User login
ANSWER
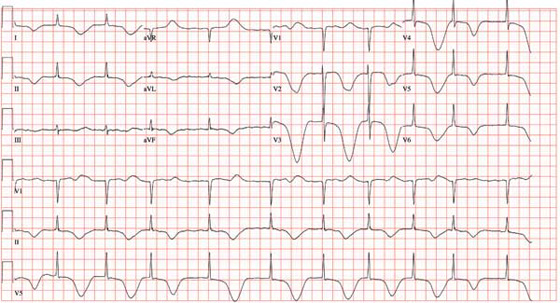
The ECG shows atrial fibrillation with a controlled ventricular response, a significantly prolonged QTc interval, and deep ST-T wave changes. The patient has chronic atrial fibrillation with a controlled ventricular response, so this arrhythmia is not unusual.
The deep ST-T wave changes and a prolonged QTc interval not seen on the previous ECG are consistent with a central nervous system injury. Cerebral disorders affect ventricular repolarization, as evidenced by depressed ST segments, flat or inverted T waves, and prolongation of the QTc interval. It is important to note that ST-segment elevations and deep T-wave changes do not always signify myocardial ischemia or injury.
This patient’s CT and MRI scans of the head showed no evidence of an intracranial bleed or cerebrovascular accident. A subsequent EEG showed epileptiform discharges, but no seizure activity.
The most likely cause of the ST-T wave changes is global intracranial hypoperfusion as a result of ventricular fibrillation with a prolonged resuscitation period. Over the course of the following two weeks, the ST-T wave changes and QTc prolongation normalized.
ANSWER
The ECG shows atrial fibrillation with a controlled ventricular response, a significantly prolonged QTc interval, and deep ST-T wave changes. The patient has chronic atrial fibrillation with a controlled ventricular response, so this arrhythmia is not unusual.
The deep ST-T wave changes and a prolonged QTc interval not seen on the previous ECG are consistent with a central nervous system injury. Cerebral disorders affect ventricular repolarization, as evidenced by depressed ST segments, flat or inverted T waves, and prolongation of the QTc interval. It is important to note that ST-segment elevations and deep T-wave changes do not always signify myocardial ischemia or injury.
This patient’s CT and MRI scans of the head showed no evidence of an intracranial bleed or cerebrovascular accident. A subsequent EEG showed epileptiform discharges, but no seizure activity.
The most likely cause of the ST-T wave changes is global intracranial hypoperfusion as a result of ventricular fibrillation with a prolonged resuscitation period. Over the course of the following two weeks, the ST-T wave changes and QTc prolongation normalized.
ANSWER
The ECG shows atrial fibrillation with a controlled ventricular response, a significantly prolonged QTc interval, and deep ST-T wave changes. The patient has chronic atrial fibrillation with a controlled ventricular response, so this arrhythmia is not unusual.
The deep ST-T wave changes and a prolonged QTc interval not seen on the previous ECG are consistent with a central nervous system injury. Cerebral disorders affect ventricular repolarization, as evidenced by depressed ST segments, flat or inverted T waves, and prolongation of the QTc interval. It is important to note that ST-segment elevations and deep T-wave changes do not always signify myocardial ischemia or injury.
This patient’s CT and MRI scans of the head showed no evidence of an intracranial bleed or cerebrovascular accident. A subsequent EEG showed epileptiform discharges, but no seizure activity.
The most likely cause of the ST-T wave changes is global intracranial hypoperfusion as a result of ventricular fibrillation with a prolonged resuscitation period. Over the course of the following two weeks, the ST-T wave changes and QTc prolongation normalized.
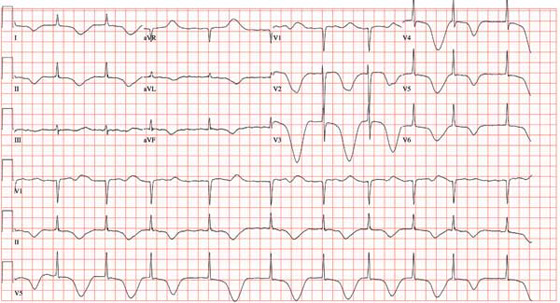
A 69-year-old man is found unconscious in a public park by a couple out for a walk. The husband tries to arouse the man to no avail; checking for a pulse and finding none, he asks his wife to call 911 while he begins CPR. His wife joins him after making the call, and they continue CPR for approximately 11 minutes, until paramedics arrive. An automatic external defibrillator is placed on the patient, who is found to be in ventricular fibrillation. The patient is intubated, and epinephrine and lidocaine are administered along with three shocks; the third restores the rhythm to normal sinus. The total resuscitation time is about 17 minutes. The patient is placed on a lidocaine drip and transported to the emergency department. On arrival, the man is unconscious but responsive to deep pain stimuli. An initial ECG shows atrial fibrillation with a controlled ventricular response. His serum troponin measures 2.7 µg/L and peaks at 3.1 µg/L. The medical record shows a history of coronary artery disease with coronary artery revascularization (left internal mammary artery–left anterior descending artery, saphenous vein graft–second diagonal artery) four years ago. The man also has a history of chronic atrial fibrillation, hypertension, hyperlipidemia, peptic ulcer disease, and a pulmonary embolus. The record also indicates that he smokes 1-1/2 packs of cigarettes per day, and drinks shots of tequila on weekends. Family history is remarkable for hypertension, diabetes, coronary artery disease, and breast cancer. He is allergic to aspirin (peptic ulcers), enalapril (cough), and penicillin. His most recent medication list includes atenolol, amlodipine, diltiazem, simvastatin, omeprazole, and warfarin. Because the patient is unconscious, a review of systems cannot be obtained. You assume care of the patient in the ICU. The nurse states that the patient’s vital signs were stable overnight, and there were no new arrhythmias. An abbreviated physical exam reveals no changes to his condition. The patient remains cool, sedated, and intubated. As you finish rounds, his nurse expresses concern that the patient has ongoing ischemia and asks you to review an ECG that was just obtained. The ECG shows the following: a ventricular rate of 62 beats/min; PR interval, indeterminate; QRS duration, 88 ms; QT/QTc interval, 718/728 ms; R axis, 35°; and T axis, 209°. What is your interpretation of this ECG, and what is the explanation for the dramatic changes overnight?