User login
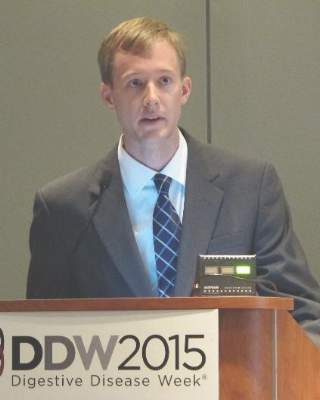
WASHINGTON – Initial misdiagnoses were common and were associated with a later disease stage at diagnosis, in a study of 313 patients diagnosed with pancreatic cancer, Dr. Douglas Swords said at the annual Digestive Disease Week.
“By far, the most common misdiagnosis was gallbladder disease,” and there was about a 3-month longer time period, on average, from the first visit to a physician to the actual cancer diagnosis, in patients who were initially misdiagnosed, said Dr. Swords, a surgery resident at the University of Utah, Salt Lake City.
In the series of 313 patients diagnosed with pancreatic cancer, 98 (31.3%) were initially misdiagnosed, with a total of 119 diagnoses other than pancreatic cancer, he said. The most common misdiagnosis was gallbladder disease, which led to a cholecystectomy in 38 cases, followed by gastroesophageal reflux disease in 15 cases, and peptic ulcer disease in 11 cases. Those initially misdiagnosed were an average of about 5 years younger.
Patients with an initial misdiagnosis had significantly greater rates of abdominal pain (about 85% vs. about 60%), weight loss (about 85% vs. about 75%), nausea/vomiting (50% vs. almost 40%), and pancreatitis (almost 30% vs. less than 5%), Dr. Swords said. In addition, patients with an initial misdiagnosis had significantly lower rates of jaundice (about 50% vs. almost 80%). The rates of diarrhea and anorexia were not significantly different between the two groups.
The study also looked at the time intervals from when the patient developed symptoms to the physician visit, from the physician visit to the cancer diagnosis, and from the physician visit to the performance of axial imaging. There was no difference in the time of symptom onset to the first visit with a physician in the two groups (0.5 month among those initially misdiagnosed and 0.7 month among those correctly diagnosed).
However, the time from the physician visit to the cancer diagnosis was 3.5 months among those initially misdiagnosed, vs. less than a month (0.6 month) among those who were correctly diagnosed, a statistically significant difference (P <.001), he said.
In addition, for those patients initially misdiagnosed, it took about 1 month longer from the physician visit to the time a CT scan or other type of axial imaging was ordered (an average of 1.1 months vs. 0.1 month, P <.001).
There was also a statistically significant association between a more advanced stage and initial misdiagnosis. Patients who were initially misdiagnosed had a 1.4-fold greater risk of having stage III or IV disease at the time of the pancreatic cancer diagnosis, Dr. Swords said.
Almost 40% (39) of those who were initially misdiagnosed were diagnosed with stage IV disease when they were correctly diagnosed, compared with 23.7% (51 patients) of those who were correctly diagnosed. The proportion diagnosed with stage III disease was similar, 21.4% among those initially misdiagnosed and 20% of those correctly diagnosed. Almost 51% of those correctly diagnosed were diagnosed with stage II disease, vs. 33.7% of those who were initially misdiagnosed. Of those initially misdiagnosed, 5.1% were diagnosed with stage I disease, compared with 5.6% of those correctly diagnosed.
However, the earlier stage at diagnosis for those with an initial correct diagnosis “did not translate into a survival difference,” Dr. Swords said, noting that there was a trend toward shorter survival among those who were initially misdiagnosed (median overall survival of 9.6 vs. 10.3 months).
Based on these results, Dr. Swords said, “surgeons should consider the diagnosis of pancreatic cancer when a patient referred for cholecystectomy has vague or atypical symptoms.”
He said he had no relevant financial disclosures.
WASHINGTON – Initial misdiagnoses were common and were associated with a later disease stage at diagnosis, in a study of 313 patients diagnosed with pancreatic cancer, Dr. Douglas Swords said at the annual Digestive Disease Week.
“By far, the most common misdiagnosis was gallbladder disease,” and there was about a 3-month longer time period, on average, from the first visit to a physician to the actual cancer diagnosis, in patients who were initially misdiagnosed, said Dr. Swords, a surgery resident at the University of Utah, Salt Lake City.
In the series of 313 patients diagnosed with pancreatic cancer, 98 (31.3%) were initially misdiagnosed, with a total of 119 diagnoses other than pancreatic cancer, he said. The most common misdiagnosis was gallbladder disease, which led to a cholecystectomy in 38 cases, followed by gastroesophageal reflux disease in 15 cases, and peptic ulcer disease in 11 cases. Those initially misdiagnosed were an average of about 5 years younger.
Patients with an initial misdiagnosis had significantly greater rates of abdominal pain (about 85% vs. about 60%), weight loss (about 85% vs. about 75%), nausea/vomiting (50% vs. almost 40%), and pancreatitis (almost 30% vs. less than 5%), Dr. Swords said. In addition, patients with an initial misdiagnosis had significantly lower rates of jaundice (about 50% vs. almost 80%). The rates of diarrhea and anorexia were not significantly different between the two groups.
The study also looked at the time intervals from when the patient developed symptoms to the physician visit, from the physician visit to the cancer diagnosis, and from the physician visit to the performance of axial imaging. There was no difference in the time of symptom onset to the first visit with a physician in the two groups (0.5 month among those initially misdiagnosed and 0.7 month among those correctly diagnosed).
However, the time from the physician visit to the cancer diagnosis was 3.5 months among those initially misdiagnosed, vs. less than a month (0.6 month) among those who were correctly diagnosed, a statistically significant difference (P <.001), he said.
In addition, for those patients initially misdiagnosed, it took about 1 month longer from the physician visit to the time a CT scan or other type of axial imaging was ordered (an average of 1.1 months vs. 0.1 month, P <.001).
There was also a statistically significant association between a more advanced stage and initial misdiagnosis. Patients who were initially misdiagnosed had a 1.4-fold greater risk of having stage III or IV disease at the time of the pancreatic cancer diagnosis, Dr. Swords said.
Almost 40% (39) of those who were initially misdiagnosed were diagnosed with stage IV disease when they were correctly diagnosed, compared with 23.7% (51 patients) of those who were correctly diagnosed. The proportion diagnosed with stage III disease was similar, 21.4% among those initially misdiagnosed and 20% of those correctly diagnosed. Almost 51% of those correctly diagnosed were diagnosed with stage II disease, vs. 33.7% of those who were initially misdiagnosed. Of those initially misdiagnosed, 5.1% were diagnosed with stage I disease, compared with 5.6% of those correctly diagnosed.
However, the earlier stage at diagnosis for those with an initial correct diagnosis “did not translate into a survival difference,” Dr. Swords said, noting that there was a trend toward shorter survival among those who were initially misdiagnosed (median overall survival of 9.6 vs. 10.3 months).
Based on these results, Dr. Swords said, “surgeons should consider the diagnosis of pancreatic cancer when a patient referred for cholecystectomy has vague or atypical symptoms.”
He said he had no relevant financial disclosures.
WASHINGTON – Initial misdiagnoses were common and were associated with a later disease stage at diagnosis, in a study of 313 patients diagnosed with pancreatic cancer, Dr. Douglas Swords said at the annual Digestive Disease Week.
“By far, the most common misdiagnosis was gallbladder disease,” and there was about a 3-month longer time period, on average, from the first visit to a physician to the actual cancer diagnosis, in patients who were initially misdiagnosed, said Dr. Swords, a surgery resident at the University of Utah, Salt Lake City.
In the series of 313 patients diagnosed with pancreatic cancer, 98 (31.3%) were initially misdiagnosed, with a total of 119 diagnoses other than pancreatic cancer, he said. The most common misdiagnosis was gallbladder disease, which led to a cholecystectomy in 38 cases, followed by gastroesophageal reflux disease in 15 cases, and peptic ulcer disease in 11 cases. Those initially misdiagnosed were an average of about 5 years younger.
Patients with an initial misdiagnosis had significantly greater rates of abdominal pain (about 85% vs. about 60%), weight loss (about 85% vs. about 75%), nausea/vomiting (50% vs. almost 40%), and pancreatitis (almost 30% vs. less than 5%), Dr. Swords said. In addition, patients with an initial misdiagnosis had significantly lower rates of jaundice (about 50% vs. almost 80%). The rates of diarrhea and anorexia were not significantly different between the two groups.
The study also looked at the time intervals from when the patient developed symptoms to the physician visit, from the physician visit to the cancer diagnosis, and from the physician visit to the performance of axial imaging. There was no difference in the time of symptom onset to the first visit with a physician in the two groups (0.5 month among those initially misdiagnosed and 0.7 month among those correctly diagnosed).
However, the time from the physician visit to the cancer diagnosis was 3.5 months among those initially misdiagnosed, vs. less than a month (0.6 month) among those who were correctly diagnosed, a statistically significant difference (P <.001), he said.
In addition, for those patients initially misdiagnosed, it took about 1 month longer from the physician visit to the time a CT scan or other type of axial imaging was ordered (an average of 1.1 months vs. 0.1 month, P <.001).
There was also a statistically significant association between a more advanced stage and initial misdiagnosis. Patients who were initially misdiagnosed had a 1.4-fold greater risk of having stage III or IV disease at the time of the pancreatic cancer diagnosis, Dr. Swords said.
Almost 40% (39) of those who were initially misdiagnosed were diagnosed with stage IV disease when they were correctly diagnosed, compared with 23.7% (51 patients) of those who were correctly diagnosed. The proportion diagnosed with stage III disease was similar, 21.4% among those initially misdiagnosed and 20% of those correctly diagnosed. Almost 51% of those correctly diagnosed were diagnosed with stage II disease, vs. 33.7% of those who were initially misdiagnosed. Of those initially misdiagnosed, 5.1% were diagnosed with stage I disease, compared with 5.6% of those correctly diagnosed.
However, the earlier stage at diagnosis for those with an initial correct diagnosis “did not translate into a survival difference,” Dr. Swords said, noting that there was a trend toward shorter survival among those who were initially misdiagnosed (median overall survival of 9.6 vs. 10.3 months).
Based on these results, Dr. Swords said, “surgeons should consider the diagnosis of pancreatic cancer when a patient referred for cholecystectomy has vague or atypical symptoms.”
He said he had no relevant financial disclosures.
AT DDW® 2015
Key clinical point: Pancreatic cancer is often misdiagnosed, and should be considered in patients with vague or atypical symptoms who are referred for a cholecystectomy.
Major finding: About 31% of patients with pancreatic cancer were initially misdiagnosed, most often with a gallbladder disease–related diagnosis.
Data source: A study of 313 patients diagnosed with pancreatic cancer comparing presenting symptoms, the time it took to reach the correct diagnosis, and other features in patients initially misdiagnosed and those who were not misdiagnosed.
Disclosures: Dr. Swords said he had no relevant financial disclosures.