User login
SAN DIEGO – The next-generation anti–B-cell maturation antigen (BCMA) chimeric antigen receptor (CAR) T-cell therapy bb21217 shows encouraging efficacy for relapsed/refractory multiple myeloma, according to early findings from the phase 1 CRB-402 study.
At a median follow-up of 26 weeks, an objective response was seen in 10 of 12 patients (83%) treated with bb21217 at a dose of 150 x 106 CAR+ T cells, Nina Shah, MD, reported at the annual meeting of the American Society of Hematology.
Immunomodulatory CAR T-cell therapy directed against BCMA has shown promising results for the treatment of relapsed/refractory multiple myeloma (RRMM) in several phase 1 clinical studies in patients with advanced disease; bb21217 is based on the investigational therapy bb2121, said Dr. Shah, a hematologist-oncologist at the University of California, San Francisco.
“It uses the same CAR construct design as bb2121. However, it is cultured in the presence of a pan-[phosphoinositide] 3 kinase inhibitor known as bb007 to enrich for T cells displaying a memory-like phenotype,” she said. “CAR T cells enriched with this phenotype may persist and function longer than nonenriched CAR T cells, and the persistence of functional CAR T cells after infusion may be one determinant of the duration of response.”
Preclinical data have supported this approach and CRB-402 – a first-in-human dose-ranging study – was designed to assess the safety, pharmacokinetics, efficacy, and duration of effect of bb21217, Dr. Shah said.
She presented only the data for the 150 x 106 cell dose.
Study subjects were adults with RRMM who had received at least three prior treatment regimens, including a proteasome inhibitor and an immunomodulatory agent, and who had at least 50% expression of BCMA on the plasma cells in bone marrow samples at screening. They had a median age of 63 years, and 58% had high-risk cytogenetic features.
“Patients tended to be pretty heavily pretreated with a median number of lines of treatment of seven,” Dr. Shah said, noting that almost all patients had prior autologous stem cell transplantation, 58% had been exposed to all five available therapies for RRMM, and 17% were refractory to all five therapies.
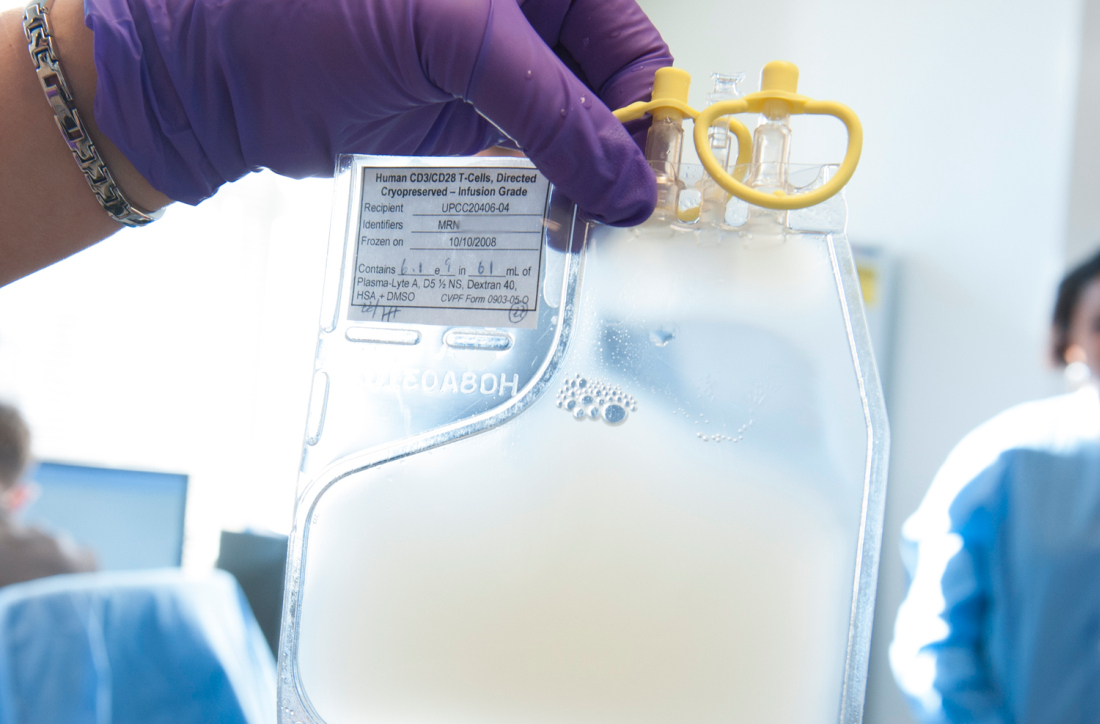
The patients underwent collection of peripheral blood mononuclear cells via leukapheresis and underwent lymphodepletion with fludarabine (30 mg/m2) and cyclophosphamide (300 mg/m2) daily for 3 days prior to receiving the single bb21217 infusion.
Grade 3 or higher adverse events occurring in more than one patient were predominantly cytopenias, which is to be expected in a clinical trial such as this, Dr. Shah said, adding that some hypophosphatemia also occurred.
In those with cytopenias, 58% recovered their absolute neutrophil count (ANC) to greater than 1,000 by day 32, and of the remaining five patients, four of them recovered by day 65.
“Therefore, 11 out of 12 had full ANC recovery by day 65,” she said.
Thrombocytopenia was seen in half of the patients, and in those six patients, two recovered platelet counts to more than 50,000 by day 32, and two more by day 65.
Overall, 10 out of 12 patients had platelet recovery to greater than 50,000 by day 65, she said.
Other adverse events of clinical interest included cytokine release syndrome (CRS) and neurotoxicity.
CRS was usually grade 1 or 2 and occurred in 8 of the 12 patients (67%). One grade 3 CRS event occurred.
“The median time to onset of the CRS was 4.5 days, and this was fairly manageable with or without tocilizumab,” she said.
Neurotoxicity occurred in 3 of 12 patients (25%), and a dose-limiting grade 4 encephalopathy and prolonged grade 3 CRS occurred in one patient with a high tumor burden and rapidly accelerating disease at baseline.
“Because of this, the dose level was expanded and we included patients equally who had high tumor burden and low tumor burden to further understand the contribution of this to this phenomenon. However, no other [dose-limiting toxicities] occurred,” she noted.
Additionally, one patient experienced a grade 3 catheter-related infection, but no other severe infections have been reported, Dr. Shah said, adding that four patients experienced one or more serious adverse events, but no deaths have occurred to date.
Of the 10 patients who achieved an objective response to bb21217, 3 had a complete response (CR) or stringent CR, and 6 patients achieved at least a very good partial response or better.
Some responses deepened over time, therefore some CRs were achieved as late as month 10. Responses are ongoing in all but one responding patient, and the first patient who was dosed continues to respond more than 1 year after treatment.
Of those with good minimal residual disease (MRD) samples available, four were responders, and all four were MRD negative. In contrast, both nonresponders who had tissue available for MRD analysis were MRD positive.
Correlative data show that bone marrow plasma cell clearance was observed early, by day 15, in these representative samples, Dr. Shah said.
“There was a dramatic decline in serum free light chain and serum BCMA ... in all responders by month 1. However, the M protein decline did have some delay, which we would expect based on the half-life, and this resulted in an evolving International Myeloma Working Group response over time,” she said.
Sustained serum BCMA suppression was observed up to month 9, which is likely consistent with ongoing plasma cell aplasia resulting from functional CAR T cell persistence, she explained.
An in vivo examination of the phenotype of the infused CAR T cells showed that while the numbers are small, “so far there seems to be an enrichment for memorylike T cells within the CAR T cell population in the blood post infusion – at least by looking at CD62-ligand T cells.”
There also was a robust and consistent CAR T cell expansion post infusion, which was independent of tumor burden.
“CAR T cells have been detectable up to 9 months post infusion,” she said.
However, the follow-up so far has been very short, she noted. “This action may be underrepresenting the true persistence of these T cells,” she added, explaining that there is only one patient at month 9, whereas all three at month 6 were positive for vector copy.
CRB-402 is ongoing with plans to enroll up to 50 patients. A 300 x 106 dosing cohort has been opened, and doses of 450, 800, and 1200 x 106 CAR+ T cells are planned.
“But longer-term follow-up in a larger patient population will further clarify the depth and durability of the bb21217 tumor response and dose response,” she said.
This study is sponsored by Bluebird Bio. Dr. Shah reported research funding from Bluebird Bio and equity ownership in Indapta Therapeutics, as well as research funding and consulting relationships with other companies.
SOURCE: Shah N et al. ASH 2018, Abstract 488.
SAN DIEGO – The next-generation anti–B-cell maturation antigen (BCMA) chimeric antigen receptor (CAR) T-cell therapy bb21217 shows encouraging efficacy for relapsed/refractory multiple myeloma, according to early findings from the phase 1 CRB-402 study.
At a median follow-up of 26 weeks, an objective response was seen in 10 of 12 patients (83%) treated with bb21217 at a dose of 150 x 106 CAR+ T cells, Nina Shah, MD, reported at the annual meeting of the American Society of Hematology.
Immunomodulatory CAR T-cell therapy directed against BCMA has shown promising results for the treatment of relapsed/refractory multiple myeloma (RRMM) in several phase 1 clinical studies in patients with advanced disease; bb21217 is based on the investigational therapy bb2121, said Dr. Shah, a hematologist-oncologist at the University of California, San Francisco.
“It uses the same CAR construct design as bb2121. However, it is cultured in the presence of a pan-[phosphoinositide] 3 kinase inhibitor known as bb007 to enrich for T cells displaying a memory-like phenotype,” she said. “CAR T cells enriched with this phenotype may persist and function longer than nonenriched CAR T cells, and the persistence of functional CAR T cells after infusion may be one determinant of the duration of response.”
Preclinical data have supported this approach and CRB-402 – a first-in-human dose-ranging study – was designed to assess the safety, pharmacokinetics, efficacy, and duration of effect of bb21217, Dr. Shah said.
She presented only the data for the 150 x 106 cell dose.
Study subjects were adults with RRMM who had received at least three prior treatment regimens, including a proteasome inhibitor and an immunomodulatory agent, and who had at least 50% expression of BCMA on the plasma cells in bone marrow samples at screening. They had a median age of 63 years, and 58% had high-risk cytogenetic features.
“Patients tended to be pretty heavily pretreated with a median number of lines of treatment of seven,” Dr. Shah said, noting that almost all patients had prior autologous stem cell transplantation, 58% had been exposed to all five available therapies for RRMM, and 17% were refractory to all five therapies.
The patients underwent collection of peripheral blood mononuclear cells via leukapheresis and underwent lymphodepletion with fludarabine (30 mg/m2) and cyclophosphamide (300 mg/m2) daily for 3 days prior to receiving the single bb21217 infusion.
Grade 3 or higher adverse events occurring in more than one patient were predominantly cytopenias, which is to be expected in a clinical trial such as this, Dr. Shah said, adding that some hypophosphatemia also occurred.
In those with cytopenias, 58% recovered their absolute neutrophil count (ANC) to greater than 1,000 by day 32, and of the remaining five patients, four of them recovered by day 65.
“Therefore, 11 out of 12 had full ANC recovery by day 65,” she said.
Thrombocytopenia was seen in half of the patients, and in those six patients, two recovered platelet counts to more than 50,000 by day 32, and two more by day 65.
Overall, 10 out of 12 patients had platelet recovery to greater than 50,000 by day 65, she said.
Other adverse events of clinical interest included cytokine release syndrome (CRS) and neurotoxicity.
CRS was usually grade 1 or 2 and occurred in 8 of the 12 patients (67%). One grade 3 CRS event occurred.
“The median time to onset of the CRS was 4.5 days, and this was fairly manageable with or without tocilizumab,” she said.
Neurotoxicity occurred in 3 of 12 patients (25%), and a dose-limiting grade 4 encephalopathy and prolonged grade 3 CRS occurred in one patient with a high tumor burden and rapidly accelerating disease at baseline.
“Because of this, the dose level was expanded and we included patients equally who had high tumor burden and low tumor burden to further understand the contribution of this to this phenomenon. However, no other [dose-limiting toxicities] occurred,” she noted.
Additionally, one patient experienced a grade 3 catheter-related infection, but no other severe infections have been reported, Dr. Shah said, adding that four patients experienced one or more serious adverse events, but no deaths have occurred to date.
Of the 10 patients who achieved an objective response to bb21217, 3 had a complete response (CR) or stringent CR, and 6 patients achieved at least a very good partial response or better.
Some responses deepened over time, therefore some CRs were achieved as late as month 10. Responses are ongoing in all but one responding patient, and the first patient who was dosed continues to respond more than 1 year after treatment.
Of those with good minimal residual disease (MRD) samples available, four were responders, and all four were MRD negative. In contrast, both nonresponders who had tissue available for MRD analysis were MRD positive.
Correlative data show that bone marrow plasma cell clearance was observed early, by day 15, in these representative samples, Dr. Shah said.
“There was a dramatic decline in serum free light chain and serum BCMA ... in all responders by month 1. However, the M protein decline did have some delay, which we would expect based on the half-life, and this resulted in an evolving International Myeloma Working Group response over time,” she said.
Sustained serum BCMA suppression was observed up to month 9, which is likely consistent with ongoing plasma cell aplasia resulting from functional CAR T cell persistence, she explained.
An in vivo examination of the phenotype of the infused CAR T cells showed that while the numbers are small, “so far there seems to be an enrichment for memorylike T cells within the CAR T cell population in the blood post infusion – at least by looking at CD62-ligand T cells.”
There also was a robust and consistent CAR T cell expansion post infusion, which was independent of tumor burden.
“CAR T cells have been detectable up to 9 months post infusion,” she said.
However, the follow-up so far has been very short, she noted. “This action may be underrepresenting the true persistence of these T cells,” she added, explaining that there is only one patient at month 9, whereas all three at month 6 were positive for vector copy.
CRB-402 is ongoing with plans to enroll up to 50 patients. A 300 x 106 dosing cohort has been opened, and doses of 450, 800, and 1200 x 106 CAR+ T cells are planned.
“But longer-term follow-up in a larger patient population will further clarify the depth and durability of the bb21217 tumor response and dose response,” she said.
This study is sponsored by Bluebird Bio. Dr. Shah reported research funding from Bluebird Bio and equity ownership in Indapta Therapeutics, as well as research funding and consulting relationships with other companies.
SOURCE: Shah N et al. ASH 2018, Abstract 488.
SAN DIEGO – The next-generation anti–B-cell maturation antigen (BCMA) chimeric antigen receptor (CAR) T-cell therapy bb21217 shows encouraging efficacy for relapsed/refractory multiple myeloma, according to early findings from the phase 1 CRB-402 study.
At a median follow-up of 26 weeks, an objective response was seen in 10 of 12 patients (83%) treated with bb21217 at a dose of 150 x 106 CAR+ T cells, Nina Shah, MD, reported at the annual meeting of the American Society of Hematology.
Immunomodulatory CAR T-cell therapy directed against BCMA has shown promising results for the treatment of relapsed/refractory multiple myeloma (RRMM) in several phase 1 clinical studies in patients with advanced disease; bb21217 is based on the investigational therapy bb2121, said Dr. Shah, a hematologist-oncologist at the University of California, San Francisco.
“It uses the same CAR construct design as bb2121. However, it is cultured in the presence of a pan-[phosphoinositide] 3 kinase inhibitor known as bb007 to enrich for T cells displaying a memory-like phenotype,” she said. “CAR T cells enriched with this phenotype may persist and function longer than nonenriched CAR T cells, and the persistence of functional CAR T cells after infusion may be one determinant of the duration of response.”
Preclinical data have supported this approach and CRB-402 – a first-in-human dose-ranging study – was designed to assess the safety, pharmacokinetics, efficacy, and duration of effect of bb21217, Dr. Shah said.
She presented only the data for the 150 x 106 cell dose.
Study subjects were adults with RRMM who had received at least three prior treatment regimens, including a proteasome inhibitor and an immunomodulatory agent, and who had at least 50% expression of BCMA on the plasma cells in bone marrow samples at screening. They had a median age of 63 years, and 58% had high-risk cytogenetic features.
“Patients tended to be pretty heavily pretreated with a median number of lines of treatment of seven,” Dr. Shah said, noting that almost all patients had prior autologous stem cell transplantation, 58% had been exposed to all five available therapies for RRMM, and 17% were refractory to all five therapies.
The patients underwent collection of peripheral blood mononuclear cells via leukapheresis and underwent lymphodepletion with fludarabine (30 mg/m2) and cyclophosphamide (300 mg/m2) daily for 3 days prior to receiving the single bb21217 infusion.
Grade 3 or higher adverse events occurring in more than one patient were predominantly cytopenias, which is to be expected in a clinical trial such as this, Dr. Shah said, adding that some hypophosphatemia also occurred.
In those with cytopenias, 58% recovered their absolute neutrophil count (ANC) to greater than 1,000 by day 32, and of the remaining five patients, four of them recovered by day 65.
“Therefore, 11 out of 12 had full ANC recovery by day 65,” she said.
Thrombocytopenia was seen in half of the patients, and in those six patients, two recovered platelet counts to more than 50,000 by day 32, and two more by day 65.
Overall, 10 out of 12 patients had platelet recovery to greater than 50,000 by day 65, she said.
Other adverse events of clinical interest included cytokine release syndrome (CRS) and neurotoxicity.
CRS was usually grade 1 or 2 and occurred in 8 of the 12 patients (67%). One grade 3 CRS event occurred.
“The median time to onset of the CRS was 4.5 days, and this was fairly manageable with or without tocilizumab,” she said.
Neurotoxicity occurred in 3 of 12 patients (25%), and a dose-limiting grade 4 encephalopathy and prolonged grade 3 CRS occurred in one patient with a high tumor burden and rapidly accelerating disease at baseline.
“Because of this, the dose level was expanded and we included patients equally who had high tumor burden and low tumor burden to further understand the contribution of this to this phenomenon. However, no other [dose-limiting toxicities] occurred,” she noted.
Additionally, one patient experienced a grade 3 catheter-related infection, but no other severe infections have been reported, Dr. Shah said, adding that four patients experienced one or more serious adverse events, but no deaths have occurred to date.
Of the 10 patients who achieved an objective response to bb21217, 3 had a complete response (CR) or stringent CR, and 6 patients achieved at least a very good partial response or better.
Some responses deepened over time, therefore some CRs were achieved as late as month 10. Responses are ongoing in all but one responding patient, and the first patient who was dosed continues to respond more than 1 year after treatment.
Of those with good minimal residual disease (MRD) samples available, four were responders, and all four were MRD negative. In contrast, both nonresponders who had tissue available for MRD analysis were MRD positive.
Correlative data show that bone marrow plasma cell clearance was observed early, by day 15, in these representative samples, Dr. Shah said.
“There was a dramatic decline in serum free light chain and serum BCMA ... in all responders by month 1. However, the M protein decline did have some delay, which we would expect based on the half-life, and this resulted in an evolving International Myeloma Working Group response over time,” she said.
Sustained serum BCMA suppression was observed up to month 9, which is likely consistent with ongoing plasma cell aplasia resulting from functional CAR T cell persistence, she explained.
An in vivo examination of the phenotype of the infused CAR T cells showed that while the numbers are small, “so far there seems to be an enrichment for memorylike T cells within the CAR T cell population in the blood post infusion – at least by looking at CD62-ligand T cells.”
There also was a robust and consistent CAR T cell expansion post infusion, which was independent of tumor burden.
“CAR T cells have been detectable up to 9 months post infusion,” she said.
However, the follow-up so far has been very short, she noted. “This action may be underrepresenting the true persistence of these T cells,” she added, explaining that there is only one patient at month 9, whereas all three at month 6 were positive for vector copy.
CRB-402 is ongoing with plans to enroll up to 50 patients. A 300 x 106 dosing cohort has been opened, and doses of 450, 800, and 1200 x 106 CAR+ T cells are planned.
“But longer-term follow-up in a larger patient population will further clarify the depth and durability of the bb21217 tumor response and dose response,” she said.
This study is sponsored by Bluebird Bio. Dr. Shah reported research funding from Bluebird Bio and equity ownership in Indapta Therapeutics, as well as research funding and consulting relationships with other companies.
SOURCE: Shah N et al. ASH 2018, Abstract 488.
REPORTING FROM ASH 2018
Key clinical point:
Major finding: Objective response rate was 83% in the first 12 treated patients.
Study details: The CRB-402 phase 1 dose-escalation of 12 patients (up to 50 planned).
Disclosures: This study is sponsored by Bluebird Bio. Dr. Shah reported research funding from Bluebird Bio and equity ownership in Indapta Therapeutics, as well as research funding and consulting relationships with other companies.
Source: Shah N et al. ASH 2018, Abstract 488.