User login
SHM Rolls Out New Structure for Leadership Academy 2017
For years, SHM’s Leadership Academy courses have been selling out. To meet and exceed the demand and expectations of attendees, SHM is rolling out a new structure designed to provide more opportunities for those who seek to advance their careers and expand their leadership skills.
New for Leadership Academy 2017, Strategic Essentials (formerly Leadership Foundations), Influential Management, and Mastering Teamwork will be available to all attendees regardless of previous attendance. SHM provides recommendations for interested registrants to allow them to determine which course fits them best in their leadership journey.
The 2017 Leadership Academy will be held October 23–26, 2017, at the JW Marriott Scottsdale Camelback Inn Resort & Spa in Arizona. The revised course structure includes:
Strategic Essentials
Learn how to evaluate personal leadership strengths and weaknesses, create and execute a communication strategy for key team members, understand key hospital finances and drivers, examine how hospital metrics are derived, and more in this four-day hands-on educational course covering various hospital medicine–focused leadership skills.
Attendees are grouped at tables of 10, each with a skilled facilitator to ensure meaningful, relevant application of concepts to hands-on activities.
The Strategic Essentials course is recommended for residents, early-career hospitalists, first-time hospitalist leaders, and hospitalist leaders wishing to strengthen their leadership skills set and advance their careers.
Influential Management
The Influential Management course provides leadership skills specific to the incorporation of meta-leadership styles, driving culture change through specific leadership behaviors and actions, financial storytelling, effective professional negotiation with proven techniques, and more.
Participants engage in several tabletop exercises throughout the four-day course, encouraging an interactive learning environment with world-renowned faculty.
The Influential Management course is recommended for early-career hospitalists to midlevel-career hospitalists and hospitalist leaders desiring to enhance their leadership skills set in specific areas.
Mastering Teamwork
Find out how to critically assess program growth opportunities and develop operational plans; utilize the principles of SWARM intelligence; lead, manage, and motivate teams in complex hospital environments; and communicate effectively in the Mastering Teamwork course.
Prominent faculty deep-dive into many of leadership skills and practices in this session to provide participants with a better understanding of team and organizational dynamics and how their personal leadership skills can strengthen teams and improve organizational growth and success.
Mastering Teamwork is recommended for hospitalists with three or more years of experience as well as hospitalist leaders looking to advance their career to the organizational strategy level.
Learn more about SHM’s Leadership Academy at www.shmleadershipacademy.org.
For years, SHM’s Leadership Academy courses have been selling out. To meet and exceed the demand and expectations of attendees, SHM is rolling out a new structure designed to provide more opportunities for those who seek to advance their careers and expand their leadership skills.
New for Leadership Academy 2017, Strategic Essentials (formerly Leadership Foundations), Influential Management, and Mastering Teamwork will be available to all attendees regardless of previous attendance. SHM provides recommendations for interested registrants to allow them to determine which course fits them best in their leadership journey.
The 2017 Leadership Academy will be held October 23–26, 2017, at the JW Marriott Scottsdale Camelback Inn Resort & Spa in Arizona. The revised course structure includes:
Strategic Essentials
Learn how to evaluate personal leadership strengths and weaknesses, create and execute a communication strategy for key team members, understand key hospital finances and drivers, examine how hospital metrics are derived, and more in this four-day hands-on educational course covering various hospital medicine–focused leadership skills.
Attendees are grouped at tables of 10, each with a skilled facilitator to ensure meaningful, relevant application of concepts to hands-on activities.
The Strategic Essentials course is recommended for residents, early-career hospitalists, first-time hospitalist leaders, and hospitalist leaders wishing to strengthen their leadership skills set and advance their careers.
Influential Management
The Influential Management course provides leadership skills specific to the incorporation of meta-leadership styles, driving culture change through specific leadership behaviors and actions, financial storytelling, effective professional negotiation with proven techniques, and more.
Participants engage in several tabletop exercises throughout the four-day course, encouraging an interactive learning environment with world-renowned faculty.
The Influential Management course is recommended for early-career hospitalists to midlevel-career hospitalists and hospitalist leaders desiring to enhance their leadership skills set in specific areas.
Mastering Teamwork
Find out how to critically assess program growth opportunities and develop operational plans; utilize the principles of SWARM intelligence; lead, manage, and motivate teams in complex hospital environments; and communicate effectively in the Mastering Teamwork course.
Prominent faculty deep-dive into many of leadership skills and practices in this session to provide participants with a better understanding of team and organizational dynamics and how their personal leadership skills can strengthen teams and improve organizational growth and success.
Mastering Teamwork is recommended for hospitalists with three or more years of experience as well as hospitalist leaders looking to advance their career to the organizational strategy level.
Learn more about SHM’s Leadership Academy at www.shmleadershipacademy.org.
For years, SHM’s Leadership Academy courses have been selling out. To meet and exceed the demand and expectations of attendees, SHM is rolling out a new structure designed to provide more opportunities for those who seek to advance their careers and expand their leadership skills.
New for Leadership Academy 2017, Strategic Essentials (formerly Leadership Foundations), Influential Management, and Mastering Teamwork will be available to all attendees regardless of previous attendance. SHM provides recommendations for interested registrants to allow them to determine which course fits them best in their leadership journey.
The 2017 Leadership Academy will be held October 23–26, 2017, at the JW Marriott Scottsdale Camelback Inn Resort & Spa in Arizona. The revised course structure includes:
Strategic Essentials
Learn how to evaluate personal leadership strengths and weaknesses, create and execute a communication strategy for key team members, understand key hospital finances and drivers, examine how hospital metrics are derived, and more in this four-day hands-on educational course covering various hospital medicine–focused leadership skills.
Attendees are grouped at tables of 10, each with a skilled facilitator to ensure meaningful, relevant application of concepts to hands-on activities.
The Strategic Essentials course is recommended for residents, early-career hospitalists, first-time hospitalist leaders, and hospitalist leaders wishing to strengthen their leadership skills set and advance their careers.
Influential Management
The Influential Management course provides leadership skills specific to the incorporation of meta-leadership styles, driving culture change through specific leadership behaviors and actions, financial storytelling, effective professional negotiation with proven techniques, and more.
Participants engage in several tabletop exercises throughout the four-day course, encouraging an interactive learning environment with world-renowned faculty.
The Influential Management course is recommended for early-career hospitalists to midlevel-career hospitalists and hospitalist leaders desiring to enhance their leadership skills set in specific areas.
Mastering Teamwork
Find out how to critically assess program growth opportunities and develop operational plans; utilize the principles of SWARM intelligence; lead, manage, and motivate teams in complex hospital environments; and communicate effectively in the Mastering Teamwork course.
Prominent faculty deep-dive into many of leadership skills and practices in this session to provide participants with a better understanding of team and organizational dynamics and how their personal leadership skills can strengthen teams and improve organizational growth and success.
Mastering Teamwork is recommended for hospitalists with three or more years of experience as well as hospitalist leaders looking to advance their career to the organizational strategy level.
Learn more about SHM’s Leadership Academy at www.shmleadershipacademy.org.
Improving the Care of Patients with COPD
In recognition of Chronic Obstructive Pulmonary Disease (COPD) Month, check out SHM’s free guide and toolkit to improve the care of patients hospitalized for an exacerbation of COPD. The toolkit can also help you make changes to COPD care at both the individual patient and institutional level.
Download the guide or view the toolkit today at www.hospitalmedicine.org/copd.
In recognition of Chronic Obstructive Pulmonary Disease (COPD) Month, check out SHM’s free guide and toolkit to improve the care of patients hospitalized for an exacerbation of COPD. The toolkit can also help you make changes to COPD care at both the individual patient and institutional level.
Download the guide or view the toolkit today at www.hospitalmedicine.org/copd.
In recognition of Chronic Obstructive Pulmonary Disease (COPD) Month, check out SHM’s free guide and toolkit to improve the care of patients hospitalized for an exacerbation of COPD. The toolkit can also help you make changes to COPD care at both the individual patient and institutional level.
Download the guide or view the toolkit today at www.hospitalmedicine.org/copd.
Help Improve Quality at Your Institution with SHM
October 16–22 is the National Association for Healthcare Quality’s “Healthcare Quality Week,” and SHM’s Center for Hospital Innovation & Improvement provides a variety of resources, tools, and programs to help address quality and patient safety issues at your institution. Find out how SHM can help you improve patient safety and outcomes through our Center for Hospital Innovation & Improvement at www.hospialmedicine.org/QI.
October 16–22 is the National Association for Healthcare Quality’s “Healthcare Quality Week,” and SHM’s Center for Hospital Innovation & Improvement provides a variety of resources, tools, and programs to help address quality and patient safety issues at your institution. Find out how SHM can help you improve patient safety and outcomes through our Center for Hospital Innovation & Improvement at www.hospialmedicine.org/QI.
October 16–22 is the National Association for Healthcare Quality’s “Healthcare Quality Week,” and SHM’s Center for Hospital Innovation & Improvement provides a variety of resources, tools, and programs to help address quality and patient safety issues at your institution. Find out how SHM can help you improve patient safety and outcomes through our Center for Hospital Innovation & Improvement at www.hospialmedicine.org/QI.
Strengthen Your Role as a Practice Administrator with SHM’s Mentor Program
- Model 1: Mentors/Mentees. Less experienced administrators will be paired with seasoned professionals to gain more experience or exposure.
- Model 2: Buddy System. Administrators at any level of expertise or experience will be paired with a peer so they both can learn from each other.
Interested in being a mentor or mentee for the 2017 program? Complete the online form at www.hospitalmedicine.org/pamentor used to match you up to other individuals who have similar needs for improvement.
- Model 1: Mentors/Mentees. Less experienced administrators will be paired with seasoned professionals to gain more experience or exposure.
- Model 2: Buddy System. Administrators at any level of expertise or experience will be paired with a peer so they both can learn from each other.
Interested in being a mentor or mentee for the 2017 program? Complete the online form at www.hospitalmedicine.org/pamentor used to match you up to other individuals who have similar needs for improvement.
- Model 1: Mentors/Mentees. Less experienced administrators will be paired with seasoned professionals to gain more experience or exposure.
- Model 2: Buddy System. Administrators at any level of expertise or experience will be paired with a peer so they both can learn from each other.
Interested in being a mentor or mentee for the 2017 program? Complete the online form at www.hospitalmedicine.org/pamentor used to match you up to other individuals who have similar needs for improvement.
Become a Fellow in Hospital Medicine
The application is open through November 30, with a decision on or before December 31, 2016. Apply now and learn how you can join other hospitalists who have earned this exclusive designation and recognition at www.hospitalmedicine.org/fellows.
The application is open through November 30, with a decision on or before December 31, 2016. Apply now and learn how you can join other hospitalists who have earned this exclusive designation and recognition at www.hospitalmedicine.org/fellows.
The application is open through November 30, with a decision on or before December 31, 2016. Apply now and learn how you can join other hospitalists who have earned this exclusive designation and recognition at www.hospitalmedicine.org/fellows.
Leadership Academy Helps SHM Member Improve Patient Flow, Satisfaction
This month, The Hospitalist spotlights G. Randy Smith Jr., MD, MS, SFHM, assistant professor in the Division of Hospital Medicine at the Northwestern University Feinberg School of Medicine and medical director of Unit 16 West at Northwestern Memorial Hospital in Chicago. Dr. Smith is an active member of SHM’s Practice Analysis Committee and a Leadership Academy veteran who has translated his learnings into more efficient rounding and patient-flow methodology.
Question: What inspired you to begin working in hospital medicine and later join SHM?
Answer: Interest in taking care of acutely ill patients inspired me to start working in hospital medicine. Evolution of this interest into care-delivery design inspired me to remain in hospital medicine. Joining SHM enabled me to make contacts nationally with people who share similar interests and engage in collaboration, which has been helpful for my growth as a physician.
Q: How has SHM provided you with resources to improve patient care during your time as a member?
A: The SHM annual meetings have provided a consistent framework for dissemination of clinically relevant innovations and discoveries. Each year I’ve attended, I’ve always learned something new from both the posters on display and from a quality improvement presentation. Last year at Hospital Medicine 2016, the HEADS-UP plenary abstract presentation was one very good example of a different approach to interdisciplinary rounding that I would not have been aware of without attending the SHM annual meeting.
Q: How did attending Leadership Academy help you grow to reach your medical director position at Northwestern Memorial?
A: Leadership Academy helped to open my mind to principles of negotiation and expectation management as well as self-awareness, which are not usually presented in medical school or residency. Many of the skills taught can be learned the hard way through the trials of life, but the Leadership Academy accelerated my real-world learning.
My hospital’s leadership recognized the skills I developed with the assistance of Leadership Academy, which helped me to maintain my effectiveness in my medical director role.
Skills obtained in the Leadership Academy helped me to incorporate ward-based afternoon throughput meetings into a hospital-wide patient-flow management network. I also learned to successfully negotiate procurement of chairs for our physicians to sit at the patient’s bedside in the hopes of improving patient satisfaction.
Q: How has your work on the Practice Analysis Committee impacted how you manage your hospital medicine teams?
A: My involvement in the Practice Analysis Committee is yet another example of an opportunity provided by SHM to develop a skills set I would not otherwise have the opportunity to develop. Working on the State of Hospital Medicine survey involves prioritizing information with the burden of the respondents’ time and effort in mind. Sensitivities to stakeholder interest play a major role as well.
Achieving balance between aspiring definitions of concepts to help drive the field and working definitions used heterogeneously throughout the country represents the hardest task of the committee members to sort; I’m very privileged to take the lessons learned through member dialogue and help colleagues apply the lessons locally.
Q: Hospital medicine is celebrating its 20th anniversary this year. How do you see the role of hospitalists evolving over the next 20 years?
A: Change has been a constant in hospital medicine since I began in 2004 and will continue to remain so. Because of the financial and documentary pressures placed on hospitals and physicians, hospital medicine finds itself in a state of flux at the moment. I believe these pressures will drive the 7-on/7-off hospitalist direct-care model as it exists today to evolve into something else. In particular, hospitalist groups, which engage solely in documentation and “decision in name” only and devolve all clinical decision making to another set of physicians in the hospital, are especially nonviable over the long term. I think many hospital administrators believe this as well. Hospital medicine must show value, including in the realm of direct clinical care.
One possibility is that we evolve into a “supervisor” model, where a program is composed of a few experienced hospitalists supervising numerous physician extenders, who in turn rely on multidisciplinary teams in the hospital for clinical decision-making input. Hospitalist physicians will slightly move away from direct clinical decision making in such a model.
Another possibility involves evolution of information support systems to a point where teams of providers organized around a single medical problem, e.g., congestive heart failure, can be replaced, leaving the hospitalist to make patient-centered clinical decisions with updated multidisciplinary input available electronically.
With information systems that provide equal access to evidence-driven guidance for optimal clinical practice, hospitalists will outperform subspecialists at the bedside on patient-centeredness, cost, and availability.
Regardless of how inpatient care evolves, hospital medicine will undoubtedly be at the epicenter of change for years to come. TH
This month, The Hospitalist spotlights G. Randy Smith Jr., MD, MS, SFHM, assistant professor in the Division of Hospital Medicine at the Northwestern University Feinberg School of Medicine and medical director of Unit 16 West at Northwestern Memorial Hospital in Chicago. Dr. Smith is an active member of SHM’s Practice Analysis Committee and a Leadership Academy veteran who has translated his learnings into more efficient rounding and patient-flow methodology.
Question: What inspired you to begin working in hospital medicine and later join SHM?
Answer: Interest in taking care of acutely ill patients inspired me to start working in hospital medicine. Evolution of this interest into care-delivery design inspired me to remain in hospital medicine. Joining SHM enabled me to make contacts nationally with people who share similar interests and engage in collaboration, which has been helpful for my growth as a physician.
Q: How has SHM provided you with resources to improve patient care during your time as a member?
A: The SHM annual meetings have provided a consistent framework for dissemination of clinically relevant innovations and discoveries. Each year I’ve attended, I’ve always learned something new from both the posters on display and from a quality improvement presentation. Last year at Hospital Medicine 2016, the HEADS-UP plenary abstract presentation was one very good example of a different approach to interdisciplinary rounding that I would not have been aware of without attending the SHM annual meeting.
Q: How did attending Leadership Academy help you grow to reach your medical director position at Northwestern Memorial?
A: Leadership Academy helped to open my mind to principles of negotiation and expectation management as well as self-awareness, which are not usually presented in medical school or residency. Many of the skills taught can be learned the hard way through the trials of life, but the Leadership Academy accelerated my real-world learning.
My hospital’s leadership recognized the skills I developed with the assistance of Leadership Academy, which helped me to maintain my effectiveness in my medical director role.
Skills obtained in the Leadership Academy helped me to incorporate ward-based afternoon throughput meetings into a hospital-wide patient-flow management network. I also learned to successfully negotiate procurement of chairs for our physicians to sit at the patient’s bedside in the hopes of improving patient satisfaction.
Q: How has your work on the Practice Analysis Committee impacted how you manage your hospital medicine teams?
A: My involvement in the Practice Analysis Committee is yet another example of an opportunity provided by SHM to develop a skills set I would not otherwise have the opportunity to develop. Working on the State of Hospital Medicine survey involves prioritizing information with the burden of the respondents’ time and effort in mind. Sensitivities to stakeholder interest play a major role as well.
Achieving balance between aspiring definitions of concepts to help drive the field and working definitions used heterogeneously throughout the country represents the hardest task of the committee members to sort; I’m very privileged to take the lessons learned through member dialogue and help colleagues apply the lessons locally.
Q: Hospital medicine is celebrating its 20th anniversary this year. How do you see the role of hospitalists evolving over the next 20 years?
A: Change has been a constant in hospital medicine since I began in 2004 and will continue to remain so. Because of the financial and documentary pressures placed on hospitals and physicians, hospital medicine finds itself in a state of flux at the moment. I believe these pressures will drive the 7-on/7-off hospitalist direct-care model as it exists today to evolve into something else. In particular, hospitalist groups, which engage solely in documentation and “decision in name” only and devolve all clinical decision making to another set of physicians in the hospital, are especially nonviable over the long term. I think many hospital administrators believe this as well. Hospital medicine must show value, including in the realm of direct clinical care.
One possibility is that we evolve into a “supervisor” model, where a program is composed of a few experienced hospitalists supervising numerous physician extenders, who in turn rely on multidisciplinary teams in the hospital for clinical decision-making input. Hospitalist physicians will slightly move away from direct clinical decision making in such a model.
Another possibility involves evolution of information support systems to a point where teams of providers organized around a single medical problem, e.g., congestive heart failure, can be replaced, leaving the hospitalist to make patient-centered clinical decisions with updated multidisciplinary input available electronically.
With information systems that provide equal access to evidence-driven guidance for optimal clinical practice, hospitalists will outperform subspecialists at the bedside on patient-centeredness, cost, and availability.
Regardless of how inpatient care evolves, hospital medicine will undoubtedly be at the epicenter of change for years to come. TH
This month, The Hospitalist spotlights G. Randy Smith Jr., MD, MS, SFHM, assistant professor in the Division of Hospital Medicine at the Northwestern University Feinberg School of Medicine and medical director of Unit 16 West at Northwestern Memorial Hospital in Chicago. Dr. Smith is an active member of SHM’s Practice Analysis Committee and a Leadership Academy veteran who has translated his learnings into more efficient rounding and patient-flow methodology.
Question: What inspired you to begin working in hospital medicine and later join SHM?
Answer: Interest in taking care of acutely ill patients inspired me to start working in hospital medicine. Evolution of this interest into care-delivery design inspired me to remain in hospital medicine. Joining SHM enabled me to make contacts nationally with people who share similar interests and engage in collaboration, which has been helpful for my growth as a physician.
Q: How has SHM provided you with resources to improve patient care during your time as a member?
A: The SHM annual meetings have provided a consistent framework for dissemination of clinically relevant innovations and discoveries. Each year I’ve attended, I’ve always learned something new from both the posters on display and from a quality improvement presentation. Last year at Hospital Medicine 2016, the HEADS-UP plenary abstract presentation was one very good example of a different approach to interdisciplinary rounding that I would not have been aware of without attending the SHM annual meeting.
Q: How did attending Leadership Academy help you grow to reach your medical director position at Northwestern Memorial?
A: Leadership Academy helped to open my mind to principles of negotiation and expectation management as well as self-awareness, which are not usually presented in medical school or residency. Many of the skills taught can be learned the hard way through the trials of life, but the Leadership Academy accelerated my real-world learning.
My hospital’s leadership recognized the skills I developed with the assistance of Leadership Academy, which helped me to maintain my effectiveness in my medical director role.
Skills obtained in the Leadership Academy helped me to incorporate ward-based afternoon throughput meetings into a hospital-wide patient-flow management network. I also learned to successfully negotiate procurement of chairs for our physicians to sit at the patient’s bedside in the hopes of improving patient satisfaction.
Q: How has your work on the Practice Analysis Committee impacted how you manage your hospital medicine teams?
A: My involvement in the Practice Analysis Committee is yet another example of an opportunity provided by SHM to develop a skills set I would not otherwise have the opportunity to develop. Working on the State of Hospital Medicine survey involves prioritizing information with the burden of the respondents’ time and effort in mind. Sensitivities to stakeholder interest play a major role as well.
Achieving balance between aspiring definitions of concepts to help drive the field and working definitions used heterogeneously throughout the country represents the hardest task of the committee members to sort; I’m very privileged to take the lessons learned through member dialogue and help colleagues apply the lessons locally.
Q: Hospital medicine is celebrating its 20th anniversary this year. How do you see the role of hospitalists evolving over the next 20 years?
A: Change has been a constant in hospital medicine since I began in 2004 and will continue to remain so. Because of the financial and documentary pressures placed on hospitals and physicians, hospital medicine finds itself in a state of flux at the moment. I believe these pressures will drive the 7-on/7-off hospitalist direct-care model as it exists today to evolve into something else. In particular, hospitalist groups, which engage solely in documentation and “decision in name” only and devolve all clinical decision making to another set of physicians in the hospital, are especially nonviable over the long term. I think many hospital administrators believe this as well. Hospital medicine must show value, including in the realm of direct clinical care.
One possibility is that we evolve into a “supervisor” model, where a program is composed of a few experienced hospitalists supervising numerous physician extenders, who in turn rely on multidisciplinary teams in the hospital for clinical decision-making input. Hospitalist physicians will slightly move away from direct clinical decision making in such a model.
Another possibility involves evolution of information support systems to a point where teams of providers organized around a single medical problem, e.g., congestive heart failure, can be replaced, leaving the hospitalist to make patient-centered clinical decisions with updated multidisciplinary input available electronically.
With information systems that provide equal access to evidence-driven guidance for optimal clinical practice, hospitalists will outperform subspecialists at the bedside on patient-centeredness, cost, and availability.
Regardless of how inpatient care evolves, hospital medicine will undoubtedly be at the epicenter of change for years to come. TH
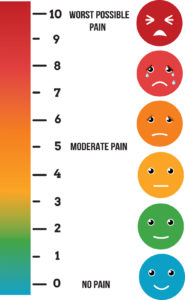
Managing Pain in Postoperative Patients: What the Hospitalist Needs to Know
Start earning free CME credits today at www.shmconsults.com.
Start earning free CME credits today at www.shmconsults.com.
Start earning free CME credits today at www.shmconsults.com.
You Can Earn CME with shmConsults
Appropriate Use of Targeted Oral Anticoagulants to Prevent Stroke in Patients with Nonvalvular Atrial Fibrillation
This activity includes thorough discussions on initial management of patients with nonvalvular atrial fibrillation (NVAF), appropriate situations for oral anticoagulation in the presence of NVAF, appropriate choice of oral anticoagulant, reversal of oral anticoagulation, and guidelines for oral anticoagulation and stroke prevention in NVAF patients and special-population NVAF patients.
Four modules addressing various aspects of anticoagulation/thrombosis have been updated and include:
- Target-Specific Oral Anticoagulants for Stroke Prophylaxis in Patients with NVAF
- Management of Postoperative Atrial Fibrillation
- Perioperative Bridging of Anticoagulant Therapy
- Perioperative Management of Anticoagulation
Appropriate Use of Targeted Oral Anticoagulants to Prevent Stroke in Patients with Nonvalvular Atrial Fibrillation
This activity includes thorough discussions on initial management of patients with nonvalvular atrial fibrillation (NVAF), appropriate situations for oral anticoagulation in the presence of NVAF, appropriate choice of oral anticoagulant, reversal of oral anticoagulation, and guidelines for oral anticoagulation and stroke prevention in NVAF patients and special-population NVAF patients.
Four modules addressing various aspects of anticoagulation/thrombosis have been updated and include:
- Target-Specific Oral Anticoagulants for Stroke Prophylaxis in Patients with NVAF
- Management of Postoperative Atrial Fibrillation
- Perioperative Bridging of Anticoagulant Therapy
- Perioperative Management of Anticoagulation
Appropriate Use of Targeted Oral Anticoagulants to Prevent Stroke in Patients with Nonvalvular Atrial Fibrillation
This activity includes thorough discussions on initial management of patients with nonvalvular atrial fibrillation (NVAF), appropriate situations for oral anticoagulation in the presence of NVAF, appropriate choice of oral anticoagulant, reversal of oral anticoagulation, and guidelines for oral anticoagulation and stroke prevention in NVAF patients and special-population NVAF patients.
Four modules addressing various aspects of anticoagulation/thrombosis have been updated and include:
- Target-Specific Oral Anticoagulants for Stroke Prophylaxis in Patients with NVAF
- Management of Postoperative Atrial Fibrillation
- Perioperative Bridging of Anticoagulant Therapy
- Perioperative Management of Anticoagulation
Compete and Solve Clinical Cases with Human Diagnosis Project
SHM recently partnered with the Human Diagnosis Project. Human Dx is the world’s first open diagnostic system, which aims to understand the fundamental data structure of diagnosis and, in the future, considerably impact the cost of, access to, and effectiveness of healthcare globally.
Human Dx’s Global Morning Reports feature weekly case competitions of differential diagnoses and clinical reasoning skills. Each day, attendings, fellows, residents, and medical students have the opportunity to solve the best cases from around the world from the prior day and submit cases for the next day. This partnership with SHM provides a unique, interactive learning platform with cases tailored to hospitalists.
The rules are simple:
- Increase your “Impact” by creating and solving cases online.
- Creating cases creates more “Impact” than solving cases.
The team and individual with the most “Impact” each week win. Sign up today and test your skills in hospital medicine diagnostics at www.humandx.org/shm/.
SHM recently partnered with the Human Diagnosis Project. Human Dx is the world’s first open diagnostic system, which aims to understand the fundamental data structure of diagnosis and, in the future, considerably impact the cost of, access to, and effectiveness of healthcare globally.
Human Dx’s Global Morning Reports feature weekly case competitions of differential diagnoses and clinical reasoning skills. Each day, attendings, fellows, residents, and medical students have the opportunity to solve the best cases from around the world from the prior day and submit cases for the next day. This partnership with SHM provides a unique, interactive learning platform with cases tailored to hospitalists.
The rules are simple:
- Increase your “Impact” by creating and solving cases online.
- Creating cases creates more “Impact” than solving cases.
The team and individual with the most “Impact” each week win. Sign up today and test your skills in hospital medicine diagnostics at www.humandx.org/shm/.
SHM recently partnered with the Human Diagnosis Project. Human Dx is the world’s first open diagnostic system, which aims to understand the fundamental data structure of diagnosis and, in the future, considerably impact the cost of, access to, and effectiveness of healthcare globally.
Human Dx’s Global Morning Reports feature weekly case competitions of differential diagnoses and clinical reasoning skills. Each day, attendings, fellows, residents, and medical students have the opportunity to solve the best cases from around the world from the prior day and submit cases for the next day. This partnership with SHM provides a unique, interactive learning platform with cases tailored to hospitalists.
The rules are simple:
- Increase your “Impact” by creating and solving cases online.
- Creating cases creates more “Impact” than solving cases.
The team and individual with the most “Impact” each week win. Sign up today and test your skills in hospital medicine diagnostics at www.humandx.org/shm/.
Delirium ABCDEF Bundle Program Implementation Toolkit Now Available
The Baylor Research Institute and SHM joined forces to provide a new resource to help accelerate adoption of a specific set of patient safety practices (collectively termed the ABCDEF bundle) to mitigate delirium in the ICU. This guide will allow you to impact care at both the individual patient and the institutional levels. It is intended for the broad, multidisciplinary spectrum of personnel involved in hospital-based quality improvement and patient safety efforts, ranging from frontline care providers to executive leaders. View the toolkit and download the guide at www.hospitalmedicine.org/delirium.
The Baylor Research Institute and SHM joined forces to provide a new resource to help accelerate adoption of a specific set of patient safety practices (collectively termed the ABCDEF bundle) to mitigate delirium in the ICU. This guide will allow you to impact care at both the individual patient and the institutional levels. It is intended for the broad, multidisciplinary spectrum of personnel involved in hospital-based quality improvement and patient safety efforts, ranging from frontline care providers to executive leaders. View the toolkit and download the guide at www.hospitalmedicine.org/delirium.
The Baylor Research Institute and SHM joined forces to provide a new resource to help accelerate adoption of a specific set of patient safety practices (collectively termed the ABCDEF bundle) to mitigate delirium in the ICU. This guide will allow you to impact care at both the individual patient and the institutional levels. It is intended for the broad, multidisciplinary spectrum of personnel involved in hospital-based quality improvement and patient safety efforts, ranging from frontline care providers to executive leaders. View the toolkit and download the guide at www.hospitalmedicine.org/delirium.