User login
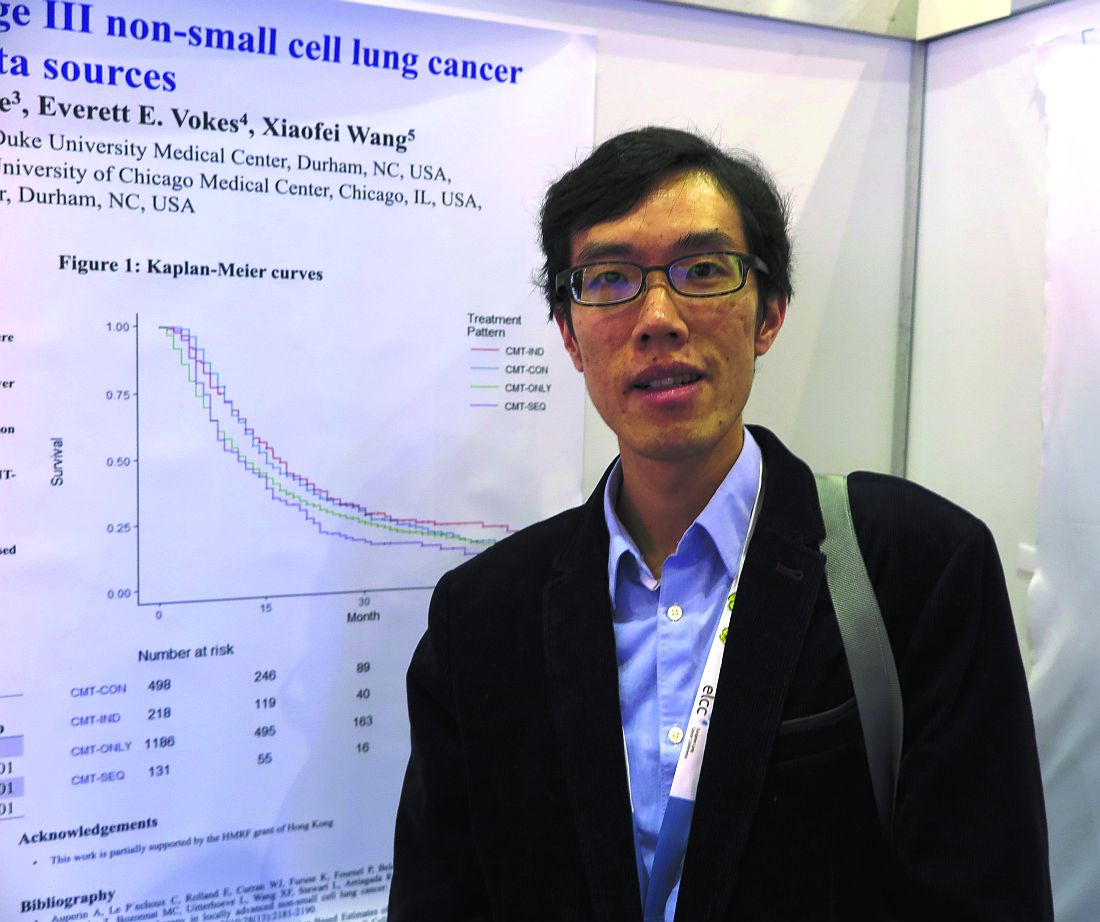
GENEVA – Among older adults with stage III non–small cell lung cancer (NSCLC), the sequencing of chemotherapy and radiation has a significant effect on overall survival, a team of investigators from Hong Kong and the United States reported.
Among 2,033 adults who were 65 years or older with locally advanced NSCLC and treated with one of four combined-modality therapy (CMT) schedules, both chemotherapy induction followed by concurrent therapy (CMT-IND) and concurrent therapy followed by consolidation chemoradiation (CMT-CON) were associated with an approximately 30% improvement in survival, compared with either sequential chemotherapy followed by radiation (CMT-SEQ) or concurrent therapy only (CMT-ONLY), reported Hei Man Herbert Pang, MD, of the University of Hong Kong and his colleagues.
The investigators used retrospective data from U.S. and Chinese sources to compare the relative survival benefits with various combined modality therapies. These included a Surveillance, Epidemiology, and End Results–Medicare cohort of patients 65 years and older with stage IIIA or IIIB NSCLC treated with CMT from 2006 through 2010 and a cohort of patients with the same age and NSCLC treated at Queen Mary Hospital in Hong Kong from 2007 through 2016.
They assessed neutropenia using inpatient claims data for episodes occurring within 130 days of the first chemotherapy cycle.
In an unadjusted analysis, they found that median overall survival, in descending order, was 16.1 months for CMT-SEQ,15.0 months for CMT-ONLY, 12.0 months for CMT-IND, and 11.0 months for CMT-CON.
When they controlled for variables, however, a different picture began to emerge.
For example, patients who were treated with CMT-SEQ had lower Charlson Comorbidity Index scores and, thus, were comparatively healthier than patients treated with other combined modalities.
Hospitalizations for neutropenia were most common with CMT-CON, occurring in 13.3% of patients, compared with 9.8% of patients treated with CMT-ONLY, 9.2% with CMT-IND, and 2.3% with CMT-SEQ.
In multivariable models controlling for sex, race, ethnicity, histology, and Charlson score, CMT-CON and CMT-IND were associated with significantly better overall, compared with CMT-SEQ, with respective hazard ratios for death of 0.68 (P less than .001) and 0.67 (P = .001). In this model, CMT-ONLY was not associated with significantly better survival.
In a propensity score model adjusted for the same factors, the respective HRs for CMT-CON, CMT-IND, and CMT-ONLY vs. CMT-SEQ were 0.69, 0.70, and 0.86 (P less than .001 for all three comparisons).
“The findings on efficacy and toxicity are quite consistent with previously reported studies based on clinical trials or observational databases,” the investigators said.
The study was supported by grants from the U.S. National Institutes of Health and the Hong Kong Health and Medical Research Fund. All authors have declared no conflicts of interest.
GENEVA – Among older adults with stage III non–small cell lung cancer (NSCLC), the sequencing of chemotherapy and radiation has a significant effect on overall survival, a team of investigators from Hong Kong and the United States reported.
Among 2,033 adults who were 65 years or older with locally advanced NSCLC and treated with one of four combined-modality therapy (CMT) schedules, both chemotherapy induction followed by concurrent therapy (CMT-IND) and concurrent therapy followed by consolidation chemoradiation (CMT-CON) were associated with an approximately 30% improvement in survival, compared with either sequential chemotherapy followed by radiation (CMT-SEQ) or concurrent therapy only (CMT-ONLY), reported Hei Man Herbert Pang, MD, of the University of Hong Kong and his colleagues.
The investigators used retrospective data from U.S. and Chinese sources to compare the relative survival benefits with various combined modality therapies. These included a Surveillance, Epidemiology, and End Results–Medicare cohort of patients 65 years and older with stage IIIA or IIIB NSCLC treated with CMT from 2006 through 2010 and a cohort of patients with the same age and NSCLC treated at Queen Mary Hospital in Hong Kong from 2007 through 2016.
They assessed neutropenia using inpatient claims data for episodes occurring within 130 days of the first chemotherapy cycle.
In an unadjusted analysis, they found that median overall survival, in descending order, was 16.1 months for CMT-SEQ,15.0 months for CMT-ONLY, 12.0 months for CMT-IND, and 11.0 months for CMT-CON.
When they controlled for variables, however, a different picture began to emerge.
For example, patients who were treated with CMT-SEQ had lower Charlson Comorbidity Index scores and, thus, were comparatively healthier than patients treated with other combined modalities.
Hospitalizations for neutropenia were most common with CMT-CON, occurring in 13.3% of patients, compared with 9.8% of patients treated with CMT-ONLY, 9.2% with CMT-IND, and 2.3% with CMT-SEQ.
In multivariable models controlling for sex, race, ethnicity, histology, and Charlson score, CMT-CON and CMT-IND were associated with significantly better overall, compared with CMT-SEQ, with respective hazard ratios for death of 0.68 (P less than .001) and 0.67 (P = .001). In this model, CMT-ONLY was not associated with significantly better survival.
In a propensity score model adjusted for the same factors, the respective HRs for CMT-CON, CMT-IND, and CMT-ONLY vs. CMT-SEQ were 0.69, 0.70, and 0.86 (P less than .001 for all three comparisons).
“The findings on efficacy and toxicity are quite consistent with previously reported studies based on clinical trials or observational databases,” the investigators said.
The study was supported by grants from the U.S. National Institutes of Health and the Hong Kong Health and Medical Research Fund. All authors have declared no conflicts of interest.
GENEVA – Among older adults with stage III non–small cell lung cancer (NSCLC), the sequencing of chemotherapy and radiation has a significant effect on overall survival, a team of investigators from Hong Kong and the United States reported.
Among 2,033 adults who were 65 years or older with locally advanced NSCLC and treated with one of four combined-modality therapy (CMT) schedules, both chemotherapy induction followed by concurrent therapy (CMT-IND) and concurrent therapy followed by consolidation chemoradiation (CMT-CON) were associated with an approximately 30% improvement in survival, compared with either sequential chemotherapy followed by radiation (CMT-SEQ) or concurrent therapy only (CMT-ONLY), reported Hei Man Herbert Pang, MD, of the University of Hong Kong and his colleagues.
The investigators used retrospective data from U.S. and Chinese sources to compare the relative survival benefits with various combined modality therapies. These included a Surveillance, Epidemiology, and End Results–Medicare cohort of patients 65 years and older with stage IIIA or IIIB NSCLC treated with CMT from 2006 through 2010 and a cohort of patients with the same age and NSCLC treated at Queen Mary Hospital in Hong Kong from 2007 through 2016.
They assessed neutropenia using inpatient claims data for episodes occurring within 130 days of the first chemotherapy cycle.
In an unadjusted analysis, they found that median overall survival, in descending order, was 16.1 months for CMT-SEQ,15.0 months for CMT-ONLY, 12.0 months for CMT-IND, and 11.0 months for CMT-CON.
When they controlled for variables, however, a different picture began to emerge.
For example, patients who were treated with CMT-SEQ had lower Charlson Comorbidity Index scores and, thus, were comparatively healthier than patients treated with other combined modalities.
Hospitalizations for neutropenia were most common with CMT-CON, occurring in 13.3% of patients, compared with 9.8% of patients treated with CMT-ONLY, 9.2% with CMT-IND, and 2.3% with CMT-SEQ.
In multivariable models controlling for sex, race, ethnicity, histology, and Charlson score, CMT-CON and CMT-IND were associated with significantly better overall, compared with CMT-SEQ, with respective hazard ratios for death of 0.68 (P less than .001) and 0.67 (P = .001). In this model, CMT-ONLY was not associated with significantly better survival.
In a propensity score model adjusted for the same factors, the respective HRs for CMT-CON, CMT-IND, and CMT-ONLY vs. CMT-SEQ were 0.69, 0.70, and 0.86 (P less than .001 for all three comparisons).
“The findings on efficacy and toxicity are quite consistent with previously reported studies based on clinical trials or observational databases,” the investigators said.
The study was supported by grants from the U.S. National Institutes of Health and the Hong Kong Health and Medical Research Fund. All authors have declared no conflicts of interest.
FROM ELCC
Key clinical point: Some combined modality therapy options for older adults with NSCLC are associated with better overall survival.
Major finding: CMT-IND and CMT-CON were associated with a 30% improvement in overall survival, compared with CMT-SEQ.
Data source: Retrospective review of data on 2,033 adults 65 years and older with NSCLC in the United States and Hong Kong.
Disclosures: The study was supported by grants from the U.S. National Institutes of Health and the Hong Kong Health and Medical Research Fund. All authors have declared no conflicts of interest.