admission for medical stabilization.79 Once admitted, however, there are no published guidelines for best practices to medically stabilize patients.7, 10 Although most experts advocate a multidisciplinary approach with weight restoration and medical stability as the goals of hospital admission,8, 9 controversy exists in the literature about how best to achieve these goals.7, 10
It is known, however, that for patients with complicated medical illnesses, such as human immunodeficiency virus (HIV) and sepsis, higher volumes of patient caseloads treated by physicians with disease‐specific expertise has been found to lead to improved outcomes in patients.11, 12 The adult patient with severe anorexia nervosa who requires inpatient medical stabilization may also benefit from a multidisciplinary trained staff familiar with the medical management of anorexia nervosa. Accordingly, we have developed the Acute Comprehensive Urgent Treatment for Eating Disorders (ACUTE) Center.
PROGRAM DESCRIPTION
The ACUTE Center at Denver Health is a 5‐bed unit dedicated to the medical stabilization of patients with severe malnutrition due to anorexia nervosa or severe electrolyte disorders due to bulimia nervosa. ACUTE accepts patients 17 years and older with medical complications related to chronic malnutrition and refeeding.
ACUTE uses a multidisciplinary approach to patient care. The physician team is composed of a hospital medicine attending physician, consultative expertise by an internal medicine specialist in the management of the medical complications of eating disorders, and a psychiatrist specializing in eating disorders. There is a dedicated team of nurses, two dieticians, physical therapists, certified nursing assistants, speech therapists, a psychotherapist, and a chaplain.
ACUTE patients are on continuous telemetry monitoring for the duration of their hospitalization to monitor for arrhythmias as well as signs of covert exercise. As part of the initial intake, a full set of vital signs is obtained, including height and weight. Patients are weighed daily with their back to the scale. There is no discussion of weight fluctuations. Patients may walk at a slow pace around the unit. No exercise is allowed.
Each patient at the ACUTE Center has an individualized meal plan and are started on an oral caloric intake 200 kcal below their basal energy expenditure (BEE). Indirect calorimetry is performed on the first hospital day. Each patient meets on a daily basis with the registered dietician to choose meals that meet their caloric goals.
All patients have a sitter continuously for their first week, and thereafter sitter time may be reduced to supervision surrounding each meal. Patients who fail to finish their prescribed meal are required to drink a liquid supplement to meet caloric goals. Calories are increased weekly until the patient's weight shows a clear pattern of weight increase. 0
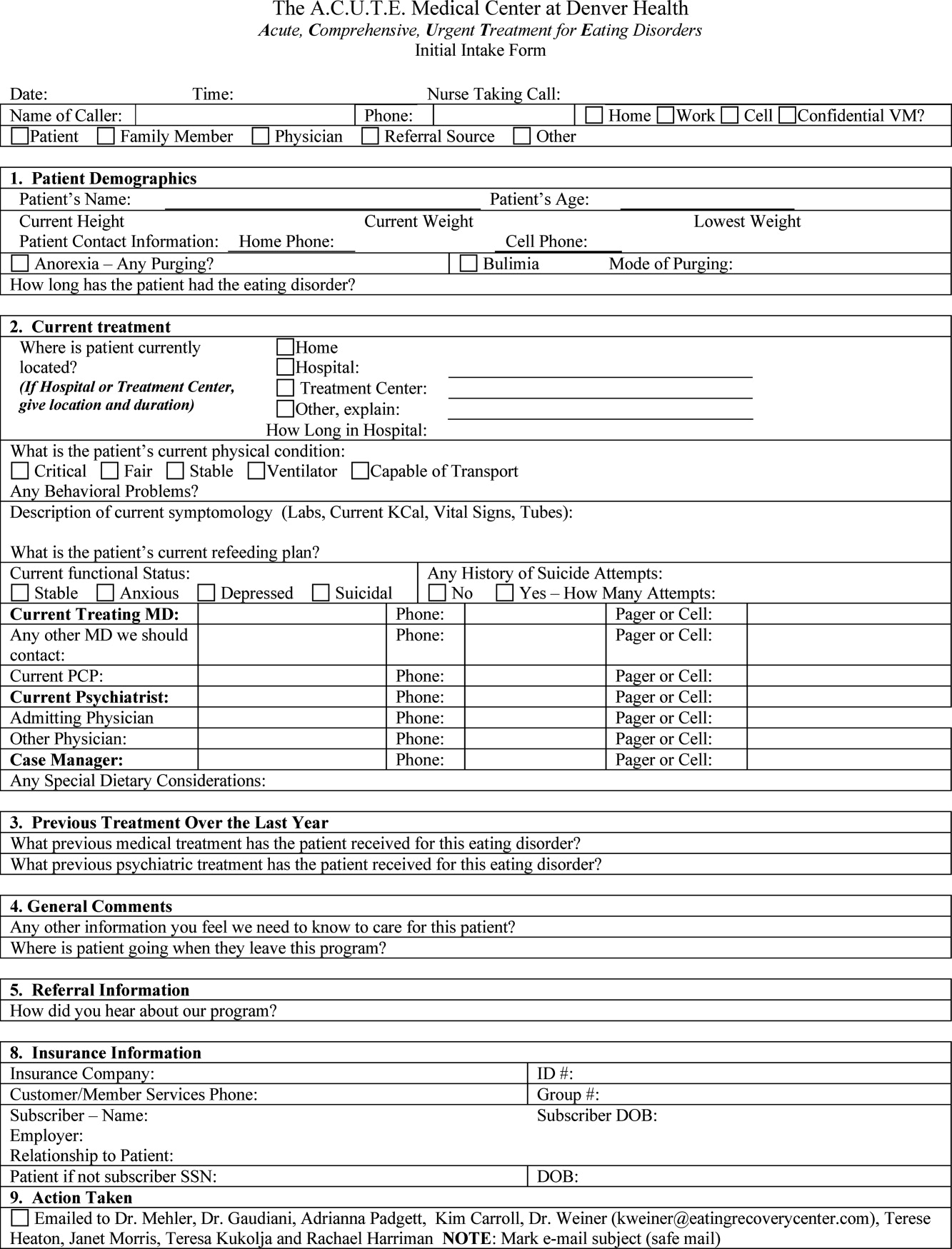
Patients are discharged from the ACUTE Center when they have achieved several basic goals: They are consuming greater than 2000 kcal per day, they are consistently gaining 23 pounds per week, their laboratory values have stabilized without electrolyte supplementation, and they are strong enough for an inpatient eating disorder program.
METHODS
Patients admitted to the ACUTE Center between October 2008 and December 2010 for medical stabilization and monitored refeeding were included. Patients with a diagnosis of bulimia nervosa were excluded. Demographic data and laboratory results were obtained electronically from our data repository, whereas weight, height, and other clinical characteristics were obtained by manual chart abstraction. The statistical analysis was conducted in SAS Enterprise Guide v4.1 (SAS Institute, Cary, NC).
RESULTS
In its first 27 months, the ACUTE Center had 76 total admissions, comprising 59 patients. Of the 76 admissions, the 62 admissions for medical stabilization and monitored refeeding of 54 patients with anorexia nervosa were included. Forty‐eight of the 54 (89%) included patients were female. Six patients were hospitalized twice, and 1 patient 3 times. There were 3 transfers to the intensive care unit, and no inpatient mortality. Of the 62 admissions, 11 (18%) discharges were to home, and 51 (82%) were to inpatient psychiatric eating disorder units.
The mean age at admission was 27 years (range 1765 years). The mean percent of ideal body weight (IBW) on admission was 62.2% 10.2%. The mean body mass index (BMI) was 12.9 2.0 kg/m2 on admission, and 13.1 1.9 kg/m2 upon discharge. The median length of stay was 16 days (interquartile range [IQR] 929 days). Median calculated BEE (1119 [10671184 IQR]) was higher than measured BEE by indirect calorimetry (792 [6341094]), (Table 1).
| Median (Interquartile Range)* | Range | |
|---|---|---|
| ||
| Age, yr | 27 (2135) | 1765 |
| Female | 56 | 90% |
| Length of hospitalization, days | 16 (929) | 570 |
| Calculated BEE | 1119 (10671184) | 9061491 |
| Measured BEE | 792 (6341094) | 5001742 |
| DEXA Z‐score | 2.2 1.1 | 4.40.7 |
| Height, in | 65 (6167) | 5774 |
| Weight on admission, lb | 76.1 14.4 | 50.8110.0 |
| % Ideal body weight on admission | 62.2 10.2 | 42.4101.0 |
| % Ideal body weight on discharge | 63.2 9.1 | 42.3 82.7 |
| BMI on admission | 12.9 2.0 | 8.719.7 |
| BMI nadir | 12.4 1.9 | 8.415.7 |
| BMI on discharge | 13.1 1.9 | 8.717.0 |
The majority of admission laboratory values, including serum albumin, blood urea nitrogen (BUN), creatinine, potassium, magnesium, and phosphate levels, were within normal limits. Fifty‐six percent were hyponatremic at admission, with a mean serum sodium level of 133 6 mmol/L (Table 2).
| Median (Interquartile Range)* | Range | |
|---|---|---|
| ||
| Sodium (135143 mmol/L) | 133 6 | 117145 |
| Potassium (3.65.1 mmol/L) | 3.8 (3.0 4.0) | 1.85.5 |
| Carbon dioxide (1827 mmol/L) | 28 (2531) | 1845 |
| Glucose (60199 mg/dL) | 85 (76105) | 41166 |
| BUN (622 mg/dL) | 16 (923) | 344 |
| Creatinine (0.61.2 mg/dL) | 0.7 (0.61.0) | 0.31.6 |
| Calcium (8.110.5 mg/dL) | 8.9 0.6 | 7.610.1 |
| Phosphorus (2.74.8 mg/dL) | 3.2 (2.83.7) | 2.15.7 |
| Magnesium (1.32.1 mEq/L) | 1.8 0.3 | 1.22.5 |
| AST (1040 U/L) | 38 (2391) | 122402 |
| ALT (745 U/L) | 45 (2498) | 152436 |
| Total bilirubin (0.01.2 mg/dL) | 0.5 (0.30.7) | 0.12.2 |
| Pre‐albumin (2052 mg/dL) | 21 7 | 842 |
| Albumin (3.05.3 g/dL) | 3.7 0.7 | 1.64.8 |
| WBC (4.510.0 k/L) | 4.0 (3.25.7) | 1.120.3 |
| Neutrophils (%) (48.069.0%) | 55.5 13.1 | 17.082.0 |
| Lymphocytes (%) (21.043.0%) | 34.9 13.0 | 10.864.0 |
| Platelet count (150450 k/L) | 266 (193371) | 40819 |
| Hematocrit (37.047.0%) | 36.1 5.4 | 19.145.7 |
| MCV (80100 fL) | 91 7 | 73105 |
| TSH (0.346.00 IU/mL) | 1.52 (0.962.84) | 0.1864.1 |
| INR (0.821.17) | 1.09 (1.001.22) | 0.812.05 |
| 1,25 Hydroxy vitamin D (3080 ng/mL) | 41 (3058) | 8171 |
DISCUSSION
Hospital Medicine is currently the fastest growing area of specialization in medicine.13 Palliative care, inpatient geriatrics, short stay units, and bedside procedures have evolved into hospitalist‐led services.1418 The management of the medical complications of severe eating disorders is another potential niche for hospitalists.
The ACUTE Center at Denver Health represents a center in which highly specialized, multidisciplinary care is provided for a rare and extremely ill population of patients. Prior to entering the ACUTE Center, the patients described in our program had each experienced prolonged and unsuccessful stays for medical stabilization in acute care hospitals across the country, after being denied treatment in eating disorder programs due to medical instability.
Patients transferred to ACUTE often received medical care reflecting a lack of specific expertise, training, and exposure. The most common management discrepancy we noted was over‐aggressive provision of intravenous fluids. Consequently, we often diurese 1020 pounds of edema weight, gained during a prior medical hospitalization, before beginning the process of weight restoration. This edema weight artificially increases admission weight and results in less than expected weight gain from admission to discharge.
Even without substantial weight gain, medical stabilization is evidenced by consistent caloric oral intake, and fluid and electrolyte stabilization after initial refeeding. Accordingly, patients who have been treated at the ACUTE Center often become eligible for admission to eating disorder programs at body weights below the typical 70% of ideal body weight that most programs use as a threshold for admission.
From a clinical research perspective, centers such as ACUTE allow for opportunities to better understand and investigate the nuances of patient care in the setting of severe malnutrition. From our cohort of patients to date, we have noted unique issues in albumin levels,19 coagulopathy,20 and liver function,21 among others. As an example, the cohort of patients with anorexia nervosa described here had profoundly low body weight, but relatively normal admission labs. Even the serum albumin, a parameter often used to reflect nutrition in an adult internal medicine setting, is usually normal, reflecting, in an otherwise generally healthy young population, the absence of a malignant, inflammatory, or infectious etiology of weight loss.19
Hospitalists also advocate for their patients by helping to maximize the benefits of their health care coverage. Many health care plans place limits on inpatient psychiatric care benefits. Patients who are severely malnourished from their eating disorder may waste valuable psychiatric care benefits undergoing medical stabilization in psychiatric units while physically unable to undergo psychotherapy. This has become increasingly important as health insurance plans continue to decrease coverage for residential care of patients with anorexia.22
In contrast, the medical benefits of most health plans are more robust. Accordingly, from the patient perspective, medical stabilization in an acute medical unit before admission to a psychiatry unit maximizes their ability to participate in the intensive psychiatric therapy which is still needed after medical stabilization. A recent study from a residential eating disorder program confirmed that a higher discharge BMI was the single best predictor of full recovery from anorexia nervosa.23
In the future, we believe that a continuing concentration of care and experience may also lend itself to the development of protocols and management guidelines which may benefit patients beyond our own unit. Severely malnourished patients with anorexia nervosa, or bulimic patients with complicated electrolyte disorders, are likely to benefit both medically and financially from centers of excellence. Inpatient or residential psychiatric eating disorder programs may act in synergy with medical eating disorders units, like ACUTE, to most efficiently care for the severely malnourished patient. Hospitalists, with the proper training and experience, are uniquely positioned to develop such centers of excellence.
- ,,,.The prevalence and correlates of eating disorders in the national comorbidity survey replication.Biol Psychiatry.2007;61:348–358.
- .The outcome of anorexia nervosa in the 20th century.Am J Psychiatry.2002;159:1284–1293.
- ,.Anorexia nervosa medical issues.J Womens Health.2003;12:331–340.
- .Diagnosis and care of patients with anorexia nervosa in primary care settings.Ann Intern Med.2001;134:1048–1059.
- ,,, et al.Mortality in eating disorders: a descriptive study.Int J Eat Disord.2000;28:20–26.
- ,,,,.Long‐term prognosis in anorexia nervosa: lessons from a 21‐year follow‐up study.Lancet.2000;355:721–722.
- ,,,,.Variations in admissions practices for adolescents with anorexia nervosa: a North American sample.J Adolesc Health.2008;43:425–431.
- American Psychiatric Association.Treatment of patients with eating disorders, third edition.Am J Psychiatry.2006;163(suppl 7):4–54.
- American Dietetic Association.Position of the American Dietetic Association: nutrition intervention in the treatment of anorexia nervosa, bulimia nervosa, and other eating disorders (ADA reports).J Am Diet Assoc.2006;106:2073–2082.
- ,.Clinical practice guidelines for treating restrictive eating disorder patients during medical hospitalization.Curr Opin Pediatr.2008;20:390–397.
- .Practice makes perfect: a volume‐outcome study of hospital patients with HIV disease.J Acquir Immune Defic Syndr.2008;47:226–233.
- ,,,.Association between physician caseload and patient outcome for sepsis treatment.Infect Control Hosp Epidemiol.2009;30:556–562.
- .Reflections: the hospitalist movement ten years later.J Hosp Med.2006;1:248–252.
- What will board certification be‐and mean‐for hospitalists?.Palliative care in hospitals.J Hosp Med.2006;1:21–28.
- .Palliative care and hospitalists: a partnership for hope.J Hosp Med.2006;1:5–6.
- ,,, et al.Impact of a bedside procedure service on general medicine inpatients: a firm‐based trial.J Hosp Med.2007;2:143–149.
- ,,,.Growth in the care of older patients by hospitalists in the United States.N Engl J Med.2009;360:1102–1112.
- ,,, et al.A hospitalist run short stay unit: features that predict length of stay and eventual admission to traditional inpatient services.J Hosp Med.2009;4:276–284.
- ,,.Serum albumin levels may not correlate with weight status in severe anorexia nervosa.Eat Disord.2009;17:322–326.
- ,,,,.The use of thrombelastography to determine coagulation status in severe anorexia nervosa: a case series.Int J Eat Disord.2010;43(4):382–385.
- ,,,.Liver function test abnormalities in anorexia nervosa—cause or effect.Int J Eat Disord.2010;43(4):378–381.
- .Eating disorders: a new front in insurance fight.New York Times. October 13, 2011. Available at: http://www.nytimes.com/2011/10/14/business/ruling‐offers‐hope‐to‐eating‐disorder‐sufferers. html?ref=business.
- ,.Long‐term outcome of residential treatment for anorexia nervosa and bulimia nervosa.Eat Disord.2011;19:132–144.
Anorexia nervosa occurs in 0.9% of women and 0.3% of men in the United States1 and is associated with a prolonged course,2 extensive medical complications that can affect almost every organ system,3, 4 and a 5% mean crude mortality rate9.6 times expected for age‐matched women in the United States.2, 5 Those with anorexia nervosa die as a complication of their illness more frequently than any other mental illness.3 Anorexia nervosa is commonly diagnosed during the adolescent years,2 with almost 25% going on to develop chronic anorexia nervosa.2, 6 Consequently, many patients with severe anorexia nervosa will receive treatment by adult medicine practitioners.
Patients with anorexia nervosa frequently require hospitalization. Published guidelines suggest that those who are 70% or less than ideal body weight, bradycardic, hypotensive, or those with severe electrolyte disturbances warrant admission for medical stabilization.79 Once admitted, however, there are no published guidelines for best practices to medically stabilize patients.7, 10 Although most experts advocate a multidisciplinary approach with weight restoration and medical stability as the goals of hospital admission,8, 9 controversy exists in the literature about how best to achieve these goals.7, 10
It is known, however, that for patients with complicated medical illnesses, such as human immunodeficiency virus (HIV) and sepsis, higher volumes of patient caseloads treated by physicians with disease‐specific expertise has been found to lead to improved outcomes in patients.11, 12 The adult patient with severe anorexia nervosa who requires inpatient medical stabilization may also benefit from a multidisciplinary trained staff familiar with the medical management of anorexia nervosa. Accordingly, we have developed the Acute Comprehensive Urgent Treatment for Eating Disorders (ACUTE) Center.
PROGRAM DESCRIPTION
The ACUTE Center at Denver Health is a 5‐bed unit dedicated to the medical stabilization of patients with severe malnutrition due to anorexia nervosa or severe electrolyte disorders due to bulimia nervosa. ACUTE accepts patients 17 years and older with medical complications related to chronic malnutrition and refeeding.
ACUTE uses a multidisciplinary approach to patient care. The physician team is composed of a hospital medicine attending physician, consultative expertise by an internal medicine specialist in the management of the medical complications of eating disorders, and a psychiatrist specializing in eating disorders. There is a dedicated team of nurses, two dieticians, physical therapists, certified nursing assistants, speech therapists, a psychotherapist, and a chaplain.
ACUTE patients are on continuous telemetry monitoring for the duration of their hospitalization to monitor for arrhythmias as well as signs of covert exercise. As part of the initial intake, a full set of vital signs is obtained, including height and weight. Patients are weighed daily with their back to the scale. There is no discussion of weight fluctuations. Patients may walk at a slow pace around the unit. No exercise is allowed.
Each patient at the ACUTE Center has an individualized meal plan and are started on an oral caloric intake 200 kcal below their basal energy expenditure (BEE). Indirect calorimetry is performed on the first hospital day. Each patient meets on a daily basis with the registered dietician to choose meals that meet their caloric goals.
All patients have a sitter continuously for their first week, and thereafter sitter time may be reduced to supervision surrounding each meal. Patients who fail to finish their prescribed meal are required to drink a liquid supplement to meet caloric goals. Calories are increased weekly until the patient's weight shows a clear pattern of weight increase. 0
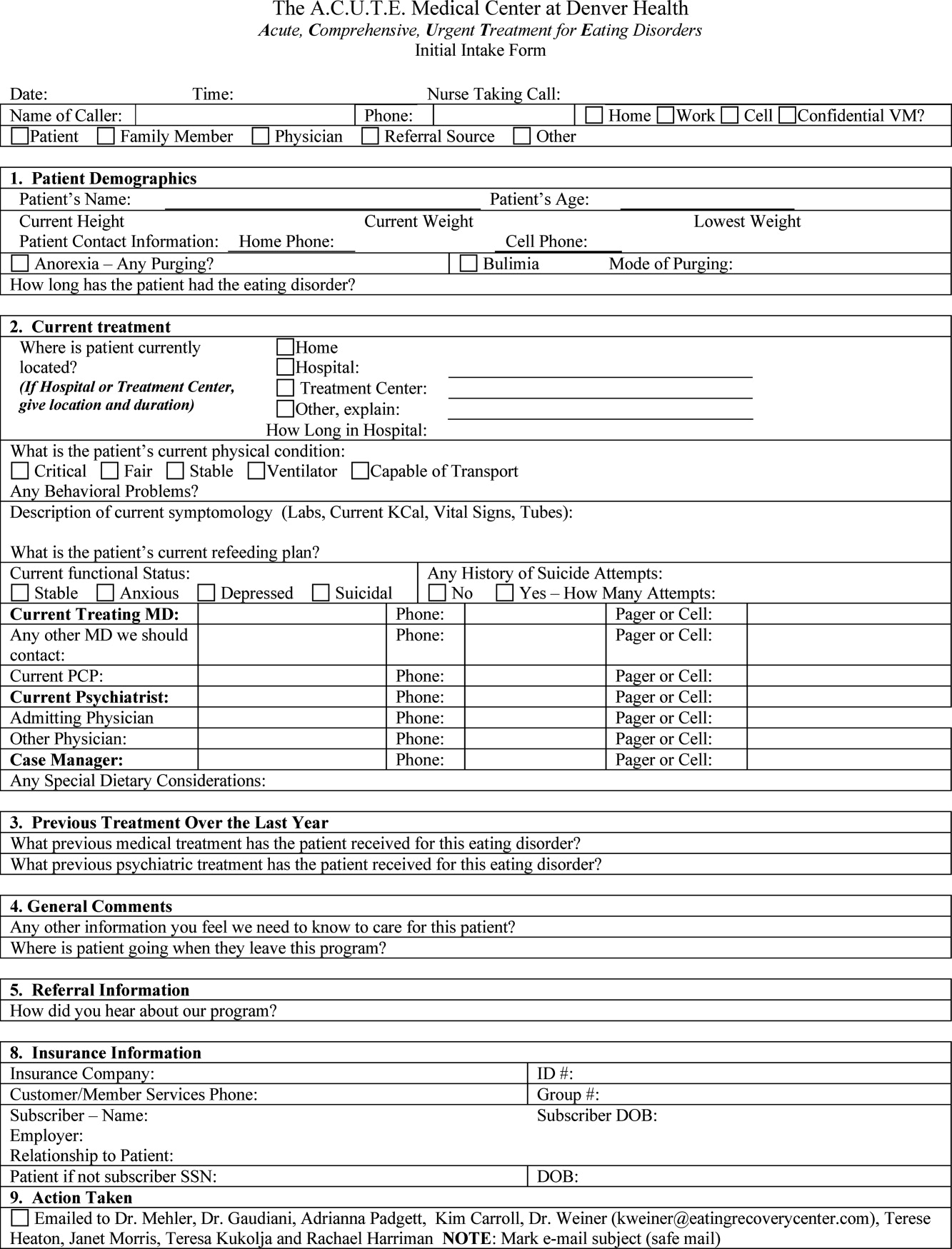
Patients are discharged from the ACUTE Center when they have achieved several basic goals: They are consuming greater than 2000 kcal per day, they are consistently gaining 23 pounds per week, their laboratory values have stabilized without electrolyte supplementation, and they are strong enough for an inpatient eating disorder program.
METHODS
Patients admitted to the ACUTE Center between October 2008 and December 2010 for medical stabilization and monitored refeeding were included. Patients with a diagnosis of bulimia nervosa were excluded. Demographic data and laboratory results were obtained electronically from our data repository, whereas weight, height, and other clinical characteristics were obtained by manual chart abstraction. The statistical analysis was conducted in SAS Enterprise Guide v4.1 (SAS Institute, Cary, NC).
RESULTS
In its first 27 months, the ACUTE Center had 76 total admissions, comprising 59 patients. Of the 76 admissions, the 62 admissions for medical stabilization and monitored refeeding of 54 patients with anorexia nervosa were included. Forty‐eight of the 54 (89%) included patients were female. Six patients were hospitalized twice, and 1 patient 3 times. There were 3 transfers to the intensive care unit, and no inpatient mortality. Of the 62 admissions, 11 (18%) discharges were to home, and 51 (82%) were to inpatient psychiatric eating disorder units.
The mean age at admission was 27 years (range 1765 years). The mean percent of ideal body weight (IBW) on admission was 62.2% 10.2%. The mean body mass index (BMI) was 12.9 2.0 kg/m2 on admission, and 13.1 1.9 kg/m2 upon discharge. The median length of stay was 16 days (interquartile range [IQR] 929 days). Median calculated BEE (1119 [10671184 IQR]) was higher than measured BEE by indirect calorimetry (792 [6341094]), (Table 1).
| Median (Interquartile Range)* | Range | |
|---|---|---|
| ||
| Age, yr | 27 (2135) | 1765 |
| Female | 56 | 90% |
| Length of hospitalization, days | 16 (929) | 570 |
| Calculated BEE | 1119 (10671184) | 9061491 |
| Measured BEE | 792 (6341094) | 5001742 |
| DEXA Z‐score | 2.2 1.1 | 4.40.7 |
| Height, in | 65 (6167) | 5774 |
| Weight on admission, lb | 76.1 14.4 | 50.8110.0 |
| % Ideal body weight on admission | 62.2 10.2 | 42.4101.0 |
| % Ideal body weight on discharge | 63.2 9.1 | 42.3 82.7 |
| BMI on admission | 12.9 2.0 | 8.719.7 |
| BMI nadir | 12.4 1.9 | 8.415.7 |
| BMI on discharge | 13.1 1.9 | 8.717.0 |
The majority of admission laboratory values, including serum albumin, blood urea nitrogen (BUN), creatinine, potassium, magnesium, and phosphate levels, were within normal limits. Fifty‐six percent were hyponatremic at admission, with a mean serum sodium level of 133 6 mmol/L (Table 2).
| Median (Interquartile Range)* | Range | |
|---|---|---|
| ||
| Sodium (135143 mmol/L) | 133 6 | 117145 |
| Potassium (3.65.1 mmol/L) | 3.8 (3.0 4.0) | 1.85.5 |
| Carbon dioxide (1827 mmol/L) | 28 (2531) | 1845 |
| Glucose (60199 mg/dL) | 85 (76105) | 41166 |
| BUN (622 mg/dL) | 16 (923) | 344 |
| Creatinine (0.61.2 mg/dL) | 0.7 (0.61.0) | 0.31.6 |
| Calcium (8.110.5 mg/dL) | 8.9 0.6 | 7.610.1 |
| Phosphorus (2.74.8 mg/dL) | 3.2 (2.83.7) | 2.15.7 |
| Magnesium (1.32.1 mEq/L) | 1.8 0.3 | 1.22.5 |
| AST (1040 U/L) | 38 (2391) | 122402 |
| ALT (745 U/L) | 45 (2498) | 152436 |
| Total bilirubin (0.01.2 mg/dL) | 0.5 (0.30.7) | 0.12.2 |
| Pre‐albumin (2052 mg/dL) | 21 7 | 842 |
| Albumin (3.05.3 g/dL) | 3.7 0.7 | 1.64.8 |
| WBC (4.510.0 k/L) | 4.0 (3.25.7) | 1.120.3 |
| Neutrophils (%) (48.069.0%) | 55.5 13.1 | 17.082.0 |
| Lymphocytes (%) (21.043.0%) | 34.9 13.0 | 10.864.0 |
| Platelet count (150450 k/L) | 266 (193371) | 40819 |
| Hematocrit (37.047.0%) | 36.1 5.4 | 19.145.7 |
| MCV (80100 fL) | 91 7 | 73105 |
| TSH (0.346.00 IU/mL) | 1.52 (0.962.84) | 0.1864.1 |
| INR (0.821.17) | 1.09 (1.001.22) | 0.812.05 |
| 1,25 Hydroxy vitamin D (3080 ng/mL) | 41 (3058) | 8171 |
DISCUSSION
Hospital Medicine is currently the fastest growing area of specialization in medicine.13 Palliative care, inpatient geriatrics, short stay units, and bedside procedures have evolved into hospitalist‐led services.1418 The management of the medical complications of severe eating disorders is another potential niche for hospitalists.
The ACUTE Center at Denver Health represents a center in which highly specialized, multidisciplinary care is provided for a rare and extremely ill population of patients. Prior to entering the ACUTE Center, the patients described in our program had each experienced prolonged and unsuccessful stays for medical stabilization in acute care hospitals across the country, after being denied treatment in eating disorder programs due to medical instability.
Patients transferred to ACUTE often received medical care reflecting a lack of specific expertise, training, and exposure. The most common management discrepancy we noted was over‐aggressive provision of intravenous fluids. Consequently, we often diurese 1020 pounds of edema weight, gained during a prior medical hospitalization, before beginning the process of weight restoration. This edema weight artificially increases admission weight and results in less than expected weight gain from admission to discharge.
Even without substantial weight gain, medical stabilization is evidenced by consistent caloric oral intake, and fluid and electrolyte stabilization after initial refeeding. Accordingly, patients who have been treated at the ACUTE Center often become eligible for admission to eating disorder programs at body weights below the typical 70% of ideal body weight that most programs use as a threshold for admission.
From a clinical research perspective, centers such as ACUTE allow for opportunities to better understand and investigate the nuances of patient care in the setting of severe malnutrition. From our cohort of patients to date, we have noted unique issues in albumin levels,19 coagulopathy,20 and liver function,21 among others. As an example, the cohort of patients with anorexia nervosa described here had profoundly low body weight, but relatively normal admission labs. Even the serum albumin, a parameter often used to reflect nutrition in an adult internal medicine setting, is usually normal, reflecting, in an otherwise generally healthy young population, the absence of a malignant, inflammatory, or infectious etiology of weight loss.19
Hospitalists also advocate for their patients by helping to maximize the benefits of their health care coverage. Many health care plans place limits on inpatient psychiatric care benefits. Patients who are severely malnourished from their eating disorder may waste valuable psychiatric care benefits undergoing medical stabilization in psychiatric units while physically unable to undergo psychotherapy. This has become increasingly important as health insurance plans continue to decrease coverage for residential care of patients with anorexia.22
In contrast, the medical benefits of most health plans are more robust. Accordingly, from the patient perspective, medical stabilization in an acute medical unit before admission to a psychiatry unit maximizes their ability to participate in the intensive psychiatric therapy which is still needed after medical stabilization. A recent study from a residential eating disorder program confirmed that a higher discharge BMI was the single best predictor of full recovery from anorexia nervosa.23
In the future, we believe that a continuing concentration of care and experience may also lend itself to the development of protocols and management guidelines which may benefit patients beyond our own unit. Severely malnourished patients with anorexia nervosa, or bulimic patients with complicated electrolyte disorders, are likely to benefit both medically and financially from centers of excellence. Inpatient or residential psychiatric eating disorder programs may act in synergy with medical eating disorders units, like ACUTE, to most efficiently care for the severely malnourished patient. Hospitalists, with the proper training and experience, are uniquely positioned to develop such centers of excellence.
Anorexia nervosa occurs in 0.9% of women and 0.3% of men in the United States1 and is associated with a prolonged course,2 extensive medical complications that can affect almost every organ system,3, 4 and a 5% mean crude mortality rate9.6 times expected for age‐matched women in the United States.2, 5 Those with anorexia nervosa die as a complication of their illness more frequently than any other mental illness.3 Anorexia nervosa is commonly diagnosed during the adolescent years,2 with almost 25% going on to develop chronic anorexia nervosa.2, 6 Consequently, many patients with severe anorexia nervosa will receive treatment by adult medicine practitioners.
Patients with anorexia nervosa frequently require hospitalization. Published guidelines suggest that those who are 70% or less than ideal body weight, bradycardic, hypotensive, or those with severe electrolyte disturbances warrant admission for medical stabilization.79 Once admitted, however, there are no published guidelines for best practices to medically stabilize patients.7, 10 Although most experts advocate a multidisciplinary approach with weight restoration and medical stability as the goals of hospital admission,8, 9 controversy exists in the literature about how best to achieve these goals.7, 10
It is known, however, that for patients with complicated medical illnesses, such as human immunodeficiency virus (HIV) and sepsis, higher volumes of patient caseloads treated by physicians with disease‐specific expertise has been found to lead to improved outcomes in patients.11, 12 The adult patient with severe anorexia nervosa who requires inpatient medical stabilization may also benefit from a multidisciplinary trained staff familiar with the medical management of anorexia nervosa. Accordingly, we have developed the Acute Comprehensive Urgent Treatment for Eating Disorders (ACUTE) Center.
PROGRAM DESCRIPTION
The ACUTE Center at Denver Health is a 5‐bed unit dedicated to the medical stabilization of patients with severe malnutrition due to anorexia nervosa or severe electrolyte disorders due to bulimia nervosa. ACUTE accepts patients 17 years and older with medical complications related to chronic malnutrition and refeeding.
ACUTE uses a multidisciplinary approach to patient care. The physician team is composed of a hospital medicine attending physician, consultative expertise by an internal medicine specialist in the management of the medical complications of eating disorders, and a psychiatrist specializing in eating disorders. There is a dedicated team of nurses, two dieticians, physical therapists, certified nursing assistants, speech therapists, a psychotherapist, and a chaplain.
ACUTE patients are on continuous telemetry monitoring for the duration of their hospitalization to monitor for arrhythmias as well as signs of covert exercise. As part of the initial intake, a full set of vital signs is obtained, including height and weight. Patients are weighed daily with their back to the scale. There is no discussion of weight fluctuations. Patients may walk at a slow pace around the unit. No exercise is allowed.
Each patient at the ACUTE Center has an individualized meal plan and are started on an oral caloric intake 200 kcal below their basal energy expenditure (BEE). Indirect calorimetry is performed on the first hospital day. Each patient meets on a daily basis with the registered dietician to choose meals that meet their caloric goals.
All patients have a sitter continuously for their first week, and thereafter sitter time may be reduced to supervision surrounding each meal. Patients who fail to finish their prescribed meal are required to drink a liquid supplement to meet caloric goals. Calories are increased weekly until the patient's weight shows a clear pattern of weight increase. 0
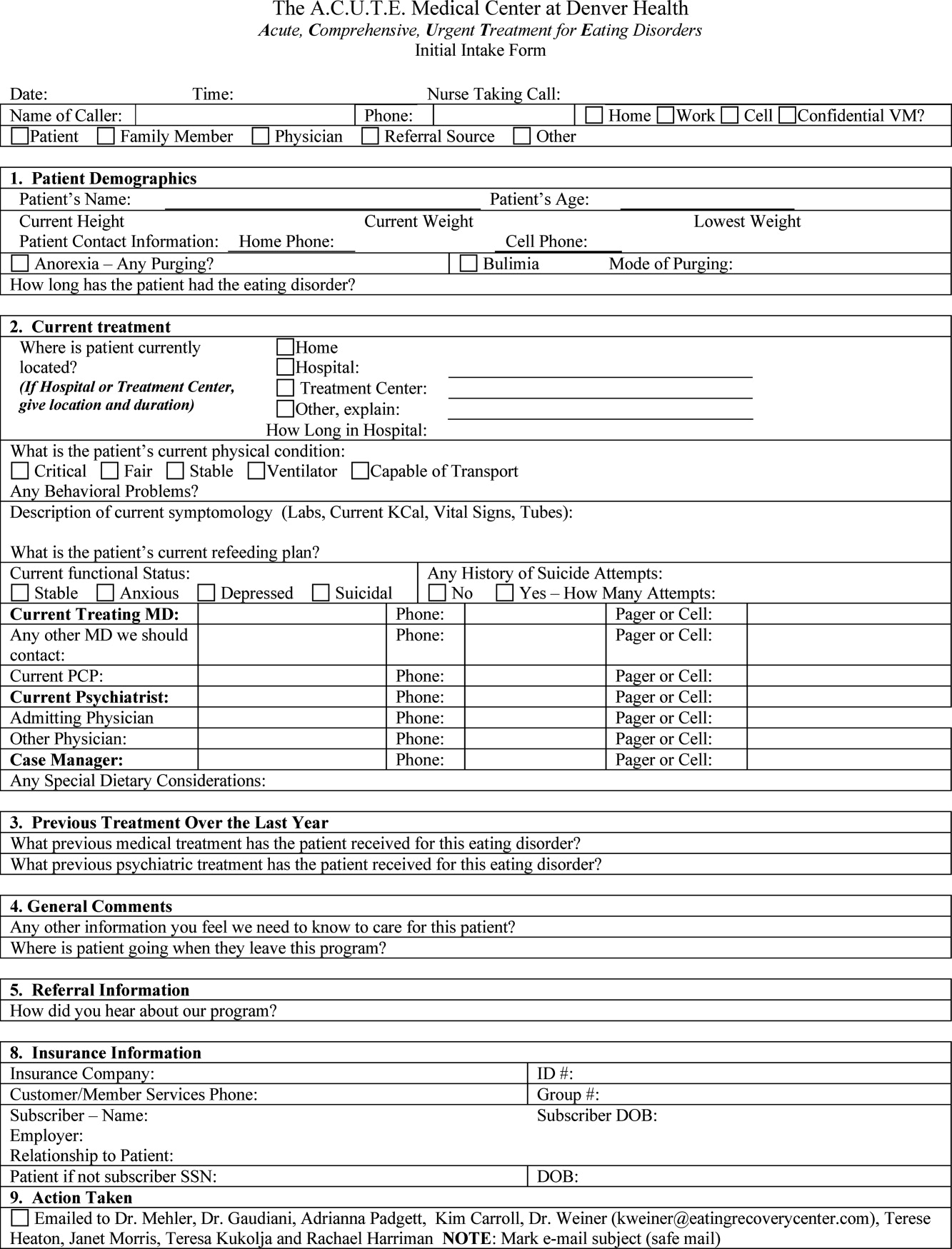
Patients are discharged from the ACUTE Center when they have achieved several basic goals: They are consuming greater than 2000 kcal per day, they are consistently gaining 23 pounds per week, their laboratory values have stabilized without electrolyte supplementation, and they are strong enough for an inpatient eating disorder program.
METHODS
Patients admitted to the ACUTE Center between October 2008 and December 2010 for medical stabilization and monitored refeeding were included. Patients with a diagnosis of bulimia nervosa were excluded. Demographic data and laboratory results were obtained electronically from our data repository, whereas weight, height, and other clinical characteristics were obtained by manual chart abstraction. The statistical analysis was conducted in SAS Enterprise Guide v4.1 (SAS Institute, Cary, NC).
RESULTS
In its first 27 months, the ACUTE Center had 76 total admissions, comprising 59 patients. Of the 76 admissions, the 62 admissions for medical stabilization and monitored refeeding of 54 patients with anorexia nervosa were included. Forty‐eight of the 54 (89%) included patients were female. Six patients were hospitalized twice, and 1 patient 3 times. There were 3 transfers to the intensive care unit, and no inpatient mortality. Of the 62 admissions, 11 (18%) discharges were to home, and 51 (82%) were to inpatient psychiatric eating disorder units.
The mean age at admission was 27 years (range 1765 years). The mean percent of ideal body weight (IBW) on admission was 62.2% 10.2%. The mean body mass index (BMI) was 12.9 2.0 kg/m2 on admission, and 13.1 1.9 kg/m2 upon discharge. The median length of stay was 16 days (interquartile range [IQR] 929 days). Median calculated BEE (1119 [10671184 IQR]) was higher than measured BEE by indirect calorimetry (792 [6341094]), (Table 1).
| Median (Interquartile Range)* | Range | |
|---|---|---|
| ||
| Age, yr | 27 (2135) | 1765 |
| Female | 56 | 90% |
| Length of hospitalization, days | 16 (929) | 570 |
| Calculated BEE | 1119 (10671184) | 9061491 |
| Measured BEE | 792 (6341094) | 5001742 |
| DEXA Z‐score | 2.2 1.1 | 4.40.7 |
| Height, in | 65 (6167) | 5774 |
| Weight on admission, lb | 76.1 14.4 | 50.8110.0 |
| % Ideal body weight on admission | 62.2 10.2 | 42.4101.0 |
| % Ideal body weight on discharge | 63.2 9.1 | 42.3 82.7 |
| BMI on admission | 12.9 2.0 | 8.719.7 |
| BMI nadir | 12.4 1.9 | 8.415.7 |
| BMI on discharge | 13.1 1.9 | 8.717.0 |
The majority of admission laboratory values, including serum albumin, blood urea nitrogen (BUN), creatinine, potassium, magnesium, and phosphate levels, were within normal limits. Fifty‐six percent were hyponatremic at admission, with a mean serum sodium level of 133 6 mmol/L (Table 2).
| Median (Interquartile Range)* | Range | |
|---|---|---|
| ||
| Sodium (135143 mmol/L) | 133 6 | 117145 |
| Potassium (3.65.1 mmol/L) | 3.8 (3.0 4.0) | 1.85.5 |
| Carbon dioxide (1827 mmol/L) | 28 (2531) | 1845 |
| Glucose (60199 mg/dL) | 85 (76105) | 41166 |
| BUN (622 mg/dL) | 16 (923) | 344 |
| Creatinine (0.61.2 mg/dL) | 0.7 (0.61.0) | 0.31.6 |
| Calcium (8.110.5 mg/dL) | 8.9 0.6 | 7.610.1 |
| Phosphorus (2.74.8 mg/dL) | 3.2 (2.83.7) | 2.15.7 |
| Magnesium (1.32.1 mEq/L) | 1.8 0.3 | 1.22.5 |
| AST (1040 U/L) | 38 (2391) | 122402 |
| ALT (745 U/L) | 45 (2498) | 152436 |
| Total bilirubin (0.01.2 mg/dL) | 0.5 (0.30.7) | 0.12.2 |
| Pre‐albumin (2052 mg/dL) | 21 7 | 842 |
| Albumin (3.05.3 g/dL) | 3.7 0.7 | 1.64.8 |
| WBC (4.510.0 k/L) | 4.0 (3.25.7) | 1.120.3 |
| Neutrophils (%) (48.069.0%) | 55.5 13.1 | 17.082.0 |
| Lymphocytes (%) (21.043.0%) | 34.9 13.0 | 10.864.0 |
| Platelet count (150450 k/L) | 266 (193371) | 40819 |
| Hematocrit (37.047.0%) | 36.1 5.4 | 19.145.7 |
| MCV (80100 fL) | 91 7 | 73105 |
| TSH (0.346.00 IU/mL) | 1.52 (0.962.84) | 0.1864.1 |
| INR (0.821.17) | 1.09 (1.001.22) | 0.812.05 |
| 1,25 Hydroxy vitamin D (3080 ng/mL) | 41 (3058) | 8171 |
DISCUSSION
Hospital Medicine is currently the fastest growing area of specialization in medicine.13 Palliative care, inpatient geriatrics, short stay units, and bedside procedures have evolved into hospitalist‐led services.1418 The management of the medical complications of severe eating disorders is another potential niche for hospitalists.
The ACUTE Center at Denver Health represents a center in which highly specialized, multidisciplinary care is provided for a rare and extremely ill population of patients. Prior to entering the ACUTE Center, the patients described in our program had each experienced prolonged and unsuccessful stays for medical stabilization in acute care hospitals across the country, after being denied treatment in eating disorder programs due to medical instability.
Patients transferred to ACUTE often received medical care reflecting a lack of specific expertise, training, and exposure. The most common management discrepancy we noted was over‐aggressive provision of intravenous fluids. Consequently, we often diurese 1020 pounds of edema weight, gained during a prior medical hospitalization, before beginning the process of weight restoration. This edema weight artificially increases admission weight and results in less than expected weight gain from admission to discharge.
Even without substantial weight gain, medical stabilization is evidenced by consistent caloric oral intake, and fluid and electrolyte stabilization after initial refeeding. Accordingly, patients who have been treated at the ACUTE Center often become eligible for admission to eating disorder programs at body weights below the typical 70% of ideal body weight that most programs use as a threshold for admission.
From a clinical research perspective, centers such as ACUTE allow for opportunities to better understand and investigate the nuances of patient care in the setting of severe malnutrition. From our cohort of patients to date, we have noted unique issues in albumin levels,19 coagulopathy,20 and liver function,21 among others. As an example, the cohort of patients with anorexia nervosa described here had profoundly low body weight, but relatively normal admission labs. Even the serum albumin, a parameter often used to reflect nutrition in an adult internal medicine setting, is usually normal, reflecting, in an otherwise generally healthy young population, the absence of a malignant, inflammatory, or infectious etiology of weight loss.19
Hospitalists also advocate for their patients by helping to maximize the benefits of their health care coverage. Many health care plans place limits on inpatient psychiatric care benefits. Patients who are severely malnourished from their eating disorder may waste valuable psychiatric care benefits undergoing medical stabilization in psychiatric units while physically unable to undergo psychotherapy. This has become increasingly important as health insurance plans continue to decrease coverage for residential care of patients with anorexia.22
In contrast, the medical benefits of most health plans are more robust. Accordingly, from the patient perspective, medical stabilization in an acute medical unit before admission to a psychiatry unit maximizes their ability to participate in the intensive psychiatric therapy which is still needed after medical stabilization. A recent study from a residential eating disorder program confirmed that a higher discharge BMI was the single best predictor of full recovery from anorexia nervosa.23
In the future, we believe that a continuing concentration of care and experience may also lend itself to the development of protocols and management guidelines which may benefit patients beyond our own unit. Severely malnourished patients with anorexia nervosa, or bulimic patients with complicated electrolyte disorders, are likely to benefit both medically and financially from centers of excellence. Inpatient or residential psychiatric eating disorder programs may act in synergy with medical eating disorders units, like ACUTE, to most efficiently care for the severely malnourished patient. Hospitalists, with the proper training and experience, are uniquely positioned to develop such centers of excellence.
- ,,,.The prevalence and correlates of eating disorders in the national comorbidity survey replication.Biol Psychiatry.2007;61:348–358.
- .The outcome of anorexia nervosa in the 20th century.Am J Psychiatry.2002;159:1284–1293.
- ,.Anorexia nervosa medical issues.J Womens Health.2003;12:331–340.
- .Diagnosis and care of patients with anorexia nervosa in primary care settings.Ann Intern Med.2001;134:1048–1059.
- ,,, et al.Mortality in eating disorders: a descriptive study.Int J Eat Disord.2000;28:20–26.
- ,,,,.Long‐term prognosis in anorexia nervosa: lessons from a 21‐year follow‐up study.Lancet.2000;355:721–722.
- ,,,,.Variations in admissions practices for adolescents with anorexia nervosa: a North American sample.J Adolesc Health.2008;43:425–431.
- American Psychiatric Association.Treatment of patients with eating disorders, third edition.Am J Psychiatry.2006;163(suppl 7):4–54.
- American Dietetic Association.Position of the American Dietetic Association: nutrition intervention in the treatment of anorexia nervosa, bulimia nervosa, and other eating disorders (ADA reports).J Am Diet Assoc.2006;106:2073–2082.
- ,.Clinical practice guidelines for treating restrictive eating disorder patients during medical hospitalization.Curr Opin Pediatr.2008;20:390–397.
- .Practice makes perfect: a volume‐outcome study of hospital patients with HIV disease.J Acquir Immune Defic Syndr.2008;47:226–233.
- ,,,.Association between physician caseload and patient outcome for sepsis treatment.Infect Control Hosp Epidemiol.2009;30:556–562.
- .Reflections: the hospitalist movement ten years later.J Hosp Med.2006;1:248–252.
- What will board certification be‐and mean‐for hospitalists?.Palliative care in hospitals.J Hosp Med.2006;1:21–28.
- .Palliative care and hospitalists: a partnership for hope.J Hosp Med.2006;1:5–6.
- ,,, et al.Impact of a bedside procedure service on general medicine inpatients: a firm‐based trial.J Hosp Med.2007;2:143–149.
- ,,,.Growth in the care of older patients by hospitalists in the United States.N Engl J Med.2009;360:1102–1112.
- ,,, et al.A hospitalist run short stay unit: features that predict length of stay and eventual admission to traditional inpatient services.J Hosp Med.2009;4:276–284.
- ,,.Serum albumin levels may not correlate with weight status in severe anorexia nervosa.Eat Disord.2009;17:322–326.
- ,,,,.The use of thrombelastography to determine coagulation status in severe anorexia nervosa: a case series.Int J Eat Disord.2010;43(4):382–385.
- ,,,.Liver function test abnormalities in anorexia nervosa—cause or effect.Int J Eat Disord.2010;43(4):378–381.
- .Eating disorders: a new front in insurance fight.New York Times. October 13, 2011. Available at: http://www.nytimes.com/2011/10/14/business/ruling‐offers‐hope‐to‐eating‐disorder‐sufferers. html?ref=business.
- ,.Long‐term outcome of residential treatment for anorexia nervosa and bulimia nervosa.Eat Disord.2011;19:132–144.
- ,,,.The prevalence and correlates of eating disorders in the national comorbidity survey replication.Biol Psychiatry.2007;61:348–358.
- .The outcome of anorexia nervosa in the 20th century.Am J Psychiatry.2002;159:1284–1293.
- ,.Anorexia nervosa medical issues.J Womens Health.2003;12:331–340.
- .Diagnosis and care of patients with anorexia nervosa in primary care settings.Ann Intern Med.2001;134:1048–1059.
- ,,, et al.Mortality in eating disorders: a descriptive study.Int J Eat Disord.2000;28:20–26.
- ,,,,.Long‐term prognosis in anorexia nervosa: lessons from a 21‐year follow‐up study.Lancet.2000;355:721–722.
- ,,,,.Variations in admissions practices for adolescents with anorexia nervosa: a North American sample.J Adolesc Health.2008;43:425–431.
- American Psychiatric Association.Treatment of patients with eating disorders, third edition.Am J Psychiatry.2006;163(suppl 7):4–54.
- American Dietetic Association.Position of the American Dietetic Association: nutrition intervention in the treatment of anorexia nervosa, bulimia nervosa, and other eating disorders (ADA reports).J Am Diet Assoc.2006;106:2073–2082.
- ,.Clinical practice guidelines for treating restrictive eating disorder patients during medical hospitalization.Curr Opin Pediatr.2008;20:390–397.
- .Practice makes perfect: a volume‐outcome study of hospital patients with HIV disease.J Acquir Immune Defic Syndr.2008;47:226–233.
- ,,,.Association between physician caseload and patient outcome for sepsis treatment.Infect Control Hosp Epidemiol.2009;30:556–562.
- .Reflections: the hospitalist movement ten years later.J Hosp Med.2006;1:248–252.
- What will board certification be‐and mean‐for hospitalists?.Palliative care in hospitals.J Hosp Med.2006;1:21–28.
- .Palliative care and hospitalists: a partnership for hope.J Hosp Med.2006;1:5–6.
- ,,, et al.Impact of a bedside procedure service on general medicine inpatients: a firm‐based trial.J Hosp Med.2007;2:143–149.
- ,,,.Growth in the care of older patients by hospitalists in the United States.N Engl J Med.2009;360:1102–1112.
- ,,, et al.A hospitalist run short stay unit: features that predict length of stay and eventual admission to traditional inpatient services.J Hosp Med.2009;4:276–284.
- ,,.Serum albumin levels may not correlate with weight status in severe anorexia nervosa.Eat Disord.2009;17:322–326.
- ,,,,.The use of thrombelastography to determine coagulation status in severe anorexia nervosa: a case series.Int J Eat Disord.2010;43(4):382–385.
- ,,,.Liver function test abnormalities in anorexia nervosa—cause or effect.Int J Eat Disord.2010;43(4):378–381.
- .Eating disorders: a new front in insurance fight.New York Times. October 13, 2011. Available at: http://www.nytimes.com/2011/10/14/business/ruling‐offers‐hope‐to‐eating‐disorder‐sufferers. html?ref=business.
- ,.Long‐term outcome of residential treatment for anorexia nervosa and bulimia nervosa.Eat Disord.2011;19:132–144.
Effectiveness of Course to Teach Handoffs
Communication failures are well‐recognized as causes of medical errors.1, 2 Specifically, handoffs of patient care responsibilities, which are increasingly prevalent in academic medical centers,3 have been cited as the most frequent cause of teamwork breakdown resulting in the harmful medical errors found in malpractice claims.1 The Institute of Medicine has recently identified patient handoffs as the moment where patient care errors are most likely to occur.4 A survey of 125 U.S. medical schools, however, found that only 8% specifically taught students how to hand off patient care.3
In July 2003, the American Council of Graduate Medical Education (ACGME) mandated that residency programs decrease resident work hours to improve patient care and safety by reducing fatigue,5 and a recent Institute of Medicine report suggests that they be decreased even further.4 Studies examining outcomes during the first 2 years after reducing duty hours did not find reductions in risk‐adjusted mortality.68 One proposed explanation for this lack of improvement is that the reduction in fatigue‐related medical errors is being offset by discontinuity of care with due to the increased number of patient handoffs resulting from shortened duty hours,911 one recent study found that omission of key information during patient sign outs frequently resulted in adverse patient care outcomes.12
In 2007, the Joint Commission developed a new National Patient Safety Goal that requires organizations to improve communication between caregivers.13 We recently developed an approach by which Internal Medicine residents hand off patient care using a structured process, written and verbal templates, formal training about handoffs, and direct attending supervision.14 Because fourth‐year medical students perform the duties of interns when working as subinterns, we recognized that education about handoffs should occur prior to the time students became interns. Accordingly, we developed a course designed to teach patient handoffs to medical students at the transition between their third and fourth years of training.
Setting
The Handoff Selective was developed by faculty of Denver Health and the University of Colorado Denver School of Medicine.
Program Description
The Selective was first offered in April 2007 as part of an Integrated Clinician's Course (ICC), a 2‐week course for students beginning their fourth year, which starts in April at the University of Colorado. The ICC includes both mandatory and selective sessions that are focused on developing clinical skills and preparing them for their subinternships. The Handoff Selective was conducted in a computerized teaching laboratory, lasted a total of 2 hours and consisted of 2 parts. Each of the 5 Denver Health Hospital Medicine faculty members versed in handoff education taught 2 sessions of 6 to 8 students.
Part 1: Didactic
During the first hour of class, the faculty presented a lecture that summarized the relevant literature on handoffs and explained the importance of the topic. The objectives of the didactic were to: (1) understand the importance of handoffs; (2) explore different communication elements and structures; (3) gain exposure to handoffs outside of healthcare; and (4) learn a structure for handoffs of patient care in hospitalized patients.
We used 3 video clips of handoffs from 2 football games to demonstrate the importance of practice, training, and 2‐way communications in handoffs. The first video clip showed a runner trying to make a spontaneous handoff while being tackled. The receiver was not expecting the handoff and was preoccupied with blocking another player. This attempted handoff resulted in a fumble, which we related to an adverse patient event.
The next 2 video clips showed 2 complex, seldom used, but well‐known football handoffsthe hook and lateral and the Statue of Liberty. Both handoffs were successfully executed presumably as a result of education, practice and the active participation of both players (handing off and receiving) in the process. We then related the teaching and practicing of complex communication to the Joint Commission on Accreditation of Healthcare Organizations (JCAHO; now simply the Joint Commission) data suggesting that most sentinel events have their root cause in communication and training failures.2
Basic communication elements and process structures were then explored using scenarios from everyday life and evidence from fields outside of medicine. We emphasized that structures for communication (modes, vehicles, and settings) must be chosen according to the occasion and that handoffs are common and important in all occupations. In discussing modes (verbal, written, or nonverbal), vehicles (paper, telephone, or e‐mail), and settings (face‐to face, virtual, or disconnected), we emphasized that the most effective structures for communication (verbal, face‐to face meetings, with written materials and other visual aids at the patient's bedside) were also the most time‐consuming (Figure 1). While our standard for resident handoffs is a face‐to‐face verbal interaction with preprinted written materials as an aid, we also emphasized that for complex patients (eg, mental status changes, concern for an acute abdomen) more robust communication is often needed. Accordingly, a more time‐consuming bedside handoff with simultaneous, focused physical exam and history‐taking by both oncoming and off‐going providers may be most appropriate.
As real‐life examples, we asked our students to communicate a happy birthday wish to their mother, who lives in another state. Almost uniformly, in addition to a written aid (birthday card), they choose the telephone as a vehicle for their verbal mode in a virtual setting with 2‐way communication possible. In contrast, when asked to propose marriage to a significant other in another state, students felt that a face‐to‐face meeting with verbal and nonverbal (ie, ring) modes was appropriate. This time‐consuming mode of communication was felt to be necessary to create a sentiment of importance and avert any possible miscommunication.
The didactic session concluded by demonstrating how to use standardized written and verbal templates for handoffs of the care of a hospitalized patient. We explore the differentiation between written and verbal handoffs in our discussion below.
Part 2: Practicum
The second hour was devoted to practicing handoffs as a group. The faculty developed 6 case scenarios that differed with respect to diagnosis, length of stay, active medical issues, and anticipated discharge (Table 1). The scenarios included extensive admission information as well as evolving issues for each patient that were specific to the day of the intended handoff. Students were given Microsoft Word table‐based handoff templates to use when creating written sign‐outs for their patients. Verbal handoffs were performed between students and sign‐outs were exchanged. The faculty then role‐played cross‐cover calls that were specific for each scenario to test the students' inclusion of integral information in their handoffs and their ability to create contingency plans.
| Diagnosis | LOS | Active Issues | Cross‐Cover |
|---|---|---|---|
| |||
| CP | 1 | CP, HTN, DM | CP, HTN, headache |
| GIB | 1 | GIB, alcohol withdrawal | Poor response to red call transfusion, coagulopathy |
| Acute pancreatitis | 2 | Pain, possible pancreatic abscess | Fever, agitation, hypoxia |
| CHF | 2 | CHF, DM, nausea | Lack of diuresis, CP, hypoglycemia |
| Acute kidney injury | 3 | None, ready for discharge | HTN, hyperglycemia |
| Community acquired pneumonia | 3 | Anxiety, discharge pending | Confusion, emesis with hypoxia |
Program Evaluation
We developed a 2‐part survey to evaluate the effectiveness of the Selective and to solicit feedback about the didactic and practicum portions of the course. The first part of the survey (Table 2) contained 16 items to assess the students' knowledge of, and attitudes toward handing off patient care, along with their comfort with the handoff process. Responses to this section were scored using a 5‐point Likert scale with 1 indicating strongly disagree and 5 indicating strongly agree. This part of the survey was administered both prior to and after the Selective.
| Competency | Selective | |
|---|---|---|
| Before | After | |
| ||
| I know how to hand off patients | 2.3 0.8 | 4.2 0.6* |
| I know how to make contingency plans for my patients | 2.1 0.8 | 3.9 0.7* |
| I know what a read‐back is | 2.3 1.3 | 4.4 0.9* |
| I know how to perform a read‐back | 2.0 1.2 | 4.2 0.9* |
| I know when to perform a read‐back | 1.6 0.8 | 4.1 1.0* |
| I am efficient at communicating patient information | 2.2 0.9 | 3.6 0.7* |
| I am effective at communicating patient information | 2.2 0.8 | 3.8 0.6* |
| I know a standard written structure for handoffs | 2.1 1.1 | 4.4 0.6* |
| I know a standard verbal structure for handoffs | 2.0 1.1 | 4.2 0.6* |
| I can choose appropriate modes of communication | 2.7 1.1 | 4.4 0.6* |
| I can choose appropriate vehicles of communication | 2.6 1.1 | 4.5 0.6* |
| I can choose appropriate settings for communication | 2.9 1.1 | 4.4 0.6* |
| Handoffs are well taught in my medical school | 1.6 0.8 | 3.5 1.0* |
| Standardization is important in handoffs | 4.3 0.9 | 4.6 0.5 |
| Handoffs are safer with attending supervision | 3.7 1.0 | 3.9 0.8 |
| I feel comfortable cross‐covering on patients | 1.6 0.7 | 3.0 1.0* |
The second part (Table 3) contained 12 items and was designed to evaluate the perceived usefulness of the different components of the class. This section was only administered at the end of the Selective. It utilized a 4‐point Likert scale with 1 indicating that the component was not useful at all, and 4 indicating that it was extremely useful. The first 6 items of the second section allowed students to evaluate the didactic portion of the handoff. The second 6 items allowed students to evaluate the practicum. Responses to all 12 items were then combined to determine an overall composite usefulness for the Selective.
| Useful [n (%)] | |
|---|---|
| |
| Overall composite usefulness | 578 (92) |
| Didactic composite usefulness | 254 (84) |
| Using fumble video clips for discussing handoffs | 32 (64)* |
| Discussion of modes of communication | 46 (88) |
| Discussion of vehicles of communication | 46 (88) |
| Discussion of settings of communication | 48 (96) |
| Choosing handoff structures for nonhealthcare handoffs | 37 (71)* |
| Discussing handoffs in industries outside of healthcare | 45 (94) |
| Practicum composite usefulness | 324(100) |
| Role playing | 54 (100) |
| Patient handoff scenarios | 54 (100) |
| Completing computerized templates | 54 (100) |
| Delivering handoffs to peer | 54 (100) |
| Receiving handoffs from peer | 54 (100) |
| Cross‐cover questions and discussion | 54 (100) |
The Selective was also evaluated qualitatively through the use of open‐ended, written comments that were solicited at the end of the survey. All surveys were administered anonymously.
Data Analysis
Student paired t test was used to compare continuous variables recorded before and after the Selective. A chi‐square test was used to assess the students' perception of the usefulness of the didactic vs. the practicum methods of teaching handoffs.
All analyses were performed using SAS (version 8.1; SAS Institute, Inc., Cary, NC). Bonferroni corrections were used for multiple comparisons such that P values of <0.003 and <0.004 were considered to be significant for continuous and categorical variables, respectively. All data are reported as mean standard deviation (SD).
The survey was approved by our local Institutional Review Board.
Results
More students chose the Selective than we had capacity to accommodate (60 of a class of 150). The pre‐ and postcourse survey response rate was 56 of 60 (93%) and 58 of 60 (97%), respectively. After the Selective, the mean score in response to whether handoffs are well taught in medical school increased from 1.6 to 3.5 (P < 0.003). Our students' self‐perceived skills and knowledge about handoffs improved after the Selective (Table 2). The greatest changes in perceived knowledge occurred in questions regarding the what, how, and when of read‐backs, and the knowledge of standard verbal and written handoff structures. The responses to the survey elements which assessed our students' attitudes regarding the importance of standardization and whether they felt handoffs were safer with faculty supervision did not change after the Selective (Table 2).
A total of 92% of the students felt that the course was extremely useful or useful. The role‐playing activity was thought to be more helpful than the didactic, but 84% of the students still rated the didactic portion as useful or extremely useful (Table 3). The element which was the least well received in the didactic portion was the use of video clips to demonstrate successful and unsuccessful (fumbled) college football handoffs, although the majority (64%) of students still found it useful.
The major theme generated from the comments section of the survey was that the Selective should be a required course.
Discussion
We know of no previously published literature that has addressed teaching handoffs to medical students. Horwitz et al.15 developed a sign‐out curriculum for Internal Medicine residents and found that none of their house‐staff had any previous training in handoffs during medical school, consistent with the finding that only 8% of U.S. medical schools provided formal instruction on handoffs.3 Prior to taking the Selective, our students had no knowledge of verbal or written templates for patient handoffs, although both before and after the course they felt that standardization was an important component of the process.
A number of verbal structures for handing off patient care have been described in the literature and there is not a consensus as to which functions best. Perhaps the most cited verbal communication format is SBAR (ie, situation, background, assessment and recommendation).16, 17 This tool was developed by Leonard et al.18 specifically for use by nurses to provide 1‐way communication to physicians pertaining to a change in patient status. We considered teaching the SBAR approach to the students but felt that it did not provide a suitable structure for handoffs because the transfer of care is not generally an event‐based situation and the literature on handoffs indicates that an optimal verbal system includes 2‐way communication.
Additional mnemonics for handoffs found in the literature include SIGNOUT (ie, Sick or DNR, Identifying information, General hospital course, New events of the day, Overall health status, Upcoming possibilities with plan, and Tasks to complete),14 I PASS the BATON (ie, Introduction, Patient, Assessment, Situation, Safety, Background, Actions, Timing, Ownership, Next)19 and the SAIF‐IR system (see boxed text).14
Verbal Structure for Patient Handoffs: SAIF‐IR
Off‐going provider performs a SAIF handoff:
Summary statement(s)
Active issues
If‐then contingency planning
Follow‐up activities
On‐coming provider makes the handoff SAIF‐IR:
Interactive questioning
Read‐backs
We developed the SAIF‐IR mnemonic to maximize efficiency and effectiveness while differentiating the verbal portion of the handoff from the written and incorporating 2‐way communication into its structure. In the Summary statement, we emphasize that this is not a history of present illness. We ask our students to summarize, in 1 to 3 sentences, the patient's presentation and working diagnosis. When discussing patient issues, we ask our students to only verbalize Active issues, although the written template has inactive, chronic issues listed. Here, we also ask our students to express their level of concern for the active issues and patient in general. If‐then's and Follow‐ups are usually verbalized together. Based on the offgoing provider's knowledge of the patient, we encourage the offgoing provider to anticipate potential problems and advise the oncoming provider on potential responses. Much of this advice is difficult to express in the written format and thus may not be found on the written handoff when the verbal handoff occurs. We encourage oncoming providers to take notes on the preprinted handoff sheet as part of the handoff process.
Through Interactive questioning and Read‐backs, we train our students and house‐staff to use the active listening techniques used outside of healthcare, in settings such as nuclear power plants and National Aeronautics and Space Administration mission control, where poor handoff communication may also result in safety concerns and adverse events.20 Interactive questioning allows the oncoming provider to correct or clarify any information given by the off‐going provider. Read‐backs are a method of confirming follow‐up activity or contingency plans. Together, the SAIF‐IR mnemonic builds a 2‐way communication structure into the patient handoff with both offgoing and oncoming providers having predefined roles.
Much of the information on our written handoff (patient identifying information, medications, language preference, code status, admission date) is not verbalized unless it is part of the active issues or the if‐then, follow‐ups (ie, medication titration for a patient admitted with an acute coronary syndrome or cor status in a patient newly made comfort care). By not reading extraneous information, we seek to emphasize the Active issues as well as the If‐then, Follow‐ups. We feel this emphasis maximizes the effectiveness of the handoff, while the purposeful nonverbalization of written materials such as identifying information maximizes its efficiency. Future work may examine which verbal and written structures for patient handoffs most benefit patient care and workflow through standard communication.
While our students found the Handoff Selective to be useful and to improve their self‐perceived ability to perform handoffs, we were not able to determine whether our program affected downstream outcomes such as adverse events relating to failures in handoff communication. Additionally, since we only taught and evaluated our Selective at the University of Colorado Denver School of Medicine, the response of our students may not generalize to other medical schools. Multicentered, prospective, randomized controlled trials may determine whether handoff education programs are successful in reducing patient adverse events related to transfers of care.
While handoffs occur frequently and are increasingly recognized as a vulnerable time in patient care, little is known about how to effectively teach handoffs to medical students during their clinical years. We developed a formal course to teach the importance of handoffs and how the process should be conducted. Our students reported that the Handoff Selective we developed improved their knowledge about the process and their perception of their ability to perform handoffs in a time‐appropriate and effective manner. In response to the feedback we received from our students, the Handoff Selective is the only course in the ICC that has been made mandatory for all students.
- , , .Communication failures: an insidious contributor to medical mishaps.Acad Med.2004;79:186–194.
- Root causes of sentinel events. The Joint Commission. Available at: http://www.jointcommission.org/NR/rdonlyres/FA465646‐5F5F‐4543‐AC8F‐E8AF6571E372/0/root_cause_se.jpg Accessed October2009.
- , , , et al.Lost in translation: challenges‐to‐physician communication during patient handoffs.Acad Med.2005;80:1094–1099.
- Institute of Medicine.Resident Duty Hours: Enhancing Sleep, Supervision and Safety.Washington, DC:National Academies Press;2008.
- ACGME duty hours. Accreditation Council for Graduate Medical Education. http://www.acgme.org/acWebsite/dutyHours/dh_ComProgrRequirmentsDutyHours0707.pdf. Accessed October2009.
- , , , et al.Mortality among hospitalized Medicare beneficiaries in the first 2 years following ACGME duty hour reform.JAMA.2007;298(9):975–983.
- , , , et al.Mortality among patient in VA hospitals in the first 2 years following ACGME duty hour reform.JAMA.2007;298(9):984–992.
- , , , .Changes in outcomes for internal medicine patients after work‐hour regulations.Ann Intern Med.2007;147(2):1–7.
- , , , et al.Transfers of patient care between house staff on internal medicine wards.Arch Intern Med.2006;166:1173–1177.
- , , , .Medical errors involving trainees.Arch Intern Med.2007;167(19):2030–2036.
- .Reducing resident work hours: unproven assumptions and unforeseen outcomes.Ann Intern Med.2006;140:814–815.
- , , et al.Consequences of inadequate sign‐out for patient care.Arch Intern Med.2008;168(16):1755–1760.
- JCAHO Handoff Communication. National patient safety goal. The Joint Commission. http://www.jointcommission.org/GeneralPublic/NPSG/07_npsgs.htm. Accessed October2009.
- , , , et al.A structured handoff program for interns.Acad Med.2009;84:347–352.
- , , .Development and implementation of an oral sign out skills curriculum.J Gen Intern Med.2007;22(10):1470–1474.
- , , , et al.Managing discontinuity in academic medical centers: strategies for a safe and effective sign out.J Hosp Med.2006;1:257–266.
- , , , .A theoretical framework and competency based approach to improving handoffs.Qual Saf Health Care.2008;17:11–14.
- , , .The human factor: the critical importance of effective teamwork in providing safe care.Qual Saf Health Care.2004;13(suppl 1):i85–i90.
- University HealthSystem Consortium Best Practice Recommendation: Patient Handoff Communication. White Paper. May 2006.Oak Brook, IL:University HealthSystem Consortium;2006.
- , , , , .Handoff strategies in settings with high consequences for failure: lessons for health care operations.Int J Qual Health Care.2004;16(2):125–132.
Communication failures are well‐recognized as causes of medical errors.1, 2 Specifically, handoffs of patient care responsibilities, which are increasingly prevalent in academic medical centers,3 have been cited as the most frequent cause of teamwork breakdown resulting in the harmful medical errors found in malpractice claims.1 The Institute of Medicine has recently identified patient handoffs as the moment where patient care errors are most likely to occur.4 A survey of 125 U.S. medical schools, however, found that only 8% specifically taught students how to hand off patient care.3
In July 2003, the American Council of Graduate Medical Education (ACGME) mandated that residency programs decrease resident work hours to improve patient care and safety by reducing fatigue,5 and a recent Institute of Medicine report suggests that they be decreased even further.4 Studies examining outcomes during the first 2 years after reducing duty hours did not find reductions in risk‐adjusted mortality.68 One proposed explanation for this lack of improvement is that the reduction in fatigue‐related medical errors is being offset by discontinuity of care with due to the increased number of patient handoffs resulting from shortened duty hours,911 one recent study found that omission of key information during patient sign outs frequently resulted in adverse patient care outcomes.12
In 2007, the Joint Commission developed a new National Patient Safety Goal that requires organizations to improve communication between caregivers.13 We recently developed an approach by which Internal Medicine residents hand off patient care using a structured process, written and verbal templates, formal training about handoffs, and direct attending supervision.14 Because fourth‐year medical students perform the duties of interns when working as subinterns, we recognized that education about handoffs should occur prior to the time students became interns. Accordingly, we developed a course designed to teach patient handoffs to medical students at the transition between their third and fourth years of training.
Setting
The Handoff Selective was developed by faculty of Denver Health and the University of Colorado Denver School of Medicine.
Program Description
The Selective was first offered in April 2007 as part of an Integrated Clinician's Course (ICC), a 2‐week course for students beginning their fourth year, which starts in April at the University of Colorado. The ICC includes both mandatory and selective sessions that are focused on developing clinical skills and preparing them for their subinternships. The Handoff Selective was conducted in a computerized teaching laboratory, lasted a total of 2 hours and consisted of 2 parts. Each of the 5 Denver Health Hospital Medicine faculty members versed in handoff education taught 2 sessions of 6 to 8 students.
Part 1: Didactic
During the first hour of class, the faculty presented a lecture that summarized the relevant literature on handoffs and explained the importance of the topic. The objectives of the didactic were to: (1) understand the importance of handoffs; (2) explore different communication elements and structures; (3) gain exposure to handoffs outside of healthcare; and (4) learn a structure for handoffs of patient care in hospitalized patients.
We used 3 video clips of handoffs from 2 football games to demonstrate the importance of practice, training, and 2‐way communications in handoffs. The first video clip showed a runner trying to make a spontaneous handoff while being tackled. The receiver was not expecting the handoff and was preoccupied with blocking another player. This attempted handoff resulted in a fumble, which we related to an adverse patient event.
The next 2 video clips showed 2 complex, seldom used, but well‐known football handoffsthe hook and lateral and the Statue of Liberty. Both handoffs were successfully executed presumably as a result of education, practice and the active participation of both players (handing off and receiving) in the process. We then related the teaching and practicing of complex communication to the Joint Commission on Accreditation of Healthcare Organizations (JCAHO; now simply the Joint Commission) data suggesting that most sentinel events have their root cause in communication and training failures.2
Basic communication elements and process structures were then explored using scenarios from everyday life and evidence from fields outside of medicine. We emphasized that structures for communication (modes, vehicles, and settings) must be chosen according to the occasion and that handoffs are common and important in all occupations. In discussing modes (verbal, written, or nonverbal), vehicles (paper, telephone, or e‐mail), and settings (face‐to face, virtual, or disconnected), we emphasized that the most effective structures for communication (verbal, face‐to face meetings, with written materials and other visual aids at the patient's bedside) were also the most time‐consuming (Figure 1). While our standard for resident handoffs is a face‐to‐face verbal interaction with preprinted written materials as an aid, we also emphasized that for complex patients (eg, mental status changes, concern for an acute abdomen) more robust communication is often needed. Accordingly, a more time‐consuming bedside handoff with simultaneous, focused physical exam and history‐taking by both oncoming and off‐going providers may be most appropriate.
As real‐life examples, we asked our students to communicate a happy birthday wish to their mother, who lives in another state. Almost uniformly, in addition to a written aid (birthday card), they choose the telephone as a vehicle for their verbal mode in a virtual setting with 2‐way communication possible. In contrast, when asked to propose marriage to a significant other in another state, students felt that a face‐to‐face meeting with verbal and nonverbal (ie, ring) modes was appropriate. This time‐consuming mode of communication was felt to be necessary to create a sentiment of importance and avert any possible miscommunication.
The didactic session concluded by demonstrating how to use standardized written and verbal templates for handoffs of the care of a hospitalized patient. We explore the differentiation between written and verbal handoffs in our discussion below.
Part 2: Practicum
The second hour was devoted to practicing handoffs as a group. The faculty developed 6 case scenarios that differed with respect to diagnosis, length of stay, active medical issues, and anticipated discharge (Table 1). The scenarios included extensive admission information as well as evolving issues for each patient that were specific to the day of the intended handoff. Students were given Microsoft Word table‐based handoff templates to use when creating written sign‐outs for their patients. Verbal handoffs were performed between students and sign‐outs were exchanged. The faculty then role‐played cross‐cover calls that were specific for each scenario to test the students' inclusion of integral information in their handoffs and their ability to create contingency plans.
| Diagnosis | LOS | Active Issues | Cross‐Cover |
|---|---|---|---|
| |||
| CP | 1 | CP, HTN, DM | CP, HTN, headache |
| GIB | 1 | GIB, alcohol withdrawal | Poor response to red call transfusion, coagulopathy |
| Acute pancreatitis | 2 | Pain, possible pancreatic abscess | Fever, agitation, hypoxia |
| CHF | 2 | CHF, DM, nausea | Lack of diuresis, CP, hypoglycemia |
| Acute kidney injury | 3 | None, ready for discharge | HTN, hyperglycemia |
| Community acquired pneumonia | 3 | Anxiety, discharge pending | Confusion, emesis with hypoxia |
Program Evaluation
We developed a 2‐part survey to evaluate the effectiveness of the Selective and to solicit feedback about the didactic and practicum portions of the course. The first part of the survey (Table 2) contained 16 items to assess the students' knowledge of, and attitudes toward handing off patient care, along with their comfort with the handoff process. Responses to this section were scored using a 5‐point Likert scale with 1 indicating strongly disagree and 5 indicating strongly agree. This part of the survey was administered both prior to and after the Selective.
| Competency | Selective | |
|---|---|---|
| Before | After | |
| ||
| I know how to hand off patients | 2.3 0.8 | 4.2 0.6* |
| I know how to make contingency plans for my patients | 2.1 0.8 | 3.9 0.7* |
| I know what a read‐back is | 2.3 1.3 | 4.4 0.9* |
| I know how to perform a read‐back | 2.0 1.2 | 4.2 0.9* |
| I know when to perform a read‐back | 1.6 0.8 | 4.1 1.0* |
| I am efficient at communicating patient information | 2.2 0.9 | 3.6 0.7* |
| I am effective at communicating patient information | 2.2 0.8 | 3.8 0.6* |
| I know a standard written structure for handoffs | 2.1 1.1 | 4.4 0.6* |
| I know a standard verbal structure for handoffs | 2.0 1.1 | 4.2 0.6* |
| I can choose appropriate modes of communication | 2.7 1.1 | 4.4 0.6* |
| I can choose appropriate vehicles of communication | 2.6 1.1 | 4.5 0.6* |
| I can choose appropriate settings for communication | 2.9 1.1 | 4.4 0.6* |
| Handoffs are well taught in my medical school | 1.6 0.8 | 3.5 1.0* |
| Standardization is important in handoffs | 4.3 0.9 | 4.6 0.5 |
| Handoffs are safer with attending supervision | 3.7 1.0 | 3.9 0.8 |
| I feel comfortable cross‐covering on patients | 1.6 0.7 | 3.0 1.0* |
The second part (Table 3) contained 12 items and was designed to evaluate the perceived usefulness of the different components of the class. This section was only administered at the end of the Selective. It utilized a 4‐point Likert scale with 1 indicating that the component was not useful at all, and 4 indicating that it was extremely useful. The first 6 items of the second section allowed students to evaluate the didactic portion of the handoff. The second 6 items allowed students to evaluate the practicum. Responses to all 12 items were then combined to determine an overall composite usefulness for the Selective.
| Useful [n (%)] | |
|---|---|
| |
| Overall composite usefulness | 578 (92) |
| Didactic composite usefulness | 254 (84) |
| Using fumble video clips for discussing handoffs | 32 (64)* |
| Discussion of modes of communication | 46 (88) |
| Discussion of vehicles of communication | 46 (88) |
| Discussion of settings of communication | 48 (96) |
| Choosing handoff structures for nonhealthcare handoffs | 37 (71)* |
| Discussing handoffs in industries outside of healthcare | 45 (94) |
| Practicum composite usefulness | 324(100) |
| Role playing | 54 (100) |
| Patient handoff scenarios | 54 (100) |
| Completing computerized templates | 54 (100) |
| Delivering handoffs to peer | 54 (100) |
| Receiving handoffs from peer | 54 (100) |
| Cross‐cover questions and discussion | 54 (100) |
The Selective was also evaluated qualitatively through the use of open‐ended, written comments that were solicited at the end of the survey. All surveys were administered anonymously.
Data Analysis
Student paired t test was used to compare continuous variables recorded before and after the Selective. A chi‐square test was used to assess the students' perception of the usefulness of the didactic vs. the practicum methods of teaching handoffs.
All analyses were performed using SAS (version 8.1; SAS Institute, Inc., Cary, NC). Bonferroni corrections were used for multiple comparisons such that P values of <0.003 and <0.004 were considered to be significant for continuous and categorical variables, respectively. All data are reported as mean standard deviation (SD).
The survey was approved by our local Institutional Review Board.
Results
More students chose the Selective than we had capacity to accommodate (60 of a class of 150). The pre‐ and postcourse survey response rate was 56 of 60 (93%) and 58 of 60 (97%), respectively. After the Selective, the mean score in response to whether handoffs are well taught in medical school increased from 1.6 to 3.5 (P < 0.003). Our students' self‐perceived skills and knowledge about handoffs improved after the Selective (Table 2). The greatest changes in perceived knowledge occurred in questions regarding the what, how, and when of read‐backs, and the knowledge of standard verbal and written handoff structures. The responses to the survey elements which assessed our students' attitudes regarding the importance of standardization and whether they felt handoffs were safer with faculty supervision did not change after the Selective (Table 2).
A total of 92% of the students felt that the course was extremely useful or useful. The role‐playing activity was thought to be more helpful than the didactic, but 84% of the students still rated the didactic portion as useful or extremely useful (Table 3). The element which was the least well received in the didactic portion was the use of video clips to demonstrate successful and unsuccessful (fumbled) college football handoffs, although the majority (64%) of students still found it useful.
The major theme generated from the comments section of the survey was that the Selective should be a required course.
Discussion
We know of no previously published literature that has addressed teaching handoffs to medical students. Horwitz et al.15 developed a sign‐out curriculum for Internal Medicine residents and found that none of their house‐staff had any previous training in handoffs during medical school, consistent with the finding that only 8% of U.S. medical schools provided formal instruction on handoffs.3 Prior to taking the Selective, our students had no knowledge of verbal or written templates for patient handoffs, although both before and after the course they felt that standardization was an important component of the process.
A number of verbal structures for handing off patient care have been described in the literature and there is not a consensus as to which functions best. Perhaps the most cited verbal communication format is SBAR (ie, situation, background, assessment and recommendation).16, 17 This tool was developed by Leonard et al.18 specifically for use by nurses to provide 1‐way communication to physicians pertaining to a change in patient status. We considered teaching the SBAR approach to the students but felt that it did not provide a suitable structure for handoffs because the transfer of care is not generally an event‐based situation and the literature on handoffs indicates that an optimal verbal system includes 2‐way communication.
Additional mnemonics for handoffs found in the literature include SIGNOUT (ie, Sick or DNR, Identifying information, General hospital course, New events of the day, Overall health status, Upcoming possibilities with plan, and Tasks to complete),14 I PASS the BATON (ie, Introduction, Patient, Assessment, Situation, Safety, Background, Actions, Timing, Ownership, Next)19 and the SAIF‐IR system (see boxed text).14
Verbal Structure for Patient Handoffs: SAIF‐IR
Off‐going provider performs a SAIF handoff:
Summary statement(s)
Active issues
If‐then contingency planning
Follow‐up activities
On‐coming provider makes the handoff SAIF‐IR:
Interactive questioning
Read‐backs
We developed the SAIF‐IR mnemonic to maximize efficiency and effectiveness while differentiating the verbal portion of the handoff from the written and incorporating 2‐way communication into its structure. In the Summary statement, we emphasize that this is not a history of present illness. We ask our students to summarize, in 1 to 3 sentences, the patient's presentation and working diagnosis. When discussing patient issues, we ask our students to only verbalize Active issues, although the written template has inactive, chronic issues listed. Here, we also ask our students to express their level of concern for the active issues and patient in general. If‐then's and Follow‐ups are usually verbalized together. Based on the offgoing provider's knowledge of the patient, we encourage the offgoing provider to anticipate potential problems and advise the oncoming provider on potential responses. Much of this advice is difficult to express in the written format and thus may not be found on the written handoff when the verbal handoff occurs. We encourage oncoming providers to take notes on the preprinted handoff sheet as part of the handoff process.
Through Interactive questioning and Read‐backs, we train our students and house‐staff to use the active listening techniques used outside of healthcare, in settings such as nuclear power plants and National Aeronautics and Space Administration mission control, where poor handoff communication may also result in safety concerns and adverse events.20 Interactive questioning allows the oncoming provider to correct or clarify any information given by the off‐going provider. Read‐backs are a method of confirming follow‐up activity or contingency plans. Together, the SAIF‐IR mnemonic builds a 2‐way communication structure into the patient handoff with both offgoing and oncoming providers having predefined roles.
Much of the information on our written handoff (patient identifying information, medications, language preference, code status, admission date) is not verbalized unless it is part of the active issues or the if‐then, follow‐ups (ie, medication titration for a patient admitted with an acute coronary syndrome or cor status in a patient newly made comfort care). By not reading extraneous information, we seek to emphasize the Active issues as well as the If‐then, Follow‐ups. We feel this emphasis maximizes the effectiveness of the handoff, while the purposeful nonverbalization of written materials such as identifying information maximizes its efficiency. Future work may examine which verbal and written structures for patient handoffs most benefit patient care and workflow through standard communication.
While our students found the Handoff Selective to be useful and to improve their self‐perceived ability to perform handoffs, we were not able to determine whether our program affected downstream outcomes such as adverse events relating to failures in handoff communication. Additionally, since we only taught and evaluated our Selective at the University of Colorado Denver School of Medicine, the response of our students may not generalize to other medical schools. Multicentered, prospective, randomized controlled trials may determine whether handoff education programs are successful in reducing patient adverse events related to transfers of care.
While handoffs occur frequently and are increasingly recognized as a vulnerable time in patient care, little is known about how to effectively teach handoffs to medical students during their clinical years. We developed a formal course to teach the importance of handoffs and how the process should be conducted. Our students reported that the Handoff Selective we developed improved their knowledge about the process and their perception of their ability to perform handoffs in a time‐appropriate and effective manner. In response to the feedback we received from our students, the Handoff Selective is the only course in the ICC that has been made mandatory for all students.
Communication failures are well‐recognized as causes of medical errors.1, 2 Specifically, handoffs of patient care responsibilities, which are increasingly prevalent in academic medical centers,3 have been cited as the most frequent cause of teamwork breakdown resulting in the harmful medical errors found in malpractice claims.1 The Institute of Medicine has recently identified patient handoffs as the moment where patient care errors are most likely to occur.4 A survey of 125 U.S. medical schools, however, found that only 8% specifically taught students how to hand off patient care.3
In July 2003, the American Council of Graduate Medical Education (ACGME) mandated that residency programs decrease resident work hours to improve patient care and safety by reducing fatigue,5 and a recent Institute of Medicine report suggests that they be decreased even further.4 Studies examining outcomes during the first 2 years after reducing duty hours did not find reductions in risk‐adjusted mortality.68 One proposed explanation for this lack of improvement is that the reduction in fatigue‐related medical errors is being offset by discontinuity of care with due to the increased number of patient handoffs resulting from shortened duty hours,911 one recent study found that omission of key information during patient sign outs frequently resulted in adverse patient care outcomes.12
In 2007, the Joint Commission developed a new National Patient Safety Goal that requires organizations to improve communication between caregivers.13 We recently developed an approach by which Internal Medicine residents hand off patient care using a structured process, written and verbal templates, formal training about handoffs, and direct attending supervision.14 Because fourth‐year medical students perform the duties of interns when working as subinterns, we recognized that education about handoffs should occur prior to the time students became interns. Accordingly, we developed a course designed to teach patient handoffs to medical students at the transition between their third and fourth years of training.
Setting
The Handoff Selective was developed by faculty of Denver Health and the University of Colorado Denver School of Medicine.
Program Description
The Selective was first offered in April 2007 as part of an Integrated Clinician's Course (ICC), a 2‐week course for students beginning their fourth year, which starts in April at the University of Colorado. The ICC includes both mandatory and selective sessions that are focused on developing clinical skills and preparing them for their subinternships. The Handoff Selective was conducted in a computerized teaching laboratory, lasted a total of 2 hours and consisted of 2 parts. Each of the 5 Denver Health Hospital Medicine faculty members versed in handoff education taught 2 sessions of 6 to 8 students.
Part 1: Didactic
During the first hour of class, the faculty presented a lecture that summarized the relevant literature on handoffs and explained the importance of the topic. The objectives of the didactic were to: (1) understand the importance of handoffs; (2) explore different communication elements and structures; (3) gain exposure to handoffs outside of healthcare; and (4) learn a structure for handoffs of patient care in hospitalized patients.
We used 3 video clips of handoffs from 2 football games to demonstrate the importance of practice, training, and 2‐way communications in handoffs. The first video clip showed a runner trying to make a spontaneous handoff while being tackled. The receiver was not expecting the handoff and was preoccupied with blocking another player. This attempted handoff resulted in a fumble, which we related to an adverse patient event.
The next 2 video clips showed 2 complex, seldom used, but well‐known football handoffsthe hook and lateral and the Statue of Liberty. Both handoffs were successfully executed presumably as a result of education, practice and the active participation of both players (handing off and receiving) in the process. We then related the teaching and practicing of complex communication to the Joint Commission on Accreditation of Healthcare Organizations (JCAHO; now simply the Joint Commission) data suggesting that most sentinel events have their root cause in communication and training failures.2
Basic communication elements and process structures were then explored using scenarios from everyday life and evidence from fields outside of medicine. We emphasized that structures for communication (modes, vehicles, and settings) must be chosen according to the occasion and that handoffs are common and important in all occupations. In discussing modes (verbal, written, or nonverbal), vehicles (paper, telephone, or e‐mail), and settings (face‐to face, virtual, or disconnected), we emphasized that the most effective structures for communication (verbal, face‐to face meetings, with written materials and other visual aids at the patient's bedside) were also the most time‐consuming (Figure 1). While our standard for resident handoffs is a face‐to‐face verbal interaction with preprinted written materials as an aid, we also emphasized that for complex patients (eg, mental status changes, concern for an acute abdomen) more robust communication is often needed. Accordingly, a more time‐consuming bedside handoff with simultaneous, focused physical exam and history‐taking by both oncoming and off‐going providers may be most appropriate.
As real‐life examples, we asked our students to communicate a happy birthday wish to their mother, who lives in another state. Almost uniformly, in addition to a written aid (birthday card), they choose the telephone as a vehicle for their verbal mode in a virtual setting with 2‐way communication possible. In contrast, when asked to propose marriage to a significant other in another state, students felt that a face‐to‐face meeting with verbal and nonverbal (ie, ring) modes was appropriate. This time‐consuming mode of communication was felt to be necessary to create a sentiment of importance and avert any possible miscommunication.
The didactic session concluded by demonstrating how to use standardized written and verbal templates for handoffs of the care of a hospitalized patient. We explore the differentiation between written and verbal handoffs in our discussion below.
Part 2: Practicum
The second hour was devoted to practicing handoffs as a group. The faculty developed 6 case scenarios that differed with respect to diagnosis, length of stay, active medical issues, and anticipated discharge (Table 1). The scenarios included extensive admission information as well as evolving issues for each patient that were specific to the day of the intended handoff. Students were given Microsoft Word table‐based handoff templates to use when creating written sign‐outs for their patients. Verbal handoffs were performed between students and sign‐outs were exchanged. The faculty then role‐played cross‐cover calls that were specific for each scenario to test the students' inclusion of integral information in their handoffs and their ability to create contingency plans.
| Diagnosis | LOS | Active Issues | Cross‐Cover |
|---|---|---|---|
| |||
| CP | 1 | CP, HTN, DM | CP, HTN, headache |
| GIB | 1 | GIB, alcohol withdrawal | Poor response to red call transfusion, coagulopathy |
| Acute pancreatitis | 2 | Pain, possible pancreatic abscess | Fever, agitation, hypoxia |
| CHF | 2 | CHF, DM, nausea | Lack of diuresis, CP, hypoglycemia |
| Acute kidney injury | 3 | None, ready for discharge | HTN, hyperglycemia |
| Community acquired pneumonia | 3 | Anxiety, discharge pending | Confusion, emesis with hypoxia |
Program Evaluation
We developed a 2‐part survey to evaluate the effectiveness of the Selective and to solicit feedback about the didactic and practicum portions of the course. The first part of the survey (Table 2) contained 16 items to assess the students' knowledge of, and attitudes toward handing off patient care, along with their comfort with the handoff process. Responses to this section were scored using a 5‐point Likert scale with 1 indicating strongly disagree and 5 indicating strongly agree. This part of the survey was administered both prior to and after the Selective.
| Competency | Selective | |
|---|---|---|
| Before | After | |
| ||
| I know how to hand off patients | 2.3 0.8 | 4.2 0.6* |
| I know how to make contingency plans for my patients | 2.1 0.8 | 3.9 0.7* |
| I know what a read‐back is | 2.3 1.3 | 4.4 0.9* |
| I know how to perform a read‐back | 2.0 1.2 | 4.2 0.9* |
| I know when to perform a read‐back | 1.6 0.8 | 4.1 1.0* |
| I am efficient at communicating patient information | 2.2 0.9 | 3.6 0.7* |
| I am effective at communicating patient information | 2.2 0.8 | 3.8 0.6* |
| I know a standard written structure for handoffs | 2.1 1.1 | 4.4 0.6* |
| I know a standard verbal structure for handoffs | 2.0 1.1 | 4.2 0.6* |
| I can choose appropriate modes of communication | 2.7 1.1 | 4.4 0.6* |
| I can choose appropriate vehicles of communication | 2.6 1.1 | 4.5 0.6* |
| I can choose appropriate settings for communication | 2.9 1.1 | 4.4 0.6* |
| Handoffs are well taught in my medical school | 1.6 0.8 | 3.5 1.0* |
| Standardization is important in handoffs | 4.3 0.9 | 4.6 0.5 |
| Handoffs are safer with attending supervision | 3.7 1.0 | 3.9 0.8 |
| I feel comfortable cross‐covering on patients | 1.6 0.7 | 3.0 1.0* |
The second part (Table 3) contained 12 items and was designed to evaluate the perceived usefulness of the different components of the class. This section was only administered at the end of the Selective. It utilized a 4‐point Likert scale with 1 indicating that the component was not useful at all, and 4 indicating that it was extremely useful. The first 6 items of the second section allowed students to evaluate the didactic portion of the handoff. The second 6 items allowed students to evaluate the practicum. Responses to all 12 items were then combined to determine an overall composite usefulness for the Selective.
| Useful [n (%)] | |
|---|---|
| |
| Overall composite usefulness | 578 (92) |
| Didactic composite usefulness | 254 (84) |
| Using fumble video clips for discussing handoffs | 32 (64)* |
| Discussion of modes of communication | 46 (88) |
| Discussion of vehicles of communication | 46 (88) |
| Discussion of settings of communication | 48 (96) |
| Choosing handoff structures for nonhealthcare handoffs | 37 (71)* |
| Discussing handoffs in industries outside of healthcare | 45 (94) |
| Practicum composite usefulness | 324(100) |
| Role playing | 54 (100) |
| Patient handoff scenarios | 54 (100) |
| Completing computerized templates | 54 (100) |
| Delivering handoffs to peer | 54 (100) |
| Receiving handoffs from peer | 54 (100) |
| Cross‐cover questions and discussion | 54 (100) |
The Selective was also evaluated qualitatively through the use of open‐ended, written comments that were solicited at the end of the survey. All surveys were administered anonymously.
Data Analysis
Student paired t test was used to compare continuous variables recorded before and after the Selective. A chi‐square test was used to assess the students' perception of the usefulness of the didactic vs. the practicum methods of teaching handoffs.
All analyses were performed using SAS (version 8.1; SAS Institute, Inc., Cary, NC). Bonferroni corrections were used for multiple comparisons such that P values of <0.003 and <0.004 were considered to be significant for continuous and categorical variables, respectively. All data are reported as mean standard deviation (SD).
The survey was approved by our local Institutional Review Board.
Results
More students chose the Selective than we had capacity to accommodate (60 of a class of 150). The pre‐ and postcourse survey response rate was 56 of 60 (93%) and 58 of 60 (97%), respectively. After the Selective, the mean score in response to whether handoffs are well taught in medical school increased from 1.6 to 3.5 (P < 0.003). Our students' self‐perceived skills and knowledge about handoffs improved after the Selective (Table 2). The greatest changes in perceived knowledge occurred in questions regarding the what, how, and when of read‐backs, and the knowledge of standard verbal and written handoff structures. The responses to the survey elements which assessed our students' attitudes regarding the importance of standardization and whether they felt handoffs were safer with faculty supervision did not change after the Selective (Table 2).
A total of 92% of the students felt that the course was extremely useful or useful. The role‐playing activity was thought to be more helpful than the didactic, but 84% of the students still rated the didactic portion as useful or extremely useful (Table 3). The element which was the least well received in the didactic portion was the use of video clips to demonstrate successful and unsuccessful (fumbled) college football handoffs, although the majority (64%) of students still found it useful.
The major theme generated from the comments section of the survey was that the Selective should be a required course.
Discussion
We know of no previously published literature that has addressed teaching handoffs to medical students. Horwitz et al.15 developed a sign‐out curriculum for Internal Medicine residents and found that none of their house‐staff had any previous training in handoffs during medical school, consistent with the finding that only 8% of U.S. medical schools provided formal instruction on handoffs.3 Prior to taking the Selective, our students had no knowledge of verbal or written templates for patient handoffs, although both before and after the course they felt that standardization was an important component of the process.
A number of verbal structures for handing off patient care have been described in the literature and there is not a consensus as to which functions best. Perhaps the most cited verbal communication format is SBAR (ie, situation, background, assessment and recommendation).16, 17 This tool was developed by Leonard et al.18 specifically for use by nurses to provide 1‐way communication to physicians pertaining to a change in patient status. We considered teaching the SBAR approach to the students but felt that it did not provide a suitable structure for handoffs because the transfer of care is not generally an event‐based situation and the literature on handoffs indicates that an optimal verbal system includes 2‐way communication.
Additional mnemonics for handoffs found in the literature include SIGNOUT (ie, Sick or DNR, Identifying information, General hospital course, New events of the day, Overall health status, Upcoming possibilities with plan, and Tasks to complete),14 I PASS the BATON (ie, Introduction, Patient, Assessment, Situation, Safety, Background, Actions, Timing, Ownership, Next)19 and the SAIF‐IR system (see boxed text).14
Verbal Structure for Patient Handoffs: SAIF‐IR
Off‐going provider performs a SAIF handoff:
Summary statement(s)
Active issues
If‐then contingency planning
Follow‐up activities
On‐coming provider makes the handoff SAIF‐IR:
Interactive questioning
Read‐backs
We developed the SAIF‐IR mnemonic to maximize efficiency and effectiveness while differentiating the verbal portion of the handoff from the written and incorporating 2‐way communication into its structure. In the Summary statement, we emphasize that this is not a history of present illness. We ask our students to summarize, in 1 to 3 sentences, the patient's presentation and working diagnosis. When discussing patient issues, we ask our students to only verbalize Active issues, although the written template has inactive, chronic issues listed. Here, we also ask our students to express their level of concern for the active issues and patient in general. If‐then's and Follow‐ups are usually verbalized together. Based on the offgoing provider's knowledge of the patient, we encourage the offgoing provider to anticipate potential problems and advise the oncoming provider on potential responses. Much of this advice is difficult to express in the written format and thus may not be found on the written handoff when the verbal handoff occurs. We encourage oncoming providers to take notes on the preprinted handoff sheet as part of the handoff process.
Through Interactive questioning and Read‐backs, we train our students and house‐staff to use the active listening techniques used outside of healthcare, in settings such as nuclear power plants and National Aeronautics and Space Administration mission control, where poor handoff communication may also result in safety concerns and adverse events.20 Interactive questioning allows the oncoming provider to correct or clarify any information given by the off‐going provider. Read‐backs are a method of confirming follow‐up activity or contingency plans. Together, the SAIF‐IR mnemonic builds a 2‐way communication structure into the patient handoff with both offgoing and oncoming providers having predefined roles.
Much of the information on our written handoff (patient identifying information, medications, language preference, code status, admission date) is not verbalized unless it is part of the active issues or the if‐then, follow‐ups (ie, medication titration for a patient admitted with an acute coronary syndrome or cor status in a patient newly made comfort care). By not reading extraneous information, we seek to emphasize the Active issues as well as the If‐then, Follow‐ups. We feel this emphasis maximizes the effectiveness of the handoff, while the purposeful nonverbalization of written materials such as identifying information maximizes its efficiency. Future work may examine which verbal and written structures for patient handoffs most benefit patient care and workflow through standard communication.
While our students found the Handoff Selective to be useful and to improve their self‐perceived ability to perform handoffs, we were not able to determine whether our program affected downstream outcomes such as adverse events relating to failures in handoff communication. Additionally, since we only taught and evaluated our Selective at the University of Colorado Denver School of Medicine, the response of our students may not generalize to other medical schools. Multicentered, prospective, randomized controlled trials may determine whether handoff education programs are successful in reducing patient adverse events related to transfers of care.
While handoffs occur frequently and are increasingly recognized as a vulnerable time in patient care, little is known about how to effectively teach handoffs to medical students during their clinical years. We developed a formal course to teach the importance of handoffs and how the process should be conducted. Our students reported that the Handoff Selective we developed improved their knowledge about the process and their perception of their ability to perform handoffs in a time‐appropriate and effective manner. In response to the feedback we received from our students, the Handoff Selective is the only course in the ICC that has been made mandatory for all students.
- , , .Communication failures: an insidious contributor to medical mishaps.Acad Med.2004;79:186–194.
- Root causes of sentinel events. The Joint Commission. Available at: http://www.jointcommission.org/NR/rdonlyres/FA465646‐5F5F‐4543‐AC8F‐E8AF6571E372/0/root_cause_se.jpg Accessed October2009.
- , , , et al.Lost in translation: challenges‐to‐physician communication during patient handoffs.Acad Med.2005;80:1094–1099.
- Institute of Medicine.Resident Duty Hours: Enhancing Sleep, Supervision and Safety.Washington, DC:National Academies Press;2008.
- ACGME duty hours. Accreditation Council for Graduate Medical Education. http://www.acgme.org/acWebsite/dutyHours/dh_ComProgrRequirmentsDutyHours0707.pdf. Accessed October2009.
- , , , et al.Mortality among hospitalized Medicare beneficiaries in the first 2 years following ACGME duty hour reform.JAMA.2007;298(9):975–983.
- , , , et al.Mortality among patient in VA hospitals in the first 2 years following ACGME duty hour reform.JAMA.2007;298(9):984–992.
- , , , .Changes in outcomes for internal medicine patients after work‐hour regulations.Ann Intern Med.2007;147(2):1–7.
- , , , et al.Transfers of patient care between house staff on internal medicine wards.Arch Intern Med.2006;166:1173–1177.
- , , , .Medical errors involving trainees.Arch Intern Med.2007;167(19):2030–2036.
- .Reducing resident work hours: unproven assumptions and unforeseen outcomes.Ann Intern Med.2006;140:814–815.
- , , et al.Consequences of inadequate sign‐out for patient care.Arch Intern Med.2008;168(16):1755–1760.
- JCAHO Handoff Communication. National patient safety goal. The Joint Commission. http://www.jointcommission.org/GeneralPublic/NPSG/07_npsgs.htm. Accessed October2009.
- , , , et al.A structured handoff program for interns.Acad Med.2009;84:347–352.
- , , .Development and implementation of an oral sign out skills curriculum.J Gen Intern Med.2007;22(10):1470–1474.
- , , , et al.Managing discontinuity in academic medical centers: strategies for a safe and effective sign out.J Hosp Med.2006;1:257–266.
- , , , .A theoretical framework and competency based approach to improving handoffs.Qual Saf Health Care.2008;17:11–14.
- , , .The human factor: the critical importance of effective teamwork in providing safe care.Qual Saf Health Care.2004;13(suppl 1):i85–i90.
- University HealthSystem Consortium Best Practice Recommendation: Patient Handoff Communication. White Paper. May 2006.Oak Brook, IL:University HealthSystem Consortium;2006.
- , , , , .Handoff strategies in settings with high consequences for failure: lessons for health care operations.Int J Qual Health Care.2004;16(2):125–132.
- , , .Communication failures: an insidious contributor to medical mishaps.Acad Med.2004;79:186–194.
- Root causes of sentinel events. The Joint Commission. Available at: http://www.jointcommission.org/NR/rdonlyres/FA465646‐5F5F‐4543‐AC8F‐E8AF6571E372/0/root_cause_se.jpg Accessed October2009.
- , , , et al.Lost in translation: challenges‐to‐physician communication during patient handoffs.Acad Med.2005;80:1094–1099.
- Institute of Medicine.Resident Duty Hours: Enhancing Sleep, Supervision and Safety.Washington, DC:National Academies Press;2008.
- ACGME duty hours. Accreditation Council for Graduate Medical Education. http://www.acgme.org/acWebsite/dutyHours/dh_ComProgrRequirmentsDutyHours0707.pdf. Accessed October2009.
- , , , et al.Mortality among hospitalized Medicare beneficiaries in the first 2 years following ACGME duty hour reform.JAMA.2007;298(9):975–983.
- , , , et al.Mortality among patient in VA hospitals in the first 2 years following ACGME duty hour reform.JAMA.2007;298(9):984–992.
- , , , .Changes in outcomes for internal medicine patients after work‐hour regulations.Ann Intern Med.2007;147(2):1–7.
- , , , et al.Transfers of patient care between house staff on internal medicine wards.Arch Intern Med.2006;166:1173–1177.
- , , , .Medical errors involving trainees.Arch Intern Med.2007;167(19):2030–2036.
- .Reducing resident work hours: unproven assumptions and unforeseen outcomes.Ann Intern Med.2006;140:814–815.
- , , et al.Consequences of inadequate sign‐out for patient care.Arch Intern Med.2008;168(16):1755–1760.
- JCAHO Handoff Communication. National patient safety goal. The Joint Commission. http://www.jointcommission.org/GeneralPublic/NPSG/07_npsgs.htm. Accessed October2009.
- , , , et al.A structured handoff program for interns.Acad Med.2009;84:347–352.
- , , .Development and implementation of an oral sign out skills curriculum.J Gen Intern Med.2007;22(10):1470–1474.
- , , , et al.Managing discontinuity in academic medical centers: strategies for a safe and effective sign out.J Hosp Med.2006;1:257–266.
- , , , .A theoretical framework and competency based approach to improving handoffs.Qual Saf Health Care.2008;17:11–14.
- , , .The human factor: the critical importance of effective teamwork in providing safe care.Qual Saf Health Care.2004;13(suppl 1):i85–i90.
- University HealthSystem Consortium Best Practice Recommendation: Patient Handoff Communication. White Paper. May 2006.Oak Brook, IL:University HealthSystem Consortium;2006.
- , , , , .Handoff strategies in settings with high consequences for failure: lessons for health care operations.Int J Qual Health Care.2004;16(2):125–132.
Copyright © 2010 Society of Hospital Medicine
In response to: A quality conundrum: Well done but not enough—Quality improvement conundrums: Looking back before moving forward
If clinician‐quality improvers are to gain traction as academicians,1 their first objective should be to bring quality improvement (QI) sandly into the world of scientific method. We believe that Dr. Chakraborti's 2 pointsthat the reasons for afferent limb failure need to be more closely investigated, and that lessons learned from 1 hospital's rapid response system (RRS) may not generalize to other hospitalsreflect the immaturity of QI as a science. In clinical science, 3 well‐defined testing phases bring 1 homogeneous, rigorously tested product to market that is monitored in a fourth phase. While Dr. Chakraborti urges us to examine our afferent limb failures more closely, the monitoring and reporting strategies used in the Josie King Patient Safety Program2 resonate with the postmarketing surveillance of Phase IV trials.
Although necessary and valid, we believe that the majority of the QI conundrum of RRS lies in the lack of premarket, stepwise testing of QI products. QI initiatives are often promulgated before an appropriate evidence base has been established. This lack of scientific rigor has resulted in RRS with calling criteria that have poor operating characteristics,3 undetermined methods for achieving afferent success,4 and efferent response arms of varying sizes and compositions.5 Consequently, a heterogeneous group of RRS have produced equivocal outcomes6 and diminished the applicability of lessons learned across institutions.
Indeed, while it is important to ask, What do we do now?, it may be more informative to answer the question, How did we get here?
- ,.Clinicians in quality improvement. A new career pathway in academic medicine.JAMA.2009;301(7):766–768.
- Josie King Foundation. Josie King Patient Safety Program. Available at: http://www.josieking.org/page.cfm?pageID=27. Accessed September2009.
- ,,,.Rapid response: a quality improvement conundrum.J Hosp Med.2009;4(4):255–257.
- .The rapid response team paradox: why doesn't anyone call for help?Crit Care Med.2008;36(2):634–636.
- ,,,.Dress for the occasion.Jt Comm J Qual Patient Saf.2009;35(6):295.
- ,,,,.Effects of rapid response systems on clinical outcomes: systematic review and meta‐analysis.J Hosp Med.2007;2(6):422–432.
If clinician‐quality improvers are to gain traction as academicians,1 their first objective should be to bring quality improvement (QI) sandly into the world of scientific method. We believe that Dr. Chakraborti's 2 pointsthat the reasons for afferent limb failure need to be more closely investigated, and that lessons learned from 1 hospital's rapid response system (RRS) may not generalize to other hospitalsreflect the immaturity of QI as a science. In clinical science, 3 well‐defined testing phases bring 1 homogeneous, rigorously tested product to market that is monitored in a fourth phase. While Dr. Chakraborti urges us to examine our afferent limb failures more closely, the monitoring and reporting strategies used in the Josie King Patient Safety Program2 resonate with the postmarketing surveillance of Phase IV trials.
Although necessary and valid, we believe that the majority of the QI conundrum of RRS lies in the lack of premarket, stepwise testing of QI products. QI initiatives are often promulgated before an appropriate evidence base has been established. This lack of scientific rigor has resulted in RRS with calling criteria that have poor operating characteristics,3 undetermined methods for achieving afferent success,4 and efferent response arms of varying sizes and compositions.5 Consequently, a heterogeneous group of RRS have produced equivocal outcomes6 and diminished the applicability of lessons learned across institutions.
Indeed, while it is important to ask, What do we do now?, it may be more informative to answer the question, How did we get here?
If clinician‐quality improvers are to gain traction as academicians,1 their first objective should be to bring quality improvement (QI) sandly into the world of scientific method. We believe that Dr. Chakraborti's 2 pointsthat the reasons for afferent limb failure need to be more closely investigated, and that lessons learned from 1 hospital's rapid response system (RRS) may not generalize to other hospitalsreflect the immaturity of QI as a science. In clinical science, 3 well‐defined testing phases bring 1 homogeneous, rigorously tested product to market that is monitored in a fourth phase. While Dr. Chakraborti urges us to examine our afferent limb failures more closely, the monitoring and reporting strategies used in the Josie King Patient Safety Program2 resonate with the postmarketing surveillance of Phase IV trials.
Although necessary and valid, we believe that the majority of the QI conundrum of RRS lies in the lack of premarket, stepwise testing of QI products. QI initiatives are often promulgated before an appropriate evidence base has been established. This lack of scientific rigor has resulted in RRS with calling criteria that have poor operating characteristics,3 undetermined methods for achieving afferent success,4 and efferent response arms of varying sizes and compositions.5 Consequently, a heterogeneous group of RRS have produced equivocal outcomes6 and diminished the applicability of lessons learned across institutions.
Indeed, while it is important to ask, What do we do now?, it may be more informative to answer the question, How did we get here?
- ,.Clinicians in quality improvement. A new career pathway in academic medicine.JAMA.2009;301(7):766–768.
- Josie King Foundation. Josie King Patient Safety Program. Available at: http://www.josieking.org/page.cfm?pageID=27. Accessed September2009.
- ,,,.Rapid response: a quality improvement conundrum.J Hosp Med.2009;4(4):255–257.
- .The rapid response team paradox: why doesn't anyone call for help?Crit Care Med.2008;36(2):634–636.
- ,,,.Dress for the occasion.Jt Comm J Qual Patient Saf.2009;35(6):295.
- ,,,,.Effects of rapid response systems on clinical outcomes: systematic review and meta‐analysis.J Hosp Med.2007;2(6):422–432.
- ,.Clinicians in quality improvement. A new career pathway in academic medicine.JAMA.2009;301(7):766–768.
- Josie King Foundation. Josie King Patient Safety Program. Available at: http://www.josieking.org/page.cfm?pageID=27. Accessed September2009.
- ,,,.Rapid response: a quality improvement conundrum.J Hosp Med.2009;4(4):255–257.
- .The rapid response team paradox: why doesn't anyone call for help?Crit Care Med.2008;36(2):634–636.
- ,,,.Dress for the occasion.Jt Comm J Qual Patient Saf.2009;35(6):295.
- ,,,,.Effects of rapid response systems on clinical outcomes: systematic review and meta‐analysis.J Hosp Med.2007;2(6):422–432.
The latest research you need to know
In This Edition
- Perioperative smoking cessation reduces postoperative complications.
- Quality of life is not diminished in heart failure patients receiving defibrillator therapy.
- Simplification of the revised Geneva score may be useful in assessing for pulmonary embolism.
- Non-cardiac surgery after drug eluting stents not associated with major cardiac risk.
- Major cardiac risk is lowest 90 days after bare metal stent percutaneous coronary intervention.
- Extensive cancer screening in unexplained VTE detects more malignancies, but does not affect cancer related mortality.
- Preadmission use of statins decreases after hospitalization mortality in pneumonia.
- Drug-eluting stents are better than bare-metal stents for PCI in acute MI, but additional randomized study is needed.
Does a short duration of perioperative smoking cessation lead to a reduction in postoperative complications?
Background: Prior studies have demonstrated a reduction in postoperative complications when patients stop smoking in the perioperative period. However, they have not clearly shown what effect a fairly short duration of cessation, such as a period of only four weeks, has on the frequency of complications.
Study design: Randomized controlled trial.
Setting: Four university-affiliated hospitals in Sweden.
Synopsis: Using 117 patients who were daily smokers for less than one year between the ages of 18-79 who were scheduled for elective general or orthopedic surgery, this study showed that a smoking-cessation intervention initiated as little as four weeks prior to surgery resulted in fewer postoperative complications. The complication rate was reduced from 41% in the control group to 21% in the intervention group, which received cessation counseling and nicotine-replacement therapy. The relative risk reduction was 49% (95% confidence interval, 3-40) with a number needed to treat of five.
Because this was a randomized controlled trial with a large observed benefit, it appears to be reasonable to endorse perioperative smoking cessation as late as four weeks before an elective surgery. The study was limited in its ability to detect a difference in wound infections by the small sample size and the possibility patients might have unblinded themselves to outcome assessors, causing an overestimation of the effect of the intervention on the primary outcome of all complications.
Bottom line: Perioperative smoking cessation reduces postoperative complications even when started just four weeks prior to surgery.
Citation: Lindstrom D, Azodi OS, Wladis A, et al. Effects of a perioperative smoking cessation intervention on postoperative complications. Ann Surg. 2008;248(5):739-745.
Does implantable-defibrillator therapy cause deterioration in quality of life for patients with heart failure?
Background: Patients with depressed left-ventricular function are known to have improved survival after receiving implantable cardioverter defibrillators (ICDs). However, there is concern ICD therapy can prolong survival at the expense of a diminished quality of life.
Study design: Randomized placebo-controlled trial.
Setting: Multiple centers in the U.S., Canada, and New Zealand.
Synopsis: Using 2,479 patients from the Sudden Cardiac Death in Heart Failure trial who were 18 and older and had stable heart failure and depressed left-ventricular function, this study demonstrated no significant quality-of-life difference at 30 months when compared with patients who received ICD, amiodarone, and state-of-the-art medical therapy or an amiodarone placebo and state-of-the-art medical therapy. While functional status did not differ at any time between the three groups, psychological well-being was improved in the ICD group at three months (p=0.01) and 12 months (p=0.03) when compared with the placebo group, but at 30 months there was no difference between the groups.
While the trial was randomized and placebo-controlled, the investigators were unable to blind patients or outcome assessors. Nevertheless, the lack of deterioration of quality of life in ICD patients is reassuring.
Bottom line: Placement of ICDs in heart failure patients with a high risk of sudden cardiac death does not appear to decrease quality of life.
Citation: Mark DB, Anstrom KJ, Sun JL, et al. Quality of life with defibrillator therapy or amiodarone in heart failure. N Engl J Med. 2008;359:999-1008.
Can a simplified, revised Geneva score retain diagnostic accuracy and clinical utility?
Background: The revised Geneva score is a validated and objective clinical decision rule, but has multiple variables with different weights. This can make the tool cumbersome and difficult to remember, and could lead to inaccurate calculations and misjudgments in patient care.
Study design: Retrospective cohort study.
Setting: Four university-affiliated European hospitals.
Synopsis: Using data from two prior prospective trials involving patients with suspected pulmonary embolism (PE), this study showed re-analysis of these patients with a simplified, revised Geneva score, which gives only one point to each clinical factor, resulted in the same level of diagnostic accuracy. Specifically, data from 1,049 patients was used to construct a receiver-operating characteristic curve analysis comparing the standardized and simplified Geneva score, which showed areas under the curve of 0.75 (95% confidence interval 0.71-0.78) and 0.74 (0.70-0.77), respectively. Additionally, the safety of using this clinical tool to rule out PE was demonstrated when using both a three-level (low-intermediate probability) and a dichotomized scheme (PE unlikely) in combination with a negative D-dimer test.
The retrospective nature of the study was its major limitation. The authors suggest a prospective study to complete validation of the simplified, revised Geneva score.
Bottom line: With prospective analysis, it might be possible to further validate a simplified, revised Geneva score.
Citation: Klok FA, Mos ICM, Nijkeuter M, et al. Simplification of the revised Geneva score for assessing clinical probability of pulmonary embolism. Arch Intern Med. 2008;168(19):2131-2136.
Is the rate of postoperative major adverse cardiac events (MACEs) inversely related to time after percutaneous coronary intervention (PCI) with a drug-eluting stent (DES)?
Background: The American College of Cardiology and the American Heart Association recently released an advisory that included a recommendation to delay elective noncardiac surgery (NCS) for one year after DES placement. However, no large study addresses the timing of NCS after PCI with DES.
Study design: Retrospective observational study.
Setting: Mayo Clinic, Rochester, Minn.
Synopsis: Looking at 520 patients who had NCS after DES at the Mayo Clinic, 5.4% experienced MACEs, but the rate of MACEs was not significantly associated with the time after stent placement to surgery (p=0.337). However, observed rates of MACEs were lower after one year. Elderly patients and those going for emergent surgery are at the highest risk for MACE. Bleeding complications were not associated with antiplatelet use.
Although this study does not provide a clear cutoff time for when it is safe to proceed to NCS after DES, it is somewhat reassuring to see the relatively small number of MACEs and the lack of bleeding complications associated with antiplatelet use. However, careful coordination between hospitalists, cardiologists, anesthesiologists, and surgeons is still needed when coordinating NCS after DES, especially in the elderly or during emergent situations.
Bottom line: While time to noncardiac surgery after drug-eluting stent placement is not associated with major adverse cardiac events, observed rates of events are lower after one year.
Citation: Rabbitts JA, Nuttall GA, Brown MJ, et al. Cardiac risk of non-cardiac surgery after percutaneous coronary intervention with drug-eluting stents. Anesthesiology.2008;109: 596-604.
Is the risk of MACEs and bleeding events for patients undergoing NCS related to the time interval between PCI with bare-metal stent?
Background: In order to prevent thrombosis of bare-metal stents (BMS) placed during percutaneous coronary intervention (PCI), antiplatelet therapy is used. This poses a risk of bleeding, if surgery is needed during the antiplatelet therapy. The American College of Cardiology and the American Heart Association recommends delaying NCS for at least six weeks after PCI with BMS.
Study design: Retrospective observational study.
Setting: Mayo Clinic, Rochester, Minn.
Synopsis: Looking at 899 patients who had NCS within one year of PCI with BMS at the Mayo Clinic between Jan. 1, 1990, and Jan. 1, 2005, this study found that when NCS was done 30 days or less after PCI with BMS, the MACEs rate was 10.5%, compared with 2.8% when NCS was done 91 or more days after PCI with BMS. After a multivariable analysis, it also was shown bleeding events were not associated with time between PCI with BMS and NCS.
While the American College of Cardiology and the American Heart Association recommends delaying NCS for at least six weeks after PCI with BMS, waiting at least 90 days would permit completion of antiplatelet therapy and re-endothelialization of the stent.
Bottom line: The risk of MACEs with noncardiac surgery is lowest when performed at least 90 days after PCI with bare-metal stent.
Citation: Nuttall GA, Brown MJ, Stombaugh JW, et al. Time and cardiac risk of surgery after bare-metal stent, percutaneous coronary intervention. Anesthesiology. 2008;109: 588-595.
Should we screen extensively for cancer in patients with newly diagnosed venous thromboembolism (VTE)?
Background: It is well known VTE can be the first manifestation of previously undiagnosed cancer. Retrospective studies have suggested “limited” cancer screening, including a history and physical examination, along with basic blood work, adequately identifies malignancy in patients with unexplained VTE. However, more recent prospective studies have suggested more extensive screening, which includes imaging studies or tumor-marker measurement, can increase the rate of cancer detection.
Study design: Systematic review.
Setting: Literature search using MEDLINE, EMBASE, the Cochrane Register of Controlled Trials, and evidence-based medicine reviews.
Synopsis: Thirty-six studies of 9,516 patients with VTE reported the period prevalence of previously undiagnosed cancer from baseline to 12 months was 6.3% (95% confidence interval (CI) of 5.6% to 6.9%) in all patients with VTE, and was even higher in patients with unprovoked VTE, 10% (95% CI 8.6% to 11.3%). Of the 34 articles used for prevalence assessment, an extensive screening strategy using CT scans of the abdomen and pelvis increased the proportion of previously undiagnosed cancer detection from 49.4% (CI, 40.2% to 58.5%; limited screening) to 69.7% (CI, 61.1% to 77.8%) in patients with unprovoked VTE. Ultrasonography of the abdomen and pelvis and tumor-marker screening did not result in a clinically significant increase in the frequency of cancer detection.
Four studies compared the rate of detection of early-stage, previously undiagnosed cancer between the limited and extensive screening strategies. Extensive screening led to an absolute decrease in cancer-related mortality of 1.9%, but this difference was not statistically significant.
In this systematic review, there is a great deal of heterogeneity in the studies. Most of the studies did not look at whether an increase in detection of new malignant conditions resulted in a change in the detection rate of early-stage cancer, or a decrease in cancer-related morbidity, cancer-related mortality, or overall mortality. Furthermore, the studies did not assess the consequences of extensive screening, such as patient anxiety and discomfort, testing complications, burden of additional tests for false-positive results, or cost-effectiveness. However, it is important for hospitalists to recognize undiagnosed cancer is common in unexplained VTE and warrants at least a limited-screening approach with more extensive screening.
Bottom line: Although the prevalence of undiagnosed cancer is common in VTE, extensive screening did not offer a cancer-related mortality benefit. CT of the abdomen and pelvis did, however, lead to a greater number of cancer diagnoses in patients with unexplained VTE.
Citation: Carrier M, Le Gal G, Wells PS, Fergusson D, Ramsay T, Rodger MA. Systematic review: the Trousseau syndrome revisited: should we screen extensively for cancer in patients with venous thromboembolism? Ann Intern Med. 2008;149: 323-333.
Does the use of preadmission statins decrease the risk of death, bacteremia, and pulmonary complications in patients admitted with pneumonia?
Background: Both experimental and clinical studies have suggested statins improve outcomes in severe infections, such as sepsis. This is thought to be due to the antithrombotic, anti-inflammatory, and immunomodulatory effects of statins. However, previous studies on the effect of statins on pneumonia have conflicting outcomes.
Study design: Population-based cohort study of 29,900 patients.
Setting: Danish Health Registry.
Synopsis: Researchers studied patients ages 15 years and older hospitalized with pneumonia for the first time between January 1997 and December 2004. While statin users had more co-morbidities than nonusers, the 30-day mortality was 10.3% in users, compared with 15.7% in nonusers, corresponding to an adjusted 30-day mortality rate ratio of 0.69 (95% CI of 0.58-0.82). The 90-day mortality ratio was 16.8% in users, compared with 22.4% in nonusers, corresponding to an adjusted 90-day mortality ratio of 0.75 (95% CI of 0.65-0.86). Former use of statins was not associated with a decreased risk of death. The adjusted risk for bacteremia and pulmonary complications was not significantly different between nonusers and users.
Because this was an observational study, a causal relationship cannot be determined. Hospitalists should be alerted to the possibility statins might, in the future, prove to be a standard treatment modality in pneumonia. A randomized, double-blind trial might help further determine the effect of the acute use of statins on pneumonia outcomes.
Bottom line: Preadmission statin use is associated with a decrease in 30- and 90-day mortality in pneumonia.
Citation: Thomsen RW, Riis A, Kornum JB, Christensen S, Johnsen SP, Sorensen HT. Preadmission use of statins and outcomes after hospitalization with pneumonia. Arch Intern Med. 2008;168(19):2081-2087.
Do outcomes differ when patients with acute myocardial infarction (MI) undergo PCI with drug-eluting stents (DES) compared with bare-metal stents?
Background: Randomized trials comparing drug-eluting stents with bare-metal stents in acute MI have been limited in size and duration. Concern exists regarding higher mortality among patients with ST-elevation MI treated with DES.
Study design: Observational, cohort study.
Setting: Patients were identified from a state-mandated database, in which all PCI performed in Massachusetts are reported.
Synopsis: Between April 2003 and September 2004, 7,217 eligible patients underwent stenting for acute MI. They were assigned to either the DES group or the bare-metal stent (BMS) group using propensity score matching. Patients in the DES group had lower mortality at two years, compared to a matched cohort of patients in the BMS group with MI (10.7% vs. 12.8%; absolute risk difference, -2.1%, CI, -3.8% to -0.4%). A statistically significant difference was noted among patients with or without ST-elevation MI.
The rates of target vessel revascularization at two years with MI were significantly lower among patients receiving DES than among those receiving BMS (9.6% vs. 14.5%; risk difference, -4.9%; CI, -6.1% to -3.1%).
The study is limited by its observational nature and residual confounding bias after matching. Importantly, this study was performed to determine if DESs were harmful, and the finding of reduced mortality was unanticipated.
Bottom line: Although patients with acute MI treated with drug-eluting stents had lower mortality and repeat revascularization rates compared with bare-metal stents, this outcome merits confirmation in randomized trials.
Citation: Mauri L, Silbaugh TS, Garg P, et al. Drug-eluting or bare-metal stents for acute myocardial infarction. N Engl J Med. 2008;359 (13):1330-1342.
In This Edition
- Perioperative smoking cessation reduces postoperative complications.
- Quality of life is not diminished in heart failure patients receiving defibrillator therapy.
- Simplification of the revised Geneva score may be useful in assessing for pulmonary embolism.
- Non-cardiac surgery after drug eluting stents not associated with major cardiac risk.
- Major cardiac risk is lowest 90 days after bare metal stent percutaneous coronary intervention.
- Extensive cancer screening in unexplained VTE detects more malignancies, but does not affect cancer related mortality.
- Preadmission use of statins decreases after hospitalization mortality in pneumonia.
- Drug-eluting stents are better than bare-metal stents for PCI in acute MI, but additional randomized study is needed.
Does a short duration of perioperative smoking cessation lead to a reduction in postoperative complications?
Background: Prior studies have demonstrated a reduction in postoperative complications when patients stop smoking in the perioperative period. However, they have not clearly shown what effect a fairly short duration of cessation, such as a period of only four weeks, has on the frequency of complications.
Study design: Randomized controlled trial.
Setting: Four university-affiliated hospitals in Sweden.
Synopsis: Using 117 patients who were daily smokers for less than one year between the ages of 18-79 who were scheduled for elective general or orthopedic surgery, this study showed that a smoking-cessation intervention initiated as little as four weeks prior to surgery resulted in fewer postoperative complications. The complication rate was reduced from 41% in the control group to 21% in the intervention group, which received cessation counseling and nicotine-replacement therapy. The relative risk reduction was 49% (95% confidence interval, 3-40) with a number needed to treat of five.
Because this was a randomized controlled trial with a large observed benefit, it appears to be reasonable to endorse perioperative smoking cessation as late as four weeks before an elective surgery. The study was limited in its ability to detect a difference in wound infections by the small sample size and the possibility patients might have unblinded themselves to outcome assessors, causing an overestimation of the effect of the intervention on the primary outcome of all complications.
Bottom line: Perioperative smoking cessation reduces postoperative complications even when started just four weeks prior to surgery.
Citation: Lindstrom D, Azodi OS, Wladis A, et al. Effects of a perioperative smoking cessation intervention on postoperative complications. Ann Surg. 2008;248(5):739-745.
Does implantable-defibrillator therapy cause deterioration in quality of life for patients with heart failure?
Background: Patients with depressed left-ventricular function are known to have improved survival after receiving implantable cardioverter defibrillators (ICDs). However, there is concern ICD therapy can prolong survival at the expense of a diminished quality of life.
Study design: Randomized placebo-controlled trial.
Setting: Multiple centers in the U.S., Canada, and New Zealand.
Synopsis: Using 2,479 patients from the Sudden Cardiac Death in Heart Failure trial who were 18 and older and had stable heart failure and depressed left-ventricular function, this study demonstrated no significant quality-of-life difference at 30 months when compared with patients who received ICD, amiodarone, and state-of-the-art medical therapy or an amiodarone placebo and state-of-the-art medical therapy. While functional status did not differ at any time between the three groups, psychological well-being was improved in the ICD group at three months (p=0.01) and 12 months (p=0.03) when compared with the placebo group, but at 30 months there was no difference between the groups.
While the trial was randomized and placebo-controlled, the investigators were unable to blind patients or outcome assessors. Nevertheless, the lack of deterioration of quality of life in ICD patients is reassuring.
Bottom line: Placement of ICDs in heart failure patients with a high risk of sudden cardiac death does not appear to decrease quality of life.
Citation: Mark DB, Anstrom KJ, Sun JL, et al. Quality of life with defibrillator therapy or amiodarone in heart failure. N Engl J Med. 2008;359:999-1008.
Can a simplified, revised Geneva score retain diagnostic accuracy and clinical utility?
Background: The revised Geneva score is a validated and objective clinical decision rule, but has multiple variables with different weights. This can make the tool cumbersome and difficult to remember, and could lead to inaccurate calculations and misjudgments in patient care.
Study design: Retrospective cohort study.
Setting: Four university-affiliated European hospitals.
Synopsis: Using data from two prior prospective trials involving patients with suspected pulmonary embolism (PE), this study showed re-analysis of these patients with a simplified, revised Geneva score, which gives only one point to each clinical factor, resulted in the same level of diagnostic accuracy. Specifically, data from 1,049 patients was used to construct a receiver-operating characteristic curve analysis comparing the standardized and simplified Geneva score, which showed areas under the curve of 0.75 (95% confidence interval 0.71-0.78) and 0.74 (0.70-0.77), respectively. Additionally, the safety of using this clinical tool to rule out PE was demonstrated when using both a three-level (low-intermediate probability) and a dichotomized scheme (PE unlikely) in combination with a negative D-dimer test.
The retrospective nature of the study was its major limitation. The authors suggest a prospective study to complete validation of the simplified, revised Geneva score.
Bottom line: With prospective analysis, it might be possible to further validate a simplified, revised Geneva score.
Citation: Klok FA, Mos ICM, Nijkeuter M, et al. Simplification of the revised Geneva score for assessing clinical probability of pulmonary embolism. Arch Intern Med. 2008;168(19):2131-2136.
Is the rate of postoperative major adverse cardiac events (MACEs) inversely related to time after percutaneous coronary intervention (PCI) with a drug-eluting stent (DES)?
Background: The American College of Cardiology and the American Heart Association recently released an advisory that included a recommendation to delay elective noncardiac surgery (NCS) for one year after DES placement. However, no large study addresses the timing of NCS after PCI with DES.
Study design: Retrospective observational study.
Setting: Mayo Clinic, Rochester, Minn.
Synopsis: Looking at 520 patients who had NCS after DES at the Mayo Clinic, 5.4% experienced MACEs, but the rate of MACEs was not significantly associated with the time after stent placement to surgery (p=0.337). However, observed rates of MACEs were lower after one year. Elderly patients and those going for emergent surgery are at the highest risk for MACE. Bleeding complications were not associated with antiplatelet use.
Although this study does not provide a clear cutoff time for when it is safe to proceed to NCS after DES, it is somewhat reassuring to see the relatively small number of MACEs and the lack of bleeding complications associated with antiplatelet use. However, careful coordination between hospitalists, cardiologists, anesthesiologists, and surgeons is still needed when coordinating NCS after DES, especially in the elderly or during emergent situations.
Bottom line: While time to noncardiac surgery after drug-eluting stent placement is not associated with major adverse cardiac events, observed rates of events are lower after one year.
Citation: Rabbitts JA, Nuttall GA, Brown MJ, et al. Cardiac risk of non-cardiac surgery after percutaneous coronary intervention with drug-eluting stents. Anesthesiology.2008;109: 596-604.
Is the risk of MACEs and bleeding events for patients undergoing NCS related to the time interval between PCI with bare-metal stent?
Background: In order to prevent thrombosis of bare-metal stents (BMS) placed during percutaneous coronary intervention (PCI), antiplatelet therapy is used. This poses a risk of bleeding, if surgery is needed during the antiplatelet therapy. The American College of Cardiology and the American Heart Association recommends delaying NCS for at least six weeks after PCI with BMS.
Study design: Retrospective observational study.
Setting: Mayo Clinic, Rochester, Minn.
Synopsis: Looking at 899 patients who had NCS within one year of PCI with BMS at the Mayo Clinic between Jan. 1, 1990, and Jan. 1, 2005, this study found that when NCS was done 30 days or less after PCI with BMS, the MACEs rate was 10.5%, compared with 2.8% when NCS was done 91 or more days after PCI with BMS. After a multivariable analysis, it also was shown bleeding events were not associated with time between PCI with BMS and NCS.
While the American College of Cardiology and the American Heart Association recommends delaying NCS for at least six weeks after PCI with BMS, waiting at least 90 days would permit completion of antiplatelet therapy and re-endothelialization of the stent.
Bottom line: The risk of MACEs with noncardiac surgery is lowest when performed at least 90 days after PCI with bare-metal stent.
Citation: Nuttall GA, Brown MJ, Stombaugh JW, et al. Time and cardiac risk of surgery after bare-metal stent, percutaneous coronary intervention. Anesthesiology. 2008;109: 588-595.
Should we screen extensively for cancer in patients with newly diagnosed venous thromboembolism (VTE)?
Background: It is well known VTE can be the first manifestation of previously undiagnosed cancer. Retrospective studies have suggested “limited” cancer screening, including a history and physical examination, along with basic blood work, adequately identifies malignancy in patients with unexplained VTE. However, more recent prospective studies have suggested more extensive screening, which includes imaging studies or tumor-marker measurement, can increase the rate of cancer detection.
Study design: Systematic review.
Setting: Literature search using MEDLINE, EMBASE, the Cochrane Register of Controlled Trials, and evidence-based medicine reviews.
Synopsis: Thirty-six studies of 9,516 patients with VTE reported the period prevalence of previously undiagnosed cancer from baseline to 12 months was 6.3% (95% confidence interval (CI) of 5.6% to 6.9%) in all patients with VTE, and was even higher in patients with unprovoked VTE, 10% (95% CI 8.6% to 11.3%). Of the 34 articles used for prevalence assessment, an extensive screening strategy using CT scans of the abdomen and pelvis increased the proportion of previously undiagnosed cancer detection from 49.4% (CI, 40.2% to 58.5%; limited screening) to 69.7% (CI, 61.1% to 77.8%) in patients with unprovoked VTE. Ultrasonography of the abdomen and pelvis and tumor-marker screening did not result in a clinically significant increase in the frequency of cancer detection.
Four studies compared the rate of detection of early-stage, previously undiagnosed cancer between the limited and extensive screening strategies. Extensive screening led to an absolute decrease in cancer-related mortality of 1.9%, but this difference was not statistically significant.
In this systematic review, there is a great deal of heterogeneity in the studies. Most of the studies did not look at whether an increase in detection of new malignant conditions resulted in a change in the detection rate of early-stage cancer, or a decrease in cancer-related morbidity, cancer-related mortality, or overall mortality. Furthermore, the studies did not assess the consequences of extensive screening, such as patient anxiety and discomfort, testing complications, burden of additional tests for false-positive results, or cost-effectiveness. However, it is important for hospitalists to recognize undiagnosed cancer is common in unexplained VTE and warrants at least a limited-screening approach with more extensive screening.
Bottom line: Although the prevalence of undiagnosed cancer is common in VTE, extensive screening did not offer a cancer-related mortality benefit. CT of the abdomen and pelvis did, however, lead to a greater number of cancer diagnoses in patients with unexplained VTE.
Citation: Carrier M, Le Gal G, Wells PS, Fergusson D, Ramsay T, Rodger MA. Systematic review: the Trousseau syndrome revisited: should we screen extensively for cancer in patients with venous thromboembolism? Ann Intern Med. 2008;149: 323-333.
Does the use of preadmission statins decrease the risk of death, bacteremia, and pulmonary complications in patients admitted with pneumonia?
Background: Both experimental and clinical studies have suggested statins improve outcomes in severe infections, such as sepsis. This is thought to be due to the antithrombotic, anti-inflammatory, and immunomodulatory effects of statins. However, previous studies on the effect of statins on pneumonia have conflicting outcomes.
Study design: Population-based cohort study of 29,900 patients.
Setting: Danish Health Registry.
Synopsis: Researchers studied patients ages 15 years and older hospitalized with pneumonia for the first time between January 1997 and December 2004. While statin users had more co-morbidities than nonusers, the 30-day mortality was 10.3% in users, compared with 15.7% in nonusers, corresponding to an adjusted 30-day mortality rate ratio of 0.69 (95% CI of 0.58-0.82). The 90-day mortality ratio was 16.8% in users, compared with 22.4% in nonusers, corresponding to an adjusted 90-day mortality ratio of 0.75 (95% CI of 0.65-0.86). Former use of statins was not associated with a decreased risk of death. The adjusted risk for bacteremia and pulmonary complications was not significantly different between nonusers and users.
Because this was an observational study, a causal relationship cannot be determined. Hospitalists should be alerted to the possibility statins might, in the future, prove to be a standard treatment modality in pneumonia. A randomized, double-blind trial might help further determine the effect of the acute use of statins on pneumonia outcomes.
Bottom line: Preadmission statin use is associated with a decrease in 30- and 90-day mortality in pneumonia.
Citation: Thomsen RW, Riis A, Kornum JB, Christensen S, Johnsen SP, Sorensen HT. Preadmission use of statins and outcomes after hospitalization with pneumonia. Arch Intern Med. 2008;168(19):2081-2087.
Do outcomes differ when patients with acute myocardial infarction (MI) undergo PCI with drug-eluting stents (DES) compared with bare-metal stents?
Background: Randomized trials comparing drug-eluting stents with bare-metal stents in acute MI have been limited in size and duration. Concern exists regarding higher mortality among patients with ST-elevation MI treated with DES.
Study design: Observational, cohort study.
Setting: Patients were identified from a state-mandated database, in which all PCI performed in Massachusetts are reported.
Synopsis: Between April 2003 and September 2004, 7,217 eligible patients underwent stenting for acute MI. They were assigned to either the DES group or the bare-metal stent (BMS) group using propensity score matching. Patients in the DES group had lower mortality at two years, compared to a matched cohort of patients in the BMS group with MI (10.7% vs. 12.8%; absolute risk difference, -2.1%, CI, -3.8% to -0.4%). A statistically significant difference was noted among patients with or without ST-elevation MI.
The rates of target vessel revascularization at two years with MI were significantly lower among patients receiving DES than among those receiving BMS (9.6% vs. 14.5%; risk difference, -4.9%; CI, -6.1% to -3.1%).
The study is limited by its observational nature and residual confounding bias after matching. Importantly, this study was performed to determine if DESs were harmful, and the finding of reduced mortality was unanticipated.
Bottom line: Although patients with acute MI treated with drug-eluting stents had lower mortality and repeat revascularization rates compared with bare-metal stents, this outcome merits confirmation in randomized trials.
Citation: Mauri L, Silbaugh TS, Garg P, et al. Drug-eluting or bare-metal stents for acute myocardial infarction. N Engl J Med. 2008;359 (13):1330-1342.
In This Edition
- Perioperative smoking cessation reduces postoperative complications.
- Quality of life is not diminished in heart failure patients receiving defibrillator therapy.
- Simplification of the revised Geneva score may be useful in assessing for pulmonary embolism.
- Non-cardiac surgery after drug eluting stents not associated with major cardiac risk.
- Major cardiac risk is lowest 90 days after bare metal stent percutaneous coronary intervention.
- Extensive cancer screening in unexplained VTE detects more malignancies, but does not affect cancer related mortality.
- Preadmission use of statins decreases after hospitalization mortality in pneumonia.
- Drug-eluting stents are better than bare-metal stents for PCI in acute MI, but additional randomized study is needed.
Does a short duration of perioperative smoking cessation lead to a reduction in postoperative complications?
Background: Prior studies have demonstrated a reduction in postoperative complications when patients stop smoking in the perioperative period. However, they have not clearly shown what effect a fairly short duration of cessation, such as a period of only four weeks, has on the frequency of complications.
Study design: Randomized controlled trial.
Setting: Four university-affiliated hospitals in Sweden.
Synopsis: Using 117 patients who were daily smokers for less than one year between the ages of 18-79 who were scheduled for elective general or orthopedic surgery, this study showed that a smoking-cessation intervention initiated as little as four weeks prior to surgery resulted in fewer postoperative complications. The complication rate was reduced from 41% in the control group to 21% in the intervention group, which received cessation counseling and nicotine-replacement therapy. The relative risk reduction was 49% (95% confidence interval, 3-40) with a number needed to treat of five.
Because this was a randomized controlled trial with a large observed benefit, it appears to be reasonable to endorse perioperative smoking cessation as late as four weeks before an elective surgery. The study was limited in its ability to detect a difference in wound infections by the small sample size and the possibility patients might have unblinded themselves to outcome assessors, causing an overestimation of the effect of the intervention on the primary outcome of all complications.
Bottom line: Perioperative smoking cessation reduces postoperative complications even when started just four weeks prior to surgery.
Citation: Lindstrom D, Azodi OS, Wladis A, et al. Effects of a perioperative smoking cessation intervention on postoperative complications. Ann Surg. 2008;248(5):739-745.
Does implantable-defibrillator therapy cause deterioration in quality of life for patients with heart failure?
Background: Patients with depressed left-ventricular function are known to have improved survival after receiving implantable cardioverter defibrillators (ICDs). However, there is concern ICD therapy can prolong survival at the expense of a diminished quality of life.
Study design: Randomized placebo-controlled trial.
Setting: Multiple centers in the U.S., Canada, and New Zealand.
Synopsis: Using 2,479 patients from the Sudden Cardiac Death in Heart Failure trial who were 18 and older and had stable heart failure and depressed left-ventricular function, this study demonstrated no significant quality-of-life difference at 30 months when compared with patients who received ICD, amiodarone, and state-of-the-art medical therapy or an amiodarone placebo and state-of-the-art medical therapy. While functional status did not differ at any time between the three groups, psychological well-being was improved in the ICD group at three months (p=0.01) and 12 months (p=0.03) when compared with the placebo group, but at 30 months there was no difference between the groups.
While the trial was randomized and placebo-controlled, the investigators were unable to blind patients or outcome assessors. Nevertheless, the lack of deterioration of quality of life in ICD patients is reassuring.
Bottom line: Placement of ICDs in heart failure patients with a high risk of sudden cardiac death does not appear to decrease quality of life.
Citation: Mark DB, Anstrom KJ, Sun JL, et al. Quality of life with defibrillator therapy or amiodarone in heart failure. N Engl J Med. 2008;359:999-1008.
Can a simplified, revised Geneva score retain diagnostic accuracy and clinical utility?
Background: The revised Geneva score is a validated and objective clinical decision rule, but has multiple variables with different weights. This can make the tool cumbersome and difficult to remember, and could lead to inaccurate calculations and misjudgments in patient care.
Study design: Retrospective cohort study.
Setting: Four university-affiliated European hospitals.
Synopsis: Using data from two prior prospective trials involving patients with suspected pulmonary embolism (PE), this study showed re-analysis of these patients with a simplified, revised Geneva score, which gives only one point to each clinical factor, resulted in the same level of diagnostic accuracy. Specifically, data from 1,049 patients was used to construct a receiver-operating characteristic curve analysis comparing the standardized and simplified Geneva score, which showed areas under the curve of 0.75 (95% confidence interval 0.71-0.78) and 0.74 (0.70-0.77), respectively. Additionally, the safety of using this clinical tool to rule out PE was demonstrated when using both a three-level (low-intermediate probability) and a dichotomized scheme (PE unlikely) in combination with a negative D-dimer test.
The retrospective nature of the study was its major limitation. The authors suggest a prospective study to complete validation of the simplified, revised Geneva score.
Bottom line: With prospective analysis, it might be possible to further validate a simplified, revised Geneva score.
Citation: Klok FA, Mos ICM, Nijkeuter M, et al. Simplification of the revised Geneva score for assessing clinical probability of pulmonary embolism. Arch Intern Med. 2008;168(19):2131-2136.
Is the rate of postoperative major adverse cardiac events (MACEs) inversely related to time after percutaneous coronary intervention (PCI) with a drug-eluting stent (DES)?
Background: The American College of Cardiology and the American Heart Association recently released an advisory that included a recommendation to delay elective noncardiac surgery (NCS) for one year after DES placement. However, no large study addresses the timing of NCS after PCI with DES.
Study design: Retrospective observational study.
Setting: Mayo Clinic, Rochester, Minn.
Synopsis: Looking at 520 patients who had NCS after DES at the Mayo Clinic, 5.4% experienced MACEs, but the rate of MACEs was not significantly associated with the time after stent placement to surgery (p=0.337). However, observed rates of MACEs were lower after one year. Elderly patients and those going for emergent surgery are at the highest risk for MACE. Bleeding complications were not associated with antiplatelet use.
Although this study does not provide a clear cutoff time for when it is safe to proceed to NCS after DES, it is somewhat reassuring to see the relatively small number of MACEs and the lack of bleeding complications associated with antiplatelet use. However, careful coordination between hospitalists, cardiologists, anesthesiologists, and surgeons is still needed when coordinating NCS after DES, especially in the elderly or during emergent situations.
Bottom line: While time to noncardiac surgery after drug-eluting stent placement is not associated with major adverse cardiac events, observed rates of events are lower after one year.
Citation: Rabbitts JA, Nuttall GA, Brown MJ, et al. Cardiac risk of non-cardiac surgery after percutaneous coronary intervention with drug-eluting stents. Anesthesiology.2008;109: 596-604.
Is the risk of MACEs and bleeding events for patients undergoing NCS related to the time interval between PCI with bare-metal stent?
Background: In order to prevent thrombosis of bare-metal stents (BMS) placed during percutaneous coronary intervention (PCI), antiplatelet therapy is used. This poses a risk of bleeding, if surgery is needed during the antiplatelet therapy. The American College of Cardiology and the American Heart Association recommends delaying NCS for at least six weeks after PCI with BMS.
Study design: Retrospective observational study.
Setting: Mayo Clinic, Rochester, Minn.
Synopsis: Looking at 899 patients who had NCS within one year of PCI with BMS at the Mayo Clinic between Jan. 1, 1990, and Jan. 1, 2005, this study found that when NCS was done 30 days or less after PCI with BMS, the MACEs rate was 10.5%, compared with 2.8% when NCS was done 91 or more days after PCI with BMS. After a multivariable analysis, it also was shown bleeding events were not associated with time between PCI with BMS and NCS.
While the American College of Cardiology and the American Heart Association recommends delaying NCS for at least six weeks after PCI with BMS, waiting at least 90 days would permit completion of antiplatelet therapy and re-endothelialization of the stent.
Bottom line: The risk of MACEs with noncardiac surgery is lowest when performed at least 90 days after PCI with bare-metal stent.
Citation: Nuttall GA, Brown MJ, Stombaugh JW, et al. Time and cardiac risk of surgery after bare-metal stent, percutaneous coronary intervention. Anesthesiology. 2008;109: 588-595.
Should we screen extensively for cancer in patients with newly diagnosed venous thromboembolism (VTE)?
Background: It is well known VTE can be the first manifestation of previously undiagnosed cancer. Retrospective studies have suggested “limited” cancer screening, including a history and physical examination, along with basic blood work, adequately identifies malignancy in patients with unexplained VTE. However, more recent prospective studies have suggested more extensive screening, which includes imaging studies or tumor-marker measurement, can increase the rate of cancer detection.
Study design: Systematic review.
Setting: Literature search using MEDLINE, EMBASE, the Cochrane Register of Controlled Trials, and evidence-based medicine reviews.
Synopsis: Thirty-six studies of 9,516 patients with VTE reported the period prevalence of previously undiagnosed cancer from baseline to 12 months was 6.3% (95% confidence interval (CI) of 5.6% to 6.9%) in all patients with VTE, and was even higher in patients with unprovoked VTE, 10% (95% CI 8.6% to 11.3%). Of the 34 articles used for prevalence assessment, an extensive screening strategy using CT scans of the abdomen and pelvis increased the proportion of previously undiagnosed cancer detection from 49.4% (CI, 40.2% to 58.5%; limited screening) to 69.7% (CI, 61.1% to 77.8%) in patients with unprovoked VTE. Ultrasonography of the abdomen and pelvis and tumor-marker screening did not result in a clinically significant increase in the frequency of cancer detection.
Four studies compared the rate of detection of early-stage, previously undiagnosed cancer between the limited and extensive screening strategies. Extensive screening led to an absolute decrease in cancer-related mortality of 1.9%, but this difference was not statistically significant.
In this systematic review, there is a great deal of heterogeneity in the studies. Most of the studies did not look at whether an increase in detection of new malignant conditions resulted in a change in the detection rate of early-stage cancer, or a decrease in cancer-related morbidity, cancer-related mortality, or overall mortality. Furthermore, the studies did not assess the consequences of extensive screening, such as patient anxiety and discomfort, testing complications, burden of additional tests for false-positive results, or cost-effectiveness. However, it is important for hospitalists to recognize undiagnosed cancer is common in unexplained VTE and warrants at least a limited-screening approach with more extensive screening.
Bottom line: Although the prevalence of undiagnosed cancer is common in VTE, extensive screening did not offer a cancer-related mortality benefit. CT of the abdomen and pelvis did, however, lead to a greater number of cancer diagnoses in patients with unexplained VTE.
Citation: Carrier M, Le Gal G, Wells PS, Fergusson D, Ramsay T, Rodger MA. Systematic review: the Trousseau syndrome revisited: should we screen extensively for cancer in patients with venous thromboembolism? Ann Intern Med. 2008;149: 323-333.
Does the use of preadmission statins decrease the risk of death, bacteremia, and pulmonary complications in patients admitted with pneumonia?
Background: Both experimental and clinical studies have suggested statins improve outcomes in severe infections, such as sepsis. This is thought to be due to the antithrombotic, anti-inflammatory, and immunomodulatory effects of statins. However, previous studies on the effect of statins on pneumonia have conflicting outcomes.
Study design: Population-based cohort study of 29,900 patients.
Setting: Danish Health Registry.
Synopsis: Researchers studied patients ages 15 years and older hospitalized with pneumonia for the first time between January 1997 and December 2004. While statin users had more co-morbidities than nonusers, the 30-day mortality was 10.3% in users, compared with 15.7% in nonusers, corresponding to an adjusted 30-day mortality rate ratio of 0.69 (95% CI of 0.58-0.82). The 90-day mortality ratio was 16.8% in users, compared with 22.4% in nonusers, corresponding to an adjusted 90-day mortality ratio of 0.75 (95% CI of 0.65-0.86). Former use of statins was not associated with a decreased risk of death. The adjusted risk for bacteremia and pulmonary complications was not significantly different between nonusers and users.
Because this was an observational study, a causal relationship cannot be determined. Hospitalists should be alerted to the possibility statins might, in the future, prove to be a standard treatment modality in pneumonia. A randomized, double-blind trial might help further determine the effect of the acute use of statins on pneumonia outcomes.
Bottom line: Preadmission statin use is associated with a decrease in 30- and 90-day mortality in pneumonia.
Citation: Thomsen RW, Riis A, Kornum JB, Christensen S, Johnsen SP, Sorensen HT. Preadmission use of statins and outcomes after hospitalization with pneumonia. Arch Intern Med. 2008;168(19):2081-2087.
Do outcomes differ when patients with acute myocardial infarction (MI) undergo PCI with drug-eluting stents (DES) compared with bare-metal stents?
Background: Randomized trials comparing drug-eluting stents with bare-metal stents in acute MI have been limited in size and duration. Concern exists regarding higher mortality among patients with ST-elevation MI treated with DES.
Study design: Observational, cohort study.
Setting: Patients were identified from a state-mandated database, in which all PCI performed in Massachusetts are reported.
Synopsis: Between April 2003 and September 2004, 7,217 eligible patients underwent stenting for acute MI. They were assigned to either the DES group or the bare-metal stent (BMS) group using propensity score matching. Patients in the DES group had lower mortality at two years, compared to a matched cohort of patients in the BMS group with MI (10.7% vs. 12.8%; absolute risk difference, -2.1%, CI, -3.8% to -0.4%). A statistically significant difference was noted among patients with or without ST-elevation MI.
The rates of target vessel revascularization at two years with MI were significantly lower among patients receiving DES than among those receiving BMS (9.6% vs. 14.5%; risk difference, -4.9%; CI, -6.1% to -3.1%).
The study is limited by its observational nature and residual confounding bias after matching. Importantly, this study was performed to determine if DESs were harmful, and the finding of reduced mortality was unanticipated.
Bottom line: Although patients with acute MI treated with drug-eluting stents had lower mortality and repeat revascularization rates compared with bare-metal stents, this outcome merits confirmation in randomized trials.
Citation: Mauri L, Silbaugh TS, Garg P, et al. Drug-eluting or bare-metal stents for acute myocardial infarction. N Engl J Med. 2008;359 (13):1330-1342.
Rapid Response: A QI Conundrum
Many in‐hospital cardiac arrests and other adverse events are heralded by warning signs that are evident in the preceding 6 to 8 hours.1 By promptly intervening before further deterioration occurs, rapid response teams (RRTs) are designed to decrease unexpected intensive care unit (ICU) transfers, cardiac arrests, and inpatient mortality. While implementing RRTs is 1 of the 6 initiatives recommended by the Institute for Healthcare Improvement,2 data supporting their effectiveness is equivocal.3, 4
In October 2006, at Denver Health Medical Center, an academic, safety net hospital, we initiated a rapid response systemclinical triggers program (RRS‐CTP).5 In our RRS‐CTP, an abrupt change in patient status (Figure 1) triggers a mandatory call by the patient's nurse to the primary team, which is then required to perform an immediate bedside evaluation. By incorporating the primary team into the RRT‐CTP, we sought to preserve as much continuity of care as possible. Also, since the same house staff compose our cardiopulmonary arrest or cor team, and staff the ICUs and non‐ICU hospital wards, we did not feel that creating a separate RRT was an efficient use of resources. Our nurses have undergone extensive education about the necessity of a prompt bedside evaluation and have been instructed and empowered to escalate concerns to senior physicians if needed. We present a case that illustrates challenges to both implementing an RRS and measuring its potential benefits.
Case
A 59‐year‐old woman with a history of bipolar mood disorder was admitted for altered mental status. At presentation, she had signs of acute mania with normal vital signs. After initial laboratory workup, her altered mental status was felt to be multifactorial due to urinary tract infection, hypernatremia (attributed to lithium‐induced nephrogenic diabetes insipidus), and acute mania (attributed to medication discontinuation). Because she was slow to recover from the acute mania, her hospital stay was prolonged. From admission, the patient was treated with heparin 5000 units subcutaneously twice daily for venous thromboembolism prophylaxis.
On hospital day 7, at 21:32, the patient was noted to have asymptomatic tachycardia at 149 beats per minute and a new oxygen requirement of 3 L/minute. The cross‐cover team was called; however, although criteria were met, the RRS‐CTP was not activated and a bedside evaluation was not performed. A chest X‐ray was found to be normal and, with the exception of the oxygen requirement, her vital signs normalized by 23:45. No further diagnostic testing was performed at the time.
The next morning, at 11:58, the patient was found to have a blood pressure of 60/40 mmHg and heart rate of 42 beats per minute. The RRS‐CTP was activated. The primary team arrived at the bedside at 12:00 and found the patient to be alert, oriented, and without complaints. Her respiratory rate was 30/minute, and her oxygen saturation was 86% on 3 L/minute. An arterial blood gas analysis demonstrated acute respiratory alkalosis with hypoxemia and an electrocardiogram showed sinus tachycardia with a new S1Q3T3 pattern. A computed tomography angiogram revealed a large, nearly occlusive pulmonary embolus (PE) filling an enlarged right pulmonary artery, as well as thrombus within the left main pulmonary artery. She was transferred to the medical ICU and alteplase was administered. The patient survived and was discharged in good clinical condition.
Discussion
Despite the strong theoretical benefit of the RRT concept, a recent review by Ranji et al.4 concluded that RRTs had not yet been shown to improve patient outcomes. In contrast to dedicated RRTs, this case illustrates a different type of RRS that was designed to address abrupt changes in patient status, while maintaining continuity of care and efficiently utilizing resources.
If one considers an RRS to have both afferent (criteria recognition) and efferent (RRT or primary team response) limbs, the afferent limb must be consistently activated in order to obtain the efferent limb's response.6 The greatest opportunities to improve RRSs are thought to lie in the afferent limb.3 Our RRS‐CTP was not triggered in 1 of 2 instances in which criteria for mandatory initiation of the system were met. This is consistent with the findings of the Medical Early Response Intervention and Therapy (MERIT) trial, in which RRTs were called in only 41% of the patients meeting criteria and subsequently having adverse events,7 and with the ongoing monitoring of the use of the system at our hospital. Had the cross‐covering team seen the patient at the bedside initially, the PE might have been diagnosed while the patient was hemodynamically stable, giving the patient nearly a 3‐fold lower relative mortality.8 When the RRS‐CTP was activated, a prompt bedside evaluation occurred, allowing for lytic therapy to be administered before cardiopulmonary arrest (attendant mortality of 90%).9
While rapid response criteria were originally based upon published sensitivity analyses, more recent studies suggest that these criteria lack diagnostic accuracy. As demonstrated by Cretikos et al,10 to reach a sensitivity of 70%, the corresponding specificity would be only 86%. Given that the prevalence of adverse events in the MERIT trial was only 0.6%, the resulting positive predictive value (PPV) of rapid response call criteria is 3%. Accordingly, 33 calls would be needed to prevent 1 unplanned ICU transfer, cardiac arrest, or death. Nurses' attempts to minimize false‐positive calls may help explain the low call rates for patients meeting RRT criteria. The 2 avenues to increase the PPV of criteria are:
-
Increase the prevalence of disease in the population screened by risk factor stratification.
-
Increase the specificity of the call criteria, which has been limited by the associated decrease in sensitivity.10
Regarding the efferent response limb of RRS, our case demonstrates that the primary team (rather than a separate group of caregivers), when alerted appropriately, can effectively respond to critical changes in patient status. Accordingly, our data show that since the inception of the program, cardiopulmonary arrests have decreased from a mean of 4.1 per month to 2.3 per month (P = 0.03).
Many clinical trials of RRTs would not capture the success demonstrated in this case. For example, due to the low prevalence of events, the MERIT trial used a composite endpoint that included unplanned ICU transfers, cardiac arrests, and mortality. Because our patient still required an unplanned ICU transfer after being evaluated by the responding team, she would have been counted as a system failure.
Conclusion
While local needs should inform the type of RRS implemented, this case illustrates one of the major obstacles ubiquitous to RRS implementation: failure of system activation. With appropriate activation, an RRS‐CTP can meet RRS goals while maintaining continuity of care and maximizing existing resources. This case also illustrates the difficulty of achieving a statistically relevant outcome, while demonstrating the potential benefits of evolving RRSs.
- ,,,,.Rapid response teams—do they make a difference.Dimens Crit Care Nurs.2007;26(6):253–260.
- Institute for Healthcare Improvement. 5 Million Lives Campaign. Available at: http://www.ihi.org/IHI/Programs/Campaign/Campaign.htm?TabId=1IHI. Accessed February2009.
- .The rapid response team paradox: why doesn't anyone call for help?Crit Care Med.2008;36(2):634–636.
- ,,,,.Effects of rapid response systems on clinical outcomes: review and meta‐analyses.J Hosp Med.2007;2:422–432.
- ,,.Clinical triggers and rapid response escalation criteria.Patient Saf Qual Healthc.2007;4(2):12–13. Available at: http://www.psqh.com/archives.html. Accessed February 2009.
- ,,, et al.Use of medical emergency team responses to reduce hospital cardiopulmonary arrest.Qual Saf Health Care.2004;13:251–254.
- MERIT Study Investigators.Introduction of the medical emergency team (MET) system: a cluster‐randomised controlled trial.Lancet.2005;365:2091–2097.
- ,,.Acute pulmonary embolism: clinical outcomes in the international cooperative pulmonary embolism registry (ICOPER).Lancet.1999;353(9162):1386–1389.
- ,,,.Early predictors of mortality for hospitalized patients suffering cardiopulmonary arrest.Chest.1990;97(2):413–419.
- ,,,,,.The objective medical emergency team activation criteria: a case–control study.Resuscitation.2007;73:62–72.
Many in‐hospital cardiac arrests and other adverse events are heralded by warning signs that are evident in the preceding 6 to 8 hours.1 By promptly intervening before further deterioration occurs, rapid response teams (RRTs) are designed to decrease unexpected intensive care unit (ICU) transfers, cardiac arrests, and inpatient mortality. While implementing RRTs is 1 of the 6 initiatives recommended by the Institute for Healthcare Improvement,2 data supporting their effectiveness is equivocal.3, 4
In October 2006, at Denver Health Medical Center, an academic, safety net hospital, we initiated a rapid response systemclinical triggers program (RRS‐CTP).5 In our RRS‐CTP, an abrupt change in patient status (Figure 1) triggers a mandatory call by the patient's nurse to the primary team, which is then required to perform an immediate bedside evaluation. By incorporating the primary team into the RRT‐CTP, we sought to preserve as much continuity of care as possible. Also, since the same house staff compose our cardiopulmonary arrest or cor team, and staff the ICUs and non‐ICU hospital wards, we did not feel that creating a separate RRT was an efficient use of resources. Our nurses have undergone extensive education about the necessity of a prompt bedside evaluation and have been instructed and empowered to escalate concerns to senior physicians if needed. We present a case that illustrates challenges to both implementing an RRS and measuring its potential benefits.
Case
A 59‐year‐old woman with a history of bipolar mood disorder was admitted for altered mental status. At presentation, she had signs of acute mania with normal vital signs. After initial laboratory workup, her altered mental status was felt to be multifactorial due to urinary tract infection, hypernatremia (attributed to lithium‐induced nephrogenic diabetes insipidus), and acute mania (attributed to medication discontinuation). Because she was slow to recover from the acute mania, her hospital stay was prolonged. From admission, the patient was treated with heparin 5000 units subcutaneously twice daily for venous thromboembolism prophylaxis.
On hospital day 7, at 21:32, the patient was noted to have asymptomatic tachycardia at 149 beats per minute and a new oxygen requirement of 3 L/minute. The cross‐cover team was called; however, although criteria were met, the RRS‐CTP was not activated and a bedside evaluation was not performed. A chest X‐ray was found to be normal and, with the exception of the oxygen requirement, her vital signs normalized by 23:45. No further diagnostic testing was performed at the time.
The next morning, at 11:58, the patient was found to have a blood pressure of 60/40 mmHg and heart rate of 42 beats per minute. The RRS‐CTP was activated. The primary team arrived at the bedside at 12:00 and found the patient to be alert, oriented, and without complaints. Her respiratory rate was 30/minute, and her oxygen saturation was 86% on 3 L/minute. An arterial blood gas analysis demonstrated acute respiratory alkalosis with hypoxemia and an electrocardiogram showed sinus tachycardia with a new S1Q3T3 pattern. A computed tomography angiogram revealed a large, nearly occlusive pulmonary embolus (PE) filling an enlarged right pulmonary artery, as well as thrombus within the left main pulmonary artery. She was transferred to the medical ICU and alteplase was administered. The patient survived and was discharged in good clinical condition.
Discussion
Despite the strong theoretical benefit of the RRT concept, a recent review by Ranji et al.4 concluded that RRTs had not yet been shown to improve patient outcomes. In contrast to dedicated RRTs, this case illustrates a different type of RRS that was designed to address abrupt changes in patient status, while maintaining continuity of care and efficiently utilizing resources.
If one considers an RRS to have both afferent (criteria recognition) and efferent (RRT or primary team response) limbs, the afferent limb must be consistently activated in order to obtain the efferent limb's response.6 The greatest opportunities to improve RRSs are thought to lie in the afferent limb.3 Our RRS‐CTP was not triggered in 1 of 2 instances in which criteria for mandatory initiation of the system were met. This is consistent with the findings of the Medical Early Response Intervention and Therapy (MERIT) trial, in which RRTs were called in only 41% of the patients meeting criteria and subsequently having adverse events,7 and with the ongoing monitoring of the use of the system at our hospital. Had the cross‐covering team seen the patient at the bedside initially, the PE might have been diagnosed while the patient was hemodynamically stable, giving the patient nearly a 3‐fold lower relative mortality.8 When the RRS‐CTP was activated, a prompt bedside evaluation occurred, allowing for lytic therapy to be administered before cardiopulmonary arrest (attendant mortality of 90%).9
While rapid response criteria were originally based upon published sensitivity analyses, more recent studies suggest that these criteria lack diagnostic accuracy. As demonstrated by Cretikos et al,10 to reach a sensitivity of 70%, the corresponding specificity would be only 86%. Given that the prevalence of adverse events in the MERIT trial was only 0.6%, the resulting positive predictive value (PPV) of rapid response call criteria is 3%. Accordingly, 33 calls would be needed to prevent 1 unplanned ICU transfer, cardiac arrest, or death. Nurses' attempts to minimize false‐positive calls may help explain the low call rates for patients meeting RRT criteria. The 2 avenues to increase the PPV of criteria are:
-
Increase the prevalence of disease in the population screened by risk factor stratification.
-
Increase the specificity of the call criteria, which has been limited by the associated decrease in sensitivity.10
Regarding the efferent response limb of RRS, our case demonstrates that the primary team (rather than a separate group of caregivers), when alerted appropriately, can effectively respond to critical changes in patient status. Accordingly, our data show that since the inception of the program, cardiopulmonary arrests have decreased from a mean of 4.1 per month to 2.3 per month (P = 0.03).
Many clinical trials of RRTs would not capture the success demonstrated in this case. For example, due to the low prevalence of events, the MERIT trial used a composite endpoint that included unplanned ICU transfers, cardiac arrests, and mortality. Because our patient still required an unplanned ICU transfer after being evaluated by the responding team, she would have been counted as a system failure.
Conclusion
While local needs should inform the type of RRS implemented, this case illustrates one of the major obstacles ubiquitous to RRS implementation: failure of system activation. With appropriate activation, an RRS‐CTP can meet RRS goals while maintaining continuity of care and maximizing existing resources. This case also illustrates the difficulty of achieving a statistically relevant outcome, while demonstrating the potential benefits of evolving RRSs.
Many in‐hospital cardiac arrests and other adverse events are heralded by warning signs that are evident in the preceding 6 to 8 hours.1 By promptly intervening before further deterioration occurs, rapid response teams (RRTs) are designed to decrease unexpected intensive care unit (ICU) transfers, cardiac arrests, and inpatient mortality. While implementing RRTs is 1 of the 6 initiatives recommended by the Institute for Healthcare Improvement,2 data supporting their effectiveness is equivocal.3, 4
In October 2006, at Denver Health Medical Center, an academic, safety net hospital, we initiated a rapid response systemclinical triggers program (RRS‐CTP).5 In our RRS‐CTP, an abrupt change in patient status (Figure 1) triggers a mandatory call by the patient's nurse to the primary team, which is then required to perform an immediate bedside evaluation. By incorporating the primary team into the RRT‐CTP, we sought to preserve as much continuity of care as possible. Also, since the same house staff compose our cardiopulmonary arrest or cor team, and staff the ICUs and non‐ICU hospital wards, we did not feel that creating a separate RRT was an efficient use of resources. Our nurses have undergone extensive education about the necessity of a prompt bedside evaluation and have been instructed and empowered to escalate concerns to senior physicians if needed. We present a case that illustrates challenges to both implementing an RRS and measuring its potential benefits.
Case
A 59‐year‐old woman with a history of bipolar mood disorder was admitted for altered mental status. At presentation, she had signs of acute mania with normal vital signs. After initial laboratory workup, her altered mental status was felt to be multifactorial due to urinary tract infection, hypernatremia (attributed to lithium‐induced nephrogenic diabetes insipidus), and acute mania (attributed to medication discontinuation). Because she was slow to recover from the acute mania, her hospital stay was prolonged. From admission, the patient was treated with heparin 5000 units subcutaneously twice daily for venous thromboembolism prophylaxis.
On hospital day 7, at 21:32, the patient was noted to have asymptomatic tachycardia at 149 beats per minute and a new oxygen requirement of 3 L/minute. The cross‐cover team was called; however, although criteria were met, the RRS‐CTP was not activated and a bedside evaluation was not performed. A chest X‐ray was found to be normal and, with the exception of the oxygen requirement, her vital signs normalized by 23:45. No further diagnostic testing was performed at the time.
The next morning, at 11:58, the patient was found to have a blood pressure of 60/40 mmHg and heart rate of 42 beats per minute. The RRS‐CTP was activated. The primary team arrived at the bedside at 12:00 and found the patient to be alert, oriented, and without complaints. Her respiratory rate was 30/minute, and her oxygen saturation was 86% on 3 L/minute. An arterial blood gas analysis demonstrated acute respiratory alkalosis with hypoxemia and an electrocardiogram showed sinus tachycardia with a new S1Q3T3 pattern. A computed tomography angiogram revealed a large, nearly occlusive pulmonary embolus (PE) filling an enlarged right pulmonary artery, as well as thrombus within the left main pulmonary artery. She was transferred to the medical ICU and alteplase was administered. The patient survived and was discharged in good clinical condition.
Discussion
Despite the strong theoretical benefit of the RRT concept, a recent review by Ranji et al.4 concluded that RRTs had not yet been shown to improve patient outcomes. In contrast to dedicated RRTs, this case illustrates a different type of RRS that was designed to address abrupt changes in patient status, while maintaining continuity of care and efficiently utilizing resources.
If one considers an RRS to have both afferent (criteria recognition) and efferent (RRT or primary team response) limbs, the afferent limb must be consistently activated in order to obtain the efferent limb's response.6 The greatest opportunities to improve RRSs are thought to lie in the afferent limb.3 Our RRS‐CTP was not triggered in 1 of 2 instances in which criteria for mandatory initiation of the system were met. This is consistent with the findings of the Medical Early Response Intervention and Therapy (MERIT) trial, in which RRTs were called in only 41% of the patients meeting criteria and subsequently having adverse events,7 and with the ongoing monitoring of the use of the system at our hospital. Had the cross‐covering team seen the patient at the bedside initially, the PE might have been diagnosed while the patient was hemodynamically stable, giving the patient nearly a 3‐fold lower relative mortality.8 When the RRS‐CTP was activated, a prompt bedside evaluation occurred, allowing for lytic therapy to be administered before cardiopulmonary arrest (attendant mortality of 90%).9
While rapid response criteria were originally based upon published sensitivity analyses, more recent studies suggest that these criteria lack diagnostic accuracy. As demonstrated by Cretikos et al,10 to reach a sensitivity of 70%, the corresponding specificity would be only 86%. Given that the prevalence of adverse events in the MERIT trial was only 0.6%, the resulting positive predictive value (PPV) of rapid response call criteria is 3%. Accordingly, 33 calls would be needed to prevent 1 unplanned ICU transfer, cardiac arrest, or death. Nurses' attempts to minimize false‐positive calls may help explain the low call rates for patients meeting RRT criteria. The 2 avenues to increase the PPV of criteria are:
-
Increase the prevalence of disease in the population screened by risk factor stratification.
-
Increase the specificity of the call criteria, which has been limited by the associated decrease in sensitivity.10
Regarding the efferent response limb of RRS, our case demonstrates that the primary team (rather than a separate group of caregivers), when alerted appropriately, can effectively respond to critical changes in patient status. Accordingly, our data show that since the inception of the program, cardiopulmonary arrests have decreased from a mean of 4.1 per month to 2.3 per month (P = 0.03).
Many clinical trials of RRTs would not capture the success demonstrated in this case. For example, due to the low prevalence of events, the MERIT trial used a composite endpoint that included unplanned ICU transfers, cardiac arrests, and mortality. Because our patient still required an unplanned ICU transfer after being evaluated by the responding team, she would have been counted as a system failure.
Conclusion
While local needs should inform the type of RRS implemented, this case illustrates one of the major obstacles ubiquitous to RRS implementation: failure of system activation. With appropriate activation, an RRS‐CTP can meet RRS goals while maintaining continuity of care and maximizing existing resources. This case also illustrates the difficulty of achieving a statistically relevant outcome, while demonstrating the potential benefits of evolving RRSs.
- ,,,,.Rapid response teams—do they make a difference.Dimens Crit Care Nurs.2007;26(6):253–260.
- Institute for Healthcare Improvement. 5 Million Lives Campaign. Available at: http://www.ihi.org/IHI/Programs/Campaign/Campaign.htm?TabId=1IHI. Accessed February2009.
- .The rapid response team paradox: why doesn't anyone call for help?Crit Care Med.2008;36(2):634–636.
- ,,,,.Effects of rapid response systems on clinical outcomes: review and meta‐analyses.J Hosp Med.2007;2:422–432.
- ,,.Clinical triggers and rapid response escalation criteria.Patient Saf Qual Healthc.2007;4(2):12–13. Available at: http://www.psqh.com/archives.html. Accessed February 2009.
- ,,, et al.Use of medical emergency team responses to reduce hospital cardiopulmonary arrest.Qual Saf Health Care.2004;13:251–254.
- MERIT Study Investigators.Introduction of the medical emergency team (MET) system: a cluster‐randomised controlled trial.Lancet.2005;365:2091–2097.
- ,,.Acute pulmonary embolism: clinical outcomes in the international cooperative pulmonary embolism registry (ICOPER).Lancet.1999;353(9162):1386–1389.
- ,,,.Early predictors of mortality for hospitalized patients suffering cardiopulmonary arrest.Chest.1990;97(2):413–419.
- ,,,,,.The objective medical emergency team activation criteria: a case–control study.Resuscitation.2007;73:62–72.
- ,,,,.Rapid response teams—do they make a difference.Dimens Crit Care Nurs.2007;26(6):253–260.
- Institute for Healthcare Improvement. 5 Million Lives Campaign. Available at: http://www.ihi.org/IHI/Programs/Campaign/Campaign.htm?TabId=1IHI. Accessed February2009.
- .The rapid response team paradox: why doesn't anyone call for help?Crit Care Med.2008;36(2):634–636.
- ,,,,.Effects of rapid response systems on clinical outcomes: review and meta‐analyses.J Hosp Med.2007;2:422–432.
- ,,.Clinical triggers and rapid response escalation criteria.Patient Saf Qual Healthc.2007;4(2):12–13. Available at: http://www.psqh.com/archives.html. Accessed February 2009.
- ,,, et al.Use of medical emergency team responses to reduce hospital cardiopulmonary arrest.Qual Saf Health Care.2004;13:251–254.
- MERIT Study Investigators.Introduction of the medical emergency team (MET) system: a cluster‐randomised controlled trial.Lancet.2005;365:2091–2097.
- ,,.Acute pulmonary embolism: clinical outcomes in the international cooperative pulmonary embolism registry (ICOPER).Lancet.1999;353(9162):1386–1389.
- ,,,.Early predictors of mortality for hospitalized patients suffering cardiopulmonary arrest.Chest.1990;97(2):413–419.
- ,,,,,.The objective medical emergency team activation criteria: a case–control study.Resuscitation.2007;73:62–72.
Time for Health Education of Hospitalized Patients
Educating patients about smoking cessation when they are hospitalized for acute coronary syndrome results in a 57% 1‐year quit rate.1 This rate is far higher than the typical 15%‐30% 1‐year quit rates observed with smoking cessation programs administered in the outpatient setting24 and suggests that hospitalized patients may be uniquely motivated to respond to health education.
Kerzman and colleagues5 found that 42% of hospitalized patients expressed a wish to receive more comprehensive counseling about their medications before being discharged from the hospital. And although the Joint Commission on Hospital Accreditation and the Centers for Medicare and Medicaid Services have established core quality measures mandating that patients hospitalized with congestive heart failure receive education as one component of a high‐quality discharge process,6, 7 approximately one third of patients nationally do not receive adequate patient education.8
Barber‐Parker9 suggested that because patient acuity in hospitals was so high and patients were so commonly absent from their nursing units for testing and treatment, there was little time available for health education during their hospitalization. Anecdotal observations in our institution suggested, however, that adult patients hospitalized on the general Internal Medicine service spent much of their day doing little more than lying in bed watching television. Accordingly, we hypothesized that considerable time might be available for patient education during a hospitalization. We therefore sought to quantify the fraction of time patients were not involved in treatment activities, diagnostic testing, or other evaluations and to determine whether during these times they wanted and were feeling well enough to participate in educational activities. We also sought to determine what patients wanted to know about their health problems and what types of educational activities they most preferred.
MATERIALS AND METHODS
We conducted a time‐motion and survey study from June 25, 2005, to August 15, 2005, at Denver Health Medical Center, an academic public safety‐net hospital affiliated with the University of Colorado School of Medicine. All patients older than 18 years of age who spoke English or Spanish and were admitted to the general Internal Medicine service were candidates for enrollment. Exclusion criteria were being admitted to the intensive care unit, having an inability to communicate, being in contact precautions, and being previously enrolled. The study was approved by the Colorado Multiple Institutional Review Board. Written informed consent was obtained for all study participants.
At 8:00 AM, all patients admitted during the previous 15 hours were assigned a random number from a random number table and were approached for consent in numeric order. With 2 data collectors working daily, a maximum of 12 patients could be enrolled each day. Consenting subjects who passed a vision test were given the Test of Functional Health Literacy in Adults at the time of enrollment and a written questionnaire (in either English or Spanish) on a daily basis for a maximum of 6 days. Some of these patients also participated in a structured interview that was designed to elicit their views on health education topics and formats for education of hospitalized patients. Others, again determined by random number, were subjects of a time‐motion study.
Demographic data collected included age, sex, language, race, comorbidities, insurance status, and discharge diagnosis.
Time‐Motion Study
Patients were observed from 8:00 AM to noon and from 1:00 to 5:00 PM7 days a week. Data were collected using TimerPro on a Dell Axim A5 pocket PC and imported daily into an Excel spreadsheet. Observations were categorized as downtime, busy time, or provider time and subcategorized as summarized in Table 1.
| First level | Second level | Third level |
|---|---|---|
| Downtime | Alone | TV |
| Resting | ||
| Sleeping | ||
| Reading | ||
| Telephone | ||
| Other | ||
| Friends/family | TV | |
| Resting | ||
| Sleeping | ||
| Reading | ||
| Telephone/talk | ||
| Other | ||
| Provider | Physician | |
| Nurse | ||
| Physician and nurse | ||
| Physician and other | ||
| Other | ||
| Busy | ADL | |
| Meal | ||
| Out of room | ||
| Other |
Questionnaire
We were unable to find a validated questionnaire in the literature that was designed to assess patient opinion or level of interest in educational activities during a hospitalization. Accordingly, we developed our own using a 5‐point Likert scale (Box 1). Two outcomes researchers with expertise in using questionnaires for clinical research independently reviewed the questionnaire to establish face validity.
Box 1. Daily Questionnaire on In‐Hospital Health Education
The following statements were read to the patients on a daily basis and answered using the following scale: 1 = Strongly Disagree, 2 = Disagree, 3 = Neutral, 4 = Agree, 5 = Strongly Agree
I feel well enough today to learn about my illness or my health.
I want to learn more about my illness or my health today.
I have time to learn about my health today.
It is important to me to learn more about my illness or health while in the hospital.
Interview
All patients were asked the open‐ended questions listed in Box 2, and the entire interview was recorded on audiotape for subsequent analysis.
Box 2. Interview Questions with Probes for Educational Preferences
What things related to your health would you like to learn more about while you are in the hospital? (list up to three topics in order of impotance to you).
How can we help you learn more about your illness or health while in the hospital?
Who should do the teaching (eg, an MD, a nurse, a dietician, a medical student, peers, physical therapists, respiratory therapists)?
Who else should be present (eg, patients with similar illness, family, no one)?
How should this teaching be done (eg, didactic sessions, hands‐on, video tape, pre‐ and post‐testing)?
Data Analysis
All analyses were performed using SAS, version 9.1 (SAS Institute, Inc., Cary, NC). A P value < 0.05 was considered significant.
Time‐Motion Data
Mixed‐effects general linear models (growth curve or repeated measures), using SAS Proc Mixed, were used to test whether the proportions of downtime, busy time, and provider time differed by day of hospitalization. Linear growth curve models were used to test whether a linear trend was present. If not, repeated‐measures models were used to obtain estimates by day of hospitalization.
Questionnaire Data
Mixed‐effects general linear models (growth curve or repeated measures) were used to determine whether patient responses differed by day of hospitalization, as described above.
Interview Data
Tape recordings were reviewed in depth to code participant responses to the structured questions. We utilized the template style of analysis, coding segments of the interviews and identifying illustrative quotes whenever possible. Key patterns and themes were summarized along with specific patient preferences regarding topics of interest and learning opportunities while in the hospital and after discharge.
RESULTS
Patient selection is described in Figure 1, and patient demographics are summarized in Tables 2 and 3.
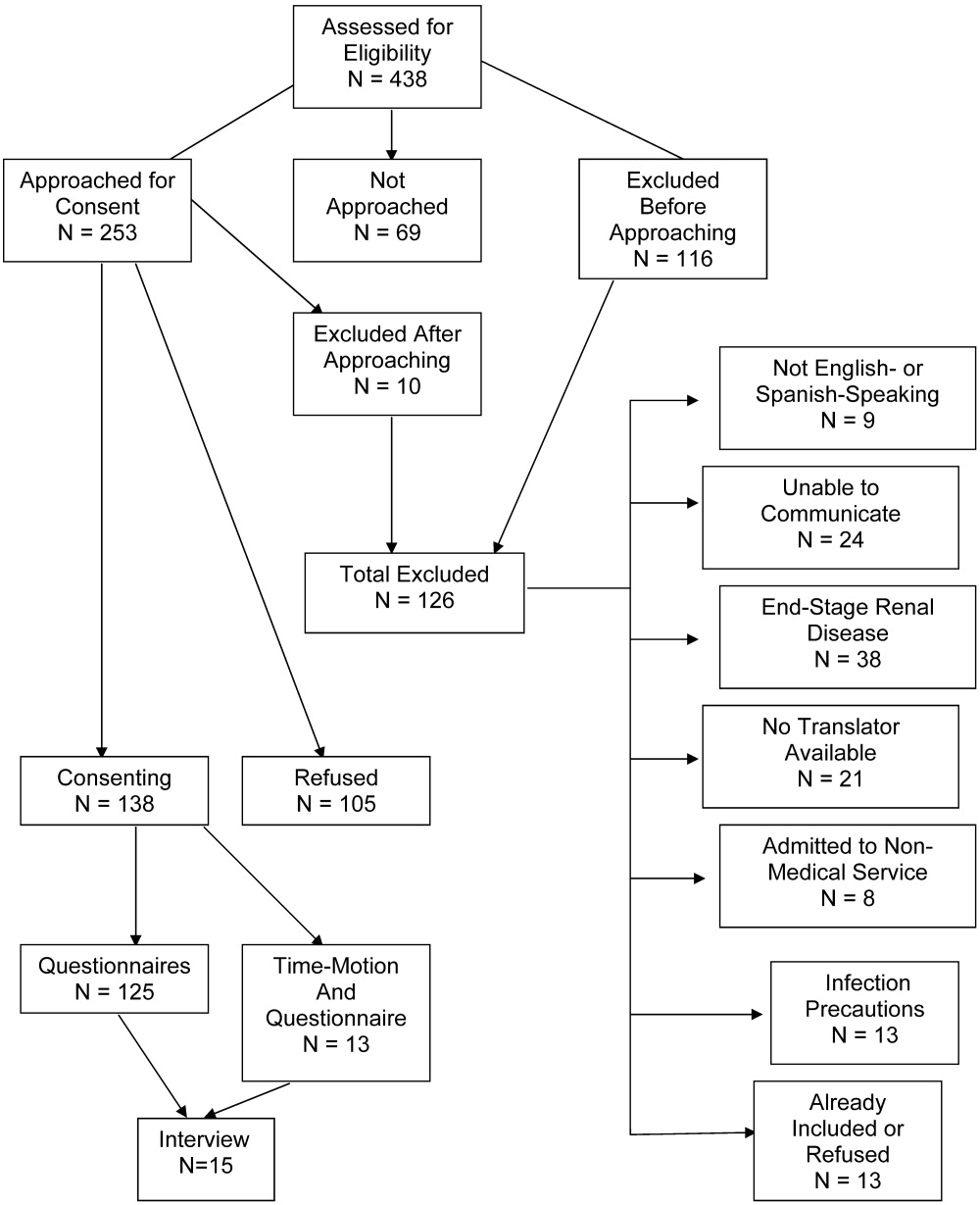
| Demographic | Time‐motion | Interview | Questionnaire |
|---|---|---|---|
| |||
| Study subjects | 13 | 15 | 125 |
| Sex | |||
| Male | 6 (46) | 7 (47) | 61 (49) |
| Female | 7 (54) | 8 (53) | 64 (51) |
| Age (years), median (IQR) | 47 (20) | 51 (20.5) | 51 (18) |
| Race/ethnicity | |||
| White, non‐Hispanic | 6 (46) | 5 (33) | 46 (37) |
| Black/African American | 3 (23) | 4 (27) | 27 (22) |
| American Indian | 0 (0) | 0 (0) | 1 (1) |
| Hispanic | 4 (31) | 6 (40) | 51 (41) |
| Primary language | |||
| English | 12 (92) | 14 (93) | 109 (87) |
| Spanish | 1 (8) | 1 (7) | 16 (13) |
| Health literacy* | |||
| Adequate | 3 (75) | 9 (82) | 60 (71) |
| Marginal | 1 (25) | 0 (0) | 6 (7) |
| Inadequate | 0 (0) | 2 (18) | 18 (22) |
| Insurance status | |||
| Self‐pay | 3 (23) | 1 (7) | 24 (19) |
| Medicaid | 1 (8) | 4 (27) | 19 (15) |
| Medicare | 3 (23) | 0 (0) | 2 (2) |
| Colorado Indigent Care Program | 3 (23) | 7 (47) | 51 (41) |
| Private | 2 (15) | 1 (7) | 5 (4) |
| Other | 1 (8) | 2 (14) | 24 (18) |
| Time‐motion | Interview | Questionnaire | |
|---|---|---|---|
| Study subjects (n) | 13 | 15 | 125 |
| Discharge diagnoses (selected) | |||
| Coronary artery disease (including angina) | 1 (8) | 2 (13) | 24 (19) |
| Congestive heart failure | 1 (8) | 1 (7) | 4 (3) |
| Upper gastrointestinal bleeding, gastritis, reflux | 2 (15) | 4 (27) | 14 (11) |
| Syncope | 2 (15) | 0 | 5 (4) |
| Acute renal failure | 0 | 0 | 5 (4) |
| Pancreatitis | 0 | 1 (7) | 6 (5) |
| Venous thromboembolism | 2 (15) | 1 (7) | 3 (2) |
| Chronic obstructive pulmonary disease | 0 | 0 | 4 (3) |
| Diabetic ketoacidosis | 1 (8) | 1 (7) | 3 (2) |
| Pyelonephritis | 0 | 0 | 5 (4) |
| Pneumonia | 2 (15) | 1 (7) | 5 (4) |
| Comorbidities | |||
| Diabetes | 5 (38) | 9 (60) | 41 (33) |
| Hypertension | 1 (8) | 9 (60) | 55 (44) |
| Dyslipidemia | 6 (46) | 2 (13) | 26 (21) |
| Tobacco | 5 (38) | 7 (47) | 55 (44) |
| Chronic obstructive pulmonary disease | 2 (15) | 4 (27) | 15 (12) |
| Congestive heart failure | 2 (15) | 2 (13) | 13 (10) |
| Coronary heart disease | 3 (23) | 3 (20) | 21 (17) |
Time‐Motion Study
Thirteen patients were studied. Of the 315 patient‐hours observed, 71% were categorized as downtime, 15% as provider time, and 14% as busy time. The proportion of downtime ranged from a low of 0.65 (SE 0.04) on hospital Day 2 to a high of 0.76 (SE 0.06) on hospital Day 4, but the differences in downtime proportions by day did not reach statistical significance (P = .65; Fig. 2). The lowest percentage of downtime observed in any patient on any day was 39%. The 125 hours of downtime observed consisted of 1317 separate blocks of time, 80% of which were less than 15 minutes in duration, 14% of which were 15 to 30 minutes in duration, and 6% of which exceeded 30 minutes in duration.
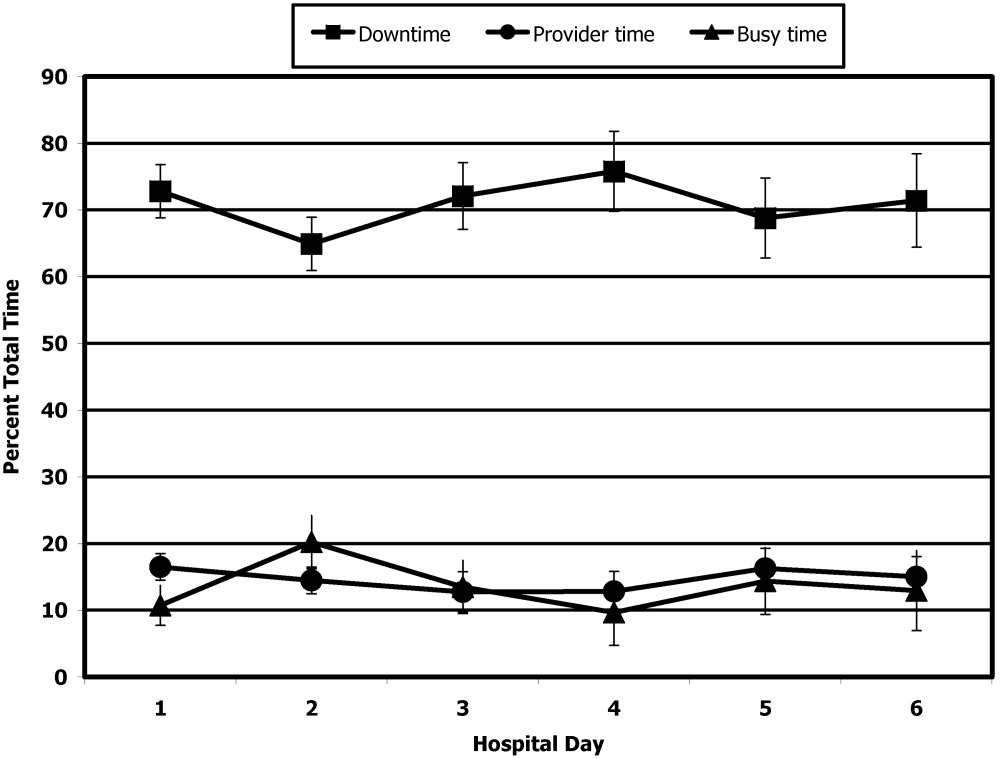
Thirty‐six full days of observation, defined as greater than 7 hours of observation in 1 day, were used to assess the amount of time spent with providers. Of the 60 minutes/day (IQR = 44) that patients spent with health care providers, 21 minutes/day (IQR = 34) was spent with phlebotomists, physical or occupational therapists, dieticians, or social workers, 25 minutes/day (IQR = 25) was spent with patients' nurses, and a median of only 9 minutes/day (IQR = 11) was spent with their physicians.
Questionnaire
A total of 311 questionnaires were administered to the 138 consenting participants. Irrespective of the day of testing, 79% to 97% strongly agreed or agreed with the 4 statements (Fig. 3). In response to the first statementI feel well enough to learnpatient scores increased steadily over the 6 days of hospitalization patients were surveyed (coefficient = 0.15, P = .004). On hospital day 1, the mean score was 3.85 (SE 0.08), and by day 6 the mean score had increased to 4.75 (SE 0.08) However, there was no significant change over time in patients' desire to learn, self‐perceived time available to learn, or importance placed on learning during their hospital stay.

Interview
Fifteen interviews were conducted. Representative comments are presented in Table 4. Responses generally indicated that the patients had anxieties and uncertainties about their health and safety after discharge. Most participants wanted to know more about the condition for which they had been hospitalized, including information pertaining to management, prevention, etiology, and prognosis of their disease. Diabetic patients asked for information on insulin dosing, nutrition, and the effect of the disease on their bodies.
| Theme | Sample quotes |
|---|---|
| Preferred topics | |
| Self‐management | I need to know what to do when I go home, how to take care of it. Medical peopledon't give enough information to the patient and patient's family so they can help themselves. You need to encourage patients to help themselves, take some responsibility for themselves. |
| Prevention of disease recurrence or progression | It's okay to tell people that they have something and give them medicine, but also tell them what they can do to prevent it or make it less painful. I've known about bronchitis for many years, but didn't know it would affect my heart. |
| What's happening to me? | Am I going to diehow long? |
| Just fix me | I came to the hospital to get fixed, not educated. I'm results‐oriented, not cause‐oriented. |
| Preferred learning methods | |
| One‐to‐one didactics with MDs | I'd like one‐to‐one time with someone who has the time to listen. One to one with doctors who can explain what can happen, what to take, what not to take. |
| Family involvement | Get the family involved so the family understands the limitations of the person, how medications affect them. To say a person has a heart condition is a very vague statement. If they [family] understand more, it's better. |
| Groups | A group of people with similar illnessI like groups where everyone listens. I'd participate in groups at the hospital but not at home. |
| Video | Hospital TV is not meeting my needs. |
| Printed material | A doctor or nurse tell me what's going on and then also handouts on dietary and nutrition. |
| Electronic learning | I learned a lot through the encyclopedia of family health care, and through Web sites |
Patients preferred to pick their own topics for education rather than having topics chosen for them. Patients also showed in interest in prevention. One diabetic patient wanted to know how to prevent her children from becoming diabetic, and a cardiac patient wanted education on heart disease prevention. Other recurrent themes included the desire to know what was causing their illness and information about prognosis.
Almost all the patients were interested in more than one type of learning experience. The most frequently cited preference was to have a doctor or other knowledgeable health care professional answer questions specific to their individual situation. Video and group learning were each mentioned by approximately half the participants. Most patients thought that having family present during educational discussions was important.
Video was the most frequently mentioned learning tool, and patients thought it would be useful to have this modality available in the hospital as well as the home. Two patients expressed interest in computerized learning (one of whom had used health Web sites before his hospitalization). Most patients wanted handouts or reading material in addition to other methods of communicating information. Although many patients said they felt comfortable discussing their problems in group settings, some did not.
DISCUSSION
The important findings of this study are that hospitalized patients have a substantial amount of time available for health education and a considerable willingness and interest in participating in health educational activities. We found that although there was a great deal of time available on all days of hospitalization studied, patients felt increasingly well enough to participate in educational activities through their hospital stay.
We are unaware of other studies that have attempted to quantify the amount of time hospitalized patients are available for educational activities or whether they feel capable of participating in these activities. McBride10 found that 95% of hospitalized patients supported a health‐promoting hospital and that almost 80% wanted to modify at least 1 aspect of their lifestyle. Martin and colleagues11 found that patient satisfaction was improved by a patient‐centered unit incorporating dedicated nursing staff to promote patient involvement and provide personalized care and education. Barber‐Parker9 suggested that high patient acuity, short durations of hospitalization, and lack of patient availability because of testing and treatment limited the opportunities that patients had for health education during their hospitalization. These conclusions were reached on the basis of surveys of nurses' perceptions, however, rather than on direct observations or assessments of patients' perceptions.
Our findings suggest that many types of patient educational approaches may be needed to achieve maximal effectiveness and that regardless of the specific approach employed, the focus should be on the primary reason for a patient's hospitalization, what the hospitalization meant, why it happened and what the patient can do to prevent hospitalization from occurring in the future.
Transitions in care have been identified as periods in which communication lapses occur and outcomes can be adversely affected.12 A recent study by Epstein and colleagues13 found that almost 12% of patients had new or worsening symptoms of disease within the first few days after discharge from the hospital and that 22% either did not pick up their medications or understand how to take them (consistent with the observations of Kerzman and colleagues).5 The most common action taken in response to these findings was nurse‐mediated patient education. Our study indicates there is potential for further educational processes in hospitals, which may improve the safety of transitions from a hospital setting to outpatient care.
Although many disease management programs have been studied in the outpatient setting,1417 very few have been extended into hospitals. Accordingly, hospitalists are ideally suited to develop and implement disease management programs in concert with outpatient efforts.18 Our study suggests there is an underutilized opportunity for hospital‐based physicians and other health care providers to work with patients at a time when they are uniquely focused on their own health and free from many of the time constraints of their normal lives.
Although JCAHO mandates that hospitalized patients receive education and training specific to the patient's needs and as appropriate to the care, treatment and services provided,19 there is a paucity of data describing the educational processes in US hospitals. Johansson and colleagues20 conducted a survey in a Finnish hospital where patient education is also mandated. Written materials were given to about 55% of the patients. Demonstration and practice were used with about one third, whereas the Internet and videotapes were used for fewer than 10%. Although patients underwent educational activities throughout their hospitalization, and most were satisfied with the process, Johansson and colleagues found that only 59% felt that what they knew about their care was sufficient, almost a third felt they did not know enough about the side effects of their medical care, and almost half felt they did not have sufficient input into what they were being taught.
Although we found a large amount of time that might be used for patient education during a hospitalization, this time was commonly limited to 15‐minute blocks, as has been noted previously.9 This observation implies that educational activities should be designed so they can be conducted over short periods and/or stopped for short periods when interruptions occur or that the processes of care during a hospitalization should be altered to create larger blocks of continuous time available for educational activities.
A number of issues could have biased our results. Only 66% of the patients who were approached to participate agreed to do so. Because those declining may have been sicker and because sicker patients may require more diagnostic testing or more invasive treatment, we may have overestimated both the amount of downtime available and the willingness of patients to participate in educational activities. If we assume, however, that all patients who refused to participate either disagreed or strongly disagreed with the statements in the questionnaire regarding their interest in educational activities, the fraction of patients agreeing or strongly agreeing with idea that they were well enough and interested would still be 57% to 75% of the population sampled. Accordingly, this potential bias, if it occurred, would not alter our conclusions.
The time‐motion studies were only performed between 8:00 AM and 5:00 PM, such that the resulting data do not reflect any diagnostic testing, therapeutic interventions, or contact with health care providers that occurred at other times. This may have contributed to the strikingly small amount of time that patients spent with their physicians and nurses. If patient time after 5:00 PM and before 8:00 AM had been observed and included, it is likely that the absolute amount of time spent with physicians and nurses would increase, whereas the overall proportion of patient time spent with providers would decrease.
We were also only able to collect data on 13 time‐motion subjects. This limited sample size from a single institution may not be representative of all hospitalized non‐ICU patients on general medical wards. Accordingly, we make no claims that our data can be generalized to the entire population of patients admitted to non‐ICU medical services. However, the results of our surveys, which sampled a much broader patient population and supported our time‐motion findings, suggest that our time‐motion findings are likely to be representative of significant underutilized time and motivation for patient education in the hospital setting.
Also, it is important to note that although the time‐motion studies were only done with 13 patients, these studies are extremely labor intensive and are rarely done with much larger samples. In addition, the SDs on the data collected from the time‐motion studies were quite small. It is possible that if a larger sample were studied, the percentage of free time might be larger or smaller than what we observed for the 13 patients we studied. However, it would be quite unlikely that the amount of free time would be so small (eg, 10%‐15%) that it would invalidate our conclusion that considerable time is available for patient education over and above what currently occurs in most hospital settings.
A patient's self‐perception of his or her ability to learn may not reflect that patient's true cognitive readiness to do so. JCAHO requirements mandate that nurses be trained to assess patients for their ability to learn and to do so as part of the admission process. After reviewing all day 1 patient responses to our questionnaires, in no instance did a nurse assess a patient as having a barrier to learning when the patient had reported feeling well enough to learn. Accordingly, although we performed no direct tests of patients' ability to learn, this retrospective independent assessment did not suggest that patients systematically overestimated their ability to learn.
Finding that hospitalized patients are unoccupied for approximately 70% of their daytime hours and that most patients are both highly motivated to learn and have few barriers to doing so indicates that educational activities during hospitalizations have substantial potential for expansion. The current structure for educating hospitalized patients should be supplemented to take these findings into account.
Acknowledgements
We thank Dr. John Steiner and Dr. Sheena Bull for their assistance in study design as well as the development of the questionnaire and interview tools. We also thank Carolyn Nowels for her assistance with the qualitative data analysis. The assistance of Dr. Bull and Dr. Steiner was made possible through NHLBI grant U01HL079160, and funding for data collection was made possible by the University of Colorado at Denver and Health Sciences Center Department of Medicine, Division of General Internal Medicine small grants program.
- ,.Randomized controlled trial of smoking cessation intervention after admission for coronary heart disease.BMJ.2003;327:1254–1257.
- .Treatment of tobacco use and dependence.N Engl J Med.2002;346:506–512.
- ,, et al.A clinical practice guideline for treating tobacco use and dependence: a US Public Health Service report.JAMA.2000;283:3244–3254.
- ,,, et al.National Institutes of Health state‐of‐the science conference statement: tobacco use: prevention, cessation and control.Ann Intern Med.2006;145:839–844.
- ,,.What do discharged patients know about their medications?Patient Educ Couns.2005;56:276–282.
- Joint Commission on Accreditation of Healthcare Organizations.A Comprehensive Review for the Development and Testing for National Implementation of Hospital Core Measures.2006:1–40.
- .ACC/AHA 2005 guideline update for the diagnosis and management of chronic heart failure in the adult: a report of the American College of Cardiology/ American Heart Association task force on practice guidelines.J Am Coll Cardiol.2005;46:1–82.
- JCAHO data. Available: https://cimprod.uhc.edu/CoreMeasures/Products/DownloadSystem/WebPages/ViewReportsDownloadList.aspx.
- .Integrating patient teaching into bedside patient care: a participant‐observation study of hospital nurses.Patient Educ Couns.2002;48:107–113.
- .Health promotion in the acute hospital setting: the receptivity of adult in‐patients.Patient Educ Couns.2004;54:73–78.
- ,,,,,.Randomized trial of a patient‐centered hospital unit.Patient Educ Couns.1998;34:125–133.
- ,,,,,.Deficits in communication and information transfer between hospital‐based and primary care physicians: implications for patient safety and continuity of care. HYPERLINK “javascript:AL_get(this,%20'jour',%20'JAMA.');”JAMA.2007;297:831–841.
- ,,,,.Frequency of new or worsening symptoms in the posthospitalization period.J Hosp Med.2007;2:58–68.
- ,,,.Patient self‐management of chronic disease in primary care.JAMA.2002;288:2469–2475.
- ,,.Effectiveness of self‐management training in type 2 diabetes.Diabetes Care.2001;24:561–587.
- ,,.Quality of life assessment after patient education a randomized controlled study on asthma and chronic obstructive pulmonary disease.Am J Respir Crit Care Med.2001;95:56–63.
- ,.The effects of a health educational and exercise program for older adults with osteoarthritis for the hip or knee.J Rheumatol.1997;24:1378–1383.
- ,,,.Expanding the roles of hospitalist physicians to include public health.J Hosp Med.2007;2:93–101.
- The Joint Commission on Accreditation of Healthcare Organizations Comprehensive Accreditation Manual for Hospitals: The Official Handbook. January2007. p.152
- ,,,.Need for change in patient education: a Finnish survey from the patient's perspective.Patient Educ Couns.2003;51:239–245.
Educating patients about smoking cessation when they are hospitalized for acute coronary syndrome results in a 57% 1‐year quit rate.1 This rate is far higher than the typical 15%‐30% 1‐year quit rates observed with smoking cessation programs administered in the outpatient setting24 and suggests that hospitalized patients may be uniquely motivated to respond to health education.
Kerzman and colleagues5 found that 42% of hospitalized patients expressed a wish to receive more comprehensive counseling about their medications before being discharged from the hospital. And although the Joint Commission on Hospital Accreditation and the Centers for Medicare and Medicaid Services have established core quality measures mandating that patients hospitalized with congestive heart failure receive education as one component of a high‐quality discharge process,6, 7 approximately one third of patients nationally do not receive adequate patient education.8
Barber‐Parker9 suggested that because patient acuity in hospitals was so high and patients were so commonly absent from their nursing units for testing and treatment, there was little time available for health education during their hospitalization. Anecdotal observations in our institution suggested, however, that adult patients hospitalized on the general Internal Medicine service spent much of their day doing little more than lying in bed watching television. Accordingly, we hypothesized that considerable time might be available for patient education during a hospitalization. We therefore sought to quantify the fraction of time patients were not involved in treatment activities, diagnostic testing, or other evaluations and to determine whether during these times they wanted and were feeling well enough to participate in educational activities. We also sought to determine what patients wanted to know about their health problems and what types of educational activities they most preferred.
MATERIALS AND METHODS
We conducted a time‐motion and survey study from June 25, 2005, to August 15, 2005, at Denver Health Medical Center, an academic public safety‐net hospital affiliated with the University of Colorado School of Medicine. All patients older than 18 years of age who spoke English or Spanish and were admitted to the general Internal Medicine service were candidates for enrollment. Exclusion criteria were being admitted to the intensive care unit, having an inability to communicate, being in contact precautions, and being previously enrolled. The study was approved by the Colorado Multiple Institutional Review Board. Written informed consent was obtained for all study participants.
At 8:00 AM, all patients admitted during the previous 15 hours were assigned a random number from a random number table and were approached for consent in numeric order. With 2 data collectors working daily, a maximum of 12 patients could be enrolled each day. Consenting subjects who passed a vision test were given the Test of Functional Health Literacy in Adults at the time of enrollment and a written questionnaire (in either English or Spanish) on a daily basis for a maximum of 6 days. Some of these patients also participated in a structured interview that was designed to elicit their views on health education topics and formats for education of hospitalized patients. Others, again determined by random number, were subjects of a time‐motion study.
Demographic data collected included age, sex, language, race, comorbidities, insurance status, and discharge diagnosis.
Time‐Motion Study
Patients were observed from 8:00 AM to noon and from 1:00 to 5:00 PM7 days a week. Data were collected using TimerPro on a Dell Axim A5 pocket PC and imported daily into an Excel spreadsheet. Observations were categorized as downtime, busy time, or provider time and subcategorized as summarized in Table 1.
| First level | Second level | Third level |
|---|---|---|
| Downtime | Alone | TV |
| Resting | ||
| Sleeping | ||
| Reading | ||
| Telephone | ||
| Other | ||
| Friends/family | TV | |
| Resting | ||
| Sleeping | ||
| Reading | ||
| Telephone/talk | ||
| Other | ||
| Provider | Physician | |
| Nurse | ||
| Physician and nurse | ||
| Physician and other | ||
| Other | ||
| Busy | ADL | |
| Meal | ||
| Out of room | ||
| Other |
Questionnaire
We were unable to find a validated questionnaire in the literature that was designed to assess patient opinion or level of interest in educational activities during a hospitalization. Accordingly, we developed our own using a 5‐point Likert scale (Box 1). Two outcomes researchers with expertise in using questionnaires for clinical research independently reviewed the questionnaire to establish face validity.
Box 1. Daily Questionnaire on In‐Hospital Health Education
The following statements were read to the patients on a daily basis and answered using the following scale: 1 = Strongly Disagree, 2 = Disagree, 3 = Neutral, 4 = Agree, 5 = Strongly Agree
I feel well enough today to learn about my illness or my health.
I want to learn more about my illness or my health today.
I have time to learn about my health today.
It is important to me to learn more about my illness or health while in the hospital.
Interview
All patients were asked the open‐ended questions listed in Box 2, and the entire interview was recorded on audiotape for subsequent analysis.
Box 2. Interview Questions with Probes for Educational Preferences
What things related to your health would you like to learn more about while you are in the hospital? (list up to three topics in order of impotance to you).
How can we help you learn more about your illness or health while in the hospital?
Who should do the teaching (eg, an MD, a nurse, a dietician, a medical student, peers, physical therapists, respiratory therapists)?
Who else should be present (eg, patients with similar illness, family, no one)?
How should this teaching be done (eg, didactic sessions, hands‐on, video tape, pre‐ and post‐testing)?
Data Analysis
All analyses were performed using SAS, version 9.1 (SAS Institute, Inc., Cary, NC). A P value < 0.05 was considered significant.
Time‐Motion Data
Mixed‐effects general linear models (growth curve or repeated measures), using SAS Proc Mixed, were used to test whether the proportions of downtime, busy time, and provider time differed by day of hospitalization. Linear growth curve models were used to test whether a linear trend was present. If not, repeated‐measures models were used to obtain estimates by day of hospitalization.
Questionnaire Data
Mixed‐effects general linear models (growth curve or repeated measures) were used to determine whether patient responses differed by day of hospitalization, as described above.
Interview Data
Tape recordings were reviewed in depth to code participant responses to the structured questions. We utilized the template style of analysis, coding segments of the interviews and identifying illustrative quotes whenever possible. Key patterns and themes were summarized along with specific patient preferences regarding topics of interest and learning opportunities while in the hospital and after discharge.
RESULTS
Patient selection is described in Figure 1, and patient demographics are summarized in Tables 2 and 3.
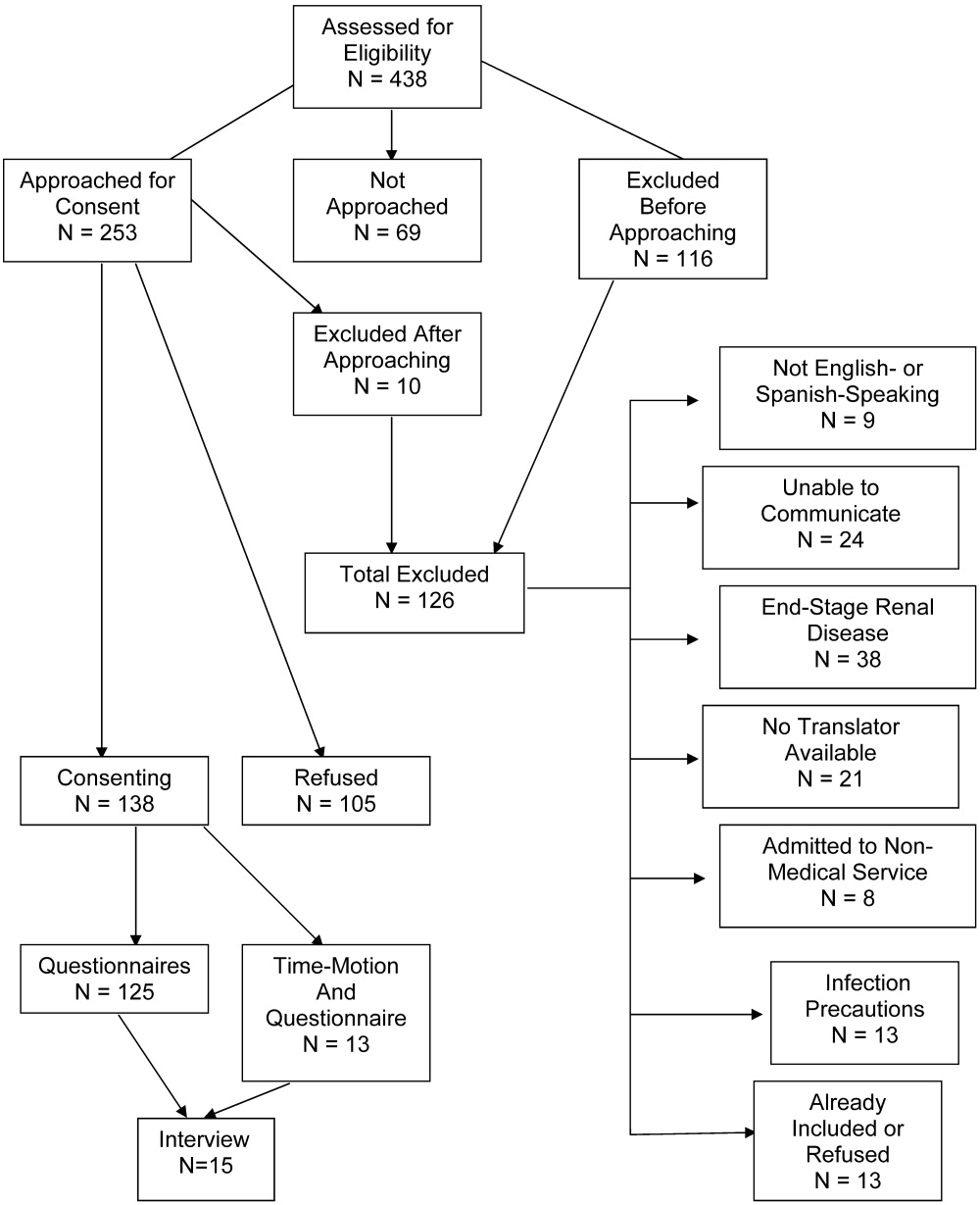
| Demographic | Time‐motion | Interview | Questionnaire |
|---|---|---|---|
| |||
| Study subjects | 13 | 15 | 125 |
| Sex | |||
| Male | 6 (46) | 7 (47) | 61 (49) |
| Female | 7 (54) | 8 (53) | 64 (51) |
| Age (years), median (IQR) | 47 (20) | 51 (20.5) | 51 (18) |
| Race/ethnicity | |||
| White, non‐Hispanic | 6 (46) | 5 (33) | 46 (37) |
| Black/African American | 3 (23) | 4 (27) | 27 (22) |
| American Indian | 0 (0) | 0 (0) | 1 (1) |
| Hispanic | 4 (31) | 6 (40) | 51 (41) |
| Primary language | |||
| English | 12 (92) | 14 (93) | 109 (87) |
| Spanish | 1 (8) | 1 (7) | 16 (13) |
| Health literacy* | |||
| Adequate | 3 (75) | 9 (82) | 60 (71) |
| Marginal | 1 (25) | 0 (0) | 6 (7) |
| Inadequate | 0 (0) | 2 (18) | 18 (22) |
| Insurance status | |||
| Self‐pay | 3 (23) | 1 (7) | 24 (19) |
| Medicaid | 1 (8) | 4 (27) | 19 (15) |
| Medicare | 3 (23) | 0 (0) | 2 (2) |
| Colorado Indigent Care Program | 3 (23) | 7 (47) | 51 (41) |
| Private | 2 (15) | 1 (7) | 5 (4) |
| Other | 1 (8) | 2 (14) | 24 (18) |
| Time‐motion | Interview | Questionnaire | |
|---|---|---|---|
| Study subjects (n) | 13 | 15 | 125 |
| Discharge diagnoses (selected) | |||
| Coronary artery disease (including angina) | 1 (8) | 2 (13) | 24 (19) |
| Congestive heart failure | 1 (8) | 1 (7) | 4 (3) |
| Upper gastrointestinal bleeding, gastritis, reflux | 2 (15) | 4 (27) | 14 (11) |
| Syncope | 2 (15) | 0 | 5 (4) |
| Acute renal failure | 0 | 0 | 5 (4) |
| Pancreatitis | 0 | 1 (7) | 6 (5) |
| Venous thromboembolism | 2 (15) | 1 (7) | 3 (2) |
| Chronic obstructive pulmonary disease | 0 | 0 | 4 (3) |
| Diabetic ketoacidosis | 1 (8) | 1 (7) | 3 (2) |
| Pyelonephritis | 0 | 0 | 5 (4) |
| Pneumonia | 2 (15) | 1 (7) | 5 (4) |
| Comorbidities | |||
| Diabetes | 5 (38) | 9 (60) | 41 (33) |
| Hypertension | 1 (8) | 9 (60) | 55 (44) |
| Dyslipidemia | 6 (46) | 2 (13) | 26 (21) |
| Tobacco | 5 (38) | 7 (47) | 55 (44) |
| Chronic obstructive pulmonary disease | 2 (15) | 4 (27) | 15 (12) |
| Congestive heart failure | 2 (15) | 2 (13) | 13 (10) |
| Coronary heart disease | 3 (23) | 3 (20) | 21 (17) |
Time‐Motion Study
Thirteen patients were studied. Of the 315 patient‐hours observed, 71% were categorized as downtime, 15% as provider time, and 14% as busy time. The proportion of downtime ranged from a low of 0.65 (SE 0.04) on hospital Day 2 to a high of 0.76 (SE 0.06) on hospital Day 4, but the differences in downtime proportions by day did not reach statistical significance (P = .65; Fig. 2). The lowest percentage of downtime observed in any patient on any day was 39%. The 125 hours of downtime observed consisted of 1317 separate blocks of time, 80% of which were less than 15 minutes in duration, 14% of which were 15 to 30 minutes in duration, and 6% of which exceeded 30 minutes in duration.
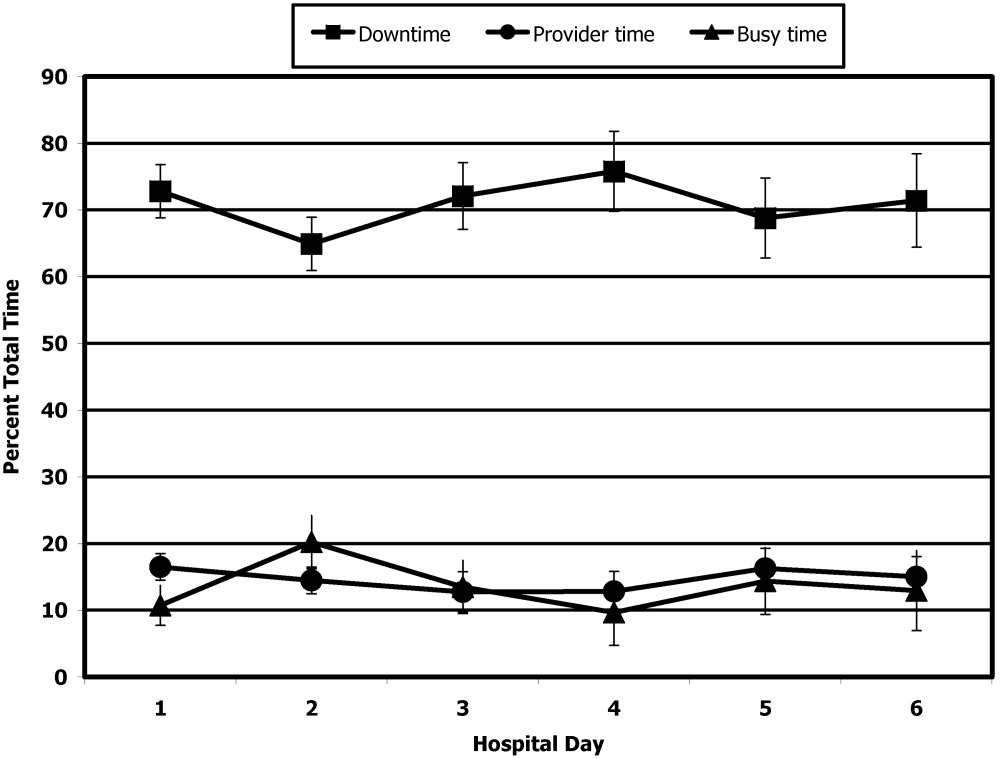
Thirty‐six full days of observation, defined as greater than 7 hours of observation in 1 day, were used to assess the amount of time spent with providers. Of the 60 minutes/day (IQR = 44) that patients spent with health care providers, 21 minutes/day (IQR = 34) was spent with phlebotomists, physical or occupational therapists, dieticians, or social workers, 25 minutes/day (IQR = 25) was spent with patients' nurses, and a median of only 9 minutes/day (IQR = 11) was spent with their physicians.
Questionnaire
A total of 311 questionnaires were administered to the 138 consenting participants. Irrespective of the day of testing, 79% to 97% strongly agreed or agreed with the 4 statements (Fig. 3). In response to the first statementI feel well enough to learnpatient scores increased steadily over the 6 days of hospitalization patients were surveyed (coefficient = 0.15, P = .004). On hospital day 1, the mean score was 3.85 (SE 0.08), and by day 6 the mean score had increased to 4.75 (SE 0.08) However, there was no significant change over time in patients' desire to learn, self‐perceived time available to learn, or importance placed on learning during their hospital stay.

Interview
Fifteen interviews were conducted. Representative comments are presented in Table 4. Responses generally indicated that the patients had anxieties and uncertainties about their health and safety after discharge. Most participants wanted to know more about the condition for which they had been hospitalized, including information pertaining to management, prevention, etiology, and prognosis of their disease. Diabetic patients asked for information on insulin dosing, nutrition, and the effect of the disease on their bodies.
| Theme | Sample quotes |
|---|---|
| Preferred topics | |
| Self‐management | I need to know what to do when I go home, how to take care of it. Medical peopledon't give enough information to the patient and patient's family so they can help themselves. You need to encourage patients to help themselves, take some responsibility for themselves. |
| Prevention of disease recurrence or progression | It's okay to tell people that they have something and give them medicine, but also tell them what they can do to prevent it or make it less painful. I've known about bronchitis for many years, but didn't know it would affect my heart. |
| What's happening to me? | Am I going to diehow long? |
| Just fix me | I came to the hospital to get fixed, not educated. I'm results‐oriented, not cause‐oriented. |
| Preferred learning methods | |
| One‐to‐one didactics with MDs | I'd like one‐to‐one time with someone who has the time to listen. One to one with doctors who can explain what can happen, what to take, what not to take. |
| Family involvement | Get the family involved so the family understands the limitations of the person, how medications affect them. To say a person has a heart condition is a very vague statement. If they [family] understand more, it's better. |
| Groups | A group of people with similar illnessI like groups where everyone listens. I'd participate in groups at the hospital but not at home. |
| Video | Hospital TV is not meeting my needs. |
| Printed material | A doctor or nurse tell me what's going on and then also handouts on dietary and nutrition. |
| Electronic learning | I learned a lot through the encyclopedia of family health care, and through Web sites |
Patients preferred to pick their own topics for education rather than having topics chosen for them. Patients also showed in interest in prevention. One diabetic patient wanted to know how to prevent her children from becoming diabetic, and a cardiac patient wanted education on heart disease prevention. Other recurrent themes included the desire to know what was causing their illness and information about prognosis.
Almost all the patients were interested in more than one type of learning experience. The most frequently cited preference was to have a doctor or other knowledgeable health care professional answer questions specific to their individual situation. Video and group learning were each mentioned by approximately half the participants. Most patients thought that having family present during educational discussions was important.
Video was the most frequently mentioned learning tool, and patients thought it would be useful to have this modality available in the hospital as well as the home. Two patients expressed interest in computerized learning (one of whom had used health Web sites before his hospitalization). Most patients wanted handouts or reading material in addition to other methods of communicating information. Although many patients said they felt comfortable discussing their problems in group settings, some did not.
DISCUSSION
The important findings of this study are that hospitalized patients have a substantial amount of time available for health education and a considerable willingness and interest in participating in health educational activities. We found that although there was a great deal of time available on all days of hospitalization studied, patients felt increasingly well enough to participate in educational activities through their hospital stay.
We are unaware of other studies that have attempted to quantify the amount of time hospitalized patients are available for educational activities or whether they feel capable of participating in these activities. McBride10 found that 95% of hospitalized patients supported a health‐promoting hospital and that almost 80% wanted to modify at least 1 aspect of their lifestyle. Martin and colleagues11 found that patient satisfaction was improved by a patient‐centered unit incorporating dedicated nursing staff to promote patient involvement and provide personalized care and education. Barber‐Parker9 suggested that high patient acuity, short durations of hospitalization, and lack of patient availability because of testing and treatment limited the opportunities that patients had for health education during their hospitalization. These conclusions were reached on the basis of surveys of nurses' perceptions, however, rather than on direct observations or assessments of patients' perceptions.
Our findings suggest that many types of patient educational approaches may be needed to achieve maximal effectiveness and that regardless of the specific approach employed, the focus should be on the primary reason for a patient's hospitalization, what the hospitalization meant, why it happened and what the patient can do to prevent hospitalization from occurring in the future.
Transitions in care have been identified as periods in which communication lapses occur and outcomes can be adversely affected.12 A recent study by Epstein and colleagues13 found that almost 12% of patients had new or worsening symptoms of disease within the first few days after discharge from the hospital and that 22% either did not pick up their medications or understand how to take them (consistent with the observations of Kerzman and colleagues).5 The most common action taken in response to these findings was nurse‐mediated patient education. Our study indicates there is potential for further educational processes in hospitals, which may improve the safety of transitions from a hospital setting to outpatient care.
Although many disease management programs have been studied in the outpatient setting,1417 very few have been extended into hospitals. Accordingly, hospitalists are ideally suited to develop and implement disease management programs in concert with outpatient efforts.18 Our study suggests there is an underutilized opportunity for hospital‐based physicians and other health care providers to work with patients at a time when they are uniquely focused on their own health and free from many of the time constraints of their normal lives.
Although JCAHO mandates that hospitalized patients receive education and training specific to the patient's needs and as appropriate to the care, treatment and services provided,19 there is a paucity of data describing the educational processes in US hospitals. Johansson and colleagues20 conducted a survey in a Finnish hospital where patient education is also mandated. Written materials were given to about 55% of the patients. Demonstration and practice were used with about one third, whereas the Internet and videotapes were used for fewer than 10%. Although patients underwent educational activities throughout their hospitalization, and most were satisfied with the process, Johansson and colleagues found that only 59% felt that what they knew about their care was sufficient, almost a third felt they did not know enough about the side effects of their medical care, and almost half felt they did not have sufficient input into what they were being taught.
Although we found a large amount of time that might be used for patient education during a hospitalization, this time was commonly limited to 15‐minute blocks, as has been noted previously.9 This observation implies that educational activities should be designed so they can be conducted over short periods and/or stopped for short periods when interruptions occur or that the processes of care during a hospitalization should be altered to create larger blocks of continuous time available for educational activities.
A number of issues could have biased our results. Only 66% of the patients who were approached to participate agreed to do so. Because those declining may have been sicker and because sicker patients may require more diagnostic testing or more invasive treatment, we may have overestimated both the amount of downtime available and the willingness of patients to participate in educational activities. If we assume, however, that all patients who refused to participate either disagreed or strongly disagreed with the statements in the questionnaire regarding their interest in educational activities, the fraction of patients agreeing or strongly agreeing with idea that they were well enough and interested would still be 57% to 75% of the population sampled. Accordingly, this potential bias, if it occurred, would not alter our conclusions.
The time‐motion studies were only performed between 8:00 AM and 5:00 PM, such that the resulting data do not reflect any diagnostic testing, therapeutic interventions, or contact with health care providers that occurred at other times. This may have contributed to the strikingly small amount of time that patients spent with their physicians and nurses. If patient time after 5:00 PM and before 8:00 AM had been observed and included, it is likely that the absolute amount of time spent with physicians and nurses would increase, whereas the overall proportion of patient time spent with providers would decrease.
We were also only able to collect data on 13 time‐motion subjects. This limited sample size from a single institution may not be representative of all hospitalized non‐ICU patients on general medical wards. Accordingly, we make no claims that our data can be generalized to the entire population of patients admitted to non‐ICU medical services. However, the results of our surveys, which sampled a much broader patient population and supported our time‐motion findings, suggest that our time‐motion findings are likely to be representative of significant underutilized time and motivation for patient education in the hospital setting.
Also, it is important to note that although the time‐motion studies were only done with 13 patients, these studies are extremely labor intensive and are rarely done with much larger samples. In addition, the SDs on the data collected from the time‐motion studies were quite small. It is possible that if a larger sample were studied, the percentage of free time might be larger or smaller than what we observed for the 13 patients we studied. However, it would be quite unlikely that the amount of free time would be so small (eg, 10%‐15%) that it would invalidate our conclusion that considerable time is available for patient education over and above what currently occurs in most hospital settings.
A patient's self‐perception of his or her ability to learn may not reflect that patient's true cognitive readiness to do so. JCAHO requirements mandate that nurses be trained to assess patients for their ability to learn and to do so as part of the admission process. After reviewing all day 1 patient responses to our questionnaires, in no instance did a nurse assess a patient as having a barrier to learning when the patient had reported feeling well enough to learn. Accordingly, although we performed no direct tests of patients' ability to learn, this retrospective independent assessment did not suggest that patients systematically overestimated their ability to learn.
Finding that hospitalized patients are unoccupied for approximately 70% of their daytime hours and that most patients are both highly motivated to learn and have few barriers to doing so indicates that educational activities during hospitalizations have substantial potential for expansion. The current structure for educating hospitalized patients should be supplemented to take these findings into account.
Acknowledgements
We thank Dr. John Steiner and Dr. Sheena Bull for their assistance in study design as well as the development of the questionnaire and interview tools. We also thank Carolyn Nowels for her assistance with the qualitative data analysis. The assistance of Dr. Bull and Dr. Steiner was made possible through NHLBI grant U01HL079160, and funding for data collection was made possible by the University of Colorado at Denver and Health Sciences Center Department of Medicine, Division of General Internal Medicine small grants program.
Educating patients about smoking cessation when they are hospitalized for acute coronary syndrome results in a 57% 1‐year quit rate.1 This rate is far higher than the typical 15%‐30% 1‐year quit rates observed with smoking cessation programs administered in the outpatient setting24 and suggests that hospitalized patients may be uniquely motivated to respond to health education.
Kerzman and colleagues5 found that 42% of hospitalized patients expressed a wish to receive more comprehensive counseling about their medications before being discharged from the hospital. And although the Joint Commission on Hospital Accreditation and the Centers for Medicare and Medicaid Services have established core quality measures mandating that patients hospitalized with congestive heart failure receive education as one component of a high‐quality discharge process,6, 7 approximately one third of patients nationally do not receive adequate patient education.8
Barber‐Parker9 suggested that because patient acuity in hospitals was so high and patients were so commonly absent from their nursing units for testing and treatment, there was little time available for health education during their hospitalization. Anecdotal observations in our institution suggested, however, that adult patients hospitalized on the general Internal Medicine service spent much of their day doing little more than lying in bed watching television. Accordingly, we hypothesized that considerable time might be available for patient education during a hospitalization. We therefore sought to quantify the fraction of time patients were not involved in treatment activities, diagnostic testing, or other evaluations and to determine whether during these times they wanted and were feeling well enough to participate in educational activities. We also sought to determine what patients wanted to know about their health problems and what types of educational activities they most preferred.
MATERIALS AND METHODS
We conducted a time‐motion and survey study from June 25, 2005, to August 15, 2005, at Denver Health Medical Center, an academic public safety‐net hospital affiliated with the University of Colorado School of Medicine. All patients older than 18 years of age who spoke English or Spanish and were admitted to the general Internal Medicine service were candidates for enrollment. Exclusion criteria were being admitted to the intensive care unit, having an inability to communicate, being in contact precautions, and being previously enrolled. The study was approved by the Colorado Multiple Institutional Review Board. Written informed consent was obtained for all study participants.
At 8:00 AM, all patients admitted during the previous 15 hours were assigned a random number from a random number table and were approached for consent in numeric order. With 2 data collectors working daily, a maximum of 12 patients could be enrolled each day. Consenting subjects who passed a vision test were given the Test of Functional Health Literacy in Adults at the time of enrollment and a written questionnaire (in either English or Spanish) on a daily basis for a maximum of 6 days. Some of these patients also participated in a structured interview that was designed to elicit their views on health education topics and formats for education of hospitalized patients. Others, again determined by random number, were subjects of a time‐motion study.
Demographic data collected included age, sex, language, race, comorbidities, insurance status, and discharge diagnosis.
Time‐Motion Study
Patients were observed from 8:00 AM to noon and from 1:00 to 5:00 PM7 days a week. Data were collected using TimerPro on a Dell Axim A5 pocket PC and imported daily into an Excel spreadsheet. Observations were categorized as downtime, busy time, or provider time and subcategorized as summarized in Table 1.
| First level | Second level | Third level |
|---|---|---|
| Downtime | Alone | TV |
| Resting | ||
| Sleeping | ||
| Reading | ||
| Telephone | ||
| Other | ||
| Friends/family | TV | |
| Resting | ||
| Sleeping | ||
| Reading | ||
| Telephone/talk | ||
| Other | ||
| Provider | Physician | |
| Nurse | ||
| Physician and nurse | ||
| Physician and other | ||
| Other | ||
| Busy | ADL | |
| Meal | ||
| Out of room | ||
| Other |
Questionnaire
We were unable to find a validated questionnaire in the literature that was designed to assess patient opinion or level of interest in educational activities during a hospitalization. Accordingly, we developed our own using a 5‐point Likert scale (Box 1). Two outcomes researchers with expertise in using questionnaires for clinical research independently reviewed the questionnaire to establish face validity.
Box 1. Daily Questionnaire on In‐Hospital Health Education
The following statements were read to the patients on a daily basis and answered using the following scale: 1 = Strongly Disagree, 2 = Disagree, 3 = Neutral, 4 = Agree, 5 = Strongly Agree
I feel well enough today to learn about my illness or my health.
I want to learn more about my illness or my health today.
I have time to learn about my health today.
It is important to me to learn more about my illness or health while in the hospital.
Interview
All patients were asked the open‐ended questions listed in Box 2, and the entire interview was recorded on audiotape for subsequent analysis.
Box 2. Interview Questions with Probes for Educational Preferences
What things related to your health would you like to learn more about while you are in the hospital? (list up to three topics in order of impotance to you).
How can we help you learn more about your illness or health while in the hospital?
Who should do the teaching (eg, an MD, a nurse, a dietician, a medical student, peers, physical therapists, respiratory therapists)?
Who else should be present (eg, patients with similar illness, family, no one)?
How should this teaching be done (eg, didactic sessions, hands‐on, video tape, pre‐ and post‐testing)?
Data Analysis
All analyses were performed using SAS, version 9.1 (SAS Institute, Inc., Cary, NC). A P value < 0.05 was considered significant.
Time‐Motion Data
Mixed‐effects general linear models (growth curve or repeated measures), using SAS Proc Mixed, were used to test whether the proportions of downtime, busy time, and provider time differed by day of hospitalization. Linear growth curve models were used to test whether a linear trend was present. If not, repeated‐measures models were used to obtain estimates by day of hospitalization.
Questionnaire Data
Mixed‐effects general linear models (growth curve or repeated measures) were used to determine whether patient responses differed by day of hospitalization, as described above.
Interview Data
Tape recordings were reviewed in depth to code participant responses to the structured questions. We utilized the template style of analysis, coding segments of the interviews and identifying illustrative quotes whenever possible. Key patterns and themes were summarized along with specific patient preferences regarding topics of interest and learning opportunities while in the hospital and after discharge.
RESULTS
Patient selection is described in Figure 1, and patient demographics are summarized in Tables 2 and 3.
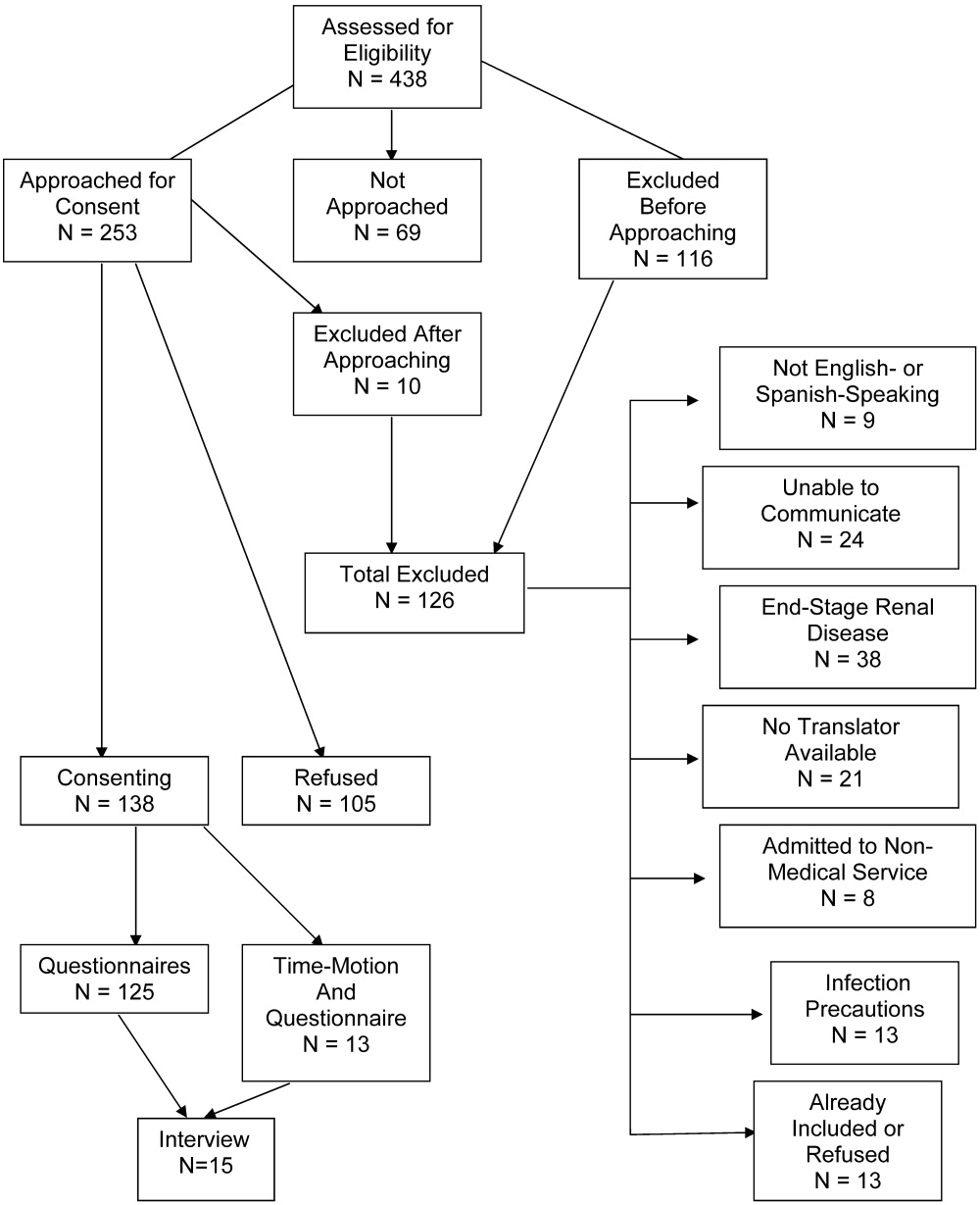
| Demographic | Time‐motion | Interview | Questionnaire |
|---|---|---|---|
| |||
| Study subjects | 13 | 15 | 125 |
| Sex | |||
| Male | 6 (46) | 7 (47) | 61 (49) |
| Female | 7 (54) | 8 (53) | 64 (51) |
| Age (years), median (IQR) | 47 (20) | 51 (20.5) | 51 (18) |
| Race/ethnicity | |||
| White, non‐Hispanic | 6 (46) | 5 (33) | 46 (37) |
| Black/African American | 3 (23) | 4 (27) | 27 (22) |
| American Indian | 0 (0) | 0 (0) | 1 (1) |
| Hispanic | 4 (31) | 6 (40) | 51 (41) |
| Primary language | |||
| English | 12 (92) | 14 (93) | 109 (87) |
| Spanish | 1 (8) | 1 (7) | 16 (13) |
| Health literacy* | |||
| Adequate | 3 (75) | 9 (82) | 60 (71) |
| Marginal | 1 (25) | 0 (0) | 6 (7) |
| Inadequate | 0 (0) | 2 (18) | 18 (22) |
| Insurance status | |||
| Self‐pay | 3 (23) | 1 (7) | 24 (19) |
| Medicaid | 1 (8) | 4 (27) | 19 (15) |
| Medicare | 3 (23) | 0 (0) | 2 (2) |
| Colorado Indigent Care Program | 3 (23) | 7 (47) | 51 (41) |
| Private | 2 (15) | 1 (7) | 5 (4) |
| Other | 1 (8) | 2 (14) | 24 (18) |
| Time‐motion | Interview | Questionnaire | |
|---|---|---|---|
| Study subjects (n) | 13 | 15 | 125 |
| Discharge diagnoses (selected) | |||
| Coronary artery disease (including angina) | 1 (8) | 2 (13) | 24 (19) |
| Congestive heart failure | 1 (8) | 1 (7) | 4 (3) |
| Upper gastrointestinal bleeding, gastritis, reflux | 2 (15) | 4 (27) | 14 (11) |
| Syncope | 2 (15) | 0 | 5 (4) |
| Acute renal failure | 0 | 0 | 5 (4) |
| Pancreatitis | 0 | 1 (7) | 6 (5) |
| Venous thromboembolism | 2 (15) | 1 (7) | 3 (2) |
| Chronic obstructive pulmonary disease | 0 | 0 | 4 (3) |
| Diabetic ketoacidosis | 1 (8) | 1 (7) | 3 (2) |
| Pyelonephritis | 0 | 0 | 5 (4) |
| Pneumonia | 2 (15) | 1 (7) | 5 (4) |
| Comorbidities | |||
| Diabetes | 5 (38) | 9 (60) | 41 (33) |
| Hypertension | 1 (8) | 9 (60) | 55 (44) |
| Dyslipidemia | 6 (46) | 2 (13) | 26 (21) |
| Tobacco | 5 (38) | 7 (47) | 55 (44) |
| Chronic obstructive pulmonary disease | 2 (15) | 4 (27) | 15 (12) |
| Congestive heart failure | 2 (15) | 2 (13) | 13 (10) |
| Coronary heart disease | 3 (23) | 3 (20) | 21 (17) |
Time‐Motion Study
Thirteen patients were studied. Of the 315 patient‐hours observed, 71% were categorized as downtime, 15% as provider time, and 14% as busy time. The proportion of downtime ranged from a low of 0.65 (SE 0.04) on hospital Day 2 to a high of 0.76 (SE 0.06) on hospital Day 4, but the differences in downtime proportions by day did not reach statistical significance (P = .65; Fig. 2). The lowest percentage of downtime observed in any patient on any day was 39%. The 125 hours of downtime observed consisted of 1317 separate blocks of time, 80% of which were less than 15 minutes in duration, 14% of which were 15 to 30 minutes in duration, and 6% of which exceeded 30 minutes in duration.
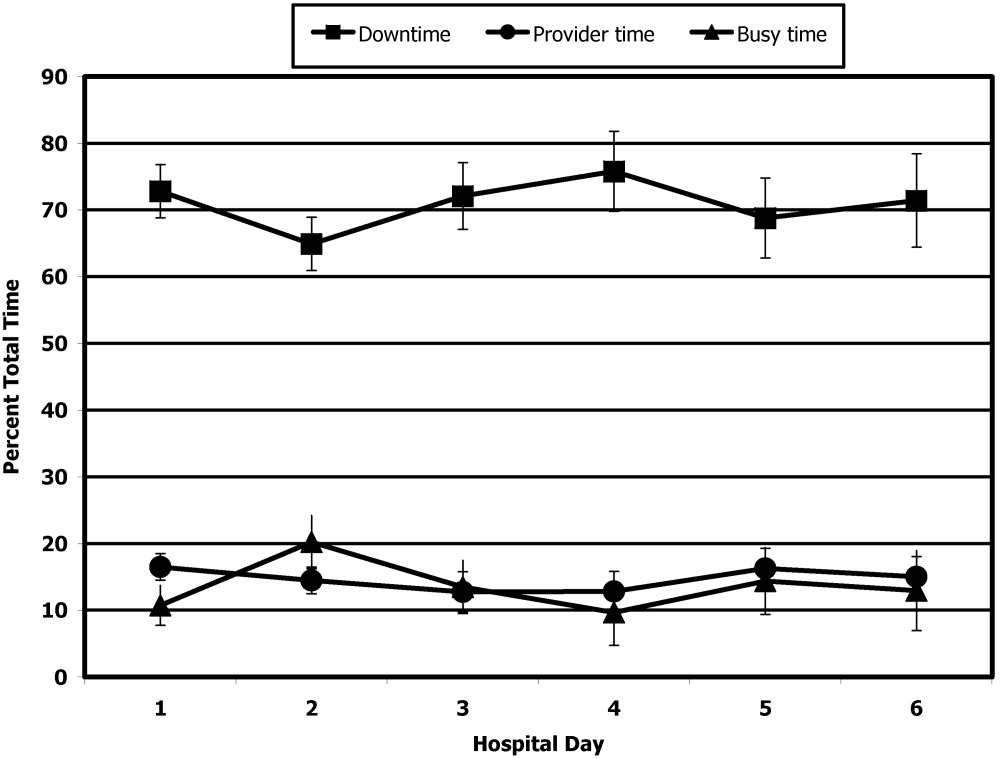
Thirty‐six full days of observation, defined as greater than 7 hours of observation in 1 day, were used to assess the amount of time spent with providers. Of the 60 minutes/day (IQR = 44) that patients spent with health care providers, 21 minutes/day (IQR = 34) was spent with phlebotomists, physical or occupational therapists, dieticians, or social workers, 25 minutes/day (IQR = 25) was spent with patients' nurses, and a median of only 9 minutes/day (IQR = 11) was spent with their physicians.
Questionnaire
A total of 311 questionnaires were administered to the 138 consenting participants. Irrespective of the day of testing, 79% to 97% strongly agreed or agreed with the 4 statements (Fig. 3). In response to the first statementI feel well enough to learnpatient scores increased steadily over the 6 days of hospitalization patients were surveyed (coefficient = 0.15, P = .004). On hospital day 1, the mean score was 3.85 (SE 0.08), and by day 6 the mean score had increased to 4.75 (SE 0.08) However, there was no significant change over time in patients' desire to learn, self‐perceived time available to learn, or importance placed on learning during their hospital stay.

Interview
Fifteen interviews were conducted. Representative comments are presented in Table 4. Responses generally indicated that the patients had anxieties and uncertainties about their health and safety after discharge. Most participants wanted to know more about the condition for which they had been hospitalized, including information pertaining to management, prevention, etiology, and prognosis of their disease. Diabetic patients asked for information on insulin dosing, nutrition, and the effect of the disease on their bodies.
| Theme | Sample quotes |
|---|---|
| Preferred topics | |
| Self‐management | I need to know what to do when I go home, how to take care of it. Medical peopledon't give enough information to the patient and patient's family so they can help themselves. You need to encourage patients to help themselves, take some responsibility for themselves. |
| Prevention of disease recurrence or progression | It's okay to tell people that they have something and give them medicine, but also tell them what they can do to prevent it or make it less painful. I've known about bronchitis for many years, but didn't know it would affect my heart. |
| What's happening to me? | Am I going to diehow long? |
| Just fix me | I came to the hospital to get fixed, not educated. I'm results‐oriented, not cause‐oriented. |
| Preferred learning methods | |
| One‐to‐one didactics with MDs | I'd like one‐to‐one time with someone who has the time to listen. One to one with doctors who can explain what can happen, what to take, what not to take. |
| Family involvement | Get the family involved so the family understands the limitations of the person, how medications affect them. To say a person has a heart condition is a very vague statement. If they [family] understand more, it's better. |
| Groups | A group of people with similar illnessI like groups where everyone listens. I'd participate in groups at the hospital but not at home. |
| Video | Hospital TV is not meeting my needs. |
| Printed material | A doctor or nurse tell me what's going on and then also handouts on dietary and nutrition. |
| Electronic learning | I learned a lot through the encyclopedia of family health care, and through Web sites |
Patients preferred to pick their own topics for education rather than having topics chosen for them. Patients also showed in interest in prevention. One diabetic patient wanted to know how to prevent her children from becoming diabetic, and a cardiac patient wanted education on heart disease prevention. Other recurrent themes included the desire to know what was causing their illness and information about prognosis.
Almost all the patients were interested in more than one type of learning experience. The most frequently cited preference was to have a doctor or other knowledgeable health care professional answer questions specific to their individual situation. Video and group learning were each mentioned by approximately half the participants. Most patients thought that having family present during educational discussions was important.
Video was the most frequently mentioned learning tool, and patients thought it would be useful to have this modality available in the hospital as well as the home. Two patients expressed interest in computerized learning (one of whom had used health Web sites before his hospitalization). Most patients wanted handouts or reading material in addition to other methods of communicating information. Although many patients said they felt comfortable discussing their problems in group settings, some did not.
DISCUSSION
The important findings of this study are that hospitalized patients have a substantial amount of time available for health education and a considerable willingness and interest in participating in health educational activities. We found that although there was a great deal of time available on all days of hospitalization studied, patients felt increasingly well enough to participate in educational activities through their hospital stay.
We are unaware of other studies that have attempted to quantify the amount of time hospitalized patients are available for educational activities or whether they feel capable of participating in these activities. McBride10 found that 95% of hospitalized patients supported a health‐promoting hospital and that almost 80% wanted to modify at least 1 aspect of their lifestyle. Martin and colleagues11 found that patient satisfaction was improved by a patient‐centered unit incorporating dedicated nursing staff to promote patient involvement and provide personalized care and education. Barber‐Parker9 suggested that high patient acuity, short durations of hospitalization, and lack of patient availability because of testing and treatment limited the opportunities that patients had for health education during their hospitalization. These conclusions were reached on the basis of surveys of nurses' perceptions, however, rather than on direct observations or assessments of patients' perceptions.
Our findings suggest that many types of patient educational approaches may be needed to achieve maximal effectiveness and that regardless of the specific approach employed, the focus should be on the primary reason for a patient's hospitalization, what the hospitalization meant, why it happened and what the patient can do to prevent hospitalization from occurring in the future.
Transitions in care have been identified as periods in which communication lapses occur and outcomes can be adversely affected.12 A recent study by Epstein and colleagues13 found that almost 12% of patients had new or worsening symptoms of disease within the first few days after discharge from the hospital and that 22% either did not pick up their medications or understand how to take them (consistent with the observations of Kerzman and colleagues).5 The most common action taken in response to these findings was nurse‐mediated patient education. Our study indicates there is potential for further educational processes in hospitals, which may improve the safety of transitions from a hospital setting to outpatient care.
Although many disease management programs have been studied in the outpatient setting,1417 very few have been extended into hospitals. Accordingly, hospitalists are ideally suited to develop and implement disease management programs in concert with outpatient efforts.18 Our study suggests there is an underutilized opportunity for hospital‐based physicians and other health care providers to work with patients at a time when they are uniquely focused on their own health and free from many of the time constraints of their normal lives.
Although JCAHO mandates that hospitalized patients receive education and training specific to the patient's needs and as appropriate to the care, treatment and services provided,19 there is a paucity of data describing the educational processes in US hospitals. Johansson and colleagues20 conducted a survey in a Finnish hospital where patient education is also mandated. Written materials were given to about 55% of the patients. Demonstration and practice were used with about one third, whereas the Internet and videotapes were used for fewer than 10%. Although patients underwent educational activities throughout their hospitalization, and most were satisfied with the process, Johansson and colleagues found that only 59% felt that what they knew about their care was sufficient, almost a third felt they did not know enough about the side effects of their medical care, and almost half felt they did not have sufficient input into what they were being taught.
Although we found a large amount of time that might be used for patient education during a hospitalization, this time was commonly limited to 15‐minute blocks, as has been noted previously.9 This observation implies that educational activities should be designed so they can be conducted over short periods and/or stopped for short periods when interruptions occur or that the processes of care during a hospitalization should be altered to create larger blocks of continuous time available for educational activities.
A number of issues could have biased our results. Only 66% of the patients who were approached to participate agreed to do so. Because those declining may have been sicker and because sicker patients may require more diagnostic testing or more invasive treatment, we may have overestimated both the amount of downtime available and the willingness of patients to participate in educational activities. If we assume, however, that all patients who refused to participate either disagreed or strongly disagreed with the statements in the questionnaire regarding their interest in educational activities, the fraction of patients agreeing or strongly agreeing with idea that they were well enough and interested would still be 57% to 75% of the population sampled. Accordingly, this potential bias, if it occurred, would not alter our conclusions.
The time‐motion studies were only performed between 8:00 AM and 5:00 PM, such that the resulting data do not reflect any diagnostic testing, therapeutic interventions, or contact with health care providers that occurred at other times. This may have contributed to the strikingly small amount of time that patients spent with their physicians and nurses. If patient time after 5:00 PM and before 8:00 AM had been observed and included, it is likely that the absolute amount of time spent with physicians and nurses would increase, whereas the overall proportion of patient time spent with providers would decrease.
We were also only able to collect data on 13 time‐motion subjects. This limited sample size from a single institution may not be representative of all hospitalized non‐ICU patients on general medical wards. Accordingly, we make no claims that our data can be generalized to the entire population of patients admitted to non‐ICU medical services. However, the results of our surveys, which sampled a much broader patient population and supported our time‐motion findings, suggest that our time‐motion findings are likely to be representative of significant underutilized time and motivation for patient education in the hospital setting.
Also, it is important to note that although the time‐motion studies were only done with 13 patients, these studies are extremely labor intensive and are rarely done with much larger samples. In addition, the SDs on the data collected from the time‐motion studies were quite small. It is possible that if a larger sample were studied, the percentage of free time might be larger or smaller than what we observed for the 13 patients we studied. However, it would be quite unlikely that the amount of free time would be so small (eg, 10%‐15%) that it would invalidate our conclusion that considerable time is available for patient education over and above what currently occurs in most hospital settings.
A patient's self‐perception of his or her ability to learn may not reflect that patient's true cognitive readiness to do so. JCAHO requirements mandate that nurses be trained to assess patients for their ability to learn and to do so as part of the admission process. After reviewing all day 1 patient responses to our questionnaires, in no instance did a nurse assess a patient as having a barrier to learning when the patient had reported feeling well enough to learn. Accordingly, although we performed no direct tests of patients' ability to learn, this retrospective independent assessment did not suggest that patients systematically overestimated their ability to learn.
Finding that hospitalized patients are unoccupied for approximately 70% of their daytime hours and that most patients are both highly motivated to learn and have few barriers to doing so indicates that educational activities during hospitalizations have substantial potential for expansion. The current structure for educating hospitalized patients should be supplemented to take these findings into account.
Acknowledgements
We thank Dr. John Steiner and Dr. Sheena Bull for their assistance in study design as well as the development of the questionnaire and interview tools. We also thank Carolyn Nowels for her assistance with the qualitative data analysis. The assistance of Dr. Bull and Dr. Steiner was made possible through NHLBI grant U01HL079160, and funding for data collection was made possible by the University of Colorado at Denver and Health Sciences Center Department of Medicine, Division of General Internal Medicine small grants program.
- ,.Randomized controlled trial of smoking cessation intervention after admission for coronary heart disease.BMJ.2003;327:1254–1257.
- .Treatment of tobacco use and dependence.N Engl J Med.2002;346:506–512.
- ,, et al.A clinical practice guideline for treating tobacco use and dependence: a US Public Health Service report.JAMA.2000;283:3244–3254.
- ,,, et al.National Institutes of Health state‐of‐the science conference statement: tobacco use: prevention, cessation and control.Ann Intern Med.2006;145:839–844.
- ,,.What do discharged patients know about their medications?Patient Educ Couns.2005;56:276–282.
- Joint Commission on Accreditation of Healthcare Organizations.A Comprehensive Review for the Development and Testing for National Implementation of Hospital Core Measures.2006:1–40.
- .ACC/AHA 2005 guideline update for the diagnosis and management of chronic heart failure in the adult: a report of the American College of Cardiology/ American Heart Association task force on practice guidelines.J Am Coll Cardiol.2005;46:1–82.
- JCAHO data. Available: https://cimprod.uhc.edu/CoreMeasures/Products/DownloadSystem/WebPages/ViewReportsDownloadList.aspx.
- .Integrating patient teaching into bedside patient care: a participant‐observation study of hospital nurses.Patient Educ Couns.2002;48:107–113.
- .Health promotion in the acute hospital setting: the receptivity of adult in‐patients.Patient Educ Couns.2004;54:73–78.
- ,,,,,.Randomized trial of a patient‐centered hospital unit.Patient Educ Couns.1998;34:125–133.
- ,,,,,.Deficits in communication and information transfer between hospital‐based and primary care physicians: implications for patient safety and continuity of care. HYPERLINK “javascript:AL_get(this,%20'jour',%20'JAMA.');”JAMA.2007;297:831–841.
- ,,,,.Frequency of new or worsening symptoms in the posthospitalization period.J Hosp Med.2007;2:58–68.
- ,,,.Patient self‐management of chronic disease in primary care.JAMA.2002;288:2469–2475.
- ,,.Effectiveness of self‐management training in type 2 diabetes.Diabetes Care.2001;24:561–587.
- ,,.Quality of life assessment after patient education a randomized controlled study on asthma and chronic obstructive pulmonary disease.Am J Respir Crit Care Med.2001;95:56–63.
- ,.The effects of a health educational and exercise program for older adults with osteoarthritis for the hip or knee.J Rheumatol.1997;24:1378–1383.
- ,,,.Expanding the roles of hospitalist physicians to include public health.J Hosp Med.2007;2:93–101.
- The Joint Commission on Accreditation of Healthcare Organizations Comprehensive Accreditation Manual for Hospitals: The Official Handbook. January2007. p.152
- ,,,.Need for change in patient education: a Finnish survey from the patient's perspective.Patient Educ Couns.2003;51:239–245.
- ,.Randomized controlled trial of smoking cessation intervention after admission for coronary heart disease.BMJ.2003;327:1254–1257.
- .Treatment of tobacco use and dependence.N Engl J Med.2002;346:506–512.
- ,, et al.A clinical practice guideline for treating tobacco use and dependence: a US Public Health Service report.JAMA.2000;283:3244–3254.
- ,,, et al.National Institutes of Health state‐of‐the science conference statement: tobacco use: prevention, cessation and control.Ann Intern Med.2006;145:839–844.
- ,,.What do discharged patients know about their medications?Patient Educ Couns.2005;56:276–282.
- Joint Commission on Accreditation of Healthcare Organizations.A Comprehensive Review for the Development and Testing for National Implementation of Hospital Core Measures.2006:1–40.
- .ACC/AHA 2005 guideline update for the diagnosis and management of chronic heart failure in the adult: a report of the American College of Cardiology/ American Heart Association task force on practice guidelines.J Am Coll Cardiol.2005;46:1–82.
- JCAHO data. Available: https://cimprod.uhc.edu/CoreMeasures/Products/DownloadSystem/WebPages/ViewReportsDownloadList.aspx.
- .Integrating patient teaching into bedside patient care: a participant‐observation study of hospital nurses.Patient Educ Couns.2002;48:107–113.
- .Health promotion in the acute hospital setting: the receptivity of adult in‐patients.Patient Educ Couns.2004;54:73–78.
- ,,,,,.Randomized trial of a patient‐centered hospital unit.Patient Educ Couns.1998;34:125–133.
- ,,,,,.Deficits in communication and information transfer between hospital‐based and primary care physicians: implications for patient safety and continuity of care. HYPERLINK “javascript:AL_get(this,%20'jour',%20'JAMA.');”JAMA.2007;297:831–841.
- ,,,,.Frequency of new or worsening symptoms in the posthospitalization period.J Hosp Med.2007;2:58–68.
- ,,,.Patient self‐management of chronic disease in primary care.JAMA.2002;288:2469–2475.
- ,,.Effectiveness of self‐management training in type 2 diabetes.Diabetes Care.2001;24:561–587.
- ,,.Quality of life assessment after patient education a randomized controlled study on asthma and chronic obstructive pulmonary disease.Am J Respir Crit Care Med.2001;95:56–63.
- ,.The effects of a health educational and exercise program for older adults with osteoarthritis for the hip or knee.J Rheumatol.1997;24:1378–1383.
- ,,,.Expanding the roles of hospitalist physicians to include public health.J Hosp Med.2007;2:93–101.
- The Joint Commission on Accreditation of Healthcare Organizations Comprehensive Accreditation Manual for Hospitals: The Official Handbook. January2007. p.152
- ,,,.Need for change in patient education: a Finnish survey from the patient's perspective.Patient Educ Couns.2003;51:239–245.
Copyright © 2008 Society of Hospital Medicine