User login
Within the last 2 years, new DNA sequencing technologies, dubbed NextGen (“next generation”), have been introduced that are revolutionizing the field of neurogenetics. As these advances gain recognition within and outside the medical community, the pace of progress is quickening, with the help of support from broad-based advocacy groups and more funding options. These technologies are already bringing greater diagnostic opportunities to practice, although the time may not yet be ripe for translating the results into information useful for the clinical management of patients.
“For rare diseases, this is a real game-changer type of technology,” commented Matthew J. Huentelman, Ph.D., a neurogeneticist affiliated with the Translational Genomics Research Institute in Phoenix. “We have had some significant leaps in what we can do with the human genome over the past couple of years, especially in the mechanics and chemistry of how sequencing is done. Several companies have built machines that sequence DNA in fundamentally different ways than we did 5-10 years ago.” Since 2007, Dr. Huentelman has been applying NextGen technology to the study of Alzheimer’s disease and autism.
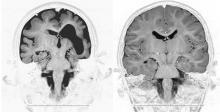
Whole exome DNA sequencing is one of the NextGen technologies that are being applied to neurologic disorders. Unlike whole genome sequencing, whole exome DNA sequencing focuses on the small portion of the genome (less than 2%) that contains protein-coding bits of DNA, known as the exome. For example, Dr. Murat Gunel, chief of the Neurovascular Surgery Program and codirector of the Program on Neurogenetics at Yale University, New Haven, Conn., recently used whole exome sequencing to determine that several distinct types of malformations of cortical development, including microcephaly, pachygyria with cortical thickening, and hypoplasia of the corpus callosum were all associated with recessive mutations in a single gene, WDR62 (Nature 2010;467:207-10). This discovery was made by analyzing the DNA of several children with microcephaly among 30 interrelated Turkish families.
The last few months have brought other reports that used whole exome sequencing to identify causative gene mutations for Perrault syndrome (Am. J. Hum. Genet. 2010;87:282-8), Joubert’s syndrome (Am. J. Hum. Genet. 2010;86:93-7), and Fowler syndrome (Human Mutation 2010;31:918-23).
One advantage of exome sequencing studies is that researchers can use smaller sample sets – with an “n” as small as 1 – in a comprehensive fashion, Dr. Huentelman said. “This is great for rare diseases or to gain a foothold in a disease that has been hard to understand at the population level. For instance, we can analyze the differences between twins discordant for autism.”
Advantages of exome sequencing include its speed and cost effectiveness. Dr. Gunel reports that in his laboratory, whole genome sequencing might take several weeks and cost about $50,000 while he can receive the results of whole exome sequencing within 9 days, at a cost of about $3,500.
“These tests are still pricey,” said Dr. Andrea Gropman, a neurogeneticist at the Children’s National Medical Center and George Washington University, both in Washington. For sequencing genes related to autism, she said that costs may range from $1,000 to $5,800, which insurance companies may or may not cover. “For some families, that means they must pay out of pocket.”
New Funding Opportunities
Advances in the field may be due, in part, to greater funding opportunities. Dr. Gunel’s research was supported in part by a $2.9 million “stimulus grant” from the National Institute of Neurological Disorders and Stroke, part of the $8.2 billion provided to the National Institutes of Health from the American Recovery and Reinvestment Act. He plans to use his stimulus money to extend whole exome sequencing to hundreds of other families affected by malformations of cortical development.
Another significant source of funds has been distributed through the NIH’s Office of Rare Diseases Research (ORDR), which allocated almost $70 million in 2003 toward the creation of 10 clinical consortia and one Data and Technology Coordinating Center.
“In the late 1990s and early 2000, we felt we didn’t have a good infrastructure in place to do research in rare diseases – of which we estimated there were at least 6,800,” said Steve C. Groft, Pharm.D., director of the ORDR. “We hoped the funds we provided could go toward establishing that infrastructure.”
Recently, a second round of funding of approximately $125 million was awarded to 19 consortia, including 6 of the 10 original groups. Nine of the consortia are related to neurologic disease, including those focusing on Angelman, Rett, and Prader-Willi syndromes; autonomic rare diseases; neurologic channelopathies; spinocerebellar ataxias; dystonias; lysosomal diseases; inherited neuropathies; brain vascular malformations; and mitochondrial diseases. Consortia have grown as they have become successful in establishing partners from other branches of NIH and industry, Dr. Groft said.
One of the most unique aspects of the Rare Disease Clinical Research Grants is the mandate to collaborate with a patient advocacy group. “We have noticed that, in order to have a successful research program for rare diseases, we need the involvement of patient advocacy groups. These groups are essential to help with patient recruitment and to act as liaisons between researchers and the group’s constituency of patients and their families,” Dr. Groft said.
In fact, a Coalition of Patient Advocacy Groups has been formed as an arm of the Rare Disease Clinical Research Network.
“The role of advocacy groups has really matured over the last several years,” Dr. Gropman said. “I work closely with an amazing advocacy group in the Urea Cycle Disorders Consortium. They have gone from a grassroots support of families to major partners in research.”
Dr. Gropman credits the group with raising important clinical questions that only those living with affected individuals might be aware of, educating patients and their families about the importance of participation in clinical trials, as well providing financial support and finding philanthropic partners.
“Patient advocates have a vested interest in moving the clinical research process along,” she said.
Another new initiative to facilitate funding for rare diseases is the R.A.R.E. (Rare Disease Advocacy, Research, and Education) Project’s Global Genes Fund, a Web site in development that aims to serve as a clearinghouse for rare disease philanthropy.
“As long as the rare disease community works in their separate disease silos, we can only get so far. ... If we can bring the community together and not focus on an individual disease, we can create a unifying campaign and rare diseases then becomes a huge public health issue, larger than the U.S. AIDS community and equal to that of breast cancer,” said Nicole Boice, founder and president of R.A.R.E.
One part of the Global Genes Fund, which is set to launch in the second quarter of 2011, will showcase innovative scientific research projects that individuals or businesses can contribute to, in donations as small as $25. Initially, Ms. Boice expects to focus on 10-20 research projects.
“As the platform grows and is successful at securing funding, this will catalyze this type of innovative funding,” she said.
Using Neurogenetics in Practice
Genetic testing can be helpful for diagnosing some neurologic disorders, but there is a “bewildering” maze of tests available, Dr. Gropman said. Vendors have put together pre-determined panels for whole exome sequencing of some disorders, such as spinal cerebellar ataxia or disorders associated with mental disabilities.
“Using a panel, you can test for a number of different genes simultaneously, but you cannot separate them,” she said.
Also coming to market are “designer” panels that allow clinicians to pick and choose which genes to target, but they require knowing a priori which mutation to focus on.
“While the technology has exploded, knowing which test to order can be baffling for many clinicians who do not have extensive backgrounds in genetics. If we find a variant but don’t know its significance, it opens up a diagnostic conundrum,” Dr. Gropman said. The field is still in flux, so many other questions must be resolved, such as how to deal with difficult or unanticipated results and whether technology and interpretation need to be standardized.
Genotyping is not just a black-and-white issue, according to Dr. Huentelman. In addition to the knowledge of a patient’s mutation status, genotyping results must also take into consideration the risk of developing clinical symptoms and the ethical and pragmatic issues that knowledge raises for patients and physicians.
As a first step, neurologists should begin educating themselves about the new technologies, potential applications, and shortcomings, by attending sessions on neurogenetics at annual professional meetings or more specialized conferences. While commercial vendors may provide varying degrees of advice about test selection, creating a professional relationship with a geneticist or genetic counselor might provide access to the most up-to-date information and options.
“You need someone fully entrenched in the field of human genetics,” said Dr. Huentelman, who advocates creating a genetics team to sort through the maze of data that can be generated by a genetic analysis.
As a specialist in translational medicine, Dr. Huentelman focuses on understanding the genetic cause of disease and then translating this information into new diagnostic tests and therapeutics. While new DNA sequencing methods are quickly making the first goal a reality, accomplishing the second goal still remains “hopes and dreams,” he said. The ultimate goal of genetic mapping is to personalize medicine by shifting clinical practice from that based on clinical symptoms to that tailored to an individual’s genetic make-up, but broad gaps in knowledge remain. The hope is to develop pharmaceuticals to correct the deficiency caused by a particular mutation or to use genetic testing to preselect patients who might benefit from a particular therapy, similar to the ongoing work on apolipoprotein E genotype status and Alzheimer’s disease.
“We are reaching the critical mass level” in neurogenetic research, Dr. Groft said. As increasing numbers of patients with genetic disorders are followed, clinicians and researchers are developing the clinical skills and diagnostic tools to advance the understanding of disease pathogenesis. At the same time, these accomplishments are piquing interest and collaboration from others in the medical community, spurred by the increasing availability of funds and non-monetary support from the government, private foundations, industry, and patient advocacy groups. It is anticipated that neurogenetics is on the cusp of major breakthroughs for clinical neurology.
Disclosures: None of the sources contacted for this article had any relevant financial disclosures.
Within the last 2 years, new DNA sequencing technologies, dubbed NextGen (“next generation”), have been introduced that are revolutionizing the field of neurogenetics. As these advances gain recognition within and outside the medical community, the pace of progress is quickening, with the help of support from broad-based advocacy groups and more funding options. These technologies are already bringing greater diagnostic opportunities to practice, although the time may not yet be ripe for translating the results into information useful for the clinical management of patients.
“For rare diseases, this is a real game-changer type of technology,” commented Matthew J. Huentelman, Ph.D., a neurogeneticist affiliated with the Translational Genomics Research Institute in Phoenix. “We have had some significant leaps in what we can do with the human genome over the past couple of years, especially in the mechanics and chemistry of how sequencing is done. Several companies have built machines that sequence DNA in fundamentally different ways than we did 5-10 years ago.” Since 2007, Dr. Huentelman has been applying NextGen technology to the study of Alzheimer’s disease and autism.
Whole exome DNA sequencing is one of the NextGen technologies that are being applied to neurologic disorders. Unlike whole genome sequencing, whole exome DNA sequencing focuses on the small portion of the genome (less than 2%) that contains protein-coding bits of DNA, known as the exome. For example, Dr. Murat Gunel, chief of the Neurovascular Surgery Program and codirector of the Program on Neurogenetics at Yale University, New Haven, Conn., recently used whole exome sequencing to determine that several distinct types of malformations of cortical development, including microcephaly, pachygyria with cortical thickening, and hypoplasia of the corpus callosum were all associated with recessive mutations in a single gene, WDR62 (Nature 2010;467:207-10). This discovery was made by analyzing the DNA of several children with microcephaly among 30 interrelated Turkish families.
The last few months have brought other reports that used whole exome sequencing to identify causative gene mutations for Perrault syndrome (Am. J. Hum. Genet. 2010;87:282-8), Joubert’s syndrome (Am. J. Hum. Genet. 2010;86:93-7), and Fowler syndrome (Human Mutation 2010;31:918-23).
One advantage of exome sequencing studies is that researchers can use smaller sample sets – with an “n” as small as 1 – in a comprehensive fashion, Dr. Huentelman said. “This is great for rare diseases or to gain a foothold in a disease that has been hard to understand at the population level. For instance, we can analyze the differences between twins discordant for autism.”
Advantages of exome sequencing include its speed and cost effectiveness. Dr. Gunel reports that in his laboratory, whole genome sequencing might take several weeks and cost about $50,000 while he can receive the results of whole exome sequencing within 9 days, at a cost of about $3,500.
“These tests are still pricey,” said Dr. Andrea Gropman, a neurogeneticist at the Children’s National Medical Center and George Washington University, both in Washington. For sequencing genes related to autism, she said that costs may range from $1,000 to $5,800, which insurance companies may or may not cover. “For some families, that means they must pay out of pocket.”
New Funding Opportunities
Advances in the field may be due, in part, to greater funding opportunities. Dr. Gunel’s research was supported in part by a $2.9 million “stimulus grant” from the National Institute of Neurological Disorders and Stroke, part of the $8.2 billion provided to the National Institutes of Health from the American Recovery and Reinvestment Act. He plans to use his stimulus money to extend whole exome sequencing to hundreds of other families affected by malformations of cortical development.
Another significant source of funds has been distributed through the NIH’s Office of Rare Diseases Research (ORDR), which allocated almost $70 million in 2003 toward the creation of 10 clinical consortia and one Data and Technology Coordinating Center.
“In the late 1990s and early 2000, we felt we didn’t have a good infrastructure in place to do research in rare diseases – of which we estimated there were at least 6,800,” said Steve C. Groft, Pharm.D., director of the ORDR. “We hoped the funds we provided could go toward establishing that infrastructure.”
Recently, a second round of funding of approximately $125 million was awarded to 19 consortia, including 6 of the 10 original groups. Nine of the consortia are related to neurologic disease, including those focusing on Angelman, Rett, and Prader-Willi syndromes; autonomic rare diseases; neurologic channelopathies; spinocerebellar ataxias; dystonias; lysosomal diseases; inherited neuropathies; brain vascular malformations; and mitochondrial diseases. Consortia have grown as they have become successful in establishing partners from other branches of NIH and industry, Dr. Groft said.
One of the most unique aspects of the Rare Disease Clinical Research Grants is the mandate to collaborate with a patient advocacy group. “We have noticed that, in order to have a successful research program for rare diseases, we need the involvement of patient advocacy groups. These groups are essential to help with patient recruitment and to act as liaisons between researchers and the group’s constituency of patients and their families,” Dr. Groft said.
In fact, a Coalition of Patient Advocacy Groups has been formed as an arm of the Rare Disease Clinical Research Network.
“The role of advocacy groups has really matured over the last several years,” Dr. Gropman said. “I work closely with an amazing advocacy group in the Urea Cycle Disorders Consortium. They have gone from a grassroots support of families to major partners in research.”
Dr. Gropman credits the group with raising important clinical questions that only those living with affected individuals might be aware of, educating patients and their families about the importance of participation in clinical trials, as well providing financial support and finding philanthropic partners.
“Patient advocates have a vested interest in moving the clinical research process along,” she said.
Another new initiative to facilitate funding for rare diseases is the R.A.R.E. (Rare Disease Advocacy, Research, and Education) Project’s Global Genes Fund, a Web site in development that aims to serve as a clearinghouse for rare disease philanthropy.
“As long as the rare disease community works in their separate disease silos, we can only get so far. ... If we can bring the community together and not focus on an individual disease, we can create a unifying campaign and rare diseases then becomes a huge public health issue, larger than the U.S. AIDS community and equal to that of breast cancer,” said Nicole Boice, founder and president of R.A.R.E.
One part of the Global Genes Fund, which is set to launch in the second quarter of 2011, will showcase innovative scientific research projects that individuals or businesses can contribute to, in donations as small as $25. Initially, Ms. Boice expects to focus on 10-20 research projects.
“As the platform grows and is successful at securing funding, this will catalyze this type of innovative funding,” she said.
Using Neurogenetics in Practice
Genetic testing can be helpful for diagnosing some neurologic disorders, but there is a “bewildering” maze of tests available, Dr. Gropman said. Vendors have put together pre-determined panels for whole exome sequencing of some disorders, such as spinal cerebellar ataxia or disorders associated with mental disabilities.
“Using a panel, you can test for a number of different genes simultaneously, but you cannot separate them,” she said.
Also coming to market are “designer” panels that allow clinicians to pick and choose which genes to target, but they require knowing a priori which mutation to focus on.
“While the technology has exploded, knowing which test to order can be baffling for many clinicians who do not have extensive backgrounds in genetics. If we find a variant but don’t know its significance, it opens up a diagnostic conundrum,” Dr. Gropman said. The field is still in flux, so many other questions must be resolved, such as how to deal with difficult or unanticipated results and whether technology and interpretation need to be standardized.
Genotyping is not just a black-and-white issue, according to Dr. Huentelman. In addition to the knowledge of a patient’s mutation status, genotyping results must also take into consideration the risk of developing clinical symptoms and the ethical and pragmatic issues that knowledge raises for patients and physicians.
As a first step, neurologists should begin educating themselves about the new technologies, potential applications, and shortcomings, by attending sessions on neurogenetics at annual professional meetings or more specialized conferences. While commercial vendors may provide varying degrees of advice about test selection, creating a professional relationship with a geneticist or genetic counselor might provide access to the most up-to-date information and options.
“You need someone fully entrenched in the field of human genetics,” said Dr. Huentelman, who advocates creating a genetics team to sort through the maze of data that can be generated by a genetic analysis.
As a specialist in translational medicine, Dr. Huentelman focuses on understanding the genetic cause of disease and then translating this information into new diagnostic tests and therapeutics. While new DNA sequencing methods are quickly making the first goal a reality, accomplishing the second goal still remains “hopes and dreams,” he said. The ultimate goal of genetic mapping is to personalize medicine by shifting clinical practice from that based on clinical symptoms to that tailored to an individual’s genetic make-up, but broad gaps in knowledge remain. The hope is to develop pharmaceuticals to correct the deficiency caused by a particular mutation or to use genetic testing to preselect patients who might benefit from a particular therapy, similar to the ongoing work on apolipoprotein E genotype status and Alzheimer’s disease.
“We are reaching the critical mass level” in neurogenetic research, Dr. Groft said. As increasing numbers of patients with genetic disorders are followed, clinicians and researchers are developing the clinical skills and diagnostic tools to advance the understanding of disease pathogenesis. At the same time, these accomplishments are piquing interest and collaboration from others in the medical community, spurred by the increasing availability of funds and non-monetary support from the government, private foundations, industry, and patient advocacy groups. It is anticipated that neurogenetics is on the cusp of major breakthroughs for clinical neurology.
Disclosures: None of the sources contacted for this article had any relevant financial disclosures.
Within the last 2 years, new DNA sequencing technologies, dubbed NextGen (“next generation”), have been introduced that are revolutionizing the field of neurogenetics. As these advances gain recognition within and outside the medical community, the pace of progress is quickening, with the help of support from broad-based advocacy groups and more funding options. These technologies are already bringing greater diagnostic opportunities to practice, although the time may not yet be ripe for translating the results into information useful for the clinical management of patients.
“For rare diseases, this is a real game-changer type of technology,” commented Matthew J. Huentelman, Ph.D., a neurogeneticist affiliated with the Translational Genomics Research Institute in Phoenix. “We have had some significant leaps in what we can do with the human genome over the past couple of years, especially in the mechanics and chemistry of how sequencing is done. Several companies have built machines that sequence DNA in fundamentally different ways than we did 5-10 years ago.” Since 2007, Dr. Huentelman has been applying NextGen technology to the study of Alzheimer’s disease and autism.
Whole exome DNA sequencing is one of the NextGen technologies that are being applied to neurologic disorders. Unlike whole genome sequencing, whole exome DNA sequencing focuses on the small portion of the genome (less than 2%) that contains protein-coding bits of DNA, known as the exome. For example, Dr. Murat Gunel, chief of the Neurovascular Surgery Program and codirector of the Program on Neurogenetics at Yale University, New Haven, Conn., recently used whole exome sequencing to determine that several distinct types of malformations of cortical development, including microcephaly, pachygyria with cortical thickening, and hypoplasia of the corpus callosum were all associated with recessive mutations in a single gene, WDR62 (Nature 2010;467:207-10). This discovery was made by analyzing the DNA of several children with microcephaly among 30 interrelated Turkish families.
The last few months have brought other reports that used whole exome sequencing to identify causative gene mutations for Perrault syndrome (Am. J. Hum. Genet. 2010;87:282-8), Joubert’s syndrome (Am. J. Hum. Genet. 2010;86:93-7), and Fowler syndrome (Human Mutation 2010;31:918-23).
One advantage of exome sequencing studies is that researchers can use smaller sample sets – with an “n” as small as 1 – in a comprehensive fashion, Dr. Huentelman said. “This is great for rare diseases or to gain a foothold in a disease that has been hard to understand at the population level. For instance, we can analyze the differences between twins discordant for autism.”
Advantages of exome sequencing include its speed and cost effectiveness. Dr. Gunel reports that in his laboratory, whole genome sequencing might take several weeks and cost about $50,000 while he can receive the results of whole exome sequencing within 9 days, at a cost of about $3,500.
“These tests are still pricey,” said Dr. Andrea Gropman, a neurogeneticist at the Children’s National Medical Center and George Washington University, both in Washington. For sequencing genes related to autism, she said that costs may range from $1,000 to $5,800, which insurance companies may or may not cover. “For some families, that means they must pay out of pocket.”
New Funding Opportunities
Advances in the field may be due, in part, to greater funding opportunities. Dr. Gunel’s research was supported in part by a $2.9 million “stimulus grant” from the National Institute of Neurological Disorders and Stroke, part of the $8.2 billion provided to the National Institutes of Health from the American Recovery and Reinvestment Act. He plans to use his stimulus money to extend whole exome sequencing to hundreds of other families affected by malformations of cortical development.
Another significant source of funds has been distributed through the NIH’s Office of Rare Diseases Research (ORDR), which allocated almost $70 million in 2003 toward the creation of 10 clinical consortia and one Data and Technology Coordinating Center.
“In the late 1990s and early 2000, we felt we didn’t have a good infrastructure in place to do research in rare diseases – of which we estimated there were at least 6,800,” said Steve C. Groft, Pharm.D., director of the ORDR. “We hoped the funds we provided could go toward establishing that infrastructure.”
Recently, a second round of funding of approximately $125 million was awarded to 19 consortia, including 6 of the 10 original groups. Nine of the consortia are related to neurologic disease, including those focusing on Angelman, Rett, and Prader-Willi syndromes; autonomic rare diseases; neurologic channelopathies; spinocerebellar ataxias; dystonias; lysosomal diseases; inherited neuropathies; brain vascular malformations; and mitochondrial diseases. Consortia have grown as they have become successful in establishing partners from other branches of NIH and industry, Dr. Groft said.
One of the most unique aspects of the Rare Disease Clinical Research Grants is the mandate to collaborate with a patient advocacy group. “We have noticed that, in order to have a successful research program for rare diseases, we need the involvement of patient advocacy groups. These groups are essential to help with patient recruitment and to act as liaisons between researchers and the group’s constituency of patients and their families,” Dr. Groft said.
In fact, a Coalition of Patient Advocacy Groups has been formed as an arm of the Rare Disease Clinical Research Network.
“The role of advocacy groups has really matured over the last several years,” Dr. Gropman said. “I work closely with an amazing advocacy group in the Urea Cycle Disorders Consortium. They have gone from a grassroots support of families to major partners in research.”
Dr. Gropman credits the group with raising important clinical questions that only those living with affected individuals might be aware of, educating patients and their families about the importance of participation in clinical trials, as well providing financial support and finding philanthropic partners.
“Patient advocates have a vested interest in moving the clinical research process along,” she said.
Another new initiative to facilitate funding for rare diseases is the R.A.R.E. (Rare Disease Advocacy, Research, and Education) Project’s Global Genes Fund, a Web site in development that aims to serve as a clearinghouse for rare disease philanthropy.
“As long as the rare disease community works in their separate disease silos, we can only get so far. ... If we can bring the community together and not focus on an individual disease, we can create a unifying campaign and rare diseases then becomes a huge public health issue, larger than the U.S. AIDS community and equal to that of breast cancer,” said Nicole Boice, founder and president of R.A.R.E.
One part of the Global Genes Fund, which is set to launch in the second quarter of 2011, will showcase innovative scientific research projects that individuals or businesses can contribute to, in donations as small as $25. Initially, Ms. Boice expects to focus on 10-20 research projects.
“As the platform grows and is successful at securing funding, this will catalyze this type of innovative funding,” she said.
Using Neurogenetics in Practice
Genetic testing can be helpful for diagnosing some neurologic disorders, but there is a “bewildering” maze of tests available, Dr. Gropman said. Vendors have put together pre-determined panels for whole exome sequencing of some disorders, such as spinal cerebellar ataxia or disorders associated with mental disabilities.
“Using a panel, you can test for a number of different genes simultaneously, but you cannot separate them,” she said.
Also coming to market are “designer” panels that allow clinicians to pick and choose which genes to target, but they require knowing a priori which mutation to focus on.
“While the technology has exploded, knowing which test to order can be baffling for many clinicians who do not have extensive backgrounds in genetics. If we find a variant but don’t know its significance, it opens up a diagnostic conundrum,” Dr. Gropman said. The field is still in flux, so many other questions must be resolved, such as how to deal with difficult or unanticipated results and whether technology and interpretation need to be standardized.
Genotyping is not just a black-and-white issue, according to Dr. Huentelman. In addition to the knowledge of a patient’s mutation status, genotyping results must also take into consideration the risk of developing clinical symptoms and the ethical and pragmatic issues that knowledge raises for patients and physicians.
As a first step, neurologists should begin educating themselves about the new technologies, potential applications, and shortcomings, by attending sessions on neurogenetics at annual professional meetings or more specialized conferences. While commercial vendors may provide varying degrees of advice about test selection, creating a professional relationship with a geneticist or genetic counselor might provide access to the most up-to-date information and options.
“You need someone fully entrenched in the field of human genetics,” said Dr. Huentelman, who advocates creating a genetics team to sort through the maze of data that can be generated by a genetic analysis.
As a specialist in translational medicine, Dr. Huentelman focuses on understanding the genetic cause of disease and then translating this information into new diagnostic tests and therapeutics. While new DNA sequencing methods are quickly making the first goal a reality, accomplishing the second goal still remains “hopes and dreams,” he said. The ultimate goal of genetic mapping is to personalize medicine by shifting clinical practice from that based on clinical symptoms to that tailored to an individual’s genetic make-up, but broad gaps in knowledge remain. The hope is to develop pharmaceuticals to correct the deficiency caused by a particular mutation or to use genetic testing to preselect patients who might benefit from a particular therapy, similar to the ongoing work on apolipoprotein E genotype status and Alzheimer’s disease.
“We are reaching the critical mass level” in neurogenetic research, Dr. Groft said. As increasing numbers of patients with genetic disorders are followed, clinicians and researchers are developing the clinical skills and diagnostic tools to advance the understanding of disease pathogenesis. At the same time, these accomplishments are piquing interest and collaboration from others in the medical community, spurred by the increasing availability of funds and non-monetary support from the government, private foundations, industry, and patient advocacy groups. It is anticipated that neurogenetics is on the cusp of major breakthroughs for clinical neurology.
Disclosures: None of the sources contacted for this article had any relevant financial disclosures.