User login
Impact of Integrated Oncology- Palliative Care Outpatient Model on Trends of Palliative Care and Hospice Care Referrals From Oncology
Background: A commonly voiced concern of oncologists, regarding the introduction of palliative care, is that patients might be immediately steered to hospice care and away from oncology care.
Objective: To assess the impact of oncology-palliative care collaboration on trends of referrals to palliative and hospice care.
Methods: In January 2015, we implemented an integrated oncology-palliative care clinic model with the following elements:
- Pre-clinic “huddle” among palliative care and oncology staff to identify palliative care needs for patients;
- Shared palliative care and oncology clinic appointments;
- Introduction of palliative care for every new oncology clinic patient, for advance care planning;
- Concurrent oncology and palliative care follow-up for all high-risk patients (aggressive histology, progressing disease, etc.) for goals of care discussions and symptom management; and
- Palliative care and oncology staff co-managing oncology patients enrolled in hospice care.
Measurements: We examined the following metrics for FY15, FY16, FY17, and FY18.
- Total number of palliative care consults;
- Number of palliative care consults from oncology;
- Percentage palliative care consults from oncology [(item 2 × 100) / item 1];
- Total number of referrals to hospice care;
- Number of referrals to hospice care from oncology; and
- Percentage hospice care referrals from oncology [(item 5 × 100) / item 4].
Results: During the period of FY15 to FY18, there was a consistent increase in total palliative care consults (355, 394, 549, and 570 respectively). There also was a consistent increase in percentage palliative care consults from oncology (24%, 34%, 38%, and 40% respectively) without an increase in percentage hospice care referrals from oncology.
Conclusion: A common concern is that palliative care in oncology care will result in patients being immediately steered to hospice care and away from continued oncology care. Although it was limited to a single clinical setting, our intervention resulted in increased palliative care consults from oncology without a proportionate increase in hospice care referrals from oncology during the same time-period, suggesting that earlier access to palliative care did not result in immediate transition to hospice care. Palliative care offers opportunities for goals of care conversations and symptom management in oncology care, prior to transition to hospice care. Future implications include robust studies to further test these findings, review of structure and training of oncology-palliative care teams, and systems redesign to develop dyad or shared clinic models.
Background: A commonly voiced concern of oncologists, regarding the introduction of palliative care, is that patients might be immediately steered to hospice care and away from oncology care.
Objective: To assess the impact of oncology-palliative care collaboration on trends of referrals to palliative and hospice care.
Methods: In January 2015, we implemented an integrated oncology-palliative care clinic model with the following elements:
- Pre-clinic “huddle” among palliative care and oncology staff to identify palliative care needs for patients;
- Shared palliative care and oncology clinic appointments;
- Introduction of palliative care for every new oncology clinic patient, for advance care planning;
- Concurrent oncology and palliative care follow-up for all high-risk patients (aggressive histology, progressing disease, etc.) for goals of care discussions and symptom management; and
- Palliative care and oncology staff co-managing oncology patients enrolled in hospice care.
Measurements: We examined the following metrics for FY15, FY16, FY17, and FY18.
- Total number of palliative care consults;
- Number of palliative care consults from oncology;
- Percentage palliative care consults from oncology [(item 2 × 100) / item 1];
- Total number of referrals to hospice care;
- Number of referrals to hospice care from oncology; and
- Percentage hospice care referrals from oncology [(item 5 × 100) / item 4].
Results: During the period of FY15 to FY18, there was a consistent increase in total palliative care consults (355, 394, 549, and 570 respectively). There also was a consistent increase in percentage palliative care consults from oncology (24%, 34%, 38%, and 40% respectively) without an increase in percentage hospice care referrals from oncology.
Conclusion: A common concern is that palliative care in oncology care will result in patients being immediately steered to hospice care and away from continued oncology care. Although it was limited to a single clinical setting, our intervention resulted in increased palliative care consults from oncology without a proportionate increase in hospice care referrals from oncology during the same time-period, suggesting that earlier access to palliative care did not result in immediate transition to hospice care. Palliative care offers opportunities for goals of care conversations and symptom management in oncology care, prior to transition to hospice care. Future implications include robust studies to further test these findings, review of structure and training of oncology-palliative care teams, and systems redesign to develop dyad or shared clinic models.
Background: A commonly voiced concern of oncologists, regarding the introduction of palliative care, is that patients might be immediately steered to hospice care and away from oncology care.
Objective: To assess the impact of oncology-palliative care collaboration on trends of referrals to palliative and hospice care.
Methods: In January 2015, we implemented an integrated oncology-palliative care clinic model with the following elements:
- Pre-clinic “huddle” among palliative care and oncology staff to identify palliative care needs for patients;
- Shared palliative care and oncology clinic appointments;
- Introduction of palliative care for every new oncology clinic patient, for advance care planning;
- Concurrent oncology and palliative care follow-up for all high-risk patients (aggressive histology, progressing disease, etc.) for goals of care discussions and symptom management; and
- Palliative care and oncology staff co-managing oncology patients enrolled in hospice care.
Measurements: We examined the following metrics for FY15, FY16, FY17, and FY18.
- Total number of palliative care consults;
- Number of palliative care consults from oncology;
- Percentage palliative care consults from oncology [(item 2 × 100) / item 1];
- Total number of referrals to hospice care;
- Number of referrals to hospice care from oncology; and
- Percentage hospice care referrals from oncology [(item 5 × 100) / item 4].
Results: During the period of FY15 to FY18, there was a consistent increase in total palliative care consults (355, 394, 549, and 570 respectively). There also was a consistent increase in percentage palliative care consults from oncology (24%, 34%, 38%, and 40% respectively) without an increase in percentage hospice care referrals from oncology.
Conclusion: A common concern is that palliative care in oncology care will result in patients being immediately steered to hospice care and away from continued oncology care. Although it was limited to a single clinical setting, our intervention resulted in increased palliative care consults from oncology without a proportionate increase in hospice care referrals from oncology during the same time-period, suggesting that earlier access to palliative care did not result in immediate transition to hospice care. Palliative care offers opportunities for goals of care conversations and symptom management in oncology care, prior to transition to hospice care. Future implications include robust studies to further test these findings, review of structure and training of oncology-palliative care teams, and systems redesign to develop dyad or shared clinic models.
Model of Integrated Oncology- Palliative Care in an Outpatient Setting
Background: Early introduction of palliative care for oncology patients has demonstrated enhanced quality of life and satisfaction. We developed a model for integrating palliative care into outpatient oncology care.
Hypothesis: Optimal integration of oncology and palliative care requires palliative care clinician’s presence at initial, and many subsequent, patient encounters.
Objective: To implement and evaluate outpatient integrated oncology and palliative care.
Method: In January 2015, we implemented an integrated outpatient practice of oncology and palliative care with: Pre-clinic “huddle” among palliative care and oncology staff to identify patients in need of palliative care; shared palliative care-oncology appointments. Initial visit: New oncology patients are seen by an oncologist and palliative care physician together. Palliative care physician introduces palliative care and initiates advance care planning. Concurrent oncology-palliative care follow-up: High-risk patients (aggressive histology, progressing disease, etc) are followed by oncologist and palliative care physician. Palliative care physician facilitates goals of care discussions and addresses symptom management. End-of-life care: Hospice care remains a part of oncology care. Palliative care physician and oncology team co-manage all oncology patients enrolled in hospice care.
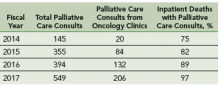
Results: Increase in palliative care consults from oncology clinics: After this intervention, there is a 10-fold increase in number of palliative care consultation requests from oncology clinics from fiscal year 2014 to 2017. Increase in percentage of inpatients deaths with prior palliative care consultation: Since the implementation of this model, there is an increase in the percentage of inpatient deaths with prior palliative care consultations; from 75% in fiscal year 2014 to 97% in fiscal year 2017.
Challenges/Limitations: Single clinic setting, with one oncologist and palliative care physician, palliative care staffing, clinic space, administrative support.
Conclusions: Studies are needed to show impact of palliative care integration on acute care utilization, hospice care accession and satisfaction with care. There is a need to explore improved training and structures for both oncology and palliative care teams.
Background: Early introduction of palliative care for oncology patients has demonstrated enhanced quality of life and satisfaction. We developed a model for integrating palliative care into outpatient oncology care.
Hypothesis: Optimal integration of oncology and palliative care requires palliative care clinician’s presence at initial, and many subsequent, patient encounters.
Objective: To implement and evaluate outpatient integrated oncology and palliative care.
Method: In January 2015, we implemented an integrated outpatient practice of oncology and palliative care with: Pre-clinic “huddle” among palliative care and oncology staff to identify patients in need of palliative care; shared palliative care-oncology appointments. Initial visit: New oncology patients are seen by an oncologist and palliative care physician together. Palliative care physician introduces palliative care and initiates advance care planning. Concurrent oncology-palliative care follow-up: High-risk patients (aggressive histology, progressing disease, etc) are followed by oncologist and palliative care physician. Palliative care physician facilitates goals of care discussions and addresses symptom management. End-of-life care: Hospice care remains a part of oncology care. Palliative care physician and oncology team co-manage all oncology patients enrolled in hospice care.
Results: Increase in palliative care consults from oncology clinics: After this intervention, there is a 10-fold increase in number of palliative care consultation requests from oncology clinics from fiscal year 2014 to 2017. Increase in percentage of inpatients deaths with prior palliative care consultation: Since the implementation of this model, there is an increase in the percentage of inpatient deaths with prior palliative care consultations; from 75% in fiscal year 2014 to 97% in fiscal year 2017.
Challenges/Limitations: Single clinic setting, with one oncologist and palliative care physician, palliative care staffing, clinic space, administrative support.
Conclusions: Studies are needed to show impact of palliative care integration on acute care utilization, hospice care accession and satisfaction with care. There is a need to explore improved training and structures for both oncology and palliative care teams.
Background: Early introduction of palliative care for oncology patients has demonstrated enhanced quality of life and satisfaction. We developed a model for integrating palliative care into outpatient oncology care.
Hypothesis: Optimal integration of oncology and palliative care requires palliative care clinician’s presence at initial, and many subsequent, patient encounters.
Objective: To implement and evaluate outpatient integrated oncology and palliative care.
Method: In January 2015, we implemented an integrated outpatient practice of oncology and palliative care with: Pre-clinic “huddle” among palliative care and oncology staff to identify patients in need of palliative care; shared palliative care-oncology appointments. Initial visit: New oncology patients are seen by an oncologist and palliative care physician together. Palliative care physician introduces palliative care and initiates advance care planning. Concurrent oncology-palliative care follow-up: High-risk patients (aggressive histology, progressing disease, etc) are followed by oncologist and palliative care physician. Palliative care physician facilitates goals of care discussions and addresses symptom management. End-of-life care: Hospice care remains a part of oncology care. Palliative care physician and oncology team co-manage all oncology patients enrolled in hospice care.
Results: Increase in palliative care consults from oncology clinics: After this intervention, there is a 10-fold increase in number of palliative care consultation requests from oncology clinics from fiscal year 2014 to 2017. Increase in percentage of inpatients deaths with prior palliative care consultation: Since the implementation of this model, there is an increase in the percentage of inpatient deaths with prior palliative care consultations; from 75% in fiscal year 2014 to 97% in fiscal year 2017.
Challenges/Limitations: Single clinic setting, with one oncologist and palliative care physician, palliative care staffing, clinic space, administrative support.
Conclusions: Studies are needed to show impact of palliative care integration on acute care utilization, hospice care accession and satisfaction with care. There is a need to explore improved training and structures for both oncology and palliative care teams.