User login
SAN DIEGO – A combination of cognitive-behavioral therapy and mindfulness meditation could reduce pain and fatigue from Crohn’s disease, researchers say.
Patients who followed the program not only felt better but were also more often able to show up for work and leisure activities, compared with a control group assigned to a wait list, said Shmuel Odes, MD, a professor of internal medicine at Ben-Gurion University of the Negev in Beersheba, Israel. He presented the finding at Digestive Diseases Week® (DDW) 2022.
Psychological and social factors affect the gut and vice versa, Dr. Odes said. Yet many inflammatory bowel disease clinics overlook psychological interventions.
To address these issues, Dr. Odes and colleagues developed cognitive-behavioral– and mindfulness-based stress reduction (COBMINDEX) training, which can be taught by clinical social workers over the Internet. “The patient learns to relax,” Dr. Odes told MDedge News. “He learns not to fight his condition.”
In a previous paper, published in the journal Inflammatory Bowel Diseases, Dr. Odes and colleagues reported that patients who learned the technique showed improvement on a variety of psychological and quality-of-life measures, accompanied by changes in inflammatory cytokines and cortisol.
In a follow-up analysis presented here, the researchers looked at measures of pain and fatigue and then examined whether these were associated with productivity at work and other daily activities.
The study investigators randomly assigned 72 patients to an intervention group who got COBMINDEX training right away, and another 70 to a control group assigned to a wait list of 12 weeks before they could get the training. At baseline, the two groups were not significantly different in any demographic or clinical variable the researchers could find.
Social workers provided COBMINDEX training for the patients in seven 60-minute session over 12 weeks. Five of the sessions were devoted to cognitive-behavioral therapy and two to mindfulness-based stress reduction. The social workers asked the patients to do exercises at least once a day and report outcomes through an app.
Twelve patients dropped out of the COBMINDEX group and four dropped from the wait-list group because of lack of interest, time constraints, pregnancy, or illness.
The researchers created a composite score with a 0-15 scale (with higher scores indicating greater pain) from three pain items from the Harvey-Bradshaw Index for Crohn’s Disease, the Short Inflammatory Bowel Disease Questionnaire, and the 12-Item Short Form Survey.
To measure fatigue, they used the Functional Assessment of Chronic Illness Therapy-Fatigue, which has a 0-52 scale, with lower scores indicating greater fatigue.
To measure impairment while working and other daily activities, they used the Work Productivity and Activity Impairment Questionnaire: Crohn’s Disease. Scores on this measure are expressed as a percentage, with higher values indicating greater impairment.
Both the COBMINDEX and the wait-list groups improved on all these scales, but the improvements were significantly greater for the COBMINDEX group.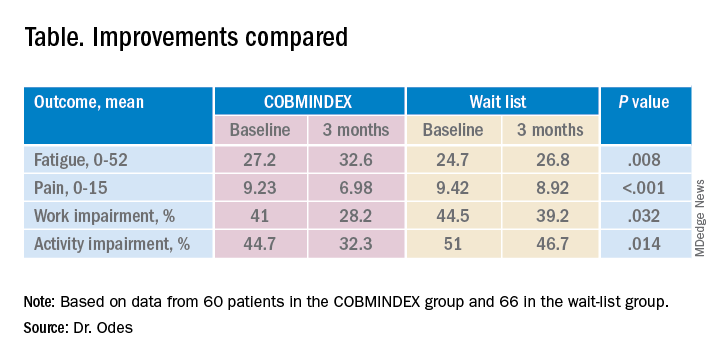
Through statistical analysis, the researchers found that the improvements in pain and fatigue indirectly caused the improvements in work and activity impairment, and that pain and fatigue improvements made independent contributions of similar magnitudes. COBMINDEX did not directly improve work or activity.
Psychological interventions are too often overlooked in Crohn’s disease, said the session comoderator Paul Moayyedi, MD, a professor of gastroenterology at McMaster University in Hamilton, Ont. “We need to realize how important this is to patients and urgently make this available,” he told MDedge.
A variety of interventions are being researched, and this study makes an important contribution, he said. However, he questioned whether people on a wait list can serve as an adequate control. “If you have to wait for something, you tend to have more pain, and you could have less productivity just because of waiting,” he said. “Ideally they should do a randomized trial with a sham intervention, not a wait list.”
Dr. Odes responded that it is very difficult to recruit people to a trial if they only have a 50% chance of getting a real treatment. And he noted that the people on the wait list in this trial did not show any signs of increased symptoms.
Physicians wanting to provide psychological help to their Crohn’s disease patients can refer them to social workers or psychotherapists, Dr. Odes said, but these professionals may lack training for applying cognitive-behavioral therapy and mindfulness-based stress reduction to patients with Crohn’s disease. His team hopes to make an app publicly available soon.
Neither Dr. Odes nor Dr. Moayyedi reported any relevant financial interests. The study was supported by a grant from the Leona M. and Harry B. Helmsley Charitable Trust.
SAN DIEGO – A combination of cognitive-behavioral therapy and mindfulness meditation could reduce pain and fatigue from Crohn’s disease, researchers say.
Patients who followed the program not only felt better but were also more often able to show up for work and leisure activities, compared with a control group assigned to a wait list, said Shmuel Odes, MD, a professor of internal medicine at Ben-Gurion University of the Negev in Beersheba, Israel. He presented the finding at Digestive Diseases Week® (DDW) 2022.
Psychological and social factors affect the gut and vice versa, Dr. Odes said. Yet many inflammatory bowel disease clinics overlook psychological interventions.
To address these issues, Dr. Odes and colleagues developed cognitive-behavioral– and mindfulness-based stress reduction (COBMINDEX) training, which can be taught by clinical social workers over the Internet. “The patient learns to relax,” Dr. Odes told MDedge News. “He learns not to fight his condition.”
In a previous paper, published in the journal Inflammatory Bowel Diseases, Dr. Odes and colleagues reported that patients who learned the technique showed improvement on a variety of psychological and quality-of-life measures, accompanied by changes in inflammatory cytokines and cortisol.
In a follow-up analysis presented here, the researchers looked at measures of pain and fatigue and then examined whether these were associated with productivity at work and other daily activities.
The study investigators randomly assigned 72 patients to an intervention group who got COBMINDEX training right away, and another 70 to a control group assigned to a wait list of 12 weeks before they could get the training. At baseline, the two groups were not significantly different in any demographic or clinical variable the researchers could find.
Social workers provided COBMINDEX training for the patients in seven 60-minute session over 12 weeks. Five of the sessions were devoted to cognitive-behavioral therapy and two to mindfulness-based stress reduction. The social workers asked the patients to do exercises at least once a day and report outcomes through an app.
Twelve patients dropped out of the COBMINDEX group and four dropped from the wait-list group because of lack of interest, time constraints, pregnancy, or illness.
The researchers created a composite score with a 0-15 scale (with higher scores indicating greater pain) from three pain items from the Harvey-Bradshaw Index for Crohn’s Disease, the Short Inflammatory Bowel Disease Questionnaire, and the 12-Item Short Form Survey.
To measure fatigue, they used the Functional Assessment of Chronic Illness Therapy-Fatigue, which has a 0-52 scale, with lower scores indicating greater fatigue.
To measure impairment while working and other daily activities, they used the Work Productivity and Activity Impairment Questionnaire: Crohn’s Disease. Scores on this measure are expressed as a percentage, with higher values indicating greater impairment.
Both the COBMINDEX and the wait-list groups improved on all these scales, but the improvements were significantly greater for the COBMINDEX group.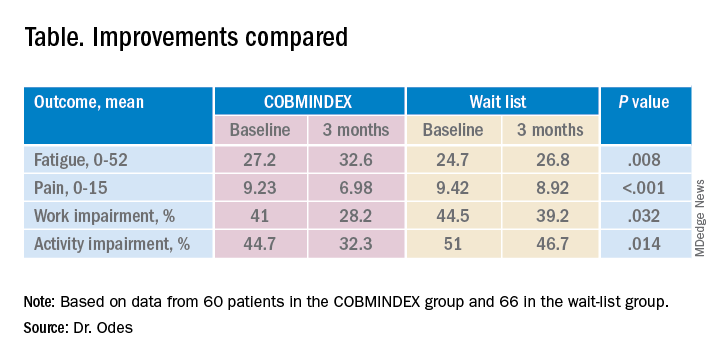
Through statistical analysis, the researchers found that the improvements in pain and fatigue indirectly caused the improvements in work and activity impairment, and that pain and fatigue improvements made independent contributions of similar magnitudes. COBMINDEX did not directly improve work or activity.
Psychological interventions are too often overlooked in Crohn’s disease, said the session comoderator Paul Moayyedi, MD, a professor of gastroenterology at McMaster University in Hamilton, Ont. “We need to realize how important this is to patients and urgently make this available,” he told MDedge.
A variety of interventions are being researched, and this study makes an important contribution, he said. However, he questioned whether people on a wait list can serve as an adequate control. “If you have to wait for something, you tend to have more pain, and you could have less productivity just because of waiting,” he said. “Ideally they should do a randomized trial with a sham intervention, not a wait list.”
Dr. Odes responded that it is very difficult to recruit people to a trial if they only have a 50% chance of getting a real treatment. And he noted that the people on the wait list in this trial did not show any signs of increased symptoms.
Physicians wanting to provide psychological help to their Crohn’s disease patients can refer them to social workers or psychotherapists, Dr. Odes said, but these professionals may lack training for applying cognitive-behavioral therapy and mindfulness-based stress reduction to patients with Crohn’s disease. His team hopes to make an app publicly available soon.
Neither Dr. Odes nor Dr. Moayyedi reported any relevant financial interests. The study was supported by a grant from the Leona M. and Harry B. Helmsley Charitable Trust.
SAN DIEGO – A combination of cognitive-behavioral therapy and mindfulness meditation could reduce pain and fatigue from Crohn’s disease, researchers say.
Patients who followed the program not only felt better but were also more often able to show up for work and leisure activities, compared with a control group assigned to a wait list, said Shmuel Odes, MD, a professor of internal medicine at Ben-Gurion University of the Negev in Beersheba, Israel. He presented the finding at Digestive Diseases Week® (DDW) 2022.
Psychological and social factors affect the gut and vice versa, Dr. Odes said. Yet many inflammatory bowel disease clinics overlook psychological interventions.
To address these issues, Dr. Odes and colleagues developed cognitive-behavioral– and mindfulness-based stress reduction (COBMINDEX) training, which can be taught by clinical social workers over the Internet. “The patient learns to relax,” Dr. Odes told MDedge News. “He learns not to fight his condition.”
In a previous paper, published in the journal Inflammatory Bowel Diseases, Dr. Odes and colleagues reported that patients who learned the technique showed improvement on a variety of psychological and quality-of-life measures, accompanied by changes in inflammatory cytokines and cortisol.
In a follow-up analysis presented here, the researchers looked at measures of pain and fatigue and then examined whether these were associated with productivity at work and other daily activities.
The study investigators randomly assigned 72 patients to an intervention group who got COBMINDEX training right away, and another 70 to a control group assigned to a wait list of 12 weeks before they could get the training. At baseline, the two groups were not significantly different in any demographic or clinical variable the researchers could find.
Social workers provided COBMINDEX training for the patients in seven 60-minute session over 12 weeks. Five of the sessions were devoted to cognitive-behavioral therapy and two to mindfulness-based stress reduction. The social workers asked the patients to do exercises at least once a day and report outcomes through an app.
Twelve patients dropped out of the COBMINDEX group and four dropped from the wait-list group because of lack of interest, time constraints, pregnancy, or illness.
The researchers created a composite score with a 0-15 scale (with higher scores indicating greater pain) from three pain items from the Harvey-Bradshaw Index for Crohn’s Disease, the Short Inflammatory Bowel Disease Questionnaire, and the 12-Item Short Form Survey.
To measure fatigue, they used the Functional Assessment of Chronic Illness Therapy-Fatigue, which has a 0-52 scale, with lower scores indicating greater fatigue.
To measure impairment while working and other daily activities, they used the Work Productivity and Activity Impairment Questionnaire: Crohn’s Disease. Scores on this measure are expressed as a percentage, with higher values indicating greater impairment.
Both the COBMINDEX and the wait-list groups improved on all these scales, but the improvements were significantly greater for the COBMINDEX group.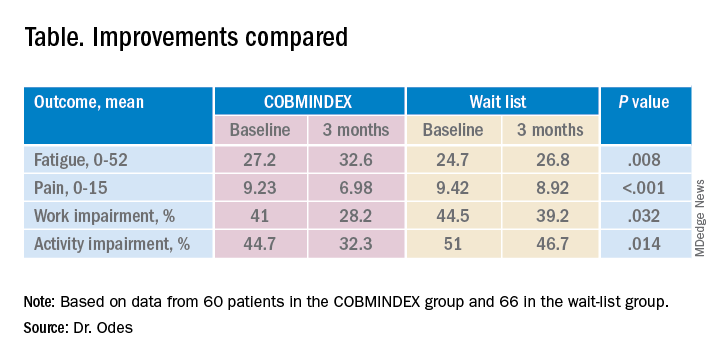
Through statistical analysis, the researchers found that the improvements in pain and fatigue indirectly caused the improvements in work and activity impairment, and that pain and fatigue improvements made independent contributions of similar magnitudes. COBMINDEX did not directly improve work or activity.
Psychological interventions are too often overlooked in Crohn’s disease, said the session comoderator Paul Moayyedi, MD, a professor of gastroenterology at McMaster University in Hamilton, Ont. “We need to realize how important this is to patients and urgently make this available,” he told MDedge.
A variety of interventions are being researched, and this study makes an important contribution, he said. However, he questioned whether people on a wait list can serve as an adequate control. “If you have to wait for something, you tend to have more pain, and you could have less productivity just because of waiting,” he said. “Ideally they should do a randomized trial with a sham intervention, not a wait list.”
Dr. Odes responded that it is very difficult to recruit people to a trial if they only have a 50% chance of getting a real treatment. And he noted that the people on the wait list in this trial did not show any signs of increased symptoms.
Physicians wanting to provide psychological help to their Crohn’s disease patients can refer them to social workers or psychotherapists, Dr. Odes said, but these professionals may lack training for applying cognitive-behavioral therapy and mindfulness-based stress reduction to patients with Crohn’s disease. His team hopes to make an app publicly available soon.
Neither Dr. Odes nor Dr. Moayyedi reported any relevant financial interests. The study was supported by a grant from the Leona M. and Harry B. Helmsley Charitable Trust.
AT DDW 2022