User login
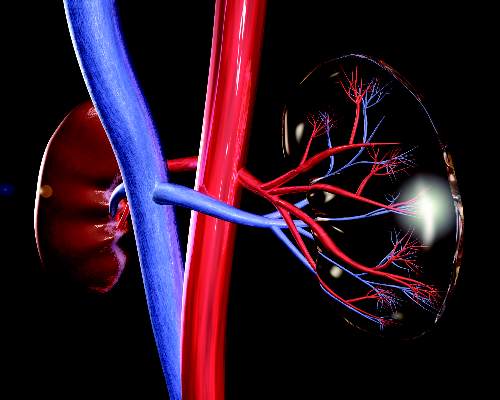
The International Myeloma Working Group has issued new recommendations for the diagnosis and management of multiple myeloma–related renal impairment. Depending on whether the condition is defined as elevated serum creatinine or decreased estimated glomerular filtration rate (eGFR), an estimated 20%-50% of patients with multiple myeloma have renal impairment at the time of diagnosis.
The guidelines recommend that all patients with multiple myeloma (MM) at diagnosis and at disease assessment should be tested for serum creatinine, eGFR, electrolytes, and serum free light chain, if available. Additionally, they recommend that all patients have urine electrophoresis of a sample from a 24-hour urine collection. All of the above are grade A recommendations (J Clin Oncol. 2016 Mar 14. doi: 10.1200/JCO.2015.65.0044).
Patients with nonselective proteinuria or significant albuminuria should undergo renal biopsy to determine the cause of the underlying impairment, the IMWG says (grade B recommendation).
For evaluation of eGFR in patients with stabilized serum creatinine, the IMWG favors the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation, but also acknowledges that eGFR can be assessed with the Modification of Diet in Renal Disease (MDRD) formula (grade A).
“CKD-EPI seems to more accurately reflect GFR than does MDRD, mostly in higher levels of GFR,” the IMWG wrote.
Because the reversibility of renal dysfunction can affect treatment choice, the recommendations noted that for patients on dialysis, achieving independence from dialysis is “strong indication of improvement. For all other patients, IMWG criteria for renal response to therapy are recommended (grade B).
Management
“Acute renal impairment is a myeloma emergency. Diagnosis should be established as fast as possible, and antimyeloma therapy should be started immediately after confirmation of diagnosis to rapidly restore renal function,” working group members wrote.
Supportive care with increased hydration – at least 3 liters per day – is “mandatory” for all with suspected MM-related renal impairment, they add.
The recommendations also noted that antimyeloma therapy should be initiated immediately to reduce the load of toxic serum free light chains, which can help to improve renal function.
“Bortezomib [Velcade]-based regimens remain the cornerstone of the management of myeloma-related renal impairment (grade A). High-dose dexamethasone should be administered at least for the first month of therapy (grade B),” the working group members wrote.
Lenalidomide (Revlimid) can be given, but because it is excreted through the kidneys, the dose must be adjusted according to the degree of renal impairment. In contrast, thalidomide is not excreted and does not require dose modification in this population.
Patients who are eligible for autologous stem cell transplant could receive bortezomib in a three-drug regimen with thalidomide and dexamethasone, or in combination with a conventional chemotherapeutic agent, either doxorubicin or cyclophosphamide. Patients who are not eligible for transplant can be treated with bortezomib, melphalan, and prednisone, the recommendations said, but add that there are no data on the use of this regimen in patients who are on dialysis.
Regarding newer proteasome inhibitors, the guidelines note that carfilzomib (Kyprolis) can be given safely to patients with creatinine clearance above 15 mL/min, and that the recently approved oral agent, ixazomib (Ninlaro), with lenalidomide and dexamethasone can be administered to patients with clearance rates above 30 mL/min (grade A).
The International Myeloma Working Group has issued new recommendations for the diagnosis and management of multiple myeloma–related renal impairment. Depending on whether the condition is defined as elevated serum creatinine or decreased estimated glomerular filtration rate (eGFR), an estimated 20%-50% of patients with multiple myeloma have renal impairment at the time of diagnosis.
The guidelines recommend that all patients with multiple myeloma (MM) at diagnosis and at disease assessment should be tested for serum creatinine, eGFR, electrolytes, and serum free light chain, if available. Additionally, they recommend that all patients have urine electrophoresis of a sample from a 24-hour urine collection. All of the above are grade A recommendations (J Clin Oncol. 2016 Mar 14. doi: 10.1200/JCO.2015.65.0044).
Patients with nonselective proteinuria or significant albuminuria should undergo renal biopsy to determine the cause of the underlying impairment, the IMWG says (grade B recommendation).
For evaluation of eGFR in patients with stabilized serum creatinine, the IMWG favors the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation, but also acknowledges that eGFR can be assessed with the Modification of Diet in Renal Disease (MDRD) formula (grade A).
“CKD-EPI seems to more accurately reflect GFR than does MDRD, mostly in higher levels of GFR,” the IMWG wrote.
Because the reversibility of renal dysfunction can affect treatment choice, the recommendations noted that for patients on dialysis, achieving independence from dialysis is “strong indication of improvement. For all other patients, IMWG criteria for renal response to therapy are recommended (grade B).
Management
“Acute renal impairment is a myeloma emergency. Diagnosis should be established as fast as possible, and antimyeloma therapy should be started immediately after confirmation of diagnosis to rapidly restore renal function,” working group members wrote.
Supportive care with increased hydration – at least 3 liters per day – is “mandatory” for all with suspected MM-related renal impairment, they add.
The recommendations also noted that antimyeloma therapy should be initiated immediately to reduce the load of toxic serum free light chains, which can help to improve renal function.
“Bortezomib [Velcade]-based regimens remain the cornerstone of the management of myeloma-related renal impairment (grade A). High-dose dexamethasone should be administered at least for the first month of therapy (grade B),” the working group members wrote.
Lenalidomide (Revlimid) can be given, but because it is excreted through the kidneys, the dose must be adjusted according to the degree of renal impairment. In contrast, thalidomide is not excreted and does not require dose modification in this population.
Patients who are eligible for autologous stem cell transplant could receive bortezomib in a three-drug regimen with thalidomide and dexamethasone, or in combination with a conventional chemotherapeutic agent, either doxorubicin or cyclophosphamide. Patients who are not eligible for transplant can be treated with bortezomib, melphalan, and prednisone, the recommendations said, but add that there are no data on the use of this regimen in patients who are on dialysis.
Regarding newer proteasome inhibitors, the guidelines note that carfilzomib (Kyprolis) can be given safely to patients with creatinine clearance above 15 mL/min, and that the recently approved oral agent, ixazomib (Ninlaro), with lenalidomide and dexamethasone can be administered to patients with clearance rates above 30 mL/min (grade A).
The International Myeloma Working Group has issued new recommendations for the diagnosis and management of multiple myeloma–related renal impairment. Depending on whether the condition is defined as elevated serum creatinine or decreased estimated glomerular filtration rate (eGFR), an estimated 20%-50% of patients with multiple myeloma have renal impairment at the time of diagnosis.
The guidelines recommend that all patients with multiple myeloma (MM) at diagnosis and at disease assessment should be tested for serum creatinine, eGFR, electrolytes, and serum free light chain, if available. Additionally, they recommend that all patients have urine electrophoresis of a sample from a 24-hour urine collection. All of the above are grade A recommendations (J Clin Oncol. 2016 Mar 14. doi: 10.1200/JCO.2015.65.0044).
Patients with nonselective proteinuria or significant albuminuria should undergo renal biopsy to determine the cause of the underlying impairment, the IMWG says (grade B recommendation).
For evaluation of eGFR in patients with stabilized serum creatinine, the IMWG favors the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation, but also acknowledges that eGFR can be assessed with the Modification of Diet in Renal Disease (MDRD) formula (grade A).
“CKD-EPI seems to more accurately reflect GFR than does MDRD, mostly in higher levels of GFR,” the IMWG wrote.
Because the reversibility of renal dysfunction can affect treatment choice, the recommendations noted that for patients on dialysis, achieving independence from dialysis is “strong indication of improvement. For all other patients, IMWG criteria for renal response to therapy are recommended (grade B).
Management
“Acute renal impairment is a myeloma emergency. Diagnosis should be established as fast as possible, and antimyeloma therapy should be started immediately after confirmation of diagnosis to rapidly restore renal function,” working group members wrote.
Supportive care with increased hydration – at least 3 liters per day – is “mandatory” for all with suspected MM-related renal impairment, they add.
The recommendations also noted that antimyeloma therapy should be initiated immediately to reduce the load of toxic serum free light chains, which can help to improve renal function.
“Bortezomib [Velcade]-based regimens remain the cornerstone of the management of myeloma-related renal impairment (grade A). High-dose dexamethasone should be administered at least for the first month of therapy (grade B),” the working group members wrote.
Lenalidomide (Revlimid) can be given, but because it is excreted through the kidneys, the dose must be adjusted according to the degree of renal impairment. In contrast, thalidomide is not excreted and does not require dose modification in this population.
Patients who are eligible for autologous stem cell transplant could receive bortezomib in a three-drug regimen with thalidomide and dexamethasone, or in combination with a conventional chemotherapeutic agent, either doxorubicin or cyclophosphamide. Patients who are not eligible for transplant can be treated with bortezomib, melphalan, and prednisone, the recommendations said, but add that there are no data on the use of this regimen in patients who are on dialysis.
Regarding newer proteasome inhibitors, the guidelines note that carfilzomib (Kyprolis) can be given safely to patients with creatinine clearance above 15 mL/min, and that the recently approved oral agent, ixazomib (Ninlaro), with lenalidomide and dexamethasone can be administered to patients with clearance rates above 30 mL/min (grade A).
FROM JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: All patients diagnosed with multiple myeloma should be evaluated for renal impairment.
Major finding: Bortezomib-based regimens are the standard of care for patients with multiple myeloma.
Data source: Evidence-based clinical recommendations.
Disclosures: Many coauthors disclosed multiple relationships with companies that make antimyeloma therapies and other medications.