User login
ANSWER
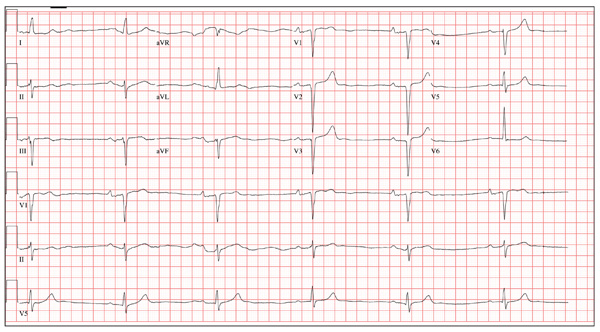
The correct interpretation includes marked sinus bradycardia with a first-degree atrioventricular (AV) block, left anterior fascicular block, and evidence of an anteroseptal MI. Marked sinus bradycardia is evidenced by a heart rate significantly less than 60 beats/min (in this case, almost half the rate). A first-degree AV block is apparent by the presence of a PR interval > 200 ms. The presence of a left anterior fascicular block (or left anterior hemiblock) includes a left-axis deviation between –45° and –90°, small Q waves with tall R waves in leads I and aVL, small R waves with deep S waves in leads II, III, and aVF, and a normal or slightly prolonged QRS duration. Finally, an anteroseptal MI is evident from the presence of deep S waves in leads V1 to V3.
The patient was directly admitted to the cardiology service for definitive workup and treatment.
ANSWER
The correct interpretation includes marked sinus bradycardia with a first-degree atrioventricular (AV) block, left anterior fascicular block, and evidence of an anteroseptal MI. Marked sinus bradycardia is evidenced by a heart rate significantly less than 60 beats/min (in this case, almost half the rate). A first-degree AV block is apparent by the presence of a PR interval > 200 ms. The presence of a left anterior fascicular block (or left anterior hemiblock) includes a left-axis deviation between –45° and –90°, small Q waves with tall R waves in leads I and aVL, small R waves with deep S waves in leads II, III, and aVF, and a normal or slightly prolonged QRS duration. Finally, an anteroseptal MI is evident from the presence of deep S waves in leads V1 to V3.
The patient was directly admitted to the cardiology service for definitive workup and treatment.
ANSWER
The correct interpretation includes marked sinus bradycardia with a first-degree atrioventricular (AV) block, left anterior fascicular block, and evidence of an anteroseptal MI. Marked sinus bradycardia is evidenced by a heart rate significantly less than 60 beats/min (in this case, almost half the rate). A first-degree AV block is apparent by the presence of a PR interval > 200 ms. The presence of a left anterior fascicular block (or left anterior hemiblock) includes a left-axis deviation between –45° and –90°, small Q waves with tall R waves in leads I and aVL, small R waves with deep S waves in leads II, III, and aVF, and a normal or slightly prolonged QRS duration. Finally, an anteroseptal MI is evident from the presence of deep S waves in leads V1 to V3.
The patient was directly admitted to the cardiology service for definitive workup and treatment.
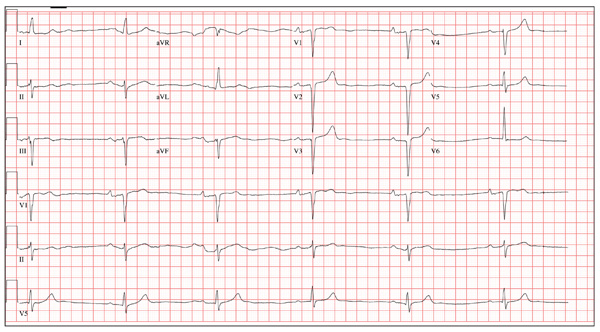
A 64-year-old man presents for follow-up to an appointment one month ago in which he reported a history of acute-onset shortness of breath, fatigue, and exercise intolerance. His health prior to that visit was described as “normal”; he had not seen a clinician since having his tonsils out at age 14. At the previous visit, a complete history documented that the patient is a rancher and farmer who makes his living from his crops and animals. He has never been married and lives out in the country. He has a history of several broken bones that he set himself, with no resultant sequelae. Aside from routine colds and flu, he has not been ill. He stopped smoking 10 years ago when it “got to be too expensive,” and he drinks one shot of whiskey at bedtime each night. He denies any drug allergies; he was taking no medications when he presented for that visit. A physical examination during that appointment revealed the presence of an irregularly irregular rhythm with a ventricular rate of 120 beats/min, a grade II/VI decrescendo diastolic murmur best heard at the right upper sternal border, a grade II/VI mid-systolic murmur best heard at the apex, a large point of maximum impulse (PMI) palpable at the anterior axillary line, and 3+ pitting edema to the level of the knees in both lower extremities. Subsequent workup, including an ECG, echocardiogram, chest x-ray, complete blood count, and chemistry panel, was performed—much to the patient’s displeasure. Pertinent results included a diagnosis of atrial fibrillation, a bicuspid aortic valve, aortic insufficiency, and mitral regurgitation. He was prescribed metoprolol and warfarin and referred to a cardiologist. During the current visit, you learn that he did not continue to take his warfarin, because his shortness of breath went away the day after the previous appointment. He states he doesn’t always remember to take his metoprolol, but when he does, he’ll often take enough to “catch up on” his dosage. He did not follow up with a cardiologist as scheduled. Additionally, he reveals that he experienced chest pain two weeks ago, which he describes as a “sharp, sticking” pain in his left chest. He did not come in because he thought he’d wait until this appointment to discuss it. He remembers being “all sweaty” when he had his chest pain, but adds that it hasn’t happened again. His review of symptoms is remarkable for fatigue since his chest pain. Physical exam reveals cardiac changes. His rhythm is now regular, but at a rate of 40 beats/min. His murmurs are unchanged from the previous visit. Another ECG is obtained, which reveals the following: a ventricular rate of 35 beats/min; PR interval, 258 ms; QRS duration, 116 ms; QT/QTc interval, 532/406 ms; P axis, 74°; R axis, –47°; and T axis, 45°. What is your interpretation of this ECG?