User login
Sudden loss of vision
Q: What causes of sudden unilateral vision loss would you consider? What would you do next?
Your examination yields the following:
Medical history
- Borderline hypertension
- Hyperlipidemia (was on a medication but discontinued it on his own)
- Smoking 25 pack-years; quit 2 years ago
- Occasional alcohol intake
- No medications
- Electrical contractor by trade
- Parents living and well; siblings have hypertension but no other illnesses.
Review of systems
Negative except for occasional nasal congestion and low back pain.
Physical examination
- Alert male in no distress. Blood pressure, 146/86 mm Hg; weight, 85 kg; heart rate, 80; respiratory rate, 20; temperature normal; skin warm and dry.
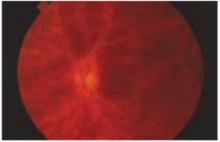
- Head, eyes, ears, nose, throat: pupils are equal, round, and reactive to light and accommodation; extraocular movement intact; retinal exam is depicted in the Figure. Tympanic membranes, throat, and neck normal; carotids normal.
- Heart and lung exam unremarkable. Spleen questionably palpable. Extremities normal. Neurologic exam normal, except for eye findings.
FIGURE
Retinal exam
Referring to Harrison’s Textbook of Medicine, you find the following entry:
“Venous occlusion of the retina is often idiopathic, but hypertension, diabetes, and glaucoma are prominent risk factors. The benefit of treatment with anticoagulants is unproven and carries the risk of hemorrhage into the vitreous. Polycythemia, thrombocythemia, or other factors leading to an underlying hypercoagulable state should be corrected.”1
You also reviewed information from UpToDate, which revealed a British article linking retinal venous occlusion with an increased risk of cardiovascular disease. It recommends that clinicians use an algorithm to determine the appropriate treatment.2 Additional research noted various interventions for the venous occlusion itself, but none had sufficient numbers to be considered reliable in recommending treatment.
You have identified 3 problems, 2 of which you deal with regularly and a third that requires consultation:
- Hypertension
- Hyperlipidemia
- Central retinal venous occlusion (CRVO) (rule out underlying hypercoagulable state).
Ophthalmologist’s report
An ophthalmologist confirms a diagnosis of left retinal vein occlusion, and recommends a period of observation, to see if vision returns. The opthalmologist also asks the patient to return to you for an investigation of possible underlying medical conditions.
Further primary care evaluation
The patient’s history suggests nothing that would inhibit a return of vision. Findings on the physical examination are unchanged except for the left fundus. The patient is quite concerned about another “stroke,” particularly in the other eye. He wants a guarantee he will be okay.
Laboratory evaluation:
- Complete blood count, normal
- Urea nitrogen (BUN), 20 mg/dL
- Creatinine kinase, 1.2 mckat/L
- Liver functions within normal limits
- Glucose, 86 mg/dL
- Cholesterol, 230 mg/dL
- Triglycerides, 186 mg/dL
- HDL, 41 mg/dL; LDL, 136 mg/dL
- Total serum protein levels, normal.
Additional time was required by the family physician to coordinate care of this patient. A team management code (99361 for 30 minutes and 99362 for 60 minutes) may not be billed on the same day as an e/m code, as carriers bundle this into the e/m. In addition, most carriers do not pay for the 99361 or 99362 codes. Therefore, the conference should ideally occur the day of an e/m code and be documented with that service. In this instance, the care occurred over several days, so no additional billing was allowed for team management.
Details of central retinal venous occlusion
You assure the patient you will coordinate care with the ophthalmologist, who subsequently offers the following summary about CRVO:
- For most patients with CRVO, vision decreases to 20/100, 20/200, or worse, usually permanently if the occlusion is indeed venous and not arterial as well. If the condition is secondary to ischemia, vision is usually limited to 20/300 or worse, permanently.
- Most patients want their vision “fixed” right away, but that is usually not possible. Hypertension control is most important. Uncommon causes include polycythemia vera, emphysema, sickle cell disease, multiple myeloma, macroglobulinemia, hyperproteinemia, cystic fibrosis of the pancreas, and peritoneal dialysis. Occasionally, it can occur secondary to hypotension, as from a ruptured aortic aneurysm, delivery-associated blood loss, or surgical trauma.
- Hypertension and other atherosclerotic risk factors must be controlled. Treatment with platelet inhibitors is often recommended and glaucoma control is very important, especially for African American patients. Chronic open-angle glaucoma can present as CRVO, and results can be devastating. African Americans are about 100 times more likely than Caucasians to have glaucoma (1/7 vs 3/2000).
Management dos and don’ts
CRVO is entirely different than retinal hemorrhage or vitreous hemorrhage. The correct diagnosis must be confirmed by an ophthalmologist, to ensure proper evaluation and management.
Reduce blood pressure
You return to your patient and share your conversation with the consultant. According to the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7) guidelines, the patient has Stage I hypertension. The goal for treatment is medical management to reduce pressure to below 120/80 mm Hg.3
The patient elects treatment with a beta-blocker rather than a thiazide diuretic; he wishes to avoid monitoring of electrolytes that would be necessary because he often becomes dehydrated on the job. He will have the nurse at his company monitor his blood pressure.
Reduce lipids
Also, according to the National Cholesterol Education Program, this patient meets criteria for treatment of hyperlipidemia.4 He is given dietary instruction, information about lipids, a prescription for a statin as he believes he has already been following a quite restrictive diet for over 4 months.
Use anticoagulant?
Finally, you consult a hematologist about the appropriate evaluation for a hypercoagulable state. Following is her report:
- The retinal vein is anatomically different from other veins, being tightly encased in a sheath with the retinal artery and optic nerve. Disorders of these structures can compress or inflame the vein, leading to thrombosis. Consequently, local factors may play a role in development of retinal vein thrombosis—a systemic disorder is not required for this process to occur. CVRO is seldom associated with an underlying hypercoagulable state.5,6
- The effectiveness of medical intervention is unproven. Acute anticoagulation is associated with retinal hemorrhage and is not recommended. Recurrent retinal venous occlusion in the contralateral eye occurs in approximately 12% of patients within 4 years. Because of the risks of anticoagulation and unproven benefits in CRVO, you both elect to avoid this treatment.
If the patient were to request anticoagulation, therapy should be withheld for 2 to 3 months, the time required for retinal perfusion to stabilize. Antiplatelet agents such as aspirin have no role in preventing recurrent venous thrombosis.
Confirmation of this controversy in treatment was obtained using a literature search. A review article in Eye discussed that while the role of thrombophilia is unclear, the need for a randomized study of anticoagulation in the patient with CRVO is needed.6
Final decisions
After considering your consultant’s suggestions, you realize that finding a prothrombotic state is unlikely and will be not change management. Moreover, medical intervention is unlikely to change the natural history of this condition, and it might lead inadvertently to insurance or employment discrimination. You review the previous complete blood count to make sure you have not missed erythrocytosis or thrombocytosis—both of which have well-defined treatments.
Follow-up monitoring was scheduled by the ophthalmologist and you continue to manage the patient’s hypertension and hyperlipidemia.
This patient had a relatively uncommon condition that necessitated consultation with 2 specialists. After weighing the evidence and likelihood of benefit of unproven therapies for CVRO, the patient elected to manage other clear risk factors for atherosclerotic vascular disease. Management of this patient melds issues of ethics and evidence, with core skills to foster a good doctor-patient relationship.
At the risk of sounding like a bad joke, I’d like to open my commentary with the question:
“Why did this patient go to the family physician?” This patient was seen in an urban setting with ample access to any medical specialist, and he had an insurance plan that allowed open access contact with most, if not all, of the physicians in the community. This patient also knew enough about his illness to know that the final answer or treatment for his presenting problem would likely not be found in the family physician’s office.
The value that the family physician brought to this patient can be described as follows:
Navigator/Coordinator: The family physician was able to help this patient through the maze of medical specialists to find the right physicians to evaluate and treat the presenting problem, and to arrange for ongoing evaluation and management after specialist consultations.
Interpreter/Translator: The family physician was able to take the information provided by the specialist physicians and translate that information into language the patient could understand. This process must occur if the patient is expected to comply with treatment, evaluation and lifestyle change recommendations.
Comprehensive caregiver: While supporting the patient in coping with his vision loss, the family physician used this unfortunate occurrence as motivation to address modifiable risk factors—hypertension, obesity, elevated blood glucose, and elevated lipids. Managing these conditions may not be glamorous, but addressing all facets of a patient’s well being is what we family physicians do best. Caring for patients, not just treating illnesses, is a core value of family medicine.
Imagine this patient’s thought process from his arrival with a loss of vision to his departure with a plan to deal with hypertension, obesity, elevated blood glucose, and elevated lipids, all in the context of his job and family and community life. The holistic management of this patient in the context of his life is the main value added by the family physician for this patient. This management also completely supports the patient’s wish to avoid “another stroke.”
One of my colleagues once asked me: “Wouldn’t you like to be the kind of physician whose patient comes in with a cold and leaves with an order for a mammogram?” Family physicians have the knowledge, skills, and perspective necessary to treat the patient, not just the illness. Let’s keep doing what we do best for our patients.
Paul Paulman, MD
1. Harrison’s Principles of Internal Medicine. 15th ed. Eds. Braunwald E, Fauci AS, Kasper DL, Hauser SL, Longo DL, Jameson JL. New York, NY: McGraw-Hill; 2001.
2. Martin SC, Butcher A, Martin N, et al. Cardiovascular risk assessment in patients with retinal vein occlusion. Br J Ophthalmol 2002;86:774-776.
3. National Heart, Lung, and Blood Institute. National High Blood Pressure Education Program. Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7). 2003. Available at: www.nhlbi.nih.gov/guidelines/hypertension/jncintro.htm. Accessed on March 16, 2004.
4. National Heart, Lung, and Blood Institute. National Cholesterol Education Program. Third Report of the Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Available at: www.nhlbi.nih.gov/guidelines/cholesterol/atp3_rpt.htm. Accessed on March 16, 2004.
5. Layey JM. Hypercoagulable states and central retinal vein occulsion. Curr Opin Pulm Med 2003;9:385-392.
6. Fegan CD. Central retinal vein occlusion and thrombophilia. Eye 2002;26:98-106.
Q: What causes of sudden unilateral vision loss would you consider? What would you do next?
Your examination yields the following:
Medical history
- Borderline hypertension
- Hyperlipidemia (was on a medication but discontinued it on his own)
- Smoking 25 pack-years; quit 2 years ago
- Occasional alcohol intake
- No medications
- Electrical contractor by trade
- Parents living and well; siblings have hypertension but no other illnesses.
Review of systems
Negative except for occasional nasal congestion and low back pain.
Physical examination
- Alert male in no distress. Blood pressure, 146/86 mm Hg; weight, 85 kg; heart rate, 80; respiratory rate, 20; temperature normal; skin warm and dry.
- Head, eyes, ears, nose, throat: pupils are equal, round, and reactive to light and accommodation; extraocular movement intact; retinal exam is depicted in the Figure. Tympanic membranes, throat, and neck normal; carotids normal.
- Heart and lung exam unremarkable. Spleen questionably palpable. Extremities normal. Neurologic exam normal, except for eye findings.
FIGURE
Retinal exam
Referring to Harrison’s Textbook of Medicine, you find the following entry:
“Venous occlusion of the retina is often idiopathic, but hypertension, diabetes, and glaucoma are prominent risk factors. The benefit of treatment with anticoagulants is unproven and carries the risk of hemorrhage into the vitreous. Polycythemia, thrombocythemia, or other factors leading to an underlying hypercoagulable state should be corrected.”1
You also reviewed information from UpToDate, which revealed a British article linking retinal venous occlusion with an increased risk of cardiovascular disease. It recommends that clinicians use an algorithm to determine the appropriate treatment.2 Additional research noted various interventions for the venous occlusion itself, but none had sufficient numbers to be considered reliable in recommending treatment.
You have identified 3 problems, 2 of which you deal with regularly and a third that requires consultation:
- Hypertension
- Hyperlipidemia
- Central retinal venous occlusion (CRVO) (rule out underlying hypercoagulable state).
Ophthalmologist’s report
An ophthalmologist confirms a diagnosis of left retinal vein occlusion, and recommends a period of observation, to see if vision returns. The opthalmologist also asks the patient to return to you for an investigation of possible underlying medical conditions.
Further primary care evaluation
The patient’s history suggests nothing that would inhibit a return of vision. Findings on the physical examination are unchanged except for the left fundus. The patient is quite concerned about another “stroke,” particularly in the other eye. He wants a guarantee he will be okay.
Laboratory evaluation:
- Complete blood count, normal
- Urea nitrogen (BUN), 20 mg/dL
- Creatinine kinase, 1.2 mckat/L
- Liver functions within normal limits
- Glucose, 86 mg/dL
- Cholesterol, 230 mg/dL
- Triglycerides, 186 mg/dL
- HDL, 41 mg/dL; LDL, 136 mg/dL
- Total serum protein levels, normal.
Additional time was required by the family physician to coordinate care of this patient. A team management code (99361 for 30 minutes and 99362 for 60 minutes) may not be billed on the same day as an e/m code, as carriers bundle this into the e/m. In addition, most carriers do not pay for the 99361 or 99362 codes. Therefore, the conference should ideally occur the day of an e/m code and be documented with that service. In this instance, the care occurred over several days, so no additional billing was allowed for team management.
Details of central retinal venous occlusion
You assure the patient you will coordinate care with the ophthalmologist, who subsequently offers the following summary about CRVO:
- For most patients with CRVO, vision decreases to 20/100, 20/200, or worse, usually permanently if the occlusion is indeed venous and not arterial as well. If the condition is secondary to ischemia, vision is usually limited to 20/300 or worse, permanently.
- Most patients want their vision “fixed” right away, but that is usually not possible. Hypertension control is most important. Uncommon causes include polycythemia vera, emphysema, sickle cell disease, multiple myeloma, macroglobulinemia, hyperproteinemia, cystic fibrosis of the pancreas, and peritoneal dialysis. Occasionally, it can occur secondary to hypotension, as from a ruptured aortic aneurysm, delivery-associated blood loss, or surgical trauma.
- Hypertension and other atherosclerotic risk factors must be controlled. Treatment with platelet inhibitors is often recommended and glaucoma control is very important, especially for African American patients. Chronic open-angle glaucoma can present as CRVO, and results can be devastating. African Americans are about 100 times more likely than Caucasians to have glaucoma (1/7 vs 3/2000).
Management dos and don’ts
CRVO is entirely different than retinal hemorrhage or vitreous hemorrhage. The correct diagnosis must be confirmed by an ophthalmologist, to ensure proper evaluation and management.
Reduce blood pressure
You return to your patient and share your conversation with the consultant. According to the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7) guidelines, the patient has Stage I hypertension. The goal for treatment is medical management to reduce pressure to below 120/80 mm Hg.3
The patient elects treatment with a beta-blocker rather than a thiazide diuretic; he wishes to avoid monitoring of electrolytes that would be necessary because he often becomes dehydrated on the job. He will have the nurse at his company monitor his blood pressure.
Reduce lipids
Also, according to the National Cholesterol Education Program, this patient meets criteria for treatment of hyperlipidemia.4 He is given dietary instruction, information about lipids, a prescription for a statin as he believes he has already been following a quite restrictive diet for over 4 months.
Use anticoagulant?
Finally, you consult a hematologist about the appropriate evaluation for a hypercoagulable state. Following is her report:
- The retinal vein is anatomically different from other veins, being tightly encased in a sheath with the retinal artery and optic nerve. Disorders of these structures can compress or inflame the vein, leading to thrombosis. Consequently, local factors may play a role in development of retinal vein thrombosis—a systemic disorder is not required for this process to occur. CVRO is seldom associated with an underlying hypercoagulable state.5,6
- The effectiveness of medical intervention is unproven. Acute anticoagulation is associated with retinal hemorrhage and is not recommended. Recurrent retinal venous occlusion in the contralateral eye occurs in approximately 12% of patients within 4 years. Because of the risks of anticoagulation and unproven benefits in CRVO, you both elect to avoid this treatment.
If the patient were to request anticoagulation, therapy should be withheld for 2 to 3 months, the time required for retinal perfusion to stabilize. Antiplatelet agents such as aspirin have no role in preventing recurrent venous thrombosis.
Confirmation of this controversy in treatment was obtained using a literature search. A review article in Eye discussed that while the role of thrombophilia is unclear, the need for a randomized study of anticoagulation in the patient with CRVO is needed.6
Final decisions
After considering your consultant’s suggestions, you realize that finding a prothrombotic state is unlikely and will be not change management. Moreover, medical intervention is unlikely to change the natural history of this condition, and it might lead inadvertently to insurance or employment discrimination. You review the previous complete blood count to make sure you have not missed erythrocytosis or thrombocytosis—both of which have well-defined treatments.
Follow-up monitoring was scheduled by the ophthalmologist and you continue to manage the patient’s hypertension and hyperlipidemia.
This patient had a relatively uncommon condition that necessitated consultation with 2 specialists. After weighing the evidence and likelihood of benefit of unproven therapies for CVRO, the patient elected to manage other clear risk factors for atherosclerotic vascular disease. Management of this patient melds issues of ethics and evidence, with core skills to foster a good doctor-patient relationship.
At the risk of sounding like a bad joke, I’d like to open my commentary with the question:
“Why did this patient go to the family physician?” This patient was seen in an urban setting with ample access to any medical specialist, and he had an insurance plan that allowed open access contact with most, if not all, of the physicians in the community. This patient also knew enough about his illness to know that the final answer or treatment for his presenting problem would likely not be found in the family physician’s office.
The value that the family physician brought to this patient can be described as follows:
Navigator/Coordinator: The family physician was able to help this patient through the maze of medical specialists to find the right physicians to evaluate and treat the presenting problem, and to arrange for ongoing evaluation and management after specialist consultations.
Interpreter/Translator: The family physician was able to take the information provided by the specialist physicians and translate that information into language the patient could understand. This process must occur if the patient is expected to comply with treatment, evaluation and lifestyle change recommendations.
Comprehensive caregiver: While supporting the patient in coping with his vision loss, the family physician used this unfortunate occurrence as motivation to address modifiable risk factors—hypertension, obesity, elevated blood glucose, and elevated lipids. Managing these conditions may not be glamorous, but addressing all facets of a patient’s well being is what we family physicians do best. Caring for patients, not just treating illnesses, is a core value of family medicine.
Imagine this patient’s thought process from his arrival with a loss of vision to his departure with a plan to deal with hypertension, obesity, elevated blood glucose, and elevated lipids, all in the context of his job and family and community life. The holistic management of this patient in the context of his life is the main value added by the family physician for this patient. This management also completely supports the patient’s wish to avoid “another stroke.”
One of my colleagues once asked me: “Wouldn’t you like to be the kind of physician whose patient comes in with a cold and leaves with an order for a mammogram?” Family physicians have the knowledge, skills, and perspective necessary to treat the patient, not just the illness. Let’s keep doing what we do best for our patients.
Paul Paulman, MD
Q: What causes of sudden unilateral vision loss would you consider? What would you do next?
Your examination yields the following:
Medical history
- Borderline hypertension
- Hyperlipidemia (was on a medication but discontinued it on his own)
- Smoking 25 pack-years; quit 2 years ago
- Occasional alcohol intake
- No medications
- Electrical contractor by trade
- Parents living and well; siblings have hypertension but no other illnesses.
Review of systems
Negative except for occasional nasal congestion and low back pain.
Physical examination
- Alert male in no distress. Blood pressure, 146/86 mm Hg; weight, 85 kg; heart rate, 80; respiratory rate, 20; temperature normal; skin warm and dry.
- Head, eyes, ears, nose, throat: pupils are equal, round, and reactive to light and accommodation; extraocular movement intact; retinal exam is depicted in the Figure. Tympanic membranes, throat, and neck normal; carotids normal.
- Heart and lung exam unremarkable. Spleen questionably palpable. Extremities normal. Neurologic exam normal, except for eye findings.
FIGURE
Retinal exam
Referring to Harrison’s Textbook of Medicine, you find the following entry:
“Venous occlusion of the retina is often idiopathic, but hypertension, diabetes, and glaucoma are prominent risk factors. The benefit of treatment with anticoagulants is unproven and carries the risk of hemorrhage into the vitreous. Polycythemia, thrombocythemia, or other factors leading to an underlying hypercoagulable state should be corrected.”1
You also reviewed information from UpToDate, which revealed a British article linking retinal venous occlusion with an increased risk of cardiovascular disease. It recommends that clinicians use an algorithm to determine the appropriate treatment.2 Additional research noted various interventions for the venous occlusion itself, but none had sufficient numbers to be considered reliable in recommending treatment.
You have identified 3 problems, 2 of which you deal with regularly and a third that requires consultation:
- Hypertension
- Hyperlipidemia
- Central retinal venous occlusion (CRVO) (rule out underlying hypercoagulable state).
Ophthalmologist’s report
An ophthalmologist confirms a diagnosis of left retinal vein occlusion, and recommends a period of observation, to see if vision returns. The opthalmologist also asks the patient to return to you for an investigation of possible underlying medical conditions.
Further primary care evaluation
The patient’s history suggests nothing that would inhibit a return of vision. Findings on the physical examination are unchanged except for the left fundus. The patient is quite concerned about another “stroke,” particularly in the other eye. He wants a guarantee he will be okay.
Laboratory evaluation:
- Complete blood count, normal
- Urea nitrogen (BUN), 20 mg/dL
- Creatinine kinase, 1.2 mckat/L
- Liver functions within normal limits
- Glucose, 86 mg/dL
- Cholesterol, 230 mg/dL
- Triglycerides, 186 mg/dL
- HDL, 41 mg/dL; LDL, 136 mg/dL
- Total serum protein levels, normal.
Additional time was required by the family physician to coordinate care of this patient. A team management code (99361 for 30 minutes and 99362 for 60 minutes) may not be billed on the same day as an e/m code, as carriers bundle this into the e/m. In addition, most carriers do not pay for the 99361 or 99362 codes. Therefore, the conference should ideally occur the day of an e/m code and be documented with that service. In this instance, the care occurred over several days, so no additional billing was allowed for team management.
Details of central retinal venous occlusion
You assure the patient you will coordinate care with the ophthalmologist, who subsequently offers the following summary about CRVO:
- For most patients with CRVO, vision decreases to 20/100, 20/200, or worse, usually permanently if the occlusion is indeed venous and not arterial as well. If the condition is secondary to ischemia, vision is usually limited to 20/300 or worse, permanently.
- Most patients want their vision “fixed” right away, but that is usually not possible. Hypertension control is most important. Uncommon causes include polycythemia vera, emphysema, sickle cell disease, multiple myeloma, macroglobulinemia, hyperproteinemia, cystic fibrosis of the pancreas, and peritoneal dialysis. Occasionally, it can occur secondary to hypotension, as from a ruptured aortic aneurysm, delivery-associated blood loss, or surgical trauma.
- Hypertension and other atherosclerotic risk factors must be controlled. Treatment with platelet inhibitors is often recommended and glaucoma control is very important, especially for African American patients. Chronic open-angle glaucoma can present as CRVO, and results can be devastating. African Americans are about 100 times more likely than Caucasians to have glaucoma (1/7 vs 3/2000).
Management dos and don’ts
CRVO is entirely different than retinal hemorrhage or vitreous hemorrhage. The correct diagnosis must be confirmed by an ophthalmologist, to ensure proper evaluation and management.
Reduce blood pressure
You return to your patient and share your conversation with the consultant. According to the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7) guidelines, the patient has Stage I hypertension. The goal for treatment is medical management to reduce pressure to below 120/80 mm Hg.3
The patient elects treatment with a beta-blocker rather than a thiazide diuretic; he wishes to avoid monitoring of electrolytes that would be necessary because he often becomes dehydrated on the job. He will have the nurse at his company monitor his blood pressure.
Reduce lipids
Also, according to the National Cholesterol Education Program, this patient meets criteria for treatment of hyperlipidemia.4 He is given dietary instruction, information about lipids, a prescription for a statin as he believes he has already been following a quite restrictive diet for over 4 months.
Use anticoagulant?
Finally, you consult a hematologist about the appropriate evaluation for a hypercoagulable state. Following is her report:
- The retinal vein is anatomically different from other veins, being tightly encased in a sheath with the retinal artery and optic nerve. Disorders of these structures can compress or inflame the vein, leading to thrombosis. Consequently, local factors may play a role in development of retinal vein thrombosis—a systemic disorder is not required for this process to occur. CVRO is seldom associated with an underlying hypercoagulable state.5,6
- The effectiveness of medical intervention is unproven. Acute anticoagulation is associated with retinal hemorrhage and is not recommended. Recurrent retinal venous occlusion in the contralateral eye occurs in approximately 12% of patients within 4 years. Because of the risks of anticoagulation and unproven benefits in CRVO, you both elect to avoid this treatment.
If the patient were to request anticoagulation, therapy should be withheld for 2 to 3 months, the time required for retinal perfusion to stabilize. Antiplatelet agents such as aspirin have no role in preventing recurrent venous thrombosis.
Confirmation of this controversy in treatment was obtained using a literature search. A review article in Eye discussed that while the role of thrombophilia is unclear, the need for a randomized study of anticoagulation in the patient with CRVO is needed.6
Final decisions
After considering your consultant’s suggestions, you realize that finding a prothrombotic state is unlikely and will be not change management. Moreover, medical intervention is unlikely to change the natural history of this condition, and it might lead inadvertently to insurance or employment discrimination. You review the previous complete blood count to make sure you have not missed erythrocytosis or thrombocytosis—both of which have well-defined treatments.
Follow-up monitoring was scheduled by the ophthalmologist and you continue to manage the patient’s hypertension and hyperlipidemia.
This patient had a relatively uncommon condition that necessitated consultation with 2 specialists. After weighing the evidence and likelihood of benefit of unproven therapies for CVRO, the patient elected to manage other clear risk factors for atherosclerotic vascular disease. Management of this patient melds issues of ethics and evidence, with core skills to foster a good doctor-patient relationship.
At the risk of sounding like a bad joke, I’d like to open my commentary with the question:
“Why did this patient go to the family physician?” This patient was seen in an urban setting with ample access to any medical specialist, and he had an insurance plan that allowed open access contact with most, if not all, of the physicians in the community. This patient also knew enough about his illness to know that the final answer or treatment for his presenting problem would likely not be found in the family physician’s office.
The value that the family physician brought to this patient can be described as follows:
Navigator/Coordinator: The family physician was able to help this patient through the maze of medical specialists to find the right physicians to evaluate and treat the presenting problem, and to arrange for ongoing evaluation and management after specialist consultations.
Interpreter/Translator: The family physician was able to take the information provided by the specialist physicians and translate that information into language the patient could understand. This process must occur if the patient is expected to comply with treatment, evaluation and lifestyle change recommendations.
Comprehensive caregiver: While supporting the patient in coping with his vision loss, the family physician used this unfortunate occurrence as motivation to address modifiable risk factors—hypertension, obesity, elevated blood glucose, and elevated lipids. Managing these conditions may not be glamorous, but addressing all facets of a patient’s well being is what we family physicians do best. Caring for patients, not just treating illnesses, is a core value of family medicine.
Imagine this patient’s thought process from his arrival with a loss of vision to his departure with a plan to deal with hypertension, obesity, elevated blood glucose, and elevated lipids, all in the context of his job and family and community life. The holistic management of this patient in the context of his life is the main value added by the family physician for this patient. This management also completely supports the patient’s wish to avoid “another stroke.”
One of my colleagues once asked me: “Wouldn’t you like to be the kind of physician whose patient comes in with a cold and leaves with an order for a mammogram?” Family physicians have the knowledge, skills, and perspective necessary to treat the patient, not just the illness. Let’s keep doing what we do best for our patients.
Paul Paulman, MD
1. Harrison’s Principles of Internal Medicine. 15th ed. Eds. Braunwald E, Fauci AS, Kasper DL, Hauser SL, Longo DL, Jameson JL. New York, NY: McGraw-Hill; 2001.
2. Martin SC, Butcher A, Martin N, et al. Cardiovascular risk assessment in patients with retinal vein occlusion. Br J Ophthalmol 2002;86:774-776.
3. National Heart, Lung, and Blood Institute. National High Blood Pressure Education Program. Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7). 2003. Available at: www.nhlbi.nih.gov/guidelines/hypertension/jncintro.htm. Accessed on March 16, 2004.
4. National Heart, Lung, and Blood Institute. National Cholesterol Education Program. Third Report of the Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Available at: www.nhlbi.nih.gov/guidelines/cholesterol/atp3_rpt.htm. Accessed on March 16, 2004.
5. Layey JM. Hypercoagulable states and central retinal vein occulsion. Curr Opin Pulm Med 2003;9:385-392.
6. Fegan CD. Central retinal vein occlusion and thrombophilia. Eye 2002;26:98-106.
1. Harrison’s Principles of Internal Medicine. 15th ed. Eds. Braunwald E, Fauci AS, Kasper DL, Hauser SL, Longo DL, Jameson JL. New York, NY: McGraw-Hill; 2001.
2. Martin SC, Butcher A, Martin N, et al. Cardiovascular risk assessment in patients with retinal vein occlusion. Br J Ophthalmol 2002;86:774-776.
3. National Heart, Lung, and Blood Institute. National High Blood Pressure Education Program. Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7). 2003. Available at: www.nhlbi.nih.gov/guidelines/hypertension/jncintro.htm. Accessed on March 16, 2004.
4. National Heart, Lung, and Blood Institute. National Cholesterol Education Program. Third Report of the Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Available at: www.nhlbi.nih.gov/guidelines/cholesterol/atp3_rpt.htm. Accessed on March 16, 2004.
5. Layey JM. Hypercoagulable states and central retinal vein occulsion. Curr Opin Pulm Med 2003;9:385-392.
6. Fegan CD. Central retinal vein occlusion and thrombophilia. Eye 2002;26:98-106.