User login
Critically ill patients with sepsis have a much higher prevalence of different viruses than do nonseptic critically ill patients and healthy controls, judging from the findings of a study of more than 800 patients.
These findings provide evidence that the reactivation of latent viruses "is extremely common in patients with prolonged sepsis and is consistent with development of immunosuppression," researchers concluded.
For some of the viruses, the levels detected in septic patients were comparable to the levels in organ transplant recipients, "who are pharmacologically immunosuppressed, providing further support that our findings are indicative of clinically relevant immunosuppression," Dr. Anthony Walton, of the department of anesthesiology, Washington University, St. Louis, and his coauthors wrote. The study was published online June 6 in PLoS One (2014;9:e98819 [doi: 10.1371/journal.pone.0098819]).
In what they said is the first study to evaluate the effect of sepsis on "multiple families of viruses," the investigators addressed whether sepsis progresses from a hyperinflammatory phase early in the course of sepsis to an immunosuppressive state, a "controversial hypothesis" for explaining the course of sepsis, they wrote.
The researchers compared levels of viruses that included cytomegalovirus (CMV), Epstein-Barr virus (EBV), herpes simplex virus (HSV), human herpesvirus 6 (HHV-6), and the anellovirus TTV in whole blood and plasma, and of the polyomaviruses BK and JC in the urine of 560 critically ill patients with sepsis and 161 critically ill patients who did not have sepsis, who were not immunocompromised at baseline; and 164 healthy, age-matched controls, who were ambulatory and whose blood sample was obtained before elective surgery. The median age of the patients was 63-64 years; the median APACHE II score was 18 in the septic group and 5 in the critically ill, nonseptic group; and the median length of stay in the intensive care unit was 11 days and 2 days, respectively; mortality was 26% and 6%, respectively. (Patients who were HIV-1 infected, organ transplant recipients, or on immunosuppressive medications were among those who were excluded.)
Among the investigators’ key findings were these:
• CMV seropositivity was detected in about 70% of the patients in the three groups, indicating they had been infected previously. Among these patients, CMV levels were markedly elevated in 24.2% of the septic patients, compared with 1.1% of the critically ill, nonseptic patients and none of the healthy controls.
• EBV was detected in 53.2% of septic patients, vs. 12.1% of the critically ill, nonseptic patients and 3.6% of the healthy controls. (Almost 9% of the septic patients had EBV detected at the level that would be the basis for reducing immunosuppressive medications in solid organ transplant recipients at Washington University, the authors pointed out.)
• HSV was detected in 14.1% of septic patients, vs. 1.5% of the critically ill, nonseptic patients and none of the healthy controls.
• HHV-6 was detected in 10.4% of septic patients, vs. less than 1% of the critically ill, nonseptic patients and 3.3% of the healthy controls.
• TTV was detected in almost 78% of the septic patients, close to 64% of the critically ill, nonseptic patients, and 60.1% of the healthy controls, but levels were lower among the latter two groups.
The authors said that it is "likely that viral detection in the setting of sepsis is not due to primary infection but rather to viral reactivation." Almost 43% of those with sepsis had evidence of at least two viruses, which, combined with the "magnitude of viral loads ... provides strong evidence that host immunity is impaired in sepsis," they added.
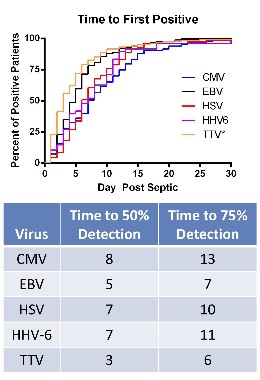
Among their other findings was that in the septic patients, the detection rate of the viruses increased for all the viruses with increasing number of days spent in the ICU, and septic patients who had CMV detected in the plasma had significantly higher 90-day mortality than did septic patients with no CMV detected.
Limitations of the study include the fact that it does not address whether the increased prevalence of viral reactivation among the septic patients "is merely a marker of impaired immunity or contributes to sepsis morbidity/mortality," they noted. But the implications of their results include the possibility that tracking the viral load of different viruses in septic patients "may be useful as a biomarker of host immunity in sepsis."
The study was funded by the National Institutes of Health. One author is an employee of Biomérieux, a company that is working on a method to monitor levels of different viruses in the blood as an indicator of immune status which is performing related research. No other author disclosures were listed.
Dr. Steven Q. Simpson, FCCP, comments: The investigators have demonstrated that reactivation of latent viral infections may well contribute to the death of critically ill septic patients. Some of the viral reactivations were associated with secondary fungal infection as well.
Although viral DNA was detected as early as 1 day into sepsis, the bulk of the manifested reactivations occurred over the subsequent 2 weeks. Viral reactivation is a clear marker that the "late" immune suppression of sepsis is a real phenomenon and leads to real sequelae.
Nevertheless, it is not yet clear exactly how this information will become useful in practice, as the cost of daily DNA screening for multiple viruses would be prohibitive, unless high-volume demand drives pricing down. One can see, under that scenario, how viral reactivation could be the signal that immune augmentation therapy is required, and that it might be beneficial. This work is not quite ready for prime time, but it is getting ever closer.
Dr. Steven Q. Simpson is professor of medicine, University of Kansas, Kansas City. He is also founder of the Kansas Sepsis Project. He had no disclosures.
Dr. Steven Q. Simpson, FCCP, comments: The investigators have demonstrated that reactivation of latent viral infections may well contribute to the death of critically ill septic patients. Some of the viral reactivations were associated with secondary fungal infection as well.
Although viral DNA was detected as early as 1 day into sepsis, the bulk of the manifested reactivations occurred over the subsequent 2 weeks. Viral reactivation is a clear marker that the "late" immune suppression of sepsis is a real phenomenon and leads to real sequelae.
Nevertheless, it is not yet clear exactly how this information will become useful in practice, as the cost of daily DNA screening for multiple viruses would be prohibitive, unless high-volume demand drives pricing down. One can see, under that scenario, how viral reactivation could be the signal that immune augmentation therapy is required, and that it might be beneficial. This work is not quite ready for prime time, but it is getting ever closer.
Dr. Steven Q. Simpson is professor of medicine, University of Kansas, Kansas City. He is also founder of the Kansas Sepsis Project. He had no disclosures.
Dr. Steven Q. Simpson, FCCP, comments: The investigators have demonstrated that reactivation of latent viral infections may well contribute to the death of critically ill septic patients. Some of the viral reactivations were associated with secondary fungal infection as well.
Although viral DNA was detected as early as 1 day into sepsis, the bulk of the manifested reactivations occurred over the subsequent 2 weeks. Viral reactivation is a clear marker that the "late" immune suppression of sepsis is a real phenomenon and leads to real sequelae.
Nevertheless, it is not yet clear exactly how this information will become useful in practice, as the cost of daily DNA screening for multiple viruses would be prohibitive, unless high-volume demand drives pricing down. One can see, under that scenario, how viral reactivation could be the signal that immune augmentation therapy is required, and that it might be beneficial. This work is not quite ready for prime time, but it is getting ever closer.
Dr. Steven Q. Simpson is professor of medicine, University of Kansas, Kansas City. He is also founder of the Kansas Sepsis Project. He had no disclosures.
Critically ill patients with sepsis have a much higher prevalence of different viruses than do nonseptic critically ill patients and healthy controls, judging from the findings of a study of more than 800 patients.
These findings provide evidence that the reactivation of latent viruses "is extremely common in patients with prolonged sepsis and is consistent with development of immunosuppression," researchers concluded.
For some of the viruses, the levels detected in septic patients were comparable to the levels in organ transplant recipients, "who are pharmacologically immunosuppressed, providing further support that our findings are indicative of clinically relevant immunosuppression," Dr. Anthony Walton, of the department of anesthesiology, Washington University, St. Louis, and his coauthors wrote. The study was published online June 6 in PLoS One (2014;9:e98819 [doi: 10.1371/journal.pone.0098819]).
In what they said is the first study to evaluate the effect of sepsis on "multiple families of viruses," the investigators addressed whether sepsis progresses from a hyperinflammatory phase early in the course of sepsis to an immunosuppressive state, a "controversial hypothesis" for explaining the course of sepsis, they wrote.
The researchers compared levels of viruses that included cytomegalovirus (CMV), Epstein-Barr virus (EBV), herpes simplex virus (HSV), human herpesvirus 6 (HHV-6), and the anellovirus TTV in whole blood and plasma, and of the polyomaviruses BK and JC in the urine of 560 critically ill patients with sepsis and 161 critically ill patients who did not have sepsis, who were not immunocompromised at baseline; and 164 healthy, age-matched controls, who were ambulatory and whose blood sample was obtained before elective surgery. The median age of the patients was 63-64 years; the median APACHE II score was 18 in the septic group and 5 in the critically ill, nonseptic group; and the median length of stay in the intensive care unit was 11 days and 2 days, respectively; mortality was 26% and 6%, respectively. (Patients who were HIV-1 infected, organ transplant recipients, or on immunosuppressive medications were among those who were excluded.)
Among the investigators’ key findings were these:
• CMV seropositivity was detected in about 70% of the patients in the three groups, indicating they had been infected previously. Among these patients, CMV levels were markedly elevated in 24.2% of the septic patients, compared with 1.1% of the critically ill, nonseptic patients and none of the healthy controls.
• EBV was detected in 53.2% of septic patients, vs. 12.1% of the critically ill, nonseptic patients and 3.6% of the healthy controls. (Almost 9% of the septic patients had EBV detected at the level that would be the basis for reducing immunosuppressive medications in solid organ transplant recipients at Washington University, the authors pointed out.)
• HSV was detected in 14.1% of septic patients, vs. 1.5% of the critically ill, nonseptic patients and none of the healthy controls.
• HHV-6 was detected in 10.4% of septic patients, vs. less than 1% of the critically ill, nonseptic patients and 3.3% of the healthy controls.
• TTV was detected in almost 78% of the septic patients, close to 64% of the critically ill, nonseptic patients, and 60.1% of the healthy controls, but levels were lower among the latter two groups.
The authors said that it is "likely that viral detection in the setting of sepsis is not due to primary infection but rather to viral reactivation." Almost 43% of those with sepsis had evidence of at least two viruses, which, combined with the "magnitude of viral loads ... provides strong evidence that host immunity is impaired in sepsis," they added.
Among their other findings was that in the septic patients, the detection rate of the viruses increased for all the viruses with increasing number of days spent in the ICU, and septic patients who had CMV detected in the plasma had significantly higher 90-day mortality than did septic patients with no CMV detected.
Limitations of the study include the fact that it does not address whether the increased prevalence of viral reactivation among the septic patients "is merely a marker of impaired immunity or contributes to sepsis morbidity/mortality," they noted. But the implications of their results include the possibility that tracking the viral load of different viruses in septic patients "may be useful as a biomarker of host immunity in sepsis."
The study was funded by the National Institutes of Health. One author is an employee of Biomérieux, a company that is working on a method to monitor levels of different viruses in the blood as an indicator of immune status which is performing related research. No other author disclosures were listed.
Critically ill patients with sepsis have a much higher prevalence of different viruses than do nonseptic critically ill patients and healthy controls, judging from the findings of a study of more than 800 patients.
These findings provide evidence that the reactivation of latent viruses "is extremely common in patients with prolonged sepsis and is consistent with development of immunosuppression," researchers concluded.
For some of the viruses, the levels detected in septic patients were comparable to the levels in organ transplant recipients, "who are pharmacologically immunosuppressed, providing further support that our findings are indicative of clinically relevant immunosuppression," Dr. Anthony Walton, of the department of anesthesiology, Washington University, St. Louis, and his coauthors wrote. The study was published online June 6 in PLoS One (2014;9:e98819 [doi: 10.1371/journal.pone.0098819]).
In what they said is the first study to evaluate the effect of sepsis on "multiple families of viruses," the investigators addressed whether sepsis progresses from a hyperinflammatory phase early in the course of sepsis to an immunosuppressive state, a "controversial hypothesis" for explaining the course of sepsis, they wrote.
The researchers compared levels of viruses that included cytomegalovirus (CMV), Epstein-Barr virus (EBV), herpes simplex virus (HSV), human herpesvirus 6 (HHV-6), and the anellovirus TTV in whole blood and plasma, and of the polyomaviruses BK and JC in the urine of 560 critically ill patients with sepsis and 161 critically ill patients who did not have sepsis, who were not immunocompromised at baseline; and 164 healthy, age-matched controls, who were ambulatory and whose blood sample was obtained before elective surgery. The median age of the patients was 63-64 years; the median APACHE II score was 18 in the septic group and 5 in the critically ill, nonseptic group; and the median length of stay in the intensive care unit was 11 days and 2 days, respectively; mortality was 26% and 6%, respectively. (Patients who were HIV-1 infected, organ transplant recipients, or on immunosuppressive medications were among those who were excluded.)
Among the investigators’ key findings were these:
• CMV seropositivity was detected in about 70% of the patients in the three groups, indicating they had been infected previously. Among these patients, CMV levels were markedly elevated in 24.2% of the septic patients, compared with 1.1% of the critically ill, nonseptic patients and none of the healthy controls.
• EBV was detected in 53.2% of septic patients, vs. 12.1% of the critically ill, nonseptic patients and 3.6% of the healthy controls. (Almost 9% of the septic patients had EBV detected at the level that would be the basis for reducing immunosuppressive medications in solid organ transplant recipients at Washington University, the authors pointed out.)
• HSV was detected in 14.1% of septic patients, vs. 1.5% of the critically ill, nonseptic patients and none of the healthy controls.
• HHV-6 was detected in 10.4% of septic patients, vs. less than 1% of the critically ill, nonseptic patients and 3.3% of the healthy controls.
• TTV was detected in almost 78% of the septic patients, close to 64% of the critically ill, nonseptic patients, and 60.1% of the healthy controls, but levels were lower among the latter two groups.
The authors said that it is "likely that viral detection in the setting of sepsis is not due to primary infection but rather to viral reactivation." Almost 43% of those with sepsis had evidence of at least two viruses, which, combined with the "magnitude of viral loads ... provides strong evidence that host immunity is impaired in sepsis," they added.
Among their other findings was that in the septic patients, the detection rate of the viruses increased for all the viruses with increasing number of days spent in the ICU, and septic patients who had CMV detected in the plasma had significantly higher 90-day mortality than did septic patients with no CMV detected.
Limitations of the study include the fact that it does not address whether the increased prevalence of viral reactivation among the septic patients "is merely a marker of impaired immunity or contributes to sepsis morbidity/mortality," they noted. But the implications of their results include the possibility that tracking the viral load of different viruses in septic patients "may be useful as a biomarker of host immunity in sepsis."
The study was funded by the National Institutes of Health. One author is an employee of Biomérieux, a company that is working on a method to monitor levels of different viruses in the blood as an indicator of immune status which is performing related research. No other author disclosures were listed.
Key clinical point: Reactivation of latent viruses may underlie the development of sepsis in critically ill patients and contribute to their death.
Major finding: Evidence of reactivation with multiple viruses in septic patients – which included almost 43% who were positive for at least two viruses – and the magnitude of viral loads in septic patients indicate that patients with sepsis are immunosuppressed.
Data source: The study compared levels of cytomegalovirus, herpes simplex, and other viruses in 560 critically ill septic patients and 161 critically ill nonseptic patients in intensive care units, and 164 healthy, age-matched controls.
Disclosures: The study was funded by the National Institutes of Health. One of the 13 authors is an employee of Biomérieux, a company that is working on a method to monitor levels of different viruses in the blood as an indicator of immune status. No other author disclosures were listed.