User login
PARIS – Bioabsorbable vascular scaffolds have caught on in Europe and elsewhere in the world as an alternative to conventional metal stents for percutaneous coronary interventions in a wide spectrum of patient types.
By May 2014, more than 50,000 bioabsorbable vascular scaffolds (BVS) of the first brand to enter the European market – the Absorb stent made by Abbott Vascular – had gone into patients since the first placement in 2007, with the vast majority placed since this scaffold entered the European market in September 2012. Use of BVS in the United States remains investigational, while in the 20-plus months since BVS first became available in Europe other brands of BVS also have entered that market.
Despite growing BVS use in Europe, as well as in Asia and Central and South America, where they are also available, large-scale data on the consequences, especially long-term consequences, of BVS placement are mostly lacking, particularly data on how BVS perform when directly compared with drug-eluting metallic stents.
"Today we have uncontrolled dissemination of the technology without comparative data," Dr. Patrick W. Serruys, a pioneer in using BVS, said during a session at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
"We need evidence to know exactly what to do" with BVS, which patients to use them in, and when they are preferable to metallic stents, said Dr. Serruys, an interventional cardiologist and professor of medicine at the Thoraxcenter of Erasmus University in Rotterdam, the Netherlands.
"In the 7 years I’ve used them, in patients with 5-year follow-up, there have been no negative signals," he said in an interview, discussing his part of the sizeable anecdotal experience that BVS are safe and effective.
Several large trials comparing BVS with metal stents are in progress, including U.S. pivotal trials, but until these results are out, all that interventionalists have to gauge BVS performance are results from registries and uncontrolled trials. Given that limitation, so far the data look uniformly excellent.
"It is clear that emerging data from real-world, expanded-use registries suggest that use of the Absorb BVS is feasible and safe in a variety of patients, from low to high risk, and from simple to complex lesions," said Dr. Gregg W. Stone in a talk at the meeting. "But attention to procedural detail and technique is essential to optimize the outcomes. BVS are a little more complicated than metallic drug-eluting stents," said Dr. Stone, professor and director of cardiovascular research and education at Columbia University in New York.
"Data from large, randomized controlled trials are necessary to demonstrate whether BVS truly improve outcomes compared with best-in-class metallic stents. We are still early in the technology," he said. Dr. Stone is a lead investigator for one of the large U.S. randomized trials comparing the Absorb BVS to the current standard for percutaneous coronary interventions, a second-generation drug-eluting metallic stent.
Hints of what BVS may deliver
Hints of some of the potential benefits that BVS might provide appeared in results from a post-hoc, across-studies analysis that Dr. Stone presented in his talk. He compared the incidence of angina during the first year following PCI in 287 patients from the Absorb EXTEND study and 602 patients who received coronary stenting with the Xience second-generation everolimus-eluting metallic stent in the SPIRIT IV trial. The analysis matched patients in the Absorb arm with those in the Xience arm by propensity scoring.
The 1-year angina rates were 28% for the patients who received a metallic stent and 16% for those who received an absorbable scaffold, a 12% absolute difference, with a hazard ratio showing a 47% relative reduction in angina in patients who received the BVS, Dr. Stone reported. "There are a variety of mechanisms" by which BVS might reduce the rate of angina compared with metallic stents, including restoration of cyclic pulsatility in the treated arteries and improved vasomotion, he said.
The two outstanding clinical issues that dog PCI with second-generation drug-eluting metallic stents are the accrual of "very late" adverse events and the slow return of angina, with an average rate of target lesion failure with second-generation stents of about 1.8% year that continues out for at least 5 years, he said. "Can BVS flatten out the ongoing event rate" and improve measures like recurrent angina? Dr. Stone asked.
In another cross-study comparison, Dr. Serruys cited a recent, still unpublished analysis on which he collaborated that compared the 1-year outcomes of 102 patients with diabetes who received a BVS and 172 patients with diabetes who received a second-generation drug-eluting metallic stent. The 12-month cumulative rate of cardiovascular death, myocardial infarction, or ischemia-driven target lesion revascularization was 34.9% in the BVS recipients and 6.4% in patients who received state-of-the-art drug-eluting stents.
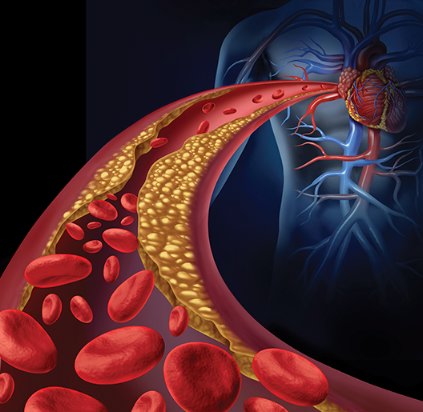
The working hypothesis behind BVS is that, by dissolving during a period of 12-24 months, the scaffold provides temporary bracing against restenosis but then disappears, allowing improved endovascular healing. During a separate session at EuroPCR, Dr. Charles A. Simonton, an interventional cardiologist and chief medical officer for Abbott Vascular, described the hypothesized impact that bioabsorbable coronary stents might have.
"Our vision is to convert interventional cardiology from mechanically oriented, plumbing-type interventions where you do mechanical things to open arteries" to a focus on tissue regeneration. "What we see when scaffolds resorb is that, at 3-5 years, the arteries look very different from what we see with a metal stent. The vessels show a highly functional neointimal layer that is functioning smooth muscle cells that protect against rupture in underlying plaque," he said.
Having BVS will allow interventional cardiologists to "transition from being mechanical plumbers to really being medical doctors. Not just opening lesions but putting in a treatment that can improve patients long term," Dr. Simonton said, presenting his best-case prediction of what BVS might achieve. "We need to generate a lot of data to make sure this is real," he added, in something of an understatement.
"There is late lumen enlargement with BVS. That is a clear fact," said Dr. Serruys.
The BVS experience
With data from studies that directly compared BVS and metallic stents still a few years off, the only indications of BVS performance now available come from either single- or multicenter registries. The thrust of much of these data presented at EuroPCR was that BVS have performed well as interventionalists have moved in the months since BVS became available for routine use to placing them in sicker patients and in patients with more complex coronary lesions.
The largest registry is ABSORB First, a voluntary-reporting registry that began in January 2013 and involves about 90 centers in countries where Absorb is commercially available in Europe, Asia, New Zealand, and Columbia. Dr. Eric Eeckhout, a cardiologist at Batiment Hospital in Lausanne, Switzerland, reported procedural and 30-day outcome data for the first 800 of the 1,305 patients enrolled in the registry as of May 2014.
Unlike previously reported multicenter series of patients getting BVS, these patients included 46% with at least two affected coronary arteries, 29% with stable angina, 15% with unstable angina, and 35% with an acute or recent MI. Significant calcification was present in 20% of the treated coronaries, 12% of the treated coronary stenoses were located at bifurcations, 12% of the coronaries featured extensive tortuosity, 11% had total occlusions, and 6% had ostial lesions. Lesion complexity scoring based on the American Heart Association and American College of Cardiology method rated 24% of the stenoses type C lesions and another 23% rated as B2 lesions. In addition, 38% of the lesions were at least 20 mm long.
Despite the challenging anatomy that many patients featured, device success occurred in 99% of the patients and procedure success in 98%, reported Dr. Eeckhout. Bailout treatment with a metal stent was needed in five patients (0.6%). During the 30 days following treatment the 800 patients had no deaths, and two cases (0.3%) of definite or probably stent thrombosis with both episodes occurring 1-30 days after scaffold placement – low rates given the complexity of the patients and lesions treated.
"These findings suggest the early safety and performance of Absorb in complex, real-world patients in daily PCI use," Dr. Eeckhout said. "Probably the operators [who treated these 800 patients] knew how to handle a BVS and they were able to expand to more complex pathology without an impact on safety or efficacy," he noted, adding that the "excellent results reflect the increasing experience of interventional cardiologists who use BVS; complexity did not impact efficacy or safety."
"These were "extraordinarily good outcomes in very complex patients," commented Dr. Stone, but he cautioned that the follow-up so far has been brief and that this was a "self-reported" registry, so it is possible that some operators failed to report some of their complications.
Other registry data reported at EuroPCR had longer follow-up, in some cases out to as long as 1 year, but in smaller patient sets and at fewer centers. These series represent "real world" use of BVS at these centers since Absorb came onto the European market in September 2012. Soon after BVS became commercially available, the interventionalists at these centers decided to use them in whichever patients they could regardless of their clinical status – in patients with acute coronary syndrome as well as stable patients, and regardless of lesion type or location. This contrasted with the initial, preapproval trials of BVS that excluded unstable patients and patients with complex coronary lesions or lesions in challenging sites, such as bifurcations or at an arterial ostium.
Findings from several ongoing registries were reported at EuroPCR:
• A group of six German centers had 1-year follow-up on 181 patients. Two thirds had class B2 or C lesions, 16% of lesions were calcified, and 14% involved side branches. These patients had a 5% rate of major adverse coronary events in the first year with no episodes of stent thrombosis, a result comparable with the pivotal trials for second-generation drug-eluting metallic stents as well as the early BVS studies that enrolled patients with simpler lesions, noted Dr. Thomas Schmitz, a cardiologist at the Contilla Heart and Vascular Center in Essen, Germany.
• Single-center experience at the Thoraxcenter in Rotterdam included 6-month follow-up on the first 180 of what are now more than 600 patients who have received BVS at the Thoraxcenter since it came onto the market. The series featured 48% of patients with calcified lesions, 41% with type B2 or C lesions, 38% of patients with multivessel disease, and lesion lengths up to 25 mm. Many patients received a BVS acutely after a ST-segment MI. Device success occurred in 98% of patients. The 6-month rate of major adverse coronary events was 3.3%, with definite or probable stent thrombosis in 2%, and 2% required target-lesion revascularization during 6 months of follow-up. "We had very good results in a complex group of patients that is getting closer to the real world by including patients with unstable and stable angina and ST-elevation myocardial infarction," said Dr. Robert-Jan van Geuns, a cardiologist at the Thoraxcenter. "We got stentlike results using a temporary scaffold. But we want to improve the flexibility of the BVS, reduce strut thickness, and make the procedures easier," he said.
• Interventionalists at Ferrarotto University Hospital in Catania, Italy, decided in March 2013 to start placing BVS when they could "regardless of lesion location or complexity." By this past May they had treated 367 lesions in 289 patients with BVS and had 6-month follow-up on 169 patients and 12-month follow-up on 48, said Dr. Corrado Tamburino, professor of cardiology and director of clinical cardiology at Ferrarotto. Half of their BVS patients had acute coronary syndrome, including 18% with ST-elevation MI, 17% with unstable angina, and 15% with non-STEMI. Half the treated lesions were class C or B2, 27% of patients had two or more lesions, 16% were at bifurcations, 9% were chronic total occlusions, and the mean lesion length was 21 mm. The operators successfully delivered BVS into 98% of patients. Among patients with 6-months’ follow-up, the incidence of major adverse coronary events was 2%, with no episodes of stent thrombosis after 30 days. The series included two deaths: one in a patient who stopped dual-antiplatelet therapy (DAPT) after 25 days and another in a patient who had an arterial dissection. All the BVS thromboses occurred within the first 30 days, "meaning it’s a technical issue. You need to always do lesion preparation, proper sizing [of the BVS for the artery it is entering], and post dilatation. If you do all that, you reduce the risk of thrombosis," he explained. The findings showed that placing "BVS is feasible and safe in the real world, and is effective at midterm follow-up. Stent thrombosis is not an issue if the procedural steps are respected. We expect similar results after 1 and 2 years, but we need to wait and be cautious," Dr. Tamburino said.
• Several centers in Poland began last year to enroll consecutive patients with acute coronary syndrome and culprit lesions that were amenable to BVS treatment. By May they had 1-year follow-up data on 94 BVS recipients, mostly patients with unstable angina or non–ST-elevation MI (NSTEMI) but also several with STEMI. The series had 100% success for BVS delivery and device success, with a 3% rate of major adverse coronary events while the patients remained initially hospitalized. After 12 months the patients had no deaths, three MIs, one target vessel revascularization, and one non–target vessel revascularization. Stent thrombosis occurred in one patient who prematurely stopped DAPT. The series so far has had no need for target-lesion revascularization. The 1-year results "show excellent outcomes. I’m amazed the results have been so good," said Dr. Dariusz Dudek, a cardiologist at University Hospital in Krakow, Poland.
• Interventionalists at two centers in Prague saw 311 consecutive patients with STEMI from December 2012 through the end of April 2014, and among these patients 79 (25%) met the group’s criteria for treatment with BVS. The operators excluded patients with a high likelihood of dying during the 2-3 year period for full BVS disappearance, with a Killip class of III or IV. They also excluded patients with an infarct-related artery less than 2.3 mm in diameter or more than 3.7 mm because of the limited size availability of BVS and because of the dangers from using incorrectly sized BVS. The 79 patients who received a BVS were a third of all patients in the series who received some form of PCI. An analysis presented by Dr. Petr Widimský, professor and head of the department of cardiology at Vinohrady Teaching Hospital in Prague, compared 9-month outcomes for these 79 patients who received BVS and 184 patients from the same series who also had Killip class I or II disease at the time of PCI. The remaining 48 patients from the series had Killip class III or IV disease and were excluded. After 9 months, event-free survival rate was 95% in the BVS recipients and 90% in the patients who received PCI with metallic stents, a nonsignificant difference. In the BVS group, 76 of the 79 patients successfully received a total of 85 BVS. Seventy-two of the 76 who received a BVS had an "ideal" procedural result, with no dissections and achievement of full blood flow through the treated lesion; the other four patients had slightly compromised blood flow after BVS placement. The 76 patients who successfully received a BVS had one death 4 hours after PCI as a result of septal rupture, and another BVS thrombosis 3 days after the patient stopped DAPT. A stroke or transient ischemic attack occurred in three patients. "We conclude that using BVS to treat acute STEMI is feasible and safe, and with currently available BVS sizes can be done in 25%-33% of STEMI patients. Having a 4.0-mm diameter BVS would substantially increase the number of patients we could treat," Dr. Widimský said.
• Cardiologists at one center in Barcelona treated 67 chronic total occlusions (CTO) since BVS became available, 49 of which could be crossed with a guidewire. Of these, the interventionalists could place a BVS in 38 patients; they excluded the other 11 patients because of excessive coronary-artery tortuosity, bifurcated lesions, or inappropriate vessel size. Among the 38 CTO patients who received BVS, three required bail-out PCI with a metallic stent because of a dissection. Average CTO length was 19 mm, and the average total lesion length was 36 mm. At 1-month follow-up, there were no deaths, no MI, no need for additional revascularization, and no BVS thrombosis. The same pattern held among the 33 patients from this group who had 6-months’ follow-up. "These surprising, extremely good results seem too good to be true," said Dr. Antonio Serra, an interventional cardiologist at Hospital Sant Pau in Barcelona. Results from the series so far "show that BVS is extremely feasible and safe for treating complex CTO. We report excellent patency and safety. The results at 6 months were outstanding."
Limits on BVS use
BVS are not for everyone. They get ruled out by substantial tortuosity of the route from the catheterization site to the affected coronary because BVS are stiffer than metallic stents and less amenable to pass through a winding arterial route. Patients need to be good candidates to remain on DAPT for at least 12 months, and the target-vessel diameter cannot veer too far from the currently available BVS diameters of 2.5, 3.0, or 3.5 mm. In most centers, these and other exclusion criteria usually rule out 75%-85% of patients, said several experienced BVS interventionalists at the meeting.
"I want patients who are healthy enough so they stay on DAPT. A BVS is not where you try 3 or 6 months of DAPT," said Dr. van Geuns. He also said that he would not use BVS for treating venous grafts, nor for in-stent restenosis because the existing metal likely would prevent late-lumen enlargement. And in some patients BVS cannot reach the lesion site despite aggressive predilation and vessel preparation.
"We’ve seen increasing breadth of use in the real world. It’s not yet true 100% all-comers, because appropriately people are learning where to use this technology," commented Dr. Stone.
"Our data represent a bias because it is not 100% of our patient population. They are the patients whom we think it is possible to implant a BVS," Dr. Tamburino said.
BVS "technology is not forgiving," Dr. van Guens pointed out. "If you leave a small lumen you will get a small lumen, and that can cause flow disturbances and perhaps a thrombus. Sometimes we are too eager with this technology. I think we can get to 100% in the future, but we should go slow because we are not there yet." He added that the number of BVS recipients and the rate of stent thrombosis were so far too small to allow meaningful analysis of which BVS recipients faced the greatest risk of stent thrombosis. Possible factors include inadequate post dilitation of the BVS, overexpansion of a BVS, and premature halt of DAPT.
"BVS is now feasible to use for every case" as long as the target vessel is no more than 10% smaller than the available BVS, Dr. Julinda Mehilli, an interventional cardiologist at the German Heart Center in Munich, said in a talk at the meeting. Preferred locations are long lesions in distal segments. Operators should be cautious using BVS to treat bifurcations, arteries with pronounced tortuosity, or arteries with moderate to severe calcification. When two BVS are needed in tandem, they should be placed as close to edge to edge as possible. She also stressed the need for systematic attention to every phase of BVS preparation and delivery, starting from selecting the appropriate BVS diameter to match the target vessel, predilation of the lesion and vessel and removal of calcium, gradual inflation of the BVS itself, and then followed by post dilitation of the BVS with a noncompliant balloon, ideally for at least 20 seconds.
"Now that we have BVS, it is the device of choice for chronic total occlusions because long term there is healing of the vessel walls when we use BVS. We often see long-term malopposition of stent struts in chronic total occlusions. With BVS the scaffold will disappear," eliminating the malopposition risk, Dr. Mehilli said.
Dr. Stone had no relevant disclosures, but he is lead investigator for an ongoing trial studying Abbot Vascular’s Absorb BVS. Dr. Serruys, Dr. Eeckhout, Dr. Schmitz, Dr. Dudek, and Dr. Serra had no disclosures. Dr. Tamburino is a consultant to Abbott Vascular and three other companies. Dr. Simonton is an employee of Abbott Vascular. Dr. van Geuns has received honoraria and research support from Abbott Vascular and other companies. Dr. Widimský has received honoraria from Abbott Vascular and other companies. Dr. Mehilli has received lecture fees from Abbott Vascular and other companies.
On Twitter @mitchelzoler
PARIS – Bioabsorbable vascular scaffolds have caught on in Europe and elsewhere in the world as an alternative to conventional metal stents for percutaneous coronary interventions in a wide spectrum of patient types.
By May 2014, more than 50,000 bioabsorbable vascular scaffolds (BVS) of the first brand to enter the European market – the Absorb stent made by Abbott Vascular – had gone into patients since the first placement in 2007, with the vast majority placed since this scaffold entered the European market in September 2012. Use of BVS in the United States remains investigational, while in the 20-plus months since BVS first became available in Europe other brands of BVS also have entered that market.
Despite growing BVS use in Europe, as well as in Asia and Central and South America, where they are also available, large-scale data on the consequences, especially long-term consequences, of BVS placement are mostly lacking, particularly data on how BVS perform when directly compared with drug-eluting metallic stents.
"Today we have uncontrolled dissemination of the technology without comparative data," Dr. Patrick W. Serruys, a pioneer in using BVS, said during a session at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
"We need evidence to know exactly what to do" with BVS, which patients to use them in, and when they are preferable to metallic stents, said Dr. Serruys, an interventional cardiologist and professor of medicine at the Thoraxcenter of Erasmus University in Rotterdam, the Netherlands.
"In the 7 years I’ve used them, in patients with 5-year follow-up, there have been no negative signals," he said in an interview, discussing his part of the sizeable anecdotal experience that BVS are safe and effective.
Several large trials comparing BVS with metal stents are in progress, including U.S. pivotal trials, but until these results are out, all that interventionalists have to gauge BVS performance are results from registries and uncontrolled trials. Given that limitation, so far the data look uniformly excellent.
"It is clear that emerging data from real-world, expanded-use registries suggest that use of the Absorb BVS is feasible and safe in a variety of patients, from low to high risk, and from simple to complex lesions," said Dr. Gregg W. Stone in a talk at the meeting. "But attention to procedural detail and technique is essential to optimize the outcomes. BVS are a little more complicated than metallic drug-eluting stents," said Dr. Stone, professor and director of cardiovascular research and education at Columbia University in New York.
"Data from large, randomized controlled trials are necessary to demonstrate whether BVS truly improve outcomes compared with best-in-class metallic stents. We are still early in the technology," he said. Dr. Stone is a lead investigator for one of the large U.S. randomized trials comparing the Absorb BVS to the current standard for percutaneous coronary interventions, a second-generation drug-eluting metallic stent.
Hints of what BVS may deliver
Hints of some of the potential benefits that BVS might provide appeared in results from a post-hoc, across-studies analysis that Dr. Stone presented in his talk. He compared the incidence of angina during the first year following PCI in 287 patients from the Absorb EXTEND study and 602 patients who received coronary stenting with the Xience second-generation everolimus-eluting metallic stent in the SPIRIT IV trial. The analysis matched patients in the Absorb arm with those in the Xience arm by propensity scoring.
The 1-year angina rates were 28% for the patients who received a metallic stent and 16% for those who received an absorbable scaffold, a 12% absolute difference, with a hazard ratio showing a 47% relative reduction in angina in patients who received the BVS, Dr. Stone reported. "There are a variety of mechanisms" by which BVS might reduce the rate of angina compared with metallic stents, including restoration of cyclic pulsatility in the treated arteries and improved vasomotion, he said.
The two outstanding clinical issues that dog PCI with second-generation drug-eluting metallic stents are the accrual of "very late" adverse events and the slow return of angina, with an average rate of target lesion failure with second-generation stents of about 1.8% year that continues out for at least 5 years, he said. "Can BVS flatten out the ongoing event rate" and improve measures like recurrent angina? Dr. Stone asked.
In another cross-study comparison, Dr. Serruys cited a recent, still unpublished analysis on which he collaborated that compared the 1-year outcomes of 102 patients with diabetes who received a BVS and 172 patients with diabetes who received a second-generation drug-eluting metallic stent. The 12-month cumulative rate of cardiovascular death, myocardial infarction, or ischemia-driven target lesion revascularization was 34.9% in the BVS recipients and 6.4% in patients who received state-of-the-art drug-eluting stents.
The working hypothesis behind BVS is that, by dissolving during a period of 12-24 months, the scaffold provides temporary bracing against restenosis but then disappears, allowing improved endovascular healing. During a separate session at EuroPCR, Dr. Charles A. Simonton, an interventional cardiologist and chief medical officer for Abbott Vascular, described the hypothesized impact that bioabsorbable coronary stents might have.
"Our vision is to convert interventional cardiology from mechanically oriented, plumbing-type interventions where you do mechanical things to open arteries" to a focus on tissue regeneration. "What we see when scaffolds resorb is that, at 3-5 years, the arteries look very different from what we see with a metal stent. The vessels show a highly functional neointimal layer that is functioning smooth muscle cells that protect against rupture in underlying plaque," he said.
Having BVS will allow interventional cardiologists to "transition from being mechanical plumbers to really being medical doctors. Not just opening lesions but putting in a treatment that can improve patients long term," Dr. Simonton said, presenting his best-case prediction of what BVS might achieve. "We need to generate a lot of data to make sure this is real," he added, in something of an understatement.
"There is late lumen enlargement with BVS. That is a clear fact," said Dr. Serruys.
The BVS experience
With data from studies that directly compared BVS and metallic stents still a few years off, the only indications of BVS performance now available come from either single- or multicenter registries. The thrust of much of these data presented at EuroPCR was that BVS have performed well as interventionalists have moved in the months since BVS became available for routine use to placing them in sicker patients and in patients with more complex coronary lesions.
The largest registry is ABSORB First, a voluntary-reporting registry that began in January 2013 and involves about 90 centers in countries where Absorb is commercially available in Europe, Asia, New Zealand, and Columbia. Dr. Eric Eeckhout, a cardiologist at Batiment Hospital in Lausanne, Switzerland, reported procedural and 30-day outcome data for the first 800 of the 1,305 patients enrolled in the registry as of May 2014.
Unlike previously reported multicenter series of patients getting BVS, these patients included 46% with at least two affected coronary arteries, 29% with stable angina, 15% with unstable angina, and 35% with an acute or recent MI. Significant calcification was present in 20% of the treated coronaries, 12% of the treated coronary stenoses were located at bifurcations, 12% of the coronaries featured extensive tortuosity, 11% had total occlusions, and 6% had ostial lesions. Lesion complexity scoring based on the American Heart Association and American College of Cardiology method rated 24% of the stenoses type C lesions and another 23% rated as B2 lesions. In addition, 38% of the lesions were at least 20 mm long.
Despite the challenging anatomy that many patients featured, device success occurred in 99% of the patients and procedure success in 98%, reported Dr. Eeckhout. Bailout treatment with a metal stent was needed in five patients (0.6%). During the 30 days following treatment the 800 patients had no deaths, and two cases (0.3%) of definite or probably stent thrombosis with both episodes occurring 1-30 days after scaffold placement – low rates given the complexity of the patients and lesions treated.
"These findings suggest the early safety and performance of Absorb in complex, real-world patients in daily PCI use," Dr. Eeckhout said. "Probably the operators [who treated these 800 patients] knew how to handle a BVS and they were able to expand to more complex pathology without an impact on safety or efficacy," he noted, adding that the "excellent results reflect the increasing experience of interventional cardiologists who use BVS; complexity did not impact efficacy or safety."
"These were "extraordinarily good outcomes in very complex patients," commented Dr. Stone, but he cautioned that the follow-up so far has been brief and that this was a "self-reported" registry, so it is possible that some operators failed to report some of their complications.
Other registry data reported at EuroPCR had longer follow-up, in some cases out to as long as 1 year, but in smaller patient sets and at fewer centers. These series represent "real world" use of BVS at these centers since Absorb came onto the European market in September 2012. Soon after BVS became commercially available, the interventionalists at these centers decided to use them in whichever patients they could regardless of their clinical status – in patients with acute coronary syndrome as well as stable patients, and regardless of lesion type or location. This contrasted with the initial, preapproval trials of BVS that excluded unstable patients and patients with complex coronary lesions or lesions in challenging sites, such as bifurcations or at an arterial ostium.
Findings from several ongoing registries were reported at EuroPCR:
• A group of six German centers had 1-year follow-up on 181 patients. Two thirds had class B2 or C lesions, 16% of lesions were calcified, and 14% involved side branches. These patients had a 5% rate of major adverse coronary events in the first year with no episodes of stent thrombosis, a result comparable with the pivotal trials for second-generation drug-eluting metallic stents as well as the early BVS studies that enrolled patients with simpler lesions, noted Dr. Thomas Schmitz, a cardiologist at the Contilla Heart and Vascular Center in Essen, Germany.
• Single-center experience at the Thoraxcenter in Rotterdam included 6-month follow-up on the first 180 of what are now more than 600 patients who have received BVS at the Thoraxcenter since it came onto the market. The series featured 48% of patients with calcified lesions, 41% with type B2 or C lesions, 38% of patients with multivessel disease, and lesion lengths up to 25 mm. Many patients received a BVS acutely after a ST-segment MI. Device success occurred in 98% of patients. The 6-month rate of major adverse coronary events was 3.3%, with definite or probable stent thrombosis in 2%, and 2% required target-lesion revascularization during 6 months of follow-up. "We had very good results in a complex group of patients that is getting closer to the real world by including patients with unstable and stable angina and ST-elevation myocardial infarction," said Dr. Robert-Jan van Geuns, a cardiologist at the Thoraxcenter. "We got stentlike results using a temporary scaffold. But we want to improve the flexibility of the BVS, reduce strut thickness, and make the procedures easier," he said.
• Interventionalists at Ferrarotto University Hospital in Catania, Italy, decided in March 2013 to start placing BVS when they could "regardless of lesion location or complexity." By this past May they had treated 367 lesions in 289 patients with BVS and had 6-month follow-up on 169 patients and 12-month follow-up on 48, said Dr. Corrado Tamburino, professor of cardiology and director of clinical cardiology at Ferrarotto. Half of their BVS patients had acute coronary syndrome, including 18% with ST-elevation MI, 17% with unstable angina, and 15% with non-STEMI. Half the treated lesions were class C or B2, 27% of patients had two or more lesions, 16% were at bifurcations, 9% were chronic total occlusions, and the mean lesion length was 21 mm. The operators successfully delivered BVS into 98% of patients. Among patients with 6-months’ follow-up, the incidence of major adverse coronary events was 2%, with no episodes of stent thrombosis after 30 days. The series included two deaths: one in a patient who stopped dual-antiplatelet therapy (DAPT) after 25 days and another in a patient who had an arterial dissection. All the BVS thromboses occurred within the first 30 days, "meaning it’s a technical issue. You need to always do lesion preparation, proper sizing [of the BVS for the artery it is entering], and post dilatation. If you do all that, you reduce the risk of thrombosis," he explained. The findings showed that placing "BVS is feasible and safe in the real world, and is effective at midterm follow-up. Stent thrombosis is not an issue if the procedural steps are respected. We expect similar results after 1 and 2 years, but we need to wait and be cautious," Dr. Tamburino said.
• Several centers in Poland began last year to enroll consecutive patients with acute coronary syndrome and culprit lesions that were amenable to BVS treatment. By May they had 1-year follow-up data on 94 BVS recipients, mostly patients with unstable angina or non–ST-elevation MI (NSTEMI) but also several with STEMI. The series had 100% success for BVS delivery and device success, with a 3% rate of major adverse coronary events while the patients remained initially hospitalized. After 12 months the patients had no deaths, three MIs, one target vessel revascularization, and one non–target vessel revascularization. Stent thrombosis occurred in one patient who prematurely stopped DAPT. The series so far has had no need for target-lesion revascularization. The 1-year results "show excellent outcomes. I’m amazed the results have been so good," said Dr. Dariusz Dudek, a cardiologist at University Hospital in Krakow, Poland.
• Interventionalists at two centers in Prague saw 311 consecutive patients with STEMI from December 2012 through the end of April 2014, and among these patients 79 (25%) met the group’s criteria for treatment with BVS. The operators excluded patients with a high likelihood of dying during the 2-3 year period for full BVS disappearance, with a Killip class of III or IV. They also excluded patients with an infarct-related artery less than 2.3 mm in diameter or more than 3.7 mm because of the limited size availability of BVS and because of the dangers from using incorrectly sized BVS. The 79 patients who received a BVS were a third of all patients in the series who received some form of PCI. An analysis presented by Dr. Petr Widimský, professor and head of the department of cardiology at Vinohrady Teaching Hospital in Prague, compared 9-month outcomes for these 79 patients who received BVS and 184 patients from the same series who also had Killip class I or II disease at the time of PCI. The remaining 48 patients from the series had Killip class III or IV disease and were excluded. After 9 months, event-free survival rate was 95% in the BVS recipients and 90% in the patients who received PCI with metallic stents, a nonsignificant difference. In the BVS group, 76 of the 79 patients successfully received a total of 85 BVS. Seventy-two of the 76 who received a BVS had an "ideal" procedural result, with no dissections and achievement of full blood flow through the treated lesion; the other four patients had slightly compromised blood flow after BVS placement. The 76 patients who successfully received a BVS had one death 4 hours after PCI as a result of septal rupture, and another BVS thrombosis 3 days after the patient stopped DAPT. A stroke or transient ischemic attack occurred in three patients. "We conclude that using BVS to treat acute STEMI is feasible and safe, and with currently available BVS sizes can be done in 25%-33% of STEMI patients. Having a 4.0-mm diameter BVS would substantially increase the number of patients we could treat," Dr. Widimský said.
• Cardiologists at one center in Barcelona treated 67 chronic total occlusions (CTO) since BVS became available, 49 of which could be crossed with a guidewire. Of these, the interventionalists could place a BVS in 38 patients; they excluded the other 11 patients because of excessive coronary-artery tortuosity, bifurcated lesions, or inappropriate vessel size. Among the 38 CTO patients who received BVS, three required bail-out PCI with a metallic stent because of a dissection. Average CTO length was 19 mm, and the average total lesion length was 36 mm. At 1-month follow-up, there were no deaths, no MI, no need for additional revascularization, and no BVS thrombosis. The same pattern held among the 33 patients from this group who had 6-months’ follow-up. "These surprising, extremely good results seem too good to be true," said Dr. Antonio Serra, an interventional cardiologist at Hospital Sant Pau in Barcelona. Results from the series so far "show that BVS is extremely feasible and safe for treating complex CTO. We report excellent patency and safety. The results at 6 months were outstanding."
Limits on BVS use
BVS are not for everyone. They get ruled out by substantial tortuosity of the route from the catheterization site to the affected coronary because BVS are stiffer than metallic stents and less amenable to pass through a winding arterial route. Patients need to be good candidates to remain on DAPT for at least 12 months, and the target-vessel diameter cannot veer too far from the currently available BVS diameters of 2.5, 3.0, or 3.5 mm. In most centers, these and other exclusion criteria usually rule out 75%-85% of patients, said several experienced BVS interventionalists at the meeting.
"I want patients who are healthy enough so they stay on DAPT. A BVS is not where you try 3 or 6 months of DAPT," said Dr. van Geuns. He also said that he would not use BVS for treating venous grafts, nor for in-stent restenosis because the existing metal likely would prevent late-lumen enlargement. And in some patients BVS cannot reach the lesion site despite aggressive predilation and vessel preparation.
"We’ve seen increasing breadth of use in the real world. It’s not yet true 100% all-comers, because appropriately people are learning where to use this technology," commented Dr. Stone.
"Our data represent a bias because it is not 100% of our patient population. They are the patients whom we think it is possible to implant a BVS," Dr. Tamburino said.
BVS "technology is not forgiving," Dr. van Guens pointed out. "If you leave a small lumen you will get a small lumen, and that can cause flow disturbances and perhaps a thrombus. Sometimes we are too eager with this technology. I think we can get to 100% in the future, but we should go slow because we are not there yet." He added that the number of BVS recipients and the rate of stent thrombosis were so far too small to allow meaningful analysis of which BVS recipients faced the greatest risk of stent thrombosis. Possible factors include inadequate post dilitation of the BVS, overexpansion of a BVS, and premature halt of DAPT.
"BVS is now feasible to use for every case" as long as the target vessel is no more than 10% smaller than the available BVS, Dr. Julinda Mehilli, an interventional cardiologist at the German Heart Center in Munich, said in a talk at the meeting. Preferred locations are long lesions in distal segments. Operators should be cautious using BVS to treat bifurcations, arteries with pronounced tortuosity, or arteries with moderate to severe calcification. When two BVS are needed in tandem, they should be placed as close to edge to edge as possible. She also stressed the need for systematic attention to every phase of BVS preparation and delivery, starting from selecting the appropriate BVS diameter to match the target vessel, predilation of the lesion and vessel and removal of calcium, gradual inflation of the BVS itself, and then followed by post dilitation of the BVS with a noncompliant balloon, ideally for at least 20 seconds.
"Now that we have BVS, it is the device of choice for chronic total occlusions because long term there is healing of the vessel walls when we use BVS. We often see long-term malopposition of stent struts in chronic total occlusions. With BVS the scaffold will disappear," eliminating the malopposition risk, Dr. Mehilli said.
Dr. Stone had no relevant disclosures, but he is lead investigator for an ongoing trial studying Abbot Vascular’s Absorb BVS. Dr. Serruys, Dr. Eeckhout, Dr. Schmitz, Dr. Dudek, and Dr. Serra had no disclosures. Dr. Tamburino is a consultant to Abbott Vascular and three other companies. Dr. Simonton is an employee of Abbott Vascular. Dr. van Geuns has received honoraria and research support from Abbott Vascular and other companies. Dr. Widimský has received honoraria from Abbott Vascular and other companies. Dr. Mehilli has received lecture fees from Abbott Vascular and other companies.
On Twitter @mitchelzoler
PARIS – Bioabsorbable vascular scaffolds have caught on in Europe and elsewhere in the world as an alternative to conventional metal stents for percutaneous coronary interventions in a wide spectrum of patient types.
By May 2014, more than 50,000 bioabsorbable vascular scaffolds (BVS) of the first brand to enter the European market – the Absorb stent made by Abbott Vascular – had gone into patients since the first placement in 2007, with the vast majority placed since this scaffold entered the European market in September 2012. Use of BVS in the United States remains investigational, while in the 20-plus months since BVS first became available in Europe other brands of BVS also have entered that market.
Despite growing BVS use in Europe, as well as in Asia and Central and South America, where they are also available, large-scale data on the consequences, especially long-term consequences, of BVS placement are mostly lacking, particularly data on how BVS perform when directly compared with drug-eluting metallic stents.
"Today we have uncontrolled dissemination of the technology without comparative data," Dr. Patrick W. Serruys, a pioneer in using BVS, said during a session at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
"We need evidence to know exactly what to do" with BVS, which patients to use them in, and when they are preferable to metallic stents, said Dr. Serruys, an interventional cardiologist and professor of medicine at the Thoraxcenter of Erasmus University in Rotterdam, the Netherlands.
"In the 7 years I’ve used them, in patients with 5-year follow-up, there have been no negative signals," he said in an interview, discussing his part of the sizeable anecdotal experience that BVS are safe and effective.
Several large trials comparing BVS with metal stents are in progress, including U.S. pivotal trials, but until these results are out, all that interventionalists have to gauge BVS performance are results from registries and uncontrolled trials. Given that limitation, so far the data look uniformly excellent.
"It is clear that emerging data from real-world, expanded-use registries suggest that use of the Absorb BVS is feasible and safe in a variety of patients, from low to high risk, and from simple to complex lesions," said Dr. Gregg W. Stone in a talk at the meeting. "But attention to procedural detail and technique is essential to optimize the outcomes. BVS are a little more complicated than metallic drug-eluting stents," said Dr. Stone, professor and director of cardiovascular research and education at Columbia University in New York.
"Data from large, randomized controlled trials are necessary to demonstrate whether BVS truly improve outcomes compared with best-in-class metallic stents. We are still early in the technology," he said. Dr. Stone is a lead investigator for one of the large U.S. randomized trials comparing the Absorb BVS to the current standard for percutaneous coronary interventions, a second-generation drug-eluting metallic stent.
Hints of what BVS may deliver
Hints of some of the potential benefits that BVS might provide appeared in results from a post-hoc, across-studies analysis that Dr. Stone presented in his talk. He compared the incidence of angina during the first year following PCI in 287 patients from the Absorb EXTEND study and 602 patients who received coronary stenting with the Xience second-generation everolimus-eluting metallic stent in the SPIRIT IV trial. The analysis matched patients in the Absorb arm with those in the Xience arm by propensity scoring.
The 1-year angina rates were 28% for the patients who received a metallic stent and 16% for those who received an absorbable scaffold, a 12% absolute difference, with a hazard ratio showing a 47% relative reduction in angina in patients who received the BVS, Dr. Stone reported. "There are a variety of mechanisms" by which BVS might reduce the rate of angina compared with metallic stents, including restoration of cyclic pulsatility in the treated arteries and improved vasomotion, he said.
The two outstanding clinical issues that dog PCI with second-generation drug-eluting metallic stents are the accrual of "very late" adverse events and the slow return of angina, with an average rate of target lesion failure with second-generation stents of about 1.8% year that continues out for at least 5 years, he said. "Can BVS flatten out the ongoing event rate" and improve measures like recurrent angina? Dr. Stone asked.
In another cross-study comparison, Dr. Serruys cited a recent, still unpublished analysis on which he collaborated that compared the 1-year outcomes of 102 patients with diabetes who received a BVS and 172 patients with diabetes who received a second-generation drug-eluting metallic stent. The 12-month cumulative rate of cardiovascular death, myocardial infarction, or ischemia-driven target lesion revascularization was 34.9% in the BVS recipients and 6.4% in patients who received state-of-the-art drug-eluting stents.
The working hypothesis behind BVS is that, by dissolving during a period of 12-24 months, the scaffold provides temporary bracing against restenosis but then disappears, allowing improved endovascular healing. During a separate session at EuroPCR, Dr. Charles A. Simonton, an interventional cardiologist and chief medical officer for Abbott Vascular, described the hypothesized impact that bioabsorbable coronary stents might have.
"Our vision is to convert interventional cardiology from mechanically oriented, plumbing-type interventions where you do mechanical things to open arteries" to a focus on tissue regeneration. "What we see when scaffolds resorb is that, at 3-5 years, the arteries look very different from what we see with a metal stent. The vessels show a highly functional neointimal layer that is functioning smooth muscle cells that protect against rupture in underlying plaque," he said.
Having BVS will allow interventional cardiologists to "transition from being mechanical plumbers to really being medical doctors. Not just opening lesions but putting in a treatment that can improve patients long term," Dr. Simonton said, presenting his best-case prediction of what BVS might achieve. "We need to generate a lot of data to make sure this is real," he added, in something of an understatement.
"There is late lumen enlargement with BVS. That is a clear fact," said Dr. Serruys.
The BVS experience
With data from studies that directly compared BVS and metallic stents still a few years off, the only indications of BVS performance now available come from either single- or multicenter registries. The thrust of much of these data presented at EuroPCR was that BVS have performed well as interventionalists have moved in the months since BVS became available for routine use to placing them in sicker patients and in patients with more complex coronary lesions.
The largest registry is ABSORB First, a voluntary-reporting registry that began in January 2013 and involves about 90 centers in countries where Absorb is commercially available in Europe, Asia, New Zealand, and Columbia. Dr. Eric Eeckhout, a cardiologist at Batiment Hospital in Lausanne, Switzerland, reported procedural and 30-day outcome data for the first 800 of the 1,305 patients enrolled in the registry as of May 2014.
Unlike previously reported multicenter series of patients getting BVS, these patients included 46% with at least two affected coronary arteries, 29% with stable angina, 15% with unstable angina, and 35% with an acute or recent MI. Significant calcification was present in 20% of the treated coronaries, 12% of the treated coronary stenoses were located at bifurcations, 12% of the coronaries featured extensive tortuosity, 11% had total occlusions, and 6% had ostial lesions. Lesion complexity scoring based on the American Heart Association and American College of Cardiology method rated 24% of the stenoses type C lesions and another 23% rated as B2 lesions. In addition, 38% of the lesions were at least 20 mm long.
Despite the challenging anatomy that many patients featured, device success occurred in 99% of the patients and procedure success in 98%, reported Dr. Eeckhout. Bailout treatment with a metal stent was needed in five patients (0.6%). During the 30 days following treatment the 800 patients had no deaths, and two cases (0.3%) of definite or probably stent thrombosis with both episodes occurring 1-30 days after scaffold placement – low rates given the complexity of the patients and lesions treated.
"These findings suggest the early safety and performance of Absorb in complex, real-world patients in daily PCI use," Dr. Eeckhout said. "Probably the operators [who treated these 800 patients] knew how to handle a BVS and they were able to expand to more complex pathology without an impact on safety or efficacy," he noted, adding that the "excellent results reflect the increasing experience of interventional cardiologists who use BVS; complexity did not impact efficacy or safety."
"These were "extraordinarily good outcomes in very complex patients," commented Dr. Stone, but he cautioned that the follow-up so far has been brief and that this was a "self-reported" registry, so it is possible that some operators failed to report some of their complications.
Other registry data reported at EuroPCR had longer follow-up, in some cases out to as long as 1 year, but in smaller patient sets and at fewer centers. These series represent "real world" use of BVS at these centers since Absorb came onto the European market in September 2012. Soon after BVS became commercially available, the interventionalists at these centers decided to use them in whichever patients they could regardless of their clinical status – in patients with acute coronary syndrome as well as stable patients, and regardless of lesion type or location. This contrasted with the initial, preapproval trials of BVS that excluded unstable patients and patients with complex coronary lesions or lesions in challenging sites, such as bifurcations or at an arterial ostium.
Findings from several ongoing registries were reported at EuroPCR:
• A group of six German centers had 1-year follow-up on 181 patients. Two thirds had class B2 or C lesions, 16% of lesions were calcified, and 14% involved side branches. These patients had a 5% rate of major adverse coronary events in the first year with no episodes of stent thrombosis, a result comparable with the pivotal trials for second-generation drug-eluting metallic stents as well as the early BVS studies that enrolled patients with simpler lesions, noted Dr. Thomas Schmitz, a cardiologist at the Contilla Heart and Vascular Center in Essen, Germany.
• Single-center experience at the Thoraxcenter in Rotterdam included 6-month follow-up on the first 180 of what are now more than 600 patients who have received BVS at the Thoraxcenter since it came onto the market. The series featured 48% of patients with calcified lesions, 41% with type B2 or C lesions, 38% of patients with multivessel disease, and lesion lengths up to 25 mm. Many patients received a BVS acutely after a ST-segment MI. Device success occurred in 98% of patients. The 6-month rate of major adverse coronary events was 3.3%, with definite or probable stent thrombosis in 2%, and 2% required target-lesion revascularization during 6 months of follow-up. "We had very good results in a complex group of patients that is getting closer to the real world by including patients with unstable and stable angina and ST-elevation myocardial infarction," said Dr. Robert-Jan van Geuns, a cardiologist at the Thoraxcenter. "We got stentlike results using a temporary scaffold. But we want to improve the flexibility of the BVS, reduce strut thickness, and make the procedures easier," he said.
• Interventionalists at Ferrarotto University Hospital in Catania, Italy, decided in March 2013 to start placing BVS when they could "regardless of lesion location or complexity." By this past May they had treated 367 lesions in 289 patients with BVS and had 6-month follow-up on 169 patients and 12-month follow-up on 48, said Dr. Corrado Tamburino, professor of cardiology and director of clinical cardiology at Ferrarotto. Half of their BVS patients had acute coronary syndrome, including 18% with ST-elevation MI, 17% with unstable angina, and 15% with non-STEMI. Half the treated lesions were class C or B2, 27% of patients had two or more lesions, 16% were at bifurcations, 9% were chronic total occlusions, and the mean lesion length was 21 mm. The operators successfully delivered BVS into 98% of patients. Among patients with 6-months’ follow-up, the incidence of major adverse coronary events was 2%, with no episodes of stent thrombosis after 30 days. The series included two deaths: one in a patient who stopped dual-antiplatelet therapy (DAPT) after 25 days and another in a patient who had an arterial dissection. All the BVS thromboses occurred within the first 30 days, "meaning it’s a technical issue. You need to always do lesion preparation, proper sizing [of the BVS for the artery it is entering], and post dilatation. If you do all that, you reduce the risk of thrombosis," he explained. The findings showed that placing "BVS is feasible and safe in the real world, and is effective at midterm follow-up. Stent thrombosis is not an issue if the procedural steps are respected. We expect similar results after 1 and 2 years, but we need to wait and be cautious," Dr. Tamburino said.
• Several centers in Poland began last year to enroll consecutive patients with acute coronary syndrome and culprit lesions that were amenable to BVS treatment. By May they had 1-year follow-up data on 94 BVS recipients, mostly patients with unstable angina or non–ST-elevation MI (NSTEMI) but also several with STEMI. The series had 100% success for BVS delivery and device success, with a 3% rate of major adverse coronary events while the patients remained initially hospitalized. After 12 months the patients had no deaths, three MIs, one target vessel revascularization, and one non–target vessel revascularization. Stent thrombosis occurred in one patient who prematurely stopped DAPT. The series so far has had no need for target-lesion revascularization. The 1-year results "show excellent outcomes. I’m amazed the results have been so good," said Dr. Dariusz Dudek, a cardiologist at University Hospital in Krakow, Poland.
• Interventionalists at two centers in Prague saw 311 consecutive patients with STEMI from December 2012 through the end of April 2014, and among these patients 79 (25%) met the group’s criteria for treatment with BVS. The operators excluded patients with a high likelihood of dying during the 2-3 year period for full BVS disappearance, with a Killip class of III or IV. They also excluded patients with an infarct-related artery less than 2.3 mm in diameter or more than 3.7 mm because of the limited size availability of BVS and because of the dangers from using incorrectly sized BVS. The 79 patients who received a BVS were a third of all patients in the series who received some form of PCI. An analysis presented by Dr. Petr Widimský, professor and head of the department of cardiology at Vinohrady Teaching Hospital in Prague, compared 9-month outcomes for these 79 patients who received BVS and 184 patients from the same series who also had Killip class I or II disease at the time of PCI. The remaining 48 patients from the series had Killip class III or IV disease and were excluded. After 9 months, event-free survival rate was 95% in the BVS recipients and 90% in the patients who received PCI with metallic stents, a nonsignificant difference. In the BVS group, 76 of the 79 patients successfully received a total of 85 BVS. Seventy-two of the 76 who received a BVS had an "ideal" procedural result, with no dissections and achievement of full blood flow through the treated lesion; the other four patients had slightly compromised blood flow after BVS placement. The 76 patients who successfully received a BVS had one death 4 hours after PCI as a result of septal rupture, and another BVS thrombosis 3 days after the patient stopped DAPT. A stroke or transient ischemic attack occurred in three patients. "We conclude that using BVS to treat acute STEMI is feasible and safe, and with currently available BVS sizes can be done in 25%-33% of STEMI patients. Having a 4.0-mm diameter BVS would substantially increase the number of patients we could treat," Dr. Widimský said.
• Cardiologists at one center in Barcelona treated 67 chronic total occlusions (CTO) since BVS became available, 49 of which could be crossed with a guidewire. Of these, the interventionalists could place a BVS in 38 patients; they excluded the other 11 patients because of excessive coronary-artery tortuosity, bifurcated lesions, or inappropriate vessel size. Among the 38 CTO patients who received BVS, three required bail-out PCI with a metallic stent because of a dissection. Average CTO length was 19 mm, and the average total lesion length was 36 mm. At 1-month follow-up, there were no deaths, no MI, no need for additional revascularization, and no BVS thrombosis. The same pattern held among the 33 patients from this group who had 6-months’ follow-up. "These surprising, extremely good results seem too good to be true," said Dr. Antonio Serra, an interventional cardiologist at Hospital Sant Pau in Barcelona. Results from the series so far "show that BVS is extremely feasible and safe for treating complex CTO. We report excellent patency and safety. The results at 6 months were outstanding."
Limits on BVS use
BVS are not for everyone. They get ruled out by substantial tortuosity of the route from the catheterization site to the affected coronary because BVS are stiffer than metallic stents and less amenable to pass through a winding arterial route. Patients need to be good candidates to remain on DAPT for at least 12 months, and the target-vessel diameter cannot veer too far from the currently available BVS diameters of 2.5, 3.0, or 3.5 mm. In most centers, these and other exclusion criteria usually rule out 75%-85% of patients, said several experienced BVS interventionalists at the meeting.
"I want patients who are healthy enough so they stay on DAPT. A BVS is not where you try 3 or 6 months of DAPT," said Dr. van Geuns. He also said that he would not use BVS for treating venous grafts, nor for in-stent restenosis because the existing metal likely would prevent late-lumen enlargement. And in some patients BVS cannot reach the lesion site despite aggressive predilation and vessel preparation.
"We’ve seen increasing breadth of use in the real world. It’s not yet true 100% all-comers, because appropriately people are learning where to use this technology," commented Dr. Stone.
"Our data represent a bias because it is not 100% of our patient population. They are the patients whom we think it is possible to implant a BVS," Dr. Tamburino said.
BVS "technology is not forgiving," Dr. van Guens pointed out. "If you leave a small lumen you will get a small lumen, and that can cause flow disturbances and perhaps a thrombus. Sometimes we are too eager with this technology. I think we can get to 100% in the future, but we should go slow because we are not there yet." He added that the number of BVS recipients and the rate of stent thrombosis were so far too small to allow meaningful analysis of which BVS recipients faced the greatest risk of stent thrombosis. Possible factors include inadequate post dilitation of the BVS, overexpansion of a BVS, and premature halt of DAPT.
"BVS is now feasible to use for every case" as long as the target vessel is no more than 10% smaller than the available BVS, Dr. Julinda Mehilli, an interventional cardiologist at the German Heart Center in Munich, said in a talk at the meeting. Preferred locations are long lesions in distal segments. Operators should be cautious using BVS to treat bifurcations, arteries with pronounced tortuosity, or arteries with moderate to severe calcification. When two BVS are needed in tandem, they should be placed as close to edge to edge as possible. She also stressed the need for systematic attention to every phase of BVS preparation and delivery, starting from selecting the appropriate BVS diameter to match the target vessel, predilation of the lesion and vessel and removal of calcium, gradual inflation of the BVS itself, and then followed by post dilitation of the BVS with a noncompliant balloon, ideally for at least 20 seconds.
"Now that we have BVS, it is the device of choice for chronic total occlusions because long term there is healing of the vessel walls when we use BVS. We often see long-term malopposition of stent struts in chronic total occlusions. With BVS the scaffold will disappear," eliminating the malopposition risk, Dr. Mehilli said.
Dr. Stone had no relevant disclosures, but he is lead investigator for an ongoing trial studying Abbot Vascular’s Absorb BVS. Dr. Serruys, Dr. Eeckhout, Dr. Schmitz, Dr. Dudek, and Dr. Serra had no disclosures. Dr. Tamburino is a consultant to Abbott Vascular and three other companies. Dr. Simonton is an employee of Abbott Vascular. Dr. van Geuns has received honoraria and research support from Abbott Vascular and other companies. Dr. Widimský has received honoraria from Abbott Vascular and other companies. Dr. Mehilli has received lecture fees from Abbott Vascular and other companies.
On Twitter @mitchelzoler
EXPERT ANALYSIS FROM EUROPCR 2014