User login
Although effective for grades III and IV hemorrhoids, conventional hemorrhoidectomy is known to entail a significant recovery period and postoperative pain (strength of recommendation [SOR]: B).
The newest treatment option for grades III and IV hemorrhoids, the procedure for prolapse and hemorrhoids, is an effective technique with the potential to incur less pain and a quicker return to work and daily activities (SOR: B).
For patients with severe hemorrhoidal symptoms who do not want, or are unable, to undergo any type of surgical procedure, rubber band ligation is a viable option (SOR: B).
Hemorrhoids represent one of the most common colorectal complaints heard by family physicians. Each year approximately 10.5 million Americans experience hemorrhoidal symptoms; one fourth of those patients consult a physician.1
The most common symptom of internal hemorrhoids is bright red blood that covers the stool or appears on toilet paper or in the toilet bowl. Other symptoms include irritation of the skin around the anus; pain, swelling, or a hard lump around the anus; hemorrhoidal protrusion; and mucous discharge. Excessive rubbing or cleaning around the anus may exacerbate symptoms and even cause a vicious cycle of irritation, bleeding, and itching termed pruritus ani. Hemorrhoids also may thrombose, causing severe pain.
More than half of men and women aged 50 years and older will develop hemorrhoidal symptoms throughout their lifetime.2 Hemorrhoidal symptoms also tend to flare up during pregnancy, when hormonal changes and the pressure of the fetus cause the hemorrhoidal vessels to enlarge.
The likelihood of hemorrhoidal disease increases with age. By age 30, the anal support structure diminishes in function.3 This microscopic evidence, along with increased sphincter tone, may contribute to the progression of hemorrhoids.4
Although hemorrhoidal symptoms may subside after several days, they most often return, causing long-lasting discomfort and pain. Many affected persons—particularly those with severe hemorrhoids—suffer in silence for years before seeking treatment.5 Fortunately, only about 10% of patients have symptoms severe enough to require surgery.6
Differential diagnosis
Many anorectal problems, including fissures, fistulae, abscesses, or irritation and itching, have symptoms similar to those of hemorrhoids and must be ruled out prior to recommending appropriate treatment. In addition, the correlation of rectal bleeding with colorectal cancer becomes stronger with age, as demonstrated in a retrospective study of the diagnostic value of rectal bleeding in relation to a subsequent diagnosis of colorectal cancer.7 Therefore, further evaluation with colonoscopy should be made in patients who are older than 50 years of age, have a family history of colon cancer, and experience fatigue or weight loss or have a palpable mass.8
Classification of hemorrhoids
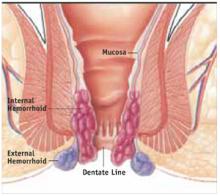
External hemorrhoids originate below the dentate line (FIGURE 1). Internal hemorrhoids are above the line and are classified according to their degree of prolapse:
- Grade I hemorrhoids protrude into the lumen of the anal canal but do not prolapse.
- Grade II hemorrhoids protrude with a bowel movement but spontaneously return when straining stops.
- Grade III hemorrhoids protrude either spontaneously or with a bowel movement, and can be manually reduced.
- Grade IV hemorrhoids have an irreducible prolapse.
This article focuses on a new treatment option for grades III and IV.
FIGURE 1 Mucosal Prolapse and Hemorrhoids
Methods of treating grades III and IV hemorrhoids
Until recently, the recommended treatments for grades III and IV hemorrhoids were limited to rubber band ligation (RBL) and conventional hemorrhoidectomy.
An office procedure not requiring anesthesia, RBL is the use of a latex band to cut off blood flow to the symptomatic hemorrhoid. The procedure is not without complications; there have been several reports of fatal and nonfatal retroperitoneal sepsis after RBL.9,10
Most conventional hemorrhoidectomies are performed in 1 of 2 ways. Outside the United States, the Milligan-Morgan technique, which excises the 3 major hemorrhoidal vessels, is considered the gold standard hemorrhoidectomy. Developed in 1937 in the United Kingdom, the surgery is also known as “open” hemorrhoidectomy because the incisions, which are separated by bridges of skin and mucosa, are left open to avoid stenosis. The Ferguson technique, developed in the United States in 1952, differs from the Milligan-Morgan procedure in that the incisions are sutured shut. Accordingly, it is commonly known as “closed” hemorrhoidectomy.
Regardless of technique, conventional hemorrhoidectomy is known to involve significant postoperative pain and an extended recovery time that precludes a fast return to work and daily activities.
A new stapling technique, the procedure for prolapse and hemorrhoids (PPH), was introduced in the mid-1990s and has been used extensively since then. Also known as stapled hemorrhoidopexy, stapled hemorrhoidectomy, or Longo stapled circumferential mucosectomy, PPH involves the use of a specially designed circular stapler that is inserted through the anus (FIGURE 2). The procedure reduces the prolapse of hemorrhoidal tissue by excising a band of the prolapsed rectal mucosa/internal hemorrhoid. The remaining hemorrhoidal tissue is drawn back into the correct anatomic position within the anal canal.
The stapling technique markedly reduces swelling by disrupting the hemorrhoidal artery blood flow, thereby reducing inflow to the hemorrhoids themselves. In addition, restoring the internal hemorrhoids to their normal anatomic position prevents prolapse and alleviates patients’ symptoms.11 The staples are placed well above the dentate line, and the majority of PPH is performed where there are autonomic nerve fibers, as opposed to somatic innervation. Thus, patients who undergo PPH tend to experience less postoperative pain than do those who undergo conventional hemorrhoidectomy, which involves the cutting of innervated perianal skin. Notably, the function and morphology of the internal anal sphincter, which have a direct bearing on anal continence, are not typically affected by PPH.12 Moreover, in patients with preoperative sensory impairment, the procedure improves anal-canal sensitivity—that is, the ability to distinguish between air and warm water in the anal canal.12 In contrast, research has shown that only about half of the patients who undergo conventional hemorrhoidectomy are able to detect water in the anal canal after surgery, and an additional 25% lose this ability within 6 months of the operation.13 Loss of anal-canal sensitivity affects internal-anal-sphincter function and morphology, which in turn affects anal continence.
Since 2000, several studies have been published confirming that PPH is associated with a low rate of compli-cations.14-16 Rare instances of sepsis following PPH have been reported. Some clinicians recommend administration of prophylactic antibiotics prior to the procedure. Guy and Seow-Choen suggest that the potential for sepsis is high only in cases where an excess amount of muscle is incorporated into the stapler housing. Thus, in recent years, the surgical technique has been refined so as to reduce the potential for postoperative infection.17,18
Randomized controlled trials
PPH versus other methods
Many individuals with extensive hemorrhoidal prolapse may not want to undergo, or will not be candidates for, any type of surgical intervention. For such patients, RBL is a viable option. Indeed, a number of studies endorse RBL as a first-line option for grade III hemorrhoids. However, one should note that RBL carries a high potential for symptomatic recurrence, which often results in the need for multiple bandings.19,20
Peng and colleagues conducted a study in which 55 patients with grade III or small grade IV hemorrhoids were randomized to either RBL or PPH.19 There was a higher incidence of pain at discharge and at 2-week follow-up in the PPH group (P<.001). Six patients in the PPH group experienced procedure-related complications, as opposed to none in the RBL group (P=.027). Despite these results, the authors recommended PPH for patients who did not want to run the risk of requiring further interventions. Notably, the group that underwent RBL had a significantly higher incidence of recurrent bleeding at 2 weeks’ follow-up (68% vs 27%, P=.002). More important, 5 patients in the RBL group needed to undergo excisional hemorrhoidectomy to resolve persistent bleeding or prolapse, whereas none of the PPH patients required further intervention (P<.05).
The earliest randomized controlled clinical trials directly comparing PPH with conventional hemorrhoidectomy reported excellent results21,22; however, patient numbers were small, and, of course, no long-term data were available. Now, reports are in from larger trials and studies with longer-term follow-up.
Shalaby and Desoky conducted a trial in which 200 patients were randomized to either Milligan-Morgan hemorrhoidectomy or PPH. Compared with hemorrhoidectomy, PPH required less operating time (9.0 vs 19.7 minutes, P<.001) and a shorter hospital stay (1.1 vs 2.2 days, P<.001), and provided a faster return to full activity (8.2 vs 53.9 days, P<.001).23 In addition, pain scores were significantly lower in the stapled group after the first 24 hours, at the time of first bowel movement, and at 1 week postoperatively (TABLE 1).
In a 100-patient, prospective, randomized trial, Ganio and colleagues compared PPH with open hemorrhoidectomy and found PPH to be as effective as conventional surgery.24 Postoperative bleeding occurred in 3 patients in each group. However, reduced postoperative pain, a shorter hospital stay, and a trend toward a quicker return to work were reported for the group of patients who underwent PPH. Moderate pain for hemorrhoidectomy patients occurred for a median of 5.3 days (range, 0–19 days) compared with only 3.1 days (range, 0–10 days) in the PPH group. Hemorrhoidectomy patients complained of severe pain for 2.3 days (range, 0–24 days), whereas the PPH patients had only 1 day (range, 0–14 days) of severe pain (P=.01). Functionally, the investigators found no difference between the 2 groups with respect to postoperative fecal incontinence. But, at 1 month, patients in the hemorrhoidectomy group were significantly less continent to flatus.25 The patients who underwent PPH also showed a statistically significant improvement in constipation scores, unlike the group who underwent conventional surgery.
In another study, Palimento and colleagues used several methods to evaluate postoperative pain in a group of 74 patients randomized either to PPH or open hemorrhoidectomy.26 Patients were encouraged to ask freely for pain relief, and the amounts of analgesic consumed were recorded. A visual analogue scale (VAS) from 0 (no pain) to 10 (worst pain imaginable) was completed by each patient at 4 and 24 hours following surgery. The researchers also requested a VAS score to evaluate pain at first defecation. In addition, patients were asked to record when they were able to have completely pain-free bowel movements and when there was pain-free return to normal activities and work. Analgesia requirements were similar between the 2 groups. Median VAS scores in the PPH group were significantly lower than in the open-hemorrhoidectomy group at 4 and 24 hours postoperatively and after first defecation (TABLE 2).
No statistically significant difference between the groups was found for incidence of postoperative bleeding. Nor did the groups differ regarding return to normal activities or return to work. However, the investigators noted that many factors affect the latter 2 outcome measures, including a patient’s motivation and his/her insurance coverage for disability, making comparisons somewhat unreliable. Hence, time to resumption of pain-free defecation was evaluated as a more objective measure and was found to be significantly less in the stapled group (10 vs 12 days, P=.001). At long-term follow-up (median, 17.5 months; range, 10–27 months), occasional pain was reported by 6 (16.2%) of the 37 patients in the PPH group and by 7 (18.9%) of the 37 patients in the open-hemorrhoidectomy group (P=1.000).
Racalbuto and colleagues performed a long-term randomized trial comparing results for 50 patients who underwent PPH with another 50 who underwent Milligan-Morgan hemorrhoidectomy.27 Patients were followed over a period of 48 months. Once again, patients who underwent PPH experienced significantly less pain and therefore were able to return to activities much more quickly than those who underwent conventional hemorrhoidectomy (8.04 ± 1.37 days vs 16.9 ± 2.50 days, P<.0001). In the long-term follow-up evaluation, none of the patients in either treatment group experienced stenosis. In addition, when comparing the 2 groups with respect to anal incontinence and recurrence of prolapse, the investigators did not find any significant differences.
TABLE 1
Mean Pain Scores for PPH vs Milligan-Morgan Hemorrhoidectomy
| PPH Mean (SD) | Milligan-Morgan Mean (SD) | P Value | |
|---|---|---|---|
| First 24 hours | 2.5 (1.3) | 7.6 (0.7) | <.001 |
| First bowel movement | 1.1 (0.3) | 6.6 (1.2) | <.001 |
| 1 week after operation | 0.4 (0.7) | 2.6 (0.6) | <.001 |
| PPH = procedure for prolapse and hemorrhoids; SD = standard deviation. | |||
| Adapted from Shalaby and Desoky.23 | |||
TABLE 2
Median Pain Scores for PPH vs Open Hemorrhoidectomy
| PPH Median (range) | Open Hemorrhoidectomy Median (range) | P Value | |
|---|---|---|---|
| 4 hours after operation | 4 (2–6) | 5 (2–8) | .001 |
| 24 hours after operation | 3 (1–6) | 5 (3–7) | .000 |
| First defecation | 5 (3–8) | 7 (3–9) | .000 |
| PPH = procedure for prolapse and hemorrhoids. | |||
| Data from Palimento et al.26 | |||
Contraindications to PPH
Contraindications to PPH include anal stenosis, that is, an anal canal that does not allow the stapler to be inserted. The PPH procedure also should be avoided in patients with an anorectal abscess, a complex fistula in ano, and perianal Crohn’s disease. As with any other type of surgery, patients undergoing anticoagulation therapy must be carefully evaluated.
Conclusion
The stapling technique is the newest treatment option for grades III and IV hemorrhoids. Although more randomized trials are needed, it appears from the research thus far that PPH is effective, with the potential to involve less pain and a shorter recovery time than conventional hemorrhoidectomy.
Disclosures
Dr Parker serves as a consultant to Ethicon Endo-Surgery. This supplement is supported by a grant from Ethicon Endo-Surgery.
1. Helton WS. for The SSAT, AGA, ASGE Consensus Panel 2001 consensus statement on benign anorectal disease. J Gastrointestinal Surg. 2002;6:302-303.
2. Bailey HR. Innovations for age-old problem: hemorrhoids in the female patient. Female Patient. 2004;29:17-23.
3. Haas PA, Fox TA, Jr, Haas GP. The pathogenesis of hemorrhoids. Dis Colon Rectum. 1984;27:442-450.
4. Hancock BD. Internal sphincter and the nature of haemorrhoids. Gut. 1977;18:651-655.
5. Pfenninger J, Zainea G. Common anorectal conditions: Part I. Symptoms and complaints. Am Fam Physician. 2001;63:2391-2398.
6. Bleday R, Pena JP, Rothenberger DA, et al. Symptomatic hemorrhoids: current incidence and complications of operative therapy. Dis Colon Rectum. 1992;35:477-481.
7. Wauters H, Van Casteren V, Buntinx F. Rectal bleeding and colorectal cancer in general practice: diagnostic study. BMJ. 2000;321:998-999.
8. Smith RA, Cokkinides V, Eyre HJ. American Cancer Society guidelines for the early detection of cancer, 2004. CA Cancer J Clin. 2004;54:41-52.
9. Quevedo-Bonilla G, Farkas AM, Abcarian H, et al. Septic complications of haemorrhoidal banding. Arch Surg. 1988;123:650-651.
10. Scarpa FJ, Hillis W, Sabetta JR. Pelvic cellulitis: a life-threatening complication of hemorrhoidal banding. Surgery. 1988;103:383-385.
11. Hetzer FH, Demartines N, Handschin AE, Clavien PA. Stapled vs excision hemorrhoidectomy: long-term results of a prospective randomized trial. Arch Surg. 2002;137:337-340.
12. Altomare DF, Rinaldi M, Sallustio PL, et al. Long-term effects of stapled haemorrhoidectomy on internal anal function and sensitivity. Br J Surg. 2001;88:1487-1491.
13. Read MG, Read NW, Haynes WG, et al. A prospective study of the effect of haemorrhoidectomy on sphincter function and faecal continence. Br J Surg. 1982;69:396-398.
14. Singer MA, Cintron JR, Fleshman JW, et al. Early experience with stapled hemorrhoidectomy in the United States. Dis Colon Rectum. 2002;45:360-367.
15. Dixon MR, Stamos MJ, Grant SR, et al. Stapled hemorrhoidectomy: a review of our early experience. Am Surg. 2003;69:862-865.
16. Hoffman GH, Firoozmand E. Hemorrhoids—To staple or not to staple: that is the question. Surg Rounds. 2004;27:213-224.
17. Guy RJ, Seow-Choen F. Septic complications after treatment of haemorrhoids. Br J Surg. 2003;90:147-156.
18. Molloy RG, Kingsmore D. Life threatening pelvic sepsis after stapled haemorrhoidectomy [letter]. Lancet. 2000;355:810.-
19. Peng BC, Jayne DG, Ho YH. Randomized trial of rubber band ligation vs. stapled hemorrhoidectomy for prolapsed piles. Dis Colon Rectum. 2003;46:291-297.
20. Komborozos VA, Skrekas GJ, Pissiotis CA. Rubber band ligation of symptomatic internal hemorrhoids: results of 500 cases. Dig Surg. 2000;17:71-76.
21. Mehigan BJ, Monson JRT, Hartley JE. Stapling procedure for haemorrhoids versus Milligan-Morgan haemorrhoidectomy: randomized controlled trial. Lancet. 2000;355:782-785.
22. Rowsell M, Bello M, Hemingway DM. Circumferential mucosectomy (stapled haemorrhoidectomy) versus conventional haemorrhoidectomy: randomized controlled trial. Lancet. 2000;355:779-781.
23. Shalaby R, Desoky A. Randomized clinical trial of stapled versus Milligan-Morgan haemorrhoidectomy. Br J Surg. 2001;88:1049-1053.
24. Ganio E, Altomare DF, Gabrielli F, et al. Prospective randomized multicentre trial comparing stapled with open haemorrhoidectomy. Br J Surg. 2001;88:669-674.
25. Williams NS, Patel J, George BD, et al. Development of an electrically stimulated neoanal sphincter. Lancet. 1991;338:1166-1169.
26. Palimento D, Picchio M, Attanasio U, et al. Stapled and open hemorrhoidectomy: randomized controlled trial of early results. World J Surg. 2003;27:203-207.
27. Racalbuto A, Aliotta I, Corsaro G, et al. Hemorrhoidal stapler prolapsectomy vs. Milligan-Morgan hemorrhoidectomy: a long-term randomized trial. Int J Colorectal Dis. 2004;19:239-244.
Although effective for grades III and IV hemorrhoids, conventional hemorrhoidectomy is known to entail a significant recovery period and postoperative pain (strength of recommendation [SOR]: B).
The newest treatment option for grades III and IV hemorrhoids, the procedure for prolapse and hemorrhoids, is an effective technique with the potential to incur less pain and a quicker return to work and daily activities (SOR: B).
For patients with severe hemorrhoidal symptoms who do not want, or are unable, to undergo any type of surgical procedure, rubber band ligation is a viable option (SOR: B).
Hemorrhoids represent one of the most common colorectal complaints heard by family physicians. Each year approximately 10.5 million Americans experience hemorrhoidal symptoms; one fourth of those patients consult a physician.1
The most common symptom of internal hemorrhoids is bright red blood that covers the stool or appears on toilet paper or in the toilet bowl. Other symptoms include irritation of the skin around the anus; pain, swelling, or a hard lump around the anus; hemorrhoidal protrusion; and mucous discharge. Excessive rubbing or cleaning around the anus may exacerbate symptoms and even cause a vicious cycle of irritation, bleeding, and itching termed pruritus ani. Hemorrhoids also may thrombose, causing severe pain.
More than half of men and women aged 50 years and older will develop hemorrhoidal symptoms throughout their lifetime.2 Hemorrhoidal symptoms also tend to flare up during pregnancy, when hormonal changes and the pressure of the fetus cause the hemorrhoidal vessels to enlarge.
The likelihood of hemorrhoidal disease increases with age. By age 30, the anal support structure diminishes in function.3 This microscopic evidence, along with increased sphincter tone, may contribute to the progression of hemorrhoids.4
Although hemorrhoidal symptoms may subside after several days, they most often return, causing long-lasting discomfort and pain. Many affected persons—particularly those with severe hemorrhoids—suffer in silence for years before seeking treatment.5 Fortunately, only about 10% of patients have symptoms severe enough to require surgery.6
Differential diagnosis
Many anorectal problems, including fissures, fistulae, abscesses, or irritation and itching, have symptoms similar to those of hemorrhoids and must be ruled out prior to recommending appropriate treatment. In addition, the correlation of rectal bleeding with colorectal cancer becomes stronger with age, as demonstrated in a retrospective study of the diagnostic value of rectal bleeding in relation to a subsequent diagnosis of colorectal cancer.7 Therefore, further evaluation with colonoscopy should be made in patients who are older than 50 years of age, have a family history of colon cancer, and experience fatigue or weight loss or have a palpable mass.8
Classification of hemorrhoids
External hemorrhoids originate below the dentate line (FIGURE 1). Internal hemorrhoids are above the line and are classified according to their degree of prolapse:
- Grade I hemorrhoids protrude into the lumen of the anal canal but do not prolapse.
- Grade II hemorrhoids protrude with a bowel movement but spontaneously return when straining stops.
- Grade III hemorrhoids protrude either spontaneously or with a bowel movement, and can be manually reduced.
- Grade IV hemorrhoids have an irreducible prolapse.
This article focuses on a new treatment option for grades III and IV.
FIGURE 1 Mucosal Prolapse and Hemorrhoids
Methods of treating grades III and IV hemorrhoids
Until recently, the recommended treatments for grades III and IV hemorrhoids were limited to rubber band ligation (RBL) and conventional hemorrhoidectomy.
An office procedure not requiring anesthesia, RBL is the use of a latex band to cut off blood flow to the symptomatic hemorrhoid. The procedure is not without complications; there have been several reports of fatal and nonfatal retroperitoneal sepsis after RBL.9,10
Most conventional hemorrhoidectomies are performed in 1 of 2 ways. Outside the United States, the Milligan-Morgan technique, which excises the 3 major hemorrhoidal vessels, is considered the gold standard hemorrhoidectomy. Developed in 1937 in the United Kingdom, the surgery is also known as “open” hemorrhoidectomy because the incisions, which are separated by bridges of skin and mucosa, are left open to avoid stenosis. The Ferguson technique, developed in the United States in 1952, differs from the Milligan-Morgan procedure in that the incisions are sutured shut. Accordingly, it is commonly known as “closed” hemorrhoidectomy.
Regardless of technique, conventional hemorrhoidectomy is known to involve significant postoperative pain and an extended recovery time that precludes a fast return to work and daily activities.
A new stapling technique, the procedure for prolapse and hemorrhoids (PPH), was introduced in the mid-1990s and has been used extensively since then. Also known as stapled hemorrhoidopexy, stapled hemorrhoidectomy, or Longo stapled circumferential mucosectomy, PPH involves the use of a specially designed circular stapler that is inserted through the anus (FIGURE 2). The procedure reduces the prolapse of hemorrhoidal tissue by excising a band of the prolapsed rectal mucosa/internal hemorrhoid. The remaining hemorrhoidal tissue is drawn back into the correct anatomic position within the anal canal.
The stapling technique markedly reduces swelling by disrupting the hemorrhoidal artery blood flow, thereby reducing inflow to the hemorrhoids themselves. In addition, restoring the internal hemorrhoids to their normal anatomic position prevents prolapse and alleviates patients’ symptoms.11 The staples are placed well above the dentate line, and the majority of PPH is performed where there are autonomic nerve fibers, as opposed to somatic innervation. Thus, patients who undergo PPH tend to experience less postoperative pain than do those who undergo conventional hemorrhoidectomy, which involves the cutting of innervated perianal skin. Notably, the function and morphology of the internal anal sphincter, which have a direct bearing on anal continence, are not typically affected by PPH.12 Moreover, in patients with preoperative sensory impairment, the procedure improves anal-canal sensitivity—that is, the ability to distinguish between air and warm water in the anal canal.12 In contrast, research has shown that only about half of the patients who undergo conventional hemorrhoidectomy are able to detect water in the anal canal after surgery, and an additional 25% lose this ability within 6 months of the operation.13 Loss of anal-canal sensitivity affects internal-anal-sphincter function and morphology, which in turn affects anal continence.
Since 2000, several studies have been published confirming that PPH is associated with a low rate of compli-cations.14-16 Rare instances of sepsis following PPH have been reported. Some clinicians recommend administration of prophylactic antibiotics prior to the procedure. Guy and Seow-Choen suggest that the potential for sepsis is high only in cases where an excess amount of muscle is incorporated into the stapler housing. Thus, in recent years, the surgical technique has been refined so as to reduce the potential for postoperative infection.17,18
Randomized controlled trials
PPH versus other methods
Many individuals with extensive hemorrhoidal prolapse may not want to undergo, or will not be candidates for, any type of surgical intervention. For such patients, RBL is a viable option. Indeed, a number of studies endorse RBL as a first-line option for grade III hemorrhoids. However, one should note that RBL carries a high potential for symptomatic recurrence, which often results in the need for multiple bandings.19,20
Peng and colleagues conducted a study in which 55 patients with grade III or small grade IV hemorrhoids were randomized to either RBL or PPH.19 There was a higher incidence of pain at discharge and at 2-week follow-up in the PPH group (P<.001). Six patients in the PPH group experienced procedure-related complications, as opposed to none in the RBL group (P=.027). Despite these results, the authors recommended PPH for patients who did not want to run the risk of requiring further interventions. Notably, the group that underwent RBL had a significantly higher incidence of recurrent bleeding at 2 weeks’ follow-up (68% vs 27%, P=.002). More important, 5 patients in the RBL group needed to undergo excisional hemorrhoidectomy to resolve persistent bleeding or prolapse, whereas none of the PPH patients required further intervention (P<.05).
The earliest randomized controlled clinical trials directly comparing PPH with conventional hemorrhoidectomy reported excellent results21,22; however, patient numbers were small, and, of course, no long-term data were available. Now, reports are in from larger trials and studies with longer-term follow-up.
Shalaby and Desoky conducted a trial in which 200 patients were randomized to either Milligan-Morgan hemorrhoidectomy or PPH. Compared with hemorrhoidectomy, PPH required less operating time (9.0 vs 19.7 minutes, P<.001) and a shorter hospital stay (1.1 vs 2.2 days, P<.001), and provided a faster return to full activity (8.2 vs 53.9 days, P<.001).23 In addition, pain scores were significantly lower in the stapled group after the first 24 hours, at the time of first bowel movement, and at 1 week postoperatively (TABLE 1).
In a 100-patient, prospective, randomized trial, Ganio and colleagues compared PPH with open hemorrhoidectomy and found PPH to be as effective as conventional surgery.24 Postoperative bleeding occurred in 3 patients in each group. However, reduced postoperative pain, a shorter hospital stay, and a trend toward a quicker return to work were reported for the group of patients who underwent PPH. Moderate pain for hemorrhoidectomy patients occurred for a median of 5.3 days (range, 0–19 days) compared with only 3.1 days (range, 0–10 days) in the PPH group. Hemorrhoidectomy patients complained of severe pain for 2.3 days (range, 0–24 days), whereas the PPH patients had only 1 day (range, 0–14 days) of severe pain (P=.01). Functionally, the investigators found no difference between the 2 groups with respect to postoperative fecal incontinence. But, at 1 month, patients in the hemorrhoidectomy group were significantly less continent to flatus.25 The patients who underwent PPH also showed a statistically significant improvement in constipation scores, unlike the group who underwent conventional surgery.
In another study, Palimento and colleagues used several methods to evaluate postoperative pain in a group of 74 patients randomized either to PPH or open hemorrhoidectomy.26 Patients were encouraged to ask freely for pain relief, and the amounts of analgesic consumed were recorded. A visual analogue scale (VAS) from 0 (no pain) to 10 (worst pain imaginable) was completed by each patient at 4 and 24 hours following surgery. The researchers also requested a VAS score to evaluate pain at first defecation. In addition, patients were asked to record when they were able to have completely pain-free bowel movements and when there was pain-free return to normal activities and work. Analgesia requirements were similar between the 2 groups. Median VAS scores in the PPH group were significantly lower than in the open-hemorrhoidectomy group at 4 and 24 hours postoperatively and after first defecation (TABLE 2).
No statistically significant difference between the groups was found for incidence of postoperative bleeding. Nor did the groups differ regarding return to normal activities or return to work. However, the investigators noted that many factors affect the latter 2 outcome measures, including a patient’s motivation and his/her insurance coverage for disability, making comparisons somewhat unreliable. Hence, time to resumption of pain-free defecation was evaluated as a more objective measure and was found to be significantly less in the stapled group (10 vs 12 days, P=.001). At long-term follow-up (median, 17.5 months; range, 10–27 months), occasional pain was reported by 6 (16.2%) of the 37 patients in the PPH group and by 7 (18.9%) of the 37 patients in the open-hemorrhoidectomy group (P=1.000).
Racalbuto and colleagues performed a long-term randomized trial comparing results for 50 patients who underwent PPH with another 50 who underwent Milligan-Morgan hemorrhoidectomy.27 Patients were followed over a period of 48 months. Once again, patients who underwent PPH experienced significantly less pain and therefore were able to return to activities much more quickly than those who underwent conventional hemorrhoidectomy (8.04 ± 1.37 days vs 16.9 ± 2.50 days, P<.0001). In the long-term follow-up evaluation, none of the patients in either treatment group experienced stenosis. In addition, when comparing the 2 groups with respect to anal incontinence and recurrence of prolapse, the investigators did not find any significant differences.
TABLE 1
Mean Pain Scores for PPH vs Milligan-Morgan Hemorrhoidectomy
| PPH Mean (SD) | Milligan-Morgan Mean (SD) | P Value | |
|---|---|---|---|
| First 24 hours | 2.5 (1.3) | 7.6 (0.7) | <.001 |
| First bowel movement | 1.1 (0.3) | 6.6 (1.2) | <.001 |
| 1 week after operation | 0.4 (0.7) | 2.6 (0.6) | <.001 |
| PPH = procedure for prolapse and hemorrhoids; SD = standard deviation. | |||
| Adapted from Shalaby and Desoky.23 | |||
TABLE 2
Median Pain Scores for PPH vs Open Hemorrhoidectomy
| PPH Median (range) | Open Hemorrhoidectomy Median (range) | P Value | |
|---|---|---|---|
| 4 hours after operation | 4 (2–6) | 5 (2–8) | .001 |
| 24 hours after operation | 3 (1–6) | 5 (3–7) | .000 |
| First defecation | 5 (3–8) | 7 (3–9) | .000 |
| PPH = procedure for prolapse and hemorrhoids. | |||
| Data from Palimento et al.26 | |||
Contraindications to PPH
Contraindications to PPH include anal stenosis, that is, an anal canal that does not allow the stapler to be inserted. The PPH procedure also should be avoided in patients with an anorectal abscess, a complex fistula in ano, and perianal Crohn’s disease. As with any other type of surgery, patients undergoing anticoagulation therapy must be carefully evaluated.
Conclusion
The stapling technique is the newest treatment option for grades III and IV hemorrhoids. Although more randomized trials are needed, it appears from the research thus far that PPH is effective, with the potential to involve less pain and a shorter recovery time than conventional hemorrhoidectomy.
Disclosures
Dr Parker serves as a consultant to Ethicon Endo-Surgery. This supplement is supported by a grant from Ethicon Endo-Surgery.
Although effective for grades III and IV hemorrhoids, conventional hemorrhoidectomy is known to entail a significant recovery period and postoperative pain (strength of recommendation [SOR]: B).
The newest treatment option for grades III and IV hemorrhoids, the procedure for prolapse and hemorrhoids, is an effective technique with the potential to incur less pain and a quicker return to work and daily activities (SOR: B).
For patients with severe hemorrhoidal symptoms who do not want, or are unable, to undergo any type of surgical procedure, rubber band ligation is a viable option (SOR: B).
Hemorrhoids represent one of the most common colorectal complaints heard by family physicians. Each year approximately 10.5 million Americans experience hemorrhoidal symptoms; one fourth of those patients consult a physician.1
The most common symptom of internal hemorrhoids is bright red blood that covers the stool or appears on toilet paper or in the toilet bowl. Other symptoms include irritation of the skin around the anus; pain, swelling, or a hard lump around the anus; hemorrhoidal protrusion; and mucous discharge. Excessive rubbing or cleaning around the anus may exacerbate symptoms and even cause a vicious cycle of irritation, bleeding, and itching termed pruritus ani. Hemorrhoids also may thrombose, causing severe pain.
More than half of men and women aged 50 years and older will develop hemorrhoidal symptoms throughout their lifetime.2 Hemorrhoidal symptoms also tend to flare up during pregnancy, when hormonal changes and the pressure of the fetus cause the hemorrhoidal vessels to enlarge.
The likelihood of hemorrhoidal disease increases with age. By age 30, the anal support structure diminishes in function.3 This microscopic evidence, along with increased sphincter tone, may contribute to the progression of hemorrhoids.4
Although hemorrhoidal symptoms may subside after several days, they most often return, causing long-lasting discomfort and pain. Many affected persons—particularly those with severe hemorrhoids—suffer in silence for years before seeking treatment.5 Fortunately, only about 10% of patients have symptoms severe enough to require surgery.6
Differential diagnosis
Many anorectal problems, including fissures, fistulae, abscesses, or irritation and itching, have symptoms similar to those of hemorrhoids and must be ruled out prior to recommending appropriate treatment. In addition, the correlation of rectal bleeding with colorectal cancer becomes stronger with age, as demonstrated in a retrospective study of the diagnostic value of rectal bleeding in relation to a subsequent diagnosis of colorectal cancer.7 Therefore, further evaluation with colonoscopy should be made in patients who are older than 50 years of age, have a family history of colon cancer, and experience fatigue or weight loss or have a palpable mass.8
Classification of hemorrhoids
External hemorrhoids originate below the dentate line (FIGURE 1). Internal hemorrhoids are above the line and are classified according to their degree of prolapse:
- Grade I hemorrhoids protrude into the lumen of the anal canal but do not prolapse.
- Grade II hemorrhoids protrude with a bowel movement but spontaneously return when straining stops.
- Grade III hemorrhoids protrude either spontaneously or with a bowel movement, and can be manually reduced.
- Grade IV hemorrhoids have an irreducible prolapse.
This article focuses on a new treatment option for grades III and IV.
FIGURE 1 Mucosal Prolapse and Hemorrhoids
Methods of treating grades III and IV hemorrhoids
Until recently, the recommended treatments for grades III and IV hemorrhoids were limited to rubber band ligation (RBL) and conventional hemorrhoidectomy.
An office procedure not requiring anesthesia, RBL is the use of a latex band to cut off blood flow to the symptomatic hemorrhoid. The procedure is not without complications; there have been several reports of fatal and nonfatal retroperitoneal sepsis after RBL.9,10
Most conventional hemorrhoidectomies are performed in 1 of 2 ways. Outside the United States, the Milligan-Morgan technique, which excises the 3 major hemorrhoidal vessels, is considered the gold standard hemorrhoidectomy. Developed in 1937 in the United Kingdom, the surgery is also known as “open” hemorrhoidectomy because the incisions, which are separated by bridges of skin and mucosa, are left open to avoid stenosis. The Ferguson technique, developed in the United States in 1952, differs from the Milligan-Morgan procedure in that the incisions are sutured shut. Accordingly, it is commonly known as “closed” hemorrhoidectomy.
Regardless of technique, conventional hemorrhoidectomy is known to involve significant postoperative pain and an extended recovery time that precludes a fast return to work and daily activities.
A new stapling technique, the procedure for prolapse and hemorrhoids (PPH), was introduced in the mid-1990s and has been used extensively since then. Also known as stapled hemorrhoidopexy, stapled hemorrhoidectomy, or Longo stapled circumferential mucosectomy, PPH involves the use of a specially designed circular stapler that is inserted through the anus (FIGURE 2). The procedure reduces the prolapse of hemorrhoidal tissue by excising a band of the prolapsed rectal mucosa/internal hemorrhoid. The remaining hemorrhoidal tissue is drawn back into the correct anatomic position within the anal canal.
The stapling technique markedly reduces swelling by disrupting the hemorrhoidal artery blood flow, thereby reducing inflow to the hemorrhoids themselves. In addition, restoring the internal hemorrhoids to their normal anatomic position prevents prolapse and alleviates patients’ symptoms.11 The staples are placed well above the dentate line, and the majority of PPH is performed where there are autonomic nerve fibers, as opposed to somatic innervation. Thus, patients who undergo PPH tend to experience less postoperative pain than do those who undergo conventional hemorrhoidectomy, which involves the cutting of innervated perianal skin. Notably, the function and morphology of the internal anal sphincter, which have a direct bearing on anal continence, are not typically affected by PPH.12 Moreover, in patients with preoperative sensory impairment, the procedure improves anal-canal sensitivity—that is, the ability to distinguish between air and warm water in the anal canal.12 In contrast, research has shown that only about half of the patients who undergo conventional hemorrhoidectomy are able to detect water in the anal canal after surgery, and an additional 25% lose this ability within 6 months of the operation.13 Loss of anal-canal sensitivity affects internal-anal-sphincter function and morphology, which in turn affects anal continence.
Since 2000, several studies have been published confirming that PPH is associated with a low rate of compli-cations.14-16 Rare instances of sepsis following PPH have been reported. Some clinicians recommend administration of prophylactic antibiotics prior to the procedure. Guy and Seow-Choen suggest that the potential for sepsis is high only in cases where an excess amount of muscle is incorporated into the stapler housing. Thus, in recent years, the surgical technique has been refined so as to reduce the potential for postoperative infection.17,18
Randomized controlled trials
PPH versus other methods
Many individuals with extensive hemorrhoidal prolapse may not want to undergo, or will not be candidates for, any type of surgical intervention. For such patients, RBL is a viable option. Indeed, a number of studies endorse RBL as a first-line option for grade III hemorrhoids. However, one should note that RBL carries a high potential for symptomatic recurrence, which often results in the need for multiple bandings.19,20
Peng and colleagues conducted a study in which 55 patients with grade III or small grade IV hemorrhoids were randomized to either RBL or PPH.19 There was a higher incidence of pain at discharge and at 2-week follow-up in the PPH group (P<.001). Six patients in the PPH group experienced procedure-related complications, as opposed to none in the RBL group (P=.027). Despite these results, the authors recommended PPH for patients who did not want to run the risk of requiring further interventions. Notably, the group that underwent RBL had a significantly higher incidence of recurrent bleeding at 2 weeks’ follow-up (68% vs 27%, P=.002). More important, 5 patients in the RBL group needed to undergo excisional hemorrhoidectomy to resolve persistent bleeding or prolapse, whereas none of the PPH patients required further intervention (P<.05).
The earliest randomized controlled clinical trials directly comparing PPH with conventional hemorrhoidectomy reported excellent results21,22; however, patient numbers were small, and, of course, no long-term data were available. Now, reports are in from larger trials and studies with longer-term follow-up.
Shalaby and Desoky conducted a trial in which 200 patients were randomized to either Milligan-Morgan hemorrhoidectomy or PPH. Compared with hemorrhoidectomy, PPH required less operating time (9.0 vs 19.7 minutes, P<.001) and a shorter hospital stay (1.1 vs 2.2 days, P<.001), and provided a faster return to full activity (8.2 vs 53.9 days, P<.001).23 In addition, pain scores were significantly lower in the stapled group after the first 24 hours, at the time of first bowel movement, and at 1 week postoperatively (TABLE 1).
In a 100-patient, prospective, randomized trial, Ganio and colleagues compared PPH with open hemorrhoidectomy and found PPH to be as effective as conventional surgery.24 Postoperative bleeding occurred in 3 patients in each group. However, reduced postoperative pain, a shorter hospital stay, and a trend toward a quicker return to work were reported for the group of patients who underwent PPH. Moderate pain for hemorrhoidectomy patients occurred for a median of 5.3 days (range, 0–19 days) compared with only 3.1 days (range, 0–10 days) in the PPH group. Hemorrhoidectomy patients complained of severe pain for 2.3 days (range, 0–24 days), whereas the PPH patients had only 1 day (range, 0–14 days) of severe pain (P=.01). Functionally, the investigators found no difference between the 2 groups with respect to postoperative fecal incontinence. But, at 1 month, patients in the hemorrhoidectomy group were significantly less continent to flatus.25 The patients who underwent PPH also showed a statistically significant improvement in constipation scores, unlike the group who underwent conventional surgery.
In another study, Palimento and colleagues used several methods to evaluate postoperative pain in a group of 74 patients randomized either to PPH or open hemorrhoidectomy.26 Patients were encouraged to ask freely for pain relief, and the amounts of analgesic consumed were recorded. A visual analogue scale (VAS) from 0 (no pain) to 10 (worst pain imaginable) was completed by each patient at 4 and 24 hours following surgery. The researchers also requested a VAS score to evaluate pain at first defecation. In addition, patients were asked to record when they were able to have completely pain-free bowel movements and when there was pain-free return to normal activities and work. Analgesia requirements were similar between the 2 groups. Median VAS scores in the PPH group were significantly lower than in the open-hemorrhoidectomy group at 4 and 24 hours postoperatively and after first defecation (TABLE 2).
No statistically significant difference between the groups was found for incidence of postoperative bleeding. Nor did the groups differ regarding return to normal activities or return to work. However, the investigators noted that many factors affect the latter 2 outcome measures, including a patient’s motivation and his/her insurance coverage for disability, making comparisons somewhat unreliable. Hence, time to resumption of pain-free defecation was evaluated as a more objective measure and was found to be significantly less in the stapled group (10 vs 12 days, P=.001). At long-term follow-up (median, 17.5 months; range, 10–27 months), occasional pain was reported by 6 (16.2%) of the 37 patients in the PPH group and by 7 (18.9%) of the 37 patients in the open-hemorrhoidectomy group (P=1.000).
Racalbuto and colleagues performed a long-term randomized trial comparing results for 50 patients who underwent PPH with another 50 who underwent Milligan-Morgan hemorrhoidectomy.27 Patients were followed over a period of 48 months. Once again, patients who underwent PPH experienced significantly less pain and therefore were able to return to activities much more quickly than those who underwent conventional hemorrhoidectomy (8.04 ± 1.37 days vs 16.9 ± 2.50 days, P<.0001). In the long-term follow-up evaluation, none of the patients in either treatment group experienced stenosis. In addition, when comparing the 2 groups with respect to anal incontinence and recurrence of prolapse, the investigators did not find any significant differences.
TABLE 1
Mean Pain Scores for PPH vs Milligan-Morgan Hemorrhoidectomy
| PPH Mean (SD) | Milligan-Morgan Mean (SD) | P Value | |
|---|---|---|---|
| First 24 hours | 2.5 (1.3) | 7.6 (0.7) | <.001 |
| First bowel movement | 1.1 (0.3) | 6.6 (1.2) | <.001 |
| 1 week after operation | 0.4 (0.7) | 2.6 (0.6) | <.001 |
| PPH = procedure for prolapse and hemorrhoids; SD = standard deviation. | |||
| Adapted from Shalaby and Desoky.23 | |||
TABLE 2
Median Pain Scores for PPH vs Open Hemorrhoidectomy
| PPH Median (range) | Open Hemorrhoidectomy Median (range) | P Value | |
|---|---|---|---|
| 4 hours after operation | 4 (2–6) | 5 (2–8) | .001 |
| 24 hours after operation | 3 (1–6) | 5 (3–7) | .000 |
| First defecation | 5 (3–8) | 7 (3–9) | .000 |
| PPH = procedure for prolapse and hemorrhoids. | |||
| Data from Palimento et al.26 | |||
Contraindications to PPH
Contraindications to PPH include anal stenosis, that is, an anal canal that does not allow the stapler to be inserted. The PPH procedure also should be avoided in patients with an anorectal abscess, a complex fistula in ano, and perianal Crohn’s disease. As with any other type of surgery, patients undergoing anticoagulation therapy must be carefully evaluated.
Conclusion
The stapling technique is the newest treatment option for grades III and IV hemorrhoids. Although more randomized trials are needed, it appears from the research thus far that PPH is effective, with the potential to involve less pain and a shorter recovery time than conventional hemorrhoidectomy.
Disclosures
Dr Parker serves as a consultant to Ethicon Endo-Surgery. This supplement is supported by a grant from Ethicon Endo-Surgery.
1. Helton WS. for The SSAT, AGA, ASGE Consensus Panel 2001 consensus statement on benign anorectal disease. J Gastrointestinal Surg. 2002;6:302-303.
2. Bailey HR. Innovations for age-old problem: hemorrhoids in the female patient. Female Patient. 2004;29:17-23.
3. Haas PA, Fox TA, Jr, Haas GP. The pathogenesis of hemorrhoids. Dis Colon Rectum. 1984;27:442-450.
4. Hancock BD. Internal sphincter and the nature of haemorrhoids. Gut. 1977;18:651-655.
5. Pfenninger J, Zainea G. Common anorectal conditions: Part I. Symptoms and complaints. Am Fam Physician. 2001;63:2391-2398.
6. Bleday R, Pena JP, Rothenberger DA, et al. Symptomatic hemorrhoids: current incidence and complications of operative therapy. Dis Colon Rectum. 1992;35:477-481.
7. Wauters H, Van Casteren V, Buntinx F. Rectal bleeding and colorectal cancer in general practice: diagnostic study. BMJ. 2000;321:998-999.
8. Smith RA, Cokkinides V, Eyre HJ. American Cancer Society guidelines for the early detection of cancer, 2004. CA Cancer J Clin. 2004;54:41-52.
9. Quevedo-Bonilla G, Farkas AM, Abcarian H, et al. Septic complications of haemorrhoidal banding. Arch Surg. 1988;123:650-651.
10. Scarpa FJ, Hillis W, Sabetta JR. Pelvic cellulitis: a life-threatening complication of hemorrhoidal banding. Surgery. 1988;103:383-385.
11. Hetzer FH, Demartines N, Handschin AE, Clavien PA. Stapled vs excision hemorrhoidectomy: long-term results of a prospective randomized trial. Arch Surg. 2002;137:337-340.
12. Altomare DF, Rinaldi M, Sallustio PL, et al. Long-term effects of stapled haemorrhoidectomy on internal anal function and sensitivity. Br J Surg. 2001;88:1487-1491.
13. Read MG, Read NW, Haynes WG, et al. A prospective study of the effect of haemorrhoidectomy on sphincter function and faecal continence. Br J Surg. 1982;69:396-398.
14. Singer MA, Cintron JR, Fleshman JW, et al. Early experience with stapled hemorrhoidectomy in the United States. Dis Colon Rectum. 2002;45:360-367.
15. Dixon MR, Stamos MJ, Grant SR, et al. Stapled hemorrhoidectomy: a review of our early experience. Am Surg. 2003;69:862-865.
16. Hoffman GH, Firoozmand E. Hemorrhoids—To staple or not to staple: that is the question. Surg Rounds. 2004;27:213-224.
17. Guy RJ, Seow-Choen F. Septic complications after treatment of haemorrhoids. Br J Surg. 2003;90:147-156.
18. Molloy RG, Kingsmore D. Life threatening pelvic sepsis after stapled haemorrhoidectomy [letter]. Lancet. 2000;355:810.-
19. Peng BC, Jayne DG, Ho YH. Randomized trial of rubber band ligation vs. stapled hemorrhoidectomy for prolapsed piles. Dis Colon Rectum. 2003;46:291-297.
20. Komborozos VA, Skrekas GJ, Pissiotis CA. Rubber band ligation of symptomatic internal hemorrhoids: results of 500 cases. Dig Surg. 2000;17:71-76.
21. Mehigan BJ, Monson JRT, Hartley JE. Stapling procedure for haemorrhoids versus Milligan-Morgan haemorrhoidectomy: randomized controlled trial. Lancet. 2000;355:782-785.
22. Rowsell M, Bello M, Hemingway DM. Circumferential mucosectomy (stapled haemorrhoidectomy) versus conventional haemorrhoidectomy: randomized controlled trial. Lancet. 2000;355:779-781.
23. Shalaby R, Desoky A. Randomized clinical trial of stapled versus Milligan-Morgan haemorrhoidectomy. Br J Surg. 2001;88:1049-1053.
24. Ganio E, Altomare DF, Gabrielli F, et al. Prospective randomized multicentre trial comparing stapled with open haemorrhoidectomy. Br J Surg. 2001;88:669-674.
25. Williams NS, Patel J, George BD, et al. Development of an electrically stimulated neoanal sphincter. Lancet. 1991;338:1166-1169.
26. Palimento D, Picchio M, Attanasio U, et al. Stapled and open hemorrhoidectomy: randomized controlled trial of early results. World J Surg. 2003;27:203-207.
27. Racalbuto A, Aliotta I, Corsaro G, et al. Hemorrhoidal stapler prolapsectomy vs. Milligan-Morgan hemorrhoidectomy: a long-term randomized trial. Int J Colorectal Dis. 2004;19:239-244.
1. Helton WS. for The SSAT, AGA, ASGE Consensus Panel 2001 consensus statement on benign anorectal disease. J Gastrointestinal Surg. 2002;6:302-303.
2. Bailey HR. Innovations for age-old problem: hemorrhoids in the female patient. Female Patient. 2004;29:17-23.
3. Haas PA, Fox TA, Jr, Haas GP. The pathogenesis of hemorrhoids. Dis Colon Rectum. 1984;27:442-450.
4. Hancock BD. Internal sphincter and the nature of haemorrhoids. Gut. 1977;18:651-655.
5. Pfenninger J, Zainea G. Common anorectal conditions: Part I. Symptoms and complaints. Am Fam Physician. 2001;63:2391-2398.
6. Bleday R, Pena JP, Rothenberger DA, et al. Symptomatic hemorrhoids: current incidence and complications of operative therapy. Dis Colon Rectum. 1992;35:477-481.
7. Wauters H, Van Casteren V, Buntinx F. Rectal bleeding and colorectal cancer in general practice: diagnostic study. BMJ. 2000;321:998-999.
8. Smith RA, Cokkinides V, Eyre HJ. American Cancer Society guidelines for the early detection of cancer, 2004. CA Cancer J Clin. 2004;54:41-52.
9. Quevedo-Bonilla G, Farkas AM, Abcarian H, et al. Septic complications of haemorrhoidal banding. Arch Surg. 1988;123:650-651.
10. Scarpa FJ, Hillis W, Sabetta JR. Pelvic cellulitis: a life-threatening complication of hemorrhoidal banding. Surgery. 1988;103:383-385.
11. Hetzer FH, Demartines N, Handschin AE, Clavien PA. Stapled vs excision hemorrhoidectomy: long-term results of a prospective randomized trial. Arch Surg. 2002;137:337-340.
12. Altomare DF, Rinaldi M, Sallustio PL, et al. Long-term effects of stapled haemorrhoidectomy on internal anal function and sensitivity. Br J Surg. 2001;88:1487-1491.
13. Read MG, Read NW, Haynes WG, et al. A prospective study of the effect of haemorrhoidectomy on sphincter function and faecal continence. Br J Surg. 1982;69:396-398.
14. Singer MA, Cintron JR, Fleshman JW, et al. Early experience with stapled hemorrhoidectomy in the United States. Dis Colon Rectum. 2002;45:360-367.
15. Dixon MR, Stamos MJ, Grant SR, et al. Stapled hemorrhoidectomy: a review of our early experience. Am Surg. 2003;69:862-865.
16. Hoffman GH, Firoozmand E. Hemorrhoids—To staple or not to staple: that is the question. Surg Rounds. 2004;27:213-224.
17. Guy RJ, Seow-Choen F. Septic complications after treatment of haemorrhoids. Br J Surg. 2003;90:147-156.
18. Molloy RG, Kingsmore D. Life threatening pelvic sepsis after stapled haemorrhoidectomy [letter]. Lancet. 2000;355:810.-
19. Peng BC, Jayne DG, Ho YH. Randomized trial of rubber band ligation vs. stapled hemorrhoidectomy for prolapsed piles. Dis Colon Rectum. 2003;46:291-297.
20. Komborozos VA, Skrekas GJ, Pissiotis CA. Rubber band ligation of symptomatic internal hemorrhoids: results of 500 cases. Dig Surg. 2000;17:71-76.
21. Mehigan BJ, Monson JRT, Hartley JE. Stapling procedure for haemorrhoids versus Milligan-Morgan haemorrhoidectomy: randomized controlled trial. Lancet. 2000;355:782-785.
22. Rowsell M, Bello M, Hemingway DM. Circumferential mucosectomy (stapled haemorrhoidectomy) versus conventional haemorrhoidectomy: randomized controlled trial. Lancet. 2000;355:779-781.
23. Shalaby R, Desoky A. Randomized clinical trial of stapled versus Milligan-Morgan haemorrhoidectomy. Br J Surg. 2001;88:1049-1053.
24. Ganio E, Altomare DF, Gabrielli F, et al. Prospective randomized multicentre trial comparing stapled with open haemorrhoidectomy. Br J Surg. 2001;88:669-674.
25. Williams NS, Patel J, George BD, et al. Development of an electrically stimulated neoanal sphincter. Lancet. 1991;338:1166-1169.
26. Palimento D, Picchio M, Attanasio U, et al. Stapled and open hemorrhoidectomy: randomized controlled trial of early results. World J Surg. 2003;27:203-207.
27. Racalbuto A, Aliotta I, Corsaro G, et al. Hemorrhoidal stapler prolapsectomy vs. Milligan-Morgan hemorrhoidectomy: a long-term randomized trial. Int J Colorectal Dis. 2004;19:239-244.