User login
Catherine Hackett is editor of MDedge's Cardiology News and Clinical Endocrinology News. She joined the company in 2003. Before that, she was a researcher and managing editor for Time-Life Books, a fact checker for Smithsonian Magazine, and a technical editor at the American Journal of Clinical Nutrition.
Join us in Chicago for the ADA meeting!
Our team of expert reporters is making its way to Chicago for the American Diabetes Association annual scientific sessions. We’ve got a lot in store for you.
The President's Oral Sessions promise to be highlights of the meeting. The first session, on Friday, will emphasize provocative basic science trials, but one presentation stands out for us: The investigators evaluated whether islet transplantation can restore glucose counterregulation in patients with long-standing type 1 diabetes. Watch upcoming newsletters for our report on the findings from that research.
Tuesday's President's Oral Session will focus on clinical research, with some data that may have an immediate affect on how you practice:
• Should your type 1 diabetes patients count carbs? A meta-analysis sorts through the evidence.
• Should you go straight to triple therapy in a newly diagnosed type 2 diabetes patient? One team of investigators studied just that.
• What more can you learn about diabetes treatment and cancer risk from the ORIGIN trial?
With nearly 2,000 abstracts being presented, we can’t stop there. Look for our live and continuing reports from oral abstract and poster sessions, symposia, and "hot topic" Current Issues sessions.
If you're attending, get the mobile app, wear red on Sunday to Stop Diabetes, sign up for the 5K@ADA fun run, and check out our recommendations on making the most of Chicago while you’re there.
Our team of expert reporters is making its way to Chicago for the American Diabetes Association annual scientific sessions. We’ve got a lot in store for you.
The President's Oral Sessions promise to be highlights of the meeting. The first session, on Friday, will emphasize provocative basic science trials, but one presentation stands out for us: The investigators evaluated whether islet transplantation can restore glucose counterregulation in patients with long-standing type 1 diabetes. Watch upcoming newsletters for our report on the findings from that research.
Tuesday's President's Oral Session will focus on clinical research, with some data that may have an immediate affect on how you practice:
• Should your type 1 diabetes patients count carbs? A meta-analysis sorts through the evidence.
• Should you go straight to triple therapy in a newly diagnosed type 2 diabetes patient? One team of investigators studied just that.
• What more can you learn about diabetes treatment and cancer risk from the ORIGIN trial?
With nearly 2,000 abstracts being presented, we can’t stop there. Look for our live and continuing reports from oral abstract and poster sessions, symposia, and "hot topic" Current Issues sessions.
If you're attending, get the mobile app, wear red on Sunday to Stop Diabetes, sign up for the 5K@ADA fun run, and check out our recommendations on making the most of Chicago while you’re there.
Our team of expert reporters is making its way to Chicago for the American Diabetes Association annual scientific sessions. We’ve got a lot in store for you.
The President's Oral Sessions promise to be highlights of the meeting. The first session, on Friday, will emphasize provocative basic science trials, but one presentation stands out for us: The investigators evaluated whether islet transplantation can restore glucose counterregulation in patients with long-standing type 1 diabetes. Watch upcoming newsletters for our report on the findings from that research.
Tuesday's President's Oral Session will focus on clinical research, with some data that may have an immediate affect on how you practice:
• Should your type 1 diabetes patients count carbs? A meta-analysis sorts through the evidence.
• Should you go straight to triple therapy in a newly diagnosed type 2 diabetes patient? One team of investigators studied just that.
• What more can you learn about diabetes treatment and cancer risk from the ORIGIN trial?
With nearly 2,000 abstracts being presented, we can’t stop there. Look for our live and continuing reports from oral abstract and poster sessions, symposia, and "hot topic" Current Issues sessions.
If you're attending, get the mobile app, wear red on Sunday to Stop Diabetes, sign up for the 5K@ADA fun run, and check out our recommendations on making the most of Chicago while you’re there.
Ahead of the Journals: ROMICAT II Results Stir Controversy
Using cardiac computed tomography angiography as part of a triage strategy in patients with possible acute coronary syndromes improved the efficiency of clinical decision making and shortened hospital stays in the ROMICAT II trial, but it increased radiation exposure and did not save any money, compared with standard ED evaluation.
That’s according to the final report of the Rule Out Myocardial Infarction/Ischemia Using Computer Assisted Tomography study, published July 25 in the New England Journal of Medicine [http://www.nejm.org/doi/full/10.1056/NEJMoa1201161]. We reported the preliminary results, presented by Dr. Udo Hoffmann of Massachusetts General Hospital in Boston at the annual meeting of the American College of Cardiology in Chicago in March 2012.
The experts we interviewed for the story noted that the cardiac computed tomography angiography (CCTA) testing did not improve diagnostic accuracy, but did expose the patients' radiation exposure, and probably overestimated the cost savings because the study included only those patients presenting during regular work hours.
Dr. Rita F. Redberg, professor of medicine and director of Women's Cardiovascular Services at the University of California, San Francisco, expanded on those themes in an editorial in response to both the ROMICAT II article and another, similar trial published in the journal in April.
“The underlying assumption of [these two studies] is that some diagnostic test must be performed before discharging these low-to-intermediate-risk patients from the emergency department. This assumption is unproven and probably unwarranted. The rationale for any test, as compared with no testing, should be that it will lead to an improved outcome, and here there is no evidence that the tests performed led to improved outcomes.”
Dr. Redberg, who as editor of the Archives of Internal Medicine started its "Less Is More" feature a couple of years ago, acknowledging that the studies showed that a CCTA can be done in less time than a stress test. She added that "it is even faster to discharge these patients without any additional diagnostic test after determining that their ECG findings and troponin levels are normal. Thus, with no evidence of benefit and definite risks, routine testing in the emergency department of patients with a low-to-intermediate risk of acute coronary syndromes should be avoided." Dr. Redberg is also on the editorial board of Cardiology News.
Using cardiac computed tomography angiography as part of a triage strategy in patients with possible acute coronary syndromes improved the efficiency of clinical decision making and shortened hospital stays in the ROMICAT II trial, but it increased radiation exposure and did not save any money, compared with standard ED evaluation.
That’s according to the final report of the Rule Out Myocardial Infarction/Ischemia Using Computer Assisted Tomography study, published July 25 in the New England Journal of Medicine [http://www.nejm.org/doi/full/10.1056/NEJMoa1201161]. We reported the preliminary results, presented by Dr. Udo Hoffmann of Massachusetts General Hospital in Boston at the annual meeting of the American College of Cardiology in Chicago in March 2012.
The experts we interviewed for the story noted that the cardiac computed tomography angiography (CCTA) testing did not improve diagnostic accuracy, but did expose the patients' radiation exposure, and probably overestimated the cost savings because the study included only those patients presenting during regular work hours.
Dr. Rita F. Redberg, professor of medicine and director of Women's Cardiovascular Services at the University of California, San Francisco, expanded on those themes in an editorial in response to both the ROMICAT II article and another, similar trial published in the journal in April.
“The underlying assumption of [these two studies] is that some diagnostic test must be performed before discharging these low-to-intermediate-risk patients from the emergency department. This assumption is unproven and probably unwarranted. The rationale for any test, as compared with no testing, should be that it will lead to an improved outcome, and here there is no evidence that the tests performed led to improved outcomes.”
Dr. Redberg, who as editor of the Archives of Internal Medicine started its "Less Is More" feature a couple of years ago, acknowledging that the studies showed that a CCTA can be done in less time than a stress test. She added that "it is even faster to discharge these patients without any additional diagnostic test after determining that their ECG findings and troponin levels are normal. Thus, with no evidence of benefit and definite risks, routine testing in the emergency department of patients with a low-to-intermediate risk of acute coronary syndromes should be avoided." Dr. Redberg is also on the editorial board of Cardiology News.
Using cardiac computed tomography angiography as part of a triage strategy in patients with possible acute coronary syndromes improved the efficiency of clinical decision making and shortened hospital stays in the ROMICAT II trial, but it increased radiation exposure and did not save any money, compared with standard ED evaluation.
That’s according to the final report of the Rule Out Myocardial Infarction/Ischemia Using Computer Assisted Tomography study, published July 25 in the New England Journal of Medicine [http://www.nejm.org/doi/full/10.1056/NEJMoa1201161]. We reported the preliminary results, presented by Dr. Udo Hoffmann of Massachusetts General Hospital in Boston at the annual meeting of the American College of Cardiology in Chicago in March 2012.
The experts we interviewed for the story noted that the cardiac computed tomography angiography (CCTA) testing did not improve diagnostic accuracy, but did expose the patients' radiation exposure, and probably overestimated the cost savings because the study included only those patients presenting during regular work hours.
Dr. Rita F. Redberg, professor of medicine and director of Women's Cardiovascular Services at the University of California, San Francisco, expanded on those themes in an editorial in response to both the ROMICAT II article and another, similar trial published in the journal in April.
“The underlying assumption of [these two studies] is that some diagnostic test must be performed before discharging these low-to-intermediate-risk patients from the emergency department. This assumption is unproven and probably unwarranted. The rationale for any test, as compared with no testing, should be that it will lead to an improved outcome, and here there is no evidence that the tests performed led to improved outcomes.”
Dr. Redberg, who as editor of the Archives of Internal Medicine started its "Less Is More" feature a couple of years ago, acknowledging that the studies showed that a CCTA can be done in less time than a stress test. She added that "it is even faster to discharge these patients without any additional diagnostic test after determining that their ECG findings and troponin levels are normal. Thus, with no evidence of benefit and definite risks, routine testing in the emergency department of patients with a low-to-intermediate risk of acute coronary syndromes should be avoided." Dr. Redberg is also on the editorial board of Cardiology News.
PCI Trial Halted After FFR's Benefit Shown
A large trial in the use of fractional flow reserve to guide percutaneous coronary intervention in patients with stable coronary disease has been halted because of the benefit shown in the patients who received the intervention.
The data safety and monitoring board of the FAME II trial recommended stopping the study early based on the positive results of an interim analysis. The board found a highly statistically significant reduction in hospital readmission and urgent revascularization in stable coronary disease patients who received a stent based on fractional flow reserve (FFR) assessment, compared with those treated with optimal drug therapy, and determined it would be unethical to continue to randomize patients to optimal medical therapy (OMT) based on the results so far, St. Jude Medical announced Jan. 18 in a statement.
The coordinating clinical investigator for the trial, Dr. Bernard De Bruyne, considered this a practice-changing step. The results show FFR "should be considered the standard of care for patients with coronary artery disease."
"What we observed to date regarding urgent revascularizations validates the profound role that FFR-guided therapy has in improving patient outcomes," Dr. De Bruyne, coordinating clinical investigator for the trial and a cardiologist at Onze-Lieve-Vrouw Clinic, Aalst, Belgium, said in St. Jude’s statement.
"[FFR] should be considered the standard of care for patients with coronary artery disease."
But such sweeping statements are premature, according to Dr. Eric Bates, professor of internal medicine at the University of Michigan Health System in Ann Arbor. "The data need to be reviewed by the scientific community."
In FAME II, just over 1,200 patients had been randomized to either FFR-guided percutaneous coronary intervention or OMT in the trial, originally designed for 1,600 patients. Investigators will continue to follow enrolled patients, but no new patients will be added to the trial.
The devices used in the trial, the PressureWire Aeris and PressureWire Certus, combine measurements of pressure and temperature, enabling calculations of fractional flow reserve, coronary flow reserve, and an index of microcirculatory resistance.
The original FAME (Fractional Flow Reserve vs. Angiography for Guiding PCI in Patients with Multivessel Coronary Artery Disease) trial studied the procedure in patients who had already been selected for PCI. In that, patients whose PCI was guided by FFR had significantly reduced rates of the composite end point of death, nonfatal myocardial infarction, and repeat revascularization at 1 year, compared with those guided by angiography alone (N. Engl. J. Med. 2009;360:213-24). But the FAME II study, begun in 2010, is evaluating use of the tool for improving the benefits of stenting in the first place as an alternative to noninvasive medical therapy.
The latest PCI guidelines from the American College of Cardiology Foundation and the American Heart Association give FFR a tepid class IIa recommendation, saying it is reasonable for assessing angiographic intermediate coronary lesions (50%-70% diameter stenosis) and for guiding revascularization decisions in patients with stable ischemic heart disease (J. Am. Coll. Cardiol. 2011;58 [doi:10.1016/j.jacc.2011.08.007]). According to Dr. Bates, who was vice chair of the writing committee, fewer than 10% of PCI patients undergo FFR.
"Interestingly, there was no difference in death or MI rates" in St. Jude’s statement, "and no mention that the registered primary end point in clinicaltrials.org was the composite of death, MI, and unplanned hospitalization leading to urgent revascularization," he said in an interview. Without the data to examine, the conclusions that it is "unethical to randomize patients to OMT alone" and that FFR has a "profound role" are at the very least hyperbole. "Moreover, the mechanism for decreasing hospital readmission and urgent revascularization rates needs to be explained to me," he added.
Yet, "adding a functional assessment to anatomic data makes great sense and is clinically encouraged." To that end, the ISCHEMIA trial will soon start randomizing 8,000 patients with a LVEF of 35% or more and at least 10% cardiac ischemia. They will undergo blinded computed tomographic angiography to rule out high-risk left main disease or normal coronary arteries, and then will be randomized to catheterization and revascularization plus OMT or to optimal medical management alone, with revascularization reserved for worsening symptoms. The primary end point will be time to cardiovascular death or nonfatal MI*. Secondary end points will include cost effectiveness and quality of life measures.
Dr. Bates had no relevant disclosures.
David Filmore of "The Gray Sheet" contributed to this report. Cardiology News and "The Gray Sheet" are both owned by Elsevier.
*Correction, 1/25/2012: An earlier version of this story listed an incorrect primary end point for the ISCHEMIA trial.
A large trial in the use of fractional flow reserve to guide percutaneous coronary intervention in patients with stable coronary disease has been halted because of the benefit shown in the patients who received the intervention.
The data safety and monitoring board of the FAME II trial recommended stopping the study early based on the positive results of an interim analysis. The board found a highly statistically significant reduction in hospital readmission and urgent revascularization in stable coronary disease patients who received a stent based on fractional flow reserve (FFR) assessment, compared with those treated with optimal drug therapy, and determined it would be unethical to continue to randomize patients to optimal medical therapy (OMT) based on the results so far, St. Jude Medical announced Jan. 18 in a statement.
The coordinating clinical investigator for the trial, Dr. Bernard De Bruyne, considered this a practice-changing step. The results show FFR "should be considered the standard of care for patients with coronary artery disease."
"What we observed to date regarding urgent revascularizations validates the profound role that FFR-guided therapy has in improving patient outcomes," Dr. De Bruyne, coordinating clinical investigator for the trial and a cardiologist at Onze-Lieve-Vrouw Clinic, Aalst, Belgium, said in St. Jude’s statement.
"[FFR] should be considered the standard of care for patients with coronary artery disease."
But such sweeping statements are premature, according to Dr. Eric Bates, professor of internal medicine at the University of Michigan Health System in Ann Arbor. "The data need to be reviewed by the scientific community."
In FAME II, just over 1,200 patients had been randomized to either FFR-guided percutaneous coronary intervention or OMT in the trial, originally designed for 1,600 patients. Investigators will continue to follow enrolled patients, but no new patients will be added to the trial.
The devices used in the trial, the PressureWire Aeris and PressureWire Certus, combine measurements of pressure and temperature, enabling calculations of fractional flow reserve, coronary flow reserve, and an index of microcirculatory resistance.
The original FAME (Fractional Flow Reserve vs. Angiography for Guiding PCI in Patients with Multivessel Coronary Artery Disease) trial studied the procedure in patients who had already been selected for PCI. In that, patients whose PCI was guided by FFR had significantly reduced rates of the composite end point of death, nonfatal myocardial infarction, and repeat revascularization at 1 year, compared with those guided by angiography alone (N. Engl. J. Med. 2009;360:213-24). But the FAME II study, begun in 2010, is evaluating use of the tool for improving the benefits of stenting in the first place as an alternative to noninvasive medical therapy.
The latest PCI guidelines from the American College of Cardiology Foundation and the American Heart Association give FFR a tepid class IIa recommendation, saying it is reasonable for assessing angiographic intermediate coronary lesions (50%-70% diameter stenosis) and for guiding revascularization decisions in patients with stable ischemic heart disease (J. Am. Coll. Cardiol. 2011;58 [doi:10.1016/j.jacc.2011.08.007]). According to Dr. Bates, who was vice chair of the writing committee, fewer than 10% of PCI patients undergo FFR.
"Interestingly, there was no difference in death or MI rates" in St. Jude’s statement, "and no mention that the registered primary end point in clinicaltrials.org was the composite of death, MI, and unplanned hospitalization leading to urgent revascularization," he said in an interview. Without the data to examine, the conclusions that it is "unethical to randomize patients to OMT alone" and that FFR has a "profound role" are at the very least hyperbole. "Moreover, the mechanism for decreasing hospital readmission and urgent revascularization rates needs to be explained to me," he added.
Yet, "adding a functional assessment to anatomic data makes great sense and is clinically encouraged." To that end, the ISCHEMIA trial will soon start randomizing 8,000 patients with a LVEF of 35% or more and at least 10% cardiac ischemia. They will undergo blinded computed tomographic angiography to rule out high-risk left main disease or normal coronary arteries, and then will be randomized to catheterization and revascularization plus OMT or to optimal medical management alone, with revascularization reserved for worsening symptoms. The primary end point will be time to cardiovascular death or nonfatal MI*. Secondary end points will include cost effectiveness and quality of life measures.
Dr. Bates had no relevant disclosures.
David Filmore of "The Gray Sheet" contributed to this report. Cardiology News and "The Gray Sheet" are both owned by Elsevier.
*Correction, 1/25/2012: An earlier version of this story listed an incorrect primary end point for the ISCHEMIA trial.
A large trial in the use of fractional flow reserve to guide percutaneous coronary intervention in patients with stable coronary disease has been halted because of the benefit shown in the patients who received the intervention.
The data safety and monitoring board of the FAME II trial recommended stopping the study early based on the positive results of an interim analysis. The board found a highly statistically significant reduction in hospital readmission and urgent revascularization in stable coronary disease patients who received a stent based on fractional flow reserve (FFR) assessment, compared with those treated with optimal drug therapy, and determined it would be unethical to continue to randomize patients to optimal medical therapy (OMT) based on the results so far, St. Jude Medical announced Jan. 18 in a statement.
The coordinating clinical investigator for the trial, Dr. Bernard De Bruyne, considered this a practice-changing step. The results show FFR "should be considered the standard of care for patients with coronary artery disease."
"What we observed to date regarding urgent revascularizations validates the profound role that FFR-guided therapy has in improving patient outcomes," Dr. De Bruyne, coordinating clinical investigator for the trial and a cardiologist at Onze-Lieve-Vrouw Clinic, Aalst, Belgium, said in St. Jude’s statement.
"[FFR] should be considered the standard of care for patients with coronary artery disease."
But such sweeping statements are premature, according to Dr. Eric Bates, professor of internal medicine at the University of Michigan Health System in Ann Arbor. "The data need to be reviewed by the scientific community."
In FAME II, just over 1,200 patients had been randomized to either FFR-guided percutaneous coronary intervention or OMT in the trial, originally designed for 1,600 patients. Investigators will continue to follow enrolled patients, but no new patients will be added to the trial.
The devices used in the trial, the PressureWire Aeris and PressureWire Certus, combine measurements of pressure and temperature, enabling calculations of fractional flow reserve, coronary flow reserve, and an index of microcirculatory resistance.
The original FAME (Fractional Flow Reserve vs. Angiography for Guiding PCI in Patients with Multivessel Coronary Artery Disease) trial studied the procedure in patients who had already been selected for PCI. In that, patients whose PCI was guided by FFR had significantly reduced rates of the composite end point of death, nonfatal myocardial infarction, and repeat revascularization at 1 year, compared with those guided by angiography alone (N. Engl. J. Med. 2009;360:213-24). But the FAME II study, begun in 2010, is evaluating use of the tool for improving the benefits of stenting in the first place as an alternative to noninvasive medical therapy.
The latest PCI guidelines from the American College of Cardiology Foundation and the American Heart Association give FFR a tepid class IIa recommendation, saying it is reasonable for assessing angiographic intermediate coronary lesions (50%-70% diameter stenosis) and for guiding revascularization decisions in patients with stable ischemic heart disease (J. Am. Coll. Cardiol. 2011;58 [doi:10.1016/j.jacc.2011.08.007]). According to Dr. Bates, who was vice chair of the writing committee, fewer than 10% of PCI patients undergo FFR.
"Interestingly, there was no difference in death or MI rates" in St. Jude’s statement, "and no mention that the registered primary end point in clinicaltrials.org was the composite of death, MI, and unplanned hospitalization leading to urgent revascularization," he said in an interview. Without the data to examine, the conclusions that it is "unethical to randomize patients to OMT alone" and that FFR has a "profound role" are at the very least hyperbole. "Moreover, the mechanism for decreasing hospital readmission and urgent revascularization rates needs to be explained to me," he added.
Yet, "adding a functional assessment to anatomic data makes great sense and is clinically encouraged." To that end, the ISCHEMIA trial will soon start randomizing 8,000 patients with a LVEF of 35% or more and at least 10% cardiac ischemia. They will undergo blinded computed tomographic angiography to rule out high-risk left main disease or normal coronary arteries, and then will be randomized to catheterization and revascularization plus OMT or to optimal medical management alone, with revascularization reserved for worsening symptoms. The primary end point will be time to cardiovascular death or nonfatal MI*. Secondary end points will include cost effectiveness and quality of life measures.
Dr. Bates had no relevant disclosures.
David Filmore of "The Gray Sheet" contributed to this report. Cardiology News and "The Gray Sheet" are both owned by Elsevier.
*Correction, 1/25/2012: An earlier version of this story listed an incorrect primary end point for the ISCHEMIA trial.
FDA Investigating Reports of Bleeding Events With Pradaxa
The Food and Drug Administration is looking into reports of serious bleeding events associated with the anticoagulant dabigatran, the agency announced on Dec. 7.
Dabigatran (Pradaxa) was approved in October 2010 for long-term anticoagulation in patients with atrial fibrillation. The bleeding events, about which the FDA’s Division of Drug Information did not provide specifics, were reported to the Adverse Events Reporting System and were evaluated in November.
"While serious, even fatal events have been reported, the FDA is analyzing the events to determine whether the reports of bleeding in patients taking Pradaxa are occurring more commonly than would be expected, based on observations in the large clinical trial that supported the approval of Pradaxa," the agency wrote.
That trial was the RE-LY (Randomized Evaluation of Long Term Anticoagulant Therapy), a noninferiority study of 18,113 patients with nonvalvular atrial fibrillation and at least one other risk factor for stroke. Only the higher of two doses tested, 110 mg and 150 mg, was approved, apparently because it was more effective than warfarin in preventing stroke and systemic embolism. The 150-mg dose was found to be associated with a significantly increased risk of major GI bleeding, compared with warfarin, but also with a significant reduction in life-threatening and total bleeding.
The agency acknowledges that determining whether the reported events are occurring more than with dabigatran’s alternative, warfarin, is problematic. "Because warfarin has been marketed for over 50 years and is well-known to cause bleeding, patients and healthcare professionals are not likely to report bleeding in association with warfarin."
The FDA reaffirmed its belief that "the benefits of Pradaxa continue to exceed the potential risks when the drug is used appropriately." Further, it urged that health care professionals continue to prescribe Pradaxa, which is manufactured by Boehringer Ingelheim, following the recommendations in the drug label.
The Food and Drug Administration is looking into reports of serious bleeding events associated with the anticoagulant dabigatran, the agency announced on Dec. 7.
Dabigatran (Pradaxa) was approved in October 2010 for long-term anticoagulation in patients with atrial fibrillation. The bleeding events, about which the FDA’s Division of Drug Information did not provide specifics, were reported to the Adverse Events Reporting System and were evaluated in November.
"While serious, even fatal events have been reported, the FDA is analyzing the events to determine whether the reports of bleeding in patients taking Pradaxa are occurring more commonly than would be expected, based on observations in the large clinical trial that supported the approval of Pradaxa," the agency wrote.
That trial was the RE-LY (Randomized Evaluation of Long Term Anticoagulant Therapy), a noninferiority study of 18,113 patients with nonvalvular atrial fibrillation and at least one other risk factor for stroke. Only the higher of two doses tested, 110 mg and 150 mg, was approved, apparently because it was more effective than warfarin in preventing stroke and systemic embolism. The 150-mg dose was found to be associated with a significantly increased risk of major GI bleeding, compared with warfarin, but also with a significant reduction in life-threatening and total bleeding.
The agency acknowledges that determining whether the reported events are occurring more than with dabigatran’s alternative, warfarin, is problematic. "Because warfarin has been marketed for over 50 years and is well-known to cause bleeding, patients and healthcare professionals are not likely to report bleeding in association with warfarin."
The FDA reaffirmed its belief that "the benefits of Pradaxa continue to exceed the potential risks when the drug is used appropriately." Further, it urged that health care professionals continue to prescribe Pradaxa, which is manufactured by Boehringer Ingelheim, following the recommendations in the drug label.
The Food and Drug Administration is looking into reports of serious bleeding events associated with the anticoagulant dabigatran, the agency announced on Dec. 7.
Dabigatran (Pradaxa) was approved in October 2010 for long-term anticoagulation in patients with atrial fibrillation. The bleeding events, about which the FDA’s Division of Drug Information did not provide specifics, were reported to the Adverse Events Reporting System and were evaluated in November.
"While serious, even fatal events have been reported, the FDA is analyzing the events to determine whether the reports of bleeding in patients taking Pradaxa are occurring more commonly than would be expected, based on observations in the large clinical trial that supported the approval of Pradaxa," the agency wrote.
That trial was the RE-LY (Randomized Evaluation of Long Term Anticoagulant Therapy), a noninferiority study of 18,113 patients with nonvalvular atrial fibrillation and at least one other risk factor for stroke. Only the higher of two doses tested, 110 mg and 150 mg, was approved, apparently because it was more effective than warfarin in preventing stroke and systemic embolism. The 150-mg dose was found to be associated with a significantly increased risk of major GI bleeding, compared with warfarin, but also with a significant reduction in life-threatening and total bleeding.
The agency acknowledges that determining whether the reported events are occurring more than with dabigatran’s alternative, warfarin, is problematic. "Because warfarin has been marketed for over 50 years and is well-known to cause bleeding, patients and healthcare professionals are not likely to report bleeding in association with warfarin."
The FDA reaffirmed its belief that "the benefits of Pradaxa continue to exceed the potential risks when the drug is used appropriately." Further, it urged that health care professionals continue to prescribe Pradaxa, which is manufactured by Boehringer Ingelheim, following the recommendations in the drug label.
IDF Backs Bariatric Surgery for Type 2 Diabetes
Bariatric surgery should be considered as a treatment option for type 2 diabetes patients with body mass indexes between 30 and 35 kg/m2 and diabetes that can’t be controlled adequately by an optimal medical regimen – particularly in patients with other major cardiovascular disease risk factors, according to a statement from the International Diabetes Federation.
The position statement, "Bariatric Surgical and Procedural Interventions in the Treatment of Obese Patients with Type 2 Diabetes" is in response to the global epidemic of obesity-related diabetes and the failure of lifestyle and medical treatments to prevent dangerous and costly comorbidities. It goes further than does the American Diabetes Association’s guidance on bariatric surgery, which cautions that type 2 diabetes patients with a BMI between 30 and 35 should only undergo surgery in the context of a clinical research study.
However, "bariatric procedures are not a public health solution for ‘diabesity,’ " cautioned Dr. Paul Zimmet, cochair of the IDF Task Force on Epidemiology and Prevention, and research is needed to continue to define the persons most likely to benefit. It will require very strict criteria for patient selection and the availability of the best circumstances – high-volume centers with competent surgeons, the best procedures, adequate follow-up, and proper evaluation of outcomes, Dr. Zimmet said in an interview.
Results from lifestyle and medical methods for weight loss are "modest and rarely sustained, particularly in the severely obese," the IDF statement noted. Furthermore, pervasive attitudes toward obesity – as a personal failure rather than a complex condition influenced by strong physical, emotional, and societal issues – effectively erect barriers to care and equal treatment at work, according to the statement.
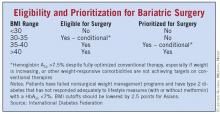
The metabolic benefits of gastrointestinal surgery go beyond that achieved by weight loss alone. Normalization not only of hyperglycemia but also of hyperlipidemia, blood pressure, and obstructive sleep apnea has been shown consistently. And long-term follow-up has shown reductions in mortality from coronary artery disease, diabetes, and cancer. Therefore, surgical intervention should be a part of diabetes treatment algorithms (see table), according to the IDF statement. In fact, because early intervention increases the likelihood of remission, and residual hyperglycemia is easier to manage after surgery, intervention for type 2 diabetes patients "should be considered early as an option for eligible patients, rather than being held back as a last resort," the IDF recommended.
Obesity and diabetes have such powerful effects on health and longevity that their surging worldwide prevalence constitutes a major global health issue that "demands urgent attention from governments, health care systems, and the medical community," said the group.
The IDF noted that the complication risks of surgery have gone down considerably over time, especially since laparoscopic procedures have been used. But the long-term risks are numerous and vary by procedure, ranging from the need for revision to nutritional deficiencies. Lifelong monitoring is required, and national registries should be established and funded.
The surgeries are cost effective for diabetes, according to the statement. Studies in the United States, Australia, and the United Kingdom have shown that an intervention leads to the rare outcome of generating "both cost savings and health benefits over the lifetime of the cohort" and "provides the most compelling evidence for funding based on economic criteria."
The IDF task force did not recommend any one type of surgery. "There is a need for well-designed, randomized, controlled trials to compare both efficacy and cost [of bariatric surgeries]. Those data do not exist," said Dr. Zimmet, director emeritus of the Baker IDI Heart and Diabetes Institute, Melbourne. But in the United States, the only procedure with Food and Drug Administration approval for patients with a BMI of 30 is adjustable gastric banding.
"This is the first time the International Diabetes Federation or any major international organization has made recommendations on this rapidly developing area of therapy," Dr. Francesco Rubino, chief of the gastrointestinal metabolic surgery at New York–Presbyterian Hospital/Weill Cornell Medical Center, New York, said in a statement. "It did so because of the urgent need for worldwide expert guidance on the use of bariatric surgery because of the increasing usage."
The announcement was made from the World Congress on Interventional Therapies for Type 2 Diabetes, held in New York and directed by Dr. Rubino.
The consensus meeting was supported with an unrestricted educational grant by Allergan Inc., Ethicon, Ethicon Endo-Surgery Inc., and MetaCure Inc. These companies played no role in the discussion or preparation of the position paper, according to the task force statement. Members of the writing group had no disclosures.
Bariatric surgery should be considered as a treatment option for type 2 diabetes patients with body mass indexes between 30 and 35 kg/m2 and diabetes that can’t be controlled adequately by an optimal medical regimen – particularly in patients with other major cardiovascular disease risk factors, according to a statement from the International Diabetes Federation.
The position statement, "Bariatric Surgical and Procedural Interventions in the Treatment of Obese Patients with Type 2 Diabetes" is in response to the global epidemic of obesity-related diabetes and the failure of lifestyle and medical treatments to prevent dangerous and costly comorbidities. It goes further than does the American Diabetes Association’s guidance on bariatric surgery, which cautions that type 2 diabetes patients with a BMI between 30 and 35 should only undergo surgery in the context of a clinical research study.
However, "bariatric procedures are not a public health solution for ‘diabesity,’ " cautioned Dr. Paul Zimmet, cochair of the IDF Task Force on Epidemiology and Prevention, and research is needed to continue to define the persons most likely to benefit. It will require very strict criteria for patient selection and the availability of the best circumstances – high-volume centers with competent surgeons, the best procedures, adequate follow-up, and proper evaluation of outcomes, Dr. Zimmet said in an interview.
Results from lifestyle and medical methods for weight loss are "modest and rarely sustained, particularly in the severely obese," the IDF statement noted. Furthermore, pervasive attitudes toward obesity – as a personal failure rather than a complex condition influenced by strong physical, emotional, and societal issues – effectively erect barriers to care and equal treatment at work, according to the statement.
The metabolic benefits of gastrointestinal surgery go beyond that achieved by weight loss alone. Normalization not only of hyperglycemia but also of hyperlipidemia, blood pressure, and obstructive sleep apnea has been shown consistently. And long-term follow-up has shown reductions in mortality from coronary artery disease, diabetes, and cancer. Therefore, surgical intervention should be a part of diabetes treatment algorithms (see table), according to the IDF statement. In fact, because early intervention increases the likelihood of remission, and residual hyperglycemia is easier to manage after surgery, intervention for type 2 diabetes patients "should be considered early as an option for eligible patients, rather than being held back as a last resort," the IDF recommended.
Obesity and diabetes have such powerful effects on health and longevity that their surging worldwide prevalence constitutes a major global health issue that "demands urgent attention from governments, health care systems, and the medical community," said the group.
The IDF noted that the complication risks of surgery have gone down considerably over time, especially since laparoscopic procedures have been used. But the long-term risks are numerous and vary by procedure, ranging from the need for revision to nutritional deficiencies. Lifelong monitoring is required, and national registries should be established and funded.
The surgeries are cost effective for diabetes, according to the statement. Studies in the United States, Australia, and the United Kingdom have shown that an intervention leads to the rare outcome of generating "both cost savings and health benefits over the lifetime of the cohort" and "provides the most compelling evidence for funding based on economic criteria."
The IDF task force did not recommend any one type of surgery. "There is a need for well-designed, randomized, controlled trials to compare both efficacy and cost [of bariatric surgeries]. Those data do not exist," said Dr. Zimmet, director emeritus of the Baker IDI Heart and Diabetes Institute, Melbourne. But in the United States, the only procedure with Food and Drug Administration approval for patients with a BMI of 30 is adjustable gastric banding.
"This is the first time the International Diabetes Federation or any major international organization has made recommendations on this rapidly developing area of therapy," Dr. Francesco Rubino, chief of the gastrointestinal metabolic surgery at New York–Presbyterian Hospital/Weill Cornell Medical Center, New York, said in a statement. "It did so because of the urgent need for worldwide expert guidance on the use of bariatric surgery because of the increasing usage."
The announcement was made from the World Congress on Interventional Therapies for Type 2 Diabetes, held in New York and directed by Dr. Rubino.
The consensus meeting was supported with an unrestricted educational grant by Allergan Inc., Ethicon, Ethicon Endo-Surgery Inc., and MetaCure Inc. These companies played no role in the discussion or preparation of the position paper, according to the task force statement. Members of the writing group had no disclosures.
Bariatric surgery should be considered as a treatment option for type 2 diabetes patients with body mass indexes between 30 and 35 kg/m2 and diabetes that can’t be controlled adequately by an optimal medical regimen – particularly in patients with other major cardiovascular disease risk factors, according to a statement from the International Diabetes Federation.
The position statement, "Bariatric Surgical and Procedural Interventions in the Treatment of Obese Patients with Type 2 Diabetes" is in response to the global epidemic of obesity-related diabetes and the failure of lifestyle and medical treatments to prevent dangerous and costly comorbidities. It goes further than does the American Diabetes Association’s guidance on bariatric surgery, which cautions that type 2 diabetes patients with a BMI between 30 and 35 should only undergo surgery in the context of a clinical research study.
However, "bariatric procedures are not a public health solution for ‘diabesity,’ " cautioned Dr. Paul Zimmet, cochair of the IDF Task Force on Epidemiology and Prevention, and research is needed to continue to define the persons most likely to benefit. It will require very strict criteria for patient selection and the availability of the best circumstances – high-volume centers with competent surgeons, the best procedures, adequate follow-up, and proper evaluation of outcomes, Dr. Zimmet said in an interview.
Results from lifestyle and medical methods for weight loss are "modest and rarely sustained, particularly in the severely obese," the IDF statement noted. Furthermore, pervasive attitudes toward obesity – as a personal failure rather than a complex condition influenced by strong physical, emotional, and societal issues – effectively erect barriers to care and equal treatment at work, according to the statement.
The metabolic benefits of gastrointestinal surgery go beyond that achieved by weight loss alone. Normalization not only of hyperglycemia but also of hyperlipidemia, blood pressure, and obstructive sleep apnea has been shown consistently. And long-term follow-up has shown reductions in mortality from coronary artery disease, diabetes, and cancer. Therefore, surgical intervention should be a part of diabetes treatment algorithms (see table), according to the IDF statement. In fact, because early intervention increases the likelihood of remission, and residual hyperglycemia is easier to manage after surgery, intervention for type 2 diabetes patients "should be considered early as an option for eligible patients, rather than being held back as a last resort," the IDF recommended.
Obesity and diabetes have such powerful effects on health and longevity that their surging worldwide prevalence constitutes a major global health issue that "demands urgent attention from governments, health care systems, and the medical community," said the group.
The IDF noted that the complication risks of surgery have gone down considerably over time, especially since laparoscopic procedures have been used. But the long-term risks are numerous and vary by procedure, ranging from the need for revision to nutritional deficiencies. Lifelong monitoring is required, and national registries should be established and funded.
The surgeries are cost effective for diabetes, according to the statement. Studies in the United States, Australia, and the United Kingdom have shown that an intervention leads to the rare outcome of generating "both cost savings and health benefits over the lifetime of the cohort" and "provides the most compelling evidence for funding based on economic criteria."
The IDF task force did not recommend any one type of surgery. "There is a need for well-designed, randomized, controlled trials to compare both efficacy and cost [of bariatric surgeries]. Those data do not exist," said Dr. Zimmet, director emeritus of the Baker IDI Heart and Diabetes Institute, Melbourne. But in the United States, the only procedure with Food and Drug Administration approval for patients with a BMI of 30 is adjustable gastric banding.
"This is the first time the International Diabetes Federation or any major international organization has made recommendations on this rapidly developing area of therapy," Dr. Francesco Rubino, chief of the gastrointestinal metabolic surgery at New York–Presbyterian Hospital/Weill Cornell Medical Center, New York, said in a statement. "It did so because of the urgent need for worldwide expert guidance on the use of bariatric surgery because of the increasing usage."
The announcement was made from the World Congress on Interventional Therapies for Type 2 Diabetes, held in New York and directed by Dr. Rubino.
The consensus meeting was supported with an unrestricted educational grant by Allergan Inc., Ethicon, Ethicon Endo-Surgery Inc., and MetaCure Inc. These companies played no role in the discussion or preparation of the position paper, according to the task force statement. Members of the writing group had no disclosures.
FROM A STATEMENT BY THE INTERNATIONAL DIABETES FEDERATION
IDF Backs Bariatric Surgery for Type 2 Diabetes
Bariatric surgery should be considered as a treatment option for type 2 diabetes patients with body mass indexes between 30 and 35 kg/m2 and diabetes that can’t be controlled adequately by an optimal medical regimen – particularly in patients with other major cardiovascular disease risk factors, according to a statement from the International Diabetes Federation.
The position statement, "Bariatric Surgical and Procedural Interventions in the Treatment of Obese Patients with Type 2 Diabetes" is in response to the global epidemic of obesity-related diabetes and the failure of lifestyle and medical treatments to prevent dangerous and costly comorbidities. It goes further than does the American Diabetes Association’s guidance on bariatric surgery, which cautions that type 2 diabetes patients with a BMI between 30 and 35 should only undergo surgery in the context of a clinical research study.
However, "bariatric procedures are not a public health solution for ‘diabesity,’ " cautioned Dr. Paul Zimmet, cochair of the IDF Task Force on Epidemiology and Prevention, and research is needed to continue to define the persons most likely to benefit. It will require very strict criteria for patient selection and the availability of the best circumstances – high-volume centers with competent surgeons, the best procedures, adequate follow-up, and proper evaluation of outcomes, Dr. Zimmet said in an interview.
Results from lifestyle and medical methods for weight loss are "modest and rarely sustained, particularly in the severely obese," the IDF statement noted. Furthermore, pervasive attitudes toward obesity – as a personal failure rather than a complex condition influenced by strong physical, emotional, and societal issues – effectively erect barriers to care and equal treatment at work, according to the statement.
The metabolic benefits of gastrointestinal surgery go beyond that achieved by weight loss alone. Normalization not only of hyperglycemia but also of hyperlipidemia, blood pressure, and obstructive sleep apnea has been shown consistently. And long-term follow-up has shown reductions in mortality from coronary artery disease, diabetes, and cancer. Therefore, surgical intervention should be a part of diabetes treatment algorithms (see table), according to the IDF statement. In fact, because early intervention increases the likelihood of remission, and residual hyperglycemia is easier to manage after surgery, intervention for type 2 diabetes patients "should be considered early as an option for eligible patients, rather than being held back as a last resort," the IDF recommended.
Obesity and diabetes have such powerful effects on health and longevity that their surging worldwide prevalence constitutes a major global health issue that "demands urgent attention from governments, health care systems, and the medical community," said the group.
The IDF noted that the complication risks of surgery have gone down considerably over time, especially since laparoscopic procedures have been used. But the long-term risks are numerous and vary by procedure, ranging from the need for revision to nutritional deficiencies. Lifelong monitoring is required, and national registries should be established and funded.
The surgeries are cost effective for diabetes, according to the statement. Studies in the United States, Australia, and the United Kingdom have shown that an intervention leads to the rare outcome of generating "both cost savings and health benefits over the lifetime of the cohort" and "provides the most compelling evidence for funding based on economic criteria."
The IDF task force did not recommend any one type of surgery. "There is a need for well-designed, randomized, controlled trials to compare both efficacy and cost [of bariatric surgeries]. Those data do not exist," said Dr. Zimmet, director emeritus of the Baker IDI Heart and Diabetes Institute, Melbourne. But in the United States, the only procedure with Food and Drug Administration approval for patients with a BMI of 30 is adjustable gastric banding.
"This is the first time the International Diabetes Federation or any major international organization has made recommendations on this rapidly developing area of therapy," Dr. Francesco Rubino, chief of the gastrointestinal metabolic surgery at New York–Presbyterian Hospital/Weill Cornell Medical Center, New York, said in a statement. "It did so because of the urgent need for worldwide expert guidance on the use of bariatric surgery because of the increasing usage."
The announcement was made from the World Congress on Interventional Therapies for Type 2 Diabetes, held in New York and directed by Dr. Rubino.
The consensus meeting was supported with an unrestricted educational grant by Allergan Inc., Ethicon, Ethicon Endo-Surgery Inc., and MetaCure Inc. These companies played no role in the discussion or preparation of the position paper, according to the task force statement. Members of the writing group had no disclosures.
Bariatric surgery should be considered as a treatment option for type 2 diabetes patients with body mass indexes between 30 and 35 kg/m2 and diabetes that can’t be controlled adequately by an optimal medical regimen – particularly in patients with other major cardiovascular disease risk factors, according to a statement from the International Diabetes Federation.
The position statement, "Bariatric Surgical and Procedural Interventions in the Treatment of Obese Patients with Type 2 Diabetes" is in response to the global epidemic of obesity-related diabetes and the failure of lifestyle and medical treatments to prevent dangerous and costly comorbidities. It goes further than does the American Diabetes Association’s guidance on bariatric surgery, which cautions that type 2 diabetes patients with a BMI between 30 and 35 should only undergo surgery in the context of a clinical research study.
However, "bariatric procedures are not a public health solution for ‘diabesity,’ " cautioned Dr. Paul Zimmet, cochair of the IDF Task Force on Epidemiology and Prevention, and research is needed to continue to define the persons most likely to benefit. It will require very strict criteria for patient selection and the availability of the best circumstances – high-volume centers with competent surgeons, the best procedures, adequate follow-up, and proper evaluation of outcomes, Dr. Zimmet said in an interview.
Results from lifestyle and medical methods for weight loss are "modest and rarely sustained, particularly in the severely obese," the IDF statement noted. Furthermore, pervasive attitudes toward obesity – as a personal failure rather than a complex condition influenced by strong physical, emotional, and societal issues – effectively erect barriers to care and equal treatment at work, according to the statement.
The metabolic benefits of gastrointestinal surgery go beyond that achieved by weight loss alone. Normalization not only of hyperglycemia but also of hyperlipidemia, blood pressure, and obstructive sleep apnea has been shown consistently. And long-term follow-up has shown reductions in mortality from coronary artery disease, diabetes, and cancer. Therefore, surgical intervention should be a part of diabetes treatment algorithms (see table), according to the IDF statement. In fact, because early intervention increases the likelihood of remission, and residual hyperglycemia is easier to manage after surgery, intervention for type 2 diabetes patients "should be considered early as an option for eligible patients, rather than being held back as a last resort," the IDF recommended.
Obesity and diabetes have such powerful effects on health and longevity that their surging worldwide prevalence constitutes a major global health issue that "demands urgent attention from governments, health care systems, and the medical community," said the group.
The IDF noted that the complication risks of surgery have gone down considerably over time, especially since laparoscopic procedures have been used. But the long-term risks are numerous and vary by procedure, ranging from the need for revision to nutritional deficiencies. Lifelong monitoring is required, and national registries should be established and funded.
The surgeries are cost effective for diabetes, according to the statement. Studies in the United States, Australia, and the United Kingdom have shown that an intervention leads to the rare outcome of generating "both cost savings and health benefits over the lifetime of the cohort" and "provides the most compelling evidence for funding based on economic criteria."
The IDF task force did not recommend any one type of surgery. "There is a need for well-designed, randomized, controlled trials to compare both efficacy and cost [of bariatric surgeries]. Those data do not exist," said Dr. Zimmet, director emeritus of the Baker IDI Heart and Diabetes Institute, Melbourne. But in the United States, the only procedure with Food and Drug Administration approval for patients with a BMI of 30 is adjustable gastric banding.
"This is the first time the International Diabetes Federation or any major international organization has made recommendations on this rapidly developing area of therapy," Dr. Francesco Rubino, chief of the gastrointestinal metabolic surgery at New York–Presbyterian Hospital/Weill Cornell Medical Center, New York, said in a statement. "It did so because of the urgent need for worldwide expert guidance on the use of bariatric surgery because of the increasing usage."
The announcement was made from the World Congress on Interventional Therapies for Type 2 Diabetes, held in New York and directed by Dr. Rubino.
The consensus meeting was supported with an unrestricted educational grant by Allergan Inc., Ethicon, Ethicon Endo-Surgery Inc., and MetaCure Inc. These companies played no role in the discussion or preparation of the position paper, according to the task force statement. Members of the writing group had no disclosures.
Bariatric surgery should be considered as a treatment option for type 2 diabetes patients with body mass indexes between 30 and 35 kg/m2 and diabetes that can’t be controlled adequately by an optimal medical regimen – particularly in patients with other major cardiovascular disease risk factors, according to a statement from the International Diabetes Federation.
The position statement, "Bariatric Surgical and Procedural Interventions in the Treatment of Obese Patients with Type 2 Diabetes" is in response to the global epidemic of obesity-related diabetes and the failure of lifestyle and medical treatments to prevent dangerous and costly comorbidities. It goes further than does the American Diabetes Association’s guidance on bariatric surgery, which cautions that type 2 diabetes patients with a BMI between 30 and 35 should only undergo surgery in the context of a clinical research study.
However, "bariatric procedures are not a public health solution for ‘diabesity,’ " cautioned Dr. Paul Zimmet, cochair of the IDF Task Force on Epidemiology and Prevention, and research is needed to continue to define the persons most likely to benefit. It will require very strict criteria for patient selection and the availability of the best circumstances – high-volume centers with competent surgeons, the best procedures, adequate follow-up, and proper evaluation of outcomes, Dr. Zimmet said in an interview.
Results from lifestyle and medical methods for weight loss are "modest and rarely sustained, particularly in the severely obese," the IDF statement noted. Furthermore, pervasive attitudes toward obesity – as a personal failure rather than a complex condition influenced by strong physical, emotional, and societal issues – effectively erect barriers to care and equal treatment at work, according to the statement.
The metabolic benefits of gastrointestinal surgery go beyond that achieved by weight loss alone. Normalization not only of hyperglycemia but also of hyperlipidemia, blood pressure, and obstructive sleep apnea has been shown consistently. And long-term follow-up has shown reductions in mortality from coronary artery disease, diabetes, and cancer. Therefore, surgical intervention should be a part of diabetes treatment algorithms (see table), according to the IDF statement. In fact, because early intervention increases the likelihood of remission, and residual hyperglycemia is easier to manage after surgery, intervention for type 2 diabetes patients "should be considered early as an option for eligible patients, rather than being held back as a last resort," the IDF recommended.
Obesity and diabetes have such powerful effects on health and longevity that their surging worldwide prevalence constitutes a major global health issue that "demands urgent attention from governments, health care systems, and the medical community," said the group.
The IDF noted that the complication risks of surgery have gone down considerably over time, especially since laparoscopic procedures have been used. But the long-term risks are numerous and vary by procedure, ranging from the need for revision to nutritional deficiencies. Lifelong monitoring is required, and national registries should be established and funded.
The surgeries are cost effective for diabetes, according to the statement. Studies in the United States, Australia, and the United Kingdom have shown that an intervention leads to the rare outcome of generating "both cost savings and health benefits over the lifetime of the cohort" and "provides the most compelling evidence for funding based on economic criteria."
The IDF task force did not recommend any one type of surgery. "There is a need for well-designed, randomized, controlled trials to compare both efficacy and cost [of bariatric surgeries]. Those data do not exist," said Dr. Zimmet, director emeritus of the Baker IDI Heart and Diabetes Institute, Melbourne. But in the United States, the only procedure with Food and Drug Administration approval for patients with a BMI of 30 is adjustable gastric banding.
"This is the first time the International Diabetes Federation or any major international organization has made recommendations on this rapidly developing area of therapy," Dr. Francesco Rubino, chief of the gastrointestinal metabolic surgery at New York–Presbyterian Hospital/Weill Cornell Medical Center, New York, said in a statement. "It did so because of the urgent need for worldwide expert guidance on the use of bariatric surgery because of the increasing usage."
The announcement was made from the World Congress on Interventional Therapies for Type 2 Diabetes, held in New York and directed by Dr. Rubino.
The consensus meeting was supported with an unrestricted educational grant by Allergan Inc., Ethicon, Ethicon Endo-Surgery Inc., and MetaCure Inc. These companies played no role in the discussion or preparation of the position paper, according to the task force statement. Members of the writing group had no disclosures.
FROM A STATEMENT BY THE INTERNATIONAL DIABETES FEDERATION
IDF Backs Bariatric Surgery for Type 2 Diabetes
Bariatric surgery should be considered as a treatment option for type 2 diabetes patients with body mass indexes between 30 and 35 kg/m2 and diabetes that can’t be controlled adequately by an optimal medical regimen – particularly in patients with other major cardiovascular disease risk factors, according to a statement from the International Diabetes Federation.
The position statement, "Bariatric Surgical and Procedural Interventions in the Treatment of Obese Patients with Type 2 Diabetes" is in response to the global epidemic of obesity-related diabetes and the failure of lifestyle and medical treatments to prevent dangerous and costly comorbidities. It goes further than does the American Diabetes Association’s guidance on bariatric surgery, which cautions that type 2 diabetes patients with a BMI between 30 and 35 should only undergo surgery in the context of a clinical research study.
However, "bariatric procedures are not a public health solution for ‘diabesity,’ " cautioned Dr. Paul Zimmet, cochair of the IDF Task Force on Epidemiology and Prevention, and research is needed to continue to define the persons most likely to benefit. It will require very strict criteria for patient selection and the availability of the best circumstances – high-volume centers with competent surgeons, the best procedures, adequate follow-up, and proper evaluation of outcomes, Dr. Zimmet said in an interview.
Results from lifestyle and medical methods for weight loss are "modest and rarely sustained, particularly in the severely obese," the IDF statement noted. Furthermore, pervasive attitudes toward obesity – as a personal failure rather than a complex condition influenced by strong physical, emotional, and societal issues – effectively erect barriers to care and equal treatment at work, according to the statement.
The metabolic benefits of gastrointestinal surgery go beyond that achieved by weight loss alone. Normalization not only of hyperglycemia but also of hyperlipidemia, blood pressure, and obstructive sleep apnea has been shown consistently. And long-term follow-up has shown reductions in mortality from coronary artery disease, diabetes, and cancer. Therefore, surgical intervention should be a part of diabetes treatment algorithms (see table), according to the IDF statement. In fact, because early intervention increases the likelihood of remission, and residual hyperglycemia is easier to manage after surgery, intervention for type 2 diabetes patients "should be considered early as an option for eligible patients, rather than being held back as a last resort," the IDF recommended.
Obesity and diabetes have such powerful effects on health and longevity that their surging worldwide prevalence constitutes a major global health issue that "demands urgent attention from governments, health care systems, and the medical community," said the group.
The IDF noted that the complication risks of surgery have gone down considerably over time, especially since laparoscopic procedures have been used. But the long-term risks are numerous and vary by procedure, ranging from the need for revision to nutritional deficiencies. Lifelong monitoring is required, and national registries should be established and funded.
The surgeries are cost effective for diabetes, according to the statement. Studies in the United States, Australia, and the United Kingdom have shown that an intervention leads to the rare outcome of generating "both cost savings and health benefits over the lifetime of the cohort" and "provides the most compelling evidence for funding based on economic criteria."
The IDF task force did not recommend any one type of surgery. "There is a need for well-designed, randomized, controlled trials to compare both efficacy and cost [of bariatric surgeries]. Those data do not exist," said Dr. Zimmet, director emeritus of the Baker IDI Heart and Diabetes Institute, Melbourne. But in the United States, the only procedure with Food and Drug Administration approval for patients with a BMI of 30 is adjustable gastric banding.
"This is the first time the International Diabetes Federation or any major international organization has made recommendations on this rapidly developing area of therapy," Dr. Francesco Rubino, chief of the gastrointestinal metabolic surgery at New York–Presbyterian Hospital/Weill Cornell Medical Center, New York, said in a statement. "It did so because of the urgent need for worldwide expert guidance on the use of bariatric surgery because of the increasing usage."
The announcement was made from the World Congress on Interventional Therapies for Type 2 Diabetes, held in New York and directed by Dr. Rubino.
The consensus meeting was supported with an unrestricted educational grant by Allergan Inc., Ethicon, Ethicon Endo-Surgery Inc., and MetaCure Inc. These companies played no role in the discussion or preparation of the position paper, according to the task force statement. Members of the writing group had no disclosures.
Bariatric surgery should be considered as a treatment option for type 2 diabetes patients with body mass indexes between 30 and 35 kg/m2 and diabetes that can’t be controlled adequately by an optimal medical regimen – particularly in patients with other major cardiovascular disease risk factors, according to a statement from the International Diabetes Federation.
The position statement, "Bariatric Surgical and Procedural Interventions in the Treatment of Obese Patients with Type 2 Diabetes" is in response to the global epidemic of obesity-related diabetes and the failure of lifestyle and medical treatments to prevent dangerous and costly comorbidities. It goes further than does the American Diabetes Association’s guidance on bariatric surgery, which cautions that type 2 diabetes patients with a BMI between 30 and 35 should only undergo surgery in the context of a clinical research study.
However, "bariatric procedures are not a public health solution for ‘diabesity,’ " cautioned Dr. Paul Zimmet, cochair of the IDF Task Force on Epidemiology and Prevention, and research is needed to continue to define the persons most likely to benefit. It will require very strict criteria for patient selection and the availability of the best circumstances – high-volume centers with competent surgeons, the best procedures, adequate follow-up, and proper evaluation of outcomes, Dr. Zimmet said in an interview.
Results from lifestyle and medical methods for weight loss are "modest and rarely sustained, particularly in the severely obese," the IDF statement noted. Furthermore, pervasive attitudes toward obesity – as a personal failure rather than a complex condition influenced by strong physical, emotional, and societal issues – effectively erect barriers to care and equal treatment at work, according to the statement.
The metabolic benefits of gastrointestinal surgery go beyond that achieved by weight loss alone. Normalization not only of hyperglycemia but also of hyperlipidemia, blood pressure, and obstructive sleep apnea has been shown consistently. And long-term follow-up has shown reductions in mortality from coronary artery disease, diabetes, and cancer. Therefore, surgical intervention should be a part of diabetes treatment algorithms (see table), according to the IDF statement. In fact, because early intervention increases the likelihood of remission, and residual hyperglycemia is easier to manage after surgery, intervention for type 2 diabetes patients "should be considered early as an option for eligible patients, rather than being held back as a last resort," the IDF recommended.
Obesity and diabetes have such powerful effects on health and longevity that their surging worldwide prevalence constitutes a major global health issue that "demands urgent attention from governments, health care systems, and the medical community," said the group.
The IDF noted that the complication risks of surgery have gone down considerably over time, especially since laparoscopic procedures have been used. But the long-term risks are numerous and vary by procedure, ranging from the need for revision to nutritional deficiencies. Lifelong monitoring is required, and national registries should be established and funded.
The surgeries are cost effective for diabetes, according to the statement. Studies in the United States, Australia, and the United Kingdom have shown that an intervention leads to the rare outcome of generating "both cost savings and health benefits over the lifetime of the cohort" and "provides the most compelling evidence for funding based on economic criteria."
The IDF task force did not recommend any one type of surgery. "There is a need for well-designed, randomized, controlled trials to compare both efficacy and cost [of bariatric surgeries]. Those data do not exist," said Dr. Zimmet, director emeritus of the Baker IDI Heart and Diabetes Institute, Melbourne. But in the United States, the only procedure with Food and Drug Administration approval for patients with a BMI of 30 is adjustable gastric banding.
"This is the first time the International Diabetes Federation or any major international organization has made recommendations on this rapidly developing area of therapy," Dr. Francesco Rubino, chief of the gastrointestinal metabolic surgery at New York–Presbyterian Hospital/Weill Cornell Medical Center, New York, said in a statement. "It did so because of the urgent need for worldwide expert guidance on the use of bariatric surgery because of the increasing usage."
The announcement was made from the World Congress on Interventional Therapies for Type 2 Diabetes, held in New York and directed by Dr. Rubino.
The consensus meeting was supported with an unrestricted educational grant by Allergan Inc., Ethicon, Ethicon Endo-Surgery Inc., and MetaCure Inc. These companies played no role in the discussion or preparation of the position paper, according to the task force statement. Members of the writing group had no disclosures.
Bariatric surgery should be considered as a treatment option for type 2 diabetes patients with body mass indexes between 30 and 35 kg/m2 and diabetes that can’t be controlled adequately by an optimal medical regimen – particularly in patients with other major cardiovascular disease risk factors, according to a statement from the International Diabetes Federation.
The position statement, "Bariatric Surgical and Procedural Interventions in the Treatment of Obese Patients with Type 2 Diabetes" is in response to the global epidemic of obesity-related diabetes and the failure of lifestyle and medical treatments to prevent dangerous and costly comorbidities. It goes further than does the American Diabetes Association’s guidance on bariatric surgery, which cautions that type 2 diabetes patients with a BMI between 30 and 35 should only undergo surgery in the context of a clinical research study.
However, "bariatric procedures are not a public health solution for ‘diabesity,’ " cautioned Dr. Paul Zimmet, cochair of the IDF Task Force on Epidemiology and Prevention, and research is needed to continue to define the persons most likely to benefit. It will require very strict criteria for patient selection and the availability of the best circumstances – high-volume centers with competent surgeons, the best procedures, adequate follow-up, and proper evaluation of outcomes, Dr. Zimmet said in an interview.
Results from lifestyle and medical methods for weight loss are "modest and rarely sustained, particularly in the severely obese," the IDF statement noted. Furthermore, pervasive attitudes toward obesity – as a personal failure rather than a complex condition influenced by strong physical, emotional, and societal issues – effectively erect barriers to care and equal treatment at work, according to the statement.
The metabolic benefits of gastrointestinal surgery go beyond that achieved by weight loss alone. Normalization not only of hyperglycemia but also of hyperlipidemia, blood pressure, and obstructive sleep apnea has been shown consistently. And long-term follow-up has shown reductions in mortality from coronary artery disease, diabetes, and cancer. Therefore, surgical intervention should be a part of diabetes treatment algorithms (see table), according to the IDF statement. In fact, because early intervention increases the likelihood of remission, and residual hyperglycemia is easier to manage after surgery, intervention for type 2 diabetes patients "should be considered early as an option for eligible patients, rather than being held back as a last resort," the IDF recommended.
Obesity and diabetes have such powerful effects on health and longevity that their surging worldwide prevalence constitutes a major global health issue that "demands urgent attention from governments, health care systems, and the medical community," said the group.
The IDF noted that the complication risks of surgery have gone down considerably over time, especially since laparoscopic procedures have been used. But the long-term risks are numerous and vary by procedure, ranging from the need for revision to nutritional deficiencies. Lifelong monitoring is required, and national registries should be established and funded.
The surgeries are cost effective for diabetes, according to the statement. Studies in the United States, Australia, and the United Kingdom have shown that an intervention leads to the rare outcome of generating "both cost savings and health benefits over the lifetime of the cohort" and "provides the most compelling evidence for funding based on economic criteria."
The IDF task force did not recommend any one type of surgery. "There is a need for well-designed, randomized, controlled trials to compare both efficacy and cost [of bariatric surgeries]. Those data do not exist," said Dr. Zimmet, director emeritus of the Baker IDI Heart and Diabetes Institute, Melbourne. But in the United States, the only procedure with Food and Drug Administration approval for patients with a BMI of 30 is adjustable gastric banding.
"This is the first time the International Diabetes Federation or any major international organization has made recommendations on this rapidly developing area of therapy," Dr. Francesco Rubino, chief of the gastrointestinal metabolic surgery at New York–Presbyterian Hospital/Weill Cornell Medical Center, New York, said in a statement. "It did so because of the urgent need for worldwide expert guidance on the use of bariatric surgery because of the increasing usage."
The announcement was made from the World Congress on Interventional Therapies for Type 2 Diabetes, held in New York and directed by Dr. Rubino.
The consensus meeting was supported with an unrestricted educational grant by Allergan Inc., Ethicon, Ethicon Endo-Surgery Inc., and MetaCure Inc. These companies played no role in the discussion or preparation of the position paper, according to the task force statement. Members of the writing group had no disclosures.
FROM A STATEMENT BY THE INTERNATIONAL DIABETES FEDERATION
Scoring System Predicts Ability Of Orthotics to Ease Knee Pain
The success of orthotic devices for patellofemoral pain can be predicted by a patient's age, height, midfoot morphometry, and pain severity, according to a small, single-center Australian study.
The use of these predictor variables can help practitioners make better informed treatment decisions, wrote Bill Vicenzino, Ph.D., in an article published online (Br. J. Sports Med. 2008 [doi:10.1136/bjsm.2008.052613]).
The researchers performed a post hoc analysis of a randomized, single-blind clinical trial in 42 patients aged 18-40 years with patellofemoral pain (PFP) of nontraumatic origin who were given one of several treatments, including flat inserts, physical therapy, and foot orthoses. The latter consisted of four pairs of prefabricated ethylene-vinyl acetate foot orthoses with a 6-degree varus wedge and built-in arch support.
Patients given foot orthoses were followed for 12 weeks. During the first 6 weeks, patients attended six 30-minute physical therapy sessions in which they rated the comfort of the orthoses on a visual analog scale, with 0 mm indicating they were too uncomfortable to wear and 100 mm indicating no discomfort.
The severity of the worst and usual patellofemoral pain experienced during the previous week also was measured on a visual analog scale, with 0 mm representing no pain and 100 mm as the worst pain imaginable.
The orthoses were then modified, and patients were encouraged to wear them throughout the study, wrote Dr. Vicenzino, head of the division of physiotherapy at the School of Health and Rehabilitation Sciences, University of Queensland, Brisbane (Australia), and colleagues.
The outcome measure was the perceived effect of the orthoses as measured on a 5-point Likert scale, with options ranging from marked improvement to marked worsening. Only those who scored “marked improvement” were considered to have a successful outcome.
For the analysis of predictor variables, morphometric foot measurements and demographic data were recorded for the 42 participants at baseline and at the first intervention appointment. Morphometric characteristics included weight-bearing (taken when equal weight is on each foot) and non-weight-bearing measures of the midfoot; weight-bearing arch height; and midfoot width difference (the change in midfoot width from a non-weight-bearing to a weight-bearing position). Demographic data included age, sex, height, weight, and body mass index.
At 12 weeks, 17 (40%) of the patients had successful outcomes, on the basis of the Likert scale. Analysis showed that four of the predictor variables—age over 25 years, height less than 165 cm, worst pain less than 53 mm, and midfoot width difference greater than 11 mm—were significantly associated with a successful outcome. Compared with the pretest probability of success in all 42 patients of 40%, patients who had three of the four predictors had a post-test probability of success of 85%. For patients with two of the identified predictors, that probability was 61%, and for patients with one variable, it was 53%. No patients had all four predictors.
The study was funded primarily by the National Health and Medical Research Council of Australia.
The success of orthotic devices for patellofemoral pain can be predicted by a patient's age, height, midfoot morphometry, and pain severity, according to a small, single-center Australian study.
The use of these predictor variables can help practitioners make better informed treatment decisions, wrote Bill Vicenzino, Ph.D., in an article published online (Br. J. Sports Med. 2008 [doi:10.1136/bjsm.2008.052613]).
The researchers performed a post hoc analysis of a randomized, single-blind clinical trial in 42 patients aged 18-40 years with patellofemoral pain (PFP) of nontraumatic origin who were given one of several treatments, including flat inserts, physical therapy, and foot orthoses. The latter consisted of four pairs of prefabricated ethylene-vinyl acetate foot orthoses with a 6-degree varus wedge and built-in arch support.
Patients given foot orthoses were followed for 12 weeks. During the first 6 weeks, patients attended six 30-minute physical therapy sessions in which they rated the comfort of the orthoses on a visual analog scale, with 0 mm indicating they were too uncomfortable to wear and 100 mm indicating no discomfort.
The severity of the worst and usual patellofemoral pain experienced during the previous week also was measured on a visual analog scale, with 0 mm representing no pain and 100 mm as the worst pain imaginable.
The orthoses were then modified, and patients were encouraged to wear them throughout the study, wrote Dr. Vicenzino, head of the division of physiotherapy at the School of Health and Rehabilitation Sciences, University of Queensland, Brisbane (Australia), and colleagues.
The outcome measure was the perceived effect of the orthoses as measured on a 5-point Likert scale, with options ranging from marked improvement to marked worsening. Only those who scored “marked improvement” were considered to have a successful outcome.
For the analysis of predictor variables, morphometric foot measurements and demographic data were recorded for the 42 participants at baseline and at the first intervention appointment. Morphometric characteristics included weight-bearing (taken when equal weight is on each foot) and non-weight-bearing measures of the midfoot; weight-bearing arch height; and midfoot width difference (the change in midfoot width from a non-weight-bearing to a weight-bearing position). Demographic data included age, sex, height, weight, and body mass index.
At 12 weeks, 17 (40%) of the patients had successful outcomes, on the basis of the Likert scale. Analysis showed that four of the predictor variables—age over 25 years, height less than 165 cm, worst pain less than 53 mm, and midfoot width difference greater than 11 mm—were significantly associated with a successful outcome. Compared with the pretest probability of success in all 42 patients of 40%, patients who had three of the four predictors had a post-test probability of success of 85%. For patients with two of the identified predictors, that probability was 61%, and for patients with one variable, it was 53%. No patients had all four predictors.
The study was funded primarily by the National Health and Medical Research Council of Australia.
The success of orthotic devices for patellofemoral pain can be predicted by a patient's age, height, midfoot morphometry, and pain severity, according to a small, single-center Australian study.
The use of these predictor variables can help practitioners make better informed treatment decisions, wrote Bill Vicenzino, Ph.D., in an article published online (Br. J. Sports Med. 2008 [doi:10.1136/bjsm.2008.052613]).
The researchers performed a post hoc analysis of a randomized, single-blind clinical trial in 42 patients aged 18-40 years with patellofemoral pain (PFP) of nontraumatic origin who were given one of several treatments, including flat inserts, physical therapy, and foot orthoses. The latter consisted of four pairs of prefabricated ethylene-vinyl acetate foot orthoses with a 6-degree varus wedge and built-in arch support.
Patients given foot orthoses were followed for 12 weeks. During the first 6 weeks, patients attended six 30-minute physical therapy sessions in which they rated the comfort of the orthoses on a visual analog scale, with 0 mm indicating they were too uncomfortable to wear and 100 mm indicating no discomfort.
The severity of the worst and usual patellofemoral pain experienced during the previous week also was measured on a visual analog scale, with 0 mm representing no pain and 100 mm as the worst pain imaginable.
The orthoses were then modified, and patients were encouraged to wear them throughout the study, wrote Dr. Vicenzino, head of the division of physiotherapy at the School of Health and Rehabilitation Sciences, University of Queensland, Brisbane (Australia), and colleagues.
The outcome measure was the perceived effect of the orthoses as measured on a 5-point Likert scale, with options ranging from marked improvement to marked worsening. Only those who scored “marked improvement” were considered to have a successful outcome.
For the analysis of predictor variables, morphometric foot measurements and demographic data were recorded for the 42 participants at baseline and at the first intervention appointment. Morphometric characteristics included weight-bearing (taken when equal weight is on each foot) and non-weight-bearing measures of the midfoot; weight-bearing arch height; and midfoot width difference (the change in midfoot width from a non-weight-bearing to a weight-bearing position). Demographic data included age, sex, height, weight, and body mass index.
At 12 weeks, 17 (40%) of the patients had successful outcomes, on the basis of the Likert scale. Analysis showed that four of the predictor variables—age over 25 years, height less than 165 cm, worst pain less than 53 mm, and midfoot width difference greater than 11 mm—were significantly associated with a successful outcome. Compared with the pretest probability of success in all 42 patients of 40%, patients who had three of the four predictors had a post-test probability of success of 85%. For patients with two of the identified predictors, that probability was 61%, and for patients with one variable, it was 53%. No patients had all four predictors.
The study was funded primarily by the National Health and Medical Research Council of Australia.
Etoricoxib, Diclofenac Pose Similar Cardiovascular Risks
CHICAGO — Prolonged treatment with the COX-2 inhibitor etoricoxib carried no increased cardiovascular risk, compared with the traditional NSAID diclofenac in a pooled analysis of nearly 35,000 arthritis patients, reported Dr. Christopher Cannon at the annual scientific sessions of the American Heart Association.
For arthritis patients “who need to take one of these types of agents long term, either one will have the same risk profile for thrombotic events such as heart attack or stroke,” he said at a press conference.
The Multinational Etoricoxib and Diclofenac Arthritis Long-Term (MEDAL) program is a prespecified pooled analysis of three studies. The largest was MEDAL, performed in 23,504 patients during June 2002-May 2006 at 1,380 sites in 46 countries. This study randomized rheumatoid arthritis (RA) patients to treatment with 90 mg etoricoxib once a day or 75 mg diclofenac twice a day. Osteoarthritis (OA) patients were randomized to receive either 75 mg diclofenac twice daily or one of two dosages of etoricoxib, 90 mg or 60 mg.
The other two studies in the analysis were the Etoricoxib vs. Diclofenac Sodium Gastrointestinal Tolerability and Effectiveness (EDGE) trial, in which 7,111 patients received 90 mg etoricoxib once daily or 50 mg diclofenac three times daily, and EDGE II, in which 4,086 patients were treated with 90 mg etoricoxib once daily or 75 mg diclofenac twice daily.
In all three studies, patients were followed out to 3 years, with an average follow-up of 18 months. Patients had a broad range of cardiovascular risk. Use of aspirin and proton pump inhibitors was allowed in appropriate patients.
In the pooled analysis of the three studies, the primary end point was the first occurrence of any fatal or nonfatal venous or arterial thrombotic event, including MI, unstable angina, intracardiac thrombus, thrombotic stroke, and transient ischemic attack. The rates were 1.24 events/100 patient-years in the etoricoxib group and 1.30 events/100 person-years in the diclofenac group, a nonsignificant difference, reported Dr. Cannon, a cardiologist at Brigham and Women's Hospital, Boston.
Secondary end points were a subset of arterial thrombotic events only and the Antiplatelet Trialists' Collaboration (APTC) end point of MI, stroke, and vascular death. There were no significant differences in these end points.
The MEDAL program provides “more information that is very valuable, but it doesn't clarify the entire issue” of the thrombotic safety of COX-2 selective and nonselective NSAIDs, Dr. Roy Altman, professor of medicine at the University of California, Los Angeles, said in an interview.
The MEDAL program was the largest-ever trial in arthritis patients, and the first to demonstrate a significant reduction of GI events with a cyclooxygenase-2 (COX-2) inhibitor, compared with traditional NSAIDs. Rates of upper GI events clinical events were lower with etoricoxib than with diclofenac (0.67 and 0.97/100 patient-years, respectively). But there was no difference between groups in complicated upper GI events, such as perforated ulcers.
The nonsignificant difference in complicated upper GI events “is probably the most bothersome thing about the study,” because etoricoxib is supposed to be GI-protective and has even more COX-2 selectivity than some other COX-2 selective NSAIDs, such as rofecoxib, Dr. Altman said.
Whether these results can be applied to other traditional NSAIDs is questionable, however, because observational studies have shown diclofenac to have the highest relative risk for myocardial infarction, Dr. Luis Alberto Garcia Rodriguez and Dr. Paola Patrignani of the Spanish Centre for Pharmacoepidemiologic Research, Madrid, wrote in an editorial accompanying the published report (Lancet 2006; DOI:10.1016/S0140–6736[06] 69667–0). “The similar risk of thrombotic events between etoricoxib and diclofenac can be explained by the profound inhibition of COX-2 shared by the two agents.”
“The hypothesis that diclofenac is partially COX-2 selective I think is not supported” because only one article has ever said that diclofenac has some COX-2 selectivity, Dr. Altman said (N. Engl. J. Med. 2001;345:433–42).
But naproxen “clearly is the one that would have been more helpful to compare” with etoricoxib, he said, because naproxen was compared against rofecoxib in Merck's VIGOR (Vioxx Gastrointestinal Outcomes Research) trial and naproxen is more widely used (over-the-counter and prescription) in the United States than diclofenac.
Dr. Cannon told reporters that although observational studies have shown differences among COX-2 inhibitors in cardiovascular risks, randomized trial data have shown no such difference, with the exception of naproxen, which carries a lesser risk that may be explained by an antiplatelet effect at high doses.
“Our results today address one question: In these patients with arthritis, a selective agent didn't increase risk compared with other agents,” said Dr. Cannon. The message to clinicians and patients is that there are options to treat arthritis. “We are moving to an era where we do have choices, and we should be choosing different treatments for different patients.”
Dr. Cannon receives research grant support from Merck, which sponsored and monitored the study, and did the statistical analysis. The results were published simultaneously with the presentation in the Lancet 2006;(DOI:10.1016/S0140–6736 [06]69666–9).
Etoricoxib is approved for use in more than 60 countries but not yet in the United States.
Several days before the presentation, Merck resubmitted its new drug application to the FDA for the approval of etoricoxib for the symptomatic treatment of only osteoarthritis, instead of indications also in rheumatoid arthritis and other conditions. In the MEDAL program, RA and OA patients had similar risk for cardiovascular thrombotic events with both drugs, but only 28% of the patients had RA. RA patients also usually require higher doses of NSAIDs, which would emphasize any cardiovascular thrombotic risk. These considerations may have had led Merck to not seek etoricoxib as an indication for RA, Dr. Altman suggested.
Senior writer Jeff Evans contributed to this report.
CHICAGO — Prolonged treatment with the COX-2 inhibitor etoricoxib carried no increased cardiovascular risk, compared with the traditional NSAID diclofenac in a pooled analysis of nearly 35,000 arthritis patients, reported Dr. Christopher Cannon at the annual scientific sessions of the American Heart Association.
For arthritis patients “who need to take one of these types of agents long term, either one will have the same risk profile for thrombotic events such as heart attack or stroke,” he said at a press conference.
The Multinational Etoricoxib and Diclofenac Arthritis Long-Term (MEDAL) program is a prespecified pooled analysis of three studies. The largest was MEDAL, performed in 23,504 patients during June 2002-May 2006 at 1,380 sites in 46 countries. This study randomized rheumatoid arthritis (RA) patients to treatment with 90 mg etoricoxib once a day or 75 mg diclofenac twice a day. Osteoarthritis (OA) patients were randomized to receive either 75 mg diclofenac twice daily or one of two dosages of etoricoxib, 90 mg or 60 mg.
The other two studies in the analysis were the Etoricoxib vs. Diclofenac Sodium Gastrointestinal Tolerability and Effectiveness (EDGE) trial, in which 7,111 patients received 90 mg etoricoxib once daily or 50 mg diclofenac three times daily, and EDGE II, in which 4,086 patients were treated with 90 mg etoricoxib once daily or 75 mg diclofenac twice daily.
In all three studies, patients were followed out to 3 years, with an average follow-up of 18 months. Patients had a broad range of cardiovascular risk. Use of aspirin and proton pump inhibitors was allowed in appropriate patients.
In the pooled analysis of the three studies, the primary end point was the first occurrence of any fatal or nonfatal venous or arterial thrombotic event, including MI, unstable angina, intracardiac thrombus, thrombotic stroke, and transient ischemic attack. The rates were 1.24 events/100 patient-years in the etoricoxib group and 1.30 events/100 person-years in the diclofenac group, a nonsignificant difference, reported Dr. Cannon, a cardiologist at Brigham and Women's Hospital, Boston.
Secondary end points were a subset of arterial thrombotic events only and the Antiplatelet Trialists' Collaboration (APTC) end point of MI, stroke, and vascular death. There were no significant differences in these end points.
The MEDAL program provides “more information that is very valuable, but it doesn't clarify the entire issue” of the thrombotic safety of COX-2 selective and nonselective NSAIDs, Dr. Roy Altman, professor of medicine at the University of California, Los Angeles, said in an interview.
The MEDAL program was the largest-ever trial in arthritis patients, and the first to demonstrate a significant reduction of GI events with a cyclooxygenase-2 (COX-2) inhibitor, compared with traditional NSAIDs. Rates of upper GI events clinical events were lower with etoricoxib than with diclofenac (0.67 and 0.97/100 patient-years, respectively). But there was no difference between groups in complicated upper GI events, such as perforated ulcers.
The nonsignificant difference in complicated upper GI events “is probably the most bothersome thing about the study,” because etoricoxib is supposed to be GI-protective and has even more COX-2 selectivity than some other COX-2 selective NSAIDs, such as rofecoxib, Dr. Altman said.
Whether these results can be applied to other traditional NSAIDs is questionable, however, because observational studies have shown diclofenac to have the highest relative risk for myocardial infarction, Dr. Luis Alberto Garcia Rodriguez and Dr. Paola Patrignani of the Spanish Centre for Pharmacoepidemiologic Research, Madrid, wrote in an editorial accompanying the published report (Lancet 2006; DOI:10.1016/S0140–6736[06] 69667–0). “The similar risk of thrombotic events between etoricoxib and diclofenac can be explained by the profound inhibition of COX-2 shared by the two agents.”
“The hypothesis that diclofenac is partially COX-2 selective I think is not supported” because only one article has ever said that diclofenac has some COX-2 selectivity, Dr. Altman said (N. Engl. J. Med. 2001;345:433–42).
But naproxen “clearly is the one that would have been more helpful to compare” with etoricoxib, he said, because naproxen was compared against rofecoxib in Merck's VIGOR (Vioxx Gastrointestinal Outcomes Research) trial and naproxen is more widely used (over-the-counter and prescription) in the United States than diclofenac.
Dr. Cannon told reporters that although observational studies have shown differences among COX-2 inhibitors in cardiovascular risks, randomized trial data have shown no such difference, with the exception of naproxen, which carries a lesser risk that may be explained by an antiplatelet effect at high doses.
“Our results today address one question: In these patients with arthritis, a selective agent didn't increase risk compared with other agents,” said Dr. Cannon. The message to clinicians and patients is that there are options to treat arthritis. “We are moving to an era where we do have choices, and we should be choosing different treatments for different patients.”
Dr. Cannon receives research grant support from Merck, which sponsored and monitored the study, and did the statistical analysis. The results were published simultaneously with the presentation in the Lancet 2006;(DOI:10.1016/S0140–6736 [06]69666–9).
Etoricoxib is approved for use in more than 60 countries but not yet in the United States.
Several days before the presentation, Merck resubmitted its new drug application to the FDA for the approval of etoricoxib for the symptomatic treatment of only osteoarthritis, instead of indications also in rheumatoid arthritis and other conditions. In the MEDAL program, RA and OA patients had similar risk for cardiovascular thrombotic events with both drugs, but only 28% of the patients had RA. RA patients also usually require higher doses of NSAIDs, which would emphasize any cardiovascular thrombotic risk. These considerations may have had led Merck to not seek etoricoxib as an indication for RA, Dr. Altman suggested.
Senior writer Jeff Evans contributed to this report.
CHICAGO — Prolonged treatment with the COX-2 inhibitor etoricoxib carried no increased cardiovascular risk, compared with the traditional NSAID diclofenac in a pooled analysis of nearly 35,000 arthritis patients, reported Dr. Christopher Cannon at the annual scientific sessions of the American Heart Association.
For arthritis patients “who need to take one of these types of agents long term, either one will have the same risk profile for thrombotic events such as heart attack or stroke,” he said at a press conference.
The Multinational Etoricoxib and Diclofenac Arthritis Long-Term (MEDAL) program is a prespecified pooled analysis of three studies. The largest was MEDAL, performed in 23,504 patients during June 2002-May 2006 at 1,380 sites in 46 countries. This study randomized rheumatoid arthritis (RA) patients to treatment with 90 mg etoricoxib once a day or 75 mg diclofenac twice a day. Osteoarthritis (OA) patients were randomized to receive either 75 mg diclofenac twice daily or one of two dosages of etoricoxib, 90 mg or 60 mg.
The other two studies in the analysis were the Etoricoxib vs. Diclofenac Sodium Gastrointestinal Tolerability and Effectiveness (EDGE) trial, in which 7,111 patients received 90 mg etoricoxib once daily or 50 mg diclofenac three times daily, and EDGE II, in which 4,086 patients were treated with 90 mg etoricoxib once daily or 75 mg diclofenac twice daily.
In all three studies, patients were followed out to 3 years, with an average follow-up of 18 months. Patients had a broad range of cardiovascular risk. Use of aspirin and proton pump inhibitors was allowed in appropriate patients.
In the pooled analysis of the three studies, the primary end point was the first occurrence of any fatal or nonfatal venous or arterial thrombotic event, including MI, unstable angina, intracardiac thrombus, thrombotic stroke, and transient ischemic attack. The rates were 1.24 events/100 patient-years in the etoricoxib group and 1.30 events/100 person-years in the diclofenac group, a nonsignificant difference, reported Dr. Cannon, a cardiologist at Brigham and Women's Hospital, Boston.
Secondary end points were a subset of arterial thrombotic events only and the Antiplatelet Trialists' Collaboration (APTC) end point of MI, stroke, and vascular death. There were no significant differences in these end points.
The MEDAL program provides “more information that is very valuable, but it doesn't clarify the entire issue” of the thrombotic safety of COX-2 selective and nonselective NSAIDs, Dr. Roy Altman, professor of medicine at the University of California, Los Angeles, said in an interview.
The MEDAL program was the largest-ever trial in arthritis patients, and the first to demonstrate a significant reduction of GI events with a cyclooxygenase-2 (COX-2) inhibitor, compared with traditional NSAIDs. Rates of upper GI events clinical events were lower with etoricoxib than with diclofenac (0.67 and 0.97/100 patient-years, respectively). But there was no difference between groups in complicated upper GI events, such as perforated ulcers.
The nonsignificant difference in complicated upper GI events “is probably the most bothersome thing about the study,” because etoricoxib is supposed to be GI-protective and has even more COX-2 selectivity than some other COX-2 selective NSAIDs, such as rofecoxib, Dr. Altman said.
Whether these results can be applied to other traditional NSAIDs is questionable, however, because observational studies have shown diclofenac to have the highest relative risk for myocardial infarction, Dr. Luis Alberto Garcia Rodriguez and Dr. Paola Patrignani of the Spanish Centre for Pharmacoepidemiologic Research, Madrid, wrote in an editorial accompanying the published report (Lancet 2006; DOI:10.1016/S0140–6736[06] 69667–0). “The similar risk of thrombotic events between etoricoxib and diclofenac can be explained by the profound inhibition of COX-2 shared by the two agents.”
“The hypothesis that diclofenac is partially COX-2 selective I think is not supported” because only one article has ever said that diclofenac has some COX-2 selectivity, Dr. Altman said (N. Engl. J. Med. 2001;345:433–42).
But naproxen “clearly is the one that would have been more helpful to compare” with etoricoxib, he said, because naproxen was compared against rofecoxib in Merck's VIGOR (Vioxx Gastrointestinal Outcomes Research) trial and naproxen is more widely used (over-the-counter and prescription) in the United States than diclofenac.
Dr. Cannon told reporters that although observational studies have shown differences among COX-2 inhibitors in cardiovascular risks, randomized trial data have shown no such difference, with the exception of naproxen, which carries a lesser risk that may be explained by an antiplatelet effect at high doses.
“Our results today address one question: In these patients with arthritis, a selective agent didn't increase risk compared with other agents,” said Dr. Cannon. The message to clinicians and patients is that there are options to treat arthritis. “We are moving to an era where we do have choices, and we should be choosing different treatments for different patients.”
Dr. Cannon receives research grant support from Merck, which sponsored and monitored the study, and did the statistical analysis. The results were published simultaneously with the presentation in the Lancet 2006;(DOI:10.1016/S0140–6736 [06]69666–9).
Etoricoxib is approved for use in more than 60 countries but not yet in the United States.
Several days before the presentation, Merck resubmitted its new drug application to the FDA for the approval of etoricoxib for the symptomatic treatment of only osteoarthritis, instead of indications also in rheumatoid arthritis and other conditions. In the MEDAL program, RA and OA patients had similar risk for cardiovascular thrombotic events with both drugs, but only 28% of the patients had RA. RA patients also usually require higher doses of NSAIDs, which would emphasize any cardiovascular thrombotic risk. These considerations may have had led Merck to not seek etoricoxib as an indication for RA, Dr. Altman suggested.
Senior writer Jeff Evans contributed to this report.
Pioglitazone Stalled Thickening of The Carotid in Type 2 Patients
CHICAGO — Treatment with pioglitazone for 18 months halted progression of atherosclerosis in patients with early type 2 diabetes, Dr. Theodore Mazzone reported at the annual scientific sessions of the American Heart Association.
Carotid intima media thickness (CIMT), which continued to progress in patients treated with glimepiride, was “virtually arrested” in the pioglitazone group in the Carotid Intima-Media Thickness in Atherosclerosis Using Pioglitazone (CHICAGO) trial. The beneficial effect improved during the mean 18 months of treatment, said Dr. Mazzone of the endocrinology, diabetes, and metabolism section of the University of Illinois, Chicago.
CIMT was used as a surrogate for risk of stroke and MI in the diabetic patients. “The thicker the intima, the higher the risk of heart attack or stroke in 5–10 years,” Dr. Mazzone said in a press briefing. The CHICAGO trial was conducted from October 2003 to May 2006 in a multiracial, multiethnic population of patients at 28 clinical sites in Chicago. The 462 patients, aged 45–85 years, were newly diagnosed with type 2 diabetes that was controlled by diet or treated with sulfonureas, metformin, or insulin. Patients taking medicine for blood glucose control were eligible if their glycosylated hemoglobin A1c (HbA1c) values were at least 6.5% but less than 9%.
Exclusion criteria included symptomatic coronary artery disease, cerebrovascular disease, New York Heart Association class III or IV heart failure, and current use of ACE inhibitors or diuretics. “We wanted patients early in the disease process,” Dr. Mazzone said.
CIMT was measured using high-resolution, B mode carotid artery ultrasound. All images were taken by the same ultrasonographer at the same location.
The primary end point was the change in mean CIMT from baseline at 72 weeks. The CIMT reduction in the pioglitazone group was 0.001 mm, compared with an increase of 0.012 mm in the glimepiride group. This beneficial effect was present regardless of age, sex, presence of hypertension, duration of type 2 diabetes, body mass index, HbA1c value, and statin use, said Dr. Mazzone, who is a consultant for and has received speaking honoraria from Takeda Pharmaceuticals North America Inc., maker of pioglitazone (Actos).
Diabetes was well controlled in the study population. The mean HbA1c value of the pioglitazone group at baseline was 7.44%, and that of the glimepiride group was 7.36%. The glycemic effects of the two drugs differed over time in the study. With glimepiride, mean HbA1c values dropped rapidly in the beginning of the trial, but rose gradually back to nearly their original level by week 72. In pioglitazone-treated patients, HbA1c values decreased gradually over 48 weeks and remained steady until 72 weeks. At the final visit, the mean HbA1c level in the pioglitazone group was 0.32% lower than that of the glimepiride group, a highly significant difference, Dr. Mazzone said.
Lipid levels were also well controlled in the CHICAGO participants, with about 70% of the patients in each group taking lipid-lowering drugs. With pioglitazone, HDL cholesterol and triglyceride levels improved significantly. HDL levels were similar between groups at baseline, at 47.6 mg/dL in the glimepiride group and 47.1 mg/dL in the pioglitazone group. By the final visit, the HDL level was 6.5% higher in the pioglitazone group than in the glimepiride group. Triglyceride levels decreased by 13.5% in the pioglitazone patients and rose by 2.1% with glimepiride.
The beneficial metabolic effects of pioglitazone would be expected on the basis of previous trials of thiazolidinediones, said discussant Dr. Peter Wilson, an endocrinologist at Emory University, Atlanta. But the effects of pioglitazone in CHICAGO may not be generalizable to other thiazolidinediones, he noted, because pioglitazone may be stronger than other drugs in the class.
Adverse effects of treatment with pioglitazone were similar to those with the sulfonylurea glimepiride, although treatment-limiting peripheral edema occurred in four pioglitazone patients and none of the glimepiride patients. Weight gain also was more frequent with pioglitazone. These effects have been seen in other randomized trials of thiazolidinediones, and raise concerns about an increased risk of heart failure with pioglitazone. But Dr. Wilson noted that because of its preselection of patients who were not likely to get into heart failure concerns, CHIGAGO “opens the window a little wider for when we can use these agents.” The results were published online simultaneously with the presentation (JAMA 2006;296:2572–81).
CHICAGO — Treatment with pioglitazone for 18 months halted progression of atherosclerosis in patients with early type 2 diabetes, Dr. Theodore Mazzone reported at the annual scientific sessions of the American Heart Association.
Carotid intima media thickness (CIMT), which continued to progress in patients treated with glimepiride, was “virtually arrested” in the pioglitazone group in the Carotid Intima-Media Thickness in Atherosclerosis Using Pioglitazone (CHICAGO) trial. The beneficial effect improved during the mean 18 months of treatment, said Dr. Mazzone of the endocrinology, diabetes, and metabolism section of the University of Illinois, Chicago.
CIMT was used as a surrogate for risk of stroke and MI in the diabetic patients. “The thicker the intima, the higher the risk of heart attack or stroke in 5–10 years,” Dr. Mazzone said in a press briefing. The CHICAGO trial was conducted from October 2003 to May 2006 in a multiracial, multiethnic population of patients at 28 clinical sites in Chicago. The 462 patients, aged 45–85 years, were newly diagnosed with type 2 diabetes that was controlled by diet or treated with sulfonureas, metformin, or insulin. Patients taking medicine for blood glucose control were eligible if their glycosylated hemoglobin A1c (HbA1c) values were at least 6.5% but less than 9%.
Exclusion criteria included symptomatic coronary artery disease, cerebrovascular disease, New York Heart Association class III or IV heart failure, and current use of ACE inhibitors or diuretics. “We wanted patients early in the disease process,” Dr. Mazzone said.
CIMT was measured using high-resolution, B mode carotid artery ultrasound. All images were taken by the same ultrasonographer at the same location.
The primary end point was the change in mean CIMT from baseline at 72 weeks. The CIMT reduction in the pioglitazone group was 0.001 mm, compared with an increase of 0.012 mm in the glimepiride group. This beneficial effect was present regardless of age, sex, presence of hypertension, duration of type 2 diabetes, body mass index, HbA1c value, and statin use, said Dr. Mazzone, who is a consultant for and has received speaking honoraria from Takeda Pharmaceuticals North America Inc., maker of pioglitazone (Actos).
Diabetes was well controlled in the study population. The mean HbA1c value of the pioglitazone group at baseline was 7.44%, and that of the glimepiride group was 7.36%. The glycemic effects of the two drugs differed over time in the study. With glimepiride, mean HbA1c values dropped rapidly in the beginning of the trial, but rose gradually back to nearly their original level by week 72. In pioglitazone-treated patients, HbA1c values decreased gradually over 48 weeks and remained steady until 72 weeks. At the final visit, the mean HbA1c level in the pioglitazone group was 0.32% lower than that of the glimepiride group, a highly significant difference, Dr. Mazzone said.
Lipid levels were also well controlled in the CHICAGO participants, with about 70% of the patients in each group taking lipid-lowering drugs. With pioglitazone, HDL cholesterol and triglyceride levels improved significantly. HDL levels were similar between groups at baseline, at 47.6 mg/dL in the glimepiride group and 47.1 mg/dL in the pioglitazone group. By the final visit, the HDL level was 6.5% higher in the pioglitazone group than in the glimepiride group. Triglyceride levels decreased by 13.5% in the pioglitazone patients and rose by 2.1% with glimepiride.
The beneficial metabolic effects of pioglitazone would be expected on the basis of previous trials of thiazolidinediones, said discussant Dr. Peter Wilson, an endocrinologist at Emory University, Atlanta. But the effects of pioglitazone in CHICAGO may not be generalizable to other thiazolidinediones, he noted, because pioglitazone may be stronger than other drugs in the class.
Adverse effects of treatment with pioglitazone were similar to those with the sulfonylurea glimepiride, although treatment-limiting peripheral edema occurred in four pioglitazone patients and none of the glimepiride patients. Weight gain also was more frequent with pioglitazone. These effects have been seen in other randomized trials of thiazolidinediones, and raise concerns about an increased risk of heart failure with pioglitazone. But Dr. Wilson noted that because of its preselection of patients who were not likely to get into heart failure concerns, CHIGAGO “opens the window a little wider for when we can use these agents.” The results were published online simultaneously with the presentation (JAMA 2006;296:2572–81).
CHICAGO — Treatment with pioglitazone for 18 months halted progression of atherosclerosis in patients with early type 2 diabetes, Dr. Theodore Mazzone reported at the annual scientific sessions of the American Heart Association.
Carotid intima media thickness (CIMT), which continued to progress in patients treated with glimepiride, was “virtually arrested” in the pioglitazone group in the Carotid Intima-Media Thickness in Atherosclerosis Using Pioglitazone (CHICAGO) trial. The beneficial effect improved during the mean 18 months of treatment, said Dr. Mazzone of the endocrinology, diabetes, and metabolism section of the University of Illinois, Chicago.
CIMT was used as a surrogate for risk of stroke and MI in the diabetic patients. “The thicker the intima, the higher the risk of heart attack or stroke in 5–10 years,” Dr. Mazzone said in a press briefing. The CHICAGO trial was conducted from October 2003 to May 2006 in a multiracial, multiethnic population of patients at 28 clinical sites in Chicago. The 462 patients, aged 45–85 years, were newly diagnosed with type 2 diabetes that was controlled by diet or treated with sulfonureas, metformin, or insulin. Patients taking medicine for blood glucose control were eligible if their glycosylated hemoglobin A1c (HbA1c) values were at least 6.5% but less than 9%.
Exclusion criteria included symptomatic coronary artery disease, cerebrovascular disease, New York Heart Association class III or IV heart failure, and current use of ACE inhibitors or diuretics. “We wanted patients early in the disease process,” Dr. Mazzone said.
CIMT was measured using high-resolution, B mode carotid artery ultrasound. All images were taken by the same ultrasonographer at the same location.
The primary end point was the change in mean CIMT from baseline at 72 weeks. The CIMT reduction in the pioglitazone group was 0.001 mm, compared with an increase of 0.012 mm in the glimepiride group. This beneficial effect was present regardless of age, sex, presence of hypertension, duration of type 2 diabetes, body mass index, HbA1c value, and statin use, said Dr. Mazzone, who is a consultant for and has received speaking honoraria from Takeda Pharmaceuticals North America Inc., maker of pioglitazone (Actos).
Diabetes was well controlled in the study population. The mean HbA1c value of the pioglitazone group at baseline was 7.44%, and that of the glimepiride group was 7.36%. The glycemic effects of the two drugs differed over time in the study. With glimepiride, mean HbA1c values dropped rapidly in the beginning of the trial, but rose gradually back to nearly their original level by week 72. In pioglitazone-treated patients, HbA1c values decreased gradually over 48 weeks and remained steady until 72 weeks. At the final visit, the mean HbA1c level in the pioglitazone group was 0.32% lower than that of the glimepiride group, a highly significant difference, Dr. Mazzone said.
Lipid levels were also well controlled in the CHICAGO participants, with about 70% of the patients in each group taking lipid-lowering drugs. With pioglitazone, HDL cholesterol and triglyceride levels improved significantly. HDL levels were similar between groups at baseline, at 47.6 mg/dL in the glimepiride group and 47.1 mg/dL in the pioglitazone group. By the final visit, the HDL level was 6.5% higher in the pioglitazone group than in the glimepiride group. Triglyceride levels decreased by 13.5% in the pioglitazone patients and rose by 2.1% with glimepiride.
The beneficial metabolic effects of pioglitazone would be expected on the basis of previous trials of thiazolidinediones, said discussant Dr. Peter Wilson, an endocrinologist at Emory University, Atlanta. But the effects of pioglitazone in CHICAGO may not be generalizable to other thiazolidinediones, he noted, because pioglitazone may be stronger than other drugs in the class.
Adverse effects of treatment with pioglitazone were similar to those with the sulfonylurea glimepiride, although treatment-limiting peripheral edema occurred in four pioglitazone patients and none of the glimepiride patients. Weight gain also was more frequent with pioglitazone. These effects have been seen in other randomized trials of thiazolidinediones, and raise concerns about an increased risk of heart failure with pioglitazone. But Dr. Wilson noted that because of its preselection of patients who were not likely to get into heart failure concerns, CHIGAGO “opens the window a little wider for when we can use these agents.” The results were published online simultaneously with the presentation (JAMA 2006;296:2572–81).