User login
THE CASE
A 24-year-old man with a history of smoking tobacco presented to the hospital with acute-onset chest tightness and dyspnea shortly after smoking cannabis. He was otherwise healthy and hemodynamically stable upon arrival to the emergency department. An electrocardiogram (EKG) was obtained.
THE DIAGNOSIS
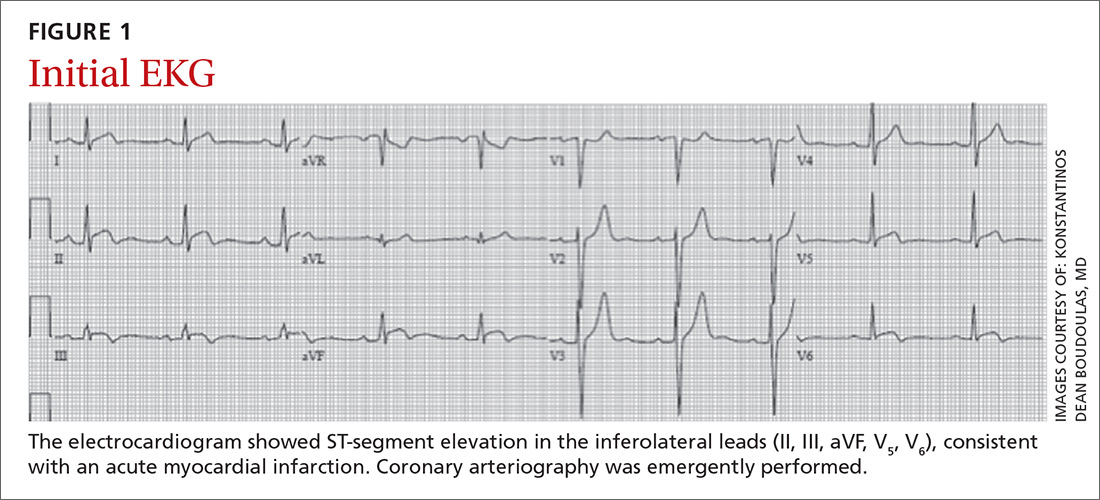
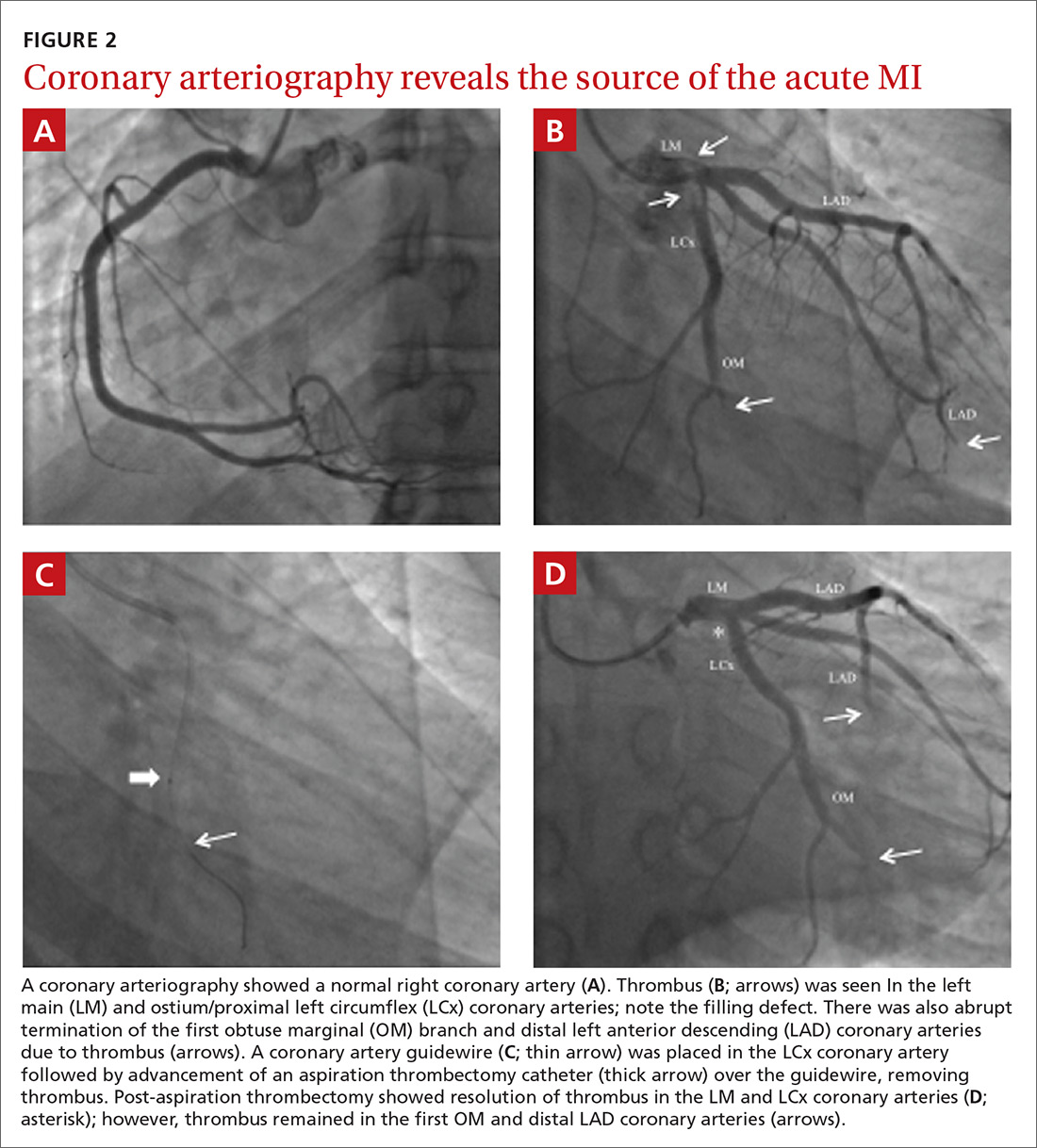
The EKG showed ST-segment elevation in the inferolateral leads, consistent with an acute myocardial infarction (AMI) (FIGURE 1). The patient was immediately transported to the cardiac catheterization laboratory, where coronary arteriography demonstrated a normal right coronary artery (FIGURE 2A). Diffuse thrombosis without atherosclerosis was seen throughout the left coronary arteries, including the left main artery, distal left anterior descending (LAD) artery, first diagonal branch of the LAD artery, ostial and proximal left circumflex (LCx) arteries, and first obtuse marginal (OM) branch of the LCx artery (FIGURE 2B).
DISCUSSION
The most common cause of AMI is underlying coronary atherosclerosis;1 however, AMI may occur due to in-situ thrombosis, thromboembolism, or coronary artery vasospasm, especially due to cocaine or other substance abuse. Occasionally, coronary arteries may be damaged due to viral myocarditis, autoimmune vasculitis, dissection of the ascending aorta, or dissection of a coronary artery, especially during pregnancy and postpartum.2,3
Cannabis and tobacco increase cardiovascular events
Smoking cannabis has been shown to increase adrenergic activity, resulting in an increased heart rate and elevated arterial pressure.4,5 These changes may increase myocardial oxygen demand and may result in a decrease in myocardial oxygen supply due to a decrease in the diastolic time.6 Smoking cannabis can also increase carboxyhemoglobin levels, which may compromise tissue oxygenation.
The risk for AMI has been shown to increase within the first hour of smoking cannabis.5 A few reports have documented cases of acute coronary syndrome following cannabis use; the majority of affected patients presented with chest pain within hours of smoking cannabis and were found to have a thrombus in a coronary artery, which was then treated medically or with percutaneous coronary intervention.7 Rare cases of cardiovascular death following cannabis use have also been reported.7,8
It has been suggested that coronary artery vasospasm may occur from cannabis use, which may precipitate thrombosis; however, this is not well defined.9 It is not clear if vasospasm was the inciting factor for thrombus formation in this case, as there was extensive and diffuse thrombus far greater than that expected solely from coronary artery vasospasm.
Continue to: AMI without atherosclerosis? Consider thrombosis
AMI without atherosclerosis? Consider thrombosis
In-situ coronary thrombosis should be considered in the differential diagnosis of a patient with an AMI without evidence of coronary atherosclerosis. Further, smoking cannabis immediately prior to symptom onset should heighten awareness for potential coronary thrombosis. Lifelong anticoagulation therapy may be indicated in these patients due to the catastrophic nature of the condition and limited data on this particular situation.
What’s recommended. Cessation of cannabis and tobacco smoking is recommended, as the use of these substances may contribute to the development of coronary thrombosis.3-7,9 A registry of patients with coronary thrombosis without coronary atherosclerosis, especially in states where cannabis is legal, would be useful to gauge the potential increase in such events. In addition, information related to the cardiovascular effects of using alternate routes of drug delivery, such as vaping devices, are limited; therefore, this practice should be closely monitored, as well.
Our patient’s outcome
Thrombus removal. In the cardiac catheterization laboratory, the majority of the thrombus was removed and coronary blood flow was improved using a thrombectomy catheter (FIGURE 2C). Residual thrombus remained in the very distal coronary arteries (FIGURE 2D), so heparin infusion was continued.
Imaging studies. Following the procedure, an echocardiogram demonstrated left ventricular (LV) regional wall motion abnormalities with moderately reduced LV systolic function and an ejection fraction (EF) of 35%. Troponin I levels peaked at 35 ng/mL. No LV apical thrombus or intracardiac defects (eg, patent foramen ovale, atrial septal defect, ventricular septal defect) that might have contributed to thromboembolism or paradoxical embolus were seen on echocardiogram or cardiac magnetic resonance imaging. In addition, ultrasound of the lower extremities did not demonstrate deep venous thrombosis.
Continue to: A toxicology screen
A toxicology screen was positive for tetrahydrocannabinol (THC) and negative for other substances. Hypercoagulable laboratory studies were normal, including anticardiolipin antibody IgG and IgM, factor V Leiden, prothrombin G20210A mutation, thrombin time, antithrombin III, and protein C and S activity. It was therefore believed that the AMI was due to in-situ coronary artery thrombus formation precipitated acutely by smoking cannabis—possibly with an underlying hypercoagulable state, even though no laboratory abnormalities were detected.
Our patient was discharged on lifelong aspirin 81 mg/d and oral rivaroxaban (maintenance dose of 20 mg/d). Metoprolol succinate 12.5 mg/d and lisinopril 2.5 mg/d were also initiated due
THE TAKEWAY
Coronary thrombosis can result in an AMI, even without underlying coronary atherosclerosis. Smoking cannabis may predispose individuals to in-situ coronary thrombosis and subsequent AMI. Although not often encountered in clinical practice, providers must be aware of this phenomenon in the differential diagnosis for AMI—particularly in young patients without traditional risk factors.
CORRESPONDENCE
Konstantinos Dean Boudoulas, MD, The Ohio State University Davis Lung and Heart Research Institute, 473 W. 12th Avenue, Suite 200, Columbus, Ohio 43210; kdboudoulas@osumc.edu
1. Davies MJ, Woolf N, Robertson WB. Pathology of acute myocardial infarction with particular reference to occlusive coronary thrombi. Br Heart J. 1976;38:659-664.
2. Pasupathy S, Air T, Dreyer RP, et al. Systematic review of patients presenting with suspected myocardial infarction and nonobstructive coronary arteries. Circulation. 2015;131:861-870.
3. Sharifi M, Frolich TG, Silverman IM. Myocardial infarction with angiographically normal coronary arteries. Chest. 1995;107:36-40.
4. Tatli E, Yilmaztepe M, Altun G, et al. Cannabis-induced coronary artery thrombosis and acute anterior myocardial infarction in a young man. Int J Cardiol. 2007;120:420-422.
5. Mittleman MA, Lewis RA, Maclure M, et al. Triggering myocardial infarction by marijuana. Circulation. 2001;103:2805-2809.
6. Boudoulas KD, Borer JS, Boudoulas H. Heart rate, life expectancy and the cardiovascular system: therapeutic considerations. Cardiology. 2015;132:199-212.
7. Yurtdas M, Aydın MK. Acute myocardial infarction in a young man; fatal blow of the marijuana: a case report. Korean Circ J. 2012;42:641-645.
8. Jouanjus E, Lapeyre-Mestre M, Micallef J; French Association of the Regional Abuse and Dependence Monitoring Centres (CEIP-A) Working Group on Cannabis Complications. Cannabis use: signal of increasing risk of serious cardiovascular disorders. J Am Heart Assoc. 2014;3:e000638.
9. Hodcroft CJ, Rossiter MC, Buch AN. Cannabis-associated myocardial infarction in a young man with normal coronary arteries. J Emerg Med. 2014;47:277-281.
THE CASE
A 24-year-old man with a history of smoking tobacco presented to the hospital with acute-onset chest tightness and dyspnea shortly after smoking cannabis. He was otherwise healthy and hemodynamically stable upon arrival to the emergency department. An electrocardiogram (EKG) was obtained.
THE DIAGNOSIS
The EKG showed ST-segment elevation in the inferolateral leads, consistent with an acute myocardial infarction (AMI) (FIGURE 1). The patient was immediately transported to the cardiac catheterization laboratory, where coronary arteriography demonstrated a normal right coronary artery (FIGURE 2A). Diffuse thrombosis without atherosclerosis was seen throughout the left coronary arteries, including the left main artery, distal left anterior descending (LAD) artery, first diagonal branch of the LAD artery, ostial and proximal left circumflex (LCx) arteries, and first obtuse marginal (OM) branch of the LCx artery (FIGURE 2B).
DISCUSSION
The most common cause of AMI is underlying coronary atherosclerosis;1 however, AMI may occur due to in-situ thrombosis, thromboembolism, or coronary artery vasospasm, especially due to cocaine or other substance abuse. Occasionally, coronary arteries may be damaged due to viral myocarditis, autoimmune vasculitis, dissection of the ascending aorta, or dissection of a coronary artery, especially during pregnancy and postpartum.2,3
Cannabis and tobacco increase cardiovascular events
Smoking cannabis has been shown to increase adrenergic activity, resulting in an increased heart rate and elevated arterial pressure.4,5 These changes may increase myocardial oxygen demand and may result in a decrease in myocardial oxygen supply due to a decrease in the diastolic time.6 Smoking cannabis can also increase carboxyhemoglobin levels, which may compromise tissue oxygenation.
The risk for AMI has been shown to increase within the first hour of smoking cannabis.5 A few reports have documented cases of acute coronary syndrome following cannabis use; the majority of affected patients presented with chest pain within hours of smoking cannabis and were found to have a thrombus in a coronary artery, which was then treated medically or with percutaneous coronary intervention.7 Rare cases of cardiovascular death following cannabis use have also been reported.7,8
It has been suggested that coronary artery vasospasm may occur from cannabis use, which may precipitate thrombosis; however, this is not well defined.9 It is not clear if vasospasm was the inciting factor for thrombus formation in this case, as there was extensive and diffuse thrombus far greater than that expected solely from coronary artery vasospasm.
Continue to: AMI without atherosclerosis? Consider thrombosis
AMI without atherosclerosis? Consider thrombosis
In-situ coronary thrombosis should be considered in the differential diagnosis of a patient with an AMI without evidence of coronary atherosclerosis. Further, smoking cannabis immediately prior to symptom onset should heighten awareness for potential coronary thrombosis. Lifelong anticoagulation therapy may be indicated in these patients due to the catastrophic nature of the condition and limited data on this particular situation.
What’s recommended. Cessation of cannabis and tobacco smoking is recommended, as the use of these substances may contribute to the development of coronary thrombosis.3-7,9 A registry of patients with coronary thrombosis without coronary atherosclerosis, especially in states where cannabis is legal, would be useful to gauge the potential increase in such events. In addition, information related to the cardiovascular effects of using alternate routes of drug delivery, such as vaping devices, are limited; therefore, this practice should be closely monitored, as well.
Our patient’s outcome
Thrombus removal. In the cardiac catheterization laboratory, the majority of the thrombus was removed and coronary blood flow was improved using a thrombectomy catheter (FIGURE 2C). Residual thrombus remained in the very distal coronary arteries (FIGURE 2D), so heparin infusion was continued.
Imaging studies. Following the procedure, an echocardiogram demonstrated left ventricular (LV) regional wall motion abnormalities with moderately reduced LV systolic function and an ejection fraction (EF) of 35%. Troponin I levels peaked at 35 ng/mL. No LV apical thrombus or intracardiac defects (eg, patent foramen ovale, atrial septal defect, ventricular septal defect) that might have contributed to thromboembolism or paradoxical embolus were seen on echocardiogram or cardiac magnetic resonance imaging. In addition, ultrasound of the lower extremities did not demonstrate deep venous thrombosis.
Continue to: A toxicology screen
A toxicology screen was positive for tetrahydrocannabinol (THC) and negative for other substances. Hypercoagulable laboratory studies were normal, including anticardiolipin antibody IgG and IgM, factor V Leiden, prothrombin G20210A mutation, thrombin time, antithrombin III, and protein C and S activity. It was therefore believed that the AMI was due to in-situ coronary artery thrombus formation precipitated acutely by smoking cannabis—possibly with an underlying hypercoagulable state, even though no laboratory abnormalities were detected.
Our patient was discharged on lifelong aspirin 81 mg/d and oral rivaroxaban (maintenance dose of 20 mg/d). Metoprolol succinate 12.5 mg/d and lisinopril 2.5 mg/d were also initiated due
THE TAKEWAY
Coronary thrombosis can result in an AMI, even without underlying coronary atherosclerosis. Smoking cannabis may predispose individuals to in-situ coronary thrombosis and subsequent AMI. Although not often encountered in clinical practice, providers must be aware of this phenomenon in the differential diagnosis for AMI—particularly in young patients without traditional risk factors.
CORRESPONDENCE
Konstantinos Dean Boudoulas, MD, The Ohio State University Davis Lung and Heart Research Institute, 473 W. 12th Avenue, Suite 200, Columbus, Ohio 43210; kdboudoulas@osumc.edu
THE CASE
A 24-year-old man with a history of smoking tobacco presented to the hospital with acute-onset chest tightness and dyspnea shortly after smoking cannabis. He was otherwise healthy and hemodynamically stable upon arrival to the emergency department. An electrocardiogram (EKG) was obtained.
THE DIAGNOSIS
The EKG showed ST-segment elevation in the inferolateral leads, consistent with an acute myocardial infarction (AMI) (FIGURE 1). The patient was immediately transported to the cardiac catheterization laboratory, where coronary arteriography demonstrated a normal right coronary artery (FIGURE 2A). Diffuse thrombosis without atherosclerosis was seen throughout the left coronary arteries, including the left main artery, distal left anterior descending (LAD) artery, first diagonal branch of the LAD artery, ostial and proximal left circumflex (LCx) arteries, and first obtuse marginal (OM) branch of the LCx artery (FIGURE 2B).
DISCUSSION
The most common cause of AMI is underlying coronary atherosclerosis;1 however, AMI may occur due to in-situ thrombosis, thromboembolism, or coronary artery vasospasm, especially due to cocaine or other substance abuse. Occasionally, coronary arteries may be damaged due to viral myocarditis, autoimmune vasculitis, dissection of the ascending aorta, or dissection of a coronary artery, especially during pregnancy and postpartum.2,3
Cannabis and tobacco increase cardiovascular events
Smoking cannabis has been shown to increase adrenergic activity, resulting in an increased heart rate and elevated arterial pressure.4,5 These changes may increase myocardial oxygen demand and may result in a decrease in myocardial oxygen supply due to a decrease in the diastolic time.6 Smoking cannabis can also increase carboxyhemoglobin levels, which may compromise tissue oxygenation.
The risk for AMI has been shown to increase within the first hour of smoking cannabis.5 A few reports have documented cases of acute coronary syndrome following cannabis use; the majority of affected patients presented with chest pain within hours of smoking cannabis and were found to have a thrombus in a coronary artery, which was then treated medically or with percutaneous coronary intervention.7 Rare cases of cardiovascular death following cannabis use have also been reported.7,8
It has been suggested that coronary artery vasospasm may occur from cannabis use, which may precipitate thrombosis; however, this is not well defined.9 It is not clear if vasospasm was the inciting factor for thrombus formation in this case, as there was extensive and diffuse thrombus far greater than that expected solely from coronary artery vasospasm.
Continue to: AMI without atherosclerosis? Consider thrombosis
AMI without atherosclerosis? Consider thrombosis
In-situ coronary thrombosis should be considered in the differential diagnosis of a patient with an AMI without evidence of coronary atherosclerosis. Further, smoking cannabis immediately prior to symptom onset should heighten awareness for potential coronary thrombosis. Lifelong anticoagulation therapy may be indicated in these patients due to the catastrophic nature of the condition and limited data on this particular situation.
What’s recommended. Cessation of cannabis and tobacco smoking is recommended, as the use of these substances may contribute to the development of coronary thrombosis.3-7,9 A registry of patients with coronary thrombosis without coronary atherosclerosis, especially in states where cannabis is legal, would be useful to gauge the potential increase in such events. In addition, information related to the cardiovascular effects of using alternate routes of drug delivery, such as vaping devices, are limited; therefore, this practice should be closely monitored, as well.
Our patient’s outcome
Thrombus removal. In the cardiac catheterization laboratory, the majority of the thrombus was removed and coronary blood flow was improved using a thrombectomy catheter (FIGURE 2C). Residual thrombus remained in the very distal coronary arteries (FIGURE 2D), so heparin infusion was continued.
Imaging studies. Following the procedure, an echocardiogram demonstrated left ventricular (LV) regional wall motion abnormalities with moderately reduced LV systolic function and an ejection fraction (EF) of 35%. Troponin I levels peaked at 35 ng/mL. No LV apical thrombus or intracardiac defects (eg, patent foramen ovale, atrial septal defect, ventricular septal defect) that might have contributed to thromboembolism or paradoxical embolus were seen on echocardiogram or cardiac magnetic resonance imaging. In addition, ultrasound of the lower extremities did not demonstrate deep venous thrombosis.
Continue to: A toxicology screen
A toxicology screen was positive for tetrahydrocannabinol (THC) and negative for other substances. Hypercoagulable laboratory studies were normal, including anticardiolipin antibody IgG and IgM, factor V Leiden, prothrombin G20210A mutation, thrombin time, antithrombin III, and protein C and S activity. It was therefore believed that the AMI was due to in-situ coronary artery thrombus formation precipitated acutely by smoking cannabis—possibly with an underlying hypercoagulable state, even though no laboratory abnormalities were detected.
Our patient was discharged on lifelong aspirin 81 mg/d and oral rivaroxaban (maintenance dose of 20 mg/d). Metoprolol succinate 12.5 mg/d and lisinopril 2.5 mg/d were also initiated due
THE TAKEWAY
Coronary thrombosis can result in an AMI, even without underlying coronary atherosclerosis. Smoking cannabis may predispose individuals to in-situ coronary thrombosis and subsequent AMI. Although not often encountered in clinical practice, providers must be aware of this phenomenon in the differential diagnosis for AMI—particularly in young patients without traditional risk factors.
CORRESPONDENCE
Konstantinos Dean Boudoulas, MD, The Ohio State University Davis Lung and Heart Research Institute, 473 W. 12th Avenue, Suite 200, Columbus, Ohio 43210; kdboudoulas@osumc.edu
1. Davies MJ, Woolf N, Robertson WB. Pathology of acute myocardial infarction with particular reference to occlusive coronary thrombi. Br Heart J. 1976;38:659-664.
2. Pasupathy S, Air T, Dreyer RP, et al. Systematic review of patients presenting with suspected myocardial infarction and nonobstructive coronary arteries. Circulation. 2015;131:861-870.
3. Sharifi M, Frolich TG, Silverman IM. Myocardial infarction with angiographically normal coronary arteries. Chest. 1995;107:36-40.
4. Tatli E, Yilmaztepe M, Altun G, et al. Cannabis-induced coronary artery thrombosis and acute anterior myocardial infarction in a young man. Int J Cardiol. 2007;120:420-422.
5. Mittleman MA, Lewis RA, Maclure M, et al. Triggering myocardial infarction by marijuana. Circulation. 2001;103:2805-2809.
6. Boudoulas KD, Borer JS, Boudoulas H. Heart rate, life expectancy and the cardiovascular system: therapeutic considerations. Cardiology. 2015;132:199-212.
7. Yurtdas M, Aydın MK. Acute myocardial infarction in a young man; fatal blow of the marijuana: a case report. Korean Circ J. 2012;42:641-645.
8. Jouanjus E, Lapeyre-Mestre M, Micallef J; French Association of the Regional Abuse and Dependence Monitoring Centres (CEIP-A) Working Group on Cannabis Complications. Cannabis use: signal of increasing risk of serious cardiovascular disorders. J Am Heart Assoc. 2014;3:e000638.
9. Hodcroft CJ, Rossiter MC, Buch AN. Cannabis-associated myocardial infarction in a young man with normal coronary arteries. J Emerg Med. 2014;47:277-281.
1. Davies MJ, Woolf N, Robertson WB. Pathology of acute myocardial infarction with particular reference to occlusive coronary thrombi. Br Heart J. 1976;38:659-664.
2. Pasupathy S, Air T, Dreyer RP, et al. Systematic review of patients presenting with suspected myocardial infarction and nonobstructive coronary arteries. Circulation. 2015;131:861-870.
3. Sharifi M, Frolich TG, Silverman IM. Myocardial infarction with angiographically normal coronary arteries. Chest. 1995;107:36-40.
4. Tatli E, Yilmaztepe M, Altun G, et al. Cannabis-induced coronary artery thrombosis and acute anterior myocardial infarction in a young man. Int J Cardiol. 2007;120:420-422.
5. Mittleman MA, Lewis RA, Maclure M, et al. Triggering myocardial infarction by marijuana. Circulation. 2001;103:2805-2809.
6. Boudoulas KD, Borer JS, Boudoulas H. Heart rate, life expectancy and the cardiovascular system: therapeutic considerations. Cardiology. 2015;132:199-212.
7. Yurtdas M, Aydın MK. Acute myocardial infarction in a young man; fatal blow of the marijuana: a case report. Korean Circ J. 2012;42:641-645.
8. Jouanjus E, Lapeyre-Mestre M, Micallef J; French Association of the Regional Abuse and Dependence Monitoring Centres (CEIP-A) Working Group on Cannabis Complications. Cannabis use: signal of increasing risk of serious cardiovascular disorders. J Am Heart Assoc. 2014;3:e000638.
9. Hodcroft CJ, Rossiter MC, Buch AN. Cannabis-associated myocardial infarction in a young man with normal coronary arteries. J Emerg Med. 2014;47:277-281.