User login
Editor’s note: This article first appeared on SHM’s “The Hospital Leader” blog.
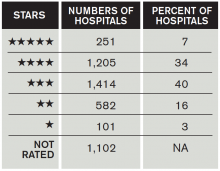
Patient satisfaction survey performance is becoming increasingly important for hospitals, because the ratings are being used by payers in pay-for-performance programs more and more (including the CMS Hospital Value-Based Purchasing program). CMS also recently released its “Five-Star Quality Rating System” for hospitals, which publicly grades hospitals, using one to five stars, based on their patient satisfaction scores.
How Did Hospitals Do in Medicare’s Patient Quality Ratings?
Unfortunately, there is little literature to guide physicians on exactly HOW to improve patient satisfaction scores for themselves or their groups. A recent publication in the Journal of Hospital Medicine found a feasible and effective intervention to improve patient satisfaction scores among trainees, the methodology of which could easily be applied to hospitalists.
Gaurav Banka, MD, a former internal medicine resident (and current cardiology fellow) at UCLA Hospital, was interviewed about his team’s recent publication in the Journal of Hospital Medicine. In the interview, he opined about “improving patient satisfaction through resident education, feedback, and incentives.” The study he published found that this combination of interventions among internal medicine residents improved relevant HCAHPS scores by approximately 8%.
The following are excerpts from a Q&A session I had with Dr. Banka:
Question: Can you briefly summarize the intervention(s)?
Answer: There were three total interventions put in place simultaneously: an educational conference on best practices in patient communication, a recognition-reward program (recognition within the department and a movie package for high performers), and real-time feedback to the residents from their patients via a survey. The last component was the most impactful to the residents. Patients were randomly surveyed on how their residents were communicating with them, and the results were sent to the resident for review and self-reflection within weeks.
Q: How did you become interested in resident interventions to improve HCAHPS?
A: I noticed as an intern [that] there was almost no emphasis placed on patient communication skills, and there was almost no feedback given to residents on how they were performing. I felt that this was a very important piece of feedback that residents were lacking and was very interested in creating a program that would help them learn new communication skills and get feedback on how they were doing.
Q: How should hospitalists use this study information to change their practice?
A: Hospital medicine programs should have some way to measure and give feedback to individual hospitalists on what the patient is experiencing with respect to communication. The intervention from this study should be easily scalable to any practice. There was almost no cost associated with the patient survey distribution, and it gave incredibly valuable individualized feedback about communication skills directly from the patients themselves. It should be feasible to implement this type of audit and feedback within any size hospital medicine program.
Q: Were there any unexpected findings in your study?
A: We were surprised at how much of an impact it had on HCAHPS scores. Not only did it impact physician communication ratings, but [it] also had an impressive impact on overall hospital ratings.
Q: Where does this take us with respect to future research efforts?
A: Our team is now working on expanding this program to other residency programs, as well as expanding it to attending physicians, within and outside the department of medicine.
In summary, Dr. Banka’s team found this relatively simple intervention was able to sizably improve the HCAHPS scores of recipient providers. Such interventions should be seriously considered by hospital medicine programs looking to improve their publicly reported patient satisfaction scores.
Editor’s note: This article first appeared on SHM’s “The Hospital Leader” blog.
Patient satisfaction survey performance is becoming increasingly important for hospitals, because the ratings are being used by payers in pay-for-performance programs more and more (including the CMS Hospital Value-Based Purchasing program). CMS also recently released its “Five-Star Quality Rating System” for hospitals, which publicly grades hospitals, using one to five stars, based on their patient satisfaction scores.
How Did Hospitals Do in Medicare’s Patient Quality Ratings?
Unfortunately, there is little literature to guide physicians on exactly HOW to improve patient satisfaction scores for themselves or their groups. A recent publication in the Journal of Hospital Medicine found a feasible and effective intervention to improve patient satisfaction scores among trainees, the methodology of which could easily be applied to hospitalists.
Gaurav Banka, MD, a former internal medicine resident (and current cardiology fellow) at UCLA Hospital, was interviewed about his team’s recent publication in the Journal of Hospital Medicine. In the interview, he opined about “improving patient satisfaction through resident education, feedback, and incentives.” The study he published found that this combination of interventions among internal medicine residents improved relevant HCAHPS scores by approximately 8%.
The following are excerpts from a Q&A session I had with Dr. Banka:
Question: Can you briefly summarize the intervention(s)?
Answer: There were three total interventions put in place simultaneously: an educational conference on best practices in patient communication, a recognition-reward program (recognition within the department and a movie package for high performers), and real-time feedback to the residents from their patients via a survey. The last component was the most impactful to the residents. Patients were randomly surveyed on how their residents were communicating with them, and the results were sent to the resident for review and self-reflection within weeks.
Q: How did you become interested in resident interventions to improve HCAHPS?
A: I noticed as an intern [that] there was almost no emphasis placed on patient communication skills, and there was almost no feedback given to residents on how they were performing. I felt that this was a very important piece of feedback that residents were lacking and was very interested in creating a program that would help them learn new communication skills and get feedback on how they were doing.
Q: How should hospitalists use this study information to change their practice?
A: Hospital medicine programs should have some way to measure and give feedback to individual hospitalists on what the patient is experiencing with respect to communication. The intervention from this study should be easily scalable to any practice. There was almost no cost associated with the patient survey distribution, and it gave incredibly valuable individualized feedback about communication skills directly from the patients themselves. It should be feasible to implement this type of audit and feedback within any size hospital medicine program.
Q: Were there any unexpected findings in your study?
A: We were surprised at how much of an impact it had on HCAHPS scores. Not only did it impact physician communication ratings, but [it] also had an impressive impact on overall hospital ratings.
Q: Where does this take us with respect to future research efforts?
A: Our team is now working on expanding this program to other residency programs, as well as expanding it to attending physicians, within and outside the department of medicine.
In summary, Dr. Banka’s team found this relatively simple intervention was able to sizably improve the HCAHPS scores of recipient providers. Such interventions should be seriously considered by hospital medicine programs looking to improve their publicly reported patient satisfaction scores.
Editor’s note: This article first appeared on SHM’s “The Hospital Leader” blog.
Patient satisfaction survey performance is becoming increasingly important for hospitals, because the ratings are being used by payers in pay-for-performance programs more and more (including the CMS Hospital Value-Based Purchasing program). CMS also recently released its “Five-Star Quality Rating System” for hospitals, which publicly grades hospitals, using one to five stars, based on their patient satisfaction scores.
How Did Hospitals Do in Medicare’s Patient Quality Ratings?
Unfortunately, there is little literature to guide physicians on exactly HOW to improve patient satisfaction scores for themselves or their groups. A recent publication in the Journal of Hospital Medicine found a feasible and effective intervention to improve patient satisfaction scores among trainees, the methodology of which could easily be applied to hospitalists.
Gaurav Banka, MD, a former internal medicine resident (and current cardiology fellow) at UCLA Hospital, was interviewed about his team’s recent publication in the Journal of Hospital Medicine. In the interview, he opined about “improving patient satisfaction through resident education, feedback, and incentives.” The study he published found that this combination of interventions among internal medicine residents improved relevant HCAHPS scores by approximately 8%.
The following are excerpts from a Q&A session I had with Dr. Banka:
Question: Can you briefly summarize the intervention(s)?
Answer: There were three total interventions put in place simultaneously: an educational conference on best practices in patient communication, a recognition-reward program (recognition within the department and a movie package for high performers), and real-time feedback to the residents from their patients via a survey. The last component was the most impactful to the residents. Patients were randomly surveyed on how their residents were communicating with them, and the results were sent to the resident for review and self-reflection within weeks.
Q: How did you become interested in resident interventions to improve HCAHPS?
A: I noticed as an intern [that] there was almost no emphasis placed on patient communication skills, and there was almost no feedback given to residents on how they were performing. I felt that this was a very important piece of feedback that residents were lacking and was very interested in creating a program that would help them learn new communication skills and get feedback on how they were doing.
Q: How should hospitalists use this study information to change their practice?
A: Hospital medicine programs should have some way to measure and give feedback to individual hospitalists on what the patient is experiencing with respect to communication. The intervention from this study should be easily scalable to any practice. There was almost no cost associated with the patient survey distribution, and it gave incredibly valuable individualized feedback about communication skills directly from the patients themselves. It should be feasible to implement this type of audit and feedback within any size hospital medicine program.
Q: Were there any unexpected findings in your study?
A: We were surprised at how much of an impact it had on HCAHPS scores. Not only did it impact physician communication ratings, but [it] also had an impressive impact on overall hospital ratings.
Q: Where does this take us with respect to future research efforts?
A: Our team is now working on expanding this program to other residency programs, as well as expanding it to attending physicians, within and outside the department of medicine.
In summary, Dr. Banka’s team found this relatively simple intervention was able to sizably improve the HCAHPS scores of recipient providers. Such interventions should be seriously considered by hospital medicine programs looking to improve their publicly reported patient satisfaction scores.