User login
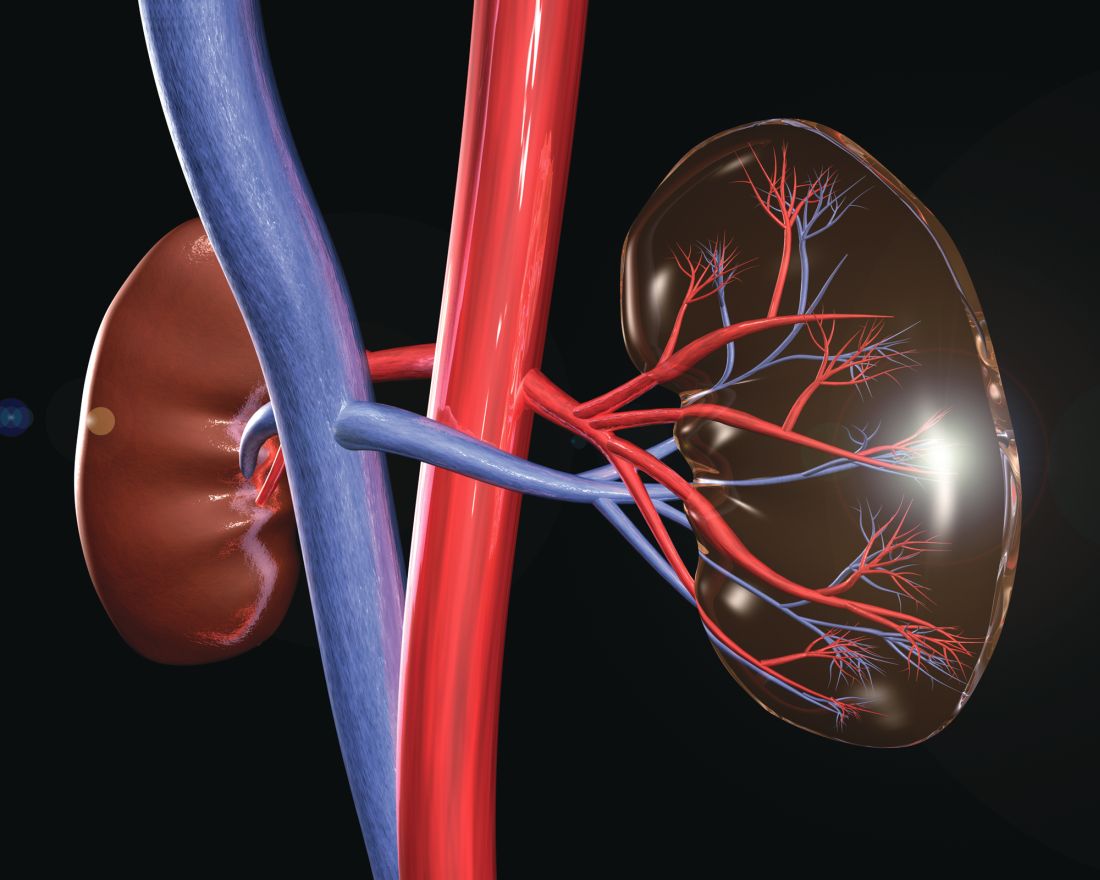
Transplanting a kidney infected with hepatitis C into individuals infected with HCV, followed by treatment, was more effective and less costly than transplanting an uninfected kidney, preceded by HCV treatment, according to Mark H. Eckman, MD, of the University of Cincinnati and his colleagues.
Largely because of the longer wait times for uninfected kidneys, a typical patient aged 58 years on hemodialysis would gain an average of 0.5 quality-adjusted life-years at a lifetime cost savings of $41,591 dollars, according to the model.
“In an era of increasing success for kidney transplants and demand that far outstrips supply, deferring antiviral therapy until after transplant of HCV-infected kidneys, when available, should be both cost saving and effective,” the researchers wrote.
The study was funded by grants from Merck Sharpe & Dohme and the National Center for Advancing Translational Science. Several of the authors reported having grants from Merck and grants and personal fees from a variety of other pharmaceutical companies.
SOURCE: Eckman MH et al. Ann Intern Med. 2018 Jul 10. doi: 10.7326/M17-3088.
Transplanting a kidney infected with hepatitis C into individuals infected with HCV, followed by treatment, was more effective and less costly than transplanting an uninfected kidney, preceded by HCV treatment, according to Mark H. Eckman, MD, of the University of Cincinnati and his colleagues.
Largely because of the longer wait times for uninfected kidneys, a typical patient aged 58 years on hemodialysis would gain an average of 0.5 quality-adjusted life-years at a lifetime cost savings of $41,591 dollars, according to the model.
“In an era of increasing success for kidney transplants and demand that far outstrips supply, deferring antiviral therapy until after transplant of HCV-infected kidneys, when available, should be both cost saving and effective,” the researchers wrote.
The study was funded by grants from Merck Sharpe & Dohme and the National Center for Advancing Translational Science. Several of the authors reported having grants from Merck and grants and personal fees from a variety of other pharmaceutical companies.
SOURCE: Eckman MH et al. Ann Intern Med. 2018 Jul 10. doi: 10.7326/M17-3088.
Transplanting a kidney infected with hepatitis C into individuals infected with HCV, followed by treatment, was more effective and less costly than transplanting an uninfected kidney, preceded by HCV treatment, according to Mark H. Eckman, MD, of the University of Cincinnati and his colleagues.
Largely because of the longer wait times for uninfected kidneys, a typical patient aged 58 years on hemodialysis would gain an average of 0.5 quality-adjusted life-years at a lifetime cost savings of $41,591 dollars, according to the model.
“In an era of increasing success for kidney transplants and demand that far outstrips supply, deferring antiviral therapy until after transplant of HCV-infected kidneys, when available, should be both cost saving and effective,” the researchers wrote.
The study was funded by grants from Merck Sharpe & Dohme and the National Center for Advancing Translational Science. Several of the authors reported having grants from Merck and grants and personal fees from a variety of other pharmaceutical companies.
SOURCE: Eckman MH et al. Ann Intern Med. 2018 Jul 10. doi: 10.7326/M17-3088.
FROM ANNALS OF INTERNAL MEDICINE