User login
CE/CME No: CR-1710
PROGRAM OVERVIEW
Earn credit by reading this article and successfully completing the posttest and evaluation. Successful completion is defined as a cumulative score of at least 70% correct.
EDUCATIONAL OBJECTIVES
• Describe the main factors involved in the pathogenesis of acne.
• Assess acne severity and classify acne as mild, moderate, or severe.
• Describe available acne therapies, including their mechanisms of action, indications, and potential adverse effects.
• Identify strategies patients can employ to mitigate the adverse effects of acne treatments.
FACULTY
Janet Purath is an Associate Professor at Washington State University in Spokane, Washington. Theresa Coyner practices at Randall Dermatology, West Lafayette, Indiana.
The authors have no financial relationships to disclose.
ACCREDITATION STATEMENT
This program has been reviewed and is approved for a maximum of 1.0 hour of American Academy of Physician Assistants (AAPA) Category 1 CME credit by the Physician Assistant Review Panel. [NPs: Both ANCC and the AANP Certification Program recognize AAPA as an approved provider of Category 1 credit.] Approval is valid through September 30, 2018.
Article begins on next page >>
Many of the 50 million persons affected by acne in the United States present to primary care. Acne severity guides treatment choices, which include topical antibiotics and retinoids, hormonal agents, and systemic antibiotics and retinoids. Formulating a treatment plan requires a thorough understanding of the dosing, mechanism of action, and potential adverse effects of available medications.
Acne vulgaris (acne) is a common skin condition that is frequently encountered in primary care. Acne affects up to 50 million people in the United States, and about 85% of teenagers experience it at some point.1 Costs for treatment exceed $3 billion per year.2 Although commonly considered a condition of adolescence and young adults (85% prevalence), acne may persist in both men and women well into their 30s and 40s (43% prevalence). In fact, 5% of women ages 40 and older may experience acne.3
Acne is associated with considerable, long-lasting psychological sequelae, even in those with mild conditions, as many affected patients experience self-esteem issues and may avoid social interactions.4 Recognition of patients’ concerns about acne will help to promote a trusting patient-provider relationship. This article describes the pathophysiology and classifications of acne and reviews therapeutic options, enabling the practitioner to initiate treatment.
PRESENTATION AND ASSESSMENT
Acne lesions may occur on the face, neck, trunk, and extremities. The severity of acne is assessed based on lesion type, number, and size, and this grading is used to inform decisions about treatment options. Mild acne is characterized by plugging of the sebaceous gland (comedones), with small numbers of inflammatory papules and pustules. Moderate acne involves a larger number of inflammatory papules/pustules as well as the presence of small cystic nodules. Severe acne is marked by the presence of large numbers of noninflammatory and inflammatory lesions and cystic nodules or widespread involvement of these lesions.5 Examples of mild, moderate, and severe acne are shown in Figure 1. Assessment should include questions about the patient’s experiences with prior therapies.

PATHOGENESIS
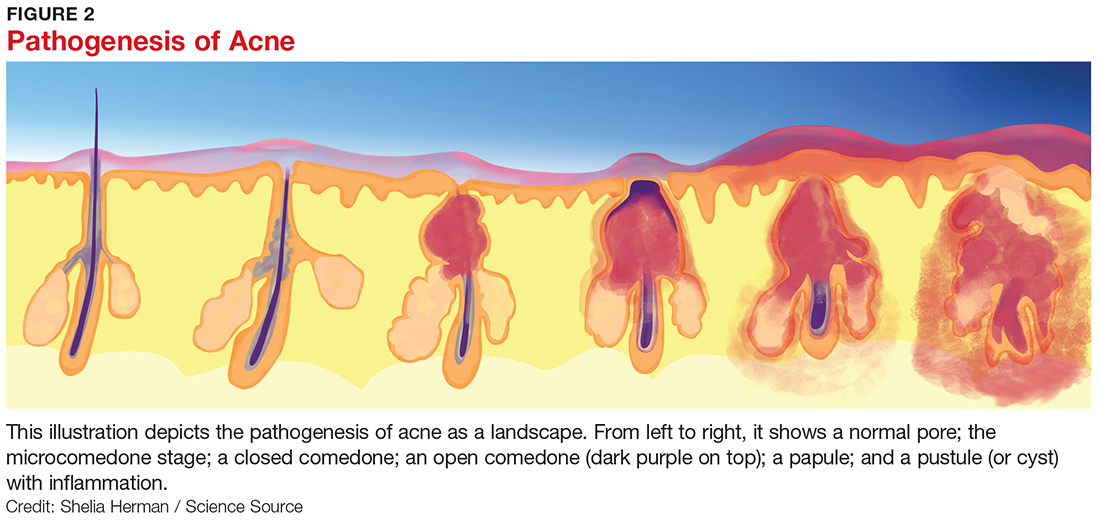
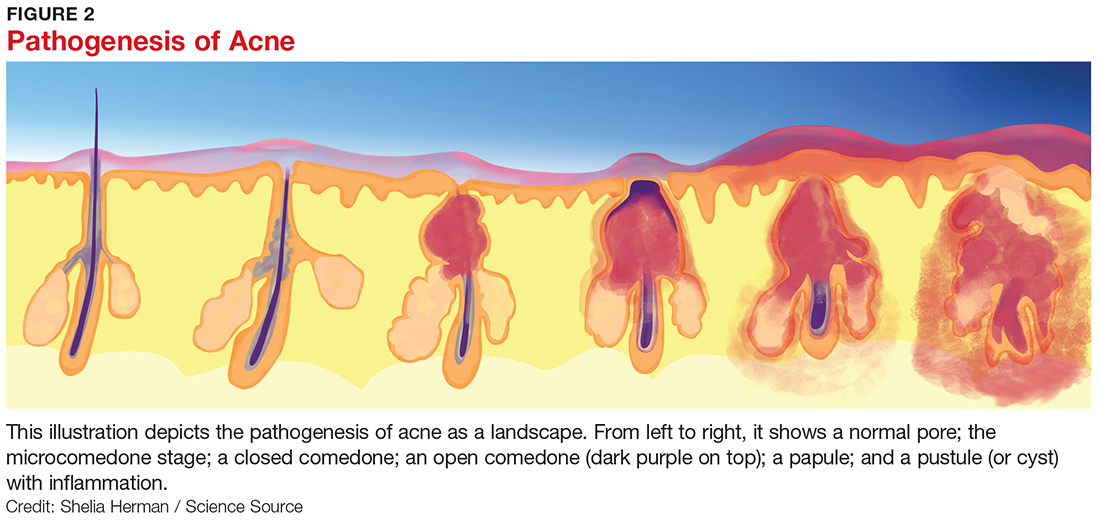
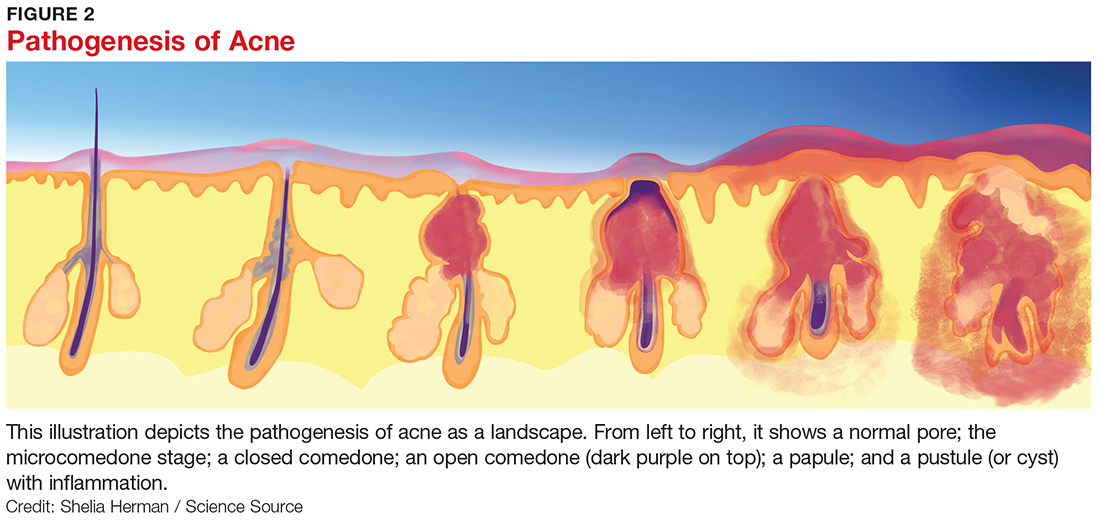
The pathogenesis of acne is a complex process involving multiple factors (see Figure 2). Knowledge about acne pathogenesis continues to evolve, but the current view is that a combination of simultaneous noninflammatory and inflammatory events involving pilosebaceous units (which consist of sebaceous glands and hair follicles) contribute to its development.6 Activation of the sebaceous glands is influenced by androgens, which increase sebum production and shedding of the keratinocytes lining the gland. Plugging of the pilosebaceous canal ensues, leading to the development of a microcomedone. Increased proliferation of Propionibacterium acnes occurs within the obstructed gland. The inflammatory response to this process includes a cascade of numerous cytokines, most notably toll-like receptor 2 (TLR-2).7 The plug at the opening of the sebaceous gland creates either an open comedone (blackhead) or a closed comedone (whitehead). Eventually, the follicular wall ruptures, leading to the formation of erythematous papules and pustules on the skin surface or deep-seated cystic structures under the skin surface. Current pharmacologic agents target one or more of these identified factors underlying acne pathogenesis.
THERAPEUTIC OPTIONS
Pharmacologic treatment options for acne include topical, systemic, and hormonal agents. Topical and systemic therapies reduce inflammation and follicular plugging. Topical treatments include antibiotics, anti-inflammatories, and retinoids. Oral treatments include antibiotics, hormones, and retinoids. The clinician must have a thorough understanding of the actions, potential adverse reactions, and drug interactions of each proposed therapy prior to formulating a treatment plan.
Topical retinoids
Topical retinoids are the most effective comedolytic agents available.1 Since comedones are thought to be the precursor of all other acne lesions, retinoids are appropriate for cases in which comedones are seen.1 Retinoids belong to a class of compounds structurally related to vitamin A. Topical retinoids act by promoting normal follicular keratinocyte desquamation, which prevents obstruction of the pilosebaceous canal and thereby inhibits the formation of microcomedones.8
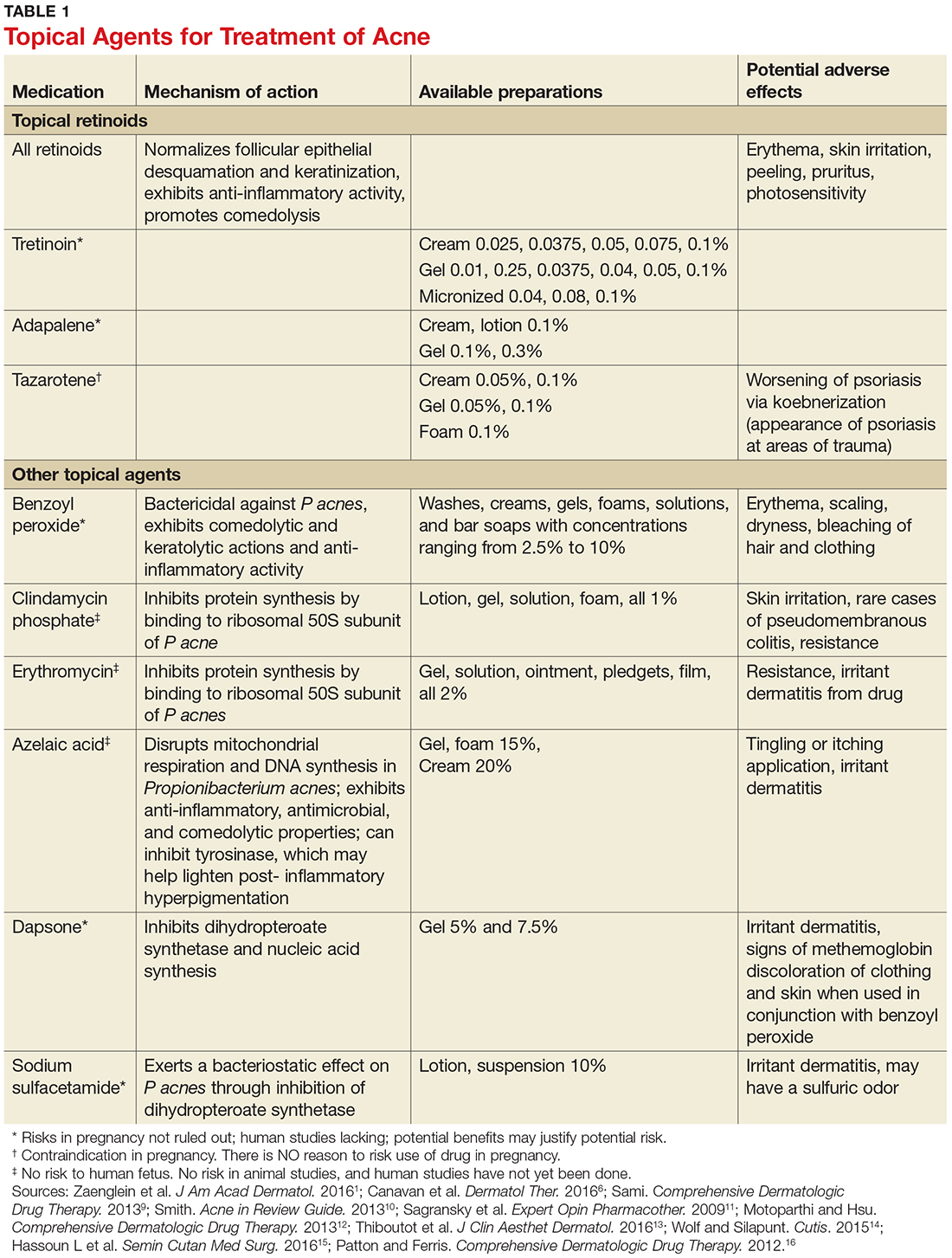
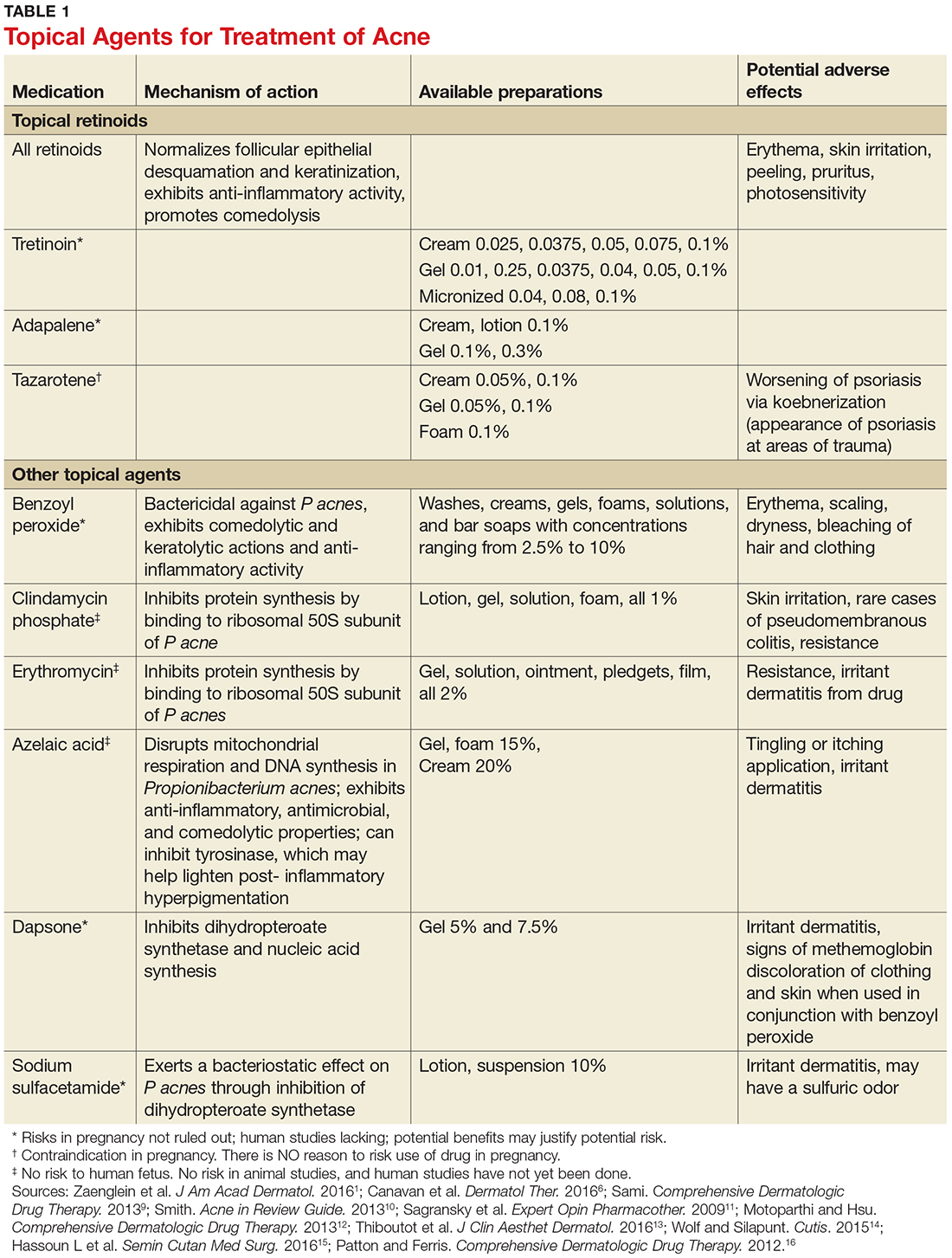
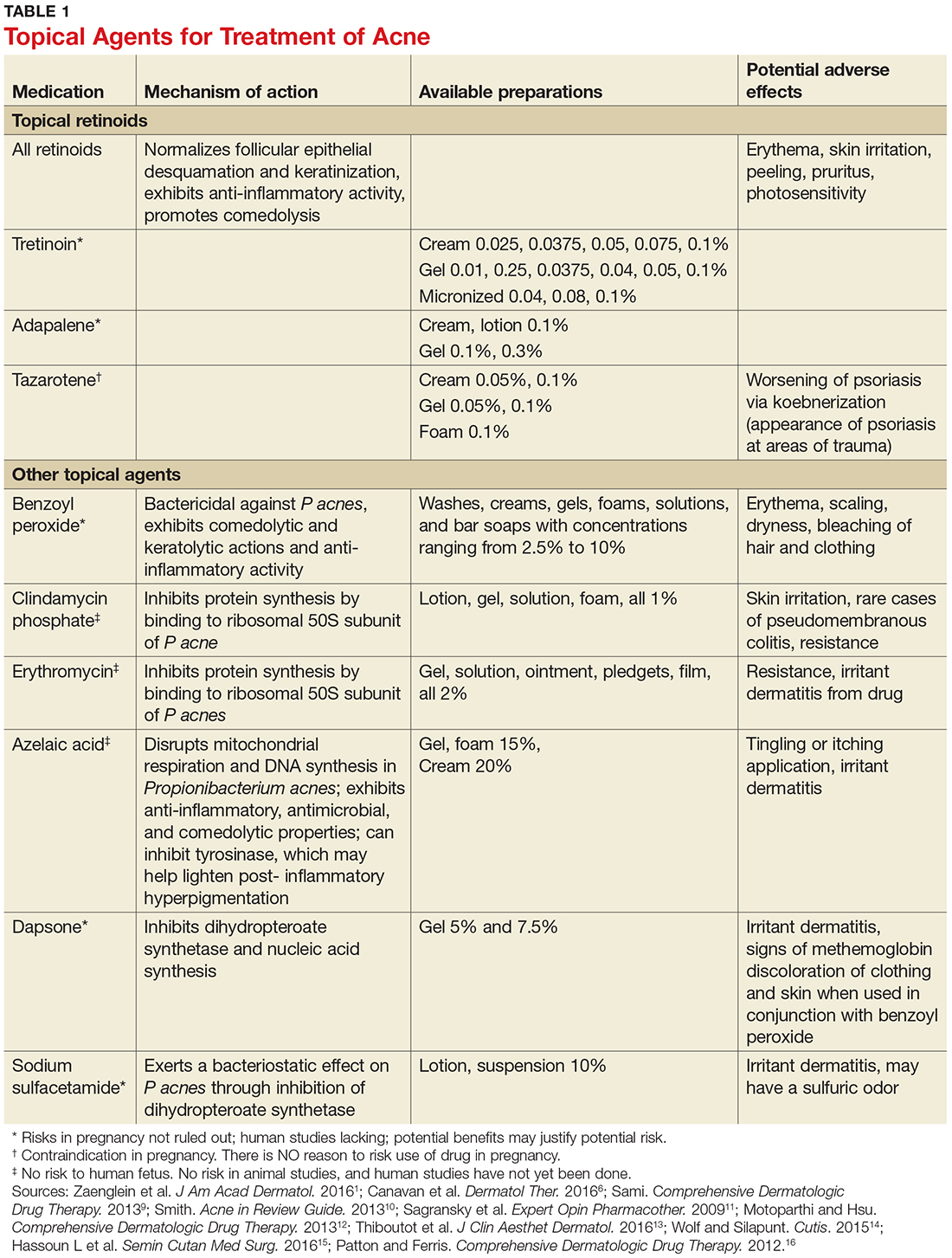
They also exhibit anti-inflammatory action via inhibition of TLR-2.9 The comedolytic and anti-inflammatory actions of topical retinoids make them a mainstay of acne treatment, although some patients are unable to tolerate their adverse effects, which include erythema and dryness related to increases in transepidermal water loss. Application of noncomedogenic emollients can improve these common effects.10 The newer micronized and time-release retinoid formulations may have less potential for irritation.8 Vehicle formulation and concentration also play a role in skin irritation, with gels and liquids and formulations with higher concentrations of retinoids generally causing more drying than creams and lower potency formulations.8 Table 1 summarizes the mechanisms of action, available formulations, and potential adverse effects of the topical retinoids and other topical agents.1,6,9-16
It is important to note that retinoids can adversely affect the developing fetus when absorbed in large quantities. Notably, tazarotene is assigned to pregnancy category X because when it is used to treat psoriasis, one of its approved indications, large surface areas may be treated, increasing absorption. Absorption amounts are extremely low when tazarotene is used to treat acne. Nevertheless, verification of a negative pregnancy test is recommended prior to initiating tazarotene therapy. Effective birth control measures should be utilized throughout therapy. Even though other commonly used retinoids (tretinoin and adapalene) are assigned to pregnancy category C, all topical retinoids should be avoided during pregnancy.9
As noted, patient education is key for increasing patient adherence to therapy. Patients should be instructed to use a small (pea-sized) amount of medication for the entire face. Providers should also inform patients that transient erythema and dryness can be expected, and that application of a noncomedolytic moisturizer may reduce irritation. Tretinoin is best used at night,1 and it is useful to advise that erythema and irritation associated with retinoid use can be reduced by initially using the medication every other night to every third night, gradually building up to nightly use.1
Topical antibiotic and anti-inflammatory agents
Topical agents used to treat inflammatory lesions include benzoyl peroxide, erythromycin, clindamycin, dapsone, azelaic acid, and sulfacetamide (Table 1).1,6,9-16 These topical agents are generally well tolerated, with most adverse reactions limited to facial irritation and erythema. They come in an array of vehicle formulations, including washes, creams, gels, solutions, foams, and lotions. Vehicle selection should be based upon patient preference and skin type. Gels and solutions have a drying effect, making them more appropriate for individuals with oily skin, whereas creams are moisturizing and appropriate for individuals with dry skin. Lotions are appropriate for all skin types.11
Benzoyl peroxide (BPO) has both keratolytic and comedolytic activity and is available in concentrations ranging from 2.5% to 10%. It is available OTC, as well as by prescription, and is thus readily accessed by the patient. Because BPO is bactericidal for P acnes, resistance to BPO among P acnes has not occurred.1 All concentrations are equally effective, but the higher concentrations are more likely to cause skin dryness and other adverse effects.12 Combination therapy with topical antibiotics, tretinoin, and BPO is more clinically effective than monotherapy.17 Combination products reduce the complexity of acne treatment and likely increase therapy adherence.11 Currently available combination products in various percentages are erythromycin with BPO, clindamycin with BPO, adapalene with BPO, and clindamycin with tretinoin.1
Oral antibiotics
Oral antibiotics should be reserved for use in situations where topical therapy is ineffective. All antibiotics are effective in treating acne due to their antimicrobial activity against P acnes.1 These agents play a key role in managing moderate to severe acne that is likely to scar, as well as in cases of widespread acne involving the face, arms, and trunk. Note that the use of oral antibiotics in acne treatment is controversial, as chronic use contributes to rising rates of bacterial resistance.18 For this reason, antibiotic therapy for acne should be limited to a duration of three months or less, and these agents should not be used as monotherapy.6 In particular, recent recommendations restrict the use of erythromycin for acne treatment due to an increase of P acnes resistance.1 Cephalosporins, macrolides, and penicillin class antibiotics are not routinely recommended due to lack of data regarding their clinical effectiveness in treating acne.1
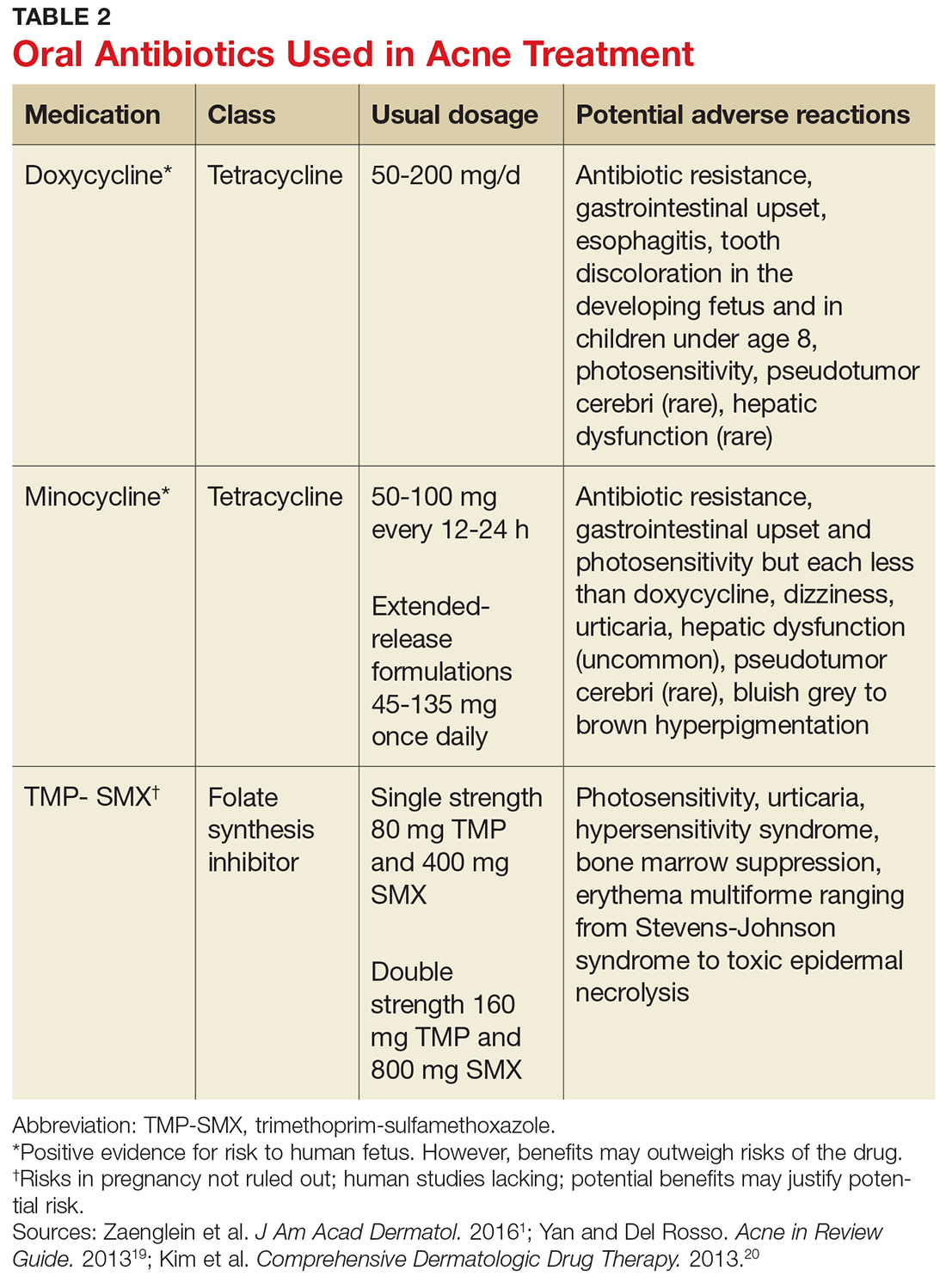
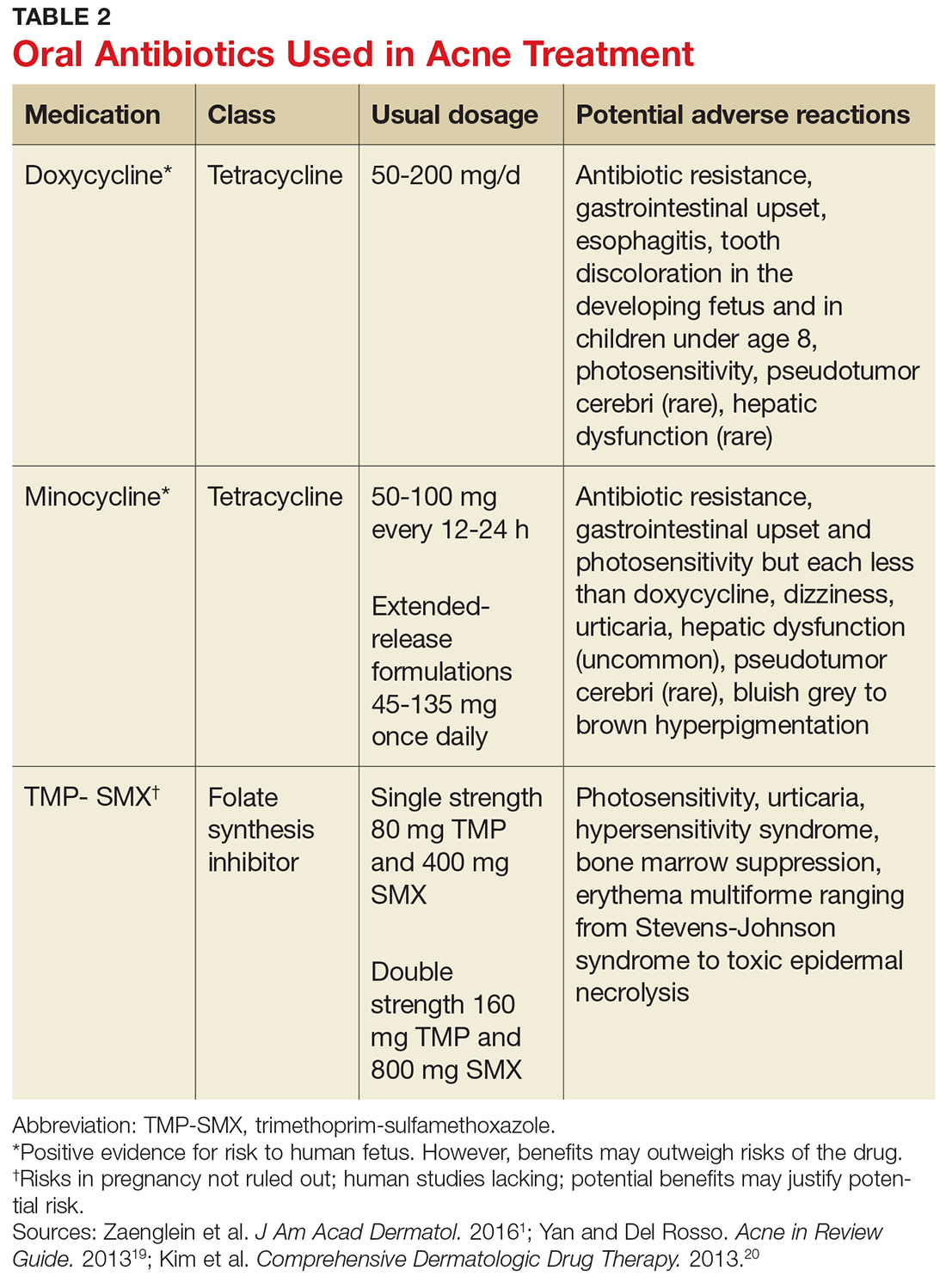
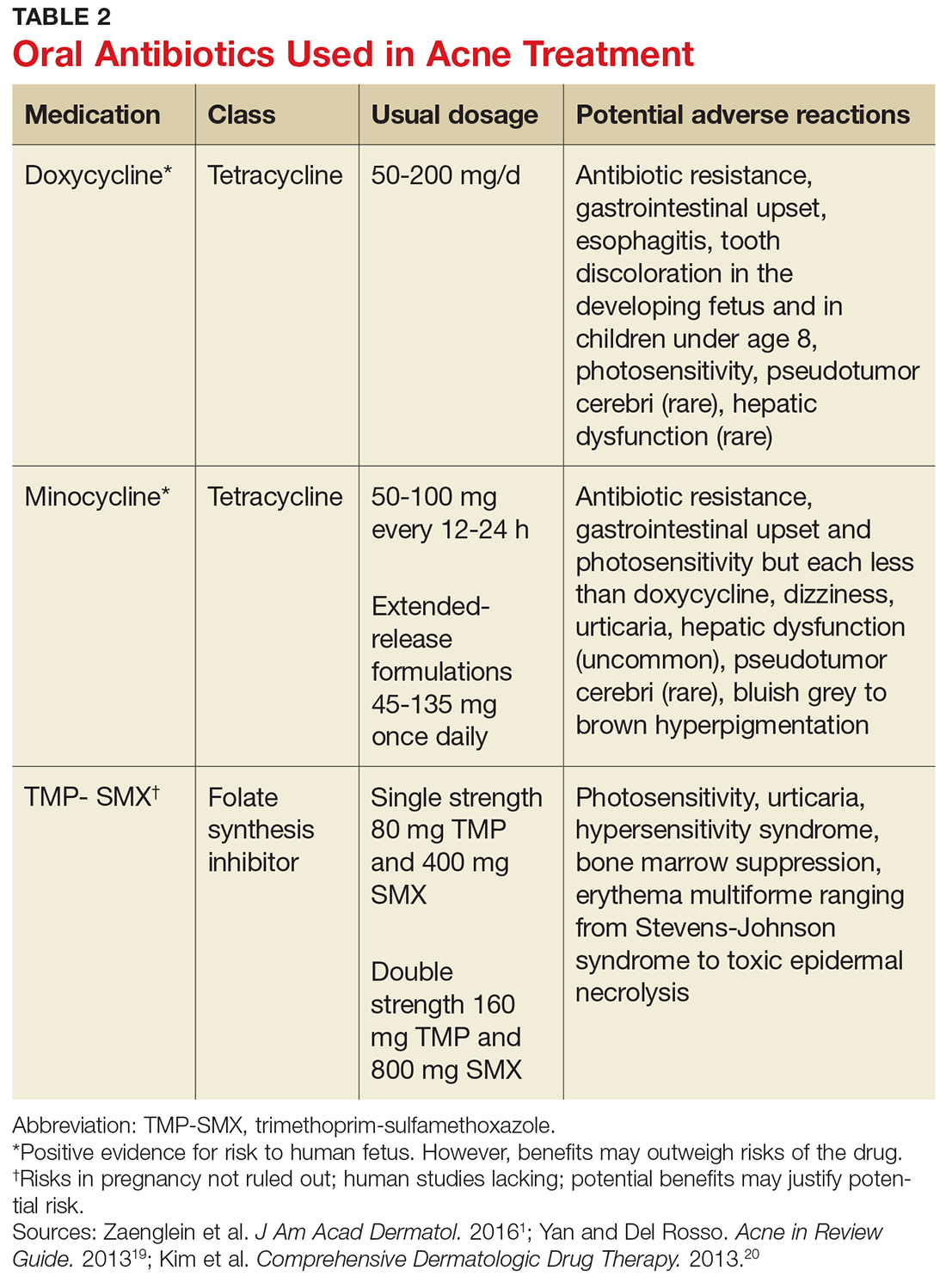
Tetracycline class antibiotics are the most commonly used oral antibiotics for acne therapy, particularly doxycycline and minocycline.5 Common adverse effects include gastrointestinal upset, photosensitivity, and some pigmentation issues.19 Trimethoprim-sulfamethoxazole (TMP-SMX) is a folate synthesis inhibitor class antibiotic also used to treat acne. Its use should be reserved for individuals who are allergic to tetracyclines or in cases of acne resistant to other antimicrobials.1 Potential adverse reactions include photosensitivity and severe hypersensitivity conditions ranging from a mild rash to toxic epidermal necrolysis.19 Table 2 summarizes the dosage ranges, pregnancy category risk, and potential adverse effects of oral antibiotics used to treat acne.1,19,20
The firstline choice for treating moderate acne with papules and pustules is oral antibiotics with topical retinoids and BPO.5 Patients should be educated about potential adverse effects of these agents, including the development of antibiotic resistance.
Hormonal agents
Hormonal therapies should be reserved for females with acne lesions influenced by fluctuations in hormone levels.21 Pubertal changes initiate the production of adrenal dehydroepiandrosterone, which leads to increased testosterone production. Testosterone is converted to dihydrotestosterone (DHT), which binds to androgen receptors in the sebaceous glands, stimulating the glands and potentially increasing production of sebum. Hormonal agents act by reducing androgen activity in the sebaceous gland. Combined oral hormones, those containing both estrogen and progesterone, reduce the amount of free testosterone and ovarian androgens by suppressing ovulation.1 Hormonal therapy can be quite effective for females of childbearing age. Females who report acne flares with their menstrual cycles may be good candidates for hormonal therapy.1
The estrogen agent most frequently used in oral contraceptives is ethinyl estradiol. Numerous progesterone agents can also be used, but those with low
Spironolactone, a potassium-sparing diuretic, may also be appropriate for treating acne in women due to its antiandrogenic properties. The drug binds androgen receptors in the skin, which then blocks testosterone and DHT. Spironolactone can be an effective firstline agent in treating hormonal-pattern acne, which presents as inflammatory lesions located on the lower face and neck. In particular, it can be an appropriate choice for women with adult-onset acne.15 Spironolactone is not approved by the FDA for acne treatment, but it has been used successfully for many years.5 Spironolactone was found in rodent studies to cause feminization of the male rat fetus, so patients taking this drug should use reliable birth control methods. It can be used concomitantly with oral contraceptives.5 Common side effects include breast tenderness, diuretic effects, headaches, and menstrual irregularities. Although the risk for hypokalemia is low in healthy young women, it may be prudent to periodically assess potassium, sodium, and renal function in patients.1 Spironolactone should be avoided in patients with renal disease and those on other diuretics.15
Isotretinoin
Isotretinoin is an oral systemic retinoid that modulates nuclear receptors and regulates gene transcription in the epidermis.16 Isotretinoin’s mechanisms of action target the main pathogenic factors underlying acne, including reduction of follicular hyperkeratosis, comedogenesis, sebum production, and inflammation and suppression of P acnes.22 These combined actions make isotretinoin a highly effective treatment option for acne.
The drug is approved by the FDA for treatment of nodular acne refractory to traditional acne therapies.23 Isotretinoin is available in 10, 20, 25, 30, and 40 mg capsules, and the recommended dosing is 0.5 to 2.0 mg/kg/d. The usual course of therapy is 15 to 20 weeks or until an accumulative dosage of 120 to 150 mg/kg is attained.23 Patients should be instructed to take isotretinoin with meals, as oral availability is increased with high-fat foods.23
Isotretinoin has major adverse effects. It is a teratogenic medication that can cause congenital anomalies in exposed fetuses, including craniofacial, cardiac, and neurologic issues.16 Due to the seriousness of the congenital anomalies, all prescribers must be registered in the iPledge program, a computer-based risk management program instituted in 2006 by the FDA and the companies that manufacture isotretinoin to eliminate congenital risks associated with isotretinoin. All patients, both male and female, must sign an informed consent form when they register in the program.
Although the iPledge program does not mandate consistent condom use for male patients, they should be informed that minute amounts of isotretinoin can be found in semen. The risk for fathering a fetus with congenital anomalies when taking isotretinoin appears to be extremely low.16 Women of childbearing potential must commit to the use of two highly reliable forms of birth control when taking the medication, including one month before starting therapy and one month after completing therapy.16 Monthly pregnancy testing is mandatory throughout the course of treatment.24 Further information regarding the risk management program can be found at iPledgeprogram.com.
Isotretinoin is metabolized by the liver and may cause lipid abnormalities and hepatic enzyme elevations. Baseline and monthly laboratory monitoring of liver enzymes and cholesterol and triglyceride levels are recommended.24 The process of initiating and monitoring isotretinoin therapy is quite complex, and unless the practitioner plans to routinely prescribe this medication, patients needing isotretinoin therapy should be referred to a dermatology practice.
PATIENT EDUCATION
Patients are more likely to adhere to treatment when simplified regimens are used and when they have realistic expectations for therapy outcomes. Providers need to educate patients that all treatments may require at least two to three months of use before visible results occur. Initial and subsequent visits should include discussions about clear expectations and strategies to reduce potential adverse effects.
PUTTING IT ALL TOGETHER
Acne therapy starts with the use of a topical retinoid in mild acne cases, unless the patient is unable to tolerate the associated skin irritability. Addition of a topical antibiotic or anti-inflammatory agent, preferably BPO, either alone or with a combination product, is also recommended for mild to moderate acne. Patients with moderate to severe acne may benefit from a short course (three months or less) of antibiotics.
Oral hormones may be an excellent therapy choice when acne treatment is needed for women of childbearing age. Isotretinoin is indicated in select cases of severe acne resistant to other treatments.
1. Zaenglein AL, Pathy AL, Schlosser BJ, et al. Guidelines of care for the management of acne vulgaris. J Am Acad Dermatol. 2016;74(5):945-973.
2. Bhate K, Williams HC. Epidemiology of acne vulgaris. Br J Dermatol. 2013;168(3):474-485.
3. Collier CN, Harper JC, Cafardi JA, et al. The prevalence of acne in adults 20 years and older. J Am Acad Dertmatol. 2008;58(1):56-59.
4. Dunn LK, O’Neill JL, Feldman SR. Acne in adolescents: quality of life, self-esteem, mood, and psychological disorders. Dermatol Online J. 2011;17(1):1.
5. Baldwin HE, Zanglein AL, Leyden JJ, Webster GF. Pharmacologic treatment options in mild, moderate, and severe acne vulgaris. Semin Cutan Med Surg. 2015;34(supp5):S82-S85.
6. Canavan TN, Chen E, Elewski BE. Optimizing non-antibiotic treatments for patients with acne: a review. Dermatol Ther. 2016;6(4):555-578.
7. Bellew S, Thiboutot D, Del Rosso JQ. Pathogenesis of acne vulgaris: what’s new, what’s interesting and what may be clinically relevant. J Drugs Dermatol. 2011;10(6):582-585.
8. Russell JJ. Topical therapy for acne. Am Fam Phys. 2000; 61(2):357-365.
9. Sami N. Topical retinoids. In: Wolverton SE, ed. Comprehensive Dermatologic Drug Therapy. 3rd ed. St. Louis: Elsevier; 2013:505-517.
10. Smith RI. Treatments: Retinoids. In: Mancini AJ, Eichenfield LF, Del Rosso JQ, eds. Acne in Review Guide. New York: Educational Testing and Assessment Systems/SanovaWorks; 2013:59-63.
11. Sagransky M, Yentzer BA, Feldman SR. Benzoyl peroxide: a review of its current use in the treatment of acne vulgaris. Expert Opin Pharmacother. 2009;10(15):2555-2562.
12. Motoparthi K, Hsu S. Topical antibacterial agents. In: Wolverton SE, ed. Comprehensive Dermatologic Drug Therapy. 3rd ed. St Louis: Elsevier; 2013:452-459.
13. Thiboutot DM, Kircik L, McMichale A, et al. Efficacy, safety, and dermal tolerability of dapsone gel, 7.5% in patients with moderate acne vulgaris: a pooled analysis of two phase 3 trials. J Clin Aesthet Dermatol. 2016;9(10):18-27.
14. Wolf K, Silapunt S. The use of sodium sulfacetamide in dermatology. Cutis. 2015;96(2):128-130.
15. Hassoun LA, Chahal DS, Sivamani RK, Larsen LN. The use of hormonal agents in the treatment of acne. Semin Cutan Med Surg. 2016;35(2):68-73.
16. Patton TJ, Ferris LK. Systemic retinoids. In: Wolverton SE, ed. Comprehensive Dermatologic Drug Therapy. 3rd ed. St Louis: Elsevier; 2012:252-268.
17. Thiboutot D, Gollnick H, Bettoli V, et al. New insights into the management of acne: an update from the Global Alliance to Improve Outcomes in Acne group. J Am Acad Dermatol. 2009;60(5 Suppl):S1-S50.
18. Walsh TR, Efthimious J, Dreno B. Systematic review of antibiotic resistance in acne: an increasing topical and oral threat. Lancet Infect Dis. 2016;16(3):e22-32.
19. Yan AC, Del Rosso JQ. Prescription oral treatments: Antibiotics. In: Mancini AJ, Eichenfield LF, Del Rosso JQ, eds. Acne in Review Guide. New York: Educational Testing and Assessment Systems/SanovaWorks; 2013:77-87.
20. Kim S, Michaels BD, Kim GK, Del Rosso JQ. Systemic antibacterial agents. In: Wolverton SE, ed. Comprehensive Dermatologic Drug Therapy. 3rd ed. St Louis: Elsevier; 2013:62-67, 70-74, 77-85.
21. Hecht CT, Sidbury R, Del Rosso JQ. Prescription oral treatments: Hormonal therapies. In: Mancini AJ, Eichenfield LF, Del Rosso JQ, eds. Acne in Review Guide. New York: Educational Testing and Assessment Systems/SanovaWorks; 2013:89-95.
22. Webster GF, Leyden JJ, Baldwin HE, Zaenglein AL. Isotretinoin: mechanism of action and patient selection. Semin Cutan Med Surg. 2015;34(supp 5):S86-S88.
23. Leyden JJ, Del Rosso JQ, Baum EW. The use of isotretinoin in the treatment of acne vulgaris. J Clin and Aesthet Dermatol. 2014;7(2 Suppl):S3-S21.
24. Zane LT, Leyden WA, Marqueling AL, Manos MM. A population-based analysis of laboratory abnormalities during isotretinoin therapy for acne vulgaris. Arch Dermatol. 2006;142(8):1016-1022.
CE/CME No: CR-1710
PROGRAM OVERVIEW
Earn credit by reading this article and successfully completing the posttest and evaluation. Successful completion is defined as a cumulative score of at least 70% correct.
EDUCATIONAL OBJECTIVES
• Describe the main factors involved in the pathogenesis of acne.
• Assess acne severity and classify acne as mild, moderate, or severe.
• Describe available acne therapies, including their mechanisms of action, indications, and potential adverse effects.
• Identify strategies patients can employ to mitigate the adverse effects of acne treatments.
FACULTY
Janet Purath is an Associate Professor at Washington State University in Spokane, Washington. Theresa Coyner practices at Randall Dermatology, West Lafayette, Indiana.
The authors have no financial relationships to disclose.
ACCREDITATION STATEMENT
This program has been reviewed and is approved for a maximum of 1.0 hour of American Academy of Physician Assistants (AAPA) Category 1 CME credit by the Physician Assistant Review Panel. [NPs: Both ANCC and the AANP Certification Program recognize AAPA as an approved provider of Category 1 credit.] Approval is valid through September 30, 2018.
Article begins on next page >>
Many of the 50 million persons affected by acne in the United States present to primary care. Acne severity guides treatment choices, which include topical antibiotics and retinoids, hormonal agents, and systemic antibiotics and retinoids. Formulating a treatment plan requires a thorough understanding of the dosing, mechanism of action, and potential adverse effects of available medications.
Acne vulgaris (acne) is a common skin condition that is frequently encountered in primary care. Acne affects up to 50 million people in the United States, and about 85% of teenagers experience it at some point.1 Costs for treatment exceed $3 billion per year.2 Although commonly considered a condition of adolescence and young adults (85% prevalence), acne may persist in both men and women well into their 30s and 40s (43% prevalence). In fact, 5% of women ages 40 and older may experience acne.3
Acne is associated with considerable, long-lasting psychological sequelae, even in those with mild conditions, as many affected patients experience self-esteem issues and may avoid social interactions.4 Recognition of patients’ concerns about acne will help to promote a trusting patient-provider relationship. This article describes the pathophysiology and classifications of acne and reviews therapeutic options, enabling the practitioner to initiate treatment.
PRESENTATION AND ASSESSMENT
Acne lesions may occur on the face, neck, trunk, and extremities. The severity of acne is assessed based on lesion type, number, and size, and this grading is used to inform decisions about treatment options. Mild acne is characterized by plugging of the sebaceous gland (comedones), with small numbers of inflammatory papules and pustules. Moderate acne involves a larger number of inflammatory papules/pustules as well as the presence of small cystic nodules. Severe acne is marked by the presence of large numbers of noninflammatory and inflammatory lesions and cystic nodules or widespread involvement of these lesions.5 Examples of mild, moderate, and severe acne are shown in Figure 1. Assessment should include questions about the patient’s experiences with prior therapies.

PATHOGENESIS
The pathogenesis of acne is a complex process involving multiple factors (see Figure 2). Knowledge about acne pathogenesis continues to evolve, but the current view is that a combination of simultaneous noninflammatory and inflammatory events involving pilosebaceous units (which consist of sebaceous glands and hair follicles) contribute to its development.6 Activation of the sebaceous glands is influenced by androgens, which increase sebum production and shedding of the keratinocytes lining the gland. Plugging of the pilosebaceous canal ensues, leading to the development of a microcomedone. Increased proliferation of Propionibacterium acnes occurs within the obstructed gland. The inflammatory response to this process includes a cascade of numerous cytokines, most notably toll-like receptor 2 (TLR-2).7 The plug at the opening of the sebaceous gland creates either an open comedone (blackhead) or a closed comedone (whitehead). Eventually, the follicular wall ruptures, leading to the formation of erythematous papules and pustules on the skin surface or deep-seated cystic structures under the skin surface. Current pharmacologic agents target one or more of these identified factors underlying acne pathogenesis.
THERAPEUTIC OPTIONS
Pharmacologic treatment options for acne include topical, systemic, and hormonal agents. Topical and systemic therapies reduce inflammation and follicular plugging. Topical treatments include antibiotics, anti-inflammatories, and retinoids. Oral treatments include antibiotics, hormones, and retinoids. The clinician must have a thorough understanding of the actions, potential adverse reactions, and drug interactions of each proposed therapy prior to formulating a treatment plan.
Topical retinoids
Topical retinoids are the most effective comedolytic agents available.1 Since comedones are thought to be the precursor of all other acne lesions, retinoids are appropriate for cases in which comedones are seen.1 Retinoids belong to a class of compounds structurally related to vitamin A. Topical retinoids act by promoting normal follicular keratinocyte desquamation, which prevents obstruction of the pilosebaceous canal and thereby inhibits the formation of microcomedones.8
They also exhibit anti-inflammatory action via inhibition of TLR-2.9 The comedolytic and anti-inflammatory actions of topical retinoids make them a mainstay of acne treatment, although some patients are unable to tolerate their adverse effects, which include erythema and dryness related to increases in transepidermal water loss. Application of noncomedogenic emollients can improve these common effects.10 The newer micronized and time-release retinoid formulations may have less potential for irritation.8 Vehicle formulation and concentration also play a role in skin irritation, with gels and liquids and formulations with higher concentrations of retinoids generally causing more drying than creams and lower potency formulations.8 Table 1 summarizes the mechanisms of action, available formulations, and potential adverse effects of the topical retinoids and other topical agents.1,6,9-16
It is important to note that retinoids can adversely affect the developing fetus when absorbed in large quantities. Notably, tazarotene is assigned to pregnancy category X because when it is used to treat psoriasis, one of its approved indications, large surface areas may be treated, increasing absorption. Absorption amounts are extremely low when tazarotene is used to treat acne. Nevertheless, verification of a negative pregnancy test is recommended prior to initiating tazarotene therapy. Effective birth control measures should be utilized throughout therapy. Even though other commonly used retinoids (tretinoin and adapalene) are assigned to pregnancy category C, all topical retinoids should be avoided during pregnancy.9
As noted, patient education is key for increasing patient adherence to therapy. Patients should be instructed to use a small (pea-sized) amount of medication for the entire face. Providers should also inform patients that transient erythema and dryness can be expected, and that application of a noncomedolytic moisturizer may reduce irritation. Tretinoin is best used at night,1 and it is useful to advise that erythema and irritation associated with retinoid use can be reduced by initially using the medication every other night to every third night, gradually building up to nightly use.1
Topical antibiotic and anti-inflammatory agents
Topical agents used to treat inflammatory lesions include benzoyl peroxide, erythromycin, clindamycin, dapsone, azelaic acid, and sulfacetamide (Table 1).1,6,9-16 These topical agents are generally well tolerated, with most adverse reactions limited to facial irritation and erythema. They come in an array of vehicle formulations, including washes, creams, gels, solutions, foams, and lotions. Vehicle selection should be based upon patient preference and skin type. Gels and solutions have a drying effect, making them more appropriate for individuals with oily skin, whereas creams are moisturizing and appropriate for individuals with dry skin. Lotions are appropriate for all skin types.11
Benzoyl peroxide (BPO) has both keratolytic and comedolytic activity and is available in concentrations ranging from 2.5% to 10%. It is available OTC, as well as by prescription, and is thus readily accessed by the patient. Because BPO is bactericidal for P acnes, resistance to BPO among P acnes has not occurred.1 All concentrations are equally effective, but the higher concentrations are more likely to cause skin dryness and other adverse effects.12 Combination therapy with topical antibiotics, tretinoin, and BPO is more clinically effective than monotherapy.17 Combination products reduce the complexity of acne treatment and likely increase therapy adherence.11 Currently available combination products in various percentages are erythromycin with BPO, clindamycin with BPO, adapalene with BPO, and clindamycin with tretinoin.1
Oral antibiotics
Oral antibiotics should be reserved for use in situations where topical therapy is ineffective. All antibiotics are effective in treating acne due to their antimicrobial activity against P acnes.1 These agents play a key role in managing moderate to severe acne that is likely to scar, as well as in cases of widespread acne involving the face, arms, and trunk. Note that the use of oral antibiotics in acne treatment is controversial, as chronic use contributes to rising rates of bacterial resistance.18 For this reason, antibiotic therapy for acne should be limited to a duration of three months or less, and these agents should not be used as monotherapy.6 In particular, recent recommendations restrict the use of erythromycin for acne treatment due to an increase of P acnes resistance.1 Cephalosporins, macrolides, and penicillin class antibiotics are not routinely recommended due to lack of data regarding their clinical effectiveness in treating acne.1
Tetracycline class antibiotics are the most commonly used oral antibiotics for acne therapy, particularly doxycycline and minocycline.5 Common adverse effects include gastrointestinal upset, photosensitivity, and some pigmentation issues.19 Trimethoprim-sulfamethoxazole (TMP-SMX) is a folate synthesis inhibitor class antibiotic also used to treat acne. Its use should be reserved for individuals who are allergic to tetracyclines or in cases of acne resistant to other antimicrobials.1 Potential adverse reactions include photosensitivity and severe hypersensitivity conditions ranging from a mild rash to toxic epidermal necrolysis.19 Table 2 summarizes the dosage ranges, pregnancy category risk, and potential adverse effects of oral antibiotics used to treat acne.1,19,20
The firstline choice for treating moderate acne with papules and pustules is oral antibiotics with topical retinoids and BPO.5 Patients should be educated about potential adverse effects of these agents, including the development of antibiotic resistance.
Hormonal agents
Hormonal therapies should be reserved for females with acne lesions influenced by fluctuations in hormone levels.21 Pubertal changes initiate the production of adrenal dehydroepiandrosterone, which leads to increased testosterone production. Testosterone is converted to dihydrotestosterone (DHT), which binds to androgen receptors in the sebaceous glands, stimulating the glands and potentially increasing production of sebum. Hormonal agents act by reducing androgen activity in the sebaceous gland. Combined oral hormones, those containing both estrogen and progesterone, reduce the amount of free testosterone and ovarian androgens by suppressing ovulation.1 Hormonal therapy can be quite effective for females of childbearing age. Females who report acne flares with their menstrual cycles may be good candidates for hormonal therapy.1
The estrogen agent most frequently used in oral contraceptives is ethinyl estradiol. Numerous progesterone agents can also be used, but those with low
Spironolactone, a potassium-sparing diuretic, may also be appropriate for treating acne in women due to its antiandrogenic properties. The drug binds androgen receptors in the skin, which then blocks testosterone and DHT. Spironolactone can be an effective firstline agent in treating hormonal-pattern acne, which presents as inflammatory lesions located on the lower face and neck. In particular, it can be an appropriate choice for women with adult-onset acne.15 Spironolactone is not approved by the FDA for acne treatment, but it has been used successfully for many years.5 Spironolactone was found in rodent studies to cause feminization of the male rat fetus, so patients taking this drug should use reliable birth control methods. It can be used concomitantly with oral contraceptives.5 Common side effects include breast tenderness, diuretic effects, headaches, and menstrual irregularities. Although the risk for hypokalemia is low in healthy young women, it may be prudent to periodically assess potassium, sodium, and renal function in patients.1 Spironolactone should be avoided in patients with renal disease and those on other diuretics.15
Isotretinoin
Isotretinoin is an oral systemic retinoid that modulates nuclear receptors and regulates gene transcription in the epidermis.16 Isotretinoin’s mechanisms of action target the main pathogenic factors underlying acne, including reduction of follicular hyperkeratosis, comedogenesis, sebum production, and inflammation and suppression of P acnes.22 These combined actions make isotretinoin a highly effective treatment option for acne.
The drug is approved by the FDA for treatment of nodular acne refractory to traditional acne therapies.23 Isotretinoin is available in 10, 20, 25, 30, and 40 mg capsules, and the recommended dosing is 0.5 to 2.0 mg/kg/d. The usual course of therapy is 15 to 20 weeks or until an accumulative dosage of 120 to 150 mg/kg is attained.23 Patients should be instructed to take isotretinoin with meals, as oral availability is increased with high-fat foods.23
Isotretinoin has major adverse effects. It is a teratogenic medication that can cause congenital anomalies in exposed fetuses, including craniofacial, cardiac, and neurologic issues.16 Due to the seriousness of the congenital anomalies, all prescribers must be registered in the iPledge program, a computer-based risk management program instituted in 2006 by the FDA and the companies that manufacture isotretinoin to eliminate congenital risks associated with isotretinoin. All patients, both male and female, must sign an informed consent form when they register in the program.
Although the iPledge program does not mandate consistent condom use for male patients, they should be informed that minute amounts of isotretinoin can be found in semen. The risk for fathering a fetus with congenital anomalies when taking isotretinoin appears to be extremely low.16 Women of childbearing potential must commit to the use of two highly reliable forms of birth control when taking the medication, including one month before starting therapy and one month after completing therapy.16 Monthly pregnancy testing is mandatory throughout the course of treatment.24 Further information regarding the risk management program can be found at iPledgeprogram.com.
Isotretinoin is metabolized by the liver and may cause lipid abnormalities and hepatic enzyme elevations. Baseline and monthly laboratory monitoring of liver enzymes and cholesterol and triglyceride levels are recommended.24 The process of initiating and monitoring isotretinoin therapy is quite complex, and unless the practitioner plans to routinely prescribe this medication, patients needing isotretinoin therapy should be referred to a dermatology practice.
PATIENT EDUCATION
Patients are more likely to adhere to treatment when simplified regimens are used and when they have realistic expectations for therapy outcomes. Providers need to educate patients that all treatments may require at least two to three months of use before visible results occur. Initial and subsequent visits should include discussions about clear expectations and strategies to reduce potential adverse effects.
PUTTING IT ALL TOGETHER
Acne therapy starts with the use of a topical retinoid in mild acne cases, unless the patient is unable to tolerate the associated skin irritability. Addition of a topical antibiotic or anti-inflammatory agent, preferably BPO, either alone or with a combination product, is also recommended for mild to moderate acne. Patients with moderate to severe acne may benefit from a short course (three months or less) of antibiotics.
Oral hormones may be an excellent therapy choice when acne treatment is needed for women of childbearing age. Isotretinoin is indicated in select cases of severe acne resistant to other treatments.
CE/CME No: CR-1710
PROGRAM OVERVIEW
Earn credit by reading this article and successfully completing the posttest and evaluation. Successful completion is defined as a cumulative score of at least 70% correct.
EDUCATIONAL OBJECTIVES
• Describe the main factors involved in the pathogenesis of acne.
• Assess acne severity and classify acne as mild, moderate, or severe.
• Describe available acne therapies, including their mechanisms of action, indications, and potential adverse effects.
• Identify strategies patients can employ to mitigate the adverse effects of acne treatments.
FACULTY
Janet Purath is an Associate Professor at Washington State University in Spokane, Washington. Theresa Coyner practices at Randall Dermatology, West Lafayette, Indiana.
The authors have no financial relationships to disclose.
ACCREDITATION STATEMENT
This program has been reviewed and is approved for a maximum of 1.0 hour of American Academy of Physician Assistants (AAPA) Category 1 CME credit by the Physician Assistant Review Panel. [NPs: Both ANCC and the AANP Certification Program recognize AAPA as an approved provider of Category 1 credit.] Approval is valid through September 30, 2018.
Article begins on next page >>
Many of the 50 million persons affected by acne in the United States present to primary care. Acne severity guides treatment choices, which include topical antibiotics and retinoids, hormonal agents, and systemic antibiotics and retinoids. Formulating a treatment plan requires a thorough understanding of the dosing, mechanism of action, and potential adverse effects of available medications.
Acne vulgaris (acne) is a common skin condition that is frequently encountered in primary care. Acne affects up to 50 million people in the United States, and about 85% of teenagers experience it at some point.1 Costs for treatment exceed $3 billion per year.2 Although commonly considered a condition of adolescence and young adults (85% prevalence), acne may persist in both men and women well into their 30s and 40s (43% prevalence). In fact, 5% of women ages 40 and older may experience acne.3
Acne is associated with considerable, long-lasting psychological sequelae, even in those with mild conditions, as many affected patients experience self-esteem issues and may avoid social interactions.4 Recognition of patients’ concerns about acne will help to promote a trusting patient-provider relationship. This article describes the pathophysiology and classifications of acne and reviews therapeutic options, enabling the practitioner to initiate treatment.
PRESENTATION AND ASSESSMENT
Acne lesions may occur on the face, neck, trunk, and extremities. The severity of acne is assessed based on lesion type, number, and size, and this grading is used to inform decisions about treatment options. Mild acne is characterized by plugging of the sebaceous gland (comedones), with small numbers of inflammatory papules and pustules. Moderate acne involves a larger number of inflammatory papules/pustules as well as the presence of small cystic nodules. Severe acne is marked by the presence of large numbers of noninflammatory and inflammatory lesions and cystic nodules or widespread involvement of these lesions.5 Examples of mild, moderate, and severe acne are shown in Figure 1. Assessment should include questions about the patient’s experiences with prior therapies.

PATHOGENESIS
The pathogenesis of acne is a complex process involving multiple factors (see Figure 2). Knowledge about acne pathogenesis continues to evolve, but the current view is that a combination of simultaneous noninflammatory and inflammatory events involving pilosebaceous units (which consist of sebaceous glands and hair follicles) contribute to its development.6 Activation of the sebaceous glands is influenced by androgens, which increase sebum production and shedding of the keratinocytes lining the gland. Plugging of the pilosebaceous canal ensues, leading to the development of a microcomedone. Increased proliferation of Propionibacterium acnes occurs within the obstructed gland. The inflammatory response to this process includes a cascade of numerous cytokines, most notably toll-like receptor 2 (TLR-2).7 The plug at the opening of the sebaceous gland creates either an open comedone (blackhead) or a closed comedone (whitehead). Eventually, the follicular wall ruptures, leading to the formation of erythematous papules and pustules on the skin surface or deep-seated cystic structures under the skin surface. Current pharmacologic agents target one or more of these identified factors underlying acne pathogenesis.
THERAPEUTIC OPTIONS
Pharmacologic treatment options for acne include topical, systemic, and hormonal agents. Topical and systemic therapies reduce inflammation and follicular plugging. Topical treatments include antibiotics, anti-inflammatories, and retinoids. Oral treatments include antibiotics, hormones, and retinoids. The clinician must have a thorough understanding of the actions, potential adverse reactions, and drug interactions of each proposed therapy prior to formulating a treatment plan.
Topical retinoids
Topical retinoids are the most effective comedolytic agents available.1 Since comedones are thought to be the precursor of all other acne lesions, retinoids are appropriate for cases in which comedones are seen.1 Retinoids belong to a class of compounds structurally related to vitamin A. Topical retinoids act by promoting normal follicular keratinocyte desquamation, which prevents obstruction of the pilosebaceous canal and thereby inhibits the formation of microcomedones.8
They also exhibit anti-inflammatory action via inhibition of TLR-2.9 The comedolytic and anti-inflammatory actions of topical retinoids make them a mainstay of acne treatment, although some patients are unable to tolerate their adverse effects, which include erythema and dryness related to increases in transepidermal water loss. Application of noncomedogenic emollients can improve these common effects.10 The newer micronized and time-release retinoid formulations may have less potential for irritation.8 Vehicle formulation and concentration also play a role in skin irritation, with gels and liquids and formulations with higher concentrations of retinoids generally causing more drying than creams and lower potency formulations.8 Table 1 summarizes the mechanisms of action, available formulations, and potential adverse effects of the topical retinoids and other topical agents.1,6,9-16
It is important to note that retinoids can adversely affect the developing fetus when absorbed in large quantities. Notably, tazarotene is assigned to pregnancy category X because when it is used to treat psoriasis, one of its approved indications, large surface areas may be treated, increasing absorption. Absorption amounts are extremely low when tazarotene is used to treat acne. Nevertheless, verification of a negative pregnancy test is recommended prior to initiating tazarotene therapy. Effective birth control measures should be utilized throughout therapy. Even though other commonly used retinoids (tretinoin and adapalene) are assigned to pregnancy category C, all topical retinoids should be avoided during pregnancy.9
As noted, patient education is key for increasing patient adherence to therapy. Patients should be instructed to use a small (pea-sized) amount of medication for the entire face. Providers should also inform patients that transient erythema and dryness can be expected, and that application of a noncomedolytic moisturizer may reduce irritation. Tretinoin is best used at night,1 and it is useful to advise that erythema and irritation associated with retinoid use can be reduced by initially using the medication every other night to every third night, gradually building up to nightly use.1
Topical antibiotic and anti-inflammatory agents
Topical agents used to treat inflammatory lesions include benzoyl peroxide, erythromycin, clindamycin, dapsone, azelaic acid, and sulfacetamide (Table 1).1,6,9-16 These topical agents are generally well tolerated, with most adverse reactions limited to facial irritation and erythema. They come in an array of vehicle formulations, including washes, creams, gels, solutions, foams, and lotions. Vehicle selection should be based upon patient preference and skin type. Gels and solutions have a drying effect, making them more appropriate for individuals with oily skin, whereas creams are moisturizing and appropriate for individuals with dry skin. Lotions are appropriate for all skin types.11
Benzoyl peroxide (BPO) has both keratolytic and comedolytic activity and is available in concentrations ranging from 2.5% to 10%. It is available OTC, as well as by prescription, and is thus readily accessed by the patient. Because BPO is bactericidal for P acnes, resistance to BPO among P acnes has not occurred.1 All concentrations are equally effective, but the higher concentrations are more likely to cause skin dryness and other adverse effects.12 Combination therapy with topical antibiotics, tretinoin, and BPO is more clinically effective than monotherapy.17 Combination products reduce the complexity of acne treatment and likely increase therapy adherence.11 Currently available combination products in various percentages are erythromycin with BPO, clindamycin with BPO, adapalene with BPO, and clindamycin with tretinoin.1
Oral antibiotics
Oral antibiotics should be reserved for use in situations where topical therapy is ineffective. All antibiotics are effective in treating acne due to their antimicrobial activity against P acnes.1 These agents play a key role in managing moderate to severe acne that is likely to scar, as well as in cases of widespread acne involving the face, arms, and trunk. Note that the use of oral antibiotics in acne treatment is controversial, as chronic use contributes to rising rates of bacterial resistance.18 For this reason, antibiotic therapy for acne should be limited to a duration of three months or less, and these agents should not be used as monotherapy.6 In particular, recent recommendations restrict the use of erythromycin for acne treatment due to an increase of P acnes resistance.1 Cephalosporins, macrolides, and penicillin class antibiotics are not routinely recommended due to lack of data regarding their clinical effectiveness in treating acne.1
Tetracycline class antibiotics are the most commonly used oral antibiotics for acne therapy, particularly doxycycline and minocycline.5 Common adverse effects include gastrointestinal upset, photosensitivity, and some pigmentation issues.19 Trimethoprim-sulfamethoxazole (TMP-SMX) is a folate synthesis inhibitor class antibiotic also used to treat acne. Its use should be reserved for individuals who are allergic to tetracyclines or in cases of acne resistant to other antimicrobials.1 Potential adverse reactions include photosensitivity and severe hypersensitivity conditions ranging from a mild rash to toxic epidermal necrolysis.19 Table 2 summarizes the dosage ranges, pregnancy category risk, and potential adverse effects of oral antibiotics used to treat acne.1,19,20
The firstline choice for treating moderate acne with papules and pustules is oral antibiotics with topical retinoids and BPO.5 Patients should be educated about potential adverse effects of these agents, including the development of antibiotic resistance.
Hormonal agents
Hormonal therapies should be reserved for females with acne lesions influenced by fluctuations in hormone levels.21 Pubertal changes initiate the production of adrenal dehydroepiandrosterone, which leads to increased testosterone production. Testosterone is converted to dihydrotestosterone (DHT), which binds to androgen receptors in the sebaceous glands, stimulating the glands and potentially increasing production of sebum. Hormonal agents act by reducing androgen activity in the sebaceous gland. Combined oral hormones, those containing both estrogen and progesterone, reduce the amount of free testosterone and ovarian androgens by suppressing ovulation.1 Hormonal therapy can be quite effective for females of childbearing age. Females who report acne flares with their menstrual cycles may be good candidates for hormonal therapy.1
The estrogen agent most frequently used in oral contraceptives is ethinyl estradiol. Numerous progesterone agents can also be used, but those with low
Spironolactone, a potassium-sparing diuretic, may also be appropriate for treating acne in women due to its antiandrogenic properties. The drug binds androgen receptors in the skin, which then blocks testosterone and DHT. Spironolactone can be an effective firstline agent in treating hormonal-pattern acne, which presents as inflammatory lesions located on the lower face and neck. In particular, it can be an appropriate choice for women with adult-onset acne.15 Spironolactone is not approved by the FDA for acne treatment, but it has been used successfully for many years.5 Spironolactone was found in rodent studies to cause feminization of the male rat fetus, so patients taking this drug should use reliable birth control methods. It can be used concomitantly with oral contraceptives.5 Common side effects include breast tenderness, diuretic effects, headaches, and menstrual irregularities. Although the risk for hypokalemia is low in healthy young women, it may be prudent to periodically assess potassium, sodium, and renal function in patients.1 Spironolactone should be avoided in patients with renal disease and those on other diuretics.15
Isotretinoin
Isotretinoin is an oral systemic retinoid that modulates nuclear receptors and regulates gene transcription in the epidermis.16 Isotretinoin’s mechanisms of action target the main pathogenic factors underlying acne, including reduction of follicular hyperkeratosis, comedogenesis, sebum production, and inflammation and suppression of P acnes.22 These combined actions make isotretinoin a highly effective treatment option for acne.
The drug is approved by the FDA for treatment of nodular acne refractory to traditional acne therapies.23 Isotretinoin is available in 10, 20, 25, 30, and 40 mg capsules, and the recommended dosing is 0.5 to 2.0 mg/kg/d. The usual course of therapy is 15 to 20 weeks or until an accumulative dosage of 120 to 150 mg/kg is attained.23 Patients should be instructed to take isotretinoin with meals, as oral availability is increased with high-fat foods.23
Isotretinoin has major adverse effects. It is a teratogenic medication that can cause congenital anomalies in exposed fetuses, including craniofacial, cardiac, and neurologic issues.16 Due to the seriousness of the congenital anomalies, all prescribers must be registered in the iPledge program, a computer-based risk management program instituted in 2006 by the FDA and the companies that manufacture isotretinoin to eliminate congenital risks associated with isotretinoin. All patients, both male and female, must sign an informed consent form when they register in the program.
Although the iPledge program does not mandate consistent condom use for male patients, they should be informed that minute amounts of isotretinoin can be found in semen. The risk for fathering a fetus with congenital anomalies when taking isotretinoin appears to be extremely low.16 Women of childbearing potential must commit to the use of two highly reliable forms of birth control when taking the medication, including one month before starting therapy and one month after completing therapy.16 Monthly pregnancy testing is mandatory throughout the course of treatment.24 Further information regarding the risk management program can be found at iPledgeprogram.com.
Isotretinoin is metabolized by the liver and may cause lipid abnormalities and hepatic enzyme elevations. Baseline and monthly laboratory monitoring of liver enzymes and cholesterol and triglyceride levels are recommended.24 The process of initiating and monitoring isotretinoin therapy is quite complex, and unless the practitioner plans to routinely prescribe this medication, patients needing isotretinoin therapy should be referred to a dermatology practice.
PATIENT EDUCATION
Patients are more likely to adhere to treatment when simplified regimens are used and when they have realistic expectations for therapy outcomes. Providers need to educate patients that all treatments may require at least two to three months of use before visible results occur. Initial and subsequent visits should include discussions about clear expectations and strategies to reduce potential adverse effects.
PUTTING IT ALL TOGETHER
Acne therapy starts with the use of a topical retinoid in mild acne cases, unless the patient is unable to tolerate the associated skin irritability. Addition of a topical antibiotic or anti-inflammatory agent, preferably BPO, either alone or with a combination product, is also recommended for mild to moderate acne. Patients with moderate to severe acne may benefit from a short course (three months or less) of antibiotics.
Oral hormones may be an excellent therapy choice when acne treatment is needed for women of childbearing age. Isotretinoin is indicated in select cases of severe acne resistant to other treatments.
1. Zaenglein AL, Pathy AL, Schlosser BJ, et al. Guidelines of care for the management of acne vulgaris. J Am Acad Dermatol. 2016;74(5):945-973.
2. Bhate K, Williams HC. Epidemiology of acne vulgaris. Br J Dermatol. 2013;168(3):474-485.
3. Collier CN, Harper JC, Cafardi JA, et al. The prevalence of acne in adults 20 years and older. J Am Acad Dertmatol. 2008;58(1):56-59.
4. Dunn LK, O’Neill JL, Feldman SR. Acne in adolescents: quality of life, self-esteem, mood, and psychological disorders. Dermatol Online J. 2011;17(1):1.
5. Baldwin HE, Zanglein AL, Leyden JJ, Webster GF. Pharmacologic treatment options in mild, moderate, and severe acne vulgaris. Semin Cutan Med Surg. 2015;34(supp5):S82-S85.
6. Canavan TN, Chen E, Elewski BE. Optimizing non-antibiotic treatments for patients with acne: a review. Dermatol Ther. 2016;6(4):555-578.
7. Bellew S, Thiboutot D, Del Rosso JQ. Pathogenesis of acne vulgaris: what’s new, what’s interesting and what may be clinically relevant. J Drugs Dermatol. 2011;10(6):582-585.
8. Russell JJ. Topical therapy for acne. Am Fam Phys. 2000; 61(2):357-365.
9. Sami N. Topical retinoids. In: Wolverton SE, ed. Comprehensive Dermatologic Drug Therapy. 3rd ed. St. Louis: Elsevier; 2013:505-517.
10. Smith RI. Treatments: Retinoids. In: Mancini AJ, Eichenfield LF, Del Rosso JQ, eds. Acne in Review Guide. New York: Educational Testing and Assessment Systems/SanovaWorks; 2013:59-63.
11. Sagransky M, Yentzer BA, Feldman SR. Benzoyl peroxide: a review of its current use in the treatment of acne vulgaris. Expert Opin Pharmacother. 2009;10(15):2555-2562.
12. Motoparthi K, Hsu S. Topical antibacterial agents. In: Wolverton SE, ed. Comprehensive Dermatologic Drug Therapy. 3rd ed. St Louis: Elsevier; 2013:452-459.
13. Thiboutot DM, Kircik L, McMichale A, et al. Efficacy, safety, and dermal tolerability of dapsone gel, 7.5% in patients with moderate acne vulgaris: a pooled analysis of two phase 3 trials. J Clin Aesthet Dermatol. 2016;9(10):18-27.
14. Wolf K, Silapunt S. The use of sodium sulfacetamide in dermatology. Cutis. 2015;96(2):128-130.
15. Hassoun LA, Chahal DS, Sivamani RK, Larsen LN. The use of hormonal agents in the treatment of acne. Semin Cutan Med Surg. 2016;35(2):68-73.
16. Patton TJ, Ferris LK. Systemic retinoids. In: Wolverton SE, ed. Comprehensive Dermatologic Drug Therapy. 3rd ed. St Louis: Elsevier; 2012:252-268.
17. Thiboutot D, Gollnick H, Bettoli V, et al. New insights into the management of acne: an update from the Global Alliance to Improve Outcomes in Acne group. J Am Acad Dermatol. 2009;60(5 Suppl):S1-S50.
18. Walsh TR, Efthimious J, Dreno B. Systematic review of antibiotic resistance in acne: an increasing topical and oral threat. Lancet Infect Dis. 2016;16(3):e22-32.
19. Yan AC, Del Rosso JQ. Prescription oral treatments: Antibiotics. In: Mancini AJ, Eichenfield LF, Del Rosso JQ, eds. Acne in Review Guide. New York: Educational Testing and Assessment Systems/SanovaWorks; 2013:77-87.
20. Kim S, Michaels BD, Kim GK, Del Rosso JQ. Systemic antibacterial agents. In: Wolverton SE, ed. Comprehensive Dermatologic Drug Therapy. 3rd ed. St Louis: Elsevier; 2013:62-67, 70-74, 77-85.
21. Hecht CT, Sidbury R, Del Rosso JQ. Prescription oral treatments: Hormonal therapies. In: Mancini AJ, Eichenfield LF, Del Rosso JQ, eds. Acne in Review Guide. New York: Educational Testing and Assessment Systems/SanovaWorks; 2013:89-95.
22. Webster GF, Leyden JJ, Baldwin HE, Zaenglein AL. Isotretinoin: mechanism of action and patient selection. Semin Cutan Med Surg. 2015;34(supp 5):S86-S88.
23. Leyden JJ, Del Rosso JQ, Baum EW. The use of isotretinoin in the treatment of acne vulgaris. J Clin and Aesthet Dermatol. 2014;7(2 Suppl):S3-S21.
24. Zane LT, Leyden WA, Marqueling AL, Manos MM. A population-based analysis of laboratory abnormalities during isotretinoin therapy for acne vulgaris. Arch Dermatol. 2006;142(8):1016-1022.
1. Zaenglein AL, Pathy AL, Schlosser BJ, et al. Guidelines of care for the management of acne vulgaris. J Am Acad Dermatol. 2016;74(5):945-973.
2. Bhate K, Williams HC. Epidemiology of acne vulgaris. Br J Dermatol. 2013;168(3):474-485.
3. Collier CN, Harper JC, Cafardi JA, et al. The prevalence of acne in adults 20 years and older. J Am Acad Dertmatol. 2008;58(1):56-59.
4. Dunn LK, O’Neill JL, Feldman SR. Acne in adolescents: quality of life, self-esteem, mood, and psychological disorders. Dermatol Online J. 2011;17(1):1.
5. Baldwin HE, Zanglein AL, Leyden JJ, Webster GF. Pharmacologic treatment options in mild, moderate, and severe acne vulgaris. Semin Cutan Med Surg. 2015;34(supp5):S82-S85.
6. Canavan TN, Chen E, Elewski BE. Optimizing non-antibiotic treatments for patients with acne: a review. Dermatol Ther. 2016;6(4):555-578.
7. Bellew S, Thiboutot D, Del Rosso JQ. Pathogenesis of acne vulgaris: what’s new, what’s interesting and what may be clinically relevant. J Drugs Dermatol. 2011;10(6):582-585.
8. Russell JJ. Topical therapy for acne. Am Fam Phys. 2000; 61(2):357-365.
9. Sami N. Topical retinoids. In: Wolverton SE, ed. Comprehensive Dermatologic Drug Therapy. 3rd ed. St. Louis: Elsevier; 2013:505-517.
10. Smith RI. Treatments: Retinoids. In: Mancini AJ, Eichenfield LF, Del Rosso JQ, eds. Acne in Review Guide. New York: Educational Testing and Assessment Systems/SanovaWorks; 2013:59-63.
11. Sagransky M, Yentzer BA, Feldman SR. Benzoyl peroxide: a review of its current use in the treatment of acne vulgaris. Expert Opin Pharmacother. 2009;10(15):2555-2562.
12. Motoparthi K, Hsu S. Topical antibacterial agents. In: Wolverton SE, ed. Comprehensive Dermatologic Drug Therapy. 3rd ed. St Louis: Elsevier; 2013:452-459.
13. Thiboutot DM, Kircik L, McMichale A, et al. Efficacy, safety, and dermal tolerability of dapsone gel, 7.5% in patients with moderate acne vulgaris: a pooled analysis of two phase 3 trials. J Clin Aesthet Dermatol. 2016;9(10):18-27.
14. Wolf K, Silapunt S. The use of sodium sulfacetamide in dermatology. Cutis. 2015;96(2):128-130.
15. Hassoun LA, Chahal DS, Sivamani RK, Larsen LN. The use of hormonal agents in the treatment of acne. Semin Cutan Med Surg. 2016;35(2):68-73.
16. Patton TJ, Ferris LK. Systemic retinoids. In: Wolverton SE, ed. Comprehensive Dermatologic Drug Therapy. 3rd ed. St Louis: Elsevier; 2012:252-268.
17. Thiboutot D, Gollnick H, Bettoli V, et al. New insights into the management of acne: an update from the Global Alliance to Improve Outcomes in Acne group. J Am Acad Dermatol. 2009;60(5 Suppl):S1-S50.
18. Walsh TR, Efthimious J, Dreno B. Systematic review of antibiotic resistance in acne: an increasing topical and oral threat. Lancet Infect Dis. 2016;16(3):e22-32.
19. Yan AC, Del Rosso JQ. Prescription oral treatments: Antibiotics. In: Mancini AJ, Eichenfield LF, Del Rosso JQ, eds. Acne in Review Guide. New York: Educational Testing and Assessment Systems/SanovaWorks; 2013:77-87.
20. Kim S, Michaels BD, Kim GK, Del Rosso JQ. Systemic antibacterial agents. In: Wolverton SE, ed. Comprehensive Dermatologic Drug Therapy. 3rd ed. St Louis: Elsevier; 2013:62-67, 70-74, 77-85.
21. Hecht CT, Sidbury R, Del Rosso JQ. Prescription oral treatments: Hormonal therapies. In: Mancini AJ, Eichenfield LF, Del Rosso JQ, eds. Acne in Review Guide. New York: Educational Testing and Assessment Systems/SanovaWorks; 2013:89-95.
22. Webster GF, Leyden JJ, Baldwin HE, Zaenglein AL. Isotretinoin: mechanism of action and patient selection. Semin Cutan Med Surg. 2015;34(supp 5):S86-S88.
23. Leyden JJ, Del Rosso JQ, Baum EW. The use of isotretinoin in the treatment of acne vulgaris. J Clin and Aesthet Dermatol. 2014;7(2 Suppl):S3-S21.
24. Zane LT, Leyden WA, Marqueling AL, Manos MM. A population-based analysis of laboratory abnormalities during isotretinoin therapy for acne vulgaris. Arch Dermatol. 2006;142(8):1016-1022.

