User login
CASE Scratching, anxious, and hopeless
Ms. L, age 74, who is paraplegic and uses a wheelchair, presents to our hospital’s emergency department (ED) accompanied by staff from the nursing home where she resides. She reports that she can feel and see bugs crawling all over her skin, biting
Ms. L experiences generalized pruritus with excoriations scattered over her upper and lower extremities and her trunk. She copes with the pruritus by scratching. She reports that the bugs are present throughout the day and are worse at night when she tries to go to bed. Nothing she does provides relief from the infestation. Earlier, at the nursing home, Ms. L had obtained a detergent powder and used it in an attempt to purge the bugs. She now has large swaths of irritated skin, mostly on her lower back and perineal region.
She says the bug infestation became unbearable 3 weeks ago, but she can’t identify any precipitants for her symptoms. Ms. L reports that the impact of the bugs on her daily activity, sleep, and quality of life is enormous. Despite her complaints, neither the nursing home staff nor the ED staff can find any evidence of bugs on Ms. L’s clothes or skin.
Because Ms. L resorted to such drastic measures in her attempt to rid her body of the bugs, she is considered a safety risk and is admitted to the psychiatric unit, although she vehemently denies any intention to harm herself.
On the psychiatric unit, Ms. L states that the infestation began approximately 2 years ago. She began to experience severe worsening of her symptoms a few weeks before presenting to the ED.
During evaluation, Ms. L is alert and oriented to person, place, and situation. She is also quite cooperative but guarded in describing her infestation. There is some degree of suspiciousness and paranoia with regards to her infestation; she is very sensitive to how the clinical staff respond to her condition. She appears worried, and exhibits anxiety, sadness, hopelessness, and tearfulness. Her thought process is goal-directed, but preoccupied by the bugs.
[polldaddy:10064801]
Continue to: The authors' observations
The authors’ observations
Delusional parasitosis is a rare disorder that is defined by an individual having a fixed, false belief that he or she is being infected or grossly invaded by a living organism. Karl A. Ekbom, a Swedish neurologist, was the first practitioner to definitively describe this affliction in 1938.1
Primary delusional parasitosis is a disease defined by this single psychotic symptom without other classic symptoms of schizophrenia; this single symptom cannot be attributed to the effects of substance abuse or a medical condition. Many affected patients remain functional in their daily lives; only a minority of patients experience delusions that interfere with usual activity.2 Secondary delusional parasitosis is a symptom of another psychiatric or medical disease.
Morgellons disease is characterized by symptoms similar to primary delusional parasitosis, but symptoms of this condition also include the delusional belief that inanimate objects, usually fibers, are in the skin as well as the parasites.3
A population-based study among individuals living in Olmsted County, Minnesota from 1976 to 2010 found that the incidence of delusional infestation was 1.9 cases (95% confidence interval, 1.5 to 2.4) per 100,000 person-years.4 In a retrospective study of 147 patients with delusional parasitosis, 33% of these patients described themselves as disabled, 28% were retired, and 26% were employed.5 In this study, the mean age of diagnosis was 57, with a female-to-male ratio of 2.89:1.5
Continue to: HISTORY Prior psychiatric hospitalization
HISTORY Prior psychiatric hospitalization
Ms. L, who is divorced and retired, lives in a nursing home and has no pets, no exposure to scabies, no recent travel, no allergies, and no difficulty with her hygiene except at the peak of her illness. She denies any alcohol or illicit drug use but reports a 6 pack year history of smoking. She has a son, 2 grandchildren, and 2 great grandchildren who all live in town and see her regularly. She reports no history of arrests or legal problems.
Ms. L has a history of depression and anxiety that culminated in a “nervous breakdown” in 1985 with a brief stay in a psychiatric hospital. She reports that she had seen a therapist for 6 years as part of her treatment following that event. During her hospitalization, she was treated with a tricyclic antidepressant and received electroconvulsive therapy. She denies being suicidal during the incident in 1985 or at any point in time before or since then. She now takes venlafaxine, 75 mg/d, for depression and anxiety.
Ms. L’s paraplegia resulted from her sixth corrective surgery for scoliosis, which occurred 6 years ago. She has had chronic pain since this surgery. Her medical history also includes hypertension, atrial fibrillation, mild neurocognitive changes, and gastroesophageal reflux disease.
EVALUATION Skin examination, blood analysis normal
On admission, Ms. L undergoes a skin examination, which yields no evidence consistent with infestation with Pediculus humanus corporis (body louse) or Sarcoptes scabiei (scabies).6 Blood analysis shows no iron deficiency, renal failure, hyperbilirubinemia, or eosinophilia. In the ED, the medical team examines Ms. L and explores other medical and dermatological causes of her condition. Because dermatological causes had been ruled out before Ms. L was admitted to the inpatient psychiatric unit, no dermatology consult is requested.
Continue to: TREATMENT A first-generation antipsychotic
TREATMENT A first-generation antipsychotic
When Ms. L is admitted to the psychiatric unit, she is started
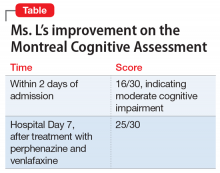
During the week, Ms. L’s perphenazine is titrated up to 24 mg twice daily and venlafaxine is titrated to 150 mg/d. A Montreal Cognitive Assessment (MoCA) is performed within the first 2 days of admission and she scores 16/30, indicating moderate cognitive impairment. On Friday, the attending physician explains that her medications should start to have therapeutic effect. During this time, this clinician engages in cognitive restructuring by providing validation of Ms. L’s suffering, verbal support, and medication compliance counseling. At this time, the treating team also suggests to Ms. L that she should expect the activity and effects of the bugs to dissipate. She is receptive to this suggestion. She also participates in the milieu, including unit activities, but is limited in her ability to engage in group therapy due to the intensity of her illness.
Throughout the weekend, the on-call physician also engages Ms. L and reports minor improvement.
OUTCOME Significant relief
On re-evaluation Monday morning—almost a week after Ms. L had been admitted to the inpatient psychiatric unit—she has achieved significant relief from her delusions. She says that she has no idea where the bugs have gone. Ms. L appears to be a completely different person. She no longer appears guarded. The suspiciousness, paranoia, hopelessness, and negative outlook she previously experienced have significantly diminished. Her MoCA score improves to 25/30, indicating no cognitive impairment (Table). She is discharged after a 7-night stay on the inpatient psychiatric unit.
Continue to: The authors' observations
The authors’ observations
During one of the clinical multidisciplinary treatment team meetings held for Ms. L, it was initially estimated that it would take at least 2 weeks for the delusional parasitosis to significantly respond to antipsychotic therapy. However, it is our professional opinion that the applied cognitive restructuring, with validation of her suffering, verbal support, and medication adherence counseling, expedited her recovery. This coincided with the aggressive titration of her antipsychotic and antidepressant, although the treatment team’s acknowledgment of Ms. L’s misery appeared to lower her guard and make her more susceptible to the power of cognitive restructuring. The efforts to validate the patient’s feelings and decrease hopelessness by telling her that the medication would make the bugs go away appeared to be the tipping point for her recovery. Patients with primary delusional parasitosis often are guarded and may feel alone in their predicament when they are met with perplexed responses from individuals with whom they discuss their symptoms. Compared with patients with schizophrenia, patients with delusional parasitosis maintain normal cognitive functioning, which may give them the insight to understand how their experience may be perceived as incompatible with reality.7 This understanding, coupled with some perceived helplessness, can lead a patient to fear having a severe mental decompensation, which can contribute to a delayed or complicated recovery.
The cognitive process described above might have been responsible for the difference in Ms. L’s MoCA scores because her performance in the initial test was hindered by her constant obsession with the bugs, which made her distracted during the test. By the time she responded to treatment, she gained significant clarity of thought, which enabled her to perform optimally in the test.
The difficulty in treating patients with delusional parasitosis may be further affected by lack of insight, and the fact that they often do not present to a psychiatrist for treatment in a timely manner because their delusion is impregnable and presents them with an alternate reality. These patients are more likely to seek out primary care physicians, dermatologists, infectious disease doctors, and entomologists because of the fervor of their delusion and the intensity of their discomfort. Because of this, a collaboration between these providers would likely lead to improved care and treatment acceptance for patients with delusional parasitosis.
Antipsychotics are the preferred medication for treating delusional parasitosis, and the literature supports their use for this purpose.6,8 The overall response rate is 60% to 100%.6 Previously, in small placebo-controlled trials, the first-generation antipsychotic (FGA) pimozide was considered first-line treatment for this disease.6 However, this antipsychotic is no longer favored because evidence is mounting that other FGAs result in comparable response rates with fewer tolerability issues.8,9
The bulk of data on the use of antipsychotics for treating delusional parasitosis comes from retrospective case reports and case series.6 Multiple antipsychotics have been shown to be effective in treating delusional parasitosis, including both FGAs and second-generation antipsychotics (SGAs).6,10 Published case reports and series have shown the effectiveness of the FGAs
Continue to: The SGAs risperidone, olanzapine, aripiprazole...
The SGAs
When selecting antipsychotic therapy for a patient diagnosed with delusional parasitosis, consider patient-specific factors, such as age, medication history, comorbidities, and the adverse-effect profile of the medication(s). These medications should be started at a low dose and titrated based on efficacy and safety. The optimal duration of therapy varies by patient. Patients should continually be assessed for possible treatment discontinuation, although if therapy is tapered off, patients need to be closely monitored for possible relapse or recurrence of symptoms.
Ms. L received perphenazine titrated up to 24 mg/d for the treatment of delusional parasitosis. The maximum dose used for Ms. L was higher than those used in previous reports, although she appeared to tolerate the medication well and respond rapidly. Her symptoms showed improvement within 1 week. Importantly, in published case reports, patients have been resistant to the use of psychotropic medications without other treatment modalities (eg, psychotherapy, various behavioral approaches). We conclude that Ms. L’s response was attributable to the use of the combination of psychotherapeutic techniques and the effectiveness of perphenazine and venlafaxine.
Bottom Line
Managing patients with primary delusional parasitosis can be challenging due to the fixed nature of the delusion. A combination of antipsychotics and psychotherapeutic techniques can benefit some patients. The optimal duration of treatment varies by patient.
Related Resource
- Trenton A, Pansare N, Tobia A, et al. Delusional parasitosis on the psychiatric consultation service-a longitudinal perspective: case study. BJPsych Open. 2017;3(3):154-158.
Drug Brand Names
Aripiprazole • Abilify
Haloperidol • Haldol
Olanzapine • Zyprexa
Paliperidone • Invega
Paliperidone palmitate • Invega Sustenna
Perphenazine • Trilafon
Pimozide • Orap
Quetiapine • Seroquel
Risperidone • Risperdal
Venlafaxine • Effexor
Ziprasidone • Geodon
1. Ekbom KA. Der präsenile dermatozoenwahn [in Swedish]. Acta Psychiatr Neurol Scand. 1938;13(3):227-259.
2. Lynch PJ. Delusions of parasitosis. Semin Dermatol. 1993;12(1):39-45.
3. Middelveen MJ, Fesler MC, Stricker RB. History of Morgellons disease: from delusion to definition. Clin Cosmet Investig Dermatol. 2018;11:71-90.
4. Bailey CH, Andersen LK, Lowe GC, et al. A population-based study of the incidence of delusional infestation in Olmsted County, Minnesota, 1976–2010. Br J Dermatol. 2014;170(5):1130-1135.
5. Foster AA, Hylwa SA, Bury JE, et al. Delusional infestation: clinical presentation in 147 patients seen at Mayo Clinic. J Am Acad Dermatol. 2012;67(4):673.e1-e10.
6. Lepping P, Russell I, Freudenmann RW. Antipsychotic treatment of primary delusional parasitosis: systematic review. Br J Psychiatry. 2007;191(3):198-205.
7. Freudenmann RW, Lepping P. Delusional infestation. Clin Microbiol Rev. 2009;22(4):690-732.
8. Mercan S, Altunay IK, Taskintuna N, et al. Atypical antipsychotic drugs in the treatment of delusional parasitosis. Intl J Psychiatry Med. 2007:37(1):29-37.
9. Trabert W. 100 years of delusional parasitosis. Meta-analysis of 1,223 case reports. Psychopathology. 1995;28(5):238-246.
10. Freudenmann RW, Lepping P. Second-generation antipsychotics in primary and secondary delusional parasitosis. J Clin Psychopharmacol. 2008;28(5):500-508.
11. Boggild AK, Nicks BA, Yen L, et al. Delusional parasitosis: six-year experience with 23 consecutive cases at an academic medical center. Int J Infect Dis. 2010;14(4):e317-e321.
CASE Scratching, anxious, and hopeless
Ms. L, age 74, who is paraplegic and uses a wheelchair, presents to our hospital’s emergency department (ED) accompanied by staff from the nursing home where she resides. She reports that she can feel and see bugs crawling all over her skin, biting
Ms. L experiences generalized pruritus with excoriations scattered over her upper and lower extremities and her trunk. She copes with the pruritus by scratching. She reports that the bugs are present throughout the day and are worse at night when she tries to go to bed. Nothing she does provides relief from the infestation. Earlier, at the nursing home, Ms. L had obtained a detergent powder and used it in an attempt to purge the bugs. She now has large swaths of irritated skin, mostly on her lower back and perineal region.
She says the bug infestation became unbearable 3 weeks ago, but she can’t identify any precipitants for her symptoms. Ms. L reports that the impact of the bugs on her daily activity, sleep, and quality of life is enormous. Despite her complaints, neither the nursing home staff nor the ED staff can find any evidence of bugs on Ms. L’s clothes or skin.
Because Ms. L resorted to such drastic measures in her attempt to rid her body of the bugs, she is considered a safety risk and is admitted to the psychiatric unit, although she vehemently denies any intention to harm herself.
On the psychiatric unit, Ms. L states that the infestation began approximately 2 years ago. She began to experience severe worsening of her symptoms a few weeks before presenting to the ED.
During evaluation, Ms. L is alert and oriented to person, place, and situation. She is also quite cooperative but guarded in describing her infestation. There is some degree of suspiciousness and paranoia with regards to her infestation; she is very sensitive to how the clinical staff respond to her condition. She appears worried, and exhibits anxiety, sadness, hopelessness, and tearfulness. Her thought process is goal-directed, but preoccupied by the bugs.
[polldaddy:10064801]
Continue to: The authors' observations
The authors’ observations
Delusional parasitosis is a rare disorder that is defined by an individual having a fixed, false belief that he or she is being infected or grossly invaded by a living organism. Karl A. Ekbom, a Swedish neurologist, was the first practitioner to definitively describe this affliction in 1938.1
Primary delusional parasitosis is a disease defined by this single psychotic symptom without other classic symptoms of schizophrenia; this single symptom cannot be attributed to the effects of substance abuse or a medical condition. Many affected patients remain functional in their daily lives; only a minority of patients experience delusions that interfere with usual activity.2 Secondary delusional parasitosis is a symptom of another psychiatric or medical disease.
Morgellons disease is characterized by symptoms similar to primary delusional parasitosis, but symptoms of this condition also include the delusional belief that inanimate objects, usually fibers, are in the skin as well as the parasites.3
A population-based study among individuals living in Olmsted County, Minnesota from 1976 to 2010 found that the incidence of delusional infestation was 1.9 cases (95% confidence interval, 1.5 to 2.4) per 100,000 person-years.4 In a retrospective study of 147 patients with delusional parasitosis, 33% of these patients described themselves as disabled, 28% were retired, and 26% were employed.5 In this study, the mean age of diagnosis was 57, with a female-to-male ratio of 2.89:1.5
Continue to: HISTORY Prior psychiatric hospitalization
HISTORY Prior psychiatric hospitalization
Ms. L, who is divorced and retired, lives in a nursing home and has no pets, no exposure to scabies, no recent travel, no allergies, and no difficulty with her hygiene except at the peak of her illness. She denies any alcohol or illicit drug use but reports a 6 pack year history of smoking. She has a son, 2 grandchildren, and 2 great grandchildren who all live in town and see her regularly. She reports no history of arrests or legal problems.
Ms. L has a history of depression and anxiety that culminated in a “nervous breakdown” in 1985 with a brief stay in a psychiatric hospital. She reports that she had seen a therapist for 6 years as part of her treatment following that event. During her hospitalization, she was treated with a tricyclic antidepressant and received electroconvulsive therapy. She denies being suicidal during the incident in 1985 or at any point in time before or since then. She now takes venlafaxine, 75 mg/d, for depression and anxiety.
Ms. L’s paraplegia resulted from her sixth corrective surgery for scoliosis, which occurred 6 years ago. She has had chronic pain since this surgery. Her medical history also includes hypertension, atrial fibrillation, mild neurocognitive changes, and gastroesophageal reflux disease.
EVALUATION Skin examination, blood analysis normal
On admission, Ms. L undergoes a skin examination, which yields no evidence consistent with infestation with Pediculus humanus corporis (body louse) or Sarcoptes scabiei (scabies).6 Blood analysis shows no iron deficiency, renal failure, hyperbilirubinemia, or eosinophilia. In the ED, the medical team examines Ms. L and explores other medical and dermatological causes of her condition. Because dermatological causes had been ruled out before Ms. L was admitted to the inpatient psychiatric unit, no dermatology consult is requested.
Continue to: TREATMENT A first-generation antipsychotic
TREATMENT A first-generation antipsychotic
When Ms. L is admitted to the psychiatric unit, she is started
During the week, Ms. L’s perphenazine is titrated up to 24 mg twice daily and venlafaxine is titrated to 150 mg/d. A Montreal Cognitive Assessment (MoCA) is performed within the first 2 days of admission and she scores 16/30, indicating moderate cognitive impairment. On Friday, the attending physician explains that her medications should start to have therapeutic effect. During this time, this clinician engages in cognitive restructuring by providing validation of Ms. L’s suffering, verbal support, and medication compliance counseling. At this time, the treating team also suggests to Ms. L that she should expect the activity and effects of the bugs to dissipate. She is receptive to this suggestion. She also participates in the milieu, including unit activities, but is limited in her ability to engage in group therapy due to the intensity of her illness.
Throughout the weekend, the on-call physician also engages Ms. L and reports minor improvement.
OUTCOME Significant relief
On re-evaluation Monday morning—almost a week after Ms. L had been admitted to the inpatient psychiatric unit—she has achieved significant relief from her delusions. She says that she has no idea where the bugs have gone. Ms. L appears to be a completely different person. She no longer appears guarded. The suspiciousness, paranoia, hopelessness, and negative outlook she previously experienced have significantly diminished. Her MoCA score improves to 25/30, indicating no cognitive impairment (Table). She is discharged after a 7-night stay on the inpatient psychiatric unit.
Continue to: The authors' observations
The authors’ observations
During one of the clinical multidisciplinary treatment team meetings held for Ms. L, it was initially estimated that it would take at least 2 weeks for the delusional parasitosis to significantly respond to antipsychotic therapy. However, it is our professional opinion that the applied cognitive restructuring, with validation of her suffering, verbal support, and medication adherence counseling, expedited her recovery. This coincided with the aggressive titration of her antipsychotic and antidepressant, although the treatment team’s acknowledgment of Ms. L’s misery appeared to lower her guard and make her more susceptible to the power of cognitive restructuring. The efforts to validate the patient’s feelings and decrease hopelessness by telling her that the medication would make the bugs go away appeared to be the tipping point for her recovery. Patients with primary delusional parasitosis often are guarded and may feel alone in their predicament when they are met with perplexed responses from individuals with whom they discuss their symptoms. Compared with patients with schizophrenia, patients with delusional parasitosis maintain normal cognitive functioning, which may give them the insight to understand how their experience may be perceived as incompatible with reality.7 This understanding, coupled with some perceived helplessness, can lead a patient to fear having a severe mental decompensation, which can contribute to a delayed or complicated recovery.
The cognitive process described above might have been responsible for the difference in Ms. L’s MoCA scores because her performance in the initial test was hindered by her constant obsession with the bugs, which made her distracted during the test. By the time she responded to treatment, she gained significant clarity of thought, which enabled her to perform optimally in the test.
The difficulty in treating patients with delusional parasitosis may be further affected by lack of insight, and the fact that they often do not present to a psychiatrist for treatment in a timely manner because their delusion is impregnable and presents them with an alternate reality. These patients are more likely to seek out primary care physicians, dermatologists, infectious disease doctors, and entomologists because of the fervor of their delusion and the intensity of their discomfort. Because of this, a collaboration between these providers would likely lead to improved care and treatment acceptance for patients with delusional parasitosis.
Antipsychotics are the preferred medication for treating delusional parasitosis, and the literature supports their use for this purpose.6,8 The overall response rate is 60% to 100%.6 Previously, in small placebo-controlled trials, the first-generation antipsychotic (FGA) pimozide was considered first-line treatment for this disease.6 However, this antipsychotic is no longer favored because evidence is mounting that other FGAs result in comparable response rates with fewer tolerability issues.8,9
The bulk of data on the use of antipsychotics for treating delusional parasitosis comes from retrospective case reports and case series.6 Multiple antipsychotics have been shown to be effective in treating delusional parasitosis, including both FGAs and second-generation antipsychotics (SGAs).6,10 Published case reports and series have shown the effectiveness of the FGAs
Continue to: The SGAs risperidone, olanzapine, aripiprazole...
The SGAs
When selecting antipsychotic therapy for a patient diagnosed with delusional parasitosis, consider patient-specific factors, such as age, medication history, comorbidities, and the adverse-effect profile of the medication(s). These medications should be started at a low dose and titrated based on efficacy and safety. The optimal duration of therapy varies by patient. Patients should continually be assessed for possible treatment discontinuation, although if therapy is tapered off, patients need to be closely monitored for possible relapse or recurrence of symptoms.
Ms. L received perphenazine titrated up to 24 mg/d for the treatment of delusional parasitosis. The maximum dose used for Ms. L was higher than those used in previous reports, although she appeared to tolerate the medication well and respond rapidly. Her symptoms showed improvement within 1 week. Importantly, in published case reports, patients have been resistant to the use of psychotropic medications without other treatment modalities (eg, psychotherapy, various behavioral approaches). We conclude that Ms. L’s response was attributable to the use of the combination of psychotherapeutic techniques and the effectiveness of perphenazine and venlafaxine.
Bottom Line
Managing patients with primary delusional parasitosis can be challenging due to the fixed nature of the delusion. A combination of antipsychotics and psychotherapeutic techniques can benefit some patients. The optimal duration of treatment varies by patient.
Related Resource
- Trenton A, Pansare N, Tobia A, et al. Delusional parasitosis on the psychiatric consultation service-a longitudinal perspective: case study. BJPsych Open. 2017;3(3):154-158.
Drug Brand Names
Aripiprazole • Abilify
Haloperidol • Haldol
Olanzapine • Zyprexa
Paliperidone • Invega
Paliperidone palmitate • Invega Sustenna
Perphenazine • Trilafon
Pimozide • Orap
Quetiapine • Seroquel
Risperidone • Risperdal
Venlafaxine • Effexor
Ziprasidone • Geodon
CASE Scratching, anxious, and hopeless
Ms. L, age 74, who is paraplegic and uses a wheelchair, presents to our hospital’s emergency department (ED) accompanied by staff from the nursing home where she resides. She reports that she can feel and see bugs crawling all over her skin, biting
Ms. L experiences generalized pruritus with excoriations scattered over her upper and lower extremities and her trunk. She copes with the pruritus by scratching. She reports that the bugs are present throughout the day and are worse at night when she tries to go to bed. Nothing she does provides relief from the infestation. Earlier, at the nursing home, Ms. L had obtained a detergent powder and used it in an attempt to purge the bugs. She now has large swaths of irritated skin, mostly on her lower back and perineal region.
She says the bug infestation became unbearable 3 weeks ago, but she can’t identify any precipitants for her symptoms. Ms. L reports that the impact of the bugs on her daily activity, sleep, and quality of life is enormous. Despite her complaints, neither the nursing home staff nor the ED staff can find any evidence of bugs on Ms. L’s clothes or skin.
Because Ms. L resorted to such drastic measures in her attempt to rid her body of the bugs, she is considered a safety risk and is admitted to the psychiatric unit, although she vehemently denies any intention to harm herself.
On the psychiatric unit, Ms. L states that the infestation began approximately 2 years ago. She began to experience severe worsening of her symptoms a few weeks before presenting to the ED.
During evaluation, Ms. L is alert and oriented to person, place, and situation. She is also quite cooperative but guarded in describing her infestation. There is some degree of suspiciousness and paranoia with regards to her infestation; she is very sensitive to how the clinical staff respond to her condition. She appears worried, and exhibits anxiety, sadness, hopelessness, and tearfulness. Her thought process is goal-directed, but preoccupied by the bugs.
[polldaddy:10064801]
Continue to: The authors' observations
The authors’ observations
Delusional parasitosis is a rare disorder that is defined by an individual having a fixed, false belief that he or she is being infected or grossly invaded by a living organism. Karl A. Ekbom, a Swedish neurologist, was the first practitioner to definitively describe this affliction in 1938.1
Primary delusional parasitosis is a disease defined by this single psychotic symptom without other classic symptoms of schizophrenia; this single symptom cannot be attributed to the effects of substance abuse or a medical condition. Many affected patients remain functional in their daily lives; only a minority of patients experience delusions that interfere with usual activity.2 Secondary delusional parasitosis is a symptom of another psychiatric or medical disease.
Morgellons disease is characterized by symptoms similar to primary delusional parasitosis, but symptoms of this condition also include the delusional belief that inanimate objects, usually fibers, are in the skin as well as the parasites.3
A population-based study among individuals living in Olmsted County, Minnesota from 1976 to 2010 found that the incidence of delusional infestation was 1.9 cases (95% confidence interval, 1.5 to 2.4) per 100,000 person-years.4 In a retrospective study of 147 patients with delusional parasitosis, 33% of these patients described themselves as disabled, 28% were retired, and 26% were employed.5 In this study, the mean age of diagnosis was 57, with a female-to-male ratio of 2.89:1.5
Continue to: HISTORY Prior psychiatric hospitalization
HISTORY Prior psychiatric hospitalization
Ms. L, who is divorced and retired, lives in a nursing home and has no pets, no exposure to scabies, no recent travel, no allergies, and no difficulty with her hygiene except at the peak of her illness. She denies any alcohol or illicit drug use but reports a 6 pack year history of smoking. She has a son, 2 grandchildren, and 2 great grandchildren who all live in town and see her regularly. She reports no history of arrests or legal problems.
Ms. L has a history of depression and anxiety that culminated in a “nervous breakdown” in 1985 with a brief stay in a psychiatric hospital. She reports that she had seen a therapist for 6 years as part of her treatment following that event. During her hospitalization, she was treated with a tricyclic antidepressant and received electroconvulsive therapy. She denies being suicidal during the incident in 1985 or at any point in time before or since then. She now takes venlafaxine, 75 mg/d, for depression and anxiety.
Ms. L’s paraplegia resulted from her sixth corrective surgery for scoliosis, which occurred 6 years ago. She has had chronic pain since this surgery. Her medical history also includes hypertension, atrial fibrillation, mild neurocognitive changes, and gastroesophageal reflux disease.
EVALUATION Skin examination, blood analysis normal
On admission, Ms. L undergoes a skin examination, which yields no evidence consistent with infestation with Pediculus humanus corporis (body louse) or Sarcoptes scabiei (scabies).6 Blood analysis shows no iron deficiency, renal failure, hyperbilirubinemia, or eosinophilia. In the ED, the medical team examines Ms. L and explores other medical and dermatological causes of her condition. Because dermatological causes had been ruled out before Ms. L was admitted to the inpatient psychiatric unit, no dermatology consult is requested.
Continue to: TREATMENT A first-generation antipsychotic
TREATMENT A first-generation antipsychotic
When Ms. L is admitted to the psychiatric unit, she is started
During the week, Ms. L’s perphenazine is titrated up to 24 mg twice daily and venlafaxine is titrated to 150 mg/d. A Montreal Cognitive Assessment (MoCA) is performed within the first 2 days of admission and she scores 16/30, indicating moderate cognitive impairment. On Friday, the attending physician explains that her medications should start to have therapeutic effect. During this time, this clinician engages in cognitive restructuring by providing validation of Ms. L’s suffering, verbal support, and medication compliance counseling. At this time, the treating team also suggests to Ms. L that she should expect the activity and effects of the bugs to dissipate. She is receptive to this suggestion. She also participates in the milieu, including unit activities, but is limited in her ability to engage in group therapy due to the intensity of her illness.
Throughout the weekend, the on-call physician also engages Ms. L and reports minor improvement.
OUTCOME Significant relief
On re-evaluation Monday morning—almost a week after Ms. L had been admitted to the inpatient psychiatric unit—she has achieved significant relief from her delusions. She says that she has no idea where the bugs have gone. Ms. L appears to be a completely different person. She no longer appears guarded. The suspiciousness, paranoia, hopelessness, and negative outlook she previously experienced have significantly diminished. Her MoCA score improves to 25/30, indicating no cognitive impairment (Table). She is discharged after a 7-night stay on the inpatient psychiatric unit.
Continue to: The authors' observations
The authors’ observations
During one of the clinical multidisciplinary treatment team meetings held for Ms. L, it was initially estimated that it would take at least 2 weeks for the delusional parasitosis to significantly respond to antipsychotic therapy. However, it is our professional opinion that the applied cognitive restructuring, with validation of her suffering, verbal support, and medication adherence counseling, expedited her recovery. This coincided with the aggressive titration of her antipsychotic and antidepressant, although the treatment team’s acknowledgment of Ms. L’s misery appeared to lower her guard and make her more susceptible to the power of cognitive restructuring. The efforts to validate the patient’s feelings and decrease hopelessness by telling her that the medication would make the bugs go away appeared to be the tipping point for her recovery. Patients with primary delusional parasitosis often are guarded and may feel alone in their predicament when they are met with perplexed responses from individuals with whom they discuss their symptoms. Compared with patients with schizophrenia, patients with delusional parasitosis maintain normal cognitive functioning, which may give them the insight to understand how their experience may be perceived as incompatible with reality.7 This understanding, coupled with some perceived helplessness, can lead a patient to fear having a severe mental decompensation, which can contribute to a delayed or complicated recovery.
The cognitive process described above might have been responsible for the difference in Ms. L’s MoCA scores because her performance in the initial test was hindered by her constant obsession with the bugs, which made her distracted during the test. By the time she responded to treatment, she gained significant clarity of thought, which enabled her to perform optimally in the test.
The difficulty in treating patients with delusional parasitosis may be further affected by lack of insight, and the fact that they often do not present to a psychiatrist for treatment in a timely manner because their delusion is impregnable and presents them with an alternate reality. These patients are more likely to seek out primary care physicians, dermatologists, infectious disease doctors, and entomologists because of the fervor of their delusion and the intensity of their discomfort. Because of this, a collaboration between these providers would likely lead to improved care and treatment acceptance for patients with delusional parasitosis.
Antipsychotics are the preferred medication for treating delusional parasitosis, and the literature supports their use for this purpose.6,8 The overall response rate is 60% to 100%.6 Previously, in small placebo-controlled trials, the first-generation antipsychotic (FGA) pimozide was considered first-line treatment for this disease.6 However, this antipsychotic is no longer favored because evidence is mounting that other FGAs result in comparable response rates with fewer tolerability issues.8,9
The bulk of data on the use of antipsychotics for treating delusional parasitosis comes from retrospective case reports and case series.6 Multiple antipsychotics have been shown to be effective in treating delusional parasitosis, including both FGAs and second-generation antipsychotics (SGAs).6,10 Published case reports and series have shown the effectiveness of the FGAs
Continue to: The SGAs risperidone, olanzapine, aripiprazole...
The SGAs
When selecting antipsychotic therapy for a patient diagnosed with delusional parasitosis, consider patient-specific factors, such as age, medication history, comorbidities, and the adverse-effect profile of the medication(s). These medications should be started at a low dose and titrated based on efficacy and safety. The optimal duration of therapy varies by patient. Patients should continually be assessed for possible treatment discontinuation, although if therapy is tapered off, patients need to be closely monitored for possible relapse or recurrence of symptoms.
Ms. L received perphenazine titrated up to 24 mg/d for the treatment of delusional parasitosis. The maximum dose used for Ms. L was higher than those used in previous reports, although she appeared to tolerate the medication well and respond rapidly. Her symptoms showed improvement within 1 week. Importantly, in published case reports, patients have been resistant to the use of psychotropic medications without other treatment modalities (eg, psychotherapy, various behavioral approaches). We conclude that Ms. L’s response was attributable to the use of the combination of psychotherapeutic techniques and the effectiveness of perphenazine and venlafaxine.
Bottom Line
Managing patients with primary delusional parasitosis can be challenging due to the fixed nature of the delusion. A combination of antipsychotics and psychotherapeutic techniques can benefit some patients. The optimal duration of treatment varies by patient.
Related Resource
- Trenton A, Pansare N, Tobia A, et al. Delusional parasitosis on the psychiatric consultation service-a longitudinal perspective: case study. BJPsych Open. 2017;3(3):154-158.
Drug Brand Names
Aripiprazole • Abilify
Haloperidol • Haldol
Olanzapine • Zyprexa
Paliperidone • Invega
Paliperidone palmitate • Invega Sustenna
Perphenazine • Trilafon
Pimozide • Orap
Quetiapine • Seroquel
Risperidone • Risperdal
Venlafaxine • Effexor
Ziprasidone • Geodon
1. Ekbom KA. Der präsenile dermatozoenwahn [in Swedish]. Acta Psychiatr Neurol Scand. 1938;13(3):227-259.
2. Lynch PJ. Delusions of parasitosis. Semin Dermatol. 1993;12(1):39-45.
3. Middelveen MJ, Fesler MC, Stricker RB. History of Morgellons disease: from delusion to definition. Clin Cosmet Investig Dermatol. 2018;11:71-90.
4. Bailey CH, Andersen LK, Lowe GC, et al. A population-based study of the incidence of delusional infestation in Olmsted County, Minnesota, 1976–2010. Br J Dermatol. 2014;170(5):1130-1135.
5. Foster AA, Hylwa SA, Bury JE, et al. Delusional infestation: clinical presentation in 147 patients seen at Mayo Clinic. J Am Acad Dermatol. 2012;67(4):673.e1-e10.
6. Lepping P, Russell I, Freudenmann RW. Antipsychotic treatment of primary delusional parasitosis: systematic review. Br J Psychiatry. 2007;191(3):198-205.
7. Freudenmann RW, Lepping P. Delusional infestation. Clin Microbiol Rev. 2009;22(4):690-732.
8. Mercan S, Altunay IK, Taskintuna N, et al. Atypical antipsychotic drugs in the treatment of delusional parasitosis. Intl J Psychiatry Med. 2007:37(1):29-37.
9. Trabert W. 100 years of delusional parasitosis. Meta-analysis of 1,223 case reports. Psychopathology. 1995;28(5):238-246.
10. Freudenmann RW, Lepping P. Second-generation antipsychotics in primary and secondary delusional parasitosis. J Clin Psychopharmacol. 2008;28(5):500-508.
11. Boggild AK, Nicks BA, Yen L, et al. Delusional parasitosis: six-year experience with 23 consecutive cases at an academic medical center. Int J Infect Dis. 2010;14(4):e317-e321.
1. Ekbom KA. Der präsenile dermatozoenwahn [in Swedish]. Acta Psychiatr Neurol Scand. 1938;13(3):227-259.
2. Lynch PJ. Delusions of parasitosis. Semin Dermatol. 1993;12(1):39-45.
3. Middelveen MJ, Fesler MC, Stricker RB. History of Morgellons disease: from delusion to definition. Clin Cosmet Investig Dermatol. 2018;11:71-90.
4. Bailey CH, Andersen LK, Lowe GC, et al. A population-based study of the incidence of delusional infestation in Olmsted County, Minnesota, 1976–2010. Br J Dermatol. 2014;170(5):1130-1135.
5. Foster AA, Hylwa SA, Bury JE, et al. Delusional infestation: clinical presentation in 147 patients seen at Mayo Clinic. J Am Acad Dermatol. 2012;67(4):673.e1-e10.
6. Lepping P, Russell I, Freudenmann RW. Antipsychotic treatment of primary delusional parasitosis: systematic review. Br J Psychiatry. 2007;191(3):198-205.
7. Freudenmann RW, Lepping P. Delusional infestation. Clin Microbiol Rev. 2009;22(4):690-732.
8. Mercan S, Altunay IK, Taskintuna N, et al. Atypical antipsychotic drugs in the treatment of delusional parasitosis. Intl J Psychiatry Med. 2007:37(1):29-37.
9. Trabert W. 100 years of delusional parasitosis. Meta-analysis of 1,223 case reports. Psychopathology. 1995;28(5):238-246.
10. Freudenmann RW, Lepping P. Second-generation antipsychotics in primary and secondary delusional parasitosis. J Clin Psychopharmacol. 2008;28(5):500-508.
11. Boggild AK, Nicks BA, Yen L, et al. Delusional parasitosis: six-year experience with 23 consecutive cases at an academic medical center. Int J Infect Dis. 2010;14(4):e317-e321.