User login
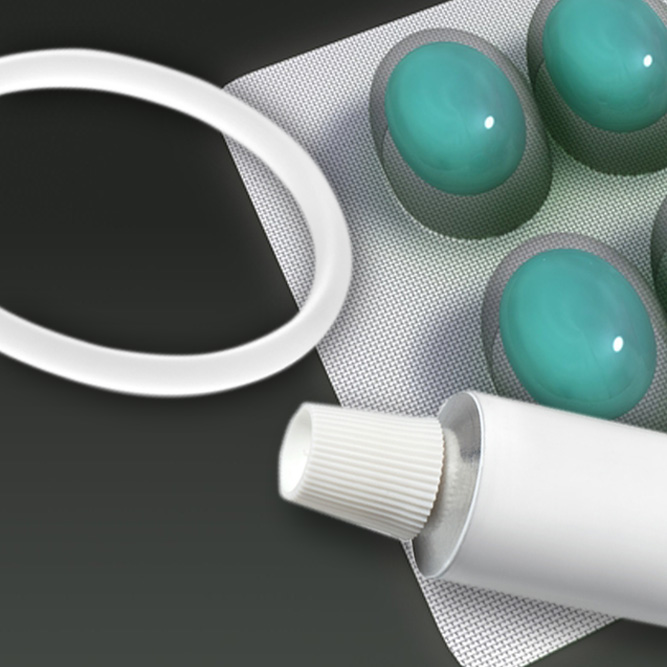
As estrogen levels decline, postmenopausal women commonly experience uncomfortable and distressing symptoms of genital atrophy, or genitourinary syndrome of menopause (GSM). Moreover, aromatase inhibitors (AIs), increasingly used as adjuvant therapy by menopausal breast cancer survivors, contribute to vaginal dryness and sexual pain. This discussion focuses on studies of several local vaginal treatments (including a recently approved agent) that ameliorate GSM symptoms but do not appreciably raise serum sex steroid levels—reassuring data for certain patient populations.
EXPERT COMMENTARY
Andrew M. Kaunitz, MD, is University of Florida Research Foundation Professor and Associate Chairman, Department of Obstetrics and Gynecology, University of Florida College of Medicine–Jacksonville. He is the Medical Director and Director of Menopause and Gynecologic Ultrasound Services, UF Women’s Health Specialists–Emerson. Dr. Kaunitz serves on the OBG Management Board of Editors.
Dr. Kaunitz reports that in 2015 he served on a contraception advisory board for Pfizer, which markets the low-dose estradiol vaginal ring.
Read expert commentary from Dr. Kaunitz
For women with early-stage breast cancer receiving an AI, is a vaginal estradiol ring or testosterone cream safe for genital atrophy?
Yes, according to results of a randomized, noncomparative short-term trial that found both agents improved vaginal dryness and sexual dysfunction and had little tendency to persistently elevate serum estradiol levels
Melisko ME, Goldman ME, Hwang J, et al. Vaginal testosterone cream vs estradiol vaginal ring for vaginal dryness or decreased libido in women receiving aromatase inhibitors for early-stage breast cancer: a randomized clinical trial [published online ahead of print November 10, 2016]. JAMA Oncol. doi: 10.1001/jamaoncol.2016.3904.
Long-term adjuvant AI therapy, which often causes vaginal dryness and sexual dysfunction, is recommended for postmenopausal women with hormone receptor-positive breast cancer. Although use of a vaginally administered low-dose 3-month estradiol ring as well as compounded testosterone cream is known to improve menopausal genital atrophy and sexual symptoms, little data address these agents' impact on serum estradiol levels in women using AIs.
In a safety evaluation study of these treatments performed at an academic US cancer center, Melisko and colleagues randomly assigned postmenopausal women with hormone receptor-positive breast cancer who reported vaginal dryness, sexual pain, or reduced sexual desire to 12 weeks of off-label treatment with an estradiol vaginal ring or intravaginal testosterone cream.
Related article:
Does extending aromatase-inhibitor use from 5 to 10 years benefit menopausal women with hormone-positive breast cancer?
Details of the study
Among 68 evaluable women (mean age, 56 years), mean baseline estradiol levels were 20 pg/mL (range, <2 to 127 pg/mL); estradiol levels were above the postmenopausal range (>10 pg/mL) in 37% of participants. During the 12-week trial, transient and persistent estradiol levels above this threshold were noted, respectively, in 4 and 0 women treated with the vaginal ring and in 4 and 4 women treated with testosterone cream. Estradiol levels assessed using commercially available (liquid chromatography and mass spectrometry) and research laboratory (radioimmune assay) methodology yielded similar results. In the testosterone cream group, persistent elevations above the normal postmenopausal range were common.
Atrophic vaginal changes, sexual desire, and sexual dysfunction improved in both treatment groups based on gynecologic examinations and sexual quality-of-life questionnaires completed at baseline and week 12.
The authors indicated that their current practice is to continue the estradiol vaginal ring or testosterone cream in AI users who experience symptomatic improvement with these formulations. They check serum estradiol levels every few months. A future large, long-term trial assessing the impact of off-label use of the estradiol vaginal ring on the incidence of recurrent disease in breast cancer survivors would provide definitive evidence of this treatment's safety.
--Andrew M. Kaunitz, MD
Read on for Dr. Kaunitz’s comments on a new dyspareunia treatment
What's new for the treatment of dyspareunia associated with GSM?
Intrarosa, a once-daily vaginal insert containing prasterone as the active ingredient, was recently approved for the treatment of moderate to severe dyspareunia, a symptom of vulvar and vaginal atrophy due to menopause
FDA approves Intrarosa for postmenopausal women experiencing pain during sex [news release]. Silver Spring, MD: US Food and Drug Administration; November 17, 2016. http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm529641.htm. Accessed December 19, 2017.
Intrarosa [package insert]. Quebec City, Canada: Endoceutics Inc; 2016.
On November 17, 2016, the US Food and Drug Administration (FDA) approved Intrarosa, vaginal dehydroepiandrosterone (DHEA)--also known as prasterone--for women experiencing moderate to severe pain during sexual intercourse due to menopause-related genital atrophy, or GSM. In clinical trials, daily treatment with a 6.5-mg vaginal ovule of DHEA was found effective in reducing symptoms of atrophy. Vaginal discharge was the most common adverse effect.
After menopause, DHEA, which is produced largely by the adrenal glands, represents the dominant source of all sex steroids. DHEA is enzymatically transformed at the intracellular level into estrogens. Because estradiol is inactivated at the site of its synthesis, use of vaginal DHEA causes little if any rise in serum estradiol levels.1,2
Related article:
2014 Update on Fertility
Details of 2 studies
A pivotal randomized, double-blind, placebo-controlled phase 3 trial of intravaginal DHEA (6.5 mg daily) for treating postmenopausal dyspareunia in women with vulvovaginal atrophy was conducted over 12 weeks.1 The trial included 325 women treated with DHEA and 157 who received placebo.
All 4 coprimary objectives measured improved with treatment compared with mean baseline levels: percentage of parabasal cells in treated participants decreased by 27.7% over placebo (P<.0001); percentage of superficial cells increased by 8.44% over placebo (P<.0001); vaginal pH decreased by 0.66 pH unit over placebo (P<.0001); and pain with sexual activity decreased by 1.42 severity score unit from baseline or 0.36 unit over placebo (P = .0002). In addition, participant-reported moderate to severe vaginal dryness (present in 84% of women at baseline) improved considerably at 12 weeks, and gynecologic evaluation revealed improvements in vaginal secretions, epithelial integrity and surface thickness, and color.1
About 6% of participants reported vaginal discharge as an adverse effect. Levels of serum steroids remained within the normal range for postmenopausal women.1
Another study, in which authors integrated data from four phase 3 clinical trials of postmenopausal women with vulvovaginal atrophy treated with vaginal DHEA (n = 723) or placebo (n = 266) for 12 weeks, analyzed serum steroid levels measured at Day 1 and Week 12 by liquid chromatography-tandem mass spectrometry.2
At 12 weeks' treatment, mean levels of the most relevant sex steroid, serum estradiol, was noted to be 3.36 pg/mL, 19% below the normal postmenopausal value of 4.17 pg/mL.The mean level of estrone sulfate was noted to be 209 pg/mL, lower than the normal 220 pg/mL level in postmenopausal women. Further, androsterone glucuronide, the primary metabolite of androgens, also remained well within normal postmenopausal values.2
The authors concluded that the study data demonstrate that a daily 6.5-mg dose of intravaginal DHEA in postmenopausal women achieves the desired local efficacy (ie, amelioration of vulvovaginal atrophy symptoms) without systemic sex steroid exposure.2
The new information detailed in this article indicates that the recently FDA-approved vaginal DHEA (prasterone) ovules, as well as the 3-month low-dose estradiol vaginal ring, improve symptoms of genital atrophy without causing appreciable elevations in serum estradiol levels. This will be welcome news for all women with symptomatic genital atrophy, including those who have been treated for estrogen-sensitive cancers. Clinicians should be aware that, although package labeling for vaginal prasterone does not list a history of breast cancer as a contraindication, a history of breast cancer is listed in the Warning and Precautions section of package labeling, noting that this medication has not been studied in women with a history of breast cancer.
-- Andrew M. Kaunitz, MD
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
- Labrie F, Archer DF, Koltun W, et al; VVA Prasterone Research Group. Efficacy of intravaginal dehydroepiandrosterone (DHEA) on moderate to severe dyspareunia and vaginal dryness, symptoms of vulvovaginal atrophy, and of the genitourinary syndrome of menopause. Menopause. 2016;23(3):243–256.
- Martel C, Labrie F, Archer DF, et al; Prasterone Clinical Research Group. Serum steroid concentrations remain within normal postmenopausal values in women receiving daily 6.5 mg intravaginal prasterone for 12 weeks. J Steroid Biochem Mol Biol. 2016;159:142–153.
As estrogen levels decline, postmenopausal women commonly experience uncomfortable and distressing symptoms of genital atrophy, or genitourinary syndrome of menopause (GSM). Moreover, aromatase inhibitors (AIs), increasingly used as adjuvant therapy by menopausal breast cancer survivors, contribute to vaginal dryness and sexual pain. This discussion focuses on studies of several local vaginal treatments (including a recently approved agent) that ameliorate GSM symptoms but do not appreciably raise serum sex steroid levels—reassuring data for certain patient populations.
EXPERT COMMENTARY
Andrew M. Kaunitz, MD, is University of Florida Research Foundation Professor and Associate Chairman, Department of Obstetrics and Gynecology, University of Florida College of Medicine–Jacksonville. He is the Medical Director and Director of Menopause and Gynecologic Ultrasound Services, UF Women’s Health Specialists–Emerson. Dr. Kaunitz serves on the OBG Management Board of Editors.
Dr. Kaunitz reports that in 2015 he served on a contraception advisory board for Pfizer, which markets the low-dose estradiol vaginal ring.
Read expert commentary from Dr. Kaunitz
For women with early-stage breast cancer receiving an AI, is a vaginal estradiol ring or testosterone cream safe for genital atrophy?
Yes, according to results of a randomized, noncomparative short-term trial that found both agents improved vaginal dryness and sexual dysfunction and had little tendency to persistently elevate serum estradiol levels
Melisko ME, Goldman ME, Hwang J, et al. Vaginal testosterone cream vs estradiol vaginal ring for vaginal dryness or decreased libido in women receiving aromatase inhibitors for early-stage breast cancer: a randomized clinical trial [published online ahead of print November 10, 2016]. JAMA Oncol. doi: 10.1001/jamaoncol.2016.3904.
Long-term adjuvant AI therapy, which often causes vaginal dryness and sexual dysfunction, is recommended for postmenopausal women with hormone receptor-positive breast cancer. Although use of a vaginally administered low-dose 3-month estradiol ring as well as compounded testosterone cream is known to improve menopausal genital atrophy and sexual symptoms, little data address these agents' impact on serum estradiol levels in women using AIs.
In a safety evaluation study of these treatments performed at an academic US cancer center, Melisko and colleagues randomly assigned postmenopausal women with hormone receptor-positive breast cancer who reported vaginal dryness, sexual pain, or reduced sexual desire to 12 weeks of off-label treatment with an estradiol vaginal ring or intravaginal testosterone cream.
Related article:
Does extending aromatase-inhibitor use from 5 to 10 years benefit menopausal women with hormone-positive breast cancer?
Details of the study
Among 68 evaluable women (mean age, 56 years), mean baseline estradiol levels were 20 pg/mL (range, <2 to 127 pg/mL); estradiol levels were above the postmenopausal range (>10 pg/mL) in 37% of participants. During the 12-week trial, transient and persistent estradiol levels above this threshold were noted, respectively, in 4 and 0 women treated with the vaginal ring and in 4 and 4 women treated with testosterone cream. Estradiol levels assessed using commercially available (liquid chromatography and mass spectrometry) and research laboratory (radioimmune assay) methodology yielded similar results. In the testosterone cream group, persistent elevations above the normal postmenopausal range were common.
Atrophic vaginal changes, sexual desire, and sexual dysfunction improved in both treatment groups based on gynecologic examinations and sexual quality-of-life questionnaires completed at baseline and week 12.
The authors indicated that their current practice is to continue the estradiol vaginal ring or testosterone cream in AI users who experience symptomatic improvement with these formulations. They check serum estradiol levels every few months. A future large, long-term trial assessing the impact of off-label use of the estradiol vaginal ring on the incidence of recurrent disease in breast cancer survivors would provide definitive evidence of this treatment's safety.
--Andrew M. Kaunitz, MD
Read on for Dr. Kaunitz’s comments on a new dyspareunia treatment
What's new for the treatment of dyspareunia associated with GSM?
Intrarosa, a once-daily vaginal insert containing prasterone as the active ingredient, was recently approved for the treatment of moderate to severe dyspareunia, a symptom of vulvar and vaginal atrophy due to menopause
FDA approves Intrarosa for postmenopausal women experiencing pain during sex [news release]. Silver Spring, MD: US Food and Drug Administration; November 17, 2016. http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm529641.htm. Accessed December 19, 2017.
Intrarosa [package insert]. Quebec City, Canada: Endoceutics Inc; 2016.
On November 17, 2016, the US Food and Drug Administration (FDA) approved Intrarosa, vaginal dehydroepiandrosterone (DHEA)--also known as prasterone--for women experiencing moderate to severe pain during sexual intercourse due to menopause-related genital atrophy, or GSM. In clinical trials, daily treatment with a 6.5-mg vaginal ovule of DHEA was found effective in reducing symptoms of atrophy. Vaginal discharge was the most common adverse effect.
After menopause, DHEA, which is produced largely by the adrenal glands, represents the dominant source of all sex steroids. DHEA is enzymatically transformed at the intracellular level into estrogens. Because estradiol is inactivated at the site of its synthesis, use of vaginal DHEA causes little if any rise in serum estradiol levels.1,2
Related article:
2014 Update on Fertility
Details of 2 studies
A pivotal randomized, double-blind, placebo-controlled phase 3 trial of intravaginal DHEA (6.5 mg daily) for treating postmenopausal dyspareunia in women with vulvovaginal atrophy was conducted over 12 weeks.1 The trial included 325 women treated with DHEA and 157 who received placebo.
All 4 coprimary objectives measured improved with treatment compared with mean baseline levels: percentage of parabasal cells in treated participants decreased by 27.7% over placebo (P<.0001); percentage of superficial cells increased by 8.44% over placebo (P<.0001); vaginal pH decreased by 0.66 pH unit over placebo (P<.0001); and pain with sexual activity decreased by 1.42 severity score unit from baseline or 0.36 unit over placebo (P = .0002). In addition, participant-reported moderate to severe vaginal dryness (present in 84% of women at baseline) improved considerably at 12 weeks, and gynecologic evaluation revealed improvements in vaginal secretions, epithelial integrity and surface thickness, and color.1
About 6% of participants reported vaginal discharge as an adverse effect. Levels of serum steroids remained within the normal range for postmenopausal women.1
Another study, in which authors integrated data from four phase 3 clinical trials of postmenopausal women with vulvovaginal atrophy treated with vaginal DHEA (n = 723) or placebo (n = 266) for 12 weeks, analyzed serum steroid levels measured at Day 1 and Week 12 by liquid chromatography-tandem mass spectrometry.2
At 12 weeks' treatment, mean levels of the most relevant sex steroid, serum estradiol, was noted to be 3.36 pg/mL, 19% below the normal postmenopausal value of 4.17 pg/mL.The mean level of estrone sulfate was noted to be 209 pg/mL, lower than the normal 220 pg/mL level in postmenopausal women. Further, androsterone glucuronide, the primary metabolite of androgens, also remained well within normal postmenopausal values.2
The authors concluded that the study data demonstrate that a daily 6.5-mg dose of intravaginal DHEA in postmenopausal women achieves the desired local efficacy (ie, amelioration of vulvovaginal atrophy symptoms) without systemic sex steroid exposure.2
The new information detailed in this article indicates that the recently FDA-approved vaginal DHEA (prasterone) ovules, as well as the 3-month low-dose estradiol vaginal ring, improve symptoms of genital atrophy without causing appreciable elevations in serum estradiol levels. This will be welcome news for all women with symptomatic genital atrophy, including those who have been treated for estrogen-sensitive cancers. Clinicians should be aware that, although package labeling for vaginal prasterone does not list a history of breast cancer as a contraindication, a history of breast cancer is listed in the Warning and Precautions section of package labeling, noting that this medication has not been studied in women with a history of breast cancer.
-- Andrew M. Kaunitz, MD
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
As estrogen levels decline, postmenopausal women commonly experience uncomfortable and distressing symptoms of genital atrophy, or genitourinary syndrome of menopause (GSM). Moreover, aromatase inhibitors (AIs), increasingly used as adjuvant therapy by menopausal breast cancer survivors, contribute to vaginal dryness and sexual pain. This discussion focuses on studies of several local vaginal treatments (including a recently approved agent) that ameliorate GSM symptoms but do not appreciably raise serum sex steroid levels—reassuring data for certain patient populations.
EXPERT COMMENTARY
Andrew M. Kaunitz, MD, is University of Florida Research Foundation Professor and Associate Chairman, Department of Obstetrics and Gynecology, University of Florida College of Medicine–Jacksonville. He is the Medical Director and Director of Menopause and Gynecologic Ultrasound Services, UF Women’s Health Specialists–Emerson. Dr. Kaunitz serves on the OBG Management Board of Editors.
Dr. Kaunitz reports that in 2015 he served on a contraception advisory board for Pfizer, which markets the low-dose estradiol vaginal ring.
Read expert commentary from Dr. Kaunitz
For women with early-stage breast cancer receiving an AI, is a vaginal estradiol ring or testosterone cream safe for genital atrophy?
Yes, according to results of a randomized, noncomparative short-term trial that found both agents improved vaginal dryness and sexual dysfunction and had little tendency to persistently elevate serum estradiol levels
Melisko ME, Goldman ME, Hwang J, et al. Vaginal testosterone cream vs estradiol vaginal ring for vaginal dryness or decreased libido in women receiving aromatase inhibitors for early-stage breast cancer: a randomized clinical trial [published online ahead of print November 10, 2016]. JAMA Oncol. doi: 10.1001/jamaoncol.2016.3904.
Long-term adjuvant AI therapy, which often causes vaginal dryness and sexual dysfunction, is recommended for postmenopausal women with hormone receptor-positive breast cancer. Although use of a vaginally administered low-dose 3-month estradiol ring as well as compounded testosterone cream is known to improve menopausal genital atrophy and sexual symptoms, little data address these agents' impact on serum estradiol levels in women using AIs.
In a safety evaluation study of these treatments performed at an academic US cancer center, Melisko and colleagues randomly assigned postmenopausal women with hormone receptor-positive breast cancer who reported vaginal dryness, sexual pain, or reduced sexual desire to 12 weeks of off-label treatment with an estradiol vaginal ring or intravaginal testosterone cream.
Related article:
Does extending aromatase-inhibitor use from 5 to 10 years benefit menopausal women with hormone-positive breast cancer?
Details of the study
Among 68 evaluable women (mean age, 56 years), mean baseline estradiol levels were 20 pg/mL (range, <2 to 127 pg/mL); estradiol levels were above the postmenopausal range (>10 pg/mL) in 37% of participants. During the 12-week trial, transient and persistent estradiol levels above this threshold were noted, respectively, in 4 and 0 women treated with the vaginal ring and in 4 and 4 women treated with testosterone cream. Estradiol levels assessed using commercially available (liquid chromatography and mass spectrometry) and research laboratory (radioimmune assay) methodology yielded similar results. In the testosterone cream group, persistent elevations above the normal postmenopausal range were common.
Atrophic vaginal changes, sexual desire, and sexual dysfunction improved in both treatment groups based on gynecologic examinations and sexual quality-of-life questionnaires completed at baseline and week 12.
The authors indicated that their current practice is to continue the estradiol vaginal ring or testosterone cream in AI users who experience symptomatic improvement with these formulations. They check serum estradiol levels every few months. A future large, long-term trial assessing the impact of off-label use of the estradiol vaginal ring on the incidence of recurrent disease in breast cancer survivors would provide definitive evidence of this treatment's safety.
--Andrew M. Kaunitz, MD
Read on for Dr. Kaunitz’s comments on a new dyspareunia treatment
What's new for the treatment of dyspareunia associated with GSM?
Intrarosa, a once-daily vaginal insert containing prasterone as the active ingredient, was recently approved for the treatment of moderate to severe dyspareunia, a symptom of vulvar and vaginal atrophy due to menopause
FDA approves Intrarosa for postmenopausal women experiencing pain during sex [news release]. Silver Spring, MD: US Food and Drug Administration; November 17, 2016. http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm529641.htm. Accessed December 19, 2017.
Intrarosa [package insert]. Quebec City, Canada: Endoceutics Inc; 2016.
On November 17, 2016, the US Food and Drug Administration (FDA) approved Intrarosa, vaginal dehydroepiandrosterone (DHEA)--also known as prasterone--for women experiencing moderate to severe pain during sexual intercourse due to menopause-related genital atrophy, or GSM. In clinical trials, daily treatment with a 6.5-mg vaginal ovule of DHEA was found effective in reducing symptoms of atrophy. Vaginal discharge was the most common adverse effect.
After menopause, DHEA, which is produced largely by the adrenal glands, represents the dominant source of all sex steroids. DHEA is enzymatically transformed at the intracellular level into estrogens. Because estradiol is inactivated at the site of its synthesis, use of vaginal DHEA causes little if any rise in serum estradiol levels.1,2
Related article:
2014 Update on Fertility
Details of 2 studies
A pivotal randomized, double-blind, placebo-controlled phase 3 trial of intravaginal DHEA (6.5 mg daily) for treating postmenopausal dyspareunia in women with vulvovaginal atrophy was conducted over 12 weeks.1 The trial included 325 women treated with DHEA and 157 who received placebo.
All 4 coprimary objectives measured improved with treatment compared with mean baseline levels: percentage of parabasal cells in treated participants decreased by 27.7% over placebo (P<.0001); percentage of superficial cells increased by 8.44% over placebo (P<.0001); vaginal pH decreased by 0.66 pH unit over placebo (P<.0001); and pain with sexual activity decreased by 1.42 severity score unit from baseline or 0.36 unit over placebo (P = .0002). In addition, participant-reported moderate to severe vaginal dryness (present in 84% of women at baseline) improved considerably at 12 weeks, and gynecologic evaluation revealed improvements in vaginal secretions, epithelial integrity and surface thickness, and color.1
About 6% of participants reported vaginal discharge as an adverse effect. Levels of serum steroids remained within the normal range for postmenopausal women.1
Another study, in which authors integrated data from four phase 3 clinical trials of postmenopausal women with vulvovaginal atrophy treated with vaginal DHEA (n = 723) or placebo (n = 266) for 12 weeks, analyzed serum steroid levels measured at Day 1 and Week 12 by liquid chromatography-tandem mass spectrometry.2
At 12 weeks' treatment, mean levels of the most relevant sex steroid, serum estradiol, was noted to be 3.36 pg/mL, 19% below the normal postmenopausal value of 4.17 pg/mL.The mean level of estrone sulfate was noted to be 209 pg/mL, lower than the normal 220 pg/mL level in postmenopausal women. Further, androsterone glucuronide, the primary metabolite of androgens, also remained well within normal postmenopausal values.2
The authors concluded that the study data demonstrate that a daily 6.5-mg dose of intravaginal DHEA in postmenopausal women achieves the desired local efficacy (ie, amelioration of vulvovaginal atrophy symptoms) without systemic sex steroid exposure.2
The new information detailed in this article indicates that the recently FDA-approved vaginal DHEA (prasterone) ovules, as well as the 3-month low-dose estradiol vaginal ring, improve symptoms of genital atrophy without causing appreciable elevations in serum estradiol levels. This will be welcome news for all women with symptomatic genital atrophy, including those who have been treated for estrogen-sensitive cancers. Clinicians should be aware that, although package labeling for vaginal prasterone does not list a history of breast cancer as a contraindication, a history of breast cancer is listed in the Warning and Precautions section of package labeling, noting that this medication has not been studied in women with a history of breast cancer.
-- Andrew M. Kaunitz, MD
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
- Labrie F, Archer DF, Koltun W, et al; VVA Prasterone Research Group. Efficacy of intravaginal dehydroepiandrosterone (DHEA) on moderate to severe dyspareunia and vaginal dryness, symptoms of vulvovaginal atrophy, and of the genitourinary syndrome of menopause. Menopause. 2016;23(3):243–256.
- Martel C, Labrie F, Archer DF, et al; Prasterone Clinical Research Group. Serum steroid concentrations remain within normal postmenopausal values in women receiving daily 6.5 mg intravaginal prasterone for 12 weeks. J Steroid Biochem Mol Biol. 2016;159:142–153.
- Labrie F, Archer DF, Koltun W, et al; VVA Prasterone Research Group. Efficacy of intravaginal dehydroepiandrosterone (DHEA) on moderate to severe dyspareunia and vaginal dryness, symptoms of vulvovaginal atrophy, and of the genitourinary syndrome of menopause. Menopause. 2016;23(3):243–256.
- Martel C, Labrie F, Archer DF, et al; Prasterone Clinical Research Group. Serum steroid concentrations remain within normal postmenopausal values in women receiving daily 6.5 mg intravaginal prasterone for 12 weeks. J Steroid Biochem Mol Biol. 2016;159:142–153.