User login
A 62-year-old man presented to the emergency department (ED) with a swollen, red, and painful right lower leg. He’d had bilateral lower leg swelling for 2 months, but the left leg became increasingly painful and red over the past 3 days. The patient also had a 3-day history of a diffuse rash that began on his right upper arm and spread to his left arm, both palms, both legs, and his back. It was mildly pruritic, but not painful.
The patient indicated that he had recently sought care from his primary care physician for lower respiratory symptoms. He had just completed a 5-day course of azithromycin and prednisone (50 mg/d for 5 days) the day before his ED visit.
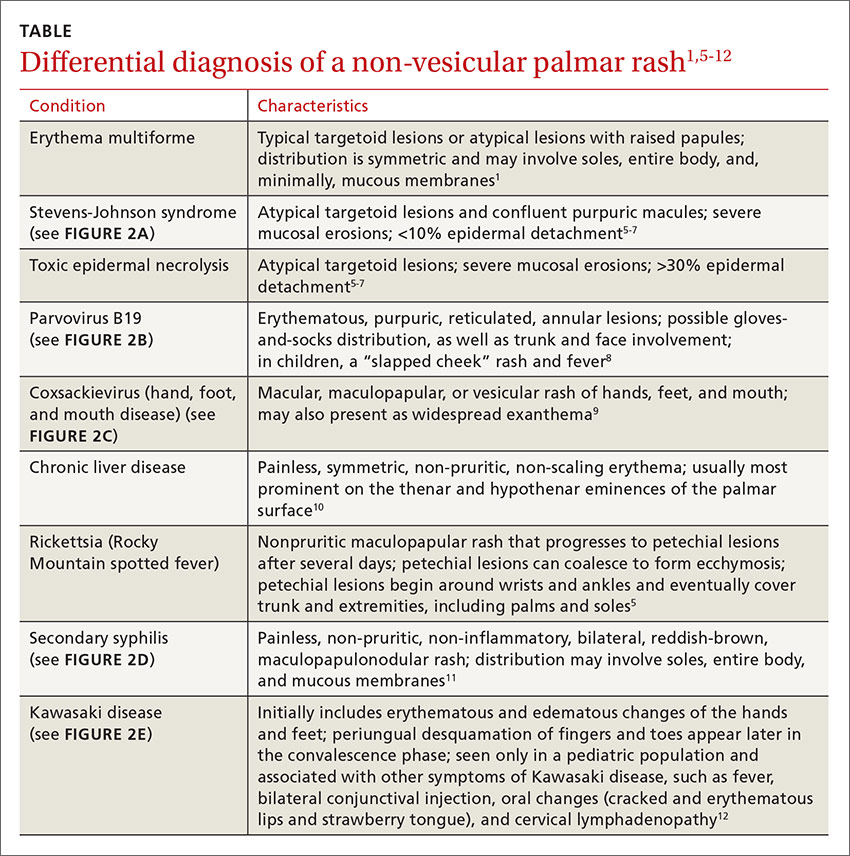
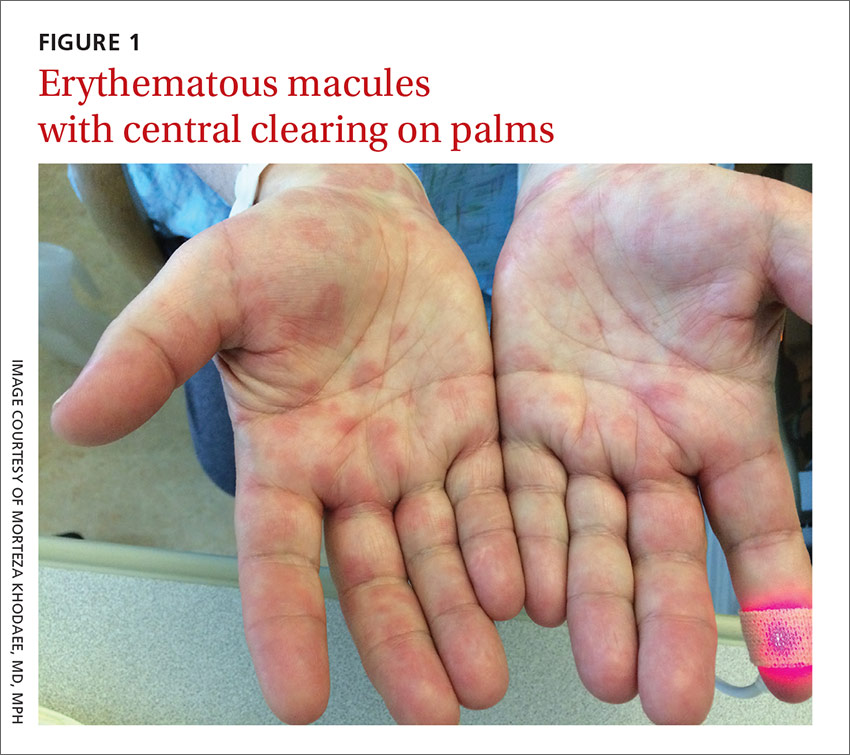
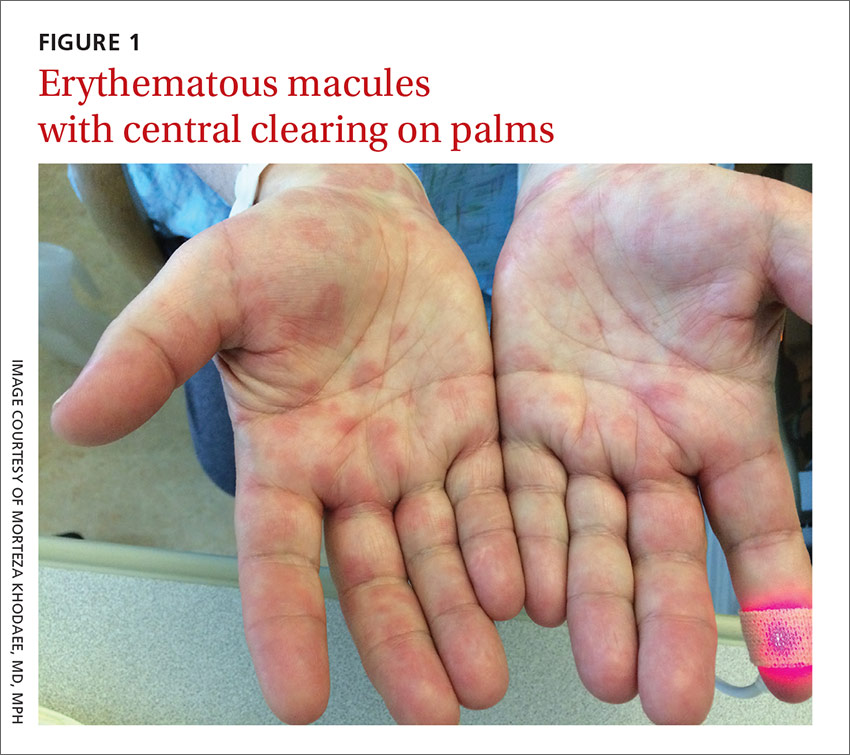
A lower extremity venous ultrasound revealed that the patient had a deep vein thrombosis (DVT). Computed tomography (CT) imaging of the chest with contrast revealed pulmonary emboli. He was treated with enoxaparin and warfarin. We diagnosed the rash based on the patient’s history and the appearance of the rash, which was comprised of blanching and erythematous macules with central clearing (FIGURE 1). (There were no blisters or mucosal involvement.)
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Erythema multiforme
The clinical exam was consistent with the diagnosis of erythema multiforme (EM). A diagnosis of EM can usually be made based on the clinical exam alone.1 Typical targetoid lesions have a round shape and 3 concentric zones: A central dusky area of epidermal necrosis that may involve bullae, a paler pink or edematous zone, and a peripheral erythematous ring.2 Atypical lesions, such as raised papules, may also be seen.2
The skin lesions of EM usually appear symmetrically on the distal extremities and spread in a centripetal manner.1 Palms, soles, and mucosa can be involved.1 EM with mucosal involvement is called “erythema multiforme major,” and EM without mucosal disease (as in our patient’s case) is called “erythema multiforme minor.”2
EM is an acute, immune-mediated eruption thought to be caused by a cell-mediated hypersensitivity to certain infections or drugs.2 Ninety percent of cases are associated with an infection; herpes simplex virus (HSV) is the most common infectious agent.3 Mycoplasma pneumoniae is another culprit, especially in children. Medications are inciting factors about 10% of the time; nonsteroidal anti-inflammatory drugs, sulfonamides, antiepileptics, and antibiotics have been linked to EM eruptions.3
Interestingly, while azithromycin—the medication our patient had taken most recently—can cause EM, it has been mainly linked to cases of Stevens-Johnson syndrome (SJS).4 So, while we suspect that azithromycin was the trigger in our patient’s case, we can’t be sure. It’s also possible that Mycoplasma pneumoniae was the trigger for our patient’s EM. However, Mycoplasma pneumoniae is more common in adolescents.
Differential includes life-threatening conditions like SJS
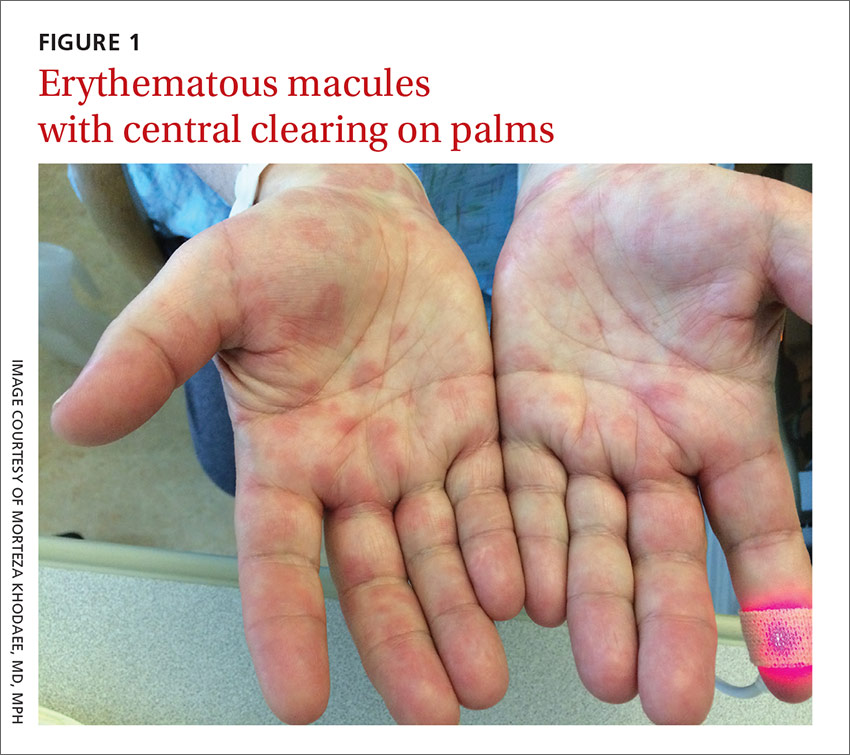
The differential diagnosis for a non-vesicular palmar rash is discussed in the TABLE.1,5-12 There is a wide spectrum of possible etiologies—from infectious and rheumatologic disorders to chronic liver disease. Histologic testing may be useful in differentiating EM from other diseases, but in most cases, it is not required to make a diagnosis.1 Laboratory testing may reveal leukocytosis, an elevated erythrocyte sedimentation rate, and elevated liver function test results, but these are nonspecific.1
It’s important to differentiate EM from life-threatening conditions like SJS and toxic epidermal necrolysis (TEN).5 EM is characterized by typical and atypical targetoid lesions with minimal mucosal involvement.6,7 SJS is characterized by flat atypical targetoid lesions, confluent purpuric macules, severe mucosal erosions, and <10% epidermal detachment.6,7 TEN is characterized by severe mucosal erosions and >30% epidermal detachment.6,7

Lesions resolve on their own, but topical steroids can provide relief
EM is a self-limiting disease; lesions resolve within about 2 weeks.3 Management begins by treating any suspected infection or discontinuing any suspected drugs.1 In patients with co-existing or recurrent HSV infection, early treatment with an oral antiviral (such as acyclovir) may lessen the number and duration of lesions.1,6 In addition, oral antihistamines and topical steroids may be used to provide symptomatic relief.1,6 Use of oral corticosteroids can be considered in severe mucosal disease, although such use is considered controversial due to a lack of evidence.1,6
Our patient remained hospitalized for 4 days. As noted earlier, his DVT and pulmonary embolism were treated with enoxaparin and the patient was sent home with a prescription for warfarin. Regarding the EM, his rash and itching
CORRESPONDENCE
Morteza Khodaee, MD, MPH, AFW Clinic, 3055 Roslyn Street, Denver, Colorado 80238; morteza.khodaee@ucdenver.edu.
1. Lamoreux MR, Sternbach MR, Hsu WT. Erythema multiforme. Am Fam Physician. 2006;74:1883-1888.
2. Patel NN, Patel DN. Erythema multiforme syndrome. Am J Med. 2009;122:623-625.
3. Sokumbi O, Wetter DA. Clinical features, diagnosis, and treatment of erythema multiforme: a review for the practicing dermatologist. Int J Dermatol. 2012;51:889-902.
4. Nambudiri VE. More than skin deep—the costs of antibiotic overuse: a teachable moment. JAMA Intern Med. 2014;174:1724-1725.
5. Usatine RP, Sandy N. Dermatologic emergencies. Am Fam Physician. 2010;82:773-780.
6. Al-Johani KA, Fedele S, Porter SR. Erythema multiforme andrelated disorders. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103:642-654.
7. Assier H, Bastuji-Garin S, Revuz J, et al. Erythema multiforme with mucous membrane involvement and Stevens-Johnson syndrome are clinically different disorders with distinct causes. Arch Dermatol. 1995;131:539-543.
8. Mage V, Lipsker D, Barbarot S, et al. Different patterns of skin manifestations associated with parvovirus B19 primary infection in adults. J Am Acad Dermatol. 2014;71:62-69.
9. Hubiche T, Schuffenecker I, Boralevi F, et al; Clinical Research Group of the French Society of Pediatric Dermatology Groupe de Recherche Clinique de la Société Française de Dermatologie Pédiatrique. Dermatological spectrum of hand, foot and mouth disease from classical to generalized exanthema. Pediatr Infect Dis J. 2014;33:e92-e98.
10. Serrao R, Zirwas M, English JC. Palmar erythema. Am J Clin Dermatol. 2007;8:347-356.
11. Meffert JJ. Photo quiz. A palmar rash. Am Fam Physician. 1999;59:1259-1260.
12. Saguil A, Fargo M, Grogan S. Diagnosis and management of Kawasaki disease. Am Fam Physician. 2015;91:365-371.
A 62-year-old man presented to the emergency department (ED) with a swollen, red, and painful right lower leg. He’d had bilateral lower leg swelling for 2 months, but the left leg became increasingly painful and red over the past 3 days. The patient also had a 3-day history of a diffuse rash that began on his right upper arm and spread to his left arm, both palms, both legs, and his back. It was mildly pruritic, but not painful.
The patient indicated that he had recently sought care from his primary care physician for lower respiratory symptoms. He had just completed a 5-day course of azithromycin and prednisone (50 mg/d for 5 days) the day before his ED visit.
A lower extremity venous ultrasound revealed that the patient had a deep vein thrombosis (DVT). Computed tomography (CT) imaging of the chest with contrast revealed pulmonary emboli. He was treated with enoxaparin and warfarin. We diagnosed the rash based on the patient’s history and the appearance of the rash, which was comprised of blanching and erythematous macules with central clearing (FIGURE 1). (There were no blisters or mucosal involvement.)
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Erythema multiforme
The clinical exam was consistent with the diagnosis of erythema multiforme (EM). A diagnosis of EM can usually be made based on the clinical exam alone.1 Typical targetoid lesions have a round shape and 3 concentric zones: A central dusky area of epidermal necrosis that may involve bullae, a paler pink or edematous zone, and a peripheral erythematous ring.2 Atypical lesions, such as raised papules, may also be seen.2
The skin lesions of EM usually appear symmetrically on the distal extremities and spread in a centripetal manner.1 Palms, soles, and mucosa can be involved.1 EM with mucosal involvement is called “erythema multiforme major,” and EM without mucosal disease (as in our patient’s case) is called “erythema multiforme minor.”2
EM is an acute, immune-mediated eruption thought to be caused by a cell-mediated hypersensitivity to certain infections or drugs.2 Ninety percent of cases are associated with an infection; herpes simplex virus (HSV) is the most common infectious agent.3 Mycoplasma pneumoniae is another culprit, especially in children. Medications are inciting factors about 10% of the time; nonsteroidal anti-inflammatory drugs, sulfonamides, antiepileptics, and antibiotics have been linked to EM eruptions.3
Interestingly, while azithromycin—the medication our patient had taken most recently—can cause EM, it has been mainly linked to cases of Stevens-Johnson syndrome (SJS).4 So, while we suspect that azithromycin was the trigger in our patient’s case, we can’t be sure. It’s also possible that Mycoplasma pneumoniae was the trigger for our patient’s EM. However, Mycoplasma pneumoniae is more common in adolescents.
Differential includes life-threatening conditions like SJS
The differential diagnosis for a non-vesicular palmar rash is discussed in the TABLE.1,5-12 There is a wide spectrum of possible etiologies—from infectious and rheumatologic disorders to chronic liver disease. Histologic testing may be useful in differentiating EM from other diseases, but in most cases, it is not required to make a diagnosis.1 Laboratory testing may reveal leukocytosis, an elevated erythrocyte sedimentation rate, and elevated liver function test results, but these are nonspecific.1
It’s important to differentiate EM from life-threatening conditions like SJS and toxic epidermal necrolysis (TEN).5 EM is characterized by typical and atypical targetoid lesions with minimal mucosal involvement.6,7 SJS is characterized by flat atypical targetoid lesions, confluent purpuric macules, severe mucosal erosions, and <10% epidermal detachment.6,7 TEN is characterized by severe mucosal erosions and >30% epidermal detachment.6,7

Lesions resolve on their own, but topical steroids can provide relief
EM is a self-limiting disease; lesions resolve within about 2 weeks.3 Management begins by treating any suspected infection or discontinuing any suspected drugs.1 In patients with co-existing or recurrent HSV infection, early treatment with an oral antiviral (such as acyclovir) may lessen the number and duration of lesions.1,6 In addition, oral antihistamines and topical steroids may be used to provide symptomatic relief.1,6 Use of oral corticosteroids can be considered in severe mucosal disease, although such use is considered controversial due to a lack of evidence.1,6
Our patient remained hospitalized for 4 days. As noted earlier, his DVT and pulmonary embolism were treated with enoxaparin and the patient was sent home with a prescription for warfarin. Regarding the EM, his rash and itching
CORRESPONDENCE
Morteza Khodaee, MD, MPH, AFW Clinic, 3055 Roslyn Street, Denver, Colorado 80238; morteza.khodaee@ucdenver.edu.
A 62-year-old man presented to the emergency department (ED) with a swollen, red, and painful right lower leg. He’d had bilateral lower leg swelling for 2 months, but the left leg became increasingly painful and red over the past 3 days. The patient also had a 3-day history of a diffuse rash that began on his right upper arm and spread to his left arm, both palms, both legs, and his back. It was mildly pruritic, but not painful.
The patient indicated that he had recently sought care from his primary care physician for lower respiratory symptoms. He had just completed a 5-day course of azithromycin and prednisone (50 mg/d for 5 days) the day before his ED visit.
A lower extremity venous ultrasound revealed that the patient had a deep vein thrombosis (DVT). Computed tomography (CT) imaging of the chest with contrast revealed pulmonary emboli. He was treated with enoxaparin and warfarin. We diagnosed the rash based on the patient’s history and the appearance of the rash, which was comprised of blanching and erythematous macules with central clearing (FIGURE 1). (There were no blisters or mucosal involvement.)
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Erythema multiforme
The clinical exam was consistent with the diagnosis of erythema multiforme (EM). A diagnosis of EM can usually be made based on the clinical exam alone.1 Typical targetoid lesions have a round shape and 3 concentric zones: A central dusky area of epidermal necrosis that may involve bullae, a paler pink or edematous zone, and a peripheral erythematous ring.2 Atypical lesions, such as raised papules, may also be seen.2
The skin lesions of EM usually appear symmetrically on the distal extremities and spread in a centripetal manner.1 Palms, soles, and mucosa can be involved.1 EM with mucosal involvement is called “erythema multiforme major,” and EM without mucosal disease (as in our patient’s case) is called “erythema multiforme minor.”2
EM is an acute, immune-mediated eruption thought to be caused by a cell-mediated hypersensitivity to certain infections or drugs.2 Ninety percent of cases are associated with an infection; herpes simplex virus (HSV) is the most common infectious agent.3 Mycoplasma pneumoniae is another culprit, especially in children. Medications are inciting factors about 10% of the time; nonsteroidal anti-inflammatory drugs, sulfonamides, antiepileptics, and antibiotics have been linked to EM eruptions.3
Interestingly, while azithromycin—the medication our patient had taken most recently—can cause EM, it has been mainly linked to cases of Stevens-Johnson syndrome (SJS).4 So, while we suspect that azithromycin was the trigger in our patient’s case, we can’t be sure. It’s also possible that Mycoplasma pneumoniae was the trigger for our patient’s EM. However, Mycoplasma pneumoniae is more common in adolescents.
Differential includes life-threatening conditions like SJS
The differential diagnosis for a non-vesicular palmar rash is discussed in the TABLE.1,5-12 There is a wide spectrum of possible etiologies—from infectious and rheumatologic disorders to chronic liver disease. Histologic testing may be useful in differentiating EM from other diseases, but in most cases, it is not required to make a diagnosis.1 Laboratory testing may reveal leukocytosis, an elevated erythrocyte sedimentation rate, and elevated liver function test results, but these are nonspecific.1
It’s important to differentiate EM from life-threatening conditions like SJS and toxic epidermal necrolysis (TEN).5 EM is characterized by typical and atypical targetoid lesions with minimal mucosal involvement.6,7 SJS is characterized by flat atypical targetoid lesions, confluent purpuric macules, severe mucosal erosions, and <10% epidermal detachment.6,7 TEN is characterized by severe mucosal erosions and >30% epidermal detachment.6,7

Lesions resolve on their own, but topical steroids can provide relief
EM is a self-limiting disease; lesions resolve within about 2 weeks.3 Management begins by treating any suspected infection or discontinuing any suspected drugs.1 In patients with co-existing or recurrent HSV infection, early treatment with an oral antiviral (such as acyclovir) may lessen the number and duration of lesions.1,6 In addition, oral antihistamines and topical steroids may be used to provide symptomatic relief.1,6 Use of oral corticosteroids can be considered in severe mucosal disease, although such use is considered controversial due to a lack of evidence.1,6
Our patient remained hospitalized for 4 days. As noted earlier, his DVT and pulmonary embolism were treated with enoxaparin and the patient was sent home with a prescription for warfarin. Regarding the EM, his rash and itching
CORRESPONDENCE
Morteza Khodaee, MD, MPH, AFW Clinic, 3055 Roslyn Street, Denver, Colorado 80238; morteza.khodaee@ucdenver.edu.
1. Lamoreux MR, Sternbach MR, Hsu WT. Erythema multiforme. Am Fam Physician. 2006;74:1883-1888.
2. Patel NN, Patel DN. Erythema multiforme syndrome. Am J Med. 2009;122:623-625.
3. Sokumbi O, Wetter DA. Clinical features, diagnosis, and treatment of erythema multiforme: a review for the practicing dermatologist. Int J Dermatol. 2012;51:889-902.
4. Nambudiri VE. More than skin deep—the costs of antibiotic overuse: a teachable moment. JAMA Intern Med. 2014;174:1724-1725.
5. Usatine RP, Sandy N. Dermatologic emergencies. Am Fam Physician. 2010;82:773-780.
6. Al-Johani KA, Fedele S, Porter SR. Erythema multiforme andrelated disorders. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103:642-654.
7. Assier H, Bastuji-Garin S, Revuz J, et al. Erythema multiforme with mucous membrane involvement and Stevens-Johnson syndrome are clinically different disorders with distinct causes. Arch Dermatol. 1995;131:539-543.
8. Mage V, Lipsker D, Barbarot S, et al. Different patterns of skin manifestations associated with parvovirus B19 primary infection in adults. J Am Acad Dermatol. 2014;71:62-69.
9. Hubiche T, Schuffenecker I, Boralevi F, et al; Clinical Research Group of the French Society of Pediatric Dermatology Groupe de Recherche Clinique de la Société Française de Dermatologie Pédiatrique. Dermatological spectrum of hand, foot and mouth disease from classical to generalized exanthema. Pediatr Infect Dis J. 2014;33:e92-e98.
10. Serrao R, Zirwas M, English JC. Palmar erythema. Am J Clin Dermatol. 2007;8:347-356.
11. Meffert JJ. Photo quiz. A palmar rash. Am Fam Physician. 1999;59:1259-1260.
12. Saguil A, Fargo M, Grogan S. Diagnosis and management of Kawasaki disease. Am Fam Physician. 2015;91:365-371.
1. Lamoreux MR, Sternbach MR, Hsu WT. Erythema multiforme. Am Fam Physician. 2006;74:1883-1888.
2. Patel NN, Patel DN. Erythema multiforme syndrome. Am J Med. 2009;122:623-625.
3. Sokumbi O, Wetter DA. Clinical features, diagnosis, and treatment of erythema multiforme: a review for the practicing dermatologist. Int J Dermatol. 2012;51:889-902.
4. Nambudiri VE. More than skin deep—the costs of antibiotic overuse: a teachable moment. JAMA Intern Med. 2014;174:1724-1725.
5. Usatine RP, Sandy N. Dermatologic emergencies. Am Fam Physician. 2010;82:773-780.
6. Al-Johani KA, Fedele S, Porter SR. Erythema multiforme andrelated disorders. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103:642-654.
7. Assier H, Bastuji-Garin S, Revuz J, et al. Erythema multiforme with mucous membrane involvement and Stevens-Johnson syndrome are clinically different disorders with distinct causes. Arch Dermatol. 1995;131:539-543.
8. Mage V, Lipsker D, Barbarot S, et al. Different patterns of skin manifestations associated with parvovirus B19 primary infection in adults. J Am Acad Dermatol. 2014;71:62-69.
9. Hubiche T, Schuffenecker I, Boralevi F, et al; Clinical Research Group of the French Society of Pediatric Dermatology Groupe de Recherche Clinique de la Société Française de Dermatologie Pédiatrique. Dermatological spectrum of hand, foot and mouth disease from classical to generalized exanthema. Pediatr Infect Dis J. 2014;33:e92-e98.
10. Serrao R, Zirwas M, English JC. Palmar erythema. Am J Clin Dermatol. 2007;8:347-356.
11. Meffert JJ. Photo quiz. A palmar rash. Am Fam Physician. 1999;59:1259-1260.
12. Saguil A, Fargo M, Grogan S. Diagnosis and management of Kawasaki disease. Am Fam Physician. 2015;91:365-371.