User login
Danielle D. Antosh, MD, of the Houston Methodist Hospital and colleagues reported in a systematic review of prospective comparative studies on pelvic organ prolapse surgery, which was published in Obstetrics & Gynecology.
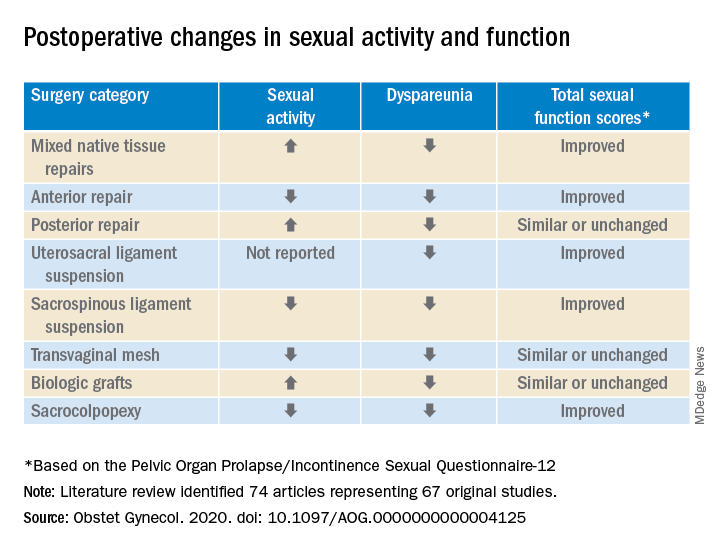
In a preliminary search of 3,124 citations, Dr. Antosh and her colleagues, who are members of the Society of Gynecologic Surgeons Systematic Review Group responsible for the study, identified and accepted 74 articles representing 67 original studies. Ten of these were ancillary studies with different reported outcomes or follow-up times, and 44 were randomized control trials. They compared the pre- and postoperative effects of pelvic organ prolapse (POP) surgery on sexual function for changes in sexual activity and function across eight different prolapse surgery categories: mixed native tissue repairs, anterior repair, posterior repair, uterosacral ligament suspension, sacrospinous ligament suspension, transvaginal mesh, biologic grafts, and sacrocolpopexy. In only three categories – posterior repair, transvaginal mesh, and biological grafts – postoperative changes in sexual function scores were similar or remained unchanged. In all other categories, total sexual function scores improved. Dyspareunia was lower after surgery for all prolapse surgery types.
“Although sexual function improves in the majority of women, it is important to note that a small proportion of women can develop de novo (new onset) dyspareunia after surgery. The rate of this ranges from 0%-9% for prolapse surgeries. However, there is limited data on posterior repairs,” Dr. Antosh said in a later interview.*
POP surgeries positively impact sexual function, dyspareunia outcomes
The researchers determined that there is “moderate to high quality data” supporting the influence of POP on sexual activity and function. They also observed a lower prevalence of dyspareunia postoperatively across all surgery types, compared with baseline. Additionally, no decrease in sexual function was reported across surgical categories; in fact, sexual activity and function improved or stayed the same after POP surgery in this review.
Across most POP surgery groups, Dr. Antosh and colleagues found that with the exception of the sacrospinous ligament suspension, transvaginal mesh, and sacrocolpopexy groups, the rate of postoperative sexual activity was modestly higher. Several studies attributed this finding to a lack of partner or partner-related issues. Another 16 studies (7.7%) cited pain as the primary factor for postoperative sexual inactivity.
Few studies included in the review “reported both preoperative and postoperative rates of sexual activity and dyspareunia, and no study reported patient-level changes in sexual activity or dyspareunia (except occasionally, for de novo activity or dyspareunia),” Dr. Antosh and associates clarified. As a result, they concluded that their findings are based primarily on qualitative comparisons of events reported pre- and postoperatively from different but overlapping sets of studies.
The finding that the prevalence of dyspareunia decreased following all types of POP surgery is consistent with previous reviews. Because the studies did not account for minimally important differences in sexual function scores, it is important to consider this when interpreting results of the review. Dr. Antosh and colleagues also noted that some studies did not define dyspareunia, and those that did frequently used measures that were not validated. They also were unable to identify the persistence of dyspareunia following surgery as this was not recorded in the literature.
Menopausal status and other considerations
Also worth noting, the mean age of women in the studies were postmenopausal, yet the “studies did not stratify sexual function outcomes based on premenopause compared with postmenopause status.”
The researchers advised that future studies using validated definitions of sexual activity, function, and dyspareunia, as well as reporting both their preoperative and postoperative measures would do much to improve the quality of research reported.
It is widely recognized that women with pelvic floor disorders experience a high rate of sexual dysfunction, so the need to achieve optimum outcomes that at least maintain if not improve sexual function postoperatively should be of key concern when planning POP surgery for patients, they cautioned. Previous studies have observed that women experiencing POP rated the need for improved sexual function second only to resolved bulge symptoms and improvement in overall function. The women also classified sexual dysfunction in the same category of adversity as having chronic pain or having to be admitted to an intensive care unit.
Study provides preoperative counseling help
David M. Jaspan, DO, chairman of the department of obstetrics and gynecology and Natasha Abdullah, MD, obstetrics and gynecology resident, both of Einstein Medical Center, Philadelphia, collaboratively commented on the study findings: “This review provides physicians with data to add to the preoperative counseling for patients undergoing pelvic organ prolapse surgery.”
In particular, they noted that, while the article “is a review of previous literature, Table 1 provides an opportunity for physicians to share with their patients the important answers to their concerns surrounding postoperative sexual activity, dyspareunia, and total changes in sexual function scores based on the Pelvic Organ Prolapse/Incontinence Sexual Questionnaire 12 (PISQ-12).”
Noting the clinical usefulness of the questionnaire, they added: “The PISQ-12 is a validated and reliable short form that evaluates sexual function in women with urinary incontinence and/or pelvic organ prolapse and predicts PISQ-31 scores. It was developed from the data of 99 of 182 women surveyed to create the long form (PISQ-31); 46 patients were recruited for further validation. Test-retest reliability was checked with a subset of 20 patients. All subsets regression analysis with R greater than 0.92 identified 12 items that predicted PISQ-31 scores. The PISQ-12 covers three domains of function: Behavioral/Emotive, Physical, and Partner-Related.”
Because ob.gyns. are trained to recognize the “multifactorial reasons (age, partner relationship, other health conditions etc.) that surround sexual activity,” Dr. Jaspan and Dr. Abdullah cautioned against prematurely concluding that the lower sexual activity score is directly related to POP surgery.
“Because sexual function is such an important postsurgical outcome for patients, this article provides significant preoperative counseling data for patients on all POP repair options,” they observed. “No surgical option worsens sexual function. The article concludes that individually validated definitions of sexual activity, function, and dyspareunia in a measuring instrument would improve the quality of data for future studies.”
The study authors reported no relevant financial disclosures. Although no direct funding was provided by the Society of Gynecologic Surgeons, they did provide meeting space, oversight, stipends for expert and statistical support, and aid in disseminating findings. Dr. Abdullah and Dr. Jaspan had no relevant financial disclosures.
SOURCE: Antosh DD et al. Obstet Gynecol. 2020. doi: 10.1097/AOG.0000000000004125.
*This article was updated on 10/28.
Danielle D. Antosh, MD, of the Houston Methodist Hospital and colleagues reported in a systematic review of prospective comparative studies on pelvic organ prolapse surgery, which was published in Obstetrics & Gynecology.
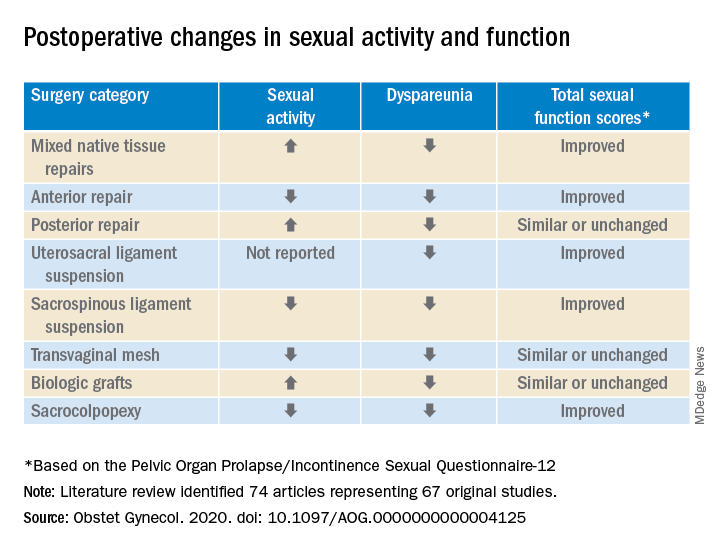
In a preliminary search of 3,124 citations, Dr. Antosh and her colleagues, who are members of the Society of Gynecologic Surgeons Systematic Review Group responsible for the study, identified and accepted 74 articles representing 67 original studies. Ten of these were ancillary studies with different reported outcomes or follow-up times, and 44 were randomized control trials. They compared the pre- and postoperative effects of pelvic organ prolapse (POP) surgery on sexual function for changes in sexual activity and function across eight different prolapse surgery categories: mixed native tissue repairs, anterior repair, posterior repair, uterosacral ligament suspension, sacrospinous ligament suspension, transvaginal mesh, biologic grafts, and sacrocolpopexy. In only three categories – posterior repair, transvaginal mesh, and biological grafts – postoperative changes in sexual function scores were similar or remained unchanged. In all other categories, total sexual function scores improved. Dyspareunia was lower after surgery for all prolapse surgery types.
“Although sexual function improves in the majority of women, it is important to note that a small proportion of women can develop de novo (new onset) dyspareunia after surgery. The rate of this ranges from 0%-9% for prolapse surgeries. However, there is limited data on posterior repairs,” Dr. Antosh said in a later interview.*
POP surgeries positively impact sexual function, dyspareunia outcomes
The researchers determined that there is “moderate to high quality data” supporting the influence of POP on sexual activity and function. They also observed a lower prevalence of dyspareunia postoperatively across all surgery types, compared with baseline. Additionally, no decrease in sexual function was reported across surgical categories; in fact, sexual activity and function improved or stayed the same after POP surgery in this review.
Across most POP surgery groups, Dr. Antosh and colleagues found that with the exception of the sacrospinous ligament suspension, transvaginal mesh, and sacrocolpopexy groups, the rate of postoperative sexual activity was modestly higher. Several studies attributed this finding to a lack of partner or partner-related issues. Another 16 studies (7.7%) cited pain as the primary factor for postoperative sexual inactivity.
Few studies included in the review “reported both preoperative and postoperative rates of sexual activity and dyspareunia, and no study reported patient-level changes in sexual activity or dyspareunia (except occasionally, for de novo activity or dyspareunia),” Dr. Antosh and associates clarified. As a result, they concluded that their findings are based primarily on qualitative comparisons of events reported pre- and postoperatively from different but overlapping sets of studies.
The finding that the prevalence of dyspareunia decreased following all types of POP surgery is consistent with previous reviews. Because the studies did not account for minimally important differences in sexual function scores, it is important to consider this when interpreting results of the review. Dr. Antosh and colleagues also noted that some studies did not define dyspareunia, and those that did frequently used measures that were not validated. They also were unable to identify the persistence of dyspareunia following surgery as this was not recorded in the literature.
Menopausal status and other considerations
Also worth noting, the mean age of women in the studies were postmenopausal, yet the “studies did not stratify sexual function outcomes based on premenopause compared with postmenopause status.”
The researchers advised that future studies using validated definitions of sexual activity, function, and dyspareunia, as well as reporting both their preoperative and postoperative measures would do much to improve the quality of research reported.
It is widely recognized that women with pelvic floor disorders experience a high rate of sexual dysfunction, so the need to achieve optimum outcomes that at least maintain if not improve sexual function postoperatively should be of key concern when planning POP surgery for patients, they cautioned. Previous studies have observed that women experiencing POP rated the need for improved sexual function second only to resolved bulge symptoms and improvement in overall function. The women also classified sexual dysfunction in the same category of adversity as having chronic pain or having to be admitted to an intensive care unit.
Study provides preoperative counseling help
David M. Jaspan, DO, chairman of the department of obstetrics and gynecology and Natasha Abdullah, MD, obstetrics and gynecology resident, both of Einstein Medical Center, Philadelphia, collaboratively commented on the study findings: “This review provides physicians with data to add to the preoperative counseling for patients undergoing pelvic organ prolapse surgery.”
In particular, they noted that, while the article “is a review of previous literature, Table 1 provides an opportunity for physicians to share with their patients the important answers to their concerns surrounding postoperative sexual activity, dyspareunia, and total changes in sexual function scores based on the Pelvic Organ Prolapse/Incontinence Sexual Questionnaire 12 (PISQ-12).”
Noting the clinical usefulness of the questionnaire, they added: “The PISQ-12 is a validated and reliable short form that evaluates sexual function in women with urinary incontinence and/or pelvic organ prolapse and predicts PISQ-31 scores. It was developed from the data of 99 of 182 women surveyed to create the long form (PISQ-31); 46 patients were recruited for further validation. Test-retest reliability was checked with a subset of 20 patients. All subsets regression analysis with R greater than 0.92 identified 12 items that predicted PISQ-31 scores. The PISQ-12 covers three domains of function: Behavioral/Emotive, Physical, and Partner-Related.”
Because ob.gyns. are trained to recognize the “multifactorial reasons (age, partner relationship, other health conditions etc.) that surround sexual activity,” Dr. Jaspan and Dr. Abdullah cautioned against prematurely concluding that the lower sexual activity score is directly related to POP surgery.
“Because sexual function is such an important postsurgical outcome for patients, this article provides significant preoperative counseling data for patients on all POP repair options,” they observed. “No surgical option worsens sexual function. The article concludes that individually validated definitions of sexual activity, function, and dyspareunia in a measuring instrument would improve the quality of data for future studies.”
The study authors reported no relevant financial disclosures. Although no direct funding was provided by the Society of Gynecologic Surgeons, they did provide meeting space, oversight, stipends for expert and statistical support, and aid in disseminating findings. Dr. Abdullah and Dr. Jaspan had no relevant financial disclosures.
SOURCE: Antosh DD et al. Obstet Gynecol. 2020. doi: 10.1097/AOG.0000000000004125.
*This article was updated on 10/28.
Danielle D. Antosh, MD, of the Houston Methodist Hospital and colleagues reported in a systematic review of prospective comparative studies on pelvic organ prolapse surgery, which was published in Obstetrics & Gynecology.
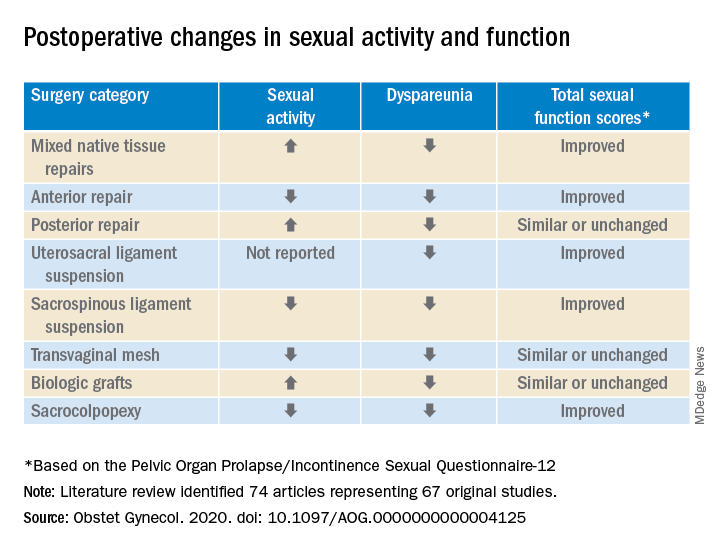
In a preliminary search of 3,124 citations, Dr. Antosh and her colleagues, who are members of the Society of Gynecologic Surgeons Systematic Review Group responsible for the study, identified and accepted 74 articles representing 67 original studies. Ten of these were ancillary studies with different reported outcomes or follow-up times, and 44 were randomized control trials. They compared the pre- and postoperative effects of pelvic organ prolapse (POP) surgery on sexual function for changes in sexual activity and function across eight different prolapse surgery categories: mixed native tissue repairs, anterior repair, posterior repair, uterosacral ligament suspension, sacrospinous ligament suspension, transvaginal mesh, biologic grafts, and sacrocolpopexy. In only three categories – posterior repair, transvaginal mesh, and biological grafts – postoperative changes in sexual function scores were similar or remained unchanged. In all other categories, total sexual function scores improved. Dyspareunia was lower after surgery for all prolapse surgery types.
“Although sexual function improves in the majority of women, it is important to note that a small proportion of women can develop de novo (new onset) dyspareunia after surgery. The rate of this ranges from 0%-9% for prolapse surgeries. However, there is limited data on posterior repairs,” Dr. Antosh said in a later interview.*
POP surgeries positively impact sexual function, dyspareunia outcomes
The researchers determined that there is “moderate to high quality data” supporting the influence of POP on sexual activity and function. They also observed a lower prevalence of dyspareunia postoperatively across all surgery types, compared with baseline. Additionally, no decrease in sexual function was reported across surgical categories; in fact, sexual activity and function improved or stayed the same after POP surgery in this review.
Across most POP surgery groups, Dr. Antosh and colleagues found that with the exception of the sacrospinous ligament suspension, transvaginal mesh, and sacrocolpopexy groups, the rate of postoperative sexual activity was modestly higher. Several studies attributed this finding to a lack of partner or partner-related issues. Another 16 studies (7.7%) cited pain as the primary factor for postoperative sexual inactivity.
Few studies included in the review “reported both preoperative and postoperative rates of sexual activity and dyspareunia, and no study reported patient-level changes in sexual activity or dyspareunia (except occasionally, for de novo activity or dyspareunia),” Dr. Antosh and associates clarified. As a result, they concluded that their findings are based primarily on qualitative comparisons of events reported pre- and postoperatively from different but overlapping sets of studies.
The finding that the prevalence of dyspareunia decreased following all types of POP surgery is consistent with previous reviews. Because the studies did not account for minimally important differences in sexual function scores, it is important to consider this when interpreting results of the review. Dr. Antosh and colleagues also noted that some studies did not define dyspareunia, and those that did frequently used measures that were not validated. They also were unable to identify the persistence of dyspareunia following surgery as this was not recorded in the literature.
Menopausal status and other considerations
Also worth noting, the mean age of women in the studies were postmenopausal, yet the “studies did not stratify sexual function outcomes based on premenopause compared with postmenopause status.”
The researchers advised that future studies using validated definitions of sexual activity, function, and dyspareunia, as well as reporting both their preoperative and postoperative measures would do much to improve the quality of research reported.
It is widely recognized that women with pelvic floor disorders experience a high rate of sexual dysfunction, so the need to achieve optimum outcomes that at least maintain if not improve sexual function postoperatively should be of key concern when planning POP surgery for patients, they cautioned. Previous studies have observed that women experiencing POP rated the need for improved sexual function second only to resolved bulge symptoms and improvement in overall function. The women also classified sexual dysfunction in the same category of adversity as having chronic pain or having to be admitted to an intensive care unit.
Study provides preoperative counseling help
David M. Jaspan, DO, chairman of the department of obstetrics and gynecology and Natasha Abdullah, MD, obstetrics and gynecology resident, both of Einstein Medical Center, Philadelphia, collaboratively commented on the study findings: “This review provides physicians with data to add to the preoperative counseling for patients undergoing pelvic organ prolapse surgery.”
In particular, they noted that, while the article “is a review of previous literature, Table 1 provides an opportunity for physicians to share with their patients the important answers to their concerns surrounding postoperative sexual activity, dyspareunia, and total changes in sexual function scores based on the Pelvic Organ Prolapse/Incontinence Sexual Questionnaire 12 (PISQ-12).”
Noting the clinical usefulness of the questionnaire, they added: “The PISQ-12 is a validated and reliable short form that evaluates sexual function in women with urinary incontinence and/or pelvic organ prolapse and predicts PISQ-31 scores. It was developed from the data of 99 of 182 women surveyed to create the long form (PISQ-31); 46 patients were recruited for further validation. Test-retest reliability was checked with a subset of 20 patients. All subsets regression analysis with R greater than 0.92 identified 12 items that predicted PISQ-31 scores. The PISQ-12 covers three domains of function: Behavioral/Emotive, Physical, and Partner-Related.”
Because ob.gyns. are trained to recognize the “multifactorial reasons (age, partner relationship, other health conditions etc.) that surround sexual activity,” Dr. Jaspan and Dr. Abdullah cautioned against prematurely concluding that the lower sexual activity score is directly related to POP surgery.
“Because sexual function is such an important postsurgical outcome for patients, this article provides significant preoperative counseling data for patients on all POP repair options,” they observed. “No surgical option worsens sexual function. The article concludes that individually validated definitions of sexual activity, function, and dyspareunia in a measuring instrument would improve the quality of data for future studies.”
The study authors reported no relevant financial disclosures. Although no direct funding was provided by the Society of Gynecologic Surgeons, they did provide meeting space, oversight, stipends for expert and statistical support, and aid in disseminating findings. Dr. Abdullah and Dr. Jaspan had no relevant financial disclosures.
SOURCE: Antosh DD et al. Obstet Gynecol. 2020. doi: 10.1097/AOG.0000000000004125.
*This article was updated on 10/28.
FROM OBSTETRICS & GYNECOLOGY

