User login
- Is hormone therapy still a valid option? 12 ObGyns address this question
Members of the OBG MANAGEMENT Virtual Board of Editors and Janelle Yates, Senior Editor (May 2011)
Dr. Kaunitz receives grant or research support from Bayer, Agile, Noven, Teva, and Medical Diagnostic Laboratories, is a consultant to Bayer, Merck, and Teva, and owns stock in Becton Dickinson.
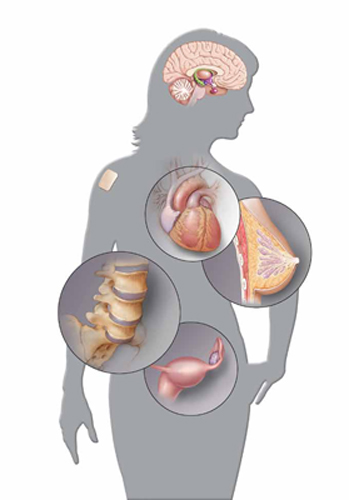
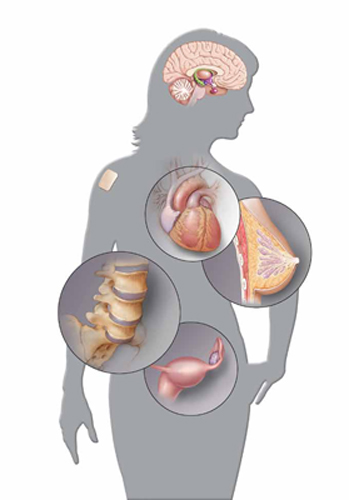
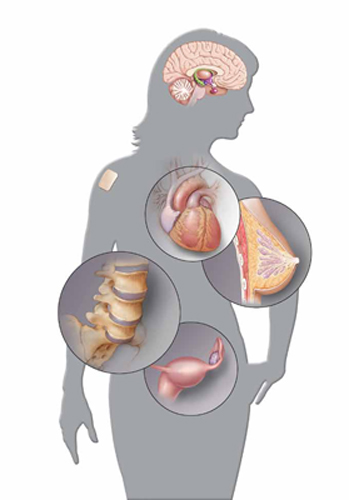
Among the developments of the past year in the care of menopausal women are:
- updated guidelines from the Institute of Medicine regarding vitamin D requirements—suggesting that fewer women are deficient in this nutrient than experts had believed
- new data from Europe on hormone therapy (HT) that highlight the safety of transdermal estrogen in comparison with oral administration
- a recent analysis from the Women’s Health Initiative (WHI), confirming a small elevated risk of breast cancer mortality with use of combination estrogen-progestin HT
- confirmation that age at initiation of HT determines its effect on cardiovascular health
- clarification of the association between HT and dementia
- new data demonstrating modest improvement in hot flushes when the serotonin reuptake inhibitor (SRI) escitalopram is used
- a brand new report from the WHI estrogen-alone arm that shows a protective effect against breast cancer.
The new data on HT suggest that we still have much to learn about its benefits and risks. We also are reaching an understanding that, for many young, symptomatic, menopausal patients, HT can represent a safe choice, with much depending on the timing and duration of therapy.
For more on how your colleagues are managing menopausal patients with and without hormone therapy, see “Is hormone therapy still a valid option? 12 ObGyns address this question,” on the facing page.
Menopausal women need less vitamin D than we thought
Institute of Medicine. Dietary reference intakes for calcium and vitamin D. Washington, DC: IOM; December 2010. http://www.iom.edu/~/media/Files/Report%20Files/2010/Dietary-Reference-Intakes-for-Calcium-and-Vitamin-D/Vitamin%20D%20and%20Calcium%202010%20Report%20Brief.pdf. Accessed March 24, 2011.
In the 2010 Update on Menopause, I summarized recent findings on vitamin D requirements, including recommendations that menopausal women should take at least 800 IU of vitamin D daily. I also described the prevailing expert opinion that many North American women are deficient in this nutrient.
What a difference a year can make! In late November, the Institute of Medicine (IOM) released a comprehensive report on vitamin D. Here are some of its conclusions:
- Vitamin D plays an important role in skeletal health but its role in other areas, including cardiovascular disease and cancer, is uncertain
- An intake of 600 IU of vitamin D daily is appropriate for girls and for women as old as 70 years; an in-take of 800 IU daily is appropriate for women older than 70 years
- A serum level of 25-hydroxy vitamin D of 20 ng/mL is consistent with adequate vitamin D status; this is lower than the threshold many have recommended
- With few exceptions, all people who live in North America—including those who have minimal or no exposure to sunlight—are receiving adequate calcium and vitamin D
- Ingestion of more than 4,000 IU of vitamin D daily can cause renal damage and injure other tissues.
The IOM report will likely prompt multivitamin manufacturers to increase the amount of vitamin D contained in their supplements to 600 IU daily. In addition, the report will probably discourage the common practice of checking serum 25-hydroxy vitamin D levels and prescribing a high dosage of vitamin D supplementation when the level is below 30 ng/mL.
I continue to recommend multivitamin supplements that include calcium and vitamin D (but no iron) to my menopausal patients. However, I no longer routinely recommend that they take additional calcium and vitamin D or undergo assessment of serum vitamin D levels.
Is transdermal estrogen safer than oral administration?
Canonico M, Fournier A, Carcaillon L, et al. Postmenopausal hormone therapy and risk of idiopathic venous thromboembolism: results from the E3N cohort study. Arterioscler Thromb Vasc Biol. 2010;30(2):340–345.
Renoux C, Dell’aniello S, Garbe E, Suissa S. Transdermal and oral hormone replacement therapy and the risk of stroke: a nested case-control study. BMJ. 2010;340:c2519. doi: 10.1136/bmj.c2519.
In the WHI, the combination of oral conjugated equine estrogen and medroxyprogesterone acetate more than doubled the risk of deep venous thrombosis and pulmonary embolism and modestly increased the risk of stroke, compared with nonuse.1
A year after publication of the initial findings of the WHI estrogen-progestin arm, the Estrogen and THromboEmbolism Risk Study Group (ESTHER) case-control study from France provided evidence that transdermal estrogen does not increase the risk of venous thrombosis.2 In France, many menopausal women use HT, and the transdermal route of administration is common.
In 2010, the E3N cohort study from France also assessed the risk of thrombosis associated with oral and transdermal HT. Investigators followed more than 80,000 postmenopausal women and found that, unlike oral HT, the transdermal route did not increase the risk of venous thrombosis.
More recent evidence also suggests a safety advantage for transdermal HT. The newest data come from the United Kingdom General Practice Research Database, which includes information on more than 870,000 women who were 50 to 70 years old from 1987 to 2006. Investigators identified more than 15,000 women who were given a diagnosis of stroke during this period and compared the use of HT in these women with that of almost 60,000 women in a control group. The risk of stroke associated with current use of transdermal HT was similar to the risk associated with nonuse of HT. Women who used a patch containing 0.05 mg of estradiol or less had a risk of stroke 19% lower than women who did not use HT.
In contrast, the risk of stroke in users of patches that contained a higher dosage of estradiol was almost twice the risk in nonusers of HT. Current users of oral HT had a risk of stroke 28% higher than that of nonusers of HT.
The WHI assessed the risks and benefits of oral HT only. Although no randomized, clinical trial has compared cardiovascular risks among users of oral and transdermal HT, I believe that a preponderance of evidence points to a superior safety profile for the transdermal route, particularly at a dosage of 0.05 mg of estradiol or less.
I encourage my patients who are initiating HT to consider the transdermal route—particularly women who have an elevated risk of cardiovascular disease, including those who are overweight, smoke cigarettes, or who have hypertension or diabetes. I suggest the transdermal route despite its higher cost (oral micronized estradiol can be purchased for as little as $4 for a month’s supply at a chain pharmacy).
When a patient prefers to avoid a patch (because of local irritation), I offer her estradiol gel or spray or the vaginal ring. (Femring is systemic estradiol, whereas Estring is local.) These formulations should provide the same safety benefits as the patch.
Estrogen-progestin HT raises the risk of death from breast cancer
Chlebowski RT, Anderson GL, Gass M, et al. Estrogen plus progestin and breast cancer incidence and mortality in postmenopausal women. JAMA. 2010;304(15):1684–1692.
Toh S, Hernandez-Diaz S, Logan R, Rossouw JE, Hernan MA. Coronary heart disease in postmenopausal recipients of estrogen plus progestin: does the increased risk ever disappear? Ann Intern Med. 2010;152(4):211–217.
In the estrogen-progestin arm of the WHI, initially published in 2002, the risk of invasive breast cancer was modestly elevated (hazard ratio [HR], 1.26) among women who had used HT longer than 5 years.3
In 2010, investigators reported on breast cancer mortality in WHI participants at a mean follow-up of 11 years. They found that combination HT users had breast cancer histology similar to that of nonusers. However, the tumors were more likely to be node-positive in combination HT users (23.7% vs 16.2%). In addition, breast cancer mortality was slightly higher among users of HT (2.6 vs 1.3 deaths in every 10,000 woman-years) (HR, 1.96; 95% confidence interval, 1.00–4.04).
Earlier observational studies had suggested that the death rate from breast cancer is lower in users of combination HT than in nonusers. Consistent with the UK Million Women Study, however, a 2010 report from the WHI found a higher mortality rate among women who have used HT.4
These new WHI findings reinforce the importance of assessing whether micronized progesterone combined with estrogen might lower the risk of death from breast cancer—a possibility suggested by findings of the French E3N cohort study.5
In addition, given the possibility that HT may be cardioprotective when it is initiated within 10 years after the onset of menopause, a WHI report that addresses long-term all-cause mortality would allow us to better counsel our menopausal patients who are trying to decide whether to start or continue HT. See, for example, the data from the California Teachers Study (below) and the estrogen-alone arm of the WHI (page 46).
The findings of this important WHI publication have strengthened the resolve of some clinicians to stop prescribing HT for menopausal women. I continue to prescribe HT to patients who have bothersome vasomotor and related symptoms, however. I also counsel women about the other benefits of HT, which include alleviation of genital atrophy and prevention of osteoporotic fractures. For patients considering or using estrogen-progestin HT, I include discussion of the small increase in their risk of developing, and dying from, breast cancer.
Age at initiation of HT determines its effect on CHD
Stram DO, Liu Y, Henderson KD, et al. Age-specific effects of hormone therapy use on overall mortality and ischemic heart disease mortality among women in the California Teachers Study. Menopause 2011;18(3):253-261.
Allison MA, Manson JE. Age, hormone therapy use, coronary heart disease, and mortality [editorial]. Menopause. 2011;18(3):243-245.
The initial findings of the WHI estrogen-progestin arm suggested that menopausal HT increases the risk of CHD. Since then, however, further analyses from the WHI and other HT trials, as well as reports from the observational Nurses’ Health Study, have suggested that the timing of initiation of HT determines its effect on cardiovascular health.
In this study from the California Teachers Study (CTS), investigators explored the effect of age at initiation of HT on cardiovascular and overall mortality. The CTS is a prospective study of more than 133,000 current and retired female teachers and administrators who returned an initial questionnaire in 1995 and 1996. Participants were then followed until late 2004, or death, whichever came first. More than 71,000 participants were eligible for analysis.
Current HT users were leaner, less likely to smoke, and more likely to exercise and consume alcohol than nonusers were. The analysis was adjusted for a variety of potential cardiovascular and other confounders.
Youngest HT users had the lowest risk of death
During follow-up, 18.3% of never-users of HT died, compared with 17.9% of former users. In contrast, 6.9% of women taking HT at the time of the baseline questionnaire died during follow-up.
Overall, current HT use was associated with a reduced risk of death from CHD (hazard ratio [HR], 0.84; 95% confidence interval, 0.74–0.95). This risk reduction was most notable (HR, 0.38) in the youngest HT users (36 to 59 years old). The risk of death from CHD gradually increased with the age of current HT users, reaching a hazard ratio of approximately 0.9 in current users who were 70 years and older. However, the CHD mortality hazard ratio did not reach or exceed the referent hazard ratio (1.0) assigned to never users of HT of any age.
The overall mortality rate was lowest for the youngest HT users (HR, 0.54) and approached 1.0 in the oldest current HT users.
The associations between overall and CHD mortality were similar among users of estrogen-only and estrogen-progestin HT.
As Allison and Manson point out in an editorial accompanying this study, the findings from the CTS are congruent with an extensive body of evidence from women and nonhuman primates. These data provide robust reassurance that HT does not increase the risk of death from CHD when it is used by recently menopausal women who have bothersome vasomotor symptoms.
Hormone therapy and dementia: Earlier use is better
Whitmer RA, Quesenberry CP, Zhou J, Yaffe K. Timing of hormone therapy and dementia: the critical window theory revisited. Ann Neurol. 2011;69(1):163–169.
Alzheimer’s disease is more common among women than men. In addition, caregivers to those who have dementia are more likely to be women. Therefore, it’s no surprise that women are especially concerned about their risk of dementia. Menopausal patients in my practice often ask whether use of HT might alter this risk.
Because vasomotor symptoms usually arise in late perimenopause or early menopause, women in observational studies (which reflect clinical practice) tend to begin HT when they are in their late 40s or early 50s. Overall, observational studies have suggested that HT is associated with a reduced risk of dementia. In contrast, the WHI clinical trial, in which the mean age of women who were randomized to HT or placebo was 63 years, found that the initiation of HT later in life increased the risk of dementia.
These observations led to the “critical window” theory regarding HT and dementia: Estrogen protects against dementia when it is taken by perimenopausal or early menopausal women, whereas it is not protective and may even accelerate cognitive decline when it is started many years after the onset of menopause.
In this recent study from the California Kaiser Permanente health maintenance organization, investigators assessed the long-term risk of dementia by timing of HT. From 1964 through 1973, menopausal “midlife” women who were 40 to 55 years old and free of dementia reported whether or not they used HT. Twenty-five to 30 years later, participants were reassessed for “late life” HT use.
Women who used HT in midlife only had the lowest prevalence of dementia, whereas those who used HT only in late life had the highest prevalence. Women who used HT at both time points had a prevalence of dementia similar to that of women who had never used HT.
Given these important findings, I believe it is now reasonable to counsel women in late perimenopause and early menopause that the use of HT may lower their risk of dementia. How long we should continue to prescribe HT depends on individual variables, including the presence of vasomotor symptoms, the risk of osteoporosis, and concerns about breast cancer.
I encourage women to taper their dosage of HT over time, aiming at complete discontinuation or a low maintenance dosage.
Are SRIs an effective alternative to HT for hot flushes?
Freeman EW, Guthrie K, Caan B, et al. Efficacy of escitalopram for hot flashes in healthy menopausal women: a randomized controlled trial. JAMA. 2011;305(3):267–274.
Interest in nonhormonal management of menopausal vasomotor symptoms continues to run high, although only hormonal therapy has FDA approval for this indication. Many trials of serotonin reuptake inhibitors (SRIs) for the treatment of vasomotor symptoms have focused on breast cancer survivors, many of whom use anti-estrogen agents that increase the prevalence of these symptoms. In contrast, this well-conducted multicenter trial, funded by the National Institutes of Health, enrolled healthy, symptomatic, menopausal women.
In the trial, 205 perimenopausal or postmenopausal women 40 to 62 years old who had at least 28 bothersome or severe episodes of hot flushes and night sweats a week were randomized to 10 mg daily of the SRI escitalopram (Lexapro) or placebo for 8 weeks. Women who did not report a reduction in hot flushes and night sweats of at least 50% at 4 weeks, or a decrease in the severity of these symptoms, were increased to a dosage of 20 mg daily of escitalopram or placebo. The mean baseline frequency of vasomotor symptoms was 9.79.
Within 1 week, women taking the SRI experienced significantly greater improvement than those taking placebo. By 8 weeks, the daily frequency of vasomotor symptoms had diminished by 4.6 hot flushes among women taking the SRI, compared with 3.20 among women taking placebo (P < .01).
Overall, adverse effects were reported by approximately 58% of participants. The pattern of these side effects was similar in the active and placebo treatment arms. No adverse events serious enough to require withdrawal from the study were reported in either arm.
Patient satisfaction with treatment was 70% in the SRI group, compared with 43% among women taking placebo (P < .001).
Although Freeman and colleagues convincingly demonstrate that escitalopram is more effective than placebo, the drug is less effective than HT. I agree with Nelson and coworkers, who, in a meta-analysis of nonhormonal treatments for vasomotor symptoms, concluded: “These therapies may be most useful for highly symptomatic women who cannot take estrogen but are not optimal choices for most women.”6
Unopposed estrogen appears to protect against breast cancer
LaCroix AZ, Chlebowski RT, Manson JE, et al; WHI Investigators. Health outcomes after stopping conjugated equine estrogens among postmenopausal women with prior hysterectomy. A randomized controlled trial. JAMA. 2011;305(13):1305–1314.
The WHI continues to surprise with its findings almost a decade after publication of initial data. In this brand new report from the estrogen-alone arm, postmenopausal, hysterectomized women who were followed for a mean of 10.7 years experienced a reduced risk of breast cancer after a mean of 5.9 years of use of conjugated equine estrogens (CEE).
They experienced no increased or diminished risk of coronary heart disease (CHD), deep venous thrombosis, stroke, hip fracture, colorectal cancer, or total mortality after post-intervention follow-up.
Keep in mind that the women in this arm were instructed to discontinue the study medication at the time the intervention phase was halted because of an increased risk of stroke among CEE users. The elevated risk of stroke attenuated with the longer follow-up.
All ages experienced a reduced risk of breast cancer
Some subgroup analyses from the WHI have found differential effects of HT by age of the user, with younger women experiencing fewer risks and more benefits than those who are more than 10 years past the menopausal transition. In this analysis, all three age groups (50–59 years, 60–69 years, and 70–79 years) of women who used CEE had a reduced risk of breast cancer, compared with placebo users.
Other risks did appear to differ by age. For example, the overall hazard ratio for CHD was 0.59 among CEE users 50 to 59 years old, but it approached unity among the older women.
As new and seemingly conflicting data are published, many clinicians and their menopausal patients may feel confused and frustrated. My perspective: It is becoming clear that age during HT use matters with respect to CHD and dementia, and that estrogen-only HT has a different impact on breast cancer risk than does combination estrogen-progestin HT. When this new information from the WHI is considered in aggregate with earlier WHI reports, as well as with data from the Nurses Health Study, the California Teachers Study, and Kaiser Permanente, we can, with growing confidence, advise our patients that menopausal HT does not increase the risk of fatal CHD and may reduce the risk of dementia when used by younger menopausal women with bothersome symptoms. I would define “younger” here as an age younger than 60 years or within 10 years of the onset of menopause.
In regard to breast cancer, it is now clear that, although estrogen-only HT lowers risk, use of combination estrogen-progestin therapy for more than approximately 5 years modestly elevates risk. Each menopausal woman may use this information to make an individual decision regarding use of HT.
In sum, current evidence allows me to feel comfortable counseling most young menopausal women who have bothersome symptoms that the initiation of HT for symptom relief is a safe and reasonable option.
We want to hear from you! Tell us what you think.
1. Rossouw JE, Anderson GL, Prentice RL, et al. Writing Group for the Women’s Health Initiative Investigators. Risks and benefits of estrogen plus progestin in healthy postmenopausal women. Principal results from the Women’s Health Initiative Randomized Controlled Trial. JAMA. 2002;288(3):321-333.
2. Scarabin PY, Oger E, Plu-Bureau G. Estrogen and THromboembolism Risk (ESTHER) Study Group. Differential association of oral and transdermal oestrogen-replacement therapy with venous thromboembolism risk. Lancet. 2003;362(9382):428-432.
3. Anderson GL, Chlebowski RT, Rossouw JE, et al. Prior hormone therapy and breast cancer risk in the Women’s Health Initiative randomized trial of estrogen and progestin. Maturitas. 2006;55(2):103-115.
4. Million Women Study Collaborators. Breast cancer and hormone-replacement therapy in the Million Women Study. Lancet. 2003;362(9382):419-427.
5. Fournier A, Fabre A, Misrine S, et al. Use of different postmenopausal hormone therapies and risk of histology- and hormone receptor-defined invasive breast cancer. J Clin Oncol. 2008;26(8):1260-1268.
6. Nelson HD, Vesco KK, Haney E, et al. Nonhormonal therapies for menopausal hot flashes: systematic review and meta-analysis. JAMA. 2006;295(17):2057-2071.
- Is hormone therapy still a valid option? 12 ObGyns address this question
Members of the OBG MANAGEMENT Virtual Board of Editors and Janelle Yates, Senior Editor (May 2011)
Dr. Kaunitz receives grant or research support from Bayer, Agile, Noven, Teva, and Medical Diagnostic Laboratories, is a consultant to Bayer, Merck, and Teva, and owns stock in Becton Dickinson.
Among the developments of the past year in the care of menopausal women are:
- updated guidelines from the Institute of Medicine regarding vitamin D requirements—suggesting that fewer women are deficient in this nutrient than experts had believed
- new data from Europe on hormone therapy (HT) that highlight the safety of transdermal estrogen in comparison with oral administration
- a recent analysis from the Women’s Health Initiative (WHI), confirming a small elevated risk of breast cancer mortality with use of combination estrogen-progestin HT
- confirmation that age at initiation of HT determines its effect on cardiovascular health
- clarification of the association between HT and dementia
- new data demonstrating modest improvement in hot flushes when the serotonin reuptake inhibitor (SRI) escitalopram is used
- a brand new report from the WHI estrogen-alone arm that shows a protective effect against breast cancer.
The new data on HT suggest that we still have much to learn about its benefits and risks. We also are reaching an understanding that, for many young, symptomatic, menopausal patients, HT can represent a safe choice, with much depending on the timing and duration of therapy.
For more on how your colleagues are managing menopausal patients with and without hormone therapy, see “Is hormone therapy still a valid option? 12 ObGyns address this question,” on the facing page.
Menopausal women need less vitamin D than we thought
Institute of Medicine. Dietary reference intakes for calcium and vitamin D. Washington, DC: IOM; December 2010. http://www.iom.edu/~/media/Files/Report%20Files/2010/Dietary-Reference-Intakes-for-Calcium-and-Vitamin-D/Vitamin%20D%20and%20Calcium%202010%20Report%20Brief.pdf. Accessed March 24, 2011.
In the 2010 Update on Menopause, I summarized recent findings on vitamin D requirements, including recommendations that menopausal women should take at least 800 IU of vitamin D daily. I also described the prevailing expert opinion that many North American women are deficient in this nutrient.
What a difference a year can make! In late November, the Institute of Medicine (IOM) released a comprehensive report on vitamin D. Here are some of its conclusions:
- Vitamin D plays an important role in skeletal health but its role in other areas, including cardiovascular disease and cancer, is uncertain
- An intake of 600 IU of vitamin D daily is appropriate for girls and for women as old as 70 years; an in-take of 800 IU daily is appropriate for women older than 70 years
- A serum level of 25-hydroxy vitamin D of 20 ng/mL is consistent with adequate vitamin D status; this is lower than the threshold many have recommended
- With few exceptions, all people who live in North America—including those who have minimal or no exposure to sunlight—are receiving adequate calcium and vitamin D
- Ingestion of more than 4,000 IU of vitamin D daily can cause renal damage and injure other tissues.
The IOM report will likely prompt multivitamin manufacturers to increase the amount of vitamin D contained in their supplements to 600 IU daily. In addition, the report will probably discourage the common practice of checking serum 25-hydroxy vitamin D levels and prescribing a high dosage of vitamin D supplementation when the level is below 30 ng/mL.
I continue to recommend multivitamin supplements that include calcium and vitamin D (but no iron) to my menopausal patients. However, I no longer routinely recommend that they take additional calcium and vitamin D or undergo assessment of serum vitamin D levels.
Is transdermal estrogen safer than oral administration?
Canonico M, Fournier A, Carcaillon L, et al. Postmenopausal hormone therapy and risk of idiopathic venous thromboembolism: results from the E3N cohort study. Arterioscler Thromb Vasc Biol. 2010;30(2):340–345.
Renoux C, Dell’aniello S, Garbe E, Suissa S. Transdermal and oral hormone replacement therapy and the risk of stroke: a nested case-control study. BMJ. 2010;340:c2519. doi: 10.1136/bmj.c2519.
In the WHI, the combination of oral conjugated equine estrogen and medroxyprogesterone acetate more than doubled the risk of deep venous thrombosis and pulmonary embolism and modestly increased the risk of stroke, compared with nonuse.1
A year after publication of the initial findings of the WHI estrogen-progestin arm, the Estrogen and THromboEmbolism Risk Study Group (ESTHER) case-control study from France provided evidence that transdermal estrogen does not increase the risk of venous thrombosis.2 In France, many menopausal women use HT, and the transdermal route of administration is common.
In 2010, the E3N cohort study from France also assessed the risk of thrombosis associated with oral and transdermal HT. Investigators followed more than 80,000 postmenopausal women and found that, unlike oral HT, the transdermal route did not increase the risk of venous thrombosis.
More recent evidence also suggests a safety advantage for transdermal HT. The newest data come from the United Kingdom General Practice Research Database, which includes information on more than 870,000 women who were 50 to 70 years old from 1987 to 2006. Investigators identified more than 15,000 women who were given a diagnosis of stroke during this period and compared the use of HT in these women with that of almost 60,000 women in a control group. The risk of stroke associated with current use of transdermal HT was similar to the risk associated with nonuse of HT. Women who used a patch containing 0.05 mg of estradiol or less had a risk of stroke 19% lower than women who did not use HT.
In contrast, the risk of stroke in users of patches that contained a higher dosage of estradiol was almost twice the risk in nonusers of HT. Current users of oral HT had a risk of stroke 28% higher than that of nonusers of HT.
The WHI assessed the risks and benefits of oral HT only. Although no randomized, clinical trial has compared cardiovascular risks among users of oral and transdermal HT, I believe that a preponderance of evidence points to a superior safety profile for the transdermal route, particularly at a dosage of 0.05 mg of estradiol or less.
I encourage my patients who are initiating HT to consider the transdermal route—particularly women who have an elevated risk of cardiovascular disease, including those who are overweight, smoke cigarettes, or who have hypertension or diabetes. I suggest the transdermal route despite its higher cost (oral micronized estradiol can be purchased for as little as $4 for a month’s supply at a chain pharmacy).
When a patient prefers to avoid a patch (because of local irritation), I offer her estradiol gel or spray or the vaginal ring. (Femring is systemic estradiol, whereas Estring is local.) These formulations should provide the same safety benefits as the patch.
Estrogen-progestin HT raises the risk of death from breast cancer
Chlebowski RT, Anderson GL, Gass M, et al. Estrogen plus progestin and breast cancer incidence and mortality in postmenopausal women. JAMA. 2010;304(15):1684–1692.
Toh S, Hernandez-Diaz S, Logan R, Rossouw JE, Hernan MA. Coronary heart disease in postmenopausal recipients of estrogen plus progestin: does the increased risk ever disappear? Ann Intern Med. 2010;152(4):211–217.
In the estrogen-progestin arm of the WHI, initially published in 2002, the risk of invasive breast cancer was modestly elevated (hazard ratio [HR], 1.26) among women who had used HT longer than 5 years.3
In 2010, investigators reported on breast cancer mortality in WHI participants at a mean follow-up of 11 years. They found that combination HT users had breast cancer histology similar to that of nonusers. However, the tumors were more likely to be node-positive in combination HT users (23.7% vs 16.2%). In addition, breast cancer mortality was slightly higher among users of HT (2.6 vs 1.3 deaths in every 10,000 woman-years) (HR, 1.96; 95% confidence interval, 1.00–4.04).
Earlier observational studies had suggested that the death rate from breast cancer is lower in users of combination HT than in nonusers. Consistent with the UK Million Women Study, however, a 2010 report from the WHI found a higher mortality rate among women who have used HT.4
These new WHI findings reinforce the importance of assessing whether micronized progesterone combined with estrogen might lower the risk of death from breast cancer—a possibility suggested by findings of the French E3N cohort study.5
In addition, given the possibility that HT may be cardioprotective when it is initiated within 10 years after the onset of menopause, a WHI report that addresses long-term all-cause mortality would allow us to better counsel our menopausal patients who are trying to decide whether to start or continue HT. See, for example, the data from the California Teachers Study (below) and the estrogen-alone arm of the WHI (page 46).
The findings of this important WHI publication have strengthened the resolve of some clinicians to stop prescribing HT for menopausal women. I continue to prescribe HT to patients who have bothersome vasomotor and related symptoms, however. I also counsel women about the other benefits of HT, which include alleviation of genital atrophy and prevention of osteoporotic fractures. For patients considering or using estrogen-progestin HT, I include discussion of the small increase in their risk of developing, and dying from, breast cancer.
Age at initiation of HT determines its effect on CHD
Stram DO, Liu Y, Henderson KD, et al. Age-specific effects of hormone therapy use on overall mortality and ischemic heart disease mortality among women in the California Teachers Study. Menopause 2011;18(3):253-261.
Allison MA, Manson JE. Age, hormone therapy use, coronary heart disease, and mortality [editorial]. Menopause. 2011;18(3):243-245.
The initial findings of the WHI estrogen-progestin arm suggested that menopausal HT increases the risk of CHD. Since then, however, further analyses from the WHI and other HT trials, as well as reports from the observational Nurses’ Health Study, have suggested that the timing of initiation of HT determines its effect on cardiovascular health.
In this study from the California Teachers Study (CTS), investigators explored the effect of age at initiation of HT on cardiovascular and overall mortality. The CTS is a prospective study of more than 133,000 current and retired female teachers and administrators who returned an initial questionnaire in 1995 and 1996. Participants were then followed until late 2004, or death, whichever came first. More than 71,000 participants were eligible for analysis.
Current HT users were leaner, less likely to smoke, and more likely to exercise and consume alcohol than nonusers were. The analysis was adjusted for a variety of potential cardiovascular and other confounders.
Youngest HT users had the lowest risk of death
During follow-up, 18.3% of never-users of HT died, compared with 17.9% of former users. In contrast, 6.9% of women taking HT at the time of the baseline questionnaire died during follow-up.
Overall, current HT use was associated with a reduced risk of death from CHD (hazard ratio [HR], 0.84; 95% confidence interval, 0.74–0.95). This risk reduction was most notable (HR, 0.38) in the youngest HT users (36 to 59 years old). The risk of death from CHD gradually increased with the age of current HT users, reaching a hazard ratio of approximately 0.9 in current users who were 70 years and older. However, the CHD mortality hazard ratio did not reach or exceed the referent hazard ratio (1.0) assigned to never users of HT of any age.
The overall mortality rate was lowest for the youngest HT users (HR, 0.54) and approached 1.0 in the oldest current HT users.
The associations between overall and CHD mortality were similar among users of estrogen-only and estrogen-progestin HT.
As Allison and Manson point out in an editorial accompanying this study, the findings from the CTS are congruent with an extensive body of evidence from women and nonhuman primates. These data provide robust reassurance that HT does not increase the risk of death from CHD when it is used by recently menopausal women who have bothersome vasomotor symptoms.
Hormone therapy and dementia: Earlier use is better
Whitmer RA, Quesenberry CP, Zhou J, Yaffe K. Timing of hormone therapy and dementia: the critical window theory revisited. Ann Neurol. 2011;69(1):163–169.
Alzheimer’s disease is more common among women than men. In addition, caregivers to those who have dementia are more likely to be women. Therefore, it’s no surprise that women are especially concerned about their risk of dementia. Menopausal patients in my practice often ask whether use of HT might alter this risk.
Because vasomotor symptoms usually arise in late perimenopause or early menopause, women in observational studies (which reflect clinical practice) tend to begin HT when they are in their late 40s or early 50s. Overall, observational studies have suggested that HT is associated with a reduced risk of dementia. In contrast, the WHI clinical trial, in which the mean age of women who were randomized to HT or placebo was 63 years, found that the initiation of HT later in life increased the risk of dementia.
These observations led to the “critical window” theory regarding HT and dementia: Estrogen protects against dementia when it is taken by perimenopausal or early menopausal women, whereas it is not protective and may even accelerate cognitive decline when it is started many years after the onset of menopause.
In this recent study from the California Kaiser Permanente health maintenance organization, investigators assessed the long-term risk of dementia by timing of HT. From 1964 through 1973, menopausal “midlife” women who were 40 to 55 years old and free of dementia reported whether or not they used HT. Twenty-five to 30 years later, participants were reassessed for “late life” HT use.
Women who used HT in midlife only had the lowest prevalence of dementia, whereas those who used HT only in late life had the highest prevalence. Women who used HT at both time points had a prevalence of dementia similar to that of women who had never used HT.
Given these important findings, I believe it is now reasonable to counsel women in late perimenopause and early menopause that the use of HT may lower their risk of dementia. How long we should continue to prescribe HT depends on individual variables, including the presence of vasomotor symptoms, the risk of osteoporosis, and concerns about breast cancer.
I encourage women to taper their dosage of HT over time, aiming at complete discontinuation or a low maintenance dosage.
Are SRIs an effective alternative to HT for hot flushes?
Freeman EW, Guthrie K, Caan B, et al. Efficacy of escitalopram for hot flashes in healthy menopausal women: a randomized controlled trial. JAMA. 2011;305(3):267–274.
Interest in nonhormonal management of menopausal vasomotor symptoms continues to run high, although only hormonal therapy has FDA approval for this indication. Many trials of serotonin reuptake inhibitors (SRIs) for the treatment of vasomotor symptoms have focused on breast cancer survivors, many of whom use anti-estrogen agents that increase the prevalence of these symptoms. In contrast, this well-conducted multicenter trial, funded by the National Institutes of Health, enrolled healthy, symptomatic, menopausal women.
In the trial, 205 perimenopausal or postmenopausal women 40 to 62 years old who had at least 28 bothersome or severe episodes of hot flushes and night sweats a week were randomized to 10 mg daily of the SRI escitalopram (Lexapro) or placebo for 8 weeks. Women who did not report a reduction in hot flushes and night sweats of at least 50% at 4 weeks, or a decrease in the severity of these symptoms, were increased to a dosage of 20 mg daily of escitalopram or placebo. The mean baseline frequency of vasomotor symptoms was 9.79.
Within 1 week, women taking the SRI experienced significantly greater improvement than those taking placebo. By 8 weeks, the daily frequency of vasomotor symptoms had diminished by 4.6 hot flushes among women taking the SRI, compared with 3.20 among women taking placebo (P < .01).
Overall, adverse effects were reported by approximately 58% of participants. The pattern of these side effects was similar in the active and placebo treatment arms. No adverse events serious enough to require withdrawal from the study were reported in either arm.
Patient satisfaction with treatment was 70% in the SRI group, compared with 43% among women taking placebo (P < .001).
Although Freeman and colleagues convincingly demonstrate that escitalopram is more effective than placebo, the drug is less effective than HT. I agree with Nelson and coworkers, who, in a meta-analysis of nonhormonal treatments for vasomotor symptoms, concluded: “These therapies may be most useful for highly symptomatic women who cannot take estrogen but are not optimal choices for most women.”6
Unopposed estrogen appears to protect against breast cancer
LaCroix AZ, Chlebowski RT, Manson JE, et al; WHI Investigators. Health outcomes after stopping conjugated equine estrogens among postmenopausal women with prior hysterectomy. A randomized controlled trial. JAMA. 2011;305(13):1305–1314.
The WHI continues to surprise with its findings almost a decade after publication of initial data. In this brand new report from the estrogen-alone arm, postmenopausal, hysterectomized women who were followed for a mean of 10.7 years experienced a reduced risk of breast cancer after a mean of 5.9 years of use of conjugated equine estrogens (CEE).
They experienced no increased or diminished risk of coronary heart disease (CHD), deep venous thrombosis, stroke, hip fracture, colorectal cancer, or total mortality after post-intervention follow-up.
Keep in mind that the women in this arm were instructed to discontinue the study medication at the time the intervention phase was halted because of an increased risk of stroke among CEE users. The elevated risk of stroke attenuated with the longer follow-up.
All ages experienced a reduced risk of breast cancer
Some subgroup analyses from the WHI have found differential effects of HT by age of the user, with younger women experiencing fewer risks and more benefits than those who are more than 10 years past the menopausal transition. In this analysis, all three age groups (50–59 years, 60–69 years, and 70–79 years) of women who used CEE had a reduced risk of breast cancer, compared with placebo users.
Other risks did appear to differ by age. For example, the overall hazard ratio for CHD was 0.59 among CEE users 50 to 59 years old, but it approached unity among the older women.
As new and seemingly conflicting data are published, many clinicians and their menopausal patients may feel confused and frustrated. My perspective: It is becoming clear that age during HT use matters with respect to CHD and dementia, and that estrogen-only HT has a different impact on breast cancer risk than does combination estrogen-progestin HT. When this new information from the WHI is considered in aggregate with earlier WHI reports, as well as with data from the Nurses Health Study, the California Teachers Study, and Kaiser Permanente, we can, with growing confidence, advise our patients that menopausal HT does not increase the risk of fatal CHD and may reduce the risk of dementia when used by younger menopausal women with bothersome symptoms. I would define “younger” here as an age younger than 60 years or within 10 years of the onset of menopause.
In regard to breast cancer, it is now clear that, although estrogen-only HT lowers risk, use of combination estrogen-progestin therapy for more than approximately 5 years modestly elevates risk. Each menopausal woman may use this information to make an individual decision regarding use of HT.
In sum, current evidence allows me to feel comfortable counseling most young menopausal women who have bothersome symptoms that the initiation of HT for symptom relief is a safe and reasonable option.
We want to hear from you! Tell us what you think.
- Is hormone therapy still a valid option? 12 ObGyns address this question
Members of the OBG MANAGEMENT Virtual Board of Editors and Janelle Yates, Senior Editor (May 2011)
Dr. Kaunitz receives grant or research support from Bayer, Agile, Noven, Teva, and Medical Diagnostic Laboratories, is a consultant to Bayer, Merck, and Teva, and owns stock in Becton Dickinson.
Among the developments of the past year in the care of menopausal women are:
- updated guidelines from the Institute of Medicine regarding vitamin D requirements—suggesting that fewer women are deficient in this nutrient than experts had believed
- new data from Europe on hormone therapy (HT) that highlight the safety of transdermal estrogen in comparison with oral administration
- a recent analysis from the Women’s Health Initiative (WHI), confirming a small elevated risk of breast cancer mortality with use of combination estrogen-progestin HT
- confirmation that age at initiation of HT determines its effect on cardiovascular health
- clarification of the association between HT and dementia
- new data demonstrating modest improvement in hot flushes when the serotonin reuptake inhibitor (SRI) escitalopram is used
- a brand new report from the WHI estrogen-alone arm that shows a protective effect against breast cancer.
The new data on HT suggest that we still have much to learn about its benefits and risks. We also are reaching an understanding that, for many young, symptomatic, menopausal patients, HT can represent a safe choice, with much depending on the timing and duration of therapy.
For more on how your colleagues are managing menopausal patients with and without hormone therapy, see “Is hormone therapy still a valid option? 12 ObGyns address this question,” on the facing page.
Menopausal women need less vitamin D than we thought
Institute of Medicine. Dietary reference intakes for calcium and vitamin D. Washington, DC: IOM; December 2010. http://www.iom.edu/~/media/Files/Report%20Files/2010/Dietary-Reference-Intakes-for-Calcium-and-Vitamin-D/Vitamin%20D%20and%20Calcium%202010%20Report%20Brief.pdf. Accessed March 24, 2011.
In the 2010 Update on Menopause, I summarized recent findings on vitamin D requirements, including recommendations that menopausal women should take at least 800 IU of vitamin D daily. I also described the prevailing expert opinion that many North American women are deficient in this nutrient.
What a difference a year can make! In late November, the Institute of Medicine (IOM) released a comprehensive report on vitamin D. Here are some of its conclusions:
- Vitamin D plays an important role in skeletal health but its role in other areas, including cardiovascular disease and cancer, is uncertain
- An intake of 600 IU of vitamin D daily is appropriate for girls and for women as old as 70 years; an in-take of 800 IU daily is appropriate for women older than 70 years
- A serum level of 25-hydroxy vitamin D of 20 ng/mL is consistent with adequate vitamin D status; this is lower than the threshold many have recommended
- With few exceptions, all people who live in North America—including those who have minimal or no exposure to sunlight—are receiving adequate calcium and vitamin D
- Ingestion of more than 4,000 IU of vitamin D daily can cause renal damage and injure other tissues.
The IOM report will likely prompt multivitamin manufacturers to increase the amount of vitamin D contained in their supplements to 600 IU daily. In addition, the report will probably discourage the common practice of checking serum 25-hydroxy vitamin D levels and prescribing a high dosage of vitamin D supplementation when the level is below 30 ng/mL.
I continue to recommend multivitamin supplements that include calcium and vitamin D (but no iron) to my menopausal patients. However, I no longer routinely recommend that they take additional calcium and vitamin D or undergo assessment of serum vitamin D levels.
Is transdermal estrogen safer than oral administration?
Canonico M, Fournier A, Carcaillon L, et al. Postmenopausal hormone therapy and risk of idiopathic venous thromboembolism: results from the E3N cohort study. Arterioscler Thromb Vasc Biol. 2010;30(2):340–345.
Renoux C, Dell’aniello S, Garbe E, Suissa S. Transdermal and oral hormone replacement therapy and the risk of stroke: a nested case-control study. BMJ. 2010;340:c2519. doi: 10.1136/bmj.c2519.
In the WHI, the combination of oral conjugated equine estrogen and medroxyprogesterone acetate more than doubled the risk of deep venous thrombosis and pulmonary embolism and modestly increased the risk of stroke, compared with nonuse.1
A year after publication of the initial findings of the WHI estrogen-progestin arm, the Estrogen and THromboEmbolism Risk Study Group (ESTHER) case-control study from France provided evidence that transdermal estrogen does not increase the risk of venous thrombosis.2 In France, many menopausal women use HT, and the transdermal route of administration is common.
In 2010, the E3N cohort study from France also assessed the risk of thrombosis associated with oral and transdermal HT. Investigators followed more than 80,000 postmenopausal women and found that, unlike oral HT, the transdermal route did not increase the risk of venous thrombosis.
More recent evidence also suggests a safety advantage for transdermal HT. The newest data come from the United Kingdom General Practice Research Database, which includes information on more than 870,000 women who were 50 to 70 years old from 1987 to 2006. Investigators identified more than 15,000 women who were given a diagnosis of stroke during this period and compared the use of HT in these women with that of almost 60,000 women in a control group. The risk of stroke associated with current use of transdermal HT was similar to the risk associated with nonuse of HT. Women who used a patch containing 0.05 mg of estradiol or less had a risk of stroke 19% lower than women who did not use HT.
In contrast, the risk of stroke in users of patches that contained a higher dosage of estradiol was almost twice the risk in nonusers of HT. Current users of oral HT had a risk of stroke 28% higher than that of nonusers of HT.
The WHI assessed the risks and benefits of oral HT only. Although no randomized, clinical trial has compared cardiovascular risks among users of oral and transdermal HT, I believe that a preponderance of evidence points to a superior safety profile for the transdermal route, particularly at a dosage of 0.05 mg of estradiol or less.
I encourage my patients who are initiating HT to consider the transdermal route—particularly women who have an elevated risk of cardiovascular disease, including those who are overweight, smoke cigarettes, or who have hypertension or diabetes. I suggest the transdermal route despite its higher cost (oral micronized estradiol can be purchased for as little as $4 for a month’s supply at a chain pharmacy).
When a patient prefers to avoid a patch (because of local irritation), I offer her estradiol gel or spray or the vaginal ring. (Femring is systemic estradiol, whereas Estring is local.) These formulations should provide the same safety benefits as the patch.
Estrogen-progestin HT raises the risk of death from breast cancer
Chlebowski RT, Anderson GL, Gass M, et al. Estrogen plus progestin and breast cancer incidence and mortality in postmenopausal women. JAMA. 2010;304(15):1684–1692.
Toh S, Hernandez-Diaz S, Logan R, Rossouw JE, Hernan MA. Coronary heart disease in postmenopausal recipients of estrogen plus progestin: does the increased risk ever disappear? Ann Intern Med. 2010;152(4):211–217.
In the estrogen-progestin arm of the WHI, initially published in 2002, the risk of invasive breast cancer was modestly elevated (hazard ratio [HR], 1.26) among women who had used HT longer than 5 years.3
In 2010, investigators reported on breast cancer mortality in WHI participants at a mean follow-up of 11 years. They found that combination HT users had breast cancer histology similar to that of nonusers. However, the tumors were more likely to be node-positive in combination HT users (23.7% vs 16.2%). In addition, breast cancer mortality was slightly higher among users of HT (2.6 vs 1.3 deaths in every 10,000 woman-years) (HR, 1.96; 95% confidence interval, 1.00–4.04).
Earlier observational studies had suggested that the death rate from breast cancer is lower in users of combination HT than in nonusers. Consistent with the UK Million Women Study, however, a 2010 report from the WHI found a higher mortality rate among women who have used HT.4
These new WHI findings reinforce the importance of assessing whether micronized progesterone combined with estrogen might lower the risk of death from breast cancer—a possibility suggested by findings of the French E3N cohort study.5
In addition, given the possibility that HT may be cardioprotective when it is initiated within 10 years after the onset of menopause, a WHI report that addresses long-term all-cause mortality would allow us to better counsel our menopausal patients who are trying to decide whether to start or continue HT. See, for example, the data from the California Teachers Study (below) and the estrogen-alone arm of the WHI (page 46).
The findings of this important WHI publication have strengthened the resolve of some clinicians to stop prescribing HT for menopausal women. I continue to prescribe HT to patients who have bothersome vasomotor and related symptoms, however. I also counsel women about the other benefits of HT, which include alleviation of genital atrophy and prevention of osteoporotic fractures. For patients considering or using estrogen-progestin HT, I include discussion of the small increase in their risk of developing, and dying from, breast cancer.
Age at initiation of HT determines its effect on CHD
Stram DO, Liu Y, Henderson KD, et al. Age-specific effects of hormone therapy use on overall mortality and ischemic heart disease mortality among women in the California Teachers Study. Menopause 2011;18(3):253-261.
Allison MA, Manson JE. Age, hormone therapy use, coronary heart disease, and mortality [editorial]. Menopause. 2011;18(3):243-245.
The initial findings of the WHI estrogen-progestin arm suggested that menopausal HT increases the risk of CHD. Since then, however, further analyses from the WHI and other HT trials, as well as reports from the observational Nurses’ Health Study, have suggested that the timing of initiation of HT determines its effect on cardiovascular health.
In this study from the California Teachers Study (CTS), investigators explored the effect of age at initiation of HT on cardiovascular and overall mortality. The CTS is a prospective study of more than 133,000 current and retired female teachers and administrators who returned an initial questionnaire in 1995 and 1996. Participants were then followed until late 2004, or death, whichever came first. More than 71,000 participants were eligible for analysis.
Current HT users were leaner, less likely to smoke, and more likely to exercise and consume alcohol than nonusers were. The analysis was adjusted for a variety of potential cardiovascular and other confounders.
Youngest HT users had the lowest risk of death
During follow-up, 18.3% of never-users of HT died, compared with 17.9% of former users. In contrast, 6.9% of women taking HT at the time of the baseline questionnaire died during follow-up.
Overall, current HT use was associated with a reduced risk of death from CHD (hazard ratio [HR], 0.84; 95% confidence interval, 0.74–0.95). This risk reduction was most notable (HR, 0.38) in the youngest HT users (36 to 59 years old). The risk of death from CHD gradually increased with the age of current HT users, reaching a hazard ratio of approximately 0.9 in current users who were 70 years and older. However, the CHD mortality hazard ratio did not reach or exceed the referent hazard ratio (1.0) assigned to never users of HT of any age.
The overall mortality rate was lowest for the youngest HT users (HR, 0.54) and approached 1.0 in the oldest current HT users.
The associations between overall and CHD mortality were similar among users of estrogen-only and estrogen-progestin HT.
As Allison and Manson point out in an editorial accompanying this study, the findings from the CTS are congruent with an extensive body of evidence from women and nonhuman primates. These data provide robust reassurance that HT does not increase the risk of death from CHD when it is used by recently menopausal women who have bothersome vasomotor symptoms.
Hormone therapy and dementia: Earlier use is better
Whitmer RA, Quesenberry CP, Zhou J, Yaffe K. Timing of hormone therapy and dementia: the critical window theory revisited. Ann Neurol. 2011;69(1):163–169.
Alzheimer’s disease is more common among women than men. In addition, caregivers to those who have dementia are more likely to be women. Therefore, it’s no surprise that women are especially concerned about their risk of dementia. Menopausal patients in my practice often ask whether use of HT might alter this risk.
Because vasomotor symptoms usually arise in late perimenopause or early menopause, women in observational studies (which reflect clinical practice) tend to begin HT when they are in their late 40s or early 50s. Overall, observational studies have suggested that HT is associated with a reduced risk of dementia. In contrast, the WHI clinical trial, in which the mean age of women who were randomized to HT or placebo was 63 years, found that the initiation of HT later in life increased the risk of dementia.
These observations led to the “critical window” theory regarding HT and dementia: Estrogen protects against dementia when it is taken by perimenopausal or early menopausal women, whereas it is not protective and may even accelerate cognitive decline when it is started many years after the onset of menopause.
In this recent study from the California Kaiser Permanente health maintenance organization, investigators assessed the long-term risk of dementia by timing of HT. From 1964 through 1973, menopausal “midlife” women who were 40 to 55 years old and free of dementia reported whether or not they used HT. Twenty-five to 30 years later, participants were reassessed for “late life” HT use.
Women who used HT in midlife only had the lowest prevalence of dementia, whereas those who used HT only in late life had the highest prevalence. Women who used HT at both time points had a prevalence of dementia similar to that of women who had never used HT.
Given these important findings, I believe it is now reasonable to counsel women in late perimenopause and early menopause that the use of HT may lower their risk of dementia. How long we should continue to prescribe HT depends on individual variables, including the presence of vasomotor symptoms, the risk of osteoporosis, and concerns about breast cancer.
I encourage women to taper their dosage of HT over time, aiming at complete discontinuation or a low maintenance dosage.
Are SRIs an effective alternative to HT for hot flushes?
Freeman EW, Guthrie K, Caan B, et al. Efficacy of escitalopram for hot flashes in healthy menopausal women: a randomized controlled trial. JAMA. 2011;305(3):267–274.
Interest in nonhormonal management of menopausal vasomotor symptoms continues to run high, although only hormonal therapy has FDA approval for this indication. Many trials of serotonin reuptake inhibitors (SRIs) for the treatment of vasomotor symptoms have focused on breast cancer survivors, many of whom use anti-estrogen agents that increase the prevalence of these symptoms. In contrast, this well-conducted multicenter trial, funded by the National Institutes of Health, enrolled healthy, symptomatic, menopausal women.
In the trial, 205 perimenopausal or postmenopausal women 40 to 62 years old who had at least 28 bothersome or severe episodes of hot flushes and night sweats a week were randomized to 10 mg daily of the SRI escitalopram (Lexapro) or placebo for 8 weeks. Women who did not report a reduction in hot flushes and night sweats of at least 50% at 4 weeks, or a decrease in the severity of these symptoms, were increased to a dosage of 20 mg daily of escitalopram or placebo. The mean baseline frequency of vasomotor symptoms was 9.79.
Within 1 week, women taking the SRI experienced significantly greater improvement than those taking placebo. By 8 weeks, the daily frequency of vasomotor symptoms had diminished by 4.6 hot flushes among women taking the SRI, compared with 3.20 among women taking placebo (P < .01).
Overall, adverse effects were reported by approximately 58% of participants. The pattern of these side effects was similar in the active and placebo treatment arms. No adverse events serious enough to require withdrawal from the study were reported in either arm.
Patient satisfaction with treatment was 70% in the SRI group, compared with 43% among women taking placebo (P < .001).
Although Freeman and colleagues convincingly demonstrate that escitalopram is more effective than placebo, the drug is less effective than HT. I agree with Nelson and coworkers, who, in a meta-analysis of nonhormonal treatments for vasomotor symptoms, concluded: “These therapies may be most useful for highly symptomatic women who cannot take estrogen but are not optimal choices for most women.”6
Unopposed estrogen appears to protect against breast cancer
LaCroix AZ, Chlebowski RT, Manson JE, et al; WHI Investigators. Health outcomes after stopping conjugated equine estrogens among postmenopausal women with prior hysterectomy. A randomized controlled trial. JAMA. 2011;305(13):1305–1314.
The WHI continues to surprise with its findings almost a decade after publication of initial data. In this brand new report from the estrogen-alone arm, postmenopausal, hysterectomized women who were followed for a mean of 10.7 years experienced a reduced risk of breast cancer after a mean of 5.9 years of use of conjugated equine estrogens (CEE).
They experienced no increased or diminished risk of coronary heart disease (CHD), deep venous thrombosis, stroke, hip fracture, colorectal cancer, or total mortality after post-intervention follow-up.
Keep in mind that the women in this arm were instructed to discontinue the study medication at the time the intervention phase was halted because of an increased risk of stroke among CEE users. The elevated risk of stroke attenuated with the longer follow-up.
All ages experienced a reduced risk of breast cancer
Some subgroup analyses from the WHI have found differential effects of HT by age of the user, with younger women experiencing fewer risks and more benefits than those who are more than 10 years past the menopausal transition. In this analysis, all three age groups (50–59 years, 60–69 years, and 70–79 years) of women who used CEE had a reduced risk of breast cancer, compared with placebo users.
Other risks did appear to differ by age. For example, the overall hazard ratio for CHD was 0.59 among CEE users 50 to 59 years old, but it approached unity among the older women.
As new and seemingly conflicting data are published, many clinicians and their menopausal patients may feel confused and frustrated. My perspective: It is becoming clear that age during HT use matters with respect to CHD and dementia, and that estrogen-only HT has a different impact on breast cancer risk than does combination estrogen-progestin HT. When this new information from the WHI is considered in aggregate with earlier WHI reports, as well as with data from the Nurses Health Study, the California Teachers Study, and Kaiser Permanente, we can, with growing confidence, advise our patients that menopausal HT does not increase the risk of fatal CHD and may reduce the risk of dementia when used by younger menopausal women with bothersome symptoms. I would define “younger” here as an age younger than 60 years or within 10 years of the onset of menopause.
In regard to breast cancer, it is now clear that, although estrogen-only HT lowers risk, use of combination estrogen-progestin therapy for more than approximately 5 years modestly elevates risk. Each menopausal woman may use this information to make an individual decision regarding use of HT.
In sum, current evidence allows me to feel comfortable counseling most young menopausal women who have bothersome symptoms that the initiation of HT for symptom relief is a safe and reasonable option.
We want to hear from you! Tell us what you think.
1. Rossouw JE, Anderson GL, Prentice RL, et al. Writing Group for the Women’s Health Initiative Investigators. Risks and benefits of estrogen plus progestin in healthy postmenopausal women. Principal results from the Women’s Health Initiative Randomized Controlled Trial. JAMA. 2002;288(3):321-333.
2. Scarabin PY, Oger E, Plu-Bureau G. Estrogen and THromboembolism Risk (ESTHER) Study Group. Differential association of oral and transdermal oestrogen-replacement therapy with venous thromboembolism risk. Lancet. 2003;362(9382):428-432.
3. Anderson GL, Chlebowski RT, Rossouw JE, et al. Prior hormone therapy and breast cancer risk in the Women’s Health Initiative randomized trial of estrogen and progestin. Maturitas. 2006;55(2):103-115.
4. Million Women Study Collaborators. Breast cancer and hormone-replacement therapy in the Million Women Study. Lancet. 2003;362(9382):419-427.
5. Fournier A, Fabre A, Misrine S, et al. Use of different postmenopausal hormone therapies and risk of histology- and hormone receptor-defined invasive breast cancer. J Clin Oncol. 2008;26(8):1260-1268.
6. Nelson HD, Vesco KK, Haney E, et al. Nonhormonal therapies for menopausal hot flashes: systematic review and meta-analysis. JAMA. 2006;295(17):2057-2071.
1. Rossouw JE, Anderson GL, Prentice RL, et al. Writing Group for the Women’s Health Initiative Investigators. Risks and benefits of estrogen plus progestin in healthy postmenopausal women. Principal results from the Women’s Health Initiative Randomized Controlled Trial. JAMA. 2002;288(3):321-333.
2. Scarabin PY, Oger E, Plu-Bureau G. Estrogen and THromboembolism Risk (ESTHER) Study Group. Differential association of oral and transdermal oestrogen-replacement therapy with venous thromboembolism risk. Lancet. 2003;362(9382):428-432.
3. Anderson GL, Chlebowski RT, Rossouw JE, et al. Prior hormone therapy and breast cancer risk in the Women’s Health Initiative randomized trial of estrogen and progestin. Maturitas. 2006;55(2):103-115.
4. Million Women Study Collaborators. Breast cancer and hormone-replacement therapy in the Million Women Study. Lancet. 2003;362(9382):419-427.
5. Fournier A, Fabre A, Misrine S, et al. Use of different postmenopausal hormone therapies and risk of histology- and hormone receptor-defined invasive breast cancer. J Clin Oncol. 2008;26(8):1260-1268.
6. Nelson HD, Vesco KK, Haney E, et al. Nonhormonal therapies for menopausal hot flashes: systematic review and meta-analysis. JAMA. 2006;295(17):2057-2071.
