User login
Generalized maculopapular rash and fever
A 29-YEAR-OLD MAN was referred to the emergency department for fever and rash. Two months prior, he had noticed painful spots on his toes (FIGURE 1). Soon after, a rash of different morphology appeared on his chest and upper extremities. Associated symptoms included hair loss, generalized arthralgias, chills, trouble with balance, and photophobia. The patient denied genital lesions but reported 3 recent cold sores.

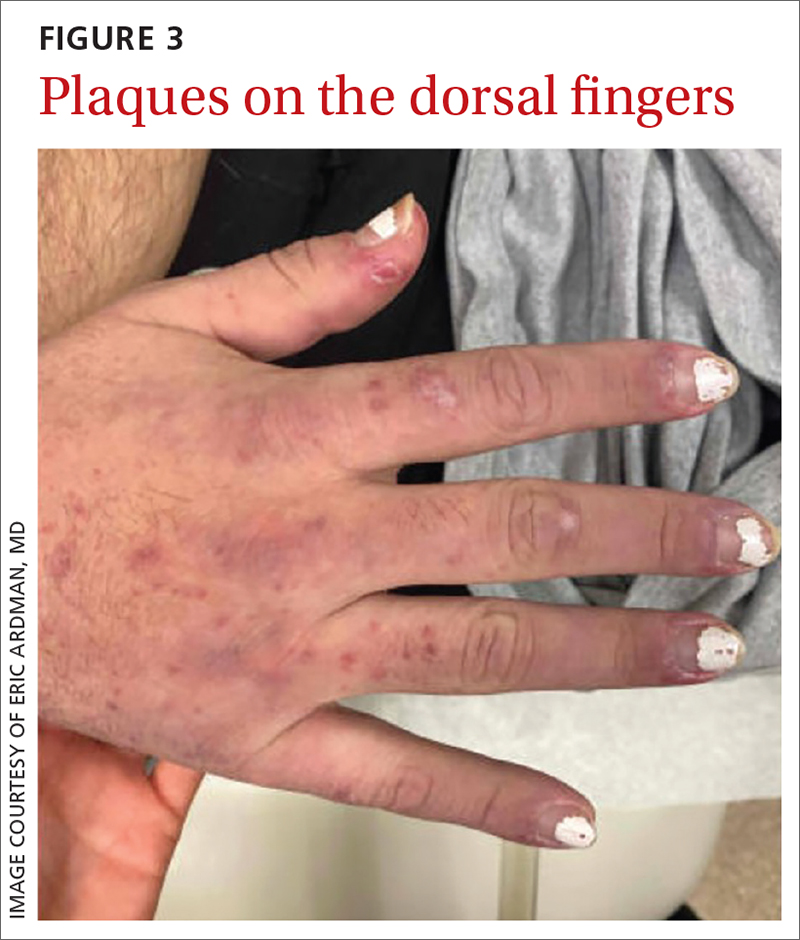
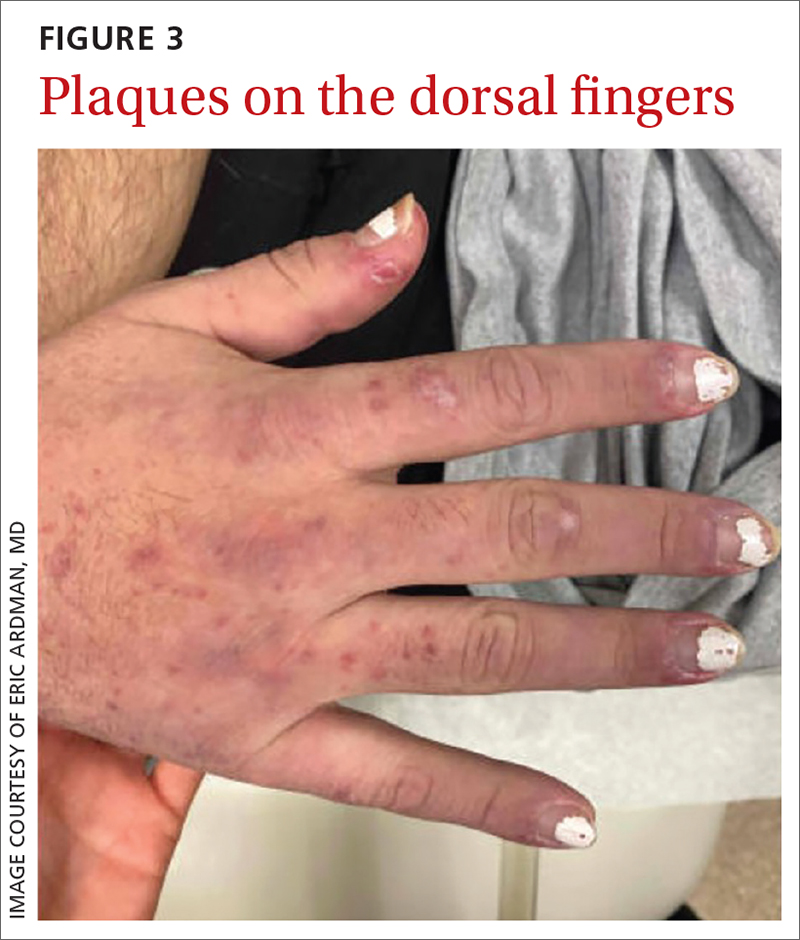
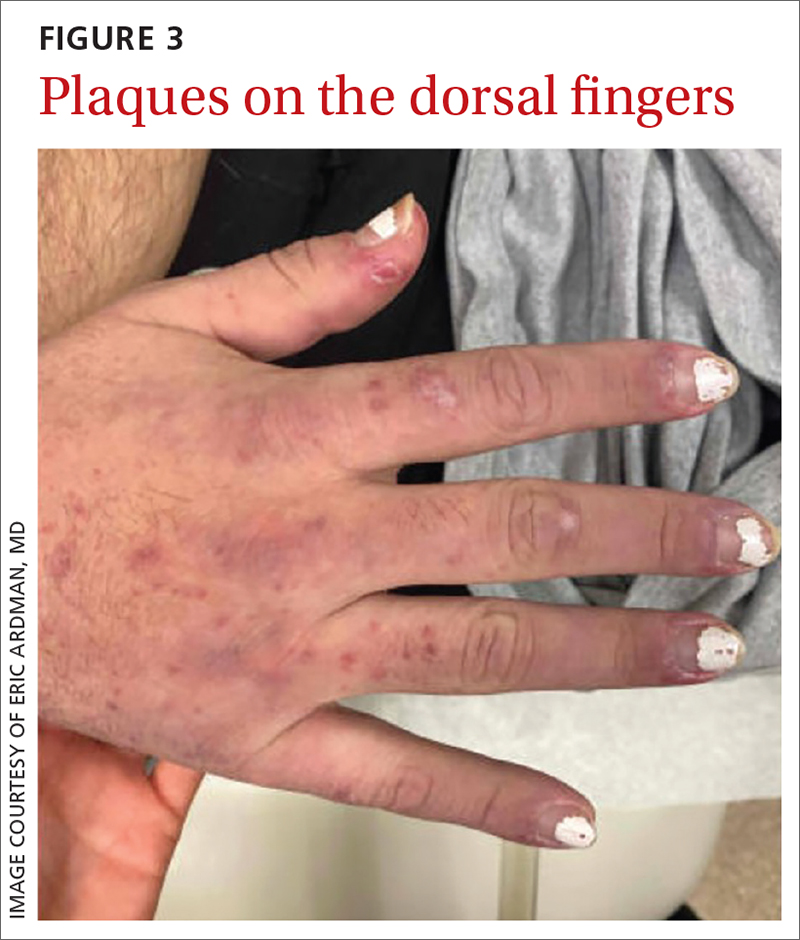
On exam, the patient was febrile (102 °F). Skin exam revealed a generalized maculopapular rash on the trunk, arms, and legs with scattered lesions on the palms (FIGURE 2). There were tender purpuric macules on the tips of his toes with areas of blanching. His hands had pink plaques on the dorsal fingers (FIGURE 3). Additionally, there was an erythematous papular rash with scale on his cheeks and nasal bridge, patchy areas of hair loss, and a single oral ulcer.

A neurologic exam was notable for mildly unstable gait, an abnormal Babinski reflex on the left side, and a positive Romberg sign. Musculoskeletal exam revealed joint tenderness in his shoulders, elbows, and wrists. Lymphadenopathy was present bilaterally in the axilla.
Lab work was ordered, including a VDRL test and a treponemal antibodies test. Skin biopsies also were taken from lesions on his arm and chest.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Systemic lupus erythematosus
Our patient’s fever and rash were highly suggestive of either systemic lupus erythematosus (SLE) or secondary syphilis (the “great masquerader”).
In addition to the joint tenderness revealed during the musculoskeletal exam, our patient had several nonspecific lupus findings on skin exam: malar rash, discoid rash on hands, subacute vasculitis (generalized rash), alopecia, and an oral ulcer; he also had the specific finding of chilblains vasculitis of the toes. Lab work and pathology results made the diagnosis clear. Lab work revealed leukopenia, an antinuclear antibody (ANA) result of 1:2560 with speckled appearance, and positive anti-SM antibodies. A dipstick was negative for protein; VDRL and treponemal antibodies tests were also negative. Histopathology showed perivascular lymph histiocytic vacuolar dermatitis with a differential of connective tissue disease, including lupus.
Our patient met the criteria
SLE is a systemic autoimmune disease resulting in chronic inflammation in multiple organ systems; it commonly manifests with vague symptoms of fatigue, fever, and weight loss. The prevalence of SLE in the United States has been reported as high as 241 per 100,000 people. 1 Women are more likely to be affected, and the incidence is highest among Black people and lowest among Caucasians.1,2 Risk factors include cigarette smoking and exposure to silica particulate air pollution.
The 2019 European League Against Rheumatism/American College of Rheumatology criteria for a diagnosis of SLE require that a patient have a positive ANA and some, but not all, additive lab, clinical, and organ-specific findings.3 Findings that clinicians should look for include3,4
- elevated ANA (≥ 1:80)
- constitutional symptoms (fever)
- hematologic findings (leukopenia, thrombocytopenia, autoimmune hemolysis)
- neuropsychiatric findings (delirium, psychosis, seizure)
- mucocutaneous findings (alopecia, oral ulcers, others)
- serosal findings (effusion, acute pericarditis)
- musculoskeletal findings (joint involvement)
- renal findings (proteinuria)
- antiphospholipid antibodies
- decreased complement proteins
- SLE-specific antibodies.
Dermatologic findings occur in more than 70% of patients with SLE.5 They can be nonspecific—eg, classic discoid rash, malar rash, alopecia, maculopapular rash (most commonly on sun-exposed areas, mimicking polymorphous light eruption)—or specific (eg, chilblains
Continue to: The differential for rash and fever is broad
The differential for rash and fever is broad
Syphilis also can manifest with rash and fever. The rash of syphilis is nonpainful and affects the torso and face, with concentration on the palms and soles.6,7
Dermatomyositis is a rare disorder of inflammation in both the skin and muscles. Symptoms include rash, muscle aches, and weakness. Lab abnormalities include elevated creatine kinase levels
Erythema multiforme is an immunologic-mediated rash consisting of firm targetoid erythematous papules distributed symmetrically on the extremities, including palms/soles. It typically appears after a viral infection, immunization, or new medications (eg, antibiotics, nonsteroidal anti-inflammatory drugs, or phenothiazines) initiated 1 to 3 weeks prior to the appearance of the rash. History and appearance inform the diagnosis.
Polymorphic light eruption is a rash of variable appearance on sun-exposed areas that results from a sensitivity to sunlight after lack of exposure for a period of time. Symptoms include burning and itching.
Treat patients with SLE with hydroxychloroquine (200-400 mg/d) to suppress inflammation and with low-dose oral steroids such as prednisone (7.5 mg/d) for intermittent exacerbations. Higher steroid doses are sometimes needed for signs of organ inflammation. Patients with increased disease activity will require immunosuppressive therapy with disease-modifying antirheumatic drugs,
Our patient was admitted for further evaluation. A lumbar puncture was performed because of his balance issues; it showed an elevated protein level, but further work-up did not find an infectious or malignant source. Balance improved with hydration. The patient remained hospitalized for 9 days, during which his fever subsided. His pain improved after initiation of hydroxychloroquine 400 mg/d. Follow-up with Rheumatology was arranged for further care.
1. Rees F, Doherty M, Grainge MJ, et al. The worldwide incidence and prevalence of systemic lupus erythematosus: a systematic review of epidemiological studies. Rheumatology (Oxford). 2017;56:1945-1961. doi: 10.1093/rheumatology/kex260
2. CDC. Systemic lupus erythematosus (SLE). Updated July 5, 2022. Accessed April 11, 2023. www.cdc.gov/lupus/facts/detailed.html
3. Aringer M, Costenbader K, Daikh D, et al. 2019 European League Against Rheumatism/American College of Rheumatology classification criteria for systemic lupus erythematosus. Arthritis Rheumatol. 2019;71:1400-1412. doi: 10.1002/art.40930
4. Lam NV, Brown JA, Sharma R. Systemic lupus erythematosus: diagnosis and treatment. Am Fam Physician. 2023;107:383-395.
5. Albrecht J, Berlin JA, Braverman IM, et al. Dermatology position paper on revision of the 1982 ACR criteria for systemic lupus erythematosus. Lupus. 2004;13:839-849. doi: 10.1191/0961203304lu2020oa
6. Dylewski J, Duong M. The rash of secondary syphilis. CMAJ. 2007;176:33-35. doi: 10.1503/cmaj.060665
7. Lautenschlager S. Cutaneous manifestations of syphilis: recognition and management. Am J Clin Dermatol. 2006;7:291-304. doi: 10.2165/00128071-200607050-00003:
8. Brown DL, Frank JE. Diagnosis and management of syphilis. Am Fam Physician. 2003;68:283-290.
9. Ricco J, Westby A. Syphilis: far from ancient history. Am Fam Physician. 2020;102:91-98.
A 29-YEAR-OLD MAN was referred to the emergency department for fever and rash. Two months prior, he had noticed painful spots on his toes (FIGURE 1). Soon after, a rash of different morphology appeared on his chest and upper extremities. Associated symptoms included hair loss, generalized arthralgias, chills, trouble with balance, and photophobia. The patient denied genital lesions but reported 3 recent cold sores.

On exam, the patient was febrile (102 °F). Skin exam revealed a generalized maculopapular rash on the trunk, arms, and legs with scattered lesions on the palms (FIGURE 2). There were tender purpuric macules on the tips of his toes with areas of blanching. His hands had pink plaques on the dorsal fingers (FIGURE 3). Additionally, there was an erythematous papular rash with scale on his cheeks and nasal bridge, patchy areas of hair loss, and a single oral ulcer.

A neurologic exam was notable for mildly unstable gait, an abnormal Babinski reflex on the left side, and a positive Romberg sign. Musculoskeletal exam revealed joint tenderness in his shoulders, elbows, and wrists. Lymphadenopathy was present bilaterally in the axilla.
Lab work was ordered, including a VDRL test and a treponemal antibodies test. Skin biopsies also were taken from lesions on his arm and chest.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Systemic lupus erythematosus
Our patient’s fever and rash were highly suggestive of either systemic lupus erythematosus (SLE) or secondary syphilis (the “great masquerader”).
In addition to the joint tenderness revealed during the musculoskeletal exam, our patient had several nonspecific lupus findings on skin exam: malar rash, discoid rash on hands, subacute vasculitis (generalized rash), alopecia, and an oral ulcer; he also had the specific finding of chilblains vasculitis of the toes. Lab work and pathology results made the diagnosis clear. Lab work revealed leukopenia, an antinuclear antibody (ANA) result of 1:2560 with speckled appearance, and positive anti-SM antibodies. A dipstick was negative for protein; VDRL and treponemal antibodies tests were also negative. Histopathology showed perivascular lymph histiocytic vacuolar dermatitis with a differential of connective tissue disease, including lupus.
Our patient met the criteria
SLE is a systemic autoimmune disease resulting in chronic inflammation in multiple organ systems; it commonly manifests with vague symptoms of fatigue, fever, and weight loss. The prevalence of SLE in the United States has been reported as high as 241 per 100,000 people. 1 Women are more likely to be affected, and the incidence is highest among Black people and lowest among Caucasians.1,2 Risk factors include cigarette smoking and exposure to silica particulate air pollution.
The 2019 European League Against Rheumatism/American College of Rheumatology criteria for a diagnosis of SLE require that a patient have a positive ANA and some, but not all, additive lab, clinical, and organ-specific findings.3 Findings that clinicians should look for include3,4
- elevated ANA (≥ 1:80)
- constitutional symptoms (fever)
- hematologic findings (leukopenia, thrombocytopenia, autoimmune hemolysis)
- neuropsychiatric findings (delirium, psychosis, seizure)
- mucocutaneous findings (alopecia, oral ulcers, others)
- serosal findings (effusion, acute pericarditis)
- musculoskeletal findings (joint involvement)
- renal findings (proteinuria)
- antiphospholipid antibodies
- decreased complement proteins
- SLE-specific antibodies.
Dermatologic findings occur in more than 70% of patients with SLE.5 They can be nonspecific—eg, classic discoid rash, malar rash, alopecia, maculopapular rash (most commonly on sun-exposed areas, mimicking polymorphous light eruption)—or specific (eg, chilblains
Continue to: The differential for rash and fever is broad
The differential for rash and fever is broad
Syphilis also can manifest with rash and fever. The rash of syphilis is nonpainful and affects the torso and face, with concentration on the palms and soles.6,7
Dermatomyositis is a rare disorder of inflammation in both the skin and muscles. Symptoms include rash, muscle aches, and weakness. Lab abnormalities include elevated creatine kinase levels
Erythema multiforme is an immunologic-mediated rash consisting of firm targetoid erythematous papules distributed symmetrically on the extremities, including palms/soles. It typically appears after a viral infection, immunization, or new medications (eg, antibiotics, nonsteroidal anti-inflammatory drugs, or phenothiazines) initiated 1 to 3 weeks prior to the appearance of the rash. History and appearance inform the diagnosis.
Polymorphic light eruption is a rash of variable appearance on sun-exposed areas that results from a sensitivity to sunlight after lack of exposure for a period of time. Symptoms include burning and itching.
Treat patients with SLE with hydroxychloroquine (200-400 mg/d) to suppress inflammation and with low-dose oral steroids such as prednisone (7.5 mg/d) for intermittent exacerbations. Higher steroid doses are sometimes needed for signs of organ inflammation. Patients with increased disease activity will require immunosuppressive therapy with disease-modifying antirheumatic drugs,
Our patient was admitted for further evaluation. A lumbar puncture was performed because of his balance issues; it showed an elevated protein level, but further work-up did not find an infectious or malignant source. Balance improved with hydration. The patient remained hospitalized for 9 days, during which his fever subsided. His pain improved after initiation of hydroxychloroquine 400 mg/d. Follow-up with Rheumatology was arranged for further care.
A 29-YEAR-OLD MAN was referred to the emergency department for fever and rash. Two months prior, he had noticed painful spots on his toes (FIGURE 1). Soon after, a rash of different morphology appeared on his chest and upper extremities. Associated symptoms included hair loss, generalized arthralgias, chills, trouble with balance, and photophobia. The patient denied genital lesions but reported 3 recent cold sores.

On exam, the patient was febrile (102 °F). Skin exam revealed a generalized maculopapular rash on the trunk, arms, and legs with scattered lesions on the palms (FIGURE 2). There were tender purpuric macules on the tips of his toes with areas of blanching. His hands had pink plaques on the dorsal fingers (FIGURE 3). Additionally, there was an erythematous papular rash with scale on his cheeks and nasal bridge, patchy areas of hair loss, and a single oral ulcer.

A neurologic exam was notable for mildly unstable gait, an abnormal Babinski reflex on the left side, and a positive Romberg sign. Musculoskeletal exam revealed joint tenderness in his shoulders, elbows, and wrists. Lymphadenopathy was present bilaterally in the axilla.
Lab work was ordered, including a VDRL test and a treponemal antibodies test. Skin biopsies also were taken from lesions on his arm and chest.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Systemic lupus erythematosus
Our patient’s fever and rash were highly suggestive of either systemic lupus erythematosus (SLE) or secondary syphilis (the “great masquerader”).
In addition to the joint tenderness revealed during the musculoskeletal exam, our patient had several nonspecific lupus findings on skin exam: malar rash, discoid rash on hands, subacute vasculitis (generalized rash), alopecia, and an oral ulcer; he also had the specific finding of chilblains vasculitis of the toes. Lab work and pathology results made the diagnosis clear. Lab work revealed leukopenia, an antinuclear antibody (ANA) result of 1:2560 with speckled appearance, and positive anti-SM antibodies. A dipstick was negative for protein; VDRL and treponemal antibodies tests were also negative. Histopathology showed perivascular lymph histiocytic vacuolar dermatitis with a differential of connective tissue disease, including lupus.
Our patient met the criteria
SLE is a systemic autoimmune disease resulting in chronic inflammation in multiple organ systems; it commonly manifests with vague symptoms of fatigue, fever, and weight loss. The prevalence of SLE in the United States has been reported as high as 241 per 100,000 people. 1 Women are more likely to be affected, and the incidence is highest among Black people and lowest among Caucasians.1,2 Risk factors include cigarette smoking and exposure to silica particulate air pollution.
The 2019 European League Against Rheumatism/American College of Rheumatology criteria for a diagnosis of SLE require that a patient have a positive ANA and some, but not all, additive lab, clinical, and organ-specific findings.3 Findings that clinicians should look for include3,4
- elevated ANA (≥ 1:80)
- constitutional symptoms (fever)
- hematologic findings (leukopenia, thrombocytopenia, autoimmune hemolysis)
- neuropsychiatric findings (delirium, psychosis, seizure)
- mucocutaneous findings (alopecia, oral ulcers, others)
- serosal findings (effusion, acute pericarditis)
- musculoskeletal findings (joint involvement)
- renal findings (proteinuria)
- antiphospholipid antibodies
- decreased complement proteins
- SLE-specific antibodies.
Dermatologic findings occur in more than 70% of patients with SLE.5 They can be nonspecific—eg, classic discoid rash, malar rash, alopecia, maculopapular rash (most commonly on sun-exposed areas, mimicking polymorphous light eruption)—or specific (eg, chilblains
Continue to: The differential for rash and fever is broad
The differential for rash and fever is broad
Syphilis also can manifest with rash and fever. The rash of syphilis is nonpainful and affects the torso and face, with concentration on the palms and soles.6,7
Dermatomyositis is a rare disorder of inflammation in both the skin and muscles. Symptoms include rash, muscle aches, and weakness. Lab abnormalities include elevated creatine kinase levels
Erythema multiforme is an immunologic-mediated rash consisting of firm targetoid erythematous papules distributed symmetrically on the extremities, including palms/soles. It typically appears after a viral infection, immunization, or new medications (eg, antibiotics, nonsteroidal anti-inflammatory drugs, or phenothiazines) initiated 1 to 3 weeks prior to the appearance of the rash. History and appearance inform the diagnosis.
Polymorphic light eruption is a rash of variable appearance on sun-exposed areas that results from a sensitivity to sunlight after lack of exposure for a period of time. Symptoms include burning and itching.
Treat patients with SLE with hydroxychloroquine (200-400 mg/d) to suppress inflammation and with low-dose oral steroids such as prednisone (7.5 mg/d) for intermittent exacerbations. Higher steroid doses are sometimes needed for signs of organ inflammation. Patients with increased disease activity will require immunosuppressive therapy with disease-modifying antirheumatic drugs,
Our patient was admitted for further evaluation. A lumbar puncture was performed because of his balance issues; it showed an elevated protein level, but further work-up did not find an infectious or malignant source. Balance improved with hydration. The patient remained hospitalized for 9 days, during which his fever subsided. His pain improved after initiation of hydroxychloroquine 400 mg/d. Follow-up with Rheumatology was arranged for further care.
1. Rees F, Doherty M, Grainge MJ, et al. The worldwide incidence and prevalence of systemic lupus erythematosus: a systematic review of epidemiological studies. Rheumatology (Oxford). 2017;56:1945-1961. doi: 10.1093/rheumatology/kex260
2. CDC. Systemic lupus erythematosus (SLE). Updated July 5, 2022. Accessed April 11, 2023. www.cdc.gov/lupus/facts/detailed.html
3. Aringer M, Costenbader K, Daikh D, et al. 2019 European League Against Rheumatism/American College of Rheumatology classification criteria for systemic lupus erythematosus. Arthritis Rheumatol. 2019;71:1400-1412. doi: 10.1002/art.40930
4. Lam NV, Brown JA, Sharma R. Systemic lupus erythematosus: diagnosis and treatment. Am Fam Physician. 2023;107:383-395.
5. Albrecht J, Berlin JA, Braverman IM, et al. Dermatology position paper on revision of the 1982 ACR criteria for systemic lupus erythematosus. Lupus. 2004;13:839-849. doi: 10.1191/0961203304lu2020oa
6. Dylewski J, Duong M. The rash of secondary syphilis. CMAJ. 2007;176:33-35. doi: 10.1503/cmaj.060665
7. Lautenschlager S. Cutaneous manifestations of syphilis: recognition and management. Am J Clin Dermatol. 2006;7:291-304. doi: 10.2165/00128071-200607050-00003:
8. Brown DL, Frank JE. Diagnosis and management of syphilis. Am Fam Physician. 2003;68:283-290.
9. Ricco J, Westby A. Syphilis: far from ancient history. Am Fam Physician. 2020;102:91-98.
1. Rees F, Doherty M, Grainge MJ, et al. The worldwide incidence and prevalence of systemic lupus erythematosus: a systematic review of epidemiological studies. Rheumatology (Oxford). 2017;56:1945-1961. doi: 10.1093/rheumatology/kex260
2. CDC. Systemic lupus erythematosus (SLE). Updated July 5, 2022. Accessed April 11, 2023. www.cdc.gov/lupus/facts/detailed.html
3. Aringer M, Costenbader K, Daikh D, et al. 2019 European League Against Rheumatism/American College of Rheumatology classification criteria for systemic lupus erythematosus. Arthritis Rheumatol. 2019;71:1400-1412. doi: 10.1002/art.40930
4. Lam NV, Brown JA, Sharma R. Systemic lupus erythematosus: diagnosis and treatment. Am Fam Physician. 2023;107:383-395.
5. Albrecht J, Berlin JA, Braverman IM, et al. Dermatology position paper on revision of the 1982 ACR criteria for systemic lupus erythematosus. Lupus. 2004;13:839-849. doi: 10.1191/0961203304lu2020oa
6. Dylewski J, Duong M. The rash of secondary syphilis. CMAJ. 2007;176:33-35. doi: 10.1503/cmaj.060665
7. Lautenschlager S. Cutaneous manifestations of syphilis: recognition and management. Am J Clin Dermatol. 2006;7:291-304. doi: 10.2165/00128071-200607050-00003:
8. Brown DL, Frank JE. Diagnosis and management of syphilis. Am Fam Physician. 2003;68:283-290.
9. Ricco J, Westby A. Syphilis: far from ancient history. Am Fam Physician. 2020;102:91-98.
