User login
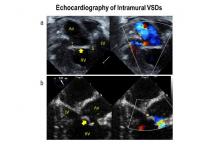
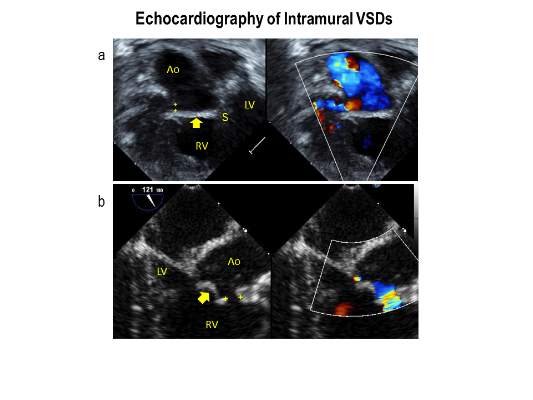
Intramural ventricular septal defects (VSD), residual defects that can occur after repair of conotruncal defects in newborns, increase the risk of complications and death if they’re not detected and closed during the index operation. While various methods have been tried to find these defects during surgery, researchers from Children’s Hospital of Philadelphia (CHOP) reported that the use of transesophageal echocardiography (TEE) has a good chance of finding VSDs and giving cardiac surgeons the opportunity to correct these residual defects.
“TEE has modest sensitivity but high specificity for identifying intramural VSDs and can identify most defects requiring reinterventions,” Jyoti Patel, MD, and her coauthors reported in a study published in the September issue of the Journal of Thoracic and Cardiovascular Surgery (2016;152:688-95).
Previous studies have shown that intraoperative TEE is safe for evaluating operations in congenital heart disease, but this is the first study to evaluate the modality for detecting intramural VSDs, Dr. Patel and her colleagues said.
Dr. Patel and her coinvestigators analyzed results of TEE and postoperative transthoracic echocardiography (TTE) in patients who had biventricular repair of conotruncal anomalies at CHOP from January 2006 through June 2013. Intramural VSDs occurred in 34 of 337 patients who met the inclusion criteria out of a total population of 903. Actually, 462 patients had biventricular repairs of conotruncal defects involving baffle closure of a VSD, but 125 were excluded for various reasons, including 105 for inadequate intraoperative TEE.
TTE identified a total of 177 residual VSDs, 34 of which were intramural in nature. Among the evaluated procedures, both TEE at the end of the index operation and TTE detected VSD in 19 patients; TTE alone found VSD in 15. “Sensitivity was 56% and specificity was 100% for TEE to identify intramural VSDs,” Dr. Patel and her colleagues said.
What’s more, both TTE and TEE combined identified peripatch VSDs in 90 patients, while TTE only in 53 and TEE only in 15, “yielding a sensitivity of 63% and specificity of 92%,” Dr. Patel and her colleagues said.
Of the VSDs that required catheterization or reintervention during surgery, intraoperative TEE detected six of seven intramural VSDs and all five peripatch VSDs, the study found.
“In this study, TEE identified most intramural VSDs and all peripatch VSDs that required subsequent reintervention,” Dr. Patel and her colleagues said.
“This finding underscores the importance of adequate imaging of the superior aspect of the VSD patch during intraoperative TEE for conotruncal anomalies, given that many intramural defects may be repaired during the initial operation.”
Coauthor Andrew Glatz, MD, disclosed receiving consulting fees from Bristol-Myers Squibb, and coauthor Chitra Ravishankar, MD, disclosed lecture fees from Danone Medical. Dr. Patel and the remaining coauthors had no financial relationships to disclose.
Because of the clinical importance of intramural VSDs, cardiac surgeons need to be highly suspicious in any operation to repair conotruncal defects where the VSD margins are close to the trabeculae, Edward Buratto, MBBS, Philip Naimo, MD, and Igor Konstantinov, MD, PhD, of Royal Children’s Hospital at the University of Melbourne said in their invited commentary (J Thorac Cardiovasc Surg. 2016;152:696-7). “The best way to resolve the problem would be to prevent it,” they said.
While intraoperative TEE can detect VSDs preemptively, the imaging technique is “not without its flaws,” the commentators said, as evidenced by the 105 subjects the CHOP study excluded because of inadequate TEE imaging. Those excluded cases comprised patients aged 30 days and younger with lower body weight and higher early death rates. “It is these patients who would benefit most from intraoperative identification of intramural VSD,” the commentators said.
They also noted that TEE in detecting intramural and peripatch VSD in children aged 30 days and older “was not perfect either,” with sensitivities of 56% and 63%, respectively. In the CHOP study, TEE was more likely to detect intramural VSD in patients older than 30 days with higher body weight, Dr. Buratto and his colleagues said.
The favored approach at Royal Children’s Hospital in Melbourne is routine epicardial echocardiograms in conotruncal repair. This imaging technique provides “superb imaging quality,” they said. “This is of particular importance in small children.” They advocate closing a significant VSD once it’s identified.
“After all, failure to close intramural VSD occurs when surgeons do not realize how close they were to success when they gave up,” the commentators said. Precise echocardiographic guidance would “dramatically facilitate” that strategy.
Dr. Buratto, Dr. Naimo, and Dr. Konstantinov had no financial relationships to disclose.
Because of the clinical importance of intramural VSDs, cardiac surgeons need to be highly suspicious in any operation to repair conotruncal defects where the VSD margins are close to the trabeculae, Edward Buratto, MBBS, Philip Naimo, MD, and Igor Konstantinov, MD, PhD, of Royal Children’s Hospital at the University of Melbourne said in their invited commentary (J Thorac Cardiovasc Surg. 2016;152:696-7). “The best way to resolve the problem would be to prevent it,” they said.
While intraoperative TEE can detect VSDs preemptively, the imaging technique is “not without its flaws,” the commentators said, as evidenced by the 105 subjects the CHOP study excluded because of inadequate TEE imaging. Those excluded cases comprised patients aged 30 days and younger with lower body weight and higher early death rates. “It is these patients who would benefit most from intraoperative identification of intramural VSD,” the commentators said.
They also noted that TEE in detecting intramural and peripatch VSD in children aged 30 days and older “was not perfect either,” with sensitivities of 56% and 63%, respectively. In the CHOP study, TEE was more likely to detect intramural VSD in patients older than 30 days with higher body weight, Dr. Buratto and his colleagues said.
The favored approach at Royal Children’s Hospital in Melbourne is routine epicardial echocardiograms in conotruncal repair. This imaging technique provides “superb imaging quality,” they said. “This is of particular importance in small children.” They advocate closing a significant VSD once it’s identified.
“After all, failure to close intramural VSD occurs when surgeons do not realize how close they were to success when they gave up,” the commentators said. Precise echocardiographic guidance would “dramatically facilitate” that strategy.
Dr. Buratto, Dr. Naimo, and Dr. Konstantinov had no financial relationships to disclose.
Because of the clinical importance of intramural VSDs, cardiac surgeons need to be highly suspicious in any operation to repair conotruncal defects where the VSD margins are close to the trabeculae, Edward Buratto, MBBS, Philip Naimo, MD, and Igor Konstantinov, MD, PhD, of Royal Children’s Hospital at the University of Melbourne said in their invited commentary (J Thorac Cardiovasc Surg. 2016;152:696-7). “The best way to resolve the problem would be to prevent it,” they said.
While intraoperative TEE can detect VSDs preemptively, the imaging technique is “not without its flaws,” the commentators said, as evidenced by the 105 subjects the CHOP study excluded because of inadequate TEE imaging. Those excluded cases comprised patients aged 30 days and younger with lower body weight and higher early death rates. “It is these patients who would benefit most from intraoperative identification of intramural VSD,” the commentators said.
They also noted that TEE in detecting intramural and peripatch VSD in children aged 30 days and older “was not perfect either,” with sensitivities of 56% and 63%, respectively. In the CHOP study, TEE was more likely to detect intramural VSD in patients older than 30 days with higher body weight, Dr. Buratto and his colleagues said.
The favored approach at Royal Children’s Hospital in Melbourne is routine epicardial echocardiograms in conotruncal repair. This imaging technique provides “superb imaging quality,” they said. “This is of particular importance in small children.” They advocate closing a significant VSD once it’s identified.
“After all, failure to close intramural VSD occurs when surgeons do not realize how close they were to success when they gave up,” the commentators said. Precise echocardiographic guidance would “dramatically facilitate” that strategy.
Dr. Buratto, Dr. Naimo, and Dr. Konstantinov had no financial relationships to disclose.
Intramural ventricular septal defects (VSD), residual defects that can occur after repair of conotruncal defects in newborns, increase the risk of complications and death if they’re not detected and closed during the index operation. While various methods have been tried to find these defects during surgery, researchers from Children’s Hospital of Philadelphia (CHOP) reported that the use of transesophageal echocardiography (TEE) has a good chance of finding VSDs and giving cardiac surgeons the opportunity to correct these residual defects.
“TEE has modest sensitivity but high specificity for identifying intramural VSDs and can identify most defects requiring reinterventions,” Jyoti Patel, MD, and her coauthors reported in a study published in the September issue of the Journal of Thoracic and Cardiovascular Surgery (2016;152:688-95).
Previous studies have shown that intraoperative TEE is safe for evaluating operations in congenital heart disease, but this is the first study to evaluate the modality for detecting intramural VSDs, Dr. Patel and her colleagues said.
Dr. Patel and her coinvestigators analyzed results of TEE and postoperative transthoracic echocardiography (TTE) in patients who had biventricular repair of conotruncal anomalies at CHOP from January 2006 through June 2013. Intramural VSDs occurred in 34 of 337 patients who met the inclusion criteria out of a total population of 903. Actually, 462 patients had biventricular repairs of conotruncal defects involving baffle closure of a VSD, but 125 were excluded for various reasons, including 105 for inadequate intraoperative TEE.
TTE identified a total of 177 residual VSDs, 34 of which were intramural in nature. Among the evaluated procedures, both TEE at the end of the index operation and TTE detected VSD in 19 patients; TTE alone found VSD in 15. “Sensitivity was 56% and specificity was 100% for TEE to identify intramural VSDs,” Dr. Patel and her colleagues said.
What’s more, both TTE and TEE combined identified peripatch VSDs in 90 patients, while TTE only in 53 and TEE only in 15, “yielding a sensitivity of 63% and specificity of 92%,” Dr. Patel and her colleagues said.
Of the VSDs that required catheterization or reintervention during surgery, intraoperative TEE detected six of seven intramural VSDs and all five peripatch VSDs, the study found.
“In this study, TEE identified most intramural VSDs and all peripatch VSDs that required subsequent reintervention,” Dr. Patel and her colleagues said.
“This finding underscores the importance of adequate imaging of the superior aspect of the VSD patch during intraoperative TEE for conotruncal anomalies, given that many intramural defects may be repaired during the initial operation.”
Coauthor Andrew Glatz, MD, disclosed receiving consulting fees from Bristol-Myers Squibb, and coauthor Chitra Ravishankar, MD, disclosed lecture fees from Danone Medical. Dr. Patel and the remaining coauthors had no financial relationships to disclose.
Intramural ventricular septal defects (VSD), residual defects that can occur after repair of conotruncal defects in newborns, increase the risk of complications and death if they’re not detected and closed during the index operation. While various methods have been tried to find these defects during surgery, researchers from Children’s Hospital of Philadelphia (CHOP) reported that the use of transesophageal echocardiography (TEE) has a good chance of finding VSDs and giving cardiac surgeons the opportunity to correct these residual defects.
“TEE has modest sensitivity but high specificity for identifying intramural VSDs and can identify most defects requiring reinterventions,” Jyoti Patel, MD, and her coauthors reported in a study published in the September issue of the Journal of Thoracic and Cardiovascular Surgery (2016;152:688-95).
Previous studies have shown that intraoperative TEE is safe for evaluating operations in congenital heart disease, but this is the first study to evaluate the modality for detecting intramural VSDs, Dr. Patel and her colleagues said.
Dr. Patel and her coinvestigators analyzed results of TEE and postoperative transthoracic echocardiography (TTE) in patients who had biventricular repair of conotruncal anomalies at CHOP from January 2006 through June 2013. Intramural VSDs occurred in 34 of 337 patients who met the inclusion criteria out of a total population of 903. Actually, 462 patients had biventricular repairs of conotruncal defects involving baffle closure of a VSD, but 125 were excluded for various reasons, including 105 for inadequate intraoperative TEE.
TTE identified a total of 177 residual VSDs, 34 of which were intramural in nature. Among the evaluated procedures, both TEE at the end of the index operation and TTE detected VSD in 19 patients; TTE alone found VSD in 15. “Sensitivity was 56% and specificity was 100% for TEE to identify intramural VSDs,” Dr. Patel and her colleagues said.
What’s more, both TTE and TEE combined identified peripatch VSDs in 90 patients, while TTE only in 53 and TEE only in 15, “yielding a sensitivity of 63% and specificity of 92%,” Dr. Patel and her colleagues said.
Of the VSDs that required catheterization or reintervention during surgery, intraoperative TEE detected six of seven intramural VSDs and all five peripatch VSDs, the study found.
“In this study, TEE identified most intramural VSDs and all peripatch VSDs that required subsequent reintervention,” Dr. Patel and her colleagues said.
“This finding underscores the importance of adequate imaging of the superior aspect of the VSD patch during intraoperative TEE for conotruncal anomalies, given that many intramural defects may be repaired during the initial operation.”
Coauthor Andrew Glatz, MD, disclosed receiving consulting fees from Bristol-Myers Squibb, and coauthor Chitra Ravishankar, MD, disclosed lecture fees from Danone Medical. Dr. Patel and the remaining coauthors had no financial relationships to disclose.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point: Intraoperative transesophageal echocardiography has modest sensitivity but high specificity for detecting ventricular septal defects after repair of conotruncal anomalies.
Major finding: TEE is useful for identifying most VSDs during the index operation, providing the opportunity to repair the defects during the index operation.
Data source: A single-institution database of 337 patients who had operations to repair conotruncal anomalies between January 2006 and June 2013.
Disclosures: Coauthor Andrew Glatz, MD, disclosed receiving consulting fees from Bristol-Myers Squibb, and coauthor Chitra Ravishankar, MD, disclosed lecture fees from Danone Medical. Dr. Patel and the remaining coauthors had no financial relationships to disclose.