User login
Postpartum Depression Screening
Maternal postpartum depression occurs in 5% to 25% of all mothers, and up to 40% to 60% in high‐risk populations such as low‐income women.[1, 2, 3, 4] Children of affected mothers suffer negative health consequences such as decreased physical growth, poor maternalchild bond, problem behavior, and child abuse.[5, 6, 7] Timely recognition of symptoms and treatment may improve child outcomes.[8] Published guidelines recommend pediatricians screen for postpartum depression at infant 1‐, 2‐, 4‐, and 6‐month outpatient visits.[9] There are no current guidelines for or studies of screening in general inpatient settings, although emergency rooms[10] and neonatal intensive care units (NICUs)[11] have been examined. Pediatric hospitalization may offer an additional opportunity for expanding screening and intervention.
Augmenting outpatient screening practices with additional inpatient screening would have several benefits. Infant health problems have been associated with postpartum depression, and therefore mothers in the hospital may be at higher risk.[12] Inpatient screening would also improve access to mothers not screened as outpatients. Missed screening could occur due to physician discomfort with screening, time constraints during busy office visits, or noncompliance with recommended visit schedules.[13, 14, 15, 16] Finally, inpatient providers would benefit from understanding the psychosocial milieu of children now under their care. Recent studies note hospital discharges may be improved and readmissions reduced by assessing socioeconomic risk factors during hospitalization.[17] The evidence‐based Peds Effective Discharge: Better Handoff to Home through Safer Transitions Better Outcomes by Optimizing Safe Transitions (Pedi‐BOOST) toolkit specifically recommends an assessment of parental psychiatric issues.[18] Postpartum depression strongly correlates with impaired maternalchild bonding,[19] which in turn negatively affects mothers' engagement with healthcare providers.[20] This could impact patient education and recommendations provided during hospitalization.
Therefore, we sought to perform postpartum depression screening during infant hospitalizations. Our primary goal was to determine rate of postpartum depression in our population and proportion of women previously unscreened who could be captured by inpatient screening. We additionally aimed to determine the proportion of women with poor maternalinfant bond. Our next goal was to identify maternal or infant factors associated with positive postpartum depression screening. Finally, we performed follow‐up calls to determine if in‐hospital interventions resulted in formal postpartum depression diagnosis, use of recommended referrals, improved maternalchild bond, and decreased symptoms of depression over time.
METHODS
Patient Selection
We conducted a prospective observational study on a convenience sample of mothers at Children's Hospital Los Angeles (CHLA), a large, urban, tertiary care hospital. Biological mothers of infants 1 year of age admitted to medicalsurgical floors and assigned to pediatric hospitalist teams between April 1, 2013 and July 30, 2014 were eligible for inclusion. Mothers were required to be age 18 years or older and able to speak and read English or Spanish. Mothers of infants aged 2 weeks were excluded to avoid confusing postpartum depression with maternal baby blues, a distinct entity causing milder symptoms of depression that should resolve by 2 weeks.[21] In an effort to reduce the impact of stress associated with prolonged hospitalization on Edinburgh Postpartum Depression Scale (EPDS) scores, we excluded mothers of children already hospitalized >72 hours. Visits from participants who were readmitted or previously enrolled in the study were excluded. All study procedures were approved by the CHLA Institutional Review Board.
Measures
After giving informed consent, mothers completed demographic forms about themselves and their infants. A 4‐item Likert scale assessed self‐perceived support from family and friends. Past mental health problems were assessed via 10‐item checklist. Self‐reported infant comorbidities and reason for hospitalization were confirmed by chart review for International Classification of Diseases, Ninth Revision diagnoses present on admission and reason for discharge. Next, mothers filled out a maternalinfant bonding scale (MIB)[22] and the EPDS,[23, 24] which has been validated in both English and Spanish.[25] There are no formal cutoffs for the MIB; higher scores indicate worse bonding. Out of a possible 30, a score of 10 or higher on the EPDS was considered a positive screen, indicating risk for postpartum depression. Scores less than 10 were negative screens, and those mothers were determined not at risk.[24] The last EPDS question asks, The thought of harming myself has occurred to me. Any mothers answering yes, quite often, sometimes, or hardly ever were further interviewed and treated per a suicidality operating protocol.
Counseling and Referral
All EPDS mothers were informed of results and did not receive further intervention during hospitalization. For EPDS+ mothers, individual social workers responded to referrals placed by the study team into infant charts and delivered 1‐on‐1 counseling. Social workers received study education prior to initiation and midway through patient recruitment and provided mothers with an educational handout, referral sheet listing online resources of local mental health clinics accepting postpartum depression patients, and help‐line numbers. Mothers who identified a primary doctor were encouraged to follow up with them.
Follow‐up
In order to assess intervention effect over time, all mothers (both EPDS+ and EPDS) were called 3 and 6 months ( 1 week) postenrollment and rescreened with the EPDS and MIB. They also answered a short survey assessing whether they spoke further to a doctor about postpartum depression; used a referral resource; received a formal postpartum depression diagnosis; and if their children visited the ER, urgent care, or hospital again since discharge. Mothers who again screened EPDS+ or newly converted to EPDS+ were provided counseling and referral via phone.
Sample Size Calculation
A priori power analysis determined a sample size of 310 mothers was required to estimate the rate of postpartum depression at CHLA with 5% precision and a 95% confidence level, assuming an estimated prevalence of 27.9% based on prior studies.[26] At this prevalence rate, screening 310 mothers was also predicted to yield at least 77 positive screens on the EPDS, yielding an appropriate sample to detect EPDS score improvements over time. This number was based on previous studies showing reduction in EPDS of 35% following appropriate referral,[26, 27] assuming 15% attrition at both the 3‐month and 6‐month follow‐up sampling points.
Statistical Analysis
After data collection was complete, characteristics between EPDS+ and EPDS groups were compared using 2 tests for dichotomous outcomes and t tests for continuous variables. Multiple logistic regression was then used to compare specific factors associated with positive EPDS screens (P 0.05). Linear regression assessed the relationship between EPDS and MIB scores. Change in average EPDS and MIB scores at the time of first successful follow‐up call between women who did and did not seek further postpartum depression evaluation were compared via 2‐way repeated measures analysis of variance. Statistical analyses were performed using R software.[28]
RESULTS
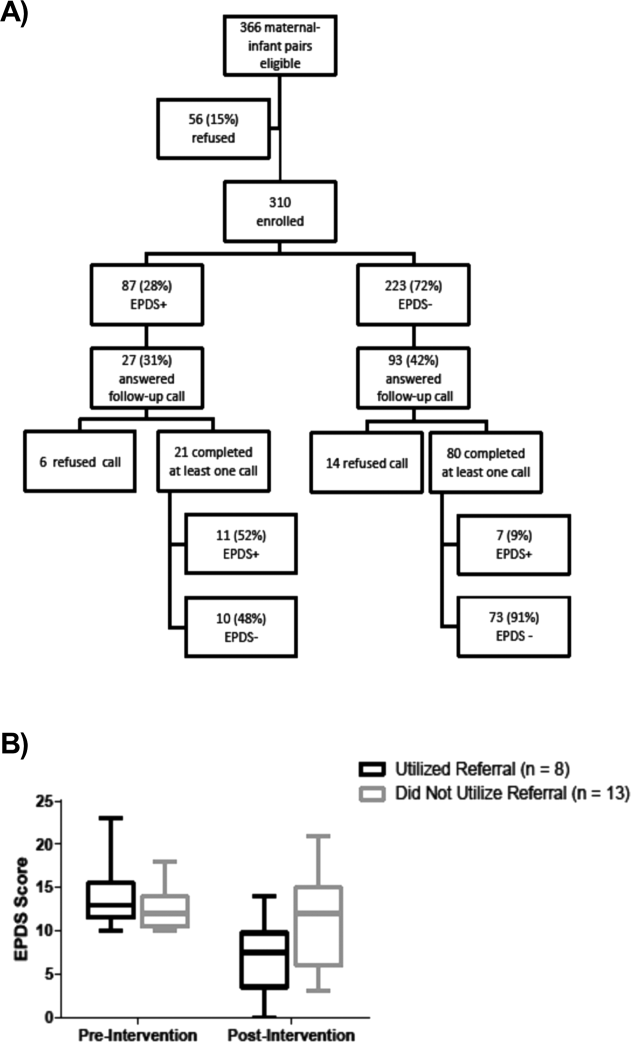
Out of 366 motherinfant pairs, 56 (15%) refused, and 310 (85%) mothers were fully enrolled (Figure 1A). Mothers had an average age of 28.17 years, were 68.3% Hispanic/Latina by self‐report, and 45.2% were married. Infants were an average of 4.24 months old, 81.9% were born term (>37 weeks), and 64.8% were previously healthy (Table 1).
| Characteristic | All Participants, n = 310 |
|---|---|
| |
| Maternal characteristics | |
| Age, y* | 28.17 6.18 |
| Race/ethnicity | |
| White | 48 (15.5%) |
| Black | 25 (8.1%) |
| Hispanic | 211(68.3%) |
| Other | 25 (8.1%) |
| EPDS language | |
| English | 231 (74.5%) |
| Spanish | 79 (25.5%) |
| People in home | 5 (4, 6) |
| No. of children | 2 (1, 3) |
| Relationship | |
| Married | 140 (45.2%) |
| In a relationship | 105 (33.9%) |
| Single | 62 (20%) |
| Any breastfeeding | 142 (45.8%) |
| Unsupportive social network | 54 (17.4%) |
| Some psychiatric disorder | 47 (15.2%) |
| MIB score | 6 (3, 10) |
| Infant characteristics | |
| Age, mo* | 4.24 3.19 |
| Gestational age, wk | 39 (37, 40) |
| Prior admission | 113 (36.5%) |
| Any comorbidity | 109 (35.2%) |
| Congenital heart disease | 27 (8.7%) |
| Neurodevelopmental | 22 (7.1%) |
| Any medical device needed | 38 (12.3%) |

(B) Postenrollment change in mean Edinburgh Postpartum Depression Scale (EPDS) score of all initially EPDS mothers who completed at least 1 follow‐up phone call, separated by if they did or did not seek referral. Mothers using referral (either spoke with physician or used resource sheet) had significantly larger reduction in score. Statistical analysis by analysis of variance, P < 0.05.
Eighty‐seven (28%) mothers were EPDS+; 223 (72%) were EPDS. Only 42 mothers reported previous postpartum depression screening since the birth of their most recent child. However, 30 infants were 1 month in age, thus outside recommended screening range. Eliminating these infants revealed a 14.6% rate of appropriate prior screening. Higher EPDS scores were associated with higher (worse) MIB scores by linear regression ( = 0.11, P 0.001). The vast majority (77%) of mothers scored a 0 or 1 on the MIB scale, indicating good bonding; further statistical comparison using the MIB scale as a secondary outcome was therefore inappropriate.
On bivariate logistic regression, Hispanic/Latina women were less likely to be EPDS+ (odds ratio [OR]: 0.43; 95% CI: 0.23‐0.84) compared to white/Caucasian women. Mothers who identified Spanish as their primary language and took the Spanish EPDS had lower odds of a positive screen (OR: 0.47; 95% CI: 0.25‐0.88). The racial differences did not persist on multivariate analysis (OR: 0.64; 95% CI: 0.30‐1.38) (Table 2). Maternal characteristics identified as potential risk factors for positive screens were poor social support (OR: 3.58; 95% CI: 1.95‐6.59) and history of a prior psychiatric diagnosis (OR: 5.07; 95% CI: 2.65‐9.72). There were no differences in age, number of children or people living in the home, relationship status, or breastfeeding rates by EPDS score.
| OR | 95% CI | P Value | |
|---|---|---|---|
| |||
| Maternal characteristics | |||
| Maternal age | 0.99 | 0.95‐1.03 | 0.660 |
| Race | |||
| White | Reference | ||
| Black | 0.93 | 0.35‐2.50 | 0.891 |
| Hispanic | 0.43 | 0.23‐0.84 | 0.013 |
| Other | 0.54 | 0.19‐1.55 | 0.254 |
| EPDS language | 0.47 | 0.25‐0.88 | 0.020 |
| People in home | 1.02 | 0.89‐1.16 | 0.799 |
| No. of children | 1.02 | 0.85‐1.23 | 0.819 |
| Relationship | |||
| Married | Reference | ||
| In a relationship | 0.93 | 0.52‐1.65 | 0.802 |
| Single | 1.37 | 0.72‐2.62 | 0.333 |
| Unsupportive social network | 3.58 | 1.95‐6.59 | 0.0001 |
| Some psychiatric disorder | 5.07 | 2.65‐9.72 | 0.0001 |
| Infant characteristics | |||
| Gestational age | 0.96 | 0.87‐1.04 | 0.316 |
| Prior admission | 0.83 | 0.49‐1.39 | 0.476 |
| Any comorbidity | 1.03 | 0.92‐1.18 | 0.551 |
| Congenital heart disease | 1.87 | 0.83‐4.22 | 0.130 |
| Neurodevelopmental | 3.41 | 1.41‐8.21 | 0.006 |
| Any medical device needed | 1.59 | 0.78‐3.24 | 0.201 |
| Multivariate logistic regression | |||
| Race | |||
| White | Reference | ||
| Black | 0.87 | 0.28‐2.70 | 0.812 |
| Hispanic | 0.64 | 0.30‐1.38 | 0.258 |
| Other | 0.88 | 0.29‐2.74 | 0.831 |
| Unsupportive social network | 4.40 | 2.27‐8.53 | 0.0001 |
| Psychiatric disorder | 5.02 | 2.49‐10.15 | 0.0001 |
| Neurodevelopmental comorbidity | 2.78 | 1.03‐7.52 | 0.004 |
Infant characteristics were next examined. Children of EPDS+ and EPDS mothers were similar in age, number of prior hospital admissions, gestational age at birth, and overall use of medical equipment (Table 2). To examine the effect of illness leading to hospitalization on EPDS+ risk, discharge diagnoses were collected and grouped into categories. Infants of EPDS+ mothers were more likely hospitalized for neurologic illness (P = 0.008) (see Supporting Table 1 in the online version of this article), but otherwise similar.
We next compared differences in long‐term infant comorbidities. The rate of having any comorbidity was similar between children of EPDS+ and EPDS mothers (39.1% vs 33.6%; P = 0.551). However, children of EPDS+ mothers were more likely to have mental retardation, hydrocephalus, or require ventriculoperitoneal shunt (VPS); however, the overall number of infants with each comorbidity was low. A neurodevelopmental comorbidity variable was created combining mental retardation, cerebral palsy, epilepsy, hydrocephalus, craniosynostosis, and VPS, resulting in 22 (7.1%) unique infants with 1 or more of these conditions. Having an infant with a neurodevelopmental comorbidity was a risk factor for positive postpartum depression screen (OR: 3.41; 95% CI: 1.41‐8.21). This continued to be significant (OR: 2.78; 95% CI: 1.03‐7.52) (Table 2) when controlling for maternal race/ethnicity, psychiatric history, and social support in multivariate logistic regression.
To determine if women screened followed through with recommendations, participants were called 3 and 6 months postenrollment. We attempted to call all women and successfully reached 120; 19 (16%) refused the call. One hundred one of the original 310 enrolled (33%) completed at least 1 follow‐up call; 47 at 3 months, 40 at 6 months, and only 14 (14%) responded at both time points. Due to this response rate, the first call at either 3 or 6 months was used as a single follow‐up time point for statistical analysis. A slightly higher proportion of EPDS‐ mothers (80/223, 36%) completed calls compared to EPDS+ mothers (21/87, 24%; P = 0.047).
Of 21 mothers initially EPDS+ who completed a follow‐up call, 10 (48%) later screened negative. Seven of these 10 (70%) reported discussing postpartum depression with their physician or using provided referral resources in the interim; 1 woman both spoke to a doctor and used a referral resource. One additional woman used resources, but repeat EPDS was still positive (Table 3). Reasons cited for not seeking evaluation included too busy (n = 4) and lost paperwork (n = 1), or no reason was given (n = 2). Mothers utilizing appropriate follow‐up had reduction in scores compared to those not (F(1,19) = 5.743, P = 0.027), although all scores decreased over time (F(1,19) = 11.54, P = 0.0030) (Figure 1B).
| Changes in Characteristics Following Enrollment | Positive EPDS, N = 21 | Negative EPDS, N = 80 | P Value |
|---|---|---|---|
| |||
| Repeat EPDS negative | 10 (47.6%) | 73 (91.3%) | 0.001 |
| Spoke to a doctor about PD | 6 (28.6%) | 27 (33.7%) | 0.360 |
| Used a study referral resource | 3 (14.3%) | NA | |
| Received a formal diagnosis of PD | 1 (4.7%) | 1 (1.3%) | 0.325 |
| Healthcare utilization* | |||
| No. of ER visits | 0 (00.5) | 0 (02) | 0.074 |
| No. of urgent care visits | 0 (00.5) | 0 (00) | 0.136 |
| No. of hospitalizations | 0 (00) | 0 (01) | 0.021 |
| Repeat MIB score | 1.09 0.38 | 0.69 0.17 | 0.357 |
Of 80 women initially EPDS, most stayed negative (73/80, 91%), but 7 (9%) became EPDS+. These mothers received education and referral information over the phone, but none completed a subsequent call. Infants of mothers initially EPDS had a higher frequency of hospitalization postenrollment compared to EPDS+ mothers (P = 0.021) (Table 3). Two (33%) mothers who converted from EPDS to EPDS+ had infants readmitted in the follow‐up period.
DISCUSSION
This study demonstrated almost a third of mothers of hospitalized infants are at risk for postpartum depression and most had not been previously screened. Stress due to hospitalization did not seem to falsely elevate EPDS scores; the proportion of EPDS+ mothers matched our prestudy prediction (28% vs 27.9%). Follow‐up calls indicated that EPDS+ mothers not pursuing further evaluation tended to remain EPDS+. Higher (worse) MIB score was strongly correlated to increased EPDS score as expected, supporting screening accuracy. Our results suggest that postpartum depression screening in hospital settings can be used to complement outpatient practice and capture mothers who would otherwise be missed.
Although we were able to screen, it is difficult to know whether this correctly identified mothers with postpartum depression. Only 2 mothers reported subsequent official diagnosis of postpartum depression, and 1 of these was EPDS originally. This reflects weakness of our survey‐based design; we only know if the mother self‐reported a formal diagnosis of postpartum depression, because we do not have access to their medical charts. We also had higher than expected loss to follow up (67%), leaving 66 initially EPDS+ mothers with unknown eventual diagnoses. The EPDS has been validated in multiple populations and has a positive predictive value ranging from 23% to 93%.[23] Therefore, somewhere between 20 and 80 women in our study should meet diagnostic criteria for postpartum depression. A limitation of children's hospital‐based screening with the EPDS is lack of adult‐trained psychiatrists who could immediately follow screening with diagnosis. Such integration may already be possible at community or hospital‐within‐a‐hospital models, and could be trialed at children's hospitals. Regardless, participation in the study seemed to increase mothers' awareness of postpartum depression. Prior to enrollment, only 14.6% of subjects reported discussing postpartum depression with a physician, although recall bias likely contributed to some mothers not remembering a screen. Promisingly, on follow‐up, 37% of called participants reported they discussed postpartum depression with a doctor following their child's hospital discharge.
Our study identified low social support and history of past psychiatric diagnosis as maternal risk factors for EPDS+ screens, which is consistent with previous reports.[29] There was a slight increase in subsequent infant hospitalizations in the EPDS group, which is contrary to reports stating that increased healthcare utilization is associated with postpartum depression.[30] However, most studies have shown an increase in only acute or emergency room care visits[30, 31] and no association between maternal depression and infant hospitalization.[30, 32] In our study, the median number of hospitalizations for both groups was 0, indicating overall low utilization. Because 2 of the mothers who converted from EPDS to EPDS+ had children readmitted, this underscores the benefit of reassessment at each medical encounter. A large proportion of mothers (36.5%) reported that the infant had been previously hospitalized, adding another potential missed screening opportunity. Our study supports others advocating repeated screenings and suggests mothers should be screened at any medical encounter that occurs in the first postpartum year.
We identified neurodevelopmental illness as the major infant characteristic associated with postpartum depression risk. Conversely, Garfield et al. did not find correlation between poorer Neurobiologic Risk Score and increased maternal depression risk in a NICU setting.[11] Perhaps our population of older and mainly full‐term infants makes consequences of neurologic insult more obvious and affects mothers more significantly. Cheng et al. reported that 26.9% of mothers of children with cognitive delay reported high depressive symptoms, compared with 17.4% of mothers of typically developing children at 4 years of age.[33] Another body of evidence suggests maternal emotional state during pregnancy influences neurodevelopmental outcome in the child. Maternal anxiety or depression has been associated with altered placental function, reduced infant gray matter density, and worse cognitive function.[34, 35] Therefore, future research may focus on mothers of infants with neurodevelopmental disease to better understand this relationship.
There were several limitations to this study. Some data collected by a survey are subject to information bias. Women may report a more supportive social network than actually exists or omit history of mental health diagnoses. We attempted to control for this by using validated measures where possible and performing chart review to verify reported infant characteristics. Our population was overwhelmingly Hispanic/Latina, and a third of infants were not previously healthy, which limits applicability to other settings. We used a convenience method that could introduce sampling bias. Our hospital's overall patient demographic is 65% Hispanic, which is similar to the 68% sampled in our study. In addition, the proportions of infant diagnoses approximate the overall rates at CHLA, so we feel our sample was fairly representative. There is a general consensus that depression studies have recruitment difficulties.[36] In the unlikely event that all 56 of women who declined to participate were EPDS+, overall proportion of at‐risk mothers would rise to 39%. If our study does show slight underestimation of risk, that would only mean more potential for intervention if screening were mandatory. Another weakness was high loss to follow‐up, which led us to combine the 3‐ and 6‐month follow‐up calls into 1 outcome. Sixty percent of calls used in analysis occurred at 3 months, so long‐term maintenance of improved EPDS scores remains unclear. Although conducting repeat EPDS via phone may affect honest answering of sensitive questions, other studies have used this technique successfully.[4]
CONCLUSION
This is the first study evaluating a screening program for maternal postpartum depression during infant hospitalizations. In our population, risk factors for positive postpartum depression screening were low social support, history of maternal psychiatric diagnosis, and having an infant with neurodevelopmental disease. We believe mothers should receive postpartum depression screening at all medical encounters during the child's first year.
Acknowledgements
The authors thank the CHLA Department of Social Work and the USC Required Scholarly Projects program, and specifically Joseph DeSena and Humberto Avila, for project assistance.
Disclosures: Dr. Trost is an Institutional Career Development Program Scholar through the Southern California Clinical and Translational Science Institute (SC‐CTSI) at the University of Southern California Keck School of Medicine. The content is solely the responsibility of the author(s) and does not represent the official view of the SC‐CTSI. Dr. Trost conceptualized and designed the study, drafted the initial manuscript, and approved the final manuscript as submitted. Dr. Molas‐Torreblanca co‐designed the study, reviewed and revised the manuscript, and approved the final manuscript as submitted. Ms. Man coordinated and supervised hospital data collection, critically reviewed the manuscript, and approved the final manuscript as submitted. Mr. Casillas coordinated and supervised the phone call data collection, critically reviewed the manuscript, and approved the final manuscript as submitted. Ms. Sapir coordinated the referral process for enrolled patients, supervised the design of patient handouts, and critically reviewed and approved the final manuscript as submitted. Dr. Schrager guided study design, supervised the statistical analysis of the final data, critically reviewed and revised the manuscript, and approved the final manuscript as submitted. The authors report no conflicts of interest.
- , , , , . Maternal depressive symptoms and infant health practices among low‐income women. Pediatrics. 2004;113(6):e523–e529.
- , , , et al.; Duke University Evidence‐based Practice Center. Effective Health Care Program. Efficacy and safety of screening for postpartum depression. Comparative effectiveness review number 106. Rockville, MD: Agency for Healthcare Research and Quality, U.S. Department of Health and Human Services; 2013: Available at: https://www.effectivehealthcare.ahrq.gov/ehc/products/379/1437/postpartum‐screening‐report‐130409.pdf. Date accessed Jan 10 2016.
- , , , , . Prevalence rates and demographic characteristics associated with depression in pregnancy and the postpartum. J Consult Clin Psychol. 1989;57(2):269–274.
- , , , , . Screening for depression in the postpartum period: a comparison of three instruments. J Womens Health (Larchmt). 2008;17(4):585–596.
- , , , . Are maternal depression or symptom severity associated with breastfeeding intention or outcomes? J Clin Psychiatry. 2010;71(8):1069–1078.
- , , , , . Impact of maternal depressive symptoms on growth of preschool‐ and school‐aged children. Pediatrics. 2012;130(4):e847–e855.
- , , , , . The timing of maternal depressive symptoms and mothers' parenting practices with young children: implications for pediatric practice. Pediatrics. 2006;118(1):e174–e182.
- , , , , . Improvements in maternal depression as a mediator of intervention effects on early childhood problem behavior. Dev Psychopathol. 2009;21(2):417–439.
- ; Committee on Psychosocial Aspects of Child and Family Health American Academy of Pediatrics. Incorporating recognition and management of perinatal and postpartum depression into pediatric practice. Pediatrics. 2010;126(5):1032–1039.
- , , . Screening for postpartum depression in a pediatric emergency department. Pediatr Emerg Care. 2011;27(9):795–800.
- , , , et al. Risk factors for postpartum depressive symptoms in low‐income women with very low‐birth‐weight infants. Adv Neonatal Care. 2015;15(1):E3–E8.
- , , . Impact of infant health problems on postnatal depression: pilot study to evaluate a health visiting system. Psychiatry Clin Neurosci. 2006;60(2):182–189.
- , , , , , . Primary care pediatricians' roles and perceived responsibilities in the identification and management of maternal depression. Pediatrics. 2002;110(6):1169–1176.
- , , , et al. Does education influence pediatricians' perceptions of physician‐specific barriers for maternal depression? Clin Pediatr (Phila). 2008;47(7):670–678.
- , , , . Pediatricians' views of postpartum depression: a self‐administered survey. Arch Womens Ment Health. 2004;7(4):231–236.
- . Compliance with well‐child visit recommendations: evidence from the Medical Expenditure Panel Survey, 2000–2002. Pediatrics. 2006;118(6):e1766–e1778.
- , , , et al. A framework of pediatric hospital discharge care informed by legislation, research, and practice. JAMA Pediatr. 2014;168(10):955–962; quiz 965–966.
- , , . Pedi‐BOOST. Peds Effective Discharge: Better Handoff to Home through Safer Transitions. 2013. https://www.hospitalmedicine.org/Web/Quality___Innovation/Implementation_Toolkit/pediBoost/Best_Practices/Best_Practices.aspx Accessed Jan 10 2016.
- , , , et al. Effects of maternal depressive symptomatology during pregnancy and the postpartum period on infant‐mother attachment. Psychiatry Clin Neurosci. 2014;68(8):631–639.
- , , , , . Examining maternal depression and attachment insecurity as moderators of the impacts of home visiting for at‐risk mothers and infants. J Consult Clin Psychol. 2009;77(4):788–799.
- , . Postpartum mood disorders: diagnosis and treatment guidelines. J Clin Psychiatry. 1998;59(suppl 2):34–40.
- , , , , . A new Mother‐to‐Infant Bonding Scale: links with early maternal mood. Arch Womens Ment Health. 2005;8(1):45–51.
- , , , , . A systematic review of studies validating the Edinburgh Postnatal Depression Scale in antepartum and postpartum women. Acta Psychiatr Scand. 2009;119(5):350–364.
- , , . Detection of postnatal depression. Development of the 10‐item Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1987;150:782–786.
- , , , . Validation of the Edinburgh Postnatal Depression Scale (EPDS) in Spanish mothers. J Affect Disord. 2003;75(1):71–76.
- , , , et al. TRIPPD: a practice‐based network effectiveness study of postpartum depression screening and management. Ann Fam Med. 2012;10(4):320–329.
- , , , , . Detection of postpartum depressive symptoms by screening at well‐child visits. Pediatrics. 2004;113(3 pt 1):551–558.
- R Core Team. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing: 2013. Available at: http://www.R‐project.org. Accessed Jan 10 2016.
- , , , , . Biological and psychosocial predictors of postpartum depression: systematic review and call for integration. Annu Rev Clin Psychol. 2015;11:99–137.
- , , , et al. Maternal depressive symptoms and children's receipt of health care in the first 3 years of life. Pediatrics. 2005;115(2):306–314.
- , . Maternal factors and child's health care use. Soc Sci Med. 1995;40(5):623–628.
- , , , , . Women's health after pregnancy and child outcomes at age 3 years: a prospective cohort study. Am J Public Health. 2002;92(8):1312–1318.
- , , , . The influence of children's cognitive delay and behavior problems on maternal depression. J Pediatr. 2015;167(3):679–686.
- , , , , . Maternal prenatal symptoms of depression and down regulation of placental monoamine oxidase A expression. J Psychosom Res. 2013;75(4):341–345.
- , , , , . High pregnancy anxiety during mid‐gestation is associated with decreased gray matter density in 6–9‐year‐old children. Psychoneuroendocrinology. 2010;35(1):141–153.
- , , , , . Factors affecting recruitment into depression trials: Systematic review, meta‐synthesis and conceptual framework. J Affect Disord. 2015;172:274–290.
Maternal postpartum depression occurs in 5% to 25% of all mothers, and up to 40% to 60% in high‐risk populations such as low‐income women.[1, 2, 3, 4] Children of affected mothers suffer negative health consequences such as decreased physical growth, poor maternalchild bond, problem behavior, and child abuse.[5, 6, 7] Timely recognition of symptoms and treatment may improve child outcomes.[8] Published guidelines recommend pediatricians screen for postpartum depression at infant 1‐, 2‐, 4‐, and 6‐month outpatient visits.[9] There are no current guidelines for or studies of screening in general inpatient settings, although emergency rooms[10] and neonatal intensive care units (NICUs)[11] have been examined. Pediatric hospitalization may offer an additional opportunity for expanding screening and intervention.
Augmenting outpatient screening practices with additional inpatient screening would have several benefits. Infant health problems have been associated with postpartum depression, and therefore mothers in the hospital may be at higher risk.[12] Inpatient screening would also improve access to mothers not screened as outpatients. Missed screening could occur due to physician discomfort with screening, time constraints during busy office visits, or noncompliance with recommended visit schedules.[13, 14, 15, 16] Finally, inpatient providers would benefit from understanding the psychosocial milieu of children now under their care. Recent studies note hospital discharges may be improved and readmissions reduced by assessing socioeconomic risk factors during hospitalization.[17] The evidence‐based Peds Effective Discharge: Better Handoff to Home through Safer Transitions Better Outcomes by Optimizing Safe Transitions (Pedi‐BOOST) toolkit specifically recommends an assessment of parental psychiatric issues.[18] Postpartum depression strongly correlates with impaired maternalchild bonding,[19] which in turn negatively affects mothers' engagement with healthcare providers.[20] This could impact patient education and recommendations provided during hospitalization.
Therefore, we sought to perform postpartum depression screening during infant hospitalizations. Our primary goal was to determine rate of postpartum depression in our population and proportion of women previously unscreened who could be captured by inpatient screening. We additionally aimed to determine the proportion of women with poor maternalinfant bond. Our next goal was to identify maternal or infant factors associated with positive postpartum depression screening. Finally, we performed follow‐up calls to determine if in‐hospital interventions resulted in formal postpartum depression diagnosis, use of recommended referrals, improved maternalchild bond, and decreased symptoms of depression over time.
METHODS
Patient Selection
We conducted a prospective observational study on a convenience sample of mothers at Children's Hospital Los Angeles (CHLA), a large, urban, tertiary care hospital. Biological mothers of infants 1 year of age admitted to medicalsurgical floors and assigned to pediatric hospitalist teams between April 1, 2013 and July 30, 2014 were eligible for inclusion. Mothers were required to be age 18 years or older and able to speak and read English or Spanish. Mothers of infants aged 2 weeks were excluded to avoid confusing postpartum depression with maternal baby blues, a distinct entity causing milder symptoms of depression that should resolve by 2 weeks.[21] In an effort to reduce the impact of stress associated with prolonged hospitalization on Edinburgh Postpartum Depression Scale (EPDS) scores, we excluded mothers of children already hospitalized >72 hours. Visits from participants who were readmitted or previously enrolled in the study were excluded. All study procedures were approved by the CHLA Institutional Review Board.
Measures
After giving informed consent, mothers completed demographic forms about themselves and their infants. A 4‐item Likert scale assessed self‐perceived support from family and friends. Past mental health problems were assessed via 10‐item checklist. Self‐reported infant comorbidities and reason for hospitalization were confirmed by chart review for International Classification of Diseases, Ninth Revision diagnoses present on admission and reason for discharge. Next, mothers filled out a maternalinfant bonding scale (MIB)[22] and the EPDS,[23, 24] which has been validated in both English and Spanish.[25] There are no formal cutoffs for the MIB; higher scores indicate worse bonding. Out of a possible 30, a score of 10 or higher on the EPDS was considered a positive screen, indicating risk for postpartum depression. Scores less than 10 were negative screens, and those mothers were determined not at risk.[24] The last EPDS question asks, The thought of harming myself has occurred to me. Any mothers answering yes, quite often, sometimes, or hardly ever were further interviewed and treated per a suicidality operating protocol.
Counseling and Referral
All EPDS mothers were informed of results and did not receive further intervention during hospitalization. For EPDS+ mothers, individual social workers responded to referrals placed by the study team into infant charts and delivered 1‐on‐1 counseling. Social workers received study education prior to initiation and midway through patient recruitment and provided mothers with an educational handout, referral sheet listing online resources of local mental health clinics accepting postpartum depression patients, and help‐line numbers. Mothers who identified a primary doctor were encouraged to follow up with them.
Follow‐up
In order to assess intervention effect over time, all mothers (both EPDS+ and EPDS) were called 3 and 6 months ( 1 week) postenrollment and rescreened with the EPDS and MIB. They also answered a short survey assessing whether they spoke further to a doctor about postpartum depression; used a referral resource; received a formal postpartum depression diagnosis; and if their children visited the ER, urgent care, or hospital again since discharge. Mothers who again screened EPDS+ or newly converted to EPDS+ were provided counseling and referral via phone.
Sample Size Calculation
A priori power analysis determined a sample size of 310 mothers was required to estimate the rate of postpartum depression at CHLA with 5% precision and a 95% confidence level, assuming an estimated prevalence of 27.9% based on prior studies.[26] At this prevalence rate, screening 310 mothers was also predicted to yield at least 77 positive screens on the EPDS, yielding an appropriate sample to detect EPDS score improvements over time. This number was based on previous studies showing reduction in EPDS of 35% following appropriate referral,[26, 27] assuming 15% attrition at both the 3‐month and 6‐month follow‐up sampling points.
Statistical Analysis
After data collection was complete, characteristics between EPDS+ and EPDS groups were compared using 2 tests for dichotomous outcomes and t tests for continuous variables. Multiple logistic regression was then used to compare specific factors associated with positive EPDS screens (P 0.05). Linear regression assessed the relationship between EPDS and MIB scores. Change in average EPDS and MIB scores at the time of first successful follow‐up call between women who did and did not seek further postpartum depression evaluation were compared via 2‐way repeated measures analysis of variance. Statistical analyses were performed using R software.[28]
RESULTS
Out of 366 motherinfant pairs, 56 (15%) refused, and 310 (85%) mothers were fully enrolled (Figure 1A). Mothers had an average age of 28.17 years, were 68.3% Hispanic/Latina by self‐report, and 45.2% were married. Infants were an average of 4.24 months old, 81.9% were born term (>37 weeks), and 64.8% were previously healthy (Table 1).
| Characteristic | All Participants, n = 310 |
|---|---|
| |
| Maternal characteristics | |
| Age, y* | 28.17 6.18 |
| Race/ethnicity | |
| White | 48 (15.5%) |
| Black | 25 (8.1%) |
| Hispanic | 211(68.3%) |
| Other | 25 (8.1%) |
| EPDS language | |
| English | 231 (74.5%) |
| Spanish | 79 (25.5%) |
| People in home | 5 (4, 6) |
| No. of children | 2 (1, 3) |
| Relationship | |
| Married | 140 (45.2%) |
| In a relationship | 105 (33.9%) |
| Single | 62 (20%) |
| Any breastfeeding | 142 (45.8%) |
| Unsupportive social network | 54 (17.4%) |
| Some psychiatric disorder | 47 (15.2%) |
| MIB score | 6 (3, 10) |
| Infant characteristics | |
| Age, mo* | 4.24 3.19 |
| Gestational age, wk | 39 (37, 40) |
| Prior admission | 113 (36.5%) |
| Any comorbidity | 109 (35.2%) |
| Congenital heart disease | 27 (8.7%) |
| Neurodevelopmental | 22 (7.1%) |
| Any medical device needed | 38 (12.3%) |

(B) Postenrollment change in mean Edinburgh Postpartum Depression Scale (EPDS) score of all initially EPDS mothers who completed at least 1 follow‐up phone call, separated by if they did or did not seek referral. Mothers using referral (either spoke with physician or used resource sheet) had significantly larger reduction in score. Statistical analysis by analysis of variance, P < 0.05.
Eighty‐seven (28%) mothers were EPDS+; 223 (72%) were EPDS. Only 42 mothers reported previous postpartum depression screening since the birth of their most recent child. However, 30 infants were 1 month in age, thus outside recommended screening range. Eliminating these infants revealed a 14.6% rate of appropriate prior screening. Higher EPDS scores were associated with higher (worse) MIB scores by linear regression ( = 0.11, P 0.001). The vast majority (77%) of mothers scored a 0 or 1 on the MIB scale, indicating good bonding; further statistical comparison using the MIB scale as a secondary outcome was therefore inappropriate.
On bivariate logistic regression, Hispanic/Latina women were less likely to be EPDS+ (odds ratio [OR]: 0.43; 95% CI: 0.23‐0.84) compared to white/Caucasian women. Mothers who identified Spanish as their primary language and took the Spanish EPDS had lower odds of a positive screen (OR: 0.47; 95% CI: 0.25‐0.88). The racial differences did not persist on multivariate analysis (OR: 0.64; 95% CI: 0.30‐1.38) (Table 2). Maternal characteristics identified as potential risk factors for positive screens were poor social support (OR: 3.58; 95% CI: 1.95‐6.59) and history of a prior psychiatric diagnosis (OR: 5.07; 95% CI: 2.65‐9.72). There were no differences in age, number of children or people living in the home, relationship status, or breastfeeding rates by EPDS score.
| OR | 95% CI | P Value | |
|---|---|---|---|
| |||
| Maternal characteristics | |||
| Maternal age | 0.99 | 0.95‐1.03 | 0.660 |
| Race | |||
| White | Reference | ||
| Black | 0.93 | 0.35‐2.50 | 0.891 |
| Hispanic | 0.43 | 0.23‐0.84 | 0.013 |
| Other | 0.54 | 0.19‐1.55 | 0.254 |
| EPDS language | 0.47 | 0.25‐0.88 | 0.020 |
| People in home | 1.02 | 0.89‐1.16 | 0.799 |
| No. of children | 1.02 | 0.85‐1.23 | 0.819 |
| Relationship | |||
| Married | Reference | ||
| In a relationship | 0.93 | 0.52‐1.65 | 0.802 |
| Single | 1.37 | 0.72‐2.62 | 0.333 |
| Unsupportive social network | 3.58 | 1.95‐6.59 | 0.0001 |
| Some psychiatric disorder | 5.07 | 2.65‐9.72 | 0.0001 |
| Infant characteristics | |||
| Gestational age | 0.96 | 0.87‐1.04 | 0.316 |
| Prior admission | 0.83 | 0.49‐1.39 | 0.476 |
| Any comorbidity | 1.03 | 0.92‐1.18 | 0.551 |
| Congenital heart disease | 1.87 | 0.83‐4.22 | 0.130 |
| Neurodevelopmental | 3.41 | 1.41‐8.21 | 0.006 |
| Any medical device needed | 1.59 | 0.78‐3.24 | 0.201 |
| Multivariate logistic regression | |||
| Race | |||
| White | Reference | ||
| Black | 0.87 | 0.28‐2.70 | 0.812 |
| Hispanic | 0.64 | 0.30‐1.38 | 0.258 |
| Other | 0.88 | 0.29‐2.74 | 0.831 |
| Unsupportive social network | 4.40 | 2.27‐8.53 | 0.0001 |
| Psychiatric disorder | 5.02 | 2.49‐10.15 | 0.0001 |
| Neurodevelopmental comorbidity | 2.78 | 1.03‐7.52 | 0.004 |
Infant characteristics were next examined. Children of EPDS+ and EPDS mothers were similar in age, number of prior hospital admissions, gestational age at birth, and overall use of medical equipment (Table 2). To examine the effect of illness leading to hospitalization on EPDS+ risk, discharge diagnoses were collected and grouped into categories. Infants of EPDS+ mothers were more likely hospitalized for neurologic illness (P = 0.008) (see Supporting Table 1 in the online version of this article), but otherwise similar.
We next compared differences in long‐term infant comorbidities. The rate of having any comorbidity was similar between children of EPDS+ and EPDS mothers (39.1% vs 33.6%; P = 0.551). However, children of EPDS+ mothers were more likely to have mental retardation, hydrocephalus, or require ventriculoperitoneal shunt (VPS); however, the overall number of infants with each comorbidity was low. A neurodevelopmental comorbidity variable was created combining mental retardation, cerebral palsy, epilepsy, hydrocephalus, craniosynostosis, and VPS, resulting in 22 (7.1%) unique infants with 1 or more of these conditions. Having an infant with a neurodevelopmental comorbidity was a risk factor for positive postpartum depression screen (OR: 3.41; 95% CI: 1.41‐8.21). This continued to be significant (OR: 2.78; 95% CI: 1.03‐7.52) (Table 2) when controlling for maternal race/ethnicity, psychiatric history, and social support in multivariate logistic regression.
To determine if women screened followed through with recommendations, participants were called 3 and 6 months postenrollment. We attempted to call all women and successfully reached 120; 19 (16%) refused the call. One hundred one of the original 310 enrolled (33%) completed at least 1 follow‐up call; 47 at 3 months, 40 at 6 months, and only 14 (14%) responded at both time points. Due to this response rate, the first call at either 3 or 6 months was used as a single follow‐up time point for statistical analysis. A slightly higher proportion of EPDS‐ mothers (80/223, 36%) completed calls compared to EPDS+ mothers (21/87, 24%; P = 0.047).
Of 21 mothers initially EPDS+ who completed a follow‐up call, 10 (48%) later screened negative. Seven of these 10 (70%) reported discussing postpartum depression with their physician or using provided referral resources in the interim; 1 woman both spoke to a doctor and used a referral resource. One additional woman used resources, but repeat EPDS was still positive (Table 3). Reasons cited for not seeking evaluation included too busy (n = 4) and lost paperwork (n = 1), or no reason was given (n = 2). Mothers utilizing appropriate follow‐up had reduction in scores compared to those not (F(1,19) = 5.743, P = 0.027), although all scores decreased over time (F(1,19) = 11.54, P = 0.0030) (Figure 1B).
| Changes in Characteristics Following Enrollment | Positive EPDS, N = 21 | Negative EPDS, N = 80 | P Value |
|---|---|---|---|
| |||
| Repeat EPDS negative | 10 (47.6%) | 73 (91.3%) | 0.001 |
| Spoke to a doctor about PD | 6 (28.6%) | 27 (33.7%) | 0.360 |
| Used a study referral resource | 3 (14.3%) | NA | |
| Received a formal diagnosis of PD | 1 (4.7%) | 1 (1.3%) | 0.325 |
| Healthcare utilization* | |||
| No. of ER visits | 0 (00.5) | 0 (02) | 0.074 |
| No. of urgent care visits | 0 (00.5) | 0 (00) | 0.136 |
| No. of hospitalizations | 0 (00) | 0 (01) | 0.021 |
| Repeat MIB score | 1.09 0.38 | 0.69 0.17 | 0.357 |
Of 80 women initially EPDS, most stayed negative (73/80, 91%), but 7 (9%) became EPDS+. These mothers received education and referral information over the phone, but none completed a subsequent call. Infants of mothers initially EPDS had a higher frequency of hospitalization postenrollment compared to EPDS+ mothers (P = 0.021) (Table 3). Two (33%) mothers who converted from EPDS to EPDS+ had infants readmitted in the follow‐up period.
DISCUSSION
This study demonstrated almost a third of mothers of hospitalized infants are at risk for postpartum depression and most had not been previously screened. Stress due to hospitalization did not seem to falsely elevate EPDS scores; the proportion of EPDS+ mothers matched our prestudy prediction (28% vs 27.9%). Follow‐up calls indicated that EPDS+ mothers not pursuing further evaluation tended to remain EPDS+. Higher (worse) MIB score was strongly correlated to increased EPDS score as expected, supporting screening accuracy. Our results suggest that postpartum depression screening in hospital settings can be used to complement outpatient practice and capture mothers who would otherwise be missed.
Although we were able to screen, it is difficult to know whether this correctly identified mothers with postpartum depression. Only 2 mothers reported subsequent official diagnosis of postpartum depression, and 1 of these was EPDS originally. This reflects weakness of our survey‐based design; we only know if the mother self‐reported a formal diagnosis of postpartum depression, because we do not have access to their medical charts. We also had higher than expected loss to follow up (67%), leaving 66 initially EPDS+ mothers with unknown eventual diagnoses. The EPDS has been validated in multiple populations and has a positive predictive value ranging from 23% to 93%.[23] Therefore, somewhere between 20 and 80 women in our study should meet diagnostic criteria for postpartum depression. A limitation of children's hospital‐based screening with the EPDS is lack of adult‐trained psychiatrists who could immediately follow screening with diagnosis. Such integration may already be possible at community or hospital‐within‐a‐hospital models, and could be trialed at children's hospitals. Regardless, participation in the study seemed to increase mothers' awareness of postpartum depression. Prior to enrollment, only 14.6% of subjects reported discussing postpartum depression with a physician, although recall bias likely contributed to some mothers not remembering a screen. Promisingly, on follow‐up, 37% of called participants reported they discussed postpartum depression with a doctor following their child's hospital discharge.
Our study identified low social support and history of past psychiatric diagnosis as maternal risk factors for EPDS+ screens, which is consistent with previous reports.[29] There was a slight increase in subsequent infant hospitalizations in the EPDS group, which is contrary to reports stating that increased healthcare utilization is associated with postpartum depression.[30] However, most studies have shown an increase in only acute or emergency room care visits[30, 31] and no association between maternal depression and infant hospitalization.[30, 32] In our study, the median number of hospitalizations for both groups was 0, indicating overall low utilization. Because 2 of the mothers who converted from EPDS to EPDS+ had children readmitted, this underscores the benefit of reassessment at each medical encounter. A large proportion of mothers (36.5%) reported that the infant had been previously hospitalized, adding another potential missed screening opportunity. Our study supports others advocating repeated screenings and suggests mothers should be screened at any medical encounter that occurs in the first postpartum year.
We identified neurodevelopmental illness as the major infant characteristic associated with postpartum depression risk. Conversely, Garfield et al. did not find correlation between poorer Neurobiologic Risk Score and increased maternal depression risk in a NICU setting.[11] Perhaps our population of older and mainly full‐term infants makes consequences of neurologic insult more obvious and affects mothers more significantly. Cheng et al. reported that 26.9% of mothers of children with cognitive delay reported high depressive symptoms, compared with 17.4% of mothers of typically developing children at 4 years of age.[33] Another body of evidence suggests maternal emotional state during pregnancy influences neurodevelopmental outcome in the child. Maternal anxiety or depression has been associated with altered placental function, reduced infant gray matter density, and worse cognitive function.[34, 35] Therefore, future research may focus on mothers of infants with neurodevelopmental disease to better understand this relationship.
There were several limitations to this study. Some data collected by a survey are subject to information bias. Women may report a more supportive social network than actually exists or omit history of mental health diagnoses. We attempted to control for this by using validated measures where possible and performing chart review to verify reported infant characteristics. Our population was overwhelmingly Hispanic/Latina, and a third of infants were not previously healthy, which limits applicability to other settings. We used a convenience method that could introduce sampling bias. Our hospital's overall patient demographic is 65% Hispanic, which is similar to the 68% sampled in our study. In addition, the proportions of infant diagnoses approximate the overall rates at CHLA, so we feel our sample was fairly representative. There is a general consensus that depression studies have recruitment difficulties.[36] In the unlikely event that all 56 of women who declined to participate were EPDS+, overall proportion of at‐risk mothers would rise to 39%. If our study does show slight underestimation of risk, that would only mean more potential for intervention if screening were mandatory. Another weakness was high loss to follow‐up, which led us to combine the 3‐ and 6‐month follow‐up calls into 1 outcome. Sixty percent of calls used in analysis occurred at 3 months, so long‐term maintenance of improved EPDS scores remains unclear. Although conducting repeat EPDS via phone may affect honest answering of sensitive questions, other studies have used this technique successfully.[4]
CONCLUSION
This is the first study evaluating a screening program for maternal postpartum depression during infant hospitalizations. In our population, risk factors for positive postpartum depression screening were low social support, history of maternal psychiatric diagnosis, and having an infant with neurodevelopmental disease. We believe mothers should receive postpartum depression screening at all medical encounters during the child's first year.
Acknowledgements
The authors thank the CHLA Department of Social Work and the USC Required Scholarly Projects program, and specifically Joseph DeSena and Humberto Avila, for project assistance.
Disclosures: Dr. Trost is an Institutional Career Development Program Scholar through the Southern California Clinical and Translational Science Institute (SC‐CTSI) at the University of Southern California Keck School of Medicine. The content is solely the responsibility of the author(s) and does not represent the official view of the SC‐CTSI. Dr. Trost conceptualized and designed the study, drafted the initial manuscript, and approved the final manuscript as submitted. Dr. Molas‐Torreblanca co‐designed the study, reviewed and revised the manuscript, and approved the final manuscript as submitted. Ms. Man coordinated and supervised hospital data collection, critically reviewed the manuscript, and approved the final manuscript as submitted. Mr. Casillas coordinated and supervised the phone call data collection, critically reviewed the manuscript, and approved the final manuscript as submitted. Ms. Sapir coordinated the referral process for enrolled patients, supervised the design of patient handouts, and critically reviewed and approved the final manuscript as submitted. Dr. Schrager guided study design, supervised the statistical analysis of the final data, critically reviewed and revised the manuscript, and approved the final manuscript as submitted. The authors report no conflicts of interest.
Maternal postpartum depression occurs in 5% to 25% of all mothers, and up to 40% to 60% in high‐risk populations such as low‐income women.[1, 2, 3, 4] Children of affected mothers suffer negative health consequences such as decreased physical growth, poor maternalchild bond, problem behavior, and child abuse.[5, 6, 7] Timely recognition of symptoms and treatment may improve child outcomes.[8] Published guidelines recommend pediatricians screen for postpartum depression at infant 1‐, 2‐, 4‐, and 6‐month outpatient visits.[9] There are no current guidelines for or studies of screening in general inpatient settings, although emergency rooms[10] and neonatal intensive care units (NICUs)[11] have been examined. Pediatric hospitalization may offer an additional opportunity for expanding screening and intervention.
Augmenting outpatient screening practices with additional inpatient screening would have several benefits. Infant health problems have been associated with postpartum depression, and therefore mothers in the hospital may be at higher risk.[12] Inpatient screening would also improve access to mothers not screened as outpatients. Missed screening could occur due to physician discomfort with screening, time constraints during busy office visits, or noncompliance with recommended visit schedules.[13, 14, 15, 16] Finally, inpatient providers would benefit from understanding the psychosocial milieu of children now under their care. Recent studies note hospital discharges may be improved and readmissions reduced by assessing socioeconomic risk factors during hospitalization.[17] The evidence‐based Peds Effective Discharge: Better Handoff to Home through Safer Transitions Better Outcomes by Optimizing Safe Transitions (Pedi‐BOOST) toolkit specifically recommends an assessment of parental psychiatric issues.[18] Postpartum depression strongly correlates with impaired maternalchild bonding,[19] which in turn negatively affects mothers' engagement with healthcare providers.[20] This could impact patient education and recommendations provided during hospitalization.
Therefore, we sought to perform postpartum depression screening during infant hospitalizations. Our primary goal was to determine rate of postpartum depression in our population and proportion of women previously unscreened who could be captured by inpatient screening. We additionally aimed to determine the proportion of women with poor maternalinfant bond. Our next goal was to identify maternal or infant factors associated with positive postpartum depression screening. Finally, we performed follow‐up calls to determine if in‐hospital interventions resulted in formal postpartum depression diagnosis, use of recommended referrals, improved maternalchild bond, and decreased symptoms of depression over time.
METHODS
Patient Selection
We conducted a prospective observational study on a convenience sample of mothers at Children's Hospital Los Angeles (CHLA), a large, urban, tertiary care hospital. Biological mothers of infants 1 year of age admitted to medicalsurgical floors and assigned to pediatric hospitalist teams between April 1, 2013 and July 30, 2014 were eligible for inclusion. Mothers were required to be age 18 years or older and able to speak and read English or Spanish. Mothers of infants aged 2 weeks were excluded to avoid confusing postpartum depression with maternal baby blues, a distinct entity causing milder symptoms of depression that should resolve by 2 weeks.[21] In an effort to reduce the impact of stress associated with prolonged hospitalization on Edinburgh Postpartum Depression Scale (EPDS) scores, we excluded mothers of children already hospitalized >72 hours. Visits from participants who were readmitted or previously enrolled in the study were excluded. All study procedures were approved by the CHLA Institutional Review Board.
Measures
After giving informed consent, mothers completed demographic forms about themselves and their infants. A 4‐item Likert scale assessed self‐perceived support from family and friends. Past mental health problems were assessed via 10‐item checklist. Self‐reported infant comorbidities and reason for hospitalization were confirmed by chart review for International Classification of Diseases, Ninth Revision diagnoses present on admission and reason for discharge. Next, mothers filled out a maternalinfant bonding scale (MIB)[22] and the EPDS,[23, 24] which has been validated in both English and Spanish.[25] There are no formal cutoffs for the MIB; higher scores indicate worse bonding. Out of a possible 30, a score of 10 or higher on the EPDS was considered a positive screen, indicating risk for postpartum depression. Scores less than 10 were negative screens, and those mothers were determined not at risk.[24] The last EPDS question asks, The thought of harming myself has occurred to me. Any mothers answering yes, quite often, sometimes, or hardly ever were further interviewed and treated per a suicidality operating protocol.
Counseling and Referral
All EPDS mothers were informed of results and did not receive further intervention during hospitalization. For EPDS+ mothers, individual social workers responded to referrals placed by the study team into infant charts and delivered 1‐on‐1 counseling. Social workers received study education prior to initiation and midway through patient recruitment and provided mothers with an educational handout, referral sheet listing online resources of local mental health clinics accepting postpartum depression patients, and help‐line numbers. Mothers who identified a primary doctor were encouraged to follow up with them.
Follow‐up
In order to assess intervention effect over time, all mothers (both EPDS+ and EPDS) were called 3 and 6 months ( 1 week) postenrollment and rescreened with the EPDS and MIB. They also answered a short survey assessing whether they spoke further to a doctor about postpartum depression; used a referral resource; received a formal postpartum depression diagnosis; and if their children visited the ER, urgent care, or hospital again since discharge. Mothers who again screened EPDS+ or newly converted to EPDS+ were provided counseling and referral via phone.
Sample Size Calculation
A priori power analysis determined a sample size of 310 mothers was required to estimate the rate of postpartum depression at CHLA with 5% precision and a 95% confidence level, assuming an estimated prevalence of 27.9% based on prior studies.[26] At this prevalence rate, screening 310 mothers was also predicted to yield at least 77 positive screens on the EPDS, yielding an appropriate sample to detect EPDS score improvements over time. This number was based on previous studies showing reduction in EPDS of 35% following appropriate referral,[26, 27] assuming 15% attrition at both the 3‐month and 6‐month follow‐up sampling points.
Statistical Analysis
After data collection was complete, characteristics between EPDS+ and EPDS groups were compared using 2 tests for dichotomous outcomes and t tests for continuous variables. Multiple logistic regression was then used to compare specific factors associated with positive EPDS screens (P 0.05). Linear regression assessed the relationship between EPDS and MIB scores. Change in average EPDS and MIB scores at the time of first successful follow‐up call between women who did and did not seek further postpartum depression evaluation were compared via 2‐way repeated measures analysis of variance. Statistical analyses were performed using R software.[28]
RESULTS
Out of 366 motherinfant pairs, 56 (15%) refused, and 310 (85%) mothers were fully enrolled (Figure 1A). Mothers had an average age of 28.17 years, were 68.3% Hispanic/Latina by self‐report, and 45.2% were married. Infants were an average of 4.24 months old, 81.9% were born term (>37 weeks), and 64.8% were previously healthy (Table 1).
| Characteristic | All Participants, n = 310 |
|---|---|
| |
| Maternal characteristics | |
| Age, y* | 28.17 6.18 |
| Race/ethnicity | |
| White | 48 (15.5%) |
| Black | 25 (8.1%) |
| Hispanic | 211(68.3%) |
| Other | 25 (8.1%) |
| EPDS language | |
| English | 231 (74.5%) |
| Spanish | 79 (25.5%) |
| People in home | 5 (4, 6) |
| No. of children | 2 (1, 3) |
| Relationship | |
| Married | 140 (45.2%) |
| In a relationship | 105 (33.9%) |
| Single | 62 (20%) |
| Any breastfeeding | 142 (45.8%) |
| Unsupportive social network | 54 (17.4%) |
| Some psychiatric disorder | 47 (15.2%) |
| MIB score | 6 (3, 10) |
| Infant characteristics | |
| Age, mo* | 4.24 3.19 |
| Gestational age, wk | 39 (37, 40) |
| Prior admission | 113 (36.5%) |
| Any comorbidity | 109 (35.2%) |
| Congenital heart disease | 27 (8.7%) |
| Neurodevelopmental | 22 (7.1%) |
| Any medical device needed | 38 (12.3%) |

(B) Postenrollment change in mean Edinburgh Postpartum Depression Scale (EPDS) score of all initially EPDS mothers who completed at least 1 follow‐up phone call, separated by if they did or did not seek referral. Mothers using referral (either spoke with physician or used resource sheet) had significantly larger reduction in score. Statistical analysis by analysis of variance, P < 0.05.
Eighty‐seven (28%) mothers were EPDS+; 223 (72%) were EPDS. Only 42 mothers reported previous postpartum depression screening since the birth of their most recent child. However, 30 infants were 1 month in age, thus outside recommended screening range. Eliminating these infants revealed a 14.6% rate of appropriate prior screening. Higher EPDS scores were associated with higher (worse) MIB scores by linear regression ( = 0.11, P 0.001). The vast majority (77%) of mothers scored a 0 or 1 on the MIB scale, indicating good bonding; further statistical comparison using the MIB scale as a secondary outcome was therefore inappropriate.
On bivariate logistic regression, Hispanic/Latina women were less likely to be EPDS+ (odds ratio [OR]: 0.43; 95% CI: 0.23‐0.84) compared to white/Caucasian women. Mothers who identified Spanish as their primary language and took the Spanish EPDS had lower odds of a positive screen (OR: 0.47; 95% CI: 0.25‐0.88). The racial differences did not persist on multivariate analysis (OR: 0.64; 95% CI: 0.30‐1.38) (Table 2). Maternal characteristics identified as potential risk factors for positive screens were poor social support (OR: 3.58; 95% CI: 1.95‐6.59) and history of a prior psychiatric diagnosis (OR: 5.07; 95% CI: 2.65‐9.72). There were no differences in age, number of children or people living in the home, relationship status, or breastfeeding rates by EPDS score.
| OR | 95% CI | P Value | |
|---|---|---|---|
| |||
| Maternal characteristics | |||
| Maternal age | 0.99 | 0.95‐1.03 | 0.660 |
| Race | |||
| White | Reference | ||
| Black | 0.93 | 0.35‐2.50 | 0.891 |
| Hispanic | 0.43 | 0.23‐0.84 | 0.013 |
| Other | 0.54 | 0.19‐1.55 | 0.254 |
| EPDS language | 0.47 | 0.25‐0.88 | 0.020 |
| People in home | 1.02 | 0.89‐1.16 | 0.799 |
| No. of children | 1.02 | 0.85‐1.23 | 0.819 |
| Relationship | |||
| Married | Reference | ||
| In a relationship | 0.93 | 0.52‐1.65 | 0.802 |
| Single | 1.37 | 0.72‐2.62 | 0.333 |
| Unsupportive social network | 3.58 | 1.95‐6.59 | 0.0001 |
| Some psychiatric disorder | 5.07 | 2.65‐9.72 | 0.0001 |
| Infant characteristics | |||
| Gestational age | 0.96 | 0.87‐1.04 | 0.316 |
| Prior admission | 0.83 | 0.49‐1.39 | 0.476 |
| Any comorbidity | 1.03 | 0.92‐1.18 | 0.551 |
| Congenital heart disease | 1.87 | 0.83‐4.22 | 0.130 |
| Neurodevelopmental | 3.41 | 1.41‐8.21 | 0.006 |
| Any medical device needed | 1.59 | 0.78‐3.24 | 0.201 |
| Multivariate logistic regression | |||
| Race | |||
| White | Reference | ||
| Black | 0.87 | 0.28‐2.70 | 0.812 |
| Hispanic | 0.64 | 0.30‐1.38 | 0.258 |
| Other | 0.88 | 0.29‐2.74 | 0.831 |
| Unsupportive social network | 4.40 | 2.27‐8.53 | 0.0001 |
| Psychiatric disorder | 5.02 | 2.49‐10.15 | 0.0001 |
| Neurodevelopmental comorbidity | 2.78 | 1.03‐7.52 | 0.004 |
Infant characteristics were next examined. Children of EPDS+ and EPDS mothers were similar in age, number of prior hospital admissions, gestational age at birth, and overall use of medical equipment (Table 2). To examine the effect of illness leading to hospitalization on EPDS+ risk, discharge diagnoses were collected and grouped into categories. Infants of EPDS+ mothers were more likely hospitalized for neurologic illness (P = 0.008) (see Supporting Table 1 in the online version of this article), but otherwise similar.
We next compared differences in long‐term infant comorbidities. The rate of having any comorbidity was similar between children of EPDS+ and EPDS mothers (39.1% vs 33.6%; P = 0.551). However, children of EPDS+ mothers were more likely to have mental retardation, hydrocephalus, or require ventriculoperitoneal shunt (VPS); however, the overall number of infants with each comorbidity was low. A neurodevelopmental comorbidity variable was created combining mental retardation, cerebral palsy, epilepsy, hydrocephalus, craniosynostosis, and VPS, resulting in 22 (7.1%) unique infants with 1 or more of these conditions. Having an infant with a neurodevelopmental comorbidity was a risk factor for positive postpartum depression screen (OR: 3.41; 95% CI: 1.41‐8.21). This continued to be significant (OR: 2.78; 95% CI: 1.03‐7.52) (Table 2) when controlling for maternal race/ethnicity, psychiatric history, and social support in multivariate logistic regression.
To determine if women screened followed through with recommendations, participants were called 3 and 6 months postenrollment. We attempted to call all women and successfully reached 120; 19 (16%) refused the call. One hundred one of the original 310 enrolled (33%) completed at least 1 follow‐up call; 47 at 3 months, 40 at 6 months, and only 14 (14%) responded at both time points. Due to this response rate, the first call at either 3 or 6 months was used as a single follow‐up time point for statistical analysis. A slightly higher proportion of EPDS‐ mothers (80/223, 36%) completed calls compared to EPDS+ mothers (21/87, 24%; P = 0.047).
Of 21 mothers initially EPDS+ who completed a follow‐up call, 10 (48%) later screened negative. Seven of these 10 (70%) reported discussing postpartum depression with their physician or using provided referral resources in the interim; 1 woman both spoke to a doctor and used a referral resource. One additional woman used resources, but repeat EPDS was still positive (Table 3). Reasons cited for not seeking evaluation included too busy (n = 4) and lost paperwork (n = 1), or no reason was given (n = 2). Mothers utilizing appropriate follow‐up had reduction in scores compared to those not (F(1,19) = 5.743, P = 0.027), although all scores decreased over time (F(1,19) = 11.54, P = 0.0030) (Figure 1B).
| Changes in Characteristics Following Enrollment | Positive EPDS, N = 21 | Negative EPDS, N = 80 | P Value |
|---|---|---|---|
| |||
| Repeat EPDS negative | 10 (47.6%) | 73 (91.3%) | 0.001 |
| Spoke to a doctor about PD | 6 (28.6%) | 27 (33.7%) | 0.360 |
| Used a study referral resource | 3 (14.3%) | NA | |
| Received a formal diagnosis of PD | 1 (4.7%) | 1 (1.3%) | 0.325 |
| Healthcare utilization* | |||
| No. of ER visits | 0 (00.5) | 0 (02) | 0.074 |
| No. of urgent care visits | 0 (00.5) | 0 (00) | 0.136 |
| No. of hospitalizations | 0 (00) | 0 (01) | 0.021 |
| Repeat MIB score | 1.09 0.38 | 0.69 0.17 | 0.357 |
Of 80 women initially EPDS, most stayed negative (73/80, 91%), but 7 (9%) became EPDS+. These mothers received education and referral information over the phone, but none completed a subsequent call. Infants of mothers initially EPDS had a higher frequency of hospitalization postenrollment compared to EPDS+ mothers (P = 0.021) (Table 3). Two (33%) mothers who converted from EPDS to EPDS+ had infants readmitted in the follow‐up period.
DISCUSSION
This study demonstrated almost a third of mothers of hospitalized infants are at risk for postpartum depression and most had not been previously screened. Stress due to hospitalization did not seem to falsely elevate EPDS scores; the proportion of EPDS+ mothers matched our prestudy prediction (28% vs 27.9%). Follow‐up calls indicated that EPDS+ mothers not pursuing further evaluation tended to remain EPDS+. Higher (worse) MIB score was strongly correlated to increased EPDS score as expected, supporting screening accuracy. Our results suggest that postpartum depression screening in hospital settings can be used to complement outpatient practice and capture mothers who would otherwise be missed.
Although we were able to screen, it is difficult to know whether this correctly identified mothers with postpartum depression. Only 2 mothers reported subsequent official diagnosis of postpartum depression, and 1 of these was EPDS originally. This reflects weakness of our survey‐based design; we only know if the mother self‐reported a formal diagnosis of postpartum depression, because we do not have access to their medical charts. We also had higher than expected loss to follow up (67%), leaving 66 initially EPDS+ mothers with unknown eventual diagnoses. The EPDS has been validated in multiple populations and has a positive predictive value ranging from 23% to 93%.[23] Therefore, somewhere between 20 and 80 women in our study should meet diagnostic criteria for postpartum depression. A limitation of children's hospital‐based screening with the EPDS is lack of adult‐trained psychiatrists who could immediately follow screening with diagnosis. Such integration may already be possible at community or hospital‐within‐a‐hospital models, and could be trialed at children's hospitals. Regardless, participation in the study seemed to increase mothers' awareness of postpartum depression. Prior to enrollment, only 14.6% of subjects reported discussing postpartum depression with a physician, although recall bias likely contributed to some mothers not remembering a screen. Promisingly, on follow‐up, 37% of called participants reported they discussed postpartum depression with a doctor following their child's hospital discharge.
Our study identified low social support and history of past psychiatric diagnosis as maternal risk factors for EPDS+ screens, which is consistent with previous reports.[29] There was a slight increase in subsequent infant hospitalizations in the EPDS group, which is contrary to reports stating that increased healthcare utilization is associated with postpartum depression.[30] However, most studies have shown an increase in only acute or emergency room care visits[30, 31] and no association between maternal depression and infant hospitalization.[30, 32] In our study, the median number of hospitalizations for both groups was 0, indicating overall low utilization. Because 2 of the mothers who converted from EPDS to EPDS+ had children readmitted, this underscores the benefit of reassessment at each medical encounter. A large proportion of mothers (36.5%) reported that the infant had been previously hospitalized, adding another potential missed screening opportunity. Our study supports others advocating repeated screenings and suggests mothers should be screened at any medical encounter that occurs in the first postpartum year.
We identified neurodevelopmental illness as the major infant characteristic associated with postpartum depression risk. Conversely, Garfield et al. did not find correlation between poorer Neurobiologic Risk Score and increased maternal depression risk in a NICU setting.[11] Perhaps our population of older and mainly full‐term infants makes consequences of neurologic insult more obvious and affects mothers more significantly. Cheng et al. reported that 26.9% of mothers of children with cognitive delay reported high depressive symptoms, compared with 17.4% of mothers of typically developing children at 4 years of age.[33] Another body of evidence suggests maternal emotional state during pregnancy influences neurodevelopmental outcome in the child. Maternal anxiety or depression has been associated with altered placental function, reduced infant gray matter density, and worse cognitive function.[34, 35] Therefore, future research may focus on mothers of infants with neurodevelopmental disease to better understand this relationship.
There were several limitations to this study. Some data collected by a survey are subject to information bias. Women may report a more supportive social network than actually exists or omit history of mental health diagnoses. We attempted to control for this by using validated measures where possible and performing chart review to verify reported infant characteristics. Our population was overwhelmingly Hispanic/Latina, and a third of infants were not previously healthy, which limits applicability to other settings. We used a convenience method that could introduce sampling bias. Our hospital's overall patient demographic is 65% Hispanic, which is similar to the 68% sampled in our study. In addition, the proportions of infant diagnoses approximate the overall rates at CHLA, so we feel our sample was fairly representative. There is a general consensus that depression studies have recruitment difficulties.[36] In the unlikely event that all 56 of women who declined to participate were EPDS+, overall proportion of at‐risk mothers would rise to 39%. If our study does show slight underestimation of risk, that would only mean more potential for intervention if screening were mandatory. Another weakness was high loss to follow‐up, which led us to combine the 3‐ and 6‐month follow‐up calls into 1 outcome. Sixty percent of calls used in analysis occurred at 3 months, so long‐term maintenance of improved EPDS scores remains unclear. Although conducting repeat EPDS via phone may affect honest answering of sensitive questions, other studies have used this technique successfully.[4]
CONCLUSION
This is the first study evaluating a screening program for maternal postpartum depression during infant hospitalizations. In our population, risk factors for positive postpartum depression screening were low social support, history of maternal psychiatric diagnosis, and having an infant with neurodevelopmental disease. We believe mothers should receive postpartum depression screening at all medical encounters during the child's first year.
Acknowledgements
The authors thank the CHLA Department of Social Work and the USC Required Scholarly Projects program, and specifically Joseph DeSena and Humberto Avila, for project assistance.
Disclosures: Dr. Trost is an Institutional Career Development Program Scholar through the Southern California Clinical and Translational Science Institute (SC‐CTSI) at the University of Southern California Keck School of Medicine. The content is solely the responsibility of the author(s) and does not represent the official view of the SC‐CTSI. Dr. Trost conceptualized and designed the study, drafted the initial manuscript, and approved the final manuscript as submitted. Dr. Molas‐Torreblanca co‐designed the study, reviewed and revised the manuscript, and approved the final manuscript as submitted. Ms. Man coordinated and supervised hospital data collection, critically reviewed the manuscript, and approved the final manuscript as submitted. Mr. Casillas coordinated and supervised the phone call data collection, critically reviewed the manuscript, and approved the final manuscript as submitted. Ms. Sapir coordinated the referral process for enrolled patients, supervised the design of patient handouts, and critically reviewed and approved the final manuscript as submitted. Dr. Schrager guided study design, supervised the statistical analysis of the final data, critically reviewed and revised the manuscript, and approved the final manuscript as submitted. The authors report no conflicts of interest.
- , , , , . Maternal depressive symptoms and infant health practices among low‐income women. Pediatrics. 2004;113(6):e523–e529.
- , , , et al.; Duke University Evidence‐based Practice Center. Effective Health Care Program. Efficacy and safety of screening for postpartum depression. Comparative effectiveness review number 106. Rockville, MD: Agency for Healthcare Research and Quality, U.S. Department of Health and Human Services; 2013: Available at: https://www.effectivehealthcare.ahrq.gov/ehc/products/379/1437/postpartum‐screening‐report‐130409.pdf. Date accessed Jan 10 2016.
- , , , , . Prevalence rates and demographic characteristics associated with depression in pregnancy and the postpartum. J Consult Clin Psychol. 1989;57(2):269–274.
- , , , , . Screening for depression in the postpartum period: a comparison of three instruments. J Womens Health (Larchmt). 2008;17(4):585–596.
- , , , . Are maternal depression or symptom severity associated with breastfeeding intention or outcomes? J Clin Psychiatry. 2010;71(8):1069–1078.
- , , , , . Impact of maternal depressive symptoms on growth of preschool‐ and school‐aged children. Pediatrics. 2012;130(4):e847–e855.
- , , , , . The timing of maternal depressive symptoms and mothers' parenting practices with young children: implications for pediatric practice. Pediatrics. 2006;118(1):e174–e182.
- , , , , . Improvements in maternal depression as a mediator of intervention effects on early childhood problem behavior. Dev Psychopathol. 2009;21(2):417–439.
- ; Committee on Psychosocial Aspects of Child and Family Health American Academy of Pediatrics. Incorporating recognition and management of perinatal and postpartum depression into pediatric practice. Pediatrics. 2010;126(5):1032–1039.
- , , . Screening for postpartum depression in a pediatric emergency department. Pediatr Emerg Care. 2011;27(9):795–800.
- , , , et al. Risk factors for postpartum depressive symptoms in low‐income women with very low‐birth‐weight infants. Adv Neonatal Care. 2015;15(1):E3–E8.
- , , . Impact of infant health problems on postnatal depression: pilot study to evaluate a health visiting system. Psychiatry Clin Neurosci. 2006;60(2):182–189.
- , , , , , . Primary care pediatricians' roles and perceived responsibilities in the identification and management of maternal depression. Pediatrics. 2002;110(6):1169–1176.
- , , , et al. Does education influence pediatricians' perceptions of physician‐specific barriers for maternal depression? Clin Pediatr (Phila). 2008;47(7):670–678.
- , , , . Pediatricians' views of postpartum depression: a self‐administered survey. Arch Womens Ment Health. 2004;7(4):231–236.
- . Compliance with well‐child visit recommendations: evidence from the Medical Expenditure Panel Survey, 2000–2002. Pediatrics. 2006;118(6):e1766–e1778.
- , , , et al. A framework of pediatric hospital discharge care informed by legislation, research, and practice. JAMA Pediatr. 2014;168(10):955–962; quiz 965–966.
- , , . Pedi‐BOOST. Peds Effective Discharge: Better Handoff to Home through Safer Transitions. 2013. https://www.hospitalmedicine.org/Web/Quality___Innovation/Implementation_Toolkit/pediBoost/Best_Practices/Best_Practices.aspx Accessed Jan 10 2016.
- , , , et al. Effects of maternal depressive symptomatology during pregnancy and the postpartum period on infant‐mother attachment. Psychiatry Clin Neurosci. 2014;68(8):631–639.
- , , , , . Examining maternal depression and attachment insecurity as moderators of the impacts of home visiting for at‐risk mothers and infants. J Consult Clin Psychol. 2009;77(4):788–799.
- , . Postpartum mood disorders: diagnosis and treatment guidelines. J Clin Psychiatry. 1998;59(suppl 2):34–40.
- , , , , . A new Mother‐to‐Infant Bonding Scale: links with early maternal mood. Arch Womens Ment Health. 2005;8(1):45–51.
- , , , , . A systematic review of studies validating the Edinburgh Postnatal Depression Scale in antepartum and postpartum women. Acta Psychiatr Scand. 2009;119(5):350–364.
- , , . Detection of postnatal depression. Development of the 10‐item Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1987;150:782–786.
- , , , . Validation of the Edinburgh Postnatal Depression Scale (EPDS) in Spanish mothers. J Affect Disord. 2003;75(1):71–76.
- , , , et al. TRIPPD: a practice‐based network effectiveness study of postpartum depression screening and management. Ann Fam Med. 2012;10(4):320–329.
- , , , , . Detection of postpartum depressive symptoms by screening at well‐child visits. Pediatrics. 2004;113(3 pt 1):551–558.
- R Core Team. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing: 2013. Available at: http://www.R‐project.org. Accessed Jan 10 2016.
- , , , , . Biological and psychosocial predictors of postpartum depression: systematic review and call for integration. Annu Rev Clin Psychol. 2015;11:99–137.
- , , , et al. Maternal depressive symptoms and children's receipt of health care in the first 3 years of life. Pediatrics. 2005;115(2):306–314.
- , . Maternal factors and child's health care use. Soc Sci Med. 1995;40(5):623–628.
- , , , , . Women's health after pregnancy and child outcomes at age 3 years: a prospective cohort study. Am J Public Health. 2002;92(8):1312–1318.
- , , , . The influence of children's cognitive delay and behavior problems on maternal depression. J Pediatr. 2015;167(3):679–686.
- , , , , . Maternal prenatal symptoms of depression and down regulation of placental monoamine oxidase A expression. J Psychosom Res. 2013;75(4):341–345.
- , , , , . High pregnancy anxiety during mid‐gestation is associated with decreased gray matter density in 6–9‐year‐old children. Psychoneuroendocrinology. 2010;35(1):141–153.
- , , , , . Factors affecting recruitment into depression trials: Systematic review, meta‐synthesis and conceptual framework. J Affect Disord. 2015;172:274–290.
- , , , , . Maternal depressive symptoms and infant health practices among low‐income women. Pediatrics. 2004;113(6):e523–e529.
- , , , et al.; Duke University Evidence‐based Practice Center. Effective Health Care Program. Efficacy and safety of screening for postpartum depression. Comparative effectiveness review number 106. Rockville, MD: Agency for Healthcare Research and Quality, U.S. Department of Health and Human Services; 2013: Available at: https://www.effectivehealthcare.ahrq.gov/ehc/products/379/1437/postpartum‐screening‐report‐130409.pdf. Date accessed Jan 10 2016.
- , , , , . Prevalence rates and demographic characteristics associated with depression in pregnancy and the postpartum. J Consult Clin Psychol. 1989;57(2):269–274.
- , , , , . Screening for depression in the postpartum period: a comparison of three instruments. J Womens Health (Larchmt). 2008;17(4):585–596.
- , , , . Are maternal depression or symptom severity associated with breastfeeding intention or outcomes? J Clin Psychiatry. 2010;71(8):1069–1078.
- , , , , . Impact of maternal depressive symptoms on growth of preschool‐ and school‐aged children. Pediatrics. 2012;130(4):e847–e855.
- , , , , . The timing of maternal depressive symptoms and mothers' parenting practices with young children: implications for pediatric practice. Pediatrics. 2006;118(1):e174–e182.
- , , , , . Improvements in maternal depression as a mediator of intervention effects on early childhood problem behavior. Dev Psychopathol. 2009;21(2):417–439.
- ; Committee on Psychosocial Aspects of Child and Family Health American Academy of Pediatrics. Incorporating recognition and management of perinatal and postpartum depression into pediatric practice. Pediatrics. 2010;126(5):1032–1039.
- , , . Screening for postpartum depression in a pediatric emergency department. Pediatr Emerg Care. 2011;27(9):795–800.
- , , , et al. Risk factors for postpartum depressive symptoms in low‐income women with very low‐birth‐weight infants. Adv Neonatal Care. 2015;15(1):E3–E8.
- , , . Impact of infant health problems on postnatal depression: pilot study to evaluate a health visiting system. Psychiatry Clin Neurosci. 2006;60(2):182–189.
- , , , , , . Primary care pediatricians' roles and perceived responsibilities in the identification and management of maternal depression. Pediatrics. 2002;110(6):1169–1176.
- , , , et al. Does education influence pediatricians' perceptions of physician‐specific barriers for maternal depression? Clin Pediatr (Phila). 2008;47(7):670–678.
- , , , . Pediatricians' views of postpartum depression: a self‐administered survey. Arch Womens Ment Health. 2004;7(4):231–236.
- . Compliance with well‐child visit recommendations: evidence from the Medical Expenditure Panel Survey, 2000–2002. Pediatrics. 2006;118(6):e1766–e1778.
- , , , et al. A framework of pediatric hospital discharge care informed by legislation, research, and practice. JAMA Pediatr. 2014;168(10):955–962; quiz 965–966.
- , , . Pedi‐BOOST. Peds Effective Discharge: Better Handoff to Home through Safer Transitions. 2013. https://www.hospitalmedicine.org/Web/Quality___Innovation/Implementation_Toolkit/pediBoost/Best_Practices/Best_Practices.aspx Accessed Jan 10 2016.
- , , , et al. Effects of maternal depressive symptomatology during pregnancy and the postpartum period on infant‐mother attachment. Psychiatry Clin Neurosci. 2014;68(8):631–639.
- , , , , . Examining maternal depression and attachment insecurity as moderators of the impacts of home visiting for at‐risk mothers and infants. J Consult Clin Psychol. 2009;77(4):788–799.
- , . Postpartum mood disorders: diagnosis and treatment guidelines. J Clin Psychiatry. 1998;59(suppl 2):34–40.
- , , , , . A new Mother‐to‐Infant Bonding Scale: links with early maternal mood. Arch Womens Ment Health. 2005;8(1):45–51.
- , , , , . A systematic review of studies validating the Edinburgh Postnatal Depression Scale in antepartum and postpartum women. Acta Psychiatr Scand. 2009;119(5):350–364.
- , , . Detection of postnatal depression. Development of the 10‐item Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1987;150:782–786.
- , , , . Validation of the Edinburgh Postnatal Depression Scale (EPDS) in Spanish mothers. J Affect Disord. 2003;75(1):71–76.
- , , , et al. TRIPPD: a practice‐based network effectiveness study of postpartum depression screening and management. Ann Fam Med. 2012;10(4):320–329.
- , , , , . Detection of postpartum depressive symptoms by screening at well‐child visits. Pediatrics. 2004;113(3 pt 1):551–558.
- R Core Team. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing: 2013. Available at: http://www.R‐project.org. Accessed Jan 10 2016.
- , , , , . Biological and psychosocial predictors of postpartum depression: systematic review and call for integration. Annu Rev Clin Psychol. 2015;11:99–137.
- , , , et al. Maternal depressive symptoms and children's receipt of health care in the first 3 years of life. Pediatrics. 2005;115(2):306–314.
- , . Maternal factors and child's health care use. Soc Sci Med. 1995;40(5):623–628.
- , , , , . Women's health after pregnancy and child outcomes at age 3 years: a prospective cohort study. Am J Public Health. 2002;92(8):1312–1318.
- , , , . The influence of children's cognitive delay and behavior problems on maternal depression. J Pediatr. 2015;167(3):679–686.
- , , , , . Maternal prenatal symptoms of depression and down regulation of placental monoamine oxidase A expression. J Psychosom Res. 2013;75(4):341–345.
- , , , , . High pregnancy anxiety during mid‐gestation is associated with decreased gray matter density in 6–9‐year‐old children. Psychoneuroendocrinology. 2010;35(1):141–153.
- , , , , . Factors affecting recruitment into depression trials: Systematic review, meta‐synthesis and conceptual framework. J Affect Disord. 2015;172:274–290.