User login
A 36-year-old Caucasian man sought care at our facility for rapidly progressive painful ulcers that were affecting his throat, tongue, genital area, and other parts of his body. He said that the lesions erupted 6 days earlier, and indicated that he had a history of recurrent oral aphthous ulcers.
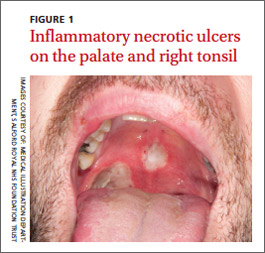
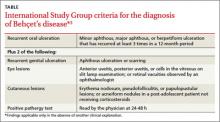
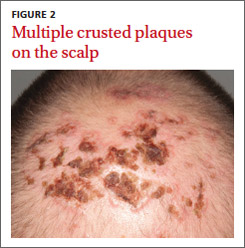
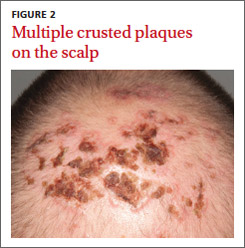
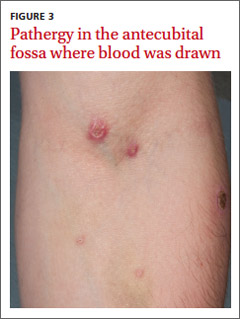
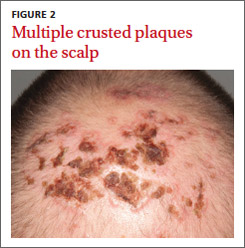
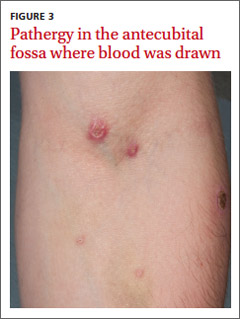
Physical examination revealed 2 large inflammatory necrotic ulcers on his palate and right tonsil, with multiple small ulcers on the border of his tongue (FIGURE 1). Skin examination revealed scattered crateriform ulcerated plaques—particularly over his forearms, back, and scalp (FIGURE 2). Genital examination revealed a large necrotic ulcer underneath his glans penis, with several satellite perigenital ulcers in the groin. Examination of the antecubital fossa revealed pathergy from a blood test and intravenous cannula (FIGURE 3). There was no ocular involvement.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Behçet’s disease
We diagnosed Behçet’s disease (BD) in this patient based on his clinical presentation.
BD was first described by Hulushi Behçet in 1937 as a triad of oral ulcers, genital ulcers, and uveitis.1 BD is a rare multisystem inflammatory disorder of unknown cause and is prevalent along the Silk Road, an ancient trade route from the Far East to the Mediterranean.
The prevalence is highest in Turkey (80-370/100,000 people) and <1/100,000 people in the United Kingdom and United States.2 Research suggests that the HLA-B*501 allele contributes to the risk of BD in places where the disease is prevalent, but not in Western countries.2
The development of ulceration at the site of superficial skin injury is typical of BD and is termed pathergy. Before he was referred to us, he had had multiple venipunctures while being investigated for a presumed infective illness.
Consider these conditions in the differential
The differential diagnosis includes erythema multiforme, herpes simplex, and Crohn’s disease.
Erythema multiforme is a type of hypersensitivity reaction that commonly occurs in response to infections such as herpes simplex and mycoplasma or medications such as barbiturates or penicillins. It often is diagnosed by the appearance of targetoid skin lesions.
Herpes simplex usually presents with grouped vesicles on an erythematous base and the diagnosis can be confirmed by virology; it responds to antiviral medication.
Crohn’s disease patients may develop abscesses and ulcers in the perineal/perianal region, but they will primarily complain of crampy abdominal pain, loss of appetite, weight loss, and bloody diarrhea.
No lab test to turn to
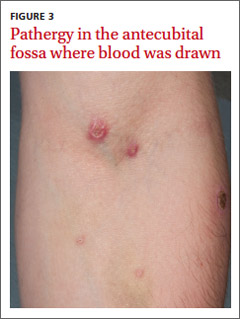
There are no diagnostic laboratory tests for BD; laboratory findings usually reflect systemic inflammation. The International Study Group for BD, however, has derived classification criteria for use in clinical research studies (TABLE).3
Recurrent mouth ulcers—which our patient reported—are essential for the diagnosis of BD. There are typically several such ulcers at any given time and they frequently involve the soft palate and oropharynx. Genital ulceration is the second most common manifestation of BD and is present in 57% to 93% of patients.4 The scrotum is most commonly involved, although the shaft and glans penis may also be affected. Ulcers in the groin and perineum also occur.
Ocular involvement is seen in 30% to 70% of patients and is more frequent and severe in men.5 Panuveitis, posterior uveitis, anterior uveitis, retinal vasculitis, optic neuritis, and retinal vein occlusion cause significant morbidity.
It is induced by a needle prick or injection and is associated with a papule or pustule on an erythematous base. A positive test is defined as a lesion that arises within 24 to 48 hours of the needle prick.
Treatment focuses on alleviating symptoms
There is no curative treatment for BD. The goals of treatment are to prevent end organ damage and alleviate the symptoms.
Mucocutaneous disease is treated with potent topical corticosteroids. Severe attacks are treated with oral corticosteroids—1 mg/kg of prednisolone.7 The drug is tapered and discontinued once the disease is under control. Colchicine or dapsone also is an option. In refractory cases, consider thalidomide (50 mg once a day) or azathioprine (1-3 mg/kg).2,7 An anti-tumor necrosis factor agent also may be considered.
A good outcome for our patient
Our patient was evaluated by an ophthalmology colleague who found no evidence of ocular involvement.
We initially prescribed prednisolone 60 mg once a day for this patient, but when he was weaned off of it, he relapsed. We then prescribed thalidomide 50 mg once a day for 4 months, and the disease resolved completely. The thalidomide was then reduced to 50 mg 3 times a week for 4 weeks, and then stopped completely.
Nearly 2 years later, our patient remains disease free.
CORRESPONDENCE
Arif Aslam, MBChB, MRCP (UK), Salford Royal NHS Foundation Trust, Stott Lane, Salford, Manchester M6 8HD United Kingdom; a.aslam@doctors.org.uk
1. Behçet H. Über rezidivierende, aphthöse, durch ein Virus verursachte Geschwüre am Mund, am Auge und an den Genitalien. Dermatol Wochenschr. 1937;36:1152-1157.
2. Sakane T, Takeno M, Suzuki N, et al. Behçet’s disease. N Engl J Med. 1999;341:1284-1291.
3. Criteria for the diagnosis of Behçet’s disease. International Study Group for Behçet’s disease. Lancet. 1990;335:1078-1080.
4. Zouboulis CC. Epidemiology of Adamantiades-Behçet’s disease. Ann Med Interne (Paris). 1999;150:488-498.
5. Kaçmaz RO, Kempen JH, Newcomb C, et al; Systemic Immunosuppressive Therapy for Eye Diseases Cohort Study Group. Ocular inflammation in Behçet’s disease: incidence of ocular complications and of loss of visual acuity. Am J Ophthalmol. 2008;146:828-836.
6. Baker MR, Smith EV, Seidi OA. Pathergy test. Pract Neurol. 2011;11:301-302.
7. Dalvi SR, Yildirim R, Yazici Y. Behcet’s syndrome. Drugs. 2012;72:2223-2241.
A 36-year-old Caucasian man sought care at our facility for rapidly progressive painful ulcers that were affecting his throat, tongue, genital area, and other parts of his body. He said that the lesions erupted 6 days earlier, and indicated that he had a history of recurrent oral aphthous ulcers.
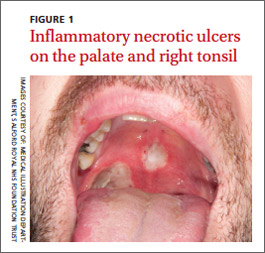
Physical examination revealed 2 large inflammatory necrotic ulcers on his palate and right tonsil, with multiple small ulcers on the border of his tongue (FIGURE 1). Skin examination revealed scattered crateriform ulcerated plaques—particularly over his forearms, back, and scalp (FIGURE 2). Genital examination revealed a large necrotic ulcer underneath his glans penis, with several satellite perigenital ulcers in the groin. Examination of the antecubital fossa revealed pathergy from a blood test and intravenous cannula (FIGURE 3). There was no ocular involvement.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Behçet’s disease
We diagnosed Behçet’s disease (BD) in this patient based on his clinical presentation.
BD was first described by Hulushi Behçet in 1937 as a triad of oral ulcers, genital ulcers, and uveitis.1 BD is a rare multisystem inflammatory disorder of unknown cause and is prevalent along the Silk Road, an ancient trade route from the Far East to the Mediterranean.
The prevalence is highest in Turkey (80-370/100,000 people) and <1/100,000 people in the United Kingdom and United States.2 Research suggests that the HLA-B*501 allele contributes to the risk of BD in places where the disease is prevalent, but not in Western countries.2
The development of ulceration at the site of superficial skin injury is typical of BD and is termed pathergy. Before he was referred to us, he had had multiple venipunctures while being investigated for a presumed infective illness.
Consider these conditions in the differential
The differential diagnosis includes erythema multiforme, herpes simplex, and Crohn’s disease.
Erythema multiforme is a type of hypersensitivity reaction that commonly occurs in response to infections such as herpes simplex and mycoplasma or medications such as barbiturates or penicillins. It often is diagnosed by the appearance of targetoid skin lesions.
Herpes simplex usually presents with grouped vesicles on an erythematous base and the diagnosis can be confirmed by virology; it responds to antiviral medication.
Crohn’s disease patients may develop abscesses and ulcers in the perineal/perianal region, but they will primarily complain of crampy abdominal pain, loss of appetite, weight loss, and bloody diarrhea.
No lab test to turn to
There are no diagnostic laboratory tests for BD; laboratory findings usually reflect systemic inflammation. The International Study Group for BD, however, has derived classification criteria for use in clinical research studies (TABLE).3
Recurrent mouth ulcers—which our patient reported—are essential for the diagnosis of BD. There are typically several such ulcers at any given time and they frequently involve the soft palate and oropharynx. Genital ulceration is the second most common manifestation of BD and is present in 57% to 93% of patients.4 The scrotum is most commonly involved, although the shaft and glans penis may also be affected. Ulcers in the groin and perineum also occur.
Ocular involvement is seen in 30% to 70% of patients and is more frequent and severe in men.5 Panuveitis, posterior uveitis, anterior uveitis, retinal vasculitis, optic neuritis, and retinal vein occlusion cause significant morbidity.
It is induced by a needle prick or injection and is associated with a papule or pustule on an erythematous base. A positive test is defined as a lesion that arises within 24 to 48 hours of the needle prick.
Treatment focuses on alleviating symptoms
There is no curative treatment for BD. The goals of treatment are to prevent end organ damage and alleviate the symptoms.
Mucocutaneous disease is treated with potent topical corticosteroids. Severe attacks are treated with oral corticosteroids—1 mg/kg of prednisolone.7 The drug is tapered and discontinued once the disease is under control. Colchicine or dapsone also is an option. In refractory cases, consider thalidomide (50 mg once a day) or azathioprine (1-3 mg/kg).2,7 An anti-tumor necrosis factor agent also may be considered.
A good outcome for our patient
Our patient was evaluated by an ophthalmology colleague who found no evidence of ocular involvement.
We initially prescribed prednisolone 60 mg once a day for this patient, but when he was weaned off of it, he relapsed. We then prescribed thalidomide 50 mg once a day for 4 months, and the disease resolved completely. The thalidomide was then reduced to 50 mg 3 times a week for 4 weeks, and then stopped completely.
Nearly 2 years later, our patient remains disease free.
CORRESPONDENCE
Arif Aslam, MBChB, MRCP (UK), Salford Royal NHS Foundation Trust, Stott Lane, Salford, Manchester M6 8HD United Kingdom; a.aslam@doctors.org.uk
A 36-year-old Caucasian man sought care at our facility for rapidly progressive painful ulcers that were affecting his throat, tongue, genital area, and other parts of his body. He said that the lesions erupted 6 days earlier, and indicated that he had a history of recurrent oral aphthous ulcers.
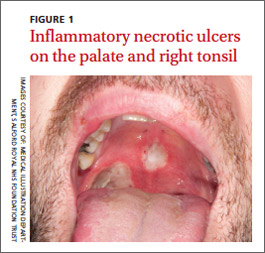
Physical examination revealed 2 large inflammatory necrotic ulcers on his palate and right tonsil, with multiple small ulcers on the border of his tongue (FIGURE 1). Skin examination revealed scattered crateriform ulcerated plaques—particularly over his forearms, back, and scalp (FIGURE 2). Genital examination revealed a large necrotic ulcer underneath his glans penis, with several satellite perigenital ulcers in the groin. Examination of the antecubital fossa revealed pathergy from a blood test and intravenous cannula (FIGURE 3). There was no ocular involvement.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Behçet’s disease
We diagnosed Behçet’s disease (BD) in this patient based on his clinical presentation.
BD was first described by Hulushi Behçet in 1937 as a triad of oral ulcers, genital ulcers, and uveitis.1 BD is a rare multisystem inflammatory disorder of unknown cause and is prevalent along the Silk Road, an ancient trade route from the Far East to the Mediterranean.
The prevalence is highest in Turkey (80-370/100,000 people) and <1/100,000 people in the United Kingdom and United States.2 Research suggests that the HLA-B*501 allele contributes to the risk of BD in places where the disease is prevalent, but not in Western countries.2
The development of ulceration at the site of superficial skin injury is typical of BD and is termed pathergy. Before he was referred to us, he had had multiple venipunctures while being investigated for a presumed infective illness.
Consider these conditions in the differential
The differential diagnosis includes erythema multiforme, herpes simplex, and Crohn’s disease.
Erythema multiforme is a type of hypersensitivity reaction that commonly occurs in response to infections such as herpes simplex and mycoplasma or medications such as barbiturates or penicillins. It often is diagnosed by the appearance of targetoid skin lesions.
Herpes simplex usually presents with grouped vesicles on an erythematous base and the diagnosis can be confirmed by virology; it responds to antiviral medication.
Crohn’s disease patients may develop abscesses and ulcers in the perineal/perianal region, but they will primarily complain of crampy abdominal pain, loss of appetite, weight loss, and bloody diarrhea.
No lab test to turn to
There are no diagnostic laboratory tests for BD; laboratory findings usually reflect systemic inflammation. The International Study Group for BD, however, has derived classification criteria for use in clinical research studies (TABLE).3
Recurrent mouth ulcers—which our patient reported—are essential for the diagnosis of BD. There are typically several such ulcers at any given time and they frequently involve the soft palate and oropharynx. Genital ulceration is the second most common manifestation of BD and is present in 57% to 93% of patients.4 The scrotum is most commonly involved, although the shaft and glans penis may also be affected. Ulcers in the groin and perineum also occur.
Ocular involvement is seen in 30% to 70% of patients and is more frequent and severe in men.5 Panuveitis, posterior uveitis, anterior uveitis, retinal vasculitis, optic neuritis, and retinal vein occlusion cause significant morbidity.
It is induced by a needle prick or injection and is associated with a papule or pustule on an erythematous base. A positive test is defined as a lesion that arises within 24 to 48 hours of the needle prick.
Treatment focuses on alleviating symptoms
There is no curative treatment for BD. The goals of treatment are to prevent end organ damage and alleviate the symptoms.
Mucocutaneous disease is treated with potent topical corticosteroids. Severe attacks are treated with oral corticosteroids—1 mg/kg of prednisolone.7 The drug is tapered and discontinued once the disease is under control. Colchicine or dapsone also is an option. In refractory cases, consider thalidomide (50 mg once a day) or azathioprine (1-3 mg/kg).2,7 An anti-tumor necrosis factor agent also may be considered.
A good outcome for our patient
Our patient was evaluated by an ophthalmology colleague who found no evidence of ocular involvement.
We initially prescribed prednisolone 60 mg once a day for this patient, but when he was weaned off of it, he relapsed. We then prescribed thalidomide 50 mg once a day for 4 months, and the disease resolved completely. The thalidomide was then reduced to 50 mg 3 times a week for 4 weeks, and then stopped completely.
Nearly 2 years later, our patient remains disease free.
CORRESPONDENCE
Arif Aslam, MBChB, MRCP (UK), Salford Royal NHS Foundation Trust, Stott Lane, Salford, Manchester M6 8HD United Kingdom; a.aslam@doctors.org.uk
1. Behçet H. Über rezidivierende, aphthöse, durch ein Virus verursachte Geschwüre am Mund, am Auge und an den Genitalien. Dermatol Wochenschr. 1937;36:1152-1157.
2. Sakane T, Takeno M, Suzuki N, et al. Behçet’s disease. N Engl J Med. 1999;341:1284-1291.
3. Criteria for the diagnosis of Behçet’s disease. International Study Group for Behçet’s disease. Lancet. 1990;335:1078-1080.
4. Zouboulis CC. Epidemiology of Adamantiades-Behçet’s disease. Ann Med Interne (Paris). 1999;150:488-498.
5. Kaçmaz RO, Kempen JH, Newcomb C, et al; Systemic Immunosuppressive Therapy for Eye Diseases Cohort Study Group. Ocular inflammation in Behçet’s disease: incidence of ocular complications and of loss of visual acuity. Am J Ophthalmol. 2008;146:828-836.
6. Baker MR, Smith EV, Seidi OA. Pathergy test. Pract Neurol. 2011;11:301-302.
7. Dalvi SR, Yildirim R, Yazici Y. Behcet’s syndrome. Drugs. 2012;72:2223-2241.
1. Behçet H. Über rezidivierende, aphthöse, durch ein Virus verursachte Geschwüre am Mund, am Auge und an den Genitalien. Dermatol Wochenschr. 1937;36:1152-1157.
2. Sakane T, Takeno M, Suzuki N, et al. Behçet’s disease. N Engl J Med. 1999;341:1284-1291.
3. Criteria for the diagnosis of Behçet’s disease. International Study Group for Behçet’s disease. Lancet. 1990;335:1078-1080.
4. Zouboulis CC. Epidemiology of Adamantiades-Behçet’s disease. Ann Med Interne (Paris). 1999;150:488-498.
5. Kaçmaz RO, Kempen JH, Newcomb C, et al; Systemic Immunosuppressive Therapy for Eye Diseases Cohort Study Group. Ocular inflammation in Behçet’s disease: incidence of ocular complications and of loss of visual acuity. Am J Ophthalmol. 2008;146:828-836.
6. Baker MR, Smith EV, Seidi OA. Pathergy test. Pract Neurol. 2011;11:301-302.
7. Dalvi SR, Yildirim R, Yazici Y. Behcet’s syndrome. Drugs. 2012;72:2223-2241.