Display Headline
Clinical Challenges - January 2018 What's your diagnosis?
The diagnosis
Answer: Posttraumatic splenosis
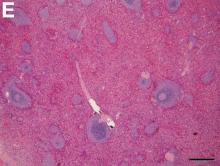
Pathologic examination of the specimen revealed a splenosis showing regular red and white pulp (Figure E). Splenosis is the heterotopic autotransplantation of splenic tissue within the abdominal or pelvic cavity and occurs in 16%–67% of patients with a history of splenic trauma or splenic surgery.1 Nevertheless, hepatic splenosis is rare.2 The literature documents only 16 case reports of hepatic splenosis, although the difficulty of diagnosis could have contributed to underreporting. Although usually harmless, splenosis is a rare cause of bowel obstruction or abdominal pain.
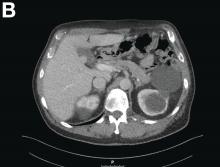
2 Moreover, splenic implants mimicking renal, intestinal, and hepatic masses have been described. 2 Usually, splenosis appears on CT as numerous round to oval structures with absent hilum, and with the same density as the spleen proper. Because CT’s differentiation between tissues can be unreliable,2 selective Tc-99m–labeled heat-denatured autologous red blood cell scintigraphy has been suggested.2 However, the lack of data on the accuracy of Tc-99m-scintigraphy renders its diagnostic efficacy questionable. In our patient with hepatitis C, a diagnostic laparoscopy was indicated to diagnose the posttraumatic splenosis at the infundibulum of the gallbladder. In high-risk patients, detection of a new liver lesion with radiologically uncertain contrast behavior, diagnostic laparoscopy including histologic workup to exclude hepatocellular carcinoma is indicated. Hepatocellular carcinoma usually presents as solitary or multifocal nodules located within the liver parenchyma. Nevertheless, several cases of superficial hepatocellular carcinoma on the surface of the liver have been reported.3 Splenosis may mimic abdominal neoplasia in patients with a history of severe splenic trauma or splenectomy and should be considered during oncologic workup.
References
1. Fleming, C.R., Dickson, E.R., Harrison, E.G. Splenosis: autotransplantation of splenic tissue. Am J Med. 1976;61:414-9.
2. D’Angelica, M., Fong, Y., Blumgart, L.H. Isolated hepatic splenosis: first reported case. HPB Surg. 1998;11:39-42.
3. Ohmoto, K., Mimura, N., Iguchi, Y. et al. Percutaneous microwave coagulation therapy for superficial hepatocellular carcinoma on the surface of the liver. Hepatogastroenterology. 2003;50:1547-51.
ginews@gastro.org
The diagnosis
Answer: Posttraumatic splenosis
Pathologic examination of the specimen revealed a splenosis showing regular red and white pulp (Figure E). Splenosis is the heterotopic autotransplantation of splenic tissue within the abdominal or pelvic cavity and occurs in 16%–67% of patients with a history of splenic trauma or splenic surgery.1 Nevertheless, hepatic splenosis is rare.2 The literature documents only 16 case reports of hepatic splenosis, although the difficulty of diagnosis could have contributed to underreporting. Although usually harmless, splenosis is a rare cause of bowel obstruction or abdominal pain.
2 Moreover, splenic implants mimicking renal, intestinal, and hepatic masses have been described. 2 Usually, splenosis appears on CT as numerous round to oval structures with absent hilum, and with the same density as the spleen proper. Because CT’s differentiation between tissues can be unreliable,2 selective Tc-99m–labeled heat-denatured autologous red blood cell scintigraphy has been suggested.2 However, the lack of data on the accuracy of Tc-99m-scintigraphy renders its diagnostic efficacy questionable. In our patient with hepatitis C, a diagnostic laparoscopy was indicated to diagnose the posttraumatic splenosis at the infundibulum of the gallbladder. In high-risk patients, detection of a new liver lesion with radiologically uncertain contrast behavior, diagnostic laparoscopy including histologic workup to exclude hepatocellular carcinoma is indicated. Hepatocellular carcinoma usually presents as solitary or multifocal nodules located within the liver parenchyma. Nevertheless, several cases of superficial hepatocellular carcinoma on the surface of the liver have been reported.3 Splenosis may mimic abdominal neoplasia in patients with a history of severe splenic trauma or splenectomy and should be considered during oncologic workup.
References
1. Fleming, C.R., Dickson, E.R., Harrison, E.G. Splenosis: autotransplantation of splenic tissue. Am J Med. 1976;61:414-9.
2. D’Angelica, M., Fong, Y., Blumgart, L.H. Isolated hepatic splenosis: first reported case. HPB Surg. 1998;11:39-42.
3. Ohmoto, K., Mimura, N., Iguchi, Y. et al. Percutaneous microwave coagulation therapy for superficial hepatocellular carcinoma on the surface of the liver. Hepatogastroenterology. 2003;50:1547-51.
ginews@gastro.org
The diagnosis
Answer: Posttraumatic splenosis
Pathologic examination of the specimen revealed a splenosis showing regular red and white pulp (Figure E). Splenosis is the heterotopic autotransplantation of splenic tissue within the abdominal or pelvic cavity and occurs in 16%–67% of patients with a history of splenic trauma or splenic surgery.1 Nevertheless, hepatic splenosis is rare.2 The literature documents only 16 case reports of hepatic splenosis, although the difficulty of diagnosis could have contributed to underreporting. Although usually harmless, splenosis is a rare cause of bowel obstruction or abdominal pain.
2 Moreover, splenic implants mimicking renal, intestinal, and hepatic masses have been described. 2 Usually, splenosis appears on CT as numerous round to oval structures with absent hilum, and with the same density as the spleen proper. Because CT’s differentiation between tissues can be unreliable,2 selective Tc-99m–labeled heat-denatured autologous red blood cell scintigraphy has been suggested.2 However, the lack of data on the accuracy of Tc-99m-scintigraphy renders its diagnostic efficacy questionable. In our patient with hepatitis C, a diagnostic laparoscopy was indicated to diagnose the posttraumatic splenosis at the infundibulum of the gallbladder. In high-risk patients, detection of a new liver lesion with radiologically uncertain contrast behavior, diagnostic laparoscopy including histologic workup to exclude hepatocellular carcinoma is indicated. Hepatocellular carcinoma usually presents as solitary or multifocal nodules located within the liver parenchyma. Nevertheless, several cases of superficial hepatocellular carcinoma on the surface of the liver have been reported.3 Splenosis may mimic abdominal neoplasia in patients with a history of severe splenic trauma or splenectomy and should be considered during oncologic workup.
References
1. Fleming, C.R., Dickson, E.R., Harrison, E.G. Splenosis: autotransplantation of splenic tissue. Am J Med. 1976;61:414-9.
2. D’Angelica, M., Fong, Y., Blumgart, L.H. Isolated hepatic splenosis: first reported case. HPB Surg. 1998;11:39-42.
3. Ohmoto, K., Mimura, N., Iguchi, Y. et al. Percutaneous microwave coagulation therapy for superficial hepatocellular carcinoma on the surface of the liver. Hepatogastroenterology. 2003;50:1547-51.
ginews@gastro.org
Display Headline
Clinical Challenges - January 2018 What's your diagnosis?
Display Headline
Clinical Challenges - January 2018 What's your diagnosis?
Content Gating
No Gating (article Unlocked/Free)