User login
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
A 46-YEAR-OLD MAN came into our family medicine clinic because he wanted a few “lumps” removed from his left medial elbow and the back of his right thigh and knee. He indicated that he’d had the painless lesions for a long time, but that recently they’d started bothering him because they were getting caught on his clothes.
Other than these lesions, his past medical, social, and surgical histories were unremarkable. He indicated that his mother and 3 of his 5 siblings had similar lesions.
On physical exam, the patient had multiple nontender, soft, pedunculated, and relatively mobile nodules in different sizes (FIGURE 1A). There were also a few well-circumscribed and light brown patches on his left medial elbow (FIGURE 1B), the back of his right thigh, and his upper back.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Neurofibromatosis type 1
Neurofibromatosis type 1 (NF1) is an autosomal dominant multisystem disorder affecting about one in 3000 people.1-3 The NF1 gene is on chromosome 17q11.2, which encodes for neurofibromin protein.2,3 About half of these patients demonstrate a spontaneous mutation.1-5 Clinical features include cutaneous, subcutaneous, skeletal, peripheral, and central nervous systems abnormalities.
3 common features
Neurofibroma is the hallmark of NF1. Cutaneous and subcutaneous neurofibromas are benign peripheral nerve sheath tumors consisting of Schwann cells, fibroblasts, peripheral cells, mast cells, axons, and blood vessels.1-5 Neurofibromas usually develop when patients are in their late teens; they are often painless.
Café-au-lait spots are well-circumscribed, evenly pigmented, light to dark brown macules and/or patches with an average size of 2 to 5 cm (FIGURE 1B). Up to 10% of the general population may have one or 2 café-au-lait spots with no other abnormalities.6 Patients with NF1 will have 6 or more.1
Skin fold freckling is the most specific feature in patients with NF1. This freckling usually occurs in the axilla and groin regions when patients are between 3 and 5 years of age. The freckles are typically small, with an average size of 1 to 3 mm.
Other less common clinical features of NF1 include plexiform neurofibroma, skeletal abnormalities (short stature, scoliosis, long bone dysplasia, and osteopenia/ osteoporosis), Lisch nodules (iris hamartomas), neurocognitive deficits, cardiovascular abnormalities, and optic pathway gliomas.1-5
FIGURE 1
Widespread cutaneous nodules with hyperpigmented patches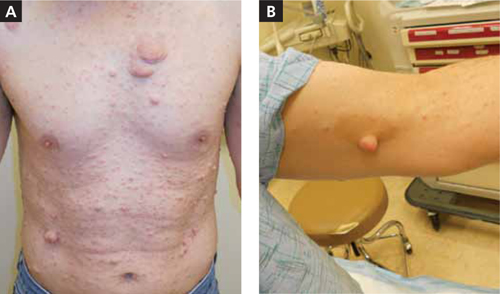
Is it neurofibromatosis type 1, or one of these 4 conditions?
Consider these conditions in the differential diagnosis of a patient who presents with soft, pedunculated nodules:
- Segmental/mosaic NF1 occurs as a result of NF1 somatic gene mutation. Clinical manifestations (pigmentary changes, tumor growths, or both) are limited to one or more body segments.3 The extent of the body parts affected depends on the time of the mutation in embryonic development.
- Neurofibromatosis 2 (NF2) is an autosomal dominant disease affecting one in 25,000 individuals.2 The characteristic feature is bilateral vestibular schwannomas.4,5 Other clinical features include meningiomas, schwannomas, gliomas, neurofibromas, and posterior subcapsular lens opacity. Café-au-lait spots are less common in NF2 than in NF1; only about one-third of NF2 patients have them.6
- Schwannomatosis is a disease with multiple subcutaneous, peripheral nerve, and spinal schwannomas.4,5 Patients do not have the vestibular schwannomas or the ophthalmologic features of NF2.
- Lipomatosis is an autosomal dominant disease featuring multiple lipomas on the trunk, proximal thighs, and distal arms. Depending on the location, the lipomas can be tender to touch. Biopsy may be necessary to differentiate lipomas from neurofibromas and schwannomas.
Diagnosis hinges on 2 of these 7 criteria
For adult patients, the diagnosis is clinical and straightforward. At least 2 of the following criteria should be present for the diagnosis:1-6
- 6 or more café-au-lait spots
- axillary or inguinal freckling
- 2 or more neurofibromas
- a first-degree relative with NF1
- 2 or more Lisch nodules
- a distinctive osseous lesion
- optic pathway glioma.
The diagnosis in youngsters, especially those younger than 8 years, can be difficult and may require genetic testing. Genetic testing is also recommended for individuals with a single sign, or with variant disorders.3 Genetic counseling and testing are also recommended in preimplantation and prenatal situations.3 Biopsy of the cutaneous and subcutaneous lesions for diagnostic purposes is not usually recommended.1-5
Management is challenging as there is no definitive treatment
The effect of NF1 on patients’ lives is significant. Management usually requires a multidisciplinary approach led by a primary care physician.3 To date, there is no definitive treatment for NF1.
Removal of symptomatic cutaneous and subcutaneous lesions is recommended; however, the recurrence rate is high1-3 (strength of recommendation [SOR]: B). About 10% of patients with NF1 will develop a malignant nerve sheath tumor, which usually arises from preexisting plexiform neurofibromas.1-4 Surgical excision with clear margins is the goal of treatment.2
A good outcome for my patient
The nodules on the patient’s medial elbow and the back of his thigh and knee were excised. The pathology confirmed the diagnosis. There was no malignant transformation.
CORRESPONDENCE Morteza Khodaee, MD, MPH, AFW Family Medicine Clinic, 3055 Roslyn Street, Denver, CO 80238; morteza.khodaee@ucdenver.edu
1. Williams VC, Lucas J, Babcock MA, et al. Neurofibromatosis type 1 revisited. Pediatrics. 2009;123:124-133.
2. Ferner RE. The neurofibromatoses. Pract Neurol. 2010;10:82-93.
3. Boyd KP, Korf BR, Theos A. Neurofibromatosis type 1. J Am Acad Dermatol. 2009;61:1-14.
4. Ferner RE, Huson SM, Thomas N, et al. Guidelines for the diagnosis and management of individuals with neurofibromatosis 1. J Med Genet. 2007;44:81-88.
5. Gerber PA, Antal AS, Neumann NJ, et al. Neurofibromatosis. Eur J Med Res. 2009;14:102-105.
6. Shah KN. The diagnostic and clinical significance of café-au-lait macules. Pediatr Clin North Am. 2010;57:1131-1153.
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
A 46-YEAR-OLD MAN came into our family medicine clinic because he wanted a few “lumps” removed from his left medial elbow and the back of his right thigh and knee. He indicated that he’d had the painless lesions for a long time, but that recently they’d started bothering him because they were getting caught on his clothes.
Other than these lesions, his past medical, social, and surgical histories were unremarkable. He indicated that his mother and 3 of his 5 siblings had similar lesions.
On physical exam, the patient had multiple nontender, soft, pedunculated, and relatively mobile nodules in different sizes (FIGURE 1A). There were also a few well-circumscribed and light brown patches on his left medial elbow (FIGURE 1B), the back of his right thigh, and his upper back.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Neurofibromatosis type 1
Neurofibromatosis type 1 (NF1) is an autosomal dominant multisystem disorder affecting about one in 3000 people.1-3 The NF1 gene is on chromosome 17q11.2, which encodes for neurofibromin protein.2,3 About half of these patients demonstrate a spontaneous mutation.1-5 Clinical features include cutaneous, subcutaneous, skeletal, peripheral, and central nervous systems abnormalities.
3 common features
Neurofibroma is the hallmark of NF1. Cutaneous and subcutaneous neurofibromas are benign peripheral nerve sheath tumors consisting of Schwann cells, fibroblasts, peripheral cells, mast cells, axons, and blood vessels.1-5 Neurofibromas usually develop when patients are in their late teens; they are often painless.
Café-au-lait spots are well-circumscribed, evenly pigmented, light to dark brown macules and/or patches with an average size of 2 to 5 cm (FIGURE 1B). Up to 10% of the general population may have one or 2 café-au-lait spots with no other abnormalities.6 Patients with NF1 will have 6 or more.1
Skin fold freckling is the most specific feature in patients with NF1. This freckling usually occurs in the axilla and groin regions when patients are between 3 and 5 years of age. The freckles are typically small, with an average size of 1 to 3 mm.
Other less common clinical features of NF1 include plexiform neurofibroma, skeletal abnormalities (short stature, scoliosis, long bone dysplasia, and osteopenia/ osteoporosis), Lisch nodules (iris hamartomas), neurocognitive deficits, cardiovascular abnormalities, and optic pathway gliomas.1-5
FIGURE 1
Widespread cutaneous nodules with hyperpigmented patches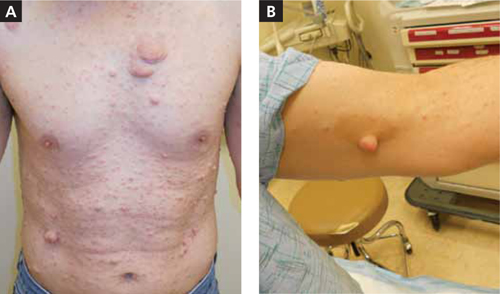
Is it neurofibromatosis type 1, or one of these 4 conditions?
Consider these conditions in the differential diagnosis of a patient who presents with soft, pedunculated nodules:
- Segmental/mosaic NF1 occurs as a result of NF1 somatic gene mutation. Clinical manifestations (pigmentary changes, tumor growths, or both) are limited to one or more body segments.3 The extent of the body parts affected depends on the time of the mutation in embryonic development.
- Neurofibromatosis 2 (NF2) is an autosomal dominant disease affecting one in 25,000 individuals.2 The characteristic feature is bilateral vestibular schwannomas.4,5 Other clinical features include meningiomas, schwannomas, gliomas, neurofibromas, and posterior subcapsular lens opacity. Café-au-lait spots are less common in NF2 than in NF1; only about one-third of NF2 patients have them.6
- Schwannomatosis is a disease with multiple subcutaneous, peripheral nerve, and spinal schwannomas.4,5 Patients do not have the vestibular schwannomas or the ophthalmologic features of NF2.
- Lipomatosis is an autosomal dominant disease featuring multiple lipomas on the trunk, proximal thighs, and distal arms. Depending on the location, the lipomas can be tender to touch. Biopsy may be necessary to differentiate lipomas from neurofibromas and schwannomas.
Diagnosis hinges on 2 of these 7 criteria
For adult patients, the diagnosis is clinical and straightforward. At least 2 of the following criteria should be present for the diagnosis:1-6
- 6 or more café-au-lait spots
- axillary or inguinal freckling
- 2 or more neurofibromas
- a first-degree relative with NF1
- 2 or more Lisch nodules
- a distinctive osseous lesion
- optic pathway glioma.
The diagnosis in youngsters, especially those younger than 8 years, can be difficult and may require genetic testing. Genetic testing is also recommended for individuals with a single sign, or with variant disorders.3 Genetic counseling and testing are also recommended in preimplantation and prenatal situations.3 Biopsy of the cutaneous and subcutaneous lesions for diagnostic purposes is not usually recommended.1-5
Management is challenging as there is no definitive treatment
The effect of NF1 on patients’ lives is significant. Management usually requires a multidisciplinary approach led by a primary care physician.3 To date, there is no definitive treatment for NF1.
Removal of symptomatic cutaneous and subcutaneous lesions is recommended; however, the recurrence rate is high1-3 (strength of recommendation [SOR]: B). About 10% of patients with NF1 will develop a malignant nerve sheath tumor, which usually arises from preexisting plexiform neurofibromas.1-4 Surgical excision with clear margins is the goal of treatment.2
A good outcome for my patient
The nodules on the patient’s medial elbow and the back of his thigh and knee were excised. The pathology confirmed the diagnosis. There was no malignant transformation.
CORRESPONDENCE Morteza Khodaee, MD, MPH, AFW Family Medicine Clinic, 3055 Roslyn Street, Denver, CO 80238; morteza.khodaee@ucdenver.edu
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
A 46-YEAR-OLD MAN came into our family medicine clinic because he wanted a few “lumps” removed from his left medial elbow and the back of his right thigh and knee. He indicated that he’d had the painless lesions for a long time, but that recently they’d started bothering him because they were getting caught on his clothes.
Other than these lesions, his past medical, social, and surgical histories were unremarkable. He indicated that his mother and 3 of his 5 siblings had similar lesions.
On physical exam, the patient had multiple nontender, soft, pedunculated, and relatively mobile nodules in different sizes (FIGURE 1A). There were also a few well-circumscribed and light brown patches on his left medial elbow (FIGURE 1B), the back of his right thigh, and his upper back.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Neurofibromatosis type 1
Neurofibromatosis type 1 (NF1) is an autosomal dominant multisystem disorder affecting about one in 3000 people.1-3 The NF1 gene is on chromosome 17q11.2, which encodes for neurofibromin protein.2,3 About half of these patients demonstrate a spontaneous mutation.1-5 Clinical features include cutaneous, subcutaneous, skeletal, peripheral, and central nervous systems abnormalities.
3 common features
Neurofibroma is the hallmark of NF1. Cutaneous and subcutaneous neurofibromas are benign peripheral nerve sheath tumors consisting of Schwann cells, fibroblasts, peripheral cells, mast cells, axons, and blood vessels.1-5 Neurofibromas usually develop when patients are in their late teens; they are often painless.
Café-au-lait spots are well-circumscribed, evenly pigmented, light to dark brown macules and/or patches with an average size of 2 to 5 cm (FIGURE 1B). Up to 10% of the general population may have one or 2 café-au-lait spots with no other abnormalities.6 Patients with NF1 will have 6 or more.1
Skin fold freckling is the most specific feature in patients with NF1. This freckling usually occurs in the axilla and groin regions when patients are between 3 and 5 years of age. The freckles are typically small, with an average size of 1 to 3 mm.
Other less common clinical features of NF1 include plexiform neurofibroma, skeletal abnormalities (short stature, scoliosis, long bone dysplasia, and osteopenia/ osteoporosis), Lisch nodules (iris hamartomas), neurocognitive deficits, cardiovascular abnormalities, and optic pathway gliomas.1-5
FIGURE 1
Widespread cutaneous nodules with hyperpigmented patches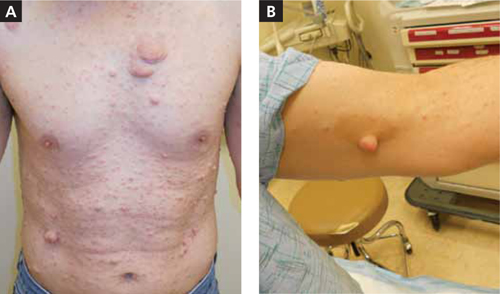
Is it neurofibromatosis type 1, or one of these 4 conditions?
Consider these conditions in the differential diagnosis of a patient who presents with soft, pedunculated nodules:
- Segmental/mosaic NF1 occurs as a result of NF1 somatic gene mutation. Clinical manifestations (pigmentary changes, tumor growths, or both) are limited to one or more body segments.3 The extent of the body parts affected depends on the time of the mutation in embryonic development.
- Neurofibromatosis 2 (NF2) is an autosomal dominant disease affecting one in 25,000 individuals.2 The characteristic feature is bilateral vestibular schwannomas.4,5 Other clinical features include meningiomas, schwannomas, gliomas, neurofibromas, and posterior subcapsular lens opacity. Café-au-lait spots are less common in NF2 than in NF1; only about one-third of NF2 patients have them.6
- Schwannomatosis is a disease with multiple subcutaneous, peripheral nerve, and spinal schwannomas.4,5 Patients do not have the vestibular schwannomas or the ophthalmologic features of NF2.
- Lipomatosis is an autosomal dominant disease featuring multiple lipomas on the trunk, proximal thighs, and distal arms. Depending on the location, the lipomas can be tender to touch. Biopsy may be necessary to differentiate lipomas from neurofibromas and schwannomas.
Diagnosis hinges on 2 of these 7 criteria
For adult patients, the diagnosis is clinical and straightforward. At least 2 of the following criteria should be present for the diagnosis:1-6
- 6 or more café-au-lait spots
- axillary or inguinal freckling
- 2 or more neurofibromas
- a first-degree relative with NF1
- 2 or more Lisch nodules
- a distinctive osseous lesion
- optic pathway glioma.
The diagnosis in youngsters, especially those younger than 8 years, can be difficult and may require genetic testing. Genetic testing is also recommended for individuals with a single sign, or with variant disorders.3 Genetic counseling and testing are also recommended in preimplantation and prenatal situations.3 Biopsy of the cutaneous and subcutaneous lesions for diagnostic purposes is not usually recommended.1-5
Management is challenging as there is no definitive treatment
The effect of NF1 on patients’ lives is significant. Management usually requires a multidisciplinary approach led by a primary care physician.3 To date, there is no definitive treatment for NF1.
Removal of symptomatic cutaneous and subcutaneous lesions is recommended; however, the recurrence rate is high1-3 (strength of recommendation [SOR]: B). About 10% of patients with NF1 will develop a malignant nerve sheath tumor, which usually arises from preexisting plexiform neurofibromas.1-4 Surgical excision with clear margins is the goal of treatment.2
A good outcome for my patient
The nodules on the patient’s medial elbow and the back of his thigh and knee were excised. The pathology confirmed the diagnosis. There was no malignant transformation.
CORRESPONDENCE Morteza Khodaee, MD, MPH, AFW Family Medicine Clinic, 3055 Roslyn Street, Denver, CO 80238; morteza.khodaee@ucdenver.edu
1. Williams VC, Lucas J, Babcock MA, et al. Neurofibromatosis type 1 revisited. Pediatrics. 2009;123:124-133.
2. Ferner RE. The neurofibromatoses. Pract Neurol. 2010;10:82-93.
3. Boyd KP, Korf BR, Theos A. Neurofibromatosis type 1. J Am Acad Dermatol. 2009;61:1-14.
4. Ferner RE, Huson SM, Thomas N, et al. Guidelines for the diagnosis and management of individuals with neurofibromatosis 1. J Med Genet. 2007;44:81-88.
5. Gerber PA, Antal AS, Neumann NJ, et al. Neurofibromatosis. Eur J Med Res. 2009;14:102-105.
6. Shah KN. The diagnostic and clinical significance of café-au-lait macules. Pediatr Clin North Am. 2010;57:1131-1153.
1. Williams VC, Lucas J, Babcock MA, et al. Neurofibromatosis type 1 revisited. Pediatrics. 2009;123:124-133.
2. Ferner RE. The neurofibromatoses. Pract Neurol. 2010;10:82-93.
3. Boyd KP, Korf BR, Theos A. Neurofibromatosis type 1. J Am Acad Dermatol. 2009;61:1-14.
4. Ferner RE, Huson SM, Thomas N, et al. Guidelines for the diagnosis and management of individuals with neurofibromatosis 1. J Med Genet. 2007;44:81-88.
5. Gerber PA, Antal AS, Neumann NJ, et al. Neurofibromatosis. Eur J Med Res. 2009;14:102-105.
6. Shah KN. The diagnostic and clinical significance of café-au-lait macules. Pediatr Clin North Am. 2010;57:1131-1153.