User login
MONTREAL – It can be a tough sell to worried patients or their caregivers, but surveillance imaging in children with a history of some treated solid tumors may not add anything to care except costs, a team of investigators suggested.
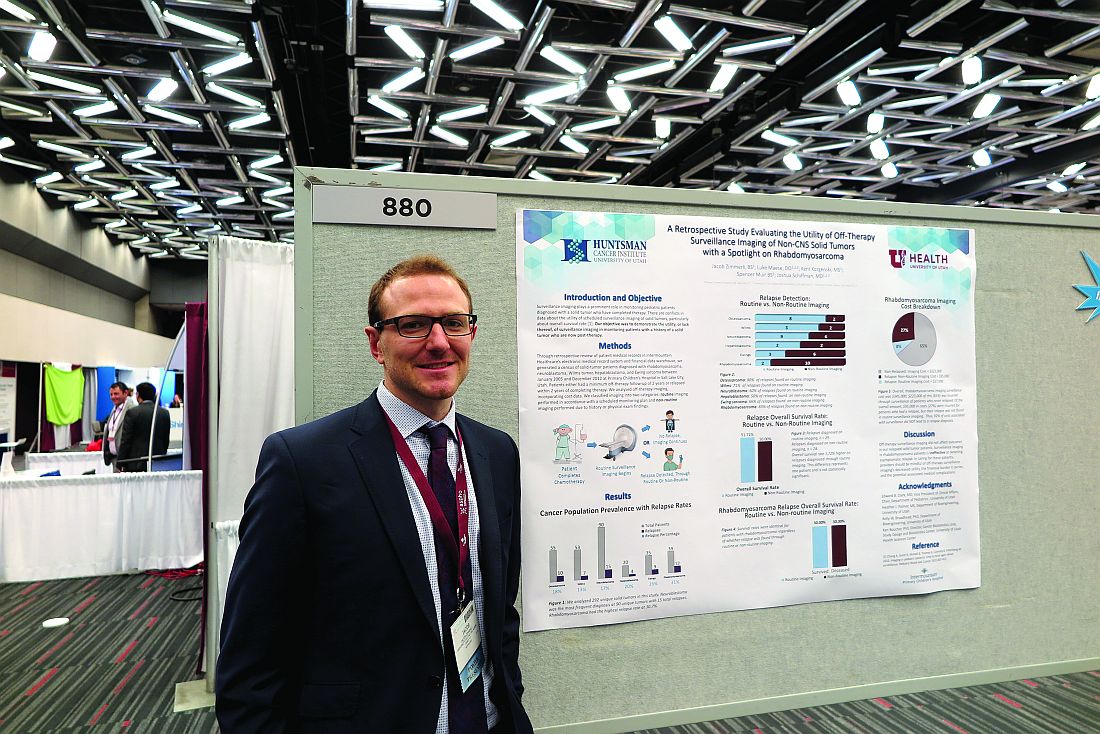
A study of the relationship between surveillance imaging and outcomes in patients who were followed after therapy for solid tumors found that “off therapy surveillance imaging did not affect outcomes in our relapsed solid tumor patients,” wrote Jacob Zimmerli and his coinvestigators at the University of Utah Huntsman Cancer Institute, Salt Lake City.
“In the case of rhabdomyosarcoma, we had a 31% relapse rate of our 39 unique cancer diagnoses that we looked at over a 10-year period. We had 12 relapses, and, of those relapses, 10 were found through nonroutine imaging,” Mr. Zimmerli said in an interview.
Survival rates for patients with rhabdomyosarcoma were identical whether their relapsed disease was detected via surveillance imaging or imaging performed when relapse was directly suspected because of clinical or physical findings, he said.
Surveillance imaging also came at a significant financial cost. Of the $345,000 total expenditure for imaging of rhabdomyosarcoma, $223,000 was spent on imaging for patients who never experienced a relapse. Additionally, $95,000 was spent on imaging for patients who had a relapse but whose relapses were not detected by routine surveillance imaging. Therefore, the investigators calculated, 92% of costs associated with surveillance did not lead to a relapse diagnosis.
“This finding in itself will lead us to look at a few more specific cancer subgroups and maybe do more cost analysis to see if there is a better way to treat these patients,” Mr. Zimmerli said.
To see whether surveillance imaging was associated with outcomes, the investigators performed a retrospective review of data on 292 patients treated at Primary Children’s Hospital in Salt Lake City for osteosarcoma, Wilms’ tumor, neuroblastoma, hepatoblastoma, Ewing sarcoma , or rhabdomyosarcoma.
All patients had either completed a minimum of 2 years of posttherapy follow-up or had a disease relapse within 2 years of completing therapy.
The investigators found that 8 of 10 osteosarcoma relapses, five of seven Wilms’ tumor relapses, and 9 of 15 neuroblastoma relapses were detected on routine imaging.
In contrast, only two of four hepatoblastoma relapses, three of nine Ewings sarcoma relapses, and 2 of 12 rhabdomyosarcoma relapses were found on routine imaging.
The overall survival rate for patients with relapses diagnosed on routine imaging was 51.72%, compared with 50% for patients whose relapses were diagnosed on imaging following the appearance of symptoms. The difference represented only one patient and was not statistically significant.
Mr. Zimmerli acknowledged that many routine posttherapy imaging studies are performed to assuage patient concerns and that it may be difficult to convince parents of children with a history of cancer that routine imaging of some tumors may not offer the assurances of relapse-free survival that they seek.
The study was supported by Intermountain Healthcare. The investigators reported no conflicts of interest.
MONTREAL – It can be a tough sell to worried patients or their caregivers, but surveillance imaging in children with a history of some treated solid tumors may not add anything to care except costs, a team of investigators suggested.
A study of the relationship between surveillance imaging and outcomes in patients who were followed after therapy for solid tumors found that “off therapy surveillance imaging did not affect outcomes in our relapsed solid tumor patients,” wrote Jacob Zimmerli and his coinvestigators at the University of Utah Huntsman Cancer Institute, Salt Lake City.
“In the case of rhabdomyosarcoma, we had a 31% relapse rate of our 39 unique cancer diagnoses that we looked at over a 10-year period. We had 12 relapses, and, of those relapses, 10 were found through nonroutine imaging,” Mr. Zimmerli said in an interview.
Survival rates for patients with rhabdomyosarcoma were identical whether their relapsed disease was detected via surveillance imaging or imaging performed when relapse was directly suspected because of clinical or physical findings, he said.
Surveillance imaging also came at a significant financial cost. Of the $345,000 total expenditure for imaging of rhabdomyosarcoma, $223,000 was spent on imaging for patients who never experienced a relapse. Additionally, $95,000 was spent on imaging for patients who had a relapse but whose relapses were not detected by routine surveillance imaging. Therefore, the investigators calculated, 92% of costs associated with surveillance did not lead to a relapse diagnosis.
“This finding in itself will lead us to look at a few more specific cancer subgroups and maybe do more cost analysis to see if there is a better way to treat these patients,” Mr. Zimmerli said.
To see whether surveillance imaging was associated with outcomes, the investigators performed a retrospective review of data on 292 patients treated at Primary Children’s Hospital in Salt Lake City for osteosarcoma, Wilms’ tumor, neuroblastoma, hepatoblastoma, Ewing sarcoma , or rhabdomyosarcoma.
All patients had either completed a minimum of 2 years of posttherapy follow-up or had a disease relapse within 2 years of completing therapy.
The investigators found that 8 of 10 osteosarcoma relapses, five of seven Wilms’ tumor relapses, and 9 of 15 neuroblastoma relapses were detected on routine imaging.
In contrast, only two of four hepatoblastoma relapses, three of nine Ewings sarcoma relapses, and 2 of 12 rhabdomyosarcoma relapses were found on routine imaging.
The overall survival rate for patients with relapses diagnosed on routine imaging was 51.72%, compared with 50% for patients whose relapses were diagnosed on imaging following the appearance of symptoms. The difference represented only one patient and was not statistically significant.
Mr. Zimmerli acknowledged that many routine posttherapy imaging studies are performed to assuage patient concerns and that it may be difficult to convince parents of children with a history of cancer that routine imaging of some tumors may not offer the assurances of relapse-free survival that they seek.
The study was supported by Intermountain Healthcare. The investigators reported no conflicts of interest.
MONTREAL – It can be a tough sell to worried patients or their caregivers, but surveillance imaging in children with a history of some treated solid tumors may not add anything to care except costs, a team of investigators suggested.
A study of the relationship between surveillance imaging and outcomes in patients who were followed after therapy for solid tumors found that “off therapy surveillance imaging did not affect outcomes in our relapsed solid tumor patients,” wrote Jacob Zimmerli and his coinvestigators at the University of Utah Huntsman Cancer Institute, Salt Lake City.
“In the case of rhabdomyosarcoma, we had a 31% relapse rate of our 39 unique cancer diagnoses that we looked at over a 10-year period. We had 12 relapses, and, of those relapses, 10 were found through nonroutine imaging,” Mr. Zimmerli said in an interview.
Survival rates for patients with rhabdomyosarcoma were identical whether their relapsed disease was detected via surveillance imaging or imaging performed when relapse was directly suspected because of clinical or physical findings, he said.
Surveillance imaging also came at a significant financial cost. Of the $345,000 total expenditure for imaging of rhabdomyosarcoma, $223,000 was spent on imaging for patients who never experienced a relapse. Additionally, $95,000 was spent on imaging for patients who had a relapse but whose relapses were not detected by routine surveillance imaging. Therefore, the investigators calculated, 92% of costs associated with surveillance did not lead to a relapse diagnosis.
“This finding in itself will lead us to look at a few more specific cancer subgroups and maybe do more cost analysis to see if there is a better way to treat these patients,” Mr. Zimmerli said.
To see whether surveillance imaging was associated with outcomes, the investigators performed a retrospective review of data on 292 patients treated at Primary Children’s Hospital in Salt Lake City for osteosarcoma, Wilms’ tumor, neuroblastoma, hepatoblastoma, Ewing sarcoma , or rhabdomyosarcoma.
All patients had either completed a minimum of 2 years of posttherapy follow-up or had a disease relapse within 2 years of completing therapy.
The investigators found that 8 of 10 osteosarcoma relapses, five of seven Wilms’ tumor relapses, and 9 of 15 neuroblastoma relapses were detected on routine imaging.
In contrast, only two of four hepatoblastoma relapses, three of nine Ewings sarcoma relapses, and 2 of 12 rhabdomyosarcoma relapses were found on routine imaging.
The overall survival rate for patients with relapses diagnosed on routine imaging was 51.72%, compared with 50% for patients whose relapses were diagnosed on imaging following the appearance of symptoms. The difference represented only one patient and was not statistically significant.
Mr. Zimmerli acknowledged that many routine posttherapy imaging studies are performed to assuage patient concerns and that it may be difficult to convince parents of children with a history of cancer that routine imaging of some tumors may not offer the assurances of relapse-free survival that they seek.
The study was supported by Intermountain Healthcare. The investigators reported no conflicts of interest.
FROM ASPHO
Key clinical point: Routine surveillance was less effective at detecting relapse of some pediatric solid tumors than imaging performed to confirm a clinical finding.
Major finding: Using imaging performed after symptoms appeared, 10 of 12 rhabdomyosarcoma relapses were detected.
Data source: A retrospective review of outcomes following routine and nonroutine imaging among children followed after treatment for one of six solid tumor types.
Disclosures: The study was supported by Intermountain Healthcare. The investigators reported no conflicts of interest.