User login
Guillain-Barré syndrome: Honing treatment strategies
Recent insights into the pathophysiology of Guillain-Barré syndrome (GBS) – which affects 1 or 2 persons for every 100,000 people annually, usually post infection – indicate that classic subtypes represent varying manifestations of a shared disease process. This knowledge is yielding new treatment strategies aimed at halting the illness in its tracks. Promising therapies include inhibitors of complement and, perhaps one day, the calcium-activated protease calpain.
Meanwhile, an association between COVID-19 and GBS has been debunked, whereas a small risk of GBS following adenovirus-vectored COVID vaccination is now accepted and quantified. Regardless of cause, the potential severity of GBS and variability in its presentation demand constant vigilance.
Shutting down the disease process
When patients present to an emergency department with sensory symptoms and increasing muscle weakness, “most of the damage has been or is being done,” said Michael P. Lunn, MBBS, MRCP, PhD, professor of clinical neurology, consultant neurologist, and clinical lead in neuroimmunology at University College London Queen Square Institute of Neurology, who spoke at length about GBS with Neurology Reviews 2023 Rare Neurological Disease Special Report. “The crucial reason that GBS treatment has not advanced significantly – and why we’re still slightly stuck where we are in terms of helping people get better more quickly – is that we need something that absolutely turns the disease off as patients come through the door.”
GBS is probably the best-understood autoimmune-mediated neurological disease, in some respects surpassing myasthenia gravis, Dr. Lunn said. “We know very frequently the organisms and stimuli that set off Guillain-Barré syndrome. We understand, to an extent, the immunology and how you break tolerance of the immune system so that an invading organism can provoke an immune response that damages peripheral nerves.”
Compared to what was known about GBS in decades past, neurologists now better understand how and where antibodies attack the nerve; how complement then damages the nodes of Ranvier and paranodes; and how an external attack results in sometimes irreparable internal nerve damage. “We’ve got a string, beginning to end, of understanding the disease,” declared Dr. Lunn.
Understanding of differences in the spectrum of pathology of GBS has led to additional diagnostic categories, said Dr. Lunn. Acute inflammatory demyelinating polyradiculoneuropathy, or typical GBS, represents the most common form in affluent Western nations. A motor variant was recognized in the 1980s; in the mid-1990s, Ho and colleagues described a cohort of patients in China who had acute motor axonal neuropathy and acute motor sensory axonal neuropathy1 – two forms that are particularly common throughout Asia and South America.
Shared mechanism
Based on the findings of electrophysiologic studies, Dr. Lunn said, experts traditionally believed that GBS attacked either axons themselves or their myelin sheaths. “That’s where the anti-ganglioside antibodies come in, providing targeting to nerve structures.” The dichotomous classification system, he added, was partially correct.
Then, through the 2010s and 2020s, neurophysiologist Antonio Uncini, MD, recognized, based partly on histologic studies by Ho and colleagues, that the myelin and axonal subtypes are both likely to stem from the same mechanism.2 When antibodies and complement damage the node of Ranvier, Dr. Lunn said, “the myelin gets stripped off and the conduction becomes slow. But then the myelin can return, and patients get better.” But if damage is severe, it severs the axon, resulting in unrecoverable motor axonal neuropathy. “It’s basically all the same spectrum of disease,” Dr. Lunn said. “Anti-ganglioside antibodies may account for different GBS ‘flavors,’ but the immunological attack all occurs at the node of Ranvier in one way or another.”
The foregoing insight has focused development efforts on the shared seminal pathway of all GBS subtypes and given rise to the concept of nodo-paranodopathy, which incorporates damage at either the node of Ranvier or nearby paranodes.3
Simultaneously, Spanish and French researchers began elucidating new antibodies responsible for neuropathology at the node of Ranvier.4 Anti-ganglioside antibodies have long been loosely associated with acute motor axonal neuropathy and poor outcomes, although, Dr. Lunn said, they fail to tell the full story. Anti-GQ1b antibodies are associated with the Miller-Fisher syndrome subtype, well recognized for its medical features: double vision, loss of tendon reflexes, and arm and leg weakness.
However, Dr. Lunn said, most GBS cases lack anti-ganglioside antibodies. In some GBS cases, antibodies attack neurofascin, contactins, and gliomedin, which are mainly adhesion proteins at nodes of Ranvier.
“Therefore,” Dr. Lunn said, “there must be an antibody-mediated attack of the node of Ranvier or the paranode. That’s an important series of discoveries, primarily because it helps us understand the immunological attack at the node of Ranvier, which goes along with what Dr. Uncini was saying. But it also divides off a group of chronic inflammatory demyelinating polyradiculoneuropathies (CIDP) that present acutely and look initially, for all purposes, like GBS.”
Recognizing acute CIDP (A-CIDP) is critically important for clinicians, Dr. Lunn stressed, because it requires treatment with rituximab (the most commonly used option), steroids, or plasma exchange.
Key clues that distinguish A-CIDP from GBS include:
• A high level of cerebrospinal fluid protein.
• Very slow nerve conduction.
• Early muscle wasting (rare in GBS).
Recognizing CIDP and A-CIDP is crucial, said Dr. Lunn, because it begins to bring all the pathology back together to make sense of GBS. Neurologists have known for decades that, if one damages a nerve with antibodies, then binds complement to those antibodies, the complement punches holes in the affected cells, resulting in death. “But it wasn’t quite clear how those cells might die,” Dr. Lunn said.
After complement-induced injury, calcium-activated calpain permanently damages the entire internal axonal structure.5 Perhaps more important, a 2022 mouse study showed that complement-mediated damage could be directed to myelin or axons using the genetically programmed presence or absence of gangliosides to understand subsequent calpain-induced destruction in either axons or myelin.6
Some of the engineered mouse cells included ganglioside; others did not. “So you can have anti-ganglioside antibodies directed at one cell type or the other, which would, or would not, have calpain within them,” Dr. Lunn said. Investigators also showed that a calpain inhibitor (AK295) or overproduction of an endogenous inhibitor, calpastatin, prevented damage to both cell types.6All existing calpain inhibitors are unsuitable for clinical use because they are highly toxic. “But if you could inhibit calpain and stop it from being activated by calcium,” Dr. Lunn explained, “you would have a mechanism for stopping cell degradation during GBS. That would be an important future target for pharmacotherapy. That whole story – from the beginning to the end of GBS – has opened up options for treatment.”
Because complement bound to antibodies, set up by infection, plays a pivotal role, complement inhibitors have become an exciting area of research over the past decade. The 36-patient Japanese Eculizumab Trial for GBS (JET-GBS) trial showed that, after 6 months, significantly more eculizumab-treated patients could run, compared with placebo-treated patients.7
“No other trials of complement inhibitors have yet been completed,” Dr. Lunn said. “But several different complement inhibitors work at different places, in a very complicated immune process. One of the complement inhibitors will become transformative in treating GBS – preventing disability and improving recovery – in the not-very-distant future.”
Additional investigational treatments that have demonstrated early promise in eliminating problem antibodies faster include imlifidase (Idefirix [Hansa Biopharma]), which destroys antibodies, and Fc receptor inhibitors such as efgartigimod alfa-fcab (Vyvgart [argenx]), which push antibodies into the natural catabolic pathway.
“We’ve been stuck with plasma exchange and intravenous immunoglobulin (IVIg) for three or four decades,” Dr. Lunn said. “We now have a series of strategies by which we can completely turn off complement and resulting nerve damage. If we can find a calpain inhibitor that turns off the end of that pathway, we will make dramatic improvements. Our understanding of the immunopathology has changed enormously and influences pharmacotherapy going forward.”
Recap of diagnosis and treatment
For decades, the diagnosis of GBS has relied on the presence of symptoms, including progressive weakness and loss of reflexes and sensations. Nerve-conduction studies and cerebrospinal fluid evaluation can help confirm the diagnosis.
IVIg shortens recovery, said Dr. Lunn, although nothing cures GBS. “And that’s a common problem: Clinicians think that they’re going to give somebody IVIg, and the patient’s going to get better immediately.” When that doesn’t happen, he said, physicians are tempted to give a second immunoglobulin dose.
However, a study published in 2021 shows that a second IVIg dose does not result in faster or better improvement – only in a significant risk of cardiovascular, cerebrovascular, and other thrombotic events 3 weeks later.8 Dr. Lunn noted that, although adverse-event data were “buried” in the supplemental materials of that study, the high cost of IVIg (approximately $12,500 per dose) means that the study has changed practice for the benefit of patients, providers, and health care systems.
COVID-19 and GBS triggers
Campylobacter jejuni infection still accounts for 30% to 40% of GBS cases, followed by other bacteria, including Mycoplasma pneumoniae and Haemophilus influenzae, and then by viruses, including cytomegalovirus and, rarely, human immunodeficiency virus. In recent years, severe acute respiratory syndrome coronavirus (SARS-CoV-2) infection – COVID-19 – and vaccines against the viral infection have captured headlines for purportedly being a cause of GBS.
The Zika virus epidemic of 2015-2016 has been linked to GBS-like illness. The 2003 severe acute respiratory syndrome (SARS) pandemic and the Middle East respiratory syndrome coronavirus (MERS-CoV) epidemic were associated with GBS – although, taken together, SARS and MERS-CoV produced fewer than 10 cases of GBS, Dr. Lunn noted. Nevertheless, heightened awareness of these viruses fueled hypervigilance regarding the prospect that COVID-19 could cause GBS. Following reports of a single such case in Wuhan and hundreds in Italy, worry over pandemic GBS grew worldwide.
Dr. Lunn and colleagues addressed the COVID-19–GBS question in a 2023 publication.9 “Because GBS is largely treated only with IVIg, and IVIg costs a lot of money, and the U.K. government insists on every dose of IVIg being logged in a government database, we were able to identify virtually every case of GBS,” he said.
GBS diagnoses were reliable, he added, because each case was confirmed by physicians outside the emergency department. Analysis revealed that, in 2020, U.K. GBS cases actually declined by around one-third. “And even when there was a second wave of COVID-19 at the end of 2020, partly caused by better counting,” Dr. Lunn said, “there was no further increase in GBS cases. We concluded that there was no link between GBS and COVID-19, as the cases simply didn’t appear.”
The foregoing findings have since been corroborated by studies in Singapore, the United States, and South America, he pointed out. Earlier case series suggesting a link between COVID-19 and GBS were selective, Dr. Lunn added, with numbers too small to support robust conclusions.
The lack of a causal link between COVID-19 and GBS suggested to Dr. Lunn that there was no reason COVID-19 vaccination should cause GBS. All COVID-19 vaccines were designed to provoke an immune response either (1) by producing the SARS-CoV-2 spike protein on the surface of virus (through a replication-incompetent adenoviral vector) or (2) through DNA or mRNA transcription, he explained. “The spike protein is only a small part of COVID-19.”
GBS: ‘Adverse event of interest’
A link between modern vaccines and GBS first appeared in the 1970s with the hastily developed swine flu vaccine. “In late 1976,” Dr. Lunn explained, “it was identified that patients who were given that vaccine seemed to be developing illnesses consistent with GBS.” By 1980, Dr. Lunn said, the risk level was determined to be only five or six cases for every 1 million doses of vaccine administered. “But the vaccine program was aborted, and swine flu never really happened.” Every year since, “there has been a surveillance program looking at the occurrence of an association of GBS with influenza vaccine.”
Minor fluctuations aside, he said, the overall incidence of GBS with influenza vaccination – 1 GBS case for every 1 million vaccine doses given – has remained consistent over several decades. “Nevertheless, GBS became an adverse event of special interest for any vaccination campaign.”
COVID-19 vaccination. Dr. Lunn and colleagues used the United Kingdom National Health Service (NHS) National Immunoglobulin Database, and other databases, to pinpoint the risk of GBS presented by the first dose of the AstraZeneca ChAdOx1 nCoV-19 adenoviral vaccine.10 As with U.K. GBS cases, every COVID-19 vaccination is linked to an NHS number. “We identified all the cases of GBS, found their NHS numbers, and went back and found the exact dates they’d been vaccinated, and with which vaccine.” Only the adenoviral-vector vaccine carried an excess risk of GBS – 5.8 cases for every 1 million doses, associated only with the first dose and peaking at approximately 25 days post vaccination – compared with other vaccines used in the United Kingdom.
Researchers looked at data from the Vaccine Adverse Event Reporting System (VAERS), a program of the Centers for Disease Control and Prevention and the Food and Drug Administration, encompassing nearly 500 million COVID-19 vaccine doses given between December 2020 and January 2022. They found that patients who received the Ad26.COV2.S vaccine (Janssen/Johnson & Johnson) had a rate of GBS (within 21 and 41 days post vaccination) that was 9 and 12 times higher, respectively, than corresponding rates for the mRNA-1273 (Moderna) and BNT162b2 (Pfizer BioNTech) COVID-19 vaccines.11 Risk was distributed relatively evenly by gender and age. Also at day 21 and day 41, observed event ratios with the adenoviral-vector vaccine (use of which has been suspended in the United States) were 3.79 and 2.34, respectively. Observed-event ratios with the other vaccines mirrored expected background rates.
The VAERS analysis confirms earlier data from the CDC’s Vaccine Safety Datalink, which showed that, among approximately 15 million U.S. vaccine doses given between mid-December 2020 and mid-November 2021, the unadjusted GBS incidence rate for every 100,000 person-years for the adenoviral vaccine, 21 days post exposure, was 32.4, compared with 1.3 for the mRNA vaccine. The adjusted relative risk with the adenoviral vaccine in the first 3 weeks post vaccination, compared to the 3- to 6-week interval post vaccination, was 6.03.12 In addition, a head-to-head comparison of adenoviral versus mRNA vaccines at 21 days revealed an adjusted rate ratio of 20.56. Mechanistically, some experts theorize that antibodies induced by the Janssen vaccine might cross-react with glycoproteins on the myelin sheath of peripheral nerve axons to cause GBS, but this remains unproven.11
The AstraZeneca vaccine uses a chimpanzee adenovirus; the Janssen vaccine uses a human adenoviral carrier. “The only commonality between the Janssen/Johnson & Johnson and AstraZeneca vaccines, and the only thing that’s different from the other vaccines, is the adenoviral vector packaging,” Dr. Lunn emphasized. “I believe it’s what generates GBS after COVID-19 vaccination. It has nothing to do with the COVID-19 vaccination, the spike protein, the nucleic acid, the DNA, or anything else.”
The adenoviral vector probably also explains why GBS peaks during winter, said Dr. Lunn. “That’s when adenovirus is circulating.” When people contract the common cold, he explained, they don’t visit their family physician and request a swab to isolate the adenovirus. “By the time you get GBS, the adenovirus has been cleared. We’ve all got antibodies to adenovirus all over the place, anyway, because we get it so often.”
It would be difficult to prove conclusively that adenovirus belongs on the list of GBS causes, Dr. Lunn allowed. “But I have a strong suspicion that it does. COVID-19 and COVID-19 vaccination have given us some new avenues into identifying GBS causation potentially in the near future.” More research is needed in this area, he said.
Dr. Lunn has been a principal investigator for argenx (efgartigimod) and an adviser to AstraZeneca (ChAdOx1 nCoV-19). He has received travel grants from CSL Behring.
References
1. Ho TW et al. Guillain-Barré syndrome in northern China. Relationship to Campylobacter jejuni infection and anti-glycolipid antibodies. Brain. 1995;118(Pt 3):597-605. doi: 10.1093/brain/118.3.597.
2. Uncini A. A common mechanism and a new categorization for anti-ganglioside antibody-mediated neuropathies. Exp Neurol. 2012;235(2):513-6. doi: 10.1016/j.expneurol.2012.03.023.
3. Uncini A and Kuwabara S. The electrodiagnosis of Guillain-Barré syndrome subtypes: where do we stand? Clin Neurophysiol. 2018;129(12):2586-93. doi: 10.1016/j.clinph.2018.09.025.
4. Delmont E et al. Autoantibodies to nodal isoforms of neurofascin in chronic inflammatory demyelinating polyneuropathy. Brain. 2017;140(7):1851-8. doi: 10.1093/brain/awx124.
5. McGonigal R et al. Anti-GD1a antibodies activate complement and calpain to injure distal motor nodes of Ranvier in mice. Brain. 2010;133(Pt 7):1944-60. doi: 10.1093/brain/awq119.
6. Cunningham ME et al. Real time imaging of intra-axonal calcium flux in an explant mouse model of axonal Guillain-Barré syndrome. Exp Neurol. 2022 Sep;355:114127. doi: 10.1016/j.expneurol.2022.114127.
7. Misawa S et al; Japanese Eculizumab Trial for GBS (JET-GBS) Study Group. Safety and efficacy of eculizumab in Guillain-Barré syndrome: a multicentre, double-blind, randomised phase 2 trial. Lancet Neurol. 2018;17(6):519-29. doi: 10.1016/S1474-4422(18)30114-5.
8. Walgaard C et al; Dutch GBS Study Group. Second intravenous immunoglobulin dose in patients with Guillain-Barré syndrome with poor prognosis (SID-GBS): a double-blind, randomised, placebo-controlled trial. Lancet Neurol. 2021;20(4):275-83. doi: 10.1016/S1474-4422(20)30494-4.
9. Keddie S et al. Epidemiological and cohort study finds no association between COVID-19 and Guillain-Barré syndrome. Brain. 2021;144(2):682-93. doi: 10.1093/brain/awaa433.
10. Keh RYS et al; BPNS/ABN COVID-19 Vaccine GBS Study Group. COVID-19 vaccination and Guillain-Barré syndrome: Analyses using the National Immunoglobulin Database. Brain. 2023;146(2):739-48. doi: 10.1093/brain/awac067.
11. Abara WE et al. Reports of Guillain-Barré syndrome after COVID-19 vaccination in the United States. JAMA Netw Open. 2023;6(2):e2253845. doi: 10.1001/jamanetworkopen.2022.53845.
12. Hanson KE et al. Incidence of Guillain-Barré syndrome after COVID-19 vaccination in the Vaccine Safety Datalink. JAMA Netw Open. 2022;5(4):e228879. doi: 10.1001/jamanetworkopen.2022.8879.
Recent insights into the pathophysiology of Guillain-Barré syndrome (GBS) – which affects 1 or 2 persons for every 100,000 people annually, usually post infection – indicate that classic subtypes represent varying manifestations of a shared disease process. This knowledge is yielding new treatment strategies aimed at halting the illness in its tracks. Promising therapies include inhibitors of complement and, perhaps one day, the calcium-activated protease calpain.
Meanwhile, an association between COVID-19 and GBS has been debunked, whereas a small risk of GBS following adenovirus-vectored COVID vaccination is now accepted and quantified. Regardless of cause, the potential severity of GBS and variability in its presentation demand constant vigilance.
Shutting down the disease process
When patients present to an emergency department with sensory symptoms and increasing muscle weakness, “most of the damage has been or is being done,” said Michael P. Lunn, MBBS, MRCP, PhD, professor of clinical neurology, consultant neurologist, and clinical lead in neuroimmunology at University College London Queen Square Institute of Neurology, who spoke at length about GBS with Neurology Reviews 2023 Rare Neurological Disease Special Report. “The crucial reason that GBS treatment has not advanced significantly – and why we’re still slightly stuck where we are in terms of helping people get better more quickly – is that we need something that absolutely turns the disease off as patients come through the door.”
GBS is probably the best-understood autoimmune-mediated neurological disease, in some respects surpassing myasthenia gravis, Dr. Lunn said. “We know very frequently the organisms and stimuli that set off Guillain-Barré syndrome. We understand, to an extent, the immunology and how you break tolerance of the immune system so that an invading organism can provoke an immune response that damages peripheral nerves.”
Compared to what was known about GBS in decades past, neurologists now better understand how and where antibodies attack the nerve; how complement then damages the nodes of Ranvier and paranodes; and how an external attack results in sometimes irreparable internal nerve damage. “We’ve got a string, beginning to end, of understanding the disease,” declared Dr. Lunn.
Understanding of differences in the spectrum of pathology of GBS has led to additional diagnostic categories, said Dr. Lunn. Acute inflammatory demyelinating polyradiculoneuropathy, or typical GBS, represents the most common form in affluent Western nations. A motor variant was recognized in the 1980s; in the mid-1990s, Ho and colleagues described a cohort of patients in China who had acute motor axonal neuropathy and acute motor sensory axonal neuropathy1 – two forms that are particularly common throughout Asia and South America.
Shared mechanism
Based on the findings of electrophysiologic studies, Dr. Lunn said, experts traditionally believed that GBS attacked either axons themselves or their myelin sheaths. “That’s where the anti-ganglioside antibodies come in, providing targeting to nerve structures.” The dichotomous classification system, he added, was partially correct.
Then, through the 2010s and 2020s, neurophysiologist Antonio Uncini, MD, recognized, based partly on histologic studies by Ho and colleagues, that the myelin and axonal subtypes are both likely to stem from the same mechanism.2 When antibodies and complement damage the node of Ranvier, Dr. Lunn said, “the myelin gets stripped off and the conduction becomes slow. But then the myelin can return, and patients get better.” But if damage is severe, it severs the axon, resulting in unrecoverable motor axonal neuropathy. “It’s basically all the same spectrum of disease,” Dr. Lunn said. “Anti-ganglioside antibodies may account for different GBS ‘flavors,’ but the immunological attack all occurs at the node of Ranvier in one way or another.”
The foregoing insight has focused development efforts on the shared seminal pathway of all GBS subtypes and given rise to the concept of nodo-paranodopathy, which incorporates damage at either the node of Ranvier or nearby paranodes.3
Simultaneously, Spanish and French researchers began elucidating new antibodies responsible for neuropathology at the node of Ranvier.4 Anti-ganglioside antibodies have long been loosely associated with acute motor axonal neuropathy and poor outcomes, although, Dr. Lunn said, they fail to tell the full story. Anti-GQ1b antibodies are associated with the Miller-Fisher syndrome subtype, well recognized for its medical features: double vision, loss of tendon reflexes, and arm and leg weakness.
However, Dr. Lunn said, most GBS cases lack anti-ganglioside antibodies. In some GBS cases, antibodies attack neurofascin, contactins, and gliomedin, which are mainly adhesion proteins at nodes of Ranvier.
“Therefore,” Dr. Lunn said, “there must be an antibody-mediated attack of the node of Ranvier or the paranode. That’s an important series of discoveries, primarily because it helps us understand the immunological attack at the node of Ranvier, which goes along with what Dr. Uncini was saying. But it also divides off a group of chronic inflammatory demyelinating polyradiculoneuropathies (CIDP) that present acutely and look initially, for all purposes, like GBS.”
Recognizing acute CIDP (A-CIDP) is critically important for clinicians, Dr. Lunn stressed, because it requires treatment with rituximab (the most commonly used option), steroids, or plasma exchange.
Key clues that distinguish A-CIDP from GBS include:
• A high level of cerebrospinal fluid protein.
• Very slow nerve conduction.
• Early muscle wasting (rare in GBS).
Recognizing CIDP and A-CIDP is crucial, said Dr. Lunn, because it begins to bring all the pathology back together to make sense of GBS. Neurologists have known for decades that, if one damages a nerve with antibodies, then binds complement to those antibodies, the complement punches holes in the affected cells, resulting in death. “But it wasn’t quite clear how those cells might die,” Dr. Lunn said.
After complement-induced injury, calcium-activated calpain permanently damages the entire internal axonal structure.5 Perhaps more important, a 2022 mouse study showed that complement-mediated damage could be directed to myelin or axons using the genetically programmed presence or absence of gangliosides to understand subsequent calpain-induced destruction in either axons or myelin.6
Some of the engineered mouse cells included ganglioside; others did not. “So you can have anti-ganglioside antibodies directed at one cell type or the other, which would, or would not, have calpain within them,” Dr. Lunn said. Investigators also showed that a calpain inhibitor (AK295) or overproduction of an endogenous inhibitor, calpastatin, prevented damage to both cell types.6All existing calpain inhibitors are unsuitable for clinical use because they are highly toxic. “But if you could inhibit calpain and stop it from being activated by calcium,” Dr. Lunn explained, “you would have a mechanism for stopping cell degradation during GBS. That would be an important future target for pharmacotherapy. That whole story – from the beginning to the end of GBS – has opened up options for treatment.”
Because complement bound to antibodies, set up by infection, plays a pivotal role, complement inhibitors have become an exciting area of research over the past decade. The 36-patient Japanese Eculizumab Trial for GBS (JET-GBS) trial showed that, after 6 months, significantly more eculizumab-treated patients could run, compared with placebo-treated patients.7
“No other trials of complement inhibitors have yet been completed,” Dr. Lunn said. “But several different complement inhibitors work at different places, in a very complicated immune process. One of the complement inhibitors will become transformative in treating GBS – preventing disability and improving recovery – in the not-very-distant future.”
Additional investigational treatments that have demonstrated early promise in eliminating problem antibodies faster include imlifidase (Idefirix [Hansa Biopharma]), which destroys antibodies, and Fc receptor inhibitors such as efgartigimod alfa-fcab (Vyvgart [argenx]), which push antibodies into the natural catabolic pathway.
“We’ve been stuck with plasma exchange and intravenous immunoglobulin (IVIg) for three or four decades,” Dr. Lunn said. “We now have a series of strategies by which we can completely turn off complement and resulting nerve damage. If we can find a calpain inhibitor that turns off the end of that pathway, we will make dramatic improvements. Our understanding of the immunopathology has changed enormously and influences pharmacotherapy going forward.”
Recap of diagnosis and treatment
For decades, the diagnosis of GBS has relied on the presence of symptoms, including progressive weakness and loss of reflexes and sensations. Nerve-conduction studies and cerebrospinal fluid evaluation can help confirm the diagnosis.
IVIg shortens recovery, said Dr. Lunn, although nothing cures GBS. “And that’s a common problem: Clinicians think that they’re going to give somebody IVIg, and the patient’s going to get better immediately.” When that doesn’t happen, he said, physicians are tempted to give a second immunoglobulin dose.
However, a study published in 2021 shows that a second IVIg dose does not result in faster or better improvement – only in a significant risk of cardiovascular, cerebrovascular, and other thrombotic events 3 weeks later.8 Dr. Lunn noted that, although adverse-event data were “buried” in the supplemental materials of that study, the high cost of IVIg (approximately $12,500 per dose) means that the study has changed practice for the benefit of patients, providers, and health care systems.
COVID-19 and GBS triggers
Campylobacter jejuni infection still accounts for 30% to 40% of GBS cases, followed by other bacteria, including Mycoplasma pneumoniae and Haemophilus influenzae, and then by viruses, including cytomegalovirus and, rarely, human immunodeficiency virus. In recent years, severe acute respiratory syndrome coronavirus (SARS-CoV-2) infection – COVID-19 – and vaccines against the viral infection have captured headlines for purportedly being a cause of GBS.
The Zika virus epidemic of 2015-2016 has been linked to GBS-like illness. The 2003 severe acute respiratory syndrome (SARS) pandemic and the Middle East respiratory syndrome coronavirus (MERS-CoV) epidemic were associated with GBS – although, taken together, SARS and MERS-CoV produced fewer than 10 cases of GBS, Dr. Lunn noted. Nevertheless, heightened awareness of these viruses fueled hypervigilance regarding the prospect that COVID-19 could cause GBS. Following reports of a single such case in Wuhan and hundreds in Italy, worry over pandemic GBS grew worldwide.
Dr. Lunn and colleagues addressed the COVID-19–GBS question in a 2023 publication.9 “Because GBS is largely treated only with IVIg, and IVIg costs a lot of money, and the U.K. government insists on every dose of IVIg being logged in a government database, we were able to identify virtually every case of GBS,” he said.
GBS diagnoses were reliable, he added, because each case was confirmed by physicians outside the emergency department. Analysis revealed that, in 2020, U.K. GBS cases actually declined by around one-third. “And even when there was a second wave of COVID-19 at the end of 2020, partly caused by better counting,” Dr. Lunn said, “there was no further increase in GBS cases. We concluded that there was no link between GBS and COVID-19, as the cases simply didn’t appear.”
The foregoing findings have since been corroborated by studies in Singapore, the United States, and South America, he pointed out. Earlier case series suggesting a link between COVID-19 and GBS were selective, Dr. Lunn added, with numbers too small to support robust conclusions.
The lack of a causal link between COVID-19 and GBS suggested to Dr. Lunn that there was no reason COVID-19 vaccination should cause GBS. All COVID-19 vaccines were designed to provoke an immune response either (1) by producing the SARS-CoV-2 spike protein on the surface of virus (through a replication-incompetent adenoviral vector) or (2) through DNA or mRNA transcription, he explained. “The spike protein is only a small part of COVID-19.”
GBS: ‘Adverse event of interest’
A link between modern vaccines and GBS first appeared in the 1970s with the hastily developed swine flu vaccine. “In late 1976,” Dr. Lunn explained, “it was identified that patients who were given that vaccine seemed to be developing illnesses consistent with GBS.” By 1980, Dr. Lunn said, the risk level was determined to be only five or six cases for every 1 million doses of vaccine administered. “But the vaccine program was aborted, and swine flu never really happened.” Every year since, “there has been a surveillance program looking at the occurrence of an association of GBS with influenza vaccine.”
Minor fluctuations aside, he said, the overall incidence of GBS with influenza vaccination – 1 GBS case for every 1 million vaccine doses given – has remained consistent over several decades. “Nevertheless, GBS became an adverse event of special interest for any vaccination campaign.”
COVID-19 vaccination. Dr. Lunn and colleagues used the United Kingdom National Health Service (NHS) National Immunoglobulin Database, and other databases, to pinpoint the risk of GBS presented by the first dose of the AstraZeneca ChAdOx1 nCoV-19 adenoviral vaccine.10 As with U.K. GBS cases, every COVID-19 vaccination is linked to an NHS number. “We identified all the cases of GBS, found their NHS numbers, and went back and found the exact dates they’d been vaccinated, and with which vaccine.” Only the adenoviral-vector vaccine carried an excess risk of GBS – 5.8 cases for every 1 million doses, associated only with the first dose and peaking at approximately 25 days post vaccination – compared with other vaccines used in the United Kingdom.
Researchers looked at data from the Vaccine Adverse Event Reporting System (VAERS), a program of the Centers for Disease Control and Prevention and the Food and Drug Administration, encompassing nearly 500 million COVID-19 vaccine doses given between December 2020 and January 2022. They found that patients who received the Ad26.COV2.S vaccine (Janssen/Johnson & Johnson) had a rate of GBS (within 21 and 41 days post vaccination) that was 9 and 12 times higher, respectively, than corresponding rates for the mRNA-1273 (Moderna) and BNT162b2 (Pfizer BioNTech) COVID-19 vaccines.11 Risk was distributed relatively evenly by gender and age. Also at day 21 and day 41, observed event ratios with the adenoviral-vector vaccine (use of which has been suspended in the United States) were 3.79 and 2.34, respectively. Observed-event ratios with the other vaccines mirrored expected background rates.
The VAERS analysis confirms earlier data from the CDC’s Vaccine Safety Datalink, which showed that, among approximately 15 million U.S. vaccine doses given between mid-December 2020 and mid-November 2021, the unadjusted GBS incidence rate for every 100,000 person-years for the adenoviral vaccine, 21 days post exposure, was 32.4, compared with 1.3 for the mRNA vaccine. The adjusted relative risk with the adenoviral vaccine in the first 3 weeks post vaccination, compared to the 3- to 6-week interval post vaccination, was 6.03.12 In addition, a head-to-head comparison of adenoviral versus mRNA vaccines at 21 days revealed an adjusted rate ratio of 20.56. Mechanistically, some experts theorize that antibodies induced by the Janssen vaccine might cross-react with glycoproteins on the myelin sheath of peripheral nerve axons to cause GBS, but this remains unproven.11
The AstraZeneca vaccine uses a chimpanzee adenovirus; the Janssen vaccine uses a human adenoviral carrier. “The only commonality between the Janssen/Johnson & Johnson and AstraZeneca vaccines, and the only thing that’s different from the other vaccines, is the adenoviral vector packaging,” Dr. Lunn emphasized. “I believe it’s what generates GBS after COVID-19 vaccination. It has nothing to do with the COVID-19 vaccination, the spike protein, the nucleic acid, the DNA, or anything else.”
The adenoviral vector probably also explains why GBS peaks during winter, said Dr. Lunn. “That’s when adenovirus is circulating.” When people contract the common cold, he explained, they don’t visit their family physician and request a swab to isolate the adenovirus. “By the time you get GBS, the adenovirus has been cleared. We’ve all got antibodies to adenovirus all over the place, anyway, because we get it so often.”
It would be difficult to prove conclusively that adenovirus belongs on the list of GBS causes, Dr. Lunn allowed. “But I have a strong suspicion that it does. COVID-19 and COVID-19 vaccination have given us some new avenues into identifying GBS causation potentially in the near future.” More research is needed in this area, he said.
Dr. Lunn has been a principal investigator for argenx (efgartigimod) and an adviser to AstraZeneca (ChAdOx1 nCoV-19). He has received travel grants from CSL Behring.
References
1. Ho TW et al. Guillain-Barré syndrome in northern China. Relationship to Campylobacter jejuni infection and anti-glycolipid antibodies. Brain. 1995;118(Pt 3):597-605. doi: 10.1093/brain/118.3.597.
2. Uncini A. A common mechanism and a new categorization for anti-ganglioside antibody-mediated neuropathies. Exp Neurol. 2012;235(2):513-6. doi: 10.1016/j.expneurol.2012.03.023.
3. Uncini A and Kuwabara S. The electrodiagnosis of Guillain-Barré syndrome subtypes: where do we stand? Clin Neurophysiol. 2018;129(12):2586-93. doi: 10.1016/j.clinph.2018.09.025.
4. Delmont E et al. Autoantibodies to nodal isoforms of neurofascin in chronic inflammatory demyelinating polyneuropathy. Brain. 2017;140(7):1851-8. doi: 10.1093/brain/awx124.
5. McGonigal R et al. Anti-GD1a antibodies activate complement and calpain to injure distal motor nodes of Ranvier in mice. Brain. 2010;133(Pt 7):1944-60. doi: 10.1093/brain/awq119.
6. Cunningham ME et al. Real time imaging of intra-axonal calcium flux in an explant mouse model of axonal Guillain-Barré syndrome. Exp Neurol. 2022 Sep;355:114127. doi: 10.1016/j.expneurol.2022.114127.
7. Misawa S et al; Japanese Eculizumab Trial for GBS (JET-GBS) Study Group. Safety and efficacy of eculizumab in Guillain-Barré syndrome: a multicentre, double-blind, randomised phase 2 trial. Lancet Neurol. 2018;17(6):519-29. doi: 10.1016/S1474-4422(18)30114-5.
8. Walgaard C et al; Dutch GBS Study Group. Second intravenous immunoglobulin dose in patients with Guillain-Barré syndrome with poor prognosis (SID-GBS): a double-blind, randomised, placebo-controlled trial. Lancet Neurol. 2021;20(4):275-83. doi: 10.1016/S1474-4422(20)30494-4.
9. Keddie S et al. Epidemiological and cohort study finds no association between COVID-19 and Guillain-Barré syndrome. Brain. 2021;144(2):682-93. doi: 10.1093/brain/awaa433.
10. Keh RYS et al; BPNS/ABN COVID-19 Vaccine GBS Study Group. COVID-19 vaccination and Guillain-Barré syndrome: Analyses using the National Immunoglobulin Database. Brain. 2023;146(2):739-48. doi: 10.1093/brain/awac067.
11. Abara WE et al. Reports of Guillain-Barré syndrome after COVID-19 vaccination in the United States. JAMA Netw Open. 2023;6(2):e2253845. doi: 10.1001/jamanetworkopen.2022.53845.
12. Hanson KE et al. Incidence of Guillain-Barré syndrome after COVID-19 vaccination in the Vaccine Safety Datalink. JAMA Netw Open. 2022;5(4):e228879. doi: 10.1001/jamanetworkopen.2022.8879.
Recent insights into the pathophysiology of Guillain-Barré syndrome (GBS) – which affects 1 or 2 persons for every 100,000 people annually, usually post infection – indicate that classic subtypes represent varying manifestations of a shared disease process. This knowledge is yielding new treatment strategies aimed at halting the illness in its tracks. Promising therapies include inhibitors of complement and, perhaps one day, the calcium-activated protease calpain.
Meanwhile, an association between COVID-19 and GBS has been debunked, whereas a small risk of GBS following adenovirus-vectored COVID vaccination is now accepted and quantified. Regardless of cause, the potential severity of GBS and variability in its presentation demand constant vigilance.
Shutting down the disease process
When patients present to an emergency department with sensory symptoms and increasing muscle weakness, “most of the damage has been or is being done,” said Michael P. Lunn, MBBS, MRCP, PhD, professor of clinical neurology, consultant neurologist, and clinical lead in neuroimmunology at University College London Queen Square Institute of Neurology, who spoke at length about GBS with Neurology Reviews 2023 Rare Neurological Disease Special Report. “The crucial reason that GBS treatment has not advanced significantly – and why we’re still slightly stuck where we are in terms of helping people get better more quickly – is that we need something that absolutely turns the disease off as patients come through the door.”
GBS is probably the best-understood autoimmune-mediated neurological disease, in some respects surpassing myasthenia gravis, Dr. Lunn said. “We know very frequently the organisms and stimuli that set off Guillain-Barré syndrome. We understand, to an extent, the immunology and how you break tolerance of the immune system so that an invading organism can provoke an immune response that damages peripheral nerves.”
Compared to what was known about GBS in decades past, neurologists now better understand how and where antibodies attack the nerve; how complement then damages the nodes of Ranvier and paranodes; and how an external attack results in sometimes irreparable internal nerve damage. “We’ve got a string, beginning to end, of understanding the disease,” declared Dr. Lunn.
Understanding of differences in the spectrum of pathology of GBS has led to additional diagnostic categories, said Dr. Lunn. Acute inflammatory demyelinating polyradiculoneuropathy, or typical GBS, represents the most common form in affluent Western nations. A motor variant was recognized in the 1980s; in the mid-1990s, Ho and colleagues described a cohort of patients in China who had acute motor axonal neuropathy and acute motor sensory axonal neuropathy1 – two forms that are particularly common throughout Asia and South America.
Shared mechanism
Based on the findings of electrophysiologic studies, Dr. Lunn said, experts traditionally believed that GBS attacked either axons themselves or their myelin sheaths. “That’s where the anti-ganglioside antibodies come in, providing targeting to nerve structures.” The dichotomous classification system, he added, was partially correct.
Then, through the 2010s and 2020s, neurophysiologist Antonio Uncini, MD, recognized, based partly on histologic studies by Ho and colleagues, that the myelin and axonal subtypes are both likely to stem from the same mechanism.2 When antibodies and complement damage the node of Ranvier, Dr. Lunn said, “the myelin gets stripped off and the conduction becomes slow. But then the myelin can return, and patients get better.” But if damage is severe, it severs the axon, resulting in unrecoverable motor axonal neuropathy. “It’s basically all the same spectrum of disease,” Dr. Lunn said. “Anti-ganglioside antibodies may account for different GBS ‘flavors,’ but the immunological attack all occurs at the node of Ranvier in one way or another.”
The foregoing insight has focused development efforts on the shared seminal pathway of all GBS subtypes and given rise to the concept of nodo-paranodopathy, which incorporates damage at either the node of Ranvier or nearby paranodes.3
Simultaneously, Spanish and French researchers began elucidating new antibodies responsible for neuropathology at the node of Ranvier.4 Anti-ganglioside antibodies have long been loosely associated with acute motor axonal neuropathy and poor outcomes, although, Dr. Lunn said, they fail to tell the full story. Anti-GQ1b antibodies are associated with the Miller-Fisher syndrome subtype, well recognized for its medical features: double vision, loss of tendon reflexes, and arm and leg weakness.
However, Dr. Lunn said, most GBS cases lack anti-ganglioside antibodies. In some GBS cases, antibodies attack neurofascin, contactins, and gliomedin, which are mainly adhesion proteins at nodes of Ranvier.
“Therefore,” Dr. Lunn said, “there must be an antibody-mediated attack of the node of Ranvier or the paranode. That’s an important series of discoveries, primarily because it helps us understand the immunological attack at the node of Ranvier, which goes along with what Dr. Uncini was saying. But it also divides off a group of chronic inflammatory demyelinating polyradiculoneuropathies (CIDP) that present acutely and look initially, for all purposes, like GBS.”
Recognizing acute CIDP (A-CIDP) is critically important for clinicians, Dr. Lunn stressed, because it requires treatment with rituximab (the most commonly used option), steroids, or plasma exchange.
Key clues that distinguish A-CIDP from GBS include:
• A high level of cerebrospinal fluid protein.
• Very slow nerve conduction.
• Early muscle wasting (rare in GBS).
Recognizing CIDP and A-CIDP is crucial, said Dr. Lunn, because it begins to bring all the pathology back together to make sense of GBS. Neurologists have known for decades that, if one damages a nerve with antibodies, then binds complement to those antibodies, the complement punches holes in the affected cells, resulting in death. “But it wasn’t quite clear how those cells might die,” Dr. Lunn said.
After complement-induced injury, calcium-activated calpain permanently damages the entire internal axonal structure.5 Perhaps more important, a 2022 mouse study showed that complement-mediated damage could be directed to myelin or axons using the genetically programmed presence or absence of gangliosides to understand subsequent calpain-induced destruction in either axons or myelin.6
Some of the engineered mouse cells included ganglioside; others did not. “So you can have anti-ganglioside antibodies directed at one cell type or the other, which would, or would not, have calpain within them,” Dr. Lunn said. Investigators also showed that a calpain inhibitor (AK295) or overproduction of an endogenous inhibitor, calpastatin, prevented damage to both cell types.6All existing calpain inhibitors are unsuitable for clinical use because they are highly toxic. “But if you could inhibit calpain and stop it from being activated by calcium,” Dr. Lunn explained, “you would have a mechanism for stopping cell degradation during GBS. That would be an important future target for pharmacotherapy. That whole story – from the beginning to the end of GBS – has opened up options for treatment.”
Because complement bound to antibodies, set up by infection, plays a pivotal role, complement inhibitors have become an exciting area of research over the past decade. The 36-patient Japanese Eculizumab Trial for GBS (JET-GBS) trial showed that, after 6 months, significantly more eculizumab-treated patients could run, compared with placebo-treated patients.7
“No other trials of complement inhibitors have yet been completed,” Dr. Lunn said. “But several different complement inhibitors work at different places, in a very complicated immune process. One of the complement inhibitors will become transformative in treating GBS – preventing disability and improving recovery – in the not-very-distant future.”
Additional investigational treatments that have demonstrated early promise in eliminating problem antibodies faster include imlifidase (Idefirix [Hansa Biopharma]), which destroys antibodies, and Fc receptor inhibitors such as efgartigimod alfa-fcab (Vyvgart [argenx]), which push antibodies into the natural catabolic pathway.
“We’ve been stuck with plasma exchange and intravenous immunoglobulin (IVIg) for three or four decades,” Dr. Lunn said. “We now have a series of strategies by which we can completely turn off complement and resulting nerve damage. If we can find a calpain inhibitor that turns off the end of that pathway, we will make dramatic improvements. Our understanding of the immunopathology has changed enormously and influences pharmacotherapy going forward.”
Recap of diagnosis and treatment
For decades, the diagnosis of GBS has relied on the presence of symptoms, including progressive weakness and loss of reflexes and sensations. Nerve-conduction studies and cerebrospinal fluid evaluation can help confirm the diagnosis.
IVIg shortens recovery, said Dr. Lunn, although nothing cures GBS. “And that’s a common problem: Clinicians think that they’re going to give somebody IVIg, and the patient’s going to get better immediately.” When that doesn’t happen, he said, physicians are tempted to give a second immunoglobulin dose.
However, a study published in 2021 shows that a second IVIg dose does not result in faster or better improvement – only in a significant risk of cardiovascular, cerebrovascular, and other thrombotic events 3 weeks later.8 Dr. Lunn noted that, although adverse-event data were “buried” in the supplemental materials of that study, the high cost of IVIg (approximately $12,500 per dose) means that the study has changed practice for the benefit of patients, providers, and health care systems.
COVID-19 and GBS triggers
Campylobacter jejuni infection still accounts for 30% to 40% of GBS cases, followed by other bacteria, including Mycoplasma pneumoniae and Haemophilus influenzae, and then by viruses, including cytomegalovirus and, rarely, human immunodeficiency virus. In recent years, severe acute respiratory syndrome coronavirus (SARS-CoV-2) infection – COVID-19 – and vaccines against the viral infection have captured headlines for purportedly being a cause of GBS.
The Zika virus epidemic of 2015-2016 has been linked to GBS-like illness. The 2003 severe acute respiratory syndrome (SARS) pandemic and the Middle East respiratory syndrome coronavirus (MERS-CoV) epidemic were associated with GBS – although, taken together, SARS and MERS-CoV produced fewer than 10 cases of GBS, Dr. Lunn noted. Nevertheless, heightened awareness of these viruses fueled hypervigilance regarding the prospect that COVID-19 could cause GBS. Following reports of a single such case in Wuhan and hundreds in Italy, worry over pandemic GBS grew worldwide.
Dr. Lunn and colleagues addressed the COVID-19–GBS question in a 2023 publication.9 “Because GBS is largely treated only with IVIg, and IVIg costs a lot of money, and the U.K. government insists on every dose of IVIg being logged in a government database, we were able to identify virtually every case of GBS,” he said.
GBS diagnoses were reliable, he added, because each case was confirmed by physicians outside the emergency department. Analysis revealed that, in 2020, U.K. GBS cases actually declined by around one-third. “And even when there was a second wave of COVID-19 at the end of 2020, partly caused by better counting,” Dr. Lunn said, “there was no further increase in GBS cases. We concluded that there was no link between GBS and COVID-19, as the cases simply didn’t appear.”
The foregoing findings have since been corroborated by studies in Singapore, the United States, and South America, he pointed out. Earlier case series suggesting a link between COVID-19 and GBS were selective, Dr. Lunn added, with numbers too small to support robust conclusions.
The lack of a causal link between COVID-19 and GBS suggested to Dr. Lunn that there was no reason COVID-19 vaccination should cause GBS. All COVID-19 vaccines were designed to provoke an immune response either (1) by producing the SARS-CoV-2 spike protein on the surface of virus (through a replication-incompetent adenoviral vector) or (2) through DNA or mRNA transcription, he explained. “The spike protein is only a small part of COVID-19.”
GBS: ‘Adverse event of interest’
A link between modern vaccines and GBS first appeared in the 1970s with the hastily developed swine flu vaccine. “In late 1976,” Dr. Lunn explained, “it was identified that patients who were given that vaccine seemed to be developing illnesses consistent with GBS.” By 1980, Dr. Lunn said, the risk level was determined to be only five or six cases for every 1 million doses of vaccine administered. “But the vaccine program was aborted, and swine flu never really happened.” Every year since, “there has been a surveillance program looking at the occurrence of an association of GBS with influenza vaccine.”
Minor fluctuations aside, he said, the overall incidence of GBS with influenza vaccination – 1 GBS case for every 1 million vaccine doses given – has remained consistent over several decades. “Nevertheless, GBS became an adverse event of special interest for any vaccination campaign.”
COVID-19 vaccination. Dr. Lunn and colleagues used the United Kingdom National Health Service (NHS) National Immunoglobulin Database, and other databases, to pinpoint the risk of GBS presented by the first dose of the AstraZeneca ChAdOx1 nCoV-19 adenoviral vaccine.10 As with U.K. GBS cases, every COVID-19 vaccination is linked to an NHS number. “We identified all the cases of GBS, found their NHS numbers, and went back and found the exact dates they’d been vaccinated, and with which vaccine.” Only the adenoviral-vector vaccine carried an excess risk of GBS – 5.8 cases for every 1 million doses, associated only with the first dose and peaking at approximately 25 days post vaccination – compared with other vaccines used in the United Kingdom.
Researchers looked at data from the Vaccine Adverse Event Reporting System (VAERS), a program of the Centers for Disease Control and Prevention and the Food and Drug Administration, encompassing nearly 500 million COVID-19 vaccine doses given between December 2020 and January 2022. They found that patients who received the Ad26.COV2.S vaccine (Janssen/Johnson & Johnson) had a rate of GBS (within 21 and 41 days post vaccination) that was 9 and 12 times higher, respectively, than corresponding rates for the mRNA-1273 (Moderna) and BNT162b2 (Pfizer BioNTech) COVID-19 vaccines.11 Risk was distributed relatively evenly by gender and age. Also at day 21 and day 41, observed event ratios with the adenoviral-vector vaccine (use of which has been suspended in the United States) were 3.79 and 2.34, respectively. Observed-event ratios with the other vaccines mirrored expected background rates.
The VAERS analysis confirms earlier data from the CDC’s Vaccine Safety Datalink, which showed that, among approximately 15 million U.S. vaccine doses given between mid-December 2020 and mid-November 2021, the unadjusted GBS incidence rate for every 100,000 person-years for the adenoviral vaccine, 21 days post exposure, was 32.4, compared with 1.3 for the mRNA vaccine. The adjusted relative risk with the adenoviral vaccine in the first 3 weeks post vaccination, compared to the 3- to 6-week interval post vaccination, was 6.03.12 In addition, a head-to-head comparison of adenoviral versus mRNA vaccines at 21 days revealed an adjusted rate ratio of 20.56. Mechanistically, some experts theorize that antibodies induced by the Janssen vaccine might cross-react with glycoproteins on the myelin sheath of peripheral nerve axons to cause GBS, but this remains unproven.11
The AstraZeneca vaccine uses a chimpanzee adenovirus; the Janssen vaccine uses a human adenoviral carrier. “The only commonality between the Janssen/Johnson & Johnson and AstraZeneca vaccines, and the only thing that’s different from the other vaccines, is the adenoviral vector packaging,” Dr. Lunn emphasized. “I believe it’s what generates GBS after COVID-19 vaccination. It has nothing to do with the COVID-19 vaccination, the spike protein, the nucleic acid, the DNA, or anything else.”
The adenoviral vector probably also explains why GBS peaks during winter, said Dr. Lunn. “That’s when adenovirus is circulating.” When people contract the common cold, he explained, they don’t visit their family physician and request a swab to isolate the adenovirus. “By the time you get GBS, the adenovirus has been cleared. We’ve all got antibodies to adenovirus all over the place, anyway, because we get it so often.”
It would be difficult to prove conclusively that adenovirus belongs on the list of GBS causes, Dr. Lunn allowed. “But I have a strong suspicion that it does. COVID-19 and COVID-19 vaccination have given us some new avenues into identifying GBS causation potentially in the near future.” More research is needed in this area, he said.
Dr. Lunn has been a principal investigator for argenx (efgartigimod) and an adviser to AstraZeneca (ChAdOx1 nCoV-19). He has received travel grants from CSL Behring.
References
1. Ho TW et al. Guillain-Barré syndrome in northern China. Relationship to Campylobacter jejuni infection and anti-glycolipid antibodies. Brain. 1995;118(Pt 3):597-605. doi: 10.1093/brain/118.3.597.
2. Uncini A. A common mechanism and a new categorization for anti-ganglioside antibody-mediated neuropathies. Exp Neurol. 2012;235(2):513-6. doi: 10.1016/j.expneurol.2012.03.023.
3. Uncini A and Kuwabara S. The electrodiagnosis of Guillain-Barré syndrome subtypes: where do we stand? Clin Neurophysiol. 2018;129(12):2586-93. doi: 10.1016/j.clinph.2018.09.025.
4. Delmont E et al. Autoantibodies to nodal isoforms of neurofascin in chronic inflammatory demyelinating polyneuropathy. Brain. 2017;140(7):1851-8. doi: 10.1093/brain/awx124.
5. McGonigal R et al. Anti-GD1a antibodies activate complement and calpain to injure distal motor nodes of Ranvier in mice. Brain. 2010;133(Pt 7):1944-60. doi: 10.1093/brain/awq119.
6. Cunningham ME et al. Real time imaging of intra-axonal calcium flux in an explant mouse model of axonal Guillain-Barré syndrome. Exp Neurol. 2022 Sep;355:114127. doi: 10.1016/j.expneurol.2022.114127.
7. Misawa S et al; Japanese Eculizumab Trial for GBS (JET-GBS) Study Group. Safety and efficacy of eculizumab in Guillain-Barré syndrome: a multicentre, double-blind, randomised phase 2 trial. Lancet Neurol. 2018;17(6):519-29. doi: 10.1016/S1474-4422(18)30114-5.
8. Walgaard C et al; Dutch GBS Study Group. Second intravenous immunoglobulin dose in patients with Guillain-Barré syndrome with poor prognosis (SID-GBS): a double-blind, randomised, placebo-controlled trial. Lancet Neurol. 2021;20(4):275-83. doi: 10.1016/S1474-4422(20)30494-4.
9. Keddie S et al. Epidemiological and cohort study finds no association between COVID-19 and Guillain-Barré syndrome. Brain. 2021;144(2):682-93. doi: 10.1093/brain/awaa433.
10. Keh RYS et al; BPNS/ABN COVID-19 Vaccine GBS Study Group. COVID-19 vaccination and Guillain-Barré syndrome: Analyses using the National Immunoglobulin Database. Brain. 2023;146(2):739-48. doi: 10.1093/brain/awac067.
11. Abara WE et al. Reports of Guillain-Barré syndrome after COVID-19 vaccination in the United States. JAMA Netw Open. 2023;6(2):e2253845. doi: 10.1001/jamanetworkopen.2022.53845.
12. Hanson KE et al. Incidence of Guillain-Barré syndrome after COVID-19 vaccination in the Vaccine Safety Datalink. JAMA Netw Open. 2022;5(4):e228879. doi: 10.1001/jamanetworkopen.2022.8879.
Advances in testing and therapeutics are improving the lives of patients with Fabry disease
Earlier diagnostic screening, routine and emerging therapies, and increased awareness are helping people with the lysosomal storage disorder Fabry disease lead longer, healthier lives. Because Fabry disease is rare, however, it can be misdiagnosed and treated incorrectly – for years and by various providers – while the patient’s health declines.
Four Fabry disease experts shared their perspectives, and recommendations, with Neurology Reviews 2023 Rare Neurological Disease Special Report.
What is Fabry disease?
Fabry disease is an X-linked lysosomal storage disorder caused by mutations in the galactosidase alpha (GLA) gene that causes reduced or absent alpha-galactosidase A (alpha-Gal A) enzyme activity. As a result, globotriaosylceramide (Gb3) accumulates, leading to cell, tissue, and organ damage in a range of systems. People with Fabry disease can develop progressive renal and cardiovascular dysfunction, neuropathy, and psychiatric disorders. They can experience cerebrovascular events; have eye, skin, gastrointestinal, and neuro-otologic involvement; and die prematurely.
Estimates of Fabry disease prevalence in the general population range from approximately 1 in 40,000 to 1 in 117,000 people. As an X-linked disorder, Fabry disease has been considered a disease mainly of males; however, affected females who are heterozygous for GLA mutations can remain asymptomatic through a normal lifespan or be as severely affected as a male would be.
Generally speaking, for every Fabry patient whose disease is diagnosed, there are five undiagnosed family members. Fabry disease affects future generations: Many patients are in their reproductive years; they want to have children and are therefore concerned about passing down the disease.
Symptoms of classic Fabry disease tend to appear during childhood or adolescence, often, and as early as 2 years of age, as acroparesthesias that intensify over time. In late-onset Fabry disease, symptoms might begin with renal failure or heart disease in the patient’s 30s, or later.
“Patients with classic Fabry disease commonly complain of acroparesthesias or whole-body pain,” said Anjay Rastogi, MD, PhD, professor of clinical medicine, clinical chief of nephrology, and director of the Fabry Disease Program at UCLA Health, Los Angeles. “With neuropathic pain, drugs like nonsteroidal anti-inflammatory drugs will probably not lessen the pain and might cause further cardiovascular, kidney, and other problems. So much of this pain is controlled by medications that are specific for nerves, including phenytoin, carbamazepine, and gabapentin.”
How do patients with Fabry disease typically present?
“Typically, with classic Fabry, young men visit the neurologist in their teenage years or later due to acroparesthesias – burning and tingling of the hands and feet,” further explained Gerald Vincent Raymond, MD, professor of genetic medicine and neurology and director of the Lysosomal Storage Disease Center at Johns Hopkins Medicine in Baltimore. “Sometimes they come to the attention of neurologists as 20- to 30-year-old men with strokes.
“These patients often undergo a long diagnostic odyssey of being misdiagnosed and treated incorrectly,” Dr. Raymond said. “Only years later, when they develop renal disease, cardiomyopathy, throw emboli, or have large- and small-vessel strokes, does a provider connect the dots.
“Neurologists should consider Fabry disease with any young patient with stroke, history of cardiomyopathy, renal disease, small-fiber peripheral neuropathy, tinnitus, hearing loss, unusual corneal whorls, or gastrointestinal issues. Because Fabry is an X-linked disease, women are usually less affected, but women can have the full manifestations of this disease.”
Who oversees the care of patients with Fabry disease?
“As a multisystem disease, Fabry disease must be managed by a multidisciplinary team, including genetics, neurology, nephrology, cardiology, psychiatry, ophthalmology, and otolaryngology,” explained Lizbeth Mellin, MD, assistant professor of pediatrics and clinical geneticist at University of Florida Health Jacksonville.
At what point does a neurologist encounter patients with Fabry disease? “Patients with Fabry disease are usually treated by rheumatologists and other specialists before they find a neurologist,” Dr. Mellin said. “Or they may see the neurologist for transient ischemic attacks or stroke, or for treatment of headaches, vascular dementia, dizziness or vertigo, hearing loss, seizures, hemiplegia, or aphasia.
“Almost 80% of adults with Fabry disease have distal neuropathic pain characterized by acroparesthesias and sensory loss starting in the palms of the hands or the soles of the feet, spreading to the entire body, and lasting for hours or days.
Dr. Mellin continued: “Neurologists play a critical role in treating manifestations such as neuropathic pain, stroke, and seizure. Without a current curative treatment for Fabry disease, the goals of its management are focused on treating manifestations and maintaining organ function, optimizing quality of life, and preserving life expectancy.”
What role does the neurologist play in ongoing management of Fabry disease? “Neurologists are involved in primary and secondary stroke prevention and pain management,” Dr. Rastogi explained, “and in diagnosing possible Fabry disease when they find cryptogenic stroke, especially in younger patients; when screening family members; and when reaching out to other appropriate Fabry providers.
“Primary care providers, geneticists, and, sometimes, nephrologists may manage the patient’s overall care. We send our patients to neurologists to evaluate and manage neuropathic pain, stroke, white-matter lesions, and cerebrovascular disease. After a stroke, a support team cares for the patient and manages the rehab.
“Neurologists tend to have organ-specific involvement, and they may treat pain. They may have their first encounter with the patient when they do nerve testing, brain scans, or other tests, or when they diagnose nervous system problems that they may continue to treat.”
How does the role of the neurologist complement others on the interdisciplinary care team? “Fabry requires management by specialists familiar with the multiple aspects of the disorder,” Dr. Raymond said. “As a geneticist and neurologist, I care for a broad portfolio of lysosomal storage diseases. Usually, a metabolic genetics center or a Fabry center will handle the therapy. Fabry requires a multidisciplinary approach, and someone needs to be quarterbacking the patient’s overall management.”
“Teamwork is about patient well-being and empowerment,” Dr. Mellin pointed out. “Patients with Fabry disease require multidisciplinary care to reduce their morbidity and improve their health-related quality of life. Early diagnosis and treatment are critical to preventing irreversible organ damage and failure. Patients with stroke are usually evaluated in a hospital setting. To protect major organs from progressive damage, the differential diagnosis must include Fabry disease.”
“It’s important to provide coordinated care to the entire patient, not only the affected organ,” Dr. Rastogi pointed out. “Taking care of patients with Fabry disease is difficult, complicated, and time-consuming. Academic programs have various specialties under the same umbrella, so it’s easier to coordinate care than in private practice. In private practice, the neurologist needs to reach out to other specialists to coordinate care.
“An interdisciplinary team approach, with integrative care in which the team members communicate with each other, is very important. The team may include geneticists, pediatricians, nephrologists, cardiologists, neurologists, gastroenterologists, and a pain management team that may use biofeedback and other non-opioid approaches. The interdisciplinary UCLA Fabry Disease Program addresses almost every aspect of Fabry. As a nephrologist, I oversee the entire care of the patient, not just the kidneys.
“Some medical practices may have only three to five patients, with a geneticist leading the care team. In others, the primary care physician oversees and coordinates care with a neurologist, nephrologist, cardiologist, pain specialist, and other specialists. Patients are often anxious and depressed, so a psychologist and psychiatrist should also be involved.
“A neurologist who diagnoses a patient with Fabry disease should contact their local Fabry disease experts. If none are available, they should refer their patients to geneticists to oversee their care. At-risk family members also need to be screened.”
Monroe Carell Jr. Children’s Hospital at Vanderbilt, in Nashville, Tenn., has a multidisciplinary Fabry Disease Clinic with specialists in genetics, neurology, and cardiology. Chelsea J. Lauderdale, DNP, MPH, APRN, CPNP-PC, in the division of medical genetics and genomic medicine, helps screen and diagnose patients with Fabry disease.
“A nurse practitioner in this setting may work closely with newborn screening and be involved in infant and adult diagnosis,” Ms. Lauderdale said. “They may identify the onset of new symptoms and aid specialists in their evaluations. Nurse practitioners may be involved throughout Fabry disease patients’ care, monitoring labs, ensuring they are treated by the appropriate specialists, and initiating treatment when indicated.”
What recent research and advances should neurologists be aware of?
Diagnostics. Tests for Fabry disease now include an enzyme assay to measure alpha-galactosidase activity in the blood of males and genetic testing in males and females to identify GLA mutations. Several states now test newborns for Fabry disease, enabling earlier diagnosis and treatment, Dr. Raymond said. Identifying Fabry disease in a boy by enzyme assay sometimes leads to identifying an uncle, a grandfather, or others in the family who have Fabry. Fabry is sometimes discovered from genetic panels to help diagnose peripheral neuropathy and from prenatal genetic testing.
“Genetic screening of at-risk family members, of any degree, in various generations, is important,” Dr. Rastogi emphasized, “so we construct a family tree to find everyone at risk. Genetic testing is much easier and more widespread than it was even 5 years ago. It’s more accessible and you don’t need to go through a geneticist to diagnose Fabry disease.
“Some patients first come to us for dialysis in their 40s or 50s, but people are being tested and treated at younger ages now, and we also have newborn screening. Genetic testing for Fabry is not common, but in several states, every newborn is tested for Fabry. And, if parents have Fabry, we test their children.”
Therapeutics. “Available and emerging therapies make the field exciting,” Dr. Raymond said. “Some current gene therapy trials look promising, and preliminary evidence suggests that gene therapy may stabilize kidney and heart function.”
“Although Fabry disease does not have a cure,” Dr. Rastogi pointed out, “two treatments for Fabry disease appear to help prevent life-threatening complications: enzyme replacement therapy (ERT) and chaperone therapy.”
Replacing enzymes. “In Fabry disease, the enzyme alpha-galactosidase A is deficient,” Dr. Rastogi explained, “causing build-up of sphingolipids in blood vessels and tissues. ERT, a great advance that we’ve had for over 20 years, replenishes that deficiency. ERT has some challenges: It’s an infusion every 2 weeks for life, and it can have infusion reactions and other complications.
“Newer, second-generation, versions of ERT are being developed, including pegunigalsidase alfa (Elfabrio, Chiesi Global Rare Diseases, Protalix Biotherapeutics), recently approved by the U.S. Food and Drug Administration to treat adults with Fabry disease.”
Chaperone therapy. “The oral drug migalastat (Galafold, Fabrazyme) is a small-molecule chaperone therapy that stabilizes the faulty alpha-galactosidase A enzyme,” Dr. Rastogi explained. “It is easier to take, every other day for life, than [undergoing] infusion. Limitations include that it is available only to patients who have the amenable mutations, and whose estimated glomerular filtration rate is greater than 30 [mL/min/1.73 m2], and they may have some adverse events including nausea or vomiting.”
On the horizon: substrate reduction, gene therapy. “[These] are also exciting avenues of research,” said Dr. Rastogi. “Substrate reduction therapy aims to reduce glycosphingolipid accumulation, and lucerastat [Idorsia Pharmaceutical]1,2 and venglustat [Sanofi Genzyme]3,4 are in active clinical trials or trials that have been completed.
Gene therapy “delivers a healthy gene that helps the body produce a previously deficient enzyme,” Dr. Rastogi explained. “This is an early, very promising field in need of more research, with many challenges involving the vector and complications.
“While it is still too early to predict how effective gene therapy will be, research is encouraging. Another promising therapy is modulation of gene expression, which changes the activity of a gene.”
“Gene therapy may potentially offer an alternative to typical ERT, which some patients find burdensome,” Ms. Lauderdale added. “If a neurologist has a patient who may be a good candidate for a gene therapy clinical trial that is recruiting participants, I encourage them to learn more about the study and its requirements.”
Dr. Mellin concurred: “Several gene therapy clinical trials show promise, but further information and evidence are required.”
How might these advances affect the trajectory of Fabry disease?
“Untreated Fabry compromises quality of life and may shorten the lifespan,” Dr. Raymond said. “I’m aware of individuals and their family members who died in their 60s. In the past, individuals would develop renal failure, stroke, or cardiomyopathy before being diagnosed and treated, but now we can begin treating them earlier and head off those outcomes.
“We have many options, and their number is increasing. We now diagnose patients when they are younger and maybe presymptomatic, when therapies have much greater potential to ameliorate their lives.”
Dr. Raymond spoke hopefully: “With gene therapy, people with Fabry disease will no longer need enzyme replacement or chaperone therapy. Ultimately, if gene therapy proves to be as efficacious as we hope, without big downsides, we will, essentially, be curing Fabry.”
Concluding remarks
In summing up, the four experts quoted in this article offered the following observations and advice for neurologists:
Dr. Mellin. “Pain has a significant impact on quality of life for patients with Fabry disease. Identifying and adequately treating neuropathic pain can be life-changing.”
Ms. Lauderdale. “Reach out to geneticists and other appropriate specialists. We all need to communicate the needs of our patients to ensure they receive the best possible patient-centered care.”
Dr. Rastogi. “Fabry disease is an area of active research that can be a prototype for, and affect the outcomes of, other genetic disorders. I expect to see more centers of excellence for the study and treatment of Fabry disease.”
Dr. Raymond. “With therapies rapidly evolving, neurologists need to consider rare diseases and think about how to build them into their diagnostic schemes.”
Dr. Raymond, Dr. Mellin, and Ms. Lauderdale, have nothing to disclose. Dr. Rastogi discloses a financial relationship with several pharmaceutical and biopharmaceutical companies involved in Fabry disease therapeutics research and development, including Amicus Therapeutics, Chiesi Global Rare Diseases, Genzyme Sanofi, Sanofi S.A., Idorsia Pharmaceuticals Ltd., and Protalix Biotherapeutics.
Additional recommended reading
Beck M et al. Twenty years of the Fabry Outcome Survey (FOS): Insights, achievements, and lessons learned from a global patient registry. Orphanet J Rare Dis. 2022;17(1):238. doi: 10.1186/s13023-022-02392-9.
Beraza-Millor M et al. Novel golden lipid nanoparticles with small interference ribonucleic acid for substrate reduction therapy in Fabry disease. Pharmaceutics. 2023;15(7):1936. doi: 10.3390/pharmaceutics15071936.
Ezgu F et al. Expert opinion on the recognition, diagnosis and management of children and adults with Fabry disease: A multidisciplinary Turkey perspective. Orphanet J Rare Dis. 2022;17(1):90. doi: 10.1186/s13023-022-02215-x.
Fabry disease registry & pregnancy sub-registry. ClinicalTrials.gov Identifier: NCT00196742. Updated July 13, 2023. Accessed Sept. 13, 2023. https://www.clinicaltrials.gov/study/NCT00196742?term=Fabry%20Disease%20Registry%20%26%20Pregnancy%20Sub-registry&rank=1.
Umer M and Kalra DK. Treatment of Fabry disease: established and emerging therapies. Pharmaceuticals. 2023;16(2):320. doi: 10.3390/ph16020320.
Weidemann F et al. Chaperone therapy in Fabry disease. Int J Mol Sci. 2022;23(3):1887. doi: 10.3390/ijms23031887.
References
1. Efficacy and safety of lucerastat oral monotherapy in adult subjects with Fabry disease (MODIFY). ClinicalTrials.gov Identifier: NCT03425539. Updated Aug. 9, 2022. Accessed Sept. 18, 2023. https://www.clinicaltrials.gov/study/NCT03425539?term=NCT03425539&rank=1.
2. A study to evaluate the long-term safety and tolerability of lucerastat in adult subjects with Fabry disease. ClinicalTrials.gov Identifier: NCT03737214. Updated Aug. 16, 2023. Accessed Sept. 18, 2023. https://www.clinicaltrials.gov/study/NCT03737214?term=NCT03737214&rank=1.
3. Evaluate the safety, pharmacodynamics, pharmacokinetics, and exploratory efficacy of GZ/SAR402671 in treatment-naive adult male patients with Fabry disease. ClinicalTrials.gov Identifier: NCT02228460. Updated Dec. 17, 2019. Accessed Sept. 18, 2023. https://www.clinicaltrials.gov/study/NCT02228460?term=NCT02228460&rank=1.
4. Evaluation of the long-term safety, pharmacodynamics, and exploratory efficacy of GZ/SAR402671 in treatment-naive adult male patients with Fabry disease. ClinicalTrials.gov Identifier: NCT02489344. Updated March 23, 2023. Accessed Sept. 18, 2023. https://www.clinicaltrials.gov/study/NCT02489344?term=NC
Earlier diagnostic screening, routine and emerging therapies, and increased awareness are helping people with the lysosomal storage disorder Fabry disease lead longer, healthier lives. Because Fabry disease is rare, however, it can be misdiagnosed and treated incorrectly – for years and by various providers – while the patient’s health declines.
Four Fabry disease experts shared their perspectives, and recommendations, with Neurology Reviews 2023 Rare Neurological Disease Special Report.
What is Fabry disease?
Fabry disease is an X-linked lysosomal storage disorder caused by mutations in the galactosidase alpha (GLA) gene that causes reduced or absent alpha-galactosidase A (alpha-Gal A) enzyme activity. As a result, globotriaosylceramide (Gb3) accumulates, leading to cell, tissue, and organ damage in a range of systems. People with Fabry disease can develop progressive renal and cardiovascular dysfunction, neuropathy, and psychiatric disorders. They can experience cerebrovascular events; have eye, skin, gastrointestinal, and neuro-otologic involvement; and die prematurely.
Estimates of Fabry disease prevalence in the general population range from approximately 1 in 40,000 to 1 in 117,000 people. As an X-linked disorder, Fabry disease has been considered a disease mainly of males; however, affected females who are heterozygous for GLA mutations can remain asymptomatic through a normal lifespan or be as severely affected as a male would be.
Generally speaking, for every Fabry patient whose disease is diagnosed, there are five undiagnosed family members. Fabry disease affects future generations: Many patients are in their reproductive years; they want to have children and are therefore concerned about passing down the disease.
Symptoms of classic Fabry disease tend to appear during childhood or adolescence, often, and as early as 2 years of age, as acroparesthesias that intensify over time. In late-onset Fabry disease, symptoms might begin with renal failure or heart disease in the patient’s 30s, or later.
“Patients with classic Fabry disease commonly complain of acroparesthesias or whole-body pain,” said Anjay Rastogi, MD, PhD, professor of clinical medicine, clinical chief of nephrology, and director of the Fabry Disease Program at UCLA Health, Los Angeles. “With neuropathic pain, drugs like nonsteroidal anti-inflammatory drugs will probably not lessen the pain and might cause further cardiovascular, kidney, and other problems. So much of this pain is controlled by medications that are specific for nerves, including phenytoin, carbamazepine, and gabapentin.”
How do patients with Fabry disease typically present?
“Typically, with classic Fabry, young men visit the neurologist in their teenage years or later due to acroparesthesias – burning and tingling of the hands and feet,” further explained Gerald Vincent Raymond, MD, professor of genetic medicine and neurology and director of the Lysosomal Storage Disease Center at Johns Hopkins Medicine in Baltimore. “Sometimes they come to the attention of neurologists as 20- to 30-year-old men with strokes.
“These patients often undergo a long diagnostic odyssey of being misdiagnosed and treated incorrectly,” Dr. Raymond said. “Only years later, when they develop renal disease, cardiomyopathy, throw emboli, or have large- and small-vessel strokes, does a provider connect the dots.
“Neurologists should consider Fabry disease with any young patient with stroke, history of cardiomyopathy, renal disease, small-fiber peripheral neuropathy, tinnitus, hearing loss, unusual corneal whorls, or gastrointestinal issues. Because Fabry is an X-linked disease, women are usually less affected, but women can have the full manifestations of this disease.”
Who oversees the care of patients with Fabry disease?
“As a multisystem disease, Fabry disease must be managed by a multidisciplinary team, including genetics, neurology, nephrology, cardiology, psychiatry, ophthalmology, and otolaryngology,” explained Lizbeth Mellin, MD, assistant professor of pediatrics and clinical geneticist at University of Florida Health Jacksonville.
At what point does a neurologist encounter patients with Fabry disease? “Patients with Fabry disease are usually treated by rheumatologists and other specialists before they find a neurologist,” Dr. Mellin said. “Or they may see the neurologist for transient ischemic attacks or stroke, or for treatment of headaches, vascular dementia, dizziness or vertigo, hearing loss, seizures, hemiplegia, or aphasia.
“Almost 80% of adults with Fabry disease have distal neuropathic pain characterized by acroparesthesias and sensory loss starting in the palms of the hands or the soles of the feet, spreading to the entire body, and lasting for hours or days.
Dr. Mellin continued: “Neurologists play a critical role in treating manifestations such as neuropathic pain, stroke, and seizure. Without a current curative treatment for Fabry disease, the goals of its management are focused on treating manifestations and maintaining organ function, optimizing quality of life, and preserving life expectancy.”
What role does the neurologist play in ongoing management of Fabry disease? “Neurologists are involved in primary and secondary stroke prevention and pain management,” Dr. Rastogi explained, “and in diagnosing possible Fabry disease when they find cryptogenic stroke, especially in younger patients; when screening family members; and when reaching out to other appropriate Fabry providers.
“Primary care providers, geneticists, and, sometimes, nephrologists may manage the patient’s overall care. We send our patients to neurologists to evaluate and manage neuropathic pain, stroke, white-matter lesions, and cerebrovascular disease. After a stroke, a support team cares for the patient and manages the rehab.
“Neurologists tend to have organ-specific involvement, and they may treat pain. They may have their first encounter with the patient when they do nerve testing, brain scans, or other tests, or when they diagnose nervous system problems that they may continue to treat.”
How does the role of the neurologist complement others on the interdisciplinary care team? “Fabry requires management by specialists familiar with the multiple aspects of the disorder,” Dr. Raymond said. “As a geneticist and neurologist, I care for a broad portfolio of lysosomal storage diseases. Usually, a metabolic genetics center or a Fabry center will handle the therapy. Fabry requires a multidisciplinary approach, and someone needs to be quarterbacking the patient’s overall management.”
“Teamwork is about patient well-being and empowerment,” Dr. Mellin pointed out. “Patients with Fabry disease require multidisciplinary care to reduce their morbidity and improve their health-related quality of life. Early diagnosis and treatment are critical to preventing irreversible organ damage and failure. Patients with stroke are usually evaluated in a hospital setting. To protect major organs from progressive damage, the differential diagnosis must include Fabry disease.”
“It’s important to provide coordinated care to the entire patient, not only the affected organ,” Dr. Rastogi pointed out. “Taking care of patients with Fabry disease is difficult, complicated, and time-consuming. Academic programs have various specialties under the same umbrella, so it’s easier to coordinate care than in private practice. In private practice, the neurologist needs to reach out to other specialists to coordinate care.
“An interdisciplinary team approach, with integrative care in which the team members communicate with each other, is very important. The team may include geneticists, pediatricians, nephrologists, cardiologists, neurologists, gastroenterologists, and a pain management team that may use biofeedback and other non-opioid approaches. The interdisciplinary UCLA Fabry Disease Program addresses almost every aspect of Fabry. As a nephrologist, I oversee the entire care of the patient, not just the kidneys.
“Some medical practices may have only three to five patients, with a geneticist leading the care team. In others, the primary care physician oversees and coordinates care with a neurologist, nephrologist, cardiologist, pain specialist, and other specialists. Patients are often anxious and depressed, so a psychologist and psychiatrist should also be involved.
“A neurologist who diagnoses a patient with Fabry disease should contact their local Fabry disease experts. If none are available, they should refer their patients to geneticists to oversee their care. At-risk family members also need to be screened.”
Monroe Carell Jr. Children’s Hospital at Vanderbilt, in Nashville, Tenn., has a multidisciplinary Fabry Disease Clinic with specialists in genetics, neurology, and cardiology. Chelsea J. Lauderdale, DNP, MPH, APRN, CPNP-PC, in the division of medical genetics and genomic medicine, helps screen and diagnose patients with Fabry disease.
“A nurse practitioner in this setting may work closely with newborn screening and be involved in infant and adult diagnosis,” Ms. Lauderdale said. “They may identify the onset of new symptoms and aid specialists in their evaluations. Nurse practitioners may be involved throughout Fabry disease patients’ care, monitoring labs, ensuring they are treated by the appropriate specialists, and initiating treatment when indicated.”
What recent research and advances should neurologists be aware of?
Diagnostics. Tests for Fabry disease now include an enzyme assay to measure alpha-galactosidase activity in the blood of males and genetic testing in males and females to identify GLA mutations. Several states now test newborns for Fabry disease, enabling earlier diagnosis and treatment, Dr. Raymond said. Identifying Fabry disease in a boy by enzyme assay sometimes leads to identifying an uncle, a grandfather, or others in the family who have Fabry. Fabry is sometimes discovered from genetic panels to help diagnose peripheral neuropathy and from prenatal genetic testing.
“Genetic screening of at-risk family members, of any degree, in various generations, is important,” Dr. Rastogi emphasized, “so we construct a family tree to find everyone at risk. Genetic testing is much easier and more widespread than it was even 5 years ago. It’s more accessible and you don’t need to go through a geneticist to diagnose Fabry disease.
“Some patients first come to us for dialysis in their 40s or 50s, but people are being tested and treated at younger ages now, and we also have newborn screening. Genetic testing for Fabry is not common, but in several states, every newborn is tested for Fabry. And, if parents have Fabry, we test their children.”
Therapeutics. “Available and emerging therapies make the field exciting,” Dr. Raymond said. “Some current gene therapy trials look promising, and preliminary evidence suggests that gene therapy may stabilize kidney and heart function.”
“Although Fabry disease does not have a cure,” Dr. Rastogi pointed out, “two treatments for Fabry disease appear to help prevent life-threatening complications: enzyme replacement therapy (ERT) and chaperone therapy.”
Replacing enzymes. “In Fabry disease, the enzyme alpha-galactosidase A is deficient,” Dr. Rastogi explained, “causing build-up of sphingolipids in blood vessels and tissues. ERT, a great advance that we’ve had for over 20 years, replenishes that deficiency. ERT has some challenges: It’s an infusion every 2 weeks for life, and it can have infusion reactions and other complications.
“Newer, second-generation, versions of ERT are being developed, including pegunigalsidase alfa (Elfabrio, Chiesi Global Rare Diseases, Protalix Biotherapeutics), recently approved by the U.S. Food and Drug Administration to treat adults with Fabry disease.”
Chaperone therapy. “The oral drug migalastat (Galafold, Fabrazyme) is a small-molecule chaperone therapy that stabilizes the faulty alpha-galactosidase A enzyme,” Dr. Rastogi explained. “It is easier to take, every other day for life, than [undergoing] infusion. Limitations include that it is available only to patients who have the amenable mutations, and whose estimated glomerular filtration rate is greater than 30 [mL/min/1.73 m2], and they may have some adverse events including nausea or vomiting.”
On the horizon: substrate reduction, gene therapy. “[These] are also exciting avenues of research,” said Dr. Rastogi. “Substrate reduction therapy aims to reduce glycosphingolipid accumulation, and lucerastat [Idorsia Pharmaceutical]1,2 and venglustat [Sanofi Genzyme]3,4 are in active clinical trials or trials that have been completed.
Gene therapy “delivers a healthy gene that helps the body produce a previously deficient enzyme,” Dr. Rastogi explained. “This is an early, very promising field in need of more research, with many challenges involving the vector and complications.
“While it is still too early to predict how effective gene therapy will be, research is encouraging. Another promising therapy is modulation of gene expression, which changes the activity of a gene.”
“Gene therapy may potentially offer an alternative to typical ERT, which some patients find burdensome,” Ms. Lauderdale added. “If a neurologist has a patient who may be a good candidate for a gene therapy clinical trial that is recruiting participants, I encourage them to learn more about the study and its requirements.”
Dr. Mellin concurred: “Several gene therapy clinical trials show promise, but further information and evidence are required.”
How might these advances affect the trajectory of Fabry disease?
“Untreated Fabry compromises quality of life and may shorten the lifespan,” Dr. Raymond said. “I’m aware of individuals and their family members who died in their 60s. In the past, individuals would develop renal failure, stroke, or cardiomyopathy before being diagnosed and treated, but now we can begin treating them earlier and head off those outcomes.
“We have many options, and their number is increasing. We now diagnose patients when they are younger and maybe presymptomatic, when therapies have much greater potential to ameliorate their lives.”
Dr. Raymond spoke hopefully: “With gene therapy, people with Fabry disease will no longer need enzyme replacement or chaperone therapy. Ultimately, if gene therapy proves to be as efficacious as we hope, without big downsides, we will, essentially, be curing Fabry.”
Concluding remarks
In summing up, the four experts quoted in this article offered the following observations and advice for neurologists:
Dr. Mellin. “Pain has a significant impact on quality of life for patients with Fabry disease. Identifying and adequately treating neuropathic pain can be life-changing.”
Ms. Lauderdale. “Reach out to geneticists and other appropriate specialists. We all need to communicate the needs of our patients to ensure they receive the best possible patient-centered care.”
Dr. Rastogi. “Fabry disease is an area of active research that can be a prototype for, and affect the outcomes of, other genetic disorders. I expect to see more centers of excellence for the study and treatment of Fabry disease.”
Dr. Raymond. “With therapies rapidly evolving, neurologists need to consider rare diseases and think about how to build them into their diagnostic schemes.”
Dr. Raymond, Dr. Mellin, and Ms. Lauderdale, have nothing to disclose. Dr. Rastogi discloses a financial relationship with several pharmaceutical and biopharmaceutical companies involved in Fabry disease therapeutics research and development, including Amicus Therapeutics, Chiesi Global Rare Diseases, Genzyme Sanofi, Sanofi S.A., Idorsia Pharmaceuticals Ltd., and Protalix Biotherapeutics.
Additional recommended reading
Beck M et al. Twenty years of the Fabry Outcome Survey (FOS): Insights, achievements, and lessons learned from a global patient registry. Orphanet J Rare Dis. 2022;17(1):238. doi: 10.1186/s13023-022-02392-9.
Beraza-Millor M et al. Novel golden lipid nanoparticles with small interference ribonucleic acid for substrate reduction therapy in Fabry disease. Pharmaceutics. 2023;15(7):1936. doi: 10.3390/pharmaceutics15071936.
Ezgu F et al. Expert opinion on the recognition, diagnosis and management of children and adults with Fabry disease: A multidisciplinary Turkey perspective. Orphanet J Rare Dis. 2022;17(1):90. doi: 10.1186/s13023-022-02215-x.
Fabry disease registry & pregnancy sub-registry. ClinicalTrials.gov Identifier: NCT00196742. Updated July 13, 2023. Accessed Sept. 13, 2023. https://www.clinicaltrials.gov/study/NCT00196742?term=Fabry%20Disease%20Registry%20%26%20Pregnancy%20Sub-registry&rank=1.
Umer M and Kalra DK. Treatment of Fabry disease: established and emerging therapies. Pharmaceuticals. 2023;16(2):320. doi: 10.3390/ph16020320.
Weidemann F et al. Chaperone therapy in Fabry disease. Int J Mol Sci. 2022;23(3):1887. doi: 10.3390/ijms23031887.
References
1. Efficacy and safety of lucerastat oral monotherapy in adult subjects with Fabry disease (MODIFY). ClinicalTrials.gov Identifier: NCT03425539. Updated Aug. 9, 2022. Accessed Sept. 18, 2023. https://www.clinicaltrials.gov/study/NCT03425539?term=NCT03425539&rank=1.
2. A study to evaluate the long-term safety and tolerability of lucerastat in adult subjects with Fabry disease. ClinicalTrials.gov Identifier: NCT03737214. Updated Aug. 16, 2023. Accessed Sept. 18, 2023. https://www.clinicaltrials.gov/study/NCT03737214?term=NCT03737214&rank=1.
3. Evaluate the safety, pharmacodynamics, pharmacokinetics, and exploratory efficacy of GZ/SAR402671 in treatment-naive adult male patients with Fabry disease. ClinicalTrials.gov Identifier: NCT02228460. Updated Dec. 17, 2019. Accessed Sept. 18, 2023. https://www.clinicaltrials.gov/study/NCT02228460?term=NCT02228460&rank=1.
4. Evaluation of the long-term safety, pharmacodynamics, and exploratory efficacy of GZ/SAR402671 in treatment-naive adult male patients with Fabry disease. ClinicalTrials.gov Identifier: NCT02489344. Updated March 23, 2023. Accessed Sept. 18, 2023. https://www.clinicaltrials.gov/study/NCT02489344?term=NC
Earlier diagnostic screening, routine and emerging therapies, and increased awareness are helping people with the lysosomal storage disorder Fabry disease lead longer, healthier lives. Because Fabry disease is rare, however, it can be misdiagnosed and treated incorrectly – for years and by various providers – while the patient’s health declines.
Four Fabry disease experts shared their perspectives, and recommendations, with Neurology Reviews 2023 Rare Neurological Disease Special Report.
What is Fabry disease?
Fabry disease is an X-linked lysosomal storage disorder caused by mutations in the galactosidase alpha (GLA) gene that causes reduced or absent alpha-galactosidase A (alpha-Gal A) enzyme activity. As a result, globotriaosylceramide (Gb3) accumulates, leading to cell, tissue, and organ damage in a range of systems. People with Fabry disease can develop progressive renal and cardiovascular dysfunction, neuropathy, and psychiatric disorders. They can experience cerebrovascular events; have eye, skin, gastrointestinal, and neuro-otologic involvement; and die prematurely.
Estimates of Fabry disease prevalence in the general population range from approximately 1 in 40,000 to 1 in 117,000 people. As an X-linked disorder, Fabry disease has been considered a disease mainly of males; however, affected females who are heterozygous for GLA mutations can remain asymptomatic through a normal lifespan or be as severely affected as a male would be.
Generally speaking, for every Fabry patient whose disease is diagnosed, there are five undiagnosed family members. Fabry disease affects future generations: Many patients are in their reproductive years; they want to have children and are therefore concerned about passing down the disease.
Symptoms of classic Fabry disease tend to appear during childhood or adolescence, often, and as early as 2 years of age, as acroparesthesias that intensify over time. In late-onset Fabry disease, symptoms might begin with renal failure or heart disease in the patient’s 30s, or later.
“Patients with classic Fabry disease commonly complain of acroparesthesias or whole-body pain,” said Anjay Rastogi, MD, PhD, professor of clinical medicine, clinical chief of nephrology, and director of the Fabry Disease Program at UCLA Health, Los Angeles. “With neuropathic pain, drugs like nonsteroidal anti-inflammatory drugs will probably not lessen the pain and might cause further cardiovascular, kidney, and other problems. So much of this pain is controlled by medications that are specific for nerves, including phenytoin, carbamazepine, and gabapentin.”
How do patients with Fabry disease typically present?
“Typically, with classic Fabry, young men visit the neurologist in their teenage years or later due to acroparesthesias – burning and tingling of the hands and feet,” further explained Gerald Vincent Raymond, MD, professor of genetic medicine and neurology and director of the Lysosomal Storage Disease Center at Johns Hopkins Medicine in Baltimore. “Sometimes they come to the attention of neurologists as 20- to 30-year-old men with strokes.
“These patients often undergo a long diagnostic odyssey of being misdiagnosed and treated incorrectly,” Dr. Raymond said. “Only years later, when they develop renal disease, cardiomyopathy, throw emboli, or have large- and small-vessel strokes, does a provider connect the dots.
“Neurologists should consider Fabry disease with any young patient with stroke, history of cardiomyopathy, renal disease, small-fiber peripheral neuropathy, tinnitus, hearing loss, unusual corneal whorls, or gastrointestinal issues. Because Fabry is an X-linked disease, women are usually less affected, but women can have the full manifestations of this disease.”
Who oversees the care of patients with Fabry disease?
“As a multisystem disease, Fabry disease must be managed by a multidisciplinary team, including genetics, neurology, nephrology, cardiology, psychiatry, ophthalmology, and otolaryngology,” explained Lizbeth Mellin, MD, assistant professor of pediatrics and clinical geneticist at University of Florida Health Jacksonville.
At what point does a neurologist encounter patients with Fabry disease? “Patients with Fabry disease are usually treated by rheumatologists and other specialists before they find a neurologist,” Dr. Mellin said. “Or they may see the neurologist for transient ischemic attacks or stroke, or for treatment of headaches, vascular dementia, dizziness or vertigo, hearing loss, seizures, hemiplegia, or aphasia.
“Almost 80% of adults with Fabry disease have distal neuropathic pain characterized by acroparesthesias and sensory loss starting in the palms of the hands or the soles of the feet, spreading to the entire body, and lasting for hours or days.
Dr. Mellin continued: “Neurologists play a critical role in treating manifestations such as neuropathic pain, stroke, and seizure. Without a current curative treatment for Fabry disease, the goals of its management are focused on treating manifestations and maintaining organ function, optimizing quality of life, and preserving life expectancy.”
What role does the neurologist play in ongoing management of Fabry disease? “Neurologists are involved in primary and secondary stroke prevention and pain management,” Dr. Rastogi explained, “and in diagnosing possible Fabry disease when they find cryptogenic stroke, especially in younger patients; when screening family members; and when reaching out to other appropriate Fabry providers.
“Primary care providers, geneticists, and, sometimes, nephrologists may manage the patient’s overall care. We send our patients to neurologists to evaluate and manage neuropathic pain, stroke, white-matter lesions, and cerebrovascular disease. After a stroke, a support team cares for the patient and manages the rehab.
“Neurologists tend to have organ-specific involvement, and they may treat pain. They may have their first encounter with the patient when they do nerve testing, brain scans, or other tests, or when they diagnose nervous system problems that they may continue to treat.”
How does the role of the neurologist complement others on the interdisciplinary care team? “Fabry requires management by specialists familiar with the multiple aspects of the disorder,” Dr. Raymond said. “As a geneticist and neurologist, I care for a broad portfolio of lysosomal storage diseases. Usually, a metabolic genetics center or a Fabry center will handle the therapy. Fabry requires a multidisciplinary approach, and someone needs to be quarterbacking the patient’s overall management.”
“Teamwork is about patient well-being and empowerment,” Dr. Mellin pointed out. “Patients with Fabry disease require multidisciplinary care to reduce their morbidity and improve their health-related quality of life. Early diagnosis and treatment are critical to preventing irreversible organ damage and failure. Patients with stroke are usually evaluated in a hospital setting. To protect major organs from progressive damage, the differential diagnosis must include Fabry disease.”
“It’s important to provide coordinated care to the entire patient, not only the affected organ,” Dr. Rastogi pointed out. “Taking care of patients with Fabry disease is difficult, complicated, and time-consuming. Academic programs have various specialties under the same umbrella, so it’s easier to coordinate care than in private practice. In private practice, the neurologist needs to reach out to other specialists to coordinate care.
“An interdisciplinary team approach, with integrative care in which the team members communicate with each other, is very important. The team may include geneticists, pediatricians, nephrologists, cardiologists, neurologists, gastroenterologists, and a pain management team that may use biofeedback and other non-opioid approaches. The interdisciplinary UCLA Fabry Disease Program addresses almost every aspect of Fabry. As a nephrologist, I oversee the entire care of the patient, not just the kidneys.
“Some medical practices may have only three to five patients, with a geneticist leading the care team. In others, the primary care physician oversees and coordinates care with a neurologist, nephrologist, cardiologist, pain specialist, and other specialists. Patients are often anxious and depressed, so a psychologist and psychiatrist should also be involved.
“A neurologist who diagnoses a patient with Fabry disease should contact their local Fabry disease experts. If none are available, they should refer their patients to geneticists to oversee their care. At-risk family members also need to be screened.”
Monroe Carell Jr. Children’s Hospital at Vanderbilt, in Nashville, Tenn., has a multidisciplinary Fabry Disease Clinic with specialists in genetics, neurology, and cardiology. Chelsea J. Lauderdale, DNP, MPH, APRN, CPNP-PC, in the division of medical genetics and genomic medicine, helps screen and diagnose patients with Fabry disease.
“A nurse practitioner in this setting may work closely with newborn screening and be involved in infant and adult diagnosis,” Ms. Lauderdale said. “They may identify the onset of new symptoms and aid specialists in their evaluations. Nurse practitioners may be involved throughout Fabry disease patients’ care, monitoring labs, ensuring they are treated by the appropriate specialists, and initiating treatment when indicated.”
What recent research and advances should neurologists be aware of?
Diagnostics. Tests for Fabry disease now include an enzyme assay to measure alpha-galactosidase activity in the blood of males and genetic testing in males and females to identify GLA mutations. Several states now test newborns for Fabry disease, enabling earlier diagnosis and treatment, Dr. Raymond said. Identifying Fabry disease in a boy by enzyme assay sometimes leads to identifying an uncle, a grandfather, or others in the family who have Fabry. Fabry is sometimes discovered from genetic panels to help diagnose peripheral neuropathy and from prenatal genetic testing.
“Genetic screening of at-risk family members, of any degree, in various generations, is important,” Dr. Rastogi emphasized, “so we construct a family tree to find everyone at risk. Genetic testing is much easier and more widespread than it was even 5 years ago. It’s more accessible and you don’t need to go through a geneticist to diagnose Fabry disease.
“Some patients first come to us for dialysis in their 40s or 50s, but people are being tested and treated at younger ages now, and we also have newborn screening. Genetic testing for Fabry is not common, but in several states, every newborn is tested for Fabry. And, if parents have Fabry, we test their children.”
Therapeutics. “Available and emerging therapies make the field exciting,” Dr. Raymond said. “Some current gene therapy trials look promising, and preliminary evidence suggests that gene therapy may stabilize kidney and heart function.”
“Although Fabry disease does not have a cure,” Dr. Rastogi pointed out, “two treatments for Fabry disease appear to help prevent life-threatening complications: enzyme replacement therapy (ERT) and chaperone therapy.”
Replacing enzymes. “In Fabry disease, the enzyme alpha-galactosidase A is deficient,” Dr. Rastogi explained, “causing build-up of sphingolipids in blood vessels and tissues. ERT, a great advance that we’ve had for over 20 years, replenishes that deficiency. ERT has some challenges: It’s an infusion every 2 weeks for life, and it can have infusion reactions and other complications.
“Newer, second-generation, versions of ERT are being developed, including pegunigalsidase alfa (Elfabrio, Chiesi Global Rare Diseases, Protalix Biotherapeutics), recently approved by the U.S. Food and Drug Administration to treat adults with Fabry disease.”
Chaperone therapy. “The oral drug migalastat (Galafold, Fabrazyme) is a small-molecule chaperone therapy that stabilizes the faulty alpha-galactosidase A enzyme,” Dr. Rastogi explained. “It is easier to take, every other day for life, than [undergoing] infusion. Limitations include that it is available only to patients who have the amenable mutations, and whose estimated glomerular filtration rate is greater than 30 [mL/min/1.73 m2], and they may have some adverse events including nausea or vomiting.”
On the horizon: substrate reduction, gene therapy. “[These] are also exciting avenues of research,” said Dr. Rastogi. “Substrate reduction therapy aims to reduce glycosphingolipid accumulation, and lucerastat [Idorsia Pharmaceutical]1,2 and venglustat [Sanofi Genzyme]3,4 are in active clinical trials or trials that have been completed.
Gene therapy “delivers a healthy gene that helps the body produce a previously deficient enzyme,” Dr. Rastogi explained. “This is an early, very promising field in need of more research, with many challenges involving the vector and complications.
“While it is still too early to predict how effective gene therapy will be, research is encouraging. Another promising therapy is modulation of gene expression, which changes the activity of a gene.”
“Gene therapy may potentially offer an alternative to typical ERT, which some patients find burdensome,” Ms. Lauderdale added. “If a neurologist has a patient who may be a good candidate for a gene therapy clinical trial that is recruiting participants, I encourage them to learn more about the study and its requirements.”
Dr. Mellin concurred: “Several gene therapy clinical trials show promise, but further information and evidence are required.”
How might these advances affect the trajectory of Fabry disease?
“Untreated Fabry compromises quality of life and may shorten the lifespan,” Dr. Raymond said. “I’m aware of individuals and their family members who died in their 60s. In the past, individuals would develop renal failure, stroke, or cardiomyopathy before being diagnosed and treated, but now we can begin treating them earlier and head off those outcomes.
“We have many options, and their number is increasing. We now diagnose patients when they are younger and maybe presymptomatic, when therapies have much greater potential to ameliorate their lives.”
Dr. Raymond spoke hopefully: “With gene therapy, people with Fabry disease will no longer need enzyme replacement or chaperone therapy. Ultimately, if gene therapy proves to be as efficacious as we hope, without big downsides, we will, essentially, be curing Fabry.”
Concluding remarks
In summing up, the four experts quoted in this article offered the following observations and advice for neurologists:
Dr. Mellin. “Pain has a significant impact on quality of life for patients with Fabry disease. Identifying and adequately treating neuropathic pain can be life-changing.”
Ms. Lauderdale. “Reach out to geneticists and other appropriate specialists. We all need to communicate the needs of our patients to ensure they receive the best possible patient-centered care.”
Dr. Rastogi. “Fabry disease is an area of active research that can be a prototype for, and affect the outcomes of, other genetic disorders. I expect to see more centers of excellence for the study and treatment of Fabry disease.”
Dr. Raymond. “With therapies rapidly evolving, neurologists need to consider rare diseases and think about how to build them into their diagnostic schemes.”
Dr. Raymond, Dr. Mellin, and Ms. Lauderdale, have nothing to disclose. Dr. Rastogi discloses a financial relationship with several pharmaceutical and biopharmaceutical companies involved in Fabry disease therapeutics research and development, including Amicus Therapeutics, Chiesi Global Rare Diseases, Genzyme Sanofi, Sanofi S.A., Idorsia Pharmaceuticals Ltd., and Protalix Biotherapeutics.
Additional recommended reading
Beck M et al. Twenty years of the Fabry Outcome Survey (FOS): Insights, achievements, and lessons learned from a global patient registry. Orphanet J Rare Dis. 2022;17(1):238. doi: 10.1186/s13023-022-02392-9.
Beraza-Millor M et al. Novel golden lipid nanoparticles with small interference ribonucleic acid for substrate reduction therapy in Fabry disease. Pharmaceutics. 2023;15(7):1936. doi: 10.3390/pharmaceutics15071936.
Ezgu F et al. Expert opinion on the recognition, diagnosis and management of children and adults with Fabry disease: A multidisciplinary Turkey perspective. Orphanet J Rare Dis. 2022;17(1):90. doi: 10.1186/s13023-022-02215-x.
Fabry disease registry & pregnancy sub-registry. ClinicalTrials.gov Identifier: NCT00196742. Updated July 13, 2023. Accessed Sept. 13, 2023. https://www.clinicaltrials.gov/study/NCT00196742?term=Fabry%20Disease%20Registry%20%26%20Pregnancy%20Sub-registry&rank=1.
Umer M and Kalra DK. Treatment of Fabry disease: established and emerging therapies. Pharmaceuticals. 2023;16(2):320. doi: 10.3390/ph16020320.
Weidemann F et al. Chaperone therapy in Fabry disease. Int J Mol Sci. 2022;23(3):1887. doi: 10.3390/ijms23031887.
References
1. Efficacy and safety of lucerastat oral monotherapy in adult subjects with Fabry disease (MODIFY). ClinicalTrials.gov Identifier: NCT03425539. Updated Aug. 9, 2022. Accessed Sept. 18, 2023. https://www.clinicaltrials.gov/study/NCT03425539?term=NCT03425539&rank=1.
2. A study to evaluate the long-term safety and tolerability of lucerastat in adult subjects with Fabry disease. ClinicalTrials.gov Identifier: NCT03737214. Updated Aug. 16, 2023. Accessed Sept. 18, 2023. https://www.clinicaltrials.gov/study/NCT03737214?term=NCT03737214&rank=1.
3. Evaluate the safety, pharmacodynamics, pharmacokinetics, and exploratory efficacy of GZ/SAR402671 in treatment-naive adult male patients with Fabry disease. ClinicalTrials.gov Identifier: NCT02228460. Updated Dec. 17, 2019. Accessed Sept. 18, 2023. https://www.clinicaltrials.gov/study/NCT02228460?term=NCT02228460&rank=1.
4. Evaluation of the long-term safety, pharmacodynamics, and exploratory efficacy of GZ/SAR402671 in treatment-naive adult male patients with Fabry disease. ClinicalTrials.gov Identifier: NCT02489344. Updated March 23, 2023. Accessed Sept. 18, 2023. https://www.clinicaltrials.gov/study/NCT02489344?term=NC
Stiff person syndrome: When a rare disorder hits the headlines
When, in 2022, singer and international celebrity Celine Dion announced what she called her “one-in-a-million diagnosis” of stiff person syndrome, clinicians and medical scientists who specialize in the disorder took a deep breath. Scott D. Newsome, DO, professor of neurology and director of the Johns Hopkins Stiff Person Syndrome Center, Baltimore – a glass-half-full kind of person – saw in Ms. Dion’s worrying announcement a huge opportunity nonetheless: To raise awareness about the rare cluster of disorders known collectively as stiff person spectrum disorders (SPSD).
“Even at the clinician level, if you don’t know the hallmark signs and symptoms, you could possibly misdiagnose it,” Dr. Newsome said in an interview.
But misdiagnosis can go either way; increased awareness of SPSD can have a downside. Thirty years ago, when Marinos C. Dalakas, MD, first began studying SPSD, the diagnosis was frequently missed – “because people were not aware of it,” he said. But now, Dr. Dalakas, professor of neurology and director of the division of neuromuscular diseases in the department of neurology at Thomas Jefferson University and the Jefferson Hospital for Neuroscience, both in Philadelphia, said overdiagnosis is also a concern, particularly with increased public awareness.
“Just this last month I saw two patients who told me: ‘I read about it, and I believe I have symptoms of stiff person,’ ” he said.
These days, most patients in whom SPSD is suspected end up with an alternate diagnosis. In a recent retrospective study that Dr. Dalakas coauthored, of 173 patients who had been referred to the Mayo Clinic in Rochester, Minn., with suspected SPSD,1 Dr. Dalakas and colleagues determined that only 48 (27.7%) actually had the disorder – meaning that the rest might have been unnecessarily exposed to immunosuppressive SPSD therapies and that treatment for their actual disorder (most often, a functional neurologic disorder or nonneurologic condition) was delayed.
At the root of both underdiagnosis and overdiagnosis of SPSD is the heterogeneity of the condition and a lack of definitive diagnostic markers.
SPSD has been considered an autoimmune disorder for a long time, and observations by Dr. Dalakas and others have shown that as many as 35% of cases co-occur with another autoimmune disease, such as vitiligo, celiac disease, rheumatologic disease, type 1 diabetes mellitus, and thyroid disease (Grave’s disease and Hashimoto’s thyroiditis).2 A more recent study by his group observed an even higher rate (42%) of comorbid autoimmunity, with autoimmune thyroid disease being most common. However, although most cases of SPDS are characterized by an elevated level of glutamic acid decarboxylase (GAD)65-IgG, these autoantibodies are not specific to SPSD (low levels are also seen in diabetes, thyroid disease, healthy controls, etc.). Some SPSD patients have less common autoantibodies and a minority has no autoantibodies. Dr. Newsome said seronegative cases and the antibody presence and titers not being associated with disease severity or treatment response are clues that “SPSD does not appear to be a primary antibody-mediated condition and that there must be other immune factors at play.”
Autoimmune process drives SPSD
Autoimmunity, even if not detected by serologic studies, is believed to inhibit expression of gamma aminobutyric acid (GABA) receptors, which, in turn, results in stiffness and spasms. Although what are known as “Dalakas criteria,” proposed in 2009,2 describe the “classic” SPSD phenotype, encompassing roughly three-quarters of SPSD patients, there have now been other phenotypes proposed under SPSD, including isolated forms (stiff limb or trunk syndrome) and “nonclassic” phenotypes like SPS-plus (classic features plus brain stem and/or cerebellar involvement),3 overlap syndromes (for example, classic features with refractory epilepsy/limbic encephalitis), and probably the most severe phenotype, progressive encephalomyelitis with rigidity and myoclonus.
Early and aggressive therapy with benzodiazepines and other GABA-ergic agonists, as well as immune-based treatments, is considered critical to slowing progression of SPSD. However, the insidious onset of what is often a cluster of vague, nonspecific symptoms is a challenge for clinicians to recognize.
“When a patient comes in with muscular spasms, with stiffness in the back, in the legs, and it’s unexplained and it’s not due to spinal cord disease, or multiple sclerosis ... think SPSD,” said Dr. Dalakas. “Check antibodies – that’s the first thing to do.”
Antibody positivity is most helpful at high levels, he added; low titers can be present in autoimmune diabetes and other conditions, as previously mentioned. The real challenge? When a patient is seronegative.
Embarking on a diagnostic odyssey
Patients “bounce from one clinician to the next looking for answers,” said Dr. Newsome. “Patients will often start with their general practitioner and be referred to physical therapy, rheumatology, or orthopedics, and other specialists, which could include neurology and/or psychiatry, among others. SPSD is often not considered as a possible diagnosis until the patient develops more concrete symptoms and/or objective signs on exam. Of course, considering this diagnosis starts at knowing that it exists.”
Task-specific phobias and exaggerated acoustic startle or sensory reflex are specific symptoms that can red-flag some SPSD patients, said Dr. Dalakas. “Impaired GABA is also important for fears and anxiety. So, when you have a reduction of GABA you have more phobic neuroses – fear of crossing the street, fear of speaking in public, and they get very tense and they cannot perform.
“If the GABA-ergic pathways are dysfunctional, then there’s a relative hyper-excitability within the nervous system,” said Dr. Newsome. “This can be evaluated with electromyography. “The muscles are unhinged and going crazy: Agonists and antagonists are contracting together, which is abnormal. We will also assess for continuous motor unit potential activity within individual muscles – angry muscles just continuously firing. In our experience, this finding appears to be a pretty specific sign of SPS, especially in the torso.” Importantly, the sudden contraction of muscles along with stiffness can lead to traumatic falls, causing major orthopedic and brain injury.
In early stages of SPSD, a careful history and clinical exam is critical to try to shorten what Dr. Newsome calls the patient’s “diagnostic odyssey.”
“It behooves the clinician to put their hands on the patient. Check their back, their abdomen – try to feel for rigidity, paraspinal muscle spasms, and tightness. These regions of the body often have a ropey feel to them, which is due to chronic muscle spasms and tightness. Most [SPSD] patients will have this present in the thoracolumbar area,” he explained. “Check for hyperlordosis, as this is a hallmark sign on exam in SPSD. Additionally, patients can have rigidity and spasticity in their legs or arms. Also, patients with nonclassical phenotypes can present with a variety of other symptoms and findings on exam, including ataxia, nystagmus, ophthalmoparesis, and dysarthria.”
Lumbar puncture can sometimes reveal signs of inflammation, such as an elevated white blood cell count and oligoclonal bands in spinal fluid.
“The classic teaching was that you can only see such findings in conditions like multiple sclerosis, but that’s not the case,” said Dr. Newsome. “You can see these findings in other autoimmune conditions, including SPSD. Hence, as part of the workup, we will have patients undergo lumbar punctures to assess for these markers of autoimmunity.”
Other mimics of SPSD, including multiple sclerosis, tumors, and spinal stenosis, should be ruled out with MRI of the brain and spine.
Treatment options
Because of wide variability in signs and symptoms of the disorder, treatment of SPSD is a highly individualized cocktail of interventions, which might include immunotherapy and GABA-ergic agonists, as well as nonmedication treatments. The response to these agents can be difficult to quantify.
Benzodiazepines (diazepam, clonazepam, baclofen) along with other oral symptomatic treatments are often recommended as first-line therapy because of their ability to enhance GABA.4
First-line immunotherapy is usually intravenous immunoglobulin, steroids, or plasmapheresis. Second- and third-line agents include rituximab, mycophenolate mofetil, azathioprine, cyclophosphamide, and combination immune treatments.
Dr. Newsome and Dr. Dalakas have independently published a step-by-step therapeutic approach to SPSD.3,5 But in patients with paraneoplastic stiff person syndrome, eradication of their cancer is critical, although, per Dr. Newsome, “this does not always cure SPS and most of these patients still have residual disability.”
But immune-based therapies are only part of what should be a multipronged treatment approach, said Dr. Newsome. He also strongly advocates for non-pharmacological interventions, such as selective physical therapy (stretching, ultrasound, and gait and balance training), heat therapy, aquatherapy, deep-tissue massage or myofascial techniques, osteopathic or chiropractic manipulation, acupuncture, and acupressure.3
Because SPSD is considered a progressive disorder for some, a reasonable goal of treatment is to prevent worsening, said Dr. Newsome. This can take time: “We don’t expect the treatments to work overnight. It involves consecutive months and, sometimes, a couple of years of immune treatment before you start to see it impact the person’s life favorably.”
Patients who are not well informed about the long-term goal of treatments might be tempted to abandon the treatments prematurely because they don’t see immediate results, Dr. Newsome added. Encouraging realistic expectations is also important, without dashing hopes.
“I have patients who were marathon runners, and they want to get back to doing marathons. I would love nothing more than for people to get back to their pre-SPSD levels of function. But this may not be a realistic goal. However, this does not mean that quality of life can’t be helped.”
Nevertheless, Dr. Newsome encourages clinicians to reassess regularly, especially because lack of disease biomarkers makes it hard to objectively monitor the impact of therapy.
“It’s always a good rule of thumb, especially in the rare disease space, to step back and ask: ‘Are we on the right treatment path or not?’ If we’re not, then it is important to make sure you have the correct diagnosis. Even when you have a patient who fits the textbook and you, yourself, diagnosed them, it is important to continue to re-evaluate the diagnosis over time, especially if there is consideration of changing treatments. It is also important to make sure there is not something else on top of the stiff person syndrome that is working in parallel to worsen their condition.”
Be alert for comorbidity
Undiagnosed comorbid conditions that can complicate SPSD include Parkinson’s disease or myasthenia gravis, to name a couple, which Dr. Newsome has seen more than once. “We’ve seen a few people over the years who have both SPSD and another autoimmune or degenerative neurological condition.”
Diabetes also co-occurs in approximately 30% of people with SPSD, said Dr. Dalakas. “Endocrinologists should also be aware of this connection.”
Paraneoplastic stiff person syndrome is thought to be triggered by cancer, which might not have been diagnosed, making it important to work up patients for malignancy – particularly breast cancer, small cell lung cancer, lymphoma, and thymoma, Dr. Newsome advised.
Although most cases of SPSD are diagnosed in mid-life, the disorder can occur in teenagers and the elderly.
“It’s not the first thing you think of when a 70-year-old patient comes with neck pain, so it’s missed more often, and the prognosis is worse,” Dr. Dalakas warned.
What does the future hold?
Like Dr. Newsome, Dr. Dalakas is encouraged when SPSD hits the headlines because, generally, awareness facilitates diagnosis and research. (Both clinicians serve on the medical advisory board of The Stiff Person Syndrome Research Foundation.)
“We are looking for better therapies that target immune factors,” said Dr. Dalakas. “There are several of those that are relevant, so we need to select the best immune marker that we think plays a role in the antibody production,” he said.
“There’s a lot of hope – at least I have a lot of hope for what the future holds with SPSD,” added Dr. Newsome. “More research is needed and it starts with awareness of SPSD.”
Dr. Newsome discloses that he has received consulting fees for serving on scientific advisory boards of Biogen, Genentech, Bristol Myers Squibb, EMD Serono, Jazz Pharmaceuticals, Novartis, Horizon Therapeutics, TG Therapeutics; is the study lead principal investigator for a Roche clinical trial; and has received research funding (paid directly to his employing institution) from Biogen, Roche, Lundbeck, Genentech, The Stiff Person Syndrome Research Foundation, National Multiple Sclerosis Society, U.S. Department of Defense, and Patient-Centered Outcomes Research Institute. Dr. Dalakas reports nothing relevant to disclose.
References
1. Chia NH et al. Ann Clin Transl Neurol. 2023;10(7):1083-94. doi: 10.1002/acn3.51791.
2. Dalakas MC.. Curr Treat Options Neurol. 2009;11(2):102-10. doi: 10.1007/s11940-009-0013-9.
3. Newsome SD and Johnson T. J Neuroimmunol. 2022;369:577915. doi: 10.1016/j.jneuroim.2022.577915.
4. Ortiz JF et al. Cureus. 2020;12(12):e11995. doi: 10.7759/cureus.11995.
5. Dalakas CD. Neurol Neuroimmunol Neuroinflamm. 2023;10(3):e200109. doi: 10.1212/NXI.0000000000200109.
When, in 2022, singer and international celebrity Celine Dion announced what she called her “one-in-a-million diagnosis” of stiff person syndrome, clinicians and medical scientists who specialize in the disorder took a deep breath. Scott D. Newsome, DO, professor of neurology and director of the Johns Hopkins Stiff Person Syndrome Center, Baltimore – a glass-half-full kind of person – saw in Ms. Dion’s worrying announcement a huge opportunity nonetheless: To raise awareness about the rare cluster of disorders known collectively as stiff person spectrum disorders (SPSD).
“Even at the clinician level, if you don’t know the hallmark signs and symptoms, you could possibly misdiagnose it,” Dr. Newsome said in an interview.
But misdiagnosis can go either way; increased awareness of SPSD can have a downside. Thirty years ago, when Marinos C. Dalakas, MD, first began studying SPSD, the diagnosis was frequently missed – “because people were not aware of it,” he said. But now, Dr. Dalakas, professor of neurology and director of the division of neuromuscular diseases in the department of neurology at Thomas Jefferson University and the Jefferson Hospital for Neuroscience, both in Philadelphia, said overdiagnosis is also a concern, particularly with increased public awareness.
“Just this last month I saw two patients who told me: ‘I read about it, and I believe I have symptoms of stiff person,’ ” he said.
These days, most patients in whom SPSD is suspected end up with an alternate diagnosis. In a recent retrospective study that Dr. Dalakas coauthored, of 173 patients who had been referred to the Mayo Clinic in Rochester, Minn., with suspected SPSD,1 Dr. Dalakas and colleagues determined that only 48 (27.7%) actually had the disorder – meaning that the rest might have been unnecessarily exposed to immunosuppressive SPSD therapies and that treatment for their actual disorder (most often, a functional neurologic disorder or nonneurologic condition) was delayed.
At the root of both underdiagnosis and overdiagnosis of SPSD is the heterogeneity of the condition and a lack of definitive diagnostic markers.
SPSD has been considered an autoimmune disorder for a long time, and observations by Dr. Dalakas and others have shown that as many as 35% of cases co-occur with another autoimmune disease, such as vitiligo, celiac disease, rheumatologic disease, type 1 diabetes mellitus, and thyroid disease (Grave’s disease and Hashimoto’s thyroiditis).2 A more recent study by his group observed an even higher rate (42%) of comorbid autoimmunity, with autoimmune thyroid disease being most common. However, although most cases of SPDS are characterized by an elevated level of glutamic acid decarboxylase (GAD)65-IgG, these autoantibodies are not specific to SPSD (low levels are also seen in diabetes, thyroid disease, healthy controls, etc.). Some SPSD patients have less common autoantibodies and a minority has no autoantibodies. Dr. Newsome said seronegative cases and the antibody presence and titers not being associated with disease severity or treatment response are clues that “SPSD does not appear to be a primary antibody-mediated condition and that there must be other immune factors at play.”
Autoimmune process drives SPSD
Autoimmunity, even if not detected by serologic studies, is believed to inhibit expression of gamma aminobutyric acid (GABA) receptors, which, in turn, results in stiffness and spasms. Although what are known as “Dalakas criteria,” proposed in 2009,2 describe the “classic” SPSD phenotype, encompassing roughly three-quarters of SPSD patients, there have now been other phenotypes proposed under SPSD, including isolated forms (stiff limb or trunk syndrome) and “nonclassic” phenotypes like SPS-plus (classic features plus brain stem and/or cerebellar involvement),3 overlap syndromes (for example, classic features with refractory epilepsy/limbic encephalitis), and probably the most severe phenotype, progressive encephalomyelitis with rigidity and myoclonus.
Early and aggressive therapy with benzodiazepines and other GABA-ergic agonists, as well as immune-based treatments, is considered critical to slowing progression of SPSD. However, the insidious onset of what is often a cluster of vague, nonspecific symptoms is a challenge for clinicians to recognize.
“When a patient comes in with muscular spasms, with stiffness in the back, in the legs, and it’s unexplained and it’s not due to spinal cord disease, or multiple sclerosis ... think SPSD,” said Dr. Dalakas. “Check antibodies – that’s the first thing to do.”
Antibody positivity is most helpful at high levels, he added; low titers can be present in autoimmune diabetes and other conditions, as previously mentioned. The real challenge? When a patient is seronegative.
Embarking on a diagnostic odyssey
Patients “bounce from one clinician to the next looking for answers,” said Dr. Newsome. “Patients will often start with their general practitioner and be referred to physical therapy, rheumatology, or orthopedics, and other specialists, which could include neurology and/or psychiatry, among others. SPSD is often not considered as a possible diagnosis until the patient develops more concrete symptoms and/or objective signs on exam. Of course, considering this diagnosis starts at knowing that it exists.”
Task-specific phobias and exaggerated acoustic startle or sensory reflex are specific symptoms that can red-flag some SPSD patients, said Dr. Dalakas. “Impaired GABA is also important for fears and anxiety. So, when you have a reduction of GABA you have more phobic neuroses – fear of crossing the street, fear of speaking in public, and they get very tense and they cannot perform.
“If the GABA-ergic pathways are dysfunctional, then there’s a relative hyper-excitability within the nervous system,” said Dr. Newsome. “This can be evaluated with electromyography. “The muscles are unhinged and going crazy: Agonists and antagonists are contracting together, which is abnormal. We will also assess for continuous motor unit potential activity within individual muscles – angry muscles just continuously firing. In our experience, this finding appears to be a pretty specific sign of SPS, especially in the torso.” Importantly, the sudden contraction of muscles along with stiffness can lead to traumatic falls, causing major orthopedic and brain injury.
In early stages of SPSD, a careful history and clinical exam is critical to try to shorten what Dr. Newsome calls the patient’s “diagnostic odyssey.”
“It behooves the clinician to put their hands on the patient. Check their back, their abdomen – try to feel for rigidity, paraspinal muscle spasms, and tightness. These regions of the body often have a ropey feel to them, which is due to chronic muscle spasms and tightness. Most [SPSD] patients will have this present in the thoracolumbar area,” he explained. “Check for hyperlordosis, as this is a hallmark sign on exam in SPSD. Additionally, patients can have rigidity and spasticity in their legs or arms. Also, patients with nonclassical phenotypes can present with a variety of other symptoms and findings on exam, including ataxia, nystagmus, ophthalmoparesis, and dysarthria.”
Lumbar puncture can sometimes reveal signs of inflammation, such as an elevated white blood cell count and oligoclonal bands in spinal fluid.
“The classic teaching was that you can only see such findings in conditions like multiple sclerosis, but that’s not the case,” said Dr. Newsome. “You can see these findings in other autoimmune conditions, including SPSD. Hence, as part of the workup, we will have patients undergo lumbar punctures to assess for these markers of autoimmunity.”
Other mimics of SPSD, including multiple sclerosis, tumors, and spinal stenosis, should be ruled out with MRI of the brain and spine.
Treatment options
Because of wide variability in signs and symptoms of the disorder, treatment of SPSD is a highly individualized cocktail of interventions, which might include immunotherapy and GABA-ergic agonists, as well as nonmedication treatments. The response to these agents can be difficult to quantify.
Benzodiazepines (diazepam, clonazepam, baclofen) along with other oral symptomatic treatments are often recommended as first-line therapy because of their ability to enhance GABA.4
First-line immunotherapy is usually intravenous immunoglobulin, steroids, or plasmapheresis. Second- and third-line agents include rituximab, mycophenolate mofetil, azathioprine, cyclophosphamide, and combination immune treatments.
Dr. Newsome and Dr. Dalakas have independently published a step-by-step therapeutic approach to SPSD.3,5 But in patients with paraneoplastic stiff person syndrome, eradication of their cancer is critical, although, per Dr. Newsome, “this does not always cure SPS and most of these patients still have residual disability.”
But immune-based therapies are only part of what should be a multipronged treatment approach, said Dr. Newsome. He also strongly advocates for non-pharmacological interventions, such as selective physical therapy (stretching, ultrasound, and gait and balance training), heat therapy, aquatherapy, deep-tissue massage or myofascial techniques, osteopathic or chiropractic manipulation, acupuncture, and acupressure.3
Because SPSD is considered a progressive disorder for some, a reasonable goal of treatment is to prevent worsening, said Dr. Newsome. This can take time: “We don’t expect the treatments to work overnight. It involves consecutive months and, sometimes, a couple of years of immune treatment before you start to see it impact the person’s life favorably.”
Patients who are not well informed about the long-term goal of treatments might be tempted to abandon the treatments prematurely because they don’t see immediate results, Dr. Newsome added. Encouraging realistic expectations is also important, without dashing hopes.
“I have patients who were marathon runners, and they want to get back to doing marathons. I would love nothing more than for people to get back to their pre-SPSD levels of function. But this may not be a realistic goal. However, this does not mean that quality of life can’t be helped.”
Nevertheless, Dr. Newsome encourages clinicians to reassess regularly, especially because lack of disease biomarkers makes it hard to objectively monitor the impact of therapy.
“It’s always a good rule of thumb, especially in the rare disease space, to step back and ask: ‘Are we on the right treatment path or not?’ If we’re not, then it is important to make sure you have the correct diagnosis. Even when you have a patient who fits the textbook and you, yourself, diagnosed them, it is important to continue to re-evaluate the diagnosis over time, especially if there is consideration of changing treatments. It is also important to make sure there is not something else on top of the stiff person syndrome that is working in parallel to worsen their condition.”
Be alert for comorbidity
Undiagnosed comorbid conditions that can complicate SPSD include Parkinson’s disease or myasthenia gravis, to name a couple, which Dr. Newsome has seen more than once. “We’ve seen a few people over the years who have both SPSD and another autoimmune or degenerative neurological condition.”
Diabetes also co-occurs in approximately 30% of people with SPSD, said Dr. Dalakas. “Endocrinologists should also be aware of this connection.”
Paraneoplastic stiff person syndrome is thought to be triggered by cancer, which might not have been diagnosed, making it important to work up patients for malignancy – particularly breast cancer, small cell lung cancer, lymphoma, and thymoma, Dr. Newsome advised.
Although most cases of SPSD are diagnosed in mid-life, the disorder can occur in teenagers and the elderly.
“It’s not the first thing you think of when a 70-year-old patient comes with neck pain, so it’s missed more often, and the prognosis is worse,” Dr. Dalakas warned.
What does the future hold?
Like Dr. Newsome, Dr. Dalakas is encouraged when SPSD hits the headlines because, generally, awareness facilitates diagnosis and research. (Both clinicians serve on the medical advisory board of The Stiff Person Syndrome Research Foundation.)
“We are looking for better therapies that target immune factors,” said Dr. Dalakas. “There are several of those that are relevant, so we need to select the best immune marker that we think plays a role in the antibody production,” he said.
“There’s a lot of hope – at least I have a lot of hope for what the future holds with SPSD,” added Dr. Newsome. “More research is needed and it starts with awareness of SPSD.”
Dr. Newsome discloses that he has received consulting fees for serving on scientific advisory boards of Biogen, Genentech, Bristol Myers Squibb, EMD Serono, Jazz Pharmaceuticals, Novartis, Horizon Therapeutics, TG Therapeutics; is the study lead principal investigator for a Roche clinical trial; and has received research funding (paid directly to his employing institution) from Biogen, Roche, Lundbeck, Genentech, The Stiff Person Syndrome Research Foundation, National Multiple Sclerosis Society, U.S. Department of Defense, and Patient-Centered Outcomes Research Institute. Dr. Dalakas reports nothing relevant to disclose.
References
1. Chia NH et al. Ann Clin Transl Neurol. 2023;10(7):1083-94. doi: 10.1002/acn3.51791.
2. Dalakas MC.. Curr Treat Options Neurol. 2009;11(2):102-10. doi: 10.1007/s11940-009-0013-9.
3. Newsome SD and Johnson T. J Neuroimmunol. 2022;369:577915. doi: 10.1016/j.jneuroim.2022.577915.
4. Ortiz JF et al. Cureus. 2020;12(12):e11995. doi: 10.7759/cureus.11995.
5. Dalakas CD. Neurol Neuroimmunol Neuroinflamm. 2023;10(3):e200109. doi: 10.1212/NXI.0000000000200109.
When, in 2022, singer and international celebrity Celine Dion announced what she called her “one-in-a-million diagnosis” of stiff person syndrome, clinicians and medical scientists who specialize in the disorder took a deep breath. Scott D. Newsome, DO, professor of neurology and director of the Johns Hopkins Stiff Person Syndrome Center, Baltimore – a glass-half-full kind of person – saw in Ms. Dion’s worrying announcement a huge opportunity nonetheless: To raise awareness about the rare cluster of disorders known collectively as stiff person spectrum disorders (SPSD).
“Even at the clinician level, if you don’t know the hallmark signs and symptoms, you could possibly misdiagnose it,” Dr. Newsome said in an interview.
But misdiagnosis can go either way; increased awareness of SPSD can have a downside. Thirty years ago, when Marinos C. Dalakas, MD, first began studying SPSD, the diagnosis was frequently missed – “because people were not aware of it,” he said. But now, Dr. Dalakas, professor of neurology and director of the division of neuromuscular diseases in the department of neurology at Thomas Jefferson University and the Jefferson Hospital for Neuroscience, both in Philadelphia, said overdiagnosis is also a concern, particularly with increased public awareness.
“Just this last month I saw two patients who told me: ‘I read about it, and I believe I have symptoms of stiff person,’ ” he said.
These days, most patients in whom SPSD is suspected end up with an alternate diagnosis. In a recent retrospective study that Dr. Dalakas coauthored, of 173 patients who had been referred to the Mayo Clinic in Rochester, Minn., with suspected SPSD,1 Dr. Dalakas and colleagues determined that only 48 (27.7%) actually had the disorder – meaning that the rest might have been unnecessarily exposed to immunosuppressive SPSD therapies and that treatment for their actual disorder (most often, a functional neurologic disorder or nonneurologic condition) was delayed.
At the root of both underdiagnosis and overdiagnosis of SPSD is the heterogeneity of the condition and a lack of definitive diagnostic markers.
SPSD has been considered an autoimmune disorder for a long time, and observations by Dr. Dalakas and others have shown that as many as 35% of cases co-occur with another autoimmune disease, such as vitiligo, celiac disease, rheumatologic disease, type 1 diabetes mellitus, and thyroid disease (Grave’s disease and Hashimoto’s thyroiditis).2 A more recent study by his group observed an even higher rate (42%) of comorbid autoimmunity, with autoimmune thyroid disease being most common. However, although most cases of SPDS are characterized by an elevated level of glutamic acid decarboxylase (GAD)65-IgG, these autoantibodies are not specific to SPSD (low levels are also seen in diabetes, thyroid disease, healthy controls, etc.). Some SPSD patients have less common autoantibodies and a minority has no autoantibodies. Dr. Newsome said seronegative cases and the antibody presence and titers not being associated with disease severity or treatment response are clues that “SPSD does not appear to be a primary antibody-mediated condition and that there must be other immune factors at play.”
Autoimmune process drives SPSD
Autoimmunity, even if not detected by serologic studies, is believed to inhibit expression of gamma aminobutyric acid (GABA) receptors, which, in turn, results in stiffness and spasms. Although what are known as “Dalakas criteria,” proposed in 2009,2 describe the “classic” SPSD phenotype, encompassing roughly three-quarters of SPSD patients, there have now been other phenotypes proposed under SPSD, including isolated forms (stiff limb or trunk syndrome) and “nonclassic” phenotypes like SPS-plus (classic features plus brain stem and/or cerebellar involvement),3 overlap syndromes (for example, classic features with refractory epilepsy/limbic encephalitis), and probably the most severe phenotype, progressive encephalomyelitis with rigidity and myoclonus.
Early and aggressive therapy with benzodiazepines and other GABA-ergic agonists, as well as immune-based treatments, is considered critical to slowing progression of SPSD. However, the insidious onset of what is often a cluster of vague, nonspecific symptoms is a challenge for clinicians to recognize.
“When a patient comes in with muscular spasms, with stiffness in the back, in the legs, and it’s unexplained and it’s not due to spinal cord disease, or multiple sclerosis ... think SPSD,” said Dr. Dalakas. “Check antibodies – that’s the first thing to do.”
Antibody positivity is most helpful at high levels, he added; low titers can be present in autoimmune diabetes and other conditions, as previously mentioned. The real challenge? When a patient is seronegative.
Embarking on a diagnostic odyssey
Patients “bounce from one clinician to the next looking for answers,” said Dr. Newsome. “Patients will often start with their general practitioner and be referred to physical therapy, rheumatology, or orthopedics, and other specialists, which could include neurology and/or psychiatry, among others. SPSD is often not considered as a possible diagnosis until the patient develops more concrete symptoms and/or objective signs on exam. Of course, considering this diagnosis starts at knowing that it exists.”
Task-specific phobias and exaggerated acoustic startle or sensory reflex are specific symptoms that can red-flag some SPSD patients, said Dr. Dalakas. “Impaired GABA is also important for fears and anxiety. So, when you have a reduction of GABA you have more phobic neuroses – fear of crossing the street, fear of speaking in public, and they get very tense and they cannot perform.
“If the GABA-ergic pathways are dysfunctional, then there’s a relative hyper-excitability within the nervous system,” said Dr. Newsome. “This can be evaluated with electromyography. “The muscles are unhinged and going crazy: Agonists and antagonists are contracting together, which is abnormal. We will also assess for continuous motor unit potential activity within individual muscles – angry muscles just continuously firing. In our experience, this finding appears to be a pretty specific sign of SPS, especially in the torso.” Importantly, the sudden contraction of muscles along with stiffness can lead to traumatic falls, causing major orthopedic and brain injury.
In early stages of SPSD, a careful history and clinical exam is critical to try to shorten what Dr. Newsome calls the patient’s “diagnostic odyssey.”
“It behooves the clinician to put their hands on the patient. Check their back, their abdomen – try to feel for rigidity, paraspinal muscle spasms, and tightness. These regions of the body often have a ropey feel to them, which is due to chronic muscle spasms and tightness. Most [SPSD] patients will have this present in the thoracolumbar area,” he explained. “Check for hyperlordosis, as this is a hallmark sign on exam in SPSD. Additionally, patients can have rigidity and spasticity in their legs or arms. Also, patients with nonclassical phenotypes can present with a variety of other symptoms and findings on exam, including ataxia, nystagmus, ophthalmoparesis, and dysarthria.”
Lumbar puncture can sometimes reveal signs of inflammation, such as an elevated white blood cell count and oligoclonal bands in spinal fluid.
“The classic teaching was that you can only see such findings in conditions like multiple sclerosis, but that’s not the case,” said Dr. Newsome. “You can see these findings in other autoimmune conditions, including SPSD. Hence, as part of the workup, we will have patients undergo lumbar punctures to assess for these markers of autoimmunity.”
Other mimics of SPSD, including multiple sclerosis, tumors, and spinal stenosis, should be ruled out with MRI of the brain and spine.
Treatment options
Because of wide variability in signs and symptoms of the disorder, treatment of SPSD is a highly individualized cocktail of interventions, which might include immunotherapy and GABA-ergic agonists, as well as nonmedication treatments. The response to these agents can be difficult to quantify.
Benzodiazepines (diazepam, clonazepam, baclofen) along with other oral symptomatic treatments are often recommended as first-line therapy because of their ability to enhance GABA.4
First-line immunotherapy is usually intravenous immunoglobulin, steroids, or plasmapheresis. Second- and third-line agents include rituximab, mycophenolate mofetil, azathioprine, cyclophosphamide, and combination immune treatments.
Dr. Newsome and Dr. Dalakas have independently published a step-by-step therapeutic approach to SPSD.3,5 But in patients with paraneoplastic stiff person syndrome, eradication of their cancer is critical, although, per Dr. Newsome, “this does not always cure SPS and most of these patients still have residual disability.”
But immune-based therapies are only part of what should be a multipronged treatment approach, said Dr. Newsome. He also strongly advocates for non-pharmacological interventions, such as selective physical therapy (stretching, ultrasound, and gait and balance training), heat therapy, aquatherapy, deep-tissue massage or myofascial techniques, osteopathic or chiropractic manipulation, acupuncture, and acupressure.3
Because SPSD is considered a progressive disorder for some, a reasonable goal of treatment is to prevent worsening, said Dr. Newsome. This can take time: “We don’t expect the treatments to work overnight. It involves consecutive months and, sometimes, a couple of years of immune treatment before you start to see it impact the person’s life favorably.”
Patients who are not well informed about the long-term goal of treatments might be tempted to abandon the treatments prematurely because they don’t see immediate results, Dr. Newsome added. Encouraging realistic expectations is also important, without dashing hopes.
“I have patients who were marathon runners, and they want to get back to doing marathons. I would love nothing more than for people to get back to their pre-SPSD levels of function. But this may not be a realistic goal. However, this does not mean that quality of life can’t be helped.”
Nevertheless, Dr. Newsome encourages clinicians to reassess regularly, especially because lack of disease biomarkers makes it hard to objectively monitor the impact of therapy.
“It’s always a good rule of thumb, especially in the rare disease space, to step back and ask: ‘Are we on the right treatment path or not?’ If we’re not, then it is important to make sure you have the correct diagnosis. Even when you have a patient who fits the textbook and you, yourself, diagnosed them, it is important to continue to re-evaluate the diagnosis over time, especially if there is consideration of changing treatments. It is also important to make sure there is not something else on top of the stiff person syndrome that is working in parallel to worsen their condition.”
Be alert for comorbidity
Undiagnosed comorbid conditions that can complicate SPSD include Parkinson’s disease or myasthenia gravis, to name a couple, which Dr. Newsome has seen more than once. “We’ve seen a few people over the years who have both SPSD and another autoimmune or degenerative neurological condition.”
Diabetes also co-occurs in approximately 30% of people with SPSD, said Dr. Dalakas. “Endocrinologists should also be aware of this connection.”
Paraneoplastic stiff person syndrome is thought to be triggered by cancer, which might not have been diagnosed, making it important to work up patients for malignancy – particularly breast cancer, small cell lung cancer, lymphoma, and thymoma, Dr. Newsome advised.
Although most cases of SPSD are diagnosed in mid-life, the disorder can occur in teenagers and the elderly.
“It’s not the first thing you think of when a 70-year-old patient comes with neck pain, so it’s missed more often, and the prognosis is worse,” Dr. Dalakas warned.
What does the future hold?
Like Dr. Newsome, Dr. Dalakas is encouraged when SPSD hits the headlines because, generally, awareness facilitates diagnosis and research. (Both clinicians serve on the medical advisory board of The Stiff Person Syndrome Research Foundation.)
“We are looking for better therapies that target immune factors,” said Dr. Dalakas. “There are several of those that are relevant, so we need to select the best immune marker that we think plays a role in the antibody production,” he said.
“There’s a lot of hope – at least I have a lot of hope for what the future holds with SPSD,” added Dr. Newsome. “More research is needed and it starts with awareness of SPSD.”
Dr. Newsome discloses that he has received consulting fees for serving on scientific advisory boards of Biogen, Genentech, Bristol Myers Squibb, EMD Serono, Jazz Pharmaceuticals, Novartis, Horizon Therapeutics, TG Therapeutics; is the study lead principal investigator for a Roche clinical trial; and has received research funding (paid directly to his employing institution) from Biogen, Roche, Lundbeck, Genentech, The Stiff Person Syndrome Research Foundation, National Multiple Sclerosis Society, U.S. Department of Defense, and Patient-Centered Outcomes Research Institute. Dr. Dalakas reports nothing relevant to disclose.
References
1. Chia NH et al. Ann Clin Transl Neurol. 2023;10(7):1083-94. doi: 10.1002/acn3.51791.
2. Dalakas MC.. Curr Treat Options Neurol. 2009;11(2):102-10. doi: 10.1007/s11940-009-0013-9.
3. Newsome SD and Johnson T. J Neuroimmunol. 2022;369:577915. doi: 10.1016/j.jneuroim.2022.577915.
4. Ortiz JF et al. Cureus. 2020;12(12):e11995. doi: 10.7759/cureus.11995.
5. Dalakas CD. Neurol Neuroimmunol Neuroinflamm. 2023;10(3):e200109. doi: 10.1212/NXI.0000000000200109.
The dawning age of therapy for Friedreich ataxia
It took 160 years but, in February 2023, the Food and Drug Administration approved the first drug specifically designed to treat the rare neuromuscular disease Friedreich ataxia (FA). The disease, first described in 1863 by German physician Nikolaus Friedreich, has an estimated incidence of 1 in 50,000 worldwide. It is the most common form of hereditary ataxia, accounting for approximately 50% of all cases of ataxia and approximately 75% of cases among patients younger than 25 years in the United States.1
FA typically presents in childhood or early adolescence; in some patients, symptoms manifest in the middle of the third decade of life. Patients exhibit symptoms such as ataxia that becomes worse over time, gait ataxia, impaired sensation in the extremities that can spread centrally, loss of normal reflexes, especially in the knees, speech disorders (dysarthria), muscle spasticity, scoliosis, and dysphagia.
Severity of disease ranges from relatively mild to completely disabling. Symptoms are progressive; patients almost inevitably require ambulatory support or a wheelchair. They might develop diabetes mellitus and can lose hearing and vision as the disease progresses. Hypertrophic cardiomyopathy is the most common cause of death among FA patients. Some patients who have less severe features might live into their 60s – even beyond that age.2There is no cure for FA. Until recently, no therapy was available other than supportive care to address associated neuromuscular, cardiovascular, and metabolic complications.
Making the diagnosis
Genetic testing can provide a definitive diagnosis of FA. (The genetic etiology of the disease is described later in this article.)
In addition to genetic screening, the workup includes a thorough medical history and physical examination that focuses on problems with balance, proprioception, absence of reflexes, and neurological signs. Tests include electromyography, nerve-conduction studies, electrocardiography, a metabolic profile, and MRI of the brain and spinal cord.
MRI utility in FA. In a paper published in July 2023 in Brain Communications, investigators from the University of Minnesota, Minneapolis, reported that various MRI techniques can be combined to detect early-stage alterations and disease progression in patients with FA.3 The researchers compared images taken at baseline and at 1, 2, and 3 years in 28 FA patients and 20 age- and gender-matched controls.
They observed that, compared with controls, patients with FA had lower cerebellar white matter volume but not lower cerebellar gray matter volume; larger cerebellar peduncle, thalamus, and brain stem structures; and a higher volume of the fourth ventricle. Using diffusion-tensor imaging and fixel-based analysis of diffusion MRI metrics, they also detected microstructural differences in several brain regions – especially in the cerebellum and corticospinal tract.
“Over time, many of these macrostructural and microstructural alterations progressed, especially cerebellar gray- and white-matter volume and microstructures of the superior cerebellar peduncle, the posterior limb of the internal capsule, and the superior corona radiata,” the investigators reported. In addition, “linear regressions showed significant associations between many of those imaging metrics and clinical scales.”
Pathophysiological basis of FA
The underlying genetic pathology of FA was first described in 1996 by investigators from the University of Valencia (Spain). They reported that FA is caused by a mutation in FXN (formerly X25), a gene that encodes for the protein frataxin, which is important for producing mitochondrial adenosine triphosphate and managing iron stores.4
The mutation results in multiple guanine-adenine-adenine repeats in FXN, or, in a few cases, a point mutation or deletion in 1 allele of FXN, with multiple GAA repeats in the other allele. A hallmark of FA is impairment of cellular antioxidative defense mechanisms – a major cause of disease progression.
The GAA repeat leads to methylation of the promoter region of FXN. This results in production and accumulation in cells of an abnormal, ineffective form of frataxin and oxidative damage to cells, particularly those that require larger amounts of energy, such as cells in the brain, heart, and pancreas.
“You would expect that the cells would be revving up all of their endogenous defenses,” David Lynch, MD, PhD, director of the Friedreich ataxia program at Children’s Hospital of Philadelphia, explained in an interview. “These oxidative damage responses are controlled by a DNA response element called the antioxidant response element, and it’s activated by the transcription factor Nrf2 [nuclear factor erythroid 2–related factor 2].”
Treatment options have been limited
Omaveloxolone. Dr. Lynch is principal investigator for the MOXIe trial of the safety, pharmacodynamics, and efficacy of omaveloxolone (marketed as Skyclarys [Reata Pharmaceuticals]),5 which received FDA orphan drug, fast track, priority review, and rare pediatric disease designations for the treatment of FA and, in February 2023, formal FDA approval.6 Development of this drug, which activates Nrf2 and induces antioxidant target genes, arose from basic science investigation into mechanisms by which cells respond to stresses.
“Omaveloxolone works on the Nrf2 pathway, which is, paradoxically, deficient in FA,” Dr. Lynch said. “This pathway should be active all the time. You would expect that, in cells from Friedreich ataxia in a person or an animal model of the disease, you’d see that Nrf2 would be very active but, in fact, what you find is the opposite,” Dr. Lynch explained. “It’s relatively inefficient, it’s localized in the cell, and the antioxidant response element genes – the things we all use to protect ourselves from mitochondrial damage – are all relatively turned off.”
In the first phase of MOXIe, 103 patients with FA were randomly assigned to receive either omaveloxolone, 15 mg orally (51 patients), or placebo (52 patients) for 48 weeks.
The primary endpoint was change in the modified Friedreich’s Ataxia Rating Scale (mFARS) score at 48 weeks. The scale is a clinically validated neurological instrument that evaluates upper- and lower-limb coordination, upright stability, and bulbar function.
Patients assigned to placebo had worsening of function at 48 weeks (mean increase in mFARS score, 0.85). In contrast, patients assigned to omaveloxolone had a mean decrease in the mFARS score of –1.56, indicating improvement. The between-group difference of –2.41 points was statistically significant in favor of omaveloxolone (P = .038).
In a 3-year, post hoc, propensity-matched analysis, patients assigned to omaveloxolone had lower mFARS scores than a matched set of untreated patients in a study of the natural history of FA.7Dimethyl fumarate (marketed as Tecfidera [Biogen]), approved in the United States and other countries for the treatment of patients with relapsing forms of multiple sclerosis, also has Nrf2 as a therapeutic target, although its precise mechanism of action is unclear. Clinical trials of this agent for the treatment of FA are under consideration in Europe, Dr. Lynch said.
Apart from these agents, treatment of patients with FA largely centers on management of metabolic and cardiac complications; physical and occupational therapy; devices such as orthopedic shoes, canes, and wheelchairs; and, when indicated, surgery to correct skeletal problems or for implantation of a cardiac-assist device.
The FA therapeutic pipeline
According to the Friedreich’s Ataxia Research Alliance, other approaches to improving mitochondrial function and reducing oxidative stress in FA are under investigation or awaiting approval, including elamipretide, for which FDA approval is pending for Barth syndrome (a rare, X-linked disorder) and for primary mitochondrial myopathy; nicotinamide adenine dinucleotide (NAD+, a coenzyme for redox reactions) plus exercise; and MIB-626, a crystalline form of nicotinamide mononucleotide, a precursor of NAD+.
Vatiquinone, an investigational inhibitor of 15-lipoxygenase, a regulator of energetic and oxidative stress pathways, failed to meet its primary endpoint of significant improvement on the mFARS score at 72 weeks of follow-up in the MOVE-FA trial, according to the manufacturer, PTC Therapeutics.8Another therapeutic approach under investigation is modulation of frataxin-controlled metabolic pathways with leriglitazone, an orally available selective peroxisome proliferator-activated receptor gamma agonist,9 or with the prodrug precursor of monomethyl fumarate plus dimethyl fumarate.
CTI-1601, a recombinant fusion protein intended to deliver human frataxin into the mitochondria of patients with FA, is in phase 1 trials. This compound has been granted rare pediatric disease designation, fast track designation, and orphan drug status by the FDA, according to the manufacturer, Larimar Therapeutics.10Etravirine, a nonnucleoside reverse transcriptase inhibitor approved for treating HIV infection, has been demonstrated to increase the frataxin protein in cells derived from FA patients and in the heart and skeletal muscle of frataxin-deficient YG8 mice. This agent recently completed a phase 2 trial in patients with FA.11
Gene therapy: Promising
Given the genetic etiology of FA, gene therapy strategies aimed at either increasing FA gene expression or editing the genome to replace defective FXN are under active investigation.
Increasing FA gene expression. DT-216 (Design Therapeutics) is a novel, gene-targeted chimera small molecule designed to target the GAA repeat expansion mutation and restore FXN expression. This agent completed phase 1 dosing studies in 2022.
Oligonucleotides, which are nucleic acid polymers primarily used for gene silencing, are also being explored for increasing the expression of FXN, in research at the University of Texas Southwestern Medical Center, Dallas, and the University of Massachusetts, Worcester.
Gene replacement strategies under investigation to treat FA include LX2006 (Lexeo Therapeutics), a gene replacement therapy using an adeno-associated viral vector to deliver FXN intravenously, with the goal of getting the gene into myocardial cells and increasing the frataxin level in mitochondria.
A similar approach is being taken by Ronald G. Crystal, MD, and colleagues at Weill Cornell Medicine, New York. The group is designing phase 1 studies of AAVrh.10hFXN, a serotype rh.10 adeno-associated virus coding for human frataxin, with the goal of treating cardiac manifestations of FA.12FA researcher Arnulf H. Koeppen, MD, from the Samuel S. Stratton Department of Veterans Affairs Medical Center, Albany, N.Y., and Albany Medical College, said in an interview that gene replacement therapy in FA is focused on the heart “because there is no blood-heart barrier, but there is a blood-brain barrier that makes it more complicated for gene therapy to reach the brain.”
Future directions
Dr. Koeppen, Dr. Lynch, and colleagues Ian H. Harding, PhD, from Monash University, Melbourne, and Massimo Pandolfo, MD, McGill University, Montreal, conducted an extensive review of FA with a focus on challenges that researchers and drug developers face crafting therapies for this complex disorder.13
They noted that FA is “characterized by marked differences in the vulnerability of neuronal systems. In general, the proprioceptive system appears to be affected early, while later in the disease, the dentate nucleus of the cerebellum and, to some degree, the corticospinal tracts degenerate.”
The authors took a deep dive into the evidence, old and new, to evaluate the effects of FA on the central and peripheral nervous systems and to look at the course of neuropathologic changes associated with the disease. They propose a comprehensive approach to identify nervous system locations that are likely to be most successfully targeted at different disease time points.
“The proprioceptive system, usually considered a major target for frataxin-restoring treatments, shows substantial evidence of hypoplasia and/or early developmental loss, with minimal evidence of progression over time,” they wrote. “It seems likely that this system is not an ideal target for therapies given after early childhood. Targeting the [dentate nucleus] of the cerebellum is likely to be most effective early in the course of the disease, when it is functionally affected, but still shows limited atrophy. The corticospinal tract degenerates over time contributing to disease progression throughout its late stages and may be considered a target.”
David Lynch, MD, PhD, and Arnulf Koeppen, MD, disclose support from the Friedreich’s Ataxia Research Alliance. Dr. Lynch also discloses support from the National Institutes of Health, U.S. Food and Drug Administration, Muscular Dystrophy Association, Reata Pharmaceuticals, and Retrotope.
References
1. Williams CT and De Jesus O. Friedreich ataxia. StatPearls. 2023 Jun 27. https://www.ncbi.nlm.nih.gov/books/NBK563199/.
2. National Institute of Neurological Disorders and Stroke. Friedreich ataxia. 2023 Sep 2. https://www.ninds.nih.gov/health-information/disorders/friedreich-ataxia.
3. Adanyeguh IM et al. Brain Commun. 2023;5(4):fcad196. doi: 10.1093/braincomms/fcad196.
4. Camapuzano V et al. Science. 1996;271(5254):1423-7. doi: 10.1126/science.271.5254.1423.
5. RTA 408 capsules in patients with Friedreich’s ataxia–MOXIe. ClinicalTrials. gov Identifier: NCT02255435. 2022 Dec 6. https://clinicaltrials.gov/study/NCT02255435.
6. Food and Drug Administration. FDA approves first treatment for Friedreich’s ataxia. 2023 Feb 28. www.fda.gov/drugs/news-events-human-drugs/fda-approves-first-treatment-friedreichs-ataxia#.
7. Lynch DR et al. Ann Clin Transl Neurol. 2023 Sep 10. doi: 10.1002/acn3.51897
8. PTC Therapeutics. PTC Therapeutics announces topline results from vatiquinone MOVE-FA registration-directed trial. 2023 May 23. https://ir.ptcbio.com/news-releases/news-release-details/ptc-therapeutics-announces-topline-results-vatiquinone-move-fa.
9. Minoryx Therapeutics. The FRAMES Clinical Study in FRDA. https://www.minoryx.com/clinical-studies/clinical-study-frames/.
10. Larimar Therapeutics. CTI-1601 for Friedreich’s ataxia. https://larimartx.com/our-programs/cti-1601/.
11. Safety and efficacy of etravirine in Friedreich ataxia patients (FAEST1). ClinicalTrials.gov Identifier: NCT04273165. 2023 Mar 20. https://clinicaltrials.gov/study/NCT04273165.
12. Phase IA study of AAVrh.10hFXN gene therapy for the cardiomyopathy of Friedreich’s ataxia. ClinicalTrials.gov Identifier: NCT05302271. https://clinicaltrials.gov/study/NCT05302271.
13. Harding IH et al. Hum Gene Ther. 2020;31(23-24):1226-36. doi: 10.1089/hum.2020.264
It took 160 years but, in February 2023, the Food and Drug Administration approved the first drug specifically designed to treat the rare neuromuscular disease Friedreich ataxia (FA). The disease, first described in 1863 by German physician Nikolaus Friedreich, has an estimated incidence of 1 in 50,000 worldwide. It is the most common form of hereditary ataxia, accounting for approximately 50% of all cases of ataxia and approximately 75% of cases among patients younger than 25 years in the United States.1
FA typically presents in childhood or early adolescence; in some patients, symptoms manifest in the middle of the third decade of life. Patients exhibit symptoms such as ataxia that becomes worse over time, gait ataxia, impaired sensation in the extremities that can spread centrally, loss of normal reflexes, especially in the knees, speech disorders (dysarthria), muscle spasticity, scoliosis, and dysphagia.
Severity of disease ranges from relatively mild to completely disabling. Symptoms are progressive; patients almost inevitably require ambulatory support or a wheelchair. They might develop diabetes mellitus and can lose hearing and vision as the disease progresses. Hypertrophic cardiomyopathy is the most common cause of death among FA patients. Some patients who have less severe features might live into their 60s – even beyond that age.2There is no cure for FA. Until recently, no therapy was available other than supportive care to address associated neuromuscular, cardiovascular, and metabolic complications.
Making the diagnosis
Genetic testing can provide a definitive diagnosis of FA. (The genetic etiology of the disease is described later in this article.)
In addition to genetic screening, the workup includes a thorough medical history and physical examination that focuses on problems with balance, proprioception, absence of reflexes, and neurological signs. Tests include electromyography, nerve-conduction studies, electrocardiography, a metabolic profile, and MRI of the brain and spinal cord.
MRI utility in FA. In a paper published in July 2023 in Brain Communications, investigators from the University of Minnesota, Minneapolis, reported that various MRI techniques can be combined to detect early-stage alterations and disease progression in patients with FA.3 The researchers compared images taken at baseline and at 1, 2, and 3 years in 28 FA patients and 20 age- and gender-matched controls.
They observed that, compared with controls, patients with FA had lower cerebellar white matter volume but not lower cerebellar gray matter volume; larger cerebellar peduncle, thalamus, and brain stem structures; and a higher volume of the fourth ventricle. Using diffusion-tensor imaging and fixel-based analysis of diffusion MRI metrics, they also detected microstructural differences in several brain regions – especially in the cerebellum and corticospinal tract.
“Over time, many of these macrostructural and microstructural alterations progressed, especially cerebellar gray- and white-matter volume and microstructures of the superior cerebellar peduncle, the posterior limb of the internal capsule, and the superior corona radiata,” the investigators reported. In addition, “linear regressions showed significant associations between many of those imaging metrics and clinical scales.”
Pathophysiological basis of FA
The underlying genetic pathology of FA was first described in 1996 by investigators from the University of Valencia (Spain). They reported that FA is caused by a mutation in FXN (formerly X25), a gene that encodes for the protein frataxin, which is important for producing mitochondrial adenosine triphosphate and managing iron stores.4
The mutation results in multiple guanine-adenine-adenine repeats in FXN, or, in a few cases, a point mutation or deletion in 1 allele of FXN, with multiple GAA repeats in the other allele. A hallmark of FA is impairment of cellular antioxidative defense mechanisms – a major cause of disease progression.
The GAA repeat leads to methylation of the promoter region of FXN. This results in production and accumulation in cells of an abnormal, ineffective form of frataxin and oxidative damage to cells, particularly those that require larger amounts of energy, such as cells in the brain, heart, and pancreas.
“You would expect that the cells would be revving up all of their endogenous defenses,” David Lynch, MD, PhD, director of the Friedreich ataxia program at Children’s Hospital of Philadelphia, explained in an interview. “These oxidative damage responses are controlled by a DNA response element called the antioxidant response element, and it’s activated by the transcription factor Nrf2 [nuclear factor erythroid 2–related factor 2].”
Treatment options have been limited
Omaveloxolone. Dr. Lynch is principal investigator for the MOXIe trial of the safety, pharmacodynamics, and efficacy of omaveloxolone (marketed as Skyclarys [Reata Pharmaceuticals]),5 which received FDA orphan drug, fast track, priority review, and rare pediatric disease designations for the treatment of FA and, in February 2023, formal FDA approval.6 Development of this drug, which activates Nrf2 and induces antioxidant target genes, arose from basic science investigation into mechanisms by which cells respond to stresses.
“Omaveloxolone works on the Nrf2 pathway, which is, paradoxically, deficient in FA,” Dr. Lynch said. “This pathway should be active all the time. You would expect that, in cells from Friedreich ataxia in a person or an animal model of the disease, you’d see that Nrf2 would be very active but, in fact, what you find is the opposite,” Dr. Lynch explained. “It’s relatively inefficient, it’s localized in the cell, and the antioxidant response element genes – the things we all use to protect ourselves from mitochondrial damage – are all relatively turned off.”
In the first phase of MOXIe, 103 patients with FA were randomly assigned to receive either omaveloxolone, 15 mg orally (51 patients), or placebo (52 patients) for 48 weeks.
The primary endpoint was change in the modified Friedreich’s Ataxia Rating Scale (mFARS) score at 48 weeks. The scale is a clinically validated neurological instrument that evaluates upper- and lower-limb coordination, upright stability, and bulbar function.
Patients assigned to placebo had worsening of function at 48 weeks (mean increase in mFARS score, 0.85). In contrast, patients assigned to omaveloxolone had a mean decrease in the mFARS score of –1.56, indicating improvement. The between-group difference of –2.41 points was statistically significant in favor of omaveloxolone (P = .038).
In a 3-year, post hoc, propensity-matched analysis, patients assigned to omaveloxolone had lower mFARS scores than a matched set of untreated patients in a study of the natural history of FA.7Dimethyl fumarate (marketed as Tecfidera [Biogen]), approved in the United States and other countries for the treatment of patients with relapsing forms of multiple sclerosis, also has Nrf2 as a therapeutic target, although its precise mechanism of action is unclear. Clinical trials of this agent for the treatment of FA are under consideration in Europe, Dr. Lynch said.
Apart from these agents, treatment of patients with FA largely centers on management of metabolic and cardiac complications; physical and occupational therapy; devices such as orthopedic shoes, canes, and wheelchairs; and, when indicated, surgery to correct skeletal problems or for implantation of a cardiac-assist device.
The FA therapeutic pipeline
According to the Friedreich’s Ataxia Research Alliance, other approaches to improving mitochondrial function and reducing oxidative stress in FA are under investigation or awaiting approval, including elamipretide, for which FDA approval is pending for Barth syndrome (a rare, X-linked disorder) and for primary mitochondrial myopathy; nicotinamide adenine dinucleotide (NAD+, a coenzyme for redox reactions) plus exercise; and MIB-626, a crystalline form of nicotinamide mononucleotide, a precursor of NAD+.
Vatiquinone, an investigational inhibitor of 15-lipoxygenase, a regulator of energetic and oxidative stress pathways, failed to meet its primary endpoint of significant improvement on the mFARS score at 72 weeks of follow-up in the MOVE-FA trial, according to the manufacturer, PTC Therapeutics.8Another therapeutic approach under investigation is modulation of frataxin-controlled metabolic pathways with leriglitazone, an orally available selective peroxisome proliferator-activated receptor gamma agonist,9 or with the prodrug precursor of monomethyl fumarate plus dimethyl fumarate.
CTI-1601, a recombinant fusion protein intended to deliver human frataxin into the mitochondria of patients with FA, is in phase 1 trials. This compound has been granted rare pediatric disease designation, fast track designation, and orphan drug status by the FDA, according to the manufacturer, Larimar Therapeutics.10Etravirine, a nonnucleoside reverse transcriptase inhibitor approved for treating HIV infection, has been demonstrated to increase the frataxin protein in cells derived from FA patients and in the heart and skeletal muscle of frataxin-deficient YG8 mice. This agent recently completed a phase 2 trial in patients with FA.11
Gene therapy: Promising
Given the genetic etiology of FA, gene therapy strategies aimed at either increasing FA gene expression or editing the genome to replace defective FXN are under active investigation.
Increasing FA gene expression. DT-216 (Design Therapeutics) is a novel, gene-targeted chimera small molecule designed to target the GAA repeat expansion mutation and restore FXN expression. This agent completed phase 1 dosing studies in 2022.
Oligonucleotides, which are nucleic acid polymers primarily used for gene silencing, are also being explored for increasing the expression of FXN, in research at the University of Texas Southwestern Medical Center, Dallas, and the University of Massachusetts, Worcester.
Gene replacement strategies under investigation to treat FA include LX2006 (Lexeo Therapeutics), a gene replacement therapy using an adeno-associated viral vector to deliver FXN intravenously, with the goal of getting the gene into myocardial cells and increasing the frataxin level in mitochondria.
A similar approach is being taken by Ronald G. Crystal, MD, and colleagues at Weill Cornell Medicine, New York. The group is designing phase 1 studies of AAVrh.10hFXN, a serotype rh.10 adeno-associated virus coding for human frataxin, with the goal of treating cardiac manifestations of FA.12FA researcher Arnulf H. Koeppen, MD, from the Samuel S. Stratton Department of Veterans Affairs Medical Center, Albany, N.Y., and Albany Medical College, said in an interview that gene replacement therapy in FA is focused on the heart “because there is no blood-heart barrier, but there is a blood-brain barrier that makes it more complicated for gene therapy to reach the brain.”
Future directions
Dr. Koeppen, Dr. Lynch, and colleagues Ian H. Harding, PhD, from Monash University, Melbourne, and Massimo Pandolfo, MD, McGill University, Montreal, conducted an extensive review of FA with a focus on challenges that researchers and drug developers face crafting therapies for this complex disorder.13
They noted that FA is “characterized by marked differences in the vulnerability of neuronal systems. In general, the proprioceptive system appears to be affected early, while later in the disease, the dentate nucleus of the cerebellum and, to some degree, the corticospinal tracts degenerate.”
The authors took a deep dive into the evidence, old and new, to evaluate the effects of FA on the central and peripheral nervous systems and to look at the course of neuropathologic changes associated with the disease. They propose a comprehensive approach to identify nervous system locations that are likely to be most successfully targeted at different disease time points.
“The proprioceptive system, usually considered a major target for frataxin-restoring treatments, shows substantial evidence of hypoplasia and/or early developmental loss, with minimal evidence of progression over time,” they wrote. “It seems likely that this system is not an ideal target for therapies given after early childhood. Targeting the [dentate nucleus] of the cerebellum is likely to be most effective early in the course of the disease, when it is functionally affected, but still shows limited atrophy. The corticospinal tract degenerates over time contributing to disease progression throughout its late stages and may be considered a target.”
David Lynch, MD, PhD, and Arnulf Koeppen, MD, disclose support from the Friedreich’s Ataxia Research Alliance. Dr. Lynch also discloses support from the National Institutes of Health, U.S. Food and Drug Administration, Muscular Dystrophy Association, Reata Pharmaceuticals, and Retrotope.
References
1. Williams CT and De Jesus O. Friedreich ataxia. StatPearls. 2023 Jun 27. https://www.ncbi.nlm.nih.gov/books/NBK563199/.
2. National Institute of Neurological Disorders and Stroke. Friedreich ataxia. 2023 Sep 2. https://www.ninds.nih.gov/health-information/disorders/friedreich-ataxia.
3. Adanyeguh IM et al. Brain Commun. 2023;5(4):fcad196. doi: 10.1093/braincomms/fcad196.
4. Camapuzano V et al. Science. 1996;271(5254):1423-7. doi: 10.1126/science.271.5254.1423.
5. RTA 408 capsules in patients with Friedreich’s ataxia–MOXIe. ClinicalTrials. gov Identifier: NCT02255435. 2022 Dec 6. https://clinicaltrials.gov/study/NCT02255435.
6. Food and Drug Administration. FDA approves first treatment for Friedreich’s ataxia. 2023 Feb 28. www.fda.gov/drugs/news-events-human-drugs/fda-approves-first-treatment-friedreichs-ataxia#.
7. Lynch DR et al. Ann Clin Transl Neurol. 2023 Sep 10. doi: 10.1002/acn3.51897
8. PTC Therapeutics. PTC Therapeutics announces topline results from vatiquinone MOVE-FA registration-directed trial. 2023 May 23. https://ir.ptcbio.com/news-releases/news-release-details/ptc-therapeutics-announces-topline-results-vatiquinone-move-fa.
9. Minoryx Therapeutics. The FRAMES Clinical Study in FRDA. https://www.minoryx.com/clinical-studies/clinical-study-frames/.
10. Larimar Therapeutics. CTI-1601 for Friedreich’s ataxia. https://larimartx.com/our-programs/cti-1601/.
11. Safety and efficacy of etravirine in Friedreich ataxia patients (FAEST1). ClinicalTrials.gov Identifier: NCT04273165. 2023 Mar 20. https://clinicaltrials.gov/study/NCT04273165.
12. Phase IA study of AAVrh.10hFXN gene therapy for the cardiomyopathy of Friedreich’s ataxia. ClinicalTrials.gov Identifier: NCT05302271. https://clinicaltrials.gov/study/NCT05302271.
13. Harding IH et al. Hum Gene Ther. 2020;31(23-24):1226-36. doi: 10.1089/hum.2020.264
It took 160 years but, in February 2023, the Food and Drug Administration approved the first drug specifically designed to treat the rare neuromuscular disease Friedreich ataxia (FA). The disease, first described in 1863 by German physician Nikolaus Friedreich, has an estimated incidence of 1 in 50,000 worldwide. It is the most common form of hereditary ataxia, accounting for approximately 50% of all cases of ataxia and approximately 75% of cases among patients younger than 25 years in the United States.1
FA typically presents in childhood or early adolescence; in some patients, symptoms manifest in the middle of the third decade of life. Patients exhibit symptoms such as ataxia that becomes worse over time, gait ataxia, impaired sensation in the extremities that can spread centrally, loss of normal reflexes, especially in the knees, speech disorders (dysarthria), muscle spasticity, scoliosis, and dysphagia.
Severity of disease ranges from relatively mild to completely disabling. Symptoms are progressive; patients almost inevitably require ambulatory support or a wheelchair. They might develop diabetes mellitus and can lose hearing and vision as the disease progresses. Hypertrophic cardiomyopathy is the most common cause of death among FA patients. Some patients who have less severe features might live into their 60s – even beyond that age.2There is no cure for FA. Until recently, no therapy was available other than supportive care to address associated neuromuscular, cardiovascular, and metabolic complications.
Making the diagnosis
Genetic testing can provide a definitive diagnosis of FA. (The genetic etiology of the disease is described later in this article.)
In addition to genetic screening, the workup includes a thorough medical history and physical examination that focuses on problems with balance, proprioception, absence of reflexes, and neurological signs. Tests include electromyography, nerve-conduction studies, electrocardiography, a metabolic profile, and MRI of the brain and spinal cord.
MRI utility in FA. In a paper published in July 2023 in Brain Communications, investigators from the University of Minnesota, Minneapolis, reported that various MRI techniques can be combined to detect early-stage alterations and disease progression in patients with FA.3 The researchers compared images taken at baseline and at 1, 2, and 3 years in 28 FA patients and 20 age- and gender-matched controls.
They observed that, compared with controls, patients with FA had lower cerebellar white matter volume but not lower cerebellar gray matter volume; larger cerebellar peduncle, thalamus, and brain stem structures; and a higher volume of the fourth ventricle. Using diffusion-tensor imaging and fixel-based analysis of diffusion MRI metrics, they also detected microstructural differences in several brain regions – especially in the cerebellum and corticospinal tract.
“Over time, many of these macrostructural and microstructural alterations progressed, especially cerebellar gray- and white-matter volume and microstructures of the superior cerebellar peduncle, the posterior limb of the internal capsule, and the superior corona radiata,” the investigators reported. In addition, “linear regressions showed significant associations between many of those imaging metrics and clinical scales.”
Pathophysiological basis of FA
The underlying genetic pathology of FA was first described in 1996 by investigators from the University of Valencia (Spain). They reported that FA is caused by a mutation in FXN (formerly X25), a gene that encodes for the protein frataxin, which is important for producing mitochondrial adenosine triphosphate and managing iron stores.4
The mutation results in multiple guanine-adenine-adenine repeats in FXN, or, in a few cases, a point mutation or deletion in 1 allele of FXN, with multiple GAA repeats in the other allele. A hallmark of FA is impairment of cellular antioxidative defense mechanisms – a major cause of disease progression.
The GAA repeat leads to methylation of the promoter region of FXN. This results in production and accumulation in cells of an abnormal, ineffective form of frataxin and oxidative damage to cells, particularly those that require larger amounts of energy, such as cells in the brain, heart, and pancreas.
“You would expect that the cells would be revving up all of their endogenous defenses,” David Lynch, MD, PhD, director of the Friedreich ataxia program at Children’s Hospital of Philadelphia, explained in an interview. “These oxidative damage responses are controlled by a DNA response element called the antioxidant response element, and it’s activated by the transcription factor Nrf2 [nuclear factor erythroid 2–related factor 2].”
Treatment options have been limited
Omaveloxolone. Dr. Lynch is principal investigator for the MOXIe trial of the safety, pharmacodynamics, and efficacy of omaveloxolone (marketed as Skyclarys [Reata Pharmaceuticals]),5 which received FDA orphan drug, fast track, priority review, and rare pediatric disease designations for the treatment of FA and, in February 2023, formal FDA approval.6 Development of this drug, which activates Nrf2 and induces antioxidant target genes, arose from basic science investigation into mechanisms by which cells respond to stresses.
“Omaveloxolone works on the Nrf2 pathway, which is, paradoxically, deficient in FA,” Dr. Lynch said. “This pathway should be active all the time. You would expect that, in cells from Friedreich ataxia in a person or an animal model of the disease, you’d see that Nrf2 would be very active but, in fact, what you find is the opposite,” Dr. Lynch explained. “It’s relatively inefficient, it’s localized in the cell, and the antioxidant response element genes – the things we all use to protect ourselves from mitochondrial damage – are all relatively turned off.”
In the first phase of MOXIe, 103 patients with FA were randomly assigned to receive either omaveloxolone, 15 mg orally (51 patients), or placebo (52 patients) for 48 weeks.
The primary endpoint was change in the modified Friedreich’s Ataxia Rating Scale (mFARS) score at 48 weeks. The scale is a clinically validated neurological instrument that evaluates upper- and lower-limb coordination, upright stability, and bulbar function.
Patients assigned to placebo had worsening of function at 48 weeks (mean increase in mFARS score, 0.85). In contrast, patients assigned to omaveloxolone had a mean decrease in the mFARS score of –1.56, indicating improvement. The between-group difference of –2.41 points was statistically significant in favor of omaveloxolone (P = .038).
In a 3-year, post hoc, propensity-matched analysis, patients assigned to omaveloxolone had lower mFARS scores than a matched set of untreated patients in a study of the natural history of FA.7Dimethyl fumarate (marketed as Tecfidera [Biogen]), approved in the United States and other countries for the treatment of patients with relapsing forms of multiple sclerosis, also has Nrf2 as a therapeutic target, although its precise mechanism of action is unclear. Clinical trials of this agent for the treatment of FA are under consideration in Europe, Dr. Lynch said.
Apart from these agents, treatment of patients with FA largely centers on management of metabolic and cardiac complications; physical and occupational therapy; devices such as orthopedic shoes, canes, and wheelchairs; and, when indicated, surgery to correct skeletal problems or for implantation of a cardiac-assist device.
The FA therapeutic pipeline
According to the Friedreich’s Ataxia Research Alliance, other approaches to improving mitochondrial function and reducing oxidative stress in FA are under investigation or awaiting approval, including elamipretide, for which FDA approval is pending for Barth syndrome (a rare, X-linked disorder) and for primary mitochondrial myopathy; nicotinamide adenine dinucleotide (NAD+, a coenzyme for redox reactions) plus exercise; and MIB-626, a crystalline form of nicotinamide mononucleotide, a precursor of NAD+.
Vatiquinone, an investigational inhibitor of 15-lipoxygenase, a regulator of energetic and oxidative stress pathways, failed to meet its primary endpoint of significant improvement on the mFARS score at 72 weeks of follow-up in the MOVE-FA trial, according to the manufacturer, PTC Therapeutics.8Another therapeutic approach under investigation is modulation of frataxin-controlled metabolic pathways with leriglitazone, an orally available selective peroxisome proliferator-activated receptor gamma agonist,9 or with the prodrug precursor of monomethyl fumarate plus dimethyl fumarate.
CTI-1601, a recombinant fusion protein intended to deliver human frataxin into the mitochondria of patients with FA, is in phase 1 trials. This compound has been granted rare pediatric disease designation, fast track designation, and orphan drug status by the FDA, according to the manufacturer, Larimar Therapeutics.10Etravirine, a nonnucleoside reverse transcriptase inhibitor approved for treating HIV infection, has been demonstrated to increase the frataxin protein in cells derived from FA patients and in the heart and skeletal muscle of frataxin-deficient YG8 mice. This agent recently completed a phase 2 trial in patients with FA.11
Gene therapy: Promising
Given the genetic etiology of FA, gene therapy strategies aimed at either increasing FA gene expression or editing the genome to replace defective FXN are under active investigation.
Increasing FA gene expression. DT-216 (Design Therapeutics) is a novel, gene-targeted chimera small molecule designed to target the GAA repeat expansion mutation and restore FXN expression. This agent completed phase 1 dosing studies in 2022.
Oligonucleotides, which are nucleic acid polymers primarily used for gene silencing, are also being explored for increasing the expression of FXN, in research at the University of Texas Southwestern Medical Center, Dallas, and the University of Massachusetts, Worcester.
Gene replacement strategies under investigation to treat FA include LX2006 (Lexeo Therapeutics), a gene replacement therapy using an adeno-associated viral vector to deliver FXN intravenously, with the goal of getting the gene into myocardial cells and increasing the frataxin level in mitochondria.
A similar approach is being taken by Ronald G. Crystal, MD, and colleagues at Weill Cornell Medicine, New York. The group is designing phase 1 studies of AAVrh.10hFXN, a serotype rh.10 adeno-associated virus coding for human frataxin, with the goal of treating cardiac manifestations of FA.12FA researcher Arnulf H. Koeppen, MD, from the Samuel S. Stratton Department of Veterans Affairs Medical Center, Albany, N.Y., and Albany Medical College, said in an interview that gene replacement therapy in FA is focused on the heart “because there is no blood-heart barrier, but there is a blood-brain barrier that makes it more complicated for gene therapy to reach the brain.”
Future directions
Dr. Koeppen, Dr. Lynch, and colleagues Ian H. Harding, PhD, from Monash University, Melbourne, and Massimo Pandolfo, MD, McGill University, Montreal, conducted an extensive review of FA with a focus on challenges that researchers and drug developers face crafting therapies for this complex disorder.13
They noted that FA is “characterized by marked differences in the vulnerability of neuronal systems. In general, the proprioceptive system appears to be affected early, while later in the disease, the dentate nucleus of the cerebellum and, to some degree, the corticospinal tracts degenerate.”
The authors took a deep dive into the evidence, old and new, to evaluate the effects of FA on the central and peripheral nervous systems and to look at the course of neuropathologic changes associated with the disease. They propose a comprehensive approach to identify nervous system locations that are likely to be most successfully targeted at different disease time points.
“The proprioceptive system, usually considered a major target for frataxin-restoring treatments, shows substantial evidence of hypoplasia and/or early developmental loss, with minimal evidence of progression over time,” they wrote. “It seems likely that this system is not an ideal target for therapies given after early childhood. Targeting the [dentate nucleus] of the cerebellum is likely to be most effective early in the course of the disease, when it is functionally affected, but still shows limited atrophy. The corticospinal tract degenerates over time contributing to disease progression throughout its late stages and may be considered a target.”
David Lynch, MD, PhD, and Arnulf Koeppen, MD, disclose support from the Friedreich’s Ataxia Research Alliance. Dr. Lynch also discloses support from the National Institutes of Health, U.S. Food and Drug Administration, Muscular Dystrophy Association, Reata Pharmaceuticals, and Retrotope.
References
1. Williams CT and De Jesus O. Friedreich ataxia. StatPearls. 2023 Jun 27. https://www.ncbi.nlm.nih.gov/books/NBK563199/.
2. National Institute of Neurological Disorders and Stroke. Friedreich ataxia. 2023 Sep 2. https://www.ninds.nih.gov/health-information/disorders/friedreich-ataxia.
3. Adanyeguh IM et al. Brain Commun. 2023;5(4):fcad196. doi: 10.1093/braincomms/fcad196.
4. Camapuzano V et al. Science. 1996;271(5254):1423-7. doi: 10.1126/science.271.5254.1423.
5. RTA 408 capsules in patients with Friedreich’s ataxia–MOXIe. ClinicalTrials. gov Identifier: NCT02255435. 2022 Dec 6. https://clinicaltrials.gov/study/NCT02255435.
6. Food and Drug Administration. FDA approves first treatment for Friedreich’s ataxia. 2023 Feb 28. www.fda.gov/drugs/news-events-human-drugs/fda-approves-first-treatment-friedreichs-ataxia#.
7. Lynch DR et al. Ann Clin Transl Neurol. 2023 Sep 10. doi: 10.1002/acn3.51897
8. PTC Therapeutics. PTC Therapeutics announces topline results from vatiquinone MOVE-FA registration-directed trial. 2023 May 23. https://ir.ptcbio.com/news-releases/news-release-details/ptc-therapeutics-announces-topline-results-vatiquinone-move-fa.
9. Minoryx Therapeutics. The FRAMES Clinical Study in FRDA. https://www.minoryx.com/clinical-studies/clinical-study-frames/.
10. Larimar Therapeutics. CTI-1601 for Friedreich’s ataxia. https://larimartx.com/our-programs/cti-1601/.
11. Safety and efficacy of etravirine in Friedreich ataxia patients (FAEST1). ClinicalTrials.gov Identifier: NCT04273165. 2023 Mar 20. https://clinicaltrials.gov/study/NCT04273165.
12. Phase IA study of AAVrh.10hFXN gene therapy for the cardiomyopathy of Friedreich’s ataxia. ClinicalTrials.gov Identifier: NCT05302271. https://clinicaltrials.gov/study/NCT05302271.
13. Harding IH et al. Hum Gene Ther. 2020;31(23-24):1226-36. doi: 10.1089/hum.2020.264
A new chapter for research on treating Huntington’s disease
The past decade has been a contradictory one for research on Huntington’s disease, marked by breakthroughs in the biology and genetics of this fatal neurodegenerative disease and painful disappointments in trials of novel therapies.
What is Huntington’s disease?
Huntington’s disease is caused by a trinucleotide repeat mutation in the huntingtin gene (HTT) and follows an autosomal dominant pattern of inheritance. In people with more than 39 copies of this CAG repeat tract expansion, the HTT protein misfolds to become toxic, with more repeats linked to earlier disease onset and a more severe course.
Huntington’s disease causes loss of neurons in the striatum and disrupts the cortical-striatal-thalamic pathway, a brain circuit that governs movement. Although behavioral symptoms can emerge earlier, signature symptoms – chorea, dystonia, and cognitive abnormalities – usually present at midlife and progress until the patient’s death.
Huntington’s disease affects an estimated 30,000 people in the United States, and an estimated 10-12 people for every 100,000 worldwide – making it rare enough that neurologists who do not specialize in movement disorders might never treat a Huntington’s patient. Yet Huntington’s disease is sufficiently prevalent to attract robust research interest and sustain large registries, which have led to remarkable findings with implications not just for Huntington’s disease but for other diseases as well.
Right now, the only Food and Drug Administration–approved treatments for Huntington’s disease are symptomatic therapies to help temper disturbances of movement, sleep, and emotions. There are two major avenues of investigation into Huntington’s disease modification:
Reduce levels of mutant HTT protein, whether through small molecules, gene therapies, or antisense oligonucleotides (ASOs) that modulate RNA processing. In March 2021, Roche announced the suspension of its phase 3 trial of tominersen, an ASO.1 Trials of other protein-lowering agents were canceled for lack of target engagement or over safety concerns, in 2021 and 2022, although this approach is still considered viable.
Modify the length of CAG repeats, which involves a more recently encountered mechanism in Huntington’s disease. The strategy is at the preclinical stage. In 2015, a group of scientists reported the game-changing discovery that a large number of genes, associated with some of the same DNA-mismatch repair pathways implicated in cancer, can modify the length of CAG repeats in cells. This gave rise to a new set of therapeutic targets, now being explored.
Neurology Reviews 2023 Rare Neurological Disease Special Report spoke with two frequently collaborating researchers at the forefront of Huntington’s disease science – Cristina Sampaio, MD, PhD, chief medical officer of CHDI Management, Princeton, N.J., and Sarah Tabrizi, MD, PhD, from University College London – about lessons learned from the past several years of Huntington’s disease drug research.
The CHDI Foundation, a nonprofit research organization, was founded in 2003 to facilitate development of Huntington’s disease therapies. Its clinical research platform, Enroll-HD, includes a global registry of some 28,000 patients and a biobank to facilitate biomarker discovery and validation. Dr. Tabrizi’s lab explores Huntington’s disease drug targets in both HTT and DNA mismatch repair, and led two CHDI-funded observational studies, TRACK-HD and TrackOn-HD, to characterize disease progression in people with Huntington’s disease. In 2022, Dr. Tabrizi and Dr. Sampaio were coauthors of a comprehensive review of Huntington’s disease drug development and published a new disease-staging system to help enable trials in presymptomatic Huntington’s disease.
“The story of Huntington’s therapeutics is very informative,” Dr. Sampaio said. “Understanding these mechanisms is relevant for any neurologist – not only for Huntington’s but because they represent a prototype development for a big group of therapies and make us better equipped to think about everything else that is happening in neurology. They’re giving us an understanding of where neurology is going.”
Tackling a tricky protein
Most Huntington’s disease research has focused on ways to attack or lower mutant HTT protein. But HTT has proven a tricky target: HTT is a large protein, present in all cells, and known to interact with more than 100 genes. Healthy HTT is critical to fetal development, but its functions in the adult body remain something of a mystery. Almost all people with Huntington’s disease have both wild-type and mutant HTT.
Tominersen, the investigative ASO developed by Roche, works to block translation of the HTT message, leading to a reduction in both healthy and mutant HTT protein. It is delivered by lumbar injection to reach the brain. Upon halting its phase 3 trial of tominersen in 2021, Roche reported that people in the high-dosage treatment group did measurably worse – although it remains unclear whether this was caused by excess protein lowering or an off-target effect. The tominersen program was the first to clearly show that it is possible to lower HTT with an intervention – a critical first step in the development of this class of drugs.
“I think the problem with the trial was the aggressive loading doses plus exposure-related toxicity,” Dr. Tabrizi said. “Whether that exposure-related toxicity was related to too much wild-type HTT lowering or the proinflammatory effects of the ASO, you can’t yet disentangle.” Roche has not given up: The company is now seeking to test lower dosages of tominersen on a younger subgroup of patients who have fewer CAG repeats, in whom a benefit of protein lowering might be more clearly seen.
Small molecules and gene therapies have also been developed to reduce mutant HTT, although most, as is the case with tominersen, will also reduce healthy protein.
“There is a long and complex debate about how much [lowering] is too much and how much is enough,” Dr. Sampaio said. “And this is a problem that has not been solved.”
Allele-specific therapy. A different class of investigative drugs, called allele-specific therapies, target only mutant HTT, sparing healthy protein. The drugs are tailored to genetic markers, or single-nucleotide polymorphisms (SNPs), that are present in different Huntington’s disease populations worldwide. Because treatments based on SNPs are highly tailored, “you need a new drug for each SNP to cover the global Huntington’s disease population,” Dr. Sampaio said. “This presents challenges from a regulatory perspective, as each drug would have to be evaluated separately.”
Two SNP-based therapies failed clinical trials in 2021, when they did not engage their targets.2 A third trial succeeded in lowering mutant HTT while preserving healthy protein and is being evaluated further in the clinic.2
Other strategies have yielded disappointing or mixed results:
A trial of branaplam, a small molecule, was stopped late in 2022 after patients developed peripheral neuropathy.3 Novartis, the drug’s manufacturer, said it would no longer investigate branaplam for Huntington’s disease.
Months earlier, in August 2022, a trial of a gene therapy to lower HTT protein – injected directly into the striatum of the brain – was halted because of adverse events in its high-dosage arm but has since resumed, with some changes to protocol.4
In neither case was excess protein-lowering thought to be the cause of safety problems.
DNA repair emerges as a promising target
Scientists have understood, since the 1990s, that the number of excess CAG repeats measured in a blood test is not the sole predictor of the onset of motor symptoms or rate of progression of Huntington’s disease.
Since the early 2000s, researchers have also known that the number of CAG repeats in cells is unstable, both in different tissues and cell types, and over time. People with Huntington’s disease turned out to be genetic mosaics, with varying, changing lengths of CAG repeats in cells. Repeats increase as a person ages, most drastically in the spiny medium neurons of the brain.
The process by which CAG repetitions grow in cells, known as somatic instability, remained poorly understood and little investigated until 2015, when a genomewide association study revealed previously unknown mechanisms.5 As it turns out, genes involved in the growth of CAG repeats are related to the DNA mismatch repair pathway, which is also important in cancer.
DNA mismatch repair refers to a complex housekeeping system, involving multiple genes and enzymes, that is fundamental to the functioning of the body as genes are continuously being translated to form proteins. Mismatch repair becomes increasingly error-prone with age: Mistakes that are not repaired become mutations, some of which are irrelevant and others that can be deleterious and lead to cancer.
In Huntington’s disease, enzymes involved in repairing DNA are the same ones that can erroneously add CAG repeats to HTT. A person with Huntington’s disease inherits what can be considered a “dyslexic” DNA repair system, Dr. Sampaio said, that misreads its template and keeps adding CAGs.
After the 2015 genomewide association study, “the DNA mismatch repair pathway became hugely important in Huntington’s disease research, and there is a lot of attention being paid now to its components. The idea is that, if we can intervene in this process, we might stop the somatic instability, the growing of the CAG repetitions, and ameliorate the progression of the disease,” Dr. Sampaio said.
In 2017 Dr. Tabrizi’s team reported that the mismatch repair gene MSH-3 was as a key driver of CAG repeats in people with Huntington’s disease.6 “I’m working really closely now with DNA repair scientists who’ve been working in cancer for 20 years. Cancer and repeat expansion diseases have really come together,” Dr. Tabrizi said.
At CHDI’s April 2023 therapeutics conference in Dubrovnik, Croatia, scientists presented findings on how to target MSH-3 and other mechanisms that underlie somatic instability.7 (Several drug companies are working on small molecules, ASOs, and other ways to inhibit MSH-3.) Researchers also presented extensively on protein lowering. The two treatment strategies are compatible for Huntington’s disease, Dr. Tabrizi said.
“I think the best way to approach Huntington’s is to target the somatic CAG repeat expansion by inhibiting MSH-3 in some way, and also target HTT lowering – but targeting it at the DNA level, as opposed to clearing the protein,” Dr. Tabrizi said. DNA-centered approaches in preclinical testing include CRISPR gene editing to inactivate mutant HTT and zinc finger proteins that allow selective targeting of DNA to reduce mutant HTT.
Recent findings on the mismatch repair pathway in Huntington’s disease have direct implications for other rare neurologic diseases caused by triplet repeat mutations, including myotonic dystrophy and cerebellar ataxias.
“There is very strong basic fundamental research in Huntington’s disease that doesn’t exist for every disease,” Dr. Sampaio said. “The fact that it is monogenic, and an adult disease that progresses relatively slowly, has made it a good disease to study, a kind of model.”
Huntington’s disease research has also generated research strategies of value in neurodegenerative diseases, such as Alzheimer’s and Parkinson’s. It provided key insights about neurofilament light, a biomarker of neuronal damage, and about the ASO drug class, which is being investigated for its utility treating in a range of diseases.
Previously, Huntington’s disease trial cohorts and registries focused on patients with late symptomatic disease. However, researchers are now pivoting to patients with less-severe disease and to preclinical mutation carriers. “We now know you have to treat early,” Dr. Tabrizi said. “This has implications for the whole field.”
Dr. Sampaio disclosed that she is an employee of CHDI Management, the administrative arm of the CHDI foundation. Dr. Tabrizi disclosed serving as a consultant to Alnylam Pharmaceuticals, Annexon, Ascidian Therapeutics, Arrowhead Pharmaceuticals, Atalanta Therapeutics, Design Therapeutics, F. Hoffmann-La Roche, HCD Economics, IQVIA, Iris Medicine, Latus Bio, LifeEdit, Novartis, Pfizer, Prilenia Therapeutics, PTC Therapeutics, Rgenta Therapeutics, Takeda Pharmaceuticals, uniQure, and Vertex Pharmaceuticals.
References
1. Genentech. Genentech Provides Update on Tominersen Program in Manifest Huntington’s Disease. https://www.gene.com/media/press-releases/14902/2021-03-22/genentech-provides-update-on-tominersen-.
2. Wave Life Sciences. Defining a new era of oligonucleotides. https://ir.wavelifesciences.com/news-releases/news-release-details/wave-life-sciences-announces-positive-update-phase-1b2a-select.
3. Novartis. Community update: Status of VIBRANT-HD, the study of branaplam/LMI070 in Huntington’s disease. https://hdsa.org/wp-content/uploads/2022/08/Novartis-FINAL-Community-Letter-8-24-22.pdf.
4. UniQure. Second Quarter 2022 Financial Results. https://uniqure.gcs-web.com/node/10856/pdf.
5. Genetic Modifiers of Huntington’s Disease (GeM-HD) Consortium. Cell. 2015 Jul 30;162(3):516-26. doi: 10.1016/j.cell.2015.07.003.
6. Moss DJH et al. Lancet Neurol. 2017 Sep;16(9):701-11. doi: 10.1016/S1474-4422(17)30161-8.
7. CHDI Foundation. Postcard from Dubrovnik 2023. https://chdifoundation.org/postcard-from-dubrovnik-2023/.
The past decade has been a contradictory one for research on Huntington’s disease, marked by breakthroughs in the biology and genetics of this fatal neurodegenerative disease and painful disappointments in trials of novel therapies.
What is Huntington’s disease?
Huntington’s disease is caused by a trinucleotide repeat mutation in the huntingtin gene (HTT) and follows an autosomal dominant pattern of inheritance. In people with more than 39 copies of this CAG repeat tract expansion, the HTT protein misfolds to become toxic, with more repeats linked to earlier disease onset and a more severe course.
Huntington’s disease causes loss of neurons in the striatum and disrupts the cortical-striatal-thalamic pathway, a brain circuit that governs movement. Although behavioral symptoms can emerge earlier, signature symptoms – chorea, dystonia, and cognitive abnormalities – usually present at midlife and progress until the patient’s death.
Huntington’s disease affects an estimated 30,000 people in the United States, and an estimated 10-12 people for every 100,000 worldwide – making it rare enough that neurologists who do not specialize in movement disorders might never treat a Huntington’s patient. Yet Huntington’s disease is sufficiently prevalent to attract robust research interest and sustain large registries, which have led to remarkable findings with implications not just for Huntington’s disease but for other diseases as well.
Right now, the only Food and Drug Administration–approved treatments for Huntington’s disease are symptomatic therapies to help temper disturbances of movement, sleep, and emotions. There are two major avenues of investigation into Huntington’s disease modification:
Reduce levels of mutant HTT protein, whether through small molecules, gene therapies, or antisense oligonucleotides (ASOs) that modulate RNA processing. In March 2021, Roche announced the suspension of its phase 3 trial of tominersen, an ASO.1 Trials of other protein-lowering agents were canceled for lack of target engagement or over safety concerns, in 2021 and 2022, although this approach is still considered viable.
Modify the length of CAG repeats, which involves a more recently encountered mechanism in Huntington’s disease. The strategy is at the preclinical stage. In 2015, a group of scientists reported the game-changing discovery that a large number of genes, associated with some of the same DNA-mismatch repair pathways implicated in cancer, can modify the length of CAG repeats in cells. This gave rise to a new set of therapeutic targets, now being explored.
Neurology Reviews 2023 Rare Neurological Disease Special Report spoke with two frequently collaborating researchers at the forefront of Huntington’s disease science – Cristina Sampaio, MD, PhD, chief medical officer of CHDI Management, Princeton, N.J., and Sarah Tabrizi, MD, PhD, from University College London – about lessons learned from the past several years of Huntington’s disease drug research.
The CHDI Foundation, a nonprofit research organization, was founded in 2003 to facilitate development of Huntington’s disease therapies. Its clinical research platform, Enroll-HD, includes a global registry of some 28,000 patients and a biobank to facilitate biomarker discovery and validation. Dr. Tabrizi’s lab explores Huntington’s disease drug targets in both HTT and DNA mismatch repair, and led two CHDI-funded observational studies, TRACK-HD and TrackOn-HD, to characterize disease progression in people with Huntington’s disease. In 2022, Dr. Tabrizi and Dr. Sampaio were coauthors of a comprehensive review of Huntington’s disease drug development and published a new disease-staging system to help enable trials in presymptomatic Huntington’s disease.
“The story of Huntington’s therapeutics is very informative,” Dr. Sampaio said. “Understanding these mechanisms is relevant for any neurologist – not only for Huntington’s but because they represent a prototype development for a big group of therapies and make us better equipped to think about everything else that is happening in neurology. They’re giving us an understanding of where neurology is going.”
Tackling a tricky protein
Most Huntington’s disease research has focused on ways to attack or lower mutant HTT protein. But HTT has proven a tricky target: HTT is a large protein, present in all cells, and known to interact with more than 100 genes. Healthy HTT is critical to fetal development, but its functions in the adult body remain something of a mystery. Almost all people with Huntington’s disease have both wild-type and mutant HTT.
Tominersen, the investigative ASO developed by Roche, works to block translation of the HTT message, leading to a reduction in both healthy and mutant HTT protein. It is delivered by lumbar injection to reach the brain. Upon halting its phase 3 trial of tominersen in 2021, Roche reported that people in the high-dosage treatment group did measurably worse – although it remains unclear whether this was caused by excess protein lowering or an off-target effect. The tominersen program was the first to clearly show that it is possible to lower HTT with an intervention – a critical first step in the development of this class of drugs.
“I think the problem with the trial was the aggressive loading doses plus exposure-related toxicity,” Dr. Tabrizi said. “Whether that exposure-related toxicity was related to too much wild-type HTT lowering or the proinflammatory effects of the ASO, you can’t yet disentangle.” Roche has not given up: The company is now seeking to test lower dosages of tominersen on a younger subgroup of patients who have fewer CAG repeats, in whom a benefit of protein lowering might be more clearly seen.
Small molecules and gene therapies have also been developed to reduce mutant HTT, although most, as is the case with tominersen, will also reduce healthy protein.
“There is a long and complex debate about how much [lowering] is too much and how much is enough,” Dr. Sampaio said. “And this is a problem that has not been solved.”
Allele-specific therapy. A different class of investigative drugs, called allele-specific therapies, target only mutant HTT, sparing healthy protein. The drugs are tailored to genetic markers, or single-nucleotide polymorphisms (SNPs), that are present in different Huntington’s disease populations worldwide. Because treatments based on SNPs are highly tailored, “you need a new drug for each SNP to cover the global Huntington’s disease population,” Dr. Sampaio said. “This presents challenges from a regulatory perspective, as each drug would have to be evaluated separately.”
Two SNP-based therapies failed clinical trials in 2021, when they did not engage their targets.2 A third trial succeeded in lowering mutant HTT while preserving healthy protein and is being evaluated further in the clinic.2
Other strategies have yielded disappointing or mixed results:
A trial of branaplam, a small molecule, was stopped late in 2022 after patients developed peripheral neuropathy.3 Novartis, the drug’s manufacturer, said it would no longer investigate branaplam for Huntington’s disease.
Months earlier, in August 2022, a trial of a gene therapy to lower HTT protein – injected directly into the striatum of the brain – was halted because of adverse events in its high-dosage arm but has since resumed, with some changes to protocol.4
In neither case was excess protein-lowering thought to be the cause of safety problems.
DNA repair emerges as a promising target
Scientists have understood, since the 1990s, that the number of excess CAG repeats measured in a blood test is not the sole predictor of the onset of motor symptoms or rate of progression of Huntington’s disease.
Since the early 2000s, researchers have also known that the number of CAG repeats in cells is unstable, both in different tissues and cell types, and over time. People with Huntington’s disease turned out to be genetic mosaics, with varying, changing lengths of CAG repeats in cells. Repeats increase as a person ages, most drastically in the spiny medium neurons of the brain.
The process by which CAG repetitions grow in cells, known as somatic instability, remained poorly understood and little investigated until 2015, when a genomewide association study revealed previously unknown mechanisms.5 As it turns out, genes involved in the growth of CAG repeats are related to the DNA mismatch repair pathway, which is also important in cancer.
DNA mismatch repair refers to a complex housekeeping system, involving multiple genes and enzymes, that is fundamental to the functioning of the body as genes are continuously being translated to form proteins. Mismatch repair becomes increasingly error-prone with age: Mistakes that are not repaired become mutations, some of which are irrelevant and others that can be deleterious and lead to cancer.
In Huntington’s disease, enzymes involved in repairing DNA are the same ones that can erroneously add CAG repeats to HTT. A person with Huntington’s disease inherits what can be considered a “dyslexic” DNA repair system, Dr. Sampaio said, that misreads its template and keeps adding CAGs.
After the 2015 genomewide association study, “the DNA mismatch repair pathway became hugely important in Huntington’s disease research, and there is a lot of attention being paid now to its components. The idea is that, if we can intervene in this process, we might stop the somatic instability, the growing of the CAG repetitions, and ameliorate the progression of the disease,” Dr. Sampaio said.
In 2017 Dr. Tabrizi’s team reported that the mismatch repair gene MSH-3 was as a key driver of CAG repeats in people with Huntington’s disease.6 “I’m working really closely now with DNA repair scientists who’ve been working in cancer for 20 years. Cancer and repeat expansion diseases have really come together,” Dr. Tabrizi said.
At CHDI’s April 2023 therapeutics conference in Dubrovnik, Croatia, scientists presented findings on how to target MSH-3 and other mechanisms that underlie somatic instability.7 (Several drug companies are working on small molecules, ASOs, and other ways to inhibit MSH-3.) Researchers also presented extensively on protein lowering. The two treatment strategies are compatible for Huntington’s disease, Dr. Tabrizi said.
“I think the best way to approach Huntington’s is to target the somatic CAG repeat expansion by inhibiting MSH-3 in some way, and also target HTT lowering – but targeting it at the DNA level, as opposed to clearing the protein,” Dr. Tabrizi said. DNA-centered approaches in preclinical testing include CRISPR gene editing to inactivate mutant HTT and zinc finger proteins that allow selective targeting of DNA to reduce mutant HTT.
Recent findings on the mismatch repair pathway in Huntington’s disease have direct implications for other rare neurologic diseases caused by triplet repeat mutations, including myotonic dystrophy and cerebellar ataxias.
“There is very strong basic fundamental research in Huntington’s disease that doesn’t exist for every disease,” Dr. Sampaio said. “The fact that it is monogenic, and an adult disease that progresses relatively slowly, has made it a good disease to study, a kind of model.”
Huntington’s disease research has also generated research strategies of value in neurodegenerative diseases, such as Alzheimer’s and Parkinson’s. It provided key insights about neurofilament light, a biomarker of neuronal damage, and about the ASO drug class, which is being investigated for its utility treating in a range of diseases.
Previously, Huntington’s disease trial cohorts and registries focused on patients with late symptomatic disease. However, researchers are now pivoting to patients with less-severe disease and to preclinical mutation carriers. “We now know you have to treat early,” Dr. Tabrizi said. “This has implications for the whole field.”
Dr. Sampaio disclosed that she is an employee of CHDI Management, the administrative arm of the CHDI foundation. Dr. Tabrizi disclosed serving as a consultant to Alnylam Pharmaceuticals, Annexon, Ascidian Therapeutics, Arrowhead Pharmaceuticals, Atalanta Therapeutics, Design Therapeutics, F. Hoffmann-La Roche, HCD Economics, IQVIA, Iris Medicine, Latus Bio, LifeEdit, Novartis, Pfizer, Prilenia Therapeutics, PTC Therapeutics, Rgenta Therapeutics, Takeda Pharmaceuticals, uniQure, and Vertex Pharmaceuticals.
References
1. Genentech. Genentech Provides Update on Tominersen Program in Manifest Huntington’s Disease. https://www.gene.com/media/press-releases/14902/2021-03-22/genentech-provides-update-on-tominersen-.
2. Wave Life Sciences. Defining a new era of oligonucleotides. https://ir.wavelifesciences.com/news-releases/news-release-details/wave-life-sciences-announces-positive-update-phase-1b2a-select.
3. Novartis. Community update: Status of VIBRANT-HD, the study of branaplam/LMI070 in Huntington’s disease. https://hdsa.org/wp-content/uploads/2022/08/Novartis-FINAL-Community-Letter-8-24-22.pdf.
4. UniQure. Second Quarter 2022 Financial Results. https://uniqure.gcs-web.com/node/10856/pdf.
5. Genetic Modifiers of Huntington’s Disease (GeM-HD) Consortium. Cell. 2015 Jul 30;162(3):516-26. doi: 10.1016/j.cell.2015.07.003.
6. Moss DJH et al. Lancet Neurol. 2017 Sep;16(9):701-11. doi: 10.1016/S1474-4422(17)30161-8.
7. CHDI Foundation. Postcard from Dubrovnik 2023. https://chdifoundation.org/postcard-from-dubrovnik-2023/.
The past decade has been a contradictory one for research on Huntington’s disease, marked by breakthroughs in the biology and genetics of this fatal neurodegenerative disease and painful disappointments in trials of novel therapies.
What is Huntington’s disease?
Huntington’s disease is caused by a trinucleotide repeat mutation in the huntingtin gene (HTT) and follows an autosomal dominant pattern of inheritance. In people with more than 39 copies of this CAG repeat tract expansion, the HTT protein misfolds to become toxic, with more repeats linked to earlier disease onset and a more severe course.
Huntington’s disease causes loss of neurons in the striatum and disrupts the cortical-striatal-thalamic pathway, a brain circuit that governs movement. Although behavioral symptoms can emerge earlier, signature symptoms – chorea, dystonia, and cognitive abnormalities – usually present at midlife and progress until the patient’s death.
Huntington’s disease affects an estimated 30,000 people in the United States, and an estimated 10-12 people for every 100,000 worldwide – making it rare enough that neurologists who do not specialize in movement disorders might never treat a Huntington’s patient. Yet Huntington’s disease is sufficiently prevalent to attract robust research interest and sustain large registries, which have led to remarkable findings with implications not just for Huntington’s disease but for other diseases as well.
Right now, the only Food and Drug Administration–approved treatments for Huntington’s disease are symptomatic therapies to help temper disturbances of movement, sleep, and emotions. There are two major avenues of investigation into Huntington’s disease modification:
Reduce levels of mutant HTT protein, whether through small molecules, gene therapies, or antisense oligonucleotides (ASOs) that modulate RNA processing. In March 2021, Roche announced the suspension of its phase 3 trial of tominersen, an ASO.1 Trials of other protein-lowering agents were canceled for lack of target engagement or over safety concerns, in 2021 and 2022, although this approach is still considered viable.
Modify the length of CAG repeats, which involves a more recently encountered mechanism in Huntington’s disease. The strategy is at the preclinical stage. In 2015, a group of scientists reported the game-changing discovery that a large number of genes, associated with some of the same DNA-mismatch repair pathways implicated in cancer, can modify the length of CAG repeats in cells. This gave rise to a new set of therapeutic targets, now being explored.
Neurology Reviews 2023 Rare Neurological Disease Special Report spoke with two frequently collaborating researchers at the forefront of Huntington’s disease science – Cristina Sampaio, MD, PhD, chief medical officer of CHDI Management, Princeton, N.J., and Sarah Tabrizi, MD, PhD, from University College London – about lessons learned from the past several years of Huntington’s disease drug research.
The CHDI Foundation, a nonprofit research organization, was founded in 2003 to facilitate development of Huntington’s disease therapies. Its clinical research platform, Enroll-HD, includes a global registry of some 28,000 patients and a biobank to facilitate biomarker discovery and validation. Dr. Tabrizi’s lab explores Huntington’s disease drug targets in both HTT and DNA mismatch repair, and led two CHDI-funded observational studies, TRACK-HD and TrackOn-HD, to characterize disease progression in people with Huntington’s disease. In 2022, Dr. Tabrizi and Dr. Sampaio were coauthors of a comprehensive review of Huntington’s disease drug development and published a new disease-staging system to help enable trials in presymptomatic Huntington’s disease.
“The story of Huntington’s therapeutics is very informative,” Dr. Sampaio said. “Understanding these mechanisms is relevant for any neurologist – not only for Huntington’s but because they represent a prototype development for a big group of therapies and make us better equipped to think about everything else that is happening in neurology. They’re giving us an understanding of where neurology is going.”
Tackling a tricky protein
Most Huntington’s disease research has focused on ways to attack or lower mutant HTT protein. But HTT has proven a tricky target: HTT is a large protein, present in all cells, and known to interact with more than 100 genes. Healthy HTT is critical to fetal development, but its functions in the adult body remain something of a mystery. Almost all people with Huntington’s disease have both wild-type and mutant HTT.
Tominersen, the investigative ASO developed by Roche, works to block translation of the HTT message, leading to a reduction in both healthy and mutant HTT protein. It is delivered by lumbar injection to reach the brain. Upon halting its phase 3 trial of tominersen in 2021, Roche reported that people in the high-dosage treatment group did measurably worse – although it remains unclear whether this was caused by excess protein lowering or an off-target effect. The tominersen program was the first to clearly show that it is possible to lower HTT with an intervention – a critical first step in the development of this class of drugs.
“I think the problem with the trial was the aggressive loading doses plus exposure-related toxicity,” Dr. Tabrizi said. “Whether that exposure-related toxicity was related to too much wild-type HTT lowering or the proinflammatory effects of the ASO, you can’t yet disentangle.” Roche has not given up: The company is now seeking to test lower dosages of tominersen on a younger subgroup of patients who have fewer CAG repeats, in whom a benefit of protein lowering might be more clearly seen.
Small molecules and gene therapies have also been developed to reduce mutant HTT, although most, as is the case with tominersen, will also reduce healthy protein.
“There is a long and complex debate about how much [lowering] is too much and how much is enough,” Dr. Sampaio said. “And this is a problem that has not been solved.”
Allele-specific therapy. A different class of investigative drugs, called allele-specific therapies, target only mutant HTT, sparing healthy protein. The drugs are tailored to genetic markers, or single-nucleotide polymorphisms (SNPs), that are present in different Huntington’s disease populations worldwide. Because treatments based on SNPs are highly tailored, “you need a new drug for each SNP to cover the global Huntington’s disease population,” Dr. Sampaio said. “This presents challenges from a regulatory perspective, as each drug would have to be evaluated separately.”
Two SNP-based therapies failed clinical trials in 2021, when they did not engage their targets.2 A third trial succeeded in lowering mutant HTT while preserving healthy protein and is being evaluated further in the clinic.2
Other strategies have yielded disappointing or mixed results:
A trial of branaplam, a small molecule, was stopped late in 2022 after patients developed peripheral neuropathy.3 Novartis, the drug’s manufacturer, said it would no longer investigate branaplam for Huntington’s disease.
Months earlier, in August 2022, a trial of a gene therapy to lower HTT protein – injected directly into the striatum of the brain – was halted because of adverse events in its high-dosage arm but has since resumed, with some changes to protocol.4
In neither case was excess protein-lowering thought to be the cause of safety problems.
DNA repair emerges as a promising target
Scientists have understood, since the 1990s, that the number of excess CAG repeats measured in a blood test is not the sole predictor of the onset of motor symptoms or rate of progression of Huntington’s disease.
Since the early 2000s, researchers have also known that the number of CAG repeats in cells is unstable, both in different tissues and cell types, and over time. People with Huntington’s disease turned out to be genetic mosaics, with varying, changing lengths of CAG repeats in cells. Repeats increase as a person ages, most drastically in the spiny medium neurons of the brain.
The process by which CAG repetitions grow in cells, known as somatic instability, remained poorly understood and little investigated until 2015, when a genomewide association study revealed previously unknown mechanisms.5 As it turns out, genes involved in the growth of CAG repeats are related to the DNA mismatch repair pathway, which is also important in cancer.
DNA mismatch repair refers to a complex housekeeping system, involving multiple genes and enzymes, that is fundamental to the functioning of the body as genes are continuously being translated to form proteins. Mismatch repair becomes increasingly error-prone with age: Mistakes that are not repaired become mutations, some of which are irrelevant and others that can be deleterious and lead to cancer.
In Huntington’s disease, enzymes involved in repairing DNA are the same ones that can erroneously add CAG repeats to HTT. A person with Huntington’s disease inherits what can be considered a “dyslexic” DNA repair system, Dr. Sampaio said, that misreads its template and keeps adding CAGs.
After the 2015 genomewide association study, “the DNA mismatch repair pathway became hugely important in Huntington’s disease research, and there is a lot of attention being paid now to its components. The idea is that, if we can intervene in this process, we might stop the somatic instability, the growing of the CAG repetitions, and ameliorate the progression of the disease,” Dr. Sampaio said.
In 2017 Dr. Tabrizi’s team reported that the mismatch repair gene MSH-3 was as a key driver of CAG repeats in people with Huntington’s disease.6 “I’m working really closely now with DNA repair scientists who’ve been working in cancer for 20 years. Cancer and repeat expansion diseases have really come together,” Dr. Tabrizi said.
At CHDI’s April 2023 therapeutics conference in Dubrovnik, Croatia, scientists presented findings on how to target MSH-3 and other mechanisms that underlie somatic instability.7 (Several drug companies are working on small molecules, ASOs, and other ways to inhibit MSH-3.) Researchers also presented extensively on protein lowering. The two treatment strategies are compatible for Huntington’s disease, Dr. Tabrizi said.
“I think the best way to approach Huntington’s is to target the somatic CAG repeat expansion by inhibiting MSH-3 in some way, and also target HTT lowering – but targeting it at the DNA level, as opposed to clearing the protein,” Dr. Tabrizi said. DNA-centered approaches in preclinical testing include CRISPR gene editing to inactivate mutant HTT and zinc finger proteins that allow selective targeting of DNA to reduce mutant HTT.
Recent findings on the mismatch repair pathway in Huntington’s disease have direct implications for other rare neurologic diseases caused by triplet repeat mutations, including myotonic dystrophy and cerebellar ataxias.
“There is very strong basic fundamental research in Huntington’s disease that doesn’t exist for every disease,” Dr. Sampaio said. “The fact that it is monogenic, and an adult disease that progresses relatively slowly, has made it a good disease to study, a kind of model.”
Huntington’s disease research has also generated research strategies of value in neurodegenerative diseases, such as Alzheimer’s and Parkinson’s. It provided key insights about neurofilament light, a biomarker of neuronal damage, and about the ASO drug class, which is being investigated for its utility treating in a range of diseases.
Previously, Huntington’s disease trial cohorts and registries focused on patients with late symptomatic disease. However, researchers are now pivoting to patients with less-severe disease and to preclinical mutation carriers. “We now know you have to treat early,” Dr. Tabrizi said. “This has implications for the whole field.”
Dr. Sampaio disclosed that she is an employee of CHDI Management, the administrative arm of the CHDI foundation. Dr. Tabrizi disclosed serving as a consultant to Alnylam Pharmaceuticals, Annexon, Ascidian Therapeutics, Arrowhead Pharmaceuticals, Atalanta Therapeutics, Design Therapeutics, F. Hoffmann-La Roche, HCD Economics, IQVIA, Iris Medicine, Latus Bio, LifeEdit, Novartis, Pfizer, Prilenia Therapeutics, PTC Therapeutics, Rgenta Therapeutics, Takeda Pharmaceuticals, uniQure, and Vertex Pharmaceuticals.
References
1. Genentech. Genentech Provides Update on Tominersen Program in Manifest Huntington’s Disease. https://www.gene.com/media/press-releases/14902/2021-03-22/genentech-provides-update-on-tominersen-.
2. Wave Life Sciences. Defining a new era of oligonucleotides. https://ir.wavelifesciences.com/news-releases/news-release-details/wave-life-sciences-announces-positive-update-phase-1b2a-select.
3. Novartis. Community update: Status of VIBRANT-HD, the study of branaplam/LMI070 in Huntington’s disease. https://hdsa.org/wp-content/uploads/2022/08/Novartis-FINAL-Community-Letter-8-24-22.pdf.
4. UniQure. Second Quarter 2022 Financial Results. https://uniqure.gcs-web.com/node/10856/pdf.
5. Genetic Modifiers of Huntington’s Disease (GeM-HD) Consortium. Cell. 2015 Jul 30;162(3):516-26. doi: 10.1016/j.cell.2015.07.003.
6. Moss DJH et al. Lancet Neurol. 2017 Sep;16(9):701-11. doi: 10.1016/S1474-4422(17)30161-8.
7. CHDI Foundation. Postcard from Dubrovnik 2023. https://chdifoundation.org/postcard-from-dubrovnik-2023/.
The Orphan Drug Act and NORD at their 40th anniversary: Dramatic achievements and ongoing innovation
In 1976, Abbey S. Meyers, a mother from Connecticut, finally got a diagnosis for her son. He had been displaying “very bizarre symptoms,” Ms. Meyers said in an interview with IndoUSRare,1 but, eventually, at 8 years of age, he was given a diagnosis of Tourette syndrome.
“They tried some medicine to try to get him to sit still, but the drugs didn’t work – or if they did, they put him to sleep,” she recounted. “The teachers would be angry that he fell asleep in the classroom.”
Ms. Meyers consulted the late Arthur K. Shapiro, MD, at what was then named the Mount Sinai School of Medicine in New York. Dr. Shapiro was conducting a small clinical trial of pimozide, a drug under investigation for schizophrenia, for its utility in children with Tourette syndrome.
“The drug worked like magic,” Ms. Meyers reported. Her son’s symptoms were substantially reduced, without sedation. He was followed by Dr. Shapiro every 3 months, at which point he would receive a 90-day refill.
However, when her son turned 10 years of age, Dr. Shapiro was no longer able to provide refills: The Food and Drug Administration (FDA) had turned down the drug manufacturer’s application for approval of pimozide for a schizophrenia indication. The company opted not to pursue further development of the drug because it was not deemed profitable.2
Pimozide became unavailable in the United States. The fact that the drug was so promising for Tourette syndrome did not warrant further investment because Tourette syndrome affected a relatively small number of people.
“I was just devastated,” Ms. Meyers reported.
Springing into advocacy
Ms. Meyers, who was working with the Tourette Syndrome Association at the time (now the Tourette Association of America), contacted people from other rare disease organizations, including the National Huntington’s Disease Association (today the Huntington’s Disease Society of America) and the Paget Foundation (today part of the Bone Health and Osteoporosis Foundation). Those organizations were experiencing similar problems with drug companies that wouldn’t engage in research and development of drugs for patients who had a rare disorder.
“We realized we had to work together to get something done to solve this problem,” Ms. Meyers said.
The sense of urgency over this roadblock increased when another patient who was taking pimozide tried to get a supply of the drug from Canada and was blocked from doing so by customs officials at the airport because the drug was not FDA approved. Working with that patient’s mother, Ms. Meyers contacted U.S. Representative Henry A. Waxman (D-Calif.), who was chair of the Subcommittee on Health and the Environment of the House Energy & Commerce Committee.
Ms. Meyers thought that Congress needed Rep. Waxman’s support if it was going to get involved with this problem. “So, we got Henry Waxman and his staff familiar with the orphan drug problem.”
ODA: Breakthrough legislation
The impetus for the Orphan Drug Act (ODA) started in 1979 with an FDA task force report calling for measures to address what was labeled the “orphan drug problem.”3
In 1982, Rep. Waxman convened a hearing and invited several pharmaceutical companies to attend. They declined the invitation. Ms. Meyers testified at the hearing, which was covered by the Los Angeles Times, giving the issue notoriety.
The issue was also addressed in the popular television series Quincy, M.E. Episodes depicted challenges facing a patient with Tourette syndrome and a patient with myoclonus. Series star Jack Klugman testified before Congress about the need for legislation regarding the development of drugs targeting the treatment of rare diseases.4
Rep. Waxman became the bill’s primary House sponsor. The ODA was approved by the House of Representatives on Dec. 14, 1982.
The combined efforts of the advocacy coalition ultimately culminated in the original ODA being signed into law by President Ronald Reagan on Jan. 4, 1983. The ODA incentivized pharmaceutical companies to allot more resources toward research on and development and distribution of therapeutics for people with a rare disease who had, until that point, been “orphaned,” so to speak, by the medical and scientific community.5
What is it to be a ‘rare disorder’ or an ‘orphan drug’?
The ODA defines a rare disorder as either a condition that affects fewer than 200,000 people or a condition that affects more than 200,000 people but for which there is no reasonable expectation that a pharmaceutical company will recoup the cost of developing a drug by selling it.5
In an interview Peter L. Saltonstall, president and CEO of the National Organization for Rare Disorders, commended Ms. Meyers on her tireless work: “She went from being a mom to a powerful advocate who got thousands of people in D.C. moving Congress to a point where they felt passing the law was necessary. In fact, she was there when the bill was signed into law.”
The FDA can grant orphan drug approval for several categories of products. These include new molecular entities, already-approved drugs for which an additional indication has been designated, and new formulations of existing or established drugs.5
Orphan-drug designation includes tax credits for the developer-manufacturer, a waiver of the usual approval fees that the company must pay to the FDA, and 7 years’ market exclusivity, during which time the FDA cannot award approval of similar treatments for the same indication.
“This [designation] ensures that the company that developed the drug can retain the opportunity for profit,” explained Mr. Saltonstall. “Companies thought: ‘We can afford to do this now. And if we market it the right way and have exclusivity, we can recover some of our profits.’”
Before the ODA, 30 drugs had been approved by the FDA for orphan conditions. By the end of 2022, more than 880 drugs were FDA approved to treat hundreds of rare disorders.
“This just shows the motivation and how the process works,” Mr. Saltonstall said. In fact, almost 50% of novel drugs approved in 2022 by the FDA were an orphan product or had an orphan indication.
In addition to the impact on drug development in the United States, enactment of the ODA had a broader ripple effect, inspiring similar changes internationally in Europe, Australia, Singapore, Japan, and other regions.5
NORD is born
The creation of NORD was initiated by the same group of advocates who lobbied tirelessly for passage of the ODA – including Ms. Meyers, who served as president of the organization for many years. Heidi Ross, MPH, NORD’s vice president of policy and regulatory affairs, called these advocates “trailblazers.”
NORD was founded in May 1983. The organization included, at that time, 40-50 disease-specific organizations. Today, NORD membership comprises more than 330 patient advocacy groups.
“The goal was to be a voice for those organizations and help get them mobilized, help them get their 501(c)3 [status], help them develop their relationship with the FDA, and similar tasks,” Mr. Saltonstall said. “We continue this important work today as the patient groups play a central role in driving care, research, and policies for their given disease. Also, there’s strength in numbers. We call upon these groups and members to help advocate in Washington for policies that impact the greater rare disease community.”
The ODA launched 4 decades of innovation and change, with NORD strengthening the rare disorder community, which encompasses more than 30 million Americans.
“The organization exists to support people living with rare disorders and tries to improve their quality of life,” according to Katie Kowalski, MPH, NORD’s associate director of education.
Education. The role of Ms. Kowalski’s department is to “educate patients and caregivers, the general public, health care professionals, and students preparing for health care careers about rare conditions,” Ms. Kowalski said. The education department maintains NORD’s Rare Disease Database,6 which contains more than 1,300 reports about rare conditions. Plus, NORD’s Rare Disease Library archives videos about specific diseases and other topics of interest to the rare disease community, including genetic testing and gene therapy.Continuing medical education programs are available for health care providers.
Events. NORD hosts:
An annual Rare Diseases and Orphan Products Breakthrough Summit for various rare disease stakeholders, including global rare disease medical experts, policy makers, regulatory agencies, industry leaders, and patient community members.
An annual patient and family conference; the 2024 edition is scheduled for June 7-8, 2024, in Los Angeles.
Membership support. NORD’s membership department supports any advocacy organization that represents a rare
disorder. “Some [organizations] are more evolved and sophisticated and can do their own educational programming,” Ms. Kowalski said. “Others are fledgling, nascent organizations that may not have the staff or money for salaries. We try to support them, teach them how to budget and raise funds and form a board of directors.”
Advocacy. NORD has a policy department that works at state and federal levels to advocate for policies affecting patients with a rare disease. Mr. Saltonstall shared that NORD was responsible for setting up and helping put together the rare disease office at the National Institutes of Health and the FDA, and continues to foster a close relationship with those offices.8,9 “In fact,” he said, “nothing happens in Washington regarding rare diseases without our being consulted or at the table.”
Focus on the patient. Mr. Saltonstall assumed his role at NORD in 2008. “By then, many fundamental things had been mastered, and we were ready to take things to the next level,” he said. “There were opportunities to leverage the ODA to help patient organizations.”
“We’re one of the only nonprofit advocacy organizations I know of without industry on the board or as members,” Mr. Saltonstall said. “The organization is completely patient focused. Everything we do comes back to committees with patients who make the decisions and management who helps implement those decisions. This makes us unique. The fact that we’re independent makes Congress trust us to be the true voice of patients.”
Spotlight: Patient care and research
Edward Neilan, MD, PhD, recently joined NORD as chief medical and scientific officer. As a pediatrician, medical geneticist, and molecular biologist, Dr. Neilan became acquainted with NORD as far back as medical school and his residency, when he used a book called the NORD Guide to Rare Disorders to help him explain certain diseases to patients and families.10 “I had a favorable view of NORD because of how useful the book was,” he said.
Dr. Neilan had also received research funding from NORD, almost 20 years ago – a pilot grant for Cockayne syndrome, an extremely rare multisystem genetic disorder characterized by premature aging. “At any given time, there are only about 100 or so identified patients with this condition.”11
Pilot grants are awarded after NORD announces a request for proposals and the proposals received are scored by rare disease medical experts, Dr. Neilan explained. “Because this grant helped me research the condition and get my academic career moving, I always had a warm spot for NORD.”
Excellence in care. Dr. Neilan assumed his position at NORD to become involved with the NORD Rare Disease Centers of Excellence program, which he describes as encouraging “collaboration with, and between, dozens of leading medical centers around the country.”
Dr. Neilan is the first physician to work full time at NORD. “Taking the step of designating and directing collaboration amongst centers of excellence around the country seemed to require having a full-time physician on board,” he said, “so I decided to jump in.”
Ms. Kowalski elaborated: “NORD’s Rare Disease Centers of Excellence includes 11 different working groups to address the big problems that need to be solved in rare diseases: working collaboratively. [This] is sometimes rare in academic medicine, but necessary, especially when there aren’t many patients with a given condition.”
Since Dr. Neilan’s arrival, NORD has designated 40 institutions across the country as a NORD Rare Disease Centers of Excellence.12
Natural history research
NORD’s research department awards seed grants to academic investigators who are researching rare disorders and has built an online patient registry platform that helps other, disease-specific patient advocacy organizations conduct natural history studies.
Dr. Neilan said that the registry program was motivated by input from the FDA indicating that companies were sometimes trying to develop drugs to treat a rare disease before fully understanding the natural history of that disease.
“There was a perceived lack of enough natural history data,” Dr. Neilan explained, “so how could the effectiveness of the drug be measured? What would be a meaningful improvement?” NORD assists in making these rare disease foundations more “research ready” so that enough will be known about the disease for drug development “to have a greater chance of success.”
“There’s a lot of promise on the horizon with gene therapy, and the new platforms may accelerate the production of these therapies,” Ms. Kowalski said.
Registries are customized to each disease and foundation by experts, patients, and families involved with that particular disease and foundation. For example: An ongoing study on the NORD platform is a study of metachromatic leukodystrophy (MLD), an autosomal-recessive lysosomal disorder that results in a buildup of sulfatides, a major lipid group in serum, which lead to destruction of the myelin sheath and progressive demyelination of the nervous system.13
“[MLD] is a tragic disorder that can first present in late infancy and may progress rapidly over 6 months or so to the point that children lose much of their neurological functioning,” Dr. Neilan said.
The FDA funded NORD to run the HOME study,14,15 in which families can participate without visiting a research site in person. This was particularly valuable during the COVID-19 pandemic, when many studies were “forced to shift gears and see how much data could be collected if patients were afraid to come to the hospital or not allowed to go to a hospital for nonemergency visits,” Dr. Neilan said.
The HOME study was designed before the onset of the COVID-19 pandemic to reduce the burden on patients of participating in research. The trial became a trend-setter in the shift to what are known as decentralized trials, in which research can be conducted through video, using a tablet that NORD mails to the family.
“This is obviously much more convenient for families who no longer have to travel long distances to the few sites in the country – which are often hundreds or even thousands of miles away – that are studying the condition,” Dr. Neilan said. The decentralized trial model is being used with other conditions, as well.
“There are infantile, juvenile, and adult-onset forms of MLD, and the limited therapeutic options may involve bone-marrow transplant, which may be at least partially effective, as donor-derived bone marrow–derived cells can provide enzymes to protect the brain,” said Dr. Neilan. Gene therapy for MLD has also been developed and is approved in Europe, but not in the United States. “MLD is typical of conditions that often start early in childhood and are progressive, so that, sometimes, by the time the parent realizes that there’s a problem, too much damage has been done to the brain for much repair to take place. Prevention of further damage is easier than reversing an ongoing disease process, so early treatment is important.” That’s why the number of movements to expand newborn screening for various conditions, to identify them before symptoms develop, is increasing.
“That’s another area where NORD has historically been active – in encouraging newborn screening,” Dr. Neilan said.
Evolution of the ODA
Since 1983, “a number of amendments ... made the original [ODA] stronger or refined it in various ways,” said Mr. Saltonstall. NORD continues to “very carefully watch any attempts to change it, alter it, move it, take pieces away from it, or – some people say – to make it ‘better.’ To us, it’s a very important law.”
Orphan Drug Credit (ODC). Ms. Ross elaborated: “In recent years, Congress has considered significant changes to the Orphan Drug Credit, which is one of several critical incentives established by the ODA.” When established in 1983, the ODC provided sponsors of a drug with a 50% tax credit for qualified clinical testing expenses associated with developing an orphan drug.
“Unfortunately, despite fierce opposition from NORD and our army of membership organizations and grassroots advocates,” Ms. Ross said, “the Tax Cuts and Jobs Act of 2017 reduced the ODC from 50% to 25%. Given the significant amount of time it takes to conduct research and development into rare diseases, we still don’t have a good sense as to the impact of the ODC being reduced to 25%.”
However, efforts to further limit the availability of the ODC during debate around the Build Back Better framework in 2021 were ultimately defeated. That defeat was, in part, a result of NORD’s rare disease community’s advocacy,16 when no changes to the ODC were included in the Inflation Reduction Act.
Patient Assistance Program. In 1987, NORD’s multifaceted patient assistance program (serving today under the umbrella name RareCare17) was founded to help patients obtain lifesaving or life-sustaining medication that they could not otherwise afford, Ms. Ross said. This was based on an unmet need for patients living and struggling with a rare disease who didn’t have access to the care and treatment they needed. “There was no other foundation equipped to do this at the time. NORD came forward to develop the first program of its kind.”
The program provides medication, financial assistance with insurance premiums and copays, diagnostic testing assistance, and travel assistance for clinical trials or consultation with disease specialists. According to Ms. Ross, “today, NORD’s patient assistance program provides, on average, $30 million to $40 million in patient assistance annually to eligible patients and families.”
Pharmaceutical companies do contribute to the patient assistance program. “However, they’re in the dark as to how the money is allocated,” said Mr. Saltonstall. “For example, a given company might donate money for patients with a particular disease but won’t know if patients who have that disease will necessarily receive funds to use toward that company’s drug. The patient might receive assistance to take a drug made by a different company – a competitor.”
There are approximately 14 foundations around the country that have worked within the constraints of the Department of Health & Human Services Office of Inspector General, which established rules about how foundations must operate. Under the broader umbrella of NORD, these foundations also help pay coinsurance costs or provide drugs at no cost to patients who meet financial criteria.
An enduring movement
Despite the successes brought about by the ODA, the search for new rare disorder treatments is far from over. We know of more than 7,000 rare diseases; scientists discover more every year. Fewer than 5% of rare disorders have an FDA-approved treatment.
Similar to advancements made in other diseases, progress in rare disease care and treatments will continue to require an all-in approach to solve what is a looming and massive public health challenge.
As NORD founder Abbey S. Meyers wrote in her 2016 book, Orphan Drugs: A Global Crusade: “It was all of us working together that built an impregnable movement demanding a solution. In the end, with the help of government and a touch of Hollywood, the forces opposing us could not win.”
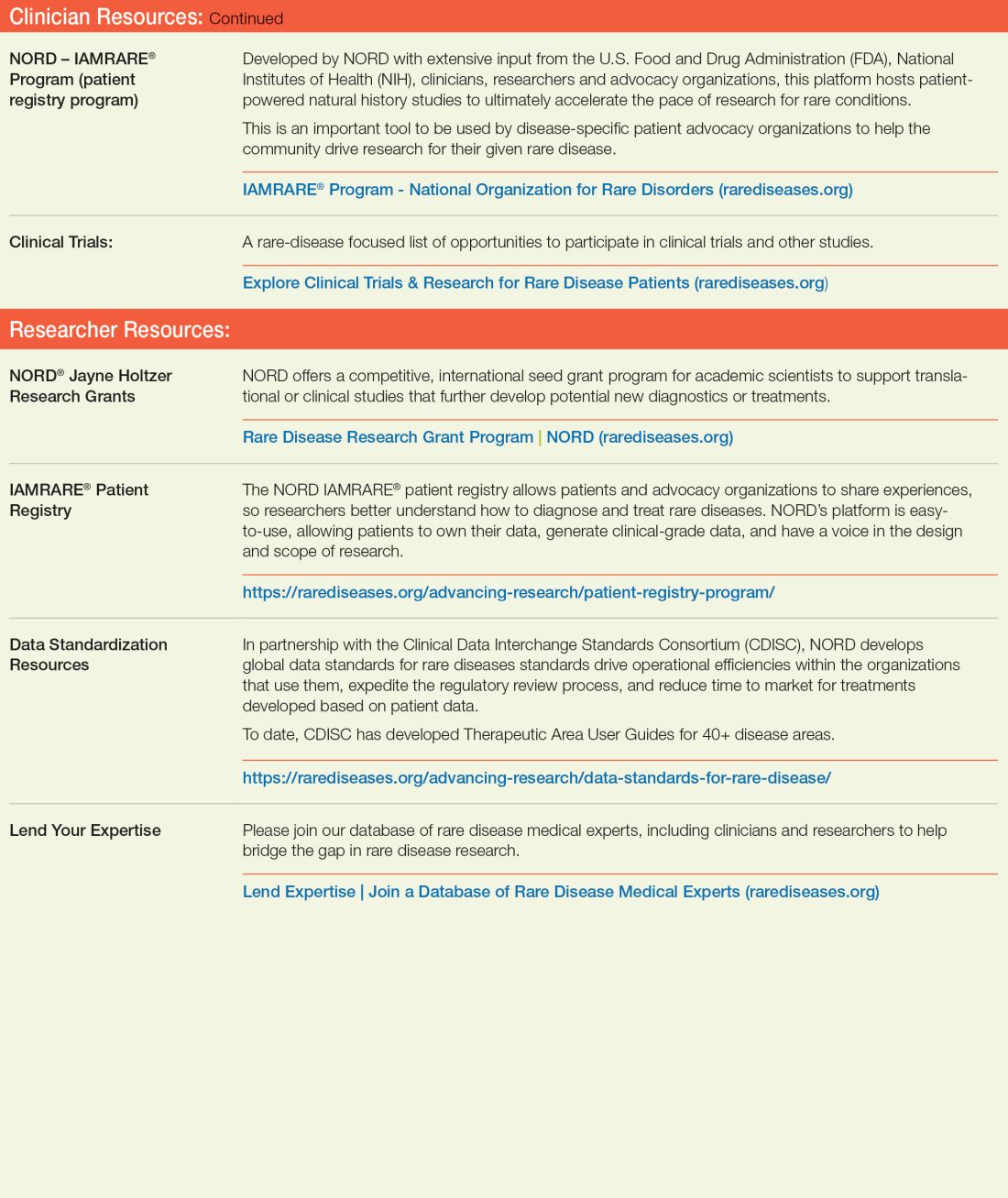
References
1. Rare Disease Day 2023 at IndoUSrare – Fireside Chat with Dr. Abbey S. Meyers. 2023 Mar 3. Indo US Organization for Rare Diseases. https://www.youtube.com/watch?v=fGTWUcQJPlU.
2. Mikami K. Soc Hist Med. 2019;32(3):609-30. doi: 10.1093/shm/hkx098.
3. National Organization for Rare Disorders. The Orphan Drug Act Turns 40: NORD Celebrates Its Impact on Rare Diseases. 2023 Jan 4. https://rarediseases.org/the-orphan-drug-act-turns-40-nord-celebrates-its-impact-on-rare-diseases. 4. Swann J. The story behind the Orphan Drug Act. US Food and Drug Administration. 2018 Feb 23. https://www.fda.gov/industry/fdas-rare-disease-day/story-behind-orphan-drug-act.
5. Roberts A-D and Wadhwa R. Orphan drug approval laws, in StatPearls (Internet). StatPearls Publishing. 2023 Jun 5. www.ncbi.nlm.nih.gov/books/NBK572052/#.
6. National Organization for Rare Disorders. Rare disease database. https://rarediseases.org/rare-diseases/.
7. National Organization for Rare Disorders. Rare disease video library. 2023 Jan 19. https://rarediseases.org/video-library/.
8. National Center for Advancing Translational Sciences. Rare disease research and resources. 2023 May 16. Accessed Sep. 17., 2023. https://ncats.nih.gov/rare-diseases.
9. Food and Drug Administration. Rare diseases team. 2023 Aug 29. https://www.fda.gov/about-fda/center-drug-evaluation-and-research-cder/rare-diseases-team.
10. National Organization for Rare Disorders. “NORD Guide to Rare Disorders,” 3rd edition. Philadelphia: Lippincott Williams & Wilkins, 2002.
11. National Organization for Rare Disorders. Cockayne syndrome. 2022 Jun 7. https://rarediseases.org/rare-diseases/cockayne-syndrome/.
12. National Organization for Rare Disorders. NORD Rare Disease Centers of Excellence. 2023 Jun 28. https://rarediseases.org/rare-disease-centers-of-excellence/.
13. National Organization for Rare Disorders. Metachromatic leukodystrophy. 2022 Mar 22. https://rarediseases.org/rare-diseases/metachromatic-leukodystrophy/#complete-report.
14. National Organization for Rare Disorders. The Natural History of Metachromatic Leukodystrophy Study. 2023 Feb 23. https://rarediseases.org/mld-home-study/.
15. The Natural History of Metachromatic Leukodystrophy Study (HOME Study). 2023 Jun 13. https://clinicaltrials.gov/study/NCT04628364?.
16. National Organization for Rare Disorders, Saltonstall PL. Letter to US Congress House Committee on Ways and Means. 2021 Sep 13. https://rarediseases.org/wp-content/uploads/2022/04/NORD_ODTC-Letter_FINAL.pdf.
17. National Organization for Rare Disorders. RareCare®: NORD’s patient assistance programs. 2022 Nov 1. https://rarediseases.org/wp-content/uploads/2022/04/NORD_ODTC-Letter_FINAL.pdf.
In 1976, Abbey S. Meyers, a mother from Connecticut, finally got a diagnosis for her son. He had been displaying “very bizarre symptoms,” Ms. Meyers said in an interview with IndoUSRare,1 but, eventually, at 8 years of age, he was given a diagnosis of Tourette syndrome.
“They tried some medicine to try to get him to sit still, but the drugs didn’t work – or if they did, they put him to sleep,” she recounted. “The teachers would be angry that he fell asleep in the classroom.”
Ms. Meyers consulted the late Arthur K. Shapiro, MD, at what was then named the Mount Sinai School of Medicine in New York. Dr. Shapiro was conducting a small clinical trial of pimozide, a drug under investigation for schizophrenia, for its utility in children with Tourette syndrome.
“The drug worked like magic,” Ms. Meyers reported. Her son’s symptoms were substantially reduced, without sedation. He was followed by Dr. Shapiro every 3 months, at which point he would receive a 90-day refill.
However, when her son turned 10 years of age, Dr. Shapiro was no longer able to provide refills: The Food and Drug Administration (FDA) had turned down the drug manufacturer’s application for approval of pimozide for a schizophrenia indication. The company opted not to pursue further development of the drug because it was not deemed profitable.2
Pimozide became unavailable in the United States. The fact that the drug was so promising for Tourette syndrome did not warrant further investment because Tourette syndrome affected a relatively small number of people.
“I was just devastated,” Ms. Meyers reported.
Springing into advocacy
Ms. Meyers, who was working with the Tourette Syndrome Association at the time (now the Tourette Association of America), contacted people from other rare disease organizations, including the National Huntington’s Disease Association (today the Huntington’s Disease Society of America) and the Paget Foundation (today part of the Bone Health and Osteoporosis Foundation). Those organizations were experiencing similar problems with drug companies that wouldn’t engage in research and development of drugs for patients who had a rare disorder.
“We realized we had to work together to get something done to solve this problem,” Ms. Meyers said.
The sense of urgency over this roadblock increased when another patient who was taking pimozide tried to get a supply of the drug from Canada and was blocked from doing so by customs officials at the airport because the drug was not FDA approved. Working with that patient’s mother, Ms. Meyers contacted U.S. Representative Henry A. Waxman (D-Calif.), who was chair of the Subcommittee on Health and the Environment of the House Energy & Commerce Committee.
Ms. Meyers thought that Congress needed Rep. Waxman’s support if it was going to get involved with this problem. “So, we got Henry Waxman and his staff familiar with the orphan drug problem.”
ODA: Breakthrough legislation
The impetus for the Orphan Drug Act (ODA) started in 1979 with an FDA task force report calling for measures to address what was labeled the “orphan drug problem.”3
In 1982, Rep. Waxman convened a hearing and invited several pharmaceutical companies to attend. They declined the invitation. Ms. Meyers testified at the hearing, which was covered by the Los Angeles Times, giving the issue notoriety.
The issue was also addressed in the popular television series Quincy, M.E. Episodes depicted challenges facing a patient with Tourette syndrome and a patient with myoclonus. Series star Jack Klugman testified before Congress about the need for legislation regarding the development of drugs targeting the treatment of rare diseases.4
Rep. Waxman became the bill’s primary House sponsor. The ODA was approved by the House of Representatives on Dec. 14, 1982.
The combined efforts of the advocacy coalition ultimately culminated in the original ODA being signed into law by President Ronald Reagan on Jan. 4, 1983. The ODA incentivized pharmaceutical companies to allot more resources toward research on and development and distribution of therapeutics for people with a rare disease who had, until that point, been “orphaned,” so to speak, by the medical and scientific community.5
What is it to be a ‘rare disorder’ or an ‘orphan drug’?
The ODA defines a rare disorder as either a condition that affects fewer than 200,000 people or a condition that affects more than 200,000 people but for which there is no reasonable expectation that a pharmaceutical company will recoup the cost of developing a drug by selling it.5
In an interview Peter L. Saltonstall, president and CEO of the National Organization for Rare Disorders, commended Ms. Meyers on her tireless work: “She went from being a mom to a powerful advocate who got thousands of people in D.C. moving Congress to a point where they felt passing the law was necessary. In fact, she was there when the bill was signed into law.”
The FDA can grant orphan drug approval for several categories of products. These include new molecular entities, already-approved drugs for which an additional indication has been designated, and new formulations of existing or established drugs.5
Orphan-drug designation includes tax credits for the developer-manufacturer, a waiver of the usual approval fees that the company must pay to the FDA, and 7 years’ market exclusivity, during which time the FDA cannot award approval of similar treatments for the same indication.
“This [designation] ensures that the company that developed the drug can retain the opportunity for profit,” explained Mr. Saltonstall. “Companies thought: ‘We can afford to do this now. And if we market it the right way and have exclusivity, we can recover some of our profits.’”
Before the ODA, 30 drugs had been approved by the FDA for orphan conditions. By the end of 2022, more than 880 drugs were FDA approved to treat hundreds of rare disorders.
“This just shows the motivation and how the process works,” Mr. Saltonstall said. In fact, almost 50% of novel drugs approved in 2022 by the FDA were an orphan product or had an orphan indication.
In addition to the impact on drug development in the United States, enactment of the ODA had a broader ripple effect, inspiring similar changes internationally in Europe, Australia, Singapore, Japan, and other regions.5
NORD is born
The creation of NORD was initiated by the same group of advocates who lobbied tirelessly for passage of the ODA – including Ms. Meyers, who served as president of the organization for many years. Heidi Ross, MPH, NORD’s vice president of policy and regulatory affairs, called these advocates “trailblazers.”
NORD was founded in May 1983. The organization included, at that time, 40-50 disease-specific organizations. Today, NORD membership comprises more than 330 patient advocacy groups.
“The goal was to be a voice for those organizations and help get them mobilized, help them get their 501(c)3 [status], help them develop their relationship with the FDA, and similar tasks,” Mr. Saltonstall said. “We continue this important work today as the patient groups play a central role in driving care, research, and policies for their given disease. Also, there’s strength in numbers. We call upon these groups and members to help advocate in Washington for policies that impact the greater rare disease community.”
The ODA launched 4 decades of innovation and change, with NORD strengthening the rare disorder community, which encompasses more than 30 million Americans.
“The organization exists to support people living with rare disorders and tries to improve their quality of life,” according to Katie Kowalski, MPH, NORD’s associate director of education.
Education. The role of Ms. Kowalski’s department is to “educate patients and caregivers, the general public, health care professionals, and students preparing for health care careers about rare conditions,” Ms. Kowalski said. The education department maintains NORD’s Rare Disease Database,6 which contains more than 1,300 reports about rare conditions. Plus, NORD’s Rare Disease Library archives videos about specific diseases and other topics of interest to the rare disease community, including genetic testing and gene therapy.Continuing medical education programs are available for health care providers.
Events. NORD hosts:
An annual Rare Diseases and Orphan Products Breakthrough Summit for various rare disease stakeholders, including global rare disease medical experts, policy makers, regulatory agencies, industry leaders, and patient community members.
An annual patient and family conference; the 2024 edition is scheduled for June 7-8, 2024, in Los Angeles.
Membership support. NORD’s membership department supports any advocacy organization that represents a rare
disorder. “Some [organizations] are more evolved and sophisticated and can do their own educational programming,” Ms. Kowalski said. “Others are fledgling, nascent organizations that may not have the staff or money for salaries. We try to support them, teach them how to budget and raise funds and form a board of directors.”
Advocacy. NORD has a policy department that works at state and federal levels to advocate for policies affecting patients with a rare disease. Mr. Saltonstall shared that NORD was responsible for setting up and helping put together the rare disease office at the National Institutes of Health and the FDA, and continues to foster a close relationship with those offices.8,9 “In fact,” he said, “nothing happens in Washington regarding rare diseases without our being consulted or at the table.”
Focus on the patient. Mr. Saltonstall assumed his role at NORD in 2008. “By then, many fundamental things had been mastered, and we were ready to take things to the next level,” he said. “There were opportunities to leverage the ODA to help patient organizations.”
“We’re one of the only nonprofit advocacy organizations I know of without industry on the board or as members,” Mr. Saltonstall said. “The organization is completely patient focused. Everything we do comes back to committees with patients who make the decisions and management who helps implement those decisions. This makes us unique. The fact that we’re independent makes Congress trust us to be the true voice of patients.”
Spotlight: Patient care and research
Edward Neilan, MD, PhD, recently joined NORD as chief medical and scientific officer. As a pediatrician, medical geneticist, and molecular biologist, Dr. Neilan became acquainted with NORD as far back as medical school and his residency, when he used a book called the NORD Guide to Rare Disorders to help him explain certain diseases to patients and families.10 “I had a favorable view of NORD because of how useful the book was,” he said.
Dr. Neilan had also received research funding from NORD, almost 20 years ago – a pilot grant for Cockayne syndrome, an extremely rare multisystem genetic disorder characterized by premature aging. “At any given time, there are only about 100 or so identified patients with this condition.”11
Pilot grants are awarded after NORD announces a request for proposals and the proposals received are scored by rare disease medical experts, Dr. Neilan explained. “Because this grant helped me research the condition and get my academic career moving, I always had a warm spot for NORD.”
Excellence in care. Dr. Neilan assumed his position at NORD to become involved with the NORD Rare Disease Centers of Excellence program, which he describes as encouraging “collaboration with, and between, dozens of leading medical centers around the country.”
Dr. Neilan is the first physician to work full time at NORD. “Taking the step of designating and directing collaboration amongst centers of excellence around the country seemed to require having a full-time physician on board,” he said, “so I decided to jump in.”
Ms. Kowalski elaborated: “NORD’s Rare Disease Centers of Excellence includes 11 different working groups to address the big problems that need to be solved in rare diseases: working collaboratively. [This] is sometimes rare in academic medicine, but necessary, especially when there aren’t many patients with a given condition.”
Since Dr. Neilan’s arrival, NORD has designated 40 institutions across the country as a NORD Rare Disease Centers of Excellence.12
Natural history research
NORD’s research department awards seed grants to academic investigators who are researching rare disorders and has built an online patient registry platform that helps other, disease-specific patient advocacy organizations conduct natural history studies.
Dr. Neilan said that the registry program was motivated by input from the FDA indicating that companies were sometimes trying to develop drugs to treat a rare disease before fully understanding the natural history of that disease.
“There was a perceived lack of enough natural history data,” Dr. Neilan explained, “so how could the effectiveness of the drug be measured? What would be a meaningful improvement?” NORD assists in making these rare disease foundations more “research ready” so that enough will be known about the disease for drug development “to have a greater chance of success.”
“There’s a lot of promise on the horizon with gene therapy, and the new platforms may accelerate the production of these therapies,” Ms. Kowalski said.
Registries are customized to each disease and foundation by experts, patients, and families involved with that particular disease and foundation. For example: An ongoing study on the NORD platform is a study of metachromatic leukodystrophy (MLD), an autosomal-recessive lysosomal disorder that results in a buildup of sulfatides, a major lipid group in serum, which lead to destruction of the myelin sheath and progressive demyelination of the nervous system.13
“[MLD] is a tragic disorder that can first present in late infancy and may progress rapidly over 6 months or so to the point that children lose much of their neurological functioning,” Dr. Neilan said.
The FDA funded NORD to run the HOME study,14,15 in which families can participate without visiting a research site in person. This was particularly valuable during the COVID-19 pandemic, when many studies were “forced to shift gears and see how much data could be collected if patients were afraid to come to the hospital or not allowed to go to a hospital for nonemergency visits,” Dr. Neilan said.
The HOME study was designed before the onset of the COVID-19 pandemic to reduce the burden on patients of participating in research. The trial became a trend-setter in the shift to what are known as decentralized trials, in which research can be conducted through video, using a tablet that NORD mails to the family.
“This is obviously much more convenient for families who no longer have to travel long distances to the few sites in the country – which are often hundreds or even thousands of miles away – that are studying the condition,” Dr. Neilan said. The decentralized trial model is being used with other conditions, as well.
“There are infantile, juvenile, and adult-onset forms of MLD, and the limited therapeutic options may involve bone-marrow transplant, which may be at least partially effective, as donor-derived bone marrow–derived cells can provide enzymes to protect the brain,” said Dr. Neilan. Gene therapy for MLD has also been developed and is approved in Europe, but not in the United States. “MLD is typical of conditions that often start early in childhood and are progressive, so that, sometimes, by the time the parent realizes that there’s a problem, too much damage has been done to the brain for much repair to take place. Prevention of further damage is easier than reversing an ongoing disease process, so early treatment is important.” That’s why the number of movements to expand newborn screening for various conditions, to identify them before symptoms develop, is increasing.
“That’s another area where NORD has historically been active – in encouraging newborn screening,” Dr. Neilan said.
Evolution of the ODA
Since 1983, “a number of amendments ... made the original [ODA] stronger or refined it in various ways,” said Mr. Saltonstall. NORD continues to “very carefully watch any attempts to change it, alter it, move it, take pieces away from it, or – some people say – to make it ‘better.’ To us, it’s a very important law.”
Orphan Drug Credit (ODC). Ms. Ross elaborated: “In recent years, Congress has considered significant changes to the Orphan Drug Credit, which is one of several critical incentives established by the ODA.” When established in 1983, the ODC provided sponsors of a drug with a 50% tax credit for qualified clinical testing expenses associated with developing an orphan drug.
“Unfortunately, despite fierce opposition from NORD and our army of membership organizations and grassroots advocates,” Ms. Ross said, “the Tax Cuts and Jobs Act of 2017 reduced the ODC from 50% to 25%. Given the significant amount of time it takes to conduct research and development into rare diseases, we still don’t have a good sense as to the impact of the ODC being reduced to 25%.”
However, efforts to further limit the availability of the ODC during debate around the Build Back Better framework in 2021 were ultimately defeated. That defeat was, in part, a result of NORD’s rare disease community’s advocacy,16 when no changes to the ODC were included in the Inflation Reduction Act.
Patient Assistance Program. In 1987, NORD’s multifaceted patient assistance program (serving today under the umbrella name RareCare17) was founded to help patients obtain lifesaving or life-sustaining medication that they could not otherwise afford, Ms. Ross said. This was based on an unmet need for patients living and struggling with a rare disease who didn’t have access to the care and treatment they needed. “There was no other foundation equipped to do this at the time. NORD came forward to develop the first program of its kind.”
The program provides medication, financial assistance with insurance premiums and copays, diagnostic testing assistance, and travel assistance for clinical trials or consultation with disease specialists. According to Ms. Ross, “today, NORD’s patient assistance program provides, on average, $30 million to $40 million in patient assistance annually to eligible patients and families.”
Pharmaceutical companies do contribute to the patient assistance program. “However, they’re in the dark as to how the money is allocated,” said Mr. Saltonstall. “For example, a given company might donate money for patients with a particular disease but won’t know if patients who have that disease will necessarily receive funds to use toward that company’s drug. The patient might receive assistance to take a drug made by a different company – a competitor.”
There are approximately 14 foundations around the country that have worked within the constraints of the Department of Health & Human Services Office of Inspector General, which established rules about how foundations must operate. Under the broader umbrella of NORD, these foundations also help pay coinsurance costs or provide drugs at no cost to patients who meet financial criteria.
An enduring movement
Despite the successes brought about by the ODA, the search for new rare disorder treatments is far from over. We know of more than 7,000 rare diseases; scientists discover more every year. Fewer than 5% of rare disorders have an FDA-approved treatment.
Similar to advancements made in other diseases, progress in rare disease care and treatments will continue to require an all-in approach to solve what is a looming and massive public health challenge.
As NORD founder Abbey S. Meyers wrote in her 2016 book, Orphan Drugs: A Global Crusade: “It was all of us working together that built an impregnable movement demanding a solution. In the end, with the help of government and a touch of Hollywood, the forces opposing us could not win.”
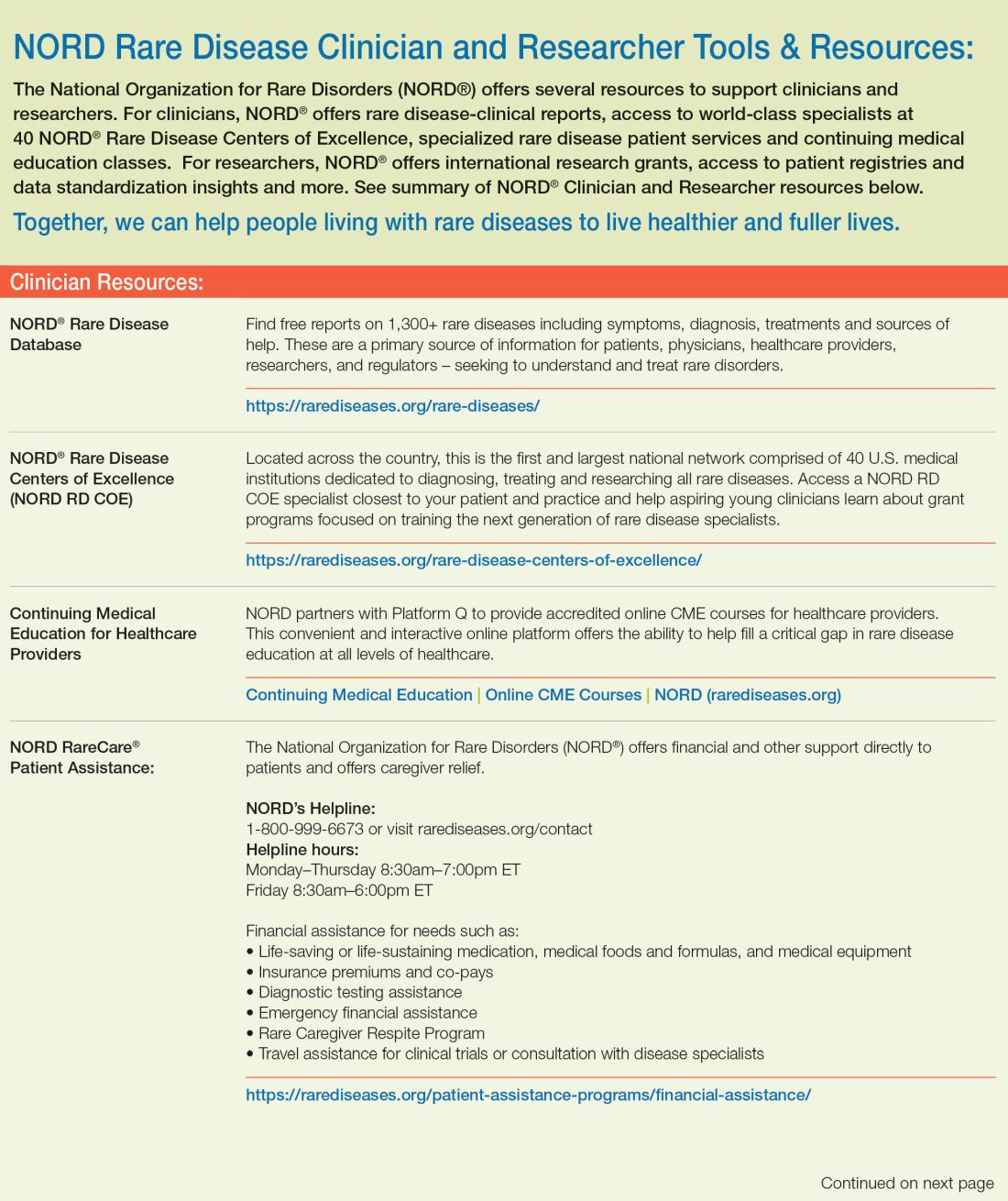
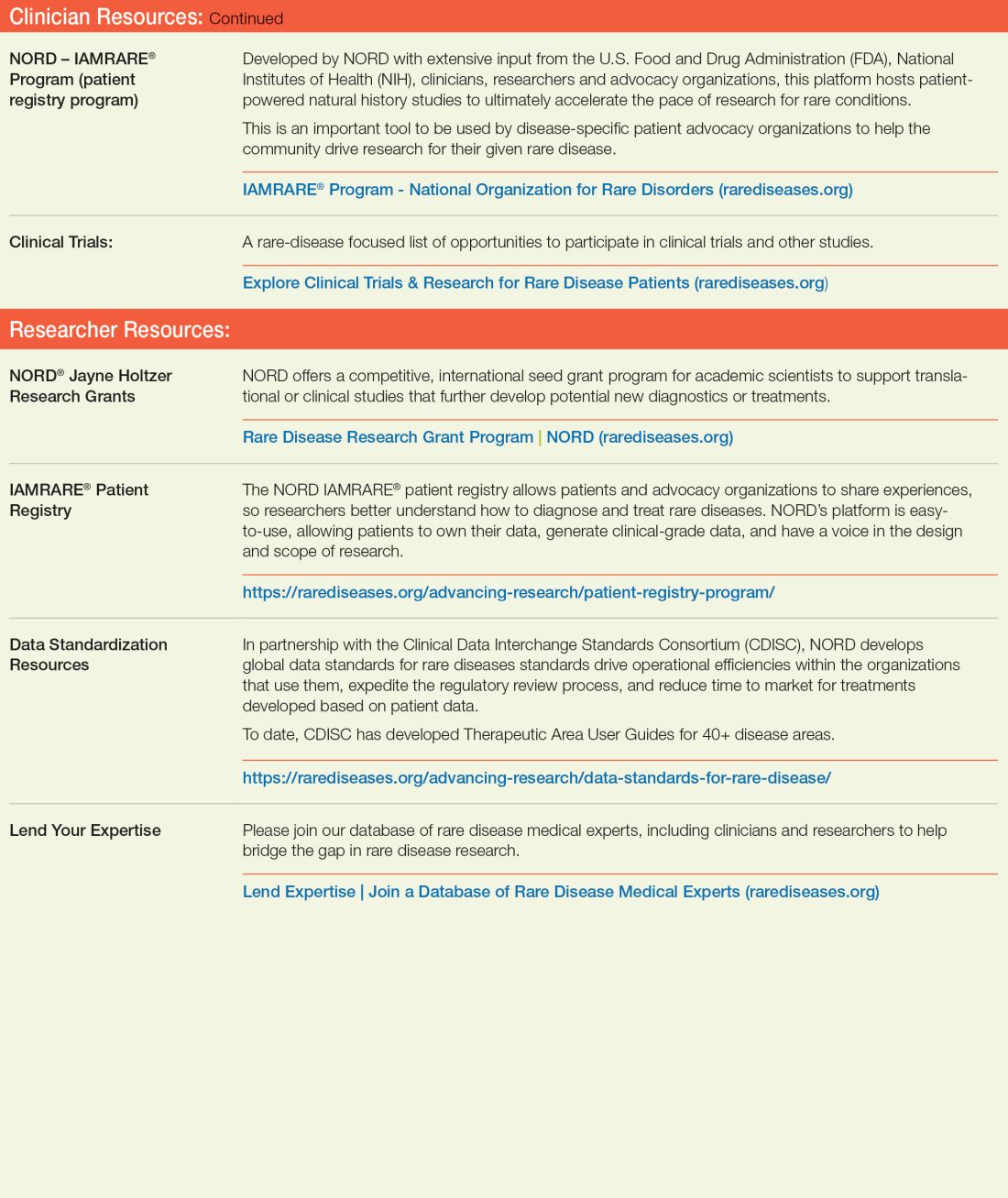
References
1. Rare Disease Day 2023 at IndoUSrare – Fireside Chat with Dr. Abbey S. Meyers. 2023 Mar 3. Indo US Organization for Rare Diseases. https://www.youtube.com/watch?v=fGTWUcQJPlU.
2. Mikami K. Soc Hist Med. 2019;32(3):609-30. doi: 10.1093/shm/hkx098.
3. National Organization for Rare Disorders. The Orphan Drug Act Turns 40: NORD Celebrates Its Impact on Rare Diseases. 2023 Jan 4. https://rarediseases.org/the-orphan-drug-act-turns-40-nord-celebrates-its-impact-on-rare-diseases. 4. Swann J. The story behind the Orphan Drug Act. US Food and Drug Administration. 2018 Feb 23. https://www.fda.gov/industry/fdas-rare-disease-day/story-behind-orphan-drug-act.
5. Roberts A-D and Wadhwa R. Orphan drug approval laws, in StatPearls (Internet). StatPearls Publishing. 2023 Jun 5. www.ncbi.nlm.nih.gov/books/NBK572052/#.
6. National Organization for Rare Disorders. Rare disease database. https://rarediseases.org/rare-diseases/.
7. National Organization for Rare Disorders. Rare disease video library. 2023 Jan 19. https://rarediseases.org/video-library/.
8. National Center for Advancing Translational Sciences. Rare disease research and resources. 2023 May 16. Accessed Sep. 17., 2023. https://ncats.nih.gov/rare-diseases.
9. Food and Drug Administration. Rare diseases team. 2023 Aug 29. https://www.fda.gov/about-fda/center-drug-evaluation-and-research-cder/rare-diseases-team.
10. National Organization for Rare Disorders. “NORD Guide to Rare Disorders,” 3rd edition. Philadelphia: Lippincott Williams & Wilkins, 2002.
11. National Organization for Rare Disorders. Cockayne syndrome. 2022 Jun 7. https://rarediseases.org/rare-diseases/cockayne-syndrome/.
12. National Organization for Rare Disorders. NORD Rare Disease Centers of Excellence. 2023 Jun 28. https://rarediseases.org/rare-disease-centers-of-excellence/.
13. National Organization for Rare Disorders. Metachromatic leukodystrophy. 2022 Mar 22. https://rarediseases.org/rare-diseases/metachromatic-leukodystrophy/#complete-report.
14. National Organization for Rare Disorders. The Natural History of Metachromatic Leukodystrophy Study. 2023 Feb 23. https://rarediseases.org/mld-home-study/.
15. The Natural History of Metachromatic Leukodystrophy Study (HOME Study). 2023 Jun 13. https://clinicaltrials.gov/study/NCT04628364?.
16. National Organization for Rare Disorders, Saltonstall PL. Letter to US Congress House Committee on Ways and Means. 2021 Sep 13. https://rarediseases.org/wp-content/uploads/2022/04/NORD_ODTC-Letter_FINAL.pdf.
17. National Organization for Rare Disorders. RareCare®: NORD’s patient assistance programs. 2022 Nov 1. https://rarediseases.org/wp-content/uploads/2022/04/NORD_ODTC-Letter_FINAL.pdf.
In 1976, Abbey S. Meyers, a mother from Connecticut, finally got a diagnosis for her son. He had been displaying “very bizarre symptoms,” Ms. Meyers said in an interview with IndoUSRare,1 but, eventually, at 8 years of age, he was given a diagnosis of Tourette syndrome.
“They tried some medicine to try to get him to sit still, but the drugs didn’t work – or if they did, they put him to sleep,” she recounted. “The teachers would be angry that he fell asleep in the classroom.”
Ms. Meyers consulted the late Arthur K. Shapiro, MD, at what was then named the Mount Sinai School of Medicine in New York. Dr. Shapiro was conducting a small clinical trial of pimozide, a drug under investigation for schizophrenia, for its utility in children with Tourette syndrome.
“The drug worked like magic,” Ms. Meyers reported. Her son’s symptoms were substantially reduced, without sedation. He was followed by Dr. Shapiro every 3 months, at which point he would receive a 90-day refill.
However, when her son turned 10 years of age, Dr. Shapiro was no longer able to provide refills: The Food and Drug Administration (FDA) had turned down the drug manufacturer’s application for approval of pimozide for a schizophrenia indication. The company opted not to pursue further development of the drug because it was not deemed profitable.2
Pimozide became unavailable in the United States. The fact that the drug was so promising for Tourette syndrome did not warrant further investment because Tourette syndrome affected a relatively small number of people.
“I was just devastated,” Ms. Meyers reported.
Springing into advocacy
Ms. Meyers, who was working with the Tourette Syndrome Association at the time (now the Tourette Association of America), contacted people from other rare disease organizations, including the National Huntington’s Disease Association (today the Huntington’s Disease Society of America) and the Paget Foundation (today part of the Bone Health and Osteoporosis Foundation). Those organizations were experiencing similar problems with drug companies that wouldn’t engage in research and development of drugs for patients who had a rare disorder.
“We realized we had to work together to get something done to solve this problem,” Ms. Meyers said.
The sense of urgency over this roadblock increased when another patient who was taking pimozide tried to get a supply of the drug from Canada and was blocked from doing so by customs officials at the airport because the drug was not FDA approved. Working with that patient’s mother, Ms. Meyers contacted U.S. Representative Henry A. Waxman (D-Calif.), who was chair of the Subcommittee on Health and the Environment of the House Energy & Commerce Committee.
Ms. Meyers thought that Congress needed Rep. Waxman’s support if it was going to get involved with this problem. “So, we got Henry Waxman and his staff familiar with the orphan drug problem.”
ODA: Breakthrough legislation
The impetus for the Orphan Drug Act (ODA) started in 1979 with an FDA task force report calling for measures to address what was labeled the “orphan drug problem.”3
In 1982, Rep. Waxman convened a hearing and invited several pharmaceutical companies to attend. They declined the invitation. Ms. Meyers testified at the hearing, which was covered by the Los Angeles Times, giving the issue notoriety.
The issue was also addressed in the popular television series Quincy, M.E. Episodes depicted challenges facing a patient with Tourette syndrome and a patient with myoclonus. Series star Jack Klugman testified before Congress about the need for legislation regarding the development of drugs targeting the treatment of rare diseases.4
Rep. Waxman became the bill’s primary House sponsor. The ODA was approved by the House of Representatives on Dec. 14, 1982.
The combined efforts of the advocacy coalition ultimately culminated in the original ODA being signed into law by President Ronald Reagan on Jan. 4, 1983. The ODA incentivized pharmaceutical companies to allot more resources toward research on and development and distribution of therapeutics for people with a rare disease who had, until that point, been “orphaned,” so to speak, by the medical and scientific community.5
What is it to be a ‘rare disorder’ or an ‘orphan drug’?
The ODA defines a rare disorder as either a condition that affects fewer than 200,000 people or a condition that affects more than 200,000 people but for which there is no reasonable expectation that a pharmaceutical company will recoup the cost of developing a drug by selling it.5
In an interview Peter L. Saltonstall, president and CEO of the National Organization for Rare Disorders, commended Ms. Meyers on her tireless work: “She went from being a mom to a powerful advocate who got thousands of people in D.C. moving Congress to a point where they felt passing the law was necessary. In fact, she was there when the bill was signed into law.”
The FDA can grant orphan drug approval for several categories of products. These include new molecular entities, already-approved drugs for which an additional indication has been designated, and new formulations of existing or established drugs.5
Orphan-drug designation includes tax credits for the developer-manufacturer, a waiver of the usual approval fees that the company must pay to the FDA, and 7 years’ market exclusivity, during which time the FDA cannot award approval of similar treatments for the same indication.
“This [designation] ensures that the company that developed the drug can retain the opportunity for profit,” explained Mr. Saltonstall. “Companies thought: ‘We can afford to do this now. And if we market it the right way and have exclusivity, we can recover some of our profits.’”
Before the ODA, 30 drugs had been approved by the FDA for orphan conditions. By the end of 2022, more than 880 drugs were FDA approved to treat hundreds of rare disorders.
“This just shows the motivation and how the process works,” Mr. Saltonstall said. In fact, almost 50% of novel drugs approved in 2022 by the FDA were an orphan product or had an orphan indication.
In addition to the impact on drug development in the United States, enactment of the ODA had a broader ripple effect, inspiring similar changes internationally in Europe, Australia, Singapore, Japan, and other regions.5
NORD is born
The creation of NORD was initiated by the same group of advocates who lobbied tirelessly for passage of the ODA – including Ms. Meyers, who served as president of the organization for many years. Heidi Ross, MPH, NORD’s vice president of policy and regulatory affairs, called these advocates “trailblazers.”
NORD was founded in May 1983. The organization included, at that time, 40-50 disease-specific organizations. Today, NORD membership comprises more than 330 patient advocacy groups.
“The goal was to be a voice for those organizations and help get them mobilized, help them get their 501(c)3 [status], help them develop their relationship with the FDA, and similar tasks,” Mr. Saltonstall said. “We continue this important work today as the patient groups play a central role in driving care, research, and policies for their given disease. Also, there’s strength in numbers. We call upon these groups and members to help advocate in Washington for policies that impact the greater rare disease community.”
The ODA launched 4 decades of innovation and change, with NORD strengthening the rare disorder community, which encompasses more than 30 million Americans.
“The organization exists to support people living with rare disorders and tries to improve their quality of life,” according to Katie Kowalski, MPH, NORD’s associate director of education.
Education. The role of Ms. Kowalski’s department is to “educate patients and caregivers, the general public, health care professionals, and students preparing for health care careers about rare conditions,” Ms. Kowalski said. The education department maintains NORD’s Rare Disease Database,6 which contains more than 1,300 reports about rare conditions. Plus, NORD’s Rare Disease Library archives videos about specific diseases and other topics of interest to the rare disease community, including genetic testing and gene therapy.Continuing medical education programs are available for health care providers.
Events. NORD hosts:
An annual Rare Diseases and Orphan Products Breakthrough Summit for various rare disease stakeholders, including global rare disease medical experts, policy makers, regulatory agencies, industry leaders, and patient community members.
An annual patient and family conference; the 2024 edition is scheduled for June 7-8, 2024, in Los Angeles.
Membership support. NORD’s membership department supports any advocacy organization that represents a rare
disorder. “Some [organizations] are more evolved and sophisticated and can do their own educational programming,” Ms. Kowalski said. “Others are fledgling, nascent organizations that may not have the staff or money for salaries. We try to support them, teach them how to budget and raise funds and form a board of directors.”
Advocacy. NORD has a policy department that works at state and federal levels to advocate for policies affecting patients with a rare disease. Mr. Saltonstall shared that NORD was responsible for setting up and helping put together the rare disease office at the National Institutes of Health and the FDA, and continues to foster a close relationship with those offices.8,9 “In fact,” he said, “nothing happens in Washington regarding rare diseases without our being consulted or at the table.”
Focus on the patient. Mr. Saltonstall assumed his role at NORD in 2008. “By then, many fundamental things had been mastered, and we were ready to take things to the next level,” he said. “There were opportunities to leverage the ODA to help patient organizations.”
“We’re one of the only nonprofit advocacy organizations I know of without industry on the board or as members,” Mr. Saltonstall said. “The organization is completely patient focused. Everything we do comes back to committees with patients who make the decisions and management who helps implement those decisions. This makes us unique. The fact that we’re independent makes Congress trust us to be the true voice of patients.”
Spotlight: Patient care and research
Edward Neilan, MD, PhD, recently joined NORD as chief medical and scientific officer. As a pediatrician, medical geneticist, and molecular biologist, Dr. Neilan became acquainted with NORD as far back as medical school and his residency, when he used a book called the NORD Guide to Rare Disorders to help him explain certain diseases to patients and families.10 “I had a favorable view of NORD because of how useful the book was,” he said.
Dr. Neilan had also received research funding from NORD, almost 20 years ago – a pilot grant for Cockayne syndrome, an extremely rare multisystem genetic disorder characterized by premature aging. “At any given time, there are only about 100 or so identified patients with this condition.”11
Pilot grants are awarded after NORD announces a request for proposals and the proposals received are scored by rare disease medical experts, Dr. Neilan explained. “Because this grant helped me research the condition and get my academic career moving, I always had a warm spot for NORD.”
Excellence in care. Dr. Neilan assumed his position at NORD to become involved with the NORD Rare Disease Centers of Excellence program, which he describes as encouraging “collaboration with, and between, dozens of leading medical centers around the country.”
Dr. Neilan is the first physician to work full time at NORD. “Taking the step of designating and directing collaboration amongst centers of excellence around the country seemed to require having a full-time physician on board,” he said, “so I decided to jump in.”
Ms. Kowalski elaborated: “NORD’s Rare Disease Centers of Excellence includes 11 different working groups to address the big problems that need to be solved in rare diseases: working collaboratively. [This] is sometimes rare in academic medicine, but necessary, especially when there aren’t many patients with a given condition.”
Since Dr. Neilan’s arrival, NORD has designated 40 institutions across the country as a NORD Rare Disease Centers of Excellence.12
Natural history research
NORD’s research department awards seed grants to academic investigators who are researching rare disorders and has built an online patient registry platform that helps other, disease-specific patient advocacy organizations conduct natural history studies.
Dr. Neilan said that the registry program was motivated by input from the FDA indicating that companies were sometimes trying to develop drugs to treat a rare disease before fully understanding the natural history of that disease.
“There was a perceived lack of enough natural history data,” Dr. Neilan explained, “so how could the effectiveness of the drug be measured? What would be a meaningful improvement?” NORD assists in making these rare disease foundations more “research ready” so that enough will be known about the disease for drug development “to have a greater chance of success.”
“There’s a lot of promise on the horizon with gene therapy, and the new platforms may accelerate the production of these therapies,” Ms. Kowalski said.
Registries are customized to each disease and foundation by experts, patients, and families involved with that particular disease and foundation. For example: An ongoing study on the NORD platform is a study of metachromatic leukodystrophy (MLD), an autosomal-recessive lysosomal disorder that results in a buildup of sulfatides, a major lipid group in serum, which lead to destruction of the myelin sheath and progressive demyelination of the nervous system.13
“[MLD] is a tragic disorder that can first present in late infancy and may progress rapidly over 6 months or so to the point that children lose much of their neurological functioning,” Dr. Neilan said.
The FDA funded NORD to run the HOME study,14,15 in which families can participate without visiting a research site in person. This was particularly valuable during the COVID-19 pandemic, when many studies were “forced to shift gears and see how much data could be collected if patients were afraid to come to the hospital or not allowed to go to a hospital for nonemergency visits,” Dr. Neilan said.
The HOME study was designed before the onset of the COVID-19 pandemic to reduce the burden on patients of participating in research. The trial became a trend-setter in the shift to what are known as decentralized trials, in which research can be conducted through video, using a tablet that NORD mails to the family.
“This is obviously much more convenient for families who no longer have to travel long distances to the few sites in the country – which are often hundreds or even thousands of miles away – that are studying the condition,” Dr. Neilan said. The decentralized trial model is being used with other conditions, as well.
“There are infantile, juvenile, and adult-onset forms of MLD, and the limited therapeutic options may involve bone-marrow transplant, which may be at least partially effective, as donor-derived bone marrow–derived cells can provide enzymes to protect the brain,” said Dr. Neilan. Gene therapy for MLD has also been developed and is approved in Europe, but not in the United States. “MLD is typical of conditions that often start early in childhood and are progressive, so that, sometimes, by the time the parent realizes that there’s a problem, too much damage has been done to the brain for much repair to take place. Prevention of further damage is easier than reversing an ongoing disease process, so early treatment is important.” That’s why the number of movements to expand newborn screening for various conditions, to identify them before symptoms develop, is increasing.
“That’s another area where NORD has historically been active – in encouraging newborn screening,” Dr. Neilan said.
Evolution of the ODA
Since 1983, “a number of amendments ... made the original [ODA] stronger or refined it in various ways,” said Mr. Saltonstall. NORD continues to “very carefully watch any attempts to change it, alter it, move it, take pieces away from it, or – some people say – to make it ‘better.’ To us, it’s a very important law.”
Orphan Drug Credit (ODC). Ms. Ross elaborated: “In recent years, Congress has considered significant changes to the Orphan Drug Credit, which is one of several critical incentives established by the ODA.” When established in 1983, the ODC provided sponsors of a drug with a 50% tax credit for qualified clinical testing expenses associated with developing an orphan drug.
“Unfortunately, despite fierce opposition from NORD and our army of membership organizations and grassroots advocates,” Ms. Ross said, “the Tax Cuts and Jobs Act of 2017 reduced the ODC from 50% to 25%. Given the significant amount of time it takes to conduct research and development into rare diseases, we still don’t have a good sense as to the impact of the ODC being reduced to 25%.”
However, efforts to further limit the availability of the ODC during debate around the Build Back Better framework in 2021 were ultimately defeated. That defeat was, in part, a result of NORD’s rare disease community’s advocacy,16 when no changes to the ODC were included in the Inflation Reduction Act.
Patient Assistance Program. In 1987, NORD’s multifaceted patient assistance program (serving today under the umbrella name RareCare17) was founded to help patients obtain lifesaving or life-sustaining medication that they could not otherwise afford, Ms. Ross said. This was based on an unmet need for patients living and struggling with a rare disease who didn’t have access to the care and treatment they needed. “There was no other foundation equipped to do this at the time. NORD came forward to develop the first program of its kind.”
The program provides medication, financial assistance with insurance premiums and copays, diagnostic testing assistance, and travel assistance for clinical trials or consultation with disease specialists. According to Ms. Ross, “today, NORD’s patient assistance program provides, on average, $30 million to $40 million in patient assistance annually to eligible patients and families.”
Pharmaceutical companies do contribute to the patient assistance program. “However, they’re in the dark as to how the money is allocated,” said Mr. Saltonstall. “For example, a given company might donate money for patients with a particular disease but won’t know if patients who have that disease will necessarily receive funds to use toward that company’s drug. The patient might receive assistance to take a drug made by a different company – a competitor.”
There are approximately 14 foundations around the country that have worked within the constraints of the Department of Health & Human Services Office of Inspector General, which established rules about how foundations must operate. Under the broader umbrella of NORD, these foundations also help pay coinsurance costs or provide drugs at no cost to patients who meet financial criteria.
An enduring movement
Despite the successes brought about by the ODA, the search for new rare disorder treatments is far from over. We know of more than 7,000 rare diseases; scientists discover more every year. Fewer than 5% of rare disorders have an FDA-approved treatment.
Similar to advancements made in other diseases, progress in rare disease care and treatments will continue to require an all-in approach to solve what is a looming and massive public health challenge.
As NORD founder Abbey S. Meyers wrote in her 2016 book, Orphan Drugs: A Global Crusade: “It was all of us working together that built an impregnable movement demanding a solution. In the end, with the help of government and a touch of Hollywood, the forces opposing us could not win.”
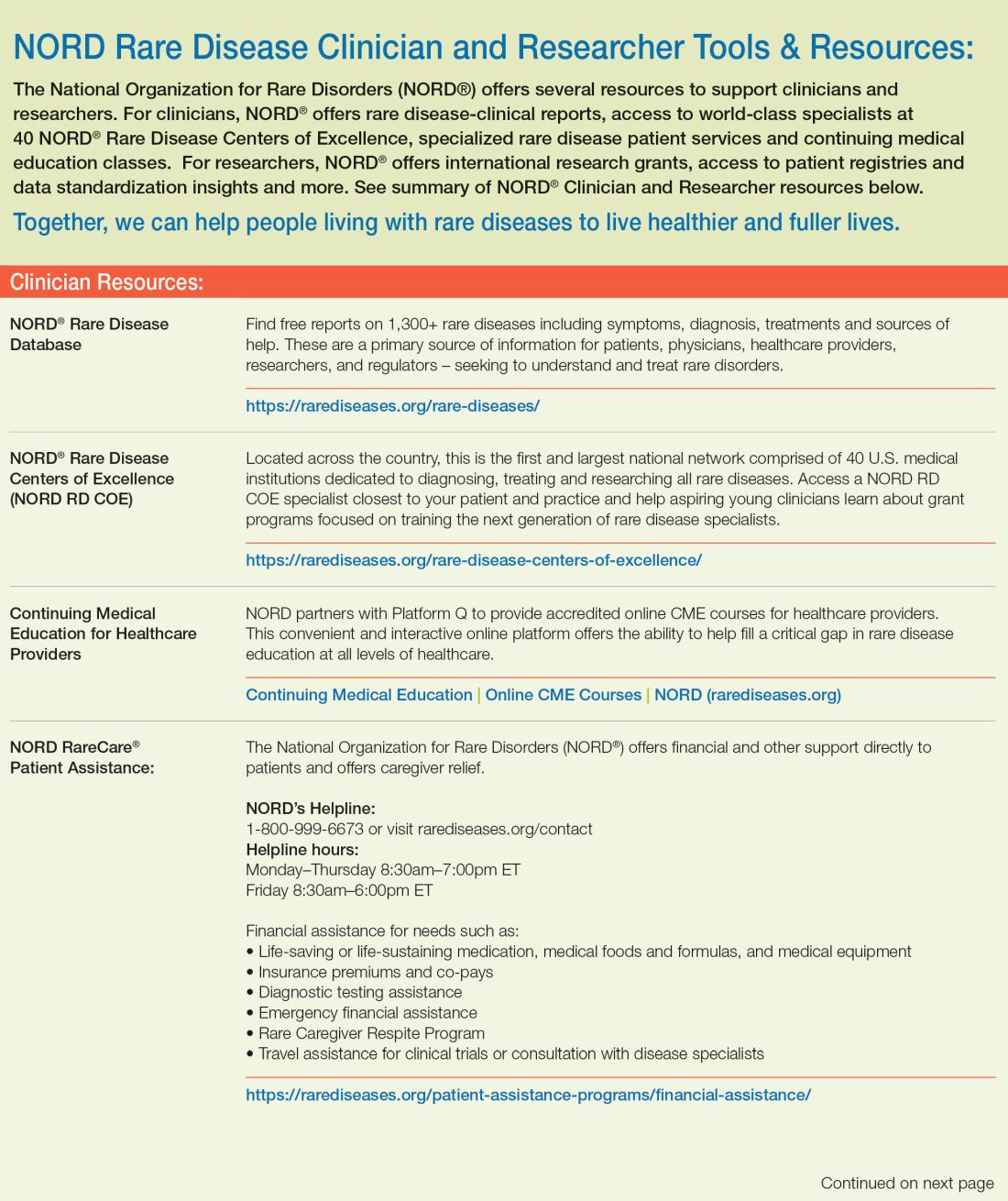
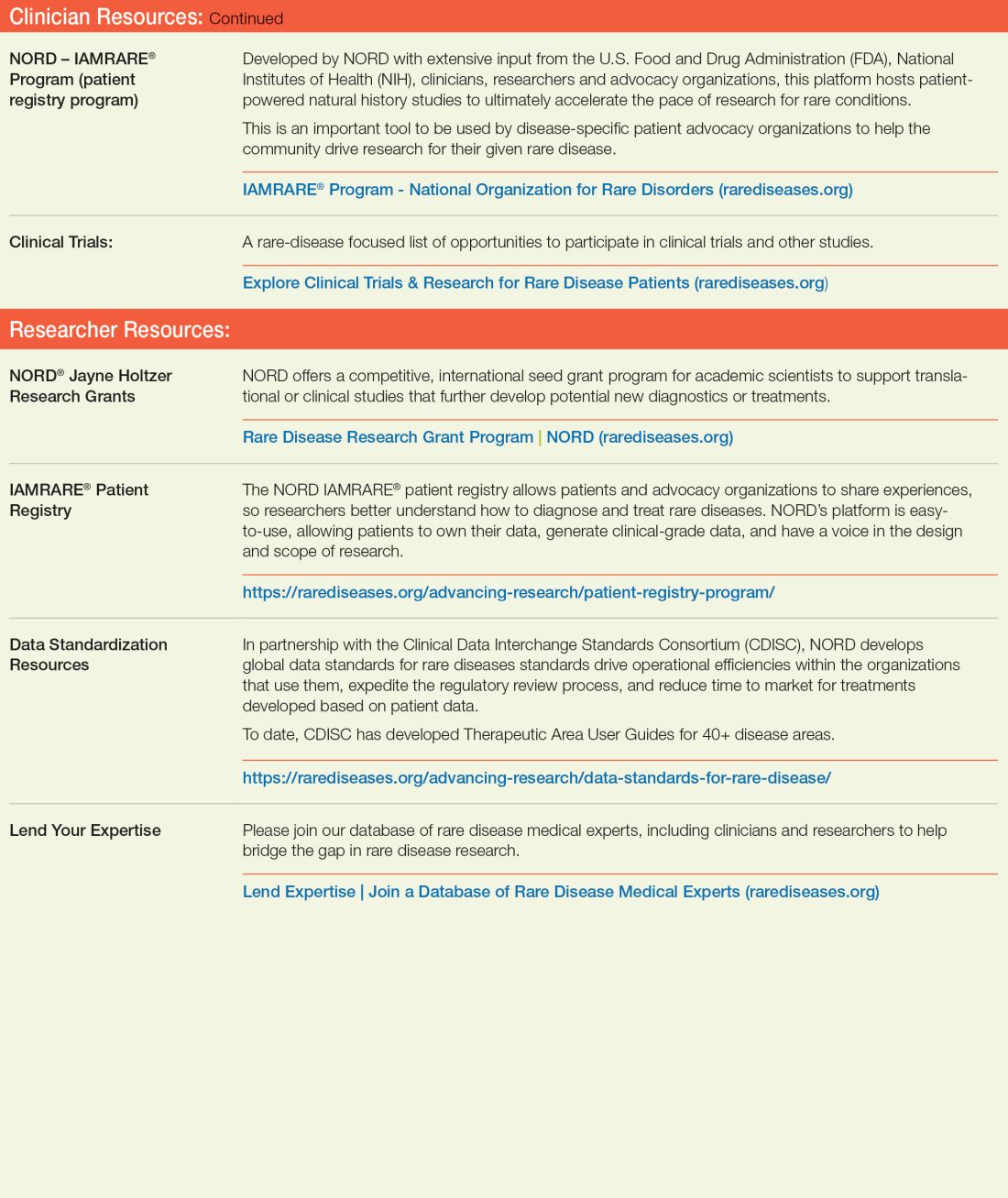
References
1. Rare Disease Day 2023 at IndoUSrare – Fireside Chat with Dr. Abbey S. Meyers. 2023 Mar 3. Indo US Organization for Rare Diseases. https://www.youtube.com/watch?v=fGTWUcQJPlU.
2. Mikami K. Soc Hist Med. 2019;32(3):609-30. doi: 10.1093/shm/hkx098.
3. National Organization for Rare Disorders. The Orphan Drug Act Turns 40: NORD Celebrates Its Impact on Rare Diseases. 2023 Jan 4. https://rarediseases.org/the-orphan-drug-act-turns-40-nord-celebrates-its-impact-on-rare-diseases. 4. Swann J. The story behind the Orphan Drug Act. US Food and Drug Administration. 2018 Feb 23. https://www.fda.gov/industry/fdas-rare-disease-day/story-behind-orphan-drug-act.
5. Roberts A-D and Wadhwa R. Orphan drug approval laws, in StatPearls (Internet). StatPearls Publishing. 2023 Jun 5. www.ncbi.nlm.nih.gov/books/NBK572052/#.
6. National Organization for Rare Disorders. Rare disease database. https://rarediseases.org/rare-diseases/.
7. National Organization for Rare Disorders. Rare disease video library. 2023 Jan 19. https://rarediseases.org/video-library/.
8. National Center for Advancing Translational Sciences. Rare disease research and resources. 2023 May 16. Accessed Sep. 17., 2023. https://ncats.nih.gov/rare-diseases.
9. Food and Drug Administration. Rare diseases team. 2023 Aug 29. https://www.fda.gov/about-fda/center-drug-evaluation-and-research-cder/rare-diseases-team.
10. National Organization for Rare Disorders. “NORD Guide to Rare Disorders,” 3rd edition. Philadelphia: Lippincott Williams & Wilkins, 2002.
11. National Organization for Rare Disorders. Cockayne syndrome. 2022 Jun 7. https://rarediseases.org/rare-diseases/cockayne-syndrome/.
12. National Organization for Rare Disorders. NORD Rare Disease Centers of Excellence. 2023 Jun 28. https://rarediseases.org/rare-disease-centers-of-excellence/.
13. National Organization for Rare Disorders. Metachromatic leukodystrophy. 2022 Mar 22. https://rarediseases.org/rare-diseases/metachromatic-leukodystrophy/#complete-report.
14. National Organization for Rare Disorders. The Natural History of Metachromatic Leukodystrophy Study. 2023 Feb 23. https://rarediseases.org/mld-home-study/.
15. The Natural History of Metachromatic Leukodystrophy Study (HOME Study). 2023 Jun 13. https://clinicaltrials.gov/study/NCT04628364?.
16. National Organization for Rare Disorders, Saltonstall PL. Letter to US Congress House Committee on Ways and Means. 2021 Sep 13. https://rarediseases.org/wp-content/uploads/2022/04/NORD_ODTC-Letter_FINAL.pdf.
17. National Organization for Rare Disorders. RareCare®: NORD’s patient assistance programs. 2022 Nov 1. https://rarediseases.org/wp-content/uploads/2022/04/NORD_ODTC-Letter_FINAL.pdf.
Rare disease roundup
Can a repurposed Parkinson’s drug slow ALS progression?
Ropinirole, a drug used for Parkinson’s disease, shows promise in slowing the progression of amyotrophic lateral sclerosis (ALS), early research suggests.
Investigators randomly assigned 20 individuals with sporadic ALS to receive either ropinirole or placebo for 24 weeks. During the double-blind period, there was no difference between the groups in terms of decline in functional status.
However, during a further open-label extension period, the ropinirole group showed significant suppression of functional decline and an average of an additional 7 months of progression-free survival.
The researchers were able to predict clinical responsiveness to ropinirole in vitro by analyzing motor neurons derived from participants’ stem cells.
The study was published online in Cell Stem Cell (2023 Jun 1. doi: 10.1016/j.stem.2023.04.017).
The trial was sponsored by K Pharma. The study drug, active drugs, and placebo were supplied free of charge by GlaxoSmithKline.
West Nile infections rising in the U.S.
Several signs are pointing to an impending surge in the number of human cases of West Nile virus in several regions of the United States. West Nile virus is spread by infected mosquitoes and currently there is no cure or virus-specific treatment. In rare cases, it can be deadly. It can infect humans, birds, horses, and other mammals.
West Nile Virus is the leading cause of mosquito-borne disease in the continental United States. As of Aug. 8, 126 human cases had been identified across 22 states, according to the Centers for Disease Control and Prevention.
“Particularly here in California, it’s peak risk right now,” said Vicki Kramer, PhD, chief of vector-borne diseases in the California Department of Public Health. She said scientists there are seeing higher mosquito and infected mosquito numbers.
Dead birds are tested for the virus and by Aug. 4, 181 of the 913 birds tested in California have been positive, three times the total testing positive by that time in 2022.
“Last year at this time, we had 60 positive dead birds out of 817 tested,” Dr. Kramer said.
Myasthenia gravis drug gets FDA nod
The Food and Drug Administration (FDA) has approved rozanolixizumab (Rystiggo, UCB) to treat adults with generalized myasthenia gravis (gMG) who are positive for anti-acetylcholine receptor (AChR) or anti–muscle-specific tyrosine kinase (MuSK) antibody, the drug’s manufacturer, UCB, has announced.
gMG is a rare autoimmune disease of the nerve muscle junction. Anti-AChR and anti-MuSK antibody-positive gMG are the two most common subtypes. Rozanolixizumab is the first FDA-approved treatment for adults with both subtypes.
Rozanolixizumab is a subcutaneous-infused humanized IgG4 monoclonal antibody that binds to the neonatal Fc
receptor (FcRn), reducing the concentration of pathogenic IgG autoantibodies.
U.S. approval is based on results of the phase 3
MycarinG study involving 200 patients with AChR or MuSK autoantibody-positive gMG. Patients were randomly assigned to one of two rozanolixizumab groups (7 mg/kg or 10 mg/kg) or placebo for 6 weeks.
As reported in The Lancet Neurology (2023 May. doi: 10.1016/S1474-4422[23]00077-7), rozanolixizumab led to statistically significant improvements in gMG-specific outcomes, including everyday activities such as breathing, talking, swallowing, and being able to rise from a chair.
Gene therapy promising for reversal of hereditary vision loss
An unapproved gene therapy for Leber hereditary optic neuropathy (LHON) led to a marked improvement in the eyesight of patients with a severe, progressive form of the disease who received the therapy as part of an early access program.
Results of a study of more than 60 patients who received lenadogene nolparvovec (Lumevoq, GenSight Biologics) as a unilateral or bilateral intravitreal injection showed that, at 2-year follow-up, 60% had experienced a clinically relevant improvement in the number of letters they could read on a visual acuity chart.
The results, said study presenter Chiara La Morgia, MD, PhD, IRCCS Istituto delle Scienze Neurologiche di Bologna (Italy), confirm in a “real-life setting” the efficacy and safety of the treatment as previously shown in clinical trials.
The findings were presented at the 2023 Congress of the European Academy of Neurology.
No funding was declared. Dr. La Morgia has relationships with Chiesi Farmaceutici, GenSight Biologics, Regulatory Pharma Net, Thenewway, Santhera Pharmaceuticals, First Class, Biologix, Stoke Therapeutics, and Reneo.
FDA OKs new drug for Fabry disease
The FDA has approved pegunigalsidase alfa (Elfabrio, Chiesi Global Rare Diseases/Protalix BioTherapeutics), an enzyme replacement therapy (ERT) to treat adults with Fabry disease.
Fabry disease is a rare inherited X-linked lysosomal disorder caused by a deficiency of the enzyme alpha-galactosidase A (GLA), which leads to the buildup of globotriaosylceramide (GL-3) in blood vessels, kidneys, heart, nerves, and other organs, increasing the risk for kidney failure, myocardial infarction, stroke, and other problems.
Elfabrio delivers a functional version of GLA. It is given by intravenous infusion every 2 weeks.
Evidence for safety, tolerability, and efficacy of Elfabrio stem from a comprehensive clinical program in more than 140 patients with up to 7.5 years of follow-up treatment.
It has been studied in both ERT-naive and ERT-experienced patients. In one head-to-head trial, Elfabrio was noninferior in safety and efficacy to agalsidase beta (Fabrazyme, Sanofi Genzyme), the companies said in a press statement announcing approval.
U.S. incidence, prevalence of myasthenia gravis are rising
There has been an increase in the incidence and prevalence of myasthenia gravis in the United States, an analysis of new claims data shows. Investigators speculate the rise of this rare disorder may be caused by “increased diagnosis and more awareness of the disease over time, which has been shown in several studies,” said study investigator Ema Rodrigues, DSc, MPH, with Alexion Pharmaceuticals, Boston.
Dr. Rodrigues presented her research at the 2023 annual meeting of the American Academy of Neurology.
Funding for the study was provided by Alexion, AstraZeneca Rare
Disease. Dr. Rodrigues receives compensation and owns stock as an employee of Alexion, AstraZeneca Rare Diseases.
Novel agent offers hope for hereditary ATTR polyneuropathy in pivotal trial
The investigational agent eplontersen (Ionis Pharmaceuticals/AstraZeneca) halted neuropathy disease progression and improved neuropathy impairment and quality of life for patients with hereditary transthyretin-mediated amyloid polyneuropathy (ATTRv-PN) in a pivotal phase 3 trial.
Eplontersen led to “clinically and statistically significant benefits at week 66 with an early and rapid sustained reduction in serum TTR [transthyretin] concentration, a halting of the progression of the neuropathy impairment, and a trend to improvement in quality of life,” said principal investigator Sami Khella, MD, professor of clinical neurology at the University of Pennsylvania, Philadelphia.
Dr. Khella reported final data from the NEURO-TTRansform trial at the annual meeting of the American Academy of Neurology.
The FDA has accepted a new drug application for eplontersen for the treatment of ATTRv-PN. The drug has a Prescription Drug User Fee Act date of Dec. 22, 2023. Eplontersen has orphan drug designation in the United States.
The study was sponsored by Ionis Pharmaceuticals. Dr. Khella has relationships with Ionis, Pfizer, Alnylam, and Eidos.
FDA gives fast-track approval to new ALS drug
The FDA has approved the first treatment that takes a genetics-based approach to slowing or stopping the progression of a rare form of amyotrophic lateral sclerosis (ALS).
The FDA fast-tracked the approval of Qalsody (Biogen) based on early trial results. The agency said in a news release that its decision was based on the demonstrated ability of the drug to reduce a protein in the blood that is a sign of degeneration of brain and nerve cells.
Qalsody is given to people via a spinal injection, with an initial course of three injections every 2 weeks. People then get the injection once every 28 days.
The new treatment is approved only for people with SOD1-ALS, which is known for a genetic mutation. While ALS affects up to 32,000 people in the United States, just 2% of people with ALS have the SOD1 gene mutation. The FDA says the number of people in the United States who could use Qalsody is about 500.
FDA OKs first treatment for Friedreich ataxia
The FDA has approved the first treatment for the neurodegenerative disorder Friedreich ataxia for use in adults and adolescents aged 16 and older.
The recommended dose of omaveloxolone (Skyclarys, Reata Pharmaceuticals) is 150 mg (three capsules) taken orally once daily on an empty stomach.
The FDA approval of omaveloxolone was supported by a randomized double-blind, placebo-controlled study comprising 103 patients with genetically confirmed Friedreich ataxia and baseline modified Friedreich Ataxia Rating Scale (mFARS) scores between 20 and 80.
Treatment with the novel medication led to statistically significant lower mFARS scores, signifying less impairment, relative to placebo, at week 48. The placebo-corrected difference between the two groups was –2.41 points (P = .0138).
Omaveloxolone received priority review and had orphan drug, fast track, and rare pediatric disease designations.
FDA OKs first drug for Rett syndrome
The FDA has approved trofinetide oral solution (Daybue, Acadia Pharmaceuticals) as the first treatment of Rett syndrome in adults and children aged 2 years and older.
Trofinetide is a synthetic analogue of the amino-terminal tripeptide of insulinlike growth factor-1, which occurs naturally in the brain. The drug is designed to treat the core symptoms of Rett syndrome by potentially reducing neuroinflammation and supporting synaptic function.
The approval of trofinetide was supported by results from the pivotal phase 3 LAVENDER study that tested the efficacy and safety of trofinetide versus placebo in 187 female patients with Rett syndrome, aged 5-20 years.
More data back Guillain-Barré risk with Janssen COVID shot
New surveillance data from the Vaccine Adverse Event Reporting System (VAERS) back previous findings of increased risk for Guillain-Barré syndrome (GBS) after receiving the Janssen COVID-19 vaccine (Ad26.COV2.S).
Over 14 months, GBS reporting rates within 21 and 42 days of administration of Janssen’s replication-incompetent adenoviral vector vaccine were approximately 9-12 times higher than after administration of the Pfizer-BioNTech (BNT162b2) or the Moderna (mRNA-1273) mRNA COVID vaccines.
Additionally, observed GBS cases after the Janssen shot were two to three times greater than expected, based on background rates within 21 and 42 days of vaccination.
Conversely, and confirming prior data, there was no increased risk for GBS with the Pfizer or Moderna vaccines and no significant difference between observed and expected numbers of GBS cases after either mRNA COVID-19 vaccine.
The findings were published online in JAMA Network Open (2023 Feb 1. doi: 10.1001/jamanetworkopen.2022.53845).
Diazepam nasal spray effective in Lennox-Gastaut syndrome
A new analysis of data from a phase 3 clinical trial suggests that an inhaled diazepam nasal spray (Valtoco, Neurelis) works about as well among patients with Lennox-Gastaut syndrome (LGS) as it does with other patients with pediatric encephalopathies.
LGS is a severe form of epilepsy that generally begins in early childhood and has a poor prognosis and seizures that are often treatment refractory. The findings of the analysis should be encouraging to physicians who may view patients with LGS as not benefiting from treatment, said Daniel C. Tarquinio, DO, who presented the results at the 2022 annual meeting of the Child Neurology Society.
Novel cannabis oil curbs tics in severe Tourette syndrome
An oral oil containing tetrahydrocannabinol (THC) and cannabidiol (CBD) led to a significant and meaningful reduction in motor and vocal tics in patients with severe Tourette syndrome, results of a double-blind, placebo-controlled, crossover study showed.
“In a methodologically robust manner (and independent of any drug company sponsorship), we provide evidence for the effectiveness of repeated dosing with THC:CBD versus placebo in tic
suppression, as well as reduction of comorbid anxiety and obsessive-compulsive disorder in severe Tourette syndrome,” neuropsychiatrist and lead investigator Philip Mosley, PhD, said in an interview.
The results offer support to people with Tourette syndrome who “want to approach their doctor to try medicinal cannabis when other drugs have not worked or are intolerable,” said
Dr. Mosley, of the Wesley Research Institute and QIMR Berghofer Medical Research Institute, Herston, Australia.
The study was published online in NEJM Evidence (2023 Jun 7. doi: 10.1056/EVIDoa2300012).
Twenty-two adults (mean age, 31 years) with severe Tourette syndrome received THC:CBD oil titrated upward over 6 weeks to a daily dose of 20 mg of THC and 20 mg of CBD, followed by a 6-week course of placebo (or vice versa). Six participants had not previously used cannabis.
The primary outcome was the total tic score on the Yale Global Tic Severity Scale (YGTSS; range, 0-50 with higher scores = greater tic severity).
The mean baseline YGTSS total tic score was 35.7. At 6 weeks, the reduction in total tic score was 8.9 with THC:CBD versus 2.5 with placebo.
A linear mixed-effects model (intention to treat) showed a significant interaction of treatment and visit number (P = .008), indicating a greater decrease (improvement) in tic score over time with THC:CBD, the study team reported.
On average, the magnitude of the tic reduction was “moderate” and comparable with the effect observed with existing treatments such as antipsychotic agents, the investigators noted.
The study was funded by the Wesley Medical Research Institute, Brisbane, and the Lambert Initiative for Cannabinoid Therapeutics, a philanthropically funded research organization at the University of Sydney, Australia.
Dr. Mosley reported no relevant financial relationships.
Can a repurposed Parkinson’s drug slow ALS progression?
Ropinirole, a drug used for Parkinson’s disease, shows promise in slowing the progression of amyotrophic lateral sclerosis (ALS), early research suggests.
Investigators randomly assigned 20 individuals with sporadic ALS to receive either ropinirole or placebo for 24 weeks. During the double-blind period, there was no difference between the groups in terms of decline in functional status.
However, during a further open-label extension period, the ropinirole group showed significant suppression of functional decline and an average of an additional 7 months of progression-free survival.
The researchers were able to predict clinical responsiveness to ropinirole in vitro by analyzing motor neurons derived from participants’ stem cells.
The study was published online in Cell Stem Cell (2023 Jun 1. doi: 10.1016/j.stem.2023.04.017).
The trial was sponsored by K Pharma. The study drug, active drugs, and placebo were supplied free of charge by GlaxoSmithKline.
West Nile infections rising in the U.S.
Several signs are pointing to an impending surge in the number of human cases of West Nile virus in several regions of the United States. West Nile virus is spread by infected mosquitoes and currently there is no cure or virus-specific treatment. In rare cases, it can be deadly. It can infect humans, birds, horses, and other mammals.
West Nile Virus is the leading cause of mosquito-borne disease in the continental United States. As of Aug. 8, 126 human cases had been identified across 22 states, according to the Centers for Disease Control and Prevention.
“Particularly here in California, it’s peak risk right now,” said Vicki Kramer, PhD, chief of vector-borne diseases in the California Department of Public Health. She said scientists there are seeing higher mosquito and infected mosquito numbers.
Dead birds are tested for the virus and by Aug. 4, 181 of the 913 birds tested in California have been positive, three times the total testing positive by that time in 2022.
“Last year at this time, we had 60 positive dead birds out of 817 tested,” Dr. Kramer said.
Myasthenia gravis drug gets FDA nod
The Food and Drug Administration (FDA) has approved rozanolixizumab (Rystiggo, UCB) to treat adults with generalized myasthenia gravis (gMG) who are positive for anti-acetylcholine receptor (AChR) or anti–muscle-specific tyrosine kinase (MuSK) antibody, the drug’s manufacturer, UCB, has announced.
gMG is a rare autoimmune disease of the nerve muscle junction. Anti-AChR and anti-MuSK antibody-positive gMG are the two most common subtypes. Rozanolixizumab is the first FDA-approved treatment for adults with both subtypes.
Rozanolixizumab is a subcutaneous-infused humanized IgG4 monoclonal antibody that binds to the neonatal Fc
receptor (FcRn), reducing the concentration of pathogenic IgG autoantibodies.
U.S. approval is based on results of the phase 3
MycarinG study involving 200 patients with AChR or MuSK autoantibody-positive gMG. Patients were randomly assigned to one of two rozanolixizumab groups (7 mg/kg or 10 mg/kg) or placebo for 6 weeks.
As reported in The Lancet Neurology (2023 May. doi: 10.1016/S1474-4422[23]00077-7), rozanolixizumab led to statistically significant improvements in gMG-specific outcomes, including everyday activities such as breathing, talking, swallowing, and being able to rise from a chair.
Gene therapy promising for reversal of hereditary vision loss
An unapproved gene therapy for Leber hereditary optic neuropathy (LHON) led to a marked improvement in the eyesight of patients with a severe, progressive form of the disease who received the therapy as part of an early access program.
Results of a study of more than 60 patients who received lenadogene nolparvovec (Lumevoq, GenSight Biologics) as a unilateral or bilateral intravitreal injection showed that, at 2-year follow-up, 60% had experienced a clinically relevant improvement in the number of letters they could read on a visual acuity chart.
The results, said study presenter Chiara La Morgia, MD, PhD, IRCCS Istituto delle Scienze Neurologiche di Bologna (Italy), confirm in a “real-life setting” the efficacy and safety of the treatment as previously shown in clinical trials.
The findings were presented at the 2023 Congress of the European Academy of Neurology.
No funding was declared. Dr. La Morgia has relationships with Chiesi Farmaceutici, GenSight Biologics, Regulatory Pharma Net, Thenewway, Santhera Pharmaceuticals, First Class, Biologix, Stoke Therapeutics, and Reneo.
FDA OKs new drug for Fabry disease
The FDA has approved pegunigalsidase alfa (Elfabrio, Chiesi Global Rare Diseases/Protalix BioTherapeutics), an enzyme replacement therapy (ERT) to treat adults with Fabry disease.
Fabry disease is a rare inherited X-linked lysosomal disorder caused by a deficiency of the enzyme alpha-galactosidase A (GLA), which leads to the buildup of globotriaosylceramide (GL-3) in blood vessels, kidneys, heart, nerves, and other organs, increasing the risk for kidney failure, myocardial infarction, stroke, and other problems.
Elfabrio delivers a functional version of GLA. It is given by intravenous infusion every 2 weeks.
Evidence for safety, tolerability, and efficacy of Elfabrio stem from a comprehensive clinical program in more than 140 patients with up to 7.5 years of follow-up treatment.
It has been studied in both ERT-naive and ERT-experienced patients. In one head-to-head trial, Elfabrio was noninferior in safety and efficacy to agalsidase beta (Fabrazyme, Sanofi Genzyme), the companies said in a press statement announcing approval.
U.S. incidence, prevalence of myasthenia gravis are rising
There has been an increase in the incidence and prevalence of myasthenia gravis in the United States, an analysis of new claims data shows. Investigators speculate the rise of this rare disorder may be caused by “increased diagnosis and more awareness of the disease over time, which has been shown in several studies,” said study investigator Ema Rodrigues, DSc, MPH, with Alexion Pharmaceuticals, Boston.
Dr. Rodrigues presented her research at the 2023 annual meeting of the American Academy of Neurology.
Funding for the study was provided by Alexion, AstraZeneca Rare
Disease. Dr. Rodrigues receives compensation and owns stock as an employee of Alexion, AstraZeneca Rare Diseases.
Novel agent offers hope for hereditary ATTR polyneuropathy in pivotal trial
The investigational agent eplontersen (Ionis Pharmaceuticals/AstraZeneca) halted neuropathy disease progression and improved neuropathy impairment and quality of life for patients with hereditary transthyretin-mediated amyloid polyneuropathy (ATTRv-PN) in a pivotal phase 3 trial.
Eplontersen led to “clinically and statistically significant benefits at week 66 with an early and rapid sustained reduction in serum TTR [transthyretin] concentration, a halting of the progression of the neuropathy impairment, and a trend to improvement in quality of life,” said principal investigator Sami Khella, MD, professor of clinical neurology at the University of Pennsylvania, Philadelphia.
Dr. Khella reported final data from the NEURO-TTRansform trial at the annual meeting of the American Academy of Neurology.
The FDA has accepted a new drug application for eplontersen for the treatment of ATTRv-PN. The drug has a Prescription Drug User Fee Act date of Dec. 22, 2023. Eplontersen has orphan drug designation in the United States.
The study was sponsored by Ionis Pharmaceuticals. Dr. Khella has relationships with Ionis, Pfizer, Alnylam, and Eidos.
FDA gives fast-track approval to new ALS drug
The FDA has approved the first treatment that takes a genetics-based approach to slowing or stopping the progression of a rare form of amyotrophic lateral sclerosis (ALS).
The FDA fast-tracked the approval of Qalsody (Biogen) based on early trial results. The agency said in a news release that its decision was based on the demonstrated ability of the drug to reduce a protein in the blood that is a sign of degeneration of brain and nerve cells.
Qalsody is given to people via a spinal injection, with an initial course of three injections every 2 weeks. People then get the injection once every 28 days.
The new treatment is approved only for people with SOD1-ALS, which is known for a genetic mutation. While ALS affects up to 32,000 people in the United States, just 2% of people with ALS have the SOD1 gene mutation. The FDA says the number of people in the United States who could use Qalsody is about 500.
FDA OKs first treatment for Friedreich ataxia
The FDA has approved the first treatment for the neurodegenerative disorder Friedreich ataxia for use in adults and adolescents aged 16 and older.
The recommended dose of omaveloxolone (Skyclarys, Reata Pharmaceuticals) is 150 mg (three capsules) taken orally once daily on an empty stomach.
The FDA approval of omaveloxolone was supported by a randomized double-blind, placebo-controlled study comprising 103 patients with genetically confirmed Friedreich ataxia and baseline modified Friedreich Ataxia Rating Scale (mFARS) scores between 20 and 80.
Treatment with the novel medication led to statistically significant lower mFARS scores, signifying less impairment, relative to placebo, at week 48. The placebo-corrected difference between the two groups was –2.41 points (P = .0138).
Omaveloxolone received priority review and had orphan drug, fast track, and rare pediatric disease designations.
FDA OKs first drug for Rett syndrome
The FDA has approved trofinetide oral solution (Daybue, Acadia Pharmaceuticals) as the first treatment of Rett syndrome in adults and children aged 2 years and older.
Trofinetide is a synthetic analogue of the amino-terminal tripeptide of insulinlike growth factor-1, which occurs naturally in the brain. The drug is designed to treat the core symptoms of Rett syndrome by potentially reducing neuroinflammation and supporting synaptic function.
The approval of trofinetide was supported by results from the pivotal phase 3 LAVENDER study that tested the efficacy and safety of trofinetide versus placebo in 187 female patients with Rett syndrome, aged 5-20 years.
More data back Guillain-Barré risk with Janssen COVID shot
New surveillance data from the Vaccine Adverse Event Reporting System (VAERS) back previous findings of increased risk for Guillain-Barré syndrome (GBS) after receiving the Janssen COVID-19 vaccine (Ad26.COV2.S).
Over 14 months, GBS reporting rates within 21 and 42 days of administration of Janssen’s replication-incompetent adenoviral vector vaccine were approximately 9-12 times higher than after administration of the Pfizer-BioNTech (BNT162b2) or the Moderna (mRNA-1273) mRNA COVID vaccines.
Additionally, observed GBS cases after the Janssen shot were two to three times greater than expected, based on background rates within 21 and 42 days of vaccination.
Conversely, and confirming prior data, there was no increased risk for GBS with the Pfizer or Moderna vaccines and no significant difference between observed and expected numbers of GBS cases after either mRNA COVID-19 vaccine.
The findings were published online in JAMA Network Open (2023 Feb 1. doi: 10.1001/jamanetworkopen.2022.53845).
Diazepam nasal spray effective in Lennox-Gastaut syndrome
A new analysis of data from a phase 3 clinical trial suggests that an inhaled diazepam nasal spray (Valtoco, Neurelis) works about as well among patients with Lennox-Gastaut syndrome (LGS) as it does with other patients with pediatric encephalopathies.
LGS is a severe form of epilepsy that generally begins in early childhood and has a poor prognosis and seizures that are often treatment refractory. The findings of the analysis should be encouraging to physicians who may view patients with LGS as not benefiting from treatment, said Daniel C. Tarquinio, DO, who presented the results at the 2022 annual meeting of the Child Neurology Society.
Novel cannabis oil curbs tics in severe Tourette syndrome
An oral oil containing tetrahydrocannabinol (THC) and cannabidiol (CBD) led to a significant and meaningful reduction in motor and vocal tics in patients with severe Tourette syndrome, results of a double-blind, placebo-controlled, crossover study showed.
“In a methodologically robust manner (and independent of any drug company sponsorship), we provide evidence for the effectiveness of repeated dosing with THC:CBD versus placebo in tic
suppression, as well as reduction of comorbid anxiety and obsessive-compulsive disorder in severe Tourette syndrome,” neuropsychiatrist and lead investigator Philip Mosley, PhD, said in an interview.
The results offer support to people with Tourette syndrome who “want to approach their doctor to try medicinal cannabis when other drugs have not worked or are intolerable,” said
Dr. Mosley, of the Wesley Research Institute and QIMR Berghofer Medical Research Institute, Herston, Australia.
The study was published online in NEJM Evidence (2023 Jun 7. doi: 10.1056/EVIDoa2300012).
Twenty-two adults (mean age, 31 years) with severe Tourette syndrome received THC:CBD oil titrated upward over 6 weeks to a daily dose of 20 mg of THC and 20 mg of CBD, followed by a 6-week course of placebo (or vice versa). Six participants had not previously used cannabis.
The primary outcome was the total tic score on the Yale Global Tic Severity Scale (YGTSS; range, 0-50 with higher scores = greater tic severity).
The mean baseline YGTSS total tic score was 35.7. At 6 weeks, the reduction in total tic score was 8.9 with THC:CBD versus 2.5 with placebo.
A linear mixed-effects model (intention to treat) showed a significant interaction of treatment and visit number (P = .008), indicating a greater decrease (improvement) in tic score over time with THC:CBD, the study team reported.
On average, the magnitude of the tic reduction was “moderate” and comparable with the effect observed with existing treatments such as antipsychotic agents, the investigators noted.
The study was funded by the Wesley Medical Research Institute, Brisbane, and the Lambert Initiative for Cannabinoid Therapeutics, a philanthropically funded research organization at the University of Sydney, Australia.
Dr. Mosley reported no relevant financial relationships.
Can a repurposed Parkinson’s drug slow ALS progression?
Ropinirole, a drug used for Parkinson’s disease, shows promise in slowing the progression of amyotrophic lateral sclerosis (ALS), early research suggests.
Investigators randomly assigned 20 individuals with sporadic ALS to receive either ropinirole or placebo for 24 weeks. During the double-blind period, there was no difference between the groups in terms of decline in functional status.
However, during a further open-label extension period, the ropinirole group showed significant suppression of functional decline and an average of an additional 7 months of progression-free survival.
The researchers were able to predict clinical responsiveness to ropinirole in vitro by analyzing motor neurons derived from participants’ stem cells.
The study was published online in Cell Stem Cell (2023 Jun 1. doi: 10.1016/j.stem.2023.04.017).
The trial was sponsored by K Pharma. The study drug, active drugs, and placebo were supplied free of charge by GlaxoSmithKline.
West Nile infections rising in the U.S.
Several signs are pointing to an impending surge in the number of human cases of West Nile virus in several regions of the United States. West Nile virus is spread by infected mosquitoes and currently there is no cure or virus-specific treatment. In rare cases, it can be deadly. It can infect humans, birds, horses, and other mammals.
West Nile Virus is the leading cause of mosquito-borne disease in the continental United States. As of Aug. 8, 126 human cases had been identified across 22 states, according to the Centers for Disease Control and Prevention.
“Particularly here in California, it’s peak risk right now,” said Vicki Kramer, PhD, chief of vector-borne diseases in the California Department of Public Health. She said scientists there are seeing higher mosquito and infected mosquito numbers.
Dead birds are tested for the virus and by Aug. 4, 181 of the 913 birds tested in California have been positive, three times the total testing positive by that time in 2022.
“Last year at this time, we had 60 positive dead birds out of 817 tested,” Dr. Kramer said.
Myasthenia gravis drug gets FDA nod
The Food and Drug Administration (FDA) has approved rozanolixizumab (Rystiggo, UCB) to treat adults with generalized myasthenia gravis (gMG) who are positive for anti-acetylcholine receptor (AChR) or anti–muscle-specific tyrosine kinase (MuSK) antibody, the drug’s manufacturer, UCB, has announced.
gMG is a rare autoimmune disease of the nerve muscle junction. Anti-AChR and anti-MuSK antibody-positive gMG are the two most common subtypes. Rozanolixizumab is the first FDA-approved treatment for adults with both subtypes.
Rozanolixizumab is a subcutaneous-infused humanized IgG4 monoclonal antibody that binds to the neonatal Fc
receptor (FcRn), reducing the concentration of pathogenic IgG autoantibodies.
U.S. approval is based on results of the phase 3
MycarinG study involving 200 patients with AChR or MuSK autoantibody-positive gMG. Patients were randomly assigned to one of two rozanolixizumab groups (7 mg/kg or 10 mg/kg) or placebo for 6 weeks.
As reported in The Lancet Neurology (2023 May. doi: 10.1016/S1474-4422[23]00077-7), rozanolixizumab led to statistically significant improvements in gMG-specific outcomes, including everyday activities such as breathing, talking, swallowing, and being able to rise from a chair.
Gene therapy promising for reversal of hereditary vision loss
An unapproved gene therapy for Leber hereditary optic neuropathy (LHON) led to a marked improvement in the eyesight of patients with a severe, progressive form of the disease who received the therapy as part of an early access program.
Results of a study of more than 60 patients who received lenadogene nolparvovec (Lumevoq, GenSight Biologics) as a unilateral or bilateral intravitreal injection showed that, at 2-year follow-up, 60% had experienced a clinically relevant improvement in the number of letters they could read on a visual acuity chart.
The results, said study presenter Chiara La Morgia, MD, PhD, IRCCS Istituto delle Scienze Neurologiche di Bologna (Italy), confirm in a “real-life setting” the efficacy and safety of the treatment as previously shown in clinical trials.
The findings were presented at the 2023 Congress of the European Academy of Neurology.
No funding was declared. Dr. La Morgia has relationships with Chiesi Farmaceutici, GenSight Biologics, Regulatory Pharma Net, Thenewway, Santhera Pharmaceuticals, First Class, Biologix, Stoke Therapeutics, and Reneo.
FDA OKs new drug for Fabry disease
The FDA has approved pegunigalsidase alfa (Elfabrio, Chiesi Global Rare Diseases/Protalix BioTherapeutics), an enzyme replacement therapy (ERT) to treat adults with Fabry disease.
Fabry disease is a rare inherited X-linked lysosomal disorder caused by a deficiency of the enzyme alpha-galactosidase A (GLA), which leads to the buildup of globotriaosylceramide (GL-3) in blood vessels, kidneys, heart, nerves, and other organs, increasing the risk for kidney failure, myocardial infarction, stroke, and other problems.
Elfabrio delivers a functional version of GLA. It is given by intravenous infusion every 2 weeks.
Evidence for safety, tolerability, and efficacy of Elfabrio stem from a comprehensive clinical program in more than 140 patients with up to 7.5 years of follow-up treatment.
It has been studied in both ERT-naive and ERT-experienced patients. In one head-to-head trial, Elfabrio was noninferior in safety and efficacy to agalsidase beta (Fabrazyme, Sanofi Genzyme), the companies said in a press statement announcing approval.
U.S. incidence, prevalence of myasthenia gravis are rising
There has been an increase in the incidence and prevalence of myasthenia gravis in the United States, an analysis of new claims data shows. Investigators speculate the rise of this rare disorder may be caused by “increased diagnosis and more awareness of the disease over time, which has been shown in several studies,” said study investigator Ema Rodrigues, DSc, MPH, with Alexion Pharmaceuticals, Boston.
Dr. Rodrigues presented her research at the 2023 annual meeting of the American Academy of Neurology.
Funding for the study was provided by Alexion, AstraZeneca Rare
Disease. Dr. Rodrigues receives compensation and owns stock as an employee of Alexion, AstraZeneca Rare Diseases.
Novel agent offers hope for hereditary ATTR polyneuropathy in pivotal trial
The investigational agent eplontersen (Ionis Pharmaceuticals/AstraZeneca) halted neuropathy disease progression and improved neuropathy impairment and quality of life for patients with hereditary transthyretin-mediated amyloid polyneuropathy (ATTRv-PN) in a pivotal phase 3 trial.
Eplontersen led to “clinically and statistically significant benefits at week 66 with an early and rapid sustained reduction in serum TTR [transthyretin] concentration, a halting of the progression of the neuropathy impairment, and a trend to improvement in quality of life,” said principal investigator Sami Khella, MD, professor of clinical neurology at the University of Pennsylvania, Philadelphia.
Dr. Khella reported final data from the NEURO-TTRansform trial at the annual meeting of the American Academy of Neurology.
The FDA has accepted a new drug application for eplontersen for the treatment of ATTRv-PN. The drug has a Prescription Drug User Fee Act date of Dec. 22, 2023. Eplontersen has orphan drug designation in the United States.
The study was sponsored by Ionis Pharmaceuticals. Dr. Khella has relationships with Ionis, Pfizer, Alnylam, and Eidos.
FDA gives fast-track approval to new ALS drug
The FDA has approved the first treatment that takes a genetics-based approach to slowing or stopping the progression of a rare form of amyotrophic lateral sclerosis (ALS).
The FDA fast-tracked the approval of Qalsody (Biogen) based on early trial results. The agency said in a news release that its decision was based on the demonstrated ability of the drug to reduce a protein in the blood that is a sign of degeneration of brain and nerve cells.
Qalsody is given to people via a spinal injection, with an initial course of three injections every 2 weeks. People then get the injection once every 28 days.
The new treatment is approved only for people with SOD1-ALS, which is known for a genetic mutation. While ALS affects up to 32,000 people in the United States, just 2% of people with ALS have the SOD1 gene mutation. The FDA says the number of people in the United States who could use Qalsody is about 500.
FDA OKs first treatment for Friedreich ataxia
The FDA has approved the first treatment for the neurodegenerative disorder Friedreich ataxia for use in adults and adolescents aged 16 and older.
The recommended dose of omaveloxolone (Skyclarys, Reata Pharmaceuticals) is 150 mg (three capsules) taken orally once daily on an empty stomach.
The FDA approval of omaveloxolone was supported by a randomized double-blind, placebo-controlled study comprising 103 patients with genetically confirmed Friedreich ataxia and baseline modified Friedreich Ataxia Rating Scale (mFARS) scores between 20 and 80.
Treatment with the novel medication led to statistically significant lower mFARS scores, signifying less impairment, relative to placebo, at week 48. The placebo-corrected difference between the two groups was –2.41 points (P = .0138).
Omaveloxolone received priority review and had orphan drug, fast track, and rare pediatric disease designations.
FDA OKs first drug for Rett syndrome
The FDA has approved trofinetide oral solution (Daybue, Acadia Pharmaceuticals) as the first treatment of Rett syndrome in adults and children aged 2 years and older.
Trofinetide is a synthetic analogue of the amino-terminal tripeptide of insulinlike growth factor-1, which occurs naturally in the brain. The drug is designed to treat the core symptoms of Rett syndrome by potentially reducing neuroinflammation and supporting synaptic function.
The approval of trofinetide was supported by results from the pivotal phase 3 LAVENDER study that tested the efficacy and safety of trofinetide versus placebo in 187 female patients with Rett syndrome, aged 5-20 years.
More data back Guillain-Barré risk with Janssen COVID shot
New surveillance data from the Vaccine Adverse Event Reporting System (VAERS) back previous findings of increased risk for Guillain-Barré syndrome (GBS) after receiving the Janssen COVID-19 vaccine (Ad26.COV2.S).
Over 14 months, GBS reporting rates within 21 and 42 days of administration of Janssen’s replication-incompetent adenoviral vector vaccine were approximately 9-12 times higher than after administration of the Pfizer-BioNTech (BNT162b2) or the Moderna (mRNA-1273) mRNA COVID vaccines.
Additionally, observed GBS cases after the Janssen shot were two to three times greater than expected, based on background rates within 21 and 42 days of vaccination.
Conversely, and confirming prior data, there was no increased risk for GBS with the Pfizer or Moderna vaccines and no significant difference between observed and expected numbers of GBS cases after either mRNA COVID-19 vaccine.
The findings were published online in JAMA Network Open (2023 Feb 1. doi: 10.1001/jamanetworkopen.2022.53845).
Diazepam nasal spray effective in Lennox-Gastaut syndrome
A new analysis of data from a phase 3 clinical trial suggests that an inhaled diazepam nasal spray (Valtoco, Neurelis) works about as well among patients with Lennox-Gastaut syndrome (LGS) as it does with other patients with pediatric encephalopathies.
LGS is a severe form of epilepsy that generally begins in early childhood and has a poor prognosis and seizures that are often treatment refractory. The findings of the analysis should be encouraging to physicians who may view patients with LGS as not benefiting from treatment, said Daniel C. Tarquinio, DO, who presented the results at the 2022 annual meeting of the Child Neurology Society.
Novel cannabis oil curbs tics in severe Tourette syndrome
An oral oil containing tetrahydrocannabinol (THC) and cannabidiol (CBD) led to a significant and meaningful reduction in motor and vocal tics in patients with severe Tourette syndrome, results of a double-blind, placebo-controlled, crossover study showed.
“In a methodologically robust manner (and independent of any drug company sponsorship), we provide evidence for the effectiveness of repeated dosing with THC:CBD versus placebo in tic
suppression, as well as reduction of comorbid anxiety and obsessive-compulsive disorder in severe Tourette syndrome,” neuropsychiatrist and lead investigator Philip Mosley, PhD, said in an interview.
The results offer support to people with Tourette syndrome who “want to approach their doctor to try medicinal cannabis when other drugs have not worked or are intolerable,” said
Dr. Mosley, of the Wesley Research Institute and QIMR Berghofer Medical Research Institute, Herston, Australia.
The study was published online in NEJM Evidence (2023 Jun 7. doi: 10.1056/EVIDoa2300012).
Twenty-two adults (mean age, 31 years) with severe Tourette syndrome received THC:CBD oil titrated upward over 6 weeks to a daily dose of 20 mg of THC and 20 mg of CBD, followed by a 6-week course of placebo (or vice versa). Six participants had not previously used cannabis.
The primary outcome was the total tic score on the Yale Global Tic Severity Scale (YGTSS; range, 0-50 with higher scores = greater tic severity).
The mean baseline YGTSS total tic score was 35.7. At 6 weeks, the reduction in total tic score was 8.9 with THC:CBD versus 2.5 with placebo.
A linear mixed-effects model (intention to treat) showed a significant interaction of treatment and visit number (P = .008), indicating a greater decrease (improvement) in tic score over time with THC:CBD, the study team reported.
On average, the magnitude of the tic reduction was “moderate” and comparable with the effect observed with existing treatments such as antipsychotic agents, the investigators noted.
The study was funded by the Wesley Medical Research Institute, Brisbane, and the Lambert Initiative for Cannabinoid Therapeutics, a philanthropically funded research organization at the University of Sydney, Australia.
Dr. Mosley reported no relevant financial relationships.
A note from NORD
We extend our sincere thanks to busy health care professionals for taking time to engage with this issue, read the latest advances, and provide the best possible care for your patients. Your dedication is an inspiration, and we value the impact you make in the lives of others.
The year 2023 marks the 40th anniversary of the Orphan Drug Act (ODA), landmark legislation that incentivized drug companies to dedicate more resources towards the development of therapies for people with rare conditions. At the same time, we celebrate NORD’s 40th anniversary. The coalition of rare disease advocates who sparked rare disease advocacy and convinced lawmakers to pass the ODA in 1983 established NORD that same year to provide an ongoing, unified voice for the needs of the rare disease community. For 4 decades, NORD has worked tirelessly to drive supportive policies, advance medical research, and provide education and services for the now 30 million Americans with a rare disease, of which half are children.
In this issue of the Rare Neurological Disease Special Report, you will learn more about the history of the Orphan Drug Act and the founding of NORD. You will also find articles from rare disease specialists on specific diseases and some of the newest therapies approved under the ODA for conditions such as Friedreich ataxia, Fabry disease, Duchenne muscular dystrophy, and amyotrophic lateral sclerosis. Also in the issue are articles about stiff person syndrome and Guillain-Barré syndrome and COVID vaccination.
We invite you to visit NORD’s webpage (www.rarediseases.org) to access resources for yourself and the patients and families you serve. NORD’s Continuing Medical Education Video Library offers cost-free, for-credit, on-demand rare disease courses developed in collaboration with Platform Q Health. NORD’s Caring for Rare quarterly newsletter provides updates on educational opportunities, events, and issues important for the rare disease community. NORD’s Rare Disease Database provides expert-reviewed reports on rare diseases in patient-friendly language.
As we celebrate the incredible progress made over the past 40 years, we also recognize that more than 95% of rare conditions still lack effective therapies. Continued research, development of new orphan products, and advances in treatment and care are needed. NORD will remain steadfast in its commitment to driving progress, inspiring innovation, and providing services for the rare community. We are deeply appreciative of the support you provide to people living with neurological conditions and encourage you to contact NORD any time we can be helpful to you.
Edward Neilan, MD, PhD
NORD’s Chief Medical Officer
We extend our sincere thanks to busy health care professionals for taking time to engage with this issue, read the latest advances, and provide the best possible care for your patients. Your dedication is an inspiration, and we value the impact you make in the lives of others.
The year 2023 marks the 40th anniversary of the Orphan Drug Act (ODA), landmark legislation that incentivized drug companies to dedicate more resources towards the development of therapies for people with rare conditions. At the same time, we celebrate NORD’s 40th anniversary. The coalition of rare disease advocates who sparked rare disease advocacy and convinced lawmakers to pass the ODA in 1983 established NORD that same year to provide an ongoing, unified voice for the needs of the rare disease community. For 4 decades, NORD has worked tirelessly to drive supportive policies, advance medical research, and provide education and services for the now 30 million Americans with a rare disease, of which half are children.
In this issue of the Rare Neurological Disease Special Report, you will learn more about the history of the Orphan Drug Act and the founding of NORD. You will also find articles from rare disease specialists on specific diseases and some of the newest therapies approved under the ODA for conditions such as Friedreich ataxia, Fabry disease, Duchenne muscular dystrophy, and amyotrophic lateral sclerosis. Also in the issue are articles about stiff person syndrome and Guillain-Barré syndrome and COVID vaccination.
We invite you to visit NORD’s webpage (www.rarediseases.org) to access resources for yourself and the patients and families you serve. NORD’s Continuing Medical Education Video Library offers cost-free, for-credit, on-demand rare disease courses developed in collaboration with Platform Q Health. NORD’s Caring for Rare quarterly newsletter provides updates on educational opportunities, events, and issues important for the rare disease community. NORD’s Rare Disease Database provides expert-reviewed reports on rare diseases in patient-friendly language.
As we celebrate the incredible progress made over the past 40 years, we also recognize that more than 95% of rare conditions still lack effective therapies. Continued research, development of new orphan products, and advances in treatment and care are needed. NORD will remain steadfast in its commitment to driving progress, inspiring innovation, and providing services for the rare community. We are deeply appreciative of the support you provide to people living with neurological conditions and encourage you to contact NORD any time we can be helpful to you.
Edward Neilan, MD, PhD
NORD’s Chief Medical Officer
We extend our sincere thanks to busy health care professionals for taking time to engage with this issue, read the latest advances, and provide the best possible care for your patients. Your dedication is an inspiration, and we value the impact you make in the lives of others.
The year 2023 marks the 40th anniversary of the Orphan Drug Act (ODA), landmark legislation that incentivized drug companies to dedicate more resources towards the development of therapies for people with rare conditions. At the same time, we celebrate NORD’s 40th anniversary. The coalition of rare disease advocates who sparked rare disease advocacy and convinced lawmakers to pass the ODA in 1983 established NORD that same year to provide an ongoing, unified voice for the needs of the rare disease community. For 4 decades, NORD has worked tirelessly to drive supportive policies, advance medical research, and provide education and services for the now 30 million Americans with a rare disease, of which half are children.
In this issue of the Rare Neurological Disease Special Report, you will learn more about the history of the Orphan Drug Act and the founding of NORD. You will also find articles from rare disease specialists on specific diseases and some of the newest therapies approved under the ODA for conditions such as Friedreich ataxia, Fabry disease, Duchenne muscular dystrophy, and amyotrophic lateral sclerosis. Also in the issue are articles about stiff person syndrome and Guillain-Barré syndrome and COVID vaccination.
We invite you to visit NORD’s webpage (www.rarediseases.org) to access resources for yourself and the patients and families you serve. NORD’s Continuing Medical Education Video Library offers cost-free, for-credit, on-demand rare disease courses developed in collaboration with Platform Q Health. NORD’s Caring for Rare quarterly newsletter provides updates on educational opportunities, events, and issues important for the rare disease community. NORD’s Rare Disease Database provides expert-reviewed reports on rare diseases in patient-friendly language.
As we celebrate the incredible progress made over the past 40 years, we also recognize that more than 95% of rare conditions still lack effective therapies. Continued research, development of new orphan products, and advances in treatment and care are needed. NORD will remain steadfast in its commitment to driving progress, inspiring innovation, and providing services for the rare community. We are deeply appreciative of the support you provide to people living with neurological conditions and encourage you to contact NORD any time we can be helpful to you.
Edward Neilan, MD, PhD
NORD’s Chief Medical Officer
Editor’s note
2023 is indeed a noteworthy year. As you will read in this issue, it marks the 40th anniversary of the landmark Orphan Drug Act and the formation of the National Organization for Rare Disorders (NORD). 2023 also marks the 30th anniversary of Neurology Reviews, the parent publication of the Rare Neurological Disease Special Report. While Neurology Reviews covers rare disease news throughout the year (see our Rare Disease Roundup in this issue), it is in our annual supplement where our rare disease news coverage and our partnership with NORD truly shines.
In this issue we take pride in taking a deeper look at some of the rare neurological diseases that have made headlines as well as the therapeutic advances and research breakthroughs that continue to benefit patients and the rare disease community as a whole. While I would prefer to humbly serve the rare disease community through our news coverage and educational efforts, I would be remiss if I didn’t mention that our 2022 Rare Neurological Disease Special Report won a Silver Regional Award in the category of annual supplement in the American Society of Business Publication Editors (Azbee) yearly competition. With that moment of bragging aside, I invite you to read this year’s issue, and I thank you for the success that this supplement has enjoyed since it launched in 2015.
Glenn S. Williams,
2023 is indeed a noteworthy year. As you will read in this issue, it marks the 40th anniversary of the landmark Orphan Drug Act and the formation of the National Organization for Rare Disorders (NORD). 2023 also marks the 30th anniversary of Neurology Reviews, the parent publication of the Rare Neurological Disease Special Report. While Neurology Reviews covers rare disease news throughout the year (see our Rare Disease Roundup in this issue), it is in our annual supplement where our rare disease news coverage and our partnership with NORD truly shines.
In this issue we take pride in taking a deeper look at some of the rare neurological diseases that have made headlines as well as the therapeutic advances and research breakthroughs that continue to benefit patients and the rare disease community as a whole. While I would prefer to humbly serve the rare disease community through our news coverage and educational efforts, I would be remiss if I didn’t mention that our 2022 Rare Neurological Disease Special Report won a Silver Regional Award in the category of annual supplement in the American Society of Business Publication Editors (Azbee) yearly competition. With that moment of bragging aside, I invite you to read this year’s issue, and I thank you for the success that this supplement has enjoyed since it launched in 2015.
Glenn S. Williams,
2023 is indeed a noteworthy year. As you will read in this issue, it marks the 40th anniversary of the landmark Orphan Drug Act and the formation of the National Organization for Rare Disorders (NORD). 2023 also marks the 30th anniversary of Neurology Reviews, the parent publication of the Rare Neurological Disease Special Report. While Neurology Reviews covers rare disease news throughout the year (see our Rare Disease Roundup in this issue), it is in our annual supplement where our rare disease news coverage and our partnership with NORD truly shines.
In this issue we take pride in taking a deeper look at some of the rare neurological diseases that have made headlines as well as the therapeutic advances and research breakthroughs that continue to benefit patients and the rare disease community as a whole. While I would prefer to humbly serve the rare disease community through our news coverage and educational efforts, I would be remiss if I didn’t mention that our 2022 Rare Neurological Disease Special Report won a Silver Regional Award in the category of annual supplement in the American Society of Business Publication Editors (Azbee) yearly competition. With that moment of bragging aside, I invite you to read this year’s issue, and I thank you for the success that this supplement has enjoyed since it launched in 2015.
Glenn S. Williams,
2023 Rare Neurological Disease Special Report
INTRODUCTIONS
Editor’s note
By Glenn S. Williams
2023 is indeed a noteworthy year. As you will read in this issue, it marks the 40th anniversary of the landmark Orphan Drug Act (ODA) and the formation of the National Organization for Rare Disorders. 2023 also marks the 30th anniversary of Neurology Reviews, the parent publication of the Rare Neurological Disease Special Report.
A note from NORD
By Edward Neilan, MD, PhD
The coalition of rare disease advocates who sparked rare disease advocacy and convinced lawmakers to pass the ODA in 1983 established NORD that same year to provide an ongoing, unified voice for the needs of the rare disease community.
Rare disease roundup
A look back at some of the 2023 rare disease headlines from Neurology Reviews.
CLINICAL REVIEWS
The Orphan Drug Act and NORD at their 40th anniversary: Dramatic achievements and ongoing innovation
By Batya Swift Yasgur, MA, MSW
The movement whose face is ODA and NORD continues to build its legacy. Next? Progress in rare disease care will require an all-in approach to solving a looming and massive public health challenge.
Emerging therapies in Duchenne and facioscapulohumeral muscular dystrophy
By Frieda Wiley, PharmD
Newly approved and investigational therapies, and enhanced diagnostics, are sparking optimism about treating MD – especially Duchenne and facioscapulohumeral types.
Has prompt diagnosis of amyotrophic lateral sclerosis become urgent?
By Ted Bosworth
Optimism is high about improving the survival and care of ALS patients. Neurologists who don’t specialize in ALS can add to the positivity by endorsing a role in speedier diagnostic pathways.
A new chapter for research on treating Huntington’s disease
By Jennie Smith
Setbacks in trials of protein-lowering therapies – mostly over their safety – mask a story of rapid advances and a more recently discovered treatment pathway that also offers promise for other diseases.
The dawning age of therapy for Friedreich ataxia
By Neil Osterweil
The first therapy to target the underlying pathology of Friedreich ataxia was approved in 2023. Other drug and genetic therapies are in the pipeline.
Stiff person syndrome: When a rare disorder hits the headlines
By Kate Johnson
Awareness of this disorder is increasing, but clinicians are challenged to apply the proper workup to avoid wrong turns in identifying affected patients.
Advances in testing and therapeutics are improving the lives of patients with Fabry disease
By Lorraine L. Janeczko, MPH
Thanks to robust research efforts, treatment options are expanding and patients are getting their diagnosis earlier – often, when they are presymptomatic and treatment has greater potential for enhancing quality of life.
Guillain-Barré syndrome: Honing treatment strategies
By John Jesitus
Classic subtypes of Guillain-Barré syndrome are varying manifestations of a shared disease process, novel insights into the disease indicate. This understanding is yielding new treatment strategies.
INTRODUCTIONS
Editor’s note
By Glenn S. Williams
2023 is indeed a noteworthy year. As you will read in this issue, it marks the 40th anniversary of the landmark Orphan Drug Act (ODA) and the formation of the National Organization for Rare Disorders. 2023 also marks the 30th anniversary of Neurology Reviews, the parent publication of the Rare Neurological Disease Special Report.
A note from NORD
By Edward Neilan, MD, PhD
The coalition of rare disease advocates who sparked rare disease advocacy and convinced lawmakers to pass the ODA in 1983 established NORD that same year to provide an ongoing, unified voice for the needs of the rare disease community.
Rare disease roundup
A look back at some of the 2023 rare disease headlines from Neurology Reviews.
CLINICAL REVIEWS
The Orphan Drug Act and NORD at their 40th anniversary: Dramatic achievements and ongoing innovation
By Batya Swift Yasgur, MA, MSW
The movement whose face is ODA and NORD continues to build its legacy. Next? Progress in rare disease care will require an all-in approach to solving a looming and massive public health challenge.
Emerging therapies in Duchenne and facioscapulohumeral muscular dystrophy
By Frieda Wiley, PharmD
Newly approved and investigational therapies, and enhanced diagnostics, are sparking optimism about treating MD – especially Duchenne and facioscapulohumeral types.
Has prompt diagnosis of amyotrophic lateral sclerosis become urgent?
By Ted Bosworth
Optimism is high about improving the survival and care of ALS patients. Neurologists who don’t specialize in ALS can add to the positivity by endorsing a role in speedier diagnostic pathways.
A new chapter for research on treating Huntington’s disease
By Jennie Smith
Setbacks in trials of protein-lowering therapies – mostly over their safety – mask a story of rapid advances and a more recently discovered treatment pathway that also offers promise for other diseases.
The dawning age of therapy for Friedreich ataxia
By Neil Osterweil
The first therapy to target the underlying pathology of Friedreich ataxia was approved in 2023. Other drug and genetic therapies are in the pipeline.
Stiff person syndrome: When a rare disorder hits the headlines
By Kate Johnson
Awareness of this disorder is increasing, but clinicians are challenged to apply the proper workup to avoid wrong turns in identifying affected patients.
Advances in testing and therapeutics are improving the lives of patients with Fabry disease
By Lorraine L. Janeczko, MPH
Thanks to robust research efforts, treatment options are expanding and patients are getting their diagnosis earlier – often, when they are presymptomatic and treatment has greater potential for enhancing quality of life.
Guillain-Barré syndrome: Honing treatment strategies
By John Jesitus
Classic subtypes of Guillain-Barré syndrome are varying manifestations of a shared disease process, novel insights into the disease indicate. This understanding is yielding new treatment strategies.
INTRODUCTIONS
Editor’s note
By Glenn S. Williams
2023 is indeed a noteworthy year. As you will read in this issue, it marks the 40th anniversary of the landmark Orphan Drug Act (ODA) and the formation of the National Organization for Rare Disorders. 2023 also marks the 30th anniversary of Neurology Reviews, the parent publication of the Rare Neurological Disease Special Report.
A note from NORD
By Edward Neilan, MD, PhD
The coalition of rare disease advocates who sparked rare disease advocacy and convinced lawmakers to pass the ODA in 1983 established NORD that same year to provide an ongoing, unified voice for the needs of the rare disease community.
Rare disease roundup
A look back at some of the 2023 rare disease headlines from Neurology Reviews.
CLINICAL REVIEWS
The Orphan Drug Act and NORD at their 40th anniversary: Dramatic achievements and ongoing innovation
By Batya Swift Yasgur, MA, MSW
The movement whose face is ODA and NORD continues to build its legacy. Next? Progress in rare disease care will require an all-in approach to solving a looming and massive public health challenge.
Emerging therapies in Duchenne and facioscapulohumeral muscular dystrophy
By Frieda Wiley, PharmD
Newly approved and investigational therapies, and enhanced diagnostics, are sparking optimism about treating MD – especially Duchenne and facioscapulohumeral types.
Has prompt diagnosis of amyotrophic lateral sclerosis become urgent?
By Ted Bosworth
Optimism is high about improving the survival and care of ALS patients. Neurologists who don’t specialize in ALS can add to the positivity by endorsing a role in speedier diagnostic pathways.
A new chapter for research on treating Huntington’s disease
By Jennie Smith
Setbacks in trials of protein-lowering therapies – mostly over their safety – mask a story of rapid advances and a more recently discovered treatment pathway that also offers promise for other diseases.
The dawning age of therapy for Friedreich ataxia
By Neil Osterweil
The first therapy to target the underlying pathology of Friedreich ataxia was approved in 2023. Other drug and genetic therapies are in the pipeline.
Stiff person syndrome: When a rare disorder hits the headlines
By Kate Johnson
Awareness of this disorder is increasing, but clinicians are challenged to apply the proper workup to avoid wrong turns in identifying affected patients.
Advances in testing and therapeutics are improving the lives of patients with Fabry disease
By Lorraine L. Janeczko, MPH
Thanks to robust research efforts, treatment options are expanding and patients are getting their diagnosis earlier – often, when they are presymptomatic and treatment has greater potential for enhancing quality of life.
Guillain-Barré syndrome: Honing treatment strategies
By John Jesitus
Classic subtypes of Guillain-Barré syndrome are varying manifestations of a shared disease process, novel insights into the disease indicate. This understanding is yielding new treatment strategies.