User login
The Hospitalist only
Face-to-Face Improvement
The American Medical Association recently released Current Procedural Terminology (CPT) 2009. New, deleted, and revised codes went into effect Jan. 1. The biggest change to hospitalist billing involves prolonged care codes (99354-99357). CPT 2009 descriptor revisions make it possible for physicians to contribute non-face-to-face time toward prolonged care services.
Inpatient Prolonged Care
Previous versions of CPT defined code 99356 as the first hour of prolonged physician [inpatient] services requiring direct (face-to-face) patient contact beyond the usual services (reportable after the initial 30 minutes); and 99357 for each additional 30 minutes of prolonged [inpatient] care beyond the first hour (reportable after the first 15 minutes of each additional segment). CPT 2009 has changed prolonged care guidelines to be more consistent with other time-based services: all unit/floor time spent by the physician is considered when reporting 99356 and 99357.1
As with most other evaluation and management services, a face-to-face encounter still must occur. In addition to the time associated with the face-to-face encounter, count the time associated with all other physician activities occurring on the unit/floor (e.g., reviewing images, obtaining information involving overnight events, discussing management options with the family) directed toward an individual patient. The cumulative time spent by the billing provider on a single calendar day is considered for billing. Time spent by someone other than the billing provider cannot be credited toward prolonged care.
As example, a physician cares for a 65-year-old male with uncontrolled diabetes, diabetic nephropathy, and congestive heart failure. Early in the day, the physician rounds, spending a total of 20 minutes reviewing the overnight course of events on the unit, re-confirming the patient history, and performing an exam with the patient. Anticipating the patient’s needs, the physician discusses post-discharge options and care with the patient and his family for 45 minutes. After the discussion, the physician spends an additional 30 minutes relaying information to the team and coordinating care. Merely reporting the highest-level subsequent hospital care service (99233), does not capture the physician’s cumulative effort. It only would account for 40 of the 95 minutes spent throughout the day. In order to capture the remaining 55 minutes, the physician reports 99356 on the same claim form as 99233.
Do not report prolonged care codes on a separate claim form. Prolonged care codes do not represent an independent service. These codes are reported along with a primary service. They must appear as a separate line item on the claim form, which includes a code representing the primary service. For prolonged care in the inpatient setting, the primary service must be initial hospital care (99221-99223), subsequent hospital care (99231-99233), inpatient consultations (99251-99255), or nursing facility services (99304-99318). Additional examples of billable prolonged care services are in Section 30.6.15.1I of the Medicare manual, available at www.cms.hhs.gov/manuals/ downloads/clm104c12.pdf.
Threshold Time
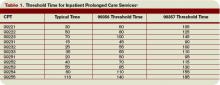
Prolonged care guidelines refer to “threshold” time. Threshold time requires the physician to exceed the time requirements associated with the “primary” codes before reporting prolonged care. Table 1 identifies the typical times associated with inpatient services qualifying for prolonged care. The physician must exceed the typical time by a minimum of 30 minutes. (For example, 99232 + 99356 = 25 minutes + 30 minutes = 55 total minutes). Additionally, the physician must document the total time spent during the face-to-face portion of the encounter, and the additional unit or floor time in one cumulative note or in separate notes representing the physician services provided to the patient throughout the day.
Prolonged Outpatient Services
Prolonged care (99354-99355) provided to outpatients remains unchanged. Physicians only report personally provided face-to-face time with the patient. Time spent by other staff members does not count toward prolonged care.
As with prolonged inpatient care, report 99354 and 99355 in addition to a primary service code. The companion outpatient codes are outpatient/office visits (99201-99205 or 99212–99215), outpatient consultation (99241–99245), domiciliary/custodial care (99324–99328 or 99334–99337), and home services (99341-99350). Hospitalists more often use outpatient prolonged care with office consultation codes for services provided in the emergency department, as appropriate.
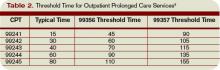
Do not report 99354 or 99355 with observation care (99217-99220) or emergency department visits (99281-99288), since these service categories typically require prolonged periods of physician monitoring, thereby prohibiting use of prolonged care codes. As with inpatient-prolonged care, the concept of threshold time exists. Refer to Table 2 (pg. 25) for the typical threshold times associated with office consultation codes.
Medicare Consideration
Although CPT has offered revisions to this code, Medicare guidelines remain unchanged. The Medicare Claims Processing Manual still states: “In the case of prolonged hospital services, time spent reviewing charts or discussion of a patient with house medical staff and not with direct face-to-face contact with the patient, or waiting for test results, for changes in the patient’s condition, for end of a therapy, or for use of facilities, cannot be billed as prolonged services.”4 It is yet to be determined if the Centers for Medicare and Medicaid Services (CMS) will issue a transmittal to revise the current description in the processing manual. Physicians and staff may access past and present transmittal information at www.cms.hhs.gov/ Transmittals/.
As always, be sure to query payers about prolonged care services, since some non-Medicare insurers may not recognize these codes.
Modifier 21
Modifier 21 has been deleted from the CPT. Modifier 21 was appended to an appropriate visit code (e.g., 99232-21) when the face-to-face or floor/unit service(s) provided is prolonged or otherwise greater than usually required for the highest level of evaluation and management service within a given category.5 Since the descriptors for codes 99354-99357 have been revised to more consistently reflect the description formerly associated with modifier 21, there is no need to maintain its existence. Additionally, Medicare and most other payers did not recognize this modifier.
Code This Case
Question: A newly diagnosed diabetic requires extensive counseling regarding lifestyle changes, medication regime, the disease process, as well as coordination of care for outpatient programs and services. The hospitalist reviews some of the pertinent information with the patient (15 minutes), and performs an abbreviated service (problem-focused history and exam). The attending physician asks the resident to assist him with the remaining counseling efforts and coordination of care (30 minutes).
Each physician documents his or her portion of the service. What visit level can the hospitalist report?
Answer: When two billing providers (i.e., two attending physicians) from the same group practice split the threshold time (e.g., physician A provided morning rounds, and physician B spoke with the family in the afternoon), only one physician can report the cumulative service, since 99356 must be reported on the same invoice as the primary visit code (e.g., 99231).6
The example above involves the resident’s time as well as the attending physician’s time. Documentation must be very clear to demonstrate the attending physician actively participated in the entire 45-minute service. Otherwise, only the attending may report the amount of time he actually spent providing the service.
Billing options for this scenario can vary. When the physician performs and documents the key components of history, exam, and decision making for the primary encounter, report 99231 (0.76 physician work relative value units; $33.90) and 99356 (1.71 physician work relative value units; $76.46) for the cumulative service. Alternatively, in those evaluation and management services for which the [primary] code level is selected based on time alone (i.e., history and exam was not performed or required), prolonged services may only be reported with the highest code level in that family of codes as the companion code.7
Therefore, this 45-minute service may be reported as 99233 (2.0 physician work relative value units; $86.92) since more than half of the total visit time was dedicated to counseling/coordi-nation of care (see Section 30.6.1B-C available at www. cms.hhs.gov/manuals/ downloads/clm104c12.pdf for additional information on billing for counseling/coordination of care time).
If a payer does not recognize prolonged care codes, only the latter billing option is possible. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is on the faculty of SHM’s inpatient coding course.
References
1. Beebe M, Dalton J, Espronceda M, Evans D, Glenn R. Current Procedural Terminology Professional Edition. Chicago, IL: American Medical Association, 2008; 25-26.
2. Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.15.1G. www.cms.hhs.gov/manuals/downloads/ clm104c12.pdf. Accessed November 19, 2008.
3. Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.15.1F. www.cms.hhs.gov/manuals/dowloads/ clm104c12.pdf. Accessed November 19, 2008.
4. Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.15.1C. www.cms.hhs.gov/manuals/ downloads/clm104c12.pdf. Accessed November 19, 2008.
5. Beebe M, Dalton J, Espronceda M, Evans D, Glenn R. Current Procedural Terminology Professional Edition. Chicago, IL: American Medical Association, 2008; 457.
6. Pohlig, C. Bill by time spent on case. The Hospitalist. Jul 2008;19.
7. Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.15.1H. www.cms.hhs.gov/manuals/downloads/ clm104c12.pdf. Accessed November 19, 2008.
The American Medical Association recently released Current Procedural Terminology (CPT) 2009. New, deleted, and revised codes went into effect Jan. 1. The biggest change to hospitalist billing involves prolonged care codes (99354-99357). CPT 2009 descriptor revisions make it possible for physicians to contribute non-face-to-face time toward prolonged care services.
Inpatient Prolonged Care
Previous versions of CPT defined code 99356 as the first hour of prolonged physician [inpatient] services requiring direct (face-to-face) patient contact beyond the usual services (reportable after the initial 30 minutes); and 99357 for each additional 30 minutes of prolonged [inpatient] care beyond the first hour (reportable after the first 15 minutes of each additional segment). CPT 2009 has changed prolonged care guidelines to be more consistent with other time-based services: all unit/floor time spent by the physician is considered when reporting 99356 and 99357.1
As with most other evaluation and management services, a face-to-face encounter still must occur. In addition to the time associated with the face-to-face encounter, count the time associated with all other physician activities occurring on the unit/floor (e.g., reviewing images, obtaining information involving overnight events, discussing management options with the family) directed toward an individual patient. The cumulative time spent by the billing provider on a single calendar day is considered for billing. Time spent by someone other than the billing provider cannot be credited toward prolonged care.
As example, a physician cares for a 65-year-old male with uncontrolled diabetes, diabetic nephropathy, and congestive heart failure. Early in the day, the physician rounds, spending a total of 20 minutes reviewing the overnight course of events on the unit, re-confirming the patient history, and performing an exam with the patient. Anticipating the patient’s needs, the physician discusses post-discharge options and care with the patient and his family for 45 minutes. After the discussion, the physician spends an additional 30 minutes relaying information to the team and coordinating care. Merely reporting the highest-level subsequent hospital care service (99233), does not capture the physician’s cumulative effort. It only would account for 40 of the 95 minutes spent throughout the day. In order to capture the remaining 55 minutes, the physician reports 99356 on the same claim form as 99233.
Do not report prolonged care codes on a separate claim form. Prolonged care codes do not represent an independent service. These codes are reported along with a primary service. They must appear as a separate line item on the claim form, which includes a code representing the primary service. For prolonged care in the inpatient setting, the primary service must be initial hospital care (99221-99223), subsequent hospital care (99231-99233), inpatient consultations (99251-99255), or nursing facility services (99304-99318). Additional examples of billable prolonged care services are in Section 30.6.15.1I of the Medicare manual, available at www.cms.hhs.gov/manuals/ downloads/clm104c12.pdf.
Threshold Time
Prolonged care guidelines refer to “threshold” time. Threshold time requires the physician to exceed the time requirements associated with the “primary” codes before reporting prolonged care. Table 1 identifies the typical times associated with inpatient services qualifying for prolonged care. The physician must exceed the typical time by a minimum of 30 minutes. (For example, 99232 + 99356 = 25 minutes + 30 minutes = 55 total minutes). Additionally, the physician must document the total time spent during the face-to-face portion of the encounter, and the additional unit or floor time in one cumulative note or in separate notes representing the physician services provided to the patient throughout the day.
Prolonged Outpatient Services
Prolonged care (99354-99355) provided to outpatients remains unchanged. Physicians only report personally provided face-to-face time with the patient. Time spent by other staff members does not count toward prolonged care.
As with prolonged inpatient care, report 99354 and 99355 in addition to a primary service code. The companion outpatient codes are outpatient/office visits (99201-99205 or 99212–99215), outpatient consultation (99241–99245), domiciliary/custodial care (99324–99328 or 99334–99337), and home services (99341-99350). Hospitalists more often use outpatient prolonged care with office consultation codes for services provided in the emergency department, as appropriate.
Do not report 99354 or 99355 with observation care (99217-99220) or emergency department visits (99281-99288), since these service categories typically require prolonged periods of physician monitoring, thereby prohibiting use of prolonged care codes. As with inpatient-prolonged care, the concept of threshold time exists. Refer to Table 2 (pg. 25) for the typical threshold times associated with office consultation codes.
Medicare Consideration
Although CPT has offered revisions to this code, Medicare guidelines remain unchanged. The Medicare Claims Processing Manual still states: “In the case of prolonged hospital services, time spent reviewing charts or discussion of a patient with house medical staff and not with direct face-to-face contact with the patient, or waiting for test results, for changes in the patient’s condition, for end of a therapy, or for use of facilities, cannot be billed as prolonged services.”4 It is yet to be determined if the Centers for Medicare and Medicaid Services (CMS) will issue a transmittal to revise the current description in the processing manual. Physicians and staff may access past and present transmittal information at www.cms.hhs.gov/ Transmittals/.
As always, be sure to query payers about prolonged care services, since some non-Medicare insurers may not recognize these codes.
Modifier 21
Modifier 21 has been deleted from the CPT. Modifier 21 was appended to an appropriate visit code (e.g., 99232-21) when the face-to-face or floor/unit service(s) provided is prolonged or otherwise greater than usually required for the highest level of evaluation and management service within a given category.5 Since the descriptors for codes 99354-99357 have been revised to more consistently reflect the description formerly associated with modifier 21, there is no need to maintain its existence. Additionally, Medicare and most other payers did not recognize this modifier.
Code This Case
Question: A newly diagnosed diabetic requires extensive counseling regarding lifestyle changes, medication regime, the disease process, as well as coordination of care for outpatient programs and services. The hospitalist reviews some of the pertinent information with the patient (15 minutes), and performs an abbreviated service (problem-focused history and exam). The attending physician asks the resident to assist him with the remaining counseling efforts and coordination of care (30 minutes).
Each physician documents his or her portion of the service. What visit level can the hospitalist report?
Answer: When two billing providers (i.e., two attending physicians) from the same group practice split the threshold time (e.g., physician A provided morning rounds, and physician B spoke with the family in the afternoon), only one physician can report the cumulative service, since 99356 must be reported on the same invoice as the primary visit code (e.g., 99231).6
The example above involves the resident’s time as well as the attending physician’s time. Documentation must be very clear to demonstrate the attending physician actively participated in the entire 45-minute service. Otherwise, only the attending may report the amount of time he actually spent providing the service.
Billing options for this scenario can vary. When the physician performs and documents the key components of history, exam, and decision making for the primary encounter, report 99231 (0.76 physician work relative value units; $33.90) and 99356 (1.71 physician work relative value units; $76.46) for the cumulative service. Alternatively, in those evaluation and management services for which the [primary] code level is selected based on time alone (i.e., history and exam was not performed or required), prolonged services may only be reported with the highest code level in that family of codes as the companion code.7
Therefore, this 45-minute service may be reported as 99233 (2.0 physician work relative value units; $86.92) since more than half of the total visit time was dedicated to counseling/coordi-nation of care (see Section 30.6.1B-C available at www. cms.hhs.gov/manuals/ downloads/clm104c12.pdf for additional information on billing for counseling/coordination of care time).
If a payer does not recognize prolonged care codes, only the latter billing option is possible. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is on the faculty of SHM’s inpatient coding course.
References
1. Beebe M, Dalton J, Espronceda M, Evans D, Glenn R. Current Procedural Terminology Professional Edition. Chicago, IL: American Medical Association, 2008; 25-26.
2. Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.15.1G. www.cms.hhs.gov/manuals/downloads/ clm104c12.pdf. Accessed November 19, 2008.
3. Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.15.1F. www.cms.hhs.gov/manuals/dowloads/ clm104c12.pdf. Accessed November 19, 2008.
4. Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.15.1C. www.cms.hhs.gov/manuals/ downloads/clm104c12.pdf. Accessed November 19, 2008.
5. Beebe M, Dalton J, Espronceda M, Evans D, Glenn R. Current Procedural Terminology Professional Edition. Chicago, IL: American Medical Association, 2008; 457.
6. Pohlig, C. Bill by time spent on case. The Hospitalist. Jul 2008;19.
7. Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.15.1H. www.cms.hhs.gov/manuals/downloads/ clm104c12.pdf. Accessed November 19, 2008.
The American Medical Association recently released Current Procedural Terminology (CPT) 2009. New, deleted, and revised codes went into effect Jan. 1. The biggest change to hospitalist billing involves prolonged care codes (99354-99357). CPT 2009 descriptor revisions make it possible for physicians to contribute non-face-to-face time toward prolonged care services.
Inpatient Prolonged Care
Previous versions of CPT defined code 99356 as the first hour of prolonged physician [inpatient] services requiring direct (face-to-face) patient contact beyond the usual services (reportable after the initial 30 minutes); and 99357 for each additional 30 minutes of prolonged [inpatient] care beyond the first hour (reportable after the first 15 minutes of each additional segment). CPT 2009 has changed prolonged care guidelines to be more consistent with other time-based services: all unit/floor time spent by the physician is considered when reporting 99356 and 99357.1
As with most other evaluation and management services, a face-to-face encounter still must occur. In addition to the time associated with the face-to-face encounter, count the time associated with all other physician activities occurring on the unit/floor (e.g., reviewing images, obtaining information involving overnight events, discussing management options with the family) directed toward an individual patient. The cumulative time spent by the billing provider on a single calendar day is considered for billing. Time spent by someone other than the billing provider cannot be credited toward prolonged care.
As example, a physician cares for a 65-year-old male with uncontrolled diabetes, diabetic nephropathy, and congestive heart failure. Early in the day, the physician rounds, spending a total of 20 minutes reviewing the overnight course of events on the unit, re-confirming the patient history, and performing an exam with the patient. Anticipating the patient’s needs, the physician discusses post-discharge options and care with the patient and his family for 45 minutes. After the discussion, the physician spends an additional 30 minutes relaying information to the team and coordinating care. Merely reporting the highest-level subsequent hospital care service (99233), does not capture the physician’s cumulative effort. It only would account for 40 of the 95 minutes spent throughout the day. In order to capture the remaining 55 minutes, the physician reports 99356 on the same claim form as 99233.
Do not report prolonged care codes on a separate claim form. Prolonged care codes do not represent an independent service. These codes are reported along with a primary service. They must appear as a separate line item on the claim form, which includes a code representing the primary service. For prolonged care in the inpatient setting, the primary service must be initial hospital care (99221-99223), subsequent hospital care (99231-99233), inpatient consultations (99251-99255), or nursing facility services (99304-99318). Additional examples of billable prolonged care services are in Section 30.6.15.1I of the Medicare manual, available at www.cms.hhs.gov/manuals/ downloads/clm104c12.pdf.
Threshold Time
Prolonged care guidelines refer to “threshold” time. Threshold time requires the physician to exceed the time requirements associated with the “primary” codes before reporting prolonged care. Table 1 identifies the typical times associated with inpatient services qualifying for prolonged care. The physician must exceed the typical time by a minimum of 30 minutes. (For example, 99232 + 99356 = 25 minutes + 30 minutes = 55 total minutes). Additionally, the physician must document the total time spent during the face-to-face portion of the encounter, and the additional unit or floor time in one cumulative note or in separate notes representing the physician services provided to the patient throughout the day.
Prolonged Outpatient Services
Prolonged care (99354-99355) provided to outpatients remains unchanged. Physicians only report personally provided face-to-face time with the patient. Time spent by other staff members does not count toward prolonged care.
As with prolonged inpatient care, report 99354 and 99355 in addition to a primary service code. The companion outpatient codes are outpatient/office visits (99201-99205 or 99212–99215), outpatient consultation (99241–99245), domiciliary/custodial care (99324–99328 or 99334–99337), and home services (99341-99350). Hospitalists more often use outpatient prolonged care with office consultation codes for services provided in the emergency department, as appropriate.
Do not report 99354 or 99355 with observation care (99217-99220) or emergency department visits (99281-99288), since these service categories typically require prolonged periods of physician monitoring, thereby prohibiting use of prolonged care codes. As with inpatient-prolonged care, the concept of threshold time exists. Refer to Table 2 (pg. 25) for the typical threshold times associated with office consultation codes.
Medicare Consideration
Although CPT has offered revisions to this code, Medicare guidelines remain unchanged. The Medicare Claims Processing Manual still states: “In the case of prolonged hospital services, time spent reviewing charts or discussion of a patient with house medical staff and not with direct face-to-face contact with the patient, or waiting for test results, for changes in the patient’s condition, for end of a therapy, or for use of facilities, cannot be billed as prolonged services.”4 It is yet to be determined if the Centers for Medicare and Medicaid Services (CMS) will issue a transmittal to revise the current description in the processing manual. Physicians and staff may access past and present transmittal information at www.cms.hhs.gov/ Transmittals/.
As always, be sure to query payers about prolonged care services, since some non-Medicare insurers may not recognize these codes.
Modifier 21
Modifier 21 has been deleted from the CPT. Modifier 21 was appended to an appropriate visit code (e.g., 99232-21) when the face-to-face or floor/unit service(s) provided is prolonged or otherwise greater than usually required for the highest level of evaluation and management service within a given category.5 Since the descriptors for codes 99354-99357 have been revised to more consistently reflect the description formerly associated with modifier 21, there is no need to maintain its existence. Additionally, Medicare and most other payers did not recognize this modifier.
Code This Case
Question: A newly diagnosed diabetic requires extensive counseling regarding lifestyle changes, medication regime, the disease process, as well as coordination of care for outpatient programs and services. The hospitalist reviews some of the pertinent information with the patient (15 minutes), and performs an abbreviated service (problem-focused history and exam). The attending physician asks the resident to assist him with the remaining counseling efforts and coordination of care (30 minutes).
Each physician documents his or her portion of the service. What visit level can the hospitalist report?
Answer: When two billing providers (i.e., two attending physicians) from the same group practice split the threshold time (e.g., physician A provided morning rounds, and physician B spoke with the family in the afternoon), only one physician can report the cumulative service, since 99356 must be reported on the same invoice as the primary visit code (e.g., 99231).6
The example above involves the resident’s time as well as the attending physician’s time. Documentation must be very clear to demonstrate the attending physician actively participated in the entire 45-minute service. Otherwise, only the attending may report the amount of time he actually spent providing the service.
Billing options for this scenario can vary. When the physician performs and documents the key components of history, exam, and decision making for the primary encounter, report 99231 (0.76 physician work relative value units; $33.90) and 99356 (1.71 physician work relative value units; $76.46) for the cumulative service. Alternatively, in those evaluation and management services for which the [primary] code level is selected based on time alone (i.e., history and exam was not performed or required), prolonged services may only be reported with the highest code level in that family of codes as the companion code.7
Therefore, this 45-minute service may be reported as 99233 (2.0 physician work relative value units; $86.92) since more than half of the total visit time was dedicated to counseling/coordi-nation of care (see Section 30.6.1B-C available at www. cms.hhs.gov/manuals/ downloads/clm104c12.pdf for additional information on billing for counseling/coordination of care time).
If a payer does not recognize prolonged care codes, only the latter billing option is possible. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is on the faculty of SHM’s inpatient coding course.
References
1. Beebe M, Dalton J, Espronceda M, Evans D, Glenn R. Current Procedural Terminology Professional Edition. Chicago, IL: American Medical Association, 2008; 25-26.
2. Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.15.1G. www.cms.hhs.gov/manuals/downloads/ clm104c12.pdf. Accessed November 19, 2008.
3. Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.15.1F. www.cms.hhs.gov/manuals/dowloads/ clm104c12.pdf. Accessed November 19, 2008.
4. Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.15.1C. www.cms.hhs.gov/manuals/ downloads/clm104c12.pdf. Accessed November 19, 2008.
5. Beebe M, Dalton J, Espronceda M, Evans D, Glenn R. Current Procedural Terminology Professional Edition. Chicago, IL: American Medical Association, 2008; 457.
6. Pohlig, C. Bill by time spent on case. The Hospitalist. Jul 2008;19.
7. Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.15.1H. www.cms.hhs.gov/manuals/downloads/ clm104c12.pdf. Accessed November 19, 2008.
Medicare Modifications
Physicians who count Medicare among their payers already know the government green-lighted a 1.1% increase in Medicare Part B payments to physicians last summer. The increase was made official by the Centers for Medicare and Medicaid Services (CMS) on Oct. 30, with the release of the Medicare Physician Fee Schedule Final Rule for fiscal year 2009. The Final Rule governs what services are reimbursed by Medicare, the reimbursement levels for those services, and other rules pertaining to Medicare. Many of these changes, additions, and deletions were dictated by the Medicare Improvements for Patients and Providers Act, or MIPPA. (See “MIPPA Matters,” December 2008, p. 18.)
The 2009 Final Rule not only makes official the short-term, 1.1% payment increase, it also marks significant increases in payments for inpatient evaluation and management services, higher bonuses for participation in the Physician Quality Reporting Initiative (PQRI), and new policies to help direct the future of healthcare.
Here is a look at a few of the key aspects of the Final Rule, of which you may not be aware:
Transparent Physicians
In a continued effort to make healthcare transparent, CMS will begin posting the names of physicians who successfully report through the 2009 PQRI on a physician compare Web site in 2010. (2007 and 2008 PQRI participants will not be included.) Just as the Hospital Compare site enables consumers to view data on facilities, this site will allow consumers to view data reported by individual doctors.
Although consumers may be interested in checking for information on their primary care physician, it is unlikely inpatients will check the site before agreeing to see a specific hospitalist. However, the Physician Compare site will have some impact on hospital medicine. “I think this is the beginning of physicians’ commitment to greater transparency,” says Eric Siegal, MD, chair of SHM’s Public Policy Committee. “In a very broad sense, physicians who agree to be listed on the Physician Compare site very clearly value transparency and quality of care. Their inclusion could be seen as a differentiator, though a small one.”
Another factor to consider regarding transparency: “Physician Compare is not just about patients,” Dr. Siegal points out. “Third-party payers will look at this, as well. If they’re looking for someone to help take care of their patients, this data might sway them in their decision.”
Telehealth and Inpatients
Medicare already reimburses for certain exchanges of medical information from off-site physicians or vendors via interactive electronic communications, also known as telehealth or telemedicine services. Under the 2009 Final Rule, CMS will create a new series of Healthcare Common Procedure Coding System (HCPCS) codes for follow-up inpatient telehealth consultations, allowing practitioners to bill for follow-up inpatient consultations delivered via telehealth.
These codes are intended for use by physicians or non-physician providers when an inpatient consultation is requested from an appropriate source, such as the patient’s attending physician. CMS emphasizes the codes are not intended for use in billing for the ongoing evaluation and management of a hospital inpatient.
E-prescribe Out of Reach
Much attention has been given to a new Medicare program, which promotes the widespread adoption of electronic prescribing (e-prescribing). Physicians who successfully participate in CMS’ Electronic Prescribing Incentive Program will earn an extra bonus; however, the program was designed for primary care programs and hospitalists are unlikely to be able to take advantage of this.
“We don’t even know if hospitalists will be able to participate,” Dr. Siegal explains. The only way a hospitalist can take part in the e-prescribing initiative is if the hospital already has an acceptable system. However, Dr. Siegal warns, “If you create a mandate requiring a system for medication reconciliation at discharge, and then require another, separate system for e-prescribing, you’ve got problems. The primary driver should be that the hospital’s system supports both. And as far as we can tell, most hospital systems don’t do this.”
In August, SHM and the American College of Emergency Physicians conducted a teleconference with CMS to voice concerns with the e-prescribe initiative. “What we wanted was an exception,” Dr. Siegal says. SHM’s concern: When CMS stops rewarding physicians for e-prescribing and begins to penalize those who don’t—currently scheduled for 2013—hospitalists who can’t participate will be penalized through their Medicare payments. The outcome of the meeting, Dr. Siegal says, is “CMS turned around and said ‘either you can participate or you can’t.’ But at least they are considering our points; they seem to understand them.”
The good news is there is time to work the problem out, “At the moment, while e-prescribing is all bonus and no penalty, there’s no urgency to address it,” Dr. Siegal says.
Patient Safety
The Final Rule also includes improvements to PQRI, which allows eligible professionals to report on 153 quality measures. Physicians who successfully report on cases during 2009 will be able to earn an incentive payment, which has been increased to 2% (up from 1.5% in 2008), of their total allowed charges for covered professional services.
“I hope that more hospitalists will get on board with this,” Dr. Siegal says. He believes PQRI will be around for a while, and any hospital medicine group waiting to see if it is worth investing in the program can safely do so. “My feeling is that there’s growing bi-partisan support for something like this. I think it’s here to stay,” Dr. Siegal says.
SHM’s Opinion Counts
One reason the Final Rule is especially hospitalist-friendly is because SHM submitted extensive comment on CMS’s proposals in August. “SHM had a fair amount to say, and there are things in the rule that dovetail with our comments,” Dr. Siegal explains. “Part of the challenge is picking which battles to fight; there is a lot covered in this rule. We ended up focusing on areas that were really important to us, and on items where we thought we had a unique voice where nobody else was going to articulate.”
The Final Rule is available at www.cms.hhs.gov/center/physician.asp under “CMS-1403-FC.” Fact sheets covering major provisions of the Final Rule are available at www.cms.hhs.gov/apps/media/ fact_sheets.asp. TH
Jane Jerrard is a medical writer based in Chicago.
Physicians who count Medicare among their payers already know the government green-lighted a 1.1% increase in Medicare Part B payments to physicians last summer. The increase was made official by the Centers for Medicare and Medicaid Services (CMS) on Oct. 30, with the release of the Medicare Physician Fee Schedule Final Rule for fiscal year 2009. The Final Rule governs what services are reimbursed by Medicare, the reimbursement levels for those services, and other rules pertaining to Medicare. Many of these changes, additions, and deletions were dictated by the Medicare Improvements for Patients and Providers Act, or MIPPA. (See “MIPPA Matters,” December 2008, p. 18.)
The 2009 Final Rule not only makes official the short-term, 1.1% payment increase, it also marks significant increases in payments for inpatient evaluation and management services, higher bonuses for participation in the Physician Quality Reporting Initiative (PQRI), and new policies to help direct the future of healthcare.
Here is a look at a few of the key aspects of the Final Rule, of which you may not be aware:
Transparent Physicians
In a continued effort to make healthcare transparent, CMS will begin posting the names of physicians who successfully report through the 2009 PQRI on a physician compare Web site in 2010. (2007 and 2008 PQRI participants will not be included.) Just as the Hospital Compare site enables consumers to view data on facilities, this site will allow consumers to view data reported by individual doctors.
Although consumers may be interested in checking for information on their primary care physician, it is unlikely inpatients will check the site before agreeing to see a specific hospitalist. However, the Physician Compare site will have some impact on hospital medicine. “I think this is the beginning of physicians’ commitment to greater transparency,” says Eric Siegal, MD, chair of SHM’s Public Policy Committee. “In a very broad sense, physicians who agree to be listed on the Physician Compare site very clearly value transparency and quality of care. Their inclusion could be seen as a differentiator, though a small one.”
Another factor to consider regarding transparency: “Physician Compare is not just about patients,” Dr. Siegal points out. “Third-party payers will look at this, as well. If they’re looking for someone to help take care of their patients, this data might sway them in their decision.”
Telehealth and Inpatients
Medicare already reimburses for certain exchanges of medical information from off-site physicians or vendors via interactive electronic communications, also known as telehealth or telemedicine services. Under the 2009 Final Rule, CMS will create a new series of Healthcare Common Procedure Coding System (HCPCS) codes for follow-up inpatient telehealth consultations, allowing practitioners to bill for follow-up inpatient consultations delivered via telehealth.
These codes are intended for use by physicians or non-physician providers when an inpatient consultation is requested from an appropriate source, such as the patient’s attending physician. CMS emphasizes the codes are not intended for use in billing for the ongoing evaluation and management of a hospital inpatient.
E-prescribe Out of Reach
Much attention has been given to a new Medicare program, which promotes the widespread adoption of electronic prescribing (e-prescribing). Physicians who successfully participate in CMS’ Electronic Prescribing Incentive Program will earn an extra bonus; however, the program was designed for primary care programs and hospitalists are unlikely to be able to take advantage of this.
“We don’t even know if hospitalists will be able to participate,” Dr. Siegal explains. The only way a hospitalist can take part in the e-prescribing initiative is if the hospital already has an acceptable system. However, Dr. Siegal warns, “If you create a mandate requiring a system for medication reconciliation at discharge, and then require another, separate system for e-prescribing, you’ve got problems. The primary driver should be that the hospital’s system supports both. And as far as we can tell, most hospital systems don’t do this.”
In August, SHM and the American College of Emergency Physicians conducted a teleconference with CMS to voice concerns with the e-prescribe initiative. “What we wanted was an exception,” Dr. Siegal says. SHM’s concern: When CMS stops rewarding physicians for e-prescribing and begins to penalize those who don’t—currently scheduled for 2013—hospitalists who can’t participate will be penalized through their Medicare payments. The outcome of the meeting, Dr. Siegal says, is “CMS turned around and said ‘either you can participate or you can’t.’ But at least they are considering our points; they seem to understand them.”
The good news is there is time to work the problem out, “At the moment, while e-prescribing is all bonus and no penalty, there’s no urgency to address it,” Dr. Siegal says.
Patient Safety
The Final Rule also includes improvements to PQRI, which allows eligible professionals to report on 153 quality measures. Physicians who successfully report on cases during 2009 will be able to earn an incentive payment, which has been increased to 2% (up from 1.5% in 2008), of their total allowed charges for covered professional services.
“I hope that more hospitalists will get on board with this,” Dr. Siegal says. He believes PQRI will be around for a while, and any hospital medicine group waiting to see if it is worth investing in the program can safely do so. “My feeling is that there’s growing bi-partisan support for something like this. I think it’s here to stay,” Dr. Siegal says.
SHM’s Opinion Counts
One reason the Final Rule is especially hospitalist-friendly is because SHM submitted extensive comment on CMS’s proposals in August. “SHM had a fair amount to say, and there are things in the rule that dovetail with our comments,” Dr. Siegal explains. “Part of the challenge is picking which battles to fight; there is a lot covered in this rule. We ended up focusing on areas that were really important to us, and on items where we thought we had a unique voice where nobody else was going to articulate.”
The Final Rule is available at www.cms.hhs.gov/center/physician.asp under “CMS-1403-FC.” Fact sheets covering major provisions of the Final Rule are available at www.cms.hhs.gov/apps/media/ fact_sheets.asp. TH
Jane Jerrard is a medical writer based in Chicago.
Physicians who count Medicare among their payers already know the government green-lighted a 1.1% increase in Medicare Part B payments to physicians last summer. The increase was made official by the Centers for Medicare and Medicaid Services (CMS) on Oct. 30, with the release of the Medicare Physician Fee Schedule Final Rule for fiscal year 2009. The Final Rule governs what services are reimbursed by Medicare, the reimbursement levels for those services, and other rules pertaining to Medicare. Many of these changes, additions, and deletions were dictated by the Medicare Improvements for Patients and Providers Act, or MIPPA. (See “MIPPA Matters,” December 2008, p. 18.)
The 2009 Final Rule not only makes official the short-term, 1.1% payment increase, it also marks significant increases in payments for inpatient evaluation and management services, higher bonuses for participation in the Physician Quality Reporting Initiative (PQRI), and new policies to help direct the future of healthcare.
Here is a look at a few of the key aspects of the Final Rule, of which you may not be aware:
Transparent Physicians
In a continued effort to make healthcare transparent, CMS will begin posting the names of physicians who successfully report through the 2009 PQRI on a physician compare Web site in 2010. (2007 and 2008 PQRI participants will not be included.) Just as the Hospital Compare site enables consumers to view data on facilities, this site will allow consumers to view data reported by individual doctors.
Although consumers may be interested in checking for information on their primary care physician, it is unlikely inpatients will check the site before agreeing to see a specific hospitalist. However, the Physician Compare site will have some impact on hospital medicine. “I think this is the beginning of physicians’ commitment to greater transparency,” says Eric Siegal, MD, chair of SHM’s Public Policy Committee. “In a very broad sense, physicians who agree to be listed on the Physician Compare site very clearly value transparency and quality of care. Their inclusion could be seen as a differentiator, though a small one.”
Another factor to consider regarding transparency: “Physician Compare is not just about patients,” Dr. Siegal points out. “Third-party payers will look at this, as well. If they’re looking for someone to help take care of their patients, this data might sway them in their decision.”
Telehealth and Inpatients
Medicare already reimburses for certain exchanges of medical information from off-site physicians or vendors via interactive electronic communications, also known as telehealth or telemedicine services. Under the 2009 Final Rule, CMS will create a new series of Healthcare Common Procedure Coding System (HCPCS) codes for follow-up inpatient telehealth consultations, allowing practitioners to bill for follow-up inpatient consultations delivered via telehealth.
These codes are intended for use by physicians or non-physician providers when an inpatient consultation is requested from an appropriate source, such as the patient’s attending physician. CMS emphasizes the codes are not intended for use in billing for the ongoing evaluation and management of a hospital inpatient.
E-prescribe Out of Reach
Much attention has been given to a new Medicare program, which promotes the widespread adoption of electronic prescribing (e-prescribing). Physicians who successfully participate in CMS’ Electronic Prescribing Incentive Program will earn an extra bonus; however, the program was designed for primary care programs and hospitalists are unlikely to be able to take advantage of this.
“We don’t even know if hospitalists will be able to participate,” Dr. Siegal explains. The only way a hospitalist can take part in the e-prescribing initiative is if the hospital already has an acceptable system. However, Dr. Siegal warns, “If you create a mandate requiring a system for medication reconciliation at discharge, and then require another, separate system for e-prescribing, you’ve got problems. The primary driver should be that the hospital’s system supports both. And as far as we can tell, most hospital systems don’t do this.”
In August, SHM and the American College of Emergency Physicians conducted a teleconference with CMS to voice concerns with the e-prescribe initiative. “What we wanted was an exception,” Dr. Siegal says. SHM’s concern: When CMS stops rewarding physicians for e-prescribing and begins to penalize those who don’t—currently scheduled for 2013—hospitalists who can’t participate will be penalized through their Medicare payments. The outcome of the meeting, Dr. Siegal says, is “CMS turned around and said ‘either you can participate or you can’t.’ But at least they are considering our points; they seem to understand them.”
The good news is there is time to work the problem out, “At the moment, while e-prescribing is all bonus and no penalty, there’s no urgency to address it,” Dr. Siegal says.
Patient Safety
The Final Rule also includes improvements to PQRI, which allows eligible professionals to report on 153 quality measures. Physicians who successfully report on cases during 2009 will be able to earn an incentive payment, which has been increased to 2% (up from 1.5% in 2008), of their total allowed charges for covered professional services.
“I hope that more hospitalists will get on board with this,” Dr. Siegal says. He believes PQRI will be around for a while, and any hospital medicine group waiting to see if it is worth investing in the program can safely do so. “My feeling is that there’s growing bi-partisan support for something like this. I think it’s here to stay,” Dr. Siegal says.
SHM’s Opinion Counts
One reason the Final Rule is especially hospitalist-friendly is because SHM submitted extensive comment on CMS’s proposals in August. “SHM had a fair amount to say, and there are things in the rule that dovetail with our comments,” Dr. Siegal explains. “Part of the challenge is picking which battles to fight; there is a lot covered in this rule. We ended up focusing on areas that were really important to us, and on items where we thought we had a unique voice where nobody else was going to articulate.”
The Final Rule is available at www.cms.hhs.gov/center/physician.asp under “CMS-1403-FC.” Fact sheets covering major provisions of the Final Rule are available at www.cms.hhs.gov/apps/media/ fact_sheets.asp. TH
Jane Jerrard is a medical writer based in Chicago.
Beware Office Politics
Hospitalists routinely confront clinical, administrative, and ethical issues. Sometimes they face less-identifiable issues, such as office politics. Webster’s Dictionary defines office politics as “factional scheming for power and status within a group.” Wikipedia describes office politics as “the use of one’s individual or assigned power within an employing organization for the purpose of obtaining advantages beyond one’s legitimate authority.”
How much does office politics affect hospital medicine?
“Of course there is office politics in any work environment,” says Heather A. Harris, MD, former director of Eden Inpatient Services in Castro Valley, Calif., and currently splitting time as a hospitalist at the University of California San Francisco and the Palo Alto Medical Foundation. Dr. Harris, however, believes office politics is rare within hospital medicine because, “It is a young field and a growing field; everyone is growing together, so things tend to be pretty democratic. This is especially true of newer groups.”
Then again, there are times hospitalists find themselves embroiled in office politics. When this happens, what should you do?
Take the High Ground
Although she’s encountered few cases of office politics in her career, Dr. Harris’ general advice for hospitalists is, “First, recognize it, and then try to be a good team player.” Stay above the fray and try to tread carefully around political situations, especially if you’re a manager or informal leader.
Mary Jo Gorman, MD, MBA, CEO of Advanced ICU Care in St. Louis, and former SHM president, advises hospitalists and group directors to “take the high ground, no matter how frustrated you become.” She stresses discretion: “You can talk about it to your spouse, but if you’re a leader, you can’t even [comment on someone’s behavior] in front of your group. You never know, especially if you’re in a relatively small community, when you’re going to need someone’s support. You need to stay on good terms with people.” Dr. Gorman’s advice for leaders holds true for individuals hospitalists caught up in office politics.
Power Struggles
The role hospital medicine groups play as change agents probably is the main reason office politics may develop. “Any time you’re introducing a new concept that somebody feels threatened by, you’re going to incur some defensive maneuvers,” Dr. Gorman warns. “Whether you’re introducing a new hospital medicine group, or trying to change something, like the admissions process in the emergency room, you’re going to disrupt someone’s actions. Then you’ll find a whole broad range of reactions. And the more a person feels threatened, the more aggressive they’ll become.”
Based on her experiences establishing Eden Inpatient Services in 2003, Dr. Harris knows bringing a hospital medicine group into a hospital for the first time can be “a very political situation.” You can be stepping on personal, professional, and financial toes. “When you’re part of a new hospital medicine group … you’re potentially poised to take a lot of business away from people,” Dr. Harris explains. “It’s difficult to navigate those waters and build relationships” with physicians you’re consulting with and with primary care physicians. “In a way, this even extends to nurses,” she says. “You’re suddenly going to be working with them on patient care, and changing the way they work.” Dr. Harris encourages hospitalists to be aware of touchy situations, so as not to inadvertently fuel the fire of office politics. “Especially for young physicians just starting out, there can be a lack of recognition of other people’s feelings and turfs,” she cautions.
Hospitalists faced with an office issue should combine the cautionary approach with a willingness to work with people, even those who are engaging in office politics. “When you’re implementing a change, regardless of what it is, you need to identify who will think it’s a good thing and who will not,” Dr. Gorman advises. “You need to speak with individuals in the latter group, or choose others to speak to them, to garner their support.”
Take, for example, proposing a new project for your hospital’s Quality Improvement committee. A cautionary approach and team building will go a long way. “You’ve got to get to the people on the committee ahead of time, explain what you want to do, and get their feedback and support,” Dr. Gorman says. “If you find someone who opposes it, make sure you have enough support to override them. Or, better yet, find someone who can approach them on the topic, maybe their partner or another member of their group. This is a very practical approach.”
Identify Informal Leadership
When considering this inclusive approach, don’t forget the indirect leadership. “You may have a member of the medical staff who has some informal authority or power, maybe they have the most years of experience, or bring a lot of patients to the hospital, or maybe they are a member of the same group as someone in power,” Dr. Gorman says. “These informal leaders can create a lot of disturbance.”
To avoid problems, either direct or indirect, with these types of people, identify them early and make it a point to include them in the plan. “Usually, you know who holds informal power within your organization or the hospital,” Dr. Gorman says. “All you have to do is talk to them and explain what you’re doing. No one likes to be surprised. You might have to make some changes to accommodate their concerns.”
If this tactic fails and you still face opposition, you might have to weigh how important the opposition is. “You may decide to move ahead, even if you have to make changes and the project takes more time,” she says. “For physicians working in hospitals, we’re all used to instant results. You have to understand that process change takes time and you may have to take something bit by bit, and not get immediate results or responses.”
Be tactful about other professionals’ territories and feelings. Keep communication open and avoid springing surprises on stakeholders. Most importantly, stick to the high ground. These simple steps can help you stay far from the minefield known as office politics. TH
Jane Jerrard is a medical writer based in Chicago. She also writes “Public Policy” for The Hospitalist.
Hospitalists routinely confront clinical, administrative, and ethical issues. Sometimes they face less-identifiable issues, such as office politics. Webster’s Dictionary defines office politics as “factional scheming for power and status within a group.” Wikipedia describes office politics as “the use of one’s individual or assigned power within an employing organization for the purpose of obtaining advantages beyond one’s legitimate authority.”
How much does office politics affect hospital medicine?
“Of course there is office politics in any work environment,” says Heather A. Harris, MD, former director of Eden Inpatient Services in Castro Valley, Calif., and currently splitting time as a hospitalist at the University of California San Francisco and the Palo Alto Medical Foundation. Dr. Harris, however, believes office politics is rare within hospital medicine because, “It is a young field and a growing field; everyone is growing together, so things tend to be pretty democratic. This is especially true of newer groups.”
Then again, there are times hospitalists find themselves embroiled in office politics. When this happens, what should you do?
Take the High Ground
Although she’s encountered few cases of office politics in her career, Dr. Harris’ general advice for hospitalists is, “First, recognize it, and then try to be a good team player.” Stay above the fray and try to tread carefully around political situations, especially if you’re a manager or informal leader.
Mary Jo Gorman, MD, MBA, CEO of Advanced ICU Care in St. Louis, and former SHM president, advises hospitalists and group directors to “take the high ground, no matter how frustrated you become.” She stresses discretion: “You can talk about it to your spouse, but if you’re a leader, you can’t even [comment on someone’s behavior] in front of your group. You never know, especially if you’re in a relatively small community, when you’re going to need someone’s support. You need to stay on good terms with people.” Dr. Gorman’s advice for leaders holds true for individuals hospitalists caught up in office politics.
Power Struggles
The role hospital medicine groups play as change agents probably is the main reason office politics may develop. “Any time you’re introducing a new concept that somebody feels threatened by, you’re going to incur some defensive maneuvers,” Dr. Gorman warns. “Whether you’re introducing a new hospital medicine group, or trying to change something, like the admissions process in the emergency room, you’re going to disrupt someone’s actions. Then you’ll find a whole broad range of reactions. And the more a person feels threatened, the more aggressive they’ll become.”
Based on her experiences establishing Eden Inpatient Services in 2003, Dr. Harris knows bringing a hospital medicine group into a hospital for the first time can be “a very political situation.” You can be stepping on personal, professional, and financial toes. “When you’re part of a new hospital medicine group … you’re potentially poised to take a lot of business away from people,” Dr. Harris explains. “It’s difficult to navigate those waters and build relationships” with physicians you’re consulting with and with primary care physicians. “In a way, this even extends to nurses,” she says. “You’re suddenly going to be working with them on patient care, and changing the way they work.” Dr. Harris encourages hospitalists to be aware of touchy situations, so as not to inadvertently fuel the fire of office politics. “Especially for young physicians just starting out, there can be a lack of recognition of other people’s feelings and turfs,” she cautions.
Hospitalists faced with an office issue should combine the cautionary approach with a willingness to work with people, even those who are engaging in office politics. “When you’re implementing a change, regardless of what it is, you need to identify who will think it’s a good thing and who will not,” Dr. Gorman advises. “You need to speak with individuals in the latter group, or choose others to speak to them, to garner their support.”
Take, for example, proposing a new project for your hospital’s Quality Improvement committee. A cautionary approach and team building will go a long way. “You’ve got to get to the people on the committee ahead of time, explain what you want to do, and get their feedback and support,” Dr. Gorman says. “If you find someone who opposes it, make sure you have enough support to override them. Or, better yet, find someone who can approach them on the topic, maybe their partner or another member of their group. This is a very practical approach.”
Identify Informal Leadership
When considering this inclusive approach, don’t forget the indirect leadership. “You may have a member of the medical staff who has some informal authority or power, maybe they have the most years of experience, or bring a lot of patients to the hospital, or maybe they are a member of the same group as someone in power,” Dr. Gorman says. “These informal leaders can create a lot of disturbance.”
To avoid problems, either direct or indirect, with these types of people, identify them early and make it a point to include them in the plan. “Usually, you know who holds informal power within your organization or the hospital,” Dr. Gorman says. “All you have to do is talk to them and explain what you’re doing. No one likes to be surprised. You might have to make some changes to accommodate their concerns.”
If this tactic fails and you still face opposition, you might have to weigh how important the opposition is. “You may decide to move ahead, even if you have to make changes and the project takes more time,” she says. “For physicians working in hospitals, we’re all used to instant results. You have to understand that process change takes time and you may have to take something bit by bit, and not get immediate results or responses.”
Be tactful about other professionals’ territories and feelings. Keep communication open and avoid springing surprises on stakeholders. Most importantly, stick to the high ground. These simple steps can help you stay far from the minefield known as office politics. TH
Jane Jerrard is a medical writer based in Chicago. She also writes “Public Policy” for The Hospitalist.
Hospitalists routinely confront clinical, administrative, and ethical issues. Sometimes they face less-identifiable issues, such as office politics. Webster’s Dictionary defines office politics as “factional scheming for power and status within a group.” Wikipedia describes office politics as “the use of one’s individual or assigned power within an employing organization for the purpose of obtaining advantages beyond one’s legitimate authority.”
How much does office politics affect hospital medicine?
“Of course there is office politics in any work environment,” says Heather A. Harris, MD, former director of Eden Inpatient Services in Castro Valley, Calif., and currently splitting time as a hospitalist at the University of California San Francisco and the Palo Alto Medical Foundation. Dr. Harris, however, believes office politics is rare within hospital medicine because, “It is a young field and a growing field; everyone is growing together, so things tend to be pretty democratic. This is especially true of newer groups.”
Then again, there are times hospitalists find themselves embroiled in office politics. When this happens, what should you do?
Take the High Ground
Although she’s encountered few cases of office politics in her career, Dr. Harris’ general advice for hospitalists is, “First, recognize it, and then try to be a good team player.” Stay above the fray and try to tread carefully around political situations, especially if you’re a manager or informal leader.
Mary Jo Gorman, MD, MBA, CEO of Advanced ICU Care in St. Louis, and former SHM president, advises hospitalists and group directors to “take the high ground, no matter how frustrated you become.” She stresses discretion: “You can talk about it to your spouse, but if you’re a leader, you can’t even [comment on someone’s behavior] in front of your group. You never know, especially if you’re in a relatively small community, when you’re going to need someone’s support. You need to stay on good terms with people.” Dr. Gorman’s advice for leaders holds true for individuals hospitalists caught up in office politics.
Power Struggles
The role hospital medicine groups play as change agents probably is the main reason office politics may develop. “Any time you’re introducing a new concept that somebody feels threatened by, you’re going to incur some defensive maneuvers,” Dr. Gorman warns. “Whether you’re introducing a new hospital medicine group, or trying to change something, like the admissions process in the emergency room, you’re going to disrupt someone’s actions. Then you’ll find a whole broad range of reactions. And the more a person feels threatened, the more aggressive they’ll become.”
Based on her experiences establishing Eden Inpatient Services in 2003, Dr. Harris knows bringing a hospital medicine group into a hospital for the first time can be “a very political situation.” You can be stepping on personal, professional, and financial toes. “When you’re part of a new hospital medicine group … you’re potentially poised to take a lot of business away from people,” Dr. Harris explains. “It’s difficult to navigate those waters and build relationships” with physicians you’re consulting with and with primary care physicians. “In a way, this even extends to nurses,” she says. “You’re suddenly going to be working with them on patient care, and changing the way they work.” Dr. Harris encourages hospitalists to be aware of touchy situations, so as not to inadvertently fuel the fire of office politics. “Especially for young physicians just starting out, there can be a lack of recognition of other people’s feelings and turfs,” she cautions.
Hospitalists faced with an office issue should combine the cautionary approach with a willingness to work with people, even those who are engaging in office politics. “When you’re implementing a change, regardless of what it is, you need to identify who will think it’s a good thing and who will not,” Dr. Gorman advises. “You need to speak with individuals in the latter group, or choose others to speak to them, to garner their support.”
Take, for example, proposing a new project for your hospital’s Quality Improvement committee. A cautionary approach and team building will go a long way. “You’ve got to get to the people on the committee ahead of time, explain what you want to do, and get their feedback and support,” Dr. Gorman says. “If you find someone who opposes it, make sure you have enough support to override them. Or, better yet, find someone who can approach them on the topic, maybe their partner or another member of their group. This is a very practical approach.”
Identify Informal Leadership
When considering this inclusive approach, don’t forget the indirect leadership. “You may have a member of the medical staff who has some informal authority or power, maybe they have the most years of experience, or bring a lot of patients to the hospital, or maybe they are a member of the same group as someone in power,” Dr. Gorman says. “These informal leaders can create a lot of disturbance.”
To avoid problems, either direct or indirect, with these types of people, identify them early and make it a point to include them in the plan. “Usually, you know who holds informal power within your organization or the hospital,” Dr. Gorman says. “All you have to do is talk to them and explain what you’re doing. No one likes to be surprised. You might have to make some changes to accommodate their concerns.”
If this tactic fails and you still face opposition, you might have to weigh how important the opposition is. “You may decide to move ahead, even if you have to make changes and the project takes more time,” she says. “For physicians working in hospitals, we’re all used to instant results. You have to understand that process change takes time and you may have to take something bit by bit, and not get immediate results or responses.”
Be tactful about other professionals’ territories and feelings. Keep communication open and avoid springing surprises on stakeholders. Most importantly, stick to the high ground. These simple steps can help you stay far from the minefield known as office politics. TH
Jane Jerrard is a medical writer based in Chicago. She also writes “Public Policy” for The Hospitalist.
The latest research you need to know
In This Edition
- Aspirin plus extended-release dipyridamole and clopidogrel provide similar outcomes in stroke.
- Traditional readings of bedside chest radiographs are insensitive in detecting intraatrial central venous catheter placement.
- Improved outcomes with bortezomib in myeloma treatment.
- ICD firings in cardiomyopathy patients are associated with worse outcomes.
- The clinical dehydration scale rapidly assesses the severity of dehydration in children.
- Liberal red blood cell transfusions may be harming patients.
- Five-year risk of colorectal neoplasia is low in patients with negative screening colonoscopy.
- Vital sign instability and oxygenation predict prognosis following hospitalization for community acquired pneumonia.
Is aspirin plus extended release dipyridamole more efficacious and safer than clopidogrel in preventing recurrent stroke?
Background: Recurrent stroke is a frequent (7% to 8% thrombotic stroke recurrence in first year) and disabling event after ischemic stroke. Multiple randomized trials demonstrate efficacy of anti-platelet agents for the prevention of recurrent stroke after non-cardioembolic stroke. However, direct comparisons and relative benefits of various antiplatelet agents are not well defined.
Study design: Randomized, double-blinded, two-by-two factorial design with intention-to-treat analysis.
Setting: A total of 20,333 patients from 695 centers in 35 countries, including the U.S.
Synopsis: This study directly compared aspirin plus extended-release dipyridamole to clopidogrel within the PRoFESS trial. A total of 20,333 patients were enrolled and followed up for a mean duration of 2.5 years. Eligible patients randomly were assigned to receive either 25 mg aspirin plus 200 mg extended-release twice a day, or clopidogrel 75 mg a day; and either telmisartan 80 mg once a day or placebo. Groups were similar at baseline.
The primary outcome of recurrent stroke was similar in both the aspirin plus extended-release dipyrimadole group and the clopidogrel group (9.0% vs. 8.8%). The composite secondary outcome of stroke, myocardial infarction or vascular death, and tertiary outcomes were similar in both groups. The trial showed statistical equivalence in the rates of recurrent stroke in the two groups.
Despite more frequent hemorrhagic strokes in the group receiving aspirin plus extended-release dipyridamole (4.1% vs. 3.6%), there was no significant difference in the risk of fatal or disabling stroke between both the groups.
Bottom line: Aspirin plus extended-release dipyridamole is equivalent to clopidogrel in the prevention of recurrent stroke, in terms of relevant efficacy and safety parameters.
Citation: Sacco RL, Diener H, Yusuf S, et.al. Aspirin and extended-release dipyridamole versus clopidogrel for recurrent stroke. N Engl J Med. 2008:359:1238-1251.
Is there a better method to judge the placement of central venous catheters?
Background: Placement of central venous catheters is common, particularly in critical care settings. Correct placement is usually confirmed by bedside chest radiography. The recommended location of the distal catheter tip is superior to the superior vena cava and right atria junction. However, determining this landmark on traditional bedside chest radiographs is frequently inaccurate.
Study design: Prospective, blinded study.
Setting: University hospital in Germany.
Synopsis: The researchers enrolled 212 patients scheduled for elective cardiac surgery. Either left or right internal jugular vein central lines were placed via EKG guidance, and more precisely evaluated by transesophageal echocardiography. Bedside chest radiographs were performed within three hours of admission to the ICU.
The radiologists were able to detect between 40% and 60% of incorrect central venous catheter placements when compared to transesophageal echocardiography. The researchers concluded TC-distance (tip of catheter to carina) of greater than 55 mm on chest X-ray performed better (98% accurate) in the detection of intra-atrial catheter placement, compared to conventional judgment by attending (93% accurate) or resident (53% accurate) radiologists. Limitations of the study include the use of only one attending radiologist. Secondly, the chest radiographs and echocardiograms were not done simultaneously, allowing for possible movement of the catheters between studies.
Bottom line: A TC distance of greater than 55 mm on chest X-ray should be further investigated as an accurate method to detect intra-atrial central venous catheters.
Citation: Wirsing M, Schummer C, Neumann R, et al. Is traditional reading of the bedside chest radiograph appropriate to detect intra-atrial central venous catheter position? Chest. 2008;134:527-533.
Does adding bortezomib to melphalan and prednisone improve outcomes in newly diagnosed myeloma?
Background: More than 50% of newly diagnosed myeloma patients are older than 65 and cannot receive optimal treatment with high-dose chemotherapy and stem-cell transplant. Previous trials have demonstrated patients with relapsed or refractory myeloma benefit from the administration of bortezomib, which sensitizes the myeloma cell lines to melphalan.
Study design: Randomized, open-label (unblinded) phase 3 study.
Setting: 151 centers, 22 countries in Asia, Europe, South and North America.
Synopsis: 682 patients with untreated multiple myeloma, who were ineligible for high-dose chemotherapy and stem cell transplant, were treated with bortezomib in combination with standard melphalan and prednisone, or melphalan and prednisone alone. The bortezomib group had improved partial or complete response (71% vs. 35%; NNT=3; p<0.001), increased median time to progression of disease (19.9 months vs. 13.1 months), and improved overall survival (87% vs. 78% over a 16-month median follow up; NNT=11; p=0.008). There were increased grade 3 adverse effects with the intervention, but no increase in grade 4 events or treatment related deaths compared to control. Limitations of the study include lack of blinding and involvement of the pharmaceutical company in data collection analysis, writing and editing of the manuscript.
Bottom line: Bortezomib is a valuable adjunct to standard treatment of multiple myeloma in patients over the age of 65 who may be ineligible for high-dose chemotherapy and stem cell transplant.
Citation: San Miguel JF, Schlag R, Khuageva NK, et al. Bortezomib plus melphalan and prednisone for the initial treatment of multiple myeloma. NEJM. 2008;359:906-917.
Does the occurrence of a shock increase the risk of death in cardiomyopathy patients with defibrillators?
Background: The SCD-HeFT trial, originally published in 2005, was instrumental in demonstrating the utility of defibrillators in the primary prevention of sudden cardiac deaths in patients with either ischemic or non-ischemic cardiomyopathy, NYHA class II or III, ejection fraction <35%, and no history of sustained ventricular tachycardia or fibrillation. This study re-examined the data derived from the SCD-HeFT trial to better understand the long-term prognosis of these patients with defibrillators who receive either appropriate shocks (ventricular fibrillation, sustained ventricular tachycardia), inappropriate shocks, or no shocks. Inappropriate shocks were defined as defibrillations due to supraventricular tachycardia, oversensing P or T waves as R waves, double counting of R waves, and artifact.
Study design: Retrospective cohort (analysis of patients randomized to implantable cardioverter-defibrillator (ICD) group in SCD-HeFT).
Setting: Multicenter trial.
Synopsis: The analysis demonstrated patients who received shocks were 11 times more likely to die compared with those who had no defibrillations (Hazard Ratio [HR]=11.3, p<0.001). These shocked patients were at more risk (HR=5.7, p<0.001) than those with inappropriate shocks (HR=2.0, p=0.002). Therefore, even inappropriate shocks themselves doubled the risk of death. Patients who received more than one shock, either appropriate or not, were at even higher odds of death (HR=8.3, p<0.001). The results highlight the higher mortality risk when patients with ICDs have received a shock (appropriate or inappropriate) and the need for further therapies to modify outcome in these patients.
Bottom Line: Appropriate or inappropriate defibrillations are associated with a poorer prognosis in patients with cardiomyopathy.
Citation: Poole JE, Johnson GW, Hellkamp AS, et al. Prognostic importance of defibrillator shocks in patients with heart failure. N Engl J Med. 2008(359):1009-1017.
Can a simple physical exam tool assess the degree of dehydration in children?
Background: Despite the frequency and the associated cost of acute gastroenteritis (AGE) in the pediatric population, there is no unified scale to assess the severity of dehydration. The authors of this paper previously reported a clinical dehydration scale (CDS) and applied it prospectively in a new cohort of patients ages 1 month to 5 years.
Study design: Prospective, observational study.
Setting: Single, tertiary care emergency department (ED) in Canada.
Synopsis: The CDS score is based purely on the physical findings of the child, including a) general appearance, b) eyes, c) mucous membranes, and d) amount of tears. On a point system, the patient is placed in one of three categories: no dehydration, some dehydration, moderate/severe dehydration. The trial enrolled 205 children and the CDS was applied by the triaging nurse. The attending ED pediatricians were blinded from this assessment. The CDS was able to predict the length of stay (mean + SD: no dehyrdation 245 + 181 mins; some dehydration, 397 + 302 mins; mod/severe dehydration, 501 + 389 mins), need for intravenous rehydration (none, 15%; some, 49%; mod/severe, 80%), and frequency of emesis/diarrhea as reported by the parents (none, 8.4 + 7.7; some, 13 + 10.7; mod/severe, 30.2 + 14.8). Only five children were categorized in the moderate/severe dehydration category, which may limit the ability to generalize the scoring system to that group of patients.
Bottom line: The CDS is an easy to use and promising tool to assess the severity of illness, expected ED length of stay, and need for intravenous rehydration in children with acute gastroenteritis.
Citation: Goldman RD, Friedman JN, Parkin PC. Validation of the clinical dehydration scale for children with acute gastroenteritis. Pediatrics. 2008;122(3):545-549.
Does maintaining a higher hemoglobin level benefit critical care patients?
Background: Historically, medical and surgical critical care patients liberally were transfused with little prospective evidence to support this approach. However, recent evidence has led to the use of a more-restricted transfusion threshold.
Study design: Systematic review and meta-analysis of cohort studies evaluating the effect of red blood cell (RBC) transfusion on patient outcomes.
Setting: Data sources include MEDLINE, Embase, and Cochrane databases.
Synopsis: The 45 cohort studies, including more than 272,000 patients, were selected due to focus on outcome measures, such as mortality, multiorgan dysfunction, acute respiratory distress syndrome, and infections. Primary studies were then placed into one of three categories: benefits outweigh the risk, neutral, or risks outweigh the benefit. Forty-two of these studies found the risks outweigh the benefits; two were neutral; and only one sub-study (in elderly patients with acute myocardial infarctions) suggested benefit outweighs the risk.
Although a systematic review of cohort studies has inherent limitations, the overwhelming direction of the results suggests statistically significant harm due to liberal transfusion practices (Summary Odd Ratios [OR] for a) death, OR = 1.69; b) infection, OR = 1.88; and c) Acute Respiratory Distress Syndrome, OR = 2.5). Due to the observational nature of the cohort studies, one might suspect RBC transfusions could simply reflect patient severity of illness. Thus, the harm suggested by the more liberal transfusion standards could just reflect the fact these patients carried a worse prognosis due to their respective illnesses.
Bottom Line: The preponderance of evidence suggests liberal transfusion practice is associated with increased morbidity and mortality of ICU patients. When considering RBC transfusions, the risks and benefits to each individual patient should be considered carefully.
Citation: Marik PE, Corwin HL. Efficacy of red blood cell transfusion in the critically ill: a systematic review of the literature. Crit Care Med. 2008; 36(9);2667-2674.
What is the appropriate frequency of rescreening for patients with initial screening colonoscopies negative for adenomas?
Background: Colonoscopy is the preferred primary screening method for the detection of colorectal cancer and precancerous polyps. Data suggest colonoscopy may be performed too frequently and for inappropriate indications.
Study design: Retrospective cohort study.
Setting: Seven sites in central Indiana.
Synopsis: In this study of 2,436 persons with no adenomas on baseline screening colonoscopies, 1,256 of them (51.6%) were rescreened a mean of 5.34 + 1.34 years later. No cancers were found on rescreening. One or more adenomas were found in 201 persons (16.0%). Nineteen advanced adenomas were found in 16 persons (1.3%). Patients in this study were relatively young (mean age at baseline was 56.7 years). Men were more likely than women to have adenomas (RR 1.88; 95% CI 1.42-2.51) and to have advanced adenomas (RR 3.31; 95% CI 1.02-10.8).
Limitations included a small cohort sample size, as well as incomplete information on persons who did not follow up with the five-year examination. Also, there is uncertainty about the clinical significance of advanced adenomas.
Bottom Line: Among persons previously screened with colonoscopy who have no colorectal adenomas, the five-year risk of detecting an advanced adenoma is extremely low (1.3%), supporting a rescreening interval of more than five years after a normal colonoscopy. Men have greater risk, and may deserve a shorter interval screening.
Citation: Imperiale TF, Glowinski EA, Lin-Cooper C, et al. Five-year risk of colorectal neoplasia after negative screening colonoscopy. N Engl J Med. 2008;359:1218-1224.
Can validated discharge instability criteria predict mortality or readmission within 30 days of hospital discharge for community acquired pneumonia (CAP)?
Background: Prior prospective cohort data have delineated instability criteria utilizing vital sign criteria at hospital discharge for CAP. However, guidelines for determining patient readiness for discharge remain largely unstudied.
Study design: Prospective, observational cohort study.
Setting: A single, non-urban teaching hospital in Spain.
Synopsis: In this study, 870 adults with CAP were evaluated following discharge. Abnormal oxygenation and vital signs were utilized to calculate an instability score. Criteria for instability were defined as temperature >37.5° C, heart rate <100, respiratory rate >24, systolic blood pressure (SBP) <90 (or diastolic blood pressure, DBP <60), and oxygen saturation <90% (or PaO2 <60).
Of all the instability criteria, only low oxygenation predicted readmission at 30 days (Hazard Ratio [HR] 1.4, p=0.03). However, mortality was significantly increased when instability criteria of temperature (HR 4.5, p=0.04), blood pressure (HR 2.6, p=0.02), respiratory rate (HR 2.4, p=0.03), or oxygenation (HR 2.4, p=0.03) were met. Elevated heart rate was not found to predict death.
The authors assigned each of the significant instability criteria a score of one or two (based on the weight of its hazard ratio), with respiratory rate, low blood pressure, and low oxygenation each assigned one point, and temperature assigned two points. Patients with an instability score of two or more had a six-fold increased risk of death (HR 5.8; 95%, p=0.0001). The negative predictive value (NPV) of an instability score less than two was very helpful (NPV=98%) in identifying patients with low mortality risk; however, the positive predictive value (PPV) of an instability score >2 is not necessarily helpful (PPV=13%) clinically.
Bottom line: Patients with a temperature >37.5° C or any combination of RR >24, SBP <90 (or DBP <60), and SpO2 <90% (or Pa02 <60) are at increased risk of death. Identifying a low instability score is most helpful in clinical practice.
Citation: Capelastegui A, Espana P, Bilbao A, et al. Pneumonia: criteria for patient instability on hospital discharge. Chest. 2008;34:595-600.
In This Edition
- Aspirin plus extended-release dipyridamole and clopidogrel provide similar outcomes in stroke.
- Traditional readings of bedside chest radiographs are insensitive in detecting intraatrial central venous catheter placement.
- Improved outcomes with bortezomib in myeloma treatment.
- ICD firings in cardiomyopathy patients are associated with worse outcomes.
- The clinical dehydration scale rapidly assesses the severity of dehydration in children.
- Liberal red blood cell transfusions may be harming patients.
- Five-year risk of colorectal neoplasia is low in patients with negative screening colonoscopy.
- Vital sign instability and oxygenation predict prognosis following hospitalization for community acquired pneumonia.
Is aspirin plus extended release dipyridamole more efficacious and safer than clopidogrel in preventing recurrent stroke?
Background: Recurrent stroke is a frequent (7% to 8% thrombotic stroke recurrence in first year) and disabling event after ischemic stroke. Multiple randomized trials demonstrate efficacy of anti-platelet agents for the prevention of recurrent stroke after non-cardioembolic stroke. However, direct comparisons and relative benefits of various antiplatelet agents are not well defined.
Study design: Randomized, double-blinded, two-by-two factorial design with intention-to-treat analysis.
Setting: A total of 20,333 patients from 695 centers in 35 countries, including the U.S.
Synopsis: This study directly compared aspirin plus extended-release dipyridamole to clopidogrel within the PRoFESS trial. A total of 20,333 patients were enrolled and followed up for a mean duration of 2.5 years. Eligible patients randomly were assigned to receive either 25 mg aspirin plus 200 mg extended-release twice a day, or clopidogrel 75 mg a day; and either telmisartan 80 mg once a day or placebo. Groups were similar at baseline.
The primary outcome of recurrent stroke was similar in both the aspirin plus extended-release dipyrimadole group and the clopidogrel group (9.0% vs. 8.8%). The composite secondary outcome of stroke, myocardial infarction or vascular death, and tertiary outcomes were similar in both groups. The trial showed statistical equivalence in the rates of recurrent stroke in the two groups.
Despite more frequent hemorrhagic strokes in the group receiving aspirin plus extended-release dipyridamole (4.1% vs. 3.6%), there was no significant difference in the risk of fatal or disabling stroke between both the groups.
Bottom line: Aspirin plus extended-release dipyridamole is equivalent to clopidogrel in the prevention of recurrent stroke, in terms of relevant efficacy and safety parameters.
Citation: Sacco RL, Diener H, Yusuf S, et.al. Aspirin and extended-release dipyridamole versus clopidogrel for recurrent stroke. N Engl J Med. 2008:359:1238-1251.
Is there a better method to judge the placement of central venous catheters?
Background: Placement of central venous catheters is common, particularly in critical care settings. Correct placement is usually confirmed by bedside chest radiography. The recommended location of the distal catheter tip is superior to the superior vena cava and right atria junction. However, determining this landmark on traditional bedside chest radiographs is frequently inaccurate.
Study design: Prospective, blinded study.
Setting: University hospital in Germany.
Synopsis: The researchers enrolled 212 patients scheduled for elective cardiac surgery. Either left or right internal jugular vein central lines were placed via EKG guidance, and more precisely evaluated by transesophageal echocardiography. Bedside chest radiographs were performed within three hours of admission to the ICU.
The radiologists were able to detect between 40% and 60% of incorrect central venous catheter placements when compared to transesophageal echocardiography. The researchers concluded TC-distance (tip of catheter to carina) of greater than 55 mm on chest X-ray performed better (98% accurate) in the detection of intra-atrial catheter placement, compared to conventional judgment by attending (93% accurate) or resident (53% accurate) radiologists. Limitations of the study include the use of only one attending radiologist. Secondly, the chest radiographs and echocardiograms were not done simultaneously, allowing for possible movement of the catheters between studies.
Bottom line: A TC distance of greater than 55 mm on chest X-ray should be further investigated as an accurate method to detect intra-atrial central venous catheters.
Citation: Wirsing M, Schummer C, Neumann R, et al. Is traditional reading of the bedside chest radiograph appropriate to detect intra-atrial central venous catheter position? Chest. 2008;134:527-533.
Does adding bortezomib to melphalan and prednisone improve outcomes in newly diagnosed myeloma?
Background: More than 50% of newly diagnosed myeloma patients are older than 65 and cannot receive optimal treatment with high-dose chemotherapy and stem-cell transplant. Previous trials have demonstrated patients with relapsed or refractory myeloma benefit from the administration of bortezomib, which sensitizes the myeloma cell lines to melphalan.
Study design: Randomized, open-label (unblinded) phase 3 study.
Setting: 151 centers, 22 countries in Asia, Europe, South and North America.
Synopsis: 682 patients with untreated multiple myeloma, who were ineligible for high-dose chemotherapy and stem cell transplant, were treated with bortezomib in combination with standard melphalan and prednisone, or melphalan and prednisone alone. The bortezomib group had improved partial or complete response (71% vs. 35%; NNT=3; p<0.001), increased median time to progression of disease (19.9 months vs. 13.1 months), and improved overall survival (87% vs. 78% over a 16-month median follow up; NNT=11; p=0.008). There were increased grade 3 adverse effects with the intervention, but no increase in grade 4 events or treatment related deaths compared to control. Limitations of the study include lack of blinding and involvement of the pharmaceutical company in data collection analysis, writing and editing of the manuscript.
Bottom line: Bortezomib is a valuable adjunct to standard treatment of multiple myeloma in patients over the age of 65 who may be ineligible for high-dose chemotherapy and stem cell transplant.
Citation: San Miguel JF, Schlag R, Khuageva NK, et al. Bortezomib plus melphalan and prednisone for the initial treatment of multiple myeloma. NEJM. 2008;359:906-917.
Does the occurrence of a shock increase the risk of death in cardiomyopathy patients with defibrillators?
Background: The SCD-HeFT trial, originally published in 2005, was instrumental in demonstrating the utility of defibrillators in the primary prevention of sudden cardiac deaths in patients with either ischemic or non-ischemic cardiomyopathy, NYHA class II or III, ejection fraction <35%, and no history of sustained ventricular tachycardia or fibrillation. This study re-examined the data derived from the SCD-HeFT trial to better understand the long-term prognosis of these patients with defibrillators who receive either appropriate shocks (ventricular fibrillation, sustained ventricular tachycardia), inappropriate shocks, or no shocks. Inappropriate shocks were defined as defibrillations due to supraventricular tachycardia, oversensing P or T waves as R waves, double counting of R waves, and artifact.
Study design: Retrospective cohort (analysis of patients randomized to implantable cardioverter-defibrillator (ICD) group in SCD-HeFT).
Setting: Multicenter trial.
Synopsis: The analysis demonstrated patients who received shocks were 11 times more likely to die compared with those who had no defibrillations (Hazard Ratio [HR]=11.3, p<0.001). These shocked patients were at more risk (HR=5.7, p<0.001) than those with inappropriate shocks (HR=2.0, p=0.002). Therefore, even inappropriate shocks themselves doubled the risk of death. Patients who received more than one shock, either appropriate or not, were at even higher odds of death (HR=8.3, p<0.001). The results highlight the higher mortality risk when patients with ICDs have received a shock (appropriate or inappropriate) and the need for further therapies to modify outcome in these patients.
Bottom Line: Appropriate or inappropriate defibrillations are associated with a poorer prognosis in patients with cardiomyopathy.
Citation: Poole JE, Johnson GW, Hellkamp AS, et al. Prognostic importance of defibrillator shocks in patients with heart failure. N Engl J Med. 2008(359):1009-1017.
Can a simple physical exam tool assess the degree of dehydration in children?
Background: Despite the frequency and the associated cost of acute gastroenteritis (AGE) in the pediatric population, there is no unified scale to assess the severity of dehydration. The authors of this paper previously reported a clinical dehydration scale (CDS) and applied it prospectively in a new cohort of patients ages 1 month to 5 years.
Study design: Prospective, observational study.
Setting: Single, tertiary care emergency department (ED) in Canada.
Synopsis: The CDS score is based purely on the physical findings of the child, including a) general appearance, b) eyes, c) mucous membranes, and d) amount of tears. On a point system, the patient is placed in one of three categories: no dehydration, some dehydration, moderate/severe dehydration. The trial enrolled 205 children and the CDS was applied by the triaging nurse. The attending ED pediatricians were blinded from this assessment. The CDS was able to predict the length of stay (mean + SD: no dehyrdation 245 + 181 mins; some dehydration, 397 + 302 mins; mod/severe dehydration, 501 + 389 mins), need for intravenous rehydration (none, 15%; some, 49%; mod/severe, 80%), and frequency of emesis/diarrhea as reported by the parents (none, 8.4 + 7.7; some, 13 + 10.7; mod/severe, 30.2 + 14.8). Only five children were categorized in the moderate/severe dehydration category, which may limit the ability to generalize the scoring system to that group of patients.
Bottom line: The CDS is an easy to use and promising tool to assess the severity of illness, expected ED length of stay, and need for intravenous rehydration in children with acute gastroenteritis.
Citation: Goldman RD, Friedman JN, Parkin PC. Validation of the clinical dehydration scale for children with acute gastroenteritis. Pediatrics. 2008;122(3):545-549.
Does maintaining a higher hemoglobin level benefit critical care patients?
Background: Historically, medical and surgical critical care patients liberally were transfused with little prospective evidence to support this approach. However, recent evidence has led to the use of a more-restricted transfusion threshold.
Study design: Systematic review and meta-analysis of cohort studies evaluating the effect of red blood cell (RBC) transfusion on patient outcomes.
Setting: Data sources include MEDLINE, Embase, and Cochrane databases.
Synopsis: The 45 cohort studies, including more than 272,000 patients, were selected due to focus on outcome measures, such as mortality, multiorgan dysfunction, acute respiratory distress syndrome, and infections. Primary studies were then placed into one of three categories: benefits outweigh the risk, neutral, or risks outweigh the benefit. Forty-two of these studies found the risks outweigh the benefits; two were neutral; and only one sub-study (in elderly patients with acute myocardial infarctions) suggested benefit outweighs the risk.
Although a systematic review of cohort studies has inherent limitations, the overwhelming direction of the results suggests statistically significant harm due to liberal transfusion practices (Summary Odd Ratios [OR] for a) death, OR = 1.69; b) infection, OR = 1.88; and c) Acute Respiratory Distress Syndrome, OR = 2.5). Due to the observational nature of the cohort studies, one might suspect RBC transfusions could simply reflect patient severity of illness. Thus, the harm suggested by the more liberal transfusion standards could just reflect the fact these patients carried a worse prognosis due to their respective illnesses.
Bottom Line: The preponderance of evidence suggests liberal transfusion practice is associated with increased morbidity and mortality of ICU patients. When considering RBC transfusions, the risks and benefits to each individual patient should be considered carefully.
Citation: Marik PE, Corwin HL. Efficacy of red blood cell transfusion in the critically ill: a systematic review of the literature. Crit Care Med. 2008; 36(9);2667-2674.
What is the appropriate frequency of rescreening for patients with initial screening colonoscopies negative for adenomas?
Background: Colonoscopy is the preferred primary screening method for the detection of colorectal cancer and precancerous polyps. Data suggest colonoscopy may be performed too frequently and for inappropriate indications.
Study design: Retrospective cohort study.
Setting: Seven sites in central Indiana.
Synopsis: In this study of 2,436 persons with no adenomas on baseline screening colonoscopies, 1,256 of them (51.6%) were rescreened a mean of 5.34 + 1.34 years later. No cancers were found on rescreening. One or more adenomas were found in 201 persons (16.0%). Nineteen advanced adenomas were found in 16 persons (1.3%). Patients in this study were relatively young (mean age at baseline was 56.7 years). Men were more likely than women to have adenomas (RR 1.88; 95% CI 1.42-2.51) and to have advanced adenomas (RR 3.31; 95% CI 1.02-10.8).
Limitations included a small cohort sample size, as well as incomplete information on persons who did not follow up with the five-year examination. Also, there is uncertainty about the clinical significance of advanced adenomas.
Bottom Line: Among persons previously screened with colonoscopy who have no colorectal adenomas, the five-year risk of detecting an advanced adenoma is extremely low (1.3%), supporting a rescreening interval of more than five years after a normal colonoscopy. Men have greater risk, and may deserve a shorter interval screening.
Citation: Imperiale TF, Glowinski EA, Lin-Cooper C, et al. Five-year risk of colorectal neoplasia after negative screening colonoscopy. N Engl J Med. 2008;359:1218-1224.
Can validated discharge instability criteria predict mortality or readmission within 30 days of hospital discharge for community acquired pneumonia (CAP)?
Background: Prior prospective cohort data have delineated instability criteria utilizing vital sign criteria at hospital discharge for CAP. However, guidelines for determining patient readiness for discharge remain largely unstudied.
Study design: Prospective, observational cohort study.
Setting: A single, non-urban teaching hospital in Spain.
Synopsis: In this study, 870 adults with CAP were evaluated following discharge. Abnormal oxygenation and vital signs were utilized to calculate an instability score. Criteria for instability were defined as temperature >37.5° C, heart rate <100, respiratory rate >24, systolic blood pressure (SBP) <90 (or diastolic blood pressure, DBP <60), and oxygen saturation <90% (or PaO2 <60).
Of all the instability criteria, only low oxygenation predicted readmission at 30 days (Hazard Ratio [HR] 1.4, p=0.03). However, mortality was significantly increased when instability criteria of temperature (HR 4.5, p=0.04), blood pressure (HR 2.6, p=0.02), respiratory rate (HR 2.4, p=0.03), or oxygenation (HR 2.4, p=0.03) were met. Elevated heart rate was not found to predict death.
The authors assigned each of the significant instability criteria a score of one or two (based on the weight of its hazard ratio), with respiratory rate, low blood pressure, and low oxygenation each assigned one point, and temperature assigned two points. Patients with an instability score of two or more had a six-fold increased risk of death (HR 5.8; 95%, p=0.0001). The negative predictive value (NPV) of an instability score less than two was very helpful (NPV=98%) in identifying patients with low mortality risk; however, the positive predictive value (PPV) of an instability score >2 is not necessarily helpful (PPV=13%) clinically.
Bottom line: Patients with a temperature >37.5° C or any combination of RR >24, SBP <90 (or DBP <60), and SpO2 <90% (or Pa02 <60) are at increased risk of death. Identifying a low instability score is most helpful in clinical practice.
Citation: Capelastegui A, Espana P, Bilbao A, et al. Pneumonia: criteria for patient instability on hospital discharge. Chest. 2008;34:595-600.
In This Edition
- Aspirin plus extended-release dipyridamole and clopidogrel provide similar outcomes in stroke.
- Traditional readings of bedside chest radiographs are insensitive in detecting intraatrial central venous catheter placement.
- Improved outcomes with bortezomib in myeloma treatment.
- ICD firings in cardiomyopathy patients are associated with worse outcomes.
- The clinical dehydration scale rapidly assesses the severity of dehydration in children.
- Liberal red blood cell transfusions may be harming patients.
- Five-year risk of colorectal neoplasia is low in patients with negative screening colonoscopy.
- Vital sign instability and oxygenation predict prognosis following hospitalization for community acquired pneumonia.
Is aspirin plus extended release dipyridamole more efficacious and safer than clopidogrel in preventing recurrent stroke?
Background: Recurrent stroke is a frequent (7% to 8% thrombotic stroke recurrence in first year) and disabling event after ischemic stroke. Multiple randomized trials demonstrate efficacy of anti-platelet agents for the prevention of recurrent stroke after non-cardioembolic stroke. However, direct comparisons and relative benefits of various antiplatelet agents are not well defined.
Study design: Randomized, double-blinded, two-by-two factorial design with intention-to-treat analysis.
Setting: A total of 20,333 patients from 695 centers in 35 countries, including the U.S.
Synopsis: This study directly compared aspirin plus extended-release dipyridamole to clopidogrel within the PRoFESS trial. A total of 20,333 patients were enrolled and followed up for a mean duration of 2.5 years. Eligible patients randomly were assigned to receive either 25 mg aspirin plus 200 mg extended-release twice a day, or clopidogrel 75 mg a day; and either telmisartan 80 mg once a day or placebo. Groups were similar at baseline.
The primary outcome of recurrent stroke was similar in both the aspirin plus extended-release dipyrimadole group and the clopidogrel group (9.0% vs. 8.8%). The composite secondary outcome of stroke, myocardial infarction or vascular death, and tertiary outcomes were similar in both groups. The trial showed statistical equivalence in the rates of recurrent stroke in the two groups.
Despite more frequent hemorrhagic strokes in the group receiving aspirin plus extended-release dipyridamole (4.1% vs. 3.6%), there was no significant difference in the risk of fatal or disabling stroke between both the groups.
Bottom line: Aspirin plus extended-release dipyridamole is equivalent to clopidogrel in the prevention of recurrent stroke, in terms of relevant efficacy and safety parameters.
Citation: Sacco RL, Diener H, Yusuf S, et.al. Aspirin and extended-release dipyridamole versus clopidogrel for recurrent stroke. N Engl J Med. 2008:359:1238-1251.
Is there a better method to judge the placement of central venous catheters?
Background: Placement of central venous catheters is common, particularly in critical care settings. Correct placement is usually confirmed by bedside chest radiography. The recommended location of the distal catheter tip is superior to the superior vena cava and right atria junction. However, determining this landmark on traditional bedside chest radiographs is frequently inaccurate.
Study design: Prospective, blinded study.
Setting: University hospital in Germany.
Synopsis: The researchers enrolled 212 patients scheduled for elective cardiac surgery. Either left or right internal jugular vein central lines were placed via EKG guidance, and more precisely evaluated by transesophageal echocardiography. Bedside chest radiographs were performed within three hours of admission to the ICU.
The radiologists were able to detect between 40% and 60% of incorrect central venous catheter placements when compared to transesophageal echocardiography. The researchers concluded TC-distance (tip of catheter to carina) of greater than 55 mm on chest X-ray performed better (98% accurate) in the detection of intra-atrial catheter placement, compared to conventional judgment by attending (93% accurate) or resident (53% accurate) radiologists. Limitations of the study include the use of only one attending radiologist. Secondly, the chest radiographs and echocardiograms were not done simultaneously, allowing for possible movement of the catheters between studies.
Bottom line: A TC distance of greater than 55 mm on chest X-ray should be further investigated as an accurate method to detect intra-atrial central venous catheters.
Citation: Wirsing M, Schummer C, Neumann R, et al. Is traditional reading of the bedside chest radiograph appropriate to detect intra-atrial central venous catheter position? Chest. 2008;134:527-533.
Does adding bortezomib to melphalan and prednisone improve outcomes in newly diagnosed myeloma?
Background: More than 50% of newly diagnosed myeloma patients are older than 65 and cannot receive optimal treatment with high-dose chemotherapy and stem-cell transplant. Previous trials have demonstrated patients with relapsed or refractory myeloma benefit from the administration of bortezomib, which sensitizes the myeloma cell lines to melphalan.
Study design: Randomized, open-label (unblinded) phase 3 study.
Setting: 151 centers, 22 countries in Asia, Europe, South and North America.
Synopsis: 682 patients with untreated multiple myeloma, who were ineligible for high-dose chemotherapy and stem cell transplant, were treated with bortezomib in combination with standard melphalan and prednisone, or melphalan and prednisone alone. The bortezomib group had improved partial or complete response (71% vs. 35%; NNT=3; p<0.001), increased median time to progression of disease (19.9 months vs. 13.1 months), and improved overall survival (87% vs. 78% over a 16-month median follow up; NNT=11; p=0.008). There were increased grade 3 adverse effects with the intervention, but no increase in grade 4 events or treatment related deaths compared to control. Limitations of the study include lack of blinding and involvement of the pharmaceutical company in data collection analysis, writing and editing of the manuscript.
Bottom line: Bortezomib is a valuable adjunct to standard treatment of multiple myeloma in patients over the age of 65 who may be ineligible for high-dose chemotherapy and stem cell transplant.
Citation: San Miguel JF, Schlag R, Khuageva NK, et al. Bortezomib plus melphalan and prednisone for the initial treatment of multiple myeloma. NEJM. 2008;359:906-917.
Does the occurrence of a shock increase the risk of death in cardiomyopathy patients with defibrillators?
Background: The SCD-HeFT trial, originally published in 2005, was instrumental in demonstrating the utility of defibrillators in the primary prevention of sudden cardiac deaths in patients with either ischemic or non-ischemic cardiomyopathy, NYHA class II or III, ejection fraction <35%, and no history of sustained ventricular tachycardia or fibrillation. This study re-examined the data derived from the SCD-HeFT trial to better understand the long-term prognosis of these patients with defibrillators who receive either appropriate shocks (ventricular fibrillation, sustained ventricular tachycardia), inappropriate shocks, or no shocks. Inappropriate shocks were defined as defibrillations due to supraventricular tachycardia, oversensing P or T waves as R waves, double counting of R waves, and artifact.
Study design: Retrospective cohort (analysis of patients randomized to implantable cardioverter-defibrillator (ICD) group in SCD-HeFT).
Setting: Multicenter trial.
Synopsis: The analysis demonstrated patients who received shocks were 11 times more likely to die compared with those who had no defibrillations (Hazard Ratio [HR]=11.3, p<0.001). These shocked patients were at more risk (HR=5.7, p<0.001) than those with inappropriate shocks (HR=2.0, p=0.002). Therefore, even inappropriate shocks themselves doubled the risk of death. Patients who received more than one shock, either appropriate or not, were at even higher odds of death (HR=8.3, p<0.001). The results highlight the higher mortality risk when patients with ICDs have received a shock (appropriate or inappropriate) and the need for further therapies to modify outcome in these patients.
Bottom Line: Appropriate or inappropriate defibrillations are associated with a poorer prognosis in patients with cardiomyopathy.
Citation: Poole JE, Johnson GW, Hellkamp AS, et al. Prognostic importance of defibrillator shocks in patients with heart failure. N Engl J Med. 2008(359):1009-1017.
Can a simple physical exam tool assess the degree of dehydration in children?
Background: Despite the frequency and the associated cost of acute gastroenteritis (AGE) in the pediatric population, there is no unified scale to assess the severity of dehydration. The authors of this paper previously reported a clinical dehydration scale (CDS) and applied it prospectively in a new cohort of patients ages 1 month to 5 years.
Study design: Prospective, observational study.
Setting: Single, tertiary care emergency department (ED) in Canada.
Synopsis: The CDS score is based purely on the physical findings of the child, including a) general appearance, b) eyes, c) mucous membranes, and d) amount of tears. On a point system, the patient is placed in one of three categories: no dehydration, some dehydration, moderate/severe dehydration. The trial enrolled 205 children and the CDS was applied by the triaging nurse. The attending ED pediatricians were blinded from this assessment. The CDS was able to predict the length of stay (mean + SD: no dehyrdation 245 + 181 mins; some dehydration, 397 + 302 mins; mod/severe dehydration, 501 + 389 mins), need for intravenous rehydration (none, 15%; some, 49%; mod/severe, 80%), and frequency of emesis/diarrhea as reported by the parents (none, 8.4 + 7.7; some, 13 + 10.7; mod/severe, 30.2 + 14.8). Only five children were categorized in the moderate/severe dehydration category, which may limit the ability to generalize the scoring system to that group of patients.
Bottom line: The CDS is an easy to use and promising tool to assess the severity of illness, expected ED length of stay, and need for intravenous rehydration in children with acute gastroenteritis.
Citation: Goldman RD, Friedman JN, Parkin PC. Validation of the clinical dehydration scale for children with acute gastroenteritis. Pediatrics. 2008;122(3):545-549.
Does maintaining a higher hemoglobin level benefit critical care patients?
Background: Historically, medical and surgical critical care patients liberally were transfused with little prospective evidence to support this approach. However, recent evidence has led to the use of a more-restricted transfusion threshold.
Study design: Systematic review and meta-analysis of cohort studies evaluating the effect of red blood cell (RBC) transfusion on patient outcomes.
Setting: Data sources include MEDLINE, Embase, and Cochrane databases.
Synopsis: The 45 cohort studies, including more than 272,000 patients, were selected due to focus on outcome measures, such as mortality, multiorgan dysfunction, acute respiratory distress syndrome, and infections. Primary studies were then placed into one of three categories: benefits outweigh the risk, neutral, or risks outweigh the benefit. Forty-two of these studies found the risks outweigh the benefits; two were neutral; and only one sub-study (in elderly patients with acute myocardial infarctions) suggested benefit outweighs the risk.
Although a systematic review of cohort studies has inherent limitations, the overwhelming direction of the results suggests statistically significant harm due to liberal transfusion practices (Summary Odd Ratios [OR] for a) death, OR = 1.69; b) infection, OR = 1.88; and c) Acute Respiratory Distress Syndrome, OR = 2.5). Due to the observational nature of the cohort studies, one might suspect RBC transfusions could simply reflect patient severity of illness. Thus, the harm suggested by the more liberal transfusion standards could just reflect the fact these patients carried a worse prognosis due to their respective illnesses.
Bottom Line: The preponderance of evidence suggests liberal transfusion practice is associated with increased morbidity and mortality of ICU patients. When considering RBC transfusions, the risks and benefits to each individual patient should be considered carefully.
Citation: Marik PE, Corwin HL. Efficacy of red blood cell transfusion in the critically ill: a systematic review of the literature. Crit Care Med. 2008; 36(9);2667-2674.
What is the appropriate frequency of rescreening for patients with initial screening colonoscopies negative for adenomas?
Background: Colonoscopy is the preferred primary screening method for the detection of colorectal cancer and precancerous polyps. Data suggest colonoscopy may be performed too frequently and for inappropriate indications.
Study design: Retrospective cohort study.
Setting: Seven sites in central Indiana.
Synopsis: In this study of 2,436 persons with no adenomas on baseline screening colonoscopies, 1,256 of them (51.6%) were rescreened a mean of 5.34 + 1.34 years later. No cancers were found on rescreening. One or more adenomas were found in 201 persons (16.0%). Nineteen advanced adenomas were found in 16 persons (1.3%). Patients in this study were relatively young (mean age at baseline was 56.7 years). Men were more likely than women to have adenomas (RR 1.88; 95% CI 1.42-2.51) and to have advanced adenomas (RR 3.31; 95% CI 1.02-10.8).
Limitations included a small cohort sample size, as well as incomplete information on persons who did not follow up with the five-year examination. Also, there is uncertainty about the clinical significance of advanced adenomas.
Bottom Line: Among persons previously screened with colonoscopy who have no colorectal adenomas, the five-year risk of detecting an advanced adenoma is extremely low (1.3%), supporting a rescreening interval of more than five years after a normal colonoscopy. Men have greater risk, and may deserve a shorter interval screening.
Citation: Imperiale TF, Glowinski EA, Lin-Cooper C, et al. Five-year risk of colorectal neoplasia after negative screening colonoscopy. N Engl J Med. 2008;359:1218-1224.
Can validated discharge instability criteria predict mortality or readmission within 30 days of hospital discharge for community acquired pneumonia (CAP)?
Background: Prior prospective cohort data have delineated instability criteria utilizing vital sign criteria at hospital discharge for CAP. However, guidelines for determining patient readiness for discharge remain largely unstudied.
Study design: Prospective, observational cohort study.
Setting: A single, non-urban teaching hospital in Spain.
Synopsis: In this study, 870 adults with CAP were evaluated following discharge. Abnormal oxygenation and vital signs were utilized to calculate an instability score. Criteria for instability were defined as temperature >37.5° C, heart rate <100, respiratory rate >24, systolic blood pressure (SBP) <90 (or diastolic blood pressure, DBP <60), and oxygen saturation <90% (or PaO2 <60).
Of all the instability criteria, only low oxygenation predicted readmission at 30 days (Hazard Ratio [HR] 1.4, p=0.03). However, mortality was significantly increased when instability criteria of temperature (HR 4.5, p=0.04), blood pressure (HR 2.6, p=0.02), respiratory rate (HR 2.4, p=0.03), or oxygenation (HR 2.4, p=0.03) were met. Elevated heart rate was not found to predict death.
The authors assigned each of the significant instability criteria a score of one or two (based on the weight of its hazard ratio), with respiratory rate, low blood pressure, and low oxygenation each assigned one point, and temperature assigned two points. Patients with an instability score of two or more had a six-fold increased risk of death (HR 5.8; 95%, p=0.0001). The negative predictive value (NPV) of an instability score less than two was very helpful (NPV=98%) in identifying patients with low mortality risk; however, the positive predictive value (PPV) of an instability score >2 is not necessarily helpful (PPV=13%) clinically.
Bottom line: Patients with a temperature >37.5° C or any combination of RR >24, SBP <90 (or DBP <60), and SpO2 <90% (or Pa02 <60) are at increased risk of death. Identifying a low instability score is most helpful in clinical practice.
Citation: Capelastegui A, Espana P, Bilbao A, et al. Pneumonia: criteria for patient instability on hospital discharge. Chest. 2008;34:595-600.
Inhaled Insulin: Troubled Drug Rises from the Ashes
Remember all the hype leading up to the approval of the dry-powder formulation of human insulin, produced by means of recombinant DNA technology, a.k.a. inhaled insulin (Exubera)? That was three years ago (January 2006). Remember all the press releases regarding the removal of inhaled insulin from the market? That was October 2007.1,2
Almost immediately after Pfizer “pulled the plug” on inhaled insulin, cases of lung cancer started being reported—albeit it had occurred in Exubera-treated patients that had a history of smoking cigarettes—a contraindication within the drug’s approved label. Some clinicians questioned whether it was due to insulin being a weak growth factor when binding to the type 1 insulin-like growth factor receptor; others wondered if it was related to smoking history.3,4 Three other collaboration efforts for inhaled insulin—NovoNordisk/Aradigm, MannKind, and Alkermes/Eli Lilly AIR insulin— were in the pipeline when Pfizer bowed out of the market. MannKind’s Technosphere insulin and Alkermes/Eli Lilly AIR insulin are still being investigated. Both are in phase 3 clinical trials.5
So, contrary to popular belief, inhaled insulin is not dead, yet. These other companies are looking to improve upon what Pfizer lost out on. The AIR system uses a smaller, breathable inhaler, which would fit into a patient’s hand. The inhaled powder has a smaller particle size and a larger surface area, which provides deeper lung penetration of drug.6
More Drugs Via the Pulmonary Route
Aside from asthma, chronic obstructive pulmonary disease, pulmonary hypertension, and cystic fibrosis, where a hospitalist could expect to use pulmonary delivered drugs, other medicines are being investigated for administration via this route. The pulmonary route may be used for tuberculosis (TB), where lower doses can be given since high doses of systemic therapy lead to significant drug toxicity.7
Inhaled vaccines are being developed, including Bacillus Calmette-Guérin (BCG) TB and respiratory syncytial virus (RSV). Parathyroid hormone for osteoporosis, human factor IX for hemophilia, and interferon α-2b for hepatitis B virus, are potential and current inhaled treatments.
New Delivery Systems: Will They Pan Out?
Knowing the lung absorbs biologic drugs with a wide range of molecular weights, solubility, and charges, is a plus for pulmonary delivery. However, pulmonary drug delivery also presents challenges. These include local toxic effects, such as cell injury, edema, and altered tissue defenses. Drug carriers, preservatives, and propellants, such as sulfites, might harm pulmonary tissue or the body.
Safety is one of the biggest concerns when companies develop new drug delivery systems. These inhaled products and methods of delivering inhaled insulin are quickly moving through clinical trials.
Only time will tell when approvals will take place, but it looks as though there will be some innovative insulin products in the near future. TH
Michele B Kaufman, PharmD, BSc, RPh, is a freelance medical writer based in New York City.
References
1. Alvey L. U.S. Food and Drug Administration. FDA ap-proves first ever inhaled insulin combination product for treatment of diabetes. www.fda.gov/bbs/topics/ news/2006/NEW01304.html. Published Jan. 27, 2006. Accessed Dec. 1, 2008.
2. U.S. Food and Drug Administration. Drug discontinuations. www.fda.gov/cder/drug/shortages/#disc. Published Oct. 19, 2007. Accessed Dec. 1, 2008.
3. von Kriegstein E, von Kriegstein K. Inhaled insulin for diabetes. N Engl J Med. 2007;356:2106-2108.
4. McMahon GT, Arky RA. Inhaled insulin for diabetes. N Engl J Med. 2007;356:497-502.
5. Opar A. Another blow for inhaled protein therapeutics. Nat Rev Drug Discov. 2008;7:189-190.
6. Dubin CH. The state of systemic pulmonary delivery: one year after Exubera’s approval. Nat Rev Drug Discov. 2007;7(4):61-67.
7. Greb E. Inhalable drugs in the launch pad: will they take off? Pharm Tech. 2008;4:48-55.
8. Riley K, Long P. FDA approves treatment for rare neurologic disease. www.fda.gov/bbs/topics/ NEWS/2008/NEW01884.html. Published Sept. 12, 2008. Accessed Dec. 1, 2008.
9. Keppra XR approved in the U.S. hugin.info/133973/ R/1251192/271964.pdf. Published Sept. 15, 2008. Accessed Sept. 15, 2008.
10. U.S. Food and Drug Administration. 2008 safety alerts for human medical products (drugs, biologics, medical devices, special nutritionals, and cosmetics). www.fda.gov/medwatch/safety/2008/rituxan_DHCP_Final%209411700.pdf Published Sept. 2008. Accessed Sept. 15, 2008.
11. U.S. Food and Drug Administration. Pregnacy and lactation labeling. www.fda.gov/cder/regulatory/ pregnancy_labeling/default.htm Published June 11, 2008. Accessed Sept. 15, 2008.
12. Cruzan S. U.S. Food and Drug Administration. FDA proposes new rule to provide updated information on the use of prescription drugs and biological products during pregnancy and breast-feeding. www. fda.gov/bbs/topics/NEWS/2008/NEW018 41.html. Published May 28, 2008. Accessed Sept. 15, 2008.
13. Peggy P. FDA to take A, B, and C out of pregnancy labeling. www.medpagetoday.com/OBGYN/Pregnancy/ tb/9626. Published May 28, 2008. Accessed Sept. 15, 2008.
Remember all the hype leading up to the approval of the dry-powder formulation of human insulin, produced by means of recombinant DNA technology, a.k.a. inhaled insulin (Exubera)? That was three years ago (January 2006). Remember all the press releases regarding the removal of inhaled insulin from the market? That was October 2007.1,2
Almost immediately after Pfizer “pulled the plug” on inhaled insulin, cases of lung cancer started being reported—albeit it had occurred in Exubera-treated patients that had a history of smoking cigarettes—a contraindication within the drug’s approved label. Some clinicians questioned whether it was due to insulin being a weak growth factor when binding to the type 1 insulin-like growth factor receptor; others wondered if it was related to smoking history.3,4 Three other collaboration efforts for inhaled insulin—NovoNordisk/Aradigm, MannKind, and Alkermes/Eli Lilly AIR insulin— were in the pipeline when Pfizer bowed out of the market. MannKind’s Technosphere insulin and Alkermes/Eli Lilly AIR insulin are still being investigated. Both are in phase 3 clinical trials.5
So, contrary to popular belief, inhaled insulin is not dead, yet. These other companies are looking to improve upon what Pfizer lost out on. The AIR system uses a smaller, breathable inhaler, which would fit into a patient’s hand. The inhaled powder has a smaller particle size and a larger surface area, which provides deeper lung penetration of drug.6
More Drugs Via the Pulmonary Route
Aside from asthma, chronic obstructive pulmonary disease, pulmonary hypertension, and cystic fibrosis, where a hospitalist could expect to use pulmonary delivered drugs, other medicines are being investigated for administration via this route. The pulmonary route may be used for tuberculosis (TB), where lower doses can be given since high doses of systemic therapy lead to significant drug toxicity.7
Inhaled vaccines are being developed, including Bacillus Calmette-Guérin (BCG) TB and respiratory syncytial virus (RSV). Parathyroid hormone for osteoporosis, human factor IX for hemophilia, and interferon α-2b for hepatitis B virus, are potential and current inhaled treatments.
New Delivery Systems: Will They Pan Out?
Knowing the lung absorbs biologic drugs with a wide range of molecular weights, solubility, and charges, is a plus for pulmonary delivery. However, pulmonary drug delivery also presents challenges. These include local toxic effects, such as cell injury, edema, and altered tissue defenses. Drug carriers, preservatives, and propellants, such as sulfites, might harm pulmonary tissue or the body.
Safety is one of the biggest concerns when companies develop new drug delivery systems. These inhaled products and methods of delivering inhaled insulin are quickly moving through clinical trials.
Only time will tell when approvals will take place, but it looks as though there will be some innovative insulin products in the near future. TH
Michele B Kaufman, PharmD, BSc, RPh, is a freelance medical writer based in New York City.
References
1. Alvey L. U.S. Food and Drug Administration. FDA ap-proves first ever inhaled insulin combination product for treatment of diabetes. www.fda.gov/bbs/topics/ news/2006/NEW01304.html. Published Jan. 27, 2006. Accessed Dec. 1, 2008.
2. U.S. Food and Drug Administration. Drug discontinuations. www.fda.gov/cder/drug/shortages/#disc. Published Oct. 19, 2007. Accessed Dec. 1, 2008.
3. von Kriegstein E, von Kriegstein K. Inhaled insulin for diabetes. N Engl J Med. 2007;356:2106-2108.
4. McMahon GT, Arky RA. Inhaled insulin for diabetes. N Engl J Med. 2007;356:497-502.
5. Opar A. Another blow for inhaled protein therapeutics. Nat Rev Drug Discov. 2008;7:189-190.
6. Dubin CH. The state of systemic pulmonary delivery: one year after Exubera’s approval. Nat Rev Drug Discov. 2007;7(4):61-67.
7. Greb E. Inhalable drugs in the launch pad: will they take off? Pharm Tech. 2008;4:48-55.
8. Riley K, Long P. FDA approves treatment for rare neurologic disease. www.fda.gov/bbs/topics/ NEWS/2008/NEW01884.html. Published Sept. 12, 2008. Accessed Dec. 1, 2008.
9. Keppra XR approved in the U.S. hugin.info/133973/ R/1251192/271964.pdf. Published Sept. 15, 2008. Accessed Sept. 15, 2008.
10. U.S. Food and Drug Administration. 2008 safety alerts for human medical products (drugs, biologics, medical devices, special nutritionals, and cosmetics). www.fda.gov/medwatch/safety/2008/rituxan_DHCP_Final%209411700.pdf Published Sept. 2008. Accessed Sept. 15, 2008.
11. U.S. Food and Drug Administration. Pregnacy and lactation labeling. www.fda.gov/cder/regulatory/ pregnancy_labeling/default.htm Published June 11, 2008. Accessed Sept. 15, 2008.
12. Cruzan S. U.S. Food and Drug Administration. FDA proposes new rule to provide updated information on the use of prescription drugs and biological products during pregnancy and breast-feeding. www. fda.gov/bbs/topics/NEWS/2008/NEW018 41.html. Published May 28, 2008. Accessed Sept. 15, 2008.
13. Peggy P. FDA to take A, B, and C out of pregnancy labeling. www.medpagetoday.com/OBGYN/Pregnancy/ tb/9626. Published May 28, 2008. Accessed Sept. 15, 2008.
Remember all the hype leading up to the approval of the dry-powder formulation of human insulin, produced by means of recombinant DNA technology, a.k.a. inhaled insulin (Exubera)? That was three years ago (January 2006). Remember all the press releases regarding the removal of inhaled insulin from the market? That was October 2007.1,2
Almost immediately after Pfizer “pulled the plug” on inhaled insulin, cases of lung cancer started being reported—albeit it had occurred in Exubera-treated patients that had a history of smoking cigarettes—a contraindication within the drug’s approved label. Some clinicians questioned whether it was due to insulin being a weak growth factor when binding to the type 1 insulin-like growth factor receptor; others wondered if it was related to smoking history.3,4 Three other collaboration efforts for inhaled insulin—NovoNordisk/Aradigm, MannKind, and Alkermes/Eli Lilly AIR insulin— were in the pipeline when Pfizer bowed out of the market. MannKind’s Technosphere insulin and Alkermes/Eli Lilly AIR insulin are still being investigated. Both are in phase 3 clinical trials.5
So, contrary to popular belief, inhaled insulin is not dead, yet. These other companies are looking to improve upon what Pfizer lost out on. The AIR system uses a smaller, breathable inhaler, which would fit into a patient’s hand. The inhaled powder has a smaller particle size and a larger surface area, which provides deeper lung penetration of drug.6
More Drugs Via the Pulmonary Route
Aside from asthma, chronic obstructive pulmonary disease, pulmonary hypertension, and cystic fibrosis, where a hospitalist could expect to use pulmonary delivered drugs, other medicines are being investigated for administration via this route. The pulmonary route may be used for tuberculosis (TB), where lower doses can be given since high doses of systemic therapy lead to significant drug toxicity.7
Inhaled vaccines are being developed, including Bacillus Calmette-Guérin (BCG) TB and respiratory syncytial virus (RSV). Parathyroid hormone for osteoporosis, human factor IX for hemophilia, and interferon α-2b for hepatitis B virus, are potential and current inhaled treatments.
New Delivery Systems: Will They Pan Out?
Knowing the lung absorbs biologic drugs with a wide range of molecular weights, solubility, and charges, is a plus for pulmonary delivery. However, pulmonary drug delivery also presents challenges. These include local toxic effects, such as cell injury, edema, and altered tissue defenses. Drug carriers, preservatives, and propellants, such as sulfites, might harm pulmonary tissue or the body.
Safety is one of the biggest concerns when companies develop new drug delivery systems. These inhaled products and methods of delivering inhaled insulin are quickly moving through clinical trials.
Only time will tell when approvals will take place, but it looks as though there will be some innovative insulin products in the near future. TH
Michele B Kaufman, PharmD, BSc, RPh, is a freelance medical writer based in New York City.
References
1. Alvey L. U.S. Food and Drug Administration. FDA ap-proves first ever inhaled insulin combination product for treatment of diabetes. www.fda.gov/bbs/topics/ news/2006/NEW01304.html. Published Jan. 27, 2006. Accessed Dec. 1, 2008.
2. U.S. Food and Drug Administration. Drug discontinuations. www.fda.gov/cder/drug/shortages/#disc. Published Oct. 19, 2007. Accessed Dec. 1, 2008.
3. von Kriegstein E, von Kriegstein K. Inhaled insulin for diabetes. N Engl J Med. 2007;356:2106-2108.
4. McMahon GT, Arky RA. Inhaled insulin for diabetes. N Engl J Med. 2007;356:497-502.
5. Opar A. Another blow for inhaled protein therapeutics. Nat Rev Drug Discov. 2008;7:189-190.
6. Dubin CH. The state of systemic pulmonary delivery: one year after Exubera’s approval. Nat Rev Drug Discov. 2007;7(4):61-67.
7. Greb E. Inhalable drugs in the launch pad: will they take off? Pharm Tech. 2008;4:48-55.
8. Riley K, Long P. FDA approves treatment for rare neurologic disease. www.fda.gov/bbs/topics/ NEWS/2008/NEW01884.html. Published Sept. 12, 2008. Accessed Dec. 1, 2008.
9. Keppra XR approved in the U.S. hugin.info/133973/ R/1251192/271964.pdf. Published Sept. 15, 2008. Accessed Sept. 15, 2008.
10. U.S. Food and Drug Administration. 2008 safety alerts for human medical products (drugs, biologics, medical devices, special nutritionals, and cosmetics). www.fda.gov/medwatch/safety/2008/rituxan_DHCP_Final%209411700.pdf Published Sept. 2008. Accessed Sept. 15, 2008.
11. U.S. Food and Drug Administration. Pregnacy and lactation labeling. www.fda.gov/cder/regulatory/ pregnancy_labeling/default.htm Published June 11, 2008. Accessed Sept. 15, 2008.
12. Cruzan S. U.S. Food and Drug Administration. FDA proposes new rule to provide updated information on the use of prescription drugs and biological products during pregnancy and breast-feeding. www. fda.gov/bbs/topics/NEWS/2008/NEW018 41.html. Published May 28, 2008. Accessed Sept. 15, 2008.
13. Peggy P. FDA to take A, B, and C out of pregnancy labeling. www.medpagetoday.com/OBGYN/Pregnancy/ tb/9626. Published May 28, 2008. Accessed Sept. 15, 2008.
The latest research you need to know
Literature at a Glance
- Tight glucose control in critically ill patients is not associated with reduction in short-term mortality, but it is associated with an increased risk of hypoglycemia.
- Intensive glucose-lowering therapy in diabetic patients at high risk for cardiovascular events increased mortality.
- Targeting normal glycated hemoglobin levels with a gliclazide-based regimen does not have an effect on preventing major macrovascular events.
- Non-invasive ventilation has no effect on short-term mortality or rates of tracheal intubation and admission to ICU
- Routine use of a rhythm-control strategy does not reduce the rate of death from cardiovascular causes.
- No clinical benefit exists in employing intensive renal replacement over a conventional approach in critically ill patients.
- Initial UFH bolus and infusion dosing used for NSTE ACS often exceeds recommended weight-adjusted dosing.
- High BNP or NT-pro-BNP levels can differentiate patients who are at a higher risk of complicated hospital course and short-term mortality.
- Use of a silver-coated ET tube reduces the incidence of VAP, as well as delays time to VAP occurrence.
Tight Glucose Control in the Intensive Care Unit (ICU) Setting Does Not Reduce Short-Term Mortality
Clinical question: Does tight glucose control for critically ill patients affect mortality?
Background: Intensive glucose control for adult ICU patients has been advocated by numerous professional societies and adopted worldwide as a means to reduce mortality of critically ill patients. Evidence from multiple randomized controlled trials of tight glucose control in the ICU setting, however, shows mixed results.
Study Design: Meta-analysis of randomized controlled trials.
Setting: 29 studies involving 8,432 critically ill patients.
Synopsis: This study evaluated 29 trials involving critically ill adult patients randomized to tight glucose control versus usual care. Comparing these patients, there was no significant difference in short-term mortality (<30 days). Stratification of trials by level of glucose control (very tight <110 mg/dL versus moderately tight <150 mg/dL) and by ICU setting (surgical, medical, or mixed medical-surgical) did not affect mortality.
Tight glucose control was associated with a reduced risk of septicemia, but only in surgical patients. There was no association between tight control and a new need for dialysis, consistent across all ICU settings, as well as with both levels of glucose control. Finally, there was an increased risk of hypoglycemia (<40 mg/dL) with tight control, higher in patients who received very tight control versus those who received moderately tight control.
Limitations of the studies evaluated in this meta-analysis include difficulties with consistently maintaining tight glucose control. Twenty one percent of the trials did not achieve a mean glucose level within 5 mg/dL of the goal. This, along with a lack of standardization in reporting glucose control, makes study comparison problematic.
Bottom Line: Tight glucose control in critically ill patients is not associated with reduction in short-term mortality, but it is associated with an increased risk of hypoglycemia.
Citation: Wiener, RS, Wiener DC, Larson, RJ. Benefits and risks of tight glucose control in critically ill adults: a meta-analysis. JAMA. 2008;300:933-944.
Intensive Glucose-Lowering Therapy Increases Mortality in High-Risk Diabetic Patients
Clinical Question: Does intensive glucose-lowering therapy reduce cardiac events in high-risk diabetic patients?
Background: Epidemiologic studies have suggested the risk of cardiovascular disease increases with higher levels of glycated hemoglobin in patients with type-2 diabetes. No definitive data from randomized trials exist to test the effect of intensive glucose-lowering therapy on the rate of cardiovascular events in high-risk diabetic patients.
Study Design: Multicenter randomized controlled trial led by the Action to Control Cardiovascular Risk in Diabetes (ACCORD) Study Group.
Setting: 77 clinical centers in the U.S. and Canada.
Synopsis: 10,251 diabetic patients with established cardiovascular disease or additional cardiovascular risk factors, and median glycated hemoglobin level of 8.1%, received either intensive therapy (targeting glycated hemoglobin level <6.0%) or standard therapy (targeting level from 7.0% to 7.9%). The primary outcome was a composite of non-fatal myocardial infarction, nonfatal stroke, or death from cardiovascular causes.
Data indicated intensive therapy did decrease the rate of non-fatal myocardial infarctions, however, it did not significantly reduce the primary composite of major cardiovascular events. Moreover, intensive therapy resulted in a significant increase in death from cardiovascular causes, as well as a relative increase of 22% of death from any cause, during follow up of three and a half years. Due to this finding, the intensive therapy regimen was discontinued 17 months before the scheduled end of the study.
Analysis of the data has not identified a cause for the unexpected increased mortality in the intensive therapy group, and has not shown any medication or combination of medications to be responsible.
Bottom Line: Intensive glucose-lowering therapy in diabetic patients at high risk for cardiovascular events increased mortality and did not significantly reduce major cardiovascular events.
Citation: Action to control cardiovascular risk in diabetes study group. Effects of intensive glucose lowering in type-2 diabetes. N Engl J Med. 2008;358:2545-2559.
Intensive Glucose Control Reduces Nephropathy but Has No Effect on Major Cardiovascular Events
Clinical Question: Does intensive glucose-lowering therapy decrease major macrovascular and microvascular events in high-risk diabetic patients?
Background: Prospective studies show a direct association between elevated glycated hemoglobin levels in diabetics and increased risk of vascular events. However, definitive evidence from randomized trials about the role of intensive glucose control in preventing vascular disease in diabetics is lacking.
Study Design: Multicenter randomized controlled trial led by the ADVANCE Collaborative Group.
Setting: 215 clinical centers in 20 countries from Asia, Australia, Europe, and North America.
Synopsis: 11,140 diabetic patients received either standard glucose therapy or intensive glucose therapy using gliclazide, as well as other drugs, to reach a targeted glycated hemoglobin of 6.5% or less. The primary outcome was a composite of major macrovascular and microvascular events, including nonfatal myocardial infarction (MI), nonfatal stroke, death from cardiovascular causes, nephropathy, and retinopathy.
Intensive glucose-lowering therapy, as compared to standard therapy, resulted in a 21% relative reduction of new or worsening nephropathy. There was no significant effect on the rate of MI, strokes, death from cardiovascular causes, or retinopathy. Furthermore, intensive glucose control was associated with an increased risk of severe hypoglycemia and increased rate of hospitalization. In contrast to the ACCORD study, intensive therapy did not result in an increase in mortality.
Bottom Line: While targeting normal glycated hemoglobin levels with a gliclazide-based regimen reduced the rate of nephropathy, this strategy did not have an effect on preventing major macrovascular events.
Citation: ADVANCE collaborative group. Intensive blood glucose control and vascular outcomes in patients with type-2 diabetes. N Eng J Med. 2008;358:2560-2572.
Non-invasive Ventilation Does Not Improve Short-Term Mortality in Patients with Acute Cardiogenic Pulmonary Edema
Clinical Question: Does non-invasive ventilation improve survival for patients with acute cardiogenic pulmonary edema?
Background: Acute cardiogenic pulmonary edema is a common medical emergency, but only small trials address outcomes of non-invasive methods of ventilation.
Study Design: A prospective, randomized control study.
Setting: 26 emergency rooms and hospitals in the United Kingdom.
Synopsis: 1,069 patients with a clinical diagnosis of acute cardiogenic pulmonary edema in the emergency room were randomized to one of three treatment strategies: standard oxygen therapy, continuous positive airway pressure (CPAP), or non-invasive intermittent positive pressure ventilation (NIPPV).
There was no significant difference in the seven-day mortality between patients receiving standard oxygen therapy (9.8%) and those treated with non-invasive ventilation (9.5%). Additionally, there was no significant difference in the combined end point of death or intubation within seven days between patients receiving CPAP and NIPPV—the primary end points of the study.
While non-invasive ventilation was associated with greater reductions in dyspnea, heart rate, acidosis, and hypercapnia than was standard oxygen therapy, rates of other secondary outcomes—including tracheal intubation, admission to the critical care unit, myocardial infarction, and 30-day mortality—were similar.
Bottom Line: Although non-invasive ventilation rapidly improves respiratory distress and metabolic disturbances for patients with acute cardiogenic pulmonary edema, it has no effect on short-term mortality or rates of tracheal intubation and admission to ICU.
Citation: Gray A, Goodacre S, Newby D, et al. Non-invasive ventilation in acute cardiogenic pulmonary edema. N Eng J Med. 2008;359:142-151.
Rhythm Control in Patients with Atrial Fibrillation and CHF Does Not Improve Mortality
Clinical Question: Does the restoration of sinus rhythm in patients with atrial fibrillation and heart failure reduce mortality from cardiovascular causes?
Background: Recent data show rhythm control provides no benefit over rate control among patients with atrial fibrillation, but limited information is available regarding its applicability to patients with heart failure.
Study Design: Multicenter, prospective, double-blind, randomized trial.
Settings: 123 medical centers worldwide.
Synopsis:1,376 patients with a left ventricular ejection fraction of 35% or less, symptoms of heart failure, and a history of atrial fibrillation were randomized (allocation not concealed) either to a rhythm-control (e.g., conversion to sinus rhythm) or rate-control strategy. The primary outcome measured was the time to death from cardiovascular causes. Secondary outcomes included death from any cause, stroke, worsening heart failure, hospitalization, quality of life, cost of therapy, and a composite of death from cardiovascular causes, stroke or worsening heart failure.
Study follow up succeeded with 94% of enrolled patients completing follow up (median=47 months for survivors) or dying. Amiodarone was the drug used most often in the rhythm-control group. Ninety percent of patients received angiotensin converting enzyme inhibitors or angiotensin II receptor blocker, and 90% received anticoagulation.
Among patients with atrial fibrillation and congestive heart failure, the number of deaths from cardiovascular causes was similar in the rate (25%) and rhythm-control group (27%). Furthermore, there were no significant differences in important secondary outcomes, including death from any cause, worsening heart failure, or stroke.
Bottom Line: For patients with heart failure from systolic dysfunction and atrial fibrillation, the routine use of a rhythm-control strategy does not reduce the rate of death from cardiovascular causes as compared with a rate-control strategy.
Citation: Roy D, Talajic M, Nattel S, et al. Rhythm control versus rate control for atrial fibrillation and heart failure. N Engl J Med. 2008;358:2667-2677.
No Benefit from Intensive Renal Replacement Therapy in Critically Ill Patients with Acute Kidney Injury (AKI)
Clinical Question: Does intensive renal replacement therapy, as compared with a conventional treatment strategy, affect outcomes in critically ill patients?
Background: The optimal timing for the initiation, method, and dosing of renal replacement therapy among patients with AKI remains uncertain. Previous single-center studies limited to single methods of renal replacement therapy have suggested more intensive therapy is associated with improved survival. These results, however, have been inconsistent.
Study Design: Randomized controlled trial.
Setting: Veterans Affairs hospitals and university affiliated medical centers.
Synopsis: This study randomized 1,124 of 4,340 eligible critically ill adults with AKI to receive either intensive renal replacement therapy or a less intensive, more conventional approach. The primary end point of death at day 60 from any cause was 53.6% with intensive therapy and 51.5 % with less intensive therapy (odds ratio, 1.09; 95% CI 0.86 to 1.40; p=0.47). No significant differences were found in secondary end points, including rate of recovery of kidney function, duration of renal-replacement therapy, or evolution of non-renal organ failure.
This study demonstrates providing hemodialysis more frequently than three times per week to hemodynamically stable patients, or providing continuous renal replacement therapy at an effluent flow rate of more than 20 ml/kg/hour to hemodynamically unstable patients, does not improve outcomes. It should be noted, however, the less-intensive treatment strategy in this study provides a dose of renal replacement therapy exceeding the normal dose given in usual care.
Bottom Line: No clinical benefit exists in employing intensive renal replacement over a conventional approach in critically ill patients.
Citation: Palevsky PM, Zhang JH, O’Connor TZ, et al. Intensity of renal support in critically ill patients with acute kidney injury. N Engl J Med. 2008;359(1):7-20.
Elderly Patients and Females with Acute Coronary Syndrome (ACS) Often Receive Excess Doses of Heparin
Clinical Question: What initial dosing of unfractionated heparin (UFH) for patients with non-ST-segment elevation (NSTE) acute coronary syndrome is most frequently used and how does it affect risk of bleeding?
Background: UFH is commonly used in clinical practice for NSTE ACS, but a wide variability continues to exist in dosing protocols. Clinical studies have shown UFH dosing based on weight provides more effective early anticoagulation. However, the relationship between increasing weight-adjusted doses of UFH and the risk of bleeding has not been well described.
Study Design: Retrospective cohort study.
Setting: 420 U.S. hospitals involved in the CRUSADE (Can Rapid Risk Stratification of Unstable Angina Patients Suppress Adverse Outcomes with Early Implementation) initiative.
Synopsis: This study used data from patients enrolled in the CRUSADE initiative to investigate UFH dosing amongst 24,021 patients presenting with NSTE ACS. The study showed despite a recommendation to use weight-adjusted UFH dosing for NSTE ACS, there is a continued preference for a fixed dosing regimen of 5,000 U bolus and 1,000 U/hr initial infusion.
This fixed dose means women and the elderly are more likely to receive an excess UFH dose due to their lower body weight. The study found 35% of the group received excess weight-adjusted doses of UFH.
A clear relationship is present between excess weight-adjusted UFH doses and major bleeding, with the risk of major bleeding increasing particularly when UFH dose exceeds the recommended dosing of 70 U/kg bolus and 15 U/kg per hour infusion.
These observations support the need to follow guidelines on weight-adjusted UFH dosing in order to minimize the risk of bleeding in patients with NSTE ACS.
Bottom line: The initial UFH bolus and infusion dosing used for NSTE ACS often exceeds recommended weight-adjusted dosing, leading to higher rates of bleeding, particularly among women and the elderly.
Citation: Melloni C, Alexander KP, Chen AY et al. Unfractionated heparin dosing and risk of major bleeding in non-ST-segment elevation acute coronary syndromes. Am Heart J. 2008;156(2):209-215.
Elevated BNP Level Is a Marker for Higher Risk of Adverse Outcomes in Patients with Pulmonary Embolism
Clinical Question: Can elevated BNP levels predict adverse outcomes in patients with acute pulmonary embolism (PE)?
Background: Plasma brain natriuretic peptide (BNP) and N-terminal proBNP (NT-proBNP) often are elevated in patients with PE and right ventricular (RV) dysfunction. The finding of RV dysfunction on echocardiography is an indicator of poor outcome in these patients. The role of BNP levels to differentiate patients with PE who are at higher risk of adverse events and poor clinical outcomes has not been determined.
Study Design: Meta analysis of prospective studies.
Settings: 13 studies involving 1,132 patients.
Synopsis: Elevated levels of BNP or NT-pro-BNP were noted in 51% of patients with acute PE. These patients had a higher rate of complicated inpatient course, as well as a higher risk of 30-day mortality (odds ratio 6.8; 95% CI 4.4-10; odds-ratio 7.6; 95% CI 3.4-17). Additionally, increased BNP levels were significantly associated with RV dysfunction (p<0.0001).
While elevated BNP levels may serve as a marker for increased risk of adverse outcomes, the investigators stress these levels alone should not be used to pursue more aggressive treatment strategies. Elevation of these markers is nonspecific and can be secondary to pre-existing heart, lung, or kidney disease, or older age. Further studies are needed to determine the role of BNP in risk stratifying patients with acute PE to different forms of therapy.
Bottom Line: High BNP or NT-pro-BNP levels can differentiate patients with PE who are at a higher risk of complicated hospital course and short-term mortality.
Citation: Klok FA, Mos IC, Huisman MV. Brain-type natriuretic peptide levels in the prediction of adverse outcome in patients with pulmonary embolism: a systematic review and meta-analysis. Am J Respir Crit Care Med 2008;178:425-430.
Silver-Coated Endotracheal Tubes Reduce Incidence of Ventilator-Associated Pneumonia (VAP)
Clinical Question: Can silver-coated endotracheal tubes reduce the incidence of VAP?
Background: Given the high morbidity linked to VAP, prevention strategies have been sought. Silver has broad-spectrum antimicrobial activity in vitro. Thus, a silver-coated endotracheal tube (ET) was designed to help prevent biofilm formation and bacterial colonization.
Study Design: A prospective, randomized, single-blind, controlled study.
Settings: 54 centers in North America.
Synopsis: Out of 9,417 potentially eligible patients, 2,003 patients expected to require mechanical ventilation for 24 hours or longer were randomized to undergo intubation with endotracheal tubes with and without silver coating. The primary outcome was incidence of VAP based on quantitative culture of bronchoalveolar lavage fluid.
The rate of microbiologically confirmed VAP in patients intubated for 24 hours or longer with the silver-coated ET tube was 4.8%, as compared to 7.5% in the control group. Using silver-coated ET tubes resulted in a 35.9% relative risk reduction of VAP incidence. Furthermore, the silver-coated ET tube was associated with a delayed time to VAP occurrence. Other outcomes, including length of intubation, duration of hospital stay, mortality, and frequency of adverse events, however, did not show statistically significant differences between the two groups.
Bottom Line: Using a silver-coated ET tube reduces the incidence of VAP, as well as delays time to VAP occurrence.
Citation: Kollef MH, Afessa B, Anzueta A, et al. Silver-coated endotracheal tubes and incidence of ventilator-associated pneumonia: the NASCENT randomized trial. JAMA. 2008;300:805-813.
Literature at a Glance
- Tight glucose control in critically ill patients is not associated with reduction in short-term mortality, but it is associated with an increased risk of hypoglycemia.
- Intensive glucose-lowering therapy in diabetic patients at high risk for cardiovascular events increased mortality.
- Targeting normal glycated hemoglobin levels with a gliclazide-based regimen does not have an effect on preventing major macrovascular events.
- Non-invasive ventilation has no effect on short-term mortality or rates of tracheal intubation and admission to ICU
- Routine use of a rhythm-control strategy does not reduce the rate of death from cardiovascular causes.
- No clinical benefit exists in employing intensive renal replacement over a conventional approach in critically ill patients.
- Initial UFH bolus and infusion dosing used for NSTE ACS often exceeds recommended weight-adjusted dosing.
- High BNP or NT-pro-BNP levels can differentiate patients who are at a higher risk of complicated hospital course and short-term mortality.
- Use of a silver-coated ET tube reduces the incidence of VAP, as well as delays time to VAP occurrence.
Tight Glucose Control in the Intensive Care Unit (ICU) Setting Does Not Reduce Short-Term Mortality
Clinical question: Does tight glucose control for critically ill patients affect mortality?
Background: Intensive glucose control for adult ICU patients has been advocated by numerous professional societies and adopted worldwide as a means to reduce mortality of critically ill patients. Evidence from multiple randomized controlled trials of tight glucose control in the ICU setting, however, shows mixed results.
Study Design: Meta-analysis of randomized controlled trials.
Setting: 29 studies involving 8,432 critically ill patients.
Synopsis: This study evaluated 29 trials involving critically ill adult patients randomized to tight glucose control versus usual care. Comparing these patients, there was no significant difference in short-term mortality (<30 days). Stratification of trials by level of glucose control (very tight <110 mg/dL versus moderately tight <150 mg/dL) and by ICU setting (surgical, medical, or mixed medical-surgical) did not affect mortality.
Tight glucose control was associated with a reduced risk of septicemia, but only in surgical patients. There was no association between tight control and a new need for dialysis, consistent across all ICU settings, as well as with both levels of glucose control. Finally, there was an increased risk of hypoglycemia (<40 mg/dL) with tight control, higher in patients who received very tight control versus those who received moderately tight control.
Limitations of the studies evaluated in this meta-analysis include difficulties with consistently maintaining tight glucose control. Twenty one percent of the trials did not achieve a mean glucose level within 5 mg/dL of the goal. This, along with a lack of standardization in reporting glucose control, makes study comparison problematic.
Bottom Line: Tight glucose control in critically ill patients is not associated with reduction in short-term mortality, but it is associated with an increased risk of hypoglycemia.
Citation: Wiener, RS, Wiener DC, Larson, RJ. Benefits and risks of tight glucose control in critically ill adults: a meta-analysis. JAMA. 2008;300:933-944.
Intensive Glucose-Lowering Therapy Increases Mortality in High-Risk Diabetic Patients
Clinical Question: Does intensive glucose-lowering therapy reduce cardiac events in high-risk diabetic patients?
Background: Epidemiologic studies have suggested the risk of cardiovascular disease increases with higher levels of glycated hemoglobin in patients with type-2 diabetes. No definitive data from randomized trials exist to test the effect of intensive glucose-lowering therapy on the rate of cardiovascular events in high-risk diabetic patients.
Study Design: Multicenter randomized controlled trial led by the Action to Control Cardiovascular Risk in Diabetes (ACCORD) Study Group.
Setting: 77 clinical centers in the U.S. and Canada.
Synopsis: 10,251 diabetic patients with established cardiovascular disease or additional cardiovascular risk factors, and median glycated hemoglobin level of 8.1%, received either intensive therapy (targeting glycated hemoglobin level <6.0%) or standard therapy (targeting level from 7.0% to 7.9%). The primary outcome was a composite of non-fatal myocardial infarction, nonfatal stroke, or death from cardiovascular causes.
Data indicated intensive therapy did decrease the rate of non-fatal myocardial infarctions, however, it did not significantly reduce the primary composite of major cardiovascular events. Moreover, intensive therapy resulted in a significant increase in death from cardiovascular causes, as well as a relative increase of 22% of death from any cause, during follow up of three and a half years. Due to this finding, the intensive therapy regimen was discontinued 17 months before the scheduled end of the study.
Analysis of the data has not identified a cause for the unexpected increased mortality in the intensive therapy group, and has not shown any medication or combination of medications to be responsible.
Bottom Line: Intensive glucose-lowering therapy in diabetic patients at high risk for cardiovascular events increased mortality and did not significantly reduce major cardiovascular events.
Citation: Action to control cardiovascular risk in diabetes study group. Effects of intensive glucose lowering in type-2 diabetes. N Engl J Med. 2008;358:2545-2559.
Intensive Glucose Control Reduces Nephropathy but Has No Effect on Major Cardiovascular Events
Clinical Question: Does intensive glucose-lowering therapy decrease major macrovascular and microvascular events in high-risk diabetic patients?
Background: Prospective studies show a direct association between elevated glycated hemoglobin levels in diabetics and increased risk of vascular events. However, definitive evidence from randomized trials about the role of intensive glucose control in preventing vascular disease in diabetics is lacking.
Study Design: Multicenter randomized controlled trial led by the ADVANCE Collaborative Group.
Setting: 215 clinical centers in 20 countries from Asia, Australia, Europe, and North America.
Synopsis: 11,140 diabetic patients received either standard glucose therapy or intensive glucose therapy using gliclazide, as well as other drugs, to reach a targeted glycated hemoglobin of 6.5% or less. The primary outcome was a composite of major macrovascular and microvascular events, including nonfatal myocardial infarction (MI), nonfatal stroke, death from cardiovascular causes, nephropathy, and retinopathy.
Intensive glucose-lowering therapy, as compared to standard therapy, resulted in a 21% relative reduction of new or worsening nephropathy. There was no significant effect on the rate of MI, strokes, death from cardiovascular causes, or retinopathy. Furthermore, intensive glucose control was associated with an increased risk of severe hypoglycemia and increased rate of hospitalization. In contrast to the ACCORD study, intensive therapy did not result in an increase in mortality.
Bottom Line: While targeting normal glycated hemoglobin levels with a gliclazide-based regimen reduced the rate of nephropathy, this strategy did not have an effect on preventing major macrovascular events.
Citation: ADVANCE collaborative group. Intensive blood glucose control and vascular outcomes in patients with type-2 diabetes. N Eng J Med. 2008;358:2560-2572.
Non-invasive Ventilation Does Not Improve Short-Term Mortality in Patients with Acute Cardiogenic Pulmonary Edema
Clinical Question: Does non-invasive ventilation improve survival for patients with acute cardiogenic pulmonary edema?
Background: Acute cardiogenic pulmonary edema is a common medical emergency, but only small trials address outcomes of non-invasive methods of ventilation.
Study Design: A prospective, randomized control study.
Setting: 26 emergency rooms and hospitals in the United Kingdom.
Synopsis: 1,069 patients with a clinical diagnosis of acute cardiogenic pulmonary edema in the emergency room were randomized to one of three treatment strategies: standard oxygen therapy, continuous positive airway pressure (CPAP), or non-invasive intermittent positive pressure ventilation (NIPPV).
There was no significant difference in the seven-day mortality between patients receiving standard oxygen therapy (9.8%) and those treated with non-invasive ventilation (9.5%). Additionally, there was no significant difference in the combined end point of death or intubation within seven days between patients receiving CPAP and NIPPV—the primary end points of the study.
While non-invasive ventilation was associated with greater reductions in dyspnea, heart rate, acidosis, and hypercapnia than was standard oxygen therapy, rates of other secondary outcomes—including tracheal intubation, admission to the critical care unit, myocardial infarction, and 30-day mortality—were similar.
Bottom Line: Although non-invasive ventilation rapidly improves respiratory distress and metabolic disturbances for patients with acute cardiogenic pulmonary edema, it has no effect on short-term mortality or rates of tracheal intubation and admission to ICU.
Citation: Gray A, Goodacre S, Newby D, et al. Non-invasive ventilation in acute cardiogenic pulmonary edema. N Eng J Med. 2008;359:142-151.
Rhythm Control in Patients with Atrial Fibrillation and CHF Does Not Improve Mortality
Clinical Question: Does the restoration of sinus rhythm in patients with atrial fibrillation and heart failure reduce mortality from cardiovascular causes?
Background: Recent data show rhythm control provides no benefit over rate control among patients with atrial fibrillation, but limited information is available regarding its applicability to patients with heart failure.
Study Design: Multicenter, prospective, double-blind, randomized trial.
Settings: 123 medical centers worldwide.
Synopsis:1,376 patients with a left ventricular ejection fraction of 35% or less, symptoms of heart failure, and a history of atrial fibrillation were randomized (allocation not concealed) either to a rhythm-control (e.g., conversion to sinus rhythm) or rate-control strategy. The primary outcome measured was the time to death from cardiovascular causes. Secondary outcomes included death from any cause, stroke, worsening heart failure, hospitalization, quality of life, cost of therapy, and a composite of death from cardiovascular causes, stroke or worsening heart failure.
Study follow up succeeded with 94% of enrolled patients completing follow up (median=47 months for survivors) or dying. Amiodarone was the drug used most often in the rhythm-control group. Ninety percent of patients received angiotensin converting enzyme inhibitors or angiotensin II receptor blocker, and 90% received anticoagulation.
Among patients with atrial fibrillation and congestive heart failure, the number of deaths from cardiovascular causes was similar in the rate (25%) and rhythm-control group (27%). Furthermore, there were no significant differences in important secondary outcomes, including death from any cause, worsening heart failure, or stroke.
Bottom Line: For patients with heart failure from systolic dysfunction and atrial fibrillation, the routine use of a rhythm-control strategy does not reduce the rate of death from cardiovascular causes as compared with a rate-control strategy.
Citation: Roy D, Talajic M, Nattel S, et al. Rhythm control versus rate control for atrial fibrillation and heart failure. N Engl J Med. 2008;358:2667-2677.
No Benefit from Intensive Renal Replacement Therapy in Critically Ill Patients with Acute Kidney Injury (AKI)
Clinical Question: Does intensive renal replacement therapy, as compared with a conventional treatment strategy, affect outcomes in critically ill patients?
Background: The optimal timing for the initiation, method, and dosing of renal replacement therapy among patients with AKI remains uncertain. Previous single-center studies limited to single methods of renal replacement therapy have suggested more intensive therapy is associated with improved survival. These results, however, have been inconsistent.
Study Design: Randomized controlled trial.
Setting: Veterans Affairs hospitals and university affiliated medical centers.
Synopsis: This study randomized 1,124 of 4,340 eligible critically ill adults with AKI to receive either intensive renal replacement therapy or a less intensive, more conventional approach. The primary end point of death at day 60 from any cause was 53.6% with intensive therapy and 51.5 % with less intensive therapy (odds ratio, 1.09; 95% CI 0.86 to 1.40; p=0.47). No significant differences were found in secondary end points, including rate of recovery of kidney function, duration of renal-replacement therapy, or evolution of non-renal organ failure.
This study demonstrates providing hemodialysis more frequently than three times per week to hemodynamically stable patients, or providing continuous renal replacement therapy at an effluent flow rate of more than 20 ml/kg/hour to hemodynamically unstable patients, does not improve outcomes. It should be noted, however, the less-intensive treatment strategy in this study provides a dose of renal replacement therapy exceeding the normal dose given in usual care.
Bottom Line: No clinical benefit exists in employing intensive renal replacement over a conventional approach in critically ill patients.
Citation: Palevsky PM, Zhang JH, O’Connor TZ, et al. Intensity of renal support in critically ill patients with acute kidney injury. N Engl J Med. 2008;359(1):7-20.
Elderly Patients and Females with Acute Coronary Syndrome (ACS) Often Receive Excess Doses of Heparin
Clinical Question: What initial dosing of unfractionated heparin (UFH) for patients with non-ST-segment elevation (NSTE) acute coronary syndrome is most frequently used and how does it affect risk of bleeding?
Background: UFH is commonly used in clinical practice for NSTE ACS, but a wide variability continues to exist in dosing protocols. Clinical studies have shown UFH dosing based on weight provides more effective early anticoagulation. However, the relationship between increasing weight-adjusted doses of UFH and the risk of bleeding has not been well described.
Study Design: Retrospective cohort study.
Setting: 420 U.S. hospitals involved in the CRUSADE (Can Rapid Risk Stratification of Unstable Angina Patients Suppress Adverse Outcomes with Early Implementation) initiative.
Synopsis: This study used data from patients enrolled in the CRUSADE initiative to investigate UFH dosing amongst 24,021 patients presenting with NSTE ACS. The study showed despite a recommendation to use weight-adjusted UFH dosing for NSTE ACS, there is a continued preference for a fixed dosing regimen of 5,000 U bolus and 1,000 U/hr initial infusion.
This fixed dose means women and the elderly are more likely to receive an excess UFH dose due to their lower body weight. The study found 35% of the group received excess weight-adjusted doses of UFH.
A clear relationship is present between excess weight-adjusted UFH doses and major bleeding, with the risk of major bleeding increasing particularly when UFH dose exceeds the recommended dosing of 70 U/kg bolus and 15 U/kg per hour infusion.
These observations support the need to follow guidelines on weight-adjusted UFH dosing in order to minimize the risk of bleeding in patients with NSTE ACS.
Bottom line: The initial UFH bolus and infusion dosing used for NSTE ACS often exceeds recommended weight-adjusted dosing, leading to higher rates of bleeding, particularly among women and the elderly.
Citation: Melloni C, Alexander KP, Chen AY et al. Unfractionated heparin dosing and risk of major bleeding in non-ST-segment elevation acute coronary syndromes. Am Heart J. 2008;156(2):209-215.
Elevated BNP Level Is a Marker for Higher Risk of Adverse Outcomes in Patients with Pulmonary Embolism
Clinical Question: Can elevated BNP levels predict adverse outcomes in patients with acute pulmonary embolism (PE)?
Background: Plasma brain natriuretic peptide (BNP) and N-terminal proBNP (NT-proBNP) often are elevated in patients with PE and right ventricular (RV) dysfunction. The finding of RV dysfunction on echocardiography is an indicator of poor outcome in these patients. The role of BNP levels to differentiate patients with PE who are at higher risk of adverse events and poor clinical outcomes has not been determined.
Study Design: Meta analysis of prospective studies.
Settings: 13 studies involving 1,132 patients.
Synopsis: Elevated levels of BNP or NT-pro-BNP were noted in 51% of patients with acute PE. These patients had a higher rate of complicated inpatient course, as well as a higher risk of 30-day mortality (odds ratio 6.8; 95% CI 4.4-10; odds-ratio 7.6; 95% CI 3.4-17). Additionally, increased BNP levels were significantly associated with RV dysfunction (p<0.0001).
While elevated BNP levels may serve as a marker for increased risk of adverse outcomes, the investigators stress these levels alone should not be used to pursue more aggressive treatment strategies. Elevation of these markers is nonspecific and can be secondary to pre-existing heart, lung, or kidney disease, or older age. Further studies are needed to determine the role of BNP in risk stratifying patients with acute PE to different forms of therapy.
Bottom Line: High BNP or NT-pro-BNP levels can differentiate patients with PE who are at a higher risk of complicated hospital course and short-term mortality.
Citation: Klok FA, Mos IC, Huisman MV. Brain-type natriuretic peptide levels in the prediction of adverse outcome in patients with pulmonary embolism: a systematic review and meta-analysis. Am J Respir Crit Care Med 2008;178:425-430.
Silver-Coated Endotracheal Tubes Reduce Incidence of Ventilator-Associated Pneumonia (VAP)
Clinical Question: Can silver-coated endotracheal tubes reduce the incidence of VAP?
Background: Given the high morbidity linked to VAP, prevention strategies have been sought. Silver has broad-spectrum antimicrobial activity in vitro. Thus, a silver-coated endotracheal tube (ET) was designed to help prevent biofilm formation and bacterial colonization.
Study Design: A prospective, randomized, single-blind, controlled study.
Settings: 54 centers in North America.
Synopsis: Out of 9,417 potentially eligible patients, 2,003 patients expected to require mechanical ventilation for 24 hours or longer were randomized to undergo intubation with endotracheal tubes with and without silver coating. The primary outcome was incidence of VAP based on quantitative culture of bronchoalveolar lavage fluid.
The rate of microbiologically confirmed VAP in patients intubated for 24 hours or longer with the silver-coated ET tube was 4.8%, as compared to 7.5% in the control group. Using silver-coated ET tubes resulted in a 35.9% relative risk reduction of VAP incidence. Furthermore, the silver-coated ET tube was associated with a delayed time to VAP occurrence. Other outcomes, including length of intubation, duration of hospital stay, mortality, and frequency of adverse events, however, did not show statistically significant differences between the two groups.
Bottom Line: Using a silver-coated ET tube reduces the incidence of VAP, as well as delays time to VAP occurrence.
Citation: Kollef MH, Afessa B, Anzueta A, et al. Silver-coated endotracheal tubes and incidence of ventilator-associated pneumonia: the NASCENT randomized trial. JAMA. 2008;300:805-813.
Literature at a Glance
- Tight glucose control in critically ill patients is not associated with reduction in short-term mortality, but it is associated with an increased risk of hypoglycemia.
- Intensive glucose-lowering therapy in diabetic patients at high risk for cardiovascular events increased mortality.
- Targeting normal glycated hemoglobin levels with a gliclazide-based regimen does not have an effect on preventing major macrovascular events.
- Non-invasive ventilation has no effect on short-term mortality or rates of tracheal intubation and admission to ICU
- Routine use of a rhythm-control strategy does not reduce the rate of death from cardiovascular causes.
- No clinical benefit exists in employing intensive renal replacement over a conventional approach in critically ill patients.
- Initial UFH bolus and infusion dosing used for NSTE ACS often exceeds recommended weight-adjusted dosing.
- High BNP or NT-pro-BNP levels can differentiate patients who are at a higher risk of complicated hospital course and short-term mortality.
- Use of a silver-coated ET tube reduces the incidence of VAP, as well as delays time to VAP occurrence.
Tight Glucose Control in the Intensive Care Unit (ICU) Setting Does Not Reduce Short-Term Mortality
Clinical question: Does tight glucose control for critically ill patients affect mortality?
Background: Intensive glucose control for adult ICU patients has been advocated by numerous professional societies and adopted worldwide as a means to reduce mortality of critically ill patients. Evidence from multiple randomized controlled trials of tight glucose control in the ICU setting, however, shows mixed results.
Study Design: Meta-analysis of randomized controlled trials.
Setting: 29 studies involving 8,432 critically ill patients.
Synopsis: This study evaluated 29 trials involving critically ill adult patients randomized to tight glucose control versus usual care. Comparing these patients, there was no significant difference in short-term mortality (<30 days). Stratification of trials by level of glucose control (very tight <110 mg/dL versus moderately tight <150 mg/dL) and by ICU setting (surgical, medical, or mixed medical-surgical) did not affect mortality.
Tight glucose control was associated with a reduced risk of septicemia, but only in surgical patients. There was no association between tight control and a new need for dialysis, consistent across all ICU settings, as well as with both levels of glucose control. Finally, there was an increased risk of hypoglycemia (<40 mg/dL) with tight control, higher in patients who received very tight control versus those who received moderately tight control.
Limitations of the studies evaluated in this meta-analysis include difficulties with consistently maintaining tight glucose control. Twenty one percent of the trials did not achieve a mean glucose level within 5 mg/dL of the goal. This, along with a lack of standardization in reporting glucose control, makes study comparison problematic.
Bottom Line: Tight glucose control in critically ill patients is not associated with reduction in short-term mortality, but it is associated with an increased risk of hypoglycemia.
Citation: Wiener, RS, Wiener DC, Larson, RJ. Benefits and risks of tight glucose control in critically ill adults: a meta-analysis. JAMA. 2008;300:933-944.
Intensive Glucose-Lowering Therapy Increases Mortality in High-Risk Diabetic Patients
Clinical Question: Does intensive glucose-lowering therapy reduce cardiac events in high-risk diabetic patients?
Background: Epidemiologic studies have suggested the risk of cardiovascular disease increases with higher levels of glycated hemoglobin in patients with type-2 diabetes. No definitive data from randomized trials exist to test the effect of intensive glucose-lowering therapy on the rate of cardiovascular events in high-risk diabetic patients.
Study Design: Multicenter randomized controlled trial led by the Action to Control Cardiovascular Risk in Diabetes (ACCORD) Study Group.
Setting: 77 clinical centers in the U.S. and Canada.
Synopsis: 10,251 diabetic patients with established cardiovascular disease or additional cardiovascular risk factors, and median glycated hemoglobin level of 8.1%, received either intensive therapy (targeting glycated hemoglobin level <6.0%) or standard therapy (targeting level from 7.0% to 7.9%). The primary outcome was a composite of non-fatal myocardial infarction, nonfatal stroke, or death from cardiovascular causes.
Data indicated intensive therapy did decrease the rate of non-fatal myocardial infarctions, however, it did not significantly reduce the primary composite of major cardiovascular events. Moreover, intensive therapy resulted in a significant increase in death from cardiovascular causes, as well as a relative increase of 22% of death from any cause, during follow up of three and a half years. Due to this finding, the intensive therapy regimen was discontinued 17 months before the scheduled end of the study.
Analysis of the data has not identified a cause for the unexpected increased mortality in the intensive therapy group, and has not shown any medication or combination of medications to be responsible.
Bottom Line: Intensive glucose-lowering therapy in diabetic patients at high risk for cardiovascular events increased mortality and did not significantly reduce major cardiovascular events.
Citation: Action to control cardiovascular risk in diabetes study group. Effects of intensive glucose lowering in type-2 diabetes. N Engl J Med. 2008;358:2545-2559.
Intensive Glucose Control Reduces Nephropathy but Has No Effect on Major Cardiovascular Events
Clinical Question: Does intensive glucose-lowering therapy decrease major macrovascular and microvascular events in high-risk diabetic patients?
Background: Prospective studies show a direct association between elevated glycated hemoglobin levels in diabetics and increased risk of vascular events. However, definitive evidence from randomized trials about the role of intensive glucose control in preventing vascular disease in diabetics is lacking.
Study Design: Multicenter randomized controlled trial led by the ADVANCE Collaborative Group.
Setting: 215 clinical centers in 20 countries from Asia, Australia, Europe, and North America.
Synopsis: 11,140 diabetic patients received either standard glucose therapy or intensive glucose therapy using gliclazide, as well as other drugs, to reach a targeted glycated hemoglobin of 6.5% or less. The primary outcome was a composite of major macrovascular and microvascular events, including nonfatal myocardial infarction (MI), nonfatal stroke, death from cardiovascular causes, nephropathy, and retinopathy.
Intensive glucose-lowering therapy, as compared to standard therapy, resulted in a 21% relative reduction of new or worsening nephropathy. There was no significant effect on the rate of MI, strokes, death from cardiovascular causes, or retinopathy. Furthermore, intensive glucose control was associated with an increased risk of severe hypoglycemia and increased rate of hospitalization. In contrast to the ACCORD study, intensive therapy did not result in an increase in mortality.
Bottom Line: While targeting normal glycated hemoglobin levels with a gliclazide-based regimen reduced the rate of nephropathy, this strategy did not have an effect on preventing major macrovascular events.
Citation: ADVANCE collaborative group. Intensive blood glucose control and vascular outcomes in patients with type-2 diabetes. N Eng J Med. 2008;358:2560-2572.
Non-invasive Ventilation Does Not Improve Short-Term Mortality in Patients with Acute Cardiogenic Pulmonary Edema
Clinical Question: Does non-invasive ventilation improve survival for patients with acute cardiogenic pulmonary edema?
Background: Acute cardiogenic pulmonary edema is a common medical emergency, but only small trials address outcomes of non-invasive methods of ventilation.
Study Design: A prospective, randomized control study.
Setting: 26 emergency rooms and hospitals in the United Kingdom.
Synopsis: 1,069 patients with a clinical diagnosis of acute cardiogenic pulmonary edema in the emergency room were randomized to one of three treatment strategies: standard oxygen therapy, continuous positive airway pressure (CPAP), or non-invasive intermittent positive pressure ventilation (NIPPV).
There was no significant difference in the seven-day mortality between patients receiving standard oxygen therapy (9.8%) and those treated with non-invasive ventilation (9.5%). Additionally, there was no significant difference in the combined end point of death or intubation within seven days between patients receiving CPAP and NIPPV—the primary end points of the study.
While non-invasive ventilation was associated with greater reductions in dyspnea, heart rate, acidosis, and hypercapnia than was standard oxygen therapy, rates of other secondary outcomes—including tracheal intubation, admission to the critical care unit, myocardial infarction, and 30-day mortality—were similar.
Bottom Line: Although non-invasive ventilation rapidly improves respiratory distress and metabolic disturbances for patients with acute cardiogenic pulmonary edema, it has no effect on short-term mortality or rates of tracheal intubation and admission to ICU.
Citation: Gray A, Goodacre S, Newby D, et al. Non-invasive ventilation in acute cardiogenic pulmonary edema. N Eng J Med. 2008;359:142-151.
Rhythm Control in Patients with Atrial Fibrillation and CHF Does Not Improve Mortality
Clinical Question: Does the restoration of sinus rhythm in patients with atrial fibrillation and heart failure reduce mortality from cardiovascular causes?
Background: Recent data show rhythm control provides no benefit over rate control among patients with atrial fibrillation, but limited information is available regarding its applicability to patients with heart failure.
Study Design: Multicenter, prospective, double-blind, randomized trial.
Settings: 123 medical centers worldwide.
Synopsis:1,376 patients with a left ventricular ejection fraction of 35% or less, symptoms of heart failure, and a history of atrial fibrillation were randomized (allocation not concealed) either to a rhythm-control (e.g., conversion to sinus rhythm) or rate-control strategy. The primary outcome measured was the time to death from cardiovascular causes. Secondary outcomes included death from any cause, stroke, worsening heart failure, hospitalization, quality of life, cost of therapy, and a composite of death from cardiovascular causes, stroke or worsening heart failure.
Study follow up succeeded with 94% of enrolled patients completing follow up (median=47 months for survivors) or dying. Amiodarone was the drug used most often in the rhythm-control group. Ninety percent of patients received angiotensin converting enzyme inhibitors or angiotensin II receptor blocker, and 90% received anticoagulation.
Among patients with atrial fibrillation and congestive heart failure, the number of deaths from cardiovascular causes was similar in the rate (25%) and rhythm-control group (27%). Furthermore, there were no significant differences in important secondary outcomes, including death from any cause, worsening heart failure, or stroke.
Bottom Line: For patients with heart failure from systolic dysfunction and atrial fibrillation, the routine use of a rhythm-control strategy does not reduce the rate of death from cardiovascular causes as compared with a rate-control strategy.
Citation: Roy D, Talajic M, Nattel S, et al. Rhythm control versus rate control for atrial fibrillation and heart failure. N Engl J Med. 2008;358:2667-2677.
No Benefit from Intensive Renal Replacement Therapy in Critically Ill Patients with Acute Kidney Injury (AKI)
Clinical Question: Does intensive renal replacement therapy, as compared with a conventional treatment strategy, affect outcomes in critically ill patients?
Background: The optimal timing for the initiation, method, and dosing of renal replacement therapy among patients with AKI remains uncertain. Previous single-center studies limited to single methods of renal replacement therapy have suggested more intensive therapy is associated with improved survival. These results, however, have been inconsistent.
Study Design: Randomized controlled trial.
Setting: Veterans Affairs hospitals and university affiliated medical centers.
Synopsis: This study randomized 1,124 of 4,340 eligible critically ill adults with AKI to receive either intensive renal replacement therapy or a less intensive, more conventional approach. The primary end point of death at day 60 from any cause was 53.6% with intensive therapy and 51.5 % with less intensive therapy (odds ratio, 1.09; 95% CI 0.86 to 1.40; p=0.47). No significant differences were found in secondary end points, including rate of recovery of kidney function, duration of renal-replacement therapy, or evolution of non-renal organ failure.
This study demonstrates providing hemodialysis more frequently than three times per week to hemodynamically stable patients, or providing continuous renal replacement therapy at an effluent flow rate of more than 20 ml/kg/hour to hemodynamically unstable patients, does not improve outcomes. It should be noted, however, the less-intensive treatment strategy in this study provides a dose of renal replacement therapy exceeding the normal dose given in usual care.
Bottom Line: No clinical benefit exists in employing intensive renal replacement over a conventional approach in critically ill patients.
Citation: Palevsky PM, Zhang JH, O’Connor TZ, et al. Intensity of renal support in critically ill patients with acute kidney injury. N Engl J Med. 2008;359(1):7-20.
Elderly Patients and Females with Acute Coronary Syndrome (ACS) Often Receive Excess Doses of Heparin
Clinical Question: What initial dosing of unfractionated heparin (UFH) for patients with non-ST-segment elevation (NSTE) acute coronary syndrome is most frequently used and how does it affect risk of bleeding?
Background: UFH is commonly used in clinical practice for NSTE ACS, but a wide variability continues to exist in dosing protocols. Clinical studies have shown UFH dosing based on weight provides more effective early anticoagulation. However, the relationship between increasing weight-adjusted doses of UFH and the risk of bleeding has not been well described.
Study Design: Retrospective cohort study.
Setting: 420 U.S. hospitals involved in the CRUSADE (Can Rapid Risk Stratification of Unstable Angina Patients Suppress Adverse Outcomes with Early Implementation) initiative.
Synopsis: This study used data from patients enrolled in the CRUSADE initiative to investigate UFH dosing amongst 24,021 patients presenting with NSTE ACS. The study showed despite a recommendation to use weight-adjusted UFH dosing for NSTE ACS, there is a continued preference for a fixed dosing regimen of 5,000 U bolus and 1,000 U/hr initial infusion.
This fixed dose means women and the elderly are more likely to receive an excess UFH dose due to their lower body weight. The study found 35% of the group received excess weight-adjusted doses of UFH.
A clear relationship is present between excess weight-adjusted UFH doses and major bleeding, with the risk of major bleeding increasing particularly when UFH dose exceeds the recommended dosing of 70 U/kg bolus and 15 U/kg per hour infusion.
These observations support the need to follow guidelines on weight-adjusted UFH dosing in order to minimize the risk of bleeding in patients with NSTE ACS.
Bottom line: The initial UFH bolus and infusion dosing used for NSTE ACS often exceeds recommended weight-adjusted dosing, leading to higher rates of bleeding, particularly among women and the elderly.
Citation: Melloni C, Alexander KP, Chen AY et al. Unfractionated heparin dosing and risk of major bleeding in non-ST-segment elevation acute coronary syndromes. Am Heart J. 2008;156(2):209-215.
Elevated BNP Level Is a Marker for Higher Risk of Adverse Outcomes in Patients with Pulmonary Embolism
Clinical Question: Can elevated BNP levels predict adverse outcomes in patients with acute pulmonary embolism (PE)?
Background: Plasma brain natriuretic peptide (BNP) and N-terminal proBNP (NT-proBNP) often are elevated in patients with PE and right ventricular (RV) dysfunction. The finding of RV dysfunction on echocardiography is an indicator of poor outcome in these patients. The role of BNP levels to differentiate patients with PE who are at higher risk of adverse events and poor clinical outcomes has not been determined.
Study Design: Meta analysis of prospective studies.
Settings: 13 studies involving 1,132 patients.
Synopsis: Elevated levels of BNP or NT-pro-BNP were noted in 51% of patients with acute PE. These patients had a higher rate of complicated inpatient course, as well as a higher risk of 30-day mortality (odds ratio 6.8; 95% CI 4.4-10; odds-ratio 7.6; 95% CI 3.4-17). Additionally, increased BNP levels were significantly associated with RV dysfunction (p<0.0001).
While elevated BNP levels may serve as a marker for increased risk of adverse outcomes, the investigators stress these levels alone should not be used to pursue more aggressive treatment strategies. Elevation of these markers is nonspecific and can be secondary to pre-existing heart, lung, or kidney disease, or older age. Further studies are needed to determine the role of BNP in risk stratifying patients with acute PE to different forms of therapy.
Bottom Line: High BNP or NT-pro-BNP levels can differentiate patients with PE who are at a higher risk of complicated hospital course and short-term mortality.
Citation: Klok FA, Mos IC, Huisman MV. Brain-type natriuretic peptide levels in the prediction of adverse outcome in patients with pulmonary embolism: a systematic review and meta-analysis. Am J Respir Crit Care Med 2008;178:425-430.
Silver-Coated Endotracheal Tubes Reduce Incidence of Ventilator-Associated Pneumonia (VAP)
Clinical Question: Can silver-coated endotracheal tubes reduce the incidence of VAP?
Background: Given the high morbidity linked to VAP, prevention strategies have been sought. Silver has broad-spectrum antimicrobial activity in vitro. Thus, a silver-coated endotracheal tube (ET) was designed to help prevent biofilm formation and bacterial colonization.
Study Design: A prospective, randomized, single-blind, controlled study.
Settings: 54 centers in North America.
Synopsis: Out of 9,417 potentially eligible patients, 2,003 patients expected to require mechanical ventilation for 24 hours or longer were randomized to undergo intubation with endotracheal tubes with and without silver coating. The primary outcome was incidence of VAP based on quantitative culture of bronchoalveolar lavage fluid.
The rate of microbiologically confirmed VAP in patients intubated for 24 hours or longer with the silver-coated ET tube was 4.8%, as compared to 7.5% in the control group. Using silver-coated ET tubes resulted in a 35.9% relative risk reduction of VAP incidence. Furthermore, the silver-coated ET tube was associated with a delayed time to VAP occurrence. Other outcomes, including length of intubation, duration of hospital stay, mortality, and frequency of adverse events, however, did not show statistically significant differences between the two groups.
Bottom Line: Using a silver-coated ET tube reduces the incidence of VAP, as well as delays time to VAP occurrence.
Citation: Kollef MH, Afessa B, Anzueta A, et al. Silver-coated endotracheal tubes and incidence of ventilator-associated pneumonia: the NASCENT randomized trial. JAMA. 2008;300:805-813.
New Faces in Key Places
Healthcare quality and patient safety is a hot topic in hospitals across the country, as well as here at The Society of Hospital Medicine (SHM). It seems like every day we hear of new regulatory requirements from the Centers for Medicare and Medicaid Services (CMS), The Joint Commission, and state health departments, or requirements from other health care organizations, including insurance companies. It’s hard to keep up with it all.
To help hospitals with their quality initiatives, SHM recently beefed up its Quality Initiatives Department by adding three new staff members, including myself. I’d like to introduce you to our newest members. My name is Jane Kelly-Cummings, and I joined SHM in July as the senior director of Quality Initiatives. I’m responsible for the strategic planning, development and implementation of quality initiatives for the society and the staff liaison for the Hospital Quality and Patient Safety Committee. I’ve been a registered nurse (RN) for more than 20 years and have been working in the quality world for more than a decade.
Linda Boclair joined SHM in June as director of Quality Initiatives. She is responsible for proposal/grant writing, managing select quality initiative projects, and department operations. She has a background in medical technology and industrial relations/organizational behavior. Linda currently is working on a medication reconciliation project, an advisory panel on pharmacoeconomics, and she is working on the new co-management taskforce.
Lauren Valentino also joined SHM in June as the departments project coordinator. She is responsible for supporting the Quality Initiatives department through project planning and implementation. Lauren also is a support resource for the society, providing documentation and coordination to the committees, task forces, and various special interest groups.
The new staffers join Joy M. Wittnebert-Barnosky, senior project manager; Tina Budnitz, senior advisor for Quality Initiatives; and Kathleen Kerr, project manager of QI Mentored Implementation in rounding out SHM’s new Quality Initiatives Department.
In order to best meet the quality initiatives needs of our members, we have been developing SHM’s quality initiatives strategic plan. We had the chance to share the plan with SHM board members at the bi-annual board meeting in October. The board received the strategic plan well, and the group is looking forward to an update at the January board meeting. SHM’s strategic quality initiative planning began in October 2007, when a group of SHM leaders met to begin the process of developing a 10-year strategic plan for quality initiatives. The output of this meeting led to six areas of focus, which we refer to as core strategies:
- Develop education programs and technical support tools in quality improvement or patient safety;
- Advance a national quality agenda for hospitals and hospitalists;
- Facilitate cultural change and develop initiatives to promote hospital medicine’s role in quality initiatives within the C-suite at our nation’s hospitals;
- Evaluate effectiveness of current offerings in quality improvement or patient safety;
- Promote adoption of health information technologies to advance patient safety and quality improvement; and
- Promote and support the new science of QI (i.e., develop a research agenda).
Linking these focus areas with SHM’s Core Competencies in Hospital Medicine and current national industry quality initiatives, such as The Joint Commission’s National Patient Safety Goals and Core Measures, is the basic foundation for SHM’s strategic quality plan. This plan will allow SHM to become more proactive in our approach to quality initiatives for the next one, three, five, and 10 years. It will help us focus on the areas identified as needs for hospitalists and hospital medicine.
Plan Breakdown
I would like to tell you about some of the newest quality initiatives currently underway. First is an advisory board on pharmacoeconomics. We are pulling together 11 industry leaders, including CEOs, chief financial officers, chief medical officers, pharmacists, and thought leaders in quality. This advisory board will be evaluating the standard operating procedures in hospitals across the country regarding the use of pharmacoeconomics in decisions to utilize medications, especially newer and more expensive agents, using venous thromboembolism (VTE) prevention as a case example.
We have assembled another advisory board, which is just underway, to look at complicated skin and skin structure infections (cSSSI). This board will include hospitalists, infection control physicians, emergency room physicians, pharmacists, wound care nurses, and quality improvement experts.
Lastly, we have a second VTE project charged with the development of an automated, electronic query for a major commercial clinical information system. The project team is tasked to develop and demonstrate how a system can dramatically increase the prevalence of VTE prophylaxis in hospitals where it will be piloted.
Collaborative Efforts
I also would like to share a few of the other exciting activities the quality department has been up to recently. SHM is in the process of collaborating on a book with the Joint Commission Resources on Hospitalists and Patient Safety. The book is scheduled for release this spring, so be on the lookout. We also are writing an article for the The Physician Executive, which is the journal of the American College of Physician Executives. The article focuses on how quality, patient safety, and patient satisfaction are becoming priorities for physician executives, and how hospitalists are a critical element of a strategy to address this priority. We also are talking with other organizations, such as the American Hospital Association and United Health Group, about potential collaborative work in the future.
So, you can see things at SHM headquarters are anything but dull. The entire QI department—both the veterans and new staff—are looking forward to helping you make your quality and patient safety initiatives more successful and improve the care of patients throughout the country. TH
Healthcare quality and patient safety is a hot topic in hospitals across the country, as well as here at The Society of Hospital Medicine (SHM). It seems like every day we hear of new regulatory requirements from the Centers for Medicare and Medicaid Services (CMS), The Joint Commission, and state health departments, or requirements from other health care organizations, including insurance companies. It’s hard to keep up with it all.
To help hospitals with their quality initiatives, SHM recently beefed up its Quality Initiatives Department by adding three new staff members, including myself. I’d like to introduce you to our newest members. My name is Jane Kelly-Cummings, and I joined SHM in July as the senior director of Quality Initiatives. I’m responsible for the strategic planning, development and implementation of quality initiatives for the society and the staff liaison for the Hospital Quality and Patient Safety Committee. I’ve been a registered nurse (RN) for more than 20 years and have been working in the quality world for more than a decade.
Linda Boclair joined SHM in June as director of Quality Initiatives. She is responsible for proposal/grant writing, managing select quality initiative projects, and department operations. She has a background in medical technology and industrial relations/organizational behavior. Linda currently is working on a medication reconciliation project, an advisory panel on pharmacoeconomics, and she is working on the new co-management taskforce.
Lauren Valentino also joined SHM in June as the departments project coordinator. She is responsible for supporting the Quality Initiatives department through project planning and implementation. Lauren also is a support resource for the society, providing documentation and coordination to the committees, task forces, and various special interest groups.
The new staffers join Joy M. Wittnebert-Barnosky, senior project manager; Tina Budnitz, senior advisor for Quality Initiatives; and Kathleen Kerr, project manager of QI Mentored Implementation in rounding out SHM’s new Quality Initiatives Department.
In order to best meet the quality initiatives needs of our members, we have been developing SHM’s quality initiatives strategic plan. We had the chance to share the plan with SHM board members at the bi-annual board meeting in October. The board received the strategic plan well, and the group is looking forward to an update at the January board meeting. SHM’s strategic quality initiative planning began in October 2007, when a group of SHM leaders met to begin the process of developing a 10-year strategic plan for quality initiatives. The output of this meeting led to six areas of focus, which we refer to as core strategies:
- Develop education programs and technical support tools in quality improvement or patient safety;
- Advance a national quality agenda for hospitals and hospitalists;
- Facilitate cultural change and develop initiatives to promote hospital medicine’s role in quality initiatives within the C-suite at our nation’s hospitals;
- Evaluate effectiveness of current offerings in quality improvement or patient safety;
- Promote adoption of health information technologies to advance patient safety and quality improvement; and
- Promote and support the new science of QI (i.e., develop a research agenda).
Linking these focus areas with SHM’s Core Competencies in Hospital Medicine and current national industry quality initiatives, such as The Joint Commission’s National Patient Safety Goals and Core Measures, is the basic foundation for SHM’s strategic quality plan. This plan will allow SHM to become more proactive in our approach to quality initiatives for the next one, three, five, and 10 years. It will help us focus on the areas identified as needs for hospitalists and hospital medicine.
Plan Breakdown
I would like to tell you about some of the newest quality initiatives currently underway. First is an advisory board on pharmacoeconomics. We are pulling together 11 industry leaders, including CEOs, chief financial officers, chief medical officers, pharmacists, and thought leaders in quality. This advisory board will be evaluating the standard operating procedures in hospitals across the country regarding the use of pharmacoeconomics in decisions to utilize medications, especially newer and more expensive agents, using venous thromboembolism (VTE) prevention as a case example.
We have assembled another advisory board, which is just underway, to look at complicated skin and skin structure infections (cSSSI). This board will include hospitalists, infection control physicians, emergency room physicians, pharmacists, wound care nurses, and quality improvement experts.
Lastly, we have a second VTE project charged with the development of an automated, electronic query for a major commercial clinical information system. The project team is tasked to develop and demonstrate how a system can dramatically increase the prevalence of VTE prophylaxis in hospitals where it will be piloted.
Collaborative Efforts
I also would like to share a few of the other exciting activities the quality department has been up to recently. SHM is in the process of collaborating on a book with the Joint Commission Resources on Hospitalists and Patient Safety. The book is scheduled for release this spring, so be on the lookout. We also are writing an article for the The Physician Executive, which is the journal of the American College of Physician Executives. The article focuses on how quality, patient safety, and patient satisfaction are becoming priorities for physician executives, and how hospitalists are a critical element of a strategy to address this priority. We also are talking with other organizations, such as the American Hospital Association and United Health Group, about potential collaborative work in the future.
So, you can see things at SHM headquarters are anything but dull. The entire QI department—both the veterans and new staff—are looking forward to helping you make your quality and patient safety initiatives more successful and improve the care of patients throughout the country. TH
Healthcare quality and patient safety is a hot topic in hospitals across the country, as well as here at The Society of Hospital Medicine (SHM). It seems like every day we hear of new regulatory requirements from the Centers for Medicare and Medicaid Services (CMS), The Joint Commission, and state health departments, or requirements from other health care organizations, including insurance companies. It’s hard to keep up with it all.
To help hospitals with their quality initiatives, SHM recently beefed up its Quality Initiatives Department by adding three new staff members, including myself. I’d like to introduce you to our newest members. My name is Jane Kelly-Cummings, and I joined SHM in July as the senior director of Quality Initiatives. I’m responsible for the strategic planning, development and implementation of quality initiatives for the society and the staff liaison for the Hospital Quality and Patient Safety Committee. I’ve been a registered nurse (RN) for more than 20 years and have been working in the quality world for more than a decade.
Linda Boclair joined SHM in June as director of Quality Initiatives. She is responsible for proposal/grant writing, managing select quality initiative projects, and department operations. She has a background in medical technology and industrial relations/organizational behavior. Linda currently is working on a medication reconciliation project, an advisory panel on pharmacoeconomics, and she is working on the new co-management taskforce.
Lauren Valentino also joined SHM in June as the departments project coordinator. She is responsible for supporting the Quality Initiatives department through project planning and implementation. Lauren also is a support resource for the society, providing documentation and coordination to the committees, task forces, and various special interest groups.
The new staffers join Joy M. Wittnebert-Barnosky, senior project manager; Tina Budnitz, senior advisor for Quality Initiatives; and Kathleen Kerr, project manager of QI Mentored Implementation in rounding out SHM’s new Quality Initiatives Department.
In order to best meet the quality initiatives needs of our members, we have been developing SHM’s quality initiatives strategic plan. We had the chance to share the plan with SHM board members at the bi-annual board meeting in October. The board received the strategic plan well, and the group is looking forward to an update at the January board meeting. SHM’s strategic quality initiative planning began in October 2007, when a group of SHM leaders met to begin the process of developing a 10-year strategic plan for quality initiatives. The output of this meeting led to six areas of focus, which we refer to as core strategies:
- Develop education programs and technical support tools in quality improvement or patient safety;
- Advance a national quality agenda for hospitals and hospitalists;
- Facilitate cultural change and develop initiatives to promote hospital medicine’s role in quality initiatives within the C-suite at our nation’s hospitals;
- Evaluate effectiveness of current offerings in quality improvement or patient safety;
- Promote adoption of health information technologies to advance patient safety and quality improvement; and
- Promote and support the new science of QI (i.e., develop a research agenda).
Linking these focus areas with SHM’s Core Competencies in Hospital Medicine and current national industry quality initiatives, such as The Joint Commission’s National Patient Safety Goals and Core Measures, is the basic foundation for SHM’s strategic quality plan. This plan will allow SHM to become more proactive in our approach to quality initiatives for the next one, three, five, and 10 years. It will help us focus on the areas identified as needs for hospitalists and hospital medicine.
Plan Breakdown
I would like to tell you about some of the newest quality initiatives currently underway. First is an advisory board on pharmacoeconomics. We are pulling together 11 industry leaders, including CEOs, chief financial officers, chief medical officers, pharmacists, and thought leaders in quality. This advisory board will be evaluating the standard operating procedures in hospitals across the country regarding the use of pharmacoeconomics in decisions to utilize medications, especially newer and more expensive agents, using venous thromboembolism (VTE) prevention as a case example.
We have assembled another advisory board, which is just underway, to look at complicated skin and skin structure infections (cSSSI). This board will include hospitalists, infection control physicians, emergency room physicians, pharmacists, wound care nurses, and quality improvement experts.
Lastly, we have a second VTE project charged with the development of an automated, electronic query for a major commercial clinical information system. The project team is tasked to develop and demonstrate how a system can dramatically increase the prevalence of VTE prophylaxis in hospitals where it will be piloted.
Collaborative Efforts
I also would like to share a few of the other exciting activities the quality department has been up to recently. SHM is in the process of collaborating on a book with the Joint Commission Resources on Hospitalists and Patient Safety. The book is scheduled for release this spring, so be on the lookout. We also are writing an article for the The Physician Executive, which is the journal of the American College of Physician Executives. The article focuses on how quality, patient safety, and patient satisfaction are becoming priorities for physician executives, and how hospitalists are a critical element of a strategy to address this priority. We also are talking with other organizations, such as the American Hospital Association and United Health Group, about potential collaborative work in the future.
So, you can see things at SHM headquarters are anything but dull. The entire QI department—both the veterans and new staff—are looking forward to helping you make your quality and patient safety initiatives more successful and improve the care of patients throughout the country. TH
Medicare Modifications
Most hospitalists vividly recall Congress overriding President Bush’s July veto to avert a hefty, 10.6% cut in Medicare Part B payments to physicians. That memorable, last-minute save (instead of a pay cut, Congress increased Part B payments by 1.1%) was just a tiny part of some important legislation. The Medicare Improvements for Patients and Providers Act (MIPPA) includes myriad provisions addressing Medicare benefits, protections for low-income beneficiaries, changes for providers, data collection requirements for correcting healthcare disparities, and much more.
Hospitalists will be particularly interested in a handful of the provisions outlined in MIPPA, some of which impact them directly and others that will affect hospitals and clinical care, and still more whose outcomes remain to be seen.
For example, MIPPA is the legislation that extends the Physician Quality Reporting Initiative (PQRI) for two years, offering a bonus payment in 2009 and 2010 of 2% (up from 1.5%) of total Medicare allowed charges. It also directs the Centers for Medicare and Medicaid Services (CMS) to publicly post the list of providers who participate in the PQRI. (See “A Permanent PQRI” in the October 2008 issue of The Hospitalist.)
MIPPA also requires CMS to establish a program to promote widespread adoption of electronic prescribing, as outlined in “e-Prescription for Success?” in the September 2008 issue of The Hospitalist. Reporting on e-prescribing is not likely to apply to hospitalists, says Bradley Flansbaum, DO, MPH, chief of hospitalist section at Lenox Hill Hospital in New York City and a member of SHM’s Public Policy Committee. “Of course, it depends on whether the hospital uses it, but no one can say whether a hospitalist will get a benefit for reporting on e-prescribing,” he says.
Lucrative Changes to E&M Codes
One provision directly impacting hospitalists is MIPPA’s changes to payments for inpatient evaluation and management codes (E&M codes). According to Laura Allendorf, SHM’s senior advisor for advocacy and government affairs, this change will result in an estimated 3% average gain in total Medicare payments to hospitalists, or $5,000 to $6,000 annually—on top of the 1.1% payment update. (It’s important to note the final 2009 physician fee schedule, published in November, could change the overall impact for individual members.) E&M payments from some private payers also could increase, since many base their fees on Medicare’s fee schedule.
Quality Research Initiatives
MIPPA requires the establishment or continuation of several quality research initiatives, designed to help CMS determine new models of efficiency of care and cost efficiency.
One of these initiatives is Patient-Centered Medical Home (PCMH), a care model that facilitates partnerships between individual patients and their personal physicians, and when appropriate, the patient’s family. Care is facilitated by registries, information technology, health information exchange, and other means to assure patients get the indicated care when and where they need and want it in a culturally and linguistically appropriate manner. MIPPA grants new funding and expanded authority for CMS’ Medical Home Demonstration Project—if certain quality and/or savings targets are achieved.
“We’ve talked a bit about Patient-Centered Medical Home,” says Dr. Flansbaum of SHM’s Public Policy Committee. “From a political standpoint, it’s a feel-good agenda item with a lot of bipartisan support. The notion of this is here, but operationalizing it—getting it to work—is an entirely different story.” By definition, PCMH will revolve around primary care physicians, and the role and responsibilities of any hospitalists involved is yet unknown—as is the reimbursement model. “This is so far away right now, it’s a notion that needs to be turned into a theory that needs to be turned into a paradigm, to paraphrase Woody Allen,” Dr. Flansbaum says.
Another initiative greenlighted by MIPPA is comparative effectiveness research, or CER. It examines the effectiveness of different therapies for a specific medical condition, or for a specific set of patients, to determine the best option. It may involve comparing competing medications, or may analyze different treatment approaches such as surgery, devices, and drug therapies. MIPPA requires the Institute of Medicine report on best practices for the review of comparative effectiveness research and the development of clinical protocols.
“Obviously, the medical device companies and the pharmaceutical companies are against this,” Dr. Flansbaum says. “But it would be helpful for physicians, because it would give some guidance in certain gray-area treatments, such as: Is this drug appropriate in treating an end-stage cancer patient?” And as far as the nation’s health care system goes, he explains, “I think we need comparative effectiveness. We can’t continue as we are—on the net, we’re going broke—our current healthcare system can’t afford to keep going.”
Not the Only Game in Town
One interesting provision of MIPPA revokes “the unique authority of the Joint Commission to deem hospitals in compliance with the Medicare Conditions of Participation,” meaning hospital compliance is an open market—subject to approval from CMS, of course.
“The Joint Commission has been the gold standard for hospitals for a long, long time,” Dr. Flansbaum points out. “Now that they’ve opened that up, DNV (Det Norske Veritas Healthcare, Inc.) [for example], can compete with the Joint Commission to certify hospitals.”
What will this mean for hospitals? Probably not much in the short term. “I believe only 15 hospitals have DNV certifications, and that all of those also have a Joint Commission certification,” Dr. Flansbaum says, adding “[DNV and the Joint Commission] have a different approach; it’s like the ACT and the SAT. Both are used for college entrance exams, but the SAT is still mostly the gold standard, like the Joint Commission. But who knows? That could change … and if it does, well, competition is good.”
Some of the MIPPA provisions, such as the quality research initiatives, could end up shaping the future of healthcare. Others, such as the continuation of PQRI, may lead to new payment models for physicians.
Only time will tell which provisions will truly improve efficiency and costs—and which will impact hospital medicine in particular. TH
Jane Jerrard is a medical writer based in Chicago.
Most hospitalists vividly recall Congress overriding President Bush’s July veto to avert a hefty, 10.6% cut in Medicare Part B payments to physicians. That memorable, last-minute save (instead of a pay cut, Congress increased Part B payments by 1.1%) was just a tiny part of some important legislation. The Medicare Improvements for Patients and Providers Act (MIPPA) includes myriad provisions addressing Medicare benefits, protections for low-income beneficiaries, changes for providers, data collection requirements for correcting healthcare disparities, and much more.
Hospitalists will be particularly interested in a handful of the provisions outlined in MIPPA, some of which impact them directly and others that will affect hospitals and clinical care, and still more whose outcomes remain to be seen.
For example, MIPPA is the legislation that extends the Physician Quality Reporting Initiative (PQRI) for two years, offering a bonus payment in 2009 and 2010 of 2% (up from 1.5%) of total Medicare allowed charges. It also directs the Centers for Medicare and Medicaid Services (CMS) to publicly post the list of providers who participate in the PQRI. (See “A Permanent PQRI” in the October 2008 issue of The Hospitalist.)
MIPPA also requires CMS to establish a program to promote widespread adoption of electronic prescribing, as outlined in “e-Prescription for Success?” in the September 2008 issue of The Hospitalist. Reporting on e-prescribing is not likely to apply to hospitalists, says Bradley Flansbaum, DO, MPH, chief of hospitalist section at Lenox Hill Hospital in New York City and a member of SHM’s Public Policy Committee. “Of course, it depends on whether the hospital uses it, but no one can say whether a hospitalist will get a benefit for reporting on e-prescribing,” he says.
Lucrative Changes to E&M Codes
One provision directly impacting hospitalists is MIPPA’s changes to payments for inpatient evaluation and management codes (E&M codes). According to Laura Allendorf, SHM’s senior advisor for advocacy and government affairs, this change will result in an estimated 3% average gain in total Medicare payments to hospitalists, or $5,000 to $6,000 annually—on top of the 1.1% payment update. (It’s important to note the final 2009 physician fee schedule, published in November, could change the overall impact for individual members.) E&M payments from some private payers also could increase, since many base their fees on Medicare’s fee schedule.
Quality Research Initiatives
MIPPA requires the establishment or continuation of several quality research initiatives, designed to help CMS determine new models of efficiency of care and cost efficiency.
One of these initiatives is Patient-Centered Medical Home (PCMH), a care model that facilitates partnerships between individual patients and their personal physicians, and when appropriate, the patient’s family. Care is facilitated by registries, information technology, health information exchange, and other means to assure patients get the indicated care when and where they need and want it in a culturally and linguistically appropriate manner. MIPPA grants new funding and expanded authority for CMS’ Medical Home Demonstration Project—if certain quality and/or savings targets are achieved.
“We’ve talked a bit about Patient-Centered Medical Home,” says Dr. Flansbaum of SHM’s Public Policy Committee. “From a political standpoint, it’s a feel-good agenda item with a lot of bipartisan support. The notion of this is here, but operationalizing it—getting it to work—is an entirely different story.” By definition, PCMH will revolve around primary care physicians, and the role and responsibilities of any hospitalists involved is yet unknown—as is the reimbursement model. “This is so far away right now, it’s a notion that needs to be turned into a theory that needs to be turned into a paradigm, to paraphrase Woody Allen,” Dr. Flansbaum says.
Another initiative greenlighted by MIPPA is comparative effectiveness research, or CER. It examines the effectiveness of different therapies for a specific medical condition, or for a specific set of patients, to determine the best option. It may involve comparing competing medications, or may analyze different treatment approaches such as surgery, devices, and drug therapies. MIPPA requires the Institute of Medicine report on best practices for the review of comparative effectiveness research and the development of clinical protocols.
“Obviously, the medical device companies and the pharmaceutical companies are against this,” Dr. Flansbaum says. “But it would be helpful for physicians, because it would give some guidance in certain gray-area treatments, such as: Is this drug appropriate in treating an end-stage cancer patient?” And as far as the nation’s health care system goes, he explains, “I think we need comparative effectiveness. We can’t continue as we are—on the net, we’re going broke—our current healthcare system can’t afford to keep going.”
Not the Only Game in Town
One interesting provision of MIPPA revokes “the unique authority of the Joint Commission to deem hospitals in compliance with the Medicare Conditions of Participation,” meaning hospital compliance is an open market—subject to approval from CMS, of course.
“The Joint Commission has been the gold standard for hospitals for a long, long time,” Dr. Flansbaum points out. “Now that they’ve opened that up, DNV (Det Norske Veritas Healthcare, Inc.) [for example], can compete with the Joint Commission to certify hospitals.”
What will this mean for hospitals? Probably not much in the short term. “I believe only 15 hospitals have DNV certifications, and that all of those also have a Joint Commission certification,” Dr. Flansbaum says, adding “[DNV and the Joint Commission] have a different approach; it’s like the ACT and the SAT. Both are used for college entrance exams, but the SAT is still mostly the gold standard, like the Joint Commission. But who knows? That could change … and if it does, well, competition is good.”
Some of the MIPPA provisions, such as the quality research initiatives, could end up shaping the future of healthcare. Others, such as the continuation of PQRI, may lead to new payment models for physicians.
Only time will tell which provisions will truly improve efficiency and costs—and which will impact hospital medicine in particular. TH
Jane Jerrard is a medical writer based in Chicago.
Most hospitalists vividly recall Congress overriding President Bush’s July veto to avert a hefty, 10.6% cut in Medicare Part B payments to physicians. That memorable, last-minute save (instead of a pay cut, Congress increased Part B payments by 1.1%) was just a tiny part of some important legislation. The Medicare Improvements for Patients and Providers Act (MIPPA) includes myriad provisions addressing Medicare benefits, protections for low-income beneficiaries, changes for providers, data collection requirements for correcting healthcare disparities, and much more.
Hospitalists will be particularly interested in a handful of the provisions outlined in MIPPA, some of which impact them directly and others that will affect hospitals and clinical care, and still more whose outcomes remain to be seen.
For example, MIPPA is the legislation that extends the Physician Quality Reporting Initiative (PQRI) for two years, offering a bonus payment in 2009 and 2010 of 2% (up from 1.5%) of total Medicare allowed charges. It also directs the Centers for Medicare and Medicaid Services (CMS) to publicly post the list of providers who participate in the PQRI. (See “A Permanent PQRI” in the October 2008 issue of The Hospitalist.)
MIPPA also requires CMS to establish a program to promote widespread adoption of electronic prescribing, as outlined in “e-Prescription for Success?” in the September 2008 issue of The Hospitalist. Reporting on e-prescribing is not likely to apply to hospitalists, says Bradley Flansbaum, DO, MPH, chief of hospitalist section at Lenox Hill Hospital in New York City and a member of SHM’s Public Policy Committee. “Of course, it depends on whether the hospital uses it, but no one can say whether a hospitalist will get a benefit for reporting on e-prescribing,” he says.
Lucrative Changes to E&M Codes
One provision directly impacting hospitalists is MIPPA’s changes to payments for inpatient evaluation and management codes (E&M codes). According to Laura Allendorf, SHM’s senior advisor for advocacy and government affairs, this change will result in an estimated 3% average gain in total Medicare payments to hospitalists, or $5,000 to $6,000 annually—on top of the 1.1% payment update. (It’s important to note the final 2009 physician fee schedule, published in November, could change the overall impact for individual members.) E&M payments from some private payers also could increase, since many base their fees on Medicare’s fee schedule.
Quality Research Initiatives
MIPPA requires the establishment or continuation of several quality research initiatives, designed to help CMS determine new models of efficiency of care and cost efficiency.
One of these initiatives is Patient-Centered Medical Home (PCMH), a care model that facilitates partnerships between individual patients and their personal physicians, and when appropriate, the patient’s family. Care is facilitated by registries, information technology, health information exchange, and other means to assure patients get the indicated care when and where they need and want it in a culturally and linguistically appropriate manner. MIPPA grants new funding and expanded authority for CMS’ Medical Home Demonstration Project—if certain quality and/or savings targets are achieved.
“We’ve talked a bit about Patient-Centered Medical Home,” says Dr. Flansbaum of SHM’s Public Policy Committee. “From a political standpoint, it’s a feel-good agenda item with a lot of bipartisan support. The notion of this is here, but operationalizing it—getting it to work—is an entirely different story.” By definition, PCMH will revolve around primary care physicians, and the role and responsibilities of any hospitalists involved is yet unknown—as is the reimbursement model. “This is so far away right now, it’s a notion that needs to be turned into a theory that needs to be turned into a paradigm, to paraphrase Woody Allen,” Dr. Flansbaum says.
Another initiative greenlighted by MIPPA is comparative effectiveness research, or CER. It examines the effectiveness of different therapies for a specific medical condition, or for a specific set of patients, to determine the best option. It may involve comparing competing medications, or may analyze different treatment approaches such as surgery, devices, and drug therapies. MIPPA requires the Institute of Medicine report on best practices for the review of comparative effectiveness research and the development of clinical protocols.
“Obviously, the medical device companies and the pharmaceutical companies are against this,” Dr. Flansbaum says. “But it would be helpful for physicians, because it would give some guidance in certain gray-area treatments, such as: Is this drug appropriate in treating an end-stage cancer patient?” And as far as the nation’s health care system goes, he explains, “I think we need comparative effectiveness. We can’t continue as we are—on the net, we’re going broke—our current healthcare system can’t afford to keep going.”
Not the Only Game in Town
One interesting provision of MIPPA revokes “the unique authority of the Joint Commission to deem hospitals in compliance with the Medicare Conditions of Participation,” meaning hospital compliance is an open market—subject to approval from CMS, of course.
“The Joint Commission has been the gold standard for hospitals for a long, long time,” Dr. Flansbaum points out. “Now that they’ve opened that up, DNV (Det Norske Veritas Healthcare, Inc.) [for example], can compete with the Joint Commission to certify hospitals.”
What will this mean for hospitals? Probably not much in the short term. “I believe only 15 hospitals have DNV certifications, and that all of those also have a Joint Commission certification,” Dr. Flansbaum says, adding “[DNV and the Joint Commission] have a different approach; it’s like the ACT and the SAT. Both are used for college entrance exams, but the SAT is still mostly the gold standard, like the Joint Commission. But who knows? That could change … and if it does, well, competition is good.”
Some of the MIPPA provisions, such as the quality research initiatives, could end up shaping the future of healthcare. Others, such as the continuation of PQRI, may lead to new payment models for physicians.
Only time will tell which provisions will truly improve efficiency and costs—and which will impact hospital medicine in particular. TH
Jane Jerrard is a medical writer based in Chicago.
Self-Study Suggestions
What are hospitalist leaders reading these days? What books, journals, and Web sites do they turn to—or recommend—for honing management skills, keeping up with industry trends, or generally staying sharp? In the January 2008 issue of The Hospitalist, four hospitalists in management positions shared their picks; here, three other leaders in the industry offer their “recommended reads.”
The President’s Picks
SHM President Patrick Cawley, MD, chief medical officer of the University of South Carolina Medical Center in Charleston, recommends a variety of resources for hospitalists in leadership positions and those who aspire to lead.
You're in Charge, Now What? The 8 Point Plan by Thomas J. Neff and James M. Citrin
“For any leader moving into a new position, this is an invaluable guide for the first six months,” Dr. Cawley says. “It was originally written for CEOs, but it works for any leadership role. Every time I have taken on a new leadership position, I have re-read it and learned something new.”
Competitive Advantage by Michael E. Porter
“This business reference classic details the underpinnings of today’s MBA programs,” Dr. Cawley explains. “The concepts of competitive advantage, value creation, and value chain are absolutes to anyone involved in strategic planning, and certainly for any hospitalist program which requires financial support.”
A Sense of Urgency by John P. Kotter
The newest book by a leading expert in change management, this book focuses on the first step of successful change. “All hospitalists who are interested in improving quality must understand the difference between false urgency and true urgency, since it is key to knowing which events can be used to successfully drive change,” Dr. Cawley states.
Getting Things Done by David Allen
“I’m always on a quest for better personal organization and time management skills,” Dr. Cawley admits. “GTD is one such method. Combine the book with the Microsoft Outlook tips and you’ll never look back.”
Harvard Business Review
“This is one of the few magazines I read cover to cover each month—Harvard Business Review is the business community’s equivalent of the New England Journal of Medicine,” Dr. Cawley says.
Hardwiring Excellence by Quint Studer
“Many hospitals across the nation have engaged the Studer Group to help improve leadership accountability and performance,” Dr. Cawley explains. “This book is the hospital version of Good to Great.”
Dr. Cawley adds, “for something really different … .”
The Prince by Machiavelli and The Politics of Life: 25 Rules for Survival in a Brutal and Manipulative World by Craig Crawford
“For any hospitalist who is part of a larger organization, and certainly for any leader, politics are a constant,” Dr. Cawley points out. “If you’re serious about understanding such motivations, you need to become not only a student of leadership, but one of politics, as well. The place to start is The Prince. Strive for the deeper understanding of Machiavelli and not the often quoted ‘ends justifies the means’ superficiality. Crawford’s book is the modern equivalent.”
A Pediatric Hospitalist Recommends…
Jack Percelay, MD, MPH, FAAP, E.L.M.O. Pediatrics, New York, also serves on SHM’s board of directors. He recommends reading these five resources:
Getting to Yes: Negotiating Agreement Without Giving In by Roger Fisher and William L. Ury
Dr. Percelay calls this book required reading, saying, “This is not new—it’s a core requirement for hospital medicine group leaders, hospitalists, or anyone who needs to negotiate for themselves.”
Hospitalists: A Guide to Building and Sustaining a Successful Program by Joseph A. Miller, John Nelson, MD, and Winthrop F. Whitcomb, MD
“This is a tremendously useful resource, if you’re having problems with your administration—if the C-suite doesn’t really ‘get’ hospitalists,” Dr. Percelay says. “It helps readers understand the philosophy behind a highly successful hospital medicine program. If you were going to convert a hospital executive to hospital medicine with one book, this is the book to give them. It’s very useful to know about for this reason.”
Crucial Conversations: Tools for Talking When Stakes are High and Crucial Confrontations by Kerry Patterson, Joseph Grenny, Ron McMillan and Al Switzler
“These books are more advanced and are targeted for those interested in developing their conflict resolution and leadership skills,” Dr. Percelay says. “They were recommended on the SHM practice management list serve, and they’re for both your personal and your professional life. These are the most useful leadership books I have read this year.”
The Cincinnati Children’s Hospital Pediatric Grand Rounds available at www.cincinnatichildrens. org/ed/cme/streaming-media/library/pgr/default.htm
“This is a pediatrics resource. Cincinnati Children’s Hospital has all of its grand rounds on the Web,” Dr. Percelay says. “For someone like me, who works in a community hospital and doesn’t have access to the latest and greatest research, this site provides free access to cutting edge, high-quality presentations. Some are very relevant to pediatric hospital medicine, and some presentations even offer free continuing medical education. Other hospitals do this, as well, but the Cincinnati site is the most user-friendly site I’ve found.”
Teaching Tools
Sylvia Cheney McKean, MD, medical director, Brigham and Women’s Hospital/Faulkner Hospitalist Service in Boston and SHM board member, uses several resources for dual purposes: to find the latest clinical information and to enhance and support her teaching.
PubMed available at www.ncbi.nlm. nih.gov/pubmed
The U.S. National Library of Medicine and the National Institutes of Health administer the PubMed site, which includes more than 18 million citations from MEDLINE and other life science journals for biomedical articles dating back to the 1950s. The site includes links to full text articles and other related resources.
“I find that most of my reading is through PubMed,” Dr. McKean says. “I get the latest, most up-to-date information. ... I generally proceed by first framing the question that needs to be answered and then looking for the best evidence. The key thing is to ask the right questions.”
American College of Physicians’ Medical Knowledge Self-Assessment Program (MKSAP) is available at www.acponline.org/products_services/ mksap/14.
“I find the ACP’s MKSAP syllabus very helpful for teaching and remaining updated,” Dr. McKean explains. “People use this to study for their boards, but it’s very helpful to teach residents ... and for viewing clinical problems.”
The Journal of Hospital Medicine
“I look at each issue cover to cover,” Dr. McKean says, “because it’s the most relevant journal of any out there. It has new research, professional development articles, and articles based on the Core Competencies of Hospital Medicine.”
SHM online research rooms available at www.hospitalmedicine.org
“SHM provides valuable resources that are being regularly updated for new hospitalists, hospitalist leaders and practicing hospitalists with the Core Competencies in Hospital Medicine as a framework,” Dr. McKean says. “There are new resource rooms coming out all the time, while the old ones are constantly updated. What I find most valuable is the quality improvement primer, a downloadable workbook which crosses all QI topics and gives physicians who have not had training in QI projects a framework to start their own … in their hospital.” TH
Jane Jerrard is a medical writer based in Chicago. She also writes “Public Policy” for The Hospitalist.
What are hospitalist leaders reading these days? What books, journals, and Web sites do they turn to—or recommend—for honing management skills, keeping up with industry trends, or generally staying sharp? In the January 2008 issue of The Hospitalist, four hospitalists in management positions shared their picks; here, three other leaders in the industry offer their “recommended reads.”
The President’s Picks
SHM President Patrick Cawley, MD, chief medical officer of the University of South Carolina Medical Center in Charleston, recommends a variety of resources for hospitalists in leadership positions and those who aspire to lead.
You're in Charge, Now What? The 8 Point Plan by Thomas J. Neff and James M. Citrin
“For any leader moving into a new position, this is an invaluable guide for the first six months,” Dr. Cawley says. “It was originally written for CEOs, but it works for any leadership role. Every time I have taken on a new leadership position, I have re-read it and learned something new.”
Competitive Advantage by Michael E. Porter
“This business reference classic details the underpinnings of today’s MBA programs,” Dr. Cawley explains. “The concepts of competitive advantage, value creation, and value chain are absolutes to anyone involved in strategic planning, and certainly for any hospitalist program which requires financial support.”
A Sense of Urgency by John P. Kotter
The newest book by a leading expert in change management, this book focuses on the first step of successful change. “All hospitalists who are interested in improving quality must understand the difference between false urgency and true urgency, since it is key to knowing which events can be used to successfully drive change,” Dr. Cawley states.
Getting Things Done by David Allen
“I’m always on a quest for better personal organization and time management skills,” Dr. Cawley admits. “GTD is one such method. Combine the book with the Microsoft Outlook tips and you’ll never look back.”
Harvard Business Review
“This is one of the few magazines I read cover to cover each month—Harvard Business Review is the business community’s equivalent of the New England Journal of Medicine,” Dr. Cawley says.
Hardwiring Excellence by Quint Studer
“Many hospitals across the nation have engaged the Studer Group to help improve leadership accountability and performance,” Dr. Cawley explains. “This book is the hospital version of Good to Great.”
Dr. Cawley adds, “for something really different … .”
The Prince by Machiavelli and The Politics of Life: 25 Rules for Survival in a Brutal and Manipulative World by Craig Crawford
“For any hospitalist who is part of a larger organization, and certainly for any leader, politics are a constant,” Dr. Cawley points out. “If you’re serious about understanding such motivations, you need to become not only a student of leadership, but one of politics, as well. The place to start is The Prince. Strive for the deeper understanding of Machiavelli and not the often quoted ‘ends justifies the means’ superficiality. Crawford’s book is the modern equivalent.”
A Pediatric Hospitalist Recommends…
Jack Percelay, MD, MPH, FAAP, E.L.M.O. Pediatrics, New York, also serves on SHM’s board of directors. He recommends reading these five resources:
Getting to Yes: Negotiating Agreement Without Giving In by Roger Fisher and William L. Ury
Dr. Percelay calls this book required reading, saying, “This is not new—it’s a core requirement for hospital medicine group leaders, hospitalists, or anyone who needs to negotiate for themselves.”
Hospitalists: A Guide to Building and Sustaining a Successful Program by Joseph A. Miller, John Nelson, MD, and Winthrop F. Whitcomb, MD
“This is a tremendously useful resource, if you’re having problems with your administration—if the C-suite doesn’t really ‘get’ hospitalists,” Dr. Percelay says. “It helps readers understand the philosophy behind a highly successful hospital medicine program. If you were going to convert a hospital executive to hospital medicine with one book, this is the book to give them. It’s very useful to know about for this reason.”
Crucial Conversations: Tools for Talking When Stakes are High and Crucial Confrontations by Kerry Patterson, Joseph Grenny, Ron McMillan and Al Switzler
“These books are more advanced and are targeted for those interested in developing their conflict resolution and leadership skills,” Dr. Percelay says. “They were recommended on the SHM practice management list serve, and they’re for both your personal and your professional life. These are the most useful leadership books I have read this year.”
The Cincinnati Children’s Hospital Pediatric Grand Rounds available at www.cincinnatichildrens. org/ed/cme/streaming-media/library/pgr/default.htm
“This is a pediatrics resource. Cincinnati Children’s Hospital has all of its grand rounds on the Web,” Dr. Percelay says. “For someone like me, who works in a community hospital and doesn’t have access to the latest and greatest research, this site provides free access to cutting edge, high-quality presentations. Some are very relevant to pediatric hospital medicine, and some presentations even offer free continuing medical education. Other hospitals do this, as well, but the Cincinnati site is the most user-friendly site I’ve found.”
Teaching Tools
Sylvia Cheney McKean, MD, medical director, Brigham and Women’s Hospital/Faulkner Hospitalist Service in Boston and SHM board member, uses several resources for dual purposes: to find the latest clinical information and to enhance and support her teaching.
PubMed available at www.ncbi.nlm. nih.gov/pubmed
The U.S. National Library of Medicine and the National Institutes of Health administer the PubMed site, which includes more than 18 million citations from MEDLINE and other life science journals for biomedical articles dating back to the 1950s. The site includes links to full text articles and other related resources.
“I find that most of my reading is through PubMed,” Dr. McKean says. “I get the latest, most up-to-date information. ... I generally proceed by first framing the question that needs to be answered and then looking for the best evidence. The key thing is to ask the right questions.”
American College of Physicians’ Medical Knowledge Self-Assessment Program (MKSAP) is available at www.acponline.org/products_services/ mksap/14.
“I find the ACP’s MKSAP syllabus very helpful for teaching and remaining updated,” Dr. McKean explains. “People use this to study for their boards, but it’s very helpful to teach residents ... and for viewing clinical problems.”
The Journal of Hospital Medicine
“I look at each issue cover to cover,” Dr. McKean says, “because it’s the most relevant journal of any out there. It has new research, professional development articles, and articles based on the Core Competencies of Hospital Medicine.”
SHM online research rooms available at www.hospitalmedicine.org
“SHM provides valuable resources that are being regularly updated for new hospitalists, hospitalist leaders and practicing hospitalists with the Core Competencies in Hospital Medicine as a framework,” Dr. McKean says. “There are new resource rooms coming out all the time, while the old ones are constantly updated. What I find most valuable is the quality improvement primer, a downloadable workbook which crosses all QI topics and gives physicians who have not had training in QI projects a framework to start their own … in their hospital.” TH
Jane Jerrard is a medical writer based in Chicago. She also writes “Public Policy” for The Hospitalist.
What are hospitalist leaders reading these days? What books, journals, and Web sites do they turn to—or recommend—for honing management skills, keeping up with industry trends, or generally staying sharp? In the January 2008 issue of The Hospitalist, four hospitalists in management positions shared their picks; here, three other leaders in the industry offer their “recommended reads.”
The President’s Picks
SHM President Patrick Cawley, MD, chief medical officer of the University of South Carolina Medical Center in Charleston, recommends a variety of resources for hospitalists in leadership positions and those who aspire to lead.
You're in Charge, Now What? The 8 Point Plan by Thomas J. Neff and James M. Citrin
“For any leader moving into a new position, this is an invaluable guide for the first six months,” Dr. Cawley says. “It was originally written for CEOs, but it works for any leadership role. Every time I have taken on a new leadership position, I have re-read it and learned something new.”
Competitive Advantage by Michael E. Porter
“This business reference classic details the underpinnings of today’s MBA programs,” Dr. Cawley explains. “The concepts of competitive advantage, value creation, and value chain are absolutes to anyone involved in strategic planning, and certainly for any hospitalist program which requires financial support.”
A Sense of Urgency by John P. Kotter
The newest book by a leading expert in change management, this book focuses on the first step of successful change. “All hospitalists who are interested in improving quality must understand the difference between false urgency and true urgency, since it is key to knowing which events can be used to successfully drive change,” Dr. Cawley states.
Getting Things Done by David Allen
“I’m always on a quest for better personal organization and time management skills,” Dr. Cawley admits. “GTD is one such method. Combine the book with the Microsoft Outlook tips and you’ll never look back.”
Harvard Business Review
“This is one of the few magazines I read cover to cover each month—Harvard Business Review is the business community’s equivalent of the New England Journal of Medicine,” Dr. Cawley says.
Hardwiring Excellence by Quint Studer
“Many hospitals across the nation have engaged the Studer Group to help improve leadership accountability and performance,” Dr. Cawley explains. “This book is the hospital version of Good to Great.”
Dr. Cawley adds, “for something really different … .”
The Prince by Machiavelli and The Politics of Life: 25 Rules for Survival in a Brutal and Manipulative World by Craig Crawford
“For any hospitalist who is part of a larger organization, and certainly for any leader, politics are a constant,” Dr. Cawley points out. “If you’re serious about understanding such motivations, you need to become not only a student of leadership, but one of politics, as well. The place to start is The Prince. Strive for the deeper understanding of Machiavelli and not the often quoted ‘ends justifies the means’ superficiality. Crawford’s book is the modern equivalent.”
A Pediatric Hospitalist Recommends…
Jack Percelay, MD, MPH, FAAP, E.L.M.O. Pediatrics, New York, also serves on SHM’s board of directors. He recommends reading these five resources:
Getting to Yes: Negotiating Agreement Without Giving In by Roger Fisher and William L. Ury
Dr. Percelay calls this book required reading, saying, “This is not new—it’s a core requirement for hospital medicine group leaders, hospitalists, or anyone who needs to negotiate for themselves.”
Hospitalists: A Guide to Building and Sustaining a Successful Program by Joseph A. Miller, John Nelson, MD, and Winthrop F. Whitcomb, MD
“This is a tremendously useful resource, if you’re having problems with your administration—if the C-suite doesn’t really ‘get’ hospitalists,” Dr. Percelay says. “It helps readers understand the philosophy behind a highly successful hospital medicine program. If you were going to convert a hospital executive to hospital medicine with one book, this is the book to give them. It’s very useful to know about for this reason.”
Crucial Conversations: Tools for Talking When Stakes are High and Crucial Confrontations by Kerry Patterson, Joseph Grenny, Ron McMillan and Al Switzler
“These books are more advanced and are targeted for those interested in developing their conflict resolution and leadership skills,” Dr. Percelay says. “They were recommended on the SHM practice management list serve, and they’re for both your personal and your professional life. These are the most useful leadership books I have read this year.”
The Cincinnati Children’s Hospital Pediatric Grand Rounds available at www.cincinnatichildrens. org/ed/cme/streaming-media/library/pgr/default.htm
“This is a pediatrics resource. Cincinnati Children’s Hospital has all of its grand rounds on the Web,” Dr. Percelay says. “For someone like me, who works in a community hospital and doesn’t have access to the latest and greatest research, this site provides free access to cutting edge, high-quality presentations. Some are very relevant to pediatric hospital medicine, and some presentations even offer free continuing medical education. Other hospitals do this, as well, but the Cincinnati site is the most user-friendly site I’ve found.”
Teaching Tools
Sylvia Cheney McKean, MD, medical director, Brigham and Women’s Hospital/Faulkner Hospitalist Service in Boston and SHM board member, uses several resources for dual purposes: to find the latest clinical information and to enhance and support her teaching.
PubMed available at www.ncbi.nlm. nih.gov/pubmed
The U.S. National Library of Medicine and the National Institutes of Health administer the PubMed site, which includes more than 18 million citations from MEDLINE and other life science journals for biomedical articles dating back to the 1950s. The site includes links to full text articles and other related resources.
“I find that most of my reading is through PubMed,” Dr. McKean says. “I get the latest, most up-to-date information. ... I generally proceed by first framing the question that needs to be answered and then looking for the best evidence. The key thing is to ask the right questions.”
American College of Physicians’ Medical Knowledge Self-Assessment Program (MKSAP) is available at www.acponline.org/products_services/ mksap/14.
“I find the ACP’s MKSAP syllabus very helpful for teaching and remaining updated,” Dr. McKean explains. “People use this to study for their boards, but it’s very helpful to teach residents ... and for viewing clinical problems.”
The Journal of Hospital Medicine
“I look at each issue cover to cover,” Dr. McKean says, “because it’s the most relevant journal of any out there. It has new research, professional development articles, and articles based on the Core Competencies of Hospital Medicine.”
SHM online research rooms available at www.hospitalmedicine.org
“SHM provides valuable resources that are being regularly updated for new hospitalists, hospitalist leaders and practicing hospitalists with the Core Competencies in Hospital Medicine as a framework,” Dr. McKean says. “There are new resource rooms coming out all the time, while the old ones are constantly updated. What I find most valuable is the quality improvement primer, a downloadable workbook which crosses all QI topics and gives physicians who have not had training in QI projects a framework to start their own … in their hospital.” TH
Jane Jerrard is a medical writer based in Chicago. She also writes “Public Policy” for The Hospitalist.
The Art of Negotiation
Got a job offer? Congratulations! The hard part of finding your first job after residency is complete. This also is a time to sit down and think about what’s important to you, as you want the details of your job to be stated in a contract. Here are some tips about contract negotiation.
Get It in Writing
Just as in practice, where we are always told, “it didn’t happen if it’s not documented in the chart,” the same holds true for your workplace contract. This is the time to prioritize what elements are important to you in order to have a satisfying and rewarding career, both professionally and financially. If a particular aspect of your employment agreement is important to you, be it salary, schedule, or malpractice insurance coverage, be sure its stated in writing in your contract. Verbal statements from your employer, such as “we’ll discuss this after you start your job,” should raise a red flag.
Know What Is Negotiable
Some residents are relieved just to secure their first job offer and they immediately accept the initial offer as-is, without attempting to negotiate. Although it’s probably unreasonable to negotiate everything, after you read the initial contract, if anything important is not to your satisfaction, it is practical to have a discussion with your employer. Employers expect this of their hires and, if done politely and professionally, this is a time to build bridges with your future supervisor. Moreover, they begin to better understand your needs and you theirs.
You may find it helpful to talk to associates in the group about what parts of their contracts were negotiable. For example, particularly in academic settings, you may find salary and benefits are not negotiable; however, other benefits, such as office space or protected research time, may be negotiable. Basically, the best time to negotiate is the “honeymoon” period, right after a job offer has been made, as the employer will be doing its best to entice a prospective employee.
Consider a Legal Opinion
In general, the more complex your contract, the more important it will be to solicit the help of an attorney experienced in healthcare. Even if your contract is very simple, contains a standardized salary and benefit structure, has no restrictive covenants, and partnership is not an issue, it may be helpful to have your contract reviewed by an attorney. Understand what is written in your contract and, if there is any doubt, hire a lawyer.
Ultimately, you will be signing the contract, not your lawyer, so be sure you understand what is in it and don’t get mired in “legalese.” Some firms offer third-party contract negotiation; they will assign an attorney to step in as an intermediary. Then again, most experts recommend against hiring a third-party negotiator, as this may increase the distance between you and your employer at a time probably best spent getting to know each other.
Maintain a Keen Eye
Specifics to look for in your new contract:
Work requirements. The employment agreement should visibly define your job responsibilities. Things to look for in your contract include the obligations of the physician, number of shifts or hours or weeks per year you are expected to work, call responsibilities, a census cap (if applicable), allotted vacation time, and continuing medical education time.
Compensation. The contract clearly should delineate how you will be paid. Some hospitalists are compensated solely via a salary; others are paid based on billing/productivity, while the majority are paid based on a combination of these methods (a base salary plus incentives). Be sure you understand the incentive and/or bonus structure of your salary. Practices basing incentives on physician productivity will incorporate your own billing practices and often is measured in relative value units (RVUs). In some settings, group incentives are based on quality targets set by the administration, such as the Joint Commission on the Accreditation of Healthcare Organi-zations (JCAHO) core measure compliance, dictation timeliness, or patient/primary care physician satisfaction.
Benefits. In addition to your salary, you should see that your benefits are spelled out. The obvious benefits include medical, dental, and vision insurance, as well as a retirement savings plan. As discussed in the July 2008 issue of The Hospitalist, as demand for hospitalists continues to exceed supply, look for signing bonuses, coverage of relocation expenses, and the possibility of student loan payoff. Other important benefits include coverage of professional dues, CME allocation, and licensing and board examination fees.
Malpractice Insurance. This can be a complicated topic. In general, there are two major classes of malpractice insurance: an occurrence policy and a claims-made policy. In respect to an occurrence policy, any malpractice incident arising while the coverage was in place, regardless of when the claim was filed, will be covered even after you have stopped practicing under that policy. A claims-made policy, on the other hand, protects physicians for any covered claim, if they are insured when the claim is made. It does not cover malpractice claims filed after the physician cancels the malpractice policy, even if the claim is about an event that occurred while the physician was insured.
If you are offered a claims-made policy, require your employer to add tail coverage, which covers you after leaving the practice for any events occurred during employment. If you are unclear about any part of the group’s malpractice coverage, consider seeking legal advice.
Restrictive covenants. These are non-compete clauses often setting geographic and time restrictions of where and when a physician can practice in the event they leave the group. Though you never know what the future holds, this becomes relevant if you were to change jobs and work at an adjacent local facility or one in a nearby county. In general, hospitalists rarely carry a panel of patients, so an employer probably should not be concerned about hospitalists taking patients with them if/when they leave the practice. Be cautious of restrictive covenants found in your contract.
Ownership/Partnership. In some private groups, partnership will be offered after a preliminary employment period, usually one to two years. Look for your contract to state when and how partnership might be offered, and what the criteria to join are. This also is the time to ask others in the group to get a sense of how many associates are offered partnership and when this might happen.
Allowable Activities. Look for any restrictions regarding your activities outside normal clinical duties, such as teaching, research, or consulting for other firms. If such restrictions are in your contract, there may be specifications about whether income from such activities is yours or whether it is shared with the rest of the practice. TH
Bryan Huang, MD, assistant clinical professor, division of hospital medicine, University of California-San Diego Department of Medicine, Bhavin Patel, MD, hospitalist at Regions Hospital, HealthPartners Medical Group, St. Paul, Minn., Bijo Chacko, MD, hospitalist program medical director, Preferred Health Partners, New York City, and chair of SHM’s Young Physician Committee.
Got a job offer? Congratulations! The hard part of finding your first job after residency is complete. This also is a time to sit down and think about what’s important to you, as you want the details of your job to be stated in a contract. Here are some tips about contract negotiation.
Get It in Writing
Just as in practice, where we are always told, “it didn’t happen if it’s not documented in the chart,” the same holds true for your workplace contract. This is the time to prioritize what elements are important to you in order to have a satisfying and rewarding career, both professionally and financially. If a particular aspect of your employment agreement is important to you, be it salary, schedule, or malpractice insurance coverage, be sure its stated in writing in your contract. Verbal statements from your employer, such as “we’ll discuss this after you start your job,” should raise a red flag.
Know What Is Negotiable
Some residents are relieved just to secure their first job offer and they immediately accept the initial offer as-is, without attempting to negotiate. Although it’s probably unreasonable to negotiate everything, after you read the initial contract, if anything important is not to your satisfaction, it is practical to have a discussion with your employer. Employers expect this of their hires and, if done politely and professionally, this is a time to build bridges with your future supervisor. Moreover, they begin to better understand your needs and you theirs.
You may find it helpful to talk to associates in the group about what parts of their contracts were negotiable. For example, particularly in academic settings, you may find salary and benefits are not negotiable; however, other benefits, such as office space or protected research time, may be negotiable. Basically, the best time to negotiate is the “honeymoon” period, right after a job offer has been made, as the employer will be doing its best to entice a prospective employee.
Consider a Legal Opinion
In general, the more complex your contract, the more important it will be to solicit the help of an attorney experienced in healthcare. Even if your contract is very simple, contains a standardized salary and benefit structure, has no restrictive covenants, and partnership is not an issue, it may be helpful to have your contract reviewed by an attorney. Understand what is written in your contract and, if there is any doubt, hire a lawyer.
Ultimately, you will be signing the contract, not your lawyer, so be sure you understand what is in it and don’t get mired in “legalese.” Some firms offer third-party contract negotiation; they will assign an attorney to step in as an intermediary. Then again, most experts recommend against hiring a third-party negotiator, as this may increase the distance between you and your employer at a time probably best spent getting to know each other.
Maintain a Keen Eye
Specifics to look for in your new contract:
Work requirements. The employment agreement should visibly define your job responsibilities. Things to look for in your contract include the obligations of the physician, number of shifts or hours or weeks per year you are expected to work, call responsibilities, a census cap (if applicable), allotted vacation time, and continuing medical education time.
Compensation. The contract clearly should delineate how you will be paid. Some hospitalists are compensated solely via a salary; others are paid based on billing/productivity, while the majority are paid based on a combination of these methods (a base salary plus incentives). Be sure you understand the incentive and/or bonus structure of your salary. Practices basing incentives on physician productivity will incorporate your own billing practices and often is measured in relative value units (RVUs). In some settings, group incentives are based on quality targets set by the administration, such as the Joint Commission on the Accreditation of Healthcare Organi-zations (JCAHO) core measure compliance, dictation timeliness, or patient/primary care physician satisfaction.
Benefits. In addition to your salary, you should see that your benefits are spelled out. The obvious benefits include medical, dental, and vision insurance, as well as a retirement savings plan. As discussed in the July 2008 issue of The Hospitalist, as demand for hospitalists continues to exceed supply, look for signing bonuses, coverage of relocation expenses, and the possibility of student loan payoff. Other important benefits include coverage of professional dues, CME allocation, and licensing and board examination fees.
Malpractice Insurance. This can be a complicated topic. In general, there are two major classes of malpractice insurance: an occurrence policy and a claims-made policy. In respect to an occurrence policy, any malpractice incident arising while the coverage was in place, regardless of when the claim was filed, will be covered even after you have stopped practicing under that policy. A claims-made policy, on the other hand, protects physicians for any covered claim, if they are insured when the claim is made. It does not cover malpractice claims filed after the physician cancels the malpractice policy, even if the claim is about an event that occurred while the physician was insured.
If you are offered a claims-made policy, require your employer to add tail coverage, which covers you after leaving the practice for any events occurred during employment. If you are unclear about any part of the group’s malpractice coverage, consider seeking legal advice.
Restrictive covenants. These are non-compete clauses often setting geographic and time restrictions of where and when a physician can practice in the event they leave the group. Though you never know what the future holds, this becomes relevant if you were to change jobs and work at an adjacent local facility or one in a nearby county. In general, hospitalists rarely carry a panel of patients, so an employer probably should not be concerned about hospitalists taking patients with them if/when they leave the practice. Be cautious of restrictive covenants found in your contract.
Ownership/Partnership. In some private groups, partnership will be offered after a preliminary employment period, usually one to two years. Look for your contract to state when and how partnership might be offered, and what the criteria to join are. This also is the time to ask others in the group to get a sense of how many associates are offered partnership and when this might happen.
Allowable Activities. Look for any restrictions regarding your activities outside normal clinical duties, such as teaching, research, or consulting for other firms. If such restrictions are in your contract, there may be specifications about whether income from such activities is yours or whether it is shared with the rest of the practice. TH
Bryan Huang, MD, assistant clinical professor, division of hospital medicine, University of California-San Diego Department of Medicine, Bhavin Patel, MD, hospitalist at Regions Hospital, HealthPartners Medical Group, St. Paul, Minn., Bijo Chacko, MD, hospitalist program medical director, Preferred Health Partners, New York City, and chair of SHM’s Young Physician Committee.
Got a job offer? Congratulations! The hard part of finding your first job after residency is complete. This also is a time to sit down and think about what’s important to you, as you want the details of your job to be stated in a contract. Here are some tips about contract negotiation.
Get It in Writing
Just as in practice, where we are always told, “it didn’t happen if it’s not documented in the chart,” the same holds true for your workplace contract. This is the time to prioritize what elements are important to you in order to have a satisfying and rewarding career, both professionally and financially. If a particular aspect of your employment agreement is important to you, be it salary, schedule, or malpractice insurance coverage, be sure its stated in writing in your contract. Verbal statements from your employer, such as “we’ll discuss this after you start your job,” should raise a red flag.
Know What Is Negotiable
Some residents are relieved just to secure their first job offer and they immediately accept the initial offer as-is, without attempting to negotiate. Although it’s probably unreasonable to negotiate everything, after you read the initial contract, if anything important is not to your satisfaction, it is practical to have a discussion with your employer. Employers expect this of their hires and, if done politely and professionally, this is a time to build bridges with your future supervisor. Moreover, they begin to better understand your needs and you theirs.
You may find it helpful to talk to associates in the group about what parts of their contracts were negotiable. For example, particularly in academic settings, you may find salary and benefits are not negotiable; however, other benefits, such as office space or protected research time, may be negotiable. Basically, the best time to negotiate is the “honeymoon” period, right after a job offer has been made, as the employer will be doing its best to entice a prospective employee.
Consider a Legal Opinion
In general, the more complex your contract, the more important it will be to solicit the help of an attorney experienced in healthcare. Even if your contract is very simple, contains a standardized salary and benefit structure, has no restrictive covenants, and partnership is not an issue, it may be helpful to have your contract reviewed by an attorney. Understand what is written in your contract and, if there is any doubt, hire a lawyer.
Ultimately, you will be signing the contract, not your lawyer, so be sure you understand what is in it and don’t get mired in “legalese.” Some firms offer third-party contract negotiation; they will assign an attorney to step in as an intermediary. Then again, most experts recommend against hiring a third-party negotiator, as this may increase the distance between you and your employer at a time probably best spent getting to know each other.
Maintain a Keen Eye
Specifics to look for in your new contract:
Work requirements. The employment agreement should visibly define your job responsibilities. Things to look for in your contract include the obligations of the physician, number of shifts or hours or weeks per year you are expected to work, call responsibilities, a census cap (if applicable), allotted vacation time, and continuing medical education time.
Compensation. The contract clearly should delineate how you will be paid. Some hospitalists are compensated solely via a salary; others are paid based on billing/productivity, while the majority are paid based on a combination of these methods (a base salary plus incentives). Be sure you understand the incentive and/or bonus structure of your salary. Practices basing incentives on physician productivity will incorporate your own billing practices and often is measured in relative value units (RVUs). In some settings, group incentives are based on quality targets set by the administration, such as the Joint Commission on the Accreditation of Healthcare Organi-zations (JCAHO) core measure compliance, dictation timeliness, or patient/primary care physician satisfaction.
Benefits. In addition to your salary, you should see that your benefits are spelled out. The obvious benefits include medical, dental, and vision insurance, as well as a retirement savings plan. As discussed in the July 2008 issue of The Hospitalist, as demand for hospitalists continues to exceed supply, look for signing bonuses, coverage of relocation expenses, and the possibility of student loan payoff. Other important benefits include coverage of professional dues, CME allocation, and licensing and board examination fees.
Malpractice Insurance. This can be a complicated topic. In general, there are two major classes of malpractice insurance: an occurrence policy and a claims-made policy. In respect to an occurrence policy, any malpractice incident arising while the coverage was in place, regardless of when the claim was filed, will be covered even after you have stopped practicing under that policy. A claims-made policy, on the other hand, protects physicians for any covered claim, if they are insured when the claim is made. It does not cover malpractice claims filed after the physician cancels the malpractice policy, even if the claim is about an event that occurred while the physician was insured.
If you are offered a claims-made policy, require your employer to add tail coverage, which covers you after leaving the practice for any events occurred during employment. If you are unclear about any part of the group’s malpractice coverage, consider seeking legal advice.
Restrictive covenants. These are non-compete clauses often setting geographic and time restrictions of where and when a physician can practice in the event they leave the group. Though you never know what the future holds, this becomes relevant if you were to change jobs and work at an adjacent local facility or one in a nearby county. In general, hospitalists rarely carry a panel of patients, so an employer probably should not be concerned about hospitalists taking patients with them if/when they leave the practice. Be cautious of restrictive covenants found in your contract.
Ownership/Partnership. In some private groups, partnership will be offered after a preliminary employment period, usually one to two years. Look for your contract to state when and how partnership might be offered, and what the criteria to join are. This also is the time to ask others in the group to get a sense of how many associates are offered partnership and when this might happen.
Allowable Activities. Look for any restrictions regarding your activities outside normal clinical duties, such as teaching, research, or consulting for other firms. If such restrictions are in your contract, there may be specifications about whether income from such activities is yours or whether it is shared with the rest of the practice. TH
Bryan Huang, MD, assistant clinical professor, division of hospital medicine, University of California-San Diego Department of Medicine, Bhavin Patel, MD, hospitalist at Regions Hospital, HealthPartners Medical Group, St. Paul, Minn., Bijo Chacko, MD, hospitalist program medical director, Preferred Health Partners, New York City, and chair of SHM’s Young Physician Committee.