User login
BALTIMORE – Tumor size and the presence of mutations of the succinate dehydrogenase complex subunit B (SDHB) gene may be reliable indicators of prognosis after surgery for pheochromocytoma and abdominal paraganglioma, investigators in a National Cancer Institute–funded study have reported.
“The staging of pheochromocytoma and abdominal paraganglioma can be difficult, but it is critical for optimal patient care,” Yasmine Assadipour, MD, of the National Cancer Institute, Bethesda, Md., and the George Washington University Hospital, Washington, reported at the annual meeting of the American Association of Endocrine Surgeons.
“Any clinically relevant grading or prognostic system should include SDHB mutation status and primary tumor size as prime features of scoring,” Dr. Assadipour said. “Histologic features such as Ki-67 or mitotic index may not be as useful for prognostic information in patients with pheochromocytoma and abdominal paraganglioma, particularly in the setting of SDHB mutation.”
Dr. Assadipour and her coinvestigators focused their investigation on mutations of the SDHB (succinate dehydrogenase complex subunit B) gene, which codes for one of four subunits comprising a mitochondrial protein.
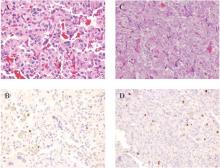
They also considered primary tumor size, functionality, pathology, surgical approach, and histologic features including Ki-67 index and mitotic index. The study was a retrospective analysis of 84 patients who had surgery for PC [pheochromocytoma] or PGL [paraganglioma] and had germ line genetic testing. Of the 84 patients, 35 patients had sporadic disease and 49 had germ line SDHB mutation. The study analyzed tumor samples for Ki-67/MIB-1 staining and mitotic index.
“In a univariate analysis, SDHB mutation, tumor size and surgical approach were associated with local regional recurrence,” Dr. Assadipour said. “In a multivariate analysis, the only independent risk factors were SDHB mutation status and tumor size; Ki-67 and mitotic index did not have any association with recurrence.”
The researchers found similar results when they looked at distant metastasis. “SDHB mutation, tumor size, abdominal paraganglioma and surgical approach were associated with distant metastasis,” Dr. Assadipour said. “Again, Ki-67 and mitotic index were not.”
In the multivariate analysis, again, only patient SDHB status and tumor size were independently associated with metastasis.”
The incidence of local recurrence in patients with the SDHB mutation was 47.6% vs. 9.1% in those without the gene mutation, Dr. Assadipour said. The rates of distant metastasis showed a similar disparity: 56.5% and 9.1%, respectively.
Patients with the SDHB mutation presented at a younger age than those without the mutation, 33 vs. 49.6 years old. Among the 65 patients who underwent R0 primary tumor resection, those with the SDHB mutation, paraganglioma, and larger tumor size had a shorter disease-free survival, Dr. Assadipour said.
In analyzing tumor size, Dr. Assadipour said two stratifications were studied: evaluating tumors sized 0-3 cm, 3-6 cm and 6 cm and larger; and 0-5 cm and 5 cm and larger. “Tumors over 6 cm had the shortest disease-free survival, and even when we applied the under-5 cm and over-5 cm scale, we clearly saw a difference in disease-free survival,” she said. Ki-67 and mitotic index were not related to disease-free survival.
The presence of a SDHB mutation had a hazard ratio of 16.2, while tumor diameter greater than 6 cm had a HR of 15.4, Dr. Assadipour said. These were the only independent risk factors for local recurrence, distant metastases and shorter disease-free interval found in the study.
During the discussion, Lawrence T. Kim, MD, of the University of North Carolina asked if the researchers found any differences in outcomes related to the surgical approach. “We were unable to identify whether any surgical approach improved or worsened outcomes on multivariate analysis” Dr. Assadipour said.
Thomas J. Fahey, MD, of New York asked what she would recommend for surgical approaches for patients with PC and PGL.
“Our general recommendation is that an adrenal pheochromocytoma that is over 6 cm carries a higher risk of recurrence and distant metastasis so an open approach with lymph node dissection ensuring negative surgical margins should be considered,” Dr. Assadipour said. “For abdominal paragangliomas, unless they are quite small and in a favorable location, we would generally recommend an open approach.”
The study was supported by the intramural program of the Center for Cancer Research, National Cancer Institute, National Institutes of Health. Dr. Assadipour and her coauthors had no financial relationships to disclose.
BALTIMORE – Tumor size and the presence of mutations of the succinate dehydrogenase complex subunit B (SDHB) gene may be reliable indicators of prognosis after surgery for pheochromocytoma and abdominal paraganglioma, investigators in a National Cancer Institute–funded study have reported.
“The staging of pheochromocytoma and abdominal paraganglioma can be difficult, but it is critical for optimal patient care,” Yasmine Assadipour, MD, of the National Cancer Institute, Bethesda, Md., and the George Washington University Hospital, Washington, reported at the annual meeting of the American Association of Endocrine Surgeons.
“Any clinically relevant grading or prognostic system should include SDHB mutation status and primary tumor size as prime features of scoring,” Dr. Assadipour said. “Histologic features such as Ki-67 or mitotic index may not be as useful for prognostic information in patients with pheochromocytoma and abdominal paraganglioma, particularly in the setting of SDHB mutation.”
Dr. Assadipour and her coinvestigators focused their investigation on mutations of the SDHB (succinate dehydrogenase complex subunit B) gene, which codes for one of four subunits comprising a mitochondrial protein.
They also considered primary tumor size, functionality, pathology, surgical approach, and histologic features including Ki-67 index and mitotic index. The study was a retrospective analysis of 84 patients who had surgery for PC [pheochromocytoma] or PGL [paraganglioma] and had germ line genetic testing. Of the 84 patients, 35 patients had sporadic disease and 49 had germ line SDHB mutation. The study analyzed tumor samples for Ki-67/MIB-1 staining and mitotic index.
“In a univariate analysis, SDHB mutation, tumor size and surgical approach were associated with local regional recurrence,” Dr. Assadipour said. “In a multivariate analysis, the only independent risk factors were SDHB mutation status and tumor size; Ki-67 and mitotic index did not have any association with recurrence.”
The researchers found similar results when they looked at distant metastasis. “SDHB mutation, tumor size, abdominal paraganglioma and surgical approach were associated with distant metastasis,” Dr. Assadipour said. “Again, Ki-67 and mitotic index were not.”
In the multivariate analysis, again, only patient SDHB status and tumor size were independently associated with metastasis.”
The incidence of local recurrence in patients with the SDHB mutation was 47.6% vs. 9.1% in those without the gene mutation, Dr. Assadipour said. The rates of distant metastasis showed a similar disparity: 56.5% and 9.1%, respectively.
Patients with the SDHB mutation presented at a younger age than those without the mutation, 33 vs. 49.6 years old. Among the 65 patients who underwent R0 primary tumor resection, those with the SDHB mutation, paraganglioma, and larger tumor size had a shorter disease-free survival, Dr. Assadipour said.
In analyzing tumor size, Dr. Assadipour said two stratifications were studied: evaluating tumors sized 0-3 cm, 3-6 cm and 6 cm and larger; and 0-5 cm and 5 cm and larger. “Tumors over 6 cm had the shortest disease-free survival, and even when we applied the under-5 cm and over-5 cm scale, we clearly saw a difference in disease-free survival,” she said. Ki-67 and mitotic index were not related to disease-free survival.
The presence of a SDHB mutation had a hazard ratio of 16.2, while tumor diameter greater than 6 cm had a HR of 15.4, Dr. Assadipour said. These were the only independent risk factors for local recurrence, distant metastases and shorter disease-free interval found in the study.
During the discussion, Lawrence T. Kim, MD, of the University of North Carolina asked if the researchers found any differences in outcomes related to the surgical approach. “We were unable to identify whether any surgical approach improved or worsened outcomes on multivariate analysis” Dr. Assadipour said.
Thomas J. Fahey, MD, of New York asked what she would recommend for surgical approaches for patients with PC and PGL.
“Our general recommendation is that an adrenal pheochromocytoma that is over 6 cm carries a higher risk of recurrence and distant metastasis so an open approach with lymph node dissection ensuring negative surgical margins should be considered,” Dr. Assadipour said. “For abdominal paragangliomas, unless they are quite small and in a favorable location, we would generally recommend an open approach.”
The study was supported by the intramural program of the Center for Cancer Research, National Cancer Institute, National Institutes of Health. Dr. Assadipour and her coauthors had no financial relationships to disclose.
BALTIMORE – Tumor size and the presence of mutations of the succinate dehydrogenase complex subunit B (SDHB) gene may be reliable indicators of prognosis after surgery for pheochromocytoma and abdominal paraganglioma, investigators in a National Cancer Institute–funded study have reported.
“The staging of pheochromocytoma and abdominal paraganglioma can be difficult, but it is critical for optimal patient care,” Yasmine Assadipour, MD, of the National Cancer Institute, Bethesda, Md., and the George Washington University Hospital, Washington, reported at the annual meeting of the American Association of Endocrine Surgeons.
“Any clinically relevant grading or prognostic system should include SDHB mutation status and primary tumor size as prime features of scoring,” Dr. Assadipour said. “Histologic features such as Ki-67 or mitotic index may not be as useful for prognostic information in patients with pheochromocytoma and abdominal paraganglioma, particularly in the setting of SDHB mutation.”
Dr. Assadipour and her coinvestigators focused their investigation on mutations of the SDHB (succinate dehydrogenase complex subunit B) gene, which codes for one of four subunits comprising a mitochondrial protein.
They also considered primary tumor size, functionality, pathology, surgical approach, and histologic features including Ki-67 index and mitotic index. The study was a retrospective analysis of 84 patients who had surgery for PC [pheochromocytoma] or PGL [paraganglioma] and had germ line genetic testing. Of the 84 patients, 35 patients had sporadic disease and 49 had germ line SDHB mutation. The study analyzed tumor samples for Ki-67/MIB-1 staining and mitotic index.
“In a univariate analysis, SDHB mutation, tumor size and surgical approach were associated with local regional recurrence,” Dr. Assadipour said. “In a multivariate analysis, the only independent risk factors were SDHB mutation status and tumor size; Ki-67 and mitotic index did not have any association with recurrence.”
The researchers found similar results when they looked at distant metastasis. “SDHB mutation, tumor size, abdominal paraganglioma and surgical approach were associated with distant metastasis,” Dr. Assadipour said. “Again, Ki-67 and mitotic index were not.”
In the multivariate analysis, again, only patient SDHB status and tumor size were independently associated with metastasis.”
The incidence of local recurrence in patients with the SDHB mutation was 47.6% vs. 9.1% in those without the gene mutation, Dr. Assadipour said. The rates of distant metastasis showed a similar disparity: 56.5% and 9.1%, respectively.
Patients with the SDHB mutation presented at a younger age than those without the mutation, 33 vs. 49.6 years old. Among the 65 patients who underwent R0 primary tumor resection, those with the SDHB mutation, paraganglioma, and larger tumor size had a shorter disease-free survival, Dr. Assadipour said.
In analyzing tumor size, Dr. Assadipour said two stratifications were studied: evaluating tumors sized 0-3 cm, 3-6 cm and 6 cm and larger; and 0-5 cm and 5 cm and larger. “Tumors over 6 cm had the shortest disease-free survival, and even when we applied the under-5 cm and over-5 cm scale, we clearly saw a difference in disease-free survival,” she said. Ki-67 and mitotic index were not related to disease-free survival.
The presence of a SDHB mutation had a hazard ratio of 16.2, while tumor diameter greater than 6 cm had a HR of 15.4, Dr. Assadipour said. These were the only independent risk factors for local recurrence, distant metastases and shorter disease-free interval found in the study.
During the discussion, Lawrence T. Kim, MD, of the University of North Carolina asked if the researchers found any differences in outcomes related to the surgical approach. “We were unable to identify whether any surgical approach improved or worsened outcomes on multivariate analysis” Dr. Assadipour said.
Thomas J. Fahey, MD, of New York asked what she would recommend for surgical approaches for patients with PC and PGL.
“Our general recommendation is that an adrenal pheochromocytoma that is over 6 cm carries a higher risk of recurrence and distant metastasis so an open approach with lymph node dissection ensuring negative surgical margins should be considered,” Dr. Assadipour said. “For abdominal paragangliomas, unless they are quite small and in a favorable location, we would generally recommend an open approach.”
The study was supported by the intramural program of the Center for Cancer Research, National Cancer Institute, National Institutes of Health. Dr. Assadipour and her coauthors had no financial relationships to disclose.
AT AAES 2016
Key clinical point: SDHB mutation and tumor size may be better predictors of outcomes in patients with pheochromocytoma and abdominal paraganglioma than are other previously identified predictors.
Major finding: The incidence of local recurrence in patients with the SDHB mutation was 47.6% vs. 9.1% in those without the gene mutation.
Data source: Retrospective analysis of 84 patients with PC/PGL evaluated by the Surgical Endocrine Oncology branch at George Washington University Hospital from 1998-2015.
Disclosures: The study was supported by the intramural program of the Center for Cancer Research, National Cancer Institute, National Institutes of Health. Dr. Assadipour and her coauthors reported having no financial disclosures.