User login
An estimated 1% to 2% of patients with chronic hypertension will at some time develop hypertensive urgency or emergency.1 According to recent data from the National Health and Nutrition Examination Survey (NHANES) 1999 to 2010,2 the prevalence of hypertension has remained stable at 30.5% among men and 28.5% among women in the United States; however, 74% of the hypertensive population is unaware of having this condition. Furthermore, 71.6% of hypertensive patients are managed for the condition, and in only 46.5% is blood pressure well controlled.2
In 2006, essential hypertension was estimated to account for more than 44 million emergency department visits in the US. The direct and indirect costs of hypertension totaled $73 billion in 2009.3,4
NEW TERMINOLOGY AND CLASSIFICATION
The terms malignant hypertension, hypertensive crisis, and accelerated hypertension have been replaced by hypertensive urgency or hypertensive emergency. Hypertensive urgency and emergency are differentiated by the absence or presence of acute end-organ damage, respectively.
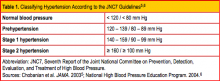
Given the inconsistent terminology used, database searches can be challenging. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC7),5,6 published in 2003, is considered the gold standard for categorizing hypertension in the outpatient setting. The JNC7 authorsclassify normal blood pressure as < 120/< 80 mm Hg. The document further classifies blood pressure into the stages shown in Table 1.5,6 Blood pressure higher than 180 mm Hg systolic and/or 120 mm Hg diastolic is generally considered severe hypertension— a designation that includes hypertensive urgency and hypertensive emergency.6
What Defines Hypertensive Urgency/Emergency?
Hypertensive urgency is defined as a diastolic blood pressure of 110 mm Hg or greater without the acute signs of end-organ damage.7 Some sources suggest that a patient must also have certain risk factors (eg, heart disease, renal disease) to be given this diagnosis.8 The presence of acute and rapidly evolving end-organ damage with an elevated diastolic blood pressure, usually greater than 120 mm Hg, establishes a diagnosis of hypertensive emergency.6,8,9
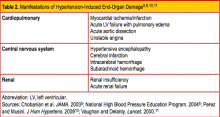
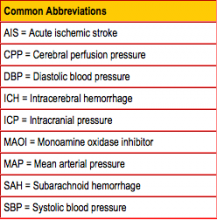
No specific blood pressure measurement indicates a hypertensive emergency, however; rather, the defining feature of this diagnosis is the presence of progressive target end-organ damage.7 This is most commonly manifested in cardiopulmonary, central nervous system, and/or renal findings; for the specific forms of end-organ damage, see Table 2.5,6,10,11 Preeclampsia and eclampsia are also considered manifestations of hypertensive end-organ damage but are beyond the scope of this article.5,11
The most common form of organ damage associated with hypertension is ischemic heart disease, in the form of either heart failure or acute coronary syndrome.12
PATHOPHYSIOLOGY
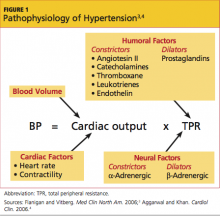
Blood pressure is calculated by cardiac output (ie, stroke volume multiplied by heart rate) multiplied by total peripheral resistance. Total peripheral resistance is influenced by a variety of humoral and neural factors, also known as vasoactive substances (see Figure 13,4). During an episode of acute hypertension, a failure of autoregulatory function occurs, precipitated by one or more of a host of potential causes. This failure of autoregulation then leads to increased systemic vascular resistance. In the setting of end-organ damage, release of inflammatory markers ensues, which ultimately causes endovascular injury and fibrin necrosis of arterioles.4,10,11
The renin-angiotensin-aldosterone system also plays a significant role in the cascade of hypertension, stimulating decreased renal perfusion and lowering tubular sodium concentration. This in turn stimulates aldosterone to increase blood pressure by maintaining excess volume through sodium retention and potassium excretion, further potentiating the cycle of uncontrolled blood pressure.4,13,14
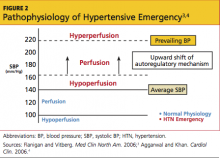
Patients with chronically elevated blood pressures have a compensatory response, lying in the threshold mechanism, that protects against end-organ damage. Acute changes in blood pressure are better tolerated in these patients because of their decreased propensity for hypoperfusion.4 In contrast, normotensive patients who experience precipitous changes in blood pressure are at increased risk for organ hypoperfusion. The main concern regarding organ hypoperfusion is that it can lead to ischemia4 (see Figure 23,4).
PATIENT HISTORY
Acute hypertensive urgency or emergency can be triggered by many factors. Systemic etiologies (including kidney disease) caused by immunologic mediators or renal artery stenosis can cause or exacerbate hypertension. The patient should be asked about his or her normal blood pressure range, as this may offer clues to medication compliance. Rebound hypertension can be seen in patients who abruptly discontinue medications such as clonidine or β-blockers, as this causes an increase in sympathetic outflow.9,15
All patients should be queried regarding their use of OTC medications and other drug use, including cocaine, methamphetamines, phencyclidine, and alcohol.1,4,11,16 Patients taking monoamine oxidase inhibitors (MAOIs) are at increased risk for serious medication interactions; concomitant administration of MAOIs with other antidepressants can lead to a hypertensive reaction, but also to serotonin syndrome.1,17 Because MAOIs inhibit the breakdown of tyramine, patients taking them should avoid tyramine-containing foods and herbal supplements (including, but not limited to, St. John's wort, ginseng, and yohimbine).1,15,18
Acute hypertensive episodes can also occur as a result of preeclampsia or eclampsia in pregnant women, pheochromocytoma, primary aldosteronism, glucocorticoid excess (Cushing syndrome), or central nervous system disorders (eg, cerebrovascular accident, head trauma, brain tumors).9,11,19
PHYSICAL EXAMINATION
The purpose of the physical examination is to determine whether end-organ damage is present.1,11 The fundoscopic exam may reveal papilledema, a sign of increased intracranial pressure (ICP). Flame hemorrhages, cotton wool spots or arteriovenous nicking suggest a long-standing history of uncontrolled hypertension or diabetes.7,9 The neck should be assessed for jugular venous distention, which may be elevated in decompensated heart failure or pulmonary edema.11
The cardiac exam may reveal an irregular rate and rhythm, displaced apical pulse, gallop, or murmur. On pulmonary exam, rales may be auscultated, suggestive of pulmonary edema.9,15
The abdominal exam should include listening for a renal artery bruit.1 The neurologic exam may demonstrate altered mental status (possibly indicating hypertensive encephalopathy) or focal findings, if the patient has had an underlying ischemic or hemorrhagic event.9
LABORATORY STUDIES AND IMAGING
In most cases, a serum chemistry panel is warranted to identify any renal dysfunction. Urinalysis may reveal proteinuria, possibly indicating renal damage.4,9,15
Any patient complaining of chest pain should have an ECG to look for ischemic changes or presence of a left bundle branch block, and serial cardiac enzymes to rule out acute coronary syndrome.15 Access to previous ECGs is helpful in differentiating between new and old conductive abnormalities.
A chest x-ray should be performed in patients who complain of shortness of breath and/or chest pain. A widened mediastinum can represent aortic dissection.4,15 Evidence of pulmonary edema should prompt the clinician to assess for left ventricular dysfunction or valvular insufficiencies by echocardiogram. Chest CT should be pursued in patients with clinical suspicion for dissection.1,15,20
Patients presenting with a headache or focal neurologic abnormalities warrant a head CT to rule out stroke.15 Urine drug screening is appropriate if the patient history suggests illicit drug use.12
"FIRST, DO NO HARM"
Treatment of hypertensive emergency and urgency varies from traditional treatment for hypertension. Aggressive blood pressure control in patients presenting with acute ischemic stroke has been associated with poorer patient outcomes.21,22 Thus, treating the patient and not the numbers is the first general recommendation for treatment of hypertensive emergency and urgency. It is important for the clinician to remember the Hippocratic oath, "First do no harm," when treating these patients.
Other general recommendations are derived from theory, physiology, and smaller clinical trials; their application must be individualized according to the patient's needs. These recommendations include aiming for a reduction in mean arterial blood pressure of no more than 10% to 25% within the first hour, a goal blood pressure of 160/90 mm Hg within the first 8 hours, and normalization of blood pressure over 8 to 24 hours.12
While the use of pharmacologic agents may be warranted, it is important to consider that elevated blood pressure may be a reaction to pain or stress and may be best treated alternatively. Recommendations for permissive hypertension in acute ischemic stroke will be discussed below.
TREATMENT: HYPERTENSIVE URGENCY
The treatment of hypertensive urgency is usually immediate and warrants close follow-up. Although elevated blood pressures can be alarming to the patient, hypertensive urgency usually develops over days to weeks.8 In this setting, it is not necessary to lower blood pressure acutely.12 A rapid decrease in blood pressure can actually cause symptomatic hypotension, resulting in hypoperfusion to the brain.5,6,8
After ruling out end-organ damage, the next step is to treat according to the guidelines for hypertensive urgency.5,6 These recommendations include the use of rapid-onset oral antihypertensive agents, such as clonidine, labetalol, or captopril.23 Use of these agents is only suggested for gradual, short-term reduction of blood pressure (ie, over 24 to 48 hours) while the patient is being monitored for potential hypertension-related organ damage, either in the emergency department or in an observational hospital setting.5,6,23
Once the short-acting agents have adequately reduced blood pressure, long-term agents can be chosen to prevent rebound hypertension.16 Patients are typically monitored for 24 hours in the hospital during this transition. Upon discharge, the patient should be scheduled for follow-up within one to two days.11 Patient education, including a discussion of medication adherence, weight loss, and reduced dietary salt, is key to prevent recurrences and optimize overall treatment compliance.
TREATMENT: HYPERTENSIVE EMERGENCY
Treatment of hypertensive emergency always warrants hospitalization, usually in the ICU.5,6 IV antihypertensive medications (eg, nicardipine, fenoldopam, labetalol, esmolol, phentolamine) are preferred. Their use often necessitates continuous blood pressure monitoring via arterial line, allowing the clinician to perform ongoing medication titration. In hypertensive emergencies, the purpose of treatment is to preserve brain, kidney, and heart function.4
Goal-directed therapy is initiated even before the patient evaluation has been fully completed. Patient assessment continues after treatment is begun to avoid overly aggressive blood pressure reduction, which can increase the risk for patient demise or morbidity.4
Exceptions in the treatment of hypertensive emergencies (particularly of specific disease states) will be discussed below, along with other treatment considerations. Patient comorbidities, for example, must be considered in the choice of antihypertensive agents.
Focused Treatment for Specific Hypertensive Emergencies
Hypertensive encephalopathy. This condition, associated with severe hypertension, is indicated by an abrupt change in mental status. During this acute end-organ damage event, a failure of cerebral autoregulation occurs, with increased pressure in the vascular endothelium leading to arteriole dilation that in turn can result in hyperperfusion of the brain, cerebral edema, and microhemorrhages.23
Because presentation of hypertensive encephalopathy may be similar to that in patients with acute stroke, hemorrhage, or brain lesions, these and other potential causes must be ruled out. While blood pressure treatment goals correspond with general recommendations,5,6 caution must be taken not to reduce blood pressure too swiftly; thus, continuous monitoring is warranted. If the patient's neurologic function worsens, treatment should be suspended and blood pressure allowed to rise slowly.4
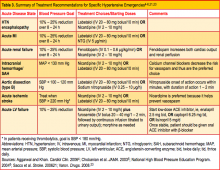
Preferred antihypertensives for patients with hypertensive encephalopathy include labetalol, nicardipine, and fenoldopam23 (see Table 34-6,21,23). Centrally acting antihypertensives, such as clonidine, methyldopa, or reserpine,24 should not be used, as they can cause central nervous system depression and may cloud the patient's sensorium further.
Myocardial ischemia/infarction. During an acute hypertensive event, the workload on the heart and activation of the renin-angiotensin-aldosterone system can lead to acute coronary ischemia or infarction.23 Treatment is aimed at increasing blood flow to the myocardium and reducing the workload on the heart. Antihypertensives are combined with reperfusion (eg, angioplasty) and/or thrombolytics to preserve myocardial structure and function. Standard agents to reduce blood pressure include IV nitroglycerin and β-blockers. Systolic blood pressure is reduced until symptoms subside or diastolic blood pressure is reduced to 100 mm Hg or lower. Adjuncts such as morphine and oxygen are used to reduce patient discomfort and improve oxygen delivery to the myocardium.4
Acute left ventricular failure. In this potential manifestation of hypertensive emergency, the left ventricle initially attempts to compensate for rising blood pressure and becomes hypertrophic. Once the myocardium can no longer meet the demand, left ventricular function decompensates, causing a flow backup that leads to acute pulmonary edema.23
Blood pressure goals mirror those in the general treatment recommendations but focus specifically on reducing preload and afterload, improving myocardial contractility and decreasing peripheral vascular resistance. The preferred agents in this setting are IV nitroglycerin and ACE inhibitors, along with loop diuretics, morphine, and oxygen.4 Medications that increase workload on the heart (eg, hydralazine, clonidine) should be avoided.23
Aortic dissection. This is a true medical emergency that can result in significant morbidity and mortality. Type A dissection occurs proximally, at the ascending aorta, whereas type B dissection occurs at the level of the descending aorta. Typically, type B dissection is managed medically, as surgical treatment carries a significant risk for paralysis.4 Both types of aortic dissection are strongly associated with uncontrolled hypertension and in some patients may be precipitated by an acute hypertensive event. In such cases, the goal for blood pressure reduction is to decrease the shearing forces associated with the dissection. This is accomplished by lowering both blood pressure and pulse rate.12
While cases of type A dissection are usually managed surgically, all affected patients will require some component of medical management and tight blood pressure control. The current recommendation for blood pressure in aortic dissection is swift downward titration to a goal systolic blood pressure of 100 to 110 mm Hg.4 A β-blocker in combination with a vasodilator, administered intravenously, should be used for swift blood pressure reduction.4,25
IV nitroprusside, a potent vasodilator, is the preferred agent, but its use requires intra-arterial blood pressure monitoring.23 Because nitroprusside is metabolized to cyanide, its use can lead to lethal toxicity, especially in patients with hepatic or renal impairment.11 In this patient population, IV labetalol or esmolol may be used instead.4,25
Acute renal failure. In the setting of an acute hypertensive episode, it is often difficult to determine whether acute renal failure is the cause or the effect. Regardless, rapid reduction in blood pressure is warranted to preserve renal function and to stop the cycle of microvascular kidney destruction. Blood pressure goals are aligned with the general treatment recommendations. The preferred antihypertensive agent is IV fenoldopam, a dopamine receptor agonist that directly dilates renal arterioles, improving renal perfusion and promoting diuresis.4,26 Nicardipine, a calcium channel blocker, may be considered as an alternative.23,27
Treatment Considerations in Stroke
Elevated blood pressure is common in the early stages of stroke. Numerous studies have analyzed overall outcomes in patients presenting with ischemic stroke and uncontrolled hypertension. In this setting, evidence suggests a poorer prognosis in patients treated aggressively with antihypertensive agents.4,21,22
The association between dramatic reduction in blood pressure and poor prognoses lies in the theory of the ischemic penumbra. This is an area around the core of ischemic tissue that receives enough blood flow to maintain neuronal activity for a few hours after initial injury, but this tissue is susceptible to further infarction. Precipitous drops in blood pressure can reduce blood flow to collateral vessels, resulting in hypoperfusion of the penumbra and leading to further neurologic damage.
Details and current treatment recommendations for each of the various types of stroke follow.
Acute intracerebral hemorrhage. Uncontrolled hypertension is often associated with intracerebral hemorrhage (ICH), either as a risk factor or a factor that contributes to the event. Once a patient has experienced an acute brain insult, blood pressure can become even more uncontrolled. Extension of the hematoma and a worsening outcome are the main concerns in treating the patient with concomitant blood pressure elevation and ICH. Also of concern is maintaining adequate perfusion to the penumbra. Additionally, transient hypoperfusion can develop when the ICP is elevated and the mean arterial pressure (MAP) is acutely lowered, thus reducing the cerebral perfusion pressure (CPP; CPP = MAP - ICP).
Researchers have acknowledged there is insufficient evidence to offer management guidelines for blood pressure reduction in patients with ICH.28 The 2007 recommendations from the American Heart Association/ American Stroke Association (AHA/ASA) for blood pressure management in patients with acute ICH29 are as follows: In the setting of ICH in patients with uncontrolled blood pressure, treatment should be aggressive if systolic blood pressure exceeds 200 mm Hg or MAP exceeds 150 mm Hg. A treatment goal to consider is reducing systolic blood pres sure to 160 mm Hg or less (or MAP to below 130 mm Hg).29 Patients with elevated ICP should undergo placement of a ventriculostomy to maintain a CPP between 60 and 80 mm Hg, although the risk for infection or intracerebral hemorrhage must be weighed against the potential benefits.29,30
When blood pressure reduction is required, the MAP should not be lowered more than 20% in a 24-hour period. Recommended agents include IV nicardipine, labetalol, enalapril, hydralazine, or esmolol.31
Acute ischemic stroke. Long-term control of blood pressure in patients who have experienced stroke remains undisputed, as it improves outcomes. However, in the setting of acute ischemic stroke (AIS), initiating blood pressure control is more liberal. Optimal control of blood pressure during management of AIS is imperative to reduce morbidity and mortality.32 Areas affected by edematous brain tissue are at increased risk for bleeding (ie, hemorrhagic expansion).
Patients who present with AIS require careful history taking to elicit their average blood pressure range; this will help the clinician determine goal pressures during management of the acute stroke phase.33 The primary rationale for treating blood pressure in this acute setting is to prevent hemorrhagic expansion at sites with potential for bleeding.34
According to the 2007 AHA/ ASA recommendations for management of blood pressure in AIS,35 patients who are eligible for thrombolysis should have a systolic blood pressure goal below 180 mm Hg and diastolic blood pressure below 105 mm Hg. Patients who will not receive thrombolytics should have blood pressure lowered only if systolic blood pressure exceeds 220 mm Hg or diastolic blood pressure exceeds 110 mm Hg.35,36 Appropriately refraining from reducing blood pressure is known as permissive hypertension.
Given the fragility of the cerebral brain tissue after AIS, permissive hypertension is intended to protect the penumbra and preserve cerebral blood flow. In patients who require blood pressure reduction because of other medical conditions (eg, decompensated heart failure), blood pressure should not be lowered more than 10% to 15% in a 24-hour period.9,31,36 No specific antihypertensives are preferred in patients with AIS: IV enalapril, esmolol, labetalol, or nicardipine can be used.31
Subarachnoid hemorrhage. The two complications of a subarachnoid hemorrhage (SAH) that most contribute to morbidity and mortality are rebleeding and vasospasms; elevated blood pressure can contribute to both. Thus, blood pressure control in patients with SAH is imperative.
Patients with acute SAH often require blood pressure monitoring via arterial line, as well as ICP monitoring. Blood pressure goals are similar to those in patients with ICH. The preferred agent for blood pressure control is nimodipine, which offers the secondary benefit of vasospasm prevention.37
CONCLUSION
Patients presenting with urgent or emergent hypertension need expeditious evaluation to avoid the significant morbidity and mortality associated with acute end-organ damage. Hypertensive urgency is defined as a diastolic blood pressure of greater than 120 mm Hg without evidence of end-organ damage.
In cases of hypertensive emergency, in which acute end-organ damage is present, lowering blood pressure should be directed by the type of end-organ damage and/or underlying comorbidities. In general, blood pressure should not be lowered more than 10% to 25% within the first hour, with normalization achieved over the next 8 to 24 hours.
In cases of acute ischemic stroke, permissive hypertension is recommended. Above all, treat patients, not numbers, bearing in mind the Hippocratic oath: Primum non nocere, or "First, do no harm."
REFERENCES
- Marik PE, Varon J. Hypertensive crises: challenges and management. Chest. 2007;131(6): 1949-1962.
- Guo F, He D, Zhang W, Walton RG. Trends in Prevalence, Awareness, Management, and Control of Hypertension Among United States Adults, 1999 to 2010. J Am Coll Cardiol. 2012;60(7):599-606.
- Flanigan JS, Vitberg D. Hypertensive emergency and severe hypertension: what to treat, who to treat, and how to treat. Med Clin North Am. 2006;90(3):439-451.
- Aggarwal M, Khan IA. Hypertensive crisis: hypertensive emergencies and urgencies. Cardiol Clin. 2006;24(1):135-146.
- Chobanian AV, Bakris GL, Black HR, et al. Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289(19):2560-2572.
- National High Blood Pressure Education Program Coordinating Committee, National Heart Lung and Blood Institute, NIH. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. NIH Publication No. 04-5230. August 2004. www .nhlbi.nih.gov/guidelines/hypertension/jnc7full.pdf. Accessed September 20, 2012.
- Houston M. Hypertensive emergencies and urgencies: pathophysiology and clinical aspects. Am Heart J. 1986;111(1):205-210.
- Kessler CS, Joudeh Y. Evaluation and treatment of severe asymptomatic hypertension. Am Fam Physician. 2010;81(4):470-476.
- Vaidya CK, Ouellette JR. Hypertensive urgency and emergency. Hosp Physician. Mar 2007:43-50. www.turner-white.com/memberfile.php?Pub Code=hp_mar07_hypertensive.pdf. Accessed September 20, 2012.
- Perez MI, Musini VM. Pharmacological interventions for hypertensive emergencies: a Cochrane systematic review. J Hum Hypertens. 2008;22(9):596-607.
- Vaughan CJ, Delanty N. Hypertensive emergencies. Lancet. 2000;356(9227):411-417.
- Stewart DL, Feinstein SE, Colgan R. Hypertensive urgencies and emergencies. Prim Care. 2006; 33(3):613-623.
- Atlas SA. The renin-angiotensin aldosterone system: pathophysiological role and pharmacologic inhibition. J Manag Care Pharm. 2007;13(8 suppl B):9-20.
- Flack JM. Epidemiology and unmet needs in hypertension. J Manag Care Pharm. 2007;13(e suppl B):2-8.
- Haas AR, Marik PE. Current diagnosis and management of hypertensive emergency. Semin Dial. 2006;19(6):502-512.
- Hebert CJ, Vidt DG. Hypertensive crises. Prim Care. 2008;35(3):475-487.
- Shulman KI, Fischer HD, Herrmann N, et al. Current prescription patterns and safety profile of irreversible monoamine oxidase inhibitors: a population-based cohort study of older adults. J Clin Psychiatry. 2009;70(12):1681-1696.
- Musso NR, Vergassola C, Pende A, Lotti G. Yohimbine effects on blood pressure and plasma catecholamines in human hypertension. Am J Hypertens. 1995;8(6):565-571.
- Baid S, Nieman LK. Glucocorticoid excess and hypertension. Curr Hypertens Rep. 2004;6(6): 493-499.
- Society of Critical Care Medicine. Fundamental Critical Care Support Course. www.sccm.org/ fccs_and_training_courses/fccs/pages/default .aspx. Accessed September 20, 2012.
- Sacco RL, Adams R, Albers G, et al. Guidelines for prevention of stroke in patients with ischemic stroke or transient ischemic attack: a statement for healthcare professionals from the American Heart Association/American Stroke Association Council on Stroke: co-sponsored by the Council on Cardiovascular Radiology and Intervention: the American Academy of Neurology affirms the value of this guideline. Stroke. 2006;37(2):577-617.
- Bernardini GL, Yavagal DR. Management of ischemic stroke: current concepts and treatment options. Hosp Physician. Sep 2006:13-23. www.turner-white.com/memberfile.php?PubCode=hp_sep06_is chemic.pdf. Accessed September 20, 2012.
- Varon J. Treatment of acute severe hypertension: current and newer agents. Drugs. 2008;68(3): 283-297.
- Webster J, Koch HF. Aspects of tolerability of centrally acting antihypertensive drugs. J Cardiovasc Pharmacol. 1996;27 suppl 3:S49-S54.
- Gupta PK, Gupta H, Khoynezhad A. Hypertensive emergency in aortic dissection and thoracic aortic aneurysm: a review of management. Pharmaceuticals. 2009;2(3):66-76.
- Post JB 4th, Frishman WH. Fenoldopam: a new dopamine agonist for the treatment of hypertensive urgencies and emergencies. J Clin Pharmacol. 1998;38(1):2-13.
- Suzuki S, Ohtsuka S, Ishikawa K, Yamaguchi I. Effects of nicardipine on coronary, vertebral and renal arterial flows in patients with essential hypertension. Hypertens Res. 2003;26(3):193-199.
- Anderson CS, Huang Y, Arima H, et al; INTERACT Investigators. Effects of early intensive blood pressure-lowering treatment on the growth of hematoma and perihematomal edema in acute intracerebral hemorrhage: the Intensive Blood Pressure Reduction in Acute Cerebral Haemorrhage Trial (INTERACT). Stroke. 2010;41(2):307-312.
- Broderick J, Connolly S, Feldmann E, et al. Quality of Care and Outcomes in Research Interdisciplinary Working Group Guidelines for the management of spontaneous intracerebral hemorrhage in adults: 2007 update: a guideline from the American Heart Association/American Stroke Association Stroke Council, High Blood Pressure Research Council, and the Quality of Care and Outcomes in Research Interdisciplinary Working Group. Circulation. 2007;116(16):e391-413.
- Morgenstern LB, Hemphill JC 3rd, Anderson C, et al. Guidelines for the management of spontaneous intracerebral hemorrhage: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2010;41(9):2108-2129.
- Brott T, Lu M, Kothari R, et al. Hypertension and its treatment in the NINDS rt-PA Stroke Trial. Stroke. 1998;29(8):1504-1509.
- Aiyagari V, Badruddin A. Management of hypertension in acute stroke. Expert Rev Cardiovasc Ther. 2009;7(6):637-646.
- Castillo J, Leira R, García MM, et al. Blood pressure decrease during the acute phase of ischemic stroke is associated with brain injury and poor stroke outcome. Stroke. 2004;35(2):520-526.
- Bonita R, Beaglehole R. The enigma of the decline in stroke deaths in the United States the search for an explanation. Stroke. 1996;27(3): 370-372.
- Adams HP Jr, del Zoppo G, Alberts MJ, et al. Guidelines for the early management of adults with ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council, Clinical Cardiology Council, Cardiovascular Radiology and Intervention Council, and the Atherosclerotic Peripheral Vascular Disease and Quality of Care Outcomes in Research Interdisciplinary Working Groups: the American Academy of Neurology affirms the value of this guideline as an educational tool for neurologists. Stroke. 2007;38(5):1655-1711.
- Heitsch L, Jauch EC. Management of hypertension in the setting of acute ischemic stroke. Curr Hypertens Rep. 2007;9(6):506-511.
- Barker FG II, Ogilvy CS. Efficacy of prophylactic nimodipine for delayed ischemic deficit after subarachnoid hemorrhage: a metaanalysis. J Neurosurg. 1996;84(3):405-414.
An estimated 1% to 2% of patients with chronic hypertension will at some time develop hypertensive urgency or emergency.1 According to recent data from the National Health and Nutrition Examination Survey (NHANES) 1999 to 2010,2 the prevalence of hypertension has remained stable at 30.5% among men and 28.5% among women in the United States; however, 74% of the hypertensive population is unaware of having this condition. Furthermore, 71.6% of hypertensive patients are managed for the condition, and in only 46.5% is blood pressure well controlled.2
In 2006, essential hypertension was estimated to account for more than 44 million emergency department visits in the US. The direct and indirect costs of hypertension totaled $73 billion in 2009.3,4
NEW TERMINOLOGY AND CLASSIFICATION
The terms malignant hypertension, hypertensive crisis, and accelerated hypertension have been replaced by hypertensive urgency or hypertensive emergency. Hypertensive urgency and emergency are differentiated by the absence or presence of acute end-organ damage, respectively.
Given the inconsistent terminology used, database searches can be challenging. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC7),5,6 published in 2003, is considered the gold standard for categorizing hypertension in the outpatient setting. The JNC7 authorsclassify normal blood pressure as < 120/< 80 mm Hg. The document further classifies blood pressure into the stages shown in Table 1.5,6 Blood pressure higher than 180 mm Hg systolic and/or 120 mm Hg diastolic is generally considered severe hypertension— a designation that includes hypertensive urgency and hypertensive emergency.6
What Defines Hypertensive Urgency/Emergency?
Hypertensive urgency is defined as a diastolic blood pressure of 110 mm Hg or greater without the acute signs of end-organ damage.7 Some sources suggest that a patient must also have certain risk factors (eg, heart disease, renal disease) to be given this diagnosis.8 The presence of acute and rapidly evolving end-organ damage with an elevated diastolic blood pressure, usually greater than 120 mm Hg, establishes a diagnosis of hypertensive emergency.6,8,9
No specific blood pressure measurement indicates a hypertensive emergency, however; rather, the defining feature of this diagnosis is the presence of progressive target end-organ damage.7 This is most commonly manifested in cardiopulmonary, central nervous system, and/or renal findings; for the specific forms of end-organ damage, see Table 2.5,6,10,11 Preeclampsia and eclampsia are also considered manifestations of hypertensive end-organ damage but are beyond the scope of this article.5,11
The most common form of organ damage associated with hypertension is ischemic heart disease, in the form of either heart failure or acute coronary syndrome.12
PATHOPHYSIOLOGY
Blood pressure is calculated by cardiac output (ie, stroke volume multiplied by heart rate) multiplied by total peripheral resistance. Total peripheral resistance is influenced by a variety of humoral and neural factors, also known as vasoactive substances (see Figure 13,4). During an episode of acute hypertension, a failure of autoregulatory function occurs, precipitated by one or more of a host of potential causes. This failure of autoregulation then leads to increased systemic vascular resistance. In the setting of end-organ damage, release of inflammatory markers ensues, which ultimately causes endovascular injury and fibrin necrosis of arterioles.4,10,11
The renin-angiotensin-aldosterone system also plays a significant role in the cascade of hypertension, stimulating decreased renal perfusion and lowering tubular sodium concentration. This in turn stimulates aldosterone to increase blood pressure by maintaining excess volume through sodium retention and potassium excretion, further potentiating the cycle of uncontrolled blood pressure.4,13,14
Patients with chronically elevated blood pressures have a compensatory response, lying in the threshold mechanism, that protects against end-organ damage. Acute changes in blood pressure are better tolerated in these patients because of their decreased propensity for hypoperfusion.4 In contrast, normotensive patients who experience precipitous changes in blood pressure are at increased risk for organ hypoperfusion. The main concern regarding organ hypoperfusion is that it can lead to ischemia4 (see Figure 23,4).
PATIENT HISTORY
Acute hypertensive urgency or emergency can be triggered by many factors. Systemic etiologies (including kidney disease) caused by immunologic mediators or renal artery stenosis can cause or exacerbate hypertension. The patient should be asked about his or her normal blood pressure range, as this may offer clues to medication compliance. Rebound hypertension can be seen in patients who abruptly discontinue medications such as clonidine or β-blockers, as this causes an increase in sympathetic outflow.9,15
All patients should be queried regarding their use of OTC medications and other drug use, including cocaine, methamphetamines, phencyclidine, and alcohol.1,4,11,16 Patients taking monoamine oxidase inhibitors (MAOIs) are at increased risk for serious medication interactions; concomitant administration of MAOIs with other antidepressants can lead to a hypertensive reaction, but also to serotonin syndrome.1,17 Because MAOIs inhibit the breakdown of tyramine, patients taking them should avoid tyramine-containing foods and herbal supplements (including, but not limited to, St. John's wort, ginseng, and yohimbine).1,15,18
Acute hypertensive episodes can also occur as a result of preeclampsia or eclampsia in pregnant women, pheochromocytoma, primary aldosteronism, glucocorticoid excess (Cushing syndrome), or central nervous system disorders (eg, cerebrovascular accident, head trauma, brain tumors).9,11,19
PHYSICAL EXAMINATION
The purpose of the physical examination is to determine whether end-organ damage is present.1,11 The fundoscopic exam may reveal papilledema, a sign of increased intracranial pressure (ICP). Flame hemorrhages, cotton wool spots or arteriovenous nicking suggest a long-standing history of uncontrolled hypertension or diabetes.7,9 The neck should be assessed for jugular venous distention, which may be elevated in decompensated heart failure or pulmonary edema.11
The cardiac exam may reveal an irregular rate and rhythm, displaced apical pulse, gallop, or murmur. On pulmonary exam, rales may be auscultated, suggestive of pulmonary edema.9,15
The abdominal exam should include listening for a renal artery bruit.1 The neurologic exam may demonstrate altered mental status (possibly indicating hypertensive encephalopathy) or focal findings, if the patient has had an underlying ischemic or hemorrhagic event.9
LABORATORY STUDIES AND IMAGING
In most cases, a serum chemistry panel is warranted to identify any renal dysfunction. Urinalysis may reveal proteinuria, possibly indicating renal damage.4,9,15
Any patient complaining of chest pain should have an ECG to look for ischemic changes or presence of a left bundle branch block, and serial cardiac enzymes to rule out acute coronary syndrome.15 Access to previous ECGs is helpful in differentiating between new and old conductive abnormalities.
A chest x-ray should be performed in patients who complain of shortness of breath and/or chest pain. A widened mediastinum can represent aortic dissection.4,15 Evidence of pulmonary edema should prompt the clinician to assess for left ventricular dysfunction or valvular insufficiencies by echocardiogram. Chest CT should be pursued in patients with clinical suspicion for dissection.1,15,20
Patients presenting with a headache or focal neurologic abnormalities warrant a head CT to rule out stroke.15 Urine drug screening is appropriate if the patient history suggests illicit drug use.12
"FIRST, DO NO HARM"
Treatment of hypertensive emergency and urgency varies from traditional treatment for hypertension. Aggressive blood pressure control in patients presenting with acute ischemic stroke has been associated with poorer patient outcomes.21,22 Thus, treating the patient and not the numbers is the first general recommendation for treatment of hypertensive emergency and urgency. It is important for the clinician to remember the Hippocratic oath, "First do no harm," when treating these patients.
Other general recommendations are derived from theory, physiology, and smaller clinical trials; their application must be individualized according to the patient's needs. These recommendations include aiming for a reduction in mean arterial blood pressure of no more than 10% to 25% within the first hour, a goal blood pressure of 160/90 mm Hg within the first 8 hours, and normalization of blood pressure over 8 to 24 hours.12
While the use of pharmacologic agents may be warranted, it is important to consider that elevated blood pressure may be a reaction to pain or stress and may be best treated alternatively. Recommendations for permissive hypertension in acute ischemic stroke will be discussed below.
TREATMENT: HYPERTENSIVE URGENCY
The treatment of hypertensive urgency is usually immediate and warrants close follow-up. Although elevated blood pressures can be alarming to the patient, hypertensive urgency usually develops over days to weeks.8 In this setting, it is not necessary to lower blood pressure acutely.12 A rapid decrease in blood pressure can actually cause symptomatic hypotension, resulting in hypoperfusion to the brain.5,6,8
After ruling out end-organ damage, the next step is to treat according to the guidelines for hypertensive urgency.5,6 These recommendations include the use of rapid-onset oral antihypertensive agents, such as clonidine, labetalol, or captopril.23 Use of these agents is only suggested for gradual, short-term reduction of blood pressure (ie, over 24 to 48 hours) while the patient is being monitored for potential hypertension-related organ damage, either in the emergency department or in an observational hospital setting.5,6,23
Once the short-acting agents have adequately reduced blood pressure, long-term agents can be chosen to prevent rebound hypertension.16 Patients are typically monitored for 24 hours in the hospital during this transition. Upon discharge, the patient should be scheduled for follow-up within one to two days.11 Patient education, including a discussion of medication adherence, weight loss, and reduced dietary salt, is key to prevent recurrences and optimize overall treatment compliance.
TREATMENT: HYPERTENSIVE EMERGENCY
Treatment of hypertensive emergency always warrants hospitalization, usually in the ICU.5,6 IV antihypertensive medications (eg, nicardipine, fenoldopam, labetalol, esmolol, phentolamine) are preferred. Their use often necessitates continuous blood pressure monitoring via arterial line, allowing the clinician to perform ongoing medication titration. In hypertensive emergencies, the purpose of treatment is to preserve brain, kidney, and heart function.4
Goal-directed therapy is initiated even before the patient evaluation has been fully completed. Patient assessment continues after treatment is begun to avoid overly aggressive blood pressure reduction, which can increase the risk for patient demise or morbidity.4
Exceptions in the treatment of hypertensive emergencies (particularly of specific disease states) will be discussed below, along with other treatment considerations. Patient comorbidities, for example, must be considered in the choice of antihypertensive agents.
Focused Treatment for Specific Hypertensive Emergencies
Hypertensive encephalopathy. This condition, associated with severe hypertension, is indicated by an abrupt change in mental status. During this acute end-organ damage event, a failure of cerebral autoregulation occurs, with increased pressure in the vascular endothelium leading to arteriole dilation that in turn can result in hyperperfusion of the brain, cerebral edema, and microhemorrhages.23
Because presentation of hypertensive encephalopathy may be similar to that in patients with acute stroke, hemorrhage, or brain lesions, these and other potential causes must be ruled out. While blood pressure treatment goals correspond with general recommendations,5,6 caution must be taken not to reduce blood pressure too swiftly; thus, continuous monitoring is warranted. If the patient's neurologic function worsens, treatment should be suspended and blood pressure allowed to rise slowly.4
Preferred antihypertensives for patients with hypertensive encephalopathy include labetalol, nicardipine, and fenoldopam23 (see Table 34-6,21,23). Centrally acting antihypertensives, such as clonidine, methyldopa, or reserpine,24 should not be used, as they can cause central nervous system depression and may cloud the patient's sensorium further.
Myocardial ischemia/infarction. During an acute hypertensive event, the workload on the heart and activation of the renin-angiotensin-aldosterone system can lead to acute coronary ischemia or infarction.23 Treatment is aimed at increasing blood flow to the myocardium and reducing the workload on the heart. Antihypertensives are combined with reperfusion (eg, angioplasty) and/or thrombolytics to preserve myocardial structure and function. Standard agents to reduce blood pressure include IV nitroglycerin and β-blockers. Systolic blood pressure is reduced until symptoms subside or diastolic blood pressure is reduced to 100 mm Hg or lower. Adjuncts such as morphine and oxygen are used to reduce patient discomfort and improve oxygen delivery to the myocardium.4
Acute left ventricular failure. In this potential manifestation of hypertensive emergency, the left ventricle initially attempts to compensate for rising blood pressure and becomes hypertrophic. Once the myocardium can no longer meet the demand, left ventricular function decompensates, causing a flow backup that leads to acute pulmonary edema.23
Blood pressure goals mirror those in the general treatment recommendations but focus specifically on reducing preload and afterload, improving myocardial contractility and decreasing peripheral vascular resistance. The preferred agents in this setting are IV nitroglycerin and ACE inhibitors, along with loop diuretics, morphine, and oxygen.4 Medications that increase workload on the heart (eg, hydralazine, clonidine) should be avoided.23
Aortic dissection. This is a true medical emergency that can result in significant morbidity and mortality. Type A dissection occurs proximally, at the ascending aorta, whereas type B dissection occurs at the level of the descending aorta. Typically, type B dissection is managed medically, as surgical treatment carries a significant risk for paralysis.4 Both types of aortic dissection are strongly associated with uncontrolled hypertension and in some patients may be precipitated by an acute hypertensive event. In such cases, the goal for blood pressure reduction is to decrease the shearing forces associated with the dissection. This is accomplished by lowering both blood pressure and pulse rate.12
While cases of type A dissection are usually managed surgically, all affected patients will require some component of medical management and tight blood pressure control. The current recommendation for blood pressure in aortic dissection is swift downward titration to a goal systolic blood pressure of 100 to 110 mm Hg.4 A β-blocker in combination with a vasodilator, administered intravenously, should be used for swift blood pressure reduction.4,25
IV nitroprusside, a potent vasodilator, is the preferred agent, but its use requires intra-arterial blood pressure monitoring.23 Because nitroprusside is metabolized to cyanide, its use can lead to lethal toxicity, especially in patients with hepatic or renal impairment.11 In this patient population, IV labetalol or esmolol may be used instead.4,25
Acute renal failure. In the setting of an acute hypertensive episode, it is often difficult to determine whether acute renal failure is the cause or the effect. Regardless, rapid reduction in blood pressure is warranted to preserve renal function and to stop the cycle of microvascular kidney destruction. Blood pressure goals are aligned with the general treatment recommendations. The preferred antihypertensive agent is IV fenoldopam, a dopamine receptor agonist that directly dilates renal arterioles, improving renal perfusion and promoting diuresis.4,26 Nicardipine, a calcium channel blocker, may be considered as an alternative.23,27
Treatment Considerations in Stroke
Elevated blood pressure is common in the early stages of stroke. Numerous studies have analyzed overall outcomes in patients presenting with ischemic stroke and uncontrolled hypertension. In this setting, evidence suggests a poorer prognosis in patients treated aggressively with antihypertensive agents.4,21,22
The association between dramatic reduction in blood pressure and poor prognoses lies in the theory of the ischemic penumbra. This is an area around the core of ischemic tissue that receives enough blood flow to maintain neuronal activity for a few hours after initial injury, but this tissue is susceptible to further infarction. Precipitous drops in blood pressure can reduce blood flow to collateral vessels, resulting in hypoperfusion of the penumbra and leading to further neurologic damage.
Details and current treatment recommendations for each of the various types of stroke follow.
Acute intracerebral hemorrhage. Uncontrolled hypertension is often associated with intracerebral hemorrhage (ICH), either as a risk factor or a factor that contributes to the event. Once a patient has experienced an acute brain insult, blood pressure can become even more uncontrolled. Extension of the hematoma and a worsening outcome are the main concerns in treating the patient with concomitant blood pressure elevation and ICH. Also of concern is maintaining adequate perfusion to the penumbra. Additionally, transient hypoperfusion can develop when the ICP is elevated and the mean arterial pressure (MAP) is acutely lowered, thus reducing the cerebral perfusion pressure (CPP; CPP = MAP - ICP).
Researchers have acknowledged there is insufficient evidence to offer management guidelines for blood pressure reduction in patients with ICH.28 The 2007 recommendations from the American Heart Association/ American Stroke Association (AHA/ASA) for blood pressure management in patients with acute ICH29 are as follows: In the setting of ICH in patients with uncontrolled blood pressure, treatment should be aggressive if systolic blood pressure exceeds 200 mm Hg or MAP exceeds 150 mm Hg. A treatment goal to consider is reducing systolic blood pres sure to 160 mm Hg or less (or MAP to below 130 mm Hg).29 Patients with elevated ICP should undergo placement of a ventriculostomy to maintain a CPP between 60 and 80 mm Hg, although the risk for infection or intracerebral hemorrhage must be weighed against the potential benefits.29,30
When blood pressure reduction is required, the MAP should not be lowered more than 20% in a 24-hour period. Recommended agents include IV nicardipine, labetalol, enalapril, hydralazine, or esmolol.31
Acute ischemic stroke. Long-term control of blood pressure in patients who have experienced stroke remains undisputed, as it improves outcomes. However, in the setting of acute ischemic stroke (AIS), initiating blood pressure control is more liberal. Optimal control of blood pressure during management of AIS is imperative to reduce morbidity and mortality.32 Areas affected by edematous brain tissue are at increased risk for bleeding (ie, hemorrhagic expansion).
Patients who present with AIS require careful history taking to elicit their average blood pressure range; this will help the clinician determine goal pressures during management of the acute stroke phase.33 The primary rationale for treating blood pressure in this acute setting is to prevent hemorrhagic expansion at sites with potential for bleeding.34
According to the 2007 AHA/ ASA recommendations for management of blood pressure in AIS,35 patients who are eligible for thrombolysis should have a systolic blood pressure goal below 180 mm Hg and diastolic blood pressure below 105 mm Hg. Patients who will not receive thrombolytics should have blood pressure lowered only if systolic blood pressure exceeds 220 mm Hg or diastolic blood pressure exceeds 110 mm Hg.35,36 Appropriately refraining from reducing blood pressure is known as permissive hypertension.
Given the fragility of the cerebral brain tissue after AIS, permissive hypertension is intended to protect the penumbra and preserve cerebral blood flow. In patients who require blood pressure reduction because of other medical conditions (eg, decompensated heart failure), blood pressure should not be lowered more than 10% to 15% in a 24-hour period.9,31,36 No specific antihypertensives are preferred in patients with AIS: IV enalapril, esmolol, labetalol, or nicardipine can be used.31
Subarachnoid hemorrhage. The two complications of a subarachnoid hemorrhage (SAH) that most contribute to morbidity and mortality are rebleeding and vasospasms; elevated blood pressure can contribute to both. Thus, blood pressure control in patients with SAH is imperative.
Patients with acute SAH often require blood pressure monitoring via arterial line, as well as ICP monitoring. Blood pressure goals are similar to those in patients with ICH. The preferred agent for blood pressure control is nimodipine, which offers the secondary benefit of vasospasm prevention.37
CONCLUSION
Patients presenting with urgent or emergent hypertension need expeditious evaluation to avoid the significant morbidity and mortality associated with acute end-organ damage. Hypertensive urgency is defined as a diastolic blood pressure of greater than 120 mm Hg without evidence of end-organ damage.
In cases of hypertensive emergency, in which acute end-organ damage is present, lowering blood pressure should be directed by the type of end-organ damage and/or underlying comorbidities. In general, blood pressure should not be lowered more than 10% to 25% within the first hour, with normalization achieved over the next 8 to 24 hours.
In cases of acute ischemic stroke, permissive hypertension is recommended. Above all, treat patients, not numbers, bearing in mind the Hippocratic oath: Primum non nocere, or "First, do no harm."
REFERENCES
- Marik PE, Varon J. Hypertensive crises: challenges and management. Chest. 2007;131(6): 1949-1962.
- Guo F, He D, Zhang W, Walton RG. Trends in Prevalence, Awareness, Management, and Control of Hypertension Among United States Adults, 1999 to 2010. J Am Coll Cardiol. 2012;60(7):599-606.
- Flanigan JS, Vitberg D. Hypertensive emergency and severe hypertension: what to treat, who to treat, and how to treat. Med Clin North Am. 2006;90(3):439-451.
- Aggarwal M, Khan IA. Hypertensive crisis: hypertensive emergencies and urgencies. Cardiol Clin. 2006;24(1):135-146.
- Chobanian AV, Bakris GL, Black HR, et al. Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289(19):2560-2572.
- National High Blood Pressure Education Program Coordinating Committee, National Heart Lung and Blood Institute, NIH. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. NIH Publication No. 04-5230. August 2004. www .nhlbi.nih.gov/guidelines/hypertension/jnc7full.pdf. Accessed September 20, 2012.
- Houston M. Hypertensive emergencies and urgencies: pathophysiology and clinical aspects. Am Heart J. 1986;111(1):205-210.
- Kessler CS, Joudeh Y. Evaluation and treatment of severe asymptomatic hypertension. Am Fam Physician. 2010;81(4):470-476.
- Vaidya CK, Ouellette JR. Hypertensive urgency and emergency. Hosp Physician. Mar 2007:43-50. www.turner-white.com/memberfile.php?Pub Code=hp_mar07_hypertensive.pdf. Accessed September 20, 2012.
- Perez MI, Musini VM. Pharmacological interventions for hypertensive emergencies: a Cochrane systematic review. J Hum Hypertens. 2008;22(9):596-607.
- Vaughan CJ, Delanty N. Hypertensive emergencies. Lancet. 2000;356(9227):411-417.
- Stewart DL, Feinstein SE, Colgan R. Hypertensive urgencies and emergencies. Prim Care. 2006; 33(3):613-623.
- Atlas SA. The renin-angiotensin aldosterone system: pathophysiological role and pharmacologic inhibition. J Manag Care Pharm. 2007;13(8 suppl B):9-20.
- Flack JM. Epidemiology and unmet needs in hypertension. J Manag Care Pharm. 2007;13(e suppl B):2-8.
- Haas AR, Marik PE. Current diagnosis and management of hypertensive emergency. Semin Dial. 2006;19(6):502-512.
- Hebert CJ, Vidt DG. Hypertensive crises. Prim Care. 2008;35(3):475-487.
- Shulman KI, Fischer HD, Herrmann N, et al. Current prescription patterns and safety profile of irreversible monoamine oxidase inhibitors: a population-based cohort study of older adults. J Clin Psychiatry. 2009;70(12):1681-1696.
- Musso NR, Vergassola C, Pende A, Lotti G. Yohimbine effects on blood pressure and plasma catecholamines in human hypertension. Am J Hypertens. 1995;8(6):565-571.
- Baid S, Nieman LK. Glucocorticoid excess and hypertension. Curr Hypertens Rep. 2004;6(6): 493-499.
- Society of Critical Care Medicine. Fundamental Critical Care Support Course. www.sccm.org/ fccs_and_training_courses/fccs/pages/default .aspx. Accessed September 20, 2012.
- Sacco RL, Adams R, Albers G, et al. Guidelines for prevention of stroke in patients with ischemic stroke or transient ischemic attack: a statement for healthcare professionals from the American Heart Association/American Stroke Association Council on Stroke: co-sponsored by the Council on Cardiovascular Radiology and Intervention: the American Academy of Neurology affirms the value of this guideline. Stroke. 2006;37(2):577-617.
- Bernardini GL, Yavagal DR. Management of ischemic stroke: current concepts and treatment options. Hosp Physician. Sep 2006:13-23. www.turner-white.com/memberfile.php?PubCode=hp_sep06_is chemic.pdf. Accessed September 20, 2012.
- Varon J. Treatment of acute severe hypertension: current and newer agents. Drugs. 2008;68(3): 283-297.
- Webster J, Koch HF. Aspects of tolerability of centrally acting antihypertensive drugs. J Cardiovasc Pharmacol. 1996;27 suppl 3:S49-S54.
- Gupta PK, Gupta H, Khoynezhad A. Hypertensive emergency in aortic dissection and thoracic aortic aneurysm: a review of management. Pharmaceuticals. 2009;2(3):66-76.
- Post JB 4th, Frishman WH. Fenoldopam: a new dopamine agonist for the treatment of hypertensive urgencies and emergencies. J Clin Pharmacol. 1998;38(1):2-13.
- Suzuki S, Ohtsuka S, Ishikawa K, Yamaguchi I. Effects of nicardipine on coronary, vertebral and renal arterial flows in patients with essential hypertension. Hypertens Res. 2003;26(3):193-199.
- Anderson CS, Huang Y, Arima H, et al; INTERACT Investigators. Effects of early intensive blood pressure-lowering treatment on the growth of hematoma and perihematomal edema in acute intracerebral hemorrhage: the Intensive Blood Pressure Reduction in Acute Cerebral Haemorrhage Trial (INTERACT). Stroke. 2010;41(2):307-312.
- Broderick J, Connolly S, Feldmann E, et al. Quality of Care and Outcomes in Research Interdisciplinary Working Group Guidelines for the management of spontaneous intracerebral hemorrhage in adults: 2007 update: a guideline from the American Heart Association/American Stroke Association Stroke Council, High Blood Pressure Research Council, and the Quality of Care and Outcomes in Research Interdisciplinary Working Group. Circulation. 2007;116(16):e391-413.
- Morgenstern LB, Hemphill JC 3rd, Anderson C, et al. Guidelines for the management of spontaneous intracerebral hemorrhage: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2010;41(9):2108-2129.
- Brott T, Lu M, Kothari R, et al. Hypertension and its treatment in the NINDS rt-PA Stroke Trial. Stroke. 1998;29(8):1504-1509.
- Aiyagari V, Badruddin A. Management of hypertension in acute stroke. Expert Rev Cardiovasc Ther. 2009;7(6):637-646.
- Castillo J, Leira R, García MM, et al. Blood pressure decrease during the acute phase of ischemic stroke is associated with brain injury and poor stroke outcome. Stroke. 2004;35(2):520-526.
- Bonita R, Beaglehole R. The enigma of the decline in stroke deaths in the United States the search for an explanation. Stroke. 1996;27(3): 370-372.
- Adams HP Jr, del Zoppo G, Alberts MJ, et al. Guidelines for the early management of adults with ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council, Clinical Cardiology Council, Cardiovascular Radiology and Intervention Council, and the Atherosclerotic Peripheral Vascular Disease and Quality of Care Outcomes in Research Interdisciplinary Working Groups: the American Academy of Neurology affirms the value of this guideline as an educational tool for neurologists. Stroke. 2007;38(5):1655-1711.
- Heitsch L, Jauch EC. Management of hypertension in the setting of acute ischemic stroke. Curr Hypertens Rep. 2007;9(6):506-511.
- Barker FG II, Ogilvy CS. Efficacy of prophylactic nimodipine for delayed ischemic deficit after subarachnoid hemorrhage: a metaanalysis. J Neurosurg. 1996;84(3):405-414.
An estimated 1% to 2% of patients with chronic hypertension will at some time develop hypertensive urgency or emergency.1 According to recent data from the National Health and Nutrition Examination Survey (NHANES) 1999 to 2010,2 the prevalence of hypertension has remained stable at 30.5% among men and 28.5% among women in the United States; however, 74% of the hypertensive population is unaware of having this condition. Furthermore, 71.6% of hypertensive patients are managed for the condition, and in only 46.5% is blood pressure well controlled.2
In 2006, essential hypertension was estimated to account for more than 44 million emergency department visits in the US. The direct and indirect costs of hypertension totaled $73 billion in 2009.3,4
NEW TERMINOLOGY AND CLASSIFICATION
The terms malignant hypertension, hypertensive crisis, and accelerated hypertension have been replaced by hypertensive urgency or hypertensive emergency. Hypertensive urgency and emergency are differentiated by the absence or presence of acute end-organ damage, respectively.
Given the inconsistent terminology used, database searches can be challenging. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC7),5,6 published in 2003, is considered the gold standard for categorizing hypertension in the outpatient setting. The JNC7 authorsclassify normal blood pressure as < 120/< 80 mm Hg. The document further classifies blood pressure into the stages shown in Table 1.5,6 Blood pressure higher than 180 mm Hg systolic and/or 120 mm Hg diastolic is generally considered severe hypertension— a designation that includes hypertensive urgency and hypertensive emergency.6
What Defines Hypertensive Urgency/Emergency?
Hypertensive urgency is defined as a diastolic blood pressure of 110 mm Hg or greater without the acute signs of end-organ damage.7 Some sources suggest that a patient must also have certain risk factors (eg, heart disease, renal disease) to be given this diagnosis.8 The presence of acute and rapidly evolving end-organ damage with an elevated diastolic blood pressure, usually greater than 120 mm Hg, establishes a diagnosis of hypertensive emergency.6,8,9
No specific blood pressure measurement indicates a hypertensive emergency, however; rather, the defining feature of this diagnosis is the presence of progressive target end-organ damage.7 This is most commonly manifested in cardiopulmonary, central nervous system, and/or renal findings; for the specific forms of end-organ damage, see Table 2.5,6,10,11 Preeclampsia and eclampsia are also considered manifestations of hypertensive end-organ damage but are beyond the scope of this article.5,11
The most common form of organ damage associated with hypertension is ischemic heart disease, in the form of either heart failure or acute coronary syndrome.12
PATHOPHYSIOLOGY
Blood pressure is calculated by cardiac output (ie, stroke volume multiplied by heart rate) multiplied by total peripheral resistance. Total peripheral resistance is influenced by a variety of humoral and neural factors, also known as vasoactive substances (see Figure 13,4). During an episode of acute hypertension, a failure of autoregulatory function occurs, precipitated by one or more of a host of potential causes. This failure of autoregulation then leads to increased systemic vascular resistance. In the setting of end-organ damage, release of inflammatory markers ensues, which ultimately causes endovascular injury and fibrin necrosis of arterioles.4,10,11
The renin-angiotensin-aldosterone system also plays a significant role in the cascade of hypertension, stimulating decreased renal perfusion and lowering tubular sodium concentration. This in turn stimulates aldosterone to increase blood pressure by maintaining excess volume through sodium retention and potassium excretion, further potentiating the cycle of uncontrolled blood pressure.4,13,14
Patients with chronically elevated blood pressures have a compensatory response, lying in the threshold mechanism, that protects against end-organ damage. Acute changes in blood pressure are better tolerated in these patients because of their decreased propensity for hypoperfusion.4 In contrast, normotensive patients who experience precipitous changes in blood pressure are at increased risk for organ hypoperfusion. The main concern regarding organ hypoperfusion is that it can lead to ischemia4 (see Figure 23,4).
PATIENT HISTORY
Acute hypertensive urgency or emergency can be triggered by many factors. Systemic etiologies (including kidney disease) caused by immunologic mediators or renal artery stenosis can cause or exacerbate hypertension. The patient should be asked about his or her normal blood pressure range, as this may offer clues to medication compliance. Rebound hypertension can be seen in patients who abruptly discontinue medications such as clonidine or β-blockers, as this causes an increase in sympathetic outflow.9,15
All patients should be queried regarding their use of OTC medications and other drug use, including cocaine, methamphetamines, phencyclidine, and alcohol.1,4,11,16 Patients taking monoamine oxidase inhibitors (MAOIs) are at increased risk for serious medication interactions; concomitant administration of MAOIs with other antidepressants can lead to a hypertensive reaction, but also to serotonin syndrome.1,17 Because MAOIs inhibit the breakdown of tyramine, patients taking them should avoid tyramine-containing foods and herbal supplements (including, but not limited to, St. John's wort, ginseng, and yohimbine).1,15,18
Acute hypertensive episodes can also occur as a result of preeclampsia or eclampsia in pregnant women, pheochromocytoma, primary aldosteronism, glucocorticoid excess (Cushing syndrome), or central nervous system disorders (eg, cerebrovascular accident, head trauma, brain tumors).9,11,19
PHYSICAL EXAMINATION
The purpose of the physical examination is to determine whether end-organ damage is present.1,11 The fundoscopic exam may reveal papilledema, a sign of increased intracranial pressure (ICP). Flame hemorrhages, cotton wool spots or arteriovenous nicking suggest a long-standing history of uncontrolled hypertension or diabetes.7,9 The neck should be assessed for jugular venous distention, which may be elevated in decompensated heart failure or pulmonary edema.11
The cardiac exam may reveal an irregular rate and rhythm, displaced apical pulse, gallop, or murmur. On pulmonary exam, rales may be auscultated, suggestive of pulmonary edema.9,15
The abdominal exam should include listening for a renal artery bruit.1 The neurologic exam may demonstrate altered mental status (possibly indicating hypertensive encephalopathy) or focal findings, if the patient has had an underlying ischemic or hemorrhagic event.9
LABORATORY STUDIES AND IMAGING
In most cases, a serum chemistry panel is warranted to identify any renal dysfunction. Urinalysis may reveal proteinuria, possibly indicating renal damage.4,9,15
Any patient complaining of chest pain should have an ECG to look for ischemic changes or presence of a left bundle branch block, and serial cardiac enzymes to rule out acute coronary syndrome.15 Access to previous ECGs is helpful in differentiating between new and old conductive abnormalities.
A chest x-ray should be performed in patients who complain of shortness of breath and/or chest pain. A widened mediastinum can represent aortic dissection.4,15 Evidence of pulmonary edema should prompt the clinician to assess for left ventricular dysfunction or valvular insufficiencies by echocardiogram. Chest CT should be pursued in patients with clinical suspicion for dissection.1,15,20
Patients presenting with a headache or focal neurologic abnormalities warrant a head CT to rule out stroke.15 Urine drug screening is appropriate if the patient history suggests illicit drug use.12
"FIRST, DO NO HARM"
Treatment of hypertensive emergency and urgency varies from traditional treatment for hypertension. Aggressive blood pressure control in patients presenting with acute ischemic stroke has been associated with poorer patient outcomes.21,22 Thus, treating the patient and not the numbers is the first general recommendation for treatment of hypertensive emergency and urgency. It is important for the clinician to remember the Hippocratic oath, "First do no harm," when treating these patients.
Other general recommendations are derived from theory, physiology, and smaller clinical trials; their application must be individualized according to the patient's needs. These recommendations include aiming for a reduction in mean arterial blood pressure of no more than 10% to 25% within the first hour, a goal blood pressure of 160/90 mm Hg within the first 8 hours, and normalization of blood pressure over 8 to 24 hours.12
While the use of pharmacologic agents may be warranted, it is important to consider that elevated blood pressure may be a reaction to pain or stress and may be best treated alternatively. Recommendations for permissive hypertension in acute ischemic stroke will be discussed below.
TREATMENT: HYPERTENSIVE URGENCY
The treatment of hypertensive urgency is usually immediate and warrants close follow-up. Although elevated blood pressures can be alarming to the patient, hypertensive urgency usually develops over days to weeks.8 In this setting, it is not necessary to lower blood pressure acutely.12 A rapid decrease in blood pressure can actually cause symptomatic hypotension, resulting in hypoperfusion to the brain.5,6,8
After ruling out end-organ damage, the next step is to treat according to the guidelines for hypertensive urgency.5,6 These recommendations include the use of rapid-onset oral antihypertensive agents, such as clonidine, labetalol, or captopril.23 Use of these agents is only suggested for gradual, short-term reduction of blood pressure (ie, over 24 to 48 hours) while the patient is being monitored for potential hypertension-related organ damage, either in the emergency department or in an observational hospital setting.5,6,23
Once the short-acting agents have adequately reduced blood pressure, long-term agents can be chosen to prevent rebound hypertension.16 Patients are typically monitored for 24 hours in the hospital during this transition. Upon discharge, the patient should be scheduled for follow-up within one to two days.11 Patient education, including a discussion of medication adherence, weight loss, and reduced dietary salt, is key to prevent recurrences and optimize overall treatment compliance.
TREATMENT: HYPERTENSIVE EMERGENCY
Treatment of hypertensive emergency always warrants hospitalization, usually in the ICU.5,6 IV antihypertensive medications (eg, nicardipine, fenoldopam, labetalol, esmolol, phentolamine) are preferred. Their use often necessitates continuous blood pressure monitoring via arterial line, allowing the clinician to perform ongoing medication titration. In hypertensive emergencies, the purpose of treatment is to preserve brain, kidney, and heart function.4
Goal-directed therapy is initiated even before the patient evaluation has been fully completed. Patient assessment continues after treatment is begun to avoid overly aggressive blood pressure reduction, which can increase the risk for patient demise or morbidity.4
Exceptions in the treatment of hypertensive emergencies (particularly of specific disease states) will be discussed below, along with other treatment considerations. Patient comorbidities, for example, must be considered in the choice of antihypertensive agents.
Focused Treatment for Specific Hypertensive Emergencies
Hypertensive encephalopathy. This condition, associated with severe hypertension, is indicated by an abrupt change in mental status. During this acute end-organ damage event, a failure of cerebral autoregulation occurs, with increased pressure in the vascular endothelium leading to arteriole dilation that in turn can result in hyperperfusion of the brain, cerebral edema, and microhemorrhages.23
Because presentation of hypertensive encephalopathy may be similar to that in patients with acute stroke, hemorrhage, or brain lesions, these and other potential causes must be ruled out. While blood pressure treatment goals correspond with general recommendations,5,6 caution must be taken not to reduce blood pressure too swiftly; thus, continuous monitoring is warranted. If the patient's neurologic function worsens, treatment should be suspended and blood pressure allowed to rise slowly.4
Preferred antihypertensives for patients with hypertensive encephalopathy include labetalol, nicardipine, and fenoldopam23 (see Table 34-6,21,23). Centrally acting antihypertensives, such as clonidine, methyldopa, or reserpine,24 should not be used, as they can cause central nervous system depression and may cloud the patient's sensorium further.
Myocardial ischemia/infarction. During an acute hypertensive event, the workload on the heart and activation of the renin-angiotensin-aldosterone system can lead to acute coronary ischemia or infarction.23 Treatment is aimed at increasing blood flow to the myocardium and reducing the workload on the heart. Antihypertensives are combined with reperfusion (eg, angioplasty) and/or thrombolytics to preserve myocardial structure and function. Standard agents to reduce blood pressure include IV nitroglycerin and β-blockers. Systolic blood pressure is reduced until symptoms subside or diastolic blood pressure is reduced to 100 mm Hg or lower. Adjuncts such as morphine and oxygen are used to reduce patient discomfort and improve oxygen delivery to the myocardium.4
Acute left ventricular failure. In this potential manifestation of hypertensive emergency, the left ventricle initially attempts to compensate for rising blood pressure and becomes hypertrophic. Once the myocardium can no longer meet the demand, left ventricular function decompensates, causing a flow backup that leads to acute pulmonary edema.23
Blood pressure goals mirror those in the general treatment recommendations but focus specifically on reducing preload and afterload, improving myocardial contractility and decreasing peripheral vascular resistance. The preferred agents in this setting are IV nitroglycerin and ACE inhibitors, along with loop diuretics, morphine, and oxygen.4 Medications that increase workload on the heart (eg, hydralazine, clonidine) should be avoided.23
Aortic dissection. This is a true medical emergency that can result in significant morbidity and mortality. Type A dissection occurs proximally, at the ascending aorta, whereas type B dissection occurs at the level of the descending aorta. Typically, type B dissection is managed medically, as surgical treatment carries a significant risk for paralysis.4 Both types of aortic dissection are strongly associated with uncontrolled hypertension and in some patients may be precipitated by an acute hypertensive event. In such cases, the goal for blood pressure reduction is to decrease the shearing forces associated with the dissection. This is accomplished by lowering both blood pressure and pulse rate.12
While cases of type A dissection are usually managed surgically, all affected patients will require some component of medical management and tight blood pressure control. The current recommendation for blood pressure in aortic dissection is swift downward titration to a goal systolic blood pressure of 100 to 110 mm Hg.4 A β-blocker in combination with a vasodilator, administered intravenously, should be used for swift blood pressure reduction.4,25
IV nitroprusside, a potent vasodilator, is the preferred agent, but its use requires intra-arterial blood pressure monitoring.23 Because nitroprusside is metabolized to cyanide, its use can lead to lethal toxicity, especially in patients with hepatic or renal impairment.11 In this patient population, IV labetalol or esmolol may be used instead.4,25
Acute renal failure. In the setting of an acute hypertensive episode, it is often difficult to determine whether acute renal failure is the cause or the effect. Regardless, rapid reduction in blood pressure is warranted to preserve renal function and to stop the cycle of microvascular kidney destruction. Blood pressure goals are aligned with the general treatment recommendations. The preferred antihypertensive agent is IV fenoldopam, a dopamine receptor agonist that directly dilates renal arterioles, improving renal perfusion and promoting diuresis.4,26 Nicardipine, a calcium channel blocker, may be considered as an alternative.23,27
Treatment Considerations in Stroke
Elevated blood pressure is common in the early stages of stroke. Numerous studies have analyzed overall outcomes in patients presenting with ischemic stroke and uncontrolled hypertension. In this setting, evidence suggests a poorer prognosis in patients treated aggressively with antihypertensive agents.4,21,22
The association between dramatic reduction in blood pressure and poor prognoses lies in the theory of the ischemic penumbra. This is an area around the core of ischemic tissue that receives enough blood flow to maintain neuronal activity for a few hours after initial injury, but this tissue is susceptible to further infarction. Precipitous drops in blood pressure can reduce blood flow to collateral vessels, resulting in hypoperfusion of the penumbra and leading to further neurologic damage.
Details and current treatment recommendations for each of the various types of stroke follow.
Acute intracerebral hemorrhage. Uncontrolled hypertension is often associated with intracerebral hemorrhage (ICH), either as a risk factor or a factor that contributes to the event. Once a patient has experienced an acute brain insult, blood pressure can become even more uncontrolled. Extension of the hematoma and a worsening outcome are the main concerns in treating the patient with concomitant blood pressure elevation and ICH. Also of concern is maintaining adequate perfusion to the penumbra. Additionally, transient hypoperfusion can develop when the ICP is elevated and the mean arterial pressure (MAP) is acutely lowered, thus reducing the cerebral perfusion pressure (CPP; CPP = MAP - ICP).
Researchers have acknowledged there is insufficient evidence to offer management guidelines for blood pressure reduction in patients with ICH.28 The 2007 recommendations from the American Heart Association/ American Stroke Association (AHA/ASA) for blood pressure management in patients with acute ICH29 are as follows: In the setting of ICH in patients with uncontrolled blood pressure, treatment should be aggressive if systolic blood pressure exceeds 200 mm Hg or MAP exceeds 150 mm Hg. A treatment goal to consider is reducing systolic blood pres sure to 160 mm Hg or less (or MAP to below 130 mm Hg).29 Patients with elevated ICP should undergo placement of a ventriculostomy to maintain a CPP between 60 and 80 mm Hg, although the risk for infection or intracerebral hemorrhage must be weighed against the potential benefits.29,30
When blood pressure reduction is required, the MAP should not be lowered more than 20% in a 24-hour period. Recommended agents include IV nicardipine, labetalol, enalapril, hydralazine, or esmolol.31
Acute ischemic stroke. Long-term control of blood pressure in patients who have experienced stroke remains undisputed, as it improves outcomes. However, in the setting of acute ischemic stroke (AIS), initiating blood pressure control is more liberal. Optimal control of blood pressure during management of AIS is imperative to reduce morbidity and mortality.32 Areas affected by edematous brain tissue are at increased risk for bleeding (ie, hemorrhagic expansion).
Patients who present with AIS require careful history taking to elicit their average blood pressure range; this will help the clinician determine goal pressures during management of the acute stroke phase.33 The primary rationale for treating blood pressure in this acute setting is to prevent hemorrhagic expansion at sites with potential for bleeding.34
According to the 2007 AHA/ ASA recommendations for management of blood pressure in AIS,35 patients who are eligible for thrombolysis should have a systolic blood pressure goal below 180 mm Hg and diastolic blood pressure below 105 mm Hg. Patients who will not receive thrombolytics should have blood pressure lowered only if systolic blood pressure exceeds 220 mm Hg or diastolic blood pressure exceeds 110 mm Hg.35,36 Appropriately refraining from reducing blood pressure is known as permissive hypertension.
Given the fragility of the cerebral brain tissue after AIS, permissive hypertension is intended to protect the penumbra and preserve cerebral blood flow. In patients who require blood pressure reduction because of other medical conditions (eg, decompensated heart failure), blood pressure should not be lowered more than 10% to 15% in a 24-hour period.9,31,36 No specific antihypertensives are preferred in patients with AIS: IV enalapril, esmolol, labetalol, or nicardipine can be used.31
Subarachnoid hemorrhage. The two complications of a subarachnoid hemorrhage (SAH) that most contribute to morbidity and mortality are rebleeding and vasospasms; elevated blood pressure can contribute to both. Thus, blood pressure control in patients with SAH is imperative.
Patients with acute SAH often require blood pressure monitoring via arterial line, as well as ICP monitoring. Blood pressure goals are similar to those in patients with ICH. The preferred agent for blood pressure control is nimodipine, which offers the secondary benefit of vasospasm prevention.37
CONCLUSION
Patients presenting with urgent or emergent hypertension need expeditious evaluation to avoid the significant morbidity and mortality associated with acute end-organ damage. Hypertensive urgency is defined as a diastolic blood pressure of greater than 120 mm Hg without evidence of end-organ damage.
In cases of hypertensive emergency, in which acute end-organ damage is present, lowering blood pressure should be directed by the type of end-organ damage and/or underlying comorbidities. In general, blood pressure should not be lowered more than 10% to 25% within the first hour, with normalization achieved over the next 8 to 24 hours.
In cases of acute ischemic stroke, permissive hypertension is recommended. Above all, treat patients, not numbers, bearing in mind the Hippocratic oath: Primum non nocere, or "First, do no harm."
REFERENCES
- Marik PE, Varon J. Hypertensive crises: challenges and management. Chest. 2007;131(6): 1949-1962.
- Guo F, He D, Zhang W, Walton RG. Trends in Prevalence, Awareness, Management, and Control of Hypertension Among United States Adults, 1999 to 2010. J Am Coll Cardiol. 2012;60(7):599-606.
- Flanigan JS, Vitberg D. Hypertensive emergency and severe hypertension: what to treat, who to treat, and how to treat. Med Clin North Am. 2006;90(3):439-451.
- Aggarwal M, Khan IA. Hypertensive crisis: hypertensive emergencies and urgencies. Cardiol Clin. 2006;24(1):135-146.
- Chobanian AV, Bakris GL, Black HR, et al. Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289(19):2560-2572.
- National High Blood Pressure Education Program Coordinating Committee, National Heart Lung and Blood Institute, NIH. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. NIH Publication No. 04-5230. August 2004. www .nhlbi.nih.gov/guidelines/hypertension/jnc7full.pdf. Accessed September 20, 2012.
- Houston M. Hypertensive emergencies and urgencies: pathophysiology and clinical aspects. Am Heart J. 1986;111(1):205-210.
- Kessler CS, Joudeh Y. Evaluation and treatment of severe asymptomatic hypertension. Am Fam Physician. 2010;81(4):470-476.
- Vaidya CK, Ouellette JR. Hypertensive urgency and emergency. Hosp Physician. Mar 2007:43-50. www.turner-white.com/memberfile.php?Pub Code=hp_mar07_hypertensive.pdf. Accessed September 20, 2012.
- Perez MI, Musini VM. Pharmacological interventions for hypertensive emergencies: a Cochrane systematic review. J Hum Hypertens. 2008;22(9):596-607.
- Vaughan CJ, Delanty N. Hypertensive emergencies. Lancet. 2000;356(9227):411-417.
- Stewart DL, Feinstein SE, Colgan R. Hypertensive urgencies and emergencies. Prim Care. 2006; 33(3):613-623.
- Atlas SA. The renin-angiotensin aldosterone system: pathophysiological role and pharmacologic inhibition. J Manag Care Pharm. 2007;13(8 suppl B):9-20.
- Flack JM. Epidemiology and unmet needs in hypertension. J Manag Care Pharm. 2007;13(e suppl B):2-8.
- Haas AR, Marik PE. Current diagnosis and management of hypertensive emergency. Semin Dial. 2006;19(6):502-512.
- Hebert CJ, Vidt DG. Hypertensive crises. Prim Care. 2008;35(3):475-487.
- Shulman KI, Fischer HD, Herrmann N, et al. Current prescription patterns and safety profile of irreversible monoamine oxidase inhibitors: a population-based cohort study of older adults. J Clin Psychiatry. 2009;70(12):1681-1696.
- Musso NR, Vergassola C, Pende A, Lotti G. Yohimbine effects on blood pressure and plasma catecholamines in human hypertension. Am J Hypertens. 1995;8(6):565-571.
- Baid S, Nieman LK. Glucocorticoid excess and hypertension. Curr Hypertens Rep. 2004;6(6): 493-499.
- Society of Critical Care Medicine. Fundamental Critical Care Support Course. www.sccm.org/ fccs_and_training_courses/fccs/pages/default .aspx. Accessed September 20, 2012.
- Sacco RL, Adams R, Albers G, et al. Guidelines for prevention of stroke in patients with ischemic stroke or transient ischemic attack: a statement for healthcare professionals from the American Heart Association/American Stroke Association Council on Stroke: co-sponsored by the Council on Cardiovascular Radiology and Intervention: the American Academy of Neurology affirms the value of this guideline. Stroke. 2006;37(2):577-617.
- Bernardini GL, Yavagal DR. Management of ischemic stroke: current concepts and treatment options. Hosp Physician. Sep 2006:13-23. www.turner-white.com/memberfile.php?PubCode=hp_sep06_is chemic.pdf. Accessed September 20, 2012.
- Varon J. Treatment of acute severe hypertension: current and newer agents. Drugs. 2008;68(3): 283-297.
- Webster J, Koch HF. Aspects of tolerability of centrally acting antihypertensive drugs. J Cardiovasc Pharmacol. 1996;27 suppl 3:S49-S54.
- Gupta PK, Gupta H, Khoynezhad A. Hypertensive emergency in aortic dissection and thoracic aortic aneurysm: a review of management. Pharmaceuticals. 2009;2(3):66-76.
- Post JB 4th, Frishman WH. Fenoldopam: a new dopamine agonist for the treatment of hypertensive urgencies and emergencies. J Clin Pharmacol. 1998;38(1):2-13.
- Suzuki S, Ohtsuka S, Ishikawa K, Yamaguchi I. Effects of nicardipine on coronary, vertebral and renal arterial flows in patients with essential hypertension. Hypertens Res. 2003;26(3):193-199.
- Anderson CS, Huang Y, Arima H, et al; INTERACT Investigators. Effects of early intensive blood pressure-lowering treatment on the growth of hematoma and perihematomal edema in acute intracerebral hemorrhage: the Intensive Blood Pressure Reduction in Acute Cerebral Haemorrhage Trial (INTERACT). Stroke. 2010;41(2):307-312.
- Broderick J, Connolly S, Feldmann E, et al. Quality of Care and Outcomes in Research Interdisciplinary Working Group Guidelines for the management of spontaneous intracerebral hemorrhage in adults: 2007 update: a guideline from the American Heart Association/American Stroke Association Stroke Council, High Blood Pressure Research Council, and the Quality of Care and Outcomes in Research Interdisciplinary Working Group. Circulation. 2007;116(16):e391-413.
- Morgenstern LB, Hemphill JC 3rd, Anderson C, et al. Guidelines for the management of spontaneous intracerebral hemorrhage: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2010;41(9):2108-2129.
- Brott T, Lu M, Kothari R, et al. Hypertension and its treatment in the NINDS rt-PA Stroke Trial. Stroke. 1998;29(8):1504-1509.
- Aiyagari V, Badruddin A. Management of hypertension in acute stroke. Expert Rev Cardiovasc Ther. 2009;7(6):637-646.
- Castillo J, Leira R, García MM, et al. Blood pressure decrease during the acute phase of ischemic stroke is associated with brain injury and poor stroke outcome. Stroke. 2004;35(2):520-526.
- Bonita R, Beaglehole R. The enigma of the decline in stroke deaths in the United States the search for an explanation. Stroke. 1996;27(3): 370-372.
- Adams HP Jr, del Zoppo G, Alberts MJ, et al. Guidelines for the early management of adults with ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council, Clinical Cardiology Council, Cardiovascular Radiology and Intervention Council, and the Atherosclerotic Peripheral Vascular Disease and Quality of Care Outcomes in Research Interdisciplinary Working Groups: the American Academy of Neurology affirms the value of this guideline as an educational tool for neurologists. Stroke. 2007;38(5):1655-1711.
- Heitsch L, Jauch EC. Management of hypertension in the setting of acute ischemic stroke. Curr Hypertens Rep. 2007;9(6):506-511.
- Barker FG II, Ogilvy CS. Efficacy of prophylactic nimodipine for delayed ischemic deficit after subarachnoid hemorrhage: a metaanalysis. J Neurosurg. 1996;84(3):405-414.