User login
A) Retained products of conception (RPOC) INCORRECT
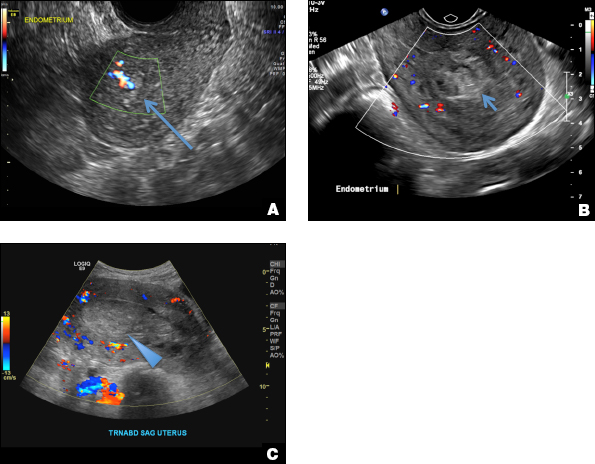
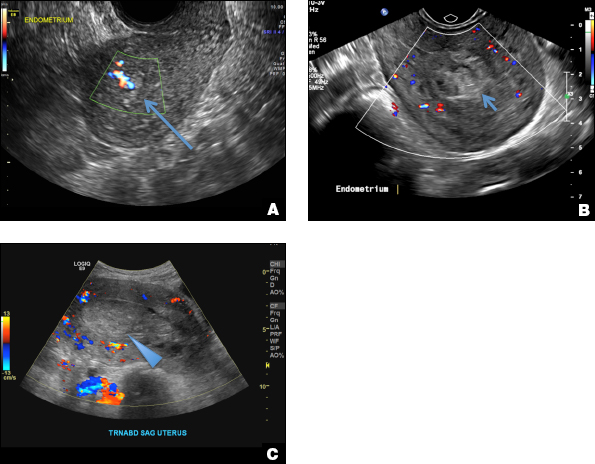
RPOC is a common complication arising from the presence of retained placental or fetal tissue after delivery, spontaneous, or elective abortion and is diagnosed by the presence of chorionic villi suggesting trophoblastic or placental tissue.1,2 Interpreting imaging findings is often a challenge secondary to the nonspecific findings of RPOC and often overlapping imaging features with blood products and enhanced myometrial vascularity (EMV) also known as arteriovenous malformation (AVM). Management usually is based on clinical findings in collaboration with supportive imaging features. On ultrasound, RPOC is suspected when there is a thickened endometrial echo complex (>8 mm to 13 mm) and/or the presence of an endometrial mass. Additionally, increased vascularity on color Doppler significantly increases the likelihood of RPOC; the absence of vascularity can be seen with both blood products and avascular RPOC.1 Vascularity in RPOC can be differentiated from EMV by its extension into the endometrium.
B) Complete hydatidiform mole INCORRECT
Complete hydatidiform mole (CHM) usually presents early in gestation with markedly elevated β-hCG. On ultrasound, it appears classically as an echogenic mass with innumerable small cystic spaces creating a “snowstorm or cluster of grape appearance” from hydropic chorionic villi along with larger irregular fluid collections and the absence of fetal parts.3 Ovarian hyperstimulation from elevated β-hCG can result in large bilateral ovarian cysts called theca lutein cysts.3
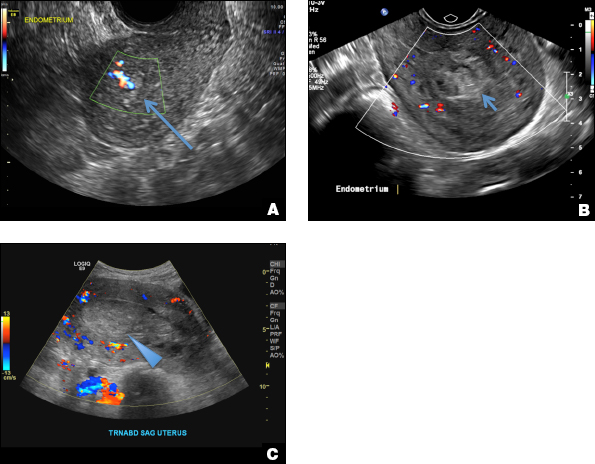
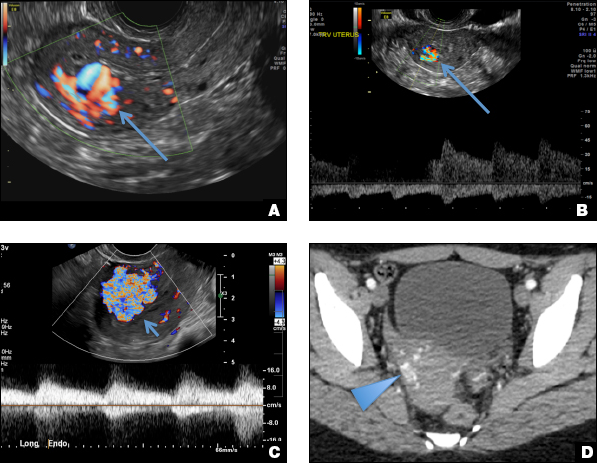
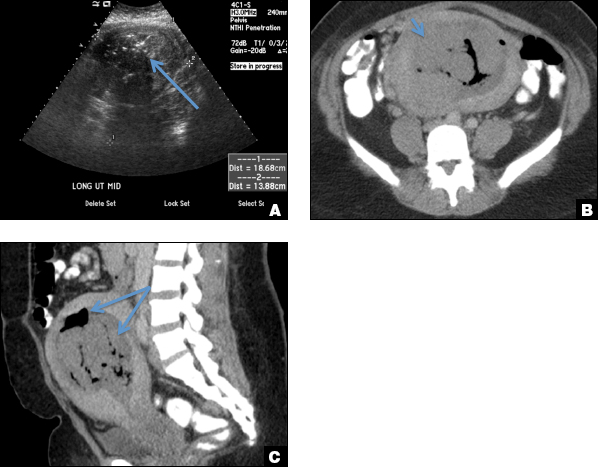
C) Enhanced myometrial vascularity (EMV) also known as arteriovenous malformation (AVM). CORRECT
EMV is an extremely rare cause of postpregnancy hemorrhage most often seen secondary to iatrogenic causes but can also be congenital or acquired from excessive hormone stimulation.2 On ultrasound, EMV appears as a hypoechoic vascular lesion or serpiginous network of vessels located in the myometrium with increased velocity and low resistance waveform on spectral Doppler.4 Subinvolution of placental site implantation where there is failure of the vessels to involute can sometimes be indistinguishable from acquired EMV and occasionally difficult to differentiate from RPOC.1 In stable patients with equivocal ultrasound findings, magnetic resonance imaging (MRI) with its superior contrast resolution can help delineate the endometrium from myometrium and clearly identify EMV as serpiginous signal voids in the myometrium with avid enhancement following contrast.5 Computed tomography (CT) angiogram is also of value in both the diagnosis and pretreatment planning of EMV prior to transcatheter uterine artery embolization.
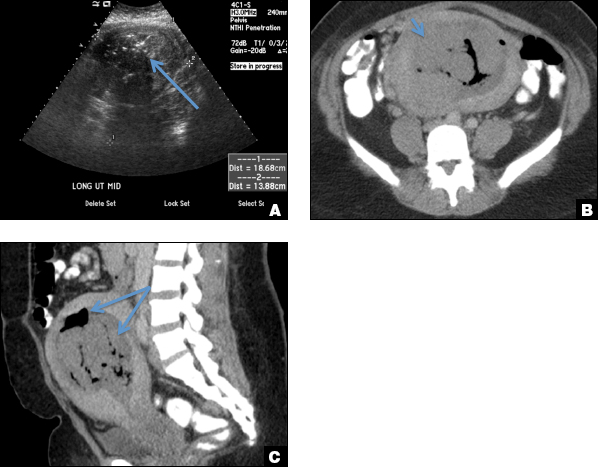
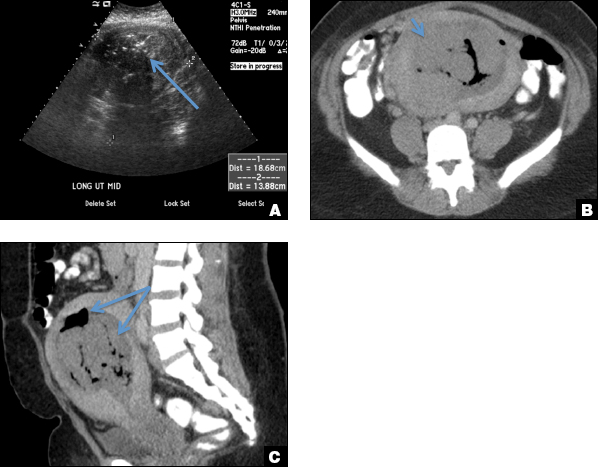
D) Endometritis INCORRECT
Endometritis is a common cause of fever and sepsis in the postpartum state, but it can also occur after procedures such as uterine fibroid embolization (UFE). On ultrasound, the endometrium usually is distended with avascular echogenic fluid. The presence of shadowing gas in the appropriate clinical setting is concerning for endometritis. CT scan can confirm the presence of gas and evaluate for septic thrombophlebitis, an uncommon, life-threatening complication of endometritis.
- Sellmyer MA, Desser TS, Maturen KE, Jeffrey RB Jr, Kamaya A. Physiologic, histologic, and imaging features of retained products of conception. RadioGraphics. 2013;33(3):781–796.
- Plunk M, Lee JH, Kani K, Dighe M. Imaging of postpartum complications: a multimodality review. AJR. 2013;200(2):W143–W154.
- Shaaban AM, Rezvani M, Haroun RR, et al. Gestational trophoblastic disease: clinical and imaging features. RadioGraphics. 2017;37(2):681–700.
- Timor-Tritsch IE, Haynes MC, Monteagudo A, Khatib N, Kovacs S. Ultrasound diagnosis and management of acquired uterine enhanced myometrial vascularity arteriovenous malformations. Am J Obstet Gynecol. 2016;214(6):731.e1–e10.
- Yoon DJ, Jones M, Taani JA, Buhimschi C, Dowell JD. A systematic review of acquired uterine arteriovenous malformations: pathophysiology, diagnosis, and transcatheter treatment. Am J Perinatol Rep. 2016;6(1):e6–e14.
A) Retained products of conception (RPOC) INCORRECT
RPOC is a common complication arising from the presence of retained placental or fetal tissue after delivery, spontaneous, or elective abortion and is diagnosed by the presence of chorionic villi suggesting trophoblastic or placental tissue.1,2 Interpreting imaging findings is often a challenge secondary to the nonspecific findings of RPOC and often overlapping imaging features with blood products and enhanced myometrial vascularity (EMV) also known as arteriovenous malformation (AVM). Management usually is based on clinical findings in collaboration with supportive imaging features. On ultrasound, RPOC is suspected when there is a thickened endometrial echo complex (>8 mm to 13 mm) and/or the presence of an endometrial mass. Additionally, increased vascularity on color Doppler significantly increases the likelihood of RPOC; the absence of vascularity can be seen with both blood products and avascular RPOC.1 Vascularity in RPOC can be differentiated from EMV by its extension into the endometrium.
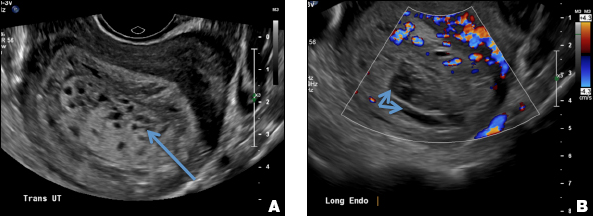
B) Complete hydatidiform mole INCORRECT
Complete hydatidiform mole (CHM) usually presents early in gestation with markedly elevated β-hCG. On ultrasound, it appears classically as an echogenic mass with innumerable small cystic spaces creating a “snowstorm or cluster of grape appearance” from hydropic chorionic villi along with larger irregular fluid collections and the absence of fetal parts.3 Ovarian hyperstimulation from elevated β-hCG can result in large bilateral ovarian cysts called theca lutein cysts.3
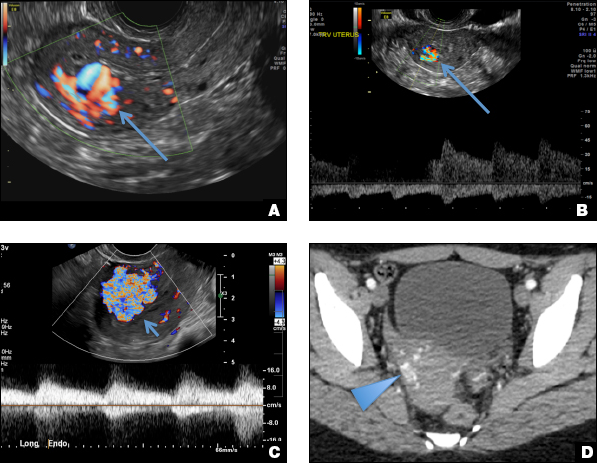
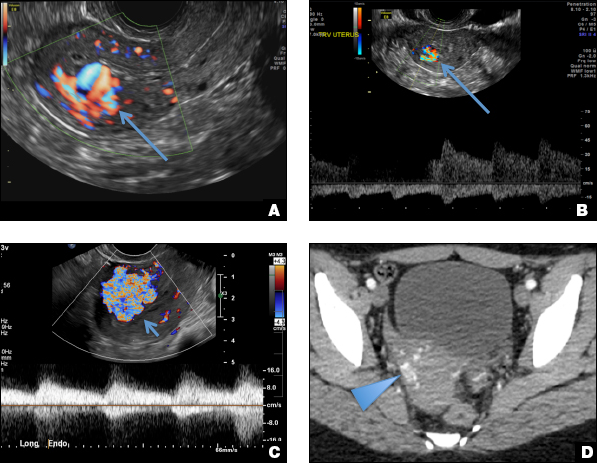
C) Enhanced myometrial vascularity (EMV) also known as arteriovenous malformation (AVM). CORRECT
EMV is an extremely rare cause of postpregnancy hemorrhage most often seen secondary to iatrogenic causes but can also be congenital or acquired from excessive hormone stimulation.2 On ultrasound, EMV appears as a hypoechoic vascular lesion or serpiginous network of vessels located in the myometrium with increased velocity and low resistance waveform on spectral Doppler.4 Subinvolution of placental site implantation where there is failure of the vessels to involute can sometimes be indistinguishable from acquired EMV and occasionally difficult to differentiate from RPOC.1 In stable patients with equivocal ultrasound findings, magnetic resonance imaging (MRI) with its superior contrast resolution can help delineate the endometrium from myometrium and clearly identify EMV as serpiginous signal voids in the myometrium with avid enhancement following contrast.5 Computed tomography (CT) angiogram is also of value in both the diagnosis and pretreatment planning of EMV prior to transcatheter uterine artery embolization.
D) Endometritis INCORRECT
Endometritis is a common cause of fever and sepsis in the postpartum state, but it can also occur after procedures such as uterine fibroid embolization (UFE). On ultrasound, the endometrium usually is distended with avascular echogenic fluid. The presence of shadowing gas in the appropriate clinical setting is concerning for endometritis. CT scan can confirm the presence of gas and evaluate for septic thrombophlebitis, an uncommon, life-threatening complication of endometritis.
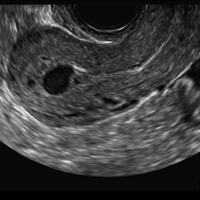
A) Retained products of conception (RPOC) INCORRECT
RPOC is a common complication arising from the presence of retained placental or fetal tissue after delivery, spontaneous, or elective abortion and is diagnosed by the presence of chorionic villi suggesting trophoblastic or placental tissue.1,2 Interpreting imaging findings is often a challenge secondary to the nonspecific findings of RPOC and often overlapping imaging features with blood products and enhanced myometrial vascularity (EMV) also known as arteriovenous malformation (AVM). Management usually is based on clinical findings in collaboration with supportive imaging features. On ultrasound, RPOC is suspected when there is a thickened endometrial echo complex (>8 mm to 13 mm) and/or the presence of an endometrial mass. Additionally, increased vascularity on color Doppler significantly increases the likelihood of RPOC; the absence of vascularity can be seen with both blood products and avascular RPOC.1 Vascularity in RPOC can be differentiated from EMV by its extension into the endometrium.
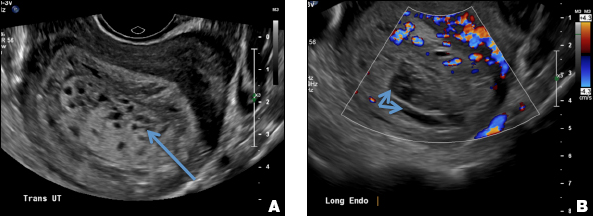
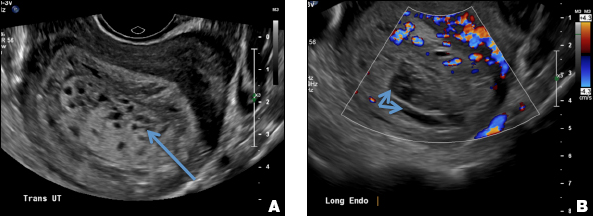
B) Complete hydatidiform mole INCORRECT
Complete hydatidiform mole (CHM) usually presents early in gestation with markedly elevated β-hCG. On ultrasound, it appears classically as an echogenic mass with innumerable small cystic spaces creating a “snowstorm or cluster of grape appearance” from hydropic chorionic villi along with larger irregular fluid collections and the absence of fetal parts.3 Ovarian hyperstimulation from elevated β-hCG can result in large bilateral ovarian cysts called theca lutein cysts.3
C) Enhanced myometrial vascularity (EMV) also known as arteriovenous malformation (AVM). CORRECT
EMV is an extremely rare cause of postpregnancy hemorrhage most often seen secondary to iatrogenic causes but can also be congenital or acquired from excessive hormone stimulation.2 On ultrasound, EMV appears as a hypoechoic vascular lesion or serpiginous network of vessels located in the myometrium with increased velocity and low resistance waveform on spectral Doppler.4 Subinvolution of placental site implantation where there is failure of the vessels to involute can sometimes be indistinguishable from acquired EMV and occasionally difficult to differentiate from RPOC.1 In stable patients with equivocal ultrasound findings, magnetic resonance imaging (MRI) with its superior contrast resolution can help delineate the endometrium from myometrium and clearly identify EMV as serpiginous signal voids in the myometrium with avid enhancement following contrast.5 Computed tomography (CT) angiogram is also of value in both the diagnosis and pretreatment planning of EMV prior to transcatheter uterine artery embolization.
D) Endometritis INCORRECT
Endometritis is a common cause of fever and sepsis in the postpartum state, but it can also occur after procedures such as uterine fibroid embolization (UFE). On ultrasound, the endometrium usually is distended with avascular echogenic fluid. The presence of shadowing gas in the appropriate clinical setting is concerning for endometritis. CT scan can confirm the presence of gas and evaluate for septic thrombophlebitis, an uncommon, life-threatening complication of endometritis.
- Sellmyer MA, Desser TS, Maturen KE, Jeffrey RB Jr, Kamaya A. Physiologic, histologic, and imaging features of retained products of conception. RadioGraphics. 2013;33(3):781–796.
- Plunk M, Lee JH, Kani K, Dighe M. Imaging of postpartum complications: a multimodality review. AJR. 2013;200(2):W143–W154.
- Shaaban AM, Rezvani M, Haroun RR, et al. Gestational trophoblastic disease: clinical and imaging features. RadioGraphics. 2017;37(2):681–700.
- Timor-Tritsch IE, Haynes MC, Monteagudo A, Khatib N, Kovacs S. Ultrasound diagnosis and management of acquired uterine enhanced myometrial vascularity arteriovenous malformations. Am J Obstet Gynecol. 2016;214(6):731.e1–e10.
- Yoon DJ, Jones M, Taani JA, Buhimschi C, Dowell JD. A systematic review of acquired uterine arteriovenous malformations: pathophysiology, diagnosis, and transcatheter treatment. Am J Perinatol Rep. 2016;6(1):e6–e14.
- Sellmyer MA, Desser TS, Maturen KE, Jeffrey RB Jr, Kamaya A. Physiologic, histologic, and imaging features of retained products of conception. RadioGraphics. 2013;33(3):781–796.
- Plunk M, Lee JH, Kani K, Dighe M. Imaging of postpartum complications: a multimodality review. AJR. 2013;200(2):W143–W154.
- Shaaban AM, Rezvani M, Haroun RR, et al. Gestational trophoblastic disease: clinical and imaging features. RadioGraphics. 2017;37(2):681–700.
- Timor-Tritsch IE, Haynes MC, Monteagudo A, Khatib N, Kovacs S. Ultrasound diagnosis and management of acquired uterine enhanced myometrial vascularity arteriovenous malformations. Am J Obstet Gynecol. 2016;214(6):731.e1–e10.
- Yoon DJ, Jones M, Taani JA, Buhimschi C, Dowell JD. A systematic review of acquired uterine arteriovenous malformations: pathophysiology, diagnosis, and transcatheter treatment. Am J Perinatol Rep. 2016;6(1):e6–e14.
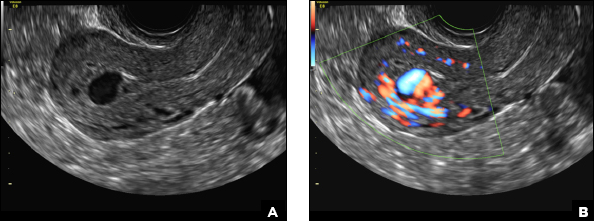
A 25-year-old woman presents to her ObGyn’s office with heavy noncyclical bleeding 6 weeks after a first-trimester suction curettage abortion. Transvaginal pelvic ultrasonography of the uterus with grayscale (A) and color Doppler (B) are performed.