User login
ANSWER
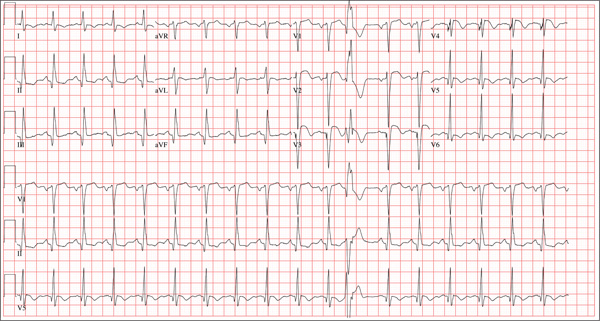
The correct interpretation includes sinus tachycardia with occasional premature ventricular complexes (PVCs), left atrial enlargement, evidence of a previous inferior MI, and an acute anterior MI. Sinus tachycardia is evidenced by a rate ≥ 100 beats/min and the presence of a P wave for every QRS complex with a constant PR interval. A single PVC is evident (12th beat of the rhythm strips V1, II, and V5).
Left atrial enlargement is evidenced by a large P wave in lead II and a biphasic P wave with the terminal portion larger than the initial portion in lead V1. An old inferior MI is evidenced by the presence of Q waves in leads II, III, and aVF.
An evolving anterior MI is diagnosed by the presence of poor R-wave progression with ST-segment elevations and T-wave inversion in leads V2, V3, and V4. This was subsequently confirmed by clinically significant elevations of serum troponin levels and by cardiac catheterization, which revealed occlusion of the left anterior descending artery distal to the internal mammary artery anastomosis.
ANSWER
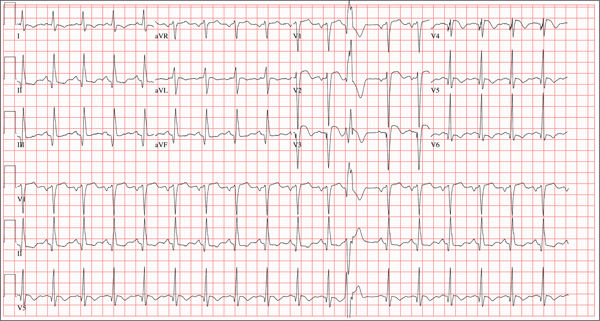
The correct interpretation includes sinus tachycardia with occasional premature ventricular complexes (PVCs), left atrial enlargement, evidence of a previous inferior MI, and an acute anterior MI. Sinus tachycardia is evidenced by a rate ≥ 100 beats/min and the presence of a P wave for every QRS complex with a constant PR interval. A single PVC is evident (12th beat of the rhythm strips V1, II, and V5).
Left atrial enlargement is evidenced by a large P wave in lead II and a biphasic P wave with the terminal portion larger than the initial portion in lead V1. An old inferior MI is evidenced by the presence of Q waves in leads II, III, and aVF.
An evolving anterior MI is diagnosed by the presence of poor R-wave progression with ST-segment elevations and T-wave inversion in leads V2, V3, and V4. This was subsequently confirmed by clinically significant elevations of serum troponin levels and by cardiac catheterization, which revealed occlusion of the left anterior descending artery distal to the internal mammary artery anastomosis.
ANSWER
The correct interpretation includes sinus tachycardia with occasional premature ventricular complexes (PVCs), left atrial enlargement, evidence of a previous inferior MI, and an acute anterior MI. Sinus tachycardia is evidenced by a rate ≥ 100 beats/min and the presence of a P wave for every QRS complex with a constant PR interval. A single PVC is evident (12th beat of the rhythm strips V1, II, and V5).
Left atrial enlargement is evidenced by a large P wave in lead II and a biphasic P wave with the terminal portion larger than the initial portion in lead V1. An old inferior MI is evidenced by the presence of Q waves in leads II, III, and aVF.
An evolving anterior MI is diagnosed by the presence of poor R-wave progression with ST-segment elevations and T-wave inversion in leads V2, V3, and V4. This was subsequently confirmed by clinically significant elevations of serum troponin levels and by cardiac catheterization, which revealed occlusion of the left anterior descending artery distal to the internal mammary artery anastomosis.
Three hours ago, this 69-year-old man started to experience substernal chest pain, nausea, and vomiting. He had stopped for lunch after spending the morning raking leaves; his chest pain began while he was at the drive-through window at a local fast food restaurant. By the time he got home, he was nauseous and had an episode of emesis. The pain is described as a “dull, heavy ache” with radiation to the left neck and arm. The patient states he is diaphoretic, but attributes it to the labor associated with his yardwork. He recalls that his first heart attack started in a similar way and fears he is having another. Following the emesis, his nausea stopped, and he rested in his recliner, hoping his symptoms would resolve. Unfortunately, the chest pain worsened, and he drove himself to the clinic rather than calling 911. (He didn’t want to go to the ED or get billed for the ambulance ride.) Review of his medical history reveals coronary artery disease, evidenced by an inferior MI in 2008. This was treated with coronary artery bypass surgery with reversed saphenous vein grafts placed to the first and second obtuse marginal branches of the circumflex coronary artery, reversed saphenous vein graft to the posterior descending artery, and an internal mammary artery graft placed to the proximal left anterior descending artery. His history is also remarkable for hyperlipidemia, hypertension, and obesity. He is a retired postal worker who has lived alone since his wife died three years ago. He drinks a six-pack of beer daily and continues to smoke one to two packs of cigarettes per day, depending on his activities. His family history includes coronary artery disease, hypertension, diabetes, and stroke. His current medications include aspirin, atorvastatin, clopidogrel, furosemide, isosorbide dinitrate, metoprolol, nicotine patch, potassium chloride, and valsartan. He is intolerant of ACE inhibitors, due to the resulting chronic, dry cough. The review of systems reveals that he has had headaches over the past week and that he recently recovered from the flu. He has had no changes in bowel or bladder function, shortness of breath, or recent weight loss or gain. Vital signs include a blood pressure of 168/100 mm Hg; pulse, 110 beats/min; respiratory rate, 18 breaths/min-1; O2 saturation, 98% on room air; and temperature, 37.2°C. His weight is 108 kg, and his height is 170 cm. Physical findings show that the lungs are clear to auscultation; his rhythm is regular with no murmurs, rubs, or gallops; and the point of maximum impulse is not displaced. The neck veins are flat, and there is no peripheral edema. A well-healed median sternotomy scar is evident, as are bilateral lower extremity saphenous vein harvest scars. The abdomen is soft and nontender, and peripheral pulses are strong and equal bilaterally. There are no neurologic abnormalities noted. Laboratory samples and an ECG are obtained. The following findings are noted on the ECG: a ventricular rate of 108 beats/min; PR interval, 140 ms; QRS duration, 116 ms; QT/QTc interval, 372/498 ms; P axis, 70°; R axis, 75°; and T axis, 167°. What is your interpretation of this ECG?